Course
Bladder Dysfunction in Multiple Sclerosis
Course Highlights
- In this Bladder Dysfunction in Multiple Sclerosis course, we will learn about an appropriate plan of care based on subjective and objective assessments of bladder dysfunction in a client with multiple sclerosis.
- You’ll also learn subtle signs and symptoms of a urinary tract infection to prevent serious complications.
- You’ll leave this course with a broader understanding of nursing interventions for bladder dysfunction in multiple sclerosis.
About
Contact Hours Awarded: 2
Course By:
Pamela Halvorson, RN, BS, MBA
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Multiple Sclerosis (MS) can lead to bladder dysfunction which occurs in approximately 80% of people with MS due to nerve damage. Bladder problems often originate with nerve or muscle dysfunction as these systems control the flow of urine. If the nerves are not functioning normally, they are unable to tell certain muscles when to tense up and when to relax. If the nerves in the spinal cord don’t send messages from the brain to the bladder, the ability of the sphincter muscles to control the flow of urine is affected.
Bladder dysfunction in MS can be managed with lifestyle changes, medications, physical therapy and nerve stimulation with the goal of decreasing potential complications and increasing the client’s ability to lead a healthier life.
Definition of Multiple Sclerosis
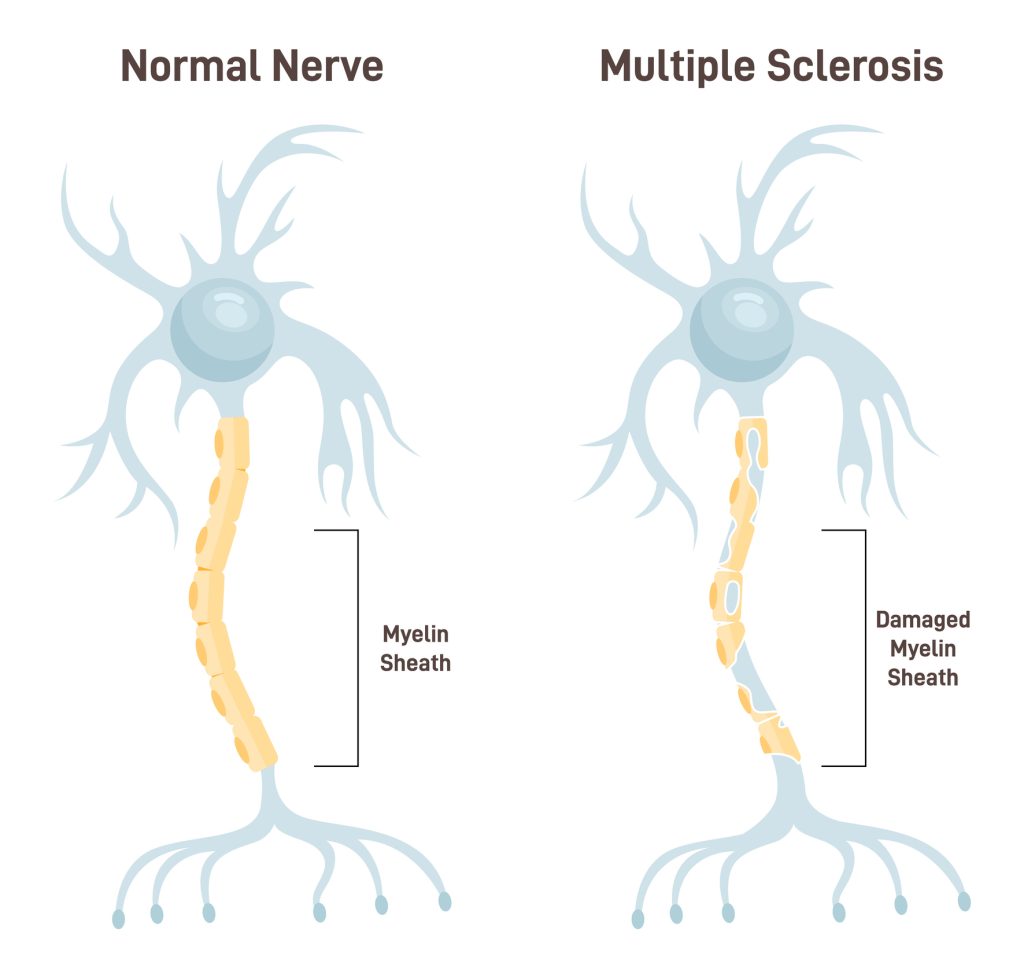
MS is a disease that causes breakdown of the protective covering of nerves. The immune system attacks the protective sheath that covers the nerve fibers which interrupts the communication between the brain and the rest of the body, eventually causing permanent damage to the nerve fibers. (1)
It is defined as an autoimmune disorder, meaning that the immune system which normally protects us from viruses, bacteria and other threats, mistakenly attacks healthy cells. Sclerosis is a term for the distinctive areas of scar-like tissue called plaques or lesions, and result from the attack on the myelin by the immune system.
Etiology
While the cause of MS is not known, it’s considered to be an immune-mediated disease in which the body’s immune system attacks its own tissues and destroys the fatty substance called myelin sheath that coats and protects the nerve fibers in the brain and spinal cord (see figure below). The myelin is what gives the brain’s white matter its whitish appearance.
A combination of genetics and environmental factors may increase the risk of MS. MS is more common in countries further away from the equator suggesting a link between sunlight and the development of MS. Sex/gender and ethnicity/race play a role as females are more likely than males to get MS and it is most common among Whites. Having a parent or sibling with MS increases the likelihood of getting it although it is not an inherited disease. There is also a connection between clients who have been infected with Epstein Barr syndrome and the triggering of MS. (2)
Signs and Symptoms of Multiple Sclerosis
MS symptoms will vary depending on the person and may change over the course of the disease depending on which nerve fibers are affected. They can depend on the severity of the attacks and the location and size of the plaques. Symptoms usually begin in young adults, between the ages of 20 and 40, affecting people differently with symptoms ranging from mild with little disability, to worsening symptoms that lead to increased disability over time.
Most people with MS have short periods of symptoms that resolve fully or partially after they appear, then there may be long stretches without noticeable symptoms. (2) While MS can cause a variety of symptoms related to muscle weakness, vision problems, tingling and numbness, and balance issues, the bladder control problems can be the most distressing for the client.

Self-Quiz
Ask Yourself...
- If there is a link between lack of sunlight and possible development of MS, should Vitamin D level screening be part of annual physical screening, especially for clients who live in northern climates?
- If the Epstein-Barr virus is an important factor in MS, is it possible that vaccines against Epstein-Barr might lead to fewer cases of MS?
- Since the diagnosing of MS can be a challenge, the earlier the diagnosis the better. What observations and education can be done to screen clients on a casual basis that might help identify MS more quickly before symptoms become very pronounced?
Effects of Multiple Sclerosis on the Bladder
Bladder dysfunction is common in MS. Clients may experience symptoms approximately six to eight years after the initial MS diagnosis, but some may present with urinary symptoms at initial diagnosis.
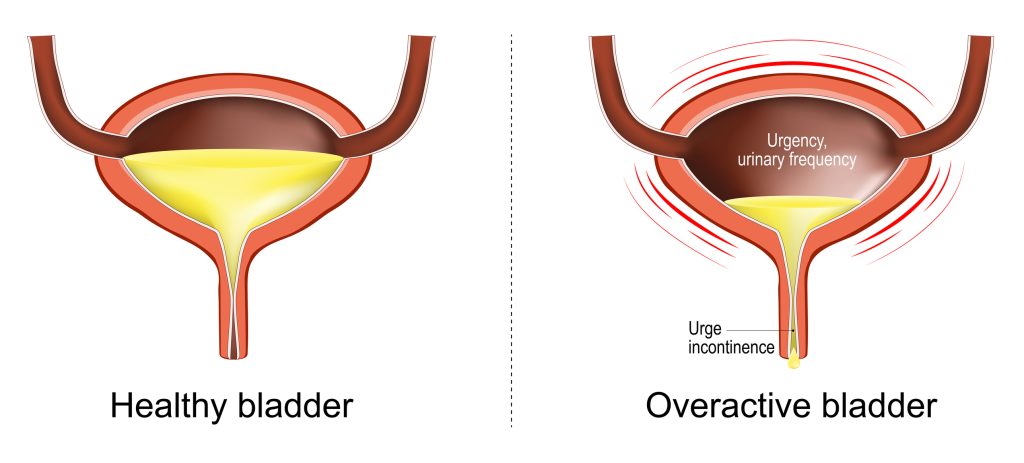
The physiological process of micturition relies on the proper coordination of the urinary bladder and urethral sphincters. Disruption of the voluntary control of micturition due to MS can lead to bladder overactivity and urge incontinence due to a neurogenic bladder or lower urinary tract dysfunction. (5)
Bladder dysfunction can be classified into three categories: impaired storage, impaired emptying or a combination of both but usually includes issues with urgency, frequency of urination or loss of bladder control. Some clients retain large amounts of urine. Many people with MS will experience one or more moderate to severe urinary symptoms and bladder disorders. The effects of MS on voiding can be based on the function of the bladder and the urethral sphincter during urine storage and emptying.
Two major muscles are involved in emptying the bladder; the detrusor muscle and the sphincter muscle. If the nerve impulses to these muscles are interrupted from the MS lesions in the brain and spinal cord, those muscles will contract or relax inappropriately.
The most frequently reported symptoms in MS involve overactive bladder symptoms. Storage of urine within the bladder involves bladder wall and detrusor relaxation and contraction of the bladder neck and internal sphincter. The inability to store or hold urine in the bladder occurs when the bladder is unable to retain urine when it accumulates. Sometimes with MS, instead of expanding when urine collects, the bladder involuntarily contracts, which creates an urgent need to go to the bathroom, even when there isn’t much urine in the bladder.
Conversely, bladder emptying involves contraction of those muscles and relaxation of the bladder neck. The flow or urine is controlled by the sphincter in the bladder, the muscle that relaxes to open and contracts to close. An inability to empty means that even though the person senses that the bladder is full, the nerve impulse telling the muscle to open is interrupted and never reaches the urinary sphincter, and the sphincter muscle closes before all the urine is emptied from the bladder. Sometimes the detrusor muscle and the sphincter muscle do not work in coordination and a person with MS can experience many bladder symptoms. (10)
Left untreated, bladder dysfunction can lead to bladder infections or kidney damage. A urinary tract infection is the leading cause of hospital admission in people with MS and can impose a significant health economic burden. Bladder dysfunction can also lead to constipation, bowel urgency and bowel incontinence, especially when people try to self-treat by not drinking enough water. The excess moisture caused by urine leakage also make skin irritation and yeast infections more likely.
Symptoms suggesting difficulty with impaired storage:
- Urgency: an intense feeling of needing to urinate immediately
- Increased frequency: taking trips to the bathroom more than eight times in 24 hours
- Frequent nocturia: waking up at night to urinate
- Incontinence with urgency, with Valsalva, or due to decreased mobility and inability to reach a bathroom in time resulting in loss of bladder control
Symptoms suggesting impaired emptying or an underactive bladder where the muscles around the urethra may remain contracted even when attempting to urinate:
- Sensation of incomplete emptying
- Urinary hesitancy or inability to void
- Slow or intermittent urinary stream
- Straining to void
- Incontinence without a sense of bladder fullness
- Retention in which the bladder never empties completely
Positive answers in both categories suggest a combined dysfunction. These symptoms are more than an inconvenience and can lead to other health issues, including bladder infections, kidney damage, and hygiene problems along with financial difficulties, decreased self-esteem, a heightened risk of falls and a greater likelihood of developing urinary tract infections. (5)

Self-Quiz
Ask Yourself...
- What is the best environment to make the above assessments?
- Would in-home assessments be more conducive to obtaining accurate information, especially if the client is embarrassed about their bladder issues?
- What are the different types of bladder dysfunction in MS and how do they each impact function?
- Are clients adequately prepared when diagnosed with MS of potential future bladder issues and what signs and symptoms to be aware of?
- Frequent nocturia is a frequent side effect of bladder dysfunction. What can be implemented in the home or facility to prevent falls when getting up to the bathroom?
Nursing Interventions
The role of the nurse in managing bladder dysfunction with MS is to understand whether the primary treatment goal is to improve the quality of life, safety, or both, and includes educating the client about bladder problems, explaining treatment options, monitoring urinary tract infections, and managing urinary urgency and incontinence. As the nurse, ask the client what they would most like to achieve, where they would like to see themselves at the end of therapy and what progress means to them.
Physical therapists may implement pelvic floor muscle training often beneficial for those with overactive bladder symptoms since the muscles that control the bladder contract involuntarily and too frequently before the bladder actually fills with urine. Implementing a bladder diary for a short time at the beginning and end of treatment can assist the nurse in establishing a baseline and demonstrate if improvement is seen in urgency episodes and urinary incontinence. (3)
Interviewing and assessing the client with MS for urinary symptoms should be done using open-ended questions and if they report urinary symptoms, then direct questions can differentiate between the different types of bladder dysfunction to guide treatment and the need for further workup.
After the initial assessment it is also important to assess for other health behaviors, co-morbid conditions, and medications that may be contributing to bladder dysfunction. Along with the nurse, the physical therapist can also ask about history of symptoms and goals, and will perform a physical assessment of the client’s pelvic, hip, and lower back. The pelvic floor muscles attach to the bottom of the pelvic bones and run from front to back and create the base of the body’s core. They also control the sphincter muscles, support the lower back, stabilize the pelvic bones and help with sexual function.
They may also look for external muscle problems and perform an internal exam. At the physical therapist’s discretion and depending on the needs of the client, this may involve a manual internal exam whereby the therapist inserts a gloved finger into the vagina or rectum as appropriate. Another option is an external exam, which uses two fingers to evaluate the muscles from the outside. (7)
These assessment methods can be integrated along with additional testing from a provider, including urodynamic testing (how well the bladder holds and empties urine) and an ultrasound or MRI to show any pelvic-floor muscle problems.
These approaches ensure a holistic approach to managing neurogenic bladder dysfunction, emphasizing the importance of subjective client-reported outcomes and objective clinical measurements to guide treatment decisions and enhance client care. Often, assessing how the bladder is functioning first involves screening for a UTI, which is very common in MS and can cause many symptoms. Treatment with an antibiotic should clear up the infection and improve the symptoms.

Self-Quiz
Ask Yourself...
- How important are cognitive assessments when caring for a client with bladder dysfunction from MS?
- Which management strategies can reduce the risk of symptomatic UTIs?
- What questions can assist in better understanding clients with MS for development of a care plan to help them to take control of bladder dysfunction?
- What is the best measurement of success in physical therapy interventions in bladder dysfunction?
Client Education for Managing Bladder Dysfunction
Educational topics nurses can teach clients for managing bladder dysfunction in multiple sclerosis include voiding, irritants and diuretics, fluid management, management of constipation, weight loss management, managing fatigue, and smoking cessation.
Voiding
Provide the following instructions/information:
- Urinate at regular intervals (ex: every two hours) to control the timing of the urination
- Timed voiding helps the person follow a schedule with set times to visit the restroom.
- Stagnant urine, caused by the bladder not emptying fully can provide a good environment for bacterial growth resulting in a UTI.
- Keeping a journal and scheduling times to urinate, whether or not they feel the urge
- Double voiding: void, urinate, wait a few minutes, then try to urinate again.
- Prompted voiding trains a caregiver to remind someone to go to the bathroom. The goal is to have fewer accidents by making the person aware that they need to urinate every so often.
- Recommend absorbent pads and condom-like sheaths for men
- The need to get up during the night to urinate. This interferes with sleep, leading to sleep deprivation and worsening of other MS symptoms, such as daytime fatigue.
Irritants and Diuretics
Provide the following instructions/information:
- Avoid citrus, spicy foods, caffeinated beverages (coffee, tea, soft drinks) and alcohol as they can all exacerbate urinary frequency or urgency.
- Avoid tobacco as nicotine can irritate the bladder and increase the urge to go.
Fluid Management
Provide the following instructions/information:
- Restrict fluid intake approximately two hours before starting any activity where no bathroom will be available and avoid drinking fluids after dinner to prevent nocturia.
- Do not restrict fluids on a continuous basis as this can increase the risk of infection by decreasing the normal flushing of the urinary tract. The body needs six to eight cups of fluids daily. Limiting water intake can lead to dehydration which can lead to constipation
- Drink water at designated times during the day and plan bathroom breaks afterward
- Drink a small glass of water all at once every few hours as this is better than sipping drinks constantly which can lead to feeling the need to urinate more often
- Stop drinking about 2 hours before going to bed
Management of Constipation, Weight Loss, and Fatigue
Implement the following interventions:
- Screen for constipation and treat as needed to reduce intraabdominal pressure.
- Counsel on dietary and lifestyle modifications to achieve a healthy weight
- Plan and prioritize tasks, incorporate time to rest, modify diet and reorganize living or workspaces to conserve energy. MS fatigue is not well understood and may be a result of damage to the myelin, necessitating alternative nerve pathways to be developed in the central nervous system. It can also be attributed to the extra exertion due to weakness, stiffness, spasticity, tremor and disturbed sleep or a combination of all of the above (14)
Smoking Cessation
Provide the following instructions/information:
- Stop smoking given that smoking irritates the bladder and worsens urinary symptoms
- Passive smoking could play a role in developing MS if a client is exposed to others’ smoking.

Self-Quiz
Ask Yourself...
- What education should be provided for the client and the caregivers about skin condition and incontinence?
- Can the addition of dietary / nutrition consults help educate the client and family on dietary changes?
- How can the implementation of a food diary and symptom tracker for the client with MS help to identify foods that could be exacerbating their bladder dysfunction?
- What non-pharmacological treatments can be taught to the client with MS related to dietary changes and the effects on bladder irritation and infections?
Physical Therapy Interventions
Physical therapy interventions for management of bladder dysfunction in clients with MS include pelvic floor exercises, electrical stimulation, acupuncture, Botox, and pelvic floor muscle assessments.
Pelvic Floor (Kegel) Exercises
Often goals for clients are to decrease incontinence pad usage, decrease trips to the bathroom during the day or at night, and empty their bladder all the way. The physical therapist can provide clients with a list of exercises that involve contracting and relaxing the muscles that support the urethra, bladder, uterus and rectum. They can train on contracting, relaxing and coordinating the muscles involved in bladder and bowel control, helping to normalize these functions. (16)
Electrical Stimulation
Electrical stimulation is a therapeutic intervention with minimal adverse effects that has been studied for lower urinary tract symptoms. There are a variety of nerve stimulation techniques available to help control and strengthen the bladder muscles. The tibial nerve can be stimulated with electrical currents to calm an overactive bladder. (16)

Image 1. Electrical stimulation therapy
Acupuncture
Acupuncture can be provided as a complementary or alternative treatment and involves inserting very thin needles into the skin, placed at specific points to stimulate the body’s natural healing abilities. (16)
Botox
Injectable Botox can ease spasticity where the muscles are abnormally stiff and tight, prone to involuntary spasms. It can also be used for neurogenic detrusor overactivity caused by nerve damage making the muscles around the bladder overactive, resulting in incontinence and reduced quality of life. Treatment involves multiple injections into the detrusor muscle, or for spasticity, injections in the upper or lower limbs divided across the affected muscles. (16)
Pelvic Floor Muscle Assessment
Pelvic floor muscle assessments are conducted through digital vaginal and rectal palpation as well as electromyography (EMG) biofeedback. These assessments identify muscle strength, functionality, and mobility issues. (4)
Treatment
Medications
When therapeutic options for bladder control do not seem to be working, medication may help. Medication options are available for people who often have sudden, intense urges to urinate called overactive bladder. They’re also available for those who have urine leaks that can happen along with overactive bladder, called urge incontinence.
The plan of care may have to be adapted around the medication for the best outcomes. Some side effects of these medications include flu-like symptoms, symptoms similar to those experienced by clients receiving chemotherapy (i.e. nausea, vomiting, bladder infections, etc.) and changes in heart rate. The typical therapy session may have to be adjusted depending on the client’s reaction to their medications.
The following medications may help with bladder dysfunction by blocking the action of the chemical messenger, acetylcholine (9). Acetylcholine sends signals to the brain that trigger bladder contractions that are associated with an overactive bladder. These contractions can cause a need to urinate even when the bladder isn’t full.
- Darifenacin: an extended-release antispasmodic/antimuscarinic medication that relaxes the bladder muscles to prevent urgent, frequent, or uncontrolled urination
- Fesoterodine
- Imipramine: an antidepressant with an anticholinergic effect that benefits bladder frequency at night. Also prescribed to manage pain in MS.
- Oxybutynin: relaxes bladder muscle spasms and the frequent urge to urinate
- Solifenacin: used to treat an overactive bladder and the associated symptoms such as frequency, urgency and incontinence.
- Tolterodine: an antimuscarinic drug that inhibits the action of the neurotransmitter acetylcholine that is used to treat bladder spasms responsible for urinary frequency, urgency or incontinence
- Trospium: relaxes the bladder muscles to prevent urgent, frequent or uncontrolled urination
- Oxytrol: skin patch that delivers the active ingredient oxybutynin through the skin into the bloodstream. It decreases bladder muscle spasms, relieving the frequent urge to urinate
- Propantheline: an antispasmodic / anticholinergic medication that relieves muscle spasms of the bladder to control urination
If treatment with any of these medications does not manage overactive bladder, doctors may recommend treatment with Botox (botulinum toxin A), a powerful nerve toxin that is approved by the FDA to treat incontinence.
Mechanical Aids
An intermittent catheter is a mechanical aid that assists the urine to drain from the bladder and can improve the quality of life for some people. It allows for complete emptying of the bladder at regular intervals, protecting the kidneys from infection and damage, lowering the risk of distending the bladder and eliminating the need for wearing a continuously draining catheter.

Image 2. Intermittent urinary catheterization kits
Other mechanical aids include (8):
- Urethral insert: thin, flexible solid tube in the urethra that blocks the flow of leaking urine
- External urethral barrier: self-adhesive patch over the urethra
- Suprapubic catheter: urinary catheter surgically inserted in through the abdominal wall just above the pubic bone and into the bladder so that urine can drain out; offered by some urologists
Clean, intermittent self-catheterization can be a daunting aspect of self-care for the client with MS. Strategies to improve adherence to this technique:
- Alleviate the client’s fears and anxieties about the procedure during the initial consultation
- Provide them with accessible anatomical information about the bladder and how complications, including infection, can occur
- Explain how this technique is designed to reduce the risk of infection and improve the quality of life
- Inform them about the process verbally, in writing and/ or with a visual aid
- Repeat the education often and as needed
- Assist the client in having choice in terms of catheter selection, with a focus on comfort, client preference and ease of use and prevention of infection
If the client develops recurrent urinary tract infection after starting clean intermittent self-catheterization (12):
- Check that their technique is correct (hand hygiene, frequency of application, and use of lubrication)
- Check if the catheter length is suitable for the client. Is it long enough to drain the bladder?
- Explain how this procedure is designed to reduce the risk of infection and improve quality of life
- Only consider prophylactic antibiotics if all other options have been ruled out. Antibiotic prophylactics should be reviewed every 6 months.
Catheter Acquired Urinary Tract Infections (CAUTIs) are often caused by hospital-based pathogens that have become resistant to antimicrobials. People with urinary catheters have a higher chance of getting a UTI. Recurrent UTIs in people with bladder dysfunction are a cause of considerable morbidity. UTIs may exacerbate incontinence, cause symptoms of malaise, and progress into upper urinary tract infections with possible loss of urinary function. Intermittent or permanent catheterization may inevitably exacerbate the problem, but incomplete bladder emptying is also a predisposing factor for UTIs.
Best practices for prevention of CAUTI include (17):
- Limit the use of indwelling urinary catheters to only appropriate indications
- Remove indwelling urinary catheters as soon as possible, since the risk of CAUTI development increases with longer duration of use
- Consider the use of a condom catheter or other external catheter or intermittent catheterization as alternatives to indwelling urinary catheters
- Use proper aseptic technique during catheter insertion
- Adhere to optimal catheter maintenance throughout the duration of catheter use
- Provide ongoing assessment and education of proper technique for the client or caregivers

Self-Quiz
Ask Yourself...
- Is intermittent catheterization a feasible option of clients with significant upper extremity weakness, poor dexterity or cognitive function?
- Does the cost of catheters for non-insured clients pose a risk for their compliance?
- What are some other non-infectious complications of urinary catheter use?
- Due to the frequency of UTIs with bladder dysfunction, how can the development of an at-home test kit for the client with MS eliminate the need for a clinic, urgent care or ER visit?
- Can transfer of urinary tract infections occur between two clients residing in the same room in care facilities?
Barriers to Optimal Rehabilitation
Rehabilitation therapy from physical and occupational therapists can help reduce urinary urgency or incontinence and ensure proper bladder emptying. This involves finding the right balance in managing symptoms related to neurogenic detrusor overactivity and bladder retention. Screening for cognitive deficits is important as an indicator of the client’s ability to participate with self-care activities. Common issues may include deficits in memory, attention, concentration, executive function, visual perception, and verbal fluency. (13)
Visual Deficits
Common visual problems include optic neuritis (optic nerve inflammation), diplopia (double vision), and nystagmus (involuntary eye movement). Visual disruption often goes unnoticed until after several therapy sessions or until an actual problem occurs (i.e. falls, decreased activity participation, spills, etc.) By catching visual deficits early, the therapist can modify their intervention planning as needed. (13)
Fatigue
Exhaustion can set in at different times and varying levels of intensity depending on the person. Assisting the client in tracking their periods of fatigue will help optimize therapy around those times. In addition, educating on energy conservation techniques when working with the client will help make therapy sessions more productive. (13)
Pain
Pain is a strong motivator to avoid therapy. Collaborate with the person about their pain, the location, the intensity, at rest, with activity, and which activities tend to exacerbate episodes. (13)
Mobility
Functional mobility can range from completely independent to ‘total assist’ depending on the type and severity of the MS. Knowing the level of mobility and assist levels will help give an idea about what approach to take; remediate (strengthening, functional activity tolerance) or compensatory (crutches, walkers, manual chairs, power chairs, etc.) (13)

Self-Quiz
Ask Yourself...
- How does a therapist address a person’s fatigue and prevent over-exertion when seeing a client with MS in a rehab setting where sessions can be long and up to five times a week?
- What evaluations and / or treatments can be done to maintain or prevent decline in hand function for a client with MS, especially one who may need to perform self-catheterization frequently?
Disease Progression and the Involvement of the Care Team
Over the course of the disease progression, it is necessary to reassess clients with MS in order to adjust their therapies. In many people, conservative and pharmacological therapies show diminishing effectiveness, which may be due to the cumulative impact of physiological, cognitive and physical changes over the course of MS. For this reason, it is important to regularly change treatment regimens of clients with MS for urological safety and to promote their quality of life. If the conservative and pharmacological treatments become ineffective, it is important for both providers and clients to understand the benefits, risks, and outcomes of secondary and tertiary treatments related to MS. (3)
Various techniques can be used to maintain continence or empty the bladder (11):
- The Crede maneuver involves manual compression of the bladder; it is used in clients with decreased bladder tone and low outlet resistance
- Increasing intravesical pressure may also be achieved through the Valsalva maneuver (i.e. abdominal straining)
- Reflex bladder contraction may be provoked by pinching or stimulating the lumbar and sacral dermatomal levels
Many clients with MS aren’t aware that bladder dysfunction is an MS-related issue and don’t bring it up to their doctors. Additionally, doctors don’t always discuss bladder dysfunction with their clients unless the client brings it up. It can be an embarrassing, uncomfortable situation and can have a major effect on quality of life. Some refuse to leave their home because they are afraid they will have an accident, making it emotionally and socially isolating which can lead to loss of self-confidence and independence. (6)
The addition of nursing and physical therapy in the treatment of bladder dysfunction in MS can assist in protecting and preserving renal function, relieving symptomatic voiding dysfunction and incontinence, preventing urinary tract infection, and eliminating risk factors for subsequent urinary complications.
Other members of the care team may include a urologist or urogynecologist trained in the management of urinary dysfunction and a nerve specialist. Often clients are referred to a urologist for impaired emptying or storage of urine, and to determine the cause and develop a treatment plan. Other reasons for a urology referral include lack of benefit or inability to tolerate standard therapies for their symptoms or if they develop secondary complications including recurrent UTIs, renal impairment, hematuria, and kidney or bladder stones. (4)
If the client is receiving in home nursing and therapy, the addition of a home health aide can assist with activity and ADLs (bathing, dressing, grooming), reinforce the treatment plan, and report changes.

Self-Quiz
Ask Yourself...
- How can the therapist and nurse on the care team deal with a person with burnout who has had MS for many years and has become more noncompliant?
- How can attainable treatment goals be continuously set for clients who may not be able to attain them but are still needed to maintain a level of independence and involvement with therapy?
- If the client is capable, or has a competent caregiver capable of performing the Crede maneuver, should this be taught as an option for clients in their home?
- When should a person be referred to a urologist?
Support for Clients with Multiple Sclerosis
One way to support clients with MS is to educate the family and / or other caregivers to better understand how the disease affects people’s lives. All members need to understand it is a lifelong condition and can be tough to face alone. Support groups for bladder dysfunction can provide practical information, resources, guidance and even long-lasting friendships. These groups aim to provide education, support, and a safe place to discuss bladder conditions because everyone in the client’s life may not understand how debilitating MS can be. Being able to talk to someone who shares their experiences can be a great help. Online support groups allow connection with people who share a common issue in a safe virtual environment.
Research suggests that approximately one-third of people with MS have contemplated suicide at some point in their disease course. Observing and monitoring a client’s emotional status can help identify those with new or worsening depression brought on by the abrupt changes in their health, intense bereavement, hopelessness, social isolation, and worrying about being a burden. There is often a fear that asking a client about suicide increases the risk of suicide but if red flags are present, it is important to assess for safety and ask questions about the client’s access to firearms and other means of suicide. (15)

Self-Quiz
Ask Yourself...
- The client with MS dealing with bladder dysfunction has many issues to deal with. What role does stress play in the functioning of the bladder and the development of UTIs?
- Does bladder incontinence cause mental health issues? How can the nurse or therapist evaluate all aspects of the client with MS when working with them for bladder dysfunction issues?
- What skills would the client need to use and/or develop to be successful in the health management of MS and their bladder dysfunction?
- What open-ended questions can be used as part of a general review of symptoms when assessing a client with MS to determine if they are having bladder issues?
- Are clients with bladder dysfunction at risk of dehydration due to withholding fluids to prevent their bladder issues? How can this be mitigated?
- When caring for a client with MS and bladder dysfunction residing in a rehab or long-term care facility, what should the nurse and/or therapist instruct the aides to observe and report? (i.e. symptoms of UTI, etc.)
- Can pelvic floor training be successful in the elderly?
- How can the care team implement virtual visits for clients with MS who have bladder dysfunction and difficulty making it into a clinic?
- An inpatient admission for a client with MS can be a stressful event and can cause further setbacks and complications. What alternative care methods can be implemented quickly and safely to avoid an inpatient admission?
- Medication compliance is of utmost importance when evaluating and treating bladder dysfunction or UTIs. What methods can be implemented in the home to assure compliance with prescribed medications?
- Is just urine testing a reliable indicator of a UTI in clients with MS who are self-catheterizing or have an indwelling or suprapubic catheter?
- What activities can home health aides do to provide ongoing monitoring of a client’s condition?
- What information, education, and support do adults with MS and their families / caregivers need to help them feel less isolated?
Conclusion
Bladder dysfunction is present in the majority of people with MS and contributes to significant disability in many. Urinary symptoms are often ignored or minimized yet if the appropriate management strategies can be implemented there can be a favorable outcome. Successful management of bladder dysfunction must be multifaceted and multidisciplinary while recognizing that desirable outcomes will vary with each client.
As a clinician caring for a client with MS and bladder dysfunction, recognize that the course of treatment and achievement of goals may be frustrating for the clinician and the client. Involving other members of the care team, including providers, can help to implement a plan of care that assists the client in adapting to the physical changes that occur as the disease progresses while supporting them through their disease process.
References + Disclaimer
- Tobin, O. (2024, November 4). What is multiple sclerosis? An expert explains. https://www.mayoclinic.org/diseases-conditions/multiplesclerosis
- National Institute of Neurological Disorders and Stroke. (2024, October 11). Multiple sclerosis. https://www.ninds.nih.gov/health-information/discorders/multiple-sclerosis
- Bientinesi, R., Gandi, C., Pierfrancesco, B. (2020, June 30). Managing urological disorders in multiple sclerosis patients: A review of available and emerging therapies. International Neurology Journal: 118-126.
- Cleveland Clinic/Neurological Institute. (2024). Management of bladder dysfunction in multiple sclerosis. https://my.clevelandclinic.org/departments/neurological/depts/multiple-sclerosis/bladder dysfunction
- Manilia, A., Roman, N., & Basalic, E. (2024, July). The effect of rehabilitation therapy in patients diagnosed with neurogenic bladder: A systemic review.1152. https://pmc.ncbi.n;m.nih.gov/articles/PMC11278912
- Sheehan, J. (2023, September). 10 ways to take back control when MS causes bladder dysfunction. https://www.everdayhealth.com/multiplesclerosis/symptoms/coping-with-bladder-dysfunction/
- Phillips, Q. (2023, February). Pelvic floor physical therapy for MS: Help for bladder, bowel, and sexual function. https://everydayhealth.com/multiple-sclerosis/pelvic-floor-physical-therapy-for-ms
- Melinossky, C. (2022, August). Multiple sclerosis and bladder control problems. https://webmd.com/multiple-sclerosis/bladder-control-problems/
- Multiple Sclerosis News Today. (2024). Managing bladder dysfunction in MS. https://multiplesclerosisnewstoday.com/therapies-for-managing-ms-sysmptoms/bladder-dysfunction/
- Hendin, B. (2023). Bladder Dysfunction. Multiple Sclerosis Association of America. https://mymsaa.org/ms-information/symptoms/bladder-dysfunction/
- Carter, G. T. (2023). Bladder dysfunction treatment & management. Medscape. https://emedicine.medscape.com/article/321273-treatment/
- Balhi and Khalil Mrabet. (2020). Management of bladder dysfunction in people with multiple sclerosis. https://www.mssociety.org/sites/default/files/2023-06/Concensus-2021-Hollister/
- Chandler, M. (2021). OT and multiple sclerosis: Treatment tips and strategies. https://www.myotspot.com/occupational-therapy-multiple-sclerosis/
- National Institute for Health and Care Excellence. (2022, June). Multiple Sclerosis in adults: Management. Nice Guideline (NG220). https://www.nice.org.uk/guidance/ng220
- Neurosciences/Advancing Patient Care. (2019). Suicide in Patients with Multiple Sclerosis: Guidance on Red Flags and Prevention. https://consultqd.clevelandclinic.org/suicide-in-patients-with-multipl-sclerosis-guidance-on-red-flags-and-prevention/
- Wexler, M. (2022). Botox (onabotulinimtoxinA) for multiple sclerosis. https://multiplesclerosisnewstoday.com/botox-onabotulinumtoxina-for-bladder-dysfunction/
- Clark, K. (2020). Catheter-associated urinary tract infections in adults: Diagnosis, treatment, and prevention. https://cdn.mdedge.com/files/s3fs-public.jhm01509552.pdf/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
