Course
Cardiac Unit Guide
Course Highlights
- In this Cardiac Unit Guide course, we will learn about recognizing common cardiac procedures.
- You’ll also learn the basic components of electrocardiograms.
- You’ll leave this course with a broader understanding of nursing interventions for patients in the cardiac unit.
About
Contact Hours Awarded: 3
Course By:
Abbie Schmitt
RN, MSN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
The cardiac unit can be one of the most intimidating areas for nurses to float. The function of the heart muscle and circulatory system can drastically change within moments, which makes nurse advocacy extremely important. However, the unit should not be feared! Poet Ralph Waldo Emerson said it perfectly, “Knowledge is the antidote to fear.” Knowledge of the patient population, common cardiac diagnoses and procedures, equipment, and nursing interventions are extremely important. Additionally, cardiac units will likely have a healthcare team of nurses, cardiologists, and technicians that can support and educate nurses who float to this unit.
Cardiac Unit
The cardiac unit provides care to those who have been diagnosed or at risk for heart or vascular disorders, and there is a perceived need for monitoring. If you are frequently floating to the cardiac unit, it is essential to know how to navigate your organization’s database on the most recent evidence-based practice guidelines and drug information on interactions, dosing, administration, adverse reactions, precautions, and intravenous (IV) compatibility. Ongoing clinical research continues to improve and modify guidelines, and the development of new cardiac drugs means the nurse needs to constantly educate themselves on these advancements.
Heart disease is the leading cause of death for men and women in the United States (3). One in every five deaths is contributed to heart disease and research proclaims that one person dies every 33 seconds in the U.S. from cardiovascular disease (3). Heart disease is not unique to the US. The World Health Organization reports 31% of all deaths in the world are caused by heart disease and 85% of those were results of a heart attack or stroke (10). Some patients in the cardiac unit may appear “fine” but acuity and attention is necessary to make sure their condition does not turn emergent.

Self-Quiz
Ask Yourself...
- Do you have experience with floating to a cardiac unit?
- Are there differences in the prevalence of cardiac conditions among men and women?
Patient Population
The cardiac unit may have a wide variety of patient demographics and conditions, but we will briefly discuss the most common admission diagnoses. Acute coronary syndrome (ACS), dysrhythmias, and heart failure are among the most common admission diagnoses (2). Patients admitted commonly have significant chronic cardiac and noncardiac comorbid conditions. The most common chronic cardiac conditions include ischemic heart disease and heart failure (2). Noncardiac comorbidities included diabetes, chronic kidney disease (CKD), chronic pulmonary, and active malignancy (2).
Demographics may vary, but the majority of patients are most likely older and male. A prominent study on the patient demographics of a cardiac unit found the median age was 65 years, and more than a third of the patients were 70 years (2). Men composed 63% of the population (2). However, men and women are both at great risk for poor outcomes with cardiovascular disease.

Self-Quiz
Ask Yourself...
- What are the most common risk factors associated with the patient population on a cardiac unit?
- How do you think the etiology of cardiac disorders differs among younger and older patients?
- Do you think that socioeconomical factors influence the prevalence and management of cardiac conditions?
- Can you name modifiable and non-modifiable risk factors for cardiac disorders?
Review of Cardiac Anatomy and Physiology
If you are floating to the cardiac unit, it is important to develop and maintain a strong foundational knowledge of cardiac anatomy to strengthen your understanding of cardiac pathophysiology. We will review normal cardiac anatomy and physiology and discuss pathophysiologic changes of diseases and manifestations.
Anatomy of the Cardiovascular System
The cardiovascular system can be compared to a muscular pump with one-way valves that sends blood through a system of large and small plumbing tubes. The brain and nervous system work together to produce cardiac function. The electrophysiology of the heart determines the rate and rhythm, while the blood pressure is maintained by the contractility of the heart muscle (8). The makeup of the heart is similar to parts of a house. Both contain walls, chambers (the rooms), valves (the doors), circulatory vessels (the plumbing), and electrical conduction system (the electricity). Often you will hear medical providers refer to “plumbing” and “electric” problems of the cardiovascular system. A “plumbing” issue may refer to a blocked artery, or an “electric” problem could refer to a heart arrhythmia.
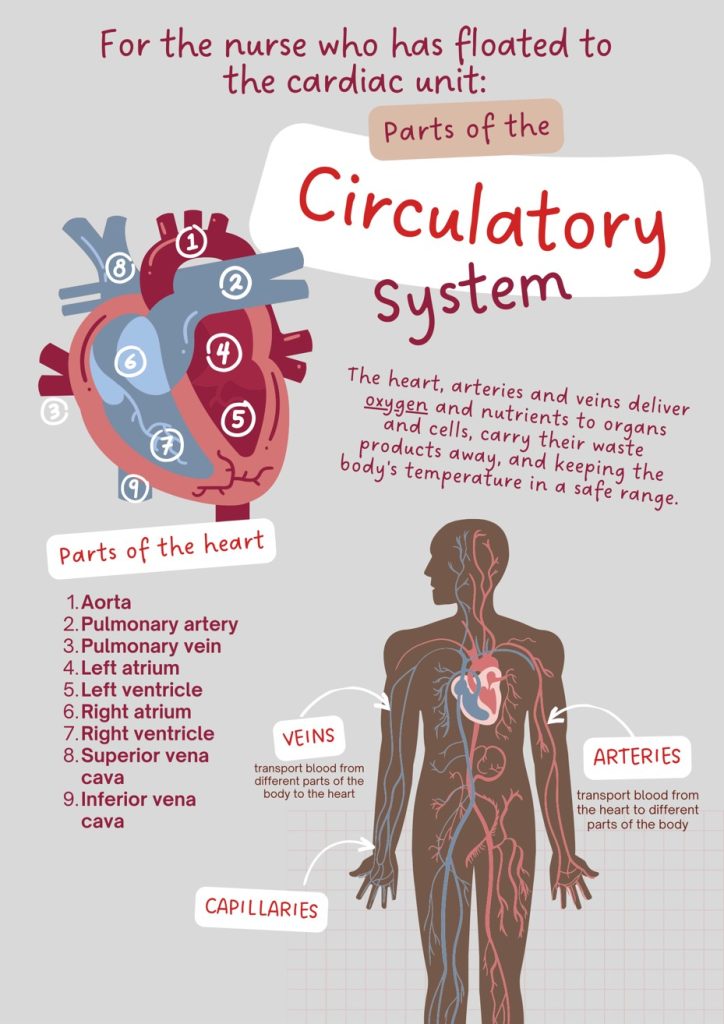
Figure 1. Parts of the Circulatory System
This design was created on Canva.com on November 20, 2023. It is copyrighted by Abbie Schmitt, RN, MSN and may not be reproduced without permission from Nursing CE Central.
The heart is divided into four chambers called the left and right atria and the left and right ventricles. Blood flows through the chambers of the heart in a particular order [See Figure 2 below].
The atrioventricular (AV) valves open between the atria and the ventricles. The two AV valves:
- Tricuspid valve: The valve between the right atrium and right ventricle.
- Mitral valve: The valve between the left atrium and left ventricle.
Semilunar (SL) valves open when blood flows out of the ventricles. The two SL valves:
- Pulmonary valve: The valve that opens when blood flows from the right ventricle into the pulmonary arteries.
- Aortic valve: The valve that opens when blood flows out of the left ventricle to the aorta.
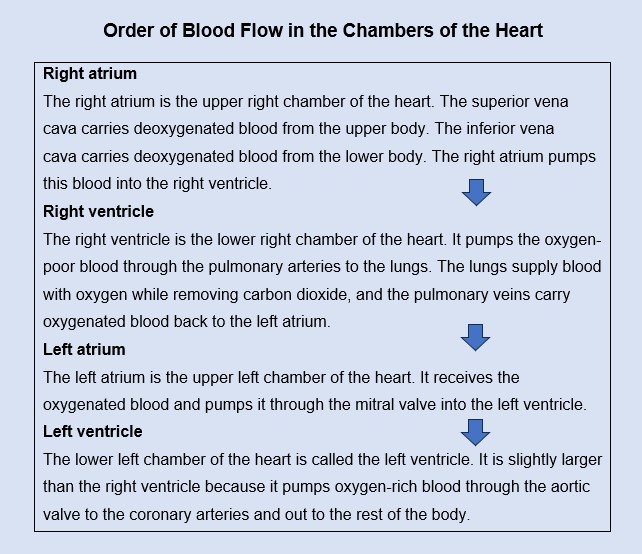
Figure 2. Order of Blood Flow in the Chambers of the Heart

Self-Quiz
Ask Yourself...
- Are you familiar with the structure and function of the heart and vascular system?
- How do the structural differences between arteries and veins relate to their cardiac function?
The Pathway of the Conduction System
The conduction system occurs systematically through:
- SA node. The depolarization wave is initiated by the sinoatrial node.
- Atrial myocardium. The wave then successively passes through the atrial myocardium.
- Atrioventricular node. The depolarization wave travels to the AV node, causing the atria to contract.
- AV bundle. The wave then passes rapidly through the AV bundle.
- Bundle branches and Purkinje fibers. The wave then continues through the right and left bundle branches, and then to the Purkinje fibers in the ventricular walls, resulting in a contraction that ejects blood out of the heart.

Self-Quiz
Ask Yourself...
- Can you describe how blood volume can impact pressure?
- Can you discuss how the circulatory system facilitates the transport and exchange of oxygen and carbon dioxide between the lungs and tissues of the body?
- How do anatomical structures impact blood flow and blood pressure?
- Are you able to describe the pathway of the heart’s conduction system?
Cardiac Procedures
Common cardiac therapies and procedures include placement of pulmonary artery catheter (PAC), central venous catheter (CVC), arterial line, intra-aortic balloon pump (IABP), red blood cell transfusion, and invasive and noninvasive ventilation. Coronary angiography and percutaneous coronary intervention during hospitalization are also common. Common cardiac therapies include initiation and titration of inotrope and vasopressor medication, and administration of antiarrhythmic therapy for ventricular arrhythmias (5).
Diagnostic testing is common for the cardiac patient as many will be under observation to rule out serious conditions. Chest radiography (X-ray) is one of the most common diagnostic tools used in the evaluation of cardiovascular disease (10). Echocardiography is also common. Echocardiography (“Echo”) is ultrasound technology to create imaging of the heart and the associated great vessels. As cardiac catheterization and invasive angiography transformed our understanding of the structure and function of the heart, echo allows this imaging noninvasively (10).
Cardiac Catheterization
Cardiac catheterization describes a group of procedures used to both diagnose and treat heart and blood vessel conditions. During cardiac catheterization, a catheter tube is inserted into a vein or artery, usually from a groin or jugular site, which is then guided into the heart (6). Diagnostic catheters are used to assess blood flow and pressures in the chambers of the heart, heart valves, and coronary arteries (10). Interventional catheters are used in closing ventricular and atrial septal defects via catheter device closure, expansion of narrowed passages (pulmonary stenosis), stent placement, ablation of abnormal electrical pathways, and widening of existing openings (balloon atrial septectomy) (10).
The procedure is done in the evaluation and the treatment of the following conditions:
- Coronary artery disease
- Evaluation and treatment of cardiac arrhythmias
- Evaluation and treatment of valvular heart disease
- Assessment pericardial and myocardial diseases
- Assessment of the congenital heart diseases
- Evaluation of heart failure
Preparation for the cardiac catheterization procedure includes a thorough history of the patient, physical examination, review of drug allergies, and lab work. The basic workup includes a complete blood count (CBC), basic metabolic panel (BMP), prothrombin time, electrocardiogram, and chest X-ray (6). Patients with CKD disease will need adequate planning to reduce the risk of worsening renal function.
Complications to be aware of include bruising or bleeding at the catheter insertion site, blood clot or blood vessel damage, arrhythmias, chest pain (angina), and nausea, itching, or hives from any contrast dye (6). As we mentioned, there are several types of cardiac catheterizations, some to treat and some to diagnose. Coronary angiograms are the most common type of cardiac catheterization procedure (6). During a coronary angiogram, contrast dye is injected to view perfusion and assess for problems.
Nursing Care for Cardiac Catheterization
Pre-procedure:
Before the exam, assess the patient for any allergies to iodine or shellfish. Remember to assess kidney function (blood urea nitrogen [BUN] and creatinine) because those with impaired kidney function may not be able to process and excrete the contrast dye well. Assess and mark your patient’s distal pulses (dorsal pedis and posterior tibial) to compare with post-procedure.
Post-procedure:
After a coronary angiogram, the following are important assessments:
- Assess the insertion site for bleeding.
- Assess the patient’s extremity, distal to the puncture site, for pulse, capillary refill, temperature, and color.
- Take vital signs every 15 minutes x4, then every hour x4 (or per facility protocol).
- The patient will need to lie flat for 4 – 6 hours after the procedure, unless contraindicated.
Cardiac Stress Testing
Cardiac stress tests are used to evaluate the function and perfusion of the heart and vessels during physical activity or when the rate is significantly elevated. It also may be called a stress exercise test or a pharmacological stress test. During the exercise stress test, the patient will be put on a treadmill or stationary bike; those who are unable to do this physical activity are given medications to create the effects of exercise and increase the heart rate. It is beneficial to use pharmacologic stress techniques for who have orthopedic limitations, peripheral vascular disease, chronic obstructive pulmonary disease (COPD), elderly patients, diabetic patients with severe neuropathy, and patients with neuromuscular conditions (10).
If your patient is scheduled for cardiac stress testing, it is important to understand why. There are many indications, including but not limited to:
- Assessment of patients with chest pain or other symptoms suspicious for coronary artery disease (CAD) or myocardial ischemia
- Examination for the presence and severity of arrhythmias
- Evaluation of the efficacy of medical, surgical, or pharmacologic treatment
- Evaluation of valvular dysfunction
- Evaluation of potential causes of syncopal episodes
- Measurement of exercise capacity in children, adolescents, or adults with congenital heart disease
- Evaluation of perioperative risk for noncardiac surgery
Ultimately, it is the role of the provider to assess the risks and benefits of cardiac stress testing for each individual patient, but the nurse serves as an advocate if any major contraindications are noted prior to the procedure.
Nursing Care for Cardiac Stress Testing
Pre-procedure:
Before the stress test, the patient will likely be instructed to fast and to restrict fluids (especially those containing caffeine) and abstain from the use of tobacco products for 4 to 6 hours prior to the procedure. The provider who ordered the testing may hold their medications for a specific time period prior to the test, so it is important for the nurse to closely assess accordingly, for example, blood pressure and pulse if antihypertensive was held. Protocols may vary among facilities. The nurse should explain to the patient to wear comfortable shoes and clothing for the exercise stress test.
Post-procedure:
After a coronary angiogram, the following are important assessments:
- Assess for pain, dizziness, changes in level of consciousness
- Take vital signs every 15 minutes x4, then every hour x4 (or per facility protocol)
- The patient will more than likely need to rest and rehydrate.

Self-Quiz
Ask Yourself...
- What specific conditions do you think would benefit from cardiac catheterizations?
- What are some nursing interventions for a patient who has just undergone a coronary angiogram?
- Are there any long-term effects from complications of these cardiac procedures?
- Why is patient education and informed consent for cardiac procedures a crucial component of care?
Heart Conditions that Require Inpatient Treatment
We will review common cardiac conditions that require inpatient treatment, but it is also important to remember that these patients will likely have comorbidities. Each patient on the cardiac unit is unique, so tunnel vision on the cardiac disorder must be avoided. The entire picture of their wellbeing is important to the care plan. Research has found that CKD, diabetes mellitus, COPD, and various types of cancers also impact those on the cardiac unit (5). It is important to constantly teach and update the patient on their condition, diagnostic results, and treatment plan.
Acute Coronary Syndrome (ACS)
Acute coronary syndrome (ACS) is not a specific condition, but a group of conditions.
ACS includes:
- ST-elevation myocardial infarction (STEMI)
- Non-ST elevation myocardial infarction (NSTEMI)
- Unstable angina
ACS is essentially a plumbing issue. The underlying pathophysiology in ACS is decreased blood flow to or from the heart, which is typically caused by plaque rupture and formation of a thrombus. (12). This results first in ischemia and then infarction of that part of the heart. ACS is a type of coronary heart disease (CHD) and is responsible for one-third of deaths among people older than 35. Those with ACS are always symptomatic.
If you are assigned a patient with an ACS diagnosis, you can anticipate treatments to possibly include IV heparin infusion, antiplatelets, supportive measures like pain control with morphine/ fentanyl, oxygen therapy in case of hypoxia, and nitroglycerin sublingual or infusion. Abundant precautions should be used for cases of inferior wall ischemia, nitroglycerine can cause severe hypotension (12). Continuous cardiac monitoring for arrhythmia is recommended. The American Heart Association (AHA) recommends an emergent catheterization and percutaneous intervention (PCI) for patients with STEMI in fewer than 90 minutes from arrival to procedure (12). Cardiac medications like beta-blockers, statins (cholesterol-lower medications), and ACE inhibitors are most likely initiated in ACS cases unless contraindications exist.
Dysrhythmias
Occasional occurrences of dysrhythmias are generally transitory and not life-threatening. However, if the deviation from the normal pattern of impulse conduction and contraction is prolonged, it is referred to as dysrhythmia or arrhythmia. Severe arrhythmias can lead to cardiac arrest, which is fatal if not treated rapidly. The American College of Cardiology (ACC), AHA, and Heart Rhythm Society (HRS) have published guidelines for various cardiac arrhythmias, including atrial fibrillation, bradycardia and cardiac conduction delays, supraventricular tachycardia, and ventricular tachycardia. The following are types of dysrhythmias.
Sinus Dysrhythmias
Sinus dysrhythmias include sinus tachycardia, sinus bradycardia, and sinus arrhythmia.
- Sinus Tachycardia
Sinus tachycardia is a heart rate greater than 100 beats per minute (BPM), but the cardiac rhythm is regular. Causes of sinus tachycardia can include physical activity, anxiety, fever, pain, anemia, medications, or as compensation for decreased cardiac output or blood pressure (10). The recommended treatment for sinus tachycardia is to treat the underlying cause. For example, if a fever is believed to be the cause the sinus tachycardia, treat the fever.
- Sinus Bradycardia
Sinus bradycardia is a heart rate of less than 60 BPM, with regular cardiac rhythm. Causes of sinus bradycardia can be excess vagal nerve stimulation, cardiovascular disease, cardiovascular infection, hypoxia, or certain medications (10). The treatment for sinus bradycardia as an abnormal finding is atropine or evaluation for a pacemaker.
Atrial Dysrhythmias
Atrial dysrhythmias include atrial fibrillation, atrial flutter, premature atrial complexes, and supraventricular tachycardia.
- Atrial Fibrillation (AFIB)
Atrial fibrillation (AFIB) is rapid and disorganized depolarization of the atria in the heart which causes the atria to quiver or “fibrillate” instead of fully contracting. Patients with AFIB are at a HIGH risk for blood clots due to the static blood collection in the atria. Treatment for atrial fibrillation includes anticoagulants, antiarrhythmics, and cardioversion (treatment that uses shock or medication to restore the regular heart rhythm).
- Atrial Flutter
Atrial flutter occurs when an abnormal electrical impulse forms in the atria of the heart, causing it to depolarize 250 – 350 times per minute (10). The treatment for atrial flutter is cardioversion and/or antiarrhythmics.
- Premature Atrial Complexes (PAC)
Premature atrial complexes (PACs) are premature electrical signal impulses in the atria of the heart. Treatment of PACs is not usually necessary. Studies show that decreasing stress and avoiding alcohol and caffeine can reduce PACs (10).
- Supraventricular Tachycardia (SVT)
SVT is a rapid heart rate that originates above (supra = above) the ventricles, typically in the atria. The treatment for SVT is often cardioversion and antiarrhythmics.
Ventricular Dysrhythmias
Ventricular dysrhythmias include premature ventricular complexes, ventricular tachycardia, ventricular fibrillation, and asystole (8).
- Premature Ventricular Complexes (PVCs)
A premature ventricular complex (PVC) is an abnormal and early impulse that originates from the ventricle. The treatment for symptomatic PVCs includes antiarrhythmics but is not always necessary.
- Ventricular Tachycardia (VT/V-tach)
Ventricular tachycardia is a rapid heart rhythm greater than 100 BPM. VT is usually due to ischemic heart disease and can often deteriorate into ventricular fibrillation. The treatment for ventricular tachycardia (when the patient has a pulse) is cardioversion, antiarrhythmics, and correcting electrolyte imbalances. The treatment for ventricular tachycardia (when the patient does not have a pulse) is defibrillation.
- Ventricular Fibrillation (VF/V-fib)
Ventricular fibrillation is quivering of the ventricles in the heart, in which there is ineffective or absent contraction. Ventricular fibrillation is an emergency. The treatment for V-fib is defibrillation.
- Asystole
Asystole is the absence of any ventricular rhythm. The EKG of asystole shows a flat line. The treatment for a patient in asystole is immediate cardiopulmonary resuscitation (CPR).
Atrioventricular Blocks (AV Blocks)
There are several types of AV blocks. These include first-degree, second-degree, and third degree (8). Risk factors for AV blocks include coronary heart disease, myocardial infarction, and certain medication use (digoxin or beta blockers).
- First-degree: prolonged impulse conduction time from the atria to the ventricles occurs due to a delay in the AV node impulse.
- Second-degree type 1: progressive increase in impulse conduction time between the atria and ventricles until one impulse finally fails to conduct.
- Second-degree type 2: sudden failure of impulse conduction from the atria to the ventricles, without a progressive increase in conduction time. Second-degree type 2 AV block usually requires a pacemaker (8).
- Third-degree: complete failure of all impulse conduction from the atria to the ventricles. A third-degree AV block requires a pacemaker for the patient.
Heart failure (HF) or Congestive Heart Failure (CHF)
Some patients on the cardiac unit may have a diagnosis or suspicion of heart failure. This condition happens when there is structural or functional impairment of ventricular filling or ejection of blood, and the heart cannot pump enough blood to meet the metabolic needs. Essentially, heart failure is poor systolic or diastolic function of the left ventricle.
HF or CHF is caused by different conditions such as chronic hypertension or coronary artery disease (8). The term refers to a clinical syndrome characterized by manifestations of volume overload and inadequate tissue perfusion, followed by pulmonary and systemic venous congestion. The signs and symptoms of heart failure are defined based on which ventricle is affected. The following are common signs and symptoms.
Left-Sided Heart Failure
- Dyspnea on exertion
- Fatigue
- Crackles in the lungs
- Weak, thready pulse
- Tachycardia
- Frothy sputum
- Signs of inadequate tissue perfusion
- Oliguria (low urine output), nocturia
Right-Sided Heart Failure
- Edema of the lower extremities
- Weight gain (from fluid retention)
- Enlargement of the liver (hepatomegaly)
- Ascites (fluid accumulation in the peritoneal space of the abdomen)
- Weakness

Self-Quiz
Ask Yourself...
- Can you name a condition within the group of Acute Coronary Syndrome (ACS)?
- Have you ever cared for a patient with an arrhythmia?
- Can you think of specific challenges that nurses may face when caring for a patient with angina? (ex: patient fear, anxiety, uncertainty)
- How could a multidisciplinary care approach benefit patients with a life-threatening dysthymia?
Cardiac Equipment
Some equipment you may see on the cardiac unit includes electrocardiograms and portable remote telemetry monitors.
Bedside Monitor- Electrocardiograms (ECGs)
As you know, a major component of the cardiac unit is the use of electrocardiograms (ECGs). ECGs use leads with electrodes placed on an individual’s body to record the electrical activity of the heart on special graph paper or on a cardiac monitor. The electrodes detect the small electrical changes of cardiac muscle depolarization followed by repolarization during each cardiac cycle (8). When interpreting a paper ECG, the vertical lines indicate voltage of a given waveform and the horizontal axis represent amounts of time as the electrical signal is conducted through the heart tissue. We will go into greater detail later in the course.
A 12-lead electrocardiogram is a diagnostic test that uses 12 leads to record information through 12 different perspectives of the heart to display a complete picture of its electrical activity. Electrodes are placed on the surface of the patient’s chest (i.e., leads V1, V2, V3, V4, V5, and V6), and four are placed bilaterally on their upper and lower extremities (i.e., RA, LA, RL, LL). Accurate placement of leads to obtain a 12-lead ECG is critical. When performed and interpreted accurately, an ECG can detect several types of heart conditions such as dysrhythmias, myocardial infarction, and those related to electrolyte imbalances (10).
Sample Checklist: If you have an order to obtain a 12-lead ECG
- Verify the provider’s order.
- Gather data related to age, gender, cardiac medications, signs and symptoms, recent pulse and blood pressure, and pain level.
- Introduce self and your role.
- Explain the procedure to the patient.
- Perform hand hygiene and put on gloves.
- Verify the patient with two identifiers and check allergies.
- Provide privacy.
- Enter demographic data as required into the equipment.
- Place patient in supine or Semi-Fowler’s position. If both positions are not feasible for the patient, you can perform the ECG with the patient in a more elevated position.
- Remove oil, moisture, and/or excess hair at lead placement points.
- Open the electrode package. Check the expiration date to ensure electrodes are not expired.
- Attach four electrodes to the extremities as indicated on the electrodes.
- Attach the six chest leads in the locations described below:
- V1 – Fourth intercostal space on the right sternal border
- V2 – Fourth intercostal space at the left sternal border
- V3 – Midway between placement of V2 and V4
- V4 – Fifth intercostal space at the midclavicular line
- V5 – Left anterior axillary line on the same horizontal level as V4
- V6 – Mid-axillary line on the same horizontal level as V4 and V5
- Press the auto button and record the ECG. Ask the patient to hold still while the machine is capturing the electrical activity of the heart to ensure a clear and accurate depiction of the heart’s electrical pattern.
- Inspect the tracing printout for quality. The ECG machine will provide an interpretation of the electrical activity, but a healthcare provider will evaluate the findings.
- If the patient has an abnormal cardiac pattern, assess their level of consciousness, carotid pulse, and for complaints of chest pain or shortness of breath. Request emergency assistance if indicated.
- Remove the electrodes and clean the skin. Assess the area for redness and irritation.
- Remove gloves and perform hand hygiene.
- Provide comfort and safety for the patient.
- Notify the health care provider of abnormalities.
In a 12-lead ECG, each lead records the electrical activity of the heart from a different angle and different anatomical areas of the heart:
- Inferior leads (II, III, and aVF): Inferior surface of the heart
- Lateral leads (I, aVL, V5, and V6): Lateral wall of the left ventricle
- Septal leads (V1 and V2): Septal surface of the heart
- Anterior leads (V3 and V4): Anterior wall of the right and left ventricles
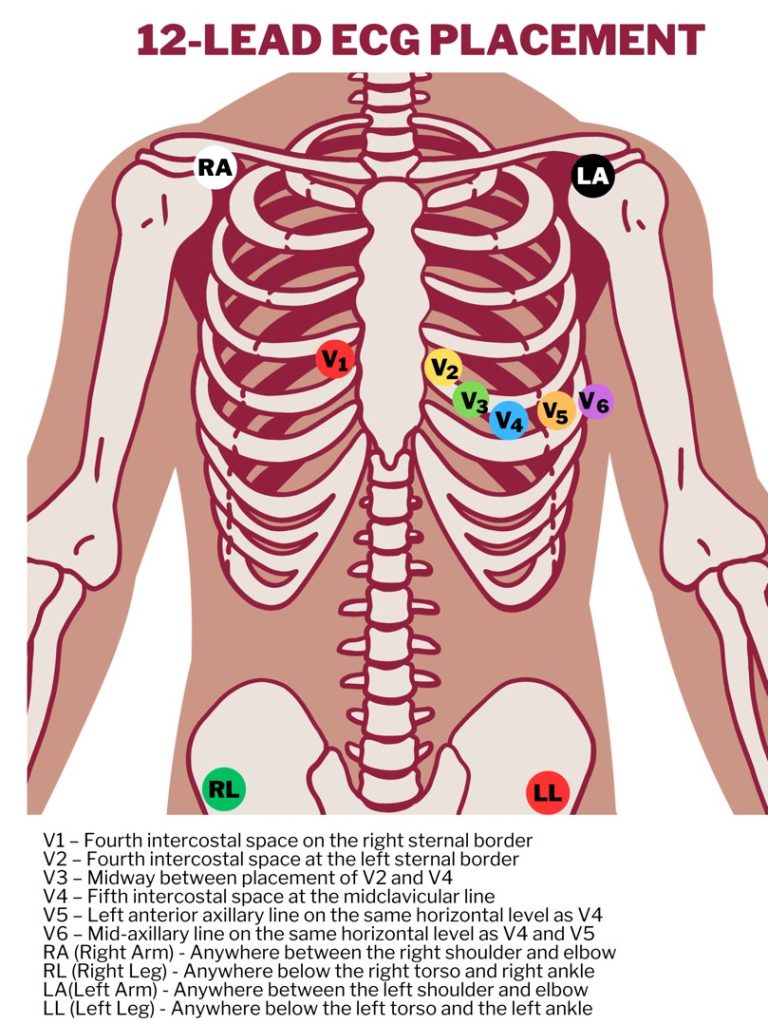
Figure 3. 12-Lead ECG Placement

Self-Quiz
Ask Yourself...
- What are the primary goals for bedside ECGs?
- Have you ever performed a 12-lead ECG on a patient?
Remote Telemetry Monitoring
Telemetry refers to a portable device used to continuously monitor an individual’s heart rhythms. The patterns are continuously monitored by technicians and nurses with specialized training to interpret the heart’s electrical activity and assess any abnormalities. Remote cardiac monitoring uses telemetry to monitor a patient’s cardiac activity from a distance. This type of monitoring is particularly useful for patients with known heart conditions, those recovering from cardiac surgery, or individuals at high risk for cardiac events (7).
Remote telemetry usually involves devices like Holter monitors, event recorders, or implantable devices like loop recorders or cardiac pacemakers (7). These devices record electrical activity of the heart, similar to that of an electrocardiogram (ECG), but over extended periods. This is crucial for detecting conditions like arrhythmias, which might not occur during a standard ECG in a healthcare setting.
Monitors can be continuous or event-triggered recordings, designed to record only when triggered by an abnormal heart rhythm or when the patient activates the device during symptoms like palpitations, dizziness, or chest pain. The recorded data is transmitted wirelessly to a healthcare provider or a monitoring center, which allows for real-time or periodic analysis of the data by medical professionals.
Limitations of remote telemetry monitoring include:
- Dependence on technology, as it requires connectivity
- The high quantity of data may be overwhelming to the provider
- Privacy issues

Self-Quiz
Ask Yourself...
- How can nurses manage frequent alarms on bedside ECGs to ensure patient safety while minimizing alarm fatigue?
- What are some examples of conditions that would benefit from continuous ECG monitoring?
- Why is it important to prep the skin (shave or remove lotions) prior to applying the leads?
- Are you familiar with any organizations that offer remote telemetry monitoring?
Abnormal EKG Readings
The steps to reviewing abnormal EKG readings includes interpreting the ECG strip, assessing the EKG waveform, analyzing the rhythm, and clinically observing the patient.
Review of ECG Interpretation
ECG graphing paper is used to record waveforms produced by the heart’s electrical current.
The horizontal axis of the ECG strip represents time (4).
- Each small square represents 0.04 seconds of time
- Each large square has 5 small squares, representing a total of 0.20 seconds
- To measure heart rate: use a 6-second strip, which consists of 30 large blocks.
The vertical axis of the ECG measures amplitude in millimeters (mm) or electrical voltage in millivolts (mV) (4).
- Each small block represents 1 mm or 0.1 mV.
- Each large block represents 5 mm or 0.5 mV.
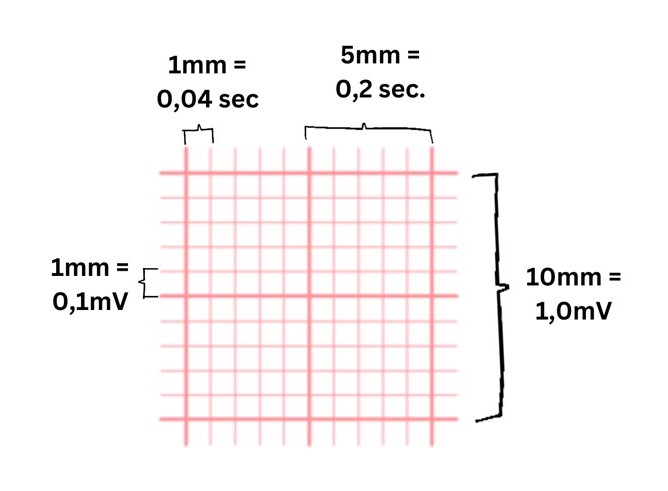
Image 1. ECG Graphing Paper Interpretation
The ECG Waveform
| Waveform | Representation | Duration | Amplitude | Shape |
| P wave | Atrial depolarization (leads to atrial contraction), which is created by the SA node. | Less than 0.12 seconds | Less than 2.5 mm | Upward, rounded, and similar appearance |
| PR interval | Starts at the beginning of the P wave and extends to the beginning of the QRS complex.
Demonstrates the amount of time it takes for the electrical signal to travel from the atria to the AV node. |
0.12-0.20 seconds | ||
| QRS complex | Ventricle depolarization begins, which leads to the contraction of the ventricles. | 0.06-0.12 seconds | 1.0-3.0 mm | Q: Downward deflection
R: Upward spike; shows electrical stimulus passing through ventricles. S: Downward deflection; shows final depolarization of Purkinje fibers |
| QT interval | Demonstrates the time it takes for electrical signals to cause the ventricles to contract and then rest.
This is a part that is measured on the ECG.
|
0.36-0.44 seconds | ||
| T wave | Ventricular repolarization.
When the ventricles relax, it creates the T wave. |
Less than 10 mm | Upward, rounded, and similar in appearance; should have a higher amplitude than P wave | |
| ST segment | Period when the ventricles are in between depolarization and repolarization. | 0.005 – 0.150 seconds | Less than 1 mm | Flat, isoelectric section of the ECG between the end of the S wave (often referred to as the J point) and the beginning of the T wave |
Table 1. Explanation of EKG Waveform (8)
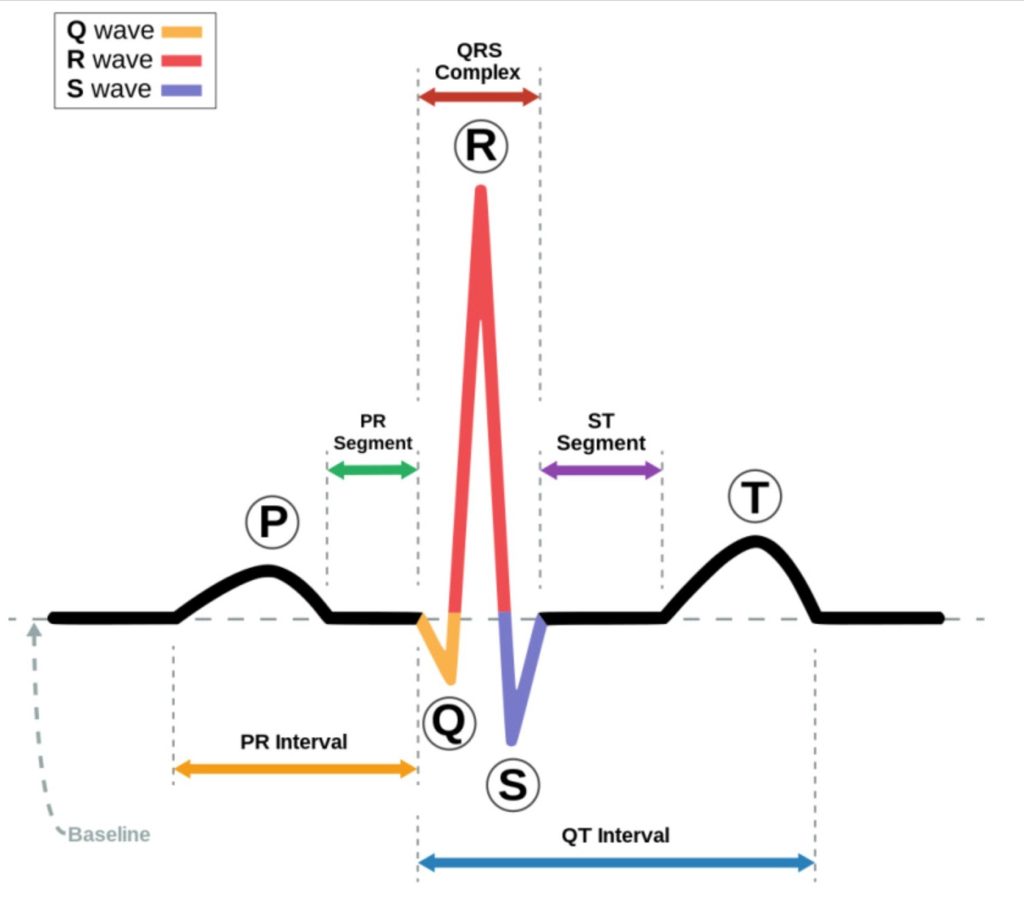
Image 2. EKG Waveform (8)
Basics for Analyzing a Rhythm
- Calculate the Rate (ventricular and atrial rates)
-
- Sample method: Count the number of R waves in a 6-second strip (i.e., over 30 large boxes) and multiply this number by 10.
-
- Make sure the rhythm strip that is used is a 6-second strip.
- Determine the Regularity of the Rhythm
-
- Assess the distances between the R waves to determine the regularity of the rhythm using a caliper or ruler [See Image 3 below]
-
- It would be helpful to have your own tools to quickly assess the regularity
-
- It is important to assess the distances across the whole strip to account for any potential abnormality.

Image 3. EKG Measuring Tool: Caliper and Ruler

Self-Quiz
Ask Yourself...
- What do you think are the most obvious abnormal rhythms on the ECG?
- What skills are essential for accurately interpreting an ECG reading?
- Why is it important to consider both the ECG rhythm and the signs and symptoms of the patient?
- How does the information gathered from ECG differ from other diagnostic tools such as echocardiograms?
Cardiac Assessment
A comprehensive cardiac assessment is essential on this unit. A focused cardiovascular assessment begins with taking a thorough health history. After getting a better understanding of the health history and current condition, along with diagnostic test results, you should begin the physical assessment. The order of examination is inspection, auscultation, then palpation.
It is important to auscultate the carotid pulse prior to any palpation. Blood pressure and heart rate should be taken as part of the cardiac assessment. Optimal patient positioning initially may be the supine position with the head of the bed elevated approximately 30 degrees, and if necessary, place the patient on the left side or sitting straight up and leaning forward. Grouping the cardiac assessment by body region minimizes position changes and helps to keep you organized.
Neck
Assessment of the neck:
- Inspection
- Observe pulsations of the carotid arteries.
- Assess the jugular veins for distention.
- Estimate the jugular venous pressure (JVP):
- Turn the patient’s head slightly away from the side you are inspecting
- Inspect both sides of the neck.
- Identify the external jugular veins and find the internal jugular vein pulsations.
- Locate the highest point of pulsation in the right jugular vein; use a card horizontally from this point and a centimeter ruler vertically from the sternal angle, to make an exact right angle.
- Measure the vertical distance in centimeters above the sternal angle where the horizontal object crosses the ruler and add to this distance 5 cm (the distance from the sternal angle to the center of the right atrium).
- Add the numbers together to get the JVP.
- JVP gives an estimation of central venous pressure, or right atrial pressure, and gives valuable information on volume status.
- Auscultation
- Auscultate the carotid arteries.
- Listen for carotid bruits bilaterally.
- Palpation
- Use your index and middle fingers to palpate the carotid arteries one at a time; note the amplitude of the pulse and the contour of the pulse wave.
- Note the presence of vibrations or thrills.
Chest
Assessment of the chest: (1)
- Inspection
- Examine the chest for visible point of maximum impulse (PMI) or heaves.
- The point of maximum impulse is usually located at the fifth intercostal space near the left midclavicular line.
- Examine the chest for visible point of maximum impulse (PMI) or heaves.
- Auscultation
- Listen to the anterior chest from base to apex, at the six points for cardiac auscultation:
- Second intercostal space (ICS), near the right sternal border (aortic area)
- Second ICS, along the left sternal border (pulmonic area)
- Third ICS, along the left sternal border
- Fourth ICS, along the left sternal border (tricuspid area)
- Fifth ICS, along the left sternal border (tricuspid area)
- Near the midclavicular line at the fifth ICS (mitral area)
- Listen to the anterior chest from base to apex, at the six points for cardiac auscultation:
- Identify the S1 and S2 heart sounds
- Note the clarity of heart tones (muffling) and listen for rubs, S3 or S4 gallops, or splitting of S2.
- Auscultate for murmurs, noting location, grade, timing, and character.
- Apical pulse assessment and location:
- As a nurse you will assess the apical pulse during a head-to-toe assessment and before administering medications like digoxin.
- Locate apical pulse: left side of the chest at the 5th intercostal space (ICS) at the midclavicular line.
- Listen to the apical pulse and count the beats for 1 full minute.
- Note rate and rhythm
- Palpation
- Palpate precordium (area over the heart) for PMI, heaves, or thrills.
Extremities
Assessment of the extremities: (1)
- Inspect for cyanosis, pallor, coolness of extremities, edema, or diaphoresis.
- Palpate peripheral pulses
Important Cardiac Assessment Notes
Tips to remember when performing a cardiac assessment: (1)
- Never palpate both carotid arteries simultaneously, as this could seriously impede blood flow to the brain.
- Use both the bell and the diaphragm of the stethoscope for auscultation.
-
- The bell is best used to identify lower pitched sounds (S3 and S4) and murmurs associated with mitral stenosis.
-
- The diaphragm is more sensitive to higher pitched sounds (S1 and S2), friction rubs, and murmurs associated with aortic and mitral regurgitation.
- Carotid stenosis or atherosclerosis may present with a bruit, so use caution if palpating the carotids in the presence of a bruit.
- Palpation of the carotid arteries may cause a vagal response.

Self-Quiz
Ask Yourself...
- What are key components of a comprehensive focused cardiac assessment?
- Are you familiar with assessing various pulse sites?
- How can a patient’s medical history and current diagnosis guide your nursing assessment?
- How does identifying risk factors impact your nursing assessment?
Pertinent Laboratory Tests
While floating to the cardiac unit, it is important to review policies and procedures for management of chest pain and other cardiac symptoms. You will more than likely be expected to recognize manifestations related to certain abnormal cardiac labs.
Troponins
Troponins are protein complexes found in both cardiac and skeletal muscle. Troponin is the gold-standard biomarker for risk stratification and diagnosis of acute MI because of the high specificity and sensitivity for detecting myocardial injury (11). This lab test is meaningful in the early diagnosis of MI because it is either low or undetectable in healthy people, but is detectable as early as 2 to 3 hours in the event of an MI.
It is recommended that troponins are drawn at time of presentation, followed by repeat sampling 3 to 6 hours later, with a rise or fall of troponin with at least one value exceeding the 99th percentile. A troponin level greater than the 99th percentile of normal reference population is indicative of myocardial necrosis (10). However, coronary ischemia is not the only cause of an elevated troponin level. Other conditions that may release troponin include tachycardia, pericarditis, heart failure, sepsis, and strenuous exercise (11).
Cardiac Enzymes
Enzymes are protein substances that catalyze chemical reactions in cells, and substrates in the cells bind to the enzymes and form products. The following are two cardiac enzymes.
- Creatine Kinase (CK)
CK is an enzyme specific to cells of the brain, myocardium, and skeletal muscle; in these organ systems, the function of CK is primarily that of energy production (10). The appearance of CK in the blood indicates cardiac, cerebral, or skeletal muscle necrosis or injury. Certain demographics impact CK levels. Serum CK declines with age and older adults have very low values, CK values measured in women are lower than those of men.
Medication also impacts CK level. Medications that can increase CK include anticoagulants, aspirin, furosemide, captopril, lidocaine, propranolol, and morphine (10). The three CK isoenzymes are named for their primary sites of isolation—the muscle (M) and brain (B). Elevated CK-MB levels have also been reported after myocardial damage from unstable angina, cardiac surgery, coronary angioplasty, after defibrillation, in vigorous exercise, and after intramuscular (IM) injections, trauma, and surgery (10).
- Myoglobin
Myoglobin is a low–molecular-weight, oxygen-binding protein found in the myocardium and skeletal muscle. Myoglobin is released into the circulation after damage to the heart or skeletal muscles. After a MI, myoglobin levels increase in 2 to 3 hours, peak in 6 to 9 hours, and return to normal (undetectable) as early as 12 hours (10). Therefore, troponin is the preferred biomarker for diagnosing MI. Elevated myoglobin levels are seen after MI, reinfarction, skeletal muscle injury, trauma, severe burns, electrical shock, polymyositis, alcoholic myopathy, delirium tremens, metabolic disorders, malignant hyperthermia, systemic lupus erythematosus, muscular dystrophy, rhabdomyolysis, and seizures. (10).
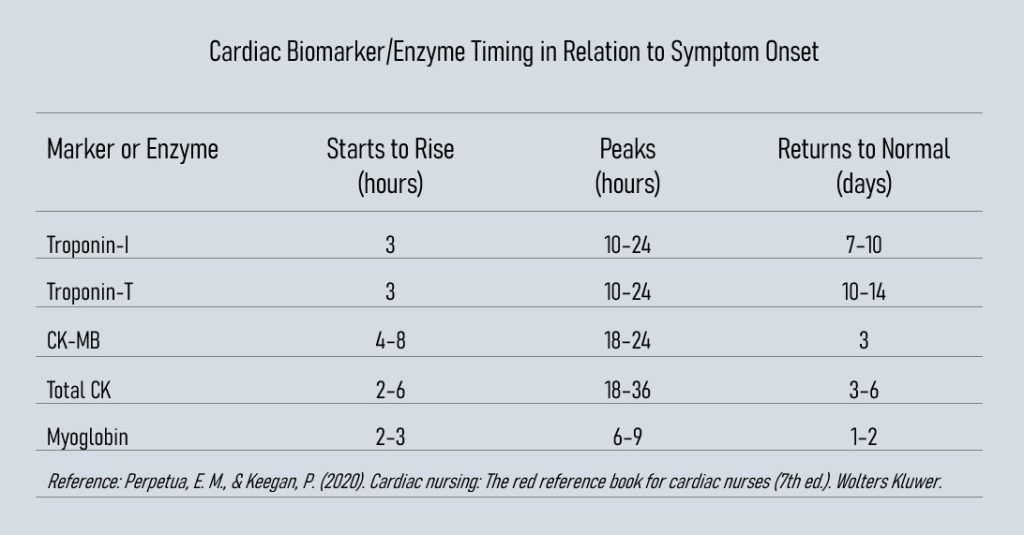
Figure 4. Timing of appearance and disappearance of commonly used cardiac biomarkers and enzymes in relation to onset of cardiac symptoms (10)

Self-Quiz
Ask Yourself...
- Can you name common laboratory tests within a cardiac unit?
- Why would it be important to auscultate the apical pulse for a full minute?
- What are some common reasons, other than cardiac conditions, that CK enzymes may be elevated?
- Can you discuss why troponins are a more commonly used biomarker when assessing for cardiac ischemia?
Nursing Interventions
- Interventions for Decreased Cardiac Output
-
- Inspects the skin for pallor or cyanosis.
-
- Strict monitor of intake and output; note decreasing output and concentrated urine.
-
- Weigh the patient daily and compare the value to the previous measurement.
-
- Note changes in level of consciousness.
-
- Assess for lethargy, confusion, disorientation, anxiety, and depression.
-
- Monitor results of laboratory and diagnostic tests.
-
- Monitor oxygen saturation and arterial blood gases (ABGs).
-
- Administer oxygen as ordered within parameters for patient’s symptoms, oxygen saturation, and ABGs.
-
- Monitor for signs and symptoms of fluid and electrolyte imbalances.
-
- Withhold digitalis (digoxin) as indicated and notify the physician if marked changes occur in cardiac rate or rhythm or signs of digitalis toxicity occur.
-
- Position the patient for optimal breathing.
- Nursing Intervention for Ineffective Tissue Perfusion
-
- Obtain IV access.
-
- Administer oxygen and other medications.
-
- Obtain 12 lead-EKG as ordered.
-
- Assess for dysrhythmias (irregular apical pulse, syncope, palpitations).
-
- Communicate rationale for monitoring and treatments to patient.
-
- Position patient to minimize discomfort and facilitate respiration.
-
- Minimize anxiety with a calm environment, reassurance, and education.
-
- Monitor vital signs.
-
- Anticipate the need to initiate CPR.
-
- Assess for contributing factors: pain, fluid and electrolyte imbalance, drug toxicity (especially digoxin), and medication non-adherence.
-
- Provide psychosocial support for the patient and family members.
-
- Educate and prepare the patient on diagnostic studies, medications, signs and symptoms to report, and planned treatments such as echocardiograms, cardioversion, and pacemaker insertion.

Self-Quiz
Ask Yourself...
- Why do you think intake and output documentation is vital on the cardiac unit?
- How can patient positioning impact cardiac perfusion?
- What are the nursing precautions when administering digoxin?
- Can you describe examples of how abnormal fluid and electrolyte levels impact cardiac rate and rhythm?
Nursing Certifications
There are over 10 nursing certifications that can be obtained for work on the cardiac unit. These include advanced cardiac life support, critical care registered nurse, certified heart failure nurse, progressive critical care nurse, and cardiac-vascular nurse, among others.
Advanced Cardiovascular Life Support (ACLS)
If you are frequently floated to a cardiac unit or are a traveling nurse assigned to this unit, becoming certified in Advanced Cardiovascular Life Support (ACLS) is critical. If you do not have this certification or it is expired, it would be helpful to reach out to your facility’s education department or your nursing manager to schedule or facilitate taking the course.
The ACLS course builds on basic life support (BLS) skills, including effective chest compressions, use of a bag-mask device, and use of an AED. The course expands significantly on reading and interpreting ECGs, understanding pharmacology during cardiac or respiratory arrest, high-performance team communication, and highlights acute dysrhythmia, stroke, and acute coronary syndromes (ACS). The AHA is the leading provider of this certification. Most organizations require the ACLS course and certification card from the AHA.
Cardiac Nursing Certifications
The following table provides professional organizations, publications, and cardiac nursing certifications.
| Organization | Publications | Cardiac Nursing Certifications |
| American Association of Critical Care Nurses (AACN) | American Journal of Critical Care
Critical Care Nurse |
Critical Care Registered Nurse—Cardiac Surgery Certified (CCRN-CSC) Critical Care Registered Nurse—Cardiac Medicine Certified (CCRN-CMC) Progressive Critical Care Nurse (PCCN) |
| American Association of Heart Failure Nurses (AAHFN) | Heart and Lung: Journal of Acute and Critical Care | Certified Heart Failure Nurse (CHFN) Certified Heart Failure Nurse, Knowledge (CHFN-K [nonclinical]) |
| American Nurses Association | American Journal of Nursing | Cardiac-Vascular Nurse Certification, Board Certified (RN-BC) |
| Preventative Cardiovascular Nursing Association (PCNA) | Journal of Cardiovascular Nursing | Registered Nurse, Board Certified (RN-BC) |
| American Association of Critical Care Nurses (AACN) | American Journal of Critical Care Critical Care Nurse |
Critical Care Registered Nurse—Cardiac Surgery Certified (CCRN-CSC) Critical Care Registered Nurse—Cardiac Medicine Certified (CCRN-CMC) Progressive Critical Care Nurse (PCCN) |
| American Association of Heart Failure Nurses (AAHFN) | Heart and Lung: Journal of Acute and Critical Care | Certified Heart Failure Nurse (CHFN) Certified Heart Failure Nurse, Knowledge (CHFN-K [nonclinical]) |
Table 2. Cardiac Nursing Certifications (10)

Self-Quiz
Ask Yourself...
- Are you familiar with the nursing organizations that provide certifications?
- Why is it important to closely follow publications and educational institutions for updated guidelines?
- Can you name various certifications unique to cardiology?
- Can you name certifications available in your current area of practice?
Cardiac Nursing as a Career
If you feel passionate about cardiac nursing, this is certainly a career path. Not only are inpatient, outpatient, and home health settings a possibility, but there are many opportunities for expanded roles for the cardiac nurse. For example, cardiac nurses can have an impact in healthcare policy, diseases management model development for cardiovascular care, global health population policies, quality improvement, and advanced practice cardiovascular care.
Evidence-Based Practice
A critical aspect of cardiac nursing is the ongoing learning and management of evidence-based practice (EBP) guidelines specific to cardiology. EBP is defined as applying the highest-quality evidence in research, practice, education, and regulations to clinical expertise, patient care, and policy (10). Cardiac nurses across many subspecialties and settings must access, appraise, and implement EBP to improve patient care and outcomes. To accomplish this, cardiac nurses should closely follow or serve with EBP producers to review the evidence from practice (e.g., data from the electronic health record, quality assessments, staff/workflow observation,) and research (e.g., published guidelines and clinical research studies).
Models of Disease Management in Cardiovascular Care Developed by Nurses
Guidelines for cardiovascular care are constantly evolving and improving, this is partly due to the support of the nursing field. Unique models designed by nurses for delivering care to individuals with chronic conditions have continued to grow since the early 1970s (10). An example is the management of hypertension and heart disease. Effective disease management involves a process of identifying at-risk populations, coordinating systems of care delivery, obtaining outcomes, and managing outcomes most appropriately to improve care. Information is obtained through hospital discharge records, health plan databases (when the aim is to reduce costs associated with certain conditions), and through a team of individuals such as nurses and physicians that strive to improve the quality of care and develop processes to meet national guidelines.
Global and Population Health
A career in cardiac nursing may also lead to research and advocacy on the global epidemiology of cardiovascular disease. An example of an impact would include development and research on population-level primary and secondary prevention interventions for reducing cardiovascular disease risk factors. Nursing research can contribute to reducing cardiovascular morbidity and mortality in underserved populations in the U.S. and across the world.
Advanced Practice Nursing and Cardiovascular Care
Advanced practice nursing is attained through theoretical and evidence-based education at the graduate level and encompasses the registered nurse role with expanded education on cardiac disease processes, diagnoses and interventions, and care for individuals or populations (10). Today, advanced practice cardiac nurses are in high demand at the national and global level to meet the increasing need for better access to health care.

Self-Quiz
Ask Yourself...
- Are you familiar with opportunities for nurses to become active in healthcare policy?
- Why is the role of the advanced practice nurse important to the field of cardiology?
- How might inpatient and outpatient cardiac nursing roles differ?
- Are you familiar with organizations that aim to eliminate global cardiovascular health disparities?
Conclusion
The cardiac unit can be an intimidating unit if you are unfamiliar with the common conditions, procedures, and equipment. Cardiology is an impactful field with many areas for nurses to become specialized in. Whether you are regularly floated to the cardiac unit or exploring the possibility of becoming a cardiac nurse, hopefully this course helped you get to the “heart” of the matter!

Self-Quiz
Ask Yourself...
- Can you name various members of the interdisciplinary team in cardiology?
- Can you name the various diagnostic studies that may be used on a cardiac unit?
- What are some examples of noninvasive evaluation for chest pain?
- Can you name nursing interventions for patients with chest pain?
- Can you name possible contributing factors for abnormal heart rhythms?
- How would inpatient care for post-operative cardiac patients differ from routine cardiac care?
- Can you think of measures to ensure privacy of patients wearing a telemetry monitor?
- Are you familiar with available resources within your organization that help to strengthen nursing skills on ECG interpretation?
- Can you think of appropriate nursing interventions for a patient scheduled for a stress test?
- How can nurses advocate for patients who have fear and anxiety about cardiac procedures?
- Can you name examples of technological advances in cardiology that improve patient outcomes?
- How can nursing research reduce the morbidity and mortality of populations at greatest risk for cardiovascular disease?
References + Disclaimer
- Bickley, L. S., Szilagyi, P. G., Hoffman, R. M., & Soriano, R. P. (2021). Bate’s guide to physical examination and history taking (13th ed.). Wolters Kluwer Health: Philadelphia.
- Bohula, E. A., Katz, J. N., van Diepen, S., Alviar, C. L., Baird-Zars, V. M., Park, J. G., Barnett, C. F., Bhattal, G., Barsness, G. W., Burke, J. A., Cremer, P. C., Cruz, J., Daniels, L. B., DeFilippis, A., Granger, C. B., Hollenberg, S., Horowitz, J. M., Keller, N., Kontos, M. C., Lawler, P. R., … Critical Care Cardiology Trials Network (2019). Demographics, Care Patterns, and Outcomes of Patients Admitted to Cardiac Intensive Care Units: The Critical Care Cardiology Trials Network Prospective North American Multicenter Registry of Cardiac Critical Illness. JAMA cardiology, 4(9), 928–935. https://doi.org/10.1001/jamacardio.2019.2467
- Centers for Disease Control and Prevention (CDC). (2023). Heart disease facts. Retrieved from https://www.cdc.gov/heartdisease/facts.htm
- Coviello, J. S. (Ed.). (2017). ECG interpretation made incredibly easy! pocket guide (Third edition.). Wolters Kluwer.
- Jentzer, J. C., Sean, v. D., Barsness, G. W., Katz, J. N., Wiley, B. M., Bennett, C. E., Mankad, S. V., Sinak, L. J., Best, P. J., Herrmann, J., Jaffe, A. S., Murphy, J. G., Morrow, D. A., Wright, R. S., Bell, M. R., & Anavekar, N. S. (2019). Changes in comorbidities, diagnoses, therapies, and outcomes in a contemporary cardiac intensive care unit population. The American Heart Journal, 215, 12-19. https://doi.org/10.1016/j.ahj.2019.05.012
- Manda, Y.R. & Baradhi, K.M. (2023). Cardiac catheterization risks and complications. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK531461/
- Mubarik A. & Iqbal A.M. (2022). Holter Monitor. In: StatPearls [Internet].
- Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538203/
- Olson, Kate. (2021). Oxford Handbook of Cardiac Nursing. (3rd ed.). Oxford University Press,
- Incorporated.
- Open Resources for Nursing (Open RN); Ernstmeyer, K. & Christman, E., editors. Nursing
- Advanced Skills: Chapter 7 Interpret Basic ECG. Eau Claire (WI): Chippewa Valley Technical College; 2023. Retrieved https://www.ncbi.nlm.nih.gov/books/NBK594493/
- Perpetua, E. M., & Keegan, Patricia. (2020). Cardiac nursing: the red reference book for cardiac nurses (7th ed.). Wolters Kluwer
- Sandoval, Y., Apple, F. S., Mahler, S. A., Body, R., Collinson, P. O., & Jaffe, A. S. (2022). High-sensitivity cardiac troponin and the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guidelines for the Evaluation and Diagnosis of Acute Chest Pain. Circulation: Journal of the American Heart Association., 146(7), 569–581. https://doi.org/10.1161/CIRCULATIONAHA.122.059678
- Singh A., Museedi A.S., & Grossman, S.A. (2023) Acute Coronary Syndrome. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459157/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
