Types of Myocardial Infarctions
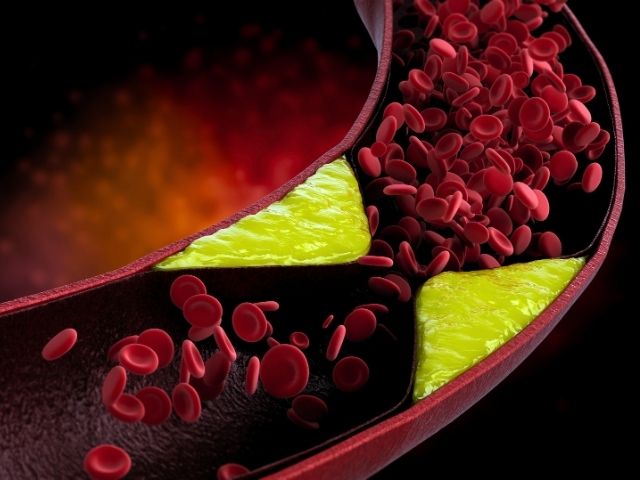
The most common type of myocardial infarction (MI) is considered Type 1. It is caused by CAD and it is the leading cause of death in the United States.
Type 1 MIs are caused by the rupturing or cracking of the plaque and the sudden occlusion of the artery by the formation of a thrombus/blood clot. Type 1 MIs include non-ST segment elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI). An NSTEMI is a partial occlusion or a distal coronary artery occlusion by an embolism while a STEMI is usually more severe and caused by a total occlusion.
A type 2 MI is transient ischemia usually characterized by chest pain or ECG changes. Type 2 MIs do not cause permanent damage or death to the heart muscle. This type of MI is related to demand ischemia or otherwise described as a mismatch of supply and demand (the amount of oxygen the heart muscle needs compared to the amount of oxygen available).
This type of infarction is self-limiting and after the underlying cause of the ischemia is corrected, it is resolved. Common causes of MI type 2 include severe anemia, atrial fibrillation with rapid ventricular rate (RVR), bradycardia, respiratory failure, shock, hypertension (HTN), or a sudden spasm of a coronary artery.
A Type 3 MI is the sudden death of a patient from a coronary cause prior to any diagnostic changes that can be evaluated by elevated troponins or ECG changes. It takes about 6 hours post MI for the troponin level to rise, so if the patient has a sudden death from a heart attack, it is commonly only diagnosed on an autopsy after a patient expires.
The last two types of myocardial infarction are related to surgery. Type 4 MI is associated with percutaneous coronary interventions – within 48 hours of a procedure or from an in-stent stenosis/occlusion. Type 5 MI is myocardial infarction that occurs within 48 hours of a coronary artery bypass grafting (CABG).