Course
2022 Kentucky Renewal Bundle
Course Highlights
- In this course we will learn about LGBTQ+ Cultural Competence, and why it is important to protect all patient rights.
- You’ll also learn the basics of Pediatric Abusive Head Trauma, Implicit Bias, and Suicide Prevention, as required by the Kentucky Board of Nursing.
- You’ll leave this course with a broader understanding of nursing ethics, communication, and more.
About
Contact Hours Awarded: 14
Course By:
Multiple Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
This 2022 Kentucky License Renewal Bundle meets all renewal requirements for Kentucky LPNs and RNs. Upon completion of this course, you will receive a certificate of completion for 14 contact hours.
This course includes multiple interesting topics in one easy course.
Course Outline:
- Pediatric Abusive Head Trauma – Kentucky
- Kentucky Implicit Bias
- Kentucky Suicide Prevention
- Opioid Abuse
- LGBTQ Cultural Competence
- Effective Communication in Nursing
- Nursing Ethics
- A Nurse’s Guide: How to Deal with Difficult Patients
- How to Reduce New Nurse Turnover
Pediatric Abusive Head Trauma – Kentucky
Introduction
Pediatric Abusive Head Trauma (AHT), also known as Shaken Baby Syndrome, includes an array of symptoms and complications resulting from injury to a child or infant’s head and brain after violent or intentional shaking or impact. There are approximately 1,300 reported cases of AHT each year and it is the leading cause of child abuse deaths nationally. For those children who survive, most suffer lifelong complications and disabilities (7).
This serious and tragic injury may be a challenge to diagnose because obvious signs of injury may not be easily detectable right away, and those responsible for the injuries may avoid taking the child for treatment (4). Therefore, it is incredibly important for healthcare professionals who work in pediatrics or emergency medicine to be able to identify at-risk individuals and recognize signs and symptoms of potential victims of AHT. It is also 100% preventable, and proper training on how to mitigate the risks and situations that lead to AHT can help healthcare professionals reduce the incidence of this horrific injury.
Epidemiology/Risk Factors
Though pediatric abusive head trauma most often occurs in children under age 5, the majority of these injuries are in children under the age of 1 year. There is a slight difference in incidence between genders, with 57.9% of victims being male and 41.9% being female. There is a peak occurrence of AHT between 3 and 8 months (4). Babies of this age are particularly vulnerable for a multitude of reasons, including large head size, weak neck muscles, fragile and developing brains, and the discrepancy in strength between infant and abuser. Sleep deprivation paired with longer and louder crying spells of very young infants sets the stage for high levels of caregiver frustration, which often precedes AHT injuries. The perpetrator is almost always a parent or caregiver (7).
Besides infant age, there are many social factors that increase the risk of AHT, including a lack of childcare experience, young or poorly supported parents, single-parent homes, low socioeconomic status, low education level, and a history of violence. These factors paired with a lack of prenatal care or parenting classes often leads to poorly prepared parents who have not been taught to anticipate crying spells or how to deal with the frustration in a safe manner (7).
Unfortunately, Kentucky has one of the highest rates of child abuse in the country. In 2019, there were more than 130,000 reports of suspected abuse or neglect, and 15,000 of those had substantial evidence to support abuse had occurred. Of those, nearly 76 were nearly fatal or fatal, and 32 of those were due to pediatric abusive head trauma(1).
Case Study
A Nursery nurse on a Labor, Delivery, and Postpartum unit is providing discharge information to the parents of a 2 day old baby girl, Violet, who is going home today. This is the first child for both parents. They are 19 years old, living in an apartment together while the mother works part time as a waitress and the father works full time for a lawn mowing company. The child’s maternal grandmother lives nearby and will be helping the mother care for the baby the first few weeks and then watching the baby a few days per week when the mother returns to work.

Self Quiz
Ask yourself...
- Which factors put this child at an increased risk of being abused?
- Which factors are protective against abuse?
- What resources might the nurse connect these parents with in order to maximize their support network once they are discharged?
Pathophysiology
While anyone can sustain a head injury, the relatively large size of young children’s heads paired with their weak and underdeveloped neck muscles is what makes them particularly susceptible to AHT. When a child’s head moves around forcefully, the brain moves around within the skull, which can tear blood vessels and nerves, causing permanent damage. Bruising and bleeding may occur when the brain collides with the inside of the skull or fractured pieces of skull. Finally, swelling of the brain may occur, which builds up pressure inside the skull and makes it difficult for the body to properly circulate oxygen to the brain (6).
It should be noted that bouncing or tossing a child in play, sudden stops or bumps in the car, and falls from furniture (or less than 4 feet) do not involve the force required to mimic the injuries of AHT (7).
Also important to understand is that AHT is a broad term used to describe the injury, but there are a collection of various mechanisms of injury within AHT. Among these different causes are Shaken Baby Syndrome (SBS), blunt impact, suffocation, intentional dropping or throwing, and strangulation. It is recommended to classify all of these injuries as AHT so as to avoid any confusion or challenges in court if multiple mechanisms of injury were involved (4).

Self Quiz
Ask yourself...
- Consider why it is important to know that falls from less than 4 feet do not typically cause much injury to babies and young children. What would you think if an infant presents with a serious brain injury and the parents state he fell off the couch?
- What sort of problems could occur in the litigation process if a child is diagnosed with Shaken Baby Syndrome but it is then revealed the child was thrown to the ground?
- Young children fall all the time while running, riding bikes, and climbing on playground equipment. What makes this less dangerous than an infant being shaken or thrown?
Diagnosis of Pediatric Abusive Head Trauma
Parents or caregivers who have inflicted injury onto a child may delay seeking treatment for fear of consequences. It is important to gather a thorough history and be on the lookout for inconsistent stories, changing details, or mechanism of injury that does not match the severity of symptoms (7).
Symptoms that typically lead caregivers to seek treatment for their child include:
- Decrease in responsiveness or change in level of consciousness
- Poor feeding
- Vomiting
- Seizures
- Apnea
- Irritability
Upon exam, these children may exhibit:
- Bradycardia
- Bulging fontanel
- Irritability or lethargy
- Apnea
- Bruising
A lack of any external injuries or obvious illnesses when presenting with these symptoms should alert the healthcare professional to the possibility of AHT, particularly in young children or infants. Additionally, unexplained fractures, particularly of the skull or long bones, bruising around the head or neck, or any bruising in a child less than 4 months are red flags (4).
An ophthalmology consult to assess for retinal hemorrhage should be obtained. The force used with AHT can cause a shearing effect with the retina and is visible with a simple fundal exam of the eye. This type of injury does not typically occur with accidental or blunt head trauma and is typically considered highly indicative of abuse. That same shearing force often causes bleeding within the brain, and subdural hematomas are often revealed on CT or MRI (4).
Any of the above criteria, or other suspicious story or injuries, should be reported for further investigation. Mild injuries are harder to detect but only occur around 15% of the time. Severe injury from AHT accounts for 70% of cases (4).
Case Study cont.
Baby Violet is now 5 weeks old and is brought to the ED by her parents. Her mother reports that she has been eating poorly and acting strange since this morning. Her father reports he thinks she has been sleeping excessively for 2 days now. On exam, the baby is found to have a bulging fontanel, slow heart rate, and a bruise on the side of her head. Her mother states she sustained that bruise when she rolled off of her changing table yesterday.

Self Quiz
Ask yourself...
- What additional exam information would be necessary/helpful at this time? Specialty consult? Imaging?
- What assessment finding or diagnostic data might alleviate some suspicion that this is an abuse case? What would contribute to the suspicion?
Outcomes and Sequelae
For children diagnosed with even mild to moderate AHT, the prognosis is fairly grim. Up to 25% of children with AHT end up dying from their injuries, and for those who survive, 80% will have lifelong disabilities of varying severity (7).
The most common complications and disabilities include: blindness, hearing loss, developmental delays, seizures, muscle weakness or spasticity, hydrocephalus, learning disabilities, and speech problems. Lifelong skilled care and therapies are often needed for these children, accruing over $70 million in healthcare costs in the United States annually (4).

Self Quiz
Ask yourself...
- What characteristics of AHT would lead to long term disabilities like blindness, muscle spasticity, and speech problems?
- How do you think the cost of social programs and parental support programs within a community might compare to the costs of abuse investigation and healthcare costs for abused children?
Legal Considerations in the State of Kentucky
In the state of Kentucky, anyone with a reasonable suspicion that abuse or neglect is occurring is mandated by law to report the incident, and there are legal consequences (from misdemeanor all the way to felony) for willfully failing to make a report. For healthcare professionals, this is particularly important to note, as you will come in contact with many different types of families, injuries, and stories, and must remain vigilant in assessing for abuse (5).
A report of suspected abuse should be made at the first available opportunity and can be made by contacting the child abuse hotline (1-877-KYSAFE1), local law enforcement, Kentucky State Police, or the Cabinet for Health and Family Services. The child’s name, approximate age and address, as well as the nature and description of injuries, and the name and relationship of the alleged abuser should all be included in the report (9).
Once a report has been made, the Department for Community Based Services will determine if an investigation is warranted. If the home is deemed to be unsafe or there is a threat of immediate danger to a child, the child will be removed from the home, but in all other cases, every effort will be made to maintain the family (5).
Case Study cont.
It is later determined that Baby Violet was violently shaken by her mother during a crying spell one evening. During legal proceedings for the incident, it is revealed that the grandmother witnessed this abuse.

Self Quiz
Ask yourself...
- Did the grandmother break any laws in this scenario?
- Is it likely that the child would stay in the home in this scenario, or do you think her safety is at a continued risk and removal would be necessary?
Prevention
While accurate detection of AHT is incredibly important, another key consideration for this injury and its poor outcomes, is that these incidents are 100% preventable. Much of the time, AHT is preceded by extreme frustration by a parent or caregiver when an infant is crying for long periods or is inconsolable. Proper education and preparedness about when and why this occurs, and what to do when it does, can help prevent AHT from occurring. For healthcare professionals who regularly care for infants, children, and expecting or new parents, there is a huge potential for positive impact (2).
Identifying those most at risk is a great starting place and new parenting courses, educational discussion and pamphlets, as well as regular check-ins are extremely beneficial for at-risk families. Young or inexperienced families, families without a lot of external support, or those with low socioeconomic status or poor education should be looked at first.
Once the most at risk families have been identified, provide them with information and services that may help reduce risks. These interventions are useful for anyone with an infant or small child, but special attention and close follow up should be given to those with more risk factors (8).
- Educate about infant crying: The PURPLE Crying program is particularly useful for this and includes facts and common symptoms of excessive or colicky infant crying. PURPLE stands for:
- Peak of Crying, with crying increasing weekly after birth and peaking around 8 weeks
- Unexpected, where crying may come and go with no apparent cause
- Resists soothing, where your baby won’t settle no matter what you try
- Pain like face, where your baby looks like they are in pain even if nothing is wrong
- Long-lasting, with crying lasting as long as 5 hours
- Evening, with excessive crying being more common in the evening or at night (8)
- Enhance parenting skills: Let parents know it is okay to feel frustrated. Take a deep breath, count to 10, place your infant in a safe place and walk away for a few minutes to collect yourself. Many parents don’t know that this is okay to do (3).
- Strengthen socioeconomic support: Make sure families are aware of and utilizing access to supportive services like WIC to help ease financial strain.
- Emphasize social support and positive parenting: Ask about nearby help in the form of relatives or friends. Encourage them to reach out for emotional support, or even a break from caring for the infant. Connect families with community resources like motherhood support groups or playdates. Schedule for early childhood home visits (2).

Self Quiz
Ask yourself...
- Think about the populations you work with. How can you check in to make sure families have adequate support and decrease their risk of child abuse?
- What areas are the easiest to address at your current job? The most difficult?
Conclusion
Though the goal is for there to be no scenarios where children suffer head trauma at the hands of an abuser, there is a long way to go before that objective can be reached. In the meantime, healthcare professionals must be vigilant in maintaining a high level of suspicion for pediatric abusive head trauma whenever they are caring for children. Understanding contributing risk factors, as well as signs and symptoms, and how to properly assess for and diagnose pediatric abusive head trauma will lead to more accurate detection, appropriate treatment, and hopefully better outcomes. On the other end of things, those in a position to influence parenting education and community health standards should consider the ways in which caregiver frustration might be better handled to prevent the abuse from even occurring. There is much work to be done when it comes to AHT, but well informed medical professionals is an essential step in the right direction.
Kentucky Implicit Bias
Health Equity is a rising area of focus in the healthcare field as renewed attention is being given to ongoing data regarding discrepancies and gaps in the accessibility, expanse, and quality of healthcare delivered across racial, gender, cultural, and other groups. Yes, there are some differences in healthcare outcomes purely based on biological differences between people of different genders or races, but more and more evidence points to the vast majority of healthcare gaps stemming from individual and systemic biases.
Policy change and restructuring is happening at an institutional level across the country, but this will only get us so far. In order for real change to occur and the gaps in healthcare to be closed, there must also be awareness and change on an individual level. Implicit, or subconscious, bias has the potential to change the way healthcare professionals deliver care in subtle but meaningful ways and must be addressed to modernize healthcare and reach true equity.
This Kentucky Implicit Bias training meets the “Implicit Bias” requirement needed for Kentucky nursing license renewal.
What is Implicit Bias?
So what is implicit bias and how is it affecting the way healthcare is delivered? Simply put, implicit bias is a subconscious attitude or opinion about a person or group of people that has the potential to influence the actions and decisions taken when providing care. This differs from explicit bias which is a conscious and controllable attitude (using racial slurs, making sexist comments, etc). Implicit bias is something that everyone has and may be largely unaware of how it is influencing their understanding of and actions towards others. The way we are raised, our unique life experiences, and an individual’s efforts to understand their own biases all affect the opinions and attitudes we have towards other people or groups (7). This Kentucky Implicit Bias training course will increase your awareness of implicit bias in your nursing practice.
This can be both a positive or a negative thing. For example if a patient’s loved ones tells you they are a nurse, you may immediately feel more connected to them and go above and beyond the expected care as a “professional courtesy.” This doesn’t mean you dislike your other patients and their loved ones, just that you feel more at ease with a fellow healthcare professional which shapes your thoughts and behaviors in a positive manner.
More often though, implicit biases have a negative connotation and can lead to care that is not as empathetic, holistic, or high quality as it should be. Common examples of implicit bias in healthcare include:
- Thinking elderly patients have lower cognitive or physical abilities
- Thinking women exaggerate their pain or have too many complaints
- Assuming patients who state they are sexually active are heterosexual
- Thinking Black patients delay seeking preventative or acute care because they are passive about their health
- Assuming a chatty college student is asking for ADHD evaluation because she is lazy and wants medication to make things easier
On a larger, more institutional and societal level, the effects of bias create barriers such as:
- Underrepresentation of minority races as providers: in 2018 56.2% of physicians were white, while only 5% were Black and 5.8% Hispanic (2)
- Crowded living conditions and food deserts for minority patients due to outdated zoning laws created during times of segregation (17).
- Difficulty obtaining health insurance for minority or even LGBTQ clients, decreasing access to healthcare (3).
- Lack of support and acceptance for LGBTQ people in the home, workplace, or school as well as lack of community resources leads to negative social and mental health outcomes.
- Due to variations in the way disabilities are assessed, the reported prevalence of disabilities ranges from 12% to 30% of the population (15).

Self Quiz
Ask yourself...
Before introducing the implications and long-term outcomes of unaddressed implicit biases in healthcare, reflect on your practice and the clients you work with. This will help as we progress through this Kentucky implicit bias training course.
- Think about the facility where you work and the different types of clients you come into contact with each day. Are there certain types of people you assume things about just based on the way they look, their gender, or their skin color?
- In what ways do you think these assumptions might affect the way you care for your clients, even if you keep these opinions internal?
- How do you think you could try and re-frame some of these assumptions?
- Do you think being more aware of your internal opinions will change your actions the next time you work?
- Before the Kentucky Implicit Bias Training course requirement, how often did you consider implict bias?
- Reflecting on your personal nursing practice, why do you think Kentucky has added a requirement on Kentucky Implict Bias training?
Implications
Once you have an understanding of what implicit bias is, you may be wondering what it looks like on a larger scale and what it means in terms of healthcare discrepancies. More and more data stacks up each year with examples that span all types of diversity, from race to gender, age, disabilities, religion, sexual identification and orientation, and even Veteran status. Examples of what subconscious biases in healthcare may look like include:
- Medical training and textbooks are mostly commonly centered around white patients, even though many rashes and conditions may look very different in patients with darker skin or different hair textures. This can lead to missed or delayed diagnoses and treatment for patients of color (9).
- A 2018 survey of LGBTQ youth revealed 80% reporting their provider assumed they were straight or did not ask (12). And in 2014, over half of gay men (56%) surveyed who had been to a doctor said they had never been recommended for HIV screening, despite increased risk for the disease (10).
- A 2010 study found that women were more verbose in their encounters with physicians and may not be able to fit all of their complaints into the designated appointment time, leading to a less accurate understanding of their symptoms by their doctor (4). For centuries, any symptoms or behaviors that women displayed (largely related to mental health) that male doctors could not diagnose fell under the umbrella of “hysteria”, a condition that was not removed from the DSM until 1980 (20).
- When treating elderly patients, providers may dismiss a treatable condition as part of aging, skip preventative screenings due to old age, or overtreat natural parts of aging as though they are a disease. Providers may be less patient, responsive, and empathetic to a patient’s concerns or even talk down to them or not explain things because they believe them to be cognitively impaired (18).
- Minority, particularly Black or Hispanic patients, are often thought to be less concerned or more neglectful of their health, but minority patients are also most often those living in poverty, which goes hand in hand with crowded living conditions and food deserts due to outdated zoning laws created during times of segregation. This means less access to nutritious foods, fresh air, or clean water which has overall negative effects on health (mude). Minority patients are also still disproportionately uninsured, which leads to delayed or no care when necessary (3).
Although these are only a few examples, there are obvious and substantial consequences of these biases; which is why it is vital that we address them in this Kentucky Implicit Bias training course.
This has obvious negative connotations or repercussions at the time of care and can lead to client dissatisfaction or suboptimal treatment and missed preventative care, but over time the effects of implicit bias can add up and lead to even larger consequences. Examples include:
- A 2020 study found that Black individuals over age 56 experience decline in memory, executive function, and global cognition at a rate much faster than their white peers, often as much as 4 years ahead in terms of cognitive decline. Data in this study attribute the difference to the cumulative effects of chronically high blood pressure more likely to be experienced and undertreated for Black Americans (16).
- Lack of health insurance keeps many minority patients from seeking care at all. 25% of Hispanic people are uninsured and 14% of Black people, compared to just 8.5% of white people. This leads to lack of preventative care and screenings, lack of management of chronic conditions, delayed or no treatment for acute conditions, and later diagnosis and poorer outcomes of life threatening conditions (3).
- A 2010 study showed men and women over age 65 were about equally likely to have visits with a primary care provider, but women were less likely to receive preventative care such as flu vaccines (75.4%) and cholesterol screening (87.3%) compared to men (77.3% and 88.8% respectively) (4).
- About 12.9% of school aged boys are diagnosed and treated for ADHD, compared to 5.6% of girls, though the actual rate of girls with the disorder is believed to be much higher (5).
- Teenagers and young adults who are part of the LGBTQ community are 4.5 times more likely to attempt suicide than straight, cis-gender peers (11).

Self Quiz
Ask yourself...
For the purpose of this Kentucky Implicit Bias training, put yourself in a patient’s perspective and reflect on the following:
- Have you ever been a patient and had a healthcare professional assume something about you without asking or getting the whole story? How did that make you feel?
- How do you think it might affect you over time if every healthcare encounter you had went the same way?
Impact of Historic Racism
In addition to discrepancies in insurance status and representation in medical textbooks and among medical professionals, there is a long history of systemic racism that has created generational trauma for minority families, leading to mistrust in the healthcare system and poorer outcomes for those marginalized communities.
Possibly one of the most infamous examples is the Tuskegee Syphilis Study. This 1932 experiment included 600 Black men, about two thirds of which had syphilis, and involved collecting blood and monitoring the progression of symptoms for research purposes in exchange for free medical exams and meals. Informed consent was not collected and participants were given no information about the study other than that they were being “treated for bad blood”, even though no treatment was actually administered. By 1943, syphilis was routinely and effectively treated with penicillin, however the men involved in the study were not offered treatment and their progressively worsening symptoms continued to be monitored and studied until 1972 when it was deemed unethical. Once the study was stopped, participants were given reparations in the form of free medical benefits for the participants and their families. The last participant of the study lived until 2004 (6).
The “father of modern gynecology,” Dr. J. Marion Sims, is another example steeped in a complicated and racially unethical past. Though he did groundbreaking work on curing many gynecological complications of childbirth, most notably vesicovaginal fistulas, he did so by practicing on unconsenting, unanesthetized, Black enslaved women. The majority of his work was done between 1845 and 1849 when slavery was legal and these women were likely unable to refuse treatment, sometimes undergoing 20-30 surgeries while positioned on all fours and not given anything for pain. Historically his work has been criticized because he achieved so much recognition and fame through an uneven power dynamic with women who have largely remained unknown and unrecognized for their contributions to medical advancement (21).
Another example is the story of Henrietta Lacks, a young Black mother who died of cervical cancer in 1951. During the course of her treatment, a sample of cells was collected from her cervix by Dr. Gey, a prominent cancer researcher at the time. Up until this point, cells being utilized in Dr. Gey’s lab died after just a few weeks and new cells needed to be collected from other patients. Henrietta Lacks’ cells were unique and groundbreaking in that they were thriving and multiplying in the lab, growing new cells (nearly double) every 24 hours. These highly prolific cells were nicknamed HeLa Cells and have been used for decades in the development of many medical breakthroughs, including studies involving viruses, toxins, hormones, and other treatments on cancer cells and even playing a prominent role in vaccine development. All of this may sound wonderful, but it is important to understand that Henrietta Lacks never gave permission for these cells to be collected or studied and her family did not even know they existed or were the foundation for so much medical research until 20 years after her death. There have since been lawsuits to give family members control over what the cells are used for, as well as requiring recognition of Henrietta in published studies and financial payments from companies who profited off of the use of her cells (13).
When considering all of the above scenarios, the common theme is a lack of informed consent for Black patients and the lack of recognition for their invaluable role in society’s advancement to modern medicine. It only makes sense that these stories, and the many others that exist, have left many Black patients mistrustful of modern medicine, medical professionals, or treatments offered to them, particularly if the provider caring for them doesn’t look like them or seems dismissive or unknowledgeable about their unique concerns. Awareness that these types of events occurred and left a lasting impact on many generations of Black families is incredibly important in order for medical professionals to provide empathetic and racially sensitive care.

Self Quiz
Ask yourself...
Consider the above-mentioned historic events and reflect on the following:
- Have you ever had a negative experience at a healthcare facility? How has that experience impacted your view of that facility or your opinion when others talk about that facility?
- How would you feel if you learned that a sample of your cells or a bodily fluid was taken without your consent and had been used for medical experimentation? What about if companies had made huge profits from something taken from your body?
- Even without monetary compensation, why do you think recognition for a person’s role in healthcare advancement through the use of their own body is important?
Exploring Areas of Bias
Culture
Cultural competence is a common buzzword used in healthcare training programs and information about various religions, ethnicities, beliefs, or practices is often integrated into medical training. Students and staff members are often reminded that the highest quality of care anticipates the unique cultural needs a client may have and aims to provide care that is holistic and respectful of cultural differences. An awareness of the potential variances in care, such as dietary needs, desire for prayer or clergy members, rituals around birth or death, beliefs surrounding and even refusal for certain types of treatments, are all certainly very important for the culturally sensitive healthcare professional to have (and the distinctions far too many for the scope of this course); however, there is also a fine line between being aware of cultural similarities and stereotyping. Since this course is a required Kentucky Implicit Bias training, it is essential that this topic is covered.
Clinicians should make sure to understand that people hold different identities, beliefs, and practices across racial, ethnic, and religious groups. Remember that just because someone looks a certain way or identifies with a certain group does not mean all people within that group are the same. Holding assumptions about clients of a particular race or religion, without getting to know the individual needs of your client, is a form of implicit bias and may cause your client to become uncomfortable or offended.
Simply asking clients if they have any cultural, dietary, or spiritual needs throughout the course of their care is often the best way to learn their needs without making assumptions or stereotyping. Overall, it should be thought of as extending care beyond cultural competence and working on partnership and advocacy for your client’s unique needs.

Self Quiz
Ask yourself...
- Have you ever cared for a client that you made an assumption about based on appearances and it turned out not to be true?
- Did your behavior or attitude towards that client change at all once you gained new information about them?
- Think about ways you could incorporate cultural questions into your plan of care and how it could improve your understanding of client needs.
Maternal Health
One of the most strikingly obvious places that implicit bias has tainted the healthcare industry is in maternal health. Repeatedly, statistics show that Black women experience twice the infant mortality rate and nearly four times the maternal mortality rate of non-Hispanic white women during childbirth.
Let those numbers sink in and realize that this is a crisis. Pregnancy and childbirth are natural processes, but do come with inherent risks for mother and baby; but in a modern society, women should feel comfortable and confident in their care, not scared they won’t be treated properly or even survive. Home births among Black women are on the rise as they seek to avoid the biases of the hospital setting and maintain control over their own experiences (19).
The reasons for this disparity and Black women fearing for their lives when birthing in hospitals are many, often centering on a lack of health insurance leading to poorer general health even before pregnancy, a lack of prenatal care, and a lack of care in the weeks following pregnancy. However, the discrepancies still exist at an alarmingly high rate even when looking at minority women with advanced education and high income, indicating that a more insidious culprit, implicit bias, is hugely responsible (19). In order for true change to come, this topic must be addressed in this Kentucky Implicit Bias training. A few notes that indicate the prevalence of implicit bias in healthcare throughout history are listed below:
- False beliefs about biological differences between white and black women date back to slavery, including the belief that Black women have fewer nerve endings, thicker skin, and thicker bones and therefore do not feel pain as intensely.
- These beliefs are obviously untrue, but subconscious bias towards those beliefs still exists as Black and Hispanic women statistically have their perceived pain rated lower by health care professionals and are offered appropriate pain management interventions less often than white peers.
- Complaints from minority patients that may indicate red flags for conditions such as preeclampsia or hypertension are often downplayed or ignored by healthcare professionals.
- Studies show healthcare professionals may believe minority patients are less capable of adhering to or understanding treatment plans and may explain their care in a condescending tone of voice not used with other patients.
- One in five Black and Hispanic women report poor treatment during pregnancy and childbirth by healthcare staff.
- These patients are less likely to feel respected or like a partner in their care and may be non compliant in treatment recommendations due to feeling this way, however this just perpetuates the attitudes held by the healthcare providers (19) .

Self Quiz
Ask yourself...
- Think about how a provider’s perception of a maternity client’s pain could snowball throughout the labor and delivery process. How do you think it might affect the rate of c-sections or other birth interventions if clients have not had their pain properly managed throughout labor?
- Pregnancy is a very vulnerable time. Think about how you would feel if you were experiencing a pregnancy and had fears or concerns and your provider did not seem to validate or respect you. Would you feel comfortable going into birth? How might added fears or stress impact the experience?
Reproductive Rights
Branching off of maternal health, is reproductive justice. Biases surrounding the reproductive decisions of women may negatively impact the care they receive when seeking care for contraception or during pregnancy. While some of these inequities may be more profound for women of color, women of all races can be and are affected by biases surrounding reproduction, which is why it is being covered in this Kentucky Implicit Bias training course. Examples of ways implicit bias may affect care include:
- Some healthcare professionals may believe there is a “right” time or way to become pregnant and feel pregnancy outside of those qualifiers is undesirable; this can stem from personal or religious beliefs. While healthcare staff are certainly entitled to hold these beliefs in their personal lives, if the resulting implicit biases are left unchecked, they can lead to attitudes and actions that are less compassionate when caring for their clients. Clients may feel shamed or judged during their experiences instead of having their needs addressed (8). Variables that may be perceived as unacceptable or less desirable include:
- Age during pregnancy. Clinicians may feel differently about pregnant clients who are very young (teenagers) or even those who are in their 40s or 50s (8).
- Marital status during pregnancy. Healthcare professionals may have beliefs that clients should be married when having children and may have bias against unmarried or single clients (8).
- Number or spacing of pregnancies. Professionals may hold beliefs about how many pregnancies are acceptable or how far apart they should be and may hold judgment against clients with a large number of children or pregnancies occurring soon after childbirth.
– Low income and minority women are more likely to report being counseled to limit the number of children they have, as opposed to their white peers (14).
- Method of conception. Some healthcare professionals may have personal beliefs about how children should be conceived and may have negative opinions about pregnancies resulting from fertility treatments such as IVF or surrogacy (8).
- Personal or religious beliefs about contraception may also cause healthcare professionals to provide less than optimal care to clients seeking methods of birth control.
- Providers may believe young or unmarried clients should not be given access to contraception because they do not believe they should be engaging in sexual activity (8).
- Providers, or even some institutions such as Catholic hospitals, may withhold contraception from clients as they believe it to be immoral to prevent pregnancy.
- Providers may push certain types or usage of contraception onto clients that they feel should limit the number of children they have, even if this does not align with the desires of the client. This includes the use of permanent contraception such as tubal ligation (14).
- Providers may provide biased information about types of contraception available, minimizing side effects or pushing for easier, more effective types of contraception (such as IUDs), despite a client’s questions, concerns, or contraindications (14).
– One study showed Black and Hispanic women felt pressured to accept a certain type of contraception based on effectiveness alone, with little concern to their individual needs or reproductive goals (14).
- Personal or religious beliefs about pregnancy termination may impact the care provided and counsel given to pregnant clients who may wish to consider termination. Providers who disagree with abortion on a personal level may find it difficult to provide clear and unbiased information about all options available to pregnant women or may have a judgemental or uncompassionate attitude when caring for clients who desire or have had an abortion (8).
Case Study
Alexandria is a 22 year old Hispanic woman who has always wanted a big family with 3-5 children. She met her current boyfriend in college when she was 19 and became pregnant shortly afterwards. It was an uneventful pregnancy, and Alexandria had a vaginal delivery to a healthy baby girl at 39 weeks. When that child turned 2, Alexandria and her partner decided they would like to have another baby. At 38 weeks gestation, Alexandria was at a prenatal appointment when her provider brought up her plans for contraception after the birth. The provider suggested an IUD and stated it could be placed immediately after birth, could be left in for 5 years, and would be 99% effective at preventing pregnancy. Alexandria stated she had an IUD when she was 17 and did not like some of the side effects, mostly abdominal cramping, and that she also might like to have another baby before the 5 year mark. Her doctor stated “All birth control has side effects, and this one is the most effective. You are so young, do you really want 3 children by age 25 anyway?”

Self Quiz
Ask yourself...
- What implicit biases does this healthcare professional hold about reproductive rights?
- How do you think those opinions are likely to affect Alexandria? Do you think she will change her mind or her future plans? Or do you think she will be more likely to disregard this provider’s advice and opinions moving forward?
- What are some potential negative consequences for Alexandria’s pregnancy prevention plans after this exchange with her doctor?
- Prior taking this Kentucky Implicit Bias course, were you aware of any implict biases regarding reproductive health?
How to Measure and Reduce Implicit Biases in Healthcare
Assessing for Bias
In order for change to occur, there is a broad spectrum of transitions in individual thought and policy that must occur. Evaluating for the presence, and the extent, of implicit bias is one of the first steps. This Kentucky Implicit Bias training will cover both individual and institutional level focuses.
On the individual level, possible action include:
- Identifying and exploring one’s own implicit biases. Everyone has them and we all need to reflect upon them. This goes beyond basic cultural competence and includes a deeper understanding of how your own experiences or environment may differ from someone else and may have caused you to feel or believe a certain way.
- Attending training or workshops provided by your job and completing exercises in self reflection will help you better understand where your biases are and the extent to which they may be impacting your behavior or actions at work and in your personal life.
- Reflecting on how one’s biases affect actions. Once you have recognized the internal opinions you hold, you can examine ways that those opinions may have been affecting your actions, behaviors, or attitudes towards others. Reflect on your care of patients at the end of each shift. Consider if you made assumptions about certain clients early on in their care. Think about ways those assumptions may have affected your interactions with the client. Think about if you cared for your clients in a way that you would want your own loved ones cared for.
- If you have the time, volunteer at events or in places that will expose you to people who are different from you. Use the opportunity to learn more about others, their lived experiences, and identify how often your implicit biases may be affecting your view of others before you even get to know them.
On an institutional level, the measurement of biases can be more streamlined and may utilize tools like surveys.
- Monitoring patient data and assessing for any broad gaps in diagnoses, preventative care and treatment rates, as well as health outcomes across racial, ethnic, gender, and other spectrums. Recognizing gaps or problem areas and assigning task forces to evaluate further and address the underlying issues.
- Regularly poll clients and employees of healthcare facilities to determine who might be experiencing effects of bias and when.
- Require employee participation in implicit bias presentations or courses, allowing employees to self identify areas where they may be biased.

Self Quiz
Ask yourself...
- In what ways will your approach be different the next time you care for a client unlike yourself?
- Can you think of a policy or practice that your facility could change in order to provide more equitable care to the clients you serve?
- Do you have a better understanding of implicit bias in healthcare after taking this Kentucky Implicit Bias course?
Acting to Reduce Bias
Once the presence and extent of bias has been identified, individuals can make small, consistent changes to recognize and address those biases in order to become more self aware and intentional in their actions. Some possible ways to address and reduce implicit bias on an individual level include:
- Educating oneself and reframing biases. In order to change patterns of thinking and subsequent behaviors that may negatively impact others, you can work on broadening your views on various topics. This can be done through reading about the experiences of others, watching informational videos or documentaries, attending speaking engagements, and just listening to the experiences of others and gaining an understanding of how their lives might be different than yours.
- Understanding and celebrating differences. Once you can learn to see others for their differences and consider how you can adapt your care to help them achieve the best outcomes for their wellbeing, you are able to provide truly equitable care to your clients. This includes understanding differences in experiences, perceptions, cultures, languages, and realities for people different from yourself, recognizing when disparities are occurring, and advocating for change and equity.
When enough people have recognized and addressed their own implicit biases, advocacy can extend beyond individual care of clients and reach the institutional level where change is more easily seen (though no more important than the small individual changes). One of the most effective ways to make institutional level changes is through representation of minority groups in positions of power and decision making. Simply keeping structures as they are and dictating change without any evolution from leadership is not likely to be effective in the long term. Including minority professionals in positions of leadership or on decision making panels has the most potential to make true and meaningful change for hospitals and healthcare facilities.
Examples of institutional level changes include:
- Medical schools will need to take a broader, more inclusive approach when admitting future doctors, incentivise minority students to choose careers in healthcare, and invest in their retention and success (9).
- Properly training and integrating professionals like midwives and doulas into routine antenatal care and investing in practices like group visits and home births will give power back to minority women while still giving them safe choices during pregnancy (1).
- Universal health insurance, basic housing regulations, access to grocery stores, and many other socio-political changes can also work towards closing the gaps in accessibility to quality healthcare and may vary by geographic location (3).
- Community programs should be available to create safe spaces for connection and acceptance for LGBTQ people. Laws and school policy need to focus on how to prevent and react to bullying and violence against LGBTQ individuals (12).
- Cultural competence training in medical professions needs to include LGBTQ issues and data collection regarding this population needs to increase and be recognized as a medical necessity (12).
- Medical professionals must be trained in the history of inequality among women, particularly in regards to mental health, and proper, modern diagnostics must be used. The differences in communication styles of men and women should be taught as well (20).
- Medical facilities should emphasize respect of a client’s views on controversial topics such as pregnancy/birth, death, and acceptance or declining of treatments even if it conflicts with a staff members’ own beliefs (14).
- Healthcare facilities can adopt practices that are standardized regardless of age and include anti-ageism and geriatric focused training, including training about elder abuse (18).
Obviously each geographic area will have differing demographics depending on the populations they serve. What works at one facility may not work at another. Hearing from the community is beneficial for keeping things individualized and allows facilities to gain perspective from the local groups they serve.
- Town Hall style meetings, keeping hospital board members and employees local rather than outsourcing from travel companies (when possible), and encouraging community involvement from staff members are all great ways to keep a community centered facility and keep the lines of communication open for clients who may be having a different experience than their neighbor.
There are many things that will need to be done in order for equitable, bias-free healthcare to become a norm nationwide. However, taking the time to learn from this Kentucky Implicit Bias training, apply it to current practices, and continue to learn about others and their respective beliefs and cultures is just the beginning.
Kentucky Suicide Prevention
Suicide risks among nurses is a public health concern. The first and most profound way to address the troubling rates of suicide among nurses is to employ suicide prevention. For that matter, mandatory training, resources, and the establishment of policies and procedures are crucial within the operation of organizations. All healthcare providers are responsible for identifying and addressing situations which warrant intervention.
This Kentucky Suicide Prevention course meets the “Suicide Prevention” requirement needed for Kentucky nursing license renewal.
Introduction
According to the Centers for Disease Control and Prevention, suicide is a leading cause of death in the United States, which is subsequently a public health concern (6). As underscored by the CDC (6), “In 2018, suicide took more than 48,000 lives and was the 10th leading cause of death in the United States”. Yet, it has been noted that suicidal ideations and attempts occur more often than suicidal deaths (17). However, suicide is preventable and from a collaborative approach, preventive strategies can help reduce an individual’s risk for a detrimental outcome (6). Some of the warning signs of suicide include, but are not limited to, the following: feeling hopeless or helpless; feeling like a burden to others or unable to find a reason for living; unbearable pain; expressing thoughts of suicide; exhibiting signs of depression or loss of interest in normal activities; aggression, impulsivity, or humiliation; or displaying a sudden sense of peace (4). From a public health standpoint, all ages are affected by suicide (6). Nevertheless, there are higher suicide rates in some groups (e.g., non-Hispanic American/Alaska Native; non-Hispanic White populations; veterans; persons residing in rural areas; individuals who identify as lesbian, gay, or bisexual; and individuals holding certain occupations often considered high stress such as healthcare providers) in comparison to others (6). As stated, individuals requiring intervention are often those with high stressors and/or have a history of other acts of violence (6). One of the most demanding professions is nursing, and nurses are deemed at a higher risk for suicide than the general population. Taking that into account, suicide awareness and prevention programs are fundamental. This Kentucky Suicide Prevention course will increase your awareness among nurses at risk for suicide and provide tools for screening and preventative measures.
The Significance of Suicide Prevention
As emphasized, suicide is a public health concern due to the nature of its adverse impact on not only the individual, but their loved ones and communities correspondingly (6). Factors such as socioeconomical issues, interpersonal problems, mental or physical health problems, substance abuse, previous suicidal attempts, occupational demands/workplace stressors, and being able to access deadly means may contribute to individuals being at a higher risk for suicide (6). Anxiety, stress disorders, and depression are all increased by the demands of the responsibilities related to the nursing profession, and sadly, those factors are interrelated to higher suicide rates among nurses (7). In saying that, nurses who work on the frontlines are heavily burdened, which is why it is so critical that support is rendered with the goal of yielding a reduction in the risks of suicide. There are many strategies that can be implemented to protect individuals from suicidal thoughts and behavior. Some of those protective factors include the following: coping and problem-solving skills; cultural and religious believes that dissuade suicide; support from friends, family, and communities; supportive affiliations with care providers; access to physical and mental health care; and restricted access to fatal means among persons at risk for suicide (6).

Self Quiz
Ask yourself...
Refelct on your prior knowledge of what you knew about suicide prior to taking this Kentucky Suicide Prevention course.
- What are contributing factors that may increase an individual’s risk for suicide?
- What are protective factors to consider regarding suicide prevention?
- Why do you think Kentucky has added a CE requirement on Kentucky Suicide Prevention ?
Suicide Risk Factors Amongst the Nursing Population
With suicide prevention being a public health concern, it is important to identify groups of persons considered at substantial risk for suicide. Nurses are often faced with high demands of responsibilities as well as easy access to fatal means. Primarily, workplace stressors and lack of personal care can lead to burnout which consequently can lead to an increased risk for suicide incidences in the nursing population. Burnout has been noted as one of the most common reasons nurses contemplate suicide, and circumstances such as short-staffing and the most recent pandemic (COVID-19) have brought about a wave of burnout among nurses who work on the front line (11). Nurses are often responsible for the care of all others (professionally and personally) while unintentionally neglecting their own needs; therefore, providing support for nurses is imperative. For example, there have been fifty-eight suicides amongst the nursing population in the state of Kentucky since 2016; however, nurses in the state of Kentucky are required to obtain recurring suicide prevention education and training (15). Hence why the Kentucky Board of Nursing has added a continuing education requirement to address suicide prevention in nursing. Furthermore, Kentucky nurses can obtain additional education on identifying signs of burnout and ways to reduce stress by viewing a suicide prevention video and engaging in a program developed by the Kentucky Nurses Action Coalition in collaboration via the support of the Kentucky Nurses Association (15).
As previously emphasized in this Kentucky Suicide Prevention course, in comparison to the general population, there is notably a higher risk of suicide amongst nurses (both females and males) (8). There are many suicide risk factors among nurses, but the following are some of the most evident: exposure to frequent trauma and death; working long, consecutive shifts; workplace bullying; neglecting self- care; social isolation or seclusion; and access to as well as knowledge of, lethal substances, such as opioids (5). Case in point, it has been proven that female nurses often opt for pharmacological poisoning (e.g., opioids and benzodiazepines) as a method to complete suicide, whereas their male counterparts utilize firearms in the same nature as the general population (8). Nurses are unlikely to seek mental health assistance in comparison to the general population due to some of the following reasons: concerns with how their careers could potentially be impacted; uncertainties regarding confidentiality; conflicts with taking time off to attend appointments as well as inability to obtain appointments; and fear of potential consequences associated with their professional licenses in the form of reprisals (11). For optimal outcomes, strategies to address suicide risks must aim to properly identify and address those exhibiting signs of burnout and depression as well as to reduce stigma and other barriers to seeking treatment (11). Next we will explore strategies to address suicide risk factors as required by the Kentucky Board of Nursing in this Kentucky Suicide Prevention course.

Self Quiz
Ask yourself...
- What are workplace concerns that you have witnessed or encountered which are associated with burnout?
- What are ways to assess for suicide risk factors in nurses?
- Are there any specific suicide risk screening tools utilized by your organization?
- Are you aware of the resources available for suicide awareness?
Strategies to Address Suicide Risks
Mental health promotion is one of the most critical strategies to help decrease incidences of suicide in the nursing population (2). Upon identifying individuals and/or groups at risk for suicide, it is important to derive pathways for proper intervention. The negative stigma associated with the treatment of mental illnesses is a well-known barrier for those in need of help, especially professionals such as nurses who are obliged to taking care of others, and this stigma prevents individuals from seeking treatment when they lack any type of support system. Organizations can better support individuals who are at risk for suicide by assuring that suicide training and screening tools for suicide risk are available to all employees, making every other member in one’s organization part of their support network. In fact, there are three primary initiative-taking strategies recommended by the Suicide Prevention Resource Center (SPRC) for organizations to implement and those strategies include establishing a respectful, inclusive work environment; identifying employees at risk for suicide; and formulating a responsive plan to enforce (12). Vitally, there should be identifying and reporting methods available for nurses to be screened anonymously (2). For example, individuals enduring a crisis can text “HOME” to 741741 to communicate with a crisis counselor (15). Another example of an anonymous suicide prevention resource is the HEAR (Healer Education Assessment and Referral) screening program (2). The HEAR program is purposed for screening, assessing, and referring nurses at risk for suicide as well as providing education pertaining to mental health, and likewise, it is aimed at removing the stigma associated with the reluctancy in seeking mental health assistance (16). In addition, managers and leaders are equipped with the knowledge necessary for providing support to their staff which, in turn, leads to healthier ways for alleviating stress and avoiding burnout (16). Essentially, organizations must convey the message to their employees that it is okay to seek assistance for mental health concerns as their well-being is priority. This can also be achieved by offering resources such as Employee Assistance Programs or displaying information for crisis hotlines (e.g., National Suicide Prevention Lifeline, Safe Call Now, Disaster Distress Helpline, or the Crisis Text Line) for individuals who are experiencing depression and/or those afflicted by suicidal thoughts/ideations (2). Trainings and in-services are also necessities.
Oftentimes, an individual may require the assistance of a peer (whether a colleague or a friend) when faced with a crisis (2). Nurses should be educated and aware of suicide prevention strategies which include assessing for risk factors, inquiring about plans (ask direct questions) as well as means, monitoring behavior, and collaboratively creating a safety plan (13). Specifically, some of the strategies recommended to prevent suicide include the following: reinforce economic supports; strengthen access and delivery of suicide care; generate protective environments; encourage connectedness; teach coping and critical thinking skills; identify and support people at risk; and reduce harms and prevent future risk (6). Though suicide prevention strategies may not be 100 percent effective in stopping an individual from executing a plan, peers need to know how to identify signs of suicide risk to properly support their colleagues in obtaining appropriate mental health assistance (2). Besides, the American Foundation for Suicide provides an abundance of suicide prevention resources (3). In essence, suicide awareness and prevention are vital.

Self Quiz
Ask yourself...
- What do you feel would be a vital strategy for assessing for signs of burnout and suicide risks in a colleague?
- Do you believe that suicide awareness education is impactful for suicide prevention?
- Does your organization utilize any specific tools to assess for suicide risk?
Additional Interventions and Protective Factors to Reduce Suicide Rates
Though assessing and safety planning are crucial in caring for nurses at risk for suicide, it is also important that appropriate referrals and follow-up interventions are implemented. As previously indicated in this Kentucky Suicide Prevention course, the HEAR program is an anonymous program that was designed to assess and refer individuals at risk for suicide. The program interactively screens the individual, categorizes the responses into tiers, then proactively provides options for counseling either online, via telephone, or in-person, and/or referrals are submitted to community providers for continuity in treatment (1). This method is remarkable for nurses who are reluctant to seek help because of the fear of having one’s career and reputation jeopardized, as their organizational safety net does what is supposed to do – recognize and report. What is also more noteworthy is that the HEAR team can be contacted for assistance by employees who have identified colleagues who are at risk (1). Correspondingly, organizations can replicate the HEAR program at their facilities by either modifying their Employee Assistance Programs to incorporate the HEAR service, establishing contracts with local or virtual mental health agencies, or by imitating the program by means of staffing provisions (1). Still, organizations can elicit protection to employees at risk by promoting safety and wellness as well as encouraging teamwork and providing support (18). Similarly, it is important that other preventive and/or protective factors are explored to achieve a reduction in suicide rates. For that matter, Hutton (2015) listed the following as preventive or protective factors for individuals at risk for suicide: “Reasons for living, perceived meaning in life, adaptive beliefs; Social support and feeling connected that may include religious affiliation; Being married, and for women, being pregnant, having children; Restricted access to firearms; Moral objection to suicide; Engaged in treatment or having access to mental or physical health care; Resilience, coping skills; Fear of social disapproval; and Cognitive flexibility”. In the same aspect, following up with an individual at risk is another intervention that can assist in prevention and protection. In this regard, one major advantage of the HEAR program is its unique outreach approach which entails counselors following up with the individual to assist him/her in seeking emergent care or to help the affected individual obtain an appointment for mental health treatment/counseling in a timely manner (10).

Self Quiz
Ask yourself...
Think about your current practice.
- Are there guidelines in place for dealing with patients or colleagues who are suicidal?
- Are debriefings held after stressful incidents?
- What type of resources does your organization have in place to address burnout and suicide prevention?
Ethical and Legal Considerations Regarding Care for Suicidal Individuals
As formerly stated, no intervention is 100% certain to prevent an individual from executing a suicidal plan, but with training and resources to help recognize and support, the resulting interventions have proven to be positively impactful in many cases. However, when providing care for suicidal individuals, ethical and legal considerations should be prioritized.
For one’s protection as well as the protection of the individual and the organization, the following legal considerations are notable when caring for persons who are at risk for suicide: become familiar with suicide policies and procedures for your organization; gain awareness regarding state laws associated with advanced directives, involuntary commitment, seclusion and restraint; familiarize yourself with HIPAA regulations and exceptions regarding confidentiality; and if dealing with a patient, document all action in his/her health record (13).
Also, if one is assisting a colleague, organizational protocol should be followed. As a nurse professional, it is crucial that one follows policies, procedures, and protocol to avoid breaching patient confidentiality as well as potentially being sued for negligence or malpractice. It is equally important to consider ethical responsibilities when dealing with individuals at risk or suicide. A nurse can reference the professional Code of Rthics as a guide for dealing with ethical concerns or he/she can consult with an ethics committee. Regarding ethical responsibilities, one should display these key attributes: be respectful and compassionate, serve as an advocate, promote health and safety, encourage autonomy, maintain confidentiality, refrain from conflict of interests, participate in collaborative care, engage in research to remain cognizant of evidence-based practices, and address ethical issues (9).

Self Quiz
Ask yourself...
- Are you competent in assessing and intervening when dealing with an individual who is at risk for suicide?
- What do you believe is the best approach for making sure individuals at risk for suicide receive appropriate care and follow-up?
- What are ethical considerations to be mindful of when dealing with patients or colleagues at risk for suicide?
- What are legal considerations to reflect on when dealing with individuals who are at risk for suicide?
Case Study
A 24-year-old novice nurse has been noted to have discrepancies in the narcotic counts of her medication cart on a few occasions. Moreover, it has also been observed by other colleagues that the nurse is often truant, and her mood is very unpredictable. She has episodes of extreme euphoria, and she has become overly generous (i.e., offering a necklace that she inherited from her late mother to a colleague). Even more so, an incident report was recently completed regarding her miscalculation of a critical medication dosage. Although the nurse’s error reflected in the incident report was a “Near Miss,” the nurse’s recent behavioral changes warrant the need for immediate intervention. Regrettably, this error has caused the nurse to feel even more overwhelmed and emotionally detached. All the above occurrences have resulted in her feeling emotionally unstable to the point of her expressing suicidal thoughts and ideations. A colleague who has established rapport with the nurse makes herself available to listen, she asks the nurse direct questions, and she provides encouragement to the nurse as well as supportive resources (i.e., phone numbers for the Employee Assistance Program, the National Suicide Prevention Lifeline, and the Crisis Text Line). What are other strategies that might be valuable to the nurse’s prognosis?
Recommendations
All nurses and healthcare professionals in the same respect should engage in continuing education which addresses suicide prevention. Principally, it takes a collaborative approach to provide individualized and organizational support to a nurse/colleague in crisis. For best results, there should be programs in place and resources available which promote suicide awareness, highlight protocol, and offer ongoing support. Ultimately, the goal of promoting mental health and wellness for nurses is to reduce the likelihood of suicide.
Opioid Abuse
What are Opiates?
Opiates are powerful substances which are commonly used to alleviate both acute and chronic pain. The history of opiate use / abuse goes back many thousands of years. The first recorded reference is from 3,400 B.C. when opium was cultivated in southwest Asia. There were even wars fought over the previous flow in the mid 1800s (1). The most famous historical event related to opium were the advent of “opium dens.” These were underground “dens” where opium was bought, sold, and used (1). Much like today, the addictive properties of opium overcame many individuals and caused great harm to the world and communities. Indeed, the opiate epidemic of the 2000’s is not the first in modern history, though it is much different and more severe than previous epidemics.
Today opiates are used for both acute and chronic pain. The ability to quickly, reliably, and (when used appropriately) safely reduce pain is what makes the drug class so valuable. Many common drugs are opiate derivatives or synthetics including morphine, codeine, oxycodone, heroin, hydromorphone, and fentanyl.
In the United States Opiates are considered controlled substances and most of them are classified as schedule II (with heroin classified as schedule I) (2). Opiates will always have a place in medicine and treatment of pain and are incredibly useful, however, the current opiate epidemic in America makes clear the potential consequences of opiate abuse.
Preventing Abuse, Misuse, and Harm
Every day 130 Americans die of opiate overdose (3). Additionally, there are 4.3 million Americans each month who engage in the non-medical (non-prescribed or illicit) use of opiates (5). However, it is key to remember that opiate-related deaths are not the only negative consequences. There are many overdoses which do not end in death, and on the other end of the spectrum many negative affects do not cause death. Addiction can cause loss of job, damage to relationships, psychologic distress, homelessness, and many more negative side-effects.
So how do healthcare professionals help reduce the impact of opiate addiction and misuse? The approach must be multi-modal, aimed at primary, secondary, and tertiary prevention.
- Primary prevention includes appropriate opiate prescribing, risk stratification with patients, and preventing opiate addiction.
- Secondary prevention is aimed at mitigating the effects of opiate addiction. This includes rehabilitation and cessation of opiates in addicted individuals, ideally in favor of non-opiate treatment options.
- Tertiary prevention is the reduction in harm from opiate addiction and overdose. This includes resuscitation of overdose patients and helping patients recover from the effects of opiate addiction.
Appropriate Prescribing
The Centers for Disease Control and Prevention (CDC) offers excellent guidance on how to appropriate prescribe opiates, though it will continue to require a great deal of knowledge and effort from individual prescribers and managers of chronic pain. For the purposes of this article, we will focus on the CDC recommendations. Below we will discuss the 12 key points of opiate management, per the CDC.
Opioids Are Not First-Line Therapy
“Nonpharmacologic therapy and nonopioid pharmacologic therapy are preferred for chronic pain. Clinicians should consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks to the patient. If opioids are used, they should be combined with nonpharmacologic therapy and nonopioid pharmacologic therapy, as appropriate.” (5)
Author’s Input
Many patients experience pain. Indeed, it is one of the most common complaints in primary care offices. When dealing with chronic pain, we should consider ALL non-opiate therapies for patients prior to prescribing opiates. This can include physical therapy, meditation, exercise / movement, treatment of underlying depression and/or psychiatric issues, meditation, modification of aggravating factors, and many more interventions. In some cases, none of these alone or combination will be enough to provide satisfactory relief, but we must utilize non-opiate and non-pharmacological solutions as much as possible to reduce opioid abuse, and dose (if opiates are necessary).
Establish Goals for Pain and Function
“Before starting opioid therapy for chronic pain, clinicians should establish treatment goals with all patients, including realistic goals for pain and function, and should consider how opioid therapy will be discontinued if benefits do not outweigh risks. Clinicians should continue opioid therapy only if there is clinically meaningful improvement in pain and function that outweighs risks to patient safety “(5).
Author’s Input
Many patients erroneously believe that cessation of pain is the goal of therapy. This is not based in fact nor is it reasonable, as many patients (even with opiate therapy) will not have complete remission of pain. The goal of the clinician should be to work with the patient to provide the minimal risk intervention that will provide acceptable pain control.
Discuss Risks and Benefits
“Before starting and periodically during opioid therapy, clinicians should discuss with patients known risks and realistic benefits of opioid therapy and patient and clinician responsibilities for managing therapy” (5).
Author’s Input
A prescription for an opiate should never be written to a patient without a through discussion of the risks and benefits. The clinician must first be convinced that the risk to benefit favors prescribing an opiate. Then, they must discuss their rationale with the patient. An individual assessment regarding the risks should be provided to each and every patient.
Prescribe Immediate-Release Opioids First
“When starting opioid therapy for chronic pain, clinicians should prescribe immediate-release opioids instead of extended-release/ long-acting (ER/LA) opioids” (5).
Author’s Input
Extended-release opioids have been associated with higher rates of overdose and higher potential for Opioid abuse. Immediate-release opioids should be utilized first, whenever possible.
Clinicians Should Prescribe the Lowest Effective Dosage
“Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when considering increasing dosage to ≥50 morphine milligram equivalents (MME)/day, and should avoid increasing dosage to ≥90 MME/day or carefully justify a decision to titrate dosage to ≥90 MME/day.”
Author’s Input
The clinician must keep in mind that the “minimum required dose” may change over time. As a patient implements more non-pharmacologic interventions the required dose may decrease. Conversely, there can be some degree of tachyphylaxis with opiates and the required dose may also increase. Dose titration requires careful clinician judgement.
Prescribe Short Durations for Acute Pain
“Long-term opioid use often begins with treatment of acute pain. When opioids are used for acute pain, clinicians should prescribe the lowest effective dose of immediate-release opioids and should prescribe no greater quantity than needed for the expected duration of pain severe enough to require opioids. Three days or less will often be sufficient; more than seven days will rarely be needed” (5).
Author’s Input
It is well established that chronic opioid therapy is not the most effective therapy for pain management. Clinicians should consider adjuncts for ongoing or chronic pain patients.
Evaluate Benefits and Harms Frequently
“Clinicians should evaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy for chronic pain or of dose escalation. Clinicians should evaluate benefits and harms of continued therapy with patients every 3 months or more frequently. If benefits do not outweigh harms of continued opioid therapy, clinicians should optimize other therapies and work with patients to taper opioids to lower dosages or to taper and discontinue opioids” (5).
Author’s Input
It is important that clinicians consider changing circumstances. A patient’s health status or life circumstances may change such that opiate therapy benefits no longer outweigh the harm, or vice-versa.
Use Strategies to Mitigate Risk
“Before starting and periodically during continuation of opioid therapy, clinicians should evaluate risk factors for opioid-related harms. Clinicians should incorporate into the management plan strategies to mitigate risk, including considering offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, higher opioid dosages (≥50 MME/day)” (5).
Author’s Input
Naloxone therapy should be considered for all patients who are at high risk of Opioid overdose.
Review Prescription Drug Monitoring Program Data
“Clinicians should review the patient’s history of controlled substance prescriptions using state prescription drug monitoring program (PDMP) data to determine whether the patient is receiving opioid dosages or dangerous combinations that put him or her at high risk for overdose. Clinicians should review PDMP data when starting opioid therapy for chronic pain and periodically during opioid therapy for chronic pain, ranging from every prescription to every 3 months” (5).
Author’s Input
Each state has robust data regarding prescription medication; utilizing this data can help reduce opioid misappropriation and concurrent prescriptions (doctor shopping).
Use Urine Drug Testing
“When prescribing opioids for chronic pain, clinicians should use urine drug testing before starting opioid therapy and consider urine drug testing at least annually to assess for prescribed medications as well as other controlled prescription drugs and illicit drugs,” (5).
Author’s Input
The author recommends that clinicians take great care in this area. Indeed, drug testing can help identify those who are already abusing other substances, but it can also harm the trusting relationship developed between a patient and clinician. The patient should be re-assured that the testing is performed for their own good and out of concern for their own health, rather than punitively or because the clinician “mistrusts” them, as these may be the default thoughts of many patients.
Avoid Concurrent Opioid and Benzodiazepine Prescribing
“Clinicians should avoid prescribing opioid pain medication and benzodiazepines concurrently ‘whenever possible’ “(5).
Author’s Input
The highest risk of overdose of opioid abuse is commonly seen when opiates and benzodiazepine (or any combination of sedating medications) are prescribed concurrently, especially in conjunction with alcohol. For this reason, clinicians should strongly consider avoiding such risks and only prescribing this combination when absolutely necessary.
Offer Treatment for Opioid Abuse Disorder (OAD)
“Clinicians should offer or arrange evidence-based treatment (usually medication-assisted treatment with buprenorphine or methadone in combination with behavioral therapies) for patients with opioid abuse disorder” (5).
Author’s Input
In acute cares settings, clinicians often view OAD as a secondary illness and it is frequently left unaddressed. However, there are now effective treatments for OAD. Given the significant morbidity, mortality, and associated quality of life issues, patients with OAD should be offered treatment, even if it not the primary reason for treatment.
Risk Factors for Opiate Harm or Misuse
The risk to benefit has been discussed many times previously and is often referenced by the CDC. The benefits of opiate therapy are typically obvious (reduced pain, increased quality of life, etc.), but the risks are less often discussed. So how do nurses know who is at higher risk of the negative effects of opiates?
According to the CDC, the major risk factors are:
- Illegal drug use; prescription drug use for non-medical reasons.
- History of substance use disorder or overdose.
- Mental health conditions (e.g., depression, anxiety).
- Sleep-disordered breathing. • Concurrent benzodiazepine use (6).
Mortality from opiates is highest in those who are middle-aged, have psychiatric conditions, and/or have previously abused substances (7). It is important that clinicians utilize this information when consider risk and benefits associated with opiate therapy.
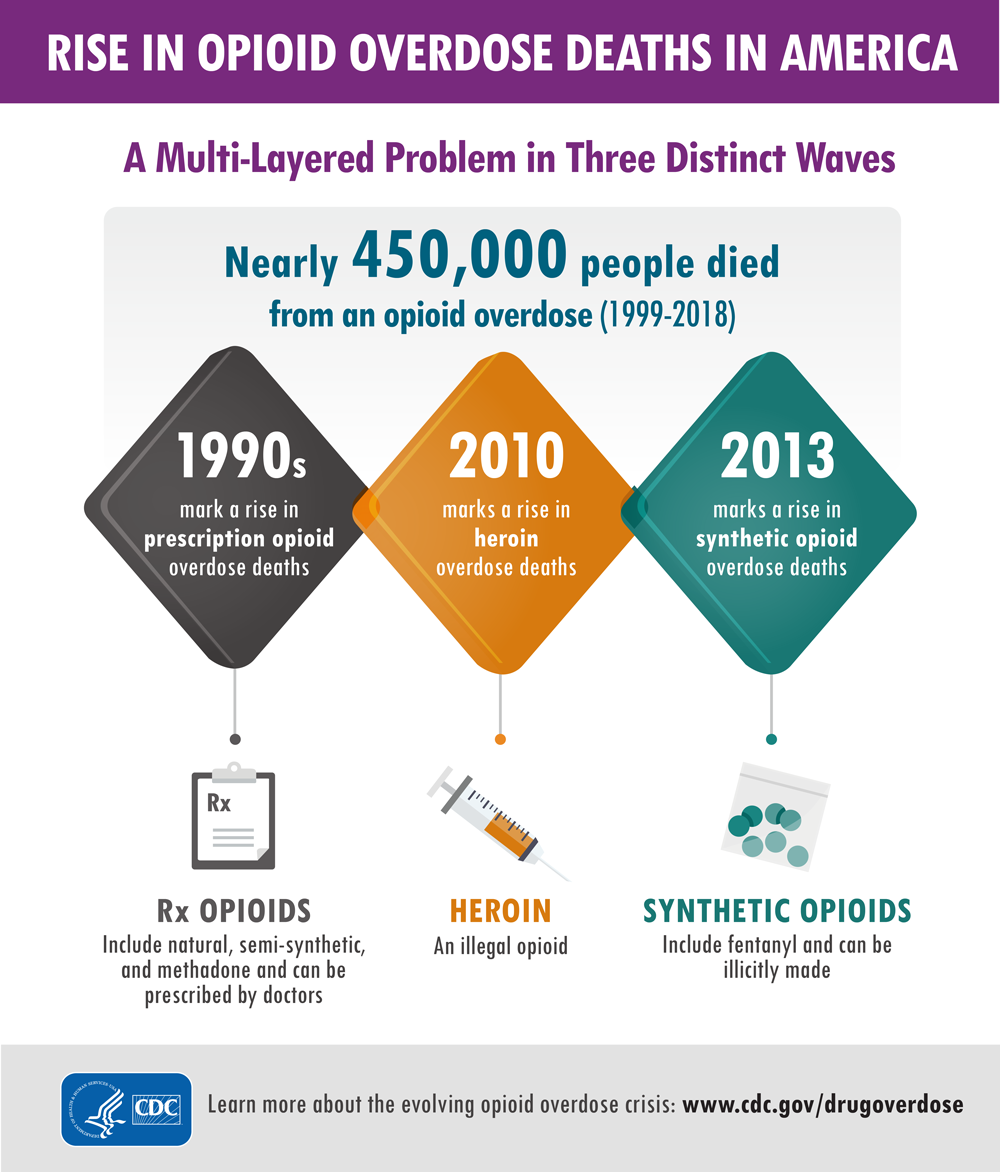
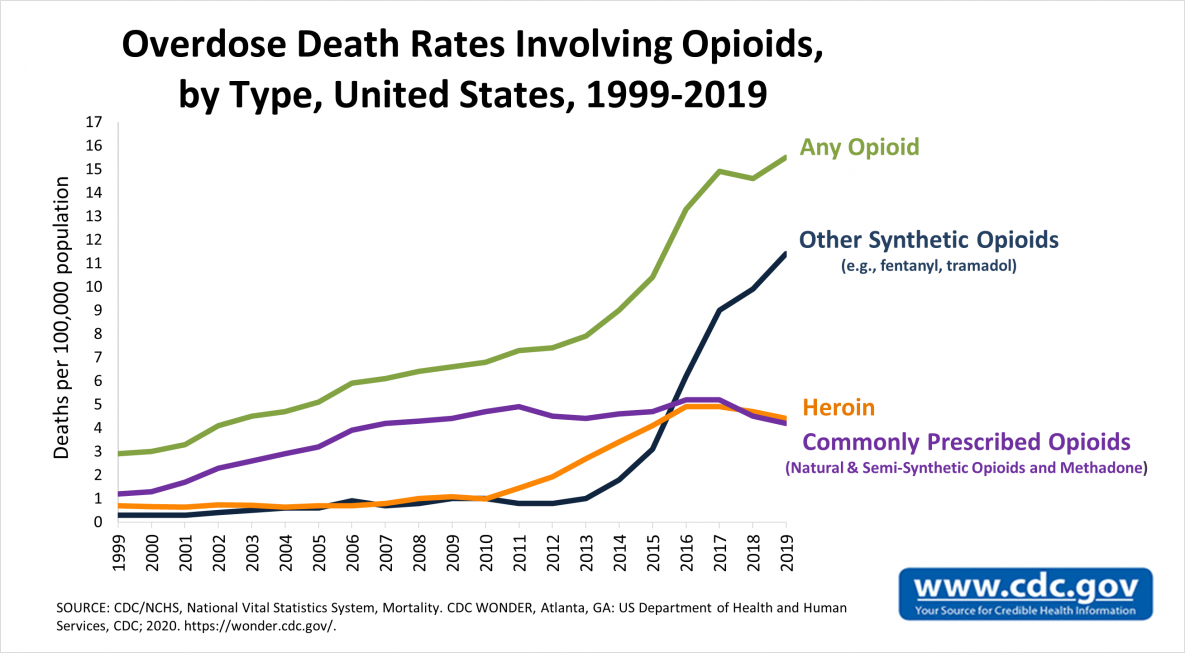
Signs of Abuse, Diversion, and Addiction
Clinicians should remain vigilant for signs of opiate use disorder, as it can occur in any patient (even those not prescribed opiates). Opiate use disorder is characterized in the DSM-5 as a desire to utilize opiates despite social and professional consequences (12). It includes dependence and addiction, with addiction being on the severe end of the spectrum (12). Opiate use disorder can be diagnosed when at least two of the following are observed in a 12-month period:
- Opioids are often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control opioid use.
- A great deal of time is spent in activities necessary to obtain the opioid, use the opioid, or recover from its effects.
- Craving, or a strong desire or urge to use opioids.
- Recurrent opioid use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of opioids.
- Important social, occupational, or recreational activities are given up or reduced because of opioid use.
- Recurrent opioid use in situations in which it is physically hazardous.
- Continued opioid use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance.
- Exhibits tolerance (discussed in the next section).
- Exhibits withdrawal (discussed in the next section) (centers for disease control, reference 13).
Urine drug screening can be useful in patients with suspected opiate abuse disorder as it may identify concurrently abused substances. If a patient is found to have opiate abuse disorder the “risk” side of the “risk-to-benefit” equation is now shifted, and the continued use should be carefully weighed against the potential for negative effects, including addiction. Addiction is defined as continued use despite adverse events or consequences (12).
For those prescribed opiates, clinicians should have candid conversations about the risks of continued use for those with OAD. The CDC offers some creative examples of how to discuss the condition with patients, which nurses may find helpful in their interactions (these are only examples, and the wording depends on the patient’s specific scenario and needs):
“Trouble controlling the use of opioid medication makes it unsafe, and long-term risk over time is substantial.”
“The medicine has become a problem in itself. You have developed a known complication of therapy that we should not ignore.”
“Continuing the current medication is not a reasonable option due to the risks, but there are options for treating what we call opioid use disorder, also known as OUD.”
“It seems as if you are running out of your medication more quickly than anticipated.”
“Sometimes people become too comfortable with the medications and start to take them for reasons other than pain.”
“You meet the criteria for opioid use disorder, also known as OUD. It’s helpful to put a name on it because it opens up a variety of approaches to help with your specific circumstance.” (All derived from source 13).
So, once we identify a patient with OAD, what do we do? At this point, as above, a candid conversation with the patient must occur. A treatment plan should be formulated, which would include a careful consideration for discontinuing for the opiate (if possible). This provides an excellent transition into our next section, opiate alternatives.
Opiate Alternatives
Opiate alternatives can be broadly classified as pharmacologic and non-pharmacologic. We will first discuss pharmacologic alternatives.
Pharmacologic:
Acetaminophen
Commonly known as Tylenol ™ is over the counter and has a very favorable safety profile when used correctly. Acetaminophen is considered first-line therapy in any pain management regimen (9).
NSAIDs (Nonsteroidal anti-inflammatory drugs)
NSAIDs can be immensely powerful in pain management, as many pain conditions are related to inflammation. However, patient tolerance can be an issue with chronic NSAID exposure. Indeed, many clinicians shy away from NSAIDS due to the perceived risk profile (9).
Tricyclic Antidepressants
TCAs provide significant pain relief to many patients, as they have the unique ability to change the perceptions of pain (5). However, tricyclics have many side-effects of their own and thus have been phased out in lieu of newer antidepressants. This in the pain realm they should be considered for certain patients, particularly those with concurrent untreated depression.
SSRI Antidepressants
SSRIs are typically tolerated better than tricyclics (9) but again are not recommend for first-line analgesia. They are typically reserved for those with concurrent psychiatric illness which may benefit from the overall effect of the drug, and on a case-by-case basis for selected patients.
Muscle Relaxants
Medications such as gabapentin can be extremely useful especially in pain originating from musculoskeletal causes. However, the mechanism of action is poorly understood (9) and side effects can be troublesome. In one study approximately 25% of patients taking muscle relaxants for chronic pain discontinued the agents due to adverse effects.
Topicals
Many topical agents now exist, including NSAIDS (9). Topicals are typically considered analgesic-sparing rather than standalone treatment (9). The American College of Rheumatology has excellent and detailed guidance on how to utilize topicals, which deserves a course of its own.
Corticosteroids
Corticosteroids have very potent anti-inflammatory effects (9) and have a proven role in pain management. Short-term therapy is typically favored over long-term therapy due to the potential issues of long-term systemic therapy (osteoporosis, immunosuppression, risk of serious or fatal infections, weight gain, muscle weakness, diabetes, Cushing’s syndrome, hypertension, glaucoma, and cataracts). Though some serious adverse events can occur with short-term therapy (psychosis, anxiety, avascular necrosis, etc.) (9). corticosteroids can be beneficial for patients with acute pain. Perhaps the best use of these agents is in targeted (injectable) delivery.
Non-Pharmacologic:
These therapies will be discussed less in-depth, as they typically require referrals for treatment. However, it is important that nurses are aware of the of the existence of these therapies and can make appropriate referrals and recommendations. Physical therapy consults are invaluable as they often utilize many of the tools below and are more knowledge about non-pharmacologic therapies in general.
- psychological interventions (including distraction, stress management, hypnosis, and other cognitive-behavioral interventions)
- acupuncture and acupressure
- transcutaneous electrical nerve stimulation
- physical therapies (including massage, heat/cold, physiotherapy, osteopathy, and chiropractic) (10)
Conclusion
Nurses should view the non-pharmacologic therapies as “tools” available to help patients dealing with acute and chronic pain. Though opiate therapy is a valuable tool as well, its potential negative effects are often under-considered, and the rate of opiate prescription currently is excessive (10).
When evaluating patients with pain, nurses should work with patients and providers to ensure that the patient is on an optimal pain regimen, which ideally should include both pharmacologic and non-pharmacologic therapies. Seeking referral and consultation from relevant professionals can also be powerful in pain management (physical therapists, chiropractors, psychiatrists, etc.).
LGBTQ+ Cultural Competence
Introduction
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ) individuals represent a rapidly growing segment of the U.S. population [1]. This rapid growth brings with it risk for stigmatization [1]. Implicit physician biases may result in LGBTQ patients receiving a lower standard of care or restricted access to services as compared to the general population [2]. Even when institutions and providers make commitments to equitable care explicit, implicit biases operating outside of conscious awareness may undermine that commitment. There is an urgent need to ensure that health care providers are prepared to identify and address their own implicit biases to ensure they do not contribute to the health care disparities experienced by LGBTQ and other vulnerable populations. Only by addressing their own implicit biases will health care providers be able to provide patient care in accordance with LGBTQ cultural competence.
LGBTQ individuals face significant disparities in physical and mental health outcomes [3]. Compared to their heterosexual counterparts, LGBTQ patients have higher rates of anal cancer [4], asthma, cardiovascular disease [5,6,7,8], obesity [6], substance abuse [8,9,10], cigarette smoking [11], and suicide [12]. Sexual minority women report fewer lifetime Pap tests [13,14,15], transgender youth have less access to health care [16], and LGBTQ individuals are more likely to delay or avoid necessary medical care [17] compared to heterosexual individuals. These disparities are due, in part, to lower health care utilization by LGBTQ individuals [3, 18,19,20]. Perceived discrimination from health care providers and denial of health care altogether are common experiences among LGBTQ patients and have been identified as contributing factors to health disparities [21,22,23,24]. Disparities in health care access and outcomes experienced by LGBTQ patients are compounded by vulnerabilities linked to racial identity [25,26,27] and geographic location [28].
Biases among health care professions students and providers toward LGBTQ patients are common [29, 30] despite commitments to patient care equality. These biases, also known as negative stereotypes, may be either explicit or implicit [31]. These biases contribute to a lack of LGBTQ cultural competence in patient care. A large study of heterosexual, first-year medical students demonstrated that about half of students reported having negative attitudes towards lesbian and gay people (i.e., explicit bias) and over 80% exhibited more negative evaluations of lesbian and gay people compared to heterosexual people that were outside of their conscious awareness (i.e., implicit bias) [29]. Research in social-cognitive psychology on intergroup processes defines explicit biases as attitudes and beliefs that are consciously accessible and controlled; they are typically assessed via self-report measures and are limited by an individual’s awareness of their attitudes, motivation to reveal these attitudes, and ability to accurately report these attitudes [32, 33]. In contrast, the term implicit bias refers to attitudes and beliefs that are unconscious (i.e., outside of conscious awareness) and automatic [34, 35]. Implicit bias can be assessed with the Implicit Association Test (IAT) [36], which measures the strength of association between concepts [37].
Health care provider biases are correlated with poorer access to services, quality of care, and health outcomes [31, 38,39,40]. Explicit biases held by health professionals towards racial/ethnic minorities, women, and older adults are known to affect clinical assessments, medical treatment, and quality of care [41]. Importantly, implicit bias measures are more strongly associated with real-world behaviors than explicit bias measures [42] and are linked to intergroup discrimination [43]. Health care provider’s implicit biases towards vulnerable patient groups may persist despite an absence of negative explicit attitudes [44], resulting in preconceived notions about patient adherence, poor doctor-patient communication, and micro-aggressions, all of which can interfere with optimal care. With less time and limited information processing capacity, provider’s decisions are increasingly governed by stereotypes and implicit biases [45]. Medical student and provider biases may contribute to health disparities in vulnerable populations by negatively impacting communication with patients and decisions about patient care [33, 35]. Taken together, these findings suggest that medical students and healthcare providers are likely to underestimate or to be unaware of their implicit biases towards LGBTQ patients, particularly when they are rushed or fatigued, which could impact their behavior and judgments in ways that contribute to health disparities experienced by LGBTQ populations. By learning about and addressing their implicit biases, health care providers can work towards demonstrating LGBTQ cultural competence and providing optimal care (Introduction section courtesy of Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P.- reference 45).

Self Quiz
Ask yourself...
- What are some cultural misconceptions regarding the LGBTQ community and providing medical care?
- How can you demonstrate LGBTQ cultural competence in everyday practice?
Terminology
Understanding the standard terminology utilized is pivotal to treating and interacting with LGBTQ patients. Below are listed some of the common terms and how they should be referenced.
Ally – A person not identifying as LGBTQ, but who promotes equality and support of LGBTQ peoples in a variety of ways.
Androgynous – Identifying as neither masculine nor feminine.
Bisexual – A person who is emotionally, romantically, or sexually attracted to more than one sex, gender, or gender identity.
Cisgender – A person who identifies with their gender which as assigned at birth. For example, a person assigned female gender at birth who identifies as female.
Gay – A person who is emotionally, romantically and/or sexually attracted to those of the same gender.
Gender-fluid – A person who identifies as a fluid or unfixed gender identity.
Lesbian – A woman who is emotionally, sexually, and/or romantically attracted to other women.
LGBTQ – Acronym for “lesbian, gay, bisexual, transgender, and queer.”
Non-binary – Adjective describing person(s) who do not identify exclusively as man nor woman.
Pansexual – A person who has the potential for romantic, emotional, and/or sexual attraction to people of any gender.
Queer – Often used interchangeably with “LGBTQ,” or to express fluid identities or orientations.
Sexual Orientation – An inherent or enduring emotional, romantic, or sexual attraction to other people.
Transgender –Umbrella term for people whose gender identity and/or expression is different from cultural expectations based on the sex they were assigned at birth. It does not imply any specific sexual orientation and transgender persons may identify as straight, gay, lesbian, bisexual, etc.
*Definitions largely derived from (46).

Self Quiz
Ask yourself...
- Which of the above definitions have you heard used interchangeably?
Best Practices
Below we will list and discuss the best practices for ensuring a positive, equitable healthcare experience for LGBTQ persons, according to the Joint Commission (this is not a comprehensive list, just highlights).
Create a welcoming environment that is inclusive of LGBT patients and demonstrates LGBTQ cultural competence.
- Prominently display the hospital nondiscrimination policy and/or patient bill of rights.
- Waiting rooms and common areas should be inclusive of LGBTQ patients and families.
- Unisex or single-stall restrooms should be available.
- Ensure that visitation policies are fair and do not discriminate (even inadvertently) against LGBTQ patients and families.
- Foster an environment that supports and nurtures all patients and families.
Avoid assumptions about sexual orientation and gender identity.
- Refrain from making assumptions about a person’s sexual orientation and/or gender identity.
- Be cognizant of bias, stereotypes, and other communication barriers.
- Recognize that self-identification and behaviors do not always align.
Facilitate disclosure of sexual orientation and gender identity but be aware that disclosure is an individual process.
- Honor and respect patient’s decisions to provide or not provide sexual and/or gender information.
- All forms should contain inclusive, gender-neutral language that allows patients to self-identify.
- Use neutral and inclusive language when communicating with patients.
- Listen to and respect patients’ choice of language when they describe their own sexual orientation.
- Conduct confidential patient satisfaction surveys that include questions regarding sexual orientation and gender identity.
*Information largely derived from Joint Commission field guide, reference 47.
For more information on best-practices in the workforce, visit the Joint Commission website by clicking here.

Self Quiz
Ask yourself...
- Have you ever misused a pronoun, or overheard a co-worker misuse a pronoun in practice? How can you make sure this doesn’t happen again?
Establishing Relationships with LGBTQ Patients
When interacting with patients, one should not assume gender or sexuality. Addressing a patient who identifies as a female as a male can cause grave harm to the relationship. Instead, nurses should use open-ended questions. For example, rather than saying “Hi sir, what brings you to the hospital,” a nurse might say, “Welcome, what brings you to the hospital today (48)?”
If a nurse uses the incorrect pronoun, the best practice is to apologize and ask the patient what pronoun and name they prefer. For example, a nurse may say, “I apologize for assuming your gender. How would you like to be addressed? (48).
In conversation, the nurse should use the name and/or pronoun the patient prefers without drawing special attention to the subject (48). For example, if a male patient prefers to be identified as his partner’s wife, you should follow suit.
The core of relationship-building with LGBTQ patients is no different than any other patient, fundamentally. If nurses have a basic understanding of best practices and a healthy dose of respect and compassion for LGBTQ patients, a positive relationship is likely to develop.

Self Quiz
Ask yourself...
- Do you have any biases which may affect the care you provide to LGBTQ patients?
- Have you worked for someone who did NOT demonstrate LGBTQ cultural competence? In what ways could they improve their practice?
Health Disparities of LGBTQ Patients
LGBT Americans are at higher risk of substance use, sexually transmitted diseases, cancer, cardiovascular disease, obesity, bullying, isolation, anxiety, depression, and suicide when compared to the general population (49). LGBT youth are frequently bullied at schools (49). In fact, early victimization and subsequent emotional distress accounted for 50% of the disparities between LGBT youth (49). In other words, LGBT Americans are discriminated against and disadvantaged from a very young age.
When home life also reflects a lack of LGBTQ cultural competence, more problems arise. A major cause of LGBT distress is family rejection. Disclosure of gender identity or sexuality can cause very significant interpersonal conflicts among family and friends of LGBT persons (49). This explains some hesitancy and should help nurses understand the importance of respecting privacy, while giving options to patients about disclosing sexuality and gender.

Self Quiz
Ask yourself...
- Are there any circumstances in which your current hospital’s policies could discriminate against LGBTQ families?
- If so, how would you begin to work with leadership to change those policies, so they reflect LGBTQ cultural competence?
Providing an Inclusive and Accepting Care Environment
LGBTQ patients often experience difficulty in finding healthcare environments in which they feel accepted and understood (48). Past negative experiences, lack of knowledge among healthcare providers, and limited access to healthcare in general may become major barriers for LGBTQ persons when seeking care (48).
The core tenant of providing an inclusive environment is understanding the needs of LGBTQ patients and working diligently to create an environment which does not disadvantage or discourage them from seeking care.
Policies and procedures at institutions should be designed to reflect a non-discriminatory environment. For example, many hospital policies dictate that only legal family spouses or partners can visit in specific circumstances. Policies such as this are inherently discriminatory toward LGBTQ patients, as they may not have legal spousal status due to social, legal, or personal reasons.

Self Quiz
Ask yourself...
- Have you ever had an experience where a colleague made a derogatory remark about a patient, based on sexual orientation or gender status? If this happened to you, how would you handle that situation differently?
Exercises on LGBTQ Cultural Competence
To help solidify your learning, please complete the following exercises at your own pace. The answers/guidance for each are provided below.
Scenario 1
A patient enters your emergency department, and you assume the patient identifies as a female. You introduce yourself and say, “Ma’am, how can we help you? What brings you in today?”
The patient appears dismayed but answers the question. The nurse is confused and does not understand why the patient appears distressed. What is the best course of action?
Answer: The nurse should apologize to the patient and ask the patient how they would like to be addressed. Then, the nurse should update the patient’s records to reflect such, to reduce further confusion.
If the nurse does not address the issue, the patient may feel uncomfortable and develop a negative association with healthcare, which can lead to disparities in the future.
Scenario 2
A patient in your ICU has had a deterioration while his husband was in the room. After a family meeting, a member of the healthcare team makes a derogatory remark about the patient’s sexuality. What is the next best action for the nurse?
Answer: Pre-conceived phobias and stigmatizations can cause significant distress to LGBTQ patients, even if not stated directly to them. These types of remarks are abusive and should not be tolerated. The nurse should confront the co-worker (if safe) and consider reporting the comments to the Human Resources department.
Scenario 3
A LGBTQ patient is being admitted and prefers not to disclose their sexuality. However, the nurse is unable to proceed with the admission process without this information. What could be done to rectify this system-level issue?
Answer: The nurse should work with administration to ensure that all charting and paperwork allows individuals to self-report sexuality and/or gender if they want. However, healthcare systems should not force patients to “come out” unless it is absolutely medically necessary.

Self Quiz
Ask yourself...
- What information from this course can you take to your facility to encourage a positive change of LGBTQ patients, and create an environment for LGBTQ cultural competence?
Conclusion
LGBTQ cultural competence must be ingrained in our healthcare systems in order to foster excellent relationships between members of the LGBTQ community and medical staff. Hospitals and healthcare systems have a great deal of work to do in becoming LGBTQ-friendly. The efforts must continue until LGBTQ patients and families do not feel disadvantaged, anxious, or frustrated when interacting with healthcare systems. As the patient’s ultimate advocate, nurses are at the front-line and should advocate for patients both individually and from a policy perspective. Nurses should work with and spearhead efforts to ensure that healthcare policies reflect best-practice and do not discriminate against LGBTQ patients in any way.
Effective Communication in Nursing
Introduction/Needs Assessment
Communication in nursing is key, and the ability to communicate effectively can be our lifeline. We depend on ourselves and others to be fluent and effective in the art of communication in order to perform our role as nurses successfully. When any link in our communication chain fails, we immediately see poor outcomes, wastage of resources, reductions in patient and staff satisfaction as well as a decline in the quality of patient care (1)
Types of Communication
In order to master effective communication in nursing, it is important to understand the various types of communication, their definitions, and the impact they can make.
Non-Verbal
This form of communication relies solely on the utilization of body language, including body and facial mannerisms, and completely lacks spoken words or sounds (2). We perform and identify non-verbal communication in nursing daily without giving it a second thought. We may see a newborn sucking on their hands, providing us a non-verbal cue that they are hungry. When assessing a patient holding their abdomen, we would look to initially target that area because they have communicated (non-verbally) that this is where they are experiencing discomfort. Smiling when the next shift nurse is walking in the door communicates to them that you are happy to see them, and that it’s about time for you to go home!
Since we perform non-verbal communication so often, it can become an incredibly powerful tool or an extremely negative one. This form of communication in nursing can be used positively to show our patients and co-workers that we have compassion, and we are engaged. Negative forms can make patients uncomfortable with sharing their medical history and result in a lower quality of patient care. Additionally, it can lead to dysfunctional teamwork among staff.
Verbal
Verbal communication occurs when we use words or sounds to discuss concepts with others (2). This form of communication in nursing has the conception to be a very easy notion, but it can create unfavorable consequences when used ineffectively. In order to produce clear verbal messages, we should always speak concisely and with confidence. As health care professionals, we have our own language, and understanding when to incorporate our medical jargon into conversations versus when to not is crucial in providing care. When communicating among co-workers, our medical knowledge can display professionalism and it is evident that they can follow along. However, when speaking with patients and their families, this may not always be the case and we must be able to effectively gauge our audience and ensure that they have a clear understanding of what we are teaching or explaining; this is an extremely valuable tool.
Written
This form of communication can be either a formal or informal transcription of words that are intended to serve as a direct communication form (2). Written communication in nursing is used daily and incorporates one of our most important duties, documentation. Throughout our nursing practice, we have learned the importance and necessity of our documentation; it can be useful for legal protection or provide critical data to other health care professionals. Written communication can also be accessed through the policies and procedures we employ to perform various tasks. Having sound, written communication, and interpretation skills is vital to the overall success of our nursing career.

Self Quiz
Ask yourself...
- What type of communication is being interpreted while watching a patient walk to the bathroom?
- Upon admission of a female patient for a fall, you are performing normal intake questions and a physical assessment. The patient is quiet and uses minimal verbal communication and looks down at the floor while you are in the room. What communication types are you interpreting?
Receiving Communication
The most common communication perception is usually directed to producing communication through non-verbal, verbal, or written forms. While the production of communication is important, the reception of it potentially holds even greater value. In nursing, ensuring our communication is received correctly affects every clinical, orientation, or job experience we have encountered thus far. Think about it…
- Taking notes in class or during a shift.
- When a preceptor or instructor educates you on a brand-new skill or piece of equipment.
- Teaching your patient, family, or student about a new diagnosis.
- Watching your patient breathe for rate, depth, and effort.
We must provide and receive communication in nursing through verbal, non-verbal, or written forms successfully. If communication fails, we will experience extremely negative effects throughout our entire nursing system.
Hearing & Listening
Hearing describes the process or act of perceiving sounds or spoken words (2). We hear sounds upon auscultation, varying frequencies of alarms, and patient concerns when they are voiced. Hearing all these sounds are heavily dependent on how they are used. To achieve successful implementation of these sounds, we must also listen to these sounds and words. To listen, we must hear and then interpret these sounds carefully (2). We interpret these sounds and words by asking additional questions, performing additional assessments, or paraphrasing the information presented.

Self Quiz
Ask yourself...
- What is the best way to ensure a patient was actively listening while performing patient education?
- Which type of scenario requires active listening skills?
- Putting blood tubing into a pump.
- Watching an EKG monitor.
- Performing a pain assessment.
- What techniques show others you are actively listening?
- Reading a document while being talked to.
- Making eye contact.
- Making noises while someone is talking.
Communication Transmission Threads
Communication in nursing occurs multiple times a day between a wide range of communication threads. The type of communication through non-verbal, verbal, and written communication produced and received, must be effectively performed. Success and implementation are heavily dependent on the communication between the nurse and the communication thread.
Nurse-Nurse
Communication among nurses is continuous throughout a shift while working within a team environment. Whether it is us passing our documentation on to another nurse for review or vice versa, there is consistent communicative flow of all variants (non-verbal, verbal, and written) between the team in order to provide care for patients.
Nurse-Ancillary Staff
Your team members will vary depending on your nursing career setting, but some items will remain consistently important despite wherever you are. We must provide clear verbal communication when delegating or reporting critical information from the nurse to ancillary staff participating in patient, client, or resident care.
Charge Nurse-Team
When stepping into a charge nurse role, there will always be unexpected tasks, staff conflicts, or emergent situations. In this position, you will be taking all the communication skills you have acquired and putting them into practice at an all-time high. As the charge nurse, you will be viewed as a leader, meaning that you are a role model for your fellow team members. Now, in addition to producing and receiving communication effectively, you will now be identifying poor communication and assisting with its correction.
Nurse-Patient
The nurse-to-patient communication thread is one of the ultimate and most important exchanges in the nursing profession. Patients need us, so we must be able to keep consistent and effective communication flow with them because any assessment, report, and administration of medication is contingent upon it.
Nurse-Family
The thread between the nurse and the patient’s family can be the foundation for your nurse-to-patient communication and its effectiveness. The family could be the responsible party or guardian for your patient and could potentially serve as your sole historian for patient information if the patient is unable to communicate at the time of data collection. Ensuring that the family is aware of and understands discharge instructions can further help them to recognize any potential signs or symptoms that could result in calling a physician or visiting the emergency room in the future.

Self Quiz
Ask yourself...
- Which of the following is a beneficial way to ensure effective communication throughout multiple threads?
- One to one conversation.
- Reviewing a policy.
- Bedside report.
Barriers & Improvements to Communication
Barriers of communication in nursing happen frequently and are sometimes out of our control. These barriers include:
Language Barriers
Utilizing available resources for language barriers through interpreter staff members or interpretation devices can ensure effective communication pathways between two individuals.
Cultural Differences
Identification of cultural differences during admission and cultural awareness will allow for effective communication management throughout each culture you are presented with.
Patient Acuity, Staffing Levels, Time Constraints
Patient acuity, staffing levels, and time constraints can be improved by utilizing staff huddles and working together with administration in order to overcome conflicts.
Emergent Situations
Emergent situations that arise during your shift can be relieved through adequate knowledge of the policies and procedures and by performing debriefs after the situation resolves. Debriefings hold valuable insight into reflections of the emergent situations we face as nurses, especially on communication performance.
In each thread and form of communication in nursing, we must remember the following items to receive information. While producing communication, we must always be clear, concise, and accurate with the correct corresponding tone when expressed to others. When we are receiving the information, we must ensure we are understanding, investigating, and acting according to the communication presented to us. Utilizing various communication platforms, including emails, boards, and group messaging apps, can help to assist in ensuring education is received.
Benefits of Effective Communication in Nursing
When we achieve effective and therapeutic communication between both our team and patients, it will create opportunities for enhancements throughout our practice. Fostering a unity of teamwork with co-workers will increase satisfaction and reduce burnout rates. Reduced health care costs through reduced readmissions or emergency room visits will be established by successful patient education and understanding. Our quality of patient care will be heavily influenced by the nursing communication threads created through their care.
Nursing Ethics
Introduction
Ethics is an important aspect of all professions, but in this case, we are going to touch on its role in nursing. From the beginning, Florence Nightingale was a strong advocate and initiated nursing ethics and morals. For the 19th consecutive year, nursing has been ranked number one by the Gallup Poll as the most honest and ethical profession (1). The designation creates a larger responsibility to understand the American Nurses Association (ANA) Code of Ethics and how to apply to practice. Daily, nurses face ethical challenges and are confronted with situations with competing values and interests (2). How do we identify the issues? How do we respond to them? To understand our responsibilities as nurses, one must be aware of the details and applications of the ANA Code of Ethics with Interpretive Statements that give voice to nursing’s social mandate (3).
History
Did nursing exist before Nightingale? Yes, but not in an organized fashion, as the formalization of an ethical model began in the mid-1800s with Nightingale. Prior to her development of a formal training program, nursing was thought to be disreputable, and many persons providing caregiving services were prostitutes. Nightingale was the first to instill morals and ethics into education and practice. In 1889, the Trained Nurse and Hospital Review journal was published, including a six-part series on ethics (3).
Following, in 1893, the Nightingale Pledge was written by Listra Gretter to be used at the Farrand Training School for Nurses in Detroit, Michigan (4). The Pledge is as follows:
“I solemnly pledge myself before God and in the presence of this assembly, to pass my life in purity and to practice my profession faithfully. I will abstain from whatever is deleterious and mischievous and will not take or knowingly administer any harmful drug. I will do all in my power to maintain and elevate the standard of my profession and will hold in confidence all personal matters committed to my keeping and all family affairs coming to my knowledge in the practice of my calling. With loyalty will I endeavor to aid the physician in his work and devote myself to the welfare of those committed to my care.” (4)
The Pledge was written 128 years ago; the changes and challenges in nursing over these years are immeasurable.
Professional Ethics
Each profession has its own board with specific rules of ethical standards and principles; these standards and principles include honesty, respect, adherence to the law, avoidance of harm, integrity, and accountability. The specifics may differ per profession, but the basics are the same.
Nursing Ethics, Principles and Values
Although nothing had yet been formalized, the idea of ethics in nursing began to spread during the early 1900s. The ANA developed the first Code of Ethics in 1950, and did not revise it until 2015. The principles of ethics rely on several terms, defined as follows:
Autonomy
This can be as simple as listening to a patients’ individual rights for self-determination, including informed consent and patient choices. How this is viewed depends on the situation (5). It is important to note, in cases of endangering or harming others, for example, through communicable diseases or acts of violence, people lose this basic right (5).
Beneficence
This term refers to doing good and is part of the Nightingale Pledge and the Hippocratic Oath. Showing acts of kindness and facilitating wellbeing are great examples. However, it is important to understand that we as nurses, may think that we know what is best for our patient, but it is never a guarantee if they will agree with us; this is referred to as paternalism (5).
Justice
This is including the principle that covers normative aspects that are often discussed in terms of solidarity and reciprocity. Fair distribution of resources and care is an important aspect of this principle (5).
Non-Maleficence
This term almost directly translates to ‘do no harm,’ and can be part of confidentiality or other acts of care that can involve possible negligence. Additionally, it is used in end-of-life situations and decisions of care with terminally or critically ill patients (5).
Fidelity
This is the basic principle of keeping your word, and can be included in providing safe, quality care (5). If you tell a patient that you will be back to check on their pain level, and you in fact, do check back, that is fidelity – you have kept your promise.
Veracity
This term requires that you be truthful, accurate, and loyal to not only your patients and their families, but your co-workers as well. Are we telling our patients the truth? Are we holding back information about their conditions? Things to think about include pain medication and dosages (5). Placebos are an example of veracity.
Accountability
This is your responsibility of judgment and actions. To whom are you accountable? Examples include yourself, your family, colleagues, employer, patient, and the nursing board. One must take responsibility for their own actions (5). The following are components of accountability:
- Obligation: a duty that usually comes with consequences.
- Willingness: accepted by choice or without reluctance.
- Intent: the purpose that accompanies the plan.
- Ownership: having power or control over something.
- Commitment: a feeling of being emotionally compelled (5)
When examining nursing ethics, one must consider that the profession has three entry levels: diploma, Associate’s, and Baccalaureate degrees. This can affect what each nurse learns about, including values and ethics as well their real-life application.

Self Quiz
Ask yourself...
- When did ethics begin to develop in nursing?
- How do you define ethics?
- What are the six principles of ethics?
- How do you view patient autonomy?
- Do you think the different entry levels for nursing make a difference in ethics?
Foundations of Nursing Ethics
Nightingale was the first to teach ethics in nursing and set strict codes for those under her supervision; today, the ANA Code of Ethics serves as a concise statement of ethical obligations and duties of every person that enters into the profession.
The first three provisions of the ANA Code of Ethics describe the most fundamental values and commitments a nurse must make. The following three include boundaries of duty and loyalty, and the last three demonstrate aspects of duties beyond individual patient encounters.
Values are an important provision that remind us as individuals that we all have morals. As young children, we begin developing these values as we developmentally progress and learn from our families. What happens when your personal values are different from the values of the profession? This can also be a part of spiritual, ethnic, and cultural differences (5).
The Worldview is inclusive of ethical and moral discussions, as well as dilemmas for nurses around the world and primarily focuses on four elements: people, practice, profession, and co-workers (6). The International Council of Nurses (ICN) is more directed toward the Worldview. Not all are included in the ANA Code of Ethics.
An interesting factor to note is that the ICN Worldview focuses on co-worker relationships: “Nurse bullying occurs in almost all care settings and units, from the patient floor to the executive suite. In fact, 60% of nurse managers, directors, and executives in one 2018 study4 said they experienced bullying in the workplace, and 26% considered the bullying “severe” (7). Workplace intimidation is any intimidating or disruptive behavior that interferes with effective healthcare communication and threatens patient safety; it is often categorized as horizontal or relational aggression. Improving how management addressed such issues in nursing may be critical not only for staff turnover, but for patient outcomes.
There is some reluctance to specify the sorts of behavior that will not be tolerated, but effective anti-bullying practices must include a statement of exactly what constitutes bullying. From an ethical perspective, the acceptance of nurses who “eat their young” should no longer be tolerated.

Self Quiz
Ask yourself...
- What is the background of the ANA Code of Ethics?
- Have you read the ANA Code of Ethics?
- Evaluate and review horizontal aggression in the workplace. Have you experienced it?
- How does your personal culture and background affect your practice?
- What workplace behaviors should not be tolerated?
Application
As patient advocates, nurses work as part of an interdisciplinary team to provide patient care. Nursing ethics have kept pace with the advancement of the profession to include a patient-centered focus rather than a physician-centered focus. Due to its main focus of providing care, nursing ethics are often different than medical ethics; and it is important for us to understand the differences.
As we discuss application, one must take into consideration the workforce of nurses today. In many facilities, nursing staff may encompass at least three and maybe even four generations. This also applies to our patients. Those generations are identified as follows:
Traditionalists or Silent Generations (1922- 1946):
- Respect authority, are hardworking, and are sacrificial for their work.
- Many have delayed retirement (8).
Baby Boomers (1946-1964):
- Possess a belief that workers must pay their dues, are a workaholic, and typically rely on traditional learning styles (8).
Generation X (1965-1977):
- Independent, a skeptic of authority, and self-reliant (8).
Generation Y (1978-1991):
- Team-oriented, tech-savvy, entrepreneurial, and has a desire to receive feedback (8).
Generation Z (1992-2010):
- Tech savvy, understand the power of text and social media. (8)
No matter what generation you fall into, it is important to understand the different personality and learning styles of everyone.
A prime example of the generational learning styles differing and potential issues that may arise is the usage of electronic health/medical records (EMR) and various other health information technologies that are often incorporated into daily nursing practice. Nurses that come from older generations may struggle with these more, as they have experienced its transition and had to adapt.
Following, as the prevalence of social networking platforms continue to rise, it is important for nurses to understand the ethics of social media. Issues of privacy confidentiality and anonymity are ethical concerns when mixing personal and professional information on a social media platform; it is also important to note that most healthcare facilities have strict policies regarding social media.
End-of-Life
End-of-life issues are filled with nursing ethics and dilemmas. If the advanced directive is not clear, family issues and other complications trigger many of the ethical principles. Self – determination (the right to stop or refuse treatment) is complicated, the patient may not always have their wishes on paper, and often, families often do not want to let go. Nurses are the backbone of allowing the patient’s wishes to be known. It is important that nurses know that they can request an ethics committee review for their patients if they feel their wishes are being violated.
Additionally, physician-assisted suicide can be extraordinarily complex issue. For both the Hippocratic Oath and the Nightingale Pledge, there are ethical issues. Currently, the following states have made physician-assisted suicide legal: California, Colorado, Hawaii, Maine, New Jersey, Oregon, Montana, The District of Columbia, and Washington (9). With the ever-expanding ability to both prolong and end life, nurses must be cognizant and prepared for all repercussions associated with life and death situations (10).
With recent societal and technological advancements in science and medicine, choices involving both life and death are seeming to become more complicated. As a result of this worldwide controversy in healthcare, many nurses nation-wide are now forced to deal with this ethical dilemma head on (10). There are and will be many debates as to the ethical issues involved in physician -assisted suicide and something on the forefront for nursing to consider.

Self Quiz
Ask yourself...
- Evaluate your work environment and the differences in generations.
- Think about what ethical dilemmas you face daily.
- Has technology increased the ethical dilemmas in your practice?
- Do you know how to access your facilities ethic committee?
- What are your thoughts on physician-assisted euthanasia?
The ANA Code of Ethics
The ANA Code of Ethics serves to guide nurses in maintaining ethical standards and in ethical decision-making. Additionally, it outlines the obligations nurses must have for their patients and the nursing profession. The provisions focus on the following as stated by Lockwood (11):
Respect for Human Dignity
The nurse must show respect for the individual and consider multiple factors (belief systems, gender/sexual identification, values, right to self-determination, and support systems) when planning and providing care. The nurse ensures patients are fully informed and prepared to make decisions about their healthcare and to carry out advance healthcare planning.
Commitment to Patients
The nurse must always remember that the primary responsibility is to the patient and help resolve conflicts between the patient and others and avoid conflicts of interest or breach of professional boundaries.
Protection of Patients’ Rights
The nurse must be aware of legal and moral responsibilities related to the patients’ rights to privacy and confidentiality (as outlined by HIPAA regulations) and research participation.
Accountability
The nurse bears primary responsibility for the care of the patient and must practice according to the Code of Ethics and the state nurse practice act and any regulations or standards of care that apply to nursing and healthcare.
Professional Growth
The nurse must strive always to promote health, safety and wellbeing of self and others. The nurse must, in all circumstances, maintain personal integrity and report violations of moral standards. The nurse has a right to refuse to participate in actions or decisions that are morally objectionable but cannot do so if this refusal is based on personal biases against others rather than legitimate moral concerns.
Improvement of Healthcare Environment
The nurse must recognize that some virtues are expected of nurses, including those associated with wisdom, honesty, and caring for others, and that the nurse has ethical obligations toward others. The nurse is also responsible for creating and sustaining a moral working environment.
Advancement of the Profession
The nurse must contribute to the profession through practicing within accepted standards, engaging in scholarly activities, and carrying out or applying research while ensuring the rights of the patients are protected.
Health Promotion Efforts
The nurse recognizes that health is a universal right for all individuals and collaborates with others to improve general health and reduce disparities. The nurse remains sensitive to cultural diversity and acts against human rights violations, such as genocide, and other situations that may endanger human rights and access to care.
Participation in Goals of the Profession
The nurse must promote and share the values of the profession and take action to ensure that social justice is central to the profession of nursing and healthcare.
Conclusion
In conclusion, nurses face ethical dilemmas in practice almost every day, which is why it is so valuable for nurses to understand the philosophy of nursing ethics and its application in practice.
A Nurse’s Guide: How to Deal with Difficult Patients
Introduction
Being in the business of caring for people when they are at their worst means we often come face-to-face with patients amid emotional outbursts of anger. We can improve patient outcomes and our work-life satisfaction by putting the abilities to understand anger, learn and become aware of what goes on in others’ brains when they are upset, and adopt optimal techniques for handling these tough situations under our belt. Learning how to deal with difficult patients and being able to resolve conflict in a positive manner is one of the most valuable skills a nurse can possess.

Self Quiz
Ask yourself...
- Think of an interaction you’ve had with a patient who was angry.
- What was the outcome?
- Was it positive, or could it have gone better?
Consider Anger
Depending on your personal life, you will likely have your own opinion about anger as an emotion. Generally, it does not feel good to experience it in ourselves, nor is it pleasant to be around others who are feeling this way. Becoming angry is a part of being human, and as a healthcare professional, we must learn more about it so we are aware of how to deal with difficult patients. Perhaps approaching this from a philosophical standpoint will further help us to see beyond our patient’s immediate anger and we can work to develop a plan to resolve the conflict.
Anger as a Motivator
First off, anger can be motivating.
Oftentimes, when we perceive that there is a problem that is causing harm or injustice – whether it is affecting ourselves, a patient, the barista at the corner coffee shop, the planet, whatever – it is often anger that pushes us to act. As a very basic (and optimistic) example, a patient might be angry about being stuck in the hospital. Optimally, the experience will bother them enough to want to follow all of the steps their physician provides them so that they do not have to be readmitted.
Catharsis
For some, the act of being angry can be cathartic. For example, when we feel angry and begin to shout or slam a door, it is actually a way of releasing that built up, negative energy. Some people achieve catharsis and release their anger in productive ways, such as exercising, talking with a friend or therapist, journaling, or cleaning. Once you have completed the action and released the anger that you had, you slowly begin to calm down (1).
If we don’t release this energy over long periods of time, it can unfortunately cause physical harm. Anger increases heart rate, blood pressure (think MI or CVA), blood sugar, and intraocular pressure; lowers our immune function and increases incidents of cancer; affects the digestive system; decreases bone density, and can be the cause of headaches and migraines. Being angry also negatively impacts our short-term memory as well as the ability to make rational decisions (2). Applying therapeutic techniques can be a beneficial method of how to deal with difficult patients, as this can provide the opportunity to help them release some of the pent-up emotion they have before it causes physical harm.
Control
When learning how to deal with difficult patients, we must consider the relationship anger has with control. When a person is in our care, there is undoubtedly at least one major thing going on with them that they cannot control; otherwise, they would be at home. Being in a hospital setting removes all of the controlled variables that the patient has been accustomed to from their daily life (i.e. foods, who they come in contact with and at what time, etc.) and a common response to this change is anger in an attempt to regain control of the situation (1).
Stress & Trauma
There is a strong correlation between people who carry a lot of anger inside of them and stressful life events, particularly childhood trauma such as neglect and physical abuse. There’s also an association between anger and psychiatric disorders such as bipolar disorder and borderline personality disorder. This is not surprising since many people with these and other psychiatric disorders experienced extreme stress and trauma in their youth (3).
I find that keeping these tidbits of information about anger in mind helps me with how to deal with difficult patients and allows me to maintain my own composure.
Explore Your Thoughts/Feelings/Opinions/Triggers
Self-awareness is extremely important when learning how to deal with difficult patients. Allowing ourselves to be aware of our own experiences, feelings, and triggers because can dictate how we respond to others in heated situations. For example, suppose you are someone who grew up in a household where you frequently experienced violence — in that case, you might respond in an unexpected, unhelpful, and unprofessional way when exposed to angry behavior from others, such as shouting back. On the flip side, perhaps you grew up in a household where there was little to no conflict and you are unsure of how to properly respond when someone behaves angrily towards you. Maybe you have been judged harshly for your feelings and/or resulting actions, and consequently, judge others the same in turn.
Oftentimes we aren’t aware of our own tendencies until we step back and intentionally evaluate them. Considering your own experiences, thoughts, judgments, and things that trigger you can help you to become aware of why you react to situations the way that you do. You’ll then be more prepared to respond in a deliberate way when you next find yourself in a scenario with a disgruntled patient.

Self Quiz
Ask yourself...
- Have you ever gotten so upset that you made a bad decision?
- Has anger ever motivated you?
- What is your opinion of anger? How do you respond to others when they are angry?
- Think of at least three benefits of getting anger out.
Common Practice
“Calm down!” and, “It’s not okay to yell!” yelled the nurse. We’ve all heard the countless ways healthcare professionals respond when figuring out how to deal with difficult patients who are angry. Maybe we have even found ourselves yelling similar statements as well, and that’s okay – we are all human, and being yelled at can be very triggering, Don’t be too hard on yourself, evaluate how you should respond next time and prepare for it as best as you can because dealing with difficult patients is inevitable.
Often, clinicians become triggered – in other words, we get angry or irritated ourselves when confronted with an angry patient. If we aren’t mindful of our own tendencies and subsequently give in to that trigger, we inadvertently make what’s going on with the patient about ourselves when the patient is the one who needs our care. How is it helpful if we become upset as well? When learning how to deal with difficult patients, keep in mind that by responding with anger or with words that are seeking to control, the patient will miss an opportunity to release their pent-up, intense energy which can result in physical harm.
I am reminded of a time when my daughter was an infant. She always had a terrible time facing backward in her car seat. We were riding with a friend of mine and her six-year-old son when my daughter began to cry. The young boy covered his ears, saying, “Why does she have to be so loud?” My friend’s golden response was, “I know, honey, it’s no fun, but think how much worse it must be for her.”
Even though this scenario is quite different from a healthcare environment, I think those same words whenever I hear one of my patients yelling or are upset about something. All I want to do is cover my ears, but by thinking of how much worse it must be for them, I’m able to avoid making it about me.
Distraction
Another common approach to dealing with difficult patients during an angry episode by utilizing distraction techniques. There are times when this application is going to be the best choice, particularly, when dealing with patients who are cognitively impaired (4). However, there are other instances where this technique may come off as insulting with otherwise oriented people and could exacerbate the issue.
An example of an appropriate time to utilize this technique would be when dealing with a patient who has dementia and gets increasingly (and repeatedly) worked up over her belief that her loved one – who hasn’t seen the patient in recent history – is stealing from her. In this case, distraction might be the only way to calm her down.
Giving Advice
I work in a psychiatric setting, and when I was new to my position, I learned first-hand one technique that was not effective.
A 40-year-old, physically tall and sturdy male patient became so upset that he started punching our walls. Staff intervened and ending up having to take him down to the carpet for everyone’s safety. Other than his increase in rate and depth of breathing, he was lying quietly, prone on the ground. I kept a safe distance and asked if he was alright: he didn’t respond. I wasn’t sure what to do or say. I was new, undoubtedly nervous, and hadn’t yet learned the value of what one of our psychiatrists refers to as “therapeutic silence.” I had learned in the past from my education and own personal experiences that breathing techniques were calming, so I tried saying, “it’s okay, just breathe.”
Subsequently, he began yelling at me. He was saying not to tell him what to do, that he hated me, and to go away. By suggesting something to him in that intense moment, he took offense. If I’m honest with myself, if I were upset and someone had said something similar to me, it might not have gone over much better.
Threatening
Although this should only be used when absolutely necessary, nurses must be able to learn and understand how to deal with difficult patients through utilizing threatening tactics. Where I work, some patients simply live for the three smokes a day that they’re allowed. An example of this threatening tactic sounds something along the lines of, “if you don’t do what I say, you’re not going to get your cigarette.” Please note that this approach should not be utilized all the time, but in some cases, it can seem like the only way to get through to your difficult patients. However, keep in mind that it is a way of trying to control the other person and is also a missed opportunity to increase trust between the patient and the nurse.

Self Quiz
Ask yourself...
- Can you think of other ways of handling patients who are angry?
- What techniques have you employed?
- How effective have they been?
Benefits of Learning How to Deal with Difficult Patients When They are Angry
As caregivers, we experience more job satisfaction when we can adequately learn to care for people who are angry. Imagine how rewarding it is to successfully manage situations and achieve positive outcomes for our patients that could’ve gone badly otherwise. Not only that but, we potentially run the risk of losing our jobs if we don’t learn this essential skill (see Case Study #2 below). Rapport increases when appropriately utilized techniques are applied in practice because they foster trust and show respect for what the patient has to say (8).
For patients, these situations serve as great opportunities for them to release some of their anger. If we can be facilitators, assisting them to come to a more even-keeled place, they will undoubtedly experience better outcomes. Additionally, a situation involving a an angry patient can become dangerous quickly, so it is critical that we learn these skills for our own safety, and that of our patients.

Self Quiz
Ask yourself...
- Can you think of other benefits?
- Can you think of a time when you experienced first-hand or observed a situation involving a patient who was angry become worse because of how it was handled?
Anatomy Review
The amygdalae are a couple of bunches of neurons found deep in each temporal lobe that play an important role in our emotions, including triggering the fight or flight response (5). The hypothalamus is near the base of the brain right under the thalamus, and is attached to the pituitary gland (6). Among many other things, it’s responsible for controlling the secretion of hormones from the pituitary gland, which is located behind the nose (7). Finally, our adrenal glands sit on top of our kidneys and put out different kinds of hormones, particularly, stress hormones (2).
The Hormone Cascade
Something triggers us (i.e. we’ve just sat down to chart, and the call light goes off for what seems like the hundredth time, and we haven’t eaten or used the bathroom all day). Our amygdalae, like canaries in a coal mine, sound the alarm by signaling the hypothalamus and release a corticotropin-releasing hormone — causing the pituitary gland to release adrenocorticotropic hormone. This chain of hormone releases tells the adrenals to drop big stress bombs: adrenaline, noradrenaline, and cortisol (2).
When there’s too much cortisol, increased calcium is allowed to get into our neurons, which can end up leading them to die. Our prefrontal cortex (PFC) and hippocampus suffer the most from this unfortunate outcome. The function of the PFC becomes suppressed, which affects our ability to have good judgment. For example, saying something hurtful or that you do not mean to someone you care about during an argument. Following, when neurons die in the hippocampus, this is where our memories are stored. So if it’s not working well, our short-term memory and ability to store new ones are affected most (2).
The presence of too much cortisol will also result in a lack of serotonin – the happiness neurotransmitter. With less serotonin, we feel more sensitive to pain, anger, increase in aggression, and more prone to depression (2).
Consider every time you’ve ever tried to reason with a person who was already upset. How did it go? Did they immediately come to see the error of their ways? I can think of several occasions where a patient was so enraged about something that fixing whatever the issue was did nothing to quell the tirade. When trying to figure out how to deal with difficult patients, understanding what is going on in their brain during these episodes of rage can help us to make sense of it all and how to plan a deliberate, appropriate, and effective way to resolve the conflict.

Self Quiz
Ask yourself...
- Have you ever experienced being so angry that you experienced an amygdala hijack?
- If so, would you have called yourself “reasonable” when you were in that state?
- Consider the last time you dealt with someone who was angry in light of the above cascade of events. Does it make more sense now (if you weren’t already aware of what happens)?
Tips for Handling Patients When They are Angry
Beyond this lesson, you will find several publications that discuss in-depth how to manage de-escalation during potentially dangerous situations. De-escalation involves maintaining a calm demeanor and avoiding attempts to control the patient. As a result, they feel respected, and the trust between the two of you builds. Every person and situation is different, so a certain amount of intuition is also essential in order to creatively develop solutions (9).
Safety First
Since we now know that during escalated, angry situations, our patient’s brains are not exactly functioning at full capacity so try your best to expect the unexpected. One moment, a patient can seem like the calmest, and most collected person in the world — then they get triggered, and who knows what could happen?
With this in mind, the first thing we always have to consider is safety – for ourselves, the patient, and others nearby. Here are some recommendations for keeping everyone as safe as possible:
- Be aware of what’s around you and your patient. Are there things that could be thrown or used as a weapon? Do you wear necklaces or long earrings that can be pulled?
- Always maintain a safe distance. If you don’t feel safe, get to safety. It’s okay to walk away from a situation if you feel that you are in danger, but never turn your back.
- Bring a co-worker if you need to go into an angry patient’s room – never go alone.
- Observe for signs of aggression. If your patient exhibits balled fists, getting too close to you, pacing, tense shoulders, glaring, tense jaw, facial flushing, shouting, or heavy breathing, be prepared.
- Try to keep the area clear of others who might be put in danger or exacerbate the situation. This might be a challenge when you’re focused on engaging with your patient. However, it is helpful if you and your coworkers are all on the same page. Consider working with management to train everyone to be on alert for potentially dangerous situations with patients and their loved ones.
What to Say or Not to Say
When I’m upset, the thing that helps me the most is feeling like I am being heard. For my patients, I have found that listening is one of the tactics that works best, but remember that in some instances, patients may have a hard time listening to others because they may become triggered. If that occurs, it can become difficult to maintain a calm demeanor that is necessary for de-escalating tense situations. If we can find a way to keep the focus on the other patient (who is coming to us with the issue), we can become better listeners and remain calm.
Listening is a skill that not everyone excels in but it can make a huge difference when figuring out how to deal with difficult patients.
Tips to improve listening skills:
- Do not interrupt.
- Give your full attention rather than getting distracted by inner thoughts or environmental stimuli.
- Repeat back what you’ve heard to affirm you got it right.
- Ask related questions to show you’re concerned and want to deepen your understanding.
- Convey a sense of empathy by using your body language, and making brief statements like, “That’s understandable.”
Since there is not a specific prescription or solution for dealing with all angry patients, we need to stay tuned and be creative to reach a mutually beneficial goal. By staying calm and truly listening, we’re better able to understand what is going on so that we can attempt to remedy whatever the problem is when the time is right. After listening, affirming, and giving the patient time to calm down, we can begin to work toward a solution. For example, I might say, “I hear that you’re upset about what happened, and that’s totally understandable. What can I do for you right now to help?” By approaching the situation this way, it affirms that I heard the patient, respect their feelings, and genuinely want to help them. When learning how to deal with difficult patients, this is an extremely valuable tool to possess.
Additionally, body language is extremely important – it conveys so much! Simple adjustments like squaring ourselves to whomever we’re listening to and conveying accurate facial expressions depending on the situation ensures in the patient that we are giving them our full, undivided attention and that we truly care about what they’re saying.
Boundaries
A word about maintaining boundaries; these are key! Just because I aim to listen and convey kindness actively does not mean that I am a pushover, and that my patients will get everything they want.
For example, as nurses, we all know that we often don’t have the time (or energy) to have deep, confiding conversations with each and every patient. However, being kind can be done swiftly, and without caving to demands. A simple “no” can be said in a respectful manner. For example, we can briefly say in a kind tone, “I know it’s frustrating, and I get it, but unfortunately, I can’t talk with you right now because I’m in the middle of passing meds. Can we talk in half an hour or so?”
There are also times when we have to set boundaries because we can see that we can’t do any good in that moment. I have a patient who shouts so loudly when she’s upset that I have to cover my ears for fear of damage! Sometimes she’s able to convey her feelings in a way that I can actively listen to, and these times seem to be helpful for her, but when she can’t, I give her boundaries. I say, “*Pema, I want to listen to you, but you’re hurting my ears.” If she’s unable to control her volume, I gently remove myself, stating, “I hear that you’re having a hard time, but I have sensitive ears, and your shouting is hurting them. Let’s talk later.”
We all have to figure out where our boundaries lie. If you are someone who gets triggered by the angry behavior of others, you might do best to excuse yourself early on to catch your breath and ask someone else to help with the situation. If you are triggered, it’ll be tough for you to make the best decisions when figuring out how to deal with difficult patients.
Not Taking Things Personally
As nurses, I am sure we have all learned early on to not take anything personally, especially when dealing with difficult patients. In most cases, an angry patient yelling in your face will not be your fault. Remember, we are not responsible for other’s feelings and reactions; those are about them, not us. As we mentioned previously, we are all probably guilty of saying something that we didn’t mean when we were upset and we wish we would have given it a second thought, and in some scenarios, this could be the case. However, there are other instances where the angry behavior of a patient then results in them wanting to speak with your manager regardless of whatever the reason is being your fault or not.
It’s helpful to recognize when a behavioral response is not in proportion to what actually happened because this can be a clue into possible long-standing issues. Of course, knowing all of this doesn’t mean we shouldn’t always do our best, but it can help us refrain from beating ourselves up too much when our best seems to fall short.
Attempt to be aware of the things we have reviewed here so you can effectively handle and devise a solution on how to deal with difficult patients who are angry. Bear in mind how challenging it can be not to have control, especially during situations where we are unable to make rational decisions.
What to Do if You’re the One to Lose Your Cool
As we discussed earlier, when we become triggered, our prefrontal cortexes (PFCs) don’t work properly, and that is when our decision-making becomes poor. The good news is that, since we know what’s going on in our brain, we can work on reactivating that precious (and potentially life-saving) PFC. At first, we might not be able to look at ourselves clearly until after an episode, but we can learn to recognize the signs of becoming triggered by examining what happened. Once we can do that in real-time, we can intentionally work toward becoming calm again.
Take Care of Yourself
Nurses are used to taking care of others all the time, but what about themselves? This is crucial. You must take care of and be kind to yourself. Our best is different every moment of every day, and that’s all just part of being human. Some days, we might be having a tough time, struggling with any number of things, just like our patients. Our temper might be shorter, our tone may be a little more on edge, but rather than judging ourselves too harshly, we should recognize our own humanity and just do our best.

Self Quiz
Ask yourself...
- What kind of training have you received where you work on safety?
- If none, is there an opportunity for growth in this area?
- List three things that help calm you if/when you get upset.
- Think of when you’re listening to a patient. What do you do to show you’re actively listening?
- What are some phrases you would feel comfortable saying that would show that you care and are actively engaged? For example, “That sounds frustrating.”
Case Studies
Case Study #1
A 46-year-old female patient received an IM injection in her right glute this morning. It is afternoon shift change, and she is complaining that her right hip has been hurting since receiving this injection. She has repeatedly been approaching the nurse’s station about this issue. The off-going day shift nurse calls over his shoulder as he’s frantically attempting to finish documenting, “I’ve already assessed you, and I don’t see anything wrong. I talked to the doctor, and he ordered Ibuprofen which you received. I have let her know that you would like to speak with her; you’ll have to wait until she rounds next.”
The patient begins yelling, stating, “None of you care about me! My doctor doesn’t care about me! Otherwise, she wouldn’t make me get these injections that hurt me!” The evening shift nurse arrives, sees that the patient she knew from the evening before is upset and that the off-going nurse is busy. The evening nurse steps behind the station desk so that there’s a barrier between her and the patient (in case she becomes more agitated and aggressive) and turns to face the patient with a concerned expression in place. “*Fiona, I see that you’re upset. How can I help?” The nurse listens, not interrupting the patient as she relays her issue. At a natural lull in the patient’s speech, the nurse responds, “It sounds like you’re frustrated about this situation. I get it; that’s totally understandable.” The patient goes on to express her feelings of not being cared for by the staff or the doctor, tearfully raising her voice. The nurse looks at the patient with concern and considers the possibility that this woman might have some history of not being cared for. She continues to listen as the patient goes on venting. Eventually, the patient shouts one last time, turns away, and stomps down the hall to her room. An hour later, she returns looking tired, a little embarrassed, but calm, and apologizes then thanks the nurse for listening.
The above is based on an episode that I experienced about a year ago. This patient is still at the facility I work at, and I have not seen any such outbursts from her since. I can also attest to experiencing very good rapport with her since this event.
Case Study #2
A 70-year-old male patient rings the call bell. The nurse answers and the patient shouts loud enough to be heard without the aid of the speaker, “Get over here! You people are useless! Because of you, I’m swimming in a puddle of my own urine.” The nurse responds, “Okay, but you don’t have to be so rude.” She slams the phone down, muttering expletives to herself. She takes her time, finishing up what she was working on, still ruminating over the patient, while he gets increasingly upset.
She walks into the patient’s room, and she sees that he’s standing next to his bed, naked, leaning precariously on his IV pole. She says, “What are you doing? You’re going to fall.” The patient responds, “Well, you’re not doing your job!” “I shouldn’t have to deal with this,” the nurse mutters under her breath as she begins to gather the soiled sheets. The nurse, whose back is turned to the patient, doesn’t see that his face has gone the color of a bag of packed RBCs, his eyes are bulging, and his knuckles are white as they grip the IV pole. The patient attempts to use the pole as a weapon to hurt the nurse but ends up slipping on his urine-wet feet, striking his head against the wall, resulting in a concussion. He files an official complaint regarding the nurse, considers suing her for damages, and gets written up for the second time. Next time, she’ll be out of a job.

Self Quiz
Ask yourself...
-
Think of one example from your practice that you have experienced or observed that went well and another that did not. What were the key elements that you think made the difference?
Conclusion
People get angry – it’s just a fact of our existence. Some, unfortunately, misbehave when they feel anger whether it’s out of frustration, stress, feelings of loss of control, or unmanaged old triggers coming to the surface. As nurses, we often have to figure out how to deal with difficult patients while being able to remain calm and composed. By understanding more about people who experience excessive anger and learning to apply the techniques discussed in this course, you will be able to form flexible and creative solutions that can result in making the best out of very challenging situations.
How to Reduce New Nurse Turnover
Introduction
Before graduating from nursing school, I was accepted into a six-month program to train for the cardiac medical ICU. I took the initial competencies and classroom trainings and was assigned an experienced preceptor on the ICU floor. My preceptor very quickly informed me that I was bothering patients by being too attentive. Soon after, she let the rest of my colleagues know that she would be retiring because the job had become dangerous now that so many new nurses were joining our unit. That was just the first week on the floor.
Throughout my first year of nursing, I was anxiety-ridden and questioned staying. Despite my rough start, I made it through and have enjoyed over 20 years as a nurse; however, many of my classmates not only resigned before their first year was over, but a few left nursing altogether.
During my tenure as a nurse, I have learned that incivility and bullying are all too common. In a 2017 report, Nurses Eat Their Young: A Novel Bullying Educational Program for Student Nurses, the author references research that indicated bullying and incivility among peers occurred to at least 30% of nurses. Among new nurses, 73% reported experiencing incivility or bullying in their first month in practice (3). Below, I have listed just one example from a nursing blog that showcases how bullying and incivility haven’t changed much from my experiences with it over 20 years ago.
“I have an orientation with a nurse educator. And she’s kind of a bully; I have to say. She puts me in uncomfortable situations. She dismisses anything I say; she gives me ridiculous and menial assignments while excluding me from doing tasks with her directly related to my new role, that I could learn better. Yet, she talks over and over about the things I already know. She gives me contradicting information. At this point, my self-esteem has got even lower than when I started” (15).
In response: “This is the issue I have with the profession… more than likely, they pounced on you because you’re new, and they’re asserting their dominance/reinforcing cliques (them vs. us). Either behavior making for toxic workplace culture… And I say this from experience” (15).

Self Quiz
Ask yourself...
- What was your own experience as a new graduate nurse, and what impact does that have on your career today?
New Graduate Nurse Turnover Rates
The overall nurse turnover rate has increased 5% over the last decade; however, the new graduate nurse turnover rate alone has increased that much in just four years (4,10).
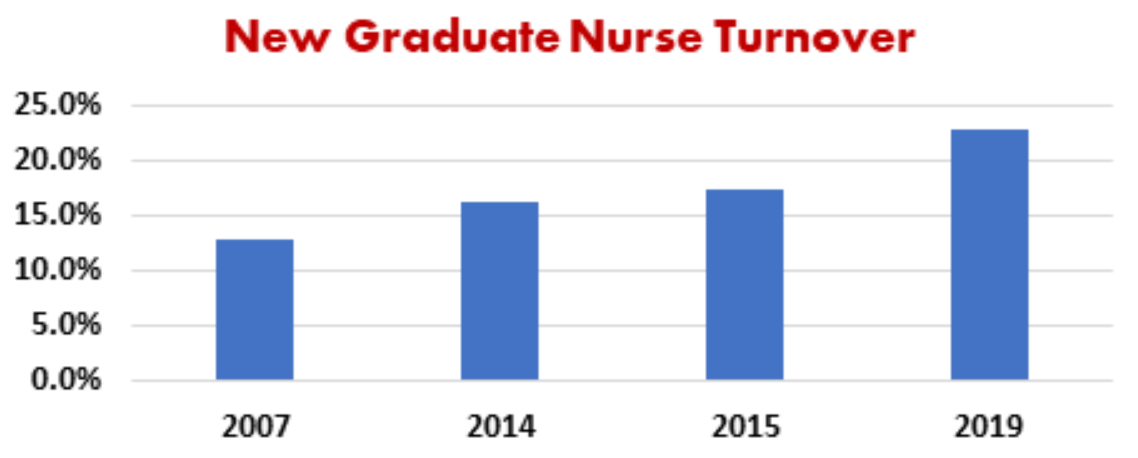
After only their first year, the new nurses’ turnover rates continue to rise until almost half of them have either left their departments or nursing in its entirety (4).
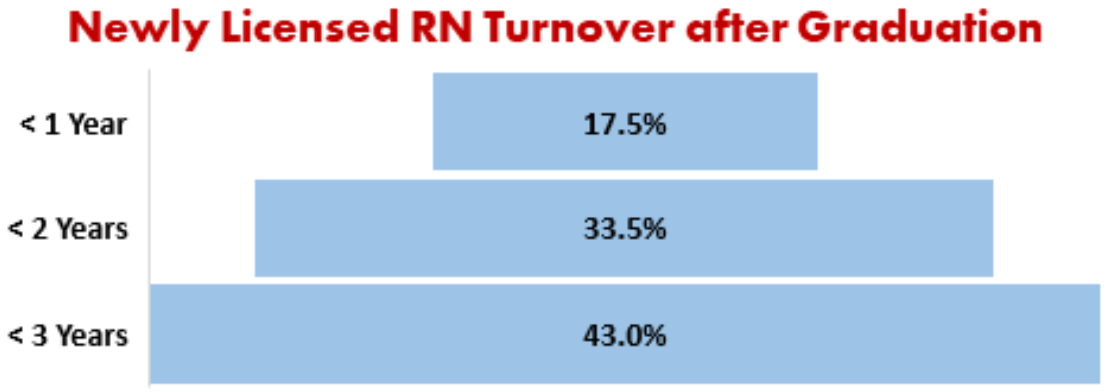
Of further concern, in a 2020 The Nursing Solutions, Inc. nurse turnover report, they project a significant increase in nurse deficits as a result of the COVID-19 pandemic (11). The report surveyed over 1000 nurses, and the results determined that 96% of respondents showed signs of burnout, and 56% reported they would be leaving either direct patient care specialties or the nursing profession in its entirety through resignation or retirement (11).

Self Quiz
Ask yourself...
- Thinking of your fellow nurse graduates, what percentage do you predict will leave the nursing field and why?
Reasons for New Nurse Turnover
There are various reasons as to why new nurses are leaving the field and contributing to the increase in nurse turnover; however, there is one trend that has remained consistent for decades. The initial peer-to-peer and orientation/precepting relationships established can truly make or break a new nurse.
Researchers often correlate the incivility and bullying of nurses to a lacking collegial or peer-to-peer relationships. Many nurses who cite bullying or incivility in the workplace often claim they are leaving the job due to their preceptors. For nurses with years of experience under our belt, since collegial relationships are a primary driver of turnover and retention for new nurses, we must assume responsibility for our part as peers and work to reduce the continuous rise in new nurse turnover.

Self Quiz
Ask yourself...
- How meaningful are collegial relationships to you at this point in your career versus your first year in nursing?
Effects of New Graduate Nurse Turnover
There is no argument that the cost of increasing new nurse turnover rates has all-encompassing effects. New graduates may lack the full in-person experience of nursing and are not fully prepared to meet all practice-based standards; this requires more hands-on training and nursing experience. Nurse-sensitive outcomes, including falls, pressure ulcers, and nosocomial infections, suffer in the hands of continual learners (8). Higher rates of mortality have been linked to higher turnover rates (6).
Although the training and precepting of new nurses is necessary on all accounts, it can be challenging and demanding for the already short-staffed and stressed nurses with experience. With the combination of continuous training and increased workload demands, patient satisfaction and community trust in the organization begins to erode (8). Employee morale for both new and experienced nurses suffer due to the increase in expectations and workload (6). In high patient volume scenarios, training and precepting may take the back burner to cover patient census, which leads to missed learning opportunities and perpetuates a lack of clinical expertise as the new nurses move forward in their career. This lack of knowledge can lead to intolerance or ridicule by the better-prepared nurse and possible disciplinary action for the up-and-coming nurse.
The cost for recruitment and hiring of new nurses along with the costs for filling vacated positions with travel and contracted nurses are estimated to be 5% of a hospital’s annual budget (6). Since labor cost accounts for up to 50% of the budget, productivity remains a top priority despite increased workload demands; leaving staff and administrators disconnected in determining actions that may positively affect patient and staff satisfaction.
I understand that these are not new statistics, and few nurses would knowingly jeopardize their safety and patient care. However, the fact remains that the culture persists, and the new nurses that receive this type of treatment pass it on. As part of the change process, our first action may start with recalling what it was like for us as new graduate nurses.

Self Quiz
Ask yourself...
- Do you have examples, either positive or negative, of nursing turnover affecting your unit’s patient care and satisfaction?
Challenges for New Nurses
New nurses typically receive the “short end of the stick” when joining an organization, as the employer will most likely fill them in the neediest shifts, including nights, rotating, weekend, and holiday shifts. While this is not ideal for the new nurse, we accept it as part of the dues that they must make.
The Nursing Times Workforce reports that many nurses come into the field with anxiety (12). When I first became a nurse, I, too, experienced anxiety. I ended up mentioning my feelings to one of my colleagues who supportively advised me that my anxiety was a good sign; it indicated that I would be a more cautious nurse. I took comfort in this, but as I now reflect, I do not believe it to be the whole truth.
Cautiousness is a characteristic in and of itself, and although it can present as anxiety, the feeling of dread can be resolved with positive experiences that lead to confidence. The anxiety that I felt, and what new nurses typically describe tends to be fear-based, whether it is real or perceived. On top of this, up to 18% of hospital nurses report symptoms of depression which is double the general population (12).
When you couple this anxiety with incivility, bullying, or general lack of support, it becomes easy to see how the rates of new nurse turnover continue to rise. Below are just a few examples of sub-Reddit postings from current new nurses and the challenges they are facing with their mental health:
“My anxiety/depression has worsened to the point where I can’t sleep the night before I work and I’m constantly overthinking or worrying about my job. I’m miserable and on edge, and I feel like this just can’t be worth it. I was looking to move out of bedside nursing and was curious what my options are, especially with less than a year of experience” (17).
“Hello! I work dayshift med surg. My biggest issue is when I get home, I’m anxious. I think about my shift and worry I forgot something. I get nervous that when I come back the next day, the night nurse will pick me apart because I missed things. I sleep terribly in between shifts. I just always worry about what I did. Need advice. Does this happen to anyone else? Best tips to not worry?” (18).
“I am fresh off orientation and am beginning to suffer from anxiety attacks while at home. I wake up in sweats thinking about my unit. I feel weak because my peers are not feeling these same things. It’s disheartening knowing that I worked my butt off in nursing school to end up feeling like crap every day. I don’t know what to do. I hear it gets better, but now I’m questioning if I should’ve ever become a nurse. Caring for people is all I wanted to do, but maybe I wasn’t cut out for this” (19).

Self Quiz
Ask yourself...
- What advice would you give to support other nurses with anxiety or depression?
Bullying and Incivility
The American Nurses Association defines bullying as “repeated, unwanted harmful actions intended to humiliate, offend and cause distress in the recipient” (2).
As previously mentioned, bullying is a prevalent issue in the field of nursing, and there are many speculations as to why it is common for nurses to bully their colleagues. One being, that nurses tend to garner less respect from other disciplines such as doctors or pharmacists. Other reasons may be due to the natural competitiveness of the healthcare professions, or the inability to control most of their work environment and patient outcomes so overstepping and bullying fellow nurses is their only constant form of control or normalcy (7). Common examples of bullying in nursing include verbal abuse and harassment.
Incivility is a form of bullying, except the intent is more ambiguous; so much so that it often goes unrecognized and can even be disguised as a learning opportunity. Incivility often gets ignored by management out of empathy for the experienced nurses being under stress, or out of fear of confronting a trained nurse and causing them to leave – contributing to the chronic short-staffing in healthcare facilities. Nurses who experience this behavior tend to pass it on as a rite of passage, leading to the perpetuation of nurses’ culture “eating their young” (4). Some signs of the behavior include (15):
| Behavior | Examples |
| Eye Rolling | Response to a new RN’s request for assistance. |
| Disrespect | Intentionally not informing a new nurse of best practice or other information relevant to the organization. |
| Gossip | Overstating or exaggerating a new nurse’s shortcomings, faux pas, or errors to co-workers. |
| Blaming | Naming a new nurse as part of an incident report. |
| Rudeness | Informing a new nurse of the burden you are undertaking by precepting. |
| Unfriendiness | Refusal to greet or include a new nurse in social conversation. |
| Ignoring | Being unavailable to the new nurse. A survey of new graduates revealed 27.5% of nurses reported preceptors were rarely or never available (4). |

Self Quiz
Ask yourself...
- Have you experienced or witnessed acts of incivility or bullying against yourself or your peers?
- Thinking back, how has your specific nursing unit handled acts of incivility or bullying?
How to Support New Nurses
In the article, “4 Compelling Theories Why Nurses ‘Eat Their Young,’” Maura Hohman says, “The number one most powerful behavior is for the witness to speak up and support the person who is being targeted (7).” While this is easier said than done, there is evidence that developing a script to confront individuals when this occurs can be useful (3). At the very least, it shows support for the new nurse. Other essential activities to improve instances of incivility and bullying in the workplace while reducing the new nurse turnover rate include:
- Becoming familiar with your organization’s policies and procedures on incivility, bullying, and workplace violence. If your organization does not address this issue, it is your responsibility to recommend and participate in developing the needed policies. The American Nurses Association’s “Nurses Bill of Rights” is a useful reference (2).
- Advocating for education on recognizing and preventing incivility and bullying through your professional association, nursing schools, and organization (3).
- Practicing “Just Culture.” Unless the same error occurs repeatedly, the new nurse’s intent is your primary tool for guiding consequences. Never blame or name if unnecessary when reporting an error. Limit your information to the facts only. Mistakes are to be investigated for the root cause, which is rarely person-related, and almost always process, culture, and system design.
- Learning opportunities are just that; don’t chastise. If you are angry or irritated, consider your real intent. Learning opportunities are rarely cultivated in an emotional environment.
- Being a supporter of other nurses.
- American Nurses Association’s civility best practices include:
- Strive to develop clear verbal and non-verbal communication. Be direct when needed and always respectful.
- Treat others with kindness, as well as collegiality, and always dignity.
- Be mindful that every individual suffers, and your actions and words affect others.
- Avoid gossip and call it out when you hear it from others.
- Rely on facts; never speculate and be slow to conclude until evidence has been discovered.
- Be collaborative and share information when appropriate.
- Offer assistance and accept appropriate refusal graciously.
- Be aware, accountable, and responsible for your actions.
- Speak directly to the person with whom you have an issue.
- Seek other points of view, perspectives, and experiences. Listen to others with interest.
- Apologize when necessary.

Self Quiz
Ask yourself...
- Are you knowledgeable of your hospital’s policies on incivility, bullying, and workplace violence?
- Do your hospital policies align with the American Nurses Association?
Recognizing Burnout and Opportunities to Reduce New Nurse Turnover
Since a lack of collegial relationships and peer-to-peer support are contributing factors leading to burnout and turnover, there is a lot you can do to prevent both. Besides following the steps above, recognizing burnout and signs of pending turnover are essential to quick intervention. The symptoms of burnout are noticeable in this at-risk population who may begin:
- Not participating in social activities.
- Not participating in improvement activities or opposing workplace changes.
- Calling off shifts, especially when they have been highly dependable.
- Arriving late for their shift.
- Taking excessive breaks or leaving the floor for support personnel activities when not necessary.
- Presenting with a negative attitude or being insensitive to patients and families.
- Verbalizing overwhelming anxiety or dread at coming to work (14).
If you notice these behaviors, it is time to intervene in order to avoid nurse turnover. One of the best strategies is to become a mentor or friend to them. Having someone to vent to helps relieve stress, and your engagement will go a long way in building positive experiences for the new nurse (14). If you have an employee assistance program, refer them to your human resources depart and inform them of all the available resources that you know of. Employee assistance programs offer confidential counseling for many personal and work-related concerns. If the situation persists, get your manager involved. It is their job to know and offer additional supportive resources to their employees.

Self Quiz
Ask yourself...
- Can you think of a nurse who your outreach may support?
Conclusion
There are many contributing factors to new nurse turnover. It is the responsibility of healthcare organizations, professional associations, and nursing educators to work together to improve the barriers that are causing this consistent increase in nurse turnover rates that are further contributing to the global nursing shortage. In order to deliver quality patient care, improve health outcomes, and increase workplace satisfaction we need nurses.
No matter how much experience you have, there are ways you can contribute to ending this increasing new nurse turnover, and that is by becoming an advocate and mentor for them. Speak up to support a new nurse and become familiar with your organization’s incivility, bullying, and workplace violence policies.
References + Disclaimer
Pediatric Abusive Head Trauma – Kentucky
- Cabinet for Health and Family Services. (2019). Child abuse and neglect annual report of child fatalities and near fatalities. Retrieved from: https://chfs.ky.gov/agencies/dcbs/dpp/cpb/Documents/reportofchildfatalitiesandnearfatalities.pdf
- Centers for Disease Control. (2020). Child abuse and neglect prevention strategies. Retrieved from: https://www.cdc.gov/violenceprevention/childabuseandneglect/prevention.html
- Healthy Children. (2020). Abusive head trauma: how to protect your baby. Retrieved from: https://www.healthychildren.org/English/safety-prevention/at-home/Pages/Abusive-Head-Trauma-Shaken-Baby-Syndrome.aspx
- Joyce, T. and Huecker, M. R. (2020). Pediatric abusive head trauma. Stat Pearls. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK499836/
- Kentucky Cabinet for Health and Family Services. (2017) Child protection branch. Retrieved from: https://chfs.ky.gov/agencies/dcbs/dpp/cpb/Pages/default.aspx
- Kids Health. (2019). Abusive head trauma (shaken baby syndrome). Retrieved from: https://kidshealth.org/en/parents/shaken.html
- National Center on Shaken Baby Syndrome. (n. d.). Facts and info. Retrieved from: https://www.dontshake.org/learn-more
- National Center on Shaken Baby Syndrome. (n. d.). The period of PURPLE crying. Retrieved from: https://www.dontshake.org/purple-crying
- Rape Abuse and Incest National Network. (2020). Mandatory reporting requirements: children Kentucky. Retrieved from: https://apps.rainn.org/policy/policy-state-laws-export.cfm?state=Kentucky&group=4
Kentucky Implicit Bias
- Adams, C, Thomas, SP (2018). Alternative prenatal care interventions to alleviate Black–White maternal/infant health disparities. Sociology Compass, 12:e12549. https://doi.org/10.1111/soc4.12549
- Association of American Medical Colleges. (2019). Diversity in medicine: facts and figures 2019. AAMC. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018
- Buchmueller, T. C. and Levy, H. G. (2020). The ACA’s Impact on racial and ethnic disparities in health insurance coverage and access to care. Health Affairs, 39(3). https://doi.org/10.1377/hlthaff.2019.01394
- Cameron, K. A., Song, J., Manheim, L. M., & Dunlop, D. D. (2010). Gender disparities in health and healthcare use among older adults. Journal of women’s health, 19(9), 1643–1650. https://doi.org/10.1089/jwh.2009.1701
- Centers for Disease Control and Prevention. (September 23, 2021). Data and statistics about ADHD. CDC.https://www.cdc.gov/ncbddd/adhd/data.html#:~:text=Boys%20are%20more%20likely%20to,12.9%25%20compared%20to%205.6%25).
- Centers for Disease Control and Prevention. (April 22, 2021). The tuskegee timeline. Retrieved from: https://www.cdc.gov/tuskegee/timeline.htm
- FitzGerald, C., and Hurst, S. (2017). Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics, 18, 19. https://doi.org/10.1186/s12910-017-0179-8
- Gothreau, C. and Acreneaux, J. (2019). The effect of implicit and explicit sexism on reproductive rights attitudes. Temple University. https://sites.temple.edu/cgothreau/files/2019/09/Sexism-Paper.pdf
- Guevara, J. P., Wade, R., and Aysola, J. (2021). Racial and ethnic diversity in medical schools- why aren’t we there yet? The New England Journal of Medicine, 385(1732-1734) DOI: 10.1056/NEJMp2105578
- Hamel, L., Firth, J., Hoff, T., Kates, J., Levine, S., and Dawson, L. (September 25, 2014). HIV/AIDS in the lives of gay and bisexual men in the united states. Kaiser Family Foundation.
- Healthy People 2020. (2020). Data 2020. HealthyPeople.gov https://www.healthypeople.gov/2020/data-search/
- Institute for Policy Research. (May 18, 2018). Communication between healthcare providers and LGBTQ youth. Northwestern. https://www.ipr.northwestern.edu/news/2018/infographic-mustanski-lgbtq-patient-communication.html
- Johns Hopkins Medicine. (n.d.). The legacy of Henrietta Lacks. Retrieved from: https://www.hopkinsmedicine.org/henriettalacks/
- Kathawa, C. A., & Arora, K. S. (2020). Implicit Bias in Counseling for Permanent Contraception: Historical Context and Recommendations for Counseling. Health equity, 4(1), 326–329. https://doi.org/10.1089/heq.2020.0025
- Krahn, G. L., Walker, D. K., & Correa-De-Araujo, R. (2015). Persons with disabilities as an unrecognized health disparity population. American journal of public health, 105 Suppl 2(Suppl 2), S198–S206. https://doi.org/10.2105/AJPH.2014.302182
- Levine DA, Gross AL, Briceño EM, et al. Association between blood pressure and later-life cognition among black and white individuals. JAMA Neurology, 7(7):810–819. doi:10.1001/jamaneurol.2020.0568
- Mude, W., Oguoma, V. M., Nyanhanda, T., Mwanri, L., & Njue, C. (2021). Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: A systematic review and meta-analysis. Journal of global health, 11, 05015. https://doi.org/10.7189/jogh.11.05015
- Regis College. (n.d.). Why ageism in healthcare is a growing concern. Regis College. https://online.regiscollege.edu/blog/why-ageism-in-health-care-is-a-growing-concern/
- Saluja, B. and Bryant, Z. (2021). How implicit bias contributes to racial disparities in maternal morbidity and mortality in the united states. Journal of Women’s Health, 30(2). https://doi.org/10.1089/jwh.2020.8874
- Tasca, C., Rapetti, M., Carta, M. G., & Fadda, B. (2012). Women and hysteria in the history of mental health. Clinical practice and epidemiology in mental health : CP & EMH, 8, 110–119. https://doi.org/10.2174/1745017901208010110
- Wall L. L. (2006). The medical ethics of Dr J Marion Sims: a fresh look at the historical record. Journal of medical ethics, 32(6), 346–350. https://doi.org/10.1136/jme.2005.012559
Kentucky Suicide Prevention
- Accardi, R., Sanchez, C., Zisook, S., Hoffman, L., Davidson, J.E. (2020). Sustainability and Outcomes of a Suicide Prevention Program for Nurses. Worldviews on Evidence-Based Nursing, 2020, 17(1), 24-31. Retrieved on July 5, 2022 from https://library.smh.com/sites/default/files/Sustainability%20and%20Outcomes%20of%20a%20Suicide%20prevention%20program%20for%20nurses.pdf.
- American Nurses Association (n.d.). Nurse Suicide Prevention/Resilience. Retrieved on June 21, 2022 from https://www.nursingworld.org/practice-policy/nurse-suicide-prevention/.
- American Foundation for Suicide Prevention (n.d.). Suicide prevention resources. Retrieved on July 6, 2022 from https://afsp.org/suicide-prevention-resources.
- Association of Clinicians for the Underserved (n.d.). Preventing Suicide in Providers and Staff: Organizational Approaches. Retrieved on July 5, 2022 from https://clinicians.org/programs/suicide-safer-care/preventing-suicide-in-providers-and-staff/.
- Bennington-Castro, J. (2021). How to Help Combat Rising Suicide Rates Among Care Providers. Retrieved on July 6, 2022 from https://huddle.florence-health.com/discover/content/article/how-to-help-combat-rising-suicide-rates-among-care-providers.
- Centers for Disease Control and Prevention (2022). Suicide Prevention: Fact About Suicide. Retrieved on June 21, 2022 from https://www.cdc.gov/suicide/facts/index.html.
- Davidson, J.E. et al. (2021). Nurse suicide prevention starts with crisis intervention: Make a plan to protect yourself and your colleagues. Retrieved on July 5, 2022 from https://www.myamericannurse.com/nurse-suicide-prevention-starts-with-crisis-intervention/.
- Davidson, J. E., Proudfoot, J., Lee, K., Terterian, G., Zisook, S. (2020). A Longitudinal Analysis of Nurse Suicide in the United States (2055-2016) With Recommendations for Action. Worldviews On Evidence-Based Nursing, 17(1), 6-15. Retrieved on June 21, 2022 from https://doi.org/10.1111/wvn.12419.
- Dowd, M. (2021). Ethical Responsibilities of Nurses. Retrieved on July 6, 2022 from https://work.chron.com/ethical-responsibilities-nurses-10778.html.
- Fischer, D. (2018). Preventing Nurse Suicides. Oncology Nursing News. Retrieved on July 6, 2022 from https://www.oncnursingnews.com/view/preventing-nurse-suicides.
- Fischer, L. (2022). Nurses Consider Suicide More Than Other US Workers. Oncology Nursing News. Retrieved on June 30, 2022 from https://www.oncnursingnews.com/view/nurses-consider-suicide-more-than-other-us-workers.
- Folmer, K., Howard, M.C. (2022). What Employers Need to Know About Suicide Prevention. Harvard Business Review. Retrieved on July 6, 2022 from https://hbr.org/2022/01/what-employers-need-to-know-about-suicide-prevention.
- Haskell, B. (2022). Suicide assessment and follow-up care: Nursing skills and implications. Retrieved on July 5, 2022 from https://www.myamericannurse.com/suicide-assessment-and-follow-up-care/.
- Hutton, A. (2015). Saving lives by preventing suicide. Retrieved on July 5, 2022 from https://www.myamericannurse.com/saving-lives-preventing-suicide/.
- Marfell, J., Norrod, P., Walmsley, L. (2022). Oped: Nurse Suicide Awareness. University of Kentucky College of Nursing. Retrieved on July 5, 2022 from https://www.uky.edu/nursing/about-us/news/oped-nurse-suicide-awareness#:~:text=In%20Kentucky%2C%20approximately%2058%20nurses,continuing%20education%20in%20suicide%20prevention.
- Merenda, L. (2019). How one program may help prevent suicide in nurses. Retrieved on July 6, 2022 from https://www.wolterskluwer.com/en/expert-insights/how-one-program-may-help-prevent-suicide-in-nurses.
- National Institute of Mental Health (n.d.). Ask Suicide-Screening Questions (ASQ) Toolkit. Retrieved on July 6, 2022 from https://www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials/index.shtml.
- Rizzo, L.H. (2018). Suicide among nurses: What we don’t know might hurt us: Research, prevention programs, and open discussion are required to reduce nurse suicide. Retrieved on July 6, 2022 from https://www.myamericannurse.com/suicide-among-nurses-might-hurt-us/.
Opioid Abuse
- https://www.deamuseum.org/ccp/opium/history.html
- https://americanaddictioncenters.org/opiates/controlled-substances
- https://www.cdc.gov/injury/features/prescription-drug-overdose/index.html
- https://www.cdc.gov/drugoverdose/prescribing/guideline.html
- https://www.cdc.gov/drugoverdose/pdf/guidelines_at-a-glance-a.pdf
- https://www.cdc.gov/drugoverdose/pdf/pdo_checklist-a.pdf
- APA Webster, Lynn R. MD Risk Factors for Opioid-Use Disorder and Overdose, Anesthesia & Analgesia: November 2017 – Volume 125 – Issue 5 – p 1741-1748 doi: 10.1213/ANE.0000000000002496
- Andrea L. Nicol, Robert W. Hurley, Honorio T. Benzon Anesth Analg. Author manuscript; available in PMC 2018 Nov 1. Published in final edited form as: Anesth Analg. 2017 Nov; 125(5): 1682–1703. doi: 10.1213/ANE.0000000000002426
- Mart van Laar, Joseph V Pergolizzi, Jr, Hans-Ulrich Mellinghoff, Ignacio Morón Merchante, Srinivas Nalamachu, Joanne O’Brien, Serge Perrot, Robert B Raffa
- Open Rheumatol J. 2012; 6: 320–330. Published online 2012 Dec 13. doi: 10.2174/1874312901206010320
- Pak, S. C., Micalos, P. S., Maria, S. J., & Lord, B. (2015). Nonpharmacological interventions for pain management in paramedicine and the emergency setting: a review of the literature. Evidence-based complementary and alternative medicine: eCAM, 2015, 873039. https://doi.org/10.1155/2015/873039
- Safer D. J. (2019). Overprescribed Medications for US Adults: Four Major Examples. Journal of clinical medicine research, 11(9), 617–622. https://doi.org/10.14740/jocmr3906
- Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2020 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553166/
- https://www.cdc.gov/drugoverdose/training/oud/accessible/index.html
LGBTQ Cultural Competence
- Waisel DB. Vulnerable populations in healthcare. Curr Opin Anesthesiol. 2013;26(2):186–92.
- Freid VM, Bernstein AB, Bush MA. Multiple chronic conditions among adults aged 45 and over: Trends over the past 10 years. NCHS Data Brief. 2012;2012(100):1–8.
- Institute of Medicine. Collecting sexual orientation and gender identity data in electronic health records: workshop summary. Washington DC: National Academy of Sciences; 2013.
- Quinn GP, Sanchez JA, Sutton SK, Vadaparampil ST, Nguyen GT, Green BL, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA-Cancer J Clin. 2015;65(5):384–400
- Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953–60.
- Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific northwest. Am J Public Health. 2010;100(3):460–7.
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802–9.
- Bauermeister J, Eaton L, Stephenson R. A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among young men who have sex with men living in metro Detroit. Behav Med. 2016;42(3):197–204.
- Smalley KB, Warren JC, Barefoot KN. Differences in health risk behaviors across understudied LGBT subgroups. Health Psychol. 2016;35(2):103–14.
- Staats C, Capatosto K, Wright RA, Jackson VW. State of the science: Implicit bias review 2016. Columbus: Kirwan Institute.
- Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003-2010 National Health and nutrition examination surveys. Am J Public Health. 2013;103(10):1837–44.
- Remafedi G, French S, Story M, Resnick MD, Blum R. The relationship between suicide risk and sexual orientation: results of a population-based study. Am J Public Health. 1998;88(1):57–60.
- Charlton BM, Corliss HL, Missmer SA, Frazier AL, Rosario M, Kahn JA, et al. Reproductive health screening disparities and sexual orientation in a cohort study of U.S. adolescent and young adult females. J Adolesc Health. 2011;49(5):505–10.
- Matthews AK, Brandenburg DL, Johnson TP, Hughes TL. Correlates of underutilization of gynecological cancer screening among lesbian and heterosexual women. Prev Med. 2004;38(1):105–13.
- Tracy JK, Lydecker AD, Ireland L. Barriers to cervical Cancer screening among lesbians. J Women’s Health. 2010;19(2):229–37.
- Grossman AH, D’Augelli AR. Transgender youth: invisible and vulnerable. J Homosex. 2006;51(1):111–28.
- Krehely J. How to close the LGBT health disparities gap. Center for American Progress; 2009. p. 1–9.
- Buchmueller T, Carpenter CS. Disparities in health insurance coverage, access, and outcomes for individuals in same-sex versus different-sex relationships, 2000-2007. Am J Public Health. 2010;100(3):489–95.
- Heck JE, Sell RL, Gorin SS. Health care access among individuals involved in same-sex relationships. Am J Public Health. 2006;96(6):1111–8.
- Kamen C, Palesh O, Gerry AA, Andrykowski MA, Heckler C, Mohile S, et al. Disparities in health risk behavior and psychological distress among gay versus heterosexual male Cancer survivors. LGBT Health. 2014;1(2):86–U103.
- Legal L. When health care Isn’t caring: lambda Legal’s survey of discrimination against LGBT people and people with HIV. New York: Lamba Legal; 2010.
- Grant JM, Mottet LA, Tanis J. National Transgender Discrimination Survey Report on health and health care. Washington DC: National Center for Transgender Equality and National Gay and Lesbian Task Force; 2010.
- Shires DA, Jaffee K. Factors associated with health care discrimination experiences among a National Sample of female-to-male transgender individuals. Health Soc Work. 2015;40(2):134–41.
- Eliason MJ, Dibble SL, Robertson PA. Lesbian, gay, bisexual, and transgender (LGBT) physicians’ experiences in the workplace. J Homosex. 2011;58(10):1355–71.
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
- Mereish EH, Bradford JB. Intersecting identities and substance use problems: sexual orientation, gender, race, and lifetime substance use problems. J Stud Alcohol Drugs. 2014;75(1):179–88.
- Torres CG, Renfrew M, Kenst K, Tan-McGrory A, Betancourt JR, Lopez L. Improving transgender health by building safe clinical environments that promote existing resilience: results from a qualitative analysis of providers. BMC Pediatr. 2015; 15:187.
- Burke SE, Dovidio JF, Przedworski JM, Hardeman RR, Perry SP, Phelan SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. 2015;90(5):645–51.
- Sabin JA, Riskind RG, Nosek BA. Health care Providers’ implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. 2015;105(9):1831–41.
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–7.
- Wilson TD, Brekke N. Mental contamination and mental correction: unwanted influences on judgments and evaluation. Psychol Bull. 1994;116(1):117–42.
- Zestcott CA, Blair IV, Stone J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Process Interg. 2016;19(4):528–42.
- Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102(1):4–27.
- Van Ryn M, Saha S. Exploring unconscious bias in disparities research and medical education. JAMA. 2011;306(9):995–6.
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74(6):1464–80.
- Nosek BA, Riskind RG. Policy implications of implicit social cognition. Soc Issue Policy Rev. 2012;6(1):113–47.
- FitzGerald C, Hurst S. Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics. 2017;18(1):19.
- Shavers VL, Fagan P, Jones D, Klein WMP, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66.
- Chapman EN, Kaatz A, Carnes M. Physicians and implicit Bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–10.
- Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal treatment: Confronting racial and ethnic disparities in health care. Brian D. Smedley, Adrienne Y. Stith, and Alan R. Nelson, Editors; Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care; Board on Health Sciences Policy; Institute of Medicine. Washington, DC; 2003.
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41.
- Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. 2015;108(4):553–61.
- Khan A, Plummer D, Hussain R, Minichiello V. Does physician bias affect the quality of care they deliver? Evidence in the care of sexually transmitted infections. Sex Transm Infect. 2008;84(2):150–1.
- Morris, M., Cooper, R. L., Ramesh, A., Tabatabai, M., Arcury, T. A., Shinn, M., Im, W., Juarez, P., & Matthews-Juarez, P. (2019). Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC medical education, 19(1), 325. https://doi.org/10.1186/s12909-019-1727-3
- Human rights campaigns. Glossary of terms. Retrieved from https://www.hrc.org/resources/glossary-of-terms
- Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care for the Lesbian, Gay, Bisexual, and Transgender (LGBT) Community, a field guide. Joint Commission. Retrieved from https://www.jointcommission.org/ /media/enterprise/tjc/imported-resource assets/documents/lgbtfieldguide_web_linked_verpdf.pdf?db=web hash=1EC363A65C710BCD1D4E14ED120CB2
- Delivering culturally sensitive care to LGBTQI Patients. The Journal for nurse practitioners. Volume 13, issue 5 p342-347.
Effective Communication in Nursing
- Ethics. (2021). Retrieved from https://www.dictionary.com/browse/ethics
- ANA. (2021). Retrieved from Ethics and Human Rights: https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/
- Dugdale, D. C. (2020, January 12). Do-not-resuscitate order. Retrieved from MedlinePlus: https://medlineplus.gov/ency/patientinstructions/000473.htm
Nursing Ethics
- Gallup Poll finds nursing is most honest and ethical profession. (2021, January). Oakland University News,, . https://oakland.edu/oumagazine/news/nursing/2021/gallup-poll-finds-nursing-is-most-honest-ethical-profession
- Rushton, C. (2017, January). Why ethics?. John Hopkins Nursing. https://magazine.nursing.jhu.edu/2017/01/why-ethics/
- Fowler, M., “Nursing’s Code of Ethics, Social Ethics, and Social Policy,” Nurses at the Table: Nursing, Ethics, and Health Policy, special report, Hastings Center Report 46, no. 5 (2016): S9-S12. DOI: 10.1002/ h
- Florence Nightingale Pledge. (2010) https://nursing.vanderbilt.edu/news/florence-nightingale-pledge/#:~:text=I%20solemnly%20pledge%20myself%20before,knowingly%20administer%20any%20harmful%20drug
- Rich, K., & Betts, J. (). Ethical theories and approaches. Jones & Bartlett Learning.
- The ICN Code of Ethics for Nurses (2021). https://www.icn.ch/system/files/documents/2020-10/CoE_Version%20for%20Consultation_October%202020_EN.pdf
- Edmonton, C. & Zelonka, C. (2019). My own worse enemy: the nurse bullying epidemic. Nursing Administration Quarterly. July – September. 43(3). 274-279.
- Bell, J.A. ( 2013). Five generations in the nursing workforce. Journal for Nurses in Professional Development 29( 4 ) https://www.sgna.org/Portals/0/Bell_FiveGenerationsInTheNursingWorkforce_2013.pdf
- Should Euthanasia Or Physician Assisted Suicide Be Legal(2019). https://euthanasia.procon.org/
- Llamas, J. V. (2018, November). The moral and ethical dilemma of physician assisted suicide. Minority Nurse, (), . https://minoritynurse.com/the-moral-and-ethical-dilemma-of-physician-assisted-suicide/
- 11. Lockwood, W. (2020, April). Jurisprudence and nursing ethics. http://file:///D:/Ethics%20in%20Nursing/Jurisprudence.pdf
A Nurse’s Guide: How to Deal with Difficult Patients
- Ratson, M. (2017, March 09). The value of ANGER: 16 reasons it’s good to get angry. Retrieved February 17, 2021, from https://www.goodtherapy.org/blog/value-of-anger-16-reasons-its-good-to-get-angry-0313175
- National Institute for the Clinical Application of Behavioral Medication. (2020, August 28). How anger affects the brain and body [infographic]. Retrieved February 18, 2021, from https://www.nicabm.com/how-anger-affects-the-brain-and-body-infographic/
- Okuda, M., Picazo, J., Olfson, M., Hasin, D., Liu, S., Bernardi, S., & Blanco, C. (2015, April). Prevalence and correlates of anger in the community: Results from a national survey. Retrieved February 19, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4384185/
- Brooker, C. (2017, July). Communication with angry patients through de-escalation. Retrieved February 18, 2021, from https://www.elsevierclinicalskills.co.uk/SampleSkill/tabid/112/sid/1727/Default.aspx
- Moyer, N. (2019, April 22). Amygdala hijack: What it is, why it happens and how to make it stop. Retrieved February 18, 2021, from https://www.healthline.com/health/stress/amygdala-hijack#overview
- Seladi-Schulman, J. (2018, March 21). Hypothalamus: Anatomy, function, diagram, conditions, health tips. Retrieved February 18, 2021, from https://www.healthline.com/human-body-maps/hypothalamus
- Seladi-Schulman, J. (2018, June 11). Pituitary gland overview. Retrieved February 18, 2021, from https://www.healthline.com/health/human-body-maps/pituitary-gland
- Awdish, R., & Berry, L. (2017, October 13). The importance of making time to really listen to your patients. Retrieved February 24, 2021, from https://www.physicianleaders.org/news/the-importance-of-making-time-to-really-listen-to-your-patients#:~:text=Actively%20listening%20conveys%20respect%20for,to%20truly%20listen%20to%20patients
- Price, O., & Baker, J. (2012). Key components of de-escalation techniques: A thematic synthesis. Retrieved February 25, 2021, from https://www.researchgate.net/profile/Owen-Price-2/publication/221837683_Key_components_of_de-escalation_techniques_A_thematic_synthesis/links/5a1e8b21458515a4c3d1faa0/Key-components-of-de-escalation-techniques-A-thematic-synthesis.pdf
How to Reduce New Nurse Turnover
- American Association of Colleges of Nursing. (2020, September). Nursing Shortage. Retrieved March 2021, from aacnnursing.org: https://www.aacnnursing.org/news-information/fact-sheets/nursing-shortage
- American Nurses Association. (2015, July 22). Practice & Advocacy. Retrieved from incivility, bullying and workplace violence: https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/incivility-bullying-and-workplace-violence/
- Boesch, M. B. (2017). Nurses Eat Their Young”: A Novel Bullying Educational Program for Student Nurses . Journal of Nursing Education and Practice, 11-21.
- Brewer, C. D. (2007). Newly licensed RNs characteristics, work attitudes, and intentions to work. American Journal Of Nursing, 58-70.
- Curtin, L. S. (2020, August). Nurse turnover: Understand it reduce it. American Nurse Journal, 57-59. Retrieved from MyAmericanNurse.com: https://www.myamericannurse.com/wp-content/uploads/2020/08/an8-Turnover-728.pdf
- HealthStream. (2017, October 11). To improve healthcare outcomes, we must focus on turnover. Retrieved from The Healthcare and Administration Blog: https://www.healthstream.com/resources/blog/blog/2017/10/11/to-improve-healthcare-quality-outcomes-we-must-focus-on-turnover
- Hohman, M. (2019, June 13). 4 compelling theories why nurses “eat their young.” Retrieved from florence-health.com: florence-health.com/career/nurse_practitioner/4-compelling-theories-as-to-why-nurses-eat-their-young/
- Kerfoot, K. (2013, September 21). New nurse turnover and patient safety: What’s the problem? Retrieved from Patient Safety & Quality Healthcare: https://www.psqh.com/news/new-nurse-turnover-and-patient-safety-whats-the-problem/
- Lockhart, L. (2020, March/April). Strategies to reduce nursing turnover. Retrieved from Nursing Made Incredibly Easy!: https://journals.lww.com/nursingmadeincrediblyeasy/fulltext/2020/03000/strategies_to_reduce_nursing_turnover.10.aspx
- Nursing Solutions, Inc. (2019). 2019 National health care retention & RN staffing report. NSI Nursing Solutions, Inc.
- Nursing Solutions, Inc. (2021). 2021 RN labor market update. NSI Nusrsing Solutions, Inc.
- Nursing Times. (2019, September 02). Nurses support their young: From competitors to mentors. Retrieved from Nursing Times-Workforce: https://www.nursingtimes.net/news/workforce/nurses-support-young-competitors-mentors-02-09-2019/
- Nursing Times. (2019, September 02). Nursing Times-Mentors. Retrieved March 2021, from Nursing Times: https://www.nursingtimes.net/roles/mentors/advertising-feature-avoid-nurse-burnout-02-09-2019/
- [email protected]. (2010, June 15). Seven strategies to avoid burnout. Retrieved from Healthleaders: https://www.healthleadersmedia.com/nursing/seven-strategies-reduce-nurse-burnout/
- Schmidt, K. (2017, August 23). How to recognize and prevent bullying in nursing. Retrieved from Nurse.com: https://www.nurse.com/blog/2017/08/23/how-to-recognize-and-prevent-bullying-in-nursing/
- u/martianteen. (2021, March). Bullying at work: nursing. . Retrieved from Reddit: https://www.reddit.com/r/nursing/comments/lxah2z/bullying_at_work/
- u/phol10. (2021, March). New nurse dealing with new onset of anxiety (r/nursing, 2021) nursing. Retrieved from Reddit: https://www.reddit.com/r/nursing/comments/lvugdi/new_nurse_dealing_with_new_onset_of_anxiety/
- u/schwee. (2021, March). Looking to leave bedside nursing; nursing. Retrieved from Reddit: https://www.reddit.com/r/nursing/comments/lyw80s/looking_to_leave_bedside_nursing/
- u/tjgirl. (2021, March). Post shift anxiety: nursing. Retrieved from Reddit: https://www.reddit.com/r/nursing/comments/lvtmwz/post_shift_anxiety/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

