Course
Common Hazardous Materials
Course Highlights
- In this Common Hazardous Materials course, we will learn about hazardous materials used in the healthcare setting.
- You’ll also learn hazardous material precautions and safety concerns.
- You’ll leave this course with a broader understanding of hazardous materials precautions in various healthcare settings.
About
Contact Hours Awarded: 1
Course By:
Kimberlee Emfield Rowett, DNP (c), MSN, MBA, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Hazardous materials, or sometimes referenced to as HAZMAT, are a group of chemicals or radioactive substances that can cause harm to the individual and/or environment upon exposure. Exposure to hazardous materials can happen for a variety of reasons, including inadvertent transportation incidents, or intentional exposure such as terrorist attacks (7). Nurses may assist in treating the community when either of these incidents occur. However, the most common exposure to hazardous materials will be work-related. Certain hazardous materials are also commonly stored, handled, and utilized in the healthcare setting. It is vital to understand which materials are hazardous, how to handle and dispose of correctly, and what precautions nurses should take in the process to protect themselves and patients in the healthcare setting (2).

Hazardous Materials
HAZAMAT is an abbreviation for hazardous materials (HAZardous MATerials). These are substances that pose a risk to health, property, and the environment. HAZMATs include toxic chemicals, nuclear waste, biological, chemical, and radiological agents, as well as fuels. They are found in a variety of forms including liquids, solids, gases, dust, vapor, mist, fumes, and smoke. HAZMATS are used in daily life in a variety of ways, making HAZMAT training important for nurses on a personal, professional, and community level (7).
Incidents and Response
HAZMAT incidents occur thousands of times per year. HAZMATs are released into the environment as a result of an accidents, natural disasters, or terrorist attack. Spills occurring on coastal waters can increase the potential harm to marine life, water sources, and impact economic stability. Coastal and inland HAZMAT accidents are referred to as HAZMAT incidents. Most commonly, trained military, first responders, and law enforcement assist with these HAZMAT incidents. However, any patient who has been negatively impacted by these HAZMATs may need to be admitted, treated, and monitored by hospital staff for appropriate recovery (7). When HAZMAT incidents occur, the National Contingency Plan outlines for appropriate response to clean, dispose of, and stop the spread of the HAZMATs appropriately, as well as treatment necessary for the exposed individuals. Healthcare organizations should also have best practice guidelines for HAZMATs, including incidents and day-to-day exposure of hazardous materials used in the healthcare setting (7).

Self-Quiz
Ask Yourself...
- What does HAZMATs stand for?
- How are nurses at risk for exposure to HAZMATs?
Hazardous Materials in Healthcare
Within the healthcare setting, there are numerous hazardous materials that may be used for treatments, to clean, disinfect or sterilize products and workspaces, as well as fix tissue specimens. Depending on the category, the precautions, risks, and treatments may vary. These hazardous materials found in the healthcare setting include chemical sterilant, high-level disinfectants, and nitrous oxide, among others. Surgical smoke is also considered hazardous material, and precautions must be taken when exposure to such is possible (7).
Treatments
Some treatments within the healthcare setting are considered hazardous materials and need to be handled carefully. The treatments that are categorized as hazardous materials include aerosolized medications, anesthetic gases, and antineoplastic drugs (7).
- Aerosolized Medications: Aerosolize medications are used to treat respiratory disease or infections. They can be provided via a nebulizer device, an aerosol bottle, or other aerosol spray techniques. Nurses can be exposed to these medications while in the healthcare setting by preparing and administering aerosolized medications to their patients as prescribed by the provider (7).
-
- Exposure Risks: Some of the medications in this group include ribavirin and pentamidine, which have been linked to reproductive concerns. Amikacin and colistin have been linked to difficulty breathing. Amikacin has also been linked to kidney toxicity, while colistin and tobramycin have been linked to asthma. The severity of adverse reactions to aerosolized medications will also depend on the exposure therein (7).
-
- Exposure Prevention: There are ways to protect against exposure that nurses should implement to reduce or eliminate the possibility of these negative side effects. Wearing personal protective equipment (PPE) when preparing, administering, and handling these aerosolized medications will greatly reduce the exposure risk. The suggested PPE for these medications include gloves and gowns as well as appropriate respiratory protection. It is also suggested that aerosol delivery devices are used. These devices have one-way valves with an expiratory filter to minimize inhalation for the non-prescribed individuals (7).
- Anesthetic Gases: General anesthesia is provided for patients during surgery to reduce their overall pain. Waste anesthetic gases, or sometimes referred to as WAGs, are gases and vapors that can leak into the surrounding room, putting healthcare workers at risk for exposure (7).
-
- Exposure Risk: Acute exposure to these gases may result in headaches, drowsiness, impaired judgment, or poor coordination. Long-term exposure can impact reproductive health or lead to cancer (7).
-
- Exposure Prevention : To prevent the harmful effects of anesthetic gases for healthcare workers, anesthetic machines with scavenging systems should be used. Closed system or low flow anesthesia should be considered if this practice is not harmful to the patients. It is also recommended that anesthetic gas flow after applying the delivery mask to the patient. A key-filler or other closed-system device when filling anesthesia vaporizers can also reduce exposure. Employees should also receive regular training on anesthetics and other hazardous gases and provide safe handling procedures (7).
- Antineoplastic Drugs: Antineoplastics drugs are medications provided to patients with cancer, arthritis, multiple sclerosis, and other non-cancer diagnosis. Chemotherapy, cytotoxic, and oncology drugs are all classified as antineoplastic drugs, and are considered hazardous. Many in this drug class are considered carcinogenic and no level of exposure is safe for healthcare professionals (7).
-
- Exposure Risk: Preparing, handling, administering, and shipping these medications all put certain healthcare workers at risk. Similarly, handlining the bodily waste or cleaning areas or linens what have been exposed still pose potential risks. Exposure can increase the risk of leukemia, other cancers, reproductive concerns, and chromosomal damage (7).
-
- Exposure Prevention: To avoid exposure to antineoplastic drugs, certain precautions and steps must be taken. First, two pairs of chemotherapy gloves and a nonabsorbent gown with tight-fitting cuffs must be worn. Before administering the medication, it is suggested the IV tubing is primed with a non-hazardous drug containing liquid, such as normal saline. Utilize supplementary engineering controls, such as closed-system drug transfer devices or needless systems. Chemo hoods and biological safety cabinets should be used when mixing and preparing antineoplastic medications. If clothing is contaminated, utilizing the hospital laundry system can prevent the need from taking these clothing items home and risk additional exposure to your family. You will need to follow appropriate laundering procedures outlined for antineoplastic medications. Finally, regular training and surveillance of appropriate antineoplastic handling and precautions should be provided and followed (7).

Self-Quiz
Ask Yourself...
- What are the three categories of HAZMATs treatments?
- What are three potential symptoms of exposure to HAZMATs treatments outlined in this section?
- Name two exposure prevention techniques for HAZMATs treatments.
Cleaning
Within the healthcare setting, it is vital that high standards of cleanliness are followed to prevent the spread of hospital-acquired illnesses and give the patients improved healing opportunities. Because cleanliness is so important, many of the cleaning agents used are strong and pose potential risk to those that use them. In this section we will review chemical sterilant and high-level disinfectants. These include ethylene oxide (EtO), hydrogen peroxide gas plasma (HPGP), vaporized hydrogen peroxide, and immersion and vapor phase peracetic acid (PAA) (7).
- Chemical Sterilant: Chemical sterilant are used to treat surgical instruments and other medical supplies. Using this form of sterilant reduces the risk of patient exposure to pathogens. However, the chemical sterilant are hazardous materials and pose risk for healthcare workers (7).
-
- Exposure Risk : Acute exposure of chemical sterilant increases the risk of respiratory irritation, headache, nausea, and shortness of breath. Certain chemical sterilant can also cause upper respiratory tract infections and skin irritation. Long-term exposure can lead to cancer, reproductive effects, mutagenic changes, neurotoxicity, and sensitization (7).
-
- Exposure Prevention: Ways to reduce exposure include appropriate training on Eto, HPGP, and PAA, as well as other sterilant. Standard operating procedures should be provided and readily available for review. The use of a single chamber sterilization process for EtO can also reduce exposure risks (7).
- High-Level Disinfectants: High-Level Disinfectants (HLDs) are chemical disinfectants used to disinfect reusable, medical, and dental devices. HLDs prevent hospital-acquired infections for patients. HLDs include Glutaraldehyde, Ortho-Phthaldehyde, Peracetic acid, Hydrogen peroxide, Hypochlorous acid, and Hypochlorite (7).
-
- Exposure Risk: HLDs exposure can lead to dermatitis, mucous membranes irritation, skin and repository tract irritation, and aggravation of pre-existing asthma and asthma-like symptoms such as wheezing or shortness of breath. Similarly, chronic exposure to HLDs include asthma-like symptoms and reproductive effects (7).
-
- Exposure Prevention: Exposure prevention for HLDs include appropriate training, use of spill kits, and use of PPE such as gloves, water-resistant gowns or other outer garments (7).

Self-Quiz
Ask Yourself...
- What are the two categories of cleaning HAZMATs?
- Name three symptoms of exposure to chemical sterilants.
- Name three symptoms of high-level disinfectants.
- Name two exposure prevention techniques for cleaning HAZMATs.
Other Hazardous Materials
While not a treatment or cleaning product, nitrous oxide and surgical smoke are also considered hazardous material. Precautions must be taken when exposure to such is possible (7).
- Nitrous Oxide: Nitrous Oxide is often used in the dental setting, used to reduce pain during dental procedures. This increases risk for dental providers and professionals (7).
-
- Exposure Risk: Acute exposure to nitrous oxide increases the risk for lightheadedness, eye and upper airway irritation, cough, shortness of breath, and decrease in mental performance. Chronic exposure to nitrous oxide increases the risk for neurological, renal, and liver disease as well as the risk for miscarriage and fertility issues (7).
-
- Exposure Prevention: To reduce the risk of nitrous oxide exposure, certain actions should be taken. First, engineering controls, such as a nasal scavenging mask, can reduce overall exposure. Similarly, employees should receive appropriate training, protocols, and policies on appropriate and safe handling of nitrous oxide. Employees can also reduce risk by using a soap solution to test for connection leaks before use (watching for bubbling). It is also recommended to start the gas flow after the nasal mask has been placed on the patient’s nose. Turning off the nitrous oxide gas before turning off the oxygen flow can reduce exposure as well. Employees should also have easy access to the safe handling procedures and receive annual refresher courses on proper handling (7).
- Surgical Smoke: Surgical smoke occurs during surgical procedures when lasers or electrosurgical devices are used. These devices can cause surgical smoke, which is characterized as having a bad odor and decreases visibility of the surgical site. Over half a million healthcare workers are exposed to surgical smoke each year. This smoke can contain toxic gases, vapors and particulates, viable and non-viable cellular material, viruses, bacteria, and potential transmission of human papillomavirus (HPV) (7).
-
- Exposure Risk: Exposure to surgical smoke increases the risk for health effects including eye, nose, and throat irritation, headache, cough, nasal congestion, asthma, and asthma-like symptoms. There is limited research about the long-term effects of surgical smoke (7).
-
- Exposure Prevention: Local exhaust ventilation (LEV) should be used for all surgical procedures that risk surgical smoke exposure. Smoke evacuators should be utilized for surgeries with considerable plume (smoke caused by laser use on skin). Room wall suction systems to control small amounts of smoke are sufficient for rooms with adequate room air ventilation. Employees should be trained on the hazards of surgical smoke and how to minimize exposure. Procedures should be made available regarding surgical smoke hazards. Employees are encouraged to use appropriate respiratory protection for particulates, including a properly fitted N95. If LEV is not available, then N95s are necessary for healthcare workers in the surgical setting where surgical smoke is predicted (7).

Self-Quiz
Ask Yourself...
- What are the two categories of the other HAZMATs?
- Name three symptoms of exposure to nitrous oxide.
- Name three symptoms of exposure to surgical smoke.
- Name two exposure prevention techniques for nitrous oxide or surgical smoke.
Occupational Safety and Health Administration (OSHA)
The Occupational Safety and Health Administration (OSHA) is an agency of the United States Department of Labor. This agency was created in 1970 to improve safety and healthy working conditions in various workplace settings. OSHA accomplishes this goal through proper training, outreach, education and assistance. OSHA is particularly important to the healthcare industry related to exposure of bloodborne pathogens, patient handling, and use of medical resources (4).
While there are multiple standards or regulations within OSHA guidelines, several apply directly to the healthcare field. Two standards of OSHA that apply directly to the use of hazardous materials:
- Hazard Communication Standard
- Personal Protective Equipment
Hazard Communication Standard
The Hazard Communication Standard (HCS) was developed by OSHA to regulate disclosure of any workplace hazards, including dangers associated with exposure to chemicals. OSHA’s Hazard Communication Standard aligns closely with the Globally Harmonized System (GHS), a globally accepted labeling standard for the same purpose. Both the Hazard Communication Standard and the GHS have defined rules for manufacturers, importers, and employers to properly label hazards. Furthermore, employers must provide Safety Data Sheets (SDS) for each chemical stored or used within the workplace.
The SDS covers sixteen items including (1):
- Identification
- Hazard identification
- Composition or ingredients
- First-aid measures
- Firefighting measures
- Accidental release measures
- Handling and storage
- Exposure controls and personal protection
- Physical and chemical properties
- Stability and reactivity
- Toxicological information
- Ecological information
- Disposal considerations
- Transport information
- Regulatory information
- Other information
Lastly, the Hazard Communication Standard dictates the need to communicate exposure to harmful chemicals, both with appropriate signage and pertinent information (5). To aid in this signage, OSHA has developed the HCS Pictograms and Hazards [see Figure 1].
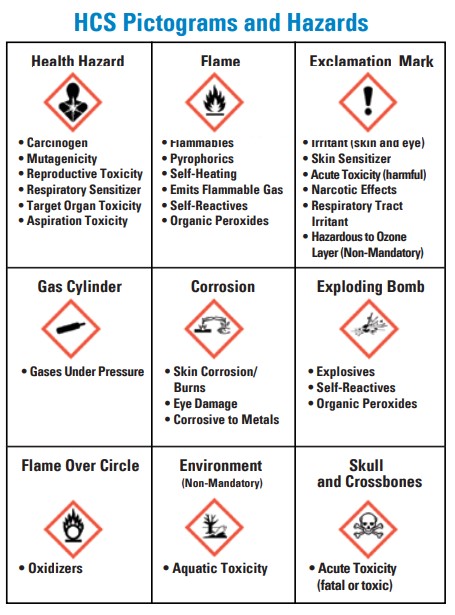
Figure 1. HCS Pictograms and Hazards (5)

Self-Quiz
Ask Yourself...
- What does OSHA stand for?
- Why was OSHA created?
- What do Safety Data Sheets include?
- What was the Hazard Communication Standard developed for?
- What is the purpose of HCS Pictograms?
Personal Protective Equipment
The Personal Protective Equipment (PPE) Standard is regulated by the Centers for Disease Control (CDC) and OSHA. This standard dictates the availability, application, and disposal of PPE by healthcare organizations. This standard is essential for healthcare systems to protect patients and employees accordingly (3).
Types of PPE
- Various type of Personal Protective Equipment (PPE) include (3):
- Gown
- Gloves
- Masks
- Respirators
- Face shields (or goggles)
- Types of Precautions
Application and Removal of PPE
The application, or donning, and removal, or doffing, of Personal Protective Equipment (PPE) must be completed in a specific order to reduce the spread of pathogens and communicable diseases:
- Donning of PPE should take place outside of patient’s room:
- Gown
- Mask or respirator
- Eye protection
- Gloves
- Doffing of PPE should take place outside of patient’s room:
- Gloves
- Eye protection
- Gown
- Mask or respirator
Chemical and Nuclear PPE
Beyond the traditional Personal Protective Equipment (PPE), there is also chemical and nuclear PPE. This is utilized for special circumstances where hazardous chemicals or nuclear exposure is possible. The HAZMAT equipment has four different types, categorized by level of exposure. Depending on the level identified, the HAZMAT equipment changes to protect the individual accordingly (6).
HAZMAT equipment (6):
- Level A:
- Positive pressure full face-piece SCBA (self-contained breathing apparatus)
- Encapsulating covering chemical protective suit
- Chemical-resistant outer gloves
- Chemical-resistant inner gloves
- Chemical-resistant boots with steel toe
- Disposable protective suit/gloves/boots
- Level B:
- Positive pressure full face-piece SCBA
- Chemical-resistant clothes with hood
- Chemical-resistant outer gloves
- Chemical-resistant inner gloves
- Chemical-resistant boots with steel toe
- Level C:
- Air purifying respirator
- Chemical-resistant clothes with hood
- Chemical-resistant outer gloves
- Chemical-resistant inner gloves
- Chemical-resistant boots with steel toe
- Level D:
- Gloves
- Coveralls
- Chemical-resistant boots/shoes with steel toe
- Safety glasses or chemical splash goggles

Self-Quiz
Ask Yourself...
- What are the four categories of HAZMATs PPE?
- When are HAZMATs PPE needed?
Conclusion
Hazardous materials, or sometimes referenced to as HAZMAT, are a group of chemicals or radioactive substances that can cause harm to the individual and/or environment upon exposure. Exposure to hazardous materials can happen for a variety of reasons, including inadvertent transportation incidents, or intentional exposure such as terrorist attacks (7). Nurses may assist in treating the community when either of these incidents occur. However, the more common exposure to hazardous materials will be work-related. By following recommendations outlined by The Occupational and Health Administration (OSHA) department, proper use of Personal Protective Equipment, accurate training in the workplace, and annual skills checks, nurses and other healthcare professionals can protect themselves, patients, and others in the hospital setting from unnecessary exposure to hazardous chemicals.
References + Disclaimer
- Brainard, J. (2022, December 1). Everything you need to know about safety data sheets. Occupational Health & Safety. https://ohsonline.com/articles/2022/12/01/everything-you-need-to-know.aspx
- CDC. (2023, July 6). Health Care Workers: Chemical hazards. Centers for Disease Control and Prevention. https://www.cdc.gov/niosh/topics/healthcare/chemical.html
- Kening, M. Z. (2023, February 22). Personal Protective Equipment. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK589639/
- Patel, R. H. (2023, May 1). Occupational Safety and Health Administration rules that affect healthcare. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK559327/
- Protective Insurance. (2021, July 27). OSHA Update: Hazard communication Standard Pictogram. https://www.protectiveinsurance.com/blog/blog-post/blog/2021/07/27/osha-update-hazard-communication-standard-pictogram
- Tupper, C. (2022, October 5). OSHA chemical hazards and communication. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK580552/
- US Department of Commerce, N. O. and A. A. (2021, March 5). What does hazmat stand for?. What Does HAZMAT Stand For? https://oceanservice.noaa.gov/facts/hazmat.html#:~:text=HAZMAT%20is%20an%20abbreviation%20for%20%E2%80%9Chazardous%20materials%E2%80%9D%E2%80%94substances%20in,%2C%20chemical%2C%20and%20radiological%20agents
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
