Pull up a chair, and let’s have a chat about mental health in the end-stage renal disease community.
Dialysis comes in different modalities, such as mainstream hemodialysis, lesser-known peritoneal dialysis, home hemodialysis, and kidney transplantation. Dialysis is the removal of toxins and/or fluid from the body, which can be completed outside or inside the body (through hemodialysis or dialysis and peritoneal dialysis or kidney transplantation, respectively). As a tangible process, dialysis can be evaluated through lab work, vital signs, dry weight, medication adherence, and dietary compliance.
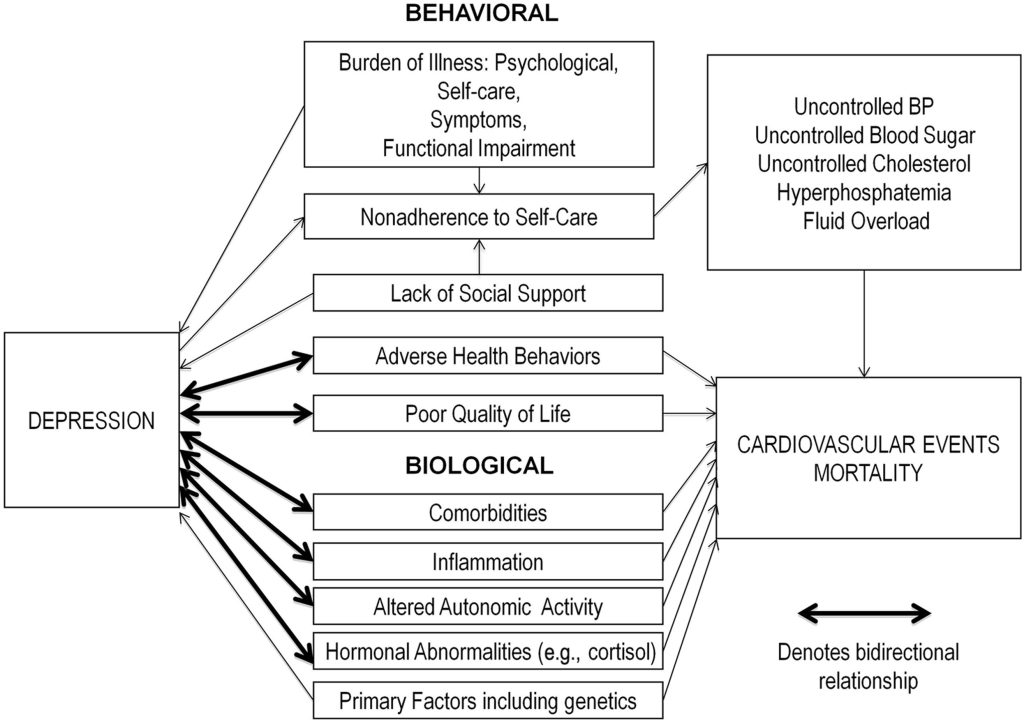
Mental health — more specifically, depression — is an intangible phenomenon that isn’t adequately addressed or discussed. And is barely recognized as something that needs to be discussed in the end-stage renal community.