Course
Comprehensive Spinal Cord Injury Review
About
Contact Hours Awarded: 3
Course By:
Joe Brandon
BSN, RN, CRRN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
This course delves into the complex world of spinal cord injuries. The goal is to help LPNs/LVNs, RNs, and APRNs gain the knowledge and skills they need to help the client with SCI on the most basic level. The learner will explore the various stages of a SCI, from learning about the most at risks populations, epidemiology and pathophysiology to the newest treatments and rehabilitation strategies. This course aims to help the clinician to develop a deeper understanding of a SCI’s impact on individuals, families, and communities.
By the end of the course, the learner should be able to discuss the latest advances in SCI management, including stem cell therapies, epidural stimulation, and exoskeleton technologies. The course will also evaluate the newest evidence-based practices, which include both pharmacological and physical therapies. SCI is a very complex and understudied area of medicine due mainly to the fact that it’s relatively uncommon in regard to other illnesses. The funds needed to educate about the disease process and the research needed to advance in treatment options is often limited.
Introduction
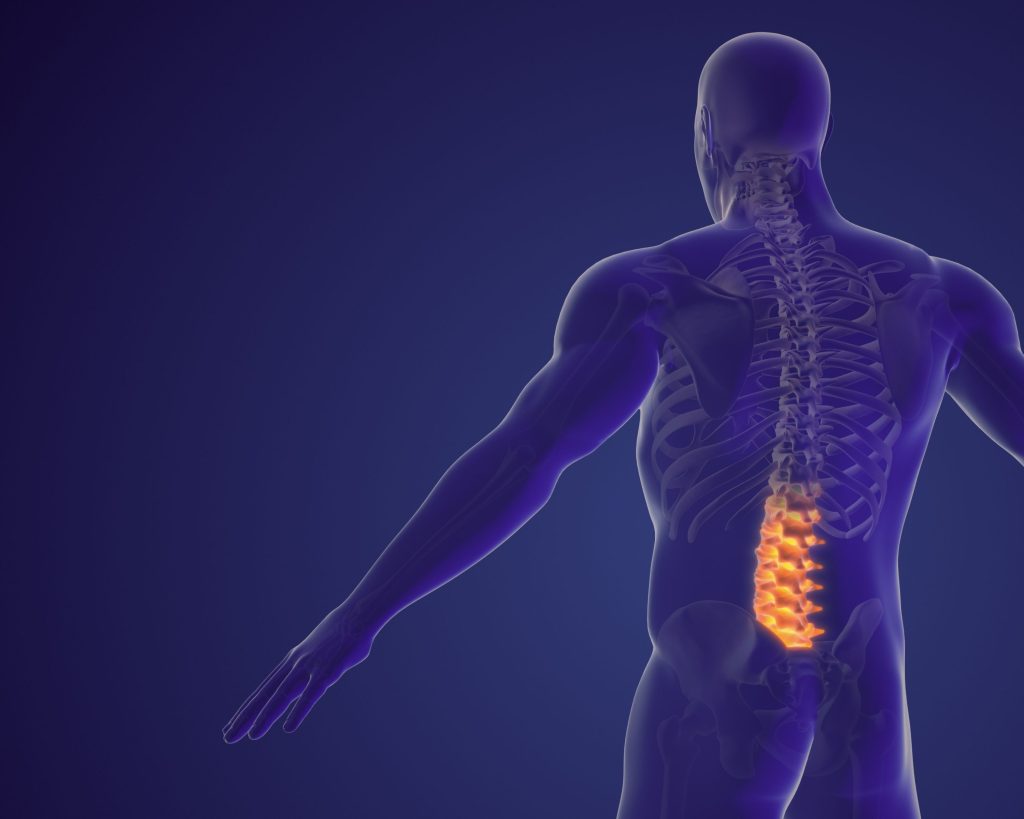
A spinal cord injury (SCI) is a serious medical condition that involves damage to the spinal cord, resulting in partial or complete loss of motor and sensory function below the level of injury (3,26). SCI can be classified into two main categories: traumatic and non-traumatic. Traumatic SCI accounts for approximately 90% of all cases and occurs when external forces, such as those sustained in motor vehicle accidents or falls, cause direct damage to the spinal cord (16). Non-traumatic SCI results from medical conditions, including cancer, spinal stenosis, infection, or vascular disorders (16).
The level of injury is also an important factor in determining the severity of SCI. Injuries that occur higher up in the spinal cord, such as those in the cervical region, can result in more severe symptoms, including quadriplegia or paralysis of all four limbs (3, 16, 26, 34). According to a study published in the Journal of Neurotrauma, the cervical spine is the most commonly injured region in traumatic SCI, accounting for approximately 55% of all injuries (4). Injuries that occur lower down in the spinal cord, such as those in the lumbar region, may result in less severe symptoms, such as weakness or numbness in the legs.
Treatment for SCI typically involves a multidisciplinary approach, including medical, surgical, and rehabilitative interventions. The primary goal of treatment is to stabilize the spine, prevent further injury, and promote reentry into the community. A study published in the Journal of Spinal Cord Medicine found that early surgical intervention can improve outcomes in clients with traumatic SCI (32). Rehabilitation, including physical therapy, occupational therapy, and speech therapy, is also an important part of the treatment process.
In addition to medical treatment, individuals with SCI may also require ongoing care and support to manage their condition. This can include assistance with daily activities, such as bathing, dressing, and feeding, as well as emotional support and counseling to cope with the psychological impact of the injury. Research has shown that psychological support can significantly improve the quality of life for individuals with SCI (26,29). Furthermore, advances in technology have improved mobility and independence for individuals with SCI, such as the use of exoskeletons and wheelchairs (11, 23)
The impact of SCI on daily life cannot be overstated. Individuals with SCI often experience significant changes in their physical abilities, social relationships, and emotional well-being. The illness also has a major impact on family members as the client often requires at least moderate care at the highest functioning level. Simple tasks, such as getting dressed or using the bathroom, can become daunting challenges. Moreover, the financial burden of SCI can be substantial, with estimated lifetime costs ranging from $1 million to $5 million (7).
Despite these challenges, many individuals with SCI lead fulfilling and productive lives. Advances in medical technology and rehabilitation strategies have improved outcomes and enhanced quality of life. Support groups and advocacy organizations also play a vital role in promoting awareness and providing resources for individuals with SCI.
The following course will examine the full spectrum of life with a spinal cord injury. An SCI is a serious medical condition that requires prompt and effective treatment. By understanding the causes, symptoms, and treatment options for SCI, individuals can make informed decisions about their care and better manage their condition and improve their overall quality of life.


Self-Quiz
Ask Yourself...
- What do you hope to learn about spinal cord injuries from this course?
- Assessing your current knowledge of spinal cord injuries, do you feel that you could properly care for someone with an SCI solely based on you currently know?
- How important is it to you to understand the client with an SCI?
- Do you think that the family’s involvement is equally as important as the client’s willingness to recover?
- What role do you feel that they may play in encouraging the client early in the recovery process?
Case Study
Alex is a 25-year-old male that sustained a spinal cord injury at the C5 level following a sports-related accident. As a result of the injury, Alex experienced a complete loss of motor and sensory function below the level of injury.
Accurate assessment of a SCI is crucial for determining prognosis and guiding treatment. The American Spinal Injury Association (ASIA) Impairment Scale (AIS) is the standard in classifying SCI severity (2). The scale grades injuries from A (complete) to E (normal). Additionally, the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) provides a comprehensive framework for assessing SCI (2). ISNCSCI evaluates sensory and motor function, as well as the presence of sacral sparing.
The ASIA Impairment Scale:
- A: No sensory or motor function in the sacral segments S4-S5
- B: Sensory function, but no motor function, in the sacral segments S4-S5
- C: Motor function is preserved below the neurological level, but more than half of key muscles have less than grade 3 strength
- D: Motor function is preserved below the neurological level, and at least half of key muscles have grade 3 or more strength
- E: Normal sensory and motor function
The initial assessment of a client with a spinal cord injury is crucial in determining their current level of functioning and identifying the most appropriate aspects of care. One of the most important aspects of caring for a client with a SCI is bowel and bladder management. The client with an SCI will often not be able to empty their bladder naturally, which is due to the lack of function in their bladder caused by what is known as a neurogenic bladder. In a neurogenic bladder, the signal that goes from the brain to the spinal cord is interrupted by the injury, resulting in the client’s body not knowing when the bladder is full and unable to let the brain know when it is time to urinate. In these clients, proper bladder management is imperative.
Often, the client will start with a urinary catheter or intermittent catheterization every four hours. Giving a bladder 4 hours before attempting to catheterize is about the average time it takes the bladder to become what is considered full, between 350-500mls. If a client goes beyond this point, then they run a risk of becoming dyslexic. Similarly, if they are not completely emptied when caught, then they can get a UTI.
In regard to emptying the bowels, clients with SCI have a couple of options. These options will be based on whether or not they have a positive or a negative bulbocavernosus reflex (BCR). If a client has a negative BCR, it is suggested that they have digital stimulation to empty their bowels. If they have a positive BCR, then a rectal suppository is often used to encourage the intestines to begin movement and expel any stool in the large and small intestines to be excreted. If the client’s bowels do not move, this can also lead to the client becoming dysreflexic or to having an involuntary bowel movement unplanned during the client’s day.
Clients with SCI who have a neurogenic bladder are at risk of developing urinary tract infections (UTIs) due to incomplete emptying of the bladder (5).
Current research has shown that early and intensive rehabilitation interventions can improve bowel and bladder function in clients with SCI as well as improve future outcomes. Clients who received early and intensive rehabilitation interventions experienced functional recovery and reduced disability [3]. There was also a study published in Cureus, the Journal of Medical Science, found that clients with a SCI who that maintained a bowel management program experienced improved bowel function and reduced risk of bowel incontinence and better satisfaction in daily life (15).
To provide effective care, healthcare professionals must understand the complexities of bowel and bladder management in clients with SCI. This includes understanding the different types of neurogenic bladder and bowel, as well as the various treatment options available. By providing individualized care and addressing the unique needs of each client, healthcare professionals can improve outcomes and enhance the quality of life for clients with SCI.
Still more, clients with SCI require ongoing education and support to manage their bowel and bladder function effectively. Client education in bowel and bladder cannot be over emphasized. This includes education on catheterization techniques, bowel management strategies, and recognition of signs and symptoms of complications. Healthcare professionals play a critical role in providing this education and support and must work collaboratively with clients and their families to ensure optimal care.
Bowel and bladder management is a critical aspect of care for clients with SCI. By understanding the complexities of neurogenic bladder and bowel, providing individualized care, and addressing the unique needs of each client, healthcare professionals can improve outcomes and enhance the quality of life for clients with SCI.

Self-Quiz
Ask Yourself...
- What is the ASIA scale?
- How do you believe the ASIA scale could be used to assess a client’s level of functionality?
- How is the client’s bladder affected through a SCI?
- What importance do you think proper bowel management plays in the client’s independence?
Epidemiology
It is estimated that SCIs affect 54 cases per 1 million people per year (27). In the United States, approximately 17,810 new SCI cases occur annually (33) Males account for 78% of SCI cases, with the average age occurring at 43 years old (33). The leading causes of traumatic SCI vary by age:
- Motor vehicle accidents (37%)
- Falls (31%)
- Violence (15%)
- Sports injuries (11%)
The global prevalence of SCIs is estimated to be over 15 million people (37). In the United States, the prevalence is approximately 294,000 people (27).SCI incidence rates vary significantly across regions, with higher rates reported in North America and Europe (10).
Young males are at the highest risk for these injuries (22). It is believed that due to the nature of sports and biology, young males take greater risks and have an over-extended confidence that puts them in this category. Much research and safety measures have been put into play in recent years to help keep this population safer. These methods include things such as additional padding during sports, increasing the driving age, and putting age limits on firearm sales. Still, there is much research and preventative measures that need to be looked at to keep this population, young males, safer and free of SCI.
Research shows young males are more likely to engage in risk-taking behaviors, such as reckless driving and substance abuse, which can increase their risk of injury (6,28). Further research has shown that young males are more likely to participate in contact sports, such as football and hockey, which can also increase their risk of injury (30). Furthermore, studies that young males are more likely to engage in high-risk behaviors, such as not wearing seatbelts or helmets, which can also increase their risk of injury (25,31).
To address these issues, it is important to implement evidence-based safety measures, such as increasing education and awareness about the risks of injury and providing young males with the skills and knowledge they need to make informed decisions about their safety. Additionally, policymakers and healthcare professionals must work together to develop and implement policies and programs that address the unique needs of young males and help to prevent injuries such as increased padding during contact sports and stricter rules in regards to penalties in such sports for excessive physical roughness.
Overall, while there have been efforts to address the issue of young males being at risk for injuries, there is still much work to be done. By continuing to conduct research and implement practices that have been shown to increase client safety, we can help to keep this population safer and free of SCI.

Self-Quiz
Ask Yourself...
- What population is most at risk of sustaining a SCI?
- What age group is most affected by SCI? Is it more prevalent in males or females?
- Do you believe that schools would benefit from courses involving safety adding courses such as driver’s education, responsible drinking behavior, the importance of wearing helmets during contact sports etc.?
Pathophysiology
SCI involves primary and secondary mechanisms. Primary injury occurs immediately after trauma, resulting in mechanical damage to the spinal cord (3). During the primary stage of the injury, the spinal cord is severed in a complete injury and inflamed in an incomplete injury. During the period of inflammation or swelling of the spinal cord, the neurons are damaged and disrupted, interfering with the signaling that goes from the point at and below the injury to the brain.
It takes an estimated one year for the swelling to decrease. In between this one year, the client may or may not regain some of their lost function as the inflamed neurons begin to decompress and return to their normal size. As is in the case with a complete spinal cord injury, all neurons from the point of the injury are severed, and the client will very likely not regain any lost function from the point of injury down. This damage disrupts the blood-spinal cord barrier, leading to ischemia, edema, and neuronal death (18).
The secondary injury involves a cascade of cellular and molecular events, including inflammation, activation of immune cells, and release of pro-inflammatory cytokines (3). It also causes oxidative stress, which produces a reactive oxygen species, leading to cellular damage (3), and lastly, apoptosis, which is programmed cell death, contributing to neuronal loss (36). One of the key components of spinal cord injury is that spinal cord neurons do not grow back after cell death. This aspect of the injury is one of the great deviations involved in the diagnosis.

Self-Quiz
Ask Yourself...
- What are the basics of cell destruction involved in a spinal cord injury?
- How do damaged neurons affect the brain and its signals throughout the body?
- Does cell regeneration hold a possible cure to SCIs?
Clinical Signs and Symptoms
SCI symptoms vary depending on injury level and severity. Common symptoms include (3, 16, 26):
- Paralysis or weakness
- Loss of sensation
- Pain
- Respiratory difficulties
- Bladder and bowel dysfunction
The level of injury determines the extent of functional impairment (3, 16, 26, 34):
- Cervical (neck) injuries: Quadriplegia or tetraplegia
- Thoracic (upper back) injuries: Paraplegia
- Lumbar (lower back) injuries: Partial paralysis or weakness
- Sensory symptoms: Numbness, tingling, or loss of sensation
- Autonomic symptoms: Impaired blood pressure regulation, temperature control, or bowel/bladder function
As previously mentioned, with an incomplete spinal cord injury, the client will not know to what level of function will return until around a year post-injury. This being the case, it will be important to monitor for signs and symptoms of improvement. These include regaining sensation in previously affected areas, regaining bladder and/or bowel function, and increasing mobility.
Individuals with incomplete spinal cord injuries have a higher change of experiencing significant improvements in motor function within the first-year post-injury (35). Additionally, research has found that individuals who received early and intensive rehabilitation interventions experienced greater improvements in mobility and functional ability compared to those who received standard care (3).
It is essential to note that every individual’s recovery process is unique, and the rate and extent of improvement can vary significantly. Therefore, it is crucial to work closely with a healthcare team to develop a personalized rehabilitation plan that addresses the individual’s specific needs and goals. By doing so, individuals with incomplete spinal cord injuries can maximize their potential for recovery and achieve the best possible outcomes.

Self-Quiz
Ask Yourself...
- Name two leading symptoms involved in a spinal cord injury diagnosis.
- What determines the severity of a SCI?
- What impact does symptom management play in improving a client’s quality of life.
Case Study Continued
Alex’s initial assessment also revealed the presence of a neurogenic bladder, leading to urinary retention. He required intermittent catheterization every four hours to empty his bladder and prevent complications such as urinary tract infections (UTIs) and autonomic dysreflexia. Upon admission to the hospital, Alex underwent an assessment using the American Spinal Injury Association (ASIA) Impairment Scale and was classified as grade A, indicating a complete injury with no sensory or motor function in the sacral segments S4-S5.
Etiology
Traumatic SCI causes include (33):
- Motor vehicle accidents (37%)
- Falls (31%)
- Violence (15%)
- Sports injuries (11%)
Non-traumatic SCI causes include (16,34):
- Cancer (e.g., spinal tumors)
- Spinal stenosis
- Infection (e.g., meningitis, abscesses)
- Vascular disorders (e.g., spinal cord infarction)
- Infectious: Meningitis, abscesses, or osteomyelitis
- Inflammatory: Multiple sclerosis, transverse myelitis, or sarcoidosis
- Neoplastic: Spinal tumors or metastatic cancer
- Vascular: Spinal cord infarction or arteriovenous malformations
The etiology of the injury plays a crucial role in determining the recovery level and rate of individuals with spinal cord injuries. In traumatic SCI, the injury is caused by blunt force, whereas in non-traumatic injury, there is an object or interference that blocks the spinal cord, such as a tumor or narrowing of space due to a disorder like spinal stenosis (16). In either case, removal of the object causing compression or widening and surgical decompression of the spinal cord function may be restored to near previous ability (17).
However, there are risks associated with having a surgical procedure done on the spinal cord. Due to the sensitive nature of spinal nerves and the fact that they do not regenerate, careful thought and teaching of the possible consequences should be given to clients before surgery. It is essential to consider the potential risks and benefits of surgery, as well as the individual’s overall health and medical history.
In addition to the risks associated with surgery, there are also risks associated with not having surgery. For example, if a tumor or other object is compressing the spinal cord, it can cause permanent damage if left untreated (17). Therefore, it is crucial to carefully weigh the potential risks and benefits of surgery and make an informed decision.
The impact of SCI on daily life cannot be overstated. Individuals with SCI often experience significant changes in their physical abilities, social relationships, and emotional well-being. Simple tasks, such as getting dressed or using the bathroom, can become daunting challenges. Moreover, the financial burden of SCI can be substantial, with estimated lifetime costs ranging from $1 million to $5 million (27).
Rehabilitation and support services play a vital role in helping individuals with SCI adapt to their new circumstances. Physical therapy, occupational therapy, and speech therapy can help improve mobility, strength, and communication skills. Support groups and counseling services can also provide emotional support and guidance.
Advances in technology have also improved the lives of individuals with SCI. Assistive devices, such as wheelchairs and prosthetics, have enhanced mobility and independence. Communication devices and computer software have facilitated communication and social interaction.
The etiology of the injury plays a significant role in determining the recovery level and rate of individuals with SCI. While surgery can be an effective treatment option, it is essential to carefully consider the potential risks and benefits and make an informed decision. By doing so, individuals with SCI can make the best decision for their specific situation and achieve the best possible outcome.

Self-Quiz
Ask Yourself...
- What are the leading causes of SCIs?
- In learning about their acquisition, can we work towards educating the most at risk?
Treatment
Treatment goals focus on stabilization, rehabilitation, and maximizing functional recovery. Immediate management involves (3, 14, 16, 17):
- Surgical decompression and stabilization
- Steroid administration (methylprednisolone)
- Respiratory support (ventilation)
- Cardiovascular management (blood pressure regulation)
- Nutritional support
Long-term rehabilitation includes:
- Physical therapy (PT): Enhancing mobility, strength, and flexibility
- Occupational therapy (OT): Improving daily living activities
- Speech therapy: Addressing communication and swallowing disorders
- Psychological support: Counseling and mental health services (26, 29)
- Spinal cord stimulation: Enhancing motor function and reducing pain
- Functional electrical stimulation: Improving muscle function
- Robotics and assistive technologies: Enhancing mobility and independence Pharmacological interventions: Managing pain, spasticity, and bowel/bladder dysfunction (11, 23)
Treatment depends on etiology and probable outcome. It should be client-focused and geared in a way that is both practical and realistic. The client will often want to walk again, yet often, that is not an option. As a healthcare provider, it will be important to be compassionate and meet a client’s treatment where their functionality is currently. It is imperative to give clients the highest chance of independence, and this will largely depend on what is taught and learned in the early stages of treatment.
Treatment plans will both meet the need for the primary injury as well as the many secondary ailments that are incumbent with an SCI. Often, the secondary effects involve symptoms that can be managed well by medications. Things like spasms, chronic pain, wounds, and UTIs are especially prevalent following an injury. Many medications are used to help spasms and pain. This medication can range from anything mild, like Tylenol and baclofen for spasms, to narcotics such as fentanyl and butrans patches. As healthcare providers, it is always important to remember that pain is what the client says it is, and it is subjective. With neurological dysfunction, signaling is often incorrect, and while the client’s leg may hurt, they may feel it in their shoulder, for instance.
Regarding treatment, perhaps one of the most important forms is preventative treatment. It will be most important to impress upon the client the importance of regular skin checks and turning. Due to the neurological defect, a client will often not be able to feel the sensation at or below the point of injury. The importance of a routine turning schedule while in bed and weight shifts while in a wheelchair cannot be stressed enough.
Physical therapy and occupational therapy play a pivotal role in the treatment plan. PT will teach the client how to get the most function out of what they currently have, and OT will teach the client how to use their current function to contribute to their ADLs, such as brushing hair or writing. These therapies can and will change as the client progresses, but it must be emphasized to work with where their function is currently, as this will give them the most independence.

Self-Quiz
Ask Yourself...
- What are some of the ways medications are used to treat and combat symptoms of SCI?
- In what ways are various other disciplines involved in the recovery and healing process?
- Being that there is a large sensory deficit, how can skin management play a role in wellness and quality of life?
- Do you believe the role of the family has an equally important role in client recovery long term?
Case Study Continued
In addition to bladder management, Alex required bowel management due to the loss of normal bowel function. With a negative bulbocavernosus reflex (BCR), he was advised to undergo digital stimulation to facilitate bowel movements. Alex’s rehabilitation plan included physical therapy to maintain muscle tone and prevent contractures, as well as psychological support to cope with the emotional impact of the injury. As part of his interdisciplinary care team, Alex worked with healthcare professionals specializing in SCI management, including nurses, physical therapists, occupational therapists, and social workers, to address his comprehensive needs.
Self-Management
- Self-management strategies for individuals with SCI include:
- Regular exercise: Maintaining physical fitness and mobility (3,16)
- Wheelchair maintenance: Ensuring proper equipment function
- Pressure ulcer prevention: Regular skin checks and pressure relief (16)
- Bowel and bladder management: Establishing routine habits (15)
- Respiratory care: Proper use of ventilators and cough assistance devices (14, 16)
- Pain management: Using medication, exercise, and relaxation techniques (16)
- Mental health support: Seeking counseling and peer support groups (26, 29)
- Nutrition and hydration: Maintaining a balanced diet and adequate fluid intake (16)
Independence is the outcome post-injury. It will be important to empower the client and allow him or her to make as many choices as possible on their own. Doing so will not only give them freedom but will give them the confidence they need to continue therapy and treatment. Successful reintegration into society will be most successful with the inclusion of family and community. Having a family member trained to do things like catheterization and bowel programs will not only help the client that is returning home from hospitalization; it will ensure that should the client become ill at home, they will be cared for. As the SCI ages, it will become more and more difficult to perform these tasks alone. Having someone who is trained and responsible will add to the quality of life and freedom that the client desires.
It will also be important that the community help the client. Handicap access is tremendously important to reentry into the community. Ensuring there is available handicapped parking, ramps, and accessible restrooms will enable the individual to enter into the community and go about their life freely.


Self-Quiz
Ask Yourself...
- Do you think compliance plays a role in the recovery rate?
- Do you think the client can find a “new normal” and regain a sense of independence?
- What community resources are available to the client that has recently returned to the community after being in an inpatient setting?
- Do you believe that case management plays an important role in advocating for the client?
Research Findings
Researching spinal cord injuries (SCIs) poses significant challenges due to the relatively small number of individuals affected, the broad and expensive areas of study required, and the need for innovative trials. The field of regenerative medicine, particularly stem cell research, has been plagued by controversy and critique, involving complex ethical considerations and regulatory hurdles such as congressional proceedings and laws. SCI research requires interdisciplinary collaborations, combining computer science and medicine to develop innovative treatments like exoskeletal devices and brain stimulators. However, ethical considerations, such as the use of embryonic stem cells (3, 13, 26), raise concerns about the potential for uncontrolled growth and tumor formation and spark debate about the moral status of human life.
Despite these challenges, researchers must prioritize innovative trial designs, ethical considerations, and collaborations to overcome the hurdles. Both government and private organizations must invest in SCI research, recognizing its potential to improve the lives of individuals with SCIs. Currently, SCI research is underfunded and underserved compared to other areas of research (1). Addressing these challenges requires a concerted effort from researchers, policymakers, and funders. By doing so, researchers can develop effective treatments and technologies to enhance the quality of life for individuals with SCIs.
Newer advancements in SCI research show an ability to truly move recovery forward more so than ever. For instance, developments in brain-computer interfaces and neuroprosthetics can aid individuals with paralysis, ALS, and other motor disorders. SCI research also greatly increases our understanding of neural plasticity, regeneration, and repair, shedding light on the complexities of the human nervous system. To aide in research, scientists must leverage new technology like artificial intelligence, machine learning, and gene editing/reproduction. By using technology, we can open new possibilities for SCI treatment and improve the lives of individuals worldwide.

Self-Quiz
Ask Yourself...
- How has stem cell therapy advanced the prognosis of the SCI client?
- Do you see a cure for spinal cord injury happening at any time in the foreseeable future?
- Do you think funding is a barrier to research, and if so, what can be done to increase awareness of the need for funding?
Clinical Trials
Clinical trials are ongoing and limited to client participation. They include both pharmacological and physiological methods that require close monitoring and compliance. It will be important to make sure that the client is aware of the compliance and time commitment that is required for such trials.
Client participation in clinical trials is crucial for the development of new treatments and therapies. However, it is essential to ensure that clients are fully informed and aware of the potential risks and benefits associated with participating in a clinical trial. Research shows clients who are well-informed about the clinical trial process are more likely to adhere to the treatment plan and complete the trial (24). This highlights the importance of clear communication and client education in clinical trials.
In addition to client education, it is also crucial to ensure that clients are aware of the time commitment required for clinical trials. Clients who are provided optimal informed consent, such as awareness of the time commitment required for a clinical trial, are more likely to participate and complete the trial (24). This suggests that transparency about the time commitment required for clinical trials is essential for client participation and retention.
Still client compliance is critical for the success of clinical trials. Research shows that client non-compliance is a significant predictor of clinical trial failure (8). This highlights the importance of ensuring that clients are aware of the compliance requirements for clinical trials and are committed to adhering to the treatment plan.
Clinical trials are ongoing and limited to client participation. It is essential to ensure that clients are fully informed and aware of the potential risks and benefits associated with participating in a clinical trial. Client education, awareness of the time commitment required, and compliance are critical for the success of clinical trials.

Self-Quiz
Ask Yourself...
- How would you decide which clients were appropriate for clinical a clinical trial?
- Would family participation play a role in whether or not a client was chosen to participate in a study?
Future Directions
The future of spinal cord injury management holds immense promise for improved outcomes and enhanced quality of life, led by advances in stem cell therapy, emerging technologies, personalized medicine, interdisciplinary collaboration, and addressing disparities. Recent studies, demonstrate the potential of human mesenchymal stem cells to promote functional recovery after SCI (3, 13, 26). Additionally, emerging technologies like exoskeletons, brain-computer interfaces (BCIs), and virtual reality are transforming SCI rehabilitation (11, 20).
Furthermore, personalized medicine approaches can optimize medication management and minimize side effects, while interdisciplinary teams can develop comprehensive care plans addressing physical, emotional, and social needs. However, disparities in SCI care persist, emphasizing the need for culturally sensitive care and health literacy initiatives. The integration of telehealth and remote monitoring, accelerated by the COVID-19 pandemic, enhances access to rehabilitation services, reduces hospitalization rates, and improves client engagement (12).
Stem cell therapy has shown significant promise in promoting cell recovery and growth post SCI. Research demonstrates the potential of human mesenchymal stem cells in improving motor function and reducing inflammation in clients with SCI (13). These findings suggest that stem cell therapy may be a valuable treatment option for clients with SCI and gives new promises in the realm of cell recovery.
Emerging technologies such as exoskeletons, BCIs, and virtual reality are transforming SCI rehabilitation. Exoskeletons enable clients with SCI to walk again, improving mobility and reducing muscle atrophy (11). BCIs enable clients with SCI to control devices with their thoughts, improving communication and independence (21). Virtual reality provides an immersive and engaging environment for clients with SCI to practice rehabilitation exercises, improving motivation and outcomes (20).
Personalized medicine approaches can optimize medication management and minimize side effects, while interdisciplinary teams can develop comprehensive care plans addressing physical, emotional, and social needs (3, 16).
Differences in client population continue to impact SCI care as much as any other healthcare field, emphasizing the need for culturally sensitive care and health literacy initiatives. Research shows that racial and ethnic minorities with SCI experience poorer health outcomes and reduced access to rehabilitation services (19). One other study found that individuals with SCI from rural areas experienced reduced access to rehabilitation services resulting in poorer health outcomes and decreased satisfaction in life (9).
The future of SCI management holds immense promise for improved outcomes and enhanced quality of life. By leveraging advances in stem cell therapy, emerging technologies, personalized medicine, interdisciplinary collaboration, and addressing disparities, the SCI community can transform the lives of individuals with SCI, ultimately improving outcomes, enhancing quality of life, and promoting inclusive and effective care.

Self-Quiz
Ask Yourself...
- Where is the future for SCI recovery and treatment headed?
- Do you see more of a medical trend and less focus on manual therapy methods?
Case Study Finale
Over time, Alex made significant progress in adapting to his new way of life, demonstrating resilience and determination in the face of his catastrophic injury. His case highlights the importance of a holistic approach to SCI management, including personalized rehabilitation strategies and ongoing support for individuals and their families.
Conclusion
Spinal cord injury is a complex and devastating condition that requires a comprehensive team approach, which includes medical, rehabilitation, and community-based interventions. Despite advancements in research and treatment options, spinal cord injuries remain a significant public health concern, affecting millions of individuals worldwide every year.
The impact of spinal cord injuries extends beyond the individual, affecting families, communities, and society as a whole. Spinal cord injuries cost the United States healthcare system billions per year (27). This staggering figure highlights the need for continued research and investment in prevention, treatment, and rehabilitation strategies.
One of the most significant challenges in managing spinal cord injuries is the lack of effective treatments for promoting regeneration and repair of damaged spinal cord tissue. While advances in stem cell research and gene therapy hold promise, more research is needed to translate these findings into clinical practice. Research highlights the potential of stem cell-based therapies for promoting spinal cord repair but notes that further studies are needed to fully understand their efficacy and safety (13).
In addition to medical interventions, community-based interventions are also critical for promoting the health and well-being of individuals with spinal cord injuries. These interventions may include accessible housing, transportation, and recreational activities, as well as support groups and counseling services. By providing individuals with the resources and support they need to live independently and participate fully in their communities, we can help promote their overall health and well-being.
Moreover, technology plays a vital role in improving the lives of individuals with spinal cord injuries. Advances in assistive technologies, such as wheelchairs, prosthetics, and communication devices, have significantly enhanced mobility, independence, and quality of life. Virtual reality and gaming technologies have also shown promise in promoting rehabilitation and improving cognitive function.
The importance of advocacy and awareness cannot be overstated. Organizations and support groups dedicated to spinal cord injury awareness and research have made significant contributions to promoting public understanding and advancing research.
In the future, continued investment in research, technology, and community-based interventions will be crucial in improving outcomes for individuals with spinal cord injuries. By working together, we can promote greater awareness, advance research, and improve the lives of millions of individuals affected by spinal cord injuries worldwide.


Self-Quiz
Ask Yourself...
- What role do imaging studies play in SCI diagnosis?
- Describe the International Standards for Neurological Classification of SCI.
- What are the limitations of clinical evaluation in SCI assessment?
- How do you assess cognitive function in individuals with SCI?
- What is the significance of spinal cord swelling in acute SCI?
- Can you distinguish between SCI and other neurological conditions?
- How do you evaluate sensory and motor function in SCI?
- What are the implications of missed diagnosis in SCI?
- What are the primary goals of SCI rehabilitation?
- Describe the role of physical therapy in SCI management.
- How do you manage pain in individuals with SCI?
- What are the benefits and risks of surgical intervention in SCI?
- Can you explain the concept of neuroplasticity in SCI rehabilitation?
- How do you address spasticity and muscle spasms in SCI?
- What are the implications of early mobilization in SCI rehabilitation?
- Describe the role of occupational therapy in SCI management.
- How do you manage bowel and bladder dysfunction in SCI?
- What are the benefits of interdisciplinary teamwork in SCI rehabilitation?
References + Disclaimer
- Afshari, F. T., Choi, D., & Russo, A. (2020). Controversies regarding mobilisation and rehabilitation following acute spinal cord injury. British Journal of Neurosurgery, 34(2), 123–126. https://doi.org/10.1080/02688697.2019.1708268
- American Spinal Injury Association & International Spinal Cord Society. (2019, April). International Standards for Neurological Classification of Spinal Cord Injuries. https://www.asia-spinalinjury.org/wp-content/uploads/2019/10/ASIA-ISCOS-Worksheet_10.2019_PRINT-Page-1-2.pdf
- Bennett, J., Das, J. M., & Emmady, P. D. (2024, December 13). Spinal cord injuries. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK560721/
- Cerro, P. D., Barriga-Martín, A., Vara, H., Romero-Muñoz, L. M., Rodríguez-De-Lope, Á., & Collazos-Castro, J. E. (2021). Neuropathological and motor impairments after incomplete cervical spinal cord injury in pigs. Journal of Neurotrauma, 38(21), 2956–2977. https://doi.org/10.1089/neu.2020.7587
- Chaggar, R., Goetz, L. L., Adler, J., Bhuiyan, M. B. A., McAvoy, S., & Tubbs, J. (2024). Management of neurogenic bladder in patients with spinal cord injuries/disorders and end stage renal disease: A case series. Spinal Cord Series and Cases, 10(1), 8. https://doi.org/10.1038/s41394-024-00623-8
- Chebat, D., Lemarié, L., Rotnemer, B., Talbi, T., & Wagner, M. (2021). The young and the reckless: Social and physical warning messages reduce dangerous driving behavior in a simulator. Journal of Retailing and Consumer Services, 63(102701). https://doi.org/10.1016/j.jretconser.2021.102701
- Christopher and Dana Reeve Foundation. (n. d.). Costs of living with sci. https://www.christopherreeve.org/todays-care/living-with-paralysis/costs-and-insurance/costs-of-living-with-spinal-cord-injury/
- Czobor, P., & Skolnick, P. (2011). The secrets of a successful clinical trial: Compliance, compliance, and compliance. Molecular Interventions, 11(2), 107–110. https://doi.org/10.1124/mi.11.2.8
- Deane, K. C., Kurapati, N., Gill, E., Vogel, L. C., & Zebracki, K. (2023). Rural-urban disparities in healthcare factors and long-term health outcomes in individuals with pediatric-onset spinal cord injury. Frontiers in Rehabilitation Sciences, 4, 1102441. https://doi.org/10.3389/fresc.2023.1102441
- Ding, W., Hu, S., Wang, P., Kang, H., Peng, R., Dong, Y., & Li, F. (2022). Spinal cord injury: The global incidence, prevalence, and disability from the global burden of disease study 2019. Spine, 47(21), 1532–1540. https://doi.org/10.1097/BRS.0000000000004417
- Forte, G., Leemhuis, E., Favieri, F., Casagrande, M., Giannini, A. M., De Gennaro, L., & Pazzaglia, M. (2022). Exoskeletons for mobility after spinal cord injury: A personalized embodied approach. Journal of Personalized Medicine, 12(3), 380. https://doi.org/10.3390/jpm12030380
- Gajarawala, S. N., & Pelkowski, J. N. (2021). Telehealth benefits and barriers. The Journal for Nurse Practitioners: JNP, 17(2), 218–221. https://doi.org/10.1016/j.nurpra.2020.09.013
- Gao, L., Peng, Y., Xu, W., He, P., Li, T., Lu, X., & Chen, G. (2020). Progress in stem cell therapy for spinal cord injury. Stem Cells International, 2020, 2853650. https://doi.org/10.1155/2020/2853650
- Glinsky, J. V., & Harvey, L. A. (2024). Physiotherapy management of people with spinal cord injuries: an update. Journal of Physiotherapy, 70(4), 256–264. https://doi.org/10.1016/j.jphys.2024.09.008
- Goyal, V., Paracka, D. J., Gaur, R., & Shukla, A. (2022). Bowel management in patients with chronic spinal cord injury: A cross-sectional survey. Cureus, 14(6), e25893. https://doi.org/10.7759/cureus.25893
- Hills, T. (2020). Caring for patients with a traumatic spinal cord injury. Nursing2025, 50(12), 30-40. doi: 10.1097/01.NURSE.0000721724.96678.5a
- ICHAN School of Medicine at Mount Sinai. (n. d.). Spinal cord trauma. https://www.mountsinai.org/health-library/diseases-conditions/spinal-cord-trauma
- Jin, L. Y., Li, J., Wang, K. F., Xia, W. W., Zhu, Z. Q., Wang, C. R., Li, X. F., & Liu, H. Y. (2021). Blood-spinal cord barrier in spinal cord injury: A Review. Journal of Neurotrauma, 38(9), 1203–1224. https://doi.org/10.1089/neu.2020.7413
- Kabangu, J. K., Heskett, C. A., De Stefano, F. A., Masri-Elyafaoui, A., Fry, L., & Ohiorhenuan, I. E. (2024). Race and socioeconomic disparities persist in treatment and outcomes of patients with cervical spinal cord injuries: An analysis of the national inpatient sample from 2016 - 2020. World Neurosurgery: X, 23, 100384. https://doi.org/10.1016/j.wnsx.2024.100384
- Leemhuis, E., Esposito, R. M., De Gennaro, L., & Pazzaglia, M. (2021). Go virtual to get real: virtual reality as a resource for spinal cord treatment. International Journal of Environmental Research and Public Health, 18(4), 1819. https://doi.org/10.3390/ijerph18041819
- Levett, J. J., Elkaim, L. M., Niazi, F., Weber, M. H., Iorio-Morin, C., Bonizzato, M., & Weil, A. G. (2024). Invasive brain computer interface for motor restoration in spinal cord injury: A systematic review. Neuromodulation: Journal of the International Neuromodulation Society, 27(4), 597–603. https://doi.org/10.1016/j.neurom.2023.10.006
- Mandadi, A. R., Koutsogiannis , P., Das, J. M., & Waseem, M. (2024). Pediatric spine trauma. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK442027/
- Morone, G., Pirrera, A., Iannone, A., & Giansanti, D. (2023). Development and use of assistive technologies in spinal cord injury: A narrative review of reviews on the evolution, opportunities, and bottlenecks of their integration in the health domain. Healthcare (Basel, Switzerland), 11(11), 1646. https://doi.org/10.3390/healthcare11111646
- Nathe, J. M., & Krakow, E. F. (2019). The challenges of informed consent in high-stakes, randomized oncology trials: A systematic review. MDM Policy & Practice, 4(1), 2381468319840322. https://doi.org/10.1177/2381468319840322
- National Highway Traffic Safety Administration. (n. d.). NHTSA’S most wanted: 45 million Americans still not buckling up. https://www.nhtsa.gov/sites/nhtsa.gov/files/mostwanted.pdf
- National Institute of Neurological Disorders and Stroke. (2025, January). Spinal cord injury. https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury
- National Spinal Cord Injury Statistical Center. (2024). Traumatic spinal cord injury facts and figures at a glance. https://msktc.org/sites/default/files/Facts-and-Figures-2024-Eng-508.pdf
- Nawi, A. M., Ismail, R., Ibrahim, F., Hassan, M. R., Manaf, M. R. A., Amit, N., Ibrahim, N., & Shafurdin, N. S. (2021). Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health, 21(1), 2088. https://doi.org/10.1186/s12889-021-11906-2
- Schultz, K. R., Mona, L. R., & Cameron, R. P. (2022). Mental health and spinal cord injury: Clinical considerations for rehabilitation providers. Current Physical Medicine and Rehabilitation Reports, 10(3), 131–139. https://doi.org/10.1007/s40141-022-00349-4
- Stracciolini, A., Casciano, R., Levey Friedman, H., Stein, C. J., Meehan, W. P., 3rd, & Micheli, L. J. (2014). Pediatric sports injuries: A comparison of males versus females. The American Journal of Sports Medicine, 42(4), 965–972. https://doi.org/10.1177/0363546514522393
- Sweatt, I. H., Barr, C., Gelinne, A., Woolard, A., & Quinsey, C. (2023). Social disparities in helmet usage in bicycle accidents involving children. Cureus, 15(7), e42017. https://doi.org/10.7759/cureus.42017
- Thompson, C., Feldman, D. E., & Mac-Thiong, J. M. (2018). Surgical management of patients following traumatic spinal cord injury: Identifying barriers to early surgery in a specialized spinal cord injury center. The Journal of Spinal Cord Medicine, 41(2), 142–148. https://doi.org/10.1080/10790268.2016.1165448
- United Spinal Association. (2022). Spinal cord injuries facts and stats. Retrieved from https://unitedspinal.org/spinal-cord-injury-facts-and-stats/
- United Spinal Association. (n.d.). What is spinal cord injury/disorder? Retrieved from https://unitedspinal.org/what-is-spinal-cord-injury-disorder-scid/
- van Middendorp, J. J., Goss, B., Urquhart, S., Atresh, S., Williams, R. P., & Schuetz, M. (2011). Diagnosis and prognosis of traumatic spinal cord injury. Global Spine Journal, 1(1), 1–8. https://doi.org/10.1055/s-0031-1296049
- Wang, S., & Cheng, L. (2024). The role of apoptosis in spinal cord injury: A bibliometric analysis from 1994 to 2023. Frontiers in Cellular Neuroscience, 17, 1334092. https://doi.org/10.3389/fncel.2023.1334092
- World Health Organization (2024, April 16). Spinal cord injury. https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
