Course
Breast Reconstruction Surgery after Mastectomy
Course Highlights
- In this Breast Reconstruction Surgery After Mastectomy course, we will learn about the different types of breast reconstructive surgeries.
- You’ll also learn common misconceptions surrounding mastectomies and breast reconstructive surgeries.
- You’ll leave this course with a broader understanding of the importance of patient education prior to and following the breast reconstructive procedure.
About
Contact Hours Awarded: 1
Course By:
Abbie Schmitt
MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Cancer is a devastating term and those given this diagnosis will more than likely be overwhelmed with fear and confusion. Although the cancer treatment itself is a large undertaking, breast reconstruction surgery following mastectomies is also a substantial procedure. However, breast reconstruction involves “building back” and restoring rather than removal. The advancements of breast reconstructive surgery should be celebrated. Nurses should be equipped with knowledge on breast cancer, statistical data, and types of mastectomies and reconstructive surgeries. It is also important to review appropriate care before and after the surgery, common misconceptions about reconstructive surgery, body image concerns, and resources.
Overview of Breast Cancer and Statistics
Breast cancer can be defined as a disease characterized by abnormal cells within the breast tissue that grow and invade surrounding tissues or spread (metastasize) to other areas of the body. This group of abnormal cells is referred to as a tumor, and the cells can spread by breaking away from the original tumor and entering blood vessels or lymph vessels, which branch into tissues throughout the body. Metastasis refers to this travelling of cancer cells that started in the breast and went to various parts of the body and begin damaging other tissues and organs.
Brief Anatomy Review on the Breast
It is a common misconception that mastectomies are rather simple because breast organs are not complicated. This could not be further from the truth. The breast organs are an intricate group of distinct and functional parts. We will review the anatomy to explain this better.
The glands of the breast are located within the anterior chest wall and consist of 15 to 20 lobes of tubuloalveolar glandular tissue, 20-40 lobules within those lobes, fibrous connective tissue, and adipose tissue between the lobules (2). Small milk ducts are attached to the lobules and joined together like branches of grape stems, which gradually form larger ducts (11). There are deep layers of the superficial fascia that lie upon the posterior surface of the breast and are connected to the deep (pectoral) fascia of the chest wall.
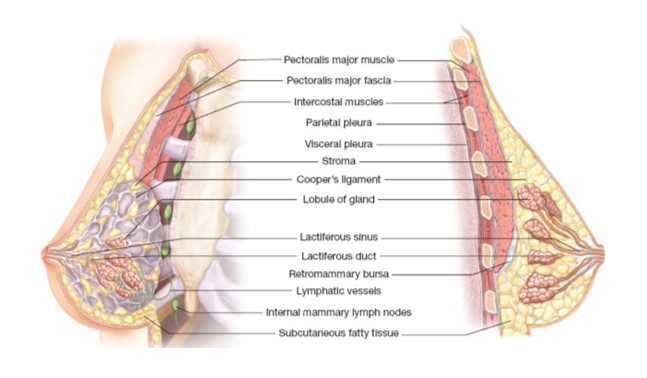
Image 1. Breast and Chest Wall Anatomical Makeup (2)
Statistics
We are fortunate to have an abundance of statistics on breast cancer epidemiology, mastectomies, and breast reconstructive surgeries. Breast cancer is one of the most common cancers diagnosed among women in the United States and is the second leading cause of death from cancer among women (lung cancer is the leader) (1). Breast cancer also represents the most common cancer that affects women within impoverished nations of the world (2).
Breast cancer incidence in the United States:
- Breast cancer is a leading cancer among women in the U.S., second only to skin cancer.
- 40% of diagnosed breast cancers are detected by women who feel a lump (6).
- 1 in 8 women, or approximately 13% of the female population in the U.S., will develop breast cancer in their lifetime (3).
- It is estimated that in 2023, approximately 30% of all new female cancer diagnoses will be breast cancer.
- Approximately 64% of breast cancer cases are diagnosed at a localized stage, which correlates with better outcomes.
- The 5-year relative survival rate for cancer diagnosed at the localized stage is 99%.
- Approximately 15% of women diagnosed have a family history of breast cancer.
- Those with a first-degree relative (mother, sister, daughter) with breast cancer are nearly twice as likely to develop breast cancer. (3)
- Caucasian women have the highest incidence rate for breast cancer, followed by Black women, Hispanic women, Asian/Pacific Islander women, and finally American Indian/Alaska Native women.
- Black women see higher death rates from breast cancer (6).

Self-Quiz
Ask Yourself...
- Are you familiar with breast cancer screening?
- Can you explain why localized breast cancer has more positive outcomes?
- How should screening and teaching be different for those with a strong family history?
Types of Mastectomies
Surgical therapy remains one of the primary modalities used to treat breast cancer (2). Mastectomy is the term describing the surgical procedure of removing breast tissue. The surgery may also include the removal of overlying skin, the nipple and areola, muscle, and the lymph nodes. There are different types of mastectomies depending on the extent and type of cancer found. A unilateral mastectomy refers to the removal of one breast and a bilateral or double mastectomy is performed when both breasts are removed (11).
Simple Total Mastectomy
The following is removed during a simple total mastectomy:
- All of breast tissue
- The nipple and areola
- A portion of the overlying skin
The muscle beneath the breast is not removed. The surgeon checks the lymph nodes for cancerous tissue during surgery.
Skin-Sparing Mastectomy
The following is removed during a skin-sparing mastectomy:
- All of breast tissue
- The nipple and areola are imminently reconstructed
This procedure is done with the intent to avoid damage to as much overlying healthy skin as possible. This is not the most effective type, especially if there is a possibility that cancer cells are close to the skin. A key principle in breast surgical oncology is the need to excise normal tissue around a cancer as well and establish clear margins; positive margins is when cancerous cells are at the edge of incision and has significant association with a higher local recurrence rate (4).
Nipple-Sparing Mastectomy
The following is removed during a nipple-sparing mastectomy:
- All of breast tissue
The nipple, areola, and overlying skin are left intact. This option allows for a more natural-looking reconstruction. This type is not appropriate if the cancer is near the nipple or detected in the margins (4).
Modified Radical Mastectomy
The surgeon removes the following during a modified radical mastectomy:
- All of breast tissue
- Skin covering the breast
- The nipple and the areola
The chest wall muscle is left intact.
Radical Mastectomy
A radical mastectomy is the most extensive type of mastectomy and is only performed when the breast cancer has spread to the muscle beneath the breast (6).
The following is removed during a radical mastectomy:
- All of breast tissue
- Skin covering the breast
- The nipple and the areola
- The chest wall muscles under the breast
- Some of the axillary lymph nodes
Breast reconstruction or prosthesis are options. Due to the extensive nature of this procedure, patients have more in-depth risks and complications (11).
Prophylactic Mastectomy
The surgeon removes the following during a prophylactic mastectomy:
- All of breast tissue without any finding of cancerous cells.
This type of mastectomy is a prophylactic measure. Indications for this type include a strong family history of breast cancer or a BRCA gene mutation (2).
Contralateral Prophylactic Mastectomy
The surgeon removes the following during a contralateral prophylactic mastectomy:
- All of breast tissue
- Lymph nodes are spared
- The removal of surrounding skin or nipple and areola depends on family history types of cancer or gene mutations
Contralateral prophylactic mastectomy refers to the surgical removal of a healthy, non-cancerous breast for prophylactic reasons following the diagnosis of cancer in the other breast. This has become more popular in the past 20 years (6).
Appropriate candidates for this type of mastectomy:
- Presence of a gene mutation linked to breast cancer
- BRCA1, BRCA2, or PALB2
- Strong family history of breast cancer in more than one first-degree relative
- First-degree: Mother, sister, or daughter
Salvage Mastectomy
This type describes a second surgery that is done if cancer has returned following a mastectomy. The amount of breast tissue removed depends on the size, nature, and invasiveness of the cancer found (11).

Self-Quiz
Ask Yourself...
- Have you cared for a patient following a mastectomy?
- Can you name risk factors for breast cancer malignancy?
- Discuss reasons minimal removal of tissues would be beneficial?
- Can you describe what “positive margins” refers to?
Types of Breast Reconstructive Surgeries
There is a reason to celebrate the development of breast reconstructive surgeries over the past century. Highly effective and minimally invasive approaches have been implemented to move from disfigurement to reconstruction. Essentially, those diagnosed with breast cancer and the need for removal of the breast have the chance to continue living with a surgical created breast that resembles the natural breast. The goal of breast reconstructive surgery is to improve patient’s confidence in appearance, restore functional needs, and promote comfort in wearing clothing. Reconstructive surgery also removes the need for uncomfortable prosthetics.
There are two main types of breast reconstruction surgeries: breast implants and flap surgery. Implantation involves surgically inserting an expander or an implant that contains either silicone gel or saline and resembles a natural breast in texture and shape (5). Flap surgery involves using tissue from the patient’s own body.
Tissue Expanders and Implants
Implant-based breast reconstruction accounts for more than 86% of breast reconstruction surgeries in the U.S. (8). In the most modern version of this procedure, the pectoralis major muscle is raised to make room for a mesh or implant. Studies show that this procedure reduces trauma and distortion of the normal anatomy of the chest wall, leading to reduced postoperative pain, quicker recovery, and a lower risk of bleeding than when other muscles are involved (8).
Implants are usually placed as part of a two-stage procedure. In the first stage, the surgeon places a tissue expander under the skin or under the chest muscle, which is slowly filled with saline during periodic visits following surgery (9). In the second stage, once the chest tissue has healed enough and expanded without complication, the expander is removed and replaced with an implant (9). The time frame for this process is 60 – 180 days after the mastectomy. In some cases, the expander can be placed in the breast during the same surgery as the mastectomy.
Breast reconstruction techniques can rebuild the nipple and recreate the areola for those who have had these removed (9). Nipple reconstruction is usually a separate surgery that occurs weeks or months after the main breast reconstruction surgery, allowing the reconstructed breast to heal and settle into a final position first (9).
Flap Reconstruction
Flap surgery involves the use of the patient’s own body tissue, such as muscle or fat, to replace the breast tissue removed (9). This tissue is called a flap. This process essentially builds back the breast using one’s own tissue from another part of the body. Flap reconstruction is a more complex surgery and requires a longer hospital stay and recovery time when compared with implantation. Flap surgeries are different from skin grafts because these flaps have their own circulatory network of vessels to provide circulation if the process is successful (ROH). Flap surgeries may also be called autologous tissue reconstruction.
Different sites in the body can provide flaps for breast reconstruction. Flaps used for breast reconstruction most often come from the abdomen or back but can also be taken from the thigh or buttocks (9).
Types of flap surgery for breast reconstruction: (9)
- DIEP flap and SIEA flap (also called SIEP flap): Tissue removed from the abdomen.
- DIEP and SIEA flaps use different set of vessels
- Contains only skin, blood vessels, and fat
- No underlying muscle
- Latissimus dorsi (LD) flap: Tissue comes from the medial or lateral back
- TRAM flap: Tissue comes from the lower abdomen
- Similar to DIEP flap, except the underlying muscle is included in flap
- IGAP flap and SGAP flap: Tissue comes from the buttocks
- IGAP and SGAP flaps use different sets of vessels
- Contains only skin, blood vessels, and fat
- No underlying muscle
- PAP flap: Tissue comes from the upper inner thigh
- Contains only skin, blood vessels, and fat
- No underlying muscle
- TUG flap: Tissue comes from the upper inner thigh
- Contains skin, blood vessels, fat, and underlying muscle
The success of the flap survival in reconstruction relies on circulation, so certain conditions can impede healing and success. Examples of conditions include uncontrolled diabetes, poor circulation, connective tissue disease, and use of tobacco.
The following may be considered contraindications for breast reconstruction surgery using flaps: (9)
- Age greater than 65 years
- Severe lung or cardiac disease
- Collagen vascular disease
- Obesity
- Current tobacco use with refusal to quit
- History of conditions or surgeries that interrupted blood supply to potential flaps
- Prior radiation therapy
- Advanced, metastatic breast cancer

Self-Quiz
Ask Yourself...
- What would be examples of fears or worries patients may have about breast reconstruction surgery?
- Can you describe why flap surgery would have a longer recovery than implant use?
Preparing for Surgery
Pre-operative planning for breast reconstruction surgery is one of the most important phases of the process. Patients undergoing breast reconstructive surgery may have feelings of anxiety or uncertainty. For the life-saving mastectomy surgery, the patient has limited to no options in aspects of that surgery, including the amount of tissue removed or location of scarring. Now is the time for their desires and voice to be integrated into the surgical plan. The result should reflect their ideal aesthetic goals as much as possible.
The initial consultation for breast reconstruction involves reviewing the patient’s medical history, understanding the type and depth of the mastectomy, completing a physical examination, and arranging for imaging (5). A thorough review of the patient’s co-morbidities is vital for determining possible risks of surgery and complications. The issue of current smoking status is also important. The patient should be made aware that the rate of mastectomy flap necrosis increases significantly in active smokers (2). This pre-operative visit also involves getting to know the patient from a personal and psychological perspective to understand their motivating factors for getting breast reconstruction surgery.
Once a type of reconstruction surgery (flap or implant) is chosen by the medical provider and patient, the pathways will vary. Preoperative imaging for both types is essential, including the mammogram, ultrasound, and MRI studies. For flap surgeries, additional preoperative imaging may be ordered by the surgeon for mapping perforator anatomy. Computerized tomography angiography (CTA) and magnetic resonance angiography (MRA) have specific protocols for obtaining useful mapping and evaluating circulation to specific locations (5).
Other topics of discussion and patient education prior to surgery:
- Types of anesthesia that will be used
- Location of the surgical sites
- How long the surgery will take
- Possible complications of surgery (long-term and short-term)
- What to expect after surgery
- Follow-up planning
Post-Operative Considerations and Incision Care
A terrific resource for nurses caring for a patient who has undergone breast reconstructive surgery is an approach called Enhanced Recovery After Surgery (ERAS). These are evidence-based guidelines to optimize hydration, nutrition, pain control, activity, self-care, and recovery time.
Possible complications:
- Bleeding
- Wound infection
- Fluid accumulation or hematoma within the reconstructed breast
- Deep vein thrombosis (DVT)
- Pulmonary embolism
- Temporary urinary retention
|
Nursing Diagnosis |
(Related to) Factors and Assessments |
|
Ineffective airway clearance |
Respiratory assessment
Airway patency Airway management |
|
Risk for bleeding |
Surgical wounds and impaired circulation
Circulatory assessments
Wound Assessments |
|
Pain |
Pain assessments, teaching on ordered pain medication, positioning, splinting, assistive devices, alternative pain treatment options. |
|
Risk for infection |
Wound Assessments |
|
Risk for activity intolerance |
Occupational and physical therapy
Pain management |
|
Risk for constipation |
Activity
Ordered medications (stool softeners) |
|
Disturbed body image |
Psychosocial assessment and interventions
Supportive resources: support groups, counseling, pastoral care |
|
Bathing self-care deficit |
Need for occupational and physical therapy |
|
Risk for peripheral neurovascular dysfunction |
Neurosensory assessments |

Self-Quiz
Ask Yourself...
- Why do you think CTA imaging is important for flap procedures?
- Can you name reasons tobacco use or conditions affecting circulation (diabetes, peripheral vascular disease) will impact flap surgery?
- What are different reasons a patient may choose to have breast reconstructive surgery?
- Can you name reasons it is important to have a required length of time between a mastectomy and reconstructive surgery?
Patient Education
There is an abundance of education topics for the patient following breast reconstructive surgery. Immediate teaching includes wound care, dressing changes, infection prevention, drain management, activity, pain management, and follow-up appointments. Patients have also verbalized an “overload of information” and reported they were unable to remember a lot of the information provided. Nurses should remember to gradually provide information and utilize different forms of teaching based on patient learning styles and foundation of knowledge. Surgeons typically provide in-depth verbal information to patients, but nurses can supplement by incorporating photographs, websites, and pamphlets that illustrate a variety of body types, procedures, and outcomes.
Topics for patient education:
- Wound assessment
- Teach the patient and caregiver about skin and wound assessment and ways to monitor for signs and symptoms of infection, complications, and proper healing.
- Importance of proper nutrition, hydration, and methods to maintain tissue integrity
- Adequate caloric intake and balance of protein and essential vitamins has been shown to improve healing (11).
- Dressing changes, wound cleansing, hand hygiene
- Pain management
- Medications
- Heat/cold therapy applications and precautions
- Drain maintenance
- Showering restrictions
- Follow-up appointments

Self-Quiz
Ask Yourself...
- Are you familiar with your facility’s database for patient education?
- For this particular subject, why would it be useful to use photographs or diagrams to explain the expected result?
Common Misconceptions
Misconception #1
Mastectomies cause lifelong disfigurement.
Breast reconstruction surgery is a personal choice, many decide not to get this procedure. However, if disfigurement or loss of feeling feminine is a concern, there have been great advancements in plastic surgery in the past decade to build back the breast to meet patient needs and desired looks.
Misconception #2
It is better to remove both (Contralateral Prophylactic Mastectomy).
A rising trend noted among those who are diagnosed with early-stage breast cancer in one breast is the choice to get a bilateral mastectomy. As we discussed earlier, a contralateral prophylactic mastectomy refers to the surgical removal of a breast for prophylactic reasons (2). However, some in the medical community, including oncologists, report a common concern: many women are choosing to have this type of mastectomy when their risk of having breast cancer in the other breast is lower than they may understand. Studies show that women with an average risk who were diagnosed with cancer in one breast, have a likelihood of developing cancer in the other breast at about 1% or less per year (3).
Misconception #3
Breast reconstructive surgery will make it more difficult to detect recurrence of cancer.
Research studies show that breast reconstruction does not increase the risk of recurrence or impede with detection and mammography (9). However, women with a breast implant should alert the radiology technician about the implant before the mammogram, as special procedures may be necessary to ensure the accuracy of the mammogram and to avoid damaging the implanted breast.
Misconception #4
Sensation to the breast will be permanently lost following mastectomy and breast reconstruction surgery.
Following mastectomies, patients may experience varying degrees of breast numbness and loss of sensation due to nerve damage when breast tissue is removed during surgery (2). However, as the severed nerves grow and regenerate, sensation can begin to return (6). Also, breast surgeons continue to make surgical advances in techniques to spare or repair damage to nerves.
Body Image Concerns
Body image, defined as an individual’s perception and feelings about their own body, can significantly impact overall well-being. Body image is influenced by internal factors such as age, gender, ethnicity, and physical condition, as well as external factors like social and environmental influences. Body image disturbance is associated with multiple mental health conditions, including depression, anxiety, disordered eating, body dysmorphia, and post-traumatic stress symptoms (11). It is expected for these patients to have a healthy amount of concern for a drastically altered part of their body, but the healthcare team should be concerned if the behavior leads to significant distress in the patient. In a recent poll among patients following a mastectomy and reconstructive surgery, 37% of the participants reported they had significant concerns about the changes in their body image (10). The nurse has a pivotal role in guiding the patient in the process.
Resources:
- Counseling or therapy
- Support groups
- Body positive movements and organizations
- Incorporating support systems (family, caregiver, friends)
Nursing Goals and Outcomes:
- Patient will verbalize understanding of body changes.
- Patient will incorporate body image change into self-concept in an accurate manner without negating self-esteem.
- Patient will appropriately look at, touch, talk about, and care for breast reconstructed areas and drains.
- Patient will verbalize adaptation and relief of anxiety.
- Patient will actively engage, ask for information, and pursue growth.
- Patient will verbalize understanding of adaptive devices/prostheses as needed.
Examples of manifestations of a client with disturbed body image:
- Verbal preoccupation with changed body part or function
- Intentional hiding of body part
- Refusal to discuss or acknowledge the change
- Refusal to look at or care for altered body part
- Change in social behavior such as withdrawal or isolation

Providing Support and Resources
The nurse and medical team should monitor for complications, some of which can occur months or even years after surgery. Patients may benefit from physical therapy to improve or maintain shoulder range of motion and use exercises to regain strength, adjust to new physical limitations, and explore ways to perform everyday activities (9). The Food and Drug Administration (FDA) recommends that those with silicone implants have periodic MRI screenings to detect rupture of the implants (9).
Ongoing support and screening are important. Organizations such as the National Breast Cancer Foundation, Inc. and National Cancer Institute provide excellent resources. Nurses in particular can pursue oncology or plastic surgery specialty certifications. The oncology nursing specialty incorporates education and experience for the reduction of cancer risks, promotion of early detection, improving the management of cancer symptoms and side effects throughout the disease, and coordination of complex care needs (11).

Self-Quiz
Ask Yourself...
- Can you name reasons why “disfiguration” may be a huge concern and misconception?
- Are you familiar with newer and less invasive methods of plastic surgery?
- What are examples of nursing specialties that may encounter patients with mastectomies or those who have had breast reconstruction surgery following a mastectomy?
Conclusion
If you notice someone wearing a pink ribbon, more than like they have experienced a battle with breast cancer themselves or with someone they love. Battling breast cancer is a long and difficult journey. The process can be compared to a difficult and unexpected journey (cancer), with a long plane ride (mastectomy), awful layovers (radiation/chemotherapy), and once you arrive to your destination, you still have a stressful taxi ride (breast reconstruction) home. Remember, those who are diagnosed with breast cancer need resources to support and guide them. Nurses who are equipped with knowledge on this type of cancer, types of mastectomies and reconstructive surgeries, and resources can help strengthen the resolve of these patients and motivate them to move forward with a more positive outlook.
References + Disclaimer
- American Cancer Society. Cancer Facts and Figures 2023. Atlanta, Ga: American Cancer Society; 2023.
- Bland, & Klimberg, V. S. (Eds.). (2019). Breast surgery (Second edition.). Wolters Kluwer Health/Lippincott Williams & Wilkins Health.
- Centers for Disease Control and Prevention (CDC). (2023). Breast cancer statistics. Retrieved from https://www.cdc.gov/cancer/breast/statistics/index.htm
- Chagpar, A.B. (2018). Margins and Breast Cancer. In: Howard-McNatt, M. (eds) Changing Paradigms in the Management of Breast Cancer. Springer, Cham. https://doi.org/10.1007/978-3-319-60336-0_5
- Cheng, A., & Losken, A. (2015). Essential elements of the preoperative breast reconstruction evaluation. Gland surgery, 4(2), 93–96. https://doi.org/10.3978/j.issn.2227-684X.2015.03.05
- Howard-McNatt (Ed.). (2018). Changing paradigms in the management of breast cancer. Springer. https://doi.org/10.1007/978-3-319-60336-0
- John Hopkins Medicine (2023). Breast cancer. Retrieved from
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/breast-cancer
- Mayer, H. (2020). Breast reconstruction: modern and promising surgical techniques. Springer. https://doi.org/10.1007/978-3-030-34603-4
- National Institute of Health (NIH): National Cancer Institute. (2017). Breast reconstruction after mastectomy. Retrieved from https://www.cancer.gov/types/breast/reconstruction-fact-sheet
- Fitch M. (2020). Living with body image changes following completion of cancer treatment. Canadian oncology nursing journal = Revue canadienne de nursing oncologique, 30(3), 231–234.
- Williams, L. S., & Hopper, P. D. (2019). Understanding medical-surgical nursing. F.A. Davis Company.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
