Course
The Relationship between Developmental Disabilities and Mental Health Issues
Course Highlights
- In this course we will learn about the relationship between mental health issues and developmental disabilities, and why it is important for nurses to be able differentiate the two.
- You’ll also learn the basics of the quandrants of care framework.
- You’ll leave this course with a understanding of how to effectively provide care for individuals that present mental health issues, developmental disabilities, or both.
About
Contact Hours Awarded: 1.5

Course By:
Amy L. White
MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Many times, healthcare workers and the direct support professional staff assisting individuals with both intellectual and developmental disabilities (IDD) fail to understand the differing characteristics of developmental disabilities and mental health issues. Even though they are two separate diagnoses, a correlation exists between the two disorders.
With the increasing number of mental health issues among individuals with developmental disabilities, it is sometimes difficult to differentiate the two. Unfortunately, it can be challenging to understand the defining characteristics of those with a developmental disability and those with mental illness. Oftentimes, it takes careful and timely observations to become aware that there is a defining relationship that exists among the two and that one affects the other. However, it is crucial that the differences are made clear so proper understanding, treatment options, and medical interventions can be made accurately in order for this special population to receive the care they need and deserve.
Justification of Knowledge
With the ever-increasing numbers of mental health disorders and those diagnosed with developmental disabilities, the facts surrounding these two issues can be confusing, inaccurate, and misunderstood.
Since both can occur simultaneously, making clear distinctions can often be challenging. Both diagnoses are important, and many times, those with developmental disabilities have concurring mental illness issues that are rarely recognized in mental health statistics, policy developments, education, training, and clinical practice (9).
In the past, the population of individuals with developmental disabilities was not nearly as “visible“ since these individuals were not a part of mainstream mental health due to the care that was received being offered in a different institutionalized setting. As institutions began to close and the emphasis on “community inclusion” became more popular, those with developmental disabilities were granted more access to medical, physical, and mental health care than other individuals without any developmental disabilities (9).
A disturbing report conducted in 2016 titled “Nowhere to Turn” revealed a four-year investigation regarding the care and treatment of adults with developmental disabilities, which revealed the following (9):
- Frequent emergency room visits
- Lengthy hospitalizations
- Incarceration
- Homelessness
- Family burnout
- Neglect
Even with mental health not being the primary focus of the investigation, the results made it clear that minimal to no identification of mental health issues can lead to various social and health problems among this population.
A national study of hospitalizations found that psychiatric hospitalizations accounted for almost half of the admissions involving those with developmental disabilities. Many of the individuals ranged in age from youth to young adults (9).
Many times, these individuals are treated by general medical providers or even those who specialize in mental health. Still, the issue evolves from these providers not feeling comfortable and being unfamiliar with how to effectively care for a population of individuals with developmental disabilities in conjunction with mental health issues (9).

Self Quiz
Ask yourself...
-
As a provider, caregiver, direct support professional, or health care personnel, what can we do to overcome the issues of these individuals with developmental disabilities not receiving the proper care and treatment?
We should be investing our efforts in improving screening procedures for mental health issues with a primary focus on early intervention, accurate diagnoses, and implementing efficient and accurate supports/treatments. As part of reaching these goals, it will be necessary for all those caring for individuals with developmental disabilities to become more knowledgeable about developmental diasbilities, proper care aspects, and mental health issues that are consistently present with these individuals. In doing so, these pract6ices will provide both the support and care needed to successfully care for those with developmental disabilities and mental illness.
Definitions of Developmental Disability, Mental Illness, and Community Inclusion
What is a Developmental Disability?
According to the Centers for Disease Control (CDC), developmental disabilities are a group of conditions due to an impairment in physical, learning, language, or behavioral areas. These conditions begin during the developmental period, may impact day-to-day functioning, and usually last throughout a person‘s lifetime (1). These individuals are typically diagnosed when a patient is younger than 18 years of age, and the diagnosis stays with the patient for a lifetime (5).
What is a Mental Health Issue?
Mental health issues and illnesses may not be lifelong but instead may serve as a temporary occurrence or occur in episodes but are not typically everlasting if treated appropriately. Mental illness or mental health issues can include mood disorders, anxiety disorders, and psychotic disorders that can change an individual‘s thought processes and perceptions (5). Many times, mental illness can also begin in early childhood or may sometimes not present until later as an adult.
What is Community Inclusion?
Community inclusion involves the idea that all people, regardless of their abilities or disabilities, should be able to fully engage in various community activities. Community inclusion provides those with developmental disabilities the opportunities to live and exist as a member of society while being recognized and valued for their uniqueness and abilities. The goal is for those with intellectual and developmental disabilities to be able to participate if able in the following (8):
- employment
- housing
- recreational activities
- leisure activities
- education
- peer support
One may ask if there are true benefits of implementing inclusion in communities. The answer is “yes,” and the following are some benefits and values of this principle.
Friendship skills, problem solving skills, increased self-image, respect for others, peer models, and a greater understanding of accepting differences in individuals with developmental disabilities are all evident when community inclusion is implemented.
Misunderstandings Among those with Developmental Disabilities and Mental Illness
To some, the following myths about developmental disabilities have been thought to be true (6):
- those with developmental disabilities are always intellectually disabled
- individuals with developmental disabilities should not live independently
- behaviors that are manifested due to developmental disabilities cannot be understood
- developmental disability is synonymous with mental illness
To some, mental illness has been thought to be the following (3):
- a form of intellectual or developmental disability
- a trait one is born with
- an indication that those with mental illness are a threat or should be considered dangerous
- a valid reason to be excluded and isolated from the community

Self Quiz
Ask yourself...
- What is the likelihood that individuals are misdiagnosed with a developmental disability or a mental health issue when it can be a combination of both or only one of them?
Due to the lack of knowledge and expertise of both developmental disabilities and mental health, it can make diagnosing individuals difficult and even inaccurate, which can then alter the effective means of treatment.
Correlation between Developmental Disability and Mental Health as an Aid in Dual Diagnosis
Individuals with developmental disabilities are more prone to develop mental health issues across their lifespan. In various studies, it has been found that psychotic disorders, mood disorders, anxiety disorders, and challenging behaviors are all increasingly seen in those with developmental disabilities (1). The Diagnostic and Statistical Manual of Mental Disorders (DSM) is used as the basis for diagnosing a mental health disorder and classification of each disorder that includes criteria for making a diagnosis.
As caregivers, healthcare personnel, family members, or medical experts caring for those with developmental disabilities, the relationship between disability and mental health issues can be extremely complex. The way mental health issues present themselves is unique and can change over time (1).
Biological, psychological, and social elements need to be assessed as these can contribute to the mental health of these individuals. Also, it is important to be mindful that the inner experience of a person with a developmental disability can be challenging to understand due to the individual having difficulty expressing his/her thoughts and feelings.
When behaviors increase in intensity but have been present with the individual for a long time, it is difficult to diagnose accurately. For example, if an individual always throws a plate on the floor to indicate he/she wants food, but has begun to throw the plate on the floor more forcefully and more frequently, and not just for food purposes, does this behavior change indicate that he/she has a new mental health problem, or could it possibly be a part of the same problem? Diagnosing mental health issues accurately in those with developmental disabilities involves various information from several sources and settings.
According to the National Coalitition on Dual Diagnosis, the impact of a dual diagnosis can have the following characteristics (1):
- Complicated medical and psychiatric needs, with services provided to the individual, but the service is frequently moved from one service to another, with many of the services not being beneficial to the individual
- Individuals with chronic medical and psychiatric problems that could have been easier to treat if caught earlier
- Over-medicated individuals because providers voice they are “better managed“ that way
- Failure of services due to service agencies feeling ill-equipped to provide adequate supports
- No support offered to help individuals manage life in the community which can lead to situations with law enforcement, jail, or being placed in psychiatric hospitals
- Often denied housing services because of their needs “being too complicated“. Life on the streets for this vulnerable group of individuals increases their risk of violence and exploitation
- Rejection by their family and individuals, leaving them without any support and are subject to homelessness
- Lost opportunities to be productive citizens due to failures in the system
- Out of control behaviors due to minimal to no help being offered, and families are unable to adequately provide the individual with the care that he/she needs

Self Quiz
Ask yourself...
-
Are we doing a sufficient job to ensure that the population of individuals with developmental disabilities and mental illness receive the proper health and support they need?
Unfortunately, health systems are working to improve in this area and to recognize the burden that is presented by mental health disorders along with those with developmental disabilities. There is a gap between the need for treatment, the active provisions for treatment, and the poor quality of care for those who actually receive treatment. These factors should encourage the importance of increased support, health, and awareness among this vulnerable population.
The Quadrant Framework (7)
In attempting to figure out the best diagnosis and treatment options for those with developmental disabilities and mental health issues, a framework was created that helped identify these individuals’ expertise (based on the severity level).
Initially, the framework was developed for individuals with a substance use problem and mental health issues only but has since been adapted and can be used for developmental disabilities and mental health concerns. While it is possible for individuals to transition back and forth among quadrants during various stages of treatment, the framework is useful in identifying the appropriate counsel for these individuals during a given category (1).
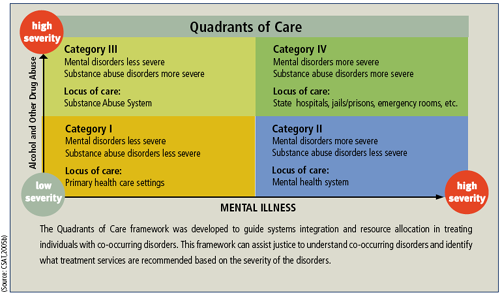
Category I – Less severe mental health disorder and less severe substance disorder
These individuals have low severity of substance use and mental disorders. These individuals can be treated in intermediate outpatient settings (relating to mental health or chemical dependency programs), with consultation between settings. Primary care settings may also be used with consultation from mental health and/or substance misuse treatment providers (7).
Category II – More severe mental health disorder and less severe substance disorder
These individuals are typically classified as a high priority with severe mental health disorders but with low severity in substance use disorders. These individuals ordinarily receive continuing care in the mental health system, are typically in full or partial remission, and may be a part of an intermediate–level mental health program (7).
Category III – Less severe mental health disorder and more severe substance disorder
These individuals have severe substance use disorders but have low or moderate level severity with mental health disorders. They are often treated in intermediate–level substance misuse treatment programs (7).
Category IV – More severe mental health disorder and more severe substance disorder
These individuals fall into two subgroups. One group includes those with serious mental illness who also have severe substance use disorders that are unstable in nature (7).
The other group includes individuals with severe and unstable substance use disorders in addition to severe and unstable behavioral health problems such as violence and the risk of suicide. These individuals require intensive, comprehensive, and integrated services for both their substance misuse and mental disorders. The treatment received can be specialized in programs such as state hospitals, jails, or other settings that provide acute care such as emergency rooms (7).

Self Quiz
Ask yourself...
- What is the concern if two sectors are not involved simultaeneously when dealing with the developmental disability and mental health aspect among individuals with both diagnoses?
It is necessary to have both sectors (those dealing with the developmental and/or intellectual disability and those dealing with the mental health aspect) for each to offer specialized knowledge in their area of expertise. The developmental sector can assist with planning issues such as the supports offered in the community and where to live, whereas the mental health sector can assist with the treatment of mental illness and recommended medications (1). Being connected is important to prevent the issues from becoming worse and unmanageable. If problems are addressed colloaboratively, the individuals are more likely to get better results with integrated services.
Treatments and Medical Interventions
To assist individuals with developmental disabilities and mental health issues, various treatment and medical modalities are used to provide the most effective outcomes. Over the past 25 years, much of the care for those with developmental disabilities has shifted from state hospitals to various community settings, which has increased the need for both medical and mental health services in the community. One of the greatest problems that has been noted with community settings is that these services are typically lacking the necessary training of both medical and psychiatric professionals.
A survey conducted by Werner and colleagues reported results that indicated that 90.2% of psychiatrists experience feelings of inadequacy and insufficient training to treat those with developmental disabilities (4).
Evidence suggests that if the problems of this population are addressed appropriately, the results can be positive, and progression instead of regression can be achieved in a collaborative manner (1).

Self Quiz
Ask yourself...
-
Many people voice that obtaining the proper treatment in a timely manner is an incredible challenge among this population. What are the major barriers to mental health treatment?
The greatest barriers include shortages of mental health workforce professionals, lack of anonymity when seeking treatment, a lack of competent care that reflects and understands different cultures, affordability of care, transportation to care sites, and a lack of or no desire to receive care.
Keys to effective treatment and management are (1):
- Correctly identifying the cause of the behavioral problems and addressing them appropriately is the first step among the management of patients with developmental and intellectual disabilities
- Accurate diagnosis based on team meetings and discussions
- Look for changes in baseline of both medical and behavioral issues
- Discuss the changes with those who know the individual best (family and Direct Support Professional staff)
- Rule out medical versus psychiatric issues
- Assess for regression in previous skills, speech, behavior, or normal activities
5 guiding principles to care for those with dual diagnosis (1):
- Individuals with dual diagnosis are still people FIRST with strengths as well as issues
- Mental health issues in individuals with developmental disabilities are common but under-identified
- Mental health issues in individuals with developmental disabilities can be difficult and complex but are understandable
- Mental health issues in individuals with developmental disabilities are challenging, but can be improved by adequate care received
- Mental health issues among this population are improved best by not separating the treatments for a developmental disability versus a mental health treatment and are best accomplished by working together conjunctively
Is it mental illness…or not? Or solely a developmental disability?
Working with someone with characteristics of both mental illness and developmental disabilities can be challenging, difficult, but also extremely rewarding at the same time. However, one may wonder if difficult or strange behavior is the result of a mental illness (unintentional) or if the behavior is being done in an effort to avoid something unfavorable or to gain something favorable (intentional).
Assessment is a crucial factor in determining what need or desire the behavior is trying to meet, how the individual need can be met before a disruptive behavior occurs. Assessment may also be able to examine what else the behavior may be communicating (problems, feelings, concerns, pain, or illness).
Case Studies
Mr. Thomas is a 38-year-old with moderate intellectual disability that presents with atypical symptoms of bipolar disorder, which require consultation with the treatment team along with his mother to establish a correct diagnosis. Thomas is also autistic with some receptive and expressive language delays and multiple medical problems: type 2 diabetes mellitus, chronic constipation with impactions, gastric ileus, sleep apnea, recurrent urinary tract infections, hypertension, and allergic rhinitis. Clinical symptoms include mood swings, impulsivity, self-injurious behavior, paranoia, schizophrenia, auditory hallucinations, multiple personality disorder, and obsessive-compulsive behaviors.
Thomas is unable to verbalize symptoms adequately due to hallucinations and multiple personalities; therefore, observation is extremely important. Depression can manifest as withdrawal, decreased appetite, and weight loss; screaming along with unexplained laughing are signs of mood swings; paranoia manifests as fearfulness, and repetitive behaviors are typically noted as obsessive compulsiveness.
Agitation and self-injurious behaviors are prone to increase during medical complications or exacerbations.
After a careful history is received and Thomas is examined, the medical problems are addressed. A team meeting is then held that involves a behavioral analysis, medication review, and assessment of environmental modifications that may need to be implemented. Sensory integration, music therapy, positive reinforcement, and frequent redirection are used, along with a few medication adjustments to assist with the current issues, in the hopes of noticing improvements.
Physical causes of abnormal behavior, including pain that may be unrecognized or masked by multiple personalities, adverse effects of medications, and seizures, may be factors related to the behaviors being noted. Environmental issues must be considered, including the level of environmental stimulation as Thomas does not like loud environments and does not like to receive excessive demands and expectations from the direct support professional staff.
Case Study #2
Ms. Virginia is a 22-year-old with a mild developmental disability and lives in a semi-supported placement. Over the time span of approximately two months, she developed progressively lower energy, hypersomnia, weakness, weight gain, and a decreased and anxious mood that she described as subjectively different from previous periods of depression. Her family physician reportedly examined her but felt the problem was psychiatric in nature.
Her placement support workers took her to the emergency department of the local hospital; after having blood drawn, the ER doctor sent her home. When she presented to her support team, and history was obtained, a test to measure her thyroid-stimulating hormone levels was ordered, and she was found to be hypothyroid.
Virginia’s case illustrates how new underlying health needs can be overlooked in the population of those with developmental disabilities and how the need for increased training for those that care for her needs to be implemented.
Case Study #3
Mr. Frank is a 54-year-old with a profound developmental disability and has had three months of severe self-injurious behaviors (SIB’s) characterized by frequently and repeatedly punching his face with his fists. This caused deep, ulcerated lesions that became infected. A systemic inquiry revealed that a long-term resident in Frank’s group home had died in the past year and that this person and Frank had been close friends for many years.
Mr. Frank had not engaged in any SIB for the previous 10 years. The systemic inquiry also revealed significant symptoms of depression, including disturbances in sleep, appetite, and increased agitation. Frank appeared to have little motivation to engage in previously enjoyed activities and seemed more “grouchy” according to staff. A physical examination indicated no obvious source of pain in his facial region, and a dental examination was scheduled.
The team behavioral consultant started tracking Frank’s SIB in an effort to identify triggers. However, the behavior was so frequent that it was difficult to assess. Eventually, major depression with complicated bereavement was diagnosed. An SSRI antidepressant was added to Frank’s long-standing antipsychotic medication, and art therapy was started. As his mood improved, his SIB became less frequent. He was encouraged to self-restrain his arms, and the group home staff were guided to help all the residents deal with grief and loss.
Frank’s case illustrates how behavioral problems can result from mental illness. Irritability is accepted by DSM-IV as a symptom of depression in children, but not in adults. However, the Diagnostic Manual-Intellectual Disability (DM-ID) does not recognize irritability as a depressive-equivalent in this population.
Frank’s case also reminds us that bereavement and grief are part of the human experience, and those with developmental disabilities are as vulnerable to this stressor as the rest of us. Staff and caregivers need to be sensitive to the effects of this life stress on this population and provide appropriate support and understanding.
Frank’s case illustrates how in-service training needs to be implemented in mental health and how direct support professionals working for those with developmental disabilities need to have the necessary training and expertise to notice subtle signs and symptoms that are not always easily detected.

Self Quiz
Ask yourself...
-
Why is the idea of shame associated with individuals with both developmental disabilities and those with mental health disorders?
Shame is a common phenomenon that underlies a variety of mental health disorders, and especially those with intellectual and developmental disabilities. The stigma associated with both of these groups often leads these individuals to be considered one of the most excluded groups in society. Individuals that fall under both of these categories have an increased vulnerability to the feelings of shame, discrimination, and characterizing stigma that typically stay with them throughout their entire life. Due to these individuals being stigmatized and excluded in many social areas, they are more likely to experience higher levels of mental health problems, anxiety, depression, and shame-related distress.
Moving Forward: The Future of Developmental Disabilities and Mental Health
With increased awareness among this vulnerable population and the increased number of individuals diagnosed with mental health disorders, the future for those caring for these individuals proves that more education needs to be provided to all those who have a part in these individuals’ overall care.
Can one serve as an advocate for positive mental health and assist those with developmental disabilities? Absolutely!
Both small and large actions can be taken as a mental health advocate in order for positive results to be obtained. First, advocate for yourself, share one‘s story, volunteer or assist in a facility that offers services to these individuals, educate yourself and your immediate circle on the facts and not the myths, serve as a mentor, and receive the necessary education and training to pursue legislative advocacy. Throughout the entire process of advocacy, these elements need to remain – confidentiality, purpose, equality, diversity, empowerment, and most importantly, placing the individual with developmental disabilities and mental disorders FIRST.
The care and treatment for the co-occurrence of both diagnoses of developmental disability and mental health disorders certainly have the capability of improving if healthcare workers, direct support professional staff, and family members are all trained and educated on the similarities and differences between these two and how they intertwine.
Education is the key to becoming more aware of the distinctions between the two. As individuals living with both diagnoses, increased knowledge and expertise in these two areas must be in place for these special individuals to receive the necessary and adequate care they each deserve.
References + Disclaimer
- Esteves, Jeffrey, et al. “Occurrence and Predictors of Challenging Behavior in Youth with Intellectual Disability with or without Autism.” Journal of Mental Health Research in Intellectual Disabilities, vol. 14, no. 2, 2021, pp. 189–201., doi:10.1080/19315864.2021.1874577.
- Facts about developmental disabilities. (2020, November 12). Retrieved March 02, 2021, from https://www.cdc.gov/ncbddd/developmentaldisabilities/facts.html
- Heusser, P. (2020, April 10). 7 myths about developmental disability in 2020. Retrieved March 02, 2021, from http://friendsofcyrus.com/blog/2020/03/03/7-myths-about-developmental-disability-in-2020/
- Issues in treating patients with intellectual disabilities. (2013, August 14). Retrieved February 28, 2021, from https://www.psychiatrictimes.com/view/issues-treating-patients-intellectual-disabilities
- Mental illness and developmental disabilities: Some basics. (n.d.). Retrieved March 02, 2021, from https://achievable.org/wp-content/uploads/2016/03/Mental-Illness-and-Developmental-Disabilities-Some-Basics.pdf
- Myths, misunderstandings and facts about mental illness. (n.d.). Retrieved March 04, 2021, from https://www1.health.gov.au/internet/publications/publishing.nsf/Content/mental-pubs-w-whatmen-toc~mental-pubs-w-whatmen-myth
- Physicians and lawyers for National drug policy. (2008). Retrieved March 05, 2021, from http://www.plndp.org/resource_guide/5c-co-occurring.php
- What is community inclusion & why is it a win-win scenario? (2019, July 08). Retrieved March 04, 2021, from https://communitymainstreaming.org/what-is-community-inclusion/#:~:text=Community%20inclusion%20is%20the%20opportunity,Housing
- Yona Lunsky Robert Balogh, Yona Lunsky Robert Balogh, Authors, Lunsky, Y., Says:, L., Says:, S., . . . Says:, A. (2021, February 23). Developmental disabilities, mental health issues often overlap. Retrieved March 02, 2021, from https://healthydebate.ca/opinions/developmental-disabilities-mental-health/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate

