Alcohol Use Disorder: Long Term Effects and Complications
Contact Hours: 2
Author(s):
Joanna Grayson BSN, RN
Course Highlights
- In this Alcohol Use Disorder: Long-Term Effects and Complications course, we will learn about the pathophysiology, diagnostics, and treatments for alcohol use disorder.
- You’ll also learn the long-term effects and complications associated with alcohol use disorder.
- You’ll leave this course with a broader understanding of the resources available to individuals with alcohol use disorder.
Introduction
Alcohol use disorder (AUD) is one of the most widespread psychiatric disorders and is estimated to affect approximately 29 million individuals aged 12 and older in the United States (9). According to the 2021 National Survey on Drug Use and Health, 28.6 million adults ages 18 and older have AUD, and roughly 900,000 adolescents ages 12 to 17 have AUD (7).
Alcohol is the most prevalent misused substance in America, with alcohol-related issues causing more than 85,000 deaths annually in the United States and three million deaths a year globally (9, 12). About 240 million people globally are affected by AUD, especially in Europe and America (9).
AUD is linked to motor vehicle accidents, dementia, depression, homicide, and suicide (9). The condition can also lead to social complications, such as legal problems, relationship issues, and economic stressors (due to the cost of alcohol, required medical care, missed time at work, and job loss). Individuals with AUD can end up isolating themselves from the individuals who are trying to help them most, including family members and friends.
Moderate alcohol use for most adults—no more than two drinks a day for men and one for women—is relatively harmless. An alcoholic drink includes 12 fluid ounces of regular beer, 10 fluid ounces of malt liquor, five fluid ounces of wine, or 1.5 fluid ounces of 80-proof distilled spirits (3, 4). Heavy alcohol drinking is defined as having four or more drinks per day or eight or more drinks per week for women and five or more drinks per day or 15 or more drinks per week for men (4).
Small amounts of alcohol, particularly red wine, can benefit cardiovascular health. Still, heavy drinking can lead to serious health issues, such as cancer, cardiovascular disease, liver disease, osteoporosis, and infections (3, 4). Men are more likely than women to develop AUD, but women’s health suffers more than men’s, even at lower levels of consumption (3)—individuals with lower levels of education and lower income experience AUD more than their counterparts (9).
Drinking can become problematic for those people who have psychological traits of impulsiveness, low self-esteem, and the constant need for attention and approval. Individuals who lack personal insight about drinking can develop AUD. For example, those who use alcohol to emotionally self-medicate (i.e., unwind from a stressful day) can develop alcohol-related issues (3).
Unfortunately, many individuals with AUD deny having a problem with alcohol and therefore do not seek treatment until faced with medical issues or legal complications. Regardless of how severe a patient’s drinking problem may seem, evidence-based treatment that includes medications, behavioral therapies, and support groups can help individuals achieve and maintain recovery.

Ask yourself...
- How extensive is AUD in the United States and globally?
- How many fluid ounces constitute an alcoholic drink for beer, malt liquor, wine, and distilled spirits?
- To which health risks does heavy drinking contribute?
- Which psychological traits can increase the risk of AUD?
Pathophysiology
Alcohol ethanol or ethyl alcohol is a chemical substance found in alcoholic beverages, such as beer, hard cider, malt liquor, wines, and distilled spirits (liquor). Alcohol is the byproduct of yeast fermentation of sugars and starches. Alcohol is also found in some medicines, mouthwashes, and household products, including vanilla extract and other flavorings (4).
Alcohol use disorder is defined by the National Institute on Alcohol Abuse and Alcoholism as a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences (7). The term alcohol use disorder includes the terms alcohol abuse, alcohol dependence, alcohol addiction, and alcoholism. The condition affects brain function and is classified as mild, moderate, or severe (7).
Several evidence-based theories explain the development of AUD in individuals. These theories are (9):
- Positive-effect regulation: This occurs when people consume alcohol to seek positive rewards like pleasure or euphoria. Alcohol may be consumed to enhance social experiences and positive emotions.
- Negative-effect regulation: Individuals may drink alcohol in response to negative or distressing situations as a means to self-medicate and alleviate feelings of anxiety, depression, or low self-worth.
- Pharmacological vulnerability: This theory explains the differences in how individuals respond to the acute and chronic effects of alcohol. Some individuals are more prone to the rewarding effects of alcohol, or they have a reduced ability to metabolize alcohol, thus increasing their chances of developing AUD.
- Deviance proneness: Individuals with a history of deviant behavior or impaired socialization during childhood are more prone to AUD because these individuals use alcohol to self-medicate to alleviate symptoms of anxiety, depression, or low self-worth.
Cytosolic alcohol dehydrogenase (ADH) is the enzyme that metabolizes alcohol in the liver, and this metabolism process produces acetaldehyde as a byproduct. Acetate is then formed by the metabolism of acetaldehyde by the enzyme aldehyde dehydrogenase (ALDH).
Acetate then enters the body’s various metabolic pathways. Additionally, ADH is present in the gastrointestinal tract and the liver, which leads to the initial metabolism of alcohol during its ingestion. This is referred to as first-pass metabolism. The enzyme CYP2E1 of the cytochrome P450 system is upregulated in chronic alcohol users, which leads to an increased rate of alcohol metabolism (9).
Several factors affect the metabolism of alcohol (9):
- Women have a higher initial blood alcohol concentration following consumption because they have a slower first-pass metabolism due to lower levels of ADH; however, women eliminate alcohol faster than men.
- Alcohol elimination declines with age, which is why older adults may experience a lower tolerance to alcohol than when younger, or why they may experience more severe hangover symptoms.
- In pregnancy, the fetal liver has an incomplete expression of enzymes CYP2E1 and ADH, leading to slower alcohol metabolism. This means that the fetus is exposed to the mother’s consumption of alcohol for a prolonged period, increasing the risk of fetal alcohol spectrum disorders.
- Native Americans have been found to metabolize alcohol faster due to the expression of beta-3 Class 1 ADH isoforms than individuals who express only the beta-1 Class 1 ADH isoform.
- When an individual fasts, alcohol metabolism is slowed due to decreased levels of ADH during a fasting state. Alternatively, food intake increases blood flow to the liver and allows fructose and other sugars to speed alcohol metabolism.
- The highest rates of alcohol elimination occur in the late evening versus during the daytime hours.
- Medications that have ADH inhibition or H2 receptor-blocking properties decrease the rate of alcohol elimination. This reduces first-pass metabolism in the stomach and increases blood alcohol levels.
- Heavy drinking increases the expression of the CYP2E1 enzyme, which increases alcohol elimination; however, this is eventually slowed in individuals with advanced liver disease.
Alcohol use can permeate every organ and tissue in the body, resulting in systemic dysfunction. The Complications and Long-Term Effects section explores how alcohol use impacts the body.
Ask yourself...
- Which terms are included in AUD?
- What are the differences between positive-effect regulation and negative-effect regulation theories?
- How does the body’s metabolism process of alcohol work?
- How do pregnancy, fasting, and medications impact the metabolism of alcohol?
Risk Factors
Several factors are believed to contribute to the development of alcohol use disorder, including the home environment, peer interactions, genetic disposition, cognitive functioning, and other mental health disorders, such as schizophrenia, depression, and personality disorders (9).
Risk factors for AUD include (3, 7, 9):
- Genetics and family history. Hereditary factors can influence AUD by as much as 60%. Parents’ drinking habits are directly correlated to the child’s development of AUD. Certain genes have been found to increase an individual’s susceptibility to AUD, including:
- GABRG2 and GABRA2, COMT Val 158Met, DRD2 Taq1A, and KIAA0040.
- Drinking at an early age. Those individuals, especially females, who begin consuming alcohol before age 15 are three times more likely to have AUD. Research indicates that younger people who wait to start consuming alcohol until age 21 are less likely to have AUD.
- Mental health disorders. Psychiatric conditions, such as depression, post-traumatic stress disorder (PTSD), and attention deficit hyperactivity disorder (ADHD) are linked to an increased risk of AUD. Childhood trauma is also strongly correlated with AUD. The presence of both AUDs and psychiatric disorders leads to a worse prognosis for both disorders.
- Social issues. Poverty and lack of education are significant risk factors for AUD.
Additionally, the risk for developing AUD can depend on how much, how often, and how quickly the individual consumes alcohol. Binge drinking and heavy drinking over time can lead to AUD (7).
Ask yourself...
- Which mental health disorders can contribute to AUD?
- Which types of drinking can lead to AUD over time?
- Which genes have been found to increase an individual’s susceptibility to AUD?
- Which social factors are significant risk factors for AUD?
Signs and Symptoms
Nurses need to perform a thorough assessment of those individuals suspected of having AUD. The Cut Down, Annoyed, Guilty, and Eye-opener (CAGE) questionnaire is the widely accepted gold-standard assessment tool and is comprised of these questions (2):
- Have you ever felt that you need to cut down on your drinking?
- Have people annoyed you by criticizing your drinking?
- Have you ever felt bad or guilty about your drinking?
- Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (eye-opener)?
The scoring for the CAGE includes 0 for “no” answers and 1 for “yes” answers, with a total score of two or greater being clinically significant for AUD. However, healthcare providers are encouraged to regard a total score of one or greater as the potential for substance abuse disorder that requires further patient exploration (2).
The Alcohol Use Disorders Identification Test (AUDIT) is a 10-item screening tool created by the World Health Organization (WHO) to assess alcohol-related conditions. There is a patient test that individuals may administer to themselves, and a test designed for healthcare providers to administer to patients. Both tests ask the same questions and use a similar scoring method. The provided answers are 0 for “never”, 1 for “monthly or less”, 2 for “2-4 times a month”, 3 for “2-3 times a week”, and 4 for “4 or more times a week”. A score of 8 or more indicates harmful alcohol use (8, 12).
The AUDIT questions are (8, 12):
- How often do you have a drink containing alcohol?
- How many drinks containing alcohol do you have on a typical day when you are drinking? (The answer options for this question are 0 for “1 or 2”, 1 for “3 or 4”, 2 for “5 or 6”, 3 for “7 to 9”, and 4 for “10 or more”.)
- How often do you have six or more drinks on one occasion?
- How often during the last year have you found that you were not able to stop drinking once you had started?
- How often in the previous year have you failed to do what was typically expected of you because of drinking?
- How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session?
- How often during the last year have you had a feeling of guilt or remorse after drinking?
- How often during the last year have you been unable to remember what happened the night before because of your drinking?
- Have you or someone else been injured because of your drinking? (The answer options for this question are “no”, “yes, but not in the last year”, and “yes, during the last year.)
- Has a relative, friend, doctor, or other healthcare worker been concerned about your drinking or suggested that you cut down? (The answer options for this question are “no”, “yes, but not in the last year”, and “yes, during the last year.)
Nurses and other healthcare professionals can ask patients the additional questions below about their alcohol use to determine the risk and presence of AUD.
In the past year, have you (7):
- Ended up drinking more or longer than you intended?
- Tried to cut back on drinking, but have been unable to do so?
- Experienced symptoms of illness (hangover) related to your drinking?
- Craved a drink so much that it distracted you from your current activity?
- Found that your drinking has interfered with maintaining your responsibilities and obligations regarding home, family, work, or education?
- Continued to drink despite knowing that it caused problems with family and friends?
- Foregone pleasurable activities (hobbies, etc.) to drink?
- Increased your risk for injury (driving, swimming, using machinery, walking in a dangerous area, engaging in unsafe sexual behavior) due to drinking?
- Continued to drink despite the social, health, or economic problems it causes?
- Experienced feelings of anxiety, depression, or memory blackout due to your drinking?
- Did I need to drink more alcohol than in the past to get the same effects?
- Experienced alcohol withdrawal symptoms, such as tremors, restlessness, irritability, nausea and vomiting, sweating, malaise, racing heartbeat, hallucinations, or seizures?
The patient’s positive response to two to three of these criteria indicates mild symptoms, four to five indicates moderate symptoms, and six or more indicates severe symptoms (7).
Patients with AUD often report frequent falls, blackout spells, motor instability and tremors, visual disturbances, hangover symptoms (headache, nausea and vomiting, dry mouth, photophobia), hypertension, heart palpitations, seizures, confusion, mood swings, and sleep disturbances. Social symptoms include school or job instability or loss, relationship separation or divorce, estrangement from family and friends, and homelessness (9). Nurses should also assess patients suspected of AUD for post-traumatic stress disorder, bipolar disorder, panic disorder, anxiety disorder, dysthymic disorder, major depressive disorder, and insomnia (9).
During the assessment of a patient with AUD, nurses may note ataxia, fine motor skill disturbances, mental status changes, mood changes, slurred speech, tachycardia, hypotension, nystagmus, asterixis, ruddy palms, jaundiced coloring, and ascites. Signs of liver disease include hepatomegaly, splenomegaly, cirrhosis, spider angiomata, and liver atrophy (9).
Ask yourself...
- What are the four CAGE alcohol use screening questions?
- When using the AUDIT screening tool, which score indicates harmful alcohol use?
- Which social symptoms are individuals with AUD likely to experience?
- Which physical symptoms may the nurse observe in patients with AUD?
Prevention
The stage in life when a person is exposed to alcohol is an important predictor for alcohol misuse. Adolescence is a time when many people begin experimenting with drinking, and research indicates that drinking before the brain is fully formed (age 26) can negatively impact brain development and compromise cognitive function. The main goal of preventing AUD is to impede, or at least delay, the onset of drinking in the youth population (6).
Adolescents and young adults seek independence and favor transitioning to adult roles. Most of this population drives automobiles and spends more time with friends than family members, thus making them easily influenced by their peer group. This also means that this population is at high risk for alcohol-related injuries, with 5,000 18- to 24-year-olds dying each year due to alcohol-related incidents (6). This group engages in binge drinking, which can lead to blackouts, alcohol poisoning, sexual assault, sexually transmitted infections, and poor academic performance.
Other factors that influence drinking behaviors that should be considered in prevention interventions are genetics, health status, cultural background, educational background, socioeconomic status, community attitudes toward alcohol use, and exposure to social media. Preventative measures should also be geared toward pregnant women and older adults since these populations have special considerations, such as the risk for fetal alcohol spectrum disorders in pregnant women and the inability to effectively metabolize alcohol in older adults that can lead to injuries (6).
Regular screenings for alcohol misuse are a key prevention strategy, and research shows that most patients do not object to being screened for alcohol use and thus are open to receiving advice about alcohol use (6). Evidence also shows that alcohol-related incidents can be prevented by both individual and environmental interventions. For example, college students who are taught to monitor their drinking and how to effectively refuse alcohol when offered can prevent AUD. College communities that restrict happy hours, enforce the minimum drinking age, and prevent alcohol price promotions can decrease the risk of AUD (6).

Ask yourself...
- Which factors are predictors of alcohol misuse?
- Which factors put adolescents and young adults at risk for alcohol-related injuries?
- How do most patients react to screenings and advice regarding alcohol use?
- Which measures can college students and college communities implement to prevent AUD?
Diagnostics and Treatment
The preliminary source used to diagnose alcohol use disorder is the Diagnostic and Statistical Manual of Mental Disorders (DSM).
According to the DSM, the criteria for alcohol use disorder include (11):
A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by two or more of the following, occurring at any time in the same 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use.
- A great deal of time is spent on activities necessary to obtain alcohol, use alcohol, or recover from its effects.
- Craving, or a strong desire or urge to use alcohol.
- Recurrent alcohol use failing to fulfill major role obligations at work, school, or home.
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol.
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use.
- Recurrent alcohol use in situations in which it is physically hazardous.
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
- Tolerance, as defined by either of the following:
- A need for markedly increased amounts of alcohol to achieve intoxication or the desired effect.
- A markedly diminished effect with continued use of the same amount of alcohol.
- Withdrawal, as manifested by either of the following:
- The characteristic withdrawal syndrome of alcohol
- Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms.
Laboratory testing in patients with AUD can indicate blood disorders; vitamin, mineral, and electrolyte imbalances; cancers; cardiovascular disease; liver disease; and pancreatitis. Alcohol-related organ damage can be determined by biomarkers, such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transpeptidase (GGT), phosphatidylethanol (PEth), fatty acid ethyl ester (FAEE), total serum sialic acid (TSA), mean corpuscular volume (MCV), cholesteryl ester transfer protein (CETP), carbohydrate-deficient transferrin (CDT), N-Acetyl-β-Hexosaminidase (Beta-Hex), macrophage migration inhibitory factor (MIF), and D-dopachrome tautomerase (DDT). Biomarkers like alcohol and ethyl glucuronide levels can determine recent alcohol consumption. CDT and PEth levels can help monitor abstinence (1, 9).
Treatment approaches for AUD involve pharmacological and nonpharmacological interventions.
The Federal Drug Administration (FDA) has approved three pharmacological treatments for AUD (9, 10):
- Naltrexone (Vivitrol) is a mu-opioid antagonist that blocks the effects of opioids and is widely used in treating addiction to narcotics. In alcoholism, the medication blocks the effects of naturally occurring opioids, such as endorphins. Therefore, the drinker does not experience any psychological benefits or “high” from the alcohol. Naltrexone also reduces the craving for alcohol, leading to improved abstention rates, reduced number of drinking days, and reduced risk of relapse. The potential side effects—nausea, headaches, and fatigue—also work as an alcohol deterrent.
- Acamprosate is a glutamate agonist that promotes a balance of inhibitory and excitatory neurotransmitters in the brain that are disrupted by alcohol abuse. The discontinued brand name is Campral, but the generic equivalent is still available. The medication can cause weight gain and severe depression.
- Disulfiram (Antabuse) is an alcohol antagonist drug that inhibits ALDH, resulting in the accumulation of acetaldehyde in the body. The purpose of disulfiram is to promote fear in the drinker because drinking alcohol in conjunction with taking the medication can result in severe adverse reactions, including flushing, headache, dyspnea, diaphoresis, dizziness, shock, and even death.
- Gabapentin (Neurontin) and topiramate (Topamax) are not yet FDA-approved for AUD, but they are currently being used to treat the disease. Gabapentin, an anticonvulsant used to treat neuropathic pain, corrects dysregulation caused by alcohol use and cessation; it also decreases alcohol cravings. Topiramate, also an anticonvulsant, decreases alcohol cravings.
The most effective non-pharmacological approach to AUD is psychological therapy, including (9):
- Motivational interviewing. This technique is most effective in those patients who are ambivalent about changing their behaviors and quitting alcohol. The approach is client-centered and helps patients recognize and address their issues. It helps them become motivated to make long-lasting, healthy changes.
- Motivational enhancement therapy (MET). MET is a manual-based intervention that includes motivational interviewing and focuses on strengthening the motivation of the patient to change their alcohol use behaviors.
- Cognitive behavioral therapy (CBT). CBT helps individuals explore the connections among their thoughts, emotions, and behaviors. This therapy can increase motivation to stop drinking, identify triggers that prompt alcohol use, and teach effective coping mechanisms to deal with alcohol cravings and alcohol-seeking behaviors. In one study, 58% of patients receiving cognitive-behavioral treatment fared better than those who did not receive this therapy (3).
Other programs that support patients with AUD are residential facilities (inpatient rehabilitation), community programs like Alcoholics Anonymous (AA) or other 12-step programs, and faith-based programs that align with the principles of specific religions.

Ask yourself...
- How does the DSM define tolerance?
- Which biomarkers can indicate AUD?
- Which three medications has the FDA approved for AUD treatment?
- What are the differences among motivational interviewing, motivational enhancement therapy, and cognitive behavioral therapy?
Complications and Long-Term Effects
AUD impacts each body system and can cause complications that have long-term negative effects. For example, alcohol impairs the brain’s ability to regulate balance, memory, speech, and judgment, which can lead to injuries. With long-term, heavy drinking, the neurons reduce in size, the brain’s mass shrinks, and the brain’s inner cavity grows larger.
Alcohol interferes with glutamate action, which inhibits the creation of new memories and leads to blackouts. Alcohol also influences the neurotransmitters dopamine and serotonin, which can cause mood dysregulation, impaired concentration, and decreased motivation. Even though alcohol can cause euphoria at first, it is a depressant that can lead to suicidal ideation, behaviors, and death.
Additionally, excessive alcohol consumption can weaken the immune system, which can lead to increased rates of infection, such as pneumonia (4).
Additional complications of AUD by the organ system are (4, 5, 7):
- Cardiac/Circulatory: Cardiomyopathy, arrhythmias, stroke, hypertension, ischemic heart disease, heart failure
- Endocrine: Acute and chronic pancreatitis, pancreatic cancer, diabetes
- Gastrointestinal: Esophageal cancer, oral cavity cancer, larynx cancer, pharynx cancer, gut leakiness, gastritis, ulcers, microbial dysbiosis, colorectal cancer, inflammatory bowel disease (IBD)
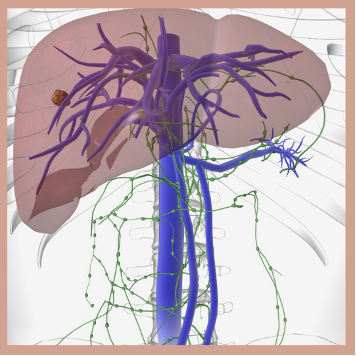
- Hepatic: Steatosis, steatohepatitis, fibrosis, cirrhosis, alcohol-associated hepatitis, liver cancer
- Immune/Lymphatic: Infections, such as tuberculosis
- Integumentary: Melanoma
- Neurologic: Ischemic stroke, amyotrophic lateral sclerosis (ALS), Alzheimer’s disease, multiple sclerosis (MS)
- Reproductive: Breast cancer, sexually transmitted infections
- Respiratory: Acute respiratory distress syndrome, alcohol-associated lung disease, pneumonia
- Skeletal: Muscle myopathy, muscle wasting, impaired bone fracture repair, reduced bone density (osteopenia, osteoporosis)
- Urinary: Kidney disease, prostate cancer
Alcohol is a toxic substance that contains carcinogens, such as nitrosamines, asbestos fibers, phenols, and hydrocarbons, which are the cause of 3.5% of cancer deaths in the United States (4).
Some cancers associated with alcohol consumption are (4):
- Head and neck cancer. Drinkers are at increased risk for oral cavity, pharynx, and larynx cancers. The risk increases among those individuals who both drink and use tobacco.
- Esophageal cancer. The risk of esophageal squamous cell carcinoma is high in moderate to heavy drinkers.
- Liver cancer. The risk for hepatocellular carcinoma and intrahepatic cholangiocarcinoma doubles in individuals who are heavy drinkers.
- Breast cancer. Light drinkers have a slightly increased risk of breast cancer, whereas moderate to heavy drinkers increase their risk substantially. Tobacco use in conjunction with alcohol use increases the risk of breast cancer.
There are multiple ways in which alcohol can increase the risk of cancer, such as (4):
- Metabolism of ethanol to acetaldehyde, which is a toxic carcinogen, acetaldehyde damages DNA and proteins.
- Oxidation can damage DNA, proteins, and lipids.
- Inability to digest and assimilate vital nutrients that can protect against cancers, such as vitamin A, vitamin B complex, vitamin C, vitamin D, vitamin E, and carotenoids.
- Increasing levels of estrogen can lead to breast cancer.
The prognosis for patients with AUD is very challenging, with less than 20% to 30% achieving long-term abstinence and with most acquiring serious to permanent health conditions that are irreversible (9).
Ask yourself...
- How does alcohol negatively impact the brain?
- How does alcohol affect the gastrointestinal and integumentary systems?
- Why does oxidation increase the risk of cancer?
- What is the prognosis of patients with AUD?
Patient Education
Nurses play a critical role in educating patients with AUD, and they should do so in a non-judgmental and non-confrontational manner.
Educational topics nurses should address with patients include (9, 10):
- Healthy diet. Most patients with AUD suffer from malnourishment, particularly regarding folate. Foods rich in folate include legumes, eggs, leafy greens, citrus fruits, nuts and seeds, and fortified grains. Patients should be taught the importance of maintaining a healthy diet that is rich in protein, complex carbohydrates, fresh fruits and vegetables, healthy fats, and vitamins and minerals.
- Reducing risky behaviors. Individuals with AUD should be taught that alcohol consumption lowers inhibitions, which can lead to risk-taking behaviors, such as driving, swimming, operating heavy machinery, and engaging in unprotected sexual practices.
- Importance of support groups. Patients with AUD are more likely to make progress and stay motivated if they are supported by family, friends, and community resources like Alcoholics Anonymous (AA). Family members should also be encouraged to attend support groups like Al-Anon.
- Maintaining a temptation-free environment. Patients should be encouraged to remove all alcohol from their homes and offices. When traveling, they can request that hotels remove alcohol from the guest room minibar.
- Maintaining health screenings is important. AUD can lead to other serious health conditions, such as cardiovascular disease, osteoporosis, and various cancers. Patients should be taught the importance of regular medical check-ups and health screenings to maintain optimal health.
Nurses should also ensure that patients can access educational and support resources in their native language and, if applicable, receive information about resources available to low-income individuals.
Ask yourself...
- Which foods high in folate should the nurse recommend for patients with AUD?
- Why do individuals with AUD engage in risky behaviors?
- Which serious health conditions are patients with AUD at risk of acquiring?
- How can alcoholics maintain a temptation-free environment at home and when traveling?
Resources
There are many resources available to assist patients with AUD.
- Alcoholics Anonymous: AA is a global fellowship community that helps individuals resolve their issues with alcohol. https://www.aa.org/
- Al-Anon Family Groups: Like AA, Al-Anon is a fellowship community that helps friends and family members of alcoholics gain the support they need. https://al-anon.org/
- Alateen: Alateen is a component of Al-Anon, a fellowship group for adolescents who have been affected by someone else’s drinking. https://al-anon.org/newcomers/teen-corner-alateen/
- Centers for Disease Control and Prevention: The CDC provides resources, such as publications, online tools, and healthcare information related to individual states. https://www.cdc.gov/alcohol/resource-center/index.html
- FindTreatment.gov: This is a national website for locating treatment facilities for mental and substance use disorders. https://findtreatment.gov/locator
- National Association for Children of Addiction (NACoA): This organization provides programs, such as The Clergy Education and Training Project, Celebrating Families, and Children’s Program Kit to support the children of addicted parents. https://nacoa.org/
- Rethinking Drinking: The National Institute on Alcohol Abuse and Alcoholism (NIAAA) website provides evidence-based information for patients and healthcare providers, as well as listings for treatment centers. https://www.rethinkingdrinking.niaaa.nih.gov/
Ask yourself...
- Which organization assists friends and family members of individuals with AUD?
- Which organization supports teenagers who are affected by someone else’s drinking?
- Which programs by NACoA support the children of addicted parents?
- Which websites provide listings for treatment centers?
Case Study
B.P. is a 32-year-old Caucasian man who presents to the emergency department after a motor vehicle accident during which B.P. lost control of his car and drove it into a roadside ditch. There were no other cars on the road at the time, making the accident a one-person collision. B.P. was brought to the hospital by his girlfriend and presented with superficial lacerations and bruising to his face from deployment of the driver’s side airbag and more serious lacerations to his left forearm that were caused by the breaking glass of the driver’s side window. He states that he thinks he may have hit his head on the automobile’s steering wheel before airbag deployment, but then says, “I’m not completely sure about that little detail.”
B.P.’s vital signs are blood pressure 158/84 mmHg, pulse 78 beats per minute, respirations 16 breaths per minute, and oxygen saturation 95%. His lung fields are clear to auscultation bilaterally, and his cardiovascular exam reveals a regular rate and rhythm without murmurs. Bowel sounds are confirmed in four quadrants via auscultation. Radial, pedal, and dorsal pedal pulses are normal bilaterally. Pupils are sluggish to react to penlight; the patient’s eyes are glassy. B.P. is oriented to place, but not day or time.
He can state his name and birthdate without hesitation, but he pauses before stating his complete address and incorrectly states his zip code. When speaking, B.P.’s words are slurred, but his bilateral hearing is intact. During the musculoskeletal and neurological assessments, B.P. cannot follow all the instructions the nurse provides, and at one point, he whines, “Can we stop now? This is super hard, and I’m so sleepy. I need to go to bed now.” The patient’s left forearm is red and edematous with two lacerations that are both roughly 1.5 inches in length.
There are evident shards of glass present in both lacerations, and bleeding has slowed significantly since the patient arrived at the hospital. B.P.’s face has several minor red contusions and several superficial lacerations. The patient denies any reports of pain, headache, nausea, or dizziness, and says that he only feels fatigued.
B.P.’s health history includes chronic hay fever, for which he takes over-the-counter antihistamines. He denies any further health issues. Due to B.P.’s noncompliance, the nurse is unable to obtain a detailed social history or family history.
After B.P.’s face and left arm are cleaned, and the left arm sutured and bandaged, he is taken for a chest x-ray, which is normal, and a computerized tomography (CT) scan of the head, which shows no intracranial hemorrhage, mass, or stroke. Blood test results reveal folate deficiency, and ALT, AST, MCV, GGT, and CETP levels consistent with heavy alcohol use. Intravenous folate and normal saline are administered during the next several hours, and the patient is consistently monitored for pain and alcohol withdrawal symptoms. As B.P. becomes sober, the nurse initiates the AUDIT questionnaire; B.P. scores a 32.
When the nurse explains B.P.’s AUDIT score, he states, “Yeah, I’m not surprised. I’ve been drinking since I was 13, and my girlfriend keeps telling me that my drinking is getting worse. I like to have a few to chill after a hard day at work; my job is super stressful. Maybe she’s right. And after tonight, I should probably look into it. These hospital and car bills aren’t going to be cheap.”
B.P. is discharged with a referral to a psychiatrist for further AUD evaluation and potential treatment. He is also given a couple of brochures about alcohol abuse and inpatient rehabilitation programs. B.P. is encouraged to follow up with his primary care physician for continued care of his injured arm.
Ask yourself...
- Which social factors about B.P.’s situation put him at risk for AUD?
- Which assessment findings indicate B.P. may have AUD?
- Is B.P.’s AUDIT score concerning? If so, why?
- Which factors indicate it was effective for the nurse to wait to administer the AUDIT to B.P.?
Conclusion
AUD puts individuals at risk for serious health complications, legal problems, and impaired interpersonal relationships. Many alcoholics do not receive appropriate medical care for AUD due to a lack of screening by healthcare providers. Therefore, nurses must use their assessment skills to evaluate patients for AUD and provide them with proper education about the disease, including its long-term effects and complications.
Healthcare screenings for cardiovascular disease and mental health disorders, as well as referrals to community support programs such as Alcoholics Anonymous, help patients take responsibility for their health and recovery.
References + Disclaimer
- Harris, J.C., Leggio, L., Farokhnia, M. (2021). Blood biomarkers of alcohol use: a scoping review. Current Addiction Reports, 8(4), 500-508. https://doi.org/10.1007/s40429-021-00402-7
- Johns Hopkins Medicine. (2023). CAGE substance abuse screening tool. Retrieved from: https://www.hopkinsmedicine.org/-/media/johns-hopkins-health-plans/documents/all_plans/cage-substance-screening-tool.pdf
- Nathan, P.E., Wallace, J., Zweben, J., Horvath, A. T. (2018). Understanding alcohol use disorders and their treatment. Retrieved from: https://www.apa.org/topics/substance-use-abuse-addiction/alcohol-disorders.
- National Cancer Institute. (2021). Alcohol and cancer risk. Retrieved from: https://www.cancer.gov/about-cancer/causes-prevention/risk/alcohol/alcohol-fact-sheet.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Alcohol’s effects on the body. Retrieved from: https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Goal 3: prevention. Retrieved from: https://www.niaaa.nih.gov/strategic-plan/prevention.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Understanding alcohol use disorder. Retrieved from: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder.
- National Institute on Drug Abuse. (2023). AUDIT. Retrieved from: https://nida.nih.gov/sites/default/files/files/AUDIT.pdf.
- Nehring, S.M., Chen, R. J., Freeman A.M. (2023). Alcohol use disorder. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK436003/.
- Substance Abuse and Mental Health Services Administration, National Institute on Alcohol Abuse and Alcoholism. (2015). Medication for the treatment of alcohol use disorder: a brief guide. Retrieved from: https://store.samhsa.gov/sites/default/files/sma15-4907.pdf.
- Thompson, W., Lande, R. G., Kalapatapu, R.K. (2020). What are the DSM-5 criteria for alcohol use disorder? Retrieved from: https://www.medscape.com/answers/285913-41535/what-are-the-dsm-5-criteria-for-%20alcohol-use-disorder?form=fpf.
- World Health Organization. (2023). AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. Retrieved from: https://www.who.int/publications/i/item/WHO-MSD-MSB-01.6a.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
