Course
Acute Kidney Injury and Dehydration in the Elderly
Course Highlights
- In this Acute Kidney Injury and Dehydration in the Elderly course, we will learn about the pathophysiology of acute kidney injury and dehydration in the geriatric population.
- You’ll also learn the etiology of acute kidney injury and dehydration in older adults.
- You’ll leave this course with a broader understanding of diagnostic and assessment tools used in the early detection of acute kidney injury and dehydration in geriatric clients.
About
Contact Hours Awarded: 2
Course By:
Abbie Schmitt, MSN-Ed, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Acute kidney injury in geriatric clients is not just a clinical concern; it’s a complex puzzle influenced by age-related physiological changes, multiple comorbidities, and the subtle onset of symptoms. Dehydration complicates this condition even further due to several interconnected factors that stem from both the aging process and the pathophysiology of AKI.
This course will help learners review renal pathophysiology, understand etiology, signs and symptoms, and apply practical interventions to prevent and manage AKI and dehydration in older adults. Join us as we explore the delicate balance between vulnerability and resilience in the aging kidney, and discover how your role as a healthcare professional can turn the tide in preventing and managing kidney injury in this growing population.
Definition
Acute Kidney Injury
Acute kidney injury (AKI), previously called acute renal failure (ARF), is a sudden and often reversible impairment of kidney function (4). The function is measured using glomerular filtration rate (GFR); however, immediately after a renal injury, blood urea nitrogen (BUN) or creatinine (Cr) levels may be within the normal range, and the only sign of AKI may be a decline in urine output.
There are two different types of kidney failure: AKI and chronic kidney disease. AKI differs from chronic kidney disease in that the loss of kidney function is sudden and possibly reversible, while chronic kidney disease results from a gradual loss of kidney function.
Acute Interstitial Nephritis
Acute interstitial nephritis (AIN) is an immune-mediated form of kidney injury characterized by infiltrating immune cells in the kidney’s tubules and interstitial tissue (7).
According to the “Kidney Disease: Improving Global Outcomes (KDIGO)” criteria, AKI is the presence of any of the following (5):
- Increase in serum creatinine by 0.3 mg/dL or more (26.5 micromoles/L or more) within 48 hours.
- Increase in serum creatinine to 1.5 times or more baseline, within the prior 7 days.
- Urine volume less than 0.5 mL/kg/h within 6 hours.
Fragility
Fragility is a term used to describe a condition characterized by the loss of biological reserve and the vulnerability to restore homeostasis after a stressful event (3). This condition implies difficulty recovering from acute illness. Fragility occurs most frequently in older adults and, similar to acute kidney injury (AKI), carries a high risk of poor outcomes such as physical disability, functional decline, frequent hospitalizations, and increased mortality (6).

Self-Quiz
Ask Yourself...
- What criteria are often used to determine AKI?
- How would you describe the difference between AKI and chronic kidney disease?
- Can you name the measurements/labs that correlate with kidney function?
- What are examples of fragility in older adults (for example: reduced skin turgor, bone fractures)?
Epidemiology
AKI is a prevalent condition, especially among hospitalized clients. Currently, 7% of hospitalized clients and 30% of ICU admissions develop AKI (4). Roughly 1% of all hospital admissions have AKI on admission (4).
Pertinent information on AKI:
- The incidence of AKI has steadily increased over the past decade, which is likely related to the increasing population of older adults.
- Elderly clients with AKI have worse renal recovery rates and higher mortality rates than younger clients with AKI (3).
- Survivors of AKI face a higher risk of complications such as the development or progression of chronic kidney disease (CKD), end-stage renal disease (ESRD), and cardiovascular disease (3).
Dehydration occurs in roughly 17% to 28% of older adults in the United States (9). Dehydration is commonly the cause of hospital admissions.
Globally, dehydration, hypotension, and volume depletion are responsible for 40% of AKI cases in both the hospital and nonhospital settings (5).
Renal Anatomy Review
The kidneys are two bean-shaped organs, each about the size of a fist. The kidneys function as vital organs in maintaining the body’s internal environment by filtering blood, regulating fluid and electrolyte balance, removing waste, and managing blood pressure. Each kidney contains roughly one million nephrons, which are the microscopic units that complete these essential functions.
The kidney regulates fluid balance, helps maintain blood pressure, and filters waste from the blood. This can be compared to a highly skilled dam engineer for a flowing river. The engineer constantly monitors and adjusts the flow of water, and regulates the pressure to ensure that the river stays balanced. The engineer redirects excess water when it’s too high and retains just enough when it’s too low.
Here’s an overview of the kidney’s anatomy:
The renal capsule is the tough, fibrous outer layer that encases the kidney; it serves to protect the kidney from injury and maintain its shape. The cortex is the outer layer of the kidney, beneath the renal capsule. The cortex contains the nephrons and is essentially where blood filtration occurs. The medulla is the inner part of the kidney and is made up of cone-shaped tissue called renal pyramids. The pyramids comprise the loops of Henle, which collect ducts of the nephrons and create concentrated urine. The renal pelvis is a funnel-shaped cavity within the kidney that stores urine from the pyramids and directs urine from the kidney into the ureter. Ureters are long, narrow tubes that transport urine from the kidney to the bladder. (5)
Nephrons are microscopic units within the kidney, each consisting of a glomerulus and a renal tubule. Nephrons filter blood to remove waste and excess substances and create urine.
The glomerulus is a network of capillaries that begin the blood filtration process.
- Bowman’s Capsule: A cup-like sac that encases the glomerulus.
- Proximal Convoluted Tubule: Reabsorbs nutrients, water, and electrolytes from the filtrate.
- Loop of Henle: Concentrates urine by reabsorbing water and salts.
- Distal Convoluted Tubule: Further refines the filtrate by reabsorbing sodium and calcium, and secreting potassium and hydrogen ions.
- Collecting Duct: Collects urine from multiple nephrons and channels it into the renal pelvis.
The renal artery is a large artery that supplies oxygenated blood to the kidneys. It branches off from the aorta. The renal vein exits the kidney and joins the inferior vena cava; the renal vein carries filtered, deoxygenated blood away from the kidney. The renal hilum is the region on the medial side of the kidney and basically serves as the entry and exit point for the renal artery, renal vein, ureter, and nerves. (5)
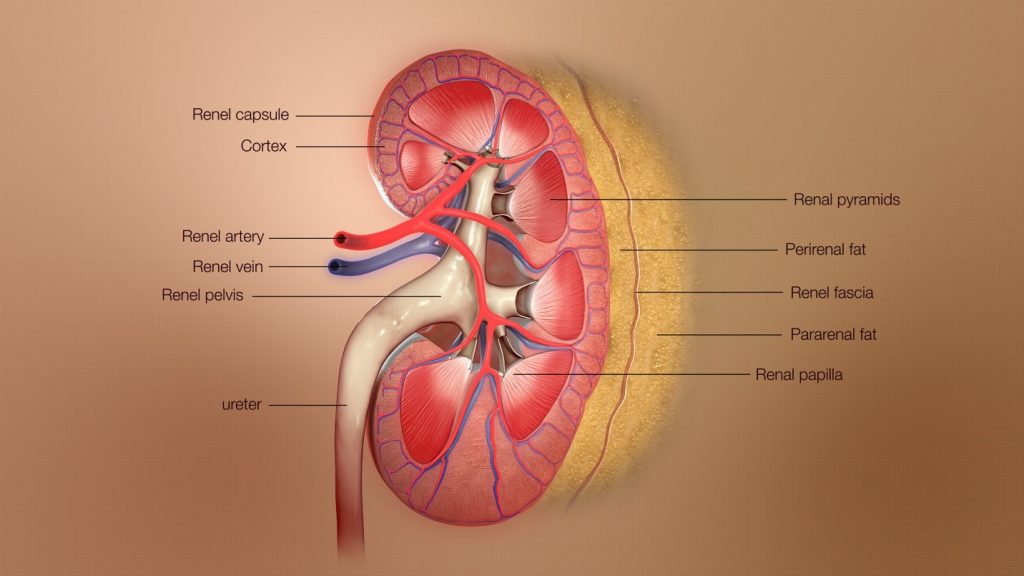
Figure 1. Anatomy of the Kidney (8)

Self-Quiz
Ask Yourself...
- What is the current percentage of ICU clients who develop AKI?
- What conditions are survivors of AKI at greater risk of developing?
- What is the major role of nephrons within the kidney?
- Can you describe the function of the kidneys?
- Why is it important to recognize the vascular supply for the kidneys?
- What is the term for the long, narrow tubes that transport urine from the kidney to the bladder?
Pathophysiology and Etiology
AKI can exacerbate dehydration by impairing the kidneys’ ability to concentrate urine and regulate fluid balance. Conversely, dehydration can trigger AKI, leading to serious complications without prompt intervention.
The pathophysiology of AKI is determined by the etiology. Remember – AKI is a condition of a sudden onset of decreased kidney function.
Glomerular filtration results from the pressure difference between the glomerulus and Bowman’s space. The resistance of vascular pathways controls this pressure. Reduced renal blood flow is a common pathologic cause of declining GFR and impaired function.
The pathophysiology of AKI has been divided into three categories:
- Prerenal
- Intrinsic renal (i.e., intrarenal)
- Postrenal
Each of these categories has many different associated causes, and some causative factors of AKI have overlapping mechanisms of injury.
Prerenal Form of AKI
The prerenal form of AKI is caused by impaired blood flow to the kidney (4). Causes can include systemic hypoperfusion resulting from hypovolemia or selective hypoperfusion of the kidneys.
Examples of prerenal AKI mechanisms include (4):
- Hypovolemia
-
- Hemorrhage, gastrointestinal fluid losses such as diarrhea, vomiting, and high ostomy output.
- Hypotension from decreased cardiac output
-
- Cardiogenic shock, pulmonary embolism, acute coronary syndrome.
- Hypotension from systemic vasodilation:
-
- Septic shock, anesthesia.
- Renal vasoconstriction
-
- NSAIDs, contrast dye, amphotericin B.
- Glomerular efferent arteriolar vasodilation (causing intraglomerular hypotension)
-
- ACE inhibitors, angiotensin receptor blockers.
Intrinsic Form of AKI
Causes of intrinsic AKI include conditions that affect the actual glomerulus or tubule, such as acute tubular necrosis and acute interstitial nephritis. Glomerular or tubular injury can lead to a release of vasoconstrictors from the renal efferent pathways.
Prolonged renal ischemia, sepsis, and nephrotoxins are the most common causes.
Examples of causes include:
- Acute tubular necrosis (ATN)
-
- Ischemia from prolonged prerenal injury
-
- Drugs such as aminoglycosides, vancomycin, amphotericin B, and pentamidine.
-
- Iodinated contrast
-
- Rhabdomyolysis
- Acute interstitial nephritis (AIN)
-
- Infection
-
- Drugs such as beta-lactam antibiotics, penicillins, NSAIDs, proton pump inhibitors (PPIs), and 5-ASA; infection; autoimmune conditions (systemic lupus erythematosus (SLE), IgG-related disease); and hereditary AIN.
- Glomerulonephritis
-
- Immunological diseases (SLE, post-infectious glomerulonephritis)
- Intratubular obstruction
-
- Toxins (such as ethylene glycol), Tumor lysis syndrome, hemolytic anemia.
Postrenal Form of AKI
Mechanisms for postrenal AKI include obstructive causes, which lead to congestion and urinary backflow of the filtration system, leading to a shift in the filtration driving forces.
Pathological injury can occur within 2 hours of obstruction, starting with decreased filtration within the glomerulus due to pressure in the upper urinary tract. This causes poor renal perfusion, inflammation, tubular atrophy, and interstitial fibrosis (4). Ongoing obstruction can lead to ESRD.
The most common etiology of postrenal AKI is bladder outlet obstruction (4). This is often caused by prostatic hypertrophy in older men, pelvic masses in older women, and nephrolithiasis in younger clients (4). Additional causes of obstruction include renal/ureteral calculi, tumors, blood clots, and neurogenic bladder. Blood clots can be a result of bladder or urinary tract malignancy.
After an obstruction is relieved, post-obstructive diuresis occurs in up to 50% of clients (4). These clients should be closely monitored for severe complications of hypovolemia and electrolyte abnormalities.

Self-Quiz
Ask Yourself...
- What is the most common etiology of postrenal AKI?
- Can you name common causes of acute tubular necrosis (ATN)?
- Significant blood loss would be a causative factor in which form of AKI?
- Which form of AKI is often caused by infection or autoimmune diseases?
Medication-Induced Acute Kidney Injury
Medications are a common cause of AKI in hospitalized clients and those in the intensive care unit; drugs were associated with AKI in 37.5% in a cross-sectional survey (Par). Although medications can cause different forms of kidney injury, drug-induced injury to the tubulointerstitial compartment is a common cause of AKI.
Medications commonly cause the following:
- Acute tubular injury due to their innate toxicity and kidney injury.
- Acute interstitial nephritis (AIN) when medications elicit a T cell-mediated immune response that promotes tubulointerstitial inflammation.
- Intratubular precipitation refers to the process where substances “precipitate” or solidify, or “crystallize” within the tubules of the kidneys. This is associated with an inflammatory response or conditions where there is an excess of certain substances in the blood, such as in cases of hypercalcemia (excess calcium), hyperuricemia (excess uric acid), or the presence of certain medications or toxins that can cause the formation of crystals.
- Pseudo-AKI is when a patient exhibits signs that mimic acute kidney injury (AKI) but does not actually have intrinsic kidney damage; this is due to a transient rise in serum creatinine or blood urea nitrogen (BUN) without a true reduction in kidney function. It can be caused by drugs that block creatinine secretion.
|
Medications Associated with Acute Tubular Injury |
|
|
Medication Class |
Individual Medications |
|
Antibiotics |
|
|
Antifungals |
|
|
Antiviral agents |
|
|
Analgesics |
|
|
Chemotherapeutic agents |
|
|
Calcineurin inhibitors |
|
|
Radiocontrast agents |
|
|
Bisphosphonates |
|
|
Reference used: (7) |
|
|
Medications Associated with Acute Interstitial Nephritis |
|
|
Medication Class |
Individual Medications |
|
* 120+ drugs are reported to cause AIN; however, antibiotics, NSAIDs, proton pump inhibitors (PPIs), and immune-checkpoint inhibitors (ICPIs) are the most common. |
|
|
Antibiotics |
|
|
Proton pump inhibitors Histamine-2 blockers |
|
|
Analgesics |
|
|
Immunotherapies |
|
|
Diuretics |
|
|
Antiviral agents |
|
|
Anticonvulsants |
|
|
Other agents |
|
|
Reference used: (7) |
|
|
Medications Associated with Crystalline Nephropathies |
|
|
Reference used: (7) |
|
Medications Associated with Pseudo-AKI |
|
|
Reference used: (7) |
It is critical to recognize the impact of medications on kidney function for the prevention of kidney injury, proper dosing, avoiding drug interactions, and early detection of kidney issues. Some medications can be nephrotoxic, meaning they can cause significant damage to the kidneys. Recognizing which medications carry this risk allows healthcare providers to monitor kidney function closely and adjust dosages or choose alternative treatments to prevent AKI.
Adjusting medication doses based on kidney function is crucial to avoid adverse effects and ensures that the medication remains effective.
Some medications can impact or reduce the kidneys’ ability to excrete other drugs, leading to potential drug interactions. For instance, nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce blood flow to the kidneys, exacerbating the effects of other nephrotoxic drugs. A sudden decline in kidney function after starting a new medication may indicate that the drug is harming the kidneys, allowing clinicians to quickly intervene.
Medications and Aging
Physiological changes of aging have a major impact on medication efficacy. Aging contributes to functional changes in organ systems and results in decreased homeostatic capacity. Aging also affects body composition, increased volume of distribution for fat-soluble drugs, reduced clearance of multiple medications (1).
Polypharmacy is the simultaneous use of 5 or more drugs (1). As adults age, the number of medications they take typically increases. The changes in older adults’ physiology coupled with polypharmacy lead to an increased risk of adverse reactions to commonly used medications, complications, and damage to organ tissue. Additional clinical consequences of polypharmacy include depression, disability, falls, postoperative complications, and mortality (1)
Multiple drug-drug and drug-disease interactions are associated with polypharmacy in the elderly. For example, anticholinergic drugs are strongly associated with cognitive impairment in older adults (1). Older adults using anticholinergic drugs had a more significant decline in memory, psychomotor speed, and cognitive flexibility when compared to non-users (1).
Observational studies have found that chronic inflammation, changes in energy metabolism, oxidative stress, and mitochondrial dysfunction in stress response contribute to cognitive decline in physically frail people (1). Essentially, these factors can further weaken older adults’ ability to recover from illness or kidney injury.
Tailoring treatment plans is key. Overall, knowledge of the impact of medications on kidney function is essential for ensuring patient safety, preserving kidney function, and optimizing outcomes.

Self-Quiz
Ask Yourself...
- Can you name certain medications that are associated with Acute Tubular Injury (ATI)?
- How can polypharmacy and the normal physiological changes of aging increase the risk of kidney injury?
- Are you familiar with medications that are associated with cognitive impairment in older adults?
- How can patient education impact the early detection of dehydration in older adults?
Dehydration
Dehydration can lead to devastating outcomes, especially in older adults. Dehydration has the potential to worsen many health conditions or lead to death. Dehydration is the most common fluid and electrolyte problem in older adults and is a major risk factor for delirium (10).
This increased risk for dehydration among older adults is related to physiologic aging changes, which include reduced total body water, changes in thirst perception, and reduced renal function (10). Additional risk factors include infection, tube feedings, and medication-related side effects.
Water has a vital role in maintaining multiple physiological functions within the body. 55% to 65% of the human body is made up of water (9). Two-thirds of that water is intracellular, and one-third is extracellular. One-fifth of extracellular water is intravascular.
Water is absorbed through the gastrointestinal tract and homeostasis is primarily controlled through osmoreceptors in the brain (9). The osmoreceptors detect dehydration, which stimulates the thirst center in the hypothalamus. These osmoreceptors can also help the kidneys conserve water. Essentially, dehydration signals the kidneys to retain water by releasing antidiuretic hormone, which stimulates the kidneys to reabsorb more water. Dehydration also commonly causes low blood pressure, which triggers renin secretion from the kidney. Renin converts angiotensin I to angiotensin II, which increases aldosterone release from the adrenals, leading to increased sodium and water absorption by the kidney. Severe dehydration can trigger these actions and ultimately reduce kidney function and lead to acute kidney injury (AKI).
Certain conditions, such as diabetes, can significantly impact hydration status. When blood glucose levels exceed a certain threshold, the kidneys cannot reabsorb all of the glucose, which remains in the urine. Glucose is osmotically active, meaning it draws water with it. As the glucose is excreted in the urine, it pulls large amounts of water along too. This process is known as osmotic diuresis. This increased water in the urine leads to a higher volume of urine production, causing frequent urination (polyuria) and depleted hydration.

Self-Quiz
Ask Yourself...
- What are factors that can mask changes in vital signs, such as hypotension or tachycardia?
- Can you name certain disease processes that affect hydration?
- Considering that dehydration signals the kidneys to retain water by releasing antidiuretic hormones, how can this impact homeostasis and fluid maintenance?
- Can you discuss the normal physiological changes of aging that increase the risk of dehydration in older adults?
Risk Factors
Acute Kidney Injury (AKI) can result from a variety of factors, often mingling with each other like an awkward family reunion.
Risk factors for AKI and dehydration can overlap and impact each other. Age, chronic kidney disease, use of certain medications, systemic conditions such as sepsis, infections, obstruction, and critical illness with ICU admission are a few examples.
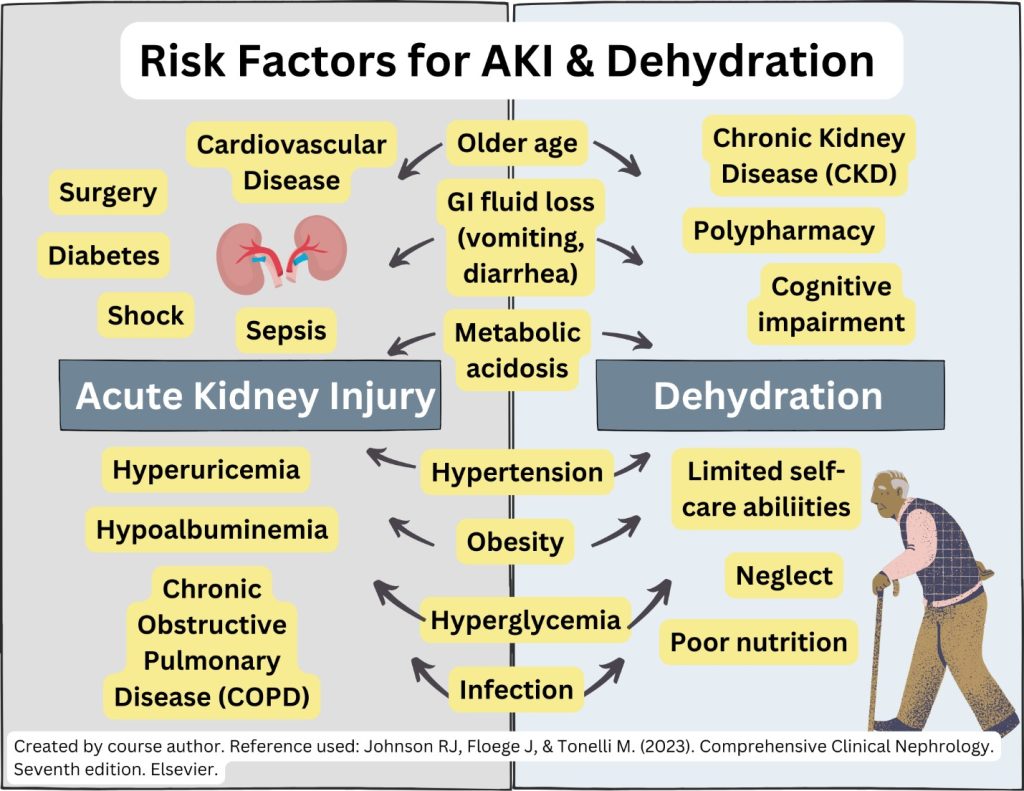
Figure 2. Risk factors for acute kidney injury and dehydration
Clinical Signs and Symptoms
Acute Kidney Injury
The signs and symptoms of AKI will reflect the kidney’s abrupt loss of its ability to filter waste and balance fluids. The subtle signs can easily be mistaken for something else. A patient may notice decreased urine output, or even stop urinating altogether, as if the body’s plumbing has slowed to a trickle.
Swelling in the legs, ankles, or around the eyes may begin to develop, caused by fluid retention initiated by the kidneys. The skin may become pale or blotchy, and blood pressure can spike or dip unpredictably.
Fatigue sets in, and the individual might feel unusually tired or weak. Nausea, vomiting, and a loss of appetite might occur. In more severe cases, confusion and disorientation might occur, as the toxins normally filtered out by the kidneys begin to impact neurological function. If left unchecked, AKI can lead to serious complications, but early recognition of these signs and symptoms is key to restoring balance and preventing further harm.
The location and source of the kidney impairment will ultimately cause varying symptoms, based on whether it occurs before reaching the kidney, within the kidney, or past the kidneys.
Dehydration in Geriatric Clients
The signs and symptoms of dehydration in older adults may be vague or even absent.
General symptoms of dehydration include but are not limited to fatigue, thirst, dry skin and lips, dark urine or decreased urine output, headaches, muscle cramps, lightheadedness, dizziness, syncope, orthostatic hypotension, and palpitations (9).
Typically, vital signs may show hypotension, tachycardia, fever, and tachypnea.
The physical examination may show dry mucosa membranes, skin tenting, sunken eyes, or cracked lips (9). A physical assessment will likely find a dry axilla, mucous membranes, tongue, increased capillary refill time, poor skin turgor, orthostatic hypotension, weak grip, decreased strength, cyanosis, and altered mental status.
It is important to recognize that hypotension does not appear until significant dehydration is present. Medications such as beta-blockers can cause an absence of tachycardia. Physical exertion, heat exposure, medications, poor access to water, fever, or fluid loss can contribute to dehydration. A thorough evaluation of medical history, current review of systems, and the medication regimen is critical.
However, vital signs may not be a reliable indicator for elderly clients due to the tachycardic response seen in volume depletion may be hidden because of cardiac conduction disturbances or medications such as β-blockers.
Skin turgor can also be difficult to discern in older adults due to normal physiological changes with aging. Incontinence can also complicate intake and output measurements, making them inaccurate. Oral dryness can be impacted by medications with anticholinergic properties. The vulnerability of older adult physiology and dehydration may only be manifested by constipation or slight orthostasis.
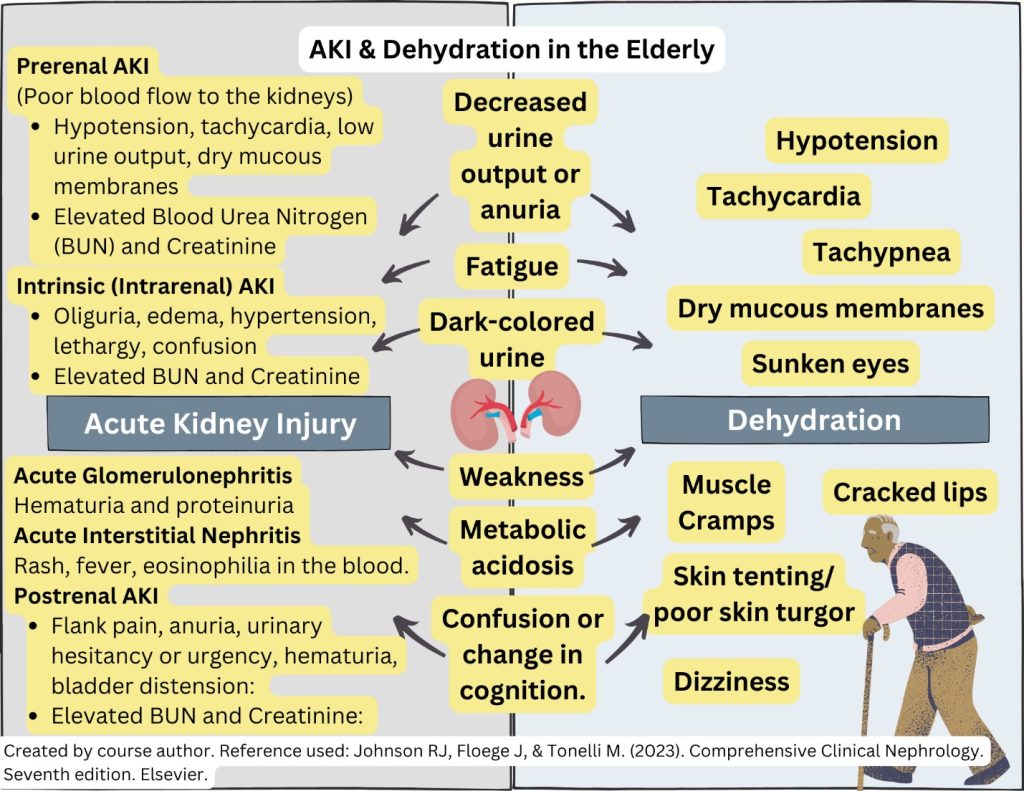
Figure 3. Clinical signs and symptoms of acute kidney injury and dehydration in the elderly
Assessment
The evaluation of AKI should begin with a complete medical history and review of medical records. A detailed physical assessment can provide extremely valuable information in establishing the etiology of AKI. Differentiating between AKI and chronic kidney disease (CKD) is essential.
Medical History
Clinicians should compare serum creatinine concentration with previous levels, and focus on the events preceding the AKI development. Events may be a systemic disease process (e.g., sepsis, rhabdomyolysis), surgery, medication changes, or volume depletion (e.g., diarrhea, vomiting).
A careful review of any comorbid conditions can help narrow down the etiology of AKI, such as cirrhosis or a history of blood clots requiring anticoagulation.
Note the use of nonsteroidal anti-inflammatory drugs (NSAIDs), renin-angiotensin-aldosterone antagonists, diuretics, antibiotics, proton pump inhibitors, chemotherapy agents, or a synthetic cannabinoid (5).
Lab Work
Initial laboratory tests are crucial for diagnosing and assessing AKI complications, including creatinine levels, blood urea nitrogen (BUN), serum sodium, potassium, bicarbonate, and urinalysis (5). Evaluation of urine volume, urinary sediment, and urinary indices helps diagnose correctly.
These tests can guide diagnosing prerenal or intrarenal etiology.
AKI can lead to the accumulation of water, sodium, and other electrolyte disturbances. Several criteria have been used to identify AKI, such as RIFLE, AKIN (Acute Kidney Injury Network), and KDIGO (Kidney Disease: Improving Global Outcomes) criteria.
KDIGO is the most recent and most commonly used tool. According to KDIGO, AKI is the presence of any of the following (5):
- Increase in serum creatinine by 0.3 mg/dL or more (26.5 μmol/L or more) within 48 hours
- Increase in serum creatinine to 1.5 times or more than the baseline of the prior 7 days
- Urine volume less than 0.5 mL/kg/h for at least 6 hours
The ratio of BUN to creatinine in healthy individuals is 10:1 to 15:1; in prerenal AKI the ratio may exceed 20:1 because of a disproportionate increase in urea reabsorption resulting from elevated serum vasopressin levels (5). However, the BUN-to-creatinine ratio cannot differentiate the type of AKI or etiology. The urine-serum concentrations of sodium compared to the urine-serum concentrations of creatinine (fractional excretion of sodium [FE Na ]) have been used to approximate kidney tubular function (5).
In the presence of systemic illness, additional laboratory evaluation may narrow the differential diagnosis of AKI.
Physical Examination
The history and physical exam should focus on determining the etiology of AKI and the progression timeline. Providers should look for inciting events such as diarrhea, nausea, vomiting, which may have caused volume loss, or any over-the-counter drugs such as NSAIDs.
History and physical examination are essential in AKI because labs often cannot provide a clear answer as to the etiology of AKI. A crucial part of the physical exam should be orthostatic vital signs, which may signify hypovolemia.
Assessment of the following systems can provide clues regarding the cause of AKI:
- Integumentary
-
- Decreased skin turgor suggests hypovolemia.
-
- Livedo reticularis, poor extremity circulation, and butterfly rash suggest vasculitis.
-
- A maculopapular rash may indicate drug-induced AIN.
-
- Livedo reticularis and skin infarcts are also seen with cholesterol emboli disease.
-
- Jaundice is present in liver disease
-
- Keratitis, iritis, and uveitis may be present in autoimmune vasculitis.
-
- Hearing loss is associated with Alport disease.
- Cardiovascular
-
- Pulse rate, blood pressure, and jugulovenous pulse can indicate volume status.
-
- Irregular cardiac rhythm may indicate electrolyte imbalance-related arrhythmias.
-
- Pericardial friction rub may be heard in uremic pericarditis
- Reduced body weight
- Orthostatic hypotension
- Lack of jugular venous distention
- Peripheral edema
Clients with prerenal AKI may present with:
- Volume overload in heart failure
- Cirrhosis
- Nephrotic syndrome
Trends in daily intake and output volumes also assist in determining the extracellular fluid volume of the critically ill patient. Monitoring urine output in the ICU is associated with improved detection of AKI, as well as reduced 30-day mortality in clients with AKI (5).
A history of urine output may give clues as to the cause of AKI. The following are some associations:
- Sudden anuria suggests acute urinary tract obstruction, acute glomerulonephritis, or vascular blockage.
- Polyuria suggests either a concentrating tubular defect, such as acute interstitial nephritis, or post-obstructive nephropathy.
Assessment of the abdomen may reveal a tender, distended bladder in a lower urinary tract obstruction, and, when this is present, sterile postvoid bladder catheterization should be performed.
A distended, tense abdominal wall may represent ascites, aggressive intravenous fluid resuscitation, or recent abdominal surgery. Intraabdominal pressure can be measured in the ICU to differentiate AKI from abdominal compartment syndrome.
| Prerenal | Intrarenal | |
| History |
|
|
| Clinical Presentation |
|
|
| Laboratory Studies | ||
| BUN/S Cr | >20 | <20 |
| Sediment | Normal or few hyaline casts | Muddy brown casts |
| U osm (mmol/kg) | >500 | <350 |
| Proteinuria | None to trace | Mild to moderate |
| U Na (mmol/L) | <20 | >40 |
| FE Na (%) | <1 | >1 |
Imaging Studies
Kidney imaging may not be necessary if the cause of the AKI is found. However, when the diagnosis is uncertain, especially if urinary obstruction or renal vascular occlusion is suspected, imaging is indicated. (5)
- Point-of-care ultrasound is an emerging tool for assessing urinary obstruction in AKI.
- A kidney ultrasound can identify urinary obstruction, polycystic kidney disease, and the size and number of kidneys. Doppler flow can evaluate renal arteries and veins.
- High-resolution, non-contrast computed tomographic (CT) imaging is the preferred test for the detection of urinary tract calculi.
- Magnetic resonance imaging without contrast is recommended to evaluate renal arterial or venous thrombosis (5)
Kidney Biopsy
Kidney biopsy is reserved for clients in whom prerenal and postrenal AKI have been excluded and the cause of intrinsic AKI remains unclear (5). Kidney biopsy is particularly useful if ischemic or nephrotoxic injury is suspected, and the suspected condition may respond to disease-specific therapy (e.g., vasculitis, systemic lupus erythematosus).

Self-Quiz
Ask Yourself...
- Can you describe the fluid and electrolyte disturbances that AKI can lead to?
- Do you think kidney biopsies are considered the first line of diagnostic evaluation?
- Why is it important to compare creatinine levels with previous measurements?
- Can you explain why the evaluation of events, injuries, illness, or surgeries is important to the assessment and management of AKI?
Classification
The RIFLE criteria define three categories of impairment: risk, injury, and failure; and two categories of long-term renal outcomes: loss and end-stage renal disease (ESRD). The criteria that show the most impairment is used for classification. When baseline Cr is unknown, a baseline GFR between 75 and 100 mL/min is assumed, or the Modification of Diet in Renal Disease (MDRD) equation can be used to calculate an estimated baseline Cr. (5)
- Risk: Cr is more than 1.5x baseline, GFR ↓ of 25%, or urine output (u/o) <0.5mL/kg/h for 6 hours.
- Injury: Cr is more than 2x baseline, GFR ↓ of 50%, or urine output (u/o) <0.5mL/kg/h for 12 hours.
- Failure: Cr is more than 3x baseline, GFR ↓ of 75 %, Cr ≥4 .0, or urine output (u/o) <0.5mL/kg/h for 12 hours.
- Loss: Loss of kidney function for over 4 weeks.
- ESRD: Loss of kidney function for over 3 months. (5)
Treatment
Renal recovery within 48 hours is typically associated with the reversal of AKI and optimal outcomes (2).
Time = Kidney Function Recovery
The clinical approach should begin with hemodynamic stabilization. The early identification of the type and cause of AKI will guide the treatment plan.
Hemodynamic stabilization is of critical significance because mechanisms that autoregulate are impaired in AKI and dehydration (2).
Particular attention should be given to medications with renal toxicity, which should be discontinued, and dose adjustment according to renal function to avoid underdosing or adverse effects.
The prompt initiation of antibiotics is crucial for cases of sepsis. Therapy may be aimed at treating hyperkalemia, metabolic acidosis, anemia, and fluid overload (2)
Treating AKI and dehydration in elderly clients requires a multifaceted approach, considering their physiological needs, comorbidities, and medications. The primary goals are to restore fluid balance, manage underlying causes, and prevent further kidney damage.
- Underlying Condition Management
-
- Management of Chronic Conditions –Conditions such as heart failure, diabetes, kidney disease, autoimmune disease, and hypertension should be closely followed and managed to support kidney function and overall health.
-
- Infections – Antibiotic therapy
- Fluid/ Volume Replacement
-
- If hypovolemia or hypotension is present, then the treatment is guided towards volume repletion.
-
- Intravenous Fluids – The type and rate of IV fluids should be carefully selected based on the patient’s overall condition, comorbidities, heart function, and electrolyte status.
-
- Oral Rehydration
- Vasopressor Drugs
-
- Following volume replenishment, vasopressor support should be considered to maintain renal perfusion and avoid positive fluid balance. The median blood pressure target for clients with AKI should be higher than 65 mmHg to ensure accurate renal perfusion. (2)
- Diuretics
-
- Diuretics may be used cautiously to manage excess fluid in cases of fluid overload.
- Medication Management
-
- Medications that are considered nephrotoxic and contribute to kidney injury, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and certain antibiotics, should be discontinued or adjusted.
-
- Dosages of essential medications may also need to be recalibrated based on kidney function.
- Electrolyte Balance
-
- Dehydration and AKI can lead to significant electrolyte disturbances, such as hyperkalemia. Prompt intervention for these imbalances is critical to prevent complications such as cardiac arrhythmias.
- Monitoring and Supportive Care
-
- Regular ongoing monitoring of kidney function and fluid status is crucial to assess the effectiveness of treatment and to make necessary adjustments.
- Nutrition and Hydration Strategies
-
- Individualized Nutrition Plans – Elderly clients may require tailored nutrition plans to ensure they receive adequate hydration and essential nutrients without overburdening the kidneys.
-
- Hydration Protocols – Establishing regular hydration schedules, especially in elderly clients with cognitive impairment or those who may forget to drink, can help prevent dehydration.
- Renal Replacement Therapy (RRT)
-
- Treatment for clients with kidney failure. As kidney function diminishes, waste and fluid build up in the blood.
-
- RRT uses various techniques to replace kidney function, including:
-
-
- Hemodialysis
-
-
-
- Peritoneal dialysis
-
-
-
- Kidney transplantation
-

Self-Quiz
Ask Yourself...
- Why should fluid replacement be done carefully in clients with cardiac conditions?
- How can nurses individualize nutrition plans for elderly clients who live alone with limited resources and comorbidities?
- Can you discuss the impact surgical procedures have on the entire body?
- If you were explaining the physiological changes of aging to a family member, what would you include in your teaching and what methods could be meaningful?
Research for Detection
Computer-based models are currently being developed within electronic health records (EHR) to predict AKI and create alerts. In one study, real-time alerts of the worsening of AKI by an AKI “sniffer” program increased the timeliness of detection, which led to early therapeutic intervention (5). Further studies are needed to further define the utility of such AKI alerts.

Self-Quiz
Ask Yourself...
- Are you familiar with software detection or alerts in EHRs?
- Do you think there should be a protocol developed for AKI or dehydration based on risk factors, similar to “fall risk”?
Conclusion
As we conclude this course on Acute Kidney Injury (AKI) and dehydration in the elderly, it is important to understand that older adults are at a higher risk for both dehydration and AKI due to age-related physiological changes, coexisting medical conditions, and the potential nephrotoxic effects of certain medications.
Recognizing the intricate relationship between kidney function and fluid balance is paramount. Essentially, dehydration can precipitate AKI, and AKI can exacerbate dehydration by impairing the kidneys’ ability to concentrate urine and regulate fluid balance.
Healthcare providers must be adept at identifying early signs of dehydration and AKI, especially in older adults, where symptoms may be subtle or misdiagnosed. Regular monitoring of fluid balance, kidney function, and medication management is crucial. A comprehensive and proactive approach to managing hydration and kidney health in older adults can significantly reduce the incidence of AKI and improve the quality of life for this vulnerable population.

References + Disclaimer
- Chippa V, Roy K. Geriatric Cognitive Decline and Polypharmacy. [Updated 2023]. StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK574575/
- Gameiro, J., Fonseca, J. A., Outerelo, C., & Lopes, J. A. (2020). Acute kidney injury: from diagnosis to prevention and treatment strategies. Journal of Clinical Medicine, 9(6), 1704. https://doi.org/10.3390/jcm9061704
- González, M.E., Fuentes, N.A., Franco, C.L., Lombardi, M., Musso, C.G., Esperatti, E.M. (2021). Frailty in Acute Kidney Injury Critical Care Patient. In: Musso, C.G., Jauregui, J.R., Macías-Núñez, J.F., Covic, A. (eds) Frailty and Kidney Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-53529-2_10
- Goyal A, Daneshpajouhnejad P, Hashmi MF, et al. Acute Kidney Injury. [Updated 2023 Nov 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441896/
- Johnson RJ, Floege J, & Tonelli M. (2023). Comprehensive Clinical Nephrology. Seventh edition. Elsevier; 2023.
- Musso CG, Jauregui JR, Macías-Núñez JF, Covic A. (2021). Frailty, and Kidney Disease : A Practical Guide to Clinical Management. Springer; 2021. doi:10.1007/978-3-030-53529-2
- Perazella, M. A., & Rosner, M. H. (2022). Drug-Induced Acute Kidney Injury. Clinical journal of the American Society of Nephrology: CJASN, 17(8), 1220–1233. https://doi.org/10.2215/CJN.11290821
- Scientific Animations. (2020). 3D medical animation still showing kidney structure, its layers, renal artery, veins & ureter. Items with VRTS permission confirmed. CC-BY-SA-4.0. https://www.scientificanimations.com/wiki-images
- Taylor K, Tripathi AK, Jones EB. Adult Dehydration. [Updated 2022 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK555956/
- Walter, L. C. (Ed.). (2021). Current diagnosis & treatment : geriatrics (3rd edition.). McGraw-Hill.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
