Course
Carotid Endarterectomy
Course Highlights
- In this Carotid Endarterectomy course, we will learn about the origin, development, and progression of carotid artery disease.
- You’ll also learn the role of carotid angioplasty and stenting (CAS) as alternatives to CEA for patients with restenosis following CEA or those with high surgical risk.
- You’ll leave this course with a broader understanding of the different surgical techniques used in CEA, including conventional and eversion endarterectomy.
About
Contact Hours Awarded: 2
Course By:
R.E. Hengsterman MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
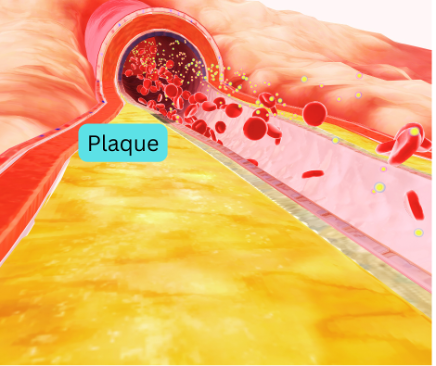
Atherosclerosis in the carotid artery can lead to stenosis, increasing an individual’s risk for cerebrovascular disease or stroke. Various revascularization techniques treat carotid artery stenosis, a significant risk factor for stroke. Carotid Endarterectomy (CEA), the gold standard, involves removing plaque from the common and internal carotid arteries to improve blood flow and reduce stroke risk [1][8].
This procedure, first performed in the early 1950s, has evolved in technique and indications, decreasing stroke risk, and improving survival in patients with moderate to severe carotid disease.
Neurologic dysfunction from microemboli can manifest as sudden or transient symptoms, including unilateral motor and sensory loss, aphasia, or dysarthria, often termed Transient Ischemic Attack (TIA) [1]. The majority of TIAs are brief, and by definition, lasting less than 24 hours [2]. A stroke, also known as a cerebrovascular accident, occurs when there is an acute disruption in cerebral perfusion or vasculature, making it a medical emergency [3].
Extracranial carotid disease often presents with symptoms caused by embolization, with arterial emboli accounting for approximately 25% of strokes in Europe and North America [3]. A majority (80%) of these emboli originate from atherosclerotic lesions in the neck at the bifurcation of the carotid artery [3]. Transcranial Doppler studies reveal that emboli are present in about 20% of patients with moderate stenosis (>50%) and are even more common in those with severe stenosis (>70%) [4] [5]. Symptomatic patients exhibited a higher incidence and frequency of emboli [4] [5].
Atherosclerotic lesions in the internal carotid artery develop along the carotid bulb wall, opposite the external carotid artery origin [3]. The bulb’s enlargement creates an area of low wall shear stress, promoting atherogenic particle interaction with the vessel walls and localized plaque formation at the bifurcation [3]. This localized atheroma’s accessibility facilitates effective plaque removal, reducing stroke risk. Without treatment, 26% of patients with TIAs and over 70% with severe stenosis will develop permanent neurological impairment within two years. Plaque removal can reduce this risk to 9% [3].
Carotid endarterectomy (CEA) is a surgical procedure aimed at unblocking a carotid artery to prevent stroke. The risk of stroke during CEA is about 2%, due to emboli or cross-clamp-related ischemia [8]. Monitoring cerebral blood supply during CEA is critical under general anesthesia, where surgeons use EEG or transcranial Doppler. Cerebral near-infrared spectroscopy (NIRS) serves as a dynamic tool for assessing and optimizing cerebral perfusion [7]. Providers use NIRS to monitor cerebral blood flow and make necessary adjustments during procedures. Inducing hypertension or placing an intracarotid shunt can maintain cerebral perfusion, though each method carries its own risks [6].
Carotid angioplasty and stenting have emerged as alternatives to CEA for treating carotid artery stenosis [9]. These techniques, similar to those used in cardiovascular disease, are useful in patients with restenosis following CEA. While EEG monitoring is not routine during these procedures, the role of these alternatives in managing symptomatic and asymptomatic carotid artery disease remains under study.

Self-Quiz
Ask Yourself...
- How does the process of plaque formation in the carotid artery bifurcation contribute to the risk of stroke, and why is carotid endarterectomy (CEA) considered the gold standard for treating this condition?
- Given the risks associated with emboli during carotid endarterectomy (CEA) and the alternatives like carotid angioplasty and stenting, what factors should clinicians consider when choosing the most appropriate treatment for a patient with severe carotid stenosis?
Anatomy and Physiology of the Carotid Arteries
The carotid arteries, a pair of vessels, transport oxygen-rich blood from the heart to the brain [10]. Traversing up either side of the neck, these arteries enter the brain, where they play a critical role in supplying most of the brain with blood [10]. The anatomical structure of the carotid arteries allows for significant redundancy; four out of five people can maintain adequate cerebral blood flow with just one carotid artery due to the anastomoses of other arteries [10]. However, the exact nature of these arterial connections can vary between individuals.
Understanding the anatomy and physiology of the carotid arteries is essential in comprehending the pathophysiology of carotid artery disease and its implications for stroke risk. This knowledge underpins the clinical approach to diagnosing, managing, and treating conditions like carotid stenosis, aiming to reduce the incidence of stroke and improve patient outcomes.

Self-Quiz
Ask Yourself...
- How does redundancy in the anatomical structure of the carotid arteries influence the management and treatment of carotid artery disease in patients?
- Why is a thorough understanding of carotid artery anatomy and physiology crucial for clinicians in reducing stroke risk and improving patient outcomes in cases of carotid stenosis?
Structure and Bifurcation
The carotid arteries consist of the common carotid arteries, which bifurcate into the internal and external carotid arteries at the level of the fourth cervical vertebra (C4), near the superior border of the thyroid cartilage [10]. This bifurcation occurs within the carotid sheath, a structure formed by the deep cervical fascia that also contains the internal jugular veins and vagus nerves [10].
The internal carotid artery (ICA) ascends into the skull to form part of the Circle of Willis, supplying blood to the brain and eyes [10]. The external carotid artery (ECA) branches off to supply blood to the neck, thyroid gland, face, and scalp [10].

Self-Quiz
Ask Yourself...
- How does the anatomical relationship between the carotid arteries, internal jugular veins, and vagus nerves within the carotid sheath impact surgical approaches to treating carotid artery disease?
- Why is the bifurcation of the common carotid artery into the internal and external carotid arteries significant in understanding the blood supply to the brain and face, and how does this knowledge influence the management of conditions like carotid stenosis?
Carotid Stenosis and Atherosclerosis
Carotid stenosis occurs when one or both carotid arteries narrow due to plaque buildup, a condition known as atherosclerosis [11]. Plaque accumulates at the bifurcation of the common carotid artery into the ICA and ECA [12]. This buildup narrows the lumen—the inside opening where blood flows—altering blood flow dynamics and increasing the risk of blood clot formation [12].
A blood clot that breaks away and travels to the brain can obstruct blood flow, leading to a stroke. While a stroke can also occur from insufficient blood flow through a narrowed carotid artery, this is rare due to the collateral circulation provided by the arterial anastomoses.

Self-Quiz
Ask Yourself...
- How does the buildup of plaque at the bifurcation of the common carotid artery into the ICA and ECA affect blood flow dynamics and increase the risk of stroke?
- In what ways does the presence of collateral circulation provided by arterial anastomoses influence the likelihood and severity of stroke in patients with carotid stenosis?
Risk Factors and Stroke
The degree of carotid artery narrowing, often reported as a percentage, is a critical factor in estimating stroke risk. Research has shown that both the severity of stenosis and the presence of symptoms influence stroke risk. A higher percentage of stenosis correlates with a greater risk of stroke if the condition is symptomatic [13].
Carotid artery stenosis is a manifestation of systemic atherosclerotic disease. Any risk factor that predisposes a patient to progressive atherosclerosis can lead to carotid artery stenosis, resulting in ischemic stroke or transient ischemic attack (TIA) symptoms [13]. Common risk factors include smoking, hyperlipidemia, male gender, and increased age [13].
In a minority of cases, in young females, fibromuscular dysplasia (FMD) plays a more significant role in carotid artery stenosis. FMD is a noninflammatory, nonatherosclerotic condition that affects medium-sized arteries, notably the carotid and renal arteries [3].

Self-Quiz
Ask Yourself...
- How does the percentage of carotid artery narrowing influence the risk of stroke, and why is the presence of symptoms a key factor in determining this risk?
- In what ways do systemic risk factors such as smoking, hyperlipidemia, and increased age contribute to the development of carotid artery stenosis, and how does fibromuscular dysplasia (FMD) differ as a cause in young females?
Indications
Carotid stenosis is a chronic condition that develops as people age due to the accumulation of excess cholesterol in the blood [11]. Low-density lipoprotein (LDL) cholesterol plays a significant role in this process. Over time, LDL cholesterol traps inside the blood vessel walls and adheres to the outside, leading to plaque formation [11]. This process, known as atherosclerosis, narrows the carotid arteries.
Numerous patients with carotid stenosis do not exhibit symptoms, and healthcare providers often discover the condition as a secondary finding. However, when the narrowing becomes symptomatic, it can cause a transient ischemic attack (TIA) or stroke. A TIA, which does not cause permanent brain damage and is undetectable on MRI or CT scans, shares similar signs with a stroke, including facial droop, speaking difficulties, comprehension, unilateral weakness or numbness, and sudden vision loss in one eye [2]. The side of the body affected by these symptoms is notable; for instance, stenosis in the left carotid artery affects the left eye and the right side of the body, and vice versa for the right carotid artery.
Amaurosis fugax (AF) is a classic symptom of carotid artery disease, presenting as transient vision loss (TVL) [38]. AF can manifest as either monocular (TMVL) or binocular (TBVL) vision loss [38]. The workup for patients with AF must be evaluated for sources of emboli and ischemia. This involves imaging studies such as bilateral carotid Doppler ultrasonography, magnetic resonance angiography (MRA), or computed tomography (CT) angiography of the neck and head [38]. These diagnostic tools help identify the underlying causes and guide appropriate treatment standards.

Self-Quiz
Ask Yourself...
- How does the accumulation of low-density lipoprotein (LDL) cholesterol contribute to the development of carotid stenosis, and what are the implications of this process for aging individuals?
- What are the differences in clinical presentation between a transient ischemic attack (TIA) and a stroke, and why is it important to recognize these differences in patients with symptomatic carotid stenosis?
- Why is amaurosis fugax (AF) considered a classic symptom of carotid artery disease, and what are the essential components of the diagnostic workup for patients presenting with transient vision loss (TVL)?
History & Physical
During a routine medical examination, a primary care provider might listen to the carotid arteries using a stethoscope to check for a bruit, a “whooshing” sound indicative of significant narrowing. If a healthcare provider detects a bruit, they will often schedule a carotid ultrasound for the patient. Carotid stenosis may cause non-specific symptoms such as dizziness, vertigo, lightheadedness, fainting, visual problems, headaches, or weakness [14].
Several factors contribute to the development of atherosclerotic plaque in the carotid arteries, including genetics, high cholesterol, smoking, a fatty diet, and physical inactivity [14]. Patients who have undergone radiation therapy for head and neck cancers may develop carotid artery stenosis as a result of radiation effects rather than plaque buildup [15]. Some inflammatory conditions can also cause irregularities in the carotid arteries [16].


Self-Quiz
Ask Yourself...
- How does the detection of a bruit during a routine examination guide further diagnostic steps for carotid artery stenosis, and what is the significance of conducting a carotid ultrasound following this finding?
- What are the range of factors that contribute to the development of atherosclerotic plaque in the carotid arteries, and how do non-specific symptoms like dizziness and headaches complicate the diagnosis of carotid stenosis?
Comprehensive Management and Treatment Strategies for Carotid Artery Disease
Vascular surgeons can perform carotid endarterectomy (CEA) under regional anesthesia in patients with severe chronic obstructive pulmonary disease, coronary artery disease (CAD), and other comorbidities. Carotid stenting is an option for patients with a history of neck irradiation, modified radical neck dissection, or re-operative CEA [3]. Consider combined CEA and coronary artery bypass grafting for patients with concurrent symptomatic carotid stenosis and coronary artery disease (CAD) [3].
Patients undergoing CEA should take antiplatelet therapy unless contraindicated [17]. A vascular surgeon or neurosurgeon can perform the procedure under general or local anesthesia, with local anesthesia allowing the patient to remain awake but sedated, feeling numb at the surgery site.
The development of significant restenosis after CEA or carotid angioplasty with stenting poses a risk of ischemic stroke [18]. Treatment strategies play a crucial role in preventing this complication. Surgeons often manage restenosis after carotid angioplasty with stenting by performing CEA and removing the stent, while managing restenosis after CEA involves performing carotid angioplasty with stenting [18] [19]. In cases where stenting is contraindicated, repeated CEA may be necessary, though it carries risks of bleeding and cranial nerve trauma.
The North American Symptomatic Carotid Endarterectomy Trial (NASCET) and the European Carotid Surgery Trial (ECST) have demonstrated the benefits of CEA over medical management alone for symptomatic patients with severe carotid stenosis [8]. The 2nd European Carotid Surgery Trial (ECST-2): recommends carotid endarterectomy for symptomatic patients with carotid stenosis of 50% or more, based on findings from randomized trials conducted 30 years ago [20].
The Asymptomatic Carotid Atherosclerosis Study (ACAS) supports using CEA for asymptomatic patients with significant stenosis [21]. CEA addresses symptomatic high-grade stenosis, symptomatic moderate stenosis, and asymptomatic high-grade stenosis of the internal carotid artery. Early intervention reduces the risk of stroke, though the benefits diminish if performed more than two weeks after symptom onset or in cases of large stroke areas, contralateral carotid occlusion, hemodynamic instability, or contralateral laryngeal palsy [17]. The ongoing CREST-2 (Carotid Revascularization, Endarterectomy Versus Stent Trial‐2 trial) aims to provide updated data comparing intensive medical therapy versus surgery in patients with asymptomatic, high-grade internal carotid stenosis [22].
Providers can screen for asymptomatic carotid stenosis using carotid duplex ultrasonography (CDU) to assess the degree of stenosis by measuring flow velocity [4]. Other imaging modalities like computed tomography angiography (CTA) and contrast-enhanced magnetic resonance angiography (CE-MRA) provide additional insights into plaque morphology, intracranial collateralization, and brain perfusion, helping to determine individual risk profiles when considering surgery [23].

Self-Quiz
Ask Yourself...
- What factors determine whether a vascular surgeon will choose carotid endarterectomy (CEA) or carotid stenting for a patient, and how do comorbid conditions influence this decision?
- How does the use of antiplatelet therapy in patients undergoing carotid endarterectomy (CEA) contribute to the prevention of complications, and what are the potential risks if this therapy is contraindicated?
- What are the key differences in managing restenosis after carotid endarterectomy (CEA) versus carotid angioplasty with stenting, and what are the associated risks with each approach?
- How do findings from the North American Symptomatic Carotid Endarterectomy Trial (NASCET) and the European Carotid Surgery Trial (ECST) support the use of carotid endarterectomy (CEA) for symptomatic patients, and what ongoing studies aim to refine these guidelines?
Evolving Surgical Methods for Carotid Artery Revascularization: CEA, TFCAS, and TCAR
The primary methods to address carotid stenosis include Carotid Endarterectomy (CEA), Transfemoral Carotid Artery Stenting (TFCAS), and Transcarotid Artery Revascularization (TCAR) [34]. CEA has long been the gold standard surgical approach, offering effective plaque removal from the carotid arteries [34].
TFCAS emerged as a less invasive alternative, beneficial for patients with severe stenosis and coexisting conditions [34]. TCAR has gained prominence for high-risk patients due to its lower stroke rates and favorable outcomes [34]. Each method offers distinct advantages, with the choice depending on patient-specific risk factors and anatomical considerations.

Self-Quiz
Ask Yourself...
- What are the distinct advantages and potential limitations of Carotid Endarterectomy (CEA), Transfemoral Carotid Artery Stenting (TFCAS), and Transcarotid Artery Revascularization (TCAR) in treating carotid stenosis, and how do patient-specific risk factors influence the choice of method?
- How has the evolution of surgical methods like TFCAS and TCAR impacted the management of carotid artery stenosis in high-risk patients, compared to the traditional CEA approach?
Carotid Endarterectomy (CEA)
Carotid endarterectomy (CEA) has been the standard operative therapy for carotid artery stenosis in both symptomatic and asymptomatic patients [1][8]. CEA involves removing plaque from the carotid artery via surgical methods to prevent stroke. Analysis of more than 100,000 patients in a cohort study highlights that 75.0% of the patients between 2015 and 2019 underwent CEA, making it the most common carotid revascularization approach [34].

Self-Quiz
Ask Yourself...
- What factors contribute to Carotid Endarterectomy (CEA) being the most common carotid revascularization approach, and how does its effectiveness compare in treating symptomatic versus asymptomatic patients?
Transfemoral Carotid Artery Stenting (TFCAS)
TFCAS accounted for 14.3% of carotid revascularization approaches in the study, reflecting its role as a viable alternative to CEA in high-risk patients [34]. Transfemoral Carotid Artery Stenting (TFCAS) treats carotid artery blockages by using a metallic stent to open a narrowed artery [34]. This procedure serves as an alternative for patients at substantial risk for open surgery and is the preferred treatment for restenosis following Carotid Endarterectomy (CEA).

Self-Quiz
Ask Yourself...
- How does Transfemoral Carotid Artery Stenting (TFCAS) compare to Carotid Endarterectomy (CEA) in terms of effectiveness and patient suitability for high-risk patients and those with restenosis?
Transcarotid Artery Revascularization (TCAR)
Transcarotid artery revascularization (TCAR) has emerged as a new method for carotid revascularization for high-risk patients [34]. Contemporary data from the Vascular Quality Initiative (VQI) show excellent results for TCAR. In the cohort analyzed from the VQI database during the years 2015-2019, 10.7% of patients underwent TCAR, highlighting its increasing use among patients at substantial risk for stroke, cranial nerve injury, or cardiovascular events [34].
TCAR has become the primary carotid revascularization approach in the US for high-risk patients, surpassing both TFCAS and CEA [34].
While CEA remains the most common overall approach, TCAR reflects advancements in medical devices and surgical techniques, offering safer and more effective options for specific patient groups and underscoring the efficiency of modern carotid revascularization techniques [34].

Self-Quiz
Ask Yourself...
- What advancements in medical devices and surgical techniques have contributed to the increased use of Transcarotid Artery Revascularization (TCAR) among high-risk patients, and how do these improvements enhance patient outcomes compared to traditional methods?
- How does the effectiveness and safety profile of TCAR compare to Carotid Endarterectomy (CEA) and Transfemoral Carotid Artery Stenting (TFCAS) in the management of carotid artery stenosis in high-risk patients?
Considerations
- Symptomatic Ill Patients: Consider carotid angioplasty and stenting (CAS) for patients who are unstable and cannot undergo open surgery. During CAS, the vascular surgeon inserts a small, flexible, mesh-like tube (stent) into the artery under local anesthesia [17]. The surgeon then expands the tube over a balloon to widen the artery’s lumen and improve blood flow.
- Peri-Procedural Risks: According to the Carotid Revascularization Endarterectomy versus Stenting Trials (CREST), both carotid endarterectomy (CEA) and CAS yield similar outcomes regarding postoperative complications such as restenosis, myocardial infarction, long-term stroke, and/or death [8]. However, the risk of peri-procedural stroke is higher in patients undergoing CAS, whereas the overall risk of myocardial infarction is higher in CEA [24].
- Radiation Therapy History: Patients with a history of neck radiation therapy face an increased risk of temporary cranial nerve injury during carotid endarterectomy (CEA), though this does not serve as an absolute contraindication [17]. These patients are also at increased risk of late cerebrovascular events and restenosis following CAS [17]. Performing CEA is more challenging in the radiated neck due to more diffuse plaques, adhesions, scar tissue, and potential wound complications resulting from radiation therapy [17].
- Gender Differences in Outcomes: Symptomatic women may be at an increased risk of postoperative complications after CEA compared to men [17][25]. However, outcomes and complications are similar between sexes for asymptomatic patients [17] [25].

Self-Quiz
Ask Yourself...
- What considerations might lead a healthcare provider to choose Carotid Angioplasty and Stenting (CAS) over Carotid Endarterectomy (CEA) for an unstable patient, and how does the local anesthesia used in CAS benefit such patients?
- How do the peri-procedural risks of stroke and myocardial infarction differ between CAS and CEA, and what implications do these differences have for patient outcomes and treatment selection?
- How does the history of neck radiation therapy complicate the process and outcomes of carotid endarterectomy (CEA), and what specific challenges does it pose for surgeons?
- Why might symptomatic women experience a higher risk of postoperative complications after CEA compared to men, and what factors might contribute to similar outcomes between sexes for asymptomatic patients?
Complications
Consider the risks of carotid endarterectomy alongside the potential benefits of the procedure. The morbidity and mortality rates of CEA depend on multiple factors, including:
- Surgical expertise
- Degree of carotid artery stenosis
- Presence of cerebral infarction
- Coexistent medical conditions including ischemic heart disease
Reported morbidity rates for CEA have varied from 0 to 20% [26]. In one multicenter study, perioperative morbidity was 2.2%, and mortality was 3.3%, resulting in a combined complication rate of 5.5% in high-risk patients [26].

Self-Quiz
Ask Yourself...
- How does the range of factors such as surgical expertise and coexistent medical conditions influence the morbidity and mortality rates in patients undergoing carotid endarterectomy (CEA)?
- Given the reported morbidity and mortality rates, how can we weigh the potential benefits of carotid endarterectomy against its risks in high-risk patients?
Major Complications
- Myocardial Infarction
- Hyperperfusion Syndrome
- Nerve Injury
-
- Cranial nerves often affected include the hypoglossal, vagus, glossopharyngeal, and facial (marginal mandibular) nerves [27].
- Perioperative Stroke
- Restenosis
- Death
Minor Complications
- Transient Ischemic Attack (TIA)
- Bleeding
- Infection
- Greater Auricular Nerve Injury
- Dysphagia

Angiography Risks
Angiography, often performed as part of the CEA procedure, carries a risk of approximately 1% [28]. The timing of cerebral revascularization after ischemic stroke is critical. Recent studies have demonstrated the safety and effectiveness of performing CEA during the acute phase of stroke:
- CEA in the acute period post-stroke leads to significant regression of neurological symptoms and is associated with a negligible risk of adverse cardiovascular events [29].
- Emergency CEA performed in the first hours after stroke development has shown satisfactory outcomes, due to thorough preoperative preparation [30]. The use of a temporary shunt reduces hemodynamic shock after internal carotid artery occlusion, though this practice is associated with a higher likelihood of hemorrhagic transformation [8].

Self-Quiz
Ask Yourself...
- Considering the range of major complications such as myocardial infarction, hyperperfusion syndrome, and perioperative stroke, how do you evaluate the risks versus the benefits of undergoing carotid endarterectomy?
- How does the timing of cerebral revascularization after ischemic stroke impact the outcomes of carotid endarterectomy, and what factors should influence the decision to perform CEA during the acute phase of stroke?
Balancing Benefits and Risks of Carotid Endarterectomy (CEA): Key Considerations and Patient Outcomes
Consider the potential benefits of carotid endarterectomy (CEA) alongside its risks. Factors such as surgical expertise, the degree of carotid artery stenosis, the presence of cerebral infarction, and coexistent medical conditions like ischemic heart disease influence the morbidity and mortality rates for CEA. Reported morbidity rates vary, with some studies indicating perioperative morbidity of 2.2% and mortality of 3.3% [30] [31].
Studies have highlighted the safety and efficacy of performing CEA during the acute phase of stroke, showing significant regression of neurological symptoms with a minimal risk of adverse cardiovascular events. However, performing CEA in proximity to stroke onset increases the risk of hemorrhagic transformation (blood from outside the brain leaks into the brain through a damaged blood-brain barrier) and other adverse outcomes [32] [33].
A 2021 multicenter study reported a symptomatic hemorrhagic transformation rate of 3.6% and a combined endpoint of adverse outcomes reaching 20.4%, suggesting caution in immediate post-stroke revascularization with CEA [32] [33]. Careful assessment and risk management are essential to optimize patient outcomes when considering CEA.

Self-Quiz
Ask Yourself...
- How do factors such as surgical expertise, degree of carotid artery stenosis, presence of cerebral infarction, and coexistent medical conditions influence the decision to undergo carotid endarterectomy, and how should providers weigh these factors against the potential benefits?
- Given the increased risk of hemorrhagic transformation and other adverse outcomes when performing carotid endarterectomy immediately after a stroke, what strategies should be employed to carefully assess and manage these risks to optimize patient outcomes?
Carotid Endarterectomy and Carotid Artery Stenting
Carotid artery stenting (CAS) is often the preferred treatment for symptomatic carotid occlusion (50-99%) in patients with multiple comorbidities, tracheostomies, or a history of neck radiation or dissection [3]. Despite the increased risk of stroke during the procedure, CAS outcomes are comparable to carotid endarterectomy (CEA) [3]. CAS is under investigation in the ongoing CREST-2 study.
In the conventional technique, the surgeon creates a longitudinal arteriotomy from the distal common carotid artery (CCA) onto the internal carotid artery (ICA), removes the plaque, and closes the arteriotomy with a patch [35]. In the eversion technique, the surgeon transects the ICA at its origin from the CCA and averts the vessel to expel the plaque [35].
CEA involves accessing the carotid sheath via a longitudinal incision along the medial border of the sternocleidomastoid muscle (SCM), isolating and controlling the distal CCA, its bifurcation, and the ICA and external carotid artery (ECA) [35]. Surgeons must decide whether to use a shunt to maintain cerebral perfusion through the ICA.

Self-Quiz
Ask Yourself...
- What factors should providers consider when choosing between carotid artery stenting (CAS) and carotid endarterectomy (CEA) for treating symptomatic carotid occlusion, especially in patients with multiple comorbidities?
- How do the conventional and eversion techniques of carotid endarterectomy (CEA) differ in terms of procedural steps and outcomes, and what implications do these differences have for surgical decision-making?
Clinical Significance
The primary purpose of carotid endarterectomy (CEA) is to prevent stroke. The benefit of CEA is dependent on achieving low morbidity and mortality rates. CEA treats symptomatic high-grade stenosis, symptomatic moderate stenosis, and asymptomatic high-grade stenosis of the internal carotid artery [17].
Implications for Current Practice
The benefit of endarterectomy lies in its ability to reduce the substantial stroke risk in treated patients [1][3]. The combined stroke and death risk of CEA ranges from 2% to 4%, with higher rates in symptomatic patients compared to asymptomatic ones. [1][3] These findings highlight the crucial role of CEA in stroke prevention for patients with significant carotid stenosis.

Self-Quiz
Ask Yourself...
- How do the varying morbidity and mortality rates of carotid endarterectomy (CEA) impact its effectiveness in preventing strokes in patients with various degrees of carotid stenosis?
Two Case Studies: Carotid Endarterectomy (CEA) for Extracranial Carotid Disease
Neurologic dysfunction from microemboli can manifest as sudden or transient symptoms, including unilateral motor and sensory loss, aphasia, or dysarthria, often termed Transient Ischemic Attack (TIA). Most TIAs are brief, lasting only minutes, and by convention, the limit for a TIA is 24 hours.
Persistent symptoms beyond this period indicate a stroke or cerebrovascular accident (CVA). An embolus to the ophthalmic artery can cause temporary or permanent vision loss, known as amaurosis fugax.
Atherosclerotic lesions in the internal carotid artery can develop along the carotid bulb wall, opposite the external carotid artery origin. The bulb’s enlargement creates an area of low wall shear stress, promoting atherogenic particle interaction with the vessel walls and localized plaque formation at the bifurcation. This localized atheroma’s accessibility facilitates effective plaque removal reducing stroke risk. Without treatment, 26% of patients with TIAs and over 70% with severe stenosis will develop permanent neurological impairment within two years. Plaque removal can reduce this risk to 9%.
Patient Case Study: Carotid Endarterectomy with Nerve Block Technique
Patient Profile:
- Age/Gender: 70-year-old female
- Medical History: Severe stenosis of the right internal carotid artery, previous history of stroke
Clinical Presentation and Diagnosis
A 70-year-old female with severe stenosis of the right internal carotid artery arrived for evaluation and treatment. Due to her age and history of stroke, the surgical team opted for carotid endarterectomy (CEA) under regional anesthesia to allow for continuous neurological monitoring during the procedure.
Nerve Block Technique: The surgical team positioned the patient supine with her neck extended and rotated away from the blocked side. Using a high-frequency linear ultrasound transducer, the surgeon visualized the cervical plexus along the posterior border of the sternocleidomastoid muscle. Using ultrasound guidance, the clinician inserted a 22-gauge, 50 mm needle in-plane. After confirming negative aspiration and correct needle placement, the clinician incrementally injected 10 mL of 0.25% bupivacaine around the cervical plexus, while monitoring for signs of intravascular or intrathecal injection.
Procedure: The surgeon performed the carotid endarterectomy to remove the atherosclerotic plaque. Throughout the procedure, regional anesthesia allowed the surgical team to monitor the patient’s neurological status.
Outcome: The procedure was successful with no immediate complications. The patient remained stable and showed no signs of post-operative neurological deterioration.
Patient Case Study: Carotid Endarterectomy in an 81-Year-Old Male with Change in Mental Status
Patient Profile:
- Age/Gender: 81-year-old male
- Medical History: Ischemic stroke, hypertension, hyperlipidemia, hypothyroidism, chronic kidney disease, previous ischemic strokes in 2003 and 2007 with residual right-sided weakness, on aspirin/dipyridamole for stroke prevention.
Clinical Presentation
An 81-year-old right-handed man presented to the Emergency Department with symptoms of dizziness, nausea, dysarthria, and a change in mental status. His history included two prior ischemic strokes, hypertension, hyperlipidemia, hypothyroidism, and chronic kidney disease.
Initial Examination:
- Vital Signs: Afebrile, BP 162/81 mmHg, HR 77 bpm, O2 sat 98% on room air
- Neurological Examination: Alert and oriented to person but disoriented to location and time. Noted poor memory, fair concentration, mild dysarthria, nonfluent aphasia, poor knowledge, and limited judgment. The pupils appeared round and reacted to light, with extraocular movements intact. No facial weakness or pronator drift, and motor and sensory examinations were nonfocal. Reflexes were symmetrical, and coordination was normal.
Laboratory Studies:
- WBC Count: 12,600/μL
- Platelet Count: 155,000/μL
- Electrolytes: Sodium 141 mEq/L, Potassium 4.3 mEq/L
- Glucose: 123 mg/dL
- Serum Creatinine: 1.50 mg/dL
Imaging:
- CT scan: No acute findings
- CTA: Remote infarct in the left parietal lobe, diminished flow in distal left MCA branches, severe atherosclerosis and stenosis of the proximal ICA, PTA supplying mid and distal basilar artery.
- MRI: Subacute infarcts in the posterior left temporal and frontal lobes, right occipital lobe, and bilateral cerebellar hemispheres.
Hospital Course
Two days after admission, the patient became nonverbal and somnolent, with a motor examination revealing right-sided hemiplegia. A repeat MRI showed new areas of restricted diffusion in the left frontoparietal region, brain stem, bilateral superior cerebellar, and occipital regions, indicating emboli from the atherosclerotic left ICA reaching the posterior fossa via the PTA.
Intervention: The medical team transferred the patient to the neuroscience intensive care unit, setting a systolic blood pressure goal of 180-200 mmHg. A carotid duplex ultrasound confirmed 80% to 99% stenosis of the proximal left ICA. One week after admission, the surgical team performed a left carotid endarterectomy and used a bovine patch for angioplasty.
Outcome: The procedure was successful with no complications. The patient’s neurological status improved, and he transitioned to a skilled nursing facility for rehabilitation without experiencing a recurrence of ischemic stroke.
Post-Endarterectomy Home Care Instructions
Ensuring patients adhere to proper home care instructions post-carotid endarterectomy is vital for a smooth recovery. During the first few days after surgery, patients should engage in quiet activities such as reading or watching television to avoid unnecessary strain.
Patients must take their prescribed medications to aid in recovery and prevent complications. It is crucial to perform a daily inspection of the incision site, monitoring for signs of infection, including redness, swelling, drainage, or warmth. The wound must remain dry until the healthcare provider permits showering, and patients should avoid scrubbing the incision area.
When shaving around the incision, patients should use an electric razor to prevent accidental cuts. Inform patients that temporary loss of sensation along the jawline, incision line, and earlobe is a normal postoperative occurrence, with sensation returning within 6 to 12 months [37].
Patients should increase their activity level but avoid strenuous activities for at least 7 to 10 days following surgery [36]. They must refrain from lifting objects heavier than 10 pounds for 2 to 3 weeks to prevent undue stress on their healing body [36]. They should not drive until their healthcare provider grants clearance, which occurs 1 to 2 weeks post-surgery.
Patients should consult their healthcare provider to determine an appropriate timeline for returning to work based on their recovery progress. Adhering to these guidelines will help ensure a safe and effective recovery process.


Self-Quiz
Ask Yourself...
- How does adhering to proper home care instructions post-carotid endarterectomy influence the recovery process and prevention of complications?
- Why is it essential for patients to avoid strenuous activities and heavy lifting during the initial weeks following a carotid endarterectomy?
Conclusion
Extracranial carotid disease, often presenting with symptoms caused by embolization, is a significant contributor to strokes in Europe and North America. Atherosclerotic lesions at the bifurcation of the carotid artery are responsible for 80% of emboli leading to these strokes. Carotid endarterectomy (CEA) addresses these lesions, reducing stroke risk by removing the plaque and restoring normal blood flow. Studies have shown that without treatment, 26% of patients with transient ischemic attacks (TIAs) and over 70% with severe stenosis will develop permanent neurological impairment within two years. CEA can reduce this risk to 9%.
Carotid endarterectomy (CEA) stands as the preferred treatment for both symptomatic and asymptomatic carotid stenosis. The procedure, which involves plaque removal from the common and internal carotid arteries, has evolved since its inception in the early 1950s, leading to improved survival rates and reduced stroke risks. While carotid angioplasty and stenting offer alternative treatments for patients with restenosis post-CEA, CEA’s effectiveness in preventing strokes in high-grade stenosis cases is well-documented.
Understanding the anatomy and physiology of the carotid arteries, along with the pathophysiology of carotid artery disease, is crucial for optimizing treatment strategies and improving patient outcomes. Providers must weigh the risks of CEA, such as myocardial infarction, hyperperfusion syndrome, nerve injury, perioperative stroke, restenosis, and death, against its benefits. However, with careful patient selection and advancements in surgical techniques and monitoring, CEA continues to be a critical intervention in managing carotid artery disease and preventing strokes.
References + Disclaimer
- Panuganti, K. K., Tadi, P., & Lui, F. (2023, July 17). Transient ischemic attack. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK459143/
- Transient Ischemic Attack (TIA). (2024). National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/transient-ischemic-attack-tia
- Qaja, E., & Kariyanna, P. T. (2023, July 24). Carotid artery surgery. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK441947/
- Kim, H. W., Regenhardt, R. W., D’Amato, S. A., Nahhas, M. I., Dmytriw, A. A., Hirsch, J. A., Silverman, S. B., & Martinez-Gutierrez, J. C. (2022). Asymptomatic carotid artery stenosis: a summary of current state of evidence for revascularization and emerging high-risk features. Journal of Neurointerventional Surgery, 15(7), 717–722. https://doi.org/10.1136/jnis-2022-018732
- Walubembe, J., Ssinabulya, I., Mubuuke, A. G., Kagwa, M. M., Babirye, D., Okot, J., Bongomin, F., Nakku, M., Ongom, D. O., & Ameda, F. (2023). Carotid Doppler findings among patients admitted with stroke in two tertiary care facilities in Uganda: A Hospital-based Cross-sectional Study. Research Square (Research Square). https://doi.org/10.21203/rs.3.rs-2800534/v1
- Jahangiri, F. R., Liang, M., Huckabey, M., Baloney, N., & Sharifi, S. (2022). Carotid endarterectomy surgeries: a multimodality intraoperative neurophysiological monitoring approach. Curēus. https://doi.org/10.7759/cureus.26556
- Lukaszewski, M., & Nelke, K. (2024). Near-Infrared Spectroscopy (NIRS) in the assessment of Cerebral tissue Oxygenation (RSO2): Methodological issues and dilemmas. Anesthesia Research, 1(1), 24–33. https://doi.org/10.3390/anesthres1010004
- Keegan, A., & Hicks, C. W. (2022). Surgical Decision-Making and outcomes in open versus endovascular repair for various vascular diseases. Anesthesiology Clinics, 40(4), 627–644. https://doi.org/10.1016/j.anclin.2022.08.008
- Vasavada, A. M., Singh, P., Firdaus, A., Sundaram, D. M., Patel, M., Singh, G., Palanisamy, L., Ansari, S. A., Thummala, S., & Pandya, H. (2023). Carotid Endarterectomy versus Stenting for the treatment of patients with carotid artery stenosis: An Updated Systematic Review and Meta-Analysis. Curēus. https://doi.org/10.7759/cureus.35070
- Charlick, M., & Das, J. M. (2023, July 24). Anatomy, head and neck: internal carotid arteries. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK556061/
- Ismail, A., Ravipati, S., Gonzalez-Hernandez, D., Mahmood, H., Imran, A., Munoz, E. J., Naeem, S., Abdin, Z. U., & Siddiqui, H. F. (2023). Carotid artery stenosis: A look into the diagnostic and management strategies, and related complications. Curēus. https://doi.org/10.7759/cureus.38794
- Yang, S., Woo, S., & Kim, D. (2022). Analysis of atherosclerotic plaque distribution in the carotid artery. Clinical Cardiology, 45(12), 1272–1276. https://doi.org/10.1002/clc.23903
- Abbott, A. (2021). Asymptomatic carotid stenosis and stroke risk. Lancet Neurology, 20(9), 698–699. https://doi.org/10.1016/s1474-4422(21)00199-x
- Dorobisz, K., Dorobisz, T., & Zatoński, T. (2020). The assessment of the balance system in cranial artery stenosis. Brain and Behavior, 10(9). https://doi.org/10.1002/brb3.1695
- American Association of Neurological Surgeons. (2024, April 26). Carotid Endarterectomy and Stenosis – AANS. AANS. https://www.aans.org/patients/conditions-treatments/carotid-endarterectomy-and-stenosis/
- Cardounell, S. Z., & Gonzalez, L. (2023, August 8). Carotid artery fibromuscular dysplasia. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538199/
- DaCosta, M., Tadi, P., & Surowiec, S. M. (2023, July 24). Carotid endarterectomy. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470582/
- Megaly, M., Alani, F., Cheng, C., & Ragina, N. (2021). Risk factors for the development of Carotid Artery In-Stent Restenosis: Multivariable analysis. Cardiovascular Revascularization Medicine, 24, 65–69. https://doi.org/10.1016/j.carrev.2020.09.005
- Stilo, F., Montelione, N., Calandrelli, R., Distefano, M., Spinelli, F., Di Lazzaro, V., & Pilato, F. (2020). The management of carotid restenosis: a comprehensive review. Annals of Translational Medicine, 8(19), 1272. https://doi.org/10.21037/atm-20-963
- Cheng, S. F., Van Velzen, T. J., Gregson, J., Richards, T., Jäger, H. R., Simister, R., Kooi, M. E., De Borst, G. J., Pizzini, F. B., Nederkoorn, P. J., Brown, M. M., & Bonati, L. H. (2022). The 2nd European Carotid Surgery Trial (ECST-2): rationale and protocol for a randomised clinical trial comparing immediate revascularisation versus optimised medical therapy alone in patients with symptomatic and asymptomatic carotid stenosis at low to intermediate risk of stroke. Trials, 23(1). https://doi.org/10.1186/s13063-022-06429-z
- Meschia, J. F. (2024). William M. Feinberg Lecture: Asymptomatic Carotid Stenosis: Current and Future Considerations. Stroke. https://doi.org/10.1161/strokeaha.124.046956
- Meschia, J. F., Edwards, L., Roubin, G., Brott, T. G., & Lal, B. K. (2024). CREST‐2 Commitment to rigorous assessment of carotid stenting for primary prevention of stroke. Stroke: Vascular and Interventional Neurology, 4(3). https://doi.org/10.1161/svin.123.001227
- Weberling, L. D., Lossnitzer, D., Frey, N., & André, F. (2022). Coronary Computed Tomography vs. Cardiac Magnetic Resonance Imaging in the Evaluation of Coronary Artery Disease. Diagnostics, 13(1), 125. https://doi.org/10.3390/diagnostics13010125
- Boulanger, M., Camelière, L., Felgueiras, R., Berger, L., Rerkasem, K., Rothwell, P. M., & Touzé, E. (2015). Periprocedural myocardial infarction after carotid endarterectomy and stenting. Stroke, 46(10), 2843–2848. https://doi.org/10.1161/strokeaha.115.010052
- Goicoechea, S., Walsh, M., Soult, M., Halandras, P. M., Bechara, C., Aulivola, B., & Crisostomo, P. R. (2022). Female gender increases risk of stroke and readmission after carotid endarterectomy and carotid artery stenting. Journal of Vascular Surgery, 75(6), 1935–1944. https://doi.org/10.1016/j.jvs.2021.10.034
- Liang, P., Solomon, Y., Swerdlow, N. J., Li, C., Varkevisser, R. R., De Guerre, L. E., & Schermerhorn, M. L. (2020). In-hospital outcomes alone underestimate rates of 30-day major adverse events after carotid artery stenting. Journal of Vascular Surgery, 71(4), 1233–1241. https://doi.org/10.1016/j.jvs.2019.06.201
- Cevik, O. M., Usseli, M. I., Babur, M., Unal, C., Eksi, M. S., Guduk, M., Ovalioglu, T. C., Aksoy, M. E., Pamir, M. N., & Bozkurt, B. (2021). The Carotid Endarterectomy Cadaveric Investigation for Cranial Nerve Injuries: Anatomical study. Brain Sciences, 11(2), 211. https://doi.org/10.3390/brainsci11020211
- Halliday, A., Bulbulia, R., Bonati, L. H., Chester, J., Cradduck-Bamford, A., Peto, R., Pan, H., Halliday, A., Bulbulia, R., Bonati, L. H., Peto, R., Pan, H., Potter, J., Eckstein, H. H., Farrell, B., Flather, M., Mansfield, A., Mihaylova, B., Rahimi, K., . . . Ramsey-Williams, V. (2021). Second asymptomatic carotid surgery trial (ACST-2): a randomised comparison of carotid artery stenting versus carotid endarterectomy. Lancet, 398(10305), 1065–1073. https://doi.org/10.1016/s0140-6736(21)01910-3
- Blay, E., Balogun, Y., Nooromid, M. J., & Eskandari, M. K. (2019). Early Carotid Endarterectomy after Acute Stroke Yields Excellent Outcomes: An Analysis of the Procedure-Targeted ACS-NSQIP. Annals of Vascular Surgery, 57, 194–200. https://doi.org/10.1016/j.avsg.2018.10.023
- Surgeon characteristics associated with mortality and morbidity following carotid endarterectomy | Neurology. (2000). Neurology. https://www.neurology.org/doi/10.1212/WNL.55.6.773
- Wadén, K., Hultgren, R., Kotopouli, M. I., Gillgren, P., Roy, J., Hedin, U., & Matic, L. (2023). Long Term Mortality Rate in Patients Treated with Carotid Endarterectomy. European Journal of Vascular and Endovascular Surgery, 65(6), 778–786. https://doi.org/10.1016/j.ejvs.2023.02.079
- Jaillard A, Cornu C, Durieux A, Moulin T, Boutitie F, Lees KR, et al. Hemorrhagic transformation in acute ischemic stroke: the mast-e study. Stroke. (1999) 30:1326–32. doi: 10.1161/01.STR.30.7.1326
- Hong, J. M., Kim, D. S., & Kim, M. (2021). Hemorrhagic transformation after ischemic Stroke: Mechanisms and management. Frontiers in Neurology, 12. https://doi.org/10.3389/fneur.2021.703258
- Stonko, D. P., Goldsborough, E., Kibrik, P., Zhang, G., Holscher, C. M., & Hicks, C. W. (2022). Use of transcarotid artery revascularization, transfemoral carotid artery stenting, and carotid endarterectomy in the US from 2015 to 2019. JAMA Network Open, 5(9), e2231944. https://doi.org/10.1001/jamanetworkopen.2022.31944
- Davidovic, L. B., & Tomic, I. Z. (2020). Eversion Carotid Endarterectomy : A Short Review. Journal of Korean Neurosurgical Society/Journal of Korean Neurosurgical Society/Daehan Sin’gyeong Oegwa Hag’hoeji, 63(3), 373–379. https://doi.org/10.3340/jkns.2019.0201
- Carotid endarterectomy – UpToDate. (2024). UpToDate. https://www.uptodate.com/contents/carotid-endarterectomy
- Vakharia, S. D., & Gupta, S. R. (2020). Sensation Loss of auricle following ear surgery by post-auricular incision: our experience. Indian Journal of Otolaryngology and Head & Neck Surgery, 74(S1), 120–124. https://doi.org/10.1007/s12070-020-01906-w
- Tadi, P., Najem, K., & Margolin, E. (2023, August 7). Amaurosis fugax. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470528/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
