Congenital Heart Defects in Newborns
Contact Hours: 1
Author(s):
Danielle Leach MSN, RNC-NIC
Course Highlights
- In this Congenital Heart Defects in Newborns course, we will learn about the different types of congenital heart defects in newborns.
- You’ll also learn methods for screening newborns for congenital heart defects.
- You’ll leave this course with a broader understanding of treatments and interventions for different congenital heart defects.
Introduction
Congenital heart defects (CHDs) are structural heart problems that neonates are born with. These conditions can affect how the heart pumps blood, resulting in blood flowing the wrong way or being obstructed from flowing in the correct pathway (22).
There are many different types of congenital heart defects with different levels of severity. The purpose of this course is to equip learners with the knowledge needed to identify, screen, and help manage the treatment of CHDs for the newborn and family.
Epidemiology
What is happening on a global scale?
Congenital heart disease (CHD) is one of the most frequently diagnosed birth defects, affecting approximately 0.8% to 1.2% of live births worldwide (27). The incidence and mortality rates, however, vary from country to country.
The incidence of CHD was relatively high in third-world areas, such as certain regions of Asia and Africa, but has remained relatively low in the most developed countries. The lowest incidence rates were found in developed countries, including France, Portugal, and Venezuela (27).
What is happening nationally?
CHDs account for about 40,000 births per year (nearly 1%) in the United States (19). The prevalence of some types of CHDs, especially the less acute types, is increasing, while the prevalence of other types has remained unchanged. The most common type of congenital heart defect in the United States is a ventricular septal defect (VSD).
Approximately one in four neonates with a heart defect has a critical CHD, which generally needs surgery or other procedures to survive (19).
Ask yourself...
- Why do you think that CHDs are more prevalent in less developed countries?
- What do you think could be implemented to help improve the CHD statistics in the United States?
Etiology
Genetic Causes
CHDs can begin to develop early in pregnancy, as early as the first six weeks (21). For some newborns, the heart defect can be caused by changes in their chromosomal makeup. Approximately 15% of CHDs are linked to genetic or chromosomal conditions such as Down Syndrome and Turner Syndrome (21).
Health Conditions or Medication Intake of the Mother
A mother’s health and lifestyle can also play a role in the development of CHDs. Conditions such as rubella, lupus, phenylketonuria, and diabetes mellitus can increase the risk of the development of heart defects. Obesity, drinking alcohol, and smoking cigarettes before or during pregnancy can also lead to an increased risk of CHDs (21).
Taking certain medications during pregnancy can put an infant at risk for developing a CHD. Some examples of medications known to cause heart defects are ACE inhibitors, lithium, statins, thalidomide, and isotretinoin (21). Pregnant mothers should be urged to talk to their provider about the risks of medications they are taking.
Ask yourself...
- What are the health conditions of the mother that can lead to an increased risk of the development of CHDs in infants?
Types of CHDs
Atrial Septal Defect
An atrial septal defect (ASD) is a congenital heart defect in which a hole in the septum divides the right and left atria (18). The defect can vary in size and may close on its own or require surgery to repair. Left-to-right shunting (a backflow of blood from systemic to pulmonary circulation) can occur. This can lead to increased pulmonary blood flow, which can result in complications such as pulmonary edema (18).
 (4)
(4)
Ventricular Septal Defect
A ventricular septal defect (VSD) is a congenital heart defect in which a hole in the septum divides the right and left ventricles (2). In a newborn with a normal heart, the left ventricle pumps oxygen-rich blood to the body, and the right ventricle pumps oxygen-poor blood to the lungs.
In newborns with a VSD, blood shunts from the left ventricle through the ventricular septal defect to the right ventricle and then into the lungs. Over time, this forces the heart to work harder. If not repaired, a VSD can increase the risk for pulmonary hypertension, heart failure, arrhythmias, and stroke (2).
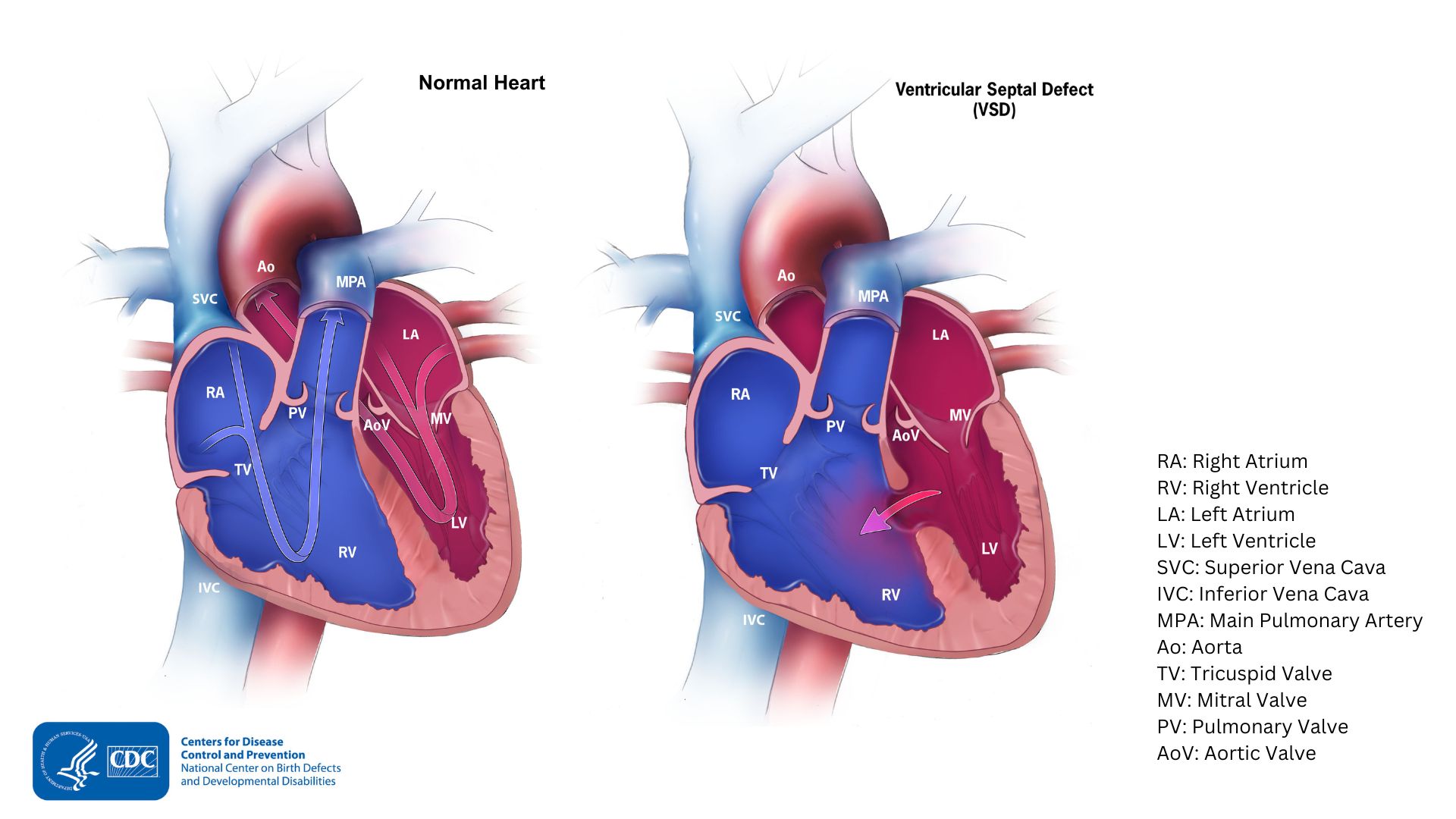
(3)
Ask yourself...
- What do ASDs and VSDs have in common?
Coarctation of the Aorta
Coarctation of the aorta is a critical congenital heart defect in which the area around the aortic arch is narrower than normal (11). The defect is usually located along the aortic arch after the area where the arteries branch to the upper body. This can cause normal blood pressure and pulses in the upper body, low blood pressure, and weak pulses in the lower extremities.
If the defect is narrow enough, blood may not be able to be adequately pumped to the lower body. If the coarctation is not repaired, heart failure can result. Coarctation of the aorta can occur with other congenital heart defects and syndromes, such as VSD and Turner Syndrome (11).
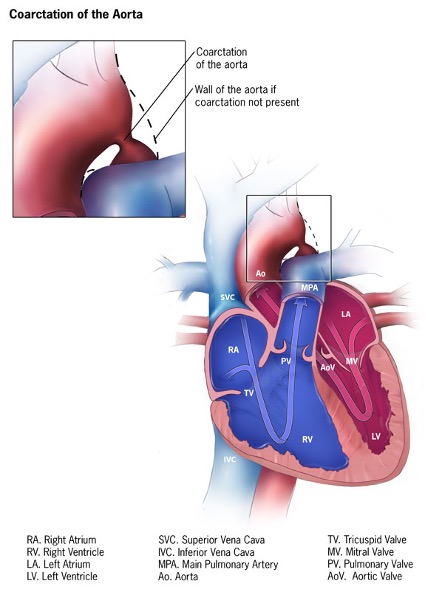
(5)
Ask yourself...
- How can coarctation of the aorta affect pulses in the lower extremities?
Transposition of the Great Vessels
Transposition of the Great Vessels is a congenital heart defect in which the two large vessels carrying blood out of the heart, the pulmonary artery and the aorta, are transposed, or switched positions (12). This is considered a critical cyanotic congenital heart defect because the infant will need procedures or surgery soon after birth.
In infants with transposition of the great vessels, oxygen-deficient blood returning from the body enters the right side of the heart. Instead of going to the lungs to be oxygenated, the oxygen-poor blood is pumped out to the rest of the body via the aorta.
Oxygen-rich blood from the lungs is pumped back into the lungs via the pulmonary artery. Newborns with transposition of the great vessels often have other heart defects, such as a VSD or ASD, which allows blood to mix so that some oxygen-rich blood is pumped to the body (12).

(9)
Ask yourself...
- What vessels are affected by transposition of the great vessels?
Hypoplastic Left Heart Syndrome
Hypoplastic Left Heart Syndrome (HLHS) is a critical congenital heart defect where the left side of the heart does not fully develop (13). In HLHS, the left ventricle is small and underdeveloped, the mitral and aortic valves are very small or not formed, and the ascending aorta is underdeveloped or too small. In infants with HLHS, the left side of the heart is too undersized to properly pump oxygen-rich blood to the body.
During the first days of life for a newborn with HLHS, the oxygen-rich blood bypasses the underdeveloped left side of the heart through the patent ductus arteriosus and the patent foramen ovale. Blood is then pumped to the lungs and body through the right side of the heart. However, for infants with HLHS, when these openings close, it becomes difficult for blood to mix and reach the rest of the body.
Often, newborns with HLHS also have an ASD, which allows blood to mix and flow to the rest of the body (13).
(6)
Ask yourself...
- Which cardiac structures are affected by HLHS?
Tetralogy of Fallot
Tetralogy of Fallot is a critical congenital heart defect comprised of four defects (16). These four defects include a VSD, pulmonary stenosis, right ventricular hypertrophy, and an enlarged aortic valve that opens to both the right and left ventricles in the area of the VSD. If the pulmonary stenosis is severe enough, the infant may be born with cyanosis, especially circumoral cyanosis. Infants may also develop cyanosis during feeding or crying, called a tet spell (16).
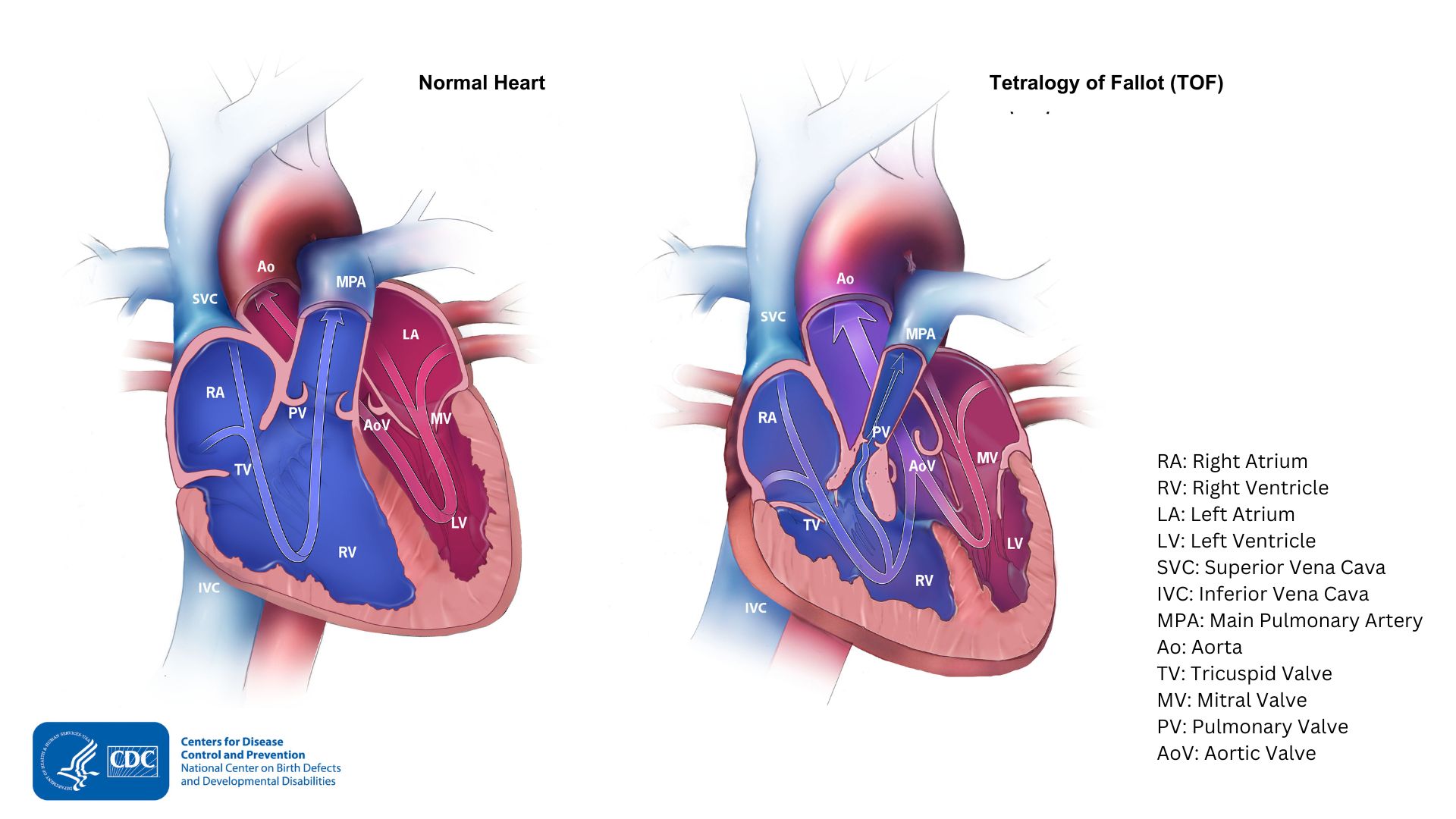
(8)
Ask yourself...
- What are the four defects that comprise Tetralogy of Fallot?
Truncus Arteriosus
Truncus Arteriosus is a critical congenital heart defect that occurs when the aorta and pulmonary artery fail to separate completely during development (17). Instead of a separate aortic and pulmonary valve, the infant has a singular truncal valve, which is usually abnormal.
In a newborn with truncus arteriosus, oxygen-rich and oxygen-deficient blood are mixed and sent to the lungs and the body. This can result in too much blood being pumped to the lungs and the heart working much harder to pump blood to the rest of the body (17).

(10)
Ask yourself...
- What do you think could result in a child with truncus arteriosus who does not have a repair?
Signs and Symptoms
Signs and symptoms of congenital heart defects can vary based on the specific diagnosed defect (22). Nurses, however, should be aware of some of the most common symptoms when assessing or screening their patients.
Common signs of congenital heart defects include:
- Murmur
- Weak or bounding pulses
- Cyanosis
- Tachycardia
- Tachypnea and respiratory distress
- Fatigue or unusual sleepiness
- Poor growth
- Edema and other signs of heart failure (22)
When encountering any of these symptoms during clinical assessment, the nurse should notify the provider.
Ask yourself...
- Can you name three signs and symptoms of CHDs?
Clinical Diagnosis
Screening
Current recommendations suggest screening all newborns greater than 24 hours of age using pulse oximetry for congenital heart defects before discharge home (15). Exact procedures can vary from state to state and may change if the neonate is in the neonatal intensive care unit or other specialty area.
Pulse oximetry screening does not always detect all critical CHDs, and a newborn may still have a CHD even with a passed screen. The nurse should apply the pulse oximetry probe to the infant’s right hand, wrist, or foot. A screening with a pulse oximetry measure greater than or equal to 95% in the right hand or foot, with less than a 3% difference in oxygen saturation between the right hand or foot, is considered a passed screen, and the screening would be complete.
An infants’ screen is considered failed if:
- Any pulse oximetry reading less than 90% (in the initial screen or in repeated screens),
- The pulse oximetry reading is less than 95% in the right hand and foot on three measures, each measure separated by one hour, or
- Pulse oximetry readings between the right hand and foot on three measures, each separated by one hour, differ by more than 3%.
A failed screen should be reported to the provider. An echocardiogram and pediatric cardiology referral may be necessary (15).
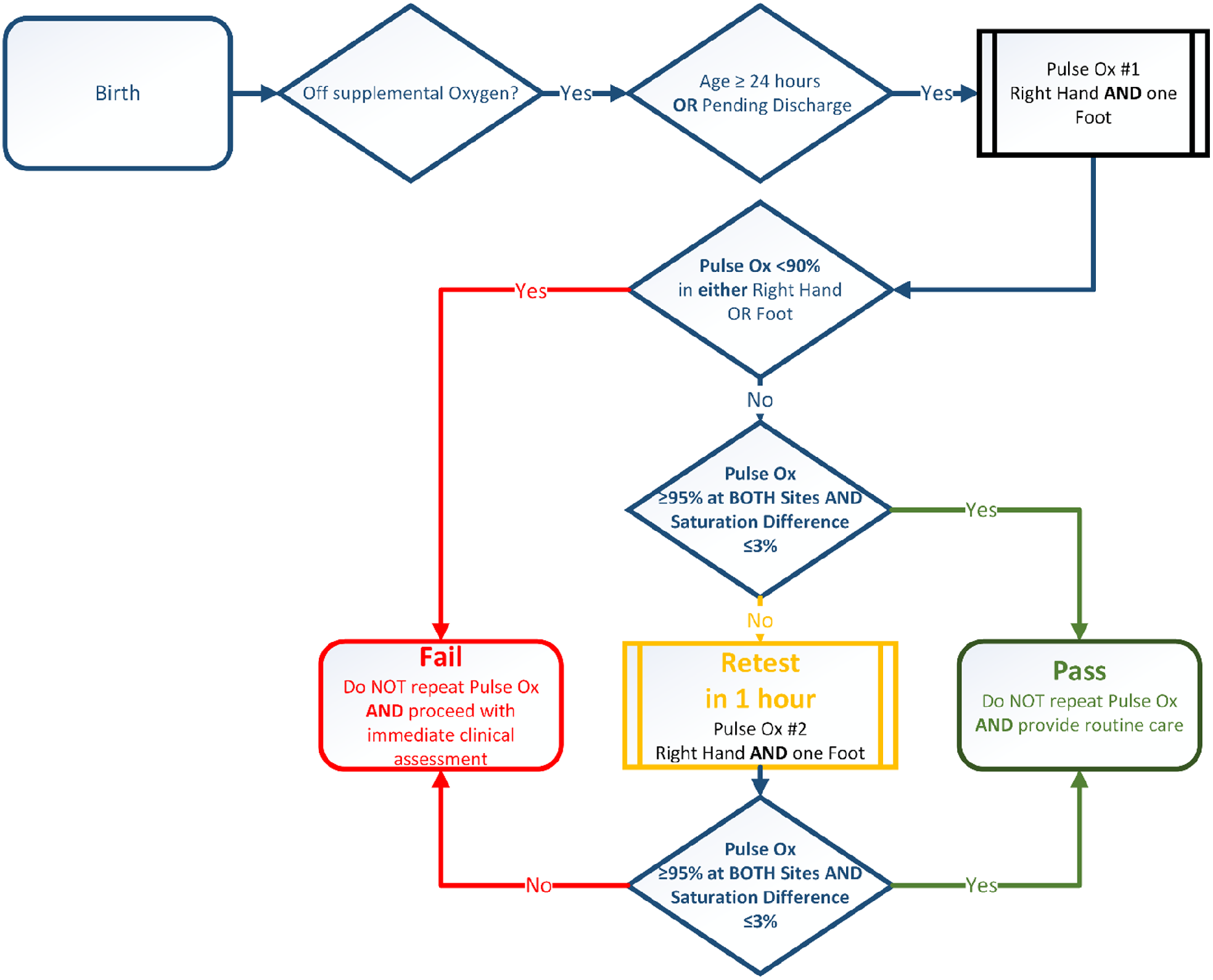
(7)
Ask yourself...
- What would be an example of a failed CHD screening test?
Diagnostic Procedures
CHDs can be diagnosed before birth or sometimes even during pregnancy (23) if an unborn child is suspected of having a CHD, a fetal echocardiogram can be ordered. Genetic testing can also be done before or after birth to determine if any associated syndromes or chromosomal abnormalities are present.
If a newborn is suspected of having a CHD or if it was already diagnosed prenatally, after birth, the provider can order diagnostic tests such as an echocardiogram, electrocardiogram, or chest x-ray. Critical CHDs may also warrant a cardiac MRI or catheterization (23).
Ask yourself...
- What do you think would be an advantage of ordering a cardiac catheterization instead of an echocardiogram?
Treatment
Treatment for CHDs will depend on the specific defect and its degree of severity (24). Most CHDs will require treatment. However, some, such as a very small ASD or VSD, may only require monitoring.
A newborn with a CHD may require:
- Cardiac catheterization to repair simple defects such as ASD or VSD.
- Surgery to repair more complex or larger defects, replace heart valves, or widen narrowed cardiac vessels.
- A heart transplant is required in conditions such as HLHS.
- Palliative surgery is used to temporarily improve oxygenation using a shunt until the infant is strong enough for more complex surgery.
- A ventricular assist device, such as Berlin Heart, can take over cardiac function while the patient is awaiting a transplant or more complex cardiac surgery.
- Medications such as digoxin, beta blockers, or prophylactic antibiotics are used to prevent endocarditis.
- Activity restrictions. (24)
Ask yourself...
- How do you think such a complex surgical procedure could affect an infant?
Developmental Impact
Children with CHDs can fall behind in their growth and development compared with other children who are the same age (26).
Heart defects cause the child’s heart to work harder to pump blood, which increases their metabolic demand. A CHD diagnosis may cause the child to be shorter, weigh less, and appear younger than others. The child may also be slower in meeting developmental milestones such as rolling over, crawling, or walking because of the impact of their diagnosis.
Genetic syndromes associated with heart defects may cause further developmental and growth issues. Frequent or prolonged hospitalizations may prevent the child from receiving the needed environmental stimuli and regular contact with caregivers, affecting their social and cognitive development (26).
The increased metabolic demand may also require adding extra calories to the infant’s breastmilk or formula (26). In severe cases, the child may need supplemental feedings via a gastrostomy tube to increase caloric intake. The child may also tire quickly, requiring frequent breaks from activities such as feeding or playing.
Ask yourself...
- Why does a cardiac defect increase a child’s metabolic demand?
- How can we help infants and children with CHD stay on track for their growth and development?
Supporting the Family
Families of infants with CHDs may be under significant stress and will need support throughout their child’s lifetime. Some children’s hospitals and larger medical centers may have specialized clinics and support groups, especially for CHDs. There are also many resources and groups online where families can be directed to learn more about their child’s specific condition and to get in contact with others affected by heart defects.
Organizations such as the March of Dimes, Conquering CHD, and Mended Little Hearts are committed to collaborating with clients, families, and providers to educate and improve the quality of life for those with CHDs and other associated issues (14).
Scan the provided QR code to access a resource of links to offer to families.

Ask yourself...
- Which source or sources would you prefer to provide to families with a child with a CHD?
Resources
A wealth of information is available for nurses to learn more about CHDs and improve their care of these fragile newborns. A handbook, Congenital Heart Disease: The Nursing Care Handbook (20), provides a theoretical background and a practical basis for nursing specializing in infants with congenital heart disease.
The Pediatric Cardiac Intensive Care Society has a webpage specifically for nursing resources and several online courses for nurses (25). Additionally, the American Academy of Pediatrics has a Congenital Heart Defects Toolkit (1) that nurses and other healthcare team members can utilize.
Ask yourself...
- Do you want to learn more about CHDs or other cardiac anomalies?
- Have you ever taken care of an infant or child with a CHD?
- Can you name and describe five different CHDs?
Conclusion
Congenital heart defects are a group of serious disorders affecting infants that contribute to increased morbidity and mortality. Care of a child with a CHD takes an effort from all members of the care team, and a systemic care plan for improving the health and life of the client. Nurses are first-line team members who are crucial to help screen for and detect CHDs.
References + Disclaimer
- American Academy of Pediatrics. (2023). Congenital heart defects toolkit. https://www.aap.org/en/patient-care/congenital-heart-defects/congenital-heart-defects-toolkit/
- Centers for Disease Control and Prevention. (2022, January 24). Facts about ventricular septal defect. https://www.cdc.gov/ncbddd/heartdefects/ventricularseptaldefect.html
- Centers for Disease Control and Prevention (2022). Ventricular septal defect (VSD). [Digital image]. https://www.cdc.gov/ncbddd/heartdefects/images/vsd_simple-sm.jpg?_=22673
- Centers for Disease Control and Prevention (2023). Atrial septal defect (ASD). [Digital image]. https://www.cdc.gov/ncbddd/heartdefects/images/asd-web.jpg?_=68661
- Centers for Disease Control and Prevention (2023). Coarctation of the aorta. [Digital image]. https://www.cdc.gov/ncbddd/heartdefects/images/coarctationlayoutv2-575px.jpg?_=22622
- Centers for Disease Control and Prevention (2023). Hypoplastic left heart syndrome (HLHS). [Digital image]. https://www.cdc.gov/ncbddd/heartdefects/images/hlhs-web_small.jpg?_=22634
- Centers for Disease Control and Prevention (2023). Screening chart for congenital heart disease. [Digital image]. https://www.cdc.gov/ncbddd/heartdefects/images/screening-chart.JPG?_=22674
- Centers for Disease Control and Prevention (2023). Tetralogy of Fallot (TOF). [Digital image]. https://www.cdc.gov/ncbddd/heartdefects/images/tetralogy-web_small.jpg?_=22600
- Centers for Disease Control and Prevention (2023). Transposition of the great vessels (TGV). [Digital image]. https://www.cdc.gov/ncbddd/heartdefects/images/transposition-sm.jpg?_=22661
- Centers for Disease Control and Prevention (2023). Truncus arteriosus. [Digital image]. https://www.cdc.gov/ncbddd/heartdefects/images/Truncus_arteriosus-sm.jpg?_=22597
- Centers for Disease Control and Prevention. (2023, February 2). Facts about coarctation of the aorta. https://www.cdc.gov/ncbddd/heartdefects/coarctationofaorta.html
- Centers for Disease Control and Prevention. (2023, February 2). Facts about dextro-Transposition of the Great Arteries (d-TGA). https://www.cdc.gov/ncbddd/heartdefects/d-tga.html
- Centers for Disease Control and Prevention. (2023, February 2). Facts about hypoplastic left heart syndrome. https://www.cdc.gov/ncbddd/heartdefects/hlhs.html
- Centers for Disease Control and Prevention. (2023, February 2). Links to other congenital heart defects resources. https://www.cdc.gov/ncbddd/heartdefects/links.html#print
- Centers for Disease Control and Prevention. (2023, February 3). Critical congenital heart defects screening methods. https://www.cdc.gov/ncbddd/heartdefects/hcp.html
- Centers for Disease Control and Prevention. (2023, February 3). Facts about tetralogy of Fallot. https://www.cdc.gov/ncbddd/heartdefects/tetralogyoffallot.html
- Centers for Disease Control and Prevention. (2023, February 3). Facts about truncus arteriosus. https://www.cdc.gov/ncbddd/heartdefects/truncusarteriosus.html
- Centers for Disease Control and Prevention. (2023, June 21). Facts about atrial septal defect. https://www.cdc.gov/ncbddd/heartdefects/atrialseptaldefect.html
- Centers for Disease Control and Prevention. (2023, September 19). Data and statistics on congenital heart defects. https://www.cdc.gov/ncbddd/heartdefects/data.html
- Flocco, Lillo, A., Dellafiore, F., & Goossens, E. (Eds.). (2019). Congenital Heart Disease: The Nursing Care Handbook (1st ed. 2019.). Springer International Publishing. https://doi.org/10.1007/978-3-319-78423-6
- March of Dimes. (2019). Congenital heart defects and critical CHDs. https://www.marchofdimes.org/find-support/topics/planning-baby/congenital-heart-defects-and-critical-chds
- MedlinePlus. (2022, August 10). Congenital heart defects. https://medlineplus.gov/congenitalheartdefects.html
- National Heart, Lung, and Blood Institute. (2022, March 24). Congenital heart defects: Diagnosis. https://www.nhlbi.nih.gov/health/congenital-heart-defects/diagnosis
- National Heart, Lung, and Blood Institute. (2022, March 24). Congenital heart defects: Treatment. https://www.nhlbi.nih.gov/health/congenital-heart-defects/treatment
- The Pediatric Cardiac Intensive Care Society. (2023). Nursing resources. https://pcics.org/education/nursing-resources/
- University of Rochester Medical Center (2023). Growth and development in children with congenital heart disease. https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=p01792#:~:text=Genetic%20problems%20linked%20to%20heart,and%20brain%20and%20nerve%20cells.
- Wu, W., He, J., & Shao, X. (2020). Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990–2017. Medicine, 99(23). Doi: 10.1097/MD.0000000000020593
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
