Course
Complex Regional Pain Syndrome (CRPS)
Course Highlights
- In this Complex Regional Pain Syndrome (CRPS) course, we will learn about the common clinical presentations, including severe health outcomes, of CRPS.
- You’ll also learn about educational strategies for pain management and alternatives to medication pain management options.
- You’ll leave this course with a broader understanding of pain management techniques for specific patient populations and the recommendations for pain management techniques and monitoring in outpatient, non-emergent settings.
About
Contact Hours Awarded: 3
Author: Sadia A, MPH, MSN, WHNP-BC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
When hearing about pain management and pain syndromes, what comes to mind? What do you think of when caring for a patient with complex pain management needs? If you’re a nurse, you’ve definitely encountered patients in pain and those with severe pain complications. Patients seek guidance and information on various health topics from nurses, including pain management.
The information in this course will serve as a valuable resource for nurses of all specialties, education levels, and backgrounds to learn more about a common pain complication – complex regional pain syndrome (CRPS).
Defining complex regional pain syndrome (CRPS)
Complex regional pain syndrome (CRPS), also known as chronic regional pain syndrome, is a common chronic neuropathic pain condition that affects millions of people nationwide. CRPS has been studied for the past few centuries and has gained more public and medical attention over the past few decades due to advances in health care, particularly in pain management. CRPS is typically defined into two categories:
Type 1 and Type 2. Type 1 CRPS, also known as reflex sympathetic dystrophy, is often characterized by sensory, motor, and autonomic abnormalities or impairments without clinical evidence of nerve lesions. Clinically evident nerve lesions or complications characterize type 2 CRPS. CRPS can be further subdivided into “warm” versus “cold” and sympathetically maintained (SMP) versus sympathetically independent (SIP).
Common signs and symptoms of CRPS include nerve pain, pain that does not go away after medical interventions, possible skin changes, and motor disturbances. When considering whether a patient has CRPS, it is essential to rule out other pain or health conditions, such as epilepsy, surgical complications, or other factors. CRPS is often noted in distal limbs, such as the forearm or calf, but it can also be found in different body parts (1,2,3).
While most severe forms of CRPS are often seen in inpatient settings, many times, with the advances in technology and health care, many patients with CRPS receive follow-up care in outpatient or home care settings. Some CRPS patients never even receive inpatient care and are diagnosed with CRPS in outpatient primary care clinics. As nurses, we must understand that pain management and assessment are part of our skill set for patients from all walks of life and various settings.
Pain management for patients with CRPS can involve a variety of options, such as prescription medications, such as opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and muscle relaxers. Other patients can also receive physical therapy, occupational therapy, nerve stimulation, psychotherapy, acupuncture, and massage, depending on the extent and location of their CRPS. Pain management and care for patients with CRPS can vary depending on patient response, cost, patient health history, resources available, and medical intervention as necessary.
Specifically, CRPS is a growing concern in health care and pain management specialists. As America and the world have an increasing aging population, mobility concerns, increased risk of physical trauma, and delayed wound healing can affect how CRPS is managed in inpatient and outpatient settings. In particular, long-term care (LTC) facilities, nursing homes, and critical care units can see several patients daily with CRPS.
Staffing concerns, documentation issues, and poor provider-patient communication can lead to several cases of CRPS being undocumented, under-treated, or poorly managed, leading to decreased quality of life and poorer health outcomes for patients (1-10).
Pain management options for patients with CRPS are used in various clinical settings for different patient needs, such as pediatric oncology nursing units, intensive care units (ICUs), and rehabilitation care centers. With the rise of technology, telehealth, home health nurses, and remote patient monitoring, thousands of patients with CRPS also self-manage their care from their homes.
While many clients receiving pain management for CRPS are in inpatient settings, as the demands for home health nursing and medical interventions shift, the reality is that many clients receive pain management options for CRPS in non-clinical settings daily. Because pain management pharmacological interventions can be used for short or long durations (as little as a few days to a lifetime), it is essential to remember that medications can have severe life-threatening side effects.
Nursing care and patient monitoring must ensure that patients receive appropriate nutrition, maintain good hydration, tolerate pain management options well, and improve health and quality of life. In particular, pain management, like all other medical interventions, is not guaranteed to have the same outcome for every client’s health. Some clients can have more severe pain management complications, such as anaphylaxis, inadequate pain management response, and worsening of client health status.
Because there are several types of pharmacological and non-pharmacological pain management interventions, doses, frequencies, concentrations, and durations must all be considered in addition to the patient response and health status when assessing for response to pain management. Because of each patient’s situation, it is essential to make sure they are aware of the role of pain management in complex wound care and educated on the risks and benefits of pain management options (1-10).

CRPS Prevalence
The exact prevalence of CRPS is unknown, as several instances of CRPS are undetected and unreported. While it is estimated that there are thousands of patients with CRPS in America, it is also estimated that CRPS is more prevalent in women and among older people. Women are suspected to have CRPS at higher rates as a result of women living longer than men and as a result of the ways pain and inflammation can affect women differently compared to men.
While CRPS is more common in older people and women, anyone of any age or gender can experience CRPS, including pediatric patients as well. While pain management prescriptions are often administered by a registered nurse (RN), some states and places of work also permit licensed practical nurses (LPNs) to administer medications. Pain medications and non-pharmacological interventions can be given at home, too, depending on the type of intervention, patient condition, and home health nurse availability.
In addition, for many patients, caregivers, such as a family member or spouse, can help monitor someone’s health with CRPS. It is important to note that many people with CRPS who do not have access to health care can self-manage their symptoms with at-home care, over-the-counter (OTC) pain medications, and rest, which can also cause discrepancies in true prevalence in various inpatient and outpatient settings (1-10).
What Causes People to Have CRPS?
Patients can have CRPS for various reasons, such as accidents, natural disasters, surgical complications, prolonged immobility, physical trauma, burns, gunshots, amputations, fractures, and more. CRPS often occurs as a result of tissue trauma with or without evident nerve trauma. CRPS is usually commonly noted after someone has experienced a fracture, but someone can experience CRPS as a result of being post-operative as well. More evidence also shows that genetics and inflammation markers may play a role in the extent and likelihood of developing CRPS, but further research is needed.
Immunological changes occurring from trauma, nerve changes, and nerve dysregulation can also influence the possibility of developing CRPS. While no single cause can trigger CRPS, CRPS is thought to have a multifactorial etiology of immunological, inflammatory, genetic, and trauma responses and influences. CRPS rarely emerges overnight, as it is a chronic, pervasive condition often a result of several factors influencing someone’s trauma, health, and overall immune system. For instance, a healthy male adult with no health conditions could experience a severe burn from a kitchen fire and require intensive hearing for their left forearm.
After a few months, they are not responding to typical pain interventions for their left forearm and see a pain management specialist who diagnoses them with CRPS. This patient now has a chronic pain condition as a result of physical trauma and is now receiving physical therapy and pharmacotherapy to have an improved quality of life (1-10).
On the other hand, another patient could be a geriatric female adult with type II diabetes who has had hip replacement surgery. This patient has been immobile for some time after the surgery, and as they begin their recovery process, they notice changes in their proper leg mobility and function. Pain and surgical specialists diagnose this patient with CRPS, and this patient is left to manage their pain in outpatient care settings as a result of changes in insurance.
Since many factors can cause the development of CRPS, taking a detailed health history and performing a thorough health assessment on patients is essential to excellent nursing care and for adequate pain management intervention (1,2,3,5,6,11,12,13).
What Are the Various Pain Management Options for CRPS?
There is no cure or definitive measure to manage CRPS, as treatment and management can vary depending on clinical presentation and patient health history. Several medications are approved by the Food and Drug Administration (FDA) to manage pain. Opioid medications are often among the first line for pain management, but not for people with CRPS as a result of impaired pain management and increased risk for opioid dependency.
As a result, careful patient monitoring and education are essential when administering opioids. While some studies recommend using opioid medications for CRPS, other evidence suggests that opioid medication might not be as effective for pain management for patients with CRPS, depending on the severity of CRPS. Bisphosphonates, antidepressants, and anticonvulsants can be used as well. Medical interventions, such as nerve blocks and stimulation, can also be considered.
Other pain medication options can include NSAIDs, such as ibuprofen, naproxen, or acetaminophen. While these medications are not as potent as opioids, titrating dosages, frequencies, and concentrations can be offered. Many times, NSAIDs, opioids, and other pain medications, such as muscle relaxers, can be administered together to manage pain, as severe and chronic pain can have devasting effects on a patient’s quality of life (1-18).
Non-pharmacological interventions for pain management for patients with CRPS can include music therapy, occupational therapy, physical therapy, talk therapy, acupuncture, massage, social support, rest, and adequate hydration and nutrition intake. While pain management is something to consider, the realities of polypharmacy, pre-existing health conditions, and the role of education for caregivers and patients are factors to consider.
Review your patient’s needs, allergies, facility protocols, condition, medication history, and overall progress when caring for a patient with CRPS. While acupuncture is often not done in inpatient settings, several patients report decreased pain when using acupuncture in outpatient settings. Social support can also play a role in pain management and wound healing (1-18).

How and Where Are Pain Management Options for CRPS Used?
As mentioned above, CRPS management is found throughout several inpatient and outpatient settings. While many people can initially start using pain management in an acute care setting, many times, patients can also begin to use pain management options in an outpatient setting after clinical evaluation or until they can access further specialized care. Pain management options can be used whenever someone can access pain management options, such as OTC medications, rest, hydration, and social support. Prescription and more advanced pain management options, such as physical therapy and nerve stimulation, are available in inpatient settings. When administering any medication, the patient should be carefully monitored for any urgent side effects or allergic reactions.
After administering medications, nurses should perform pain and wound assessments to monitor for response to therapy. Everyone’s response to pain management can vary, so that is something to remember. With the rise of home health and telehealth interventions, many patients can receive CRPS care in an inpatient setting and then be transferred to care with an outpatient pain management specialist or primary care provider. Because of the growing prevalence of at-home nursing care and pain management outside of clinical settings, it is essential to remember the role of patient education and nursing care in CRPS management (1-18).
What is the Clinical criteria for CRPS?
There are no set clinical criteria for diagnosing or managing CRPS, as it is a chronic health condition with much research but few defined answers. Clinical criteria for CRPS often depend on the patient’s clinical presentation and health history. CRPS is usually diagnosed after ruling out other possible causes, such as surgical complications or another nerve condition like multiple sclerosis. Historically and presently, for a patient to be diagnosed with CRPS, the patient should have at least one symptom related to three of the four categories: sensory, vasomotor, sudomotor, or motor.
Patients must also display at least one visible possible complication of CRPS, such as hyperalgesia, skin changes, temperature changes, tremors, or the like. CRPS is often a diagnosis of exclusion after all other possible conditions have been ruled out, making this diagnosis usually a long, lengthy process for many patients.
Overall, clinician judgment and patient response should guide pain management, as pain management is often used for various clinical indications and varied durations. Consultations with neurologists, pain management specialists, therapists, and other specialists can also be considered for pain management for patients with suspected CRPS (1-18).
What is the Average Cost for CRPS Management?
The cost of pain management options for CRPS can significantly vary depending on the type of pain medication administered, concentration, dosage, frequency, patient age, insurance, duration, and other factors. Pain management is often an expensive and lengthy medical intervention. Still, for many patients, it is essential care and possibly the only way for some patients to improve their health and quality of life, given their health situation.
Cost is a leading reason many patients cannot maintain their medication and healthcare regime, especially if pharmacological and non-pharmacological pain management options are recommended in an outpatient setting. If cost concerns your patient, consider contacting your local patient care teams to find cost-effective solutions (1,12,19).
How Can Patients Self-Manage CRPS?
Depending on the nature and extent of CRPS, many patients might consider self-managing suspected CRPS well before accessing health care services. However, patients might have been receiving care for CRPS, be discharged from a facility, and be left to self-manage their care at their own discretion. Because of the varied situations people living with CRPS are in, patients can self-manage their complex wounds with prescribed pain medications, non-pharmacological interventions, or OTC medications.
While patients in acute settings monitored by nurses and other health care professionals do not need to self-manage their responses to pain management therapy, patients can be aware of possible pain management complications regardless of their setting. Patients can be mindful of possible symptoms to alert for medical attention, such as trouble breathing, chest pain, facial pain, confusion, headache, and fatigue.
Caregivers or loved ones can be aware of pain medication administration, benefits, and risks. Common ways for patients receiving pain management for CRPS to self-manage themselves include having access to medical care in the event of increased pain, having follow-up appointments scheduled with their pain management team, and having a support system (1-18).
What Happens to Patients Who Do Not Have Access to Care for CRPS?
Patients who do not receive adequate pain management for their CRPS might experience a decline in their health or progression of more health complications. Truthfully, if someone is experiencing CRPS without proper management, this can lead to an increased likelihood of delayed wound healing, depression, loss of income, decreased quality of life, and more. CRPS can affect people in different ways and affect different limbs, causing this condition to severely influence the quality of life for several people.
For instance, a patient with CRPS who has CRPS in their left leg might not be able to work as much or at all as a result of the unmanaged pain, leading to decreased income and decreased quality of life. Another patient with CRPS in their left forearm can have difficulty cooking, going to the bathroom, and cleaning, causing a strain in their daily activities. As a result, it is essential to educate patients on the importance of consistency in their treatment regime and the risks and benefits of being on pain management for CRPS in addition to prompt, evidence-based treatment (1-19).

Self-Quiz
Ask Yourself...
- What are some possible complications of CRPS?
- What are some possible complications of pain management options?
- What are some possible ways cost can influence access to pain management?
- How has pain management evolved over the past few decades?
- How do you see pain management done in your place of work?
CRPS’ Special Considerations for Specific Patient Populations
Given the wide range of pain management and CRPS in various patient populations, special considerations are made for patients of certain age groups or with certain health conditions.
CRPS Considerations in Pediatric Populations:
Pain management among pediatric patients is becoming increasingly common in pediatric care across America. While CRPS is often diagnosed and seen in women and elderly populations, anyone can experience CRPS, including children. CRPS in this population can pose a serious risk to someone’s quality of life, educational accessibility, ability to care (or learn to care) for oneself, and more. From toddlers to adolescents, pediatric patients have their own unique set of pain management and CRPS needs.
For instance, burns, physical trauma, gunshots, prolonged immobility, nerve damage, and more can affect the pediatric population, causing many healthcare providers and caregivers to wonder about the next steps for pain management in this population. For instance, a toddler experienced a fracture in their right femur six months ago. After several consults with the pediatrician, the pediatrician referred this patient to a pediatric pain management specialist, where it was determined that the child had CRPS after several tests were performed.
Another example of a pediatric patient with CRPS is an adolescent patient who survived after being burned on their right arm. This patient has tried several therapies and medications with little to no pain relief, causing the pediatrician to refer this patient to a pain management specialist, where they were diagnosed with CRPS (1-18,20,21,22).
Weight, dosing, frequency, cost, accessibility, and patient and caregiver education are all factors to consider when considering pain management options in this population. In addition, CRPS can significantly depend on the overall health of the patient, any pre-existing health conditions, and pain severity. While there are several stances and guidelines on pain management and wound care for pediatric populations, there is still much discrepancy among consistent guidelines and evidence-based research on its usage and effectiveness in this population, especially regarding CRPS.
Educating parents, caregivers, and family members about pain management is essential, especially if treatment and monitoring continue after hospital discharge. More hospitals and pediatric critical care units are exploring the long-term effects of pain management weeks after discharge to monitor for improvement and possibly delay or eliminate the need for surgery or more aggressive treatment options (1-18, 20, 21, 22).
Medication administration in pediatric patients must also be monitored carefully, as children use much smaller doses, concentrations, needle sizes, infusion pumps, and vital sign parameters. Unlike adult populations, children might not be able to verbalize their pain or comfort levels during medical interventions. Despite this, comfort measures and pain medication can be offered and administered, such as play therapy, music therapy, talk therapy, and other non-pharmacological interventions.
Taking the time to educate and inform parents about these interventions is essential. Because of the differences in organ development and acute monitoring needed for pain management for CRPS in pediatric patients, this unique population requires a good eye for detail, clear documentation, and excellent patient care. It is also essential to ensure that patients are progressing on their care plans, which can involve a variety of care options, such as nerve stimulation, therapies, and medical appointments (1-18,20,21,22).

Self-Quiz
Ask Yourself...
- How can CRPS affect pediatric physical and psychosocial development?
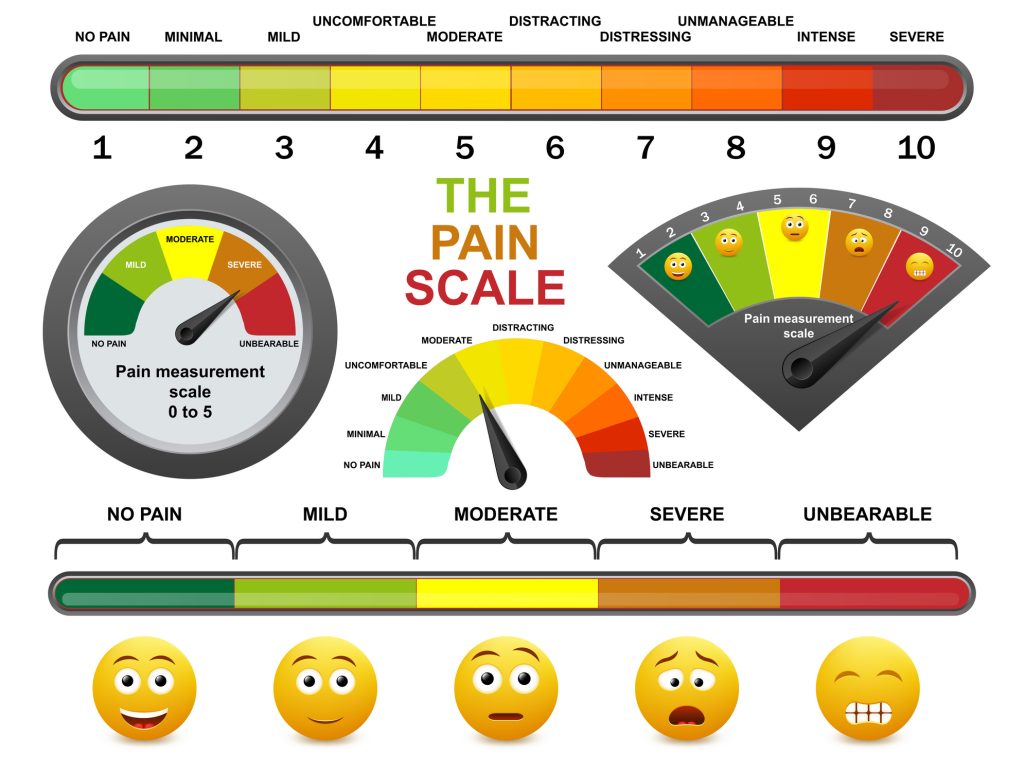
- How would you assess pain in a pediatric patient compared to an adult patient?
- How can non-pharmacological interventions vary among pediatric patients compared to adults?
CRPS Considerations in Geriatric Populations
The geriatric population is one of the largest growing patient populations in America and continues to increase with the rise of America’s aging population. In addition, the geriatric population is the most likely to experience CRPS. Elderly patients have several factors that could contribute to the likelihood of developing CRPS, such as their immunocompromised status, often complex medical history, increased risk of falls and physical injury, increased risk of surgeries, and medication use.
Because of their decreased skin integrity, possible increased mobility issues, and polypharmacy concerns, pain management for CRPS in the geriatric population is a growing concern in health and among evidence-based research guidelines. CRPS in this population can pose a serious risk to someone’s quality of life, income, ability to care for oneself, and more.
While several guidelines for pain management among the geriatric population exist, much discussion remains about the role of CRPS management. CRPS has several inconsistencies, often leaving providers at their clinical discretion based on resources and patient situations. For instance, an 84-year-old patient might be admitted to the surgical unit for a knee replacement.
Months after surgery, this patient is reporting pain in their calf with no symptom relief, going from doctor to doctor, and being unable to drive anymore. Another patient might be 75 years old and experienced a car accident. While the accident was months ago, this patient is having sweating and pain in their left forearm that is not going away, despite medication intervention, leading to their inability to use the bathroom on their own or maintain their own home independently. Like all other patients, patients must be assessed before pain management is used to determine the need, extent, duration, frequency, dosage, and strength (1-18,23-30).


Self-Quiz
Ask Yourself...
- How can CRPS affect geriatric physical and psychosocial quality of life?
- How would you assess for pain in a patient after surgery?
- How can non-pharmacological interventions vary among geriatric patients compared to adults?
The Role of Telemonitoring in Inpatient and Outpatient Care for Patients with CRPS
With the rise of at-home patient care, telehealth, and remote patient monitoring, several patients receive pain management for their CRPS. While telemonitoring has expanded significantly in the past decade due to the rise of telehealth nursing, technological advances, and more widespread insurance and Internet coverage, making sure patients know the risks and benefits of pain management options and complications from CRPS is essential to nursing care.
While patients receiving pain management should routinely seek advice and guidance from their medical care provider, many times, patients and caregivers can self-monitor their reactions to medical interventions for emergent complications or inadequate treatment resolution. Patients should be aware that they should tell the nurse immediately if they suspect any complications with their pain management plan, such as trouble breathing, increased pain or discomfort, or chest pain.
Even though there are many possible complications from pharmacological pain management options, many patients report high satisfaction with remote monitoring, such as more independence in their daily activities and less time in transit to medical appointments. Furthermore, many therapies, nerve stimulation, and other non-pharmacological pain management options can be done in outpatient settings or at home (1,2,3,6,29,30).

Self-Quiz
Ask Yourself...
- How would you assess a patient’s knowledge of at-home pain management options?
- How would you assess the caregiver’s knowledge of CRPS management?
- What are some of your facility’s protocols for pain management documentation?
Nursing Considerations
What Is the Nurses’ Role in CRPS Education and Management?
Nurses remain the most trusted profession for a reason. They are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for nurses’ role in pain management or CRPS patient education, here are some suggestions to provide quality care for patients receiving pain management for their complex wounds (1,2,3,4,11,12,13,15,27,28,29,30).
- Take a detailed health history of the patient. Vital signs and history-taking can be complex, especially in acute settings. Pain management is often initiated in acute settings and then transitioned to home use or less-acute settings. As nurses, it is essential to be involved in the vital signs and history-taking process to learn about noticing any abnormalities or medical concerns that warrant medical attention. Also, it is necessary to assess the patient for any skin changes or mobility concerns that can increase the possible risk of CRPS development. If a patient is complaining of symptoms that could be related to CRPS, such as burning of the skin, numbness, or pain in one area, inquire more about that complaint.
- Ask the patient if they have allergies, especially to certain adhesives or medications. Pain medications can be derived from various sources, making them possible to trigger an allergic reaction. Monitor their skin integrity and breathing for any changes as well.
- Educate the patient and caregivers on pain medication administration and non-pharmacological interventions. Educate the patient to inform the nurse of any redness, pain, or swelling. Take time to answer any questions about the therapies and confirm the orders.
- Regardless of how long a client has been receiving treatment, if the client complains of any new symptom, ask how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates them. If you feel like other healthcare professionals are not taking a patient’s complaint seriously, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Oftentimes, in busy clinical settings, reviewing health records can be overwhelming, especially for patients with a complex medical history. Several patients taking pain medications have a complex medical history. Millions of people take medications for various reasons, and people’s medication histories can look similar over time. Ask each patient about how they are feeling on the medication, how they are feeling with their wound, if their symptoms are improving, and if there are any changes to medication history.
- Be willing to answer questions about CRPS and pain management. Many people do not know about the side effects, risk factors to be aware of, and lifestyle changes that can influence outpatient care and wound healing. Be willing to be honest with yourself about your comfort level, discuss topics, and provide education on pain medication and complex wound care.
- Communicate the care plan to other staff involved for continuity of care. For several patients, especially patients with CRPS, care often consists of a team of nurses, specialists, pharmacies, caregivers, and more. Ensure that patients’ records are up to date for ease in record sharing and continuity of care.
- Stay current on continuing education related to CRPS and pain management, as evidence-based information is constantly evolving. You can then present your new learnings and findings to other healthcare professionals and educate your patients with the latest information.

Self-Quiz
Ask Yourself...
- What are some ways nurses can obtain a detailed health history?
- What health factors can influence someone’s responses to pain management interventions?
- If a patient developed an allergic reaction to the pain medication, how would you handle that situation?
How can nurses identify if someone needs more intervention for their pain management?
Unfortunately, it is not possible to look at someone with the naked eye and determine if they are receiving pain medications or have CRPS. For many patients, CRPS can occur in a distal limb, and those limbs can be covered with clothing and not visible upon initial assessment. While some might have notable complications, such as oozing sweat onto their clothing or sheets, trouble breathing, or sharp headaches, the most common presentation for CRSP or pain management complications varies widely.
In addition, nurses can answer questions and concerns regarding CRPS and pain management for patients and their caregivers. Nurses can provide quality care by completing health history, listening to patients’ problems, addressing caregivers’ concerns, and administering pain medication (1,2,3,25,26,27,28,29,30).
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors)
- Tell the health care provider of any existing lifestyle concerns, such as alcohol use, other drug use, sleep habits, diet, surgical history, and allergies (need to identify lifestyle factors that can influence the likelihood of developing CRPS and medication and other medical interventions)
- Tell the health care provider if you have any changes to your body, such as pain with breathing, trouble with movement, changes in urinary habits, changes in bowel habits, changes in sleep habits, or increased fatigue (potential systemic pain management complication symptoms)
- Tell the nurse or health care provider if you experience any pain that becomes increasingly severe or interferes with your quality of life, especially if the pain or discomfort is near a distal limb.
- Keep track of your health, medication use, machine function, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries.
- Tell the provider about any interventions or medications you have tried previously, including OTC medications.
- Tell the health care provider if you notice any changes while receiving pain management therapy (potential worsening or improving health situation)

Self-Quiz
Ask Yourself...
- How can patients and their caregivers keep track of their responses to pain management therapy?
- How can caregivers affect a patient’s health history?
- If a patient tells you they do not have consistent insurance coverage for pain management, how would you manage the conversation and provide the next steps?
Research Findings
What Research on CRPS exists Presently?
Extensive, publicly available literature on pain management and complex wound care is available through the National Institutes of Health (NIH) and other evidence-based journals.
What are some ways for people who have experienced CRPS to become a part of research?
Patients interested in participating in clinical trial research can seek more information on clinical trials from local universities and healthcare organizations.

Self-Quiz
Ask Yourself...
- Why would someone want to enroll in clinical trials?
- What are some latest trends you have seen in CRPS throughout your nursing career?
- How has the way you have managed pain management complications in your nursing career changed?
Conclusion
CRPS is a complex chronic pain condition that affects thousands of people daily. Using pain management options to assist with CRPS often requires extensive medical care, several visits, and constant follow-up. While pain management options can be life-saving for many patients, because of the risks, a serious overview of risks and benefits must be considered prior to starting pain management. Education and awareness of different pain management options and ways to manage CRPS can influence many people’s lives in a healthy way.
Case Study #1
Wendy is a single mom to an 8-year-old living in a major US city. She works as an accountant, and her child, Brittany, is in the third grade. Wendy received a call from the elementary school that Brittany had fallen down while playing soccer and possibly fractured her leg. Wendy heads to the local hospital and sees that Brittany is very emotional, upset, and crying and wants to speak to her mom immediately.
Examination at the hospital shows that Brittany fractured her tibia in her left leg. Wendy is educated that Brittany will need to be in a cast for some time, given some medications, and might need some physical therapy afterward. Wendy wants to know if this will affect Brittany in the long term and if there is anything else she needs to do. The hospital staff reassured her that the tibia could be healed in an outpatient setting and that she should follow up with the pediatrician and a pediatric orthopedic specialist. Brittany says she is in pain, and she would like to rest and then go home where it is quiet.

Self-Quiz
Ask Yourself...
- What specific questions would you want to ask Wendy about Bob’s health?
- What are some health history questions you’d want to highlight?
- How would you perform an initial assessment on this patient?
- How would a nurse educate a parent in the hospital about fractures and pain management options for a young child?
- How would a nurse educate a parent on pain management in an 8-year-old?
- What are some contraindications for pain medications in a pediatric patient?
- What are some ways to assess wound healing in children?
- How can rest influence wound healing?
Case Study #1 Continued
Brittany was discharged from the hospital, and she is recovering at home. After a few months, the cast was removed, and Brittany is following up with the pediatrician and her mom. Brittany says she feels her left leg is in much pain and has trouble standing.
Wendy is concerned since Brittany has never talked about being in pain like this before, and she would like a second opinion. The pediatrician refers Brittany to the pediatric orthopedic specialist, and they ask Brittany some questions. The pediatric orthopedic specialist assigns Brittany to a nurse manager for further care instructions.
Brittany and Wendy leave the pediatric orthopedic specialist’s office with referrals to an occupational therapist, physical therapist, child psychologist, and pediatric pain management specialist. Wendy is overwhelmed with all the medical appointments and working full-time. Brittany is going to school, but she is in increasing pain and is having difficulties playing with her friends and focusing on school.
Her grades have started to slip a bit, and Wendy is considering whether she can see the pain specialist sooner. Wendy schedules an occupational therapist to visit her home, and the pediatric orthopedic specialist’s nurse manager calls to assess Brittany’s progress.
Brittany has been in occupational therapy for two months and saw the child psychologist once. She has been unable to visit the physical therapist because of insurance issues. Brittany has a follow-up with the pediatric pain management specialist because the pain is not going away. Upon examination, Brittany’s left leg is sweating more than her right leg, and she is reporting more pain in the left leg than the right leg. Brittany states that the therapy is helpful, but she is still in pain and wants her life to go back to normal.
Brittany states that summer break is in a few weeks, and she wants to enjoy time with her friends more. The pediatric pain management specialist asks Brittany and Wendy some more questions. The specialist notes that Brittany’s left leg is more sensitive to touch, has more weakness than the other leg, and is sweating more than the other leg. The specialist reviews Brittany’s chart, labs, exams, and documents and diagnoses Brittany with CRPS. Wendy starts to cry and wants to know more about this condition.

Self-Quiz
Ask Yourself...
- How would you assess for pain management needs in an 8-year-old?
- What exams or tests would be recommended for Brittany now?
- What non-pharmacological interventions would be recommended here?
- What pharmacological interventions can be recommended here?
- How would you monitor this patient for an allergic reaction to medication?
- What are some complications from unmanaged pain in children?
- How can nurses address caregiver strain and burnout?
- How can caring for a child with a disability affect a parent?
- How would you explain CRPS to an emotional parent and child in pain?
- How would you explain pain complications to a child?
- What sort of caregiver resources can you provide to Wendy?
Case Study #2
Carol is a 75-year-old widow living alone in rural America. She has hypertension and diabetes, both of which she takes regular medication for, and she sees her doctors regularly. Carol was cleaning her home earlier and hit herself by accident, leading her to injure her left arm. She went to the local emergency room, where they diagnosed her with a fractured left forearm. Carol was told to wear a cast for a few months and follow up with an orthopedic specialist and her primary care in a few months.

Self-Quiz
Ask Yourself...
- What specific questions would you want to ask about Carol’s health?
- What are some health history questions you’d want to highlight?
- How would you perform an initial assessment on this patient?
- How does cost influence someone’s ability to access healthcare services?
- How can a fracture in someone’s arm affect their quality of life and daily activities?
Case Study #2 Continued
Carol rested her arm for a few months and went to the local orthopedic specialist to remove her cast. The orthopedic specialist asked if she was doing well, and Carol said that she still had some pain and numbness. The orthopedic specialist gave her a prescription for opioids to take as needed and recommended OTC medications as well. Carol left the office, and for the past few months, the pain in her left arm has started to increase.
She also notices having trouble holding onto the steering wheel more often. Her left arm is also beginning to have some skin changes, but Carol thinks that is because of her age. Carol takes the opioid medications more often now, and she has her annual follow-up with her primary care provider.
Carol sees her primary care provider (PCP), and her lab work is done by the PCP every day. Her diabetes and hypertension are still well-managed with medications, and she is having no issues with her blood sugar or blood pressure readings presently. The PCP refers Carol to a pain management specialist regarding her left arm, but the closest one is five hours away.
The pain management specialist is also unavailable for three months for a new patient. The PCP writes another prescription for opioids for a few days and recommends OTC medications. The PCP also recommends possible physical therapy, but Carol’s insurance does not want to cover the physical therapy without further diagnosis.
Carol is doing her best to maintain her independence, but her left arm pain and sensations are getting worse. Carol has to ask her neighbor to help keep her garden and is considering taking more OTC medication to help with the pain.
Carol sees the pain management specialist after waiting for three months. She had to skip her monthly book club meeting to make it to this appointment, which is five hours away, and she wonders if she will be OK driving home in the dark by the time the appointment is over. Carol has no children living nearby and hopes the pain management specialist can help her return to normal.
The pain management specialist refers Carol to an occupational therapist, physical therapist, and psychologist, all of whom can be seen online. Carol is overwhelmed by the medical appointments and possible situation costs. She is also assigned to a nurse case manager at the pain management practice and hopes these interventions work.
She tells the pain management specialist that she also wants to continue medication if it can help as well. Nine months after the initial fracture in her left arm, Carol sees the pain management specialist virtually, and she is diagnosed with CRPS since the pain medication is not helping as much as it used to. Carol wonders if she can continue to live alone since the pain is not getting better, even with the therapies.

Self-Quiz
Ask Yourself...
- How can opioid medications influence motor function?
- How can OTC pain medications affect pain sensation?
- What are some possible signs of CRPS Carol is exhibiting?
- What ways can the primary care provider assess for pain?
- How would a nurse educate on pain management in a 75-year-old patient?
- How does living in a rural area affect access to care?
- What are some barriers to care Carol is currently experiencing?
- How can OTC pain medications interfere with blood pressure and diabetic management medications?
- What are some complications from unmanaged pain in older people?
- How can remote telehealth services influence the lives of patients in rural areas?
- What exams can be done to assess for pain management complications in this patient?
- How would a psychologist help with pain management in this patient?
- What would be your next steps as a nurse with this patient?
References + Disclaimer
- https://www.ncbi.nlm.nih.gov/books/NBK430719/
- Sobeeh, M.G. et al. Pain mechanisms in complex regional pain syndrome: a systematic review and meta-analysis of quantitative sensory testing outcomes. J Orthop Surg Res 18, 2 (2023). https://doi.org/10.1186/s13018-022-03461-2
- Taylor, SS., et al. Complex Regional Pain Syndrome: A Comprehensive Review. Pain Ther 10, 875–892 (2021). https://doi.org/10.1007/s40122-021-00279-4
- Mesaroli, G et al. Screening and diagnostic tools for complex regional pain syndrome: a systematic review. PAIN 162(5):p 1295-1304, May 2021. | DOI: 10.1097/j.pain.0000000000002146
- Melf-Marzi A, Böhringer B, Wiehle M, Hausteiner-Wiehle C. Modern Principles of Diagnosis and Treatment in Complex Regional Pain Syndrome. Dtsch Arztebl Int. 2022;119(51-52):879-886. doi:10.3238/arztebl.m2022.0358
- Wie, C., et al. Interventional Modalities to Treat Complex Regional Pain Syndrome. Curr Pain Headache Rep 25, 10 (2021). https://doi.org/10.1007/s11916-020-00904-5
- Wen, B., et al. (2023). The Role of Neuroinflammation in Complex Regional Pain Syndrome: A Comprehensive Review. Journal of Pain Research, 16, 3061–3073. https://doi.org/10.2147/JPR.S423733
- Farzad, M., et al. (2021). Factors associated with disability and pain intensity in patients with complex regional pain syndrome. Disability and Rehabilitation, 44(26), 8243–8251. https://doi.org/10.1080/09638288.2021.2009045
- Cutts S, et al. Complex regional pain syndrome: an evolving perspective, Postgraduate Medical Journal, 2021, 97(1146):250–255, https://doi.org/10.1136/postgradmedj-2020-137808
- Harden R, et al. Complex Regional Pain Syndrome: Practical Diagnostic and Treatment Guidelines, 5th Edition, Pain Medicine, 2022, 23,S1–S53 https://doi.org/10.1093/pm/pnac046
- Prasad M, Chakravarthy M. Review of complex regional pain syndrome and the role of the neuroimmune axis. Molecular Pain. 2021;17. doi:10.1177/17448069211006617
- Sipilä R, et al. Pain catastrophizing levels differentiate between common diseases with pain: HIV, fibromyalgia, complex regional pain syndrome, and breast cancer survivors. Scandinavian Journal of Pain. 2024;24(1): 20240049. https://doi.org/10.1515/sjpain-2024-0049
- Limerick, G., et al. Complex Regional Pain Syndrome: Evidence-Based Advances in Concepts and Treatments. Curr Pain Headache Rep 27, 269–298 (2023). https://doi.org/10.1007/s11916-023-01130-5
- Ferraro MC, et al. Complex regional pain syndrome: advances in epidemiology, pathophysiology, diagnosis, and treatment. The Lancet: Neurology. 2024:23(5):522-533. DOI: 10.1016/S1474-4422(24)00076-0
- Zhou X, et al. (2024) Economic evaluation of management strategies for complex regional pain syndrome (CRPS). Front. Pharmacol. 15:1297927. doi: 10.3389/fphar.2024.1297927
- Chang C, et al. Complex regional pain syndrome – Autoimmune or functional neurologic syndrome. Journal of Translational Autoimmunity. 2021(4):100080. https://doi.org/10.1016/j.jtauto.2020.100080
- Halicka M, et al. Neuropsychological Changes in Complex Regional Pain Syndrome (CRPS). Behav Neurol. 2020;4561831. doi:10.1155/2020/4561831
- Mosquera-Moscoso J, et al. Interventional pain management of CRPS in the pediatric population: A literature review. Interventional Pain Medicine. 2024;3(4):100532. https://doi.org/10.1016/j.inpm.2024.100532
- Rohatgi KW, et al. 2021. Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. doi.org/10.3122/jabfm.2021.03.200361
- Matas OAM, et al. Pediatric complex regional pain syndrome: a review. European Psychiatry. 2022;65(S1):S477-S477. doi:10.1192/j.eurpsy.2022.1212
- Tay MC, Rider JV. Pediatric Complex Regional Pain Syndrome and Occupational Therapy Intervention: A Scoping Review. OTJR: Occupational Therapy Journal of Research. 2024;44(2):168-178. doi:10.1177/15394492231197612
- Mesaroli, G, et al. Age and Sex Differences in Pediatric Neuropathic Pain and Complex Regional Pain Syndrome: A Scoping Review. The Clinical Journal of Pain 40(7):p 428-439, 2024. | DOI: 10.1097/AJP.0000000000001217
- Charipova, K, et al. 2021. Chronic Regional Pain Syndrome in the Geriatric Patient. In: Lawson, E.F., Castellanos, J.P. (eds) Complex Regional Pain Syndrome. Springer, Cham. https://doi.org/10.1007/978-3-030-75373-3_15
- Giovannini S, et al. Neuropathic Pain in the Elderly. Diagnostics. 2021; 11(4):613. https://doi.org/10.3390/diagnostics11040613
- Mookerjee N, et al. Association of Risk Factors and Comorbidities With Chronic Pain in the Elderly Population. Journal of Primary Care & Community Health. 2024;15. doi:10.1177/21501319241233463
- Ghaly L, Bargnes V, Rahman S, Tawfik G-A, Bergese S, Caldwell W. Interventional Treatment of Complex Regional Pain Syndrome. Biomedicines. 2023; 11(8):2263. https://doi.org/10.3390/biomedicines11082263
- Harnik, M. et al. Complex Regional Pain Syndrome (CRPS) and the Value of Early Detection. Curr Pain Headache Rep 27, 417–427 (2023). https://doi.org/10.1007/s11916-023-01124-3
- Iolascon, G, et al. (2024). An update on the pharmacotherapeutic options for complex regional pain syndrome. Expert Review of Neurotherapeutics, 24(2), 177–190. https://doi.org/10.1080/14737175.2024.2307490
- Shafiee, E et al. The Effectiveness of Rehabilitation Interventions on Pain and Disability for Complex Regional Pain Syndrome: A Systematic Review and Meta-analysis. The Clinical Journal of Pain 39(2):p 91-105, February 2023. | DOI: 10.1097/AJP.0000000000001089
- Mangnus, T.J.P., Bharwani, K.D., Dirckx, M. et al. From a Symptom-Based to a Mechanism-Based Pharmacotherapeutic Treatment in Complex Regional Pain Syndrome. Drugs 82, 511–531 (2022). https://doi.org/10.1007/s40265-022-01685-4
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
