An Overview of Pulmonary Hypertension
Contact Hours: 2
Author(s):
Nonnie Breytspraak MSN, RN, CEN, TCRN
Course Highlights
- In this An Overview of Pulmonary Hypertension course, we will learn about the hemodynamic and clinical definitions of pulmonary hypertension.
- You’ll also learn how to recognize the signs and symptoms of pulmonary hypertension.
- You’ll leave this course with a broader understanding of the treatment for pulmonary hypertension.
Introduction
Pulmonary hypertension (PH) is a rare disease with a poor prognosis. It is characterized by elevated pressures in the lungs, which ultimately leads to right-sided heart failure.
PH is a reasonably young disease with an evolving definition and complicated classification system based on its underlying etiology. The initial symptoms are non-specific and may be overlooked, often leading to a delayed diagnosis and even poorer outcomes.
As nurses, understanding the signs and symptoms and the associated underlying etiologies is crucial in advocating for the appropriate assessments and diagnostic testing for our patients. This active role could lead to an earlier diagnosis and better outcomes, underscoring our value in the healthcare team.
If the underlying etiology of PH is known, treatment aims at it. Supportive care is based on the functional class of PH.
History
The history of PH is brief because it is a relatively young disease regarding documentation, research, and treatment. Ernst Von Romberg, a German physician, was the first to provide a pathological description of pulmonary hypertension in 1891, which he termed “pulmonary vascular sclerosis.” (2, 3)
In 1929, a medical student named Werner Forssmann was completing his surgical training near Berlin when he performed the first successful right heart catheterization—on himself! (2) This was before the introduction of Institutional Review Boards.
Two physicians in the United States, Dickinson Richards and Andre Cournard, built on Forssmann’s new diagnostic right heart catheterization to develop an understanding of human pulmonary circulation and pulmonary vascular disease. (2) Forssmann, Richards, and Cournard won a Nobel Prize for Physiology or Medicine in 1956 for their groundbreaking work. (2)
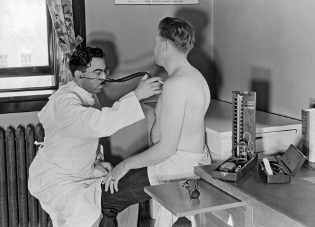 (27)
(27)
In 1952, a British cardiologist named Paul Wood, for whom the Wood unit of measurement in pulmonary vascular resistance is named, was the first to describe PH’s hemodynamic and clinical characteristics. (3) For many years to follow, little was published until an epidemic of PH emerged because of the appetite suppressant drug aminorex in 1965. (3) The drug was removed from the market in 1972, but it spurred new developments in PH.
In 1973, the World Health Organization (WHO) convened the First World Symposium on “Primary Pulmonary Hypertension” to address the epidemic. (2) American physician Norm Shumway published the first successful treatment for PH in 1982, documenting his first heart and lung transplant, performed in 1981. (2) Also in 1982, Drs. Bergstrom, Samuelson, and Vane won the Nobel Prize for Physiology or Medicine for their work demonstrating the beneficial effects of intravenous prostacyclin on PH. Still, it took until 1995 for the first prostacyclin drug to receive FDA approval. (2)
Ask yourself...
- To whom did Werner Forssmann complete the first right heart catheterization?
- What was Dr. Norm Shumway’s successful treatment for PH?
- In what year did intravenous prostacyclin receive FDA approval to treat PH?
Definition and Etiology
PH is a complex group of medical conditions defined by their etiology and hemodynamics and further delineated by their functional classification.
Clinical Definition
The WHO defines five PH groups defined by etiology or underlying mechanism.
Group 1 – Pulmonary arterial hypertension (PAH)
This is a precapillary PH, which includes many subgroups:
- Idiopathic PAH
- Hereditary PAH, including BMPR2 and ALK2 gene mutations
- Toxin- and drug-induced PAH
- Confirmed risk factors include aminorex, fenfluramine, dexfenfluramine, benfluorex, methamphetamines, dasatinib, mitomycin C, and toxic rapeseed oil.
- Suspected risk factors include cocaine, phenylpropanolamine, L-tryptophan, St. John’s wort, amphetamines, IFN-α and -β, alkylating agents, bosutinib, leflunomide, and direct-acting antiviral agents against the hepatitis C virus.
- Conditions with lesions in the small pulmonary arterioles, including collagen-vascular disease (scleroderma/ CREST syndrome), HIV-associated pulmonary hypertension, portal hypertension, congenital left-to-right shunts, and schistosomiasis.
- Pulmonary veno-occlusive disease (PVOD) and pulmonary capillary hemangiomatosis (PCH)
- Persistent pulmonary hypertension of the newborn (3, 13, 15, 16, 17, 21, 22, 23)
Group 2 – PH due to left-sided heart failure
This is a postcapillary PH and includes:
- Heart failure with preserved ejection fraction
- Heart failure with reduced ejection fraction
- Valvular heart disease
- Congenital or acquired cardiovascular conditions leading to postcapillary PH (3, 5, 12, 13, 23, 25)
Group 3 – PH due to lung disease and/or hypoxia
This is a precapillary PH and includes:
- Obstructive lung diseases such as chronic obstructive pulmonary disease (COPD), obstructive sleep apnea (OSA), or emphysema
- Restrictive lung diseases such as interstitial lung disease (ILD)
- Lung disease with mixed obstructive/restrictive pattern
- Hypoventilation syndromes
- Hypoxia without lung disease, such as high-altitude
- Developmental lung disorders (3, 6, 11, 13, 16, 17, 23, 25)
Group 4 – PH due to pulmonary artery obstruction
This is a precapillary PH and includes:
- Chronic thromboembolic PH (CTEPH)
- Malignant and non-malignant tumors
- Arteritis without connective tissue disease
- Congenital pulmonary artery stenosis
- Parasites such as hydatidosis (2, 3, 13, 16, 17, 23, 25)
Group 5 – PH with unclear and/or multifactorial etiologies
This is a primarily precapillary PH but encompasses postcapillary and combined PH and includes:
- Hematological disorders such as myeloproliferative disorders
- Systemic disorders such as sarcoidosis, pulmonary Langerhans cell histiocytosis, lymphangioleiomyomatosis, neurofibromatosis, and vasculitis
- Metabolic disorders such as glycogen storage disease, Gaucher disease, and thyroid disorders
- Chronic renal failure with or without hemodialysis
- Pulmonary tumor thrombotic microangiopathy
- Fibrosing mediastinitis (1, 3, 13, 21, 23, 25)
Ask yourself...
- How many groups of PH are there, according to the WHO?
- How are the PH groups defined?
- Is Group 2 PH a pre- or postcapillary PH?
- In which group would you classify hereditary PH?
- In which group would you classify PH with multifactorial etiology?
 (28)
(28)
Hemodynamic Definition
PH was initially hemodynamically defined at the WHO’s First World Symposium on Primary Pulmonary Hypertension in 1973 and published in 1975 as:
- mean pulmonary artery pressure (mPAP) > 25 mm Hg at rest
- mPAP > 30 mm Hg during exercise
- pulmonary artery wedge pressure (PAWP) ≤12 mm Hg for precapillary PH and PAWP ≥ 12 mm Hg for postcapillary PH (3, 13, 14)
The initial definition for mPAP > 25 mm Hg was somewhat arbitrary despite widely accepted knowledge that the resting mPAP seldom exceeded 15 mm Hg at rest. (13) Two areas of research helped to refine this definition.
- First, a meta-analysis of more than 1,000 healthy individuals demonstrated that mPAP is 14.0 ± 3.3 mm Hg and defined the upper limit of normal as 20.6 mm Hg, or two standard deviations above the mean. (13) This is far below the arbitrary mPAP >25 mm Hg initially set forth by the WHO.
- Second, several retrospective studies reviewed more than 25,000 patient cases and found physiological adverse remodeling and increased risk of death for those with mPAP between 19 and 24 mm Hg. (13)
The initial PAWP of ≤12 mm Hg for precapillary PH and PAWP ≥ 12 mm Hg for postcapillary PH was set because a PAWP of 12 mm Hg is the scientifically defined upper limit of normal in healthy individuals. (13, 14) However:
- The European Society of Cardiology Heart Failure Association recommends PAWP ≤15 mm Hg for the diagnosis of heart failure. (13)
- Many randomized control studies for PH have adopted the PAWP ≤15 mm Hg threshold. (13)
Pulmonary vascular resistance (PVR) was not introduced to the PH hemodynamic definition until 2003 at the Third World Symposium on Pulmonary Hypertension. Like the initial threshold for mPAP, the initial threshold for PVR was mostly arbitrary at ≥3 WU. (3, 13, 14) Again, two areas of research helped to inform the PVR criteria better:
- Systematic reviews have now established a PVR <2 as the upper limit of normal in healthy individuals. (13, 14)
- Retrospective studies have demonstrated reduced functional abilities and higher mortality rates for patients with a PVR > 2. (13, 14)
As our understanding of hemodynamics and PH has evolved, so have the hemodynamic definitions of PH. The latest changes were made at the Sixth World Symposium on Pulmonary Hypertension in 2018 and by the task force for the diagnosis and treatment of PH of the European Society of Cardiology and the European Respiratory Society, published in 2022. The current hemodynamic definitions are:
Precapillary PH –
- mPAP > 20 mm Hg
- PAWP ≤ 15 mm Hg
- Pulmonary Vascular Resistance (PVR) > 2 Wood units (WU)
Isolated Postcapillary PH –
- mPAP > 20 mm Hg
- PAWP > 15 mm Hg
- PVR ≤ 2 WU
Combined Pre- and Postcapillary PH –
- mPAP > 20 mm Hg
- PAWP > 15 mm Hg
- PVR > 2 WU (3, 13, 14)
The new hemodynamic definitions lowered the mPAP and PVR thresholds for PH diagnosis based on scientific data while increasing the threshold for PAWP based on consensus.
Don’t get too comfortable with this PAWP definition. The gray area between a PAWP of 12 and 15 mm Hg will likely be studied and may reveal similar outcomes found for a mPAP between 19 and 24 mm Hg.
Ask yourself...
- Why was the mPAP lowered from > 25 mm Hg to > 20 mm Hg?
- Why was the PAWP increased from 12 mm Hg to 15 mm Hg?
- What new hemodynamic measurement was added to the PH definition in 2003?
Functional Classification
In addition to etiological and hemodynamic definitions, the WHO further categorizes PH into functional classes. This is a measurement of the effect of PH on the patient and was published in 1998. (10, 21)
Assigning a functional class is a risk assessment method and can guide treatment planning. (10) For those aware of the New York Heart Association classifications of heart failure, these may look familiar. There are four classes of PH:
- Class I – Most PH patients are not yet diagnosed in class I because they are mainly asymptomatic. PH patients in class meet the hemodynamic definitions of PH but can complete all of their activities of daily living without any shortness of breath, fatigue, chest pain, near-syncope, or syncopal episodes. (21)
- Class II – PH patients in this class are comfortable at rest but have slight limitations in their activities of daily living due to shortness of breath, fatigue, chest pain, or near syncope when exerting themselves. (21)
- Class III – PH patients in class 3 experience pronounced limitations in their activities of daily living. They are still comfortable at rest, but even minor activities of daily living provoke shortness of breath, fatigue, chest pain, near-syncope, or even syncopal episodes. (21)
- Class IV – PH patients are unable to perform any activities of daily living without experiencing shortness of breath, fatigue, chest pain, near-syncope, or syncopal episodes. These patients may even experience discomfort at rest. (21)
Ask yourself...
- Who defined the PH functional classes?
- How many PH functional classes are there?
- In which class would a PH patient experience chest pain when climbing stairs?
- In which class would a PH patient experience shortness of breath while making a sandwich?
- In which class would a PH patient experience shortness of breath at rest?
Epidemiology
PH is relatively rare. An estimated 1% of the population has PH. Still, this figure is expected to rise as more data is collected after the revised hemodynamic definition of PH was changed in 2018 and published in 2022. (3, 9, 13, 14) Women are affected by PH more than men, and outside of idiopathic and hereditary PH, it is most often diagnosed in patients aged 65 and older. (3, 9, 13, 14, 23, 25)
PH is even more rare in children. The estimated prevalence of PH in children is between 3 and 20 cases per million children. (16, 17) It is usually in children less than one-year-old and related to congenital lung disease or persistent pulmonary hypertension of the newborn (PPHN). (16, 17)
Group 2 PH is the most common type, with some studies estimating prevalence of 50 to 70% and others estimating as high as 65 to 80%. (3, 12,14, 15, 26) Group 3 PH is the second most common type, with 30 to 50% prevalence estimates. (3, 14, 15, 26) Groups 1, 4, and 5 are very rare. (14)
While the prevalence of PH is relatively rare, the economic impact of PH can be devastating for patients. PH patients in the later functional classes of III and IV are often hospitalized, with multiple readmissions from complications, at an estimated cost of approximately $45,000 per hospitalization. (18) Another breakdown of the PH-related direct cost estimates is anywhere from $25,000 to $110,000 per patient annually. (18)
The indirect costs are hard to quantify but are equally distressing for patients and their families. 85% of PH patients report having their employment impacted in some way by their PH, and 45 to 71% report missing work for extended periods or not being able to work at all. (18)
The overall survival rates for PH from the time of diagnosis are reported to be:
- 86% at one year,
- 67% at three years, and
- 54% in five years. (13, 14, 26)
Survival rates are lower than these averages for groups 2 and 3, as their underlying etiologies and co-morbidities are often more aggressive. (11, 12)
Ask yourself...
- What percentage of the population has PH?
- Which PH group is most common?
- Which PH group is the second most common?
Group 1 PH
While group 1 PH is rare, there is a lot of research and data on this group, possibly because it predominantly affects younger females (7, 8, 21). Over half of group 1 PH cases are idiopathic; roughly 73% of idiopathic cases are found in females in their thirties, forties, and fifties. (20, 21, 23) Another 10% of cases are hereditary, but this percentage may increase as genetic testing becomes more widely used. (21)
Registries in the United States and Europe report a prevalence rate of 6.6 to 26.0 patients per million adults:
- 73% Caucasian,
- 12% African American,
- 9% Latino, and
- 3% Asian. (3, 20, 21)
According to the Registry to Evaluate Early and Long-term PAH Disease Management (REVEAL registry), the survival rates from the time of diagnosis of group 1 PH are:
- 85% at one year,
- 68% at three years,
- 57% at five years, and
- 49% in seven years. (7)
The prognosis is worse for methamphetamine use-related group 1 PH, which is on the rise with an estimated 50 million users worldwide. (7, 15)
The REVEAL registry includes data on five-year survival rates for group 1 PH based on functional classification:
- Class I – 72.2%
- Class II – 71.7%
- Class III – 60.0%
- Class IV – 43.8%
Group 2 PH
Heart failure-related PH is the most common type of PH, with studies reporting an average of 70% prevalence among all PH. (3, 12,14, 15, 26) Approximately 60% of all patients with heart failure are also noted to have group 2 PH, and most are 65 years of age or older. (12) The three-year mortality rate for patients with group 2 PH is 28% higher compared to heart failure patients without PH. (12)
Group 3 PH
This is the second most common form of PH after group 2 and is more prevalent in patients 65 years of age and older. (3, 11, 14, 15, 26) Registries indicate the prevalence of group 3 PH by underlying etiology:
- COPD – 5 to 25% in patients with mild to moderate COPD and up to 90% in patients with severe COPD
- Idiopathic Pulmonary Fibrosis (IPF) – 8 to 15% in patients with early IPF, 30 to 50% in patients with advanced IPF, and more than 60% in patients with end-stage IPF.
- Obstructive Sleep Apnea – 20 to 30% of patients
- Obesity Hypoventilation Syndrome – up to 58% of patients
- High Altitude Related Lung Diseases – 5% (3, 11)
Adding group 3 PH to the underlying etiology increases the patient mortality rate, but more research is needed to determine how much. (11)
Group 4 PH
Chronic thromboembolic PH (CTEPH) is the most common etiology in group 4 PH, but it is extremely rare, with a prevalence rate of 3% in those who have had embolic disease. (3, 13, 15) The three-year survival rate for patients with CTEPH is 70% compared to 89% for those with a previous embolism without the development of CTEPH. (15)
Group 5 PH
Group 5 PH is rare and often associated with underlying etiologies such as sickle cell disease and chronic kidney disease. (1) The prevalence of group 5 PH is difficult to measure because these underlying etiologies are multifactorial and can sometimes cross over into other groups of PH. (1)
- Sickle Cell Disease—It is estimated that 6 to 10.5% of patients meet the hemodynamic criteria, but they often develop other complications, such as thromboembolism, which may reclassify them as group 4 PH. (1, 3, 19)
- Chronic Kidney Disease – Many end-stage renal disease (ESRD) patients are too medically fragile to verify the hemodynamics meeting PH criteria, and they often develop other complications such as heart failure and OSA, which may reclassify them as group 2 or group 3 PH, respectively. (1, 19)

Ask yourself...
- Which three PH groups are extremely rare?
- Which PH group has little prevalence data because of its multifactorial nature?
- Are men or women more often affected by PH?
- What is the typical age range for a diagnosis of PH?
Pathophysiology
PH is a perfect storm combining an underlying etiology with vascular mediator dysfunction. (7, 8)
Any of the etiologies outlined in the clinical definition section of this course can cause:
- Increased pulmonary vascular resistance,
- Increased pulmonary vascular flow and
- Increased pulmonary venous pressure
(6, 7, 8, 11, 12, 19, 20)
These increases – resistance, flow, and pressure – lead to pulmonary vasculature remodeling. (7, 8, 20) The pulmonary vascular changes include vasoconstriction, cell proliferation, and fibrosis. Pulmonary arteries develop hypertrophy and hyperplasia in all three layers of the vascular wall. (7, 8)
These vascular changes can be graded using the Heath and Edwards pathological classification system:
- Grade I – medial layer hypertrophy
- Grade II – medial layer hypertrophy and intimal layer proliferation
- Grade III – progressive fibrous vascular occlusion
- Grade IV – plexiform lesions in muscular arteries and plexiform capillary channels
- Grade V – complex plexiform lesions, angiomatosis, and cavernous lesions
- Grade VI – necrotizing arteritis and fibrinoid necrosis (7, 8, 20)
In PH, the vascular remodeling is exacerbated by vascular mediator dysfunction:
- Increased endothelin (vasoconstrictor) levels, which promote vasoconstriction,
- Decreased nitric oxide (vasodilator) levels, which prevent vasodilation and promote proliferation and/or
- Decreased prostacyclin (vasodilator) levels prevent vasodilation and promote proliferation and platelet function. (7, 8, 11, 19, 20)
This perfect storm of an underlying PH etiology and vascular mediator dysfunction ultimately leads to right-sided heart failure. (1, 3, 5, 14)
The first three grades in the Heath and Edwards scale are thought to be reversible. This theory and the vascular mediator dysfunction form the basis for many of the drugs developed for treating PH, as we will see in the treatment section of this course. (3, 4)
Ask yourself...
- What does increased pulmonary vascular resistance, flow, and pressure lead to?
- How many grades are in the Heath Edwards pathological grading system?
- Which grades in the Heath Edwards scale are thought to be reversible?
- What is endothelin, nitric oxide, and prostacyclin?
- What does PH ultimately lead to?
Clinical Signs and Symptoms
The most common signs and symptoms of PH are non-specific and can include:
- Shortness of breath with exertion
- Fatigue
- Weakness
- Chest pain with exertion
- Heart palpitations
- Near-syncope or syncope
- Nausea and vomiting
- Loss of appetite
- Right upper quadrant pain
- Edema in the feet, legs, or abdomen (4, 21, 23, 24, 25)
Less common symptoms may include:
- Cough
- Hemoptysis
- Hoarseness or Ortner’s syndrome may be caused by the distended pulmonary artery compressing the recurrent laryngeal nerve. (21)
All of these symptoms are vague and could indicate many more common illnesses. This is why there is, on average, a 2-and-a-half-year delay from the onset of symptoms and a definitive diagnosis of PH. (9, 14, 15) The latest guidelines encourage providers to keep pulmonary hypertension in their differential diagnosis when patients present with these non-specific symptoms. (9)

Ask yourself...
- Name three common signs and symptoms of PH.
- Name one less common sign and symptom of PH.
- What is Ortner’s syndrome caused by?
- How long is the average delay between the onset of PH symptoms and a definitive diagnosis?
Case Study
Judy, a 67-year-old female, presents with a complaint of fatigue and shortness of breath, which started four months ago. She reports she ignored the symptoms initially because she thought she was just overwhelmed planning her daughter’s wedding, but the wedding was two months ago. She feels tired and short of breath and experienced chest discomfort while climbing stairs last week.
Assessment and Diagnostics
The approach to diagnosing PH is two-pronged:
- Identify PH early
- Identify any underlying diseases associated with the PH for appropriate classification, risk assessment, and treatment. (9)
The first step in any assessment is a thorough patient and family history to identify risk factors. The second step is a physical examination of the patient, which could reveal:
- Signs of PH include cyanosis, an accentuated pulmonary component in the second heart sound, a systolic murmur of tricuspid regurgitation, and a diastolic murmur of pulmonary regurgitation. (9)
- Signs of right ventricular backward failure such as distended and pulsating jugular veins, abdominal distention, hepatomegaly, ascites, and peripheral edema. (9)
- Signs of right ventricular forward failure such as peripheral cyanosis, dizziness, pallor, cool extremities, and prolonged capillary refill. (9)
During the patient and family history, it is revealed that Judy has a history of hypertension, diabetes, and acid reflux. She reports not always remembering to take her medication, and she does not check her blood pressure at home. Judy states that her parents both had high blood pressure and diabetes, and her mother passed away at the age of 57 after suffering from a stroke.
On the physical exam, Judy is mildly obese, has a tricuspid murmur, and 1+ pitting edema in her feet and ankles. Her HR is 84, BP 164/91, RR 17, and 95% O2 saturation on room air at rest.
Diagnostic Studies
The latest guidelines for diagnosing and treating PH recommend diagnostic tests. An overview of these tests follows.
Blood Tests
Labs should include blood counts, electrolyte levels, kidney function panels, liver function panels, iron status, immunology panels, coagulation studies, and thyroid panels. These tests may provide clues regarding underlying PH etiologies. (5, 9, 11, 12, 19, 21)
Electrocardiogram (ECG)
An ECG should be completed for any patient with unexplained shortness of breath. Some findings suggestive of right heart failure with potential predictive value for PH are atrial fibrillation, a right axis deviation, right ventricular hypertrophy, and/or a right bundle branch block. (9,12, 15 21)
Chest X-ray
This may reveal signs of underlying lung disease, pulmonary artery enlargement, or cardiac enlargement. (9, 12, 15, 21)
Echocardiography
An echocardiogram cannot definitively diagnose PH, but it can confirm suspicions of PH by calculating peak tricuspid regurgitation velocity (TRV). The current guidelines recommend proceeding to the definitive diagnostic tool if the peak TRV is greater than 3.4 m/s or if it is between 2.9 and 3.4 m/s with additional risk factors or underlying etiologies for PH or other evidence of PH on the echocardiogram such as signs of left heart failure. (9, 12, 15, 21)
Right Heart Catheterization (RHC)
This is the definitive diagnostic tool for PH as it allows for measuring the hemodynamic criteria for PH. (1, 2, 3, 5, 9, 11, 12, 13, 15, 21)
During RHC, vasoreactivity testing is recommended for some populations to evaluate if the patient is a “responder” who may be treated with high-dose calcium channel blockers (CCB). (3, 7, 8, 12. 15) This vasoreactivity test is performed by administering inhaled nitric oxide or inhaled iloprost, and a positive response is indicated by a decrease in mPAP by more than 10 mm Hg to reach a value of at least 40 mm Hg or less with an increased or unchanged cardiac output. (7, 8, 9, 20)
RHC vasoreactivity testing is only recommended in the following populations:
- Group 1 PH that is idiopathic, hereditary, or drug-induced to determine CCB response,
- Group 2 PH to determine heart transplantation candidacy and
- Group 2 PH with a congenital shunt to assess the viability of defect closure. (9, 15)
Ask yourself...
- What is the first step in assessing a patient for PH?
- Can you name at least two findings on a physical exam that could indicate PH?
Additional Tests
If the patient is not yet stable enough to undergo an RHC, additional tests may be performed before an RHC to obtain more evidence of PH. Additional tests may also be performed after a confirmatory RHC to classify the correct PH group, uncover any comorbidities, determine the severity of PH, and assess the need for supplemental oxygenation. These tests may include:
- Pulmonary Function Tests
- Arterial Blood Gas Tests
- Ventilation/Perfusion Lung Scan
- Chest Computed Tomography
- Cardiac Magnetic Resonance Imaging
- Abdominal Ultrasound
- Cardiopulmonary Exercise Testing
- Exercise Right Heart Catheterization
- Fluid Challenge
- Genetic Testing (9, 15)
CASE STUDY: Judy has completed her diagnostic workup. Her findings of note include:
- NT-proBNP is 8,000 pg/ml
- ECG shows normal sinus rhythm with a right-axis deviation
- Chest X-ray shows pulmonary artery enlargement and an enlarged cardiac silhouette
- Echocardiography shows a peak TVR > 3.4 m/s
- RHC reveals mPAP of 47 mm Hg, PAWP of 19 mm Hg, and PVR of 2 WU

Ask yourself...
- What is the definitive diagnostic tool for PH?
- What populations should receive vasoreactivity testing?
- In which PH group would you classify Judy?
- Should Judy receive vasoreactivity testing?
Treatment
The treatment for PH depends on the type of PH diagnosed and is limited. (3) The recommended treatment for each group is reviewed below. The mainstay of PH treatment is managing the underlying etiology and symptoms.
All PH patients should be referred to a specialized PH treatment center for management and may be referred for a supervised exercise called pulmonary rehabilitation to improve or maintain exercise capacity. (3, 15, 21, 22)
Lung transplantation may be an option for some patients, but the post-transplantation survival rates are poor. (21) Additionally, each group may require supportive treatment, such as supplemental oxygen, as they advance to functional classes III and IV.
Group 1 PH
There is no cure for group 1 PH. Symptoms may be managed through targeted drug therapy and by treating the underlying etiology. (3, 8, 21)
About 10 to 20% of patients with group 1 PH that is drug-induced, idiopathic, or hereditary respond positively to the vasoreactivity test and may be treated with high-dose calcium channel blockers; however, this is only successful in managing symptoms for about half of patients. (3, 8, 21)
Other drug therapies target the dysfunctional vascular mediator pathways:
- Prostacyclin Pathway – Prostacyclin receptor agonists and prostacyclin analogs induce vasodilation by increasing levels of cyclic AMP. Examples include epoprostenol, iloprost, selexipag, and treprostinil. (3, 8, 15, 21)
- Nitric Oxide Pathway – Phosphodiesterase inhibitors, such as sildenafil and tadalafil, and the guanylate cyclase activator riociguat target the nitric oxide pathway. (3, 8, 21)
- Endothelin Pathway – Receptor antagonists such as bosentan, ambrisentan, and macitentan target the endothelin pathway. (3, 8, 21)
Combination drug therapy is recommended as symptoms progress.
Group 2 PH
There is no cure for group 2 PH, and there are no specialized drugs developed to date for this group of PH. The recommended treatment plan is to treat the underlying heart condition with antihypertensives, diuretics, and sodium and fluid restrictions as needed. (3, 12, 21)
Heart transplantation may be an option for patients with end-stage heart failure, but the post-transplant survival rates are poor. (12)
Group 3 PH
There is no cure for group 3 PH. One drug, inhaled treprostinil, has been approved for group 3 PH patients with ILD only, and it has been shown to improve exercise capacity. (3, 6, 11, 15, 21) Managing the underlying lung disease and symptoms is the recommended treatment plan. (3, 11)
Group 4 PH
This is the only PH group with a potential cure: remove the obstructing embolism through pulmonary thromboendarterectomy or balloon pulmonary angioplasty. (2, 3, 21) Riociguat, a vasodilator, is the only drug approved for group 4 PH, and it has been shown to improve exercise capacity. (2, 3) Otherwise, the recommended treatment plan is to manage the underlying etiology and symptoms. (2, 3, 21)
Group 5 PH
There is no cure for group 5 PH, and currently, no FDA-approved drug treatment; however, some pulmonary vasodilators have been used off-label with anecdotal success. (1, 3, 21) Managing the underlying lung disease and symptoms is the recommended treatment plan. (1, 3, 21)
Ask yourself...
- Which PH group has a potential cure?
- Which PH group may be treated with high-dose calcium channel blockers?
- Which PH groups have FDA-approved PH-specific drug therapies in their treatment plan?
- What is the mainstay of PH treatment?
- What is Judy’s treatment plan?
- Should Judy participate in pulmonary rehabilitation?
Self-Management
Recommendations for patients include:
- Adhering to the treatment plan discussed with their provider
- Maintaining a healthy body weight
- Eating a balanced diet
- Remaining physically active for as long as they are able
- Refraining from smoking and drugs (3, 15, 21, 23, 24)

Research
Many questions remain about PH. Current research is focused on developing a better understanding of the risk factors and pathophysiology, discovering any new pathways that may be targeted by drug therapy, prevention, and reversing pulmonary vascular remodeling. (3)
The National Heart, Lung, and Blood Institute (NHLBI) and many other investigators are studying the multiple facets of and potential treatments for PH. Some of these studies include:
- Elafin – a drug that may block enzymes called proteases that cause inflammation and vascular remodeling in people with PH
- Estrogen metabolites and how they may play a role in PH risk since women are at greater risk for PH than men
- Genetic mutations, ion channels, and cell membrane receptors and the role they may play in pulmonary vascular remodeling
- Hormonal and metabolic causes of vascular dysfunction (3, 22)
Conclusion
We are still learning about PH. Based on new evidence, the clinical and hemodynamic definitions of PH will likely continue to evolve.
Because the signs and symptoms of PH are often nonspecific, there is usually a two-and-a-half-year delay from symptom onset to diagnosis. During this period, pulmonary vascular remodeling occurs, potentially decreasing the patient’s PH functional class and quality of life.
As nurses, we play a vital role in recognizing symptoms early and advocating for appropriate assessments and diagnostics for our patients. An earlier diagnosis and symptom management could help provide a better quality of life for the PH patient.
References + Disclaimer
- Al-Qadi, M., LeVarge, B., & Ford, H. J. (2021). Epidemiology, Pathogenesis, and Clinical Approach in Group 5 Pulmonary Hypertension. Frontiers in Medicine, 7. https://doi.org/10.3389/fmed.2020.616720
- Anderson, R. J., Malhotra, A., & Kim, N. H. (2016). Pulmonary hypertension: evolution of pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Journal of Thoracic Disease, 8(S7), S562–S565. https://doi.org/10.21037/jtd.2016.07.33
- Bousseau, S., Sobrano Fais, R., Gu, S., Frump, A., & Lahm, T. (2023). Pathophysiology and new advances in pulmonary hypertension. BMJ Medicine, 2(1). https://doi.org/10.1136/bmjmed-2022-000137
- Centers for Disease Control and Prevention. (2019, December 3). Pulmonary hypertension. Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/pulmonary_hypertension.htm
- Connolly, H.M., & Frantz, R.P. (2022, December 08). Pulmonary hypertension with congenital heart disease: Clinical manifestations and diagnosis. UpToDate. https://www.uptodate.com/contents/pulmonary-hypertension-with-congenital- heart-disease-clinical-manifestations-and- diagnosis?search=Pulmonary%20Hypertension&source=search_ result&selectedTitle=10%7E150&usage_type=default&display_rank=10
- Frantz, R. P., & DuBrock, H. M. (2024, January 16). Pulmonary hypertension due to lung disease and/or hypoxemia (group 3 pulmonary hypertension): Treatment and prognosis. UpToDate. https://www.uptodate.com/contents/pulmonary- hypertension-due-to-lung-disease-and-or-hypoxemia-group-3-pulmonary- hypertension-treatment-and-prognosis?search=Pulmonary+Hypertension&source =search _result&selectedTitle=3~150&usage_type=default&display_rank=3
- Hopkins, W., & Rubin, L.J. (2023, November 08). Treatment and prognosis of pulmonary arterial hypertension in adults (group 1). UpToDate. https://www.uptodate.com/contents/treatment-and-prognosis-of-pulmonary- arterial-hypertension-in-adults-group-?search=Pulmonary%20Hypertension&source =search_result&selectedTitle =9%7E150&usage_type=default&display_rank=9
- Hopkins, W., & Rubin, L. J. (2023, October 3). Treatment of pulmonary arterial hypertension (group 1) in adults: Pulmonary hypertension-specific therapy. UpToDate. https://www.uptodate.com/contents/treatment-of-pulmonary-arterial- hypertension-group-1-in-adults-pulmonary-hypertension-specific- therapy?search=Pulmonary+Hypertension&source=search_result&selectedTitle =2~150&usage_type=default&display_rank=2
- Humbert, M., Kovacs, G., Hoeper, M. M., Badagliacca, R., Berger, R. M. F., Brida, M., Carlsen, J., Coats, A. J. S., Escribano-Subias, P., Ferrari, P., Ferreira, D. S., Ghofrani, H. A., Giannakoulas, G., Kiely, D. G., Mayer, E., Meszaros, G., Nagavci, B., Olsson, K. M., Pepke-Zaba, J., … Rosenkranz, S. (2022). 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. European Respiratory Journal, 61(1), 2200879. https://doi.org/10.1183/13993003.00879-2022
- Kim, N. H., Fisher, M., Poch, D., Zhao, C., Shah, M., & Bartolome, S. (2020). Long‐term outcomes in pulmonary arterial hypertension by functional class: a meta‐analysis of randomized controlled trials and observational registries. Pulmonary Circulation, 10(4), 1–10. https://doi.org/10.1177/2045894020935291
- Klings, E.S. (2023, September 27). Pulmonary hypertension due to lung disease and/or hypoxemia (group 3 pulmonary hypertension): Epidemiology, pathogenesis, and diagnostic evaluation in adults. UpToDate. https://www.uptodate.com/contents/pulmonary-hypertension-due-to-lung- disease-and-or-hypoxemia-group-3-pulmonary-hypertension-epidemiology- pathogenesis-and-diagnostic-evaluation-in- adults?search=Pulmonary%20Hypertension&source=search_result&selectedTitle =8%7E150&usage_type=default&display_rank=8
- Krishnan, U., & Horn, E. (2022, June 8). Pulmonary hypertension due to left heart disease (group 2 pulmonary hypertension) in adults. UpToDate. https://www.uptodate.com/contents/pulmonary-hypertension-due-to-left-heart- disease-group-2-pulmonary-hypertension-in- adults?search=Pulmonary+Hypertension&source=search_result&selectedTitle= 4~150&usage_type=default&display_rank=4
- Kularatne, M., Gerges, C., Jevnikar, M., Humbert, M., & Montani, D. (2024). Updated Clinical Classification and Hemodynamic Definitions of Pulmonary Hypertension and Its Clinical Implications. Journal of Cardiovascular Development and Disease, 11(3), 78. https://doi.org/10.3390/jcdd11030078
- Maron, B. A. (2023). Revised definition of pulmonary hypertension and approach to management: A clinical primer. Journal of the American Heart Association, 12(8). https://doi.org/10.1161/jaha.122.029024
- Maron, B. A., Abman, S. H., Elliott, C. G., Frantz, R. P., Hopper, R. K., Horn, E. M., Nicolls, M. R., Shlobin, O. A., Shah, S. J., Kovacs, G., Olschewski, H., & Rosenzweig, E. B. (2021). Pulmonary Arterial Hypertension: Diagnosis, Treatment, and Novel Advances. American Journal of Respiratory and Critical Care Medicine, 203(12), 1472–1487. https://doi.org/10.1164/rccm.202012-4317so
- Mullen, M. P. (2023, April 04). Pulmonary hypertension in children: Classification, evaluation, and diagnosis. UpToDate. https://www.uptodate.com/contents/pulmonary-hypertension-in-children- classification-evaluation-and- diagnosis?search=Pulmonary%20Hypertension&source=search_result&selected Title=5%7E150&usage_type=default&display_rank=5
- Mullen, M.P. (2023, June 15). Pulmonary hypertension in children: Management and prognosis. UpToDate. https://www.uptodate.com/contents/pulmonary- hypertension-in-children-management-and- prognosis?search=Pulmonary%20Hypertension&source=search_ result&selectedTitle=7%7E150&usage_type=default&display_rank=7
- Ogbomo, A., Tsang, Y., Mallampati, R., & Panjabi, S. (2022). The direct and indirect health care costs associated with pulmonary arterial hypertension among commercially insured patients in the United States. Journal of Managed Care & Specialty Pharmacy, 28(6), 608–616. https://doi.org/10.18553/jmcp.2022.28.6.608
- Rubin, L. J., & Hopkins, W. (2023, August 4). Clinical features and diagnosis of pulmonary hypertension of unclear etiology in adults. UpToDate. https://www.uptodate.com/contents/clinical-features-and-diagnosis-of- pulmonary-hypertension-of-unclear-etiology-in- adults?search=Pulmonary+Hypertension&source=search_result&selectedTitle= 1~150&usage_type=default&display_rank=1
- Rubin, L.J., & Hopkins, W. (2024, April 04). The epidemiology and pathogenesis of pulmonary arterial hypertension (Group 1). UpToDate. https://www.uptodate.com/contents/the-epidemiology-and-pathogenesis-of- pulmonary- arterial-hypertension-group- 1?search=Pulmonary%20Hypertension&source=search_ result&selectedTitle=6%7E150&usage_type=default&display_rank=6%7E150& usage_type=default&display_rank=6
- Schwab, K. E. (2024, April 1). Pulmonary arterial hypertension. Practice Essentials, Pathophysiology, Etiology. https://emedicine.medscape.com/article/303098- overview
- U.S. Department of Health and Human Services. (2022, March 24). Pulmonary Hypertension Research. National Heat Lund and Blood Institute. https://www.nhlbi.nih.gov/research/pulmonary-hypertension
- U.S. Department of Health and Human Services. (2023, May 1). What is pulmonary hypertension? National Heart Lung and Blood Institute. https://www.nhlbi.nih.gov/health/pulmonary-hypertension
- U.S. National Library of Medicine. (2024, January 19). Pulmonary hypertension | ph. MedlinePlus. https://medlineplus.gov/pulmonaryhypertension.html
- Walter, K. (2021). Pulmonary hypertension. JAMA, 326(11), 1116. https://doi.org/10.1001/jama.2021.11054
- Wijeratne, D. T., Lajkosz, K., Brogly, S. B., Lougheed, M. D., Jiang, L., Housin, A., Barber, D., Johnson, A., Doliszny, K. M., & Archer, S. L. (2018). Increasing Incidence and Prevalence of World Health Organization Groups 1 to 4 Pulmonary Hypertension. Circulation: Cardiovascular Quality and Outcomes, 11(2). https://doi.org/10.1161/circoutcomes.117.003973
- Photo Credit: CDC via Unsplash+
- Photo Credit: Robina Weermeijer on Unsplash+
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
