Aesthetic Nursing: Injectables
Contact Hours: 2
Author(s):
Abbie Schmitt MSN, RN
Course Highlights
- In this Aesthetic Nursing: Injectables course, we will learn about the actions of neurotoxin injections and dermal fillers.
- You’ll also learn the possible complications and side effects of aesthetic injectables.
- This course will give you a broader understanding of aesthetic injectable post-treatment care interventions and patient education topics.
Introduction
There is a common thread among nursing specialties in aiming to improve individuals’ quality of life. Aesthetic nursing involves advocating for those who want to improve or change their physical appearance. It is a rapidly growing specialty, with injectables becoming a prominent treatment. This course is designed to help you better understand neurotoxin and dermal filler injections, how they work, areas they can treat, and pertinent topics for patient education.
Aesthetic Nursing: An Overview
Registered nurses who wish to enter the field of aesthetic nursing can obtain specialized training in aesthetic and cosmetic services. Aesthetic nurses’ duties can include neurotoxin injections, dermal filler injections, tattoo removal, dermabrasion, laser hair removal, chemical peels, and non-surgical body contouring (2). Nurses in this field also have the following duties:
- Discuss and consult with patients to understand their aesthetic concerns
- Scheduling patients for procedures
- Performing medical assessments, screening, and physical nursing exams
- Noninvasive cosmetic treatments
- Performing pre- and post-operative nursing assessment and care
- Preparing and sterilizing instruments and surgery suites
- Assisting with surgeries and procedures
Certification is required in each specific injection before being qualified; for example, Botox certification courses are available to take and become certified (2). Education programs are available from a variety of institutions, but it is vital that they are accredited. The certifications typically involve hands-on experience with aesthetic nurses or physicians. The following specialties would yield appropriate experience:
- Plastic surgery
- Aesthetic surgery
- Cosmetic surgery
- Facial plastic surgery
- Dermatology
- Ophthalmology
Experienced aesthetic nurses can become a Certified Aesthetic Nurse Specialist (CANS) through the Plastic Surgical Nursing Certification Board (2). The CANS certification exam requires the following prerequisites: (2)
- Current registered nurse (RN) license
- At least two years of experience as an RN working with a board-certified doctor in plastic surgery or another related specialty
- At least 1,000 practice hours in a medical aesthetic specialty in the last two years
- Approval from a supervising board-certified physician
Ask yourself...
- Can you identify various healthcare environments or offices that would employ a nurse with an aesthetic specialty certification?
- How would nursing knowledge of anatomy and physiology apply to aesthetic or cosmetology?
Neurotoxin Injections
Neurotoxin use in the medical aesthetic field is the ultimate example of “When life gives you lemons, make lemonade.” Except in this case, when life gives you botulism, use it as an injectable that makes you feel youthful and beautiful.
Injection of neurotoxins, or botulinum neurotoxins type A (BoNT/A), is the most commonly performed non-surgical aesthetic procedure in the world (7). Clostridium botulinum is an anaerobic, spore-forming bacterium that creates a toxin under certain conditions (7). This neurotoxin has an interesting history of incidental findings leading to research and procurement. Botulism, which is a dangerous form of food poisoning that causes symmetric overall muscle paralysis and death, was first described by Dr. Justinus Kerner in 1817. Physicians and scientists were perplexed by the neurotoxin effects. In 1985, following an illness outbreak among people who ate raw, unsalted ham, a professor discovered and studied this bacterium and toxin; this led to years of continued research and isolation of the molecule by other scientists (7).
Although botulinum toxin is widely known for cosmetic use, the toxin was originally used for the treatment of dystonia and other involuntary muscle movements (7). The United States Food and Drug Administration (FDA) approved the use of botulinum neurotoxin type A for cosmetic purposes in 2002. Its popularity and use have grown significantly since that time.
How Neurotoxin Injections Work
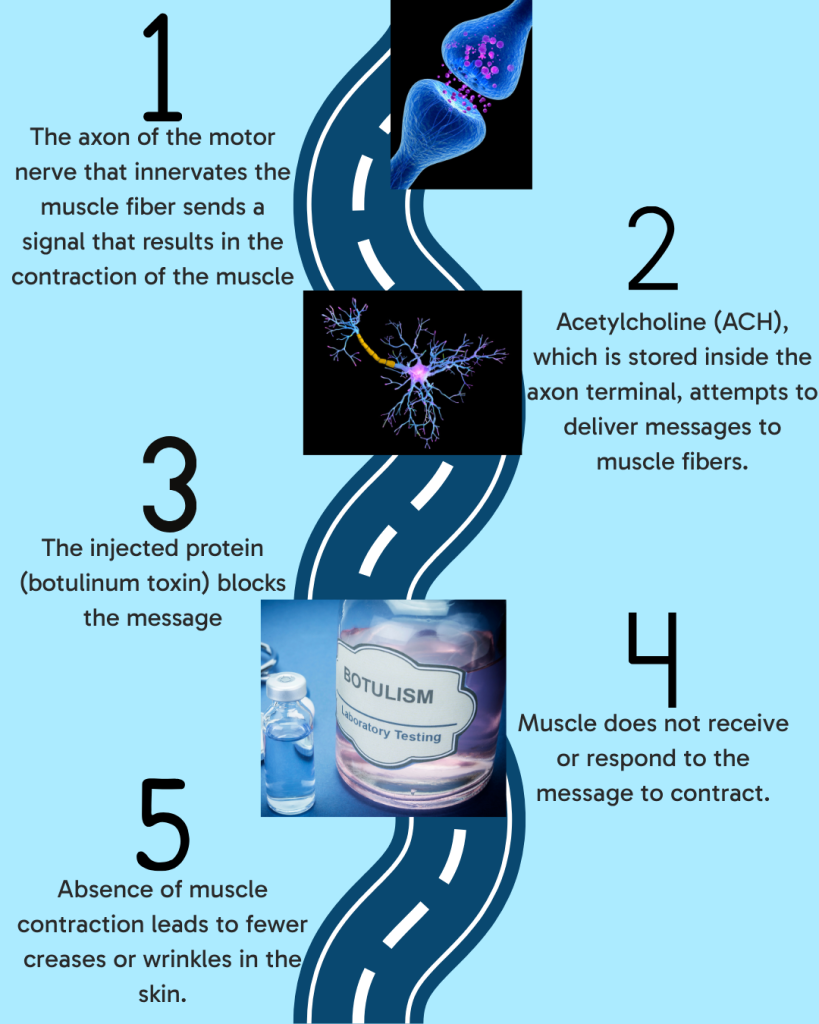
Clostridium Botulinum is a bacterium that produces a double-chain polypeptide molecule, known as the botulinum toxin. A brief explanation of botulinum toxin action is that the toxin blocks nerve signals that result in muscle contraction. Once the muscles relax, it firms the skin and reduces the lines created by expressions (smiling, frowning).
For nurses, it’s important to dig a little deeper into the mechanism of action. The pathophysiology of muscles and nerve fibers is important to examine when understanding the action of the toxin, as the toxin blocks certain normal actions. The axon of the motor nerve innervates the muscular fiber at the motor end plate (8). Acetylcholine (Ach) is stored inside the axon terminal. Acetylcholine is a neurotransmitter, which is a messenger that delivers messages or stimulation from the nerve to the muscle. Following the stimulus of the motor neuron, the acetylcholine vesicle binds with the SNARE complex attached to the presynaptic membrane, resulting in a change to the membrane and contraction of the muscle (8).
Botulinum toxins act at four different sites: the neuromuscular junction, autonomic ganglia, postganglionic parasympathetic nerve endings, and postganglionic sympathetic nerve endings that release acetylcholine. The toxin blocks the message encoded in acetylcholine. Essentially, intramuscular administration of botulinum toxin acts at the neuromuscular junction to cause muscle paralysis by inhibiting the release of acetylcholine from presynaptic motor neurons. The toxin acts as a roadblock in the pathway of neurotransmission.
Ask yourself...
- Can you describe the pathway of a message from the neural system to the muscular system?
- What is the basic function of the neurotransmitter acetylcholine?
- Why would paralyzing the muscle lead to fewer folds in the skin?
Available Neurotoxins and Benefits
Over the years, researchers have discovered multiple subtypes of botulinum toxin type A and explored the benefits. A different manufacturer produces each. In 2009, the US FDA mandated non-trade names for all approved BoNT/A in an effort to clarify differences in the formulations (7). The chemical formulations of the four BoNT/A are commonly known as Onabotulinum Toxin (Botox®), Abobotulinum Toxin (Dysport®), Incobotulinum Toxin (Xeomin®), and Prabotulinumtoxin-xvfs (Jeuveau™) (7). The formulations have different dosing curves and formulary ratios and cannot be substituted by pharmaceutical companies.
The dose of BoNT/A is measured in units. The formulations vary depending on each manufacturer’s production and process. Essentially, the potency of each BoNT/A is different and not interchangeable (7). For example, the concentration of onabotulinumtoxinA (Botox®) is 4 units per 0.1 mL and sold as 100 units in 2.5 mL solution per vial. In comparison, abobotulinumtoxinA (Dysport®) is 10 units per 0.1 mL and sold as 300 units in 3.0 mL solution per vial (5).
Although the formulary and dosing differ, all the neurotoxin formularies work in a similar manner and primarily function by inhibiting muscle contractions.
- Medical Uses:
- Muscle spasms
- Hyperhidrosis (excessive sweating)
- Dystonia
- Chronic migraines
- Overactive bladder
- Aesthetics or Cosmetic Use:
- Facial wrinkle or line reduction
Types of BoNT/A neurotoxins
- OnabotulinumtoxinA (1)
- The most common and widely recognized botulinum toxin
- Known as the “Botox” brand
- Manufactured by Allergan Aesthetics
- AbobotulinumtoxinA (5)
- Similar use of neurotoxin action to induce muscle paralysis and a loss of muscle contraction
- Faster onset of action and broader diffusion than OnabotulinumtoxinA
- The most notable manufacturer is the French company Ipsen
- The brand name is Dysport (studies found that Dysport had greater amounts of active neurotoxin, which may result in a clinically longer duration of action)
- IncobotulinumtoxinA (5)
- Considered a “naked” toxin without complexing proteins, which possibly reduces the risk of antibody formation
- Xeomin is the most notable brand, produced by Merz
- PrabotulinumtoxinA (8)
- Brand names are Nabota and Jeuveau
- Slightly different protein structure than other BoNT/A neurotoxins
Treatment Areas
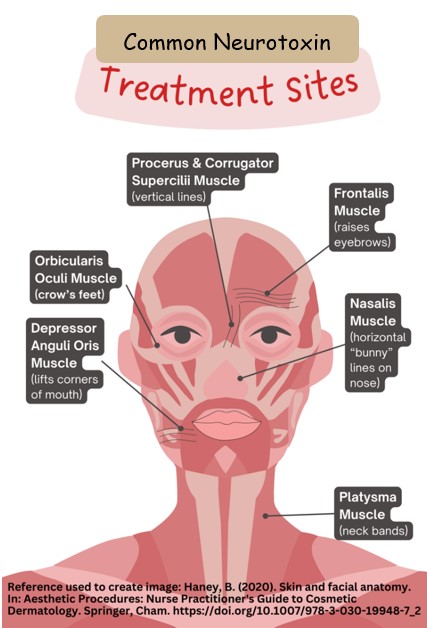
A thorough knowledge of facial muscles of expression and mastication is essential for more positive outcomes. The aesthetic nurse must recognize that facial muscles lie in three dimensions, rather than just two dimensions. The dimensions overlap one another while having opposite functions. Depth is a key component because it may appear the injection is going into a specific muscle, but it is possible to pass into another muscle incidentally. It is also essential to know where each muscle originates and inserts when determining which depth to inject.
To get a better understanding of treatment areas, it is helpful to look in the mirror and make different facial expressions such as smiling, frowning, and laughing. The areas that crease and show signs of wrinkles in the skin would be a possible treatment area. These wrinkles are referred to as rhytids and result from repeated contraction of the muscle underneath the facial skin. Our facial structure consists of skin, subcutaneous fat, fascia, muscle, and bone. There are 40 muscles that make up the face, and each has a specific function that results in expression (6).
The goal of targeting these muscles is to reduce the contraction, either voluntary or involuntary, of specific muscles. Common muscular targets for neurotoxin injections in the upper face include the orbicularis oculi, procerus, and corrugator supercilli muscles (3). The orbicularis oculi muscle is responsible for closing the eyelids, so contraction of the muscle causes creasing in the skin that may lead to wrinkles. The procerus and corrugator supercilia muscles are known as the culprits in the development of glabellar frown lines in the forehead area. The frontalis muscles lift the eyebrows, causing the skin layers to fold, and can lead to wrinkles (6). Considering every person has unique facial expressions and habits, there may be other areas that could benefit from neurotoxin injections.
It is important to understand that FDA approvals for injectable neurotoxins are for specific muscles and are not blanket approvals (10). Several muscles should not be injected.
Contraindications
The following are contraindications for neurotoxins: (3, 7)
- Peripheral motor neuropathies or neuromuscular disorders are the main contraindications
- This includes the following: amyotrophic lateral sclerosis, Lambert-Eaton syndrome, multiple sclerosis, myasthenia gravis (3)
- The neurotoxin injection could exacerbate muscle weakness and complications
- Active infection at injection sites
- History of allergic reaction to botulinum toxin constituents
- Body dysmorphic disorder (BDD)
- Mental disorder characterized by a persistent, intense focus, and anxiety over perceived body defects
- Studies show that cosmetic procedures intensify BDD symptoms and have led to suicidal and violent behavior in some patients
- Pregnancy and breastfeeding
- The FDA classifies botulinum toxin as a category C drug (7, 9,10)
- There is a precaution due to a lack of evidence and studies on injection during pregnancy and breastfeeding
- Botulinum toxin is not expected to enter the systemic circulation and should not cross the placental barrier, but additional evidence that supports its safety during pregnancy is needed before the neurotoxin is offered to pregnant women or breastfeeding mothers
Side Effects
- Localized side effects
- Injection site pain
- Redness
- Bruising
- Bleeding at the injection site
- Headaches
- Flu-like symptoms
Complications
Complications with neurotoxin injections can be placed into two categories: local injection reaction and undesired effects (3, 8)
- Infection
- Paresthesia or dysesthesia
- Unintended muscle effect (adjacent muscle can be affected unintentionally, thus unintended aesthetic effect may occur, such as eyelid droop or altered smile)
- Diffusion of toxin into neighboring muscles and nerve endings
- Sustained neurotransmission blockade producing effects akin to anatomic denervation
- Development of antibodies with subsequent immunosuppression or resistance
- Facial asymmetry
- Allergic reaction (rare occurrence, less than 0.1%)
The actions and effects of these neurotoxins have been studied extensively, and no indications of long-term neuronal damage with repeated use of therapeutic doses used in aesthetics have been found (6). However, long-term use may alter the appearance of the recipient, not always matching their desires and expectations.
It is important to recognize antidotes when understanding pharmacology. As nurses, we are typically aware of antidotes, such as naloxone HCl (Narcan) for the reversal of opioids. However, this is not the case for neurotoxins, as there are currently no available drugs to counteract the effects. A key component of patient education is to communicate that BoNT/A cannot be reversed once injected, and its activity continues until it naturally ceases.
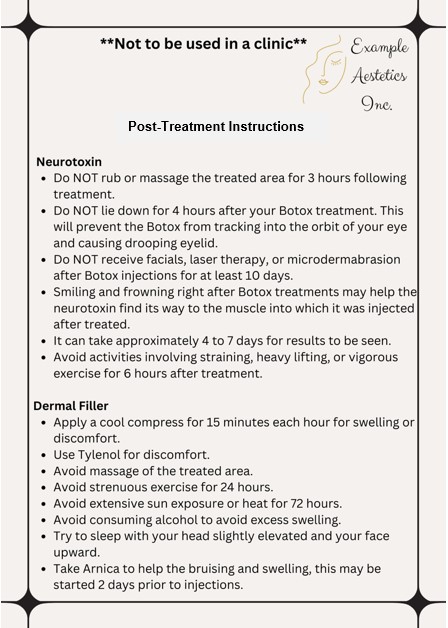
After Care
Patient education is important following neurotoxin injections to avoid complications or the spread of toxins to the surrounding area
Interventions
- Pain control
- Patient Education
Examples of precautions after treatment
- Avoid lying supine following treatment for four hours
- Avoid massaging or applying heat to the treatment area
- Avoid restrictive headwear (hats, bands)
- Avoid activities that cause flushing or sweating on the day of treatment (the certified provider of injections will determine time frame)
- Exercising heavily
- Consuming alcohol
- Hot tub use
Ask yourself...
- Can you name the available neurotoxin injection products?
- Why do you think there are only certain muscles approved for neurotoxin injections?
- What are the typical, expected side effects of neurotoxin injectables?
- Are the effects of neurotoxins reversible once injected?
Duration
Studies have found that each patient has a different duration of effects. The relaxation of the treated muscles starts to become noticeable in about 1-5 days (7). The peak of effect is about two to four weeks (8). The effect typically lasts about three to four months in skeletal muscle nerve terminals for facial cosmetic injections and about one year for injections into the autonomic nerve terminals (7). A concern is how this toxin is excreted. The unbound toxin is believed to be diluted in the lymphatic system, unable to bind elsewhere due to low concentration, and excreted from the kidneys as a waste byproduct (7).
The effects and properties of BoNT/A have been studied extensively, and there are no indications of long-term neuronal damage with repeated use of therapeutic doses for cosmetic use (7). An additional characteristic of BoNT/A is that it cannot be reversed once injected, and its activity continues until it naturally ceases. Currently, there are no available drugs to counteract the effects of the neurotoxin.
Ask yourself...
- What is the duration and peak of effect for BoNT/A?
- Can you discuss why an individual with Body Dysmorphic Disorder would not be a good candidate for this procedure?
- Have you cared for a patient with nerve damage and loss of muscle contractility?
- Why do you think it is important to recognize the different dosages and concentrations of neurotoxin injection brands?
Dermal Fillers
Aesthetic nurses can also specialize in injecting dermal fillers. Temporary dermal fillers are the second most requested, nonsurgical aesthetic procedure worldwide, with neurotoxin injections being the most popular (7).
How Dermal Fillers Work
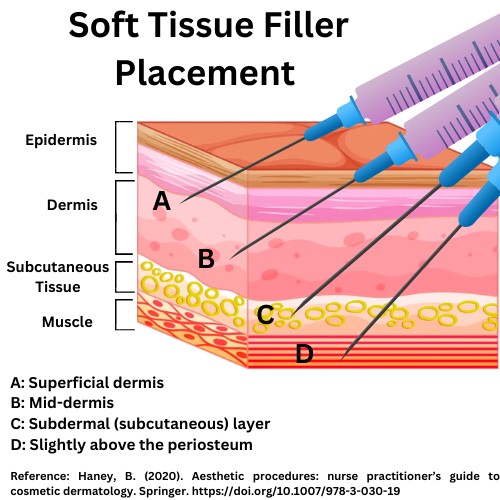
When you consider dermal fillers, recognize the term filler, and think “volume” and “plumpness.” Imagine a road you frequently travel on, and it is filled with potholes and cracks. A company would use a material with similar consistency (asphalt, concrete) to fill in the imperfections, creating a smooth surface. Dermal fillers use naturally occurring components or biocompatible synthetic material in the gel to fill in areas such as lines, wrinkles, or hollow areas. They can also add volume to lips and various areas of the body where the patient desires “plumpness.”
The dermal filler is injected underneath the top layer of skin. The depth can vary depending on whether the goal is to reduce lines or wrinkles or to create definition. Wrinkle or crease reduction would be more superficial, while facial contouring is achieved with deeper injections (4).
Ask yourself...
- Can you explain how the angle of insertion should be modified for subcutaneous vs. intramuscular?
- Why do you think symptoms may differ based on the depth of the injection?
- Can you think of reasons the injected material should be biocompatible and biodegradable?
Available Dermal Fillers and Benefits
Knowledge of available dermal filler pharmacology is an important aspect of aesthetic practice. There are several different types of fillers: temporary or biodegradable, stimulant, and permanent or non-biodegradable fillers. Each type of filler has specific properties, and the choice depends on the desired result and longevity. The most commonly used temporary fillers are hyaluronic acid (HA), calcium hydroxyapatite (CaHA), and poly-L-lactic acid (PLLA) (7).
Hyaluronic Acid (HA)
Hyaluronan, or HA, is a linear polysaccharide found in the skin, as well as epithelial, connective, and other tissues (7). Polysaccharides are responsible for the skin’s natural ability to hydrate and retain water, so as we age, it is believed that HA diminishes and can lead to decreased tightness of skin. Providers find this product convenient because allergy testing is unnecessary, as it is already found in the skin and does not contain protein molecules (7). HA fillers can be reversed with hyaluronidase, which makes them an attractive option for many providers and patients (7).
Developers of HA fillers use slightly different technologies. Several HA filler products consist of sterile, biodegradable, and clear gel implants produced by Streptococcus bacteria and are developed with a fermentation process and chemically crosslinked butanediol diglycidyl ether (BDDE) (7). If the natural form of HA were injected, it would break down quickly, so these processes have made injectable HA stable and more resistant to breakdown.
Calcium Hydroxylapatite (CaHA)
Calcium hydroxyapatite (CaHA) is made of the same compound as human bone (7). CaHA is an opaque, sterile, semi-solid, cohesive implant, whose principal component is synthetic calcium hydroxylapatite suspended in a gel carrier of glycerin, sodium carboxymethylcellulose, 0.3% lidocaine hydrochloride, and sterile water (7). The carrier gel dissipates within several weeks, and the CaHA slowly breaks down into calcium and phosphate ions (7). The characteristics of CaHA make it radiopaque and visible on computed tomography (CT) scans and X-ray studies. CaHA was initially used as a marker for imaging studies for urinary stress incontinence. The consistency of a CaHA filler is typically thicker and effects last longer than hyaluronic acid fillers. Calcium hydroxylapatite is also reported to help stimulate natural collagen production, and it is typically used for deeper lines and wrinkles.
Poly-L-lactic Acid (PLLA)
Poly-L-lactic Acid (PLLA) is a temporary filler, and the active ingredient is a synthetic biodegradable polymer that is used for soft tissue augmentation (7). Unlike the others, this filler is synthetic instead of a natural component of the body. However, it is biocompatible and biodegradable, which means it has proper biological requirements that are not harmful to living tissue. The product is a freeze-dried powder of PLLA and must be rehydrated with 5 mL sterile water per vial prior to injection (7). PLLA has been used for years in devices, such as dissolvable stitches.
Other Dermal Fillers
- Polymethylmethacrylate (PMMA)
- Synthetic, biocompatible substance
- Takes the form of a tiny ball that remains beneath the skin
- FDA approved
- Contains collagen
- Autologous fat injections
- Autologous (“from the patient”) fat used for injection
- Requires surgery that harvests fat from another site, typically using liposuction
- Should only be performed by an experienced, board-certified cosmetic surgeon
Ask yourself...
- Can you think of various drugs that have reversal medications?
- Have you ever administered a reversal agent?
- Can you name the components of HA and CaHA injections?
- Are you familiar with biocompatible materials?
Treatment Areas
Common treatments using dermal fillers include cheek augmentation, lip enhancement, perioral and naso-labial areas, glabellar region, temples, jawline, earlobes, hands, and sub-orbital areas. Scar treatments can be used with the proper use of dermal fillers (4). The selection of the treatment area should focus solely on the concern of the patient. Realistic goals and expectations are important. It is important for patients to incorporate the depth of injection into expectations, as deeper injections may yield more noticeable results.
Contraindications
The following are contraindications for dermal fillers:
- Active infection at an adjacent site
- Intraoral, mucosal, or dental infection
- Herpes labialis for lip injection
- History of allergic reaction or hypersensitivity to the filler
- Allergy to lidocaine
- Glabellar necrosis (7)
- Skin necrosis due to interruption of the vascular supply to the area from compression or obstruction of the vessel
- Rare but severe potential complications after injection of hyaluronic acid (HA)
- Documented cases
- Body dysmorphic disorder (BDD)
- Mental disorder characterized by intense anxiety over perceived body defects
- As mentioned earlier, studies show that cosmetic procedures intensify BDD symptoms and have led to suicidal and violent behavior in some patients
Side Effects
The side effects of dermal filler injection procedures can be broken down into injection site reactions, adverse effects resulting from an improper injection technique, allergic reactions, and vascular-mediated events.
Injection site reaction
The site of the filler injection can result in swelling, bruising, redness, pain, itching, and infections from the needle puncture of the skin. A small-to-moderate amount of swelling and bruising is expected and usually lasts no more than a few days (4). The swelling and bruising can be improved by applying icepacks before, after, or at both times during a treatment session, and unnecessary anti-coagulant use should be avoided.
Infection of the injection site is not common but would typically result from inadequate cleaning of the treatment area or equipment. Etiologies include fungal, bacterial, or viral, and depending on the etiology, infections can present as redness, tenderness, swelling, fever, and the presence of pustules, papules, or vesicles (7). Patients who have recurrent herpes simplex virus (HSV) eruptions may develop an outbreak as a result of treatment, so prophylaxis may be advised.
Adverse effects from improper injection technique
Accidental intramuscular injection of a synthetic filler other than hyaluronic acid and collagen may create lumps of material and cause migration to distant sites due to the contraction of the muscle (7). Unevenness or asymmetry can also result from improper injection of the filler. Massage following the injection can correct some faults during the procedure (4).
The Tyndall effect occurs when clear gel fillers are placed too superficially in the dermis, causing a bluish discoloration of the skin. This appearance is due to the gel’s refraction of light and the melanin in the dermis (7). The Tyndall effect will usually persist for long periods of time until the product is removed.
Allergic or hypersensitivity reactions
Unwanted immune reactions are rare but have been reported. Recent studies find that these sensitivities are more commonly delayed and not immediately noted (4). Granuloma formation is a systemic immune response (type IV hypersensitivity reaction), and the tissue at every site of injection would react at the same time (7). Acute assessment is important to differentiate between a granuloma and a nodule. While nodules may have a variety of causes, they are not considered an immune response.
Vascular-mediated events
Obstruction of blood vessels causes necrosis of the tissues, so pressure or blocking of veins and arteries in the filler procedure should be avoided. Aspiration should always be performed (4). To avoid false-negative results, at least a 27-gauge needle should be used (4). The injector should keep the instrument moving throughout the injection, as static injection in one area increases the risk of vascular pressure and should be avoided.
Hair loss and blindness are rare occurrences. Temporary and reversible alopecia has been reported following large subdermal bolus injections behind the hairline (4). The glabella (the area between the eyebrows, just above the nose) is at greatest risk for complications because it is supplied by the supratrochlear artery, which is connected to the ophthalmic artery. There is a risk of retinal embolism with intravascular injections to this area.
After Care
Immediately after the treatment, the most commonly reported side effects include temporary tenderness, bruising, and/or swelling at the injection site. The majority of patients have complete resolution at or before 14 days (7). Each provider will have specific post-treatment instructions.
Examples of Suggested Post-Treatment Recommendations:
- Swelling: Cold compresses, sleeping with the head elevated, and/or the use of an antihistamine may be recommended
- Bruising: Cold compresses
- Mild pain: Tylenol may be recommended; aspirin or Ibuprofen are not recommended as they may cause more bruising (7)
- Avoid exercise or any kind of strenuous activity for a period of time (example: 24 hours)
- Avoid alcohol intake: Alcohol can make bruising and swelling worse
- Skip the lipstick: For the first day after your injection, avoid putting on lipstick, instead using Aquaphor or Vaseline applied with a clean Q-Tip
- Avoid sun exposure
- Follow-up visits
Duration
Dermal fillers have an effect duration from approximately 6–24 months, depending on the type and depth of placement of the filler. Aesthetic results and the amount of time before noticing results vary among the types of fillers as well. The duration also depends on the amount of movement in the location. For example, the frown line area is more frequently moved due to facial expression, while the ear lobes are not. The less movement and creasing of the area will lead to longer-lasting effects of fillers.
The effects of HA fillers are noticed immediately and generally last up to two years, depending on the location and desired effects (7). PLLA will yield results over time and is not immediately noticeable. It can take more than one session for the patient to notice a change in appearance (7). Modifying expectations is an important aspect of patient education for patients receiving PLLA. The tiny particles of PLLA become encapsulated by fibrous tissue and provide visible volume for more than 18 months (7). CaHA has an immediate effect and lasts about one to two years (7).
Patient Education
Teaching is one of the most important interventions that nurses can provide to their patients. Teaching individuals receiving an aesthetic injection equips them with the information they need to make the best decisions for their health and well-being. Teaching also helps patients to perform self-care and identify risks and complications. Patients are unique in their knowledge base and understanding.
Causes of Knowledge Deficit (Related to):
- Lack of exposure to aesthetic procedures
- Misunderstanding of information
- Complexity of components of neurotoxins and dermal fillers
- Cognitive limitations
- Lack of interest/refusal to learn
Expected Outcomes
- The patient will verbalize understanding of the specific injection and all available options.
- The patient will identify risk factors and complications.
- The patient will identify expected side effects.
- The patient will participate in the learning process.
Nursing Interventions
- Create a quiet learning environment
- Include the patient in their plan
- Use multiple teaching methods:
- Verbal instructions
- Written materials
- Instructional videos
- Illustrations of what to expect
- Provide continued learning resources:
- Accredited websites
- Support groups
- Avoid overloading
- Encourage questions
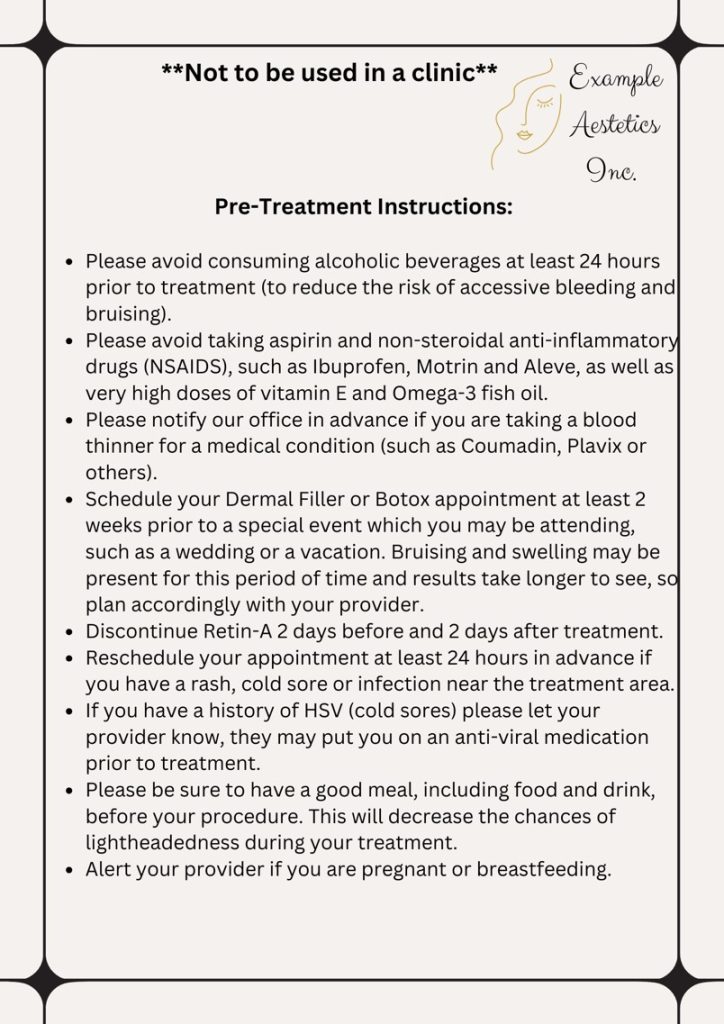
Teaching Before Treatment
Prior to treatment, the patient should receive teaching on the type of dermal fillers available, specific injection site decisions, and risks associated with the injection. Visuals are important to explain what to expect. A comprehensive evaluation of each client’s desires is vital to complete the appropriate treatment. As mentioned, patients should be alerted to the reversibility of the procedures. The provider should complete a medical history evaluation and a physical examination and review pertinent conditions that could be considered contraindications.
Nurses should also reinforce the following recommendations established by the FDA: (10)
- Seek a licensed health care provider with experience in the fields of dermatology or plastic surgery
- Select a health care provider who is trained to perform the neurotoxin or dermal filler injection procedure
- Do not inject yourself with dermal fillers
- Do not purchase dermal filler products online, as they should only be distributed to licensed health care providers
Available Dermal Fillers and Benefits
Knowledge of available dermal filler pharmacology is an important aspect of aesthetic practice. There are several different types of fillers: temporary or biodegradable, stimulant, and permanent or non-biodegradable fillers. Each type of filler has specific properties, and the choice depends on the desired result and longevity. The most commonly used temporary fillers are hyaluronic acid (HA), calcium hydroxyapatite (CaHA), and poly-L-lactic acid (PLLA) (7).
Hyaluronic Acid (HA)
Hyaluronan, or HA, is a linear polysaccharide found in the skin, as well as epithelial, connective, and other tissues (7). Polysaccharides are responsible for the skin’s natural ability to hydrate and retain water, so as we age, it is believed that HA diminishes and can lead to decreased tightness of skin. Providers find this product convenient because allergy testing is unnecessary, as it is already found in the skin and does not contain protein molecules (7). HA fillers can be reversed with hyaluronidase, which makes them an attractive option for many providers and patients (7).
Developers of HA fillers use slightly different technologies. Several HA filler products consist of sterile, biodegradable, and clear gel implants produced by Streptococcus bacteria and are developed with a fermentation process and chemically crosslinked butanediol diglycidyl ether (BDDE) (7). If the natural form of HA were injected, it would break down quickly, so these processes have made injectable HA stable and more resistant to breakdown.
Calcium Hydroxylapatite (CaHA)
Calcium hydroxyapatite (CaHA) is made of the same compound as human bone (7). CaHA is an opaque, sterile, semi-solid, cohesive implant, whose principal component is synthetic calcium hydroxylapatite suspended in a gel carrier of glycerin, sodium carboxymethylcellulose, 0.3% lidocaine hydrochloride, and sterile water (7). The carrier gel dissipates within several weeks, and the CaHA slowly breaks down into calcium and phosphate ions (7). The characteristics of CaHA make it radiopaque and visible on computed tomography (CT) scans and X-ray studies. CaHA was initially used as a marker for imaging studies for urinary stress incontinence. The consistency of a CaHA filler is typically thicker and effects last longer than hyaluronic acid fillers. Calcium hydroxylapatite is also reported to help stimulate natural collagen production, and it is typically used for deeper lines and wrinkles.
Poly-L-lactic Acid (PLLA)
Poly-L-lactic Acid (PLLA) is a temporary filler, and the active ingredient is a synthetic biodegradable polymer that is used for soft tissue augmentation (7). Unlike the others, this filler is synthetic instead of a natural component of the body. However, it is biocompatible and biodegradable, which means it has proper biological requirements that are not harmful to living tissue. The product is a freeze-dried powder of PLLA and must be rehydrated with 5 mL sterile water per vial prior to injection (7). PLLA has been used for years in devices, such as dissolvable stitches.
Other Dermal Fillers
- Polymethylmethacrylate (PMMA)
- Synthetic, biocompatible substance
- Takes the form of a tiny ball that remains beneath the skin
- FDA approved
- Contains collagen
- Autologous fat injections
- Autologous (“from the patient”) fat used for injection
- Requires surgery that harvests fat from another site, typically using liposuction
- Should only be performed by an experienced, board-certified cosmetic surgeon
Example of Pre-Treatment Instructions:
Ask yourself...
- What are some of the FDA warnings and recommendations for aesthetic injections?
- Can you describe different tools for patient education?
- What are some medications to avoid before receiving aesthetic injections?
- Are there any reasons to cancel injection procedures?
Teaching After Treatment
Each aesthetic provider should provide thorough educational materials to clients to support the initial verbal instructions.
Teaching Topics include:
- Education of pain relief measures (example: ice, Tylenol)
- Education on activities to avoid (exercise, sun exposure)
- Education on when to seek immediate medical attention:
- Severe pain
- Vision changes
- White, gray, or blue appearance of skin near the injection site
- Signs of a stroke (difficulty speaking, numbness or weakness in your face, arms, or legs, difficulty walking, visual changes, face drooping, and/or severe headache; B.E.F.A.S.T. Stroke Algorithm)
Example of Post-Treatment Instructions:
Ask yourself...
- What are examples of reasons a patient should seek immediate medical attention after an injection procedure?
- What actions or movements can impact the effect or appearance of the injections?
- Why do you think facials or dermabrasion should be avoided after treatment?
- Have you cared for a patient who had anxiety following a procedure?
Conclusion
Hopefully, you will better understand neurotoxin and dermal filler injections, how they work, areas they can treat, and pertinent topics for patient education. Whether you are an aesthetic nurse or considering pursuing this specialty, knowledge of injectables is valuable. The popularity and prevalence of aesthetic nursing will likely continue to grow and advance.
Ask yourself...
- Can you discuss the scope of practice of an aesthetic nurse?
- Why do you think nurses must obtain additional certification for aesthetic injectables?
- Why do you think fat injections from the patient’s own body may have benefits?
- Have you ever cared for a patient with a cosmetic treatment with undesirable results?
- What topics should the aesthetic nurse prioritize for patient education?
References + Disclaimer
- Allergan. (2017). Botox® cosmetic prescribing information [package insert]. Irvine: Allergan. Retrieved from https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/103000s5302lbl.pdf
- American Association of Aesthetic Medicine & Surgery (AAAMS). (2023). What you need to know before starting your aesthetic nurse training. Retrieved from https://aaams.net/considering-becoming-an-aesthetic-nurse-heres-what-you-need-to-know/
- Biello A., Oney R., & Zhu, B. (2022). Botulinum toxin treatment of the upper face. Treasure Island (FL): StatPearls Publishing. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK574523/
- Chao, & Cotofana, S. (Eds.). (2022). Adapting dermal fillers in clinical practice (First edition.). CRC Press.
- Field, M., Splevins, A., Picaut, P., van der Schans, M., Langenberg, J., Noort, D., Snyder, D., & Foster, K. (2018). AbobotulinumtoxinA (Dysport®), OnabotulinumtoxinA (Botox®), and IncobotulinumtoxinA (Xeomin®) neurotoxin content and potential implications for duration of response in patients. Toxins, 10(12), 535. https://doi.org/10.3390/toxins10120535
- Han, J., He, Y., Liu, K., & Yang, Q. (2018). Necrosis of the glabella after injection with hyaluronic acid into the forehead. The Journal of craniofacial surgery, 29(7), e726–e727. https://doi.org/10.1097/SCS.0000000000004987
- Haney, B. (2020). Aesthetic procedures: nurse practitioner’s guide to cosmetic dermatology. Springer. https://doi.org/10.1007/978-3-030-19
- Loghem, J. (2023). Botulinum toxin in aesthetic medicine: injection protocols and complication management. CRC Press. https://doi.org/10.1201/9781003370185
- Naik P. P. (2021). Utilities of botulinum toxins in dermatology and cosmetology. Clinical, cosmetic, and investigational dermatology, 14, 1319–1330. https://doi.org/10.2147/CCID.S332247
- U.S. Food & Drug Administration (FDA). (2023). Dermal filler do’s and don’ts for wrinkles, lips and more. Retrieved from https://www.fda.gov/consumers/consumer-updates/dermal-filler-dos-and-donts-wrinkles-lips-and-more
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
