Course
Connecticut APRN Bundle Part 1
Course Highlights
In this course we will cover a variety of nursing topics pertinent in the state of Connecticut. This course is appropriate for APRNs. Upon completion of this single module you will receive a certificate for 20 contact hours.
About
Contact Hours Awarded:
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
Cultural Competence in Nursing
Introduction
There is no doubt that modern medicine has made many technological advancements over the last few decades, forging the way for highly intricate diagnostic and treatment methods and improving the quality and longevity of many lives. To keep up with changing times, however, healthcare professionals must consider much more than the technical aspects of healthcare delivery.
They must take a closer look and a more conscientious approach to delivering care, particularly across various demographics and characteristics. Ensuring care is delivered with empathy, respect, and equity, noting and honoring a patient's differences, is how care transforms from good to great. Practicing diversity, equity, and inclusion (DEI) and cultural competence in nursing must become a standard.
Health Disparities
When covering cultural competence in nursing, a provider must know that each patient is unique. However, some characteristics such as race, gender, age, sexual orientation, or disability can create gaps in the availability, distribution, and quality of healthcare delivered.
These gaps can create lasting negative impacts on patients mentally, physically, spiritually, and emotionally and even lead to poorer outcomes than patients not within a particular population. Modern healthcare professionals are responsible for learning to identify risks, provide sensitive and inclusive care, and advocate for equity in much the same way that they are responsible for understanding how the human body, medications, or hospital equipment works.
Epidemiology
Let's turn to data to understand the importance of cultural competence in nursing and the best practices for DEI in healthcare.
Healthy People 2020 provides a myriad of data that includes countless implications for changes needed in healthcare settings for equitable care of all populations. The data includes statistics such as:
- 12.6% of Black/African American children have a diagnosis of asthma, compared to 7.7% of white children (11).
- The rate of depression in women ages 65+ is 5% higher than that of men of the same age across all races (11).
- Teenagers and young adults who are part of the LGBTQ community are 4.5 times more likely to attempt suicide than straight, cis-gender peers (11).
- 16.1% of Hispanics report not having health insurance, compared to 5.9% of white populations (11).
- The national average of infant deaths per 1,000 live births is 5.8. The rate for Black/African American infants is nearly double at 11 deaths per 1,000 births (11).
- 12.5% of veterans are homeless, compared to 6.5% of the general U.S. population (11).
Additional disparities are seemingly endless and unquestionably point to the fact that healthcare professionals cannot be uninformed about cultural competence and DEI awareness. This course aims to outline and explore the most common or severe healthcare disparities, address ways healthcare delivery needs to be adjusted, and start the conversations needed to create a new generation of healthcare professionals who will close these gaps.
Understanding DEI best practices in the health setting and possessing cultural competence in nursing is vital in making positive changes for all populations.


Self Quiz
Ask yourself...
- How do characteristics like race, gender, age, sexual orientation, or disability contribute to disparities in healthcare delivery, and why is it essential for providers to recognize these gaps?
- Why do you think programs like Healthy People gather statistics about specific demographics and gaps between populations?
- How has our collection of and attention to this type of data changed over the years, and how might that impact our historical knowledge about healthcare?
- Why must modern clinicians integrate cultural competence into their education, training, and general approach to patient care? How is this different from the delivery of healthcare in the past?
- What inequities have you witnessed or even experienced yourself regarding healthcare delivery?
Impact of Implicit Bias
Nurses must first understand implicit bias and how it impacts care delivery when working toward culturally competent care. Implicit bias is a subconscious attitude of opinion about an individual or a group that could influence the actions and decisions of the clinician. (It is important to note that this differs from explicit bias, which is a controllable attitude or action such as making sexist comments or using racial slurs.) (30)
Everyone has implicit biases; they are essentially our own unique lens through which we view the world, shaped by our upbringing and life experiences. What is important is that clinicians develop an awareness of that lens, recognize that their viewpoint is not objective, and understand ways that bias may be impacting their feelings, attitudes, or actions toward others (30).
Sometimes, implicit biases impact care in a positive way. If you care for a client who tells you they are retired from nursing, you may feel a connection or warmth towards them and go above and beyond the level of care required due to this positive connection.
In the context of cultural competence, however, we must consider how implicit bias might negatively impact care delivery. Common examples of the effects of implicit bias in healthcare include:
- Assuming elderly clients have cognitive or physical limitations
- Feeling female clients have too many complaints or are exaggerating
- Assuming sexually active clients are heterosexual
- Suspecting a chatty client asking for an ADHD evaluation is just lazy and wants medication to make things easier
- Assuming someone without a visible disability is able-bodied (30)
Over time, these negative connotations can create dissatisfied clients or more considerable repercussions like missed diagnoses, lack of clear communication, delayed treatment, and reduced quality of care and outcomes.
To deliver culturally competent care, individual clinicians and institutions must assess for and identify biases and the ways they have shaped healthcare. On a personal level, this can be done through self-reflection, attending training or workshops, and working or volunteering with populations that challenge one's biases or are different from one's own.
On an institutional level, clinics and hospitals should monitor client data and assess for gaps and trends in those gaps. They may also poll clients on satisfaction with care or suggestions for improvement and ensure that staff demonstrate compliance with implicit bias and cultural competence training (30).
There is much more to be explored with implicit bias. Still, for the scope of this course, it is essential to introduce the concept and for readers to keep this in mind while further exploring groups that experience the most health-related disparities.

Self Quiz
Ask yourself...
- Think about the difference between implicit and explicit bias. Why is this distinction important when delivering patient care?
- How might implicit bias influence the quality of care you deliver, even if it is a positive bias?
- Why do you think it is essential to recognize your thoughts and attitudes are not objective? How does this recognition affect cultural competence?
- Are there any systematic changes your healthcare facility could make to address implicit bias?
- What are some potential challenges to clinicians engaging in self-reflection about implicit biases?
Race & Ethnicity
One of the most significant disparities in healthcare, and the one garnering the most attention and campaigns for change in recent years, is race and ethnicity. However, when covering the best practices for cultural competence in nursing, we must go over this topic. Studies in recent years have revealed that minority groups, particularly Black Americans, are sicker and die younger than white Americans. Examples include:
Current data shows that Black men are more likely to be diagnosed with prostate cancer and 2.2 times more likely to die from it than their white peers. Black men are also diagnosed at a younger age, about two years earlier, yet less likely to be screened or treated aggressively than white men.
Lillard et al.(2022) explored the demographic, health literacy, and population trends impacting the differences in identifying and treating this condition. They found many contributing differences in the way Black men receive and engage with healthcare (16). Among the most impactful differences were cultural mistrust of the healthcare system, poor physician-patient communication, undereducation about prostate cancer within the Black community, and lack of access to care (both geographic and financial) for Black men (16).
A 2020 study found that Black individuals over age 56 experience a decline in memory, executive function, and global cognition at a rate much faster than their white peers, often as much as 4 years ahead in terms of cognitive decline. Data in this study attribute the difference to the cumulative effects of chronically high blood pressure, more likely to be experienced by Black Americans (14).
Black women experience twice the infant mortality rate and nearly four times the maternal mortality rate of non-Hispanic white women during childbirth. One in five Black and Hispanic women report poor treatment during pregnancy and childbirth by healthcare staff. Studies indicate that in addition to biases within the healthcare system, some of these poor outcomes may also be attributed to cumulative effects of lifelong inferior healthcare (15).
Lack of health insurance keeps many minority patients from seeking care at all. 25% of Hispanic people are uninsured and 14% of Black people, compared to just 8.5% of white people. This leads to a lack of preventative care and screenings, a lack of management of chronic conditions, delayed or no treatment for acute conditions, and later diagnosis and poorer outcomes of life-threatening conditions (2).
Emerging data indicates that hospitalizations and deaths from COVID-19 are disproportionately affecting Black and Hispanic Americans, with Black people being 153% more likely to be hospitalized and 105% to die from the disease than white people. Hispanic people are 51% more likely to be hospitalized and 15% more likely to die from COVID-19 than white people (18).
There are many potential reasons, from genetics to environmental factors such as socioeconomic status. However, data repeatedly shows that these factors are not enough to account for the disproportionate health outcomes; it eventually comes down to inequity in the structure of the healthcare systems in which we all live. For example:
Medical training and textbooks are mostly commonly centered around white patients, even though many rashes and conditions may look very different in patients with darker skin or different hair textures (9).
There is also a lack of diversity in physicians; in 2018, 56.2% were white, while only 5% were Black and 5.8% Hispanic. More often than not, patients will see a physician of a different race than they are, which can mean their particular experiences as a minority person and how that relates to their health are not well understood by their physician (1).
While the Affordable Care Act increased the number of people who have access to health insurance, minority patients are still disproportionately uninsured, which leads to delayed or no care when necessary (2).
Minority patients are also often those living in poverty, which goes hand in hand with crowded living conditions and food deserts due to outdated zoning laws created during times of segregation. This means less access to nutritious foods, fresh air, or clean water, which negatively affects health (18).
Potential solutions to these problems are in the works across many fronts, but the breakdown and resetting of old institutions will likely require change on a broader political level.
Medical school admission committees could adopt a more inclusive approach during the admission process. For example, they should pay more attention to the background and perspectives of their applicants and the circumstances/scenarios they came from as opposed to their involvement in extracurriculars (or lack thereof) and former education.
Incentivizing minority students to choose careers in healthcare and investing in their retention and success should become a priority in the admissions process (9). This is one of the main drivers and only possible paths to having minority representation in healthcare systems nationwide.
Properly training and integrating professionals like midwives and doulas into routine antenatal care and investing in practices like group visits and home births will give power back to minority women while still giving them safe choices during pregnancy (15).
Universal health insurance, basic housing regulations, access to grocery stores, and many other socio-political changes could also help close the gaps in accessibility to quality healthcare, which may vary by geographic location.


Self Quiz
Ask yourself...
- When you have a medical appointment, how do you get there?
- How do you pay for the services?
- Do you have a provider that understands your unique needs?
- How might the answer to those questions vary for someone of a different race living in the same town?
- How might having a healthcare provider of the same race impact a client's healthcare experience?
LGBTQ+
Another highly at-risk group for healthcare inequity are members of the Lesbian, Gay, Bisexual, Transexual, and Queer (LGBTQ+) community. When practicing cultural competence in nursing, the provider must know that this population is vulnerable, especially in healthcare settings. Risks and examples of disparities within the LGBTQ+ community include:
- Youth are 2-3 times more likely to attempt suicide.
- More likely to be homeless.
- Women are less likely to get preventative screenings for cancer.
- Women are more likely to be overweight or obese.
- Men are more likely to contract HIV, particularly in communities of color.
- Highest rates of alcohol, tobacco, and drug usage
- Increased risk of victimization and violence
- Transgender individuals are at an increased risk for mental health disorders, substance abuse, and suicide and are more likely to be uninsured than any other LGBTQ+ individuals (12)
Current data suggests that most of the health disparities faced by this group of people are due to social stigma, discrimination, lack of access or referral to community programs, and implicit bias from providers, leading to missed screenings or care opportunities.
Support systems and social acceptance are strongly linked to the mental health and safety of these individuals. Lack of support and acceptance in the home, workplace, or school leads to adverse outcomes. Also, a lack of social programs to connect LBGTQ+ individuals and build a community of safety and acceptance creates further gaps.
There is currently still discrimination in access to health insurance and employment for this population, which can affect the accessibility of quality health care as well as affordable coverage.
Following this, a compilation of recent data showcases significant issues with the quality and delivery of care provided to those in the LGBTQ+ community. This data includes:
- A 2022 study of the healthcare experiences of LGBTQ+ individuals revealed
- 18% admit to avoiding medical care due to fear of discrimination over gender identity.
- 22% of transgender individuals have avoided healthcare for fear of discrimination
- 31% of transgender individuals did not have a primary healthcare provider at all (27)
- The same study found that, upon chart review of 1376 healthcare facilities and nearly 26 million patients, 77.1% did not have a sexual orientation or gender identity documented in the health record (2022).
- A 2023 nationwide survey found that 80.6% of endocrinologists and 82.5% of emergency providers reported never receiving any training about caring for transgender patients, despite 80% and 88%, respectively, reporting having transgender patients on their caseload (29).
- The same study revealed that 79% of nurses in the San Francisco area reported never receiving LGBTQ training despite regularly encountering LGBTQ+ patients in their work setting (29).
To improve these conditions and close the gap for LGBTQ+ individuals, much can be done on the community level and in medical training:
- Community programs should be available to create safe spaces for connection and acceptance.
- Laws and school policies can focus on how to prevent and react to bullying and violence against LGBTQ+ individuals.
- Cultural competence training in medical professions needs to include LGBTQ+ issues.
- Data collection regarding this population needs to increase and be recognized as a medical necessity, as it is currently largely ignored.
Providers must stay current on changes and health trends among LGBTQ+ populations, as healthcare delivery methods may require adjustments over time; this is critical when learning about cultural competence in nursing.
Understanding these risk factors is essential for healthcare professionals, and addressing implicit biases is necessary to help close gaps in care for this population. At the root of many of the biases regarding LGBTQ+ clients is a lack of understanding or cultural competence when caring for people in this community. Healthcare professionals need to familiarize themselves with the definitions and differences in sexuality, gender identity, and the many terms within those categories to have a better understanding of how these factors affect the health and safety of clients. The following list should provide a basic understanding and clarification for healthcare professionals working towards greater comfort in caring with this population:
- Sex: A label, typically of male or female, assigned at birth, based on the genitals or chromosomes of a person. Sometimes, the label is "intersex" when genitals or chromosomes do not fit into the typical categories of male and female. This is static throughout life, though surgery or medications can attempt to alter physical characteristics related to sex.
- Gender: Gender is more nuanced than sex and is related to socially constructed expectations about appearance, behavior, and characteristics based on gender. Gender identity is how a person feels about themselves internally and how this matches (or doesn't) the sex they were assigned at birth. Gender identity is not related to who a person finds physically or sexually attractive. Gender identity is on a spectrum and does not have to be purely feminine or masculine; it can also be fluid and change throughout a person's life.
- Cis-gender: When a person identifies with the sex they were assigned at birth and feels innately feminine or masculine.
- Transgender: When a person identifies with the opposite sex they were assigned at birth. This can lead to gender dysphoria or feeling distressed and uncomfortable when conforming to expected gender appearances, roles, or behaviors.
- Nonbinary: When a person does not feel innately or overwhelming feminine or masculine. A nonbinary person can identify with some aspects of both male and female genders or reject both entirely.
- Sexual orientation: A person's identity about who they are attracted to romantically, physically, and sexually. This can be fluid and change over time, so do not assume a client has always or will always identify with the same sexual orientation throughout their life.
Types of sexual orientation include:
- Heterosexual/Straight: Being attracted to the opposite sex or gender as oneself
- Homosexual/Gay/Lesbian: Being attracted to the same sex or gender as oneself.
- Bisexual: Being attracted to both the same and opposite sex or gender as oneself
- Pansexual: Being attracted to any person across the gender spectrum, including non-binary people

Self Quiz
Ask yourself...
- Think about a patient you have cared for that did not come in with a significant other. Did you make any assumptions about that client’s sexual orientation or gender identity?
- Would there have been different risk screenings you needed to perform if they were part of the LGBTQ+ community?
- Think about what you know about psychological development during the teenage years. Why do you think suicide risk is so much higher among LGBTQ+ youth?
- Why do you think a robust support system is protective against suicide in this population?
- What is your experience or comfort level caring for transgender clients, and how do you think it impacts your care?
- What protocols could healthcare facilities implement to improve culturally competent care for this population?
Gender & Sex
Gender and sex play a significant role in health risks, conditions, and outcomes due to a combination of factors, including biological, social, and economic elements. Among the differences in health data related to gender are:
- Women are twice as likely to experience depression than men across all adult age groups (13).
- About 12.9% of school-aged boys are diagnosed and treated for ADHD, compared to 5.6% of girls, though the actual rate of girls with the disorder is believed to be much higher (5).
- A 2021 study showed that older women have a higher frailty index (69%) compared to older men (61%) (19).
- Heart disease is the leading cause of death in women, yet women are shown to have lower treatment rates for heart failure and post-heart attack care, as well as lower prevalence but higher death rates from hypertension than men (3).
It is also essential to differentiate gender and sex when practicing cultural competence in nursing.
Sex is the biological and genetic differentiation between males and females, whereas gender is a social construct of differences in societal norms or expectations surrounding men and women. Knowing this differentiation is essential for someone looking to better practice cultural competence in nursing and provide equitable and inclusive care.
Some health conditions are undeniably attributable to the anatomical and hormonal differences of biological sex; for example, uterine cancer can only be experienced by those who are biologically female. However, many of the inequalities listed above disproportionately burden women due to the social and economic differences they encounter in society; for example, 1 in 4 women experience intimate partner violence as compared to 1 in 9 men (20).
What are the reasons for this? A lot of it has to do with how women are perceived in society, how their symptoms may present differently than their male counterparts, or how their symptoms are presented to and received by medical professionals.
- For centuries, any symptoms or behaviors that women displayed (primarily mental health-related) that male doctors could not diagnose fell under the umbrella of hysteria. The recommended treatment for this condition was anything from herbs, isolation, sex, or abstinence, and it is only in the last one hundred years or so that more accurate medical diagnoses began to be given to women. Hysteria was not deleted from the DSM until 1980 (26).
- Nair found that women were more verbose in their encounters with physicians and may not be able to fit all of their complaints into the designated appointment time, leading to a less accurate understanding of their symptoms by their doctor (19).
- A 2024 article notes that 40% of women felt rushed through doctor appointments or their concerns were not fully addressed (23).
- Symptoms of mental health disorders like ADHD may look different in girls than in boys. Girls with difficulty focusing may be categorized as "chatty" or "daydreamers" by teachers. In contrast, boys are more likely to draw attention for being hyperactive or disruptive when both are experiencing symptoms of ADHD and could benefit from treatment (7).
The way that teachers, doctors, and nurses view and respond to girls and women must be adjusted to close these gaps and ensure equitable care for men and women.
- Children who are struggling in school should be examined more comprehensively, and differences in learning styles should be widely understood.
- Screening questionnaires and standard preventive care are used when caring for clients in primary care.
- Social services should be utilized to help determine whether women are neglecting their own healthcare needs due to responsibilities at home.
- Medical professionals must be trained in the history of inequality among women, particularly regarding mental health, and proper, modern diagnostics must be used.
- The differences in communication styles of men and women should be understood when caring for patients.

Self Quiz
Ask yourself...
- Think about a patient you cared for recently and how they communicated their needs and symptoms to you. How might this have differed if they had been a different gender?
- In what ways do you think the history of “hysteria” in women may still be subtly present today?
- Why do you think it is essential for nurses to understand and address the differences between sex (biological) and gender (social construct)?
- Why might women’s symptoms be underrecognized or misdiagnosed compared to men’s symptoms, particularly for mental health conditions?
- What societal or historical factors surrounding women's health have impacted how women are perceived and treated in healthcare? How might those influences still be affecting today's healthcare system?
- How do you think having a care provider of the same gender may impact a client's care or even their perception of their care?
Religion
Religion can impact when patients seek care, which treatments they will participate in, and how they perceive their care. Even advanced technology in healthcare can be perceived as unsatisfactory if it violates the religious preferences of patients. Hence, healthcare professionals must know specific religious preferences to provide the most competent and sensitive care possible. Consequences of culturally incompetent care include:
- Adverse health outcomes due to not participating in care that violates their religious beliefs.
- Patient relationships with healthcare professionals can suffer if they feel disrespected or misunderstood, causing patients to delay or avoid seeking care altogether.
- Dissatisfaction with care can even lead to long-term trauma surrounding significant events like birth, death, or chronic disease if a patient feels uninvolved or disrespected in their care (28).
Many religions have different practices and ordinances, but we will cover some more central and common implications regarding health practices here. Typically, views on pregnancy/birth, death, diet, modesty, and treatment for illness are the most critical areas for healthcare professionals to understand. Providers must continue to educate themselves on the practices and preferences of various religions; it is essential to practicing cultural competence in nursing.
Disclaimer: Each religion has many variations, and not all practices may be the same. The following information has been sourced from "Cultural Religion Competency in Clinical Practice," written by Drs. Diana Swihart, Siva Naga S. Yarrarapu, and Romaine L. Martin (Swihart).
Buddhism
They study and meditate on life, cause and effect, and karma, working towards personal enlightenment and wisdom. They believe the state of mind at death determines their rebirth and prefer a calm and peaceful environment without sedating drugs. They have ceremonies around birth and death. Their diet is usually vegetarian (28).
Christian Science
Based on the belief that illness can only be healed through prayer, they typically choose spiritual healing for disease or illness prevention and treatment. They often refuse vaccines and delay treatment for acute illnesses. They avoid tobacco and alcohol but have no other dietary restrictions (28).
The Church of Jesus Christ of Latter-Day Saints/Mormon
Heavily family-oriented, family involvement in major health/life events is essential—strict abstinence outside of heterosexual marriage. Fasting is required monthly, but it is exempt during illness. Blood or blood products are accepted. Abortion is prohibited unless it is a result of rape or the mother's life is in danger. Two elders present to bless those ill or dying (28).
Hinduism
It centers on leading a life that allows you to reunite with God after death. Believes in reincarnation, so the environment around dying people must be peaceful. The presence of family and priests during the end of life is preferable. After death, the body is washed and not left alone until cremated. Euthanasia is forbidden. Often vegetarian, the right hand is used for eating (28).
Islam
Belief in God and the prophet Abraham. Prayer is required five times daily. Observe Ramadan, a month of fasting and abstinence during daylight (children and pregnant women are exempt from fasting). Autopsies should only be performed if legally necessary. Must eat clean, halal food, excluding pork, shellfish, and alcohol. Female patients require female healthcare providers. Abortion is prohibited (28).
Jehovah’s Witness
Belief destruction of the present world is coming, and faithful followers of God will be resurrected. Do not celebrate birthdays or holidays. I believe death is a state of unconscious waiting. Euthanasia prohibited. Refuse blood and blood products. Abortion is prohibited. Pregnancy through artificial means (IUI, IVF) is not permitted (28).
Judaism
Belief in an all-powerful God and varying levels of interpretation/observance of laws and traditions. Cremation is discouraged or prohibited. Prayer is essential for the sick and dying; after death, the body is not left alone. Must eat kosher foods, excludes pork. Amputated limbs must be saved and buried where the person will one day be buried. Abortion is allowed in certain circumstances (28).
Protestant
Christian faith formed in resistance to Roman Catholicism. Autopsy and organ donation are acceptable. Euthanasia is not sufficient. There are no restrictions on diet or traditional Western medicine treatments (28).
Roman Catholicism
Christian faith is steeped in tradition and observance of sacraments. The clergy is present at the end of life for the sacrament of Last Rites. Avoid meat on Fridays during Lent. Mass and Communion on Sundays are obligations, and they may require a clergy member to visit during hospitalization. Abortion and birth control (other than natural family planning) are prohibited. Artificial conception is discouraged. Newborns with a grave prognosis need to be baptized (28).
To better practice cultural competence in nursing and improve the quality of care given that respects a patient’s faith and religious boundaries, one should focus on:
- Understanding fundamental differences and preferences between various religions and providing staff training is essential.
- We are encouraging families to participate in health decision-making where appropriate.
- We are providing interpreters where needed.
- Promoting an environment that allows clergy, healers, or other religious figures of comfort to visit and participate in care if desired.
- Providing dietary choices that are considerate of religious nutritional preferences.
- Recruiting staff that are minorities or of various religions.
- Respecting a client's views on controversial topics such as pregnancy/birth, death, and acceptance or decline of treatments, even if it conflicts with staff members' own beliefs (28).


Self Quiz
Ask yourself...
- Imagine you work on a maternity unit and are caring for a new mother who observes the Islamic faith. What needs might she have to feel respected and comfortable with her care?
- You are caring for a patient in the critical care unit who is a Jehovah's Witness. In what ways might this client's faith impact their care?
- How might the level of respect for a client's religious beliefs affect how they perceive their care, regardless of health outcomes?
- What challenges might occur if a client's religious practices conflict with standard medical practices, and how can you navigate such a situation?
- Suppose you have a different perspective on topics like pregnancy, death, or treatment of medical conditions than your client. Why is it important to remain nonjudgmental and not express your views?
Case Study
Scenario
Mr. Nadir is a 46-year-old male patient admitted to the hospital for postoperative pain management following a surgical hernia repair. Mr. Nadir practices Islam and expresses concern about halal foods that are free from pork or alcohol. He is also currently observing Ramadan and fasting during the day.
Culturally competent approach to care
The nurse assigned to Mr. Nadir includes his religious needs and dietary requirements in his chart. The nurse contacts the pharmacy and ensures that all his ordered medications meet halal guidelines. Acceptable foods are also ensured to be available during times when Mr. Nadir can break his fast. The nurse also arranges care around his prayer schedule. He is encouraged to contact a religious leader if he needs further guidance or information about medical exemptions that may be acceptable during his hospitalization.
Outcome
Mr. Nadir feels understood and respected, which reduces his anxiety about the hospital stay. The nursing staff, pharmacy, and nutrition services take a collaborative approach, ensuring that he can receive necessary medical care without compromising his religious beliefs. He expresses satisfaction with the care he received.

Self Quiz
Ask yourself...
- What problems might have arisen if Mr. Nadir did not express his religious needs and the nurse did not ask?
- What hospital policies or protocols could be in place to prevent information like this from going unrecognized?
- How might ignoring or being unable to accommodate Mr. Nadir’s needs during his hospitalization impact his overall trust in the healthcare system?
- How will this experience likely impact Mr. Nadir’s future willingness to seek care when he needs it?
- What resources could be used to support patients like Mr. Nadir?
Age
As the Baby Boomer generation ages, there is a growing number of older adults in the U.S. In 2016, 73.6 million adults over 65 were expected to grow to 77 million by 2034. As of 2016, 1 in 5 older adults reported experiencing ageism in the healthcare setting (25). As the number of older adults needing healthcare expands, the issue of ageism must be addressed. For providers looking to improve cultural competence in nursing practices, ageism must be addressed as it flies under the radar. Ageism is defined as stereotyping or discrimination against people simply because they are old. Ways in which ageism is present in healthcare include:
- Dismissing is a treatable condition as part of aging.
- Overtreating natural parts of aging as though they are a disease.
- Stereotyping or assuming a patient's physical and cognitive abilities purely based on age.
- Providers who are less patient, responsive, and empathetic to patients' concerns talk down to patients or do not explain things because they believe them to be cognitively impaired.
- Elderly patients may internalize these attitudes and seek care less often, forgo primary or preventative screenings, and have untreated fatigue, pain, depression, or anxiety.
- Signs of elder abuse may be ignored or brushed off as easy bruising from medication or being clumsy (25).
There are many reasons why ageist attitudes in healthcare may occur, including:
- Misconceptions and biases among staff members, particularly those who have worked with a frail older population, assume all older adults are frail.
- Lack of training in geriatrics and the needs and abilities of this population.
- Standardizing screenings and treatments by age may help streamline the treatment process but can lead to stereotyping.
- Changing this process and encouraging an individual approach may be resisted by staff and viewed as less efficient.
To combat ageism and make sure healthcare is appropriately informed to provide respectful, equitable care:
- Healthcare professionals can adopt a person-centered approach rather than categorizing care into groups based on age.
- Facilities can adopt practices that are standardized regardless of age.
- Facilities can include anti-ageism and geriatric-focused training, including training about elder abuse.
- Healthcare providers can work with their elderly patients to combat ageist attitudes, including internalized ones about their abilities (25).
Although it does not always appear first in a conversation regarding cultural competence in nursing

Self Quiz
Ask yourself...
- Have you ever cared for two patients of the same age who seemed drastically different in their overall health and independence? Why do you think that is?
- Think about your attitudes about older adults. What biases or assumptions do you have about the cognitive and physical abilities of people who are 65? 75? 85?
- What can healthcare providers do to ensure equitable treatment of clients, regardless of age?
- How can healthcare providers empower older adults to advocate for their health and needs?
- What challenges may arise for a healthcare facility implementing practices to reduce ageism?
Veterans
Veterans are a unique population that faces many health concerns that are unique to the conditions of their time in service. Much of veteran health care is provided through the Veteran Affairs (VA) facilities, a nationalized form of healthcare involving government-owned hospitals, clinics, and government-employed healthcare professionals. Again, this course aims to educate providers on how to practice cultural competence in nursing; however, let's introduce the disparities found within this population by utilizing a few statistics.
- 1 in 5 veterans experience persistent pain, and 1 in 3 veterans have a diagnosis related to chronic pain (4).
- Approximately 12% of veterans experience symptoms of PTSD in their lifetime, compared to 6% of the general population, and 80% of those with PTSD also experience another mental health disorder such as anxiety or depression (4).
- More than 1 out of every 10 veterans experiences some substance use disorder (alcohol, drugs), which is higher than the rate for non-veterans (4).
- From 2022 to 2023, there was a 7.4% increase in homeless veterans (8).
- Veterans account for 20% of all suicides in the U.S., despite only about 8% of the U.S. population serving in the military (4).
- Disparities also exist within the veteran population and veterans who are of a minority race or female experience these issues at an even higher rate.
- For example, veteran women are more likely to experience homelessness than veteran men (8).
The causes of these troubling issues for veterans are multifaceted; some of them relate to the nature of work in the U.S. Military and increased exposure to trauma (particularly with those involved in combat), and some of them relate to the care of veterans, and their mental health during and after their service.
- 87% of veterans are exposed to traumatic events at some point during their service (4).
- Current data suggests fewer than half of eligible veterans utilize VA health benefits.
- For some, this means they are receiving care at a non-VA facility, and for others, it means they are not receiving care at all.
- Care at civilian facilities involves healthcare professionals who may not fully understand veteran issues (24).
- Less than 50% of veterans returning from deployment receive any mental health services (21).
All service members exiting the military must participate in the Transition Assistance Program (TAP), an information and training program designed to help veterans transition back to civilian life, either before leaving the military or retiring. The program is evaluated annually for effectiveness and includes components about skills and training for civilian jobs and individual counseling regarding plans after exit.
- Adding or strengthening components of TAP surrounding mental health care and utilization of VA healthcare services would be beneficial and help reduce disparities.
- Changing the military culture surrounding mental health to strengthen and mandate training and using debriefing for active-duty military could also be beneficial.
- Incentivizing the usage of the VA healthcare system for routine preventative and mental healthcare would help reach more veterans who may be in need.
- Additional training for healthcare professionals working within the VA with an emphasis on mental health disorders would ensure high-quality care for veterans utilizing their services.


Self Quiz
Ask yourself...
- The Transitional Assistance Program was established in 1991. How do you think veterans' experiences of leaving or retiring from the military differed before and after this program was established?
- In what ways do you think that trauma is the catalyst for many of the other veteran-specific issues they experience?
- How could trauma better be handled for these patients to reduce their risk of all the other related issues?
- What are some specific challenges that are unique to caring for veterans?
- What protocols do you think healthcare facilities could implement to reduce health disparities in veterans?
Mental Illness & Disability
Disabilities have emerged as an under-recognized risk factor for health disparities in recent years, and this new recognition is a welcome change as more than 18% of the U.S. (15) population is considered disabled. Disabilities can be congenital or acquired and include conditions that people are born with (such as Down Syndrome, limb differences, blindness, deafness), those presenting in early childhood (Autism, language delays), mental health disorders (bipolar, schizophrenia), acquired injuries (spinal cord injuries, limb amputations, change in hearing/vision), and age-related issues (dementia, mobility impairment).
Public health surveys vary from state to state. Still, most categorize a condition as a disability based on the following: 1) blindness or deafness in any capacity at any age, 2) severe difficulties with concentrating, remembering, and decision-making, 3) difficulty walking or climbing stairs, 4) difficulty with self-care activities such as dressing or bathing, 5) and difficulty completing errands, such as going to an appointment, alone over the age of 15 (17).
Health disparities affecting people with disabilities can include the way they are recognized, their access and use of care, and their engagement in unhealthy behaviors. To practice cultural competence in nursing, understanding the disparities that those with disabilities face is essential.
- Due to variations in the way disabilities are assessed, the reported prevalence of disabilities ranges from 12% to 30% of the population (17).
- People with disabilities are less likely to receive needed preventative care and screenings (6).
- 1 in 6 disabled adults have not had a routine health check within the last year (6)
- 1 in 4 adults do not have a regular health care provider (6)
- People with disabilities are at an increased risk of chronic health conditions and have poorer outcomes (10).
- 40.5% of disabled adults are obese compared to 30.3% of adults without disability
- 10.4% of disabled adults have heart disease compared to 3.7% of non-disabled adults
- 16.6% of disabled adults have diabetes compared to 7.9% of non-disabled adults (6)
- People with disabilities are more likely to engage in unhealthy behaviors such as cigarette smoking and lack of physical exercise than people without disabilities (10).
Many of the health differences between those with and without disabilities come down to social factors. Compared to non-disabled people, individuals with disabilities are:
- Less likely to finish high school
- Less likely to maintain steady employment
- Less likely to have at-home access to the internet
- Have a lower annual income
- Have adequate health insurance coverage (6)
If access to necessary preventive and acute health care is to be increased for those with disabilities, much must be changed regarding the social determinants affecting this population. Community, state, and federal policy changes will be needed to provide the social and economic support these people need. Potential solutions include:
- Streamline and standardize the process of identifying people with disabilities so they can be eligible for assistance as needed.
- School programs to help people with disabilities graduate and find jobs within their ability level.
- Community participation ensures transportation, buildings, and facilities are accessible to all.
- Make internet access an essential and affordable utility, like running water and electricity.
- Address the inequities in health insurance accessibility and coverage.
- Provide social and economic support programs for parents of children with disabilities and provide transitional support as those children become adults (10).

Self Quiz
Ask yourself...
- Have you ever cared for a patient with a severe disability? Consider how even getting to the clinic or hospital where you work might be different or more challenging than for patients without a disability.
- What resources for people with disabilities are available in your community?
- How might those resources vary in surrounding areas?
- How might addressing social determinants of health (socioeconomic status, education level, neighborhoods, etc) improve health outcomes for people with disabilities?
- Why is it important to standardize the identification process, and how could this impact access to care for clients with disabilities?
Case Study
Scenario
Mrs. Donaldson is an 82-year-old woman who presents to her primary care provider with complaints of stiffness in her arms and legs, difficulty with balance, and a fine tremor in her right hand when playing piano at church. She reports feeling tired and slower in her movements lately.
Her primary care provider discusses typical signs of aging with her and recommends increasing physical activity, sleep hygiene, and a balanced diet. No further diagnostic workup is done.
Over the next 4 months, her symptoms worsen. The tremor becomes much worse, and she begins to have difficulty completing daily tasks. Her family encourages her to seek a second opinion, so she schedules an appointment with a neurologist who diagnoses her with Parkinson's disease.
Outcome
Because of her primary care provider’s assumption that her symptoms were due to Mrs. Donaldson’s advancing age, her diagnosis was delayed by several months, disrupting her quality of life and ultimately reducing the outcomes of her treatment.
Culturally competent alternative
Parkinson's presents subtly and may sometimes be mistaken for natural aging processes. Further evaluation, like a neurological exam, imaging, or additional testing, would have revealed a more severe diagnosis and given Mrs. Donaldson the prompt treatment she needed. Even if advancing age is a potential differential diagnosis, it should only be assumed to cause further workup.

Self Quiz
Ask yourself...
- How might this experience impact Mrs. Donaldson’s trust in the healthcare system?
- What steps could have been taken at Mrs. Donaldson’s initial visit to ensure she received a more thorough evaluation?
- How do you think implicit bias impacts the diagnosis of conditions like Parkinson's that typically affect older adults?
- Even though Mrs. Donaldson eventually received the correct diagnosis, how do you think her scenario might have been different if she had received a more thorough assessment at her first encounter for these symptoms?
- What role did patient advocacy (by the patient or her family) play in this scenario?
Conclusion
In short, cultural competence in nursing means that although a provider may not share the same beliefs, values, or experiences as their patients, they understand that to meet their needs, they must tailor their care delivery. Nurses are patient advocates, and they must ensure they provide equitable and inclusive care to all populations.
However, cultural competence in nursing is ever-changing, and it is the provider's responsibility to stay up-to-date to offer the best patient experience.
Connecticut Mental Health Conditions
Introduction
Mental health conditions are common in the United States, with one in five adults suffering symptoms ranging from mild to severe each year. Despite this fairly high prevalence, 2020 data indicates that only 46% of adults with a mental health condition received medical services related to those symptoms (10). Furthermore, experiencing one mental health disorder increases the risk of developing a second or third disorder by two to three fold (13). Comorbid mental health diagnoses also increase the severity of symptoms, negative impacts on quality of life, and risk of suicidal ideations (3)
Current practices surrounding mental health leave many people at risk of being undiagnosed or untreated and increased awareness and education is needed for medical professionals to help close these gaps in care. This Connecticut mental health training aims to provide a thorough understanding of certain common mental health disorders, how to screen for them and coordinate resources for clients in need, and how to navigate suicide prevention for optimum client safety.
Epidemiology
Every year, millions of people nationwide suffer from mental health related symptoms that impact their ability to work, attend school, maintain relationships, and enjoy their lives. Recent data indicates that one in five United States adults experiences symptoms of mental illness each year and one in twenty experiences severe symptoms (6). One in six United States children experiences mental illness symptoms each year and suicide is the second leading cause of death in the 10-14 year age group (6).
As of 2020, anxiety disorders were the most prevalent, with 19.1% of all US adults experiencing some form of anxiety annually. Depression is next, with a prevalence of 8.4%, Post-traumatic Stress Disorder (PTSD) experienced by 3.6%, and bipolar disorder experienced by 2.8% of adults (6).
There is mild variance among races, with annual prevalence among races outlined as follows:
- Non-Hispanic multiracial people: 35.8%
- Non-Hispanic white: 22.6%
- Non-Hispanic American Indian: 18.7%
- Hispanic or Latino 18.4%
- Non-Hispanic black: 17.3%
- Non-Hispanic Asian: 13.9%
(6)
Women are more likely to experience mental illness than men, with 25.8% of women 15.8% of men reporting symptoms annually (NIH). Being part of the LGBTQ community is one of the greatest risk factors, with 47.4% of LGBTQ people experiencing mental illness (6).
In addition to the factors that increase risk of mental health disorders, experiencing mental health issues also increases other health related risks. Suffering depression increases the risk of cardiovascular and metabolic disorder by 40-50% over the rest of the population, depending on severity. Thirty-two percent of people with mental illness also experience substance abuse disorders, as compared to 10% of the general population (6). The rate of academic struggles and dropping out of school are 2-3 times higher for children and teens with mental health diagnoses, which in part contributes to the higher rates of unemployment (6.4% vs 5.1%) experienced by people with mental health disorders (6). On a more global scale, it is estimated over $1 trillion is lost in productivity due to depression and anxiety disorders each year (6).
On the severe end of mental health consequences is suicide, currently the 12th leading cause of death nationwide (12). Overall, there has been a slight decrease in suicide rates in recent years, declining from 14.2 per 100,000 people annually in 2000 to 13.5 per 100,000 people in 2020 (12). Still, suicide is a devastating problem with twice as many people dying by suicide as homicide in recent years. Risk varies by many demographic factors with men being about 4 times more likely to commit suicide than women across all ages. Among women, suicide rate is highest for those ages 45-64, at 7.9 people per 100,000. And among men, the rate is highest for those age 75 and older, at 40.5 per 100,000. By race, American Indians and White men are significantly more affected (12).
When looking at younger populations, the biggest risk factor seems to be sexuality and gender identity. Gay, Lesbian, and bisexual teens are 4 times more likely to attempt suicide than straight peers and transgender teens are 9 times more likely to attempt suicide than cis-gender peers. Each year, 45% of LBGTQ teens report experiencing serious thoughts of suicide at least once (6).
Despite these serious implications and high rates of prevalence, less than half of affected people receive appropriate, regular mental health services. These statistics are staggering. This is the reason of why the Connecticut Department of Public Health implemented the Connecticut mental health training CE requirement to improve mental health outcomes. Lack of proximity to resources, prescription problems, delayed or canceled appointments, and complications due to the pandemic or even just symptoms causing poor compliance all serve as barriers to appropriate treatment (6). Healthcare professionals are guaranteed to encounter patients with mental health needs no matter what area of healthcare they work in, and universal improvements in education and preparedness to deal with mental health concerns is desperately needed and can serve to improve outcomes for patients everywhere.

Self Quiz
Ask yourself...
-
Think about the population you serve...How often does your job involve assessing the mental health needs of your clients? Given the statistics above, do you think your attention to mental health is sufficient or needs to be increased?
-
If a client you encountered admitted that they were suffering from symptoms of depression or anxiety, what resources are available for you to connect them with? If you are unsure, how could you compile a list of resources?
Signs, Symptoms and Criteria for Common Mental Health Diagnoses
Unless you work specifically in mental health, you may only have a vague understanding of what exactly certain mental health diagnoses mean, how they are treated, or what symptoms your clients are dealing with. A more in depth understanding of how mental health problems present and diagnostic criteria is one of the first steps towards better detection and treatment for vulnerable clients. The Connecticut Department of Public Health added this CE requirement of Connecticut mental health training in order to better serve the patient population.
Depression
Known as Major Depressive Disorder (MDD) or Clinical Depression, this is one of the most common mental health disorders. While this disorder may stereotypically be known as being sad or down, the actual criteria for depression is much more detailed and nuanced (9). According to the Diagnostics and Statistics Manual for mental health (DSM-5), MDD is defined as experiencing at least five of the following symptoms for at least a two week time period and at least one of the symptoms must be one of the first two on the list:
- Sad, depressed, or even flat or detached mood most days, for the majority of the day
- Decreased or lack of interest or pleasure in any activities throughout the day
- Decrease in appetite or significant weight loss without trying to lose weight
- Slowed thought process and movement, noticeable by others
- Fatigue or low energy levels most days
- Feeling worthless or unnecessarily guilty most days
- Decreased ability to think, concentrate, or make decisions most days
- Recurrent thoughts of death, with or without a plan, or thoughts that things would be easier if one was dead (9)
The number, combination, and severity of symptoms will vary by individual. Typically symptoms are severe enough to interfere with a person’s ability to work, attend school, or maintain their relationships as well as they would like. People with depression may also experience excessive worries about their health or increased rates of general physical complaints like headache or abdominal pain. MDD may occur as a single episode, but often occurs in recurrent episodes, lasting for a few weeks to months and then resolving for a period of time before returning. Persistent symptoms lasting two years or more, though often less severe in intensity, is known as dysthymia. Depression can also occur from hormonal changes during or after pregnancy and is known as perinatal depression. Some individuals suffer from depressive symptoms only at certain times of year, typically in the dark and cold months of fall and winter in the northern hemisphere; this is known as seasonal depression (9).
It is important to separate depression from grief which is a response to loss with similar, often overlapping, but distinguishably different from depression symptoms. In grief, there is an identifiable loss, whereas depression can occur without any particular precipitating event (for “no reason”). Grief involves sad or hopeless feelings intermixed with feelings of joy or peace, whereas depression is persistently low mood. Being close to loved ones often offers comfort or healing in grief, but isolation and withdrawing are more common with depression. And with grief, thoughts of death may occur as a person desires to reunite with a deceased loved one, while in depression thoughts of death center around feeling worthless or hopeless and no longer wishing to live (4).
Risk factors for depression include personal or family history of any depressive disorder, certain medical conditions that negatively impact quality of life, or even medications taken for other conditions. Major life events or traumas, including death of a loved one, divorce, moving, job changes, birth of child, abuse, or traumatic events can all increase the risk of subsequent depression (9).

Self Quiz
Ask yourself...
-
How can you differentiate a bad day (or several) with many of the symptoms of depression, from a true diagnosis of MDD?
-
How might someone grieving the loss of a loved one present differently than someone with depression after the same loss?
Anxiety
All people experience worries or stress over things throughout their lives. But anxiety disorders extend beyond normal worries in their frequency and intensity, occurring often enough and at a severity level that interferes with a person’s ability to function at work, school, or in their relationships with others. There are several distinct disorders that fall under the umbrella of anxiety and the differences lie in the triggers and the expression of symptoms, but the criteria of excessive worry is a common theme across all anxiety disorders (8).
Generalized anxiety disorder (GAD) is a common form of anxiety that involves a general sense of dread of anxiousness, typically about anything and everything rather than specific events. People with GAD may feel restless, on edge, have difficulty concentrating, become tired easily, be irritable or have difficulty regulating their emotions, have difficulty sleeping, or have frequent general physical complaints like headaches or stomach aches (8).
Panic disorder involves more extreme physical symptoms of anxiety, known as panic attacks. Sudden, intense bursts of anxiety involving a racing heart, chest pain, shortness of breath, shaking, intense feelings of dread, or an intense desire to flee a situation are considered panic attacks. They may occur in relation to stressful events or for no reason at all. Anyone can experience a panic attack, but experiencing them frequently and being unable to function at work, school, or home because of them is considered panic disorder (8).
Social anxiety disorder is anxiety triggered by situations with people outside of one’s home. This can be people you know, like classmates or extended family, or strangers like cashiers or healthcare professionals. Symptoms include feeling judged or watched by others, racing heart, being unable to speak up or speak clearly to others, avoiding eye contact, or feeling very self conscious (8).
Phobias are anxiety related symptoms that center on a very specific trigger or event. People with phobias will do everything they can to avoid the trigger, including refusing to go to a certain place or leave home. Common phobias include agoraphobia (fear of leaving home), blood, heights, airplanes, vomit or vomiting, certain animals (such as snakes, spiders, or dogs), needles or injections, or separation from parents (for children) (8).
Risk factors for anxiety include exposure to traumatic events (especially early in life), drug or alcohol use, frequent exposure to a stressful environment (at job or school), and family history of anxiety disorders. Certain medications and stimulants like nicotine and caffeine can increase the symptoms of anxiety (8).

Self Quiz
Ask yourself...
-
Have you ever felt so nervous about something that you wanted to stay home or avoid the event altogether? How do you think it might affect your daily life if you felt that same level of anxiety every day?
Post-Traumatic Stress Disorder
Post-Traumatic Stress Disorder (PTSD) is a type of mental health disorder that develops as a response to experiencing a particularly dangerous, scary, or shocking event. An extreme response of “fight-or-flight” during a high stress event is very normal, but many people recover quickly, within a few days to weeks, and do not experience continued distress after the event is over. For other people, the intense symptoms of fear or anxiety continue long after the danger has resolved (11).
Symptoms that occur in response to an identifiable event, last more than a month, and are interfering with a person’s ability to function at work, school, or in relationships are considered to have PTSD. Symptoms include:
- Re-experiencing the event such as through flashbacks or nightmares
- Avoidance symptoms such as staying away from certain people, places, objects, or even music that serves as a reminder of the event
- Arousal symptoms of feeling on edge, angry, tense, easily startled, or having difficulty sleeping
- Cognition and mood symptoms such as difficulty remembering details surrounding the event, negative outlook on the world or about self, feelings of guilt or blame, lack of interest in things
- Children may experience symptoms of regression such as bedwetting or daytime accidents when previously continent, being unable to speak, acting out the event with toys, increased clinginess or fear of separation from parents or caregivers (10)
Risk factors for PTSD include experiencing war (both as a member of the military or a civilian), physical or sexual assault/abuse, car accidents, natural disasters, seeing someone be seriously injured or die, history of mental illness or substance abuse, and having few to no support systems in place during times of stress (11).

Self Quiz
Ask yourself...
-
Have you ever cared for a client who lived through a traumatic event? How did they talk about the event?
-
What sort of feelings or emotions did they seem to experience while discussing their trauma?
Suicide
Suicide by definition is the death of an individual from self-injurious behaviors and the intent to die from those behaviors. Reckless behaviors resulting in unintentional death are not considered suicide because there was no intent to die. People who attempt or commit suicide often feel worthless, hopeless, or that their life is a burden to others and the only escape from their symptoms or guilt is to end their life (12). Warning signs that individuals may be planning or preparing for suicide include increase agitation and substance use, withdrawing from others, researching methods of suicide, stating they have thought about or have the ability to commit suicide, sleeping too much or not at all, giving away possessions or calling/writing letters to say goodbye to loved ones, or a sudden and extreme improvement in depression symptoms (usually from the resolve to commit suicide) (2).
A suicide attempt is any self-injurious behavior engaged in as an attempt to die but which ultimately is non-fatal. Suicide attempts can be actions which do not even result in injury, but if death was the individual’s intent, it is considered a suicide attempt. Suicidal ideations are any thoughts, considerations, or detail planning related to ending one’s own life (12).
The leading method of suicide in recent years is firearms, accounting for more than half of all suicides (11).
Risk factors for suicide include existing mental illness (especially depression, anxiety, bipolar disorder, or schizophrenia), substance abuse problems, terminal health diagnosis (particularly those that are very painful), persistent bullying or relationship problems, unemployment, highly stressful life events like divorce, family history of suicide or personal past attempts, and childhood trauma or neglect. Having access to guns, knives, pills, or other potentially lethal materials increases the risk of suicide as well (2).

Self Quiz
Ask yourself...
- Have you ever cared for a client who was contemplating suicide? What life events had occurred leading up to these thoughts?
Case Study
Jason is a 78 year old male who presents at the Internal Medicine office for his annual physical. When the nurse is collecting vitals, she chats with him about his plans for the summer. He states that he and his late wife used to garden together and he has kept up with it for the last 3 years since her death but this year he does not feel up to planning it or doing the work. The nurse asks if he has other plans for how to occupy his time and he states he usually has a group of friends he gets coffee with twice a week, but he hasn’t been waking up early enough to go to it and has decided to sleep in instead. The nurse documents his vitals and reports off to the physician, attributing his “slowing down” to his advancing age. During the visit, his doctor asks how he is coping with his wife’s loss to which Jason replies, “I’m okay. It never gets easier, but you do get used to it.” The physician orders labs to check his iron levels for fatigue and provides a pamphlet for a support group for widows and widowers at the end of the visit. He recommends Jason follow up in another 3-4 months if his fatigue hasn’t improved.

Self Quiz
Ask yourself...
-
Do you feel confident that the nurse and the physician have a thorough understanding of Jason’s mental health at the end of this visit?
-
What are Jason’s risk factors for mental health diagnoses? What symptoms of depression is he experiencing?
-
How might grief resources fall short of addressing Jason’s symptoms?
Screening
Regardless of which area of healthcare you work in, there will always be clients who are struggling with mental health symptoms, even if that is not their primary reason for seeking care at your facility. Routine and standardized screening for these symptoms can help ensure more clients who need help are identified and prevent many from falling through the cracks. Earlier detection of symptoms ultimately leads to better mental health outcomes as well, so simple and routine screenings serve to improve identification and distribution of care to those in need. Improving mental health outcomes is the primary goal of Connecticut implementing this CE requirement of Connecticut mental health training. So who should undergo screening, when should the screenings occur, and what are some of the best or most common screening tools available?
Let’s start with children since over 50% of all lifetime mental health disorders first appear by age 14.. At every wellness visit, it is recommended to ask general questions about family psychosocial wellness such as childcare resources, availability of food, parent coping with the stressors of parenthood, and normal psychosocial development in the child such as language, eye contact, bonding with family members, play, and age appropriate response to praise and consequences. Families where problems are suspected should be evaluated further. Starting at age 11, the use of more streamlined screening tools is recommended by the American Academy of Pediatrics. The Patient Health Questionnaire (PHQ-9) and/or Pediatric Symptoms Checklist (PSC) should be used annually to detect increased risk of depression, anxiety, or suicidal thoughts. The CRAFFT questionnaire is recommended annually for screening of substance use, starting at age 11. For children who seem anxious or where excessive worries or behavior problems are a concern, a SCARED questionnaire can assess more specifically for anxiety disorders (1).
Once into adulthood, the PHQ-9 is still a reliable and easy to use tool and should be administered at all annual wellness visits. The General Anxiety Disorder (GAD-7) tool is also quick to administer and can pick up on clients who may be experiencing excessive worries (5). In more acute settings like urgent cares or emergency departments, a simple screening question such as “Do you feel safe at home?” can determine situations that may need acute interventions for clients who may not be receiving regular primary care.
In addition to annual screening, healthcare providers should be aware of life events that may increase a person’s risk of experiencing a mental health disorder and perform additional screening as needed. In obstetrics and gynecology settings, women should be screened throughout pregnancy and postpartum for perinatal mood disorders using an Edinburg Questionnaire. Pediatric offices can also screen mothers of infant clients since women often see their child’s pediatrician much more frequently than their own obstetrician or midwife (5). Older adults are more likely to be experiencing declining health, chronic medical diagnoses, or life events such as retirement or the loss of a spouse that increase their risk of depression or anxiety. Assuming their age alone is the cause of certain symptoms should be avoided, while energy and activity levels may indeed decline in later life, a lack of interest or pleasure in things or feelings of hopelessness are not normal signs of aging and should not be brushed off. Updated information on recent life events is important and increased screening should be done accordingly. War veterans, disaster or abuse survivors, and others may find themselves seeking care for physical symptoms related to trauma, but their mental health should be considered and assessed immediately after the event as well as regularly for several months afterwards (5).

Self Quiz
Ask yourself...
-
Think about the population you work with. What factors (age, life stage, general health) put them most at risk for mental health symptoms?
-
What screening questionnaires, if any, do you routinely use at your facility? What additional screening tools could you use to improve your detection rates?
Taking Action
The next step in closing the gap for early detection of mental health disorders is knowing what to do when clients screen positive or when they come to you specifically with a mental health concern or symptoms. A primary goal of the Connecticut mental health training is to prepare nurses with the knowledge and resources needed to get paitents on the right plan of care. Many facilities are surprised once they begin screening, just how many clients present with positive results or the need for further help.
The first thing to do is gather more information directly from the client. Ask about symptoms they have been feeling, how long it has been going on, recent life events that may be contributing to these feelings, and ways in which the symptoms have been impacting their performance at work, in school, or in other aspects of life. Gather a family history that focuses specifically on mental health disorders to better assess disorders for which a client is at risk. Determine the client’s overall safety; the best way to do this is to ask directly if they are having thoughts of wanting to harm themselves or others. This will help determine if intervention is needed urgently or if a more routine connection with resources is appropriate (2).
Once more thorough information has been gathered about a client’s particular scenario, providers can determine the best course of action and what resources to connect them with. It is useful for facilities to have a list of resources available. Appropriate resources include providers who can diagnose and prescribe treatment for mental health disorders (this can often be done in primary care settings, but specialists like psychiatry may be more appropriate), therapists or counselors, group therapies or support groups with common themes, and crisis resources like suicide hotlines or facilities that can be accessed 24/7 in the event of a crisis. When connecting clients with resources, plan for appropriate follow up as well to ensure they received the help they needed (2).

Self Quiz
Ask yourself...
-
What resources are available in your area for routine therapy or counseling? Are there any support groups that you know of for grief or loss, LGBTQ people, or veterans?
-
How do you think it might make a client feel if they admitted to struggling with depression or anxiety and were not given any resources or next steps at the end of their experience at your facility?
-
What are the risks involved with not appropriately addressing their symptoms at the time of care?
Suicide Prevention
On a broad scale, healthcare professionals can participate in suicide prevention by advocating for screening and early detection of mental illness, as well as identifying risk factors and protective factors for their clients to determine who may need connection with available resources. On a community health level, strengthening available resources and the community’s access to them can promote social change needed for prevention (7).
On a more individual level, familiarity with what to do when encountering suicidal clients is always useful, though the actually frequency at which you encounter such clients may vary greatly depending on where you work. If you have concerns or a client fails a screening tool, it is always okay to ask them outright if they have thoughts of wanting to hurt themselves. It is a myth that asking someone this will give them the idea and no studies indicate asking this would contribute to suicide risk. If a client indicates they are having thoughts of suicide or self harm, the next steps should be to determine how often these thoughts are occurring and if they have a plan. It can feel awkward to ask these types of questions, but it is extremely important for client safety and studies indicate that most people would like the help and support extended to them. If they admit to having a plan, the next step is to determine if they have the means to enact the plan. If they say they want to take a lethal dose of pills, determine what medicines they have available to them; if they say they have thought about using a firearm, determine if firearms and ammunition are accessible to them (7).
Clients with an active plan and the means to enact said plan will need crisis intervention and likely involuntary hospital admission. Anyone with thoughts of suicide, even passive ones with no plan, will require further evaluation with a counselor or provider experienced in mental health. Specific plans moving forward for these clients is beyond the scope of this course, but often involve the development of Safety Plans, initiation of psychiatric medication, and connection with resources such as individual or group therapists. The important thing for healthcare professionals in general is to be able to determine when clients are a risk to themselves or others and ensure they are connected with resources before leaving your care (7). This is what the Connecticut Department of Public Health wants to educate nurses on and is why they implemented a CE requirement of the Connecticut mental health training.
Revisit Case Study
Let’s take a look at Jason’s case again and consider how things might have gone differently with better mental health protocols for the facility.
Jason is a 78 year old male who presents at the Internal Medicine office for his annual physical. When the nurse is collecting vitals, she chats with him about his plans for the summer. He states that he and his late wife used to garden together and he has kept up with it for the last 3 years since her death but this year he does not feel up to planning it or doing the work. The nurse asks if he has other plans for how to occupy his time and he states he usually has a group of friends he gets coffee with twice a week, but he hasn’t been waking up early enough to go to it and has decided to sleep in instead. The nurse notes the PHQ-9 questionnaire Jason completed at check in and sees the score is 20/27, which is indicative of depression.
The nurse documents his vitals and reports off to the physician, mentioning Jason’s PHQ score and his lack of interest in his usual activities. During the visit, his doctor asks how he has been feeling lately and if he has been sad or lonely. Jason discloses that he has been feeling down lately and not wanting to do the usual things that he enjoys. His doctor asks if he has any thoughts of suicide or wanting to hurt himself which Jason denies. After a thorough assessment, Jason is diagnosed with MDD and given a trial of fluoxetine. His doctor also recommends Jason establish with a therapist. Follow up is scheduled in 3 weeks to check in on how the new medication is going.

Self Quiz
Ask yourself...
- What improvements do you note in the way this scenario played out?
- How is depression differentiated from grief in this scenario? In what ways is the management of depression different from that of grief?
- Why is close follow-up beneficial in this scenario?
Alzheimer’s Nursing Care
Introduction
Alzheimer's disease is a destructive, progressive, and irreversible brain disorder that slowly destroys memory and thinking. Alzheimer's is the most common cause of dementia in older adults (1). For most people who have Alzheimer's disease, symptoms first appear in their mid 60's (1).
Studies suggest more than 5.5 million Americans, most 65 or older, may have dementia caused by Alzheimer's (1). It is currently listed as the sixth leading cause of death in the United States. It is essential to understand the signs and symptoms of Alzheimer's dementia and how to manage the care of a patient, family member, or friend suffering from the disease.
Dementia is the loss of cognitive functioning, such as thinking, remembering, reasoning, and behavioral abilities, such as a decreased ability to perform activities of daily living (1). The severity of dementia ranges from mild to severe. Dmentia's mildest stage often begins with forgetfulness, while its most severe stage consists of complete dependence on others for general activities of daily living (1).
History of Alzheimer's
Alzheimer's disease is named after Dr. Alois Alzheimer. In the early 1900s, Dr. Alzheimer noticed changes in the brain tissue of a patient who had died of an unknown mental illness. The patient’s symptoms included memory loss, language problems, and unpredictable behavior.
After her death, her brain was examined and was noted to have abnormal clumps known as amyloid plaques and tangled bundled fibers, known as neurofibrillary or tau tangles (1). These plaques and tangles within the brain are considered some of the main features of Alzheimer's disease. Another feature includes connections of neurons in the brain. Neurons are a type of nerve cell responsible for sending messages between different parts of the brain and from the brain to other parts of the body (1).
Scientists are continuing to study the complex brain changes involved with the disease of Alzheimer's. The changes in the brain could begin ten years or more before cognitive problems start to surface.
During this stage of the disease, people affected seem to be symptom-free; however, toxin changes occur within the brain (1). Initial damage in the brain occurs within the hippocampus and entorhinal cortex, which are the parts of the brain that are necessary for memory formation. As the disease progresses, additional aspects of the brain become affected, and overall brain tissue shrinks significantly (1).

Signs and Symptoms & Diagnosis of Alzheimer's Disease
Memory problems are typically among the first signs of cognitive impairment related to Alzheimer's disease. Some people with memory problems have Mild Cognitive Impairment (MCI) (2). In this condition, people have more memory problems than usual for their age; however, their symptoms do not interfere with their daily lives.
Older people with MCI are at increased risk of developing Alzheimer's disease. The first symptoms of Alzheimer’s may vary from person to person. Many people display a decline in non-memory-related aspects of cognition, such as word-finding, visual issues, impaired judgment, or reasoning (2).
Healthcare providers use several methods and tools to determine the diagnosis of Alzheimer's Dementia. Diagnosis and evaluation involve memory, problem-solving, attention, counting, and language tests. Healthcare providers may perform brain scans, including CVT. MRI or PET is used to rule out other causes of symptoms.
Various tests may be repeated to give doctors information about how memory and cognitive functions change over time. They can help diagnose different causes of memory problems, such as stroke, tumors, Parkinson's disease, and vascular dementia. Alzheimer's disease can be diagnosed only after death by linking clinical measures with an examination of brain tissue in an autopsy (3).

Self Quiz
Ask yourself...
- Have you experienced a patient in your practice with dementia or Alzheimer’s disease? What did their symptoms look like?
- What standard diagnostic tools do healthcare providers use to diagnose this disease?
- What is the definitive diagnosis of Alzheimer’s disease?
Stages of Disease
Mild Alzheimer's
People experience significant memory loss and other cognitive problems as the disease progresses. Most people are diagnosed in this stage (1).
- Wandering/getting lost
- Trouble handling money or paying bills
- Repeating questions
- Taking longer to complete basic daily tasks
- Personality/behavioral changes (1)
Moderate Alzheimer's
In this stage, damage occurs in the area of the brain that controls language, reasoning, sensory processing, and conscious thought (1).
- Memory and confusion worsen.
- Problems recognizing family and friends
- Unable to learn new things
- Trouble with multi-step tasks such as getting dressed
- Trouble coping with situations
- Hallucinations/delusions/paranoia (1)
Severe Alzheimer's
- Plaques and tangles spread throughout the brain, and brain tissue shrinks significantly.
- Cannot communicate
- Entirely dependent on others for care
- Bedridden - most often as the body shuts down

Self Quiz
Ask yourself...
- What are some of the signs and symptoms that differentiate each stage of Alzheimer’s disease?
- A person is in what stage of Alzheimer's disease when they struggle to recognize family members and friends?
Prevention
Many aging patients worry about developing Alzheimer's disease and dementia. Especially if they have had a family member who suffered from the disease, patients may worry about genetic risk. Although there have been many ongoing studies on the prevention of the disease, nothing has been proven to prevent or delay dementia caused by Alzheimer's disease (2).
More research suggests that women are more likely to develop dementia and Alzheimer's compared to men. Further research is needed to determine the role between genetics, sex, and Alzheimer's risk (4).
A review led by experts from the National Academies of Sciences, Engineering, and Medicine found encouraging yet inconclusive evidence for three types of interventions related to ways to prevent or delay Alzheimer's Dementia or age-related cognitive decline (2):
- Increased physical activity
- Blood pressure control
- Cognitive training

Treatment of the Disease
Alzheimer's disease is complex and is continuously being studied. Current treatment approaches focus on helping people maintain their mental function, manage behavioral symptoms, and lower the severity of symptoms. The FDA has approved several prescription drugs to treat those diagnosed with Alzheimer's (3).
Treating symptoms of Alzheimer's can provide patients with comfort, dignity, and independence for a more significant amount of time while simultaneously assisting their caregivers. The approved medications are most beneficial in the early or middle stages of the disease (3).
Cholinesterase inhibitors are prescribed for mild to moderate Alzheimer's disease; they may help to reduce symptoms. Medications include Rzadyne®, Exelon®, and Aricept® (3). Scientists do not fully understand how cholinesterase inhibitors work to treat the disease; however, research indicates that they prevent acetylcholine breakdown. Acetylcholine is a brain chemical believed to help memory and thinking (3).
For those suffering from moderate to severe Alzheimer's disease, a medication known as Namenda®, which is an N-methyl D-aspartate (NMDA) antagonist, can be prescribed. This drug helps to decrease symptoms, allowing some people to maintain certain essential daily functions slightly longer than they would without medication (3).
For example, this medication could help a person in the later stage of the disease maintain their ability to use the bathroom independently for several more months, benefiting the patient and the caregiver (3). This drug works by regulating glutamate, an essential chemical in the brain. When it is produced in large amounts, glutamate may lead to brain cell death. Because NMDA antagonists work differently from cholinesterase inhibitors, these rugs can be prescribed in combination (3).

Self Quiz
Ask yourself...
- Is there a cure for this disease?
- What are some of the treatment forms that have been used for the management of Alzheimer's disease?
- Can medications be used in conjunction with one another to treat the disease?
Medications to be Used with Caution in those Diagnosed with Alzheimer's
Some medications, such as sleep aids, anxiety medications, anticonvulsants, and antipsychotics, should only be taken by a patient diagnosed with Alzheimer's after the prescriber has explained the risks and side effects of the medications (3).
Sleep aids: They help people get to sleep and stay asleep. People with Alzheimer's should not take these drugs regularly because they could make the person more confused and at a higher risk for falls.
Anti-anxiety: These treat agitation and can cause sleepiness, dizziness, falls, and confusion (3).
Anticonvulsants: These are used to treat severe aggression and have possible side effects of mood changes, confusion, drowsiness, and loss of balance.
Antipsychotics: they are used to treat paranoia, hallucinations, agitation, and aggression. Side effects can include the risk of death in older people with dementia. They would only be given when the provider agrees the symptoms are severe enough to justify the risk (3).
Caregiving
Coping with Agitation and Aggression
People with Alzheimer's disease may become agitated or aggressive as the disease progresses. Agitation causes restlessness and causes someone to be unable to settle down. It may also cause pacing, sleeplessness, or aggression (5). As a caregiver, it is essential to remember that agitation and aggression are usually happening for reasons such as pain, depression, stress, lack of sleep, constipation, soiled underwear, a sudden change in routine, loneliness, and the interaction of medications (5). Look for the signs of aggression and agitation. It is helpful to prevent problems before they happen.
Ways to cope with agitation and aggression (5):
- Reassure the person. Speak calmly. Listen to concerns and frustrations.
- Allow the person to keep as much control as possible.
- Build in quiet times along with activities.
- Keep a routine.
- Try gently touching, soothing music, reading, or walks.
- Reduce noise and clutter.
- Distract with snacks, objects, or activities.
Common Medical Problems
In addition to the symptoms of Alzheimer's disease, a person with Alzheimer's may have other medical conditions over time. These additional health conditions can cause confusion and behavior changes. The person may be unable to communicate with you about their circumstances. As a caregiver, it is essential to watch for various signs of illness and know when to seek medical attention for the person being cared for (6).
Fever
Fever could indicate potential infection, dehydration, heatstroke, or constipation (6).
Flu and Pneumonia
These are easily transmissible. Patients 65 years or older should get the flu and Pneumonia shot each year. Flu and Pneumonia may cause fever, chills, aches, vomiting, coughing, or trouble breathing (6).
Falls
As the disease progresses, the person may have trouble with balance and ambulation. They may also have changes in depth perception. To reduce the chance of falls, clean up clutter, remove throw rugs, use armchairs, and use good lighting inside (6).
Dehydration
It is important to remember to ensure the person gets enough fluid. Signs of dehydration include dry mouth, dizziness, hallucinations, and rapid heart rate (6).
Wandering
Many people with Alzheimer's disease wander away from their homes or caregivers. As the caregiver, it is essential to know how to limit wandering and prevent the person from becoming lost (7).
Steps to follow before a person wanders (7)
- Ensure the person carries an ID or wears a medical bracelet.
- Consider enrolling the person in the Medic Alert® + Alzheimer's Association Safe Return Program®.
- Alert neighbors and local police that the person tends to wander and ask them to alert you immediately if they are seen alone.
- Place labels on garments to aid in identification.
Tips to Prevent Wandering (7)
- Keep doors locked. Consider a key or deadbolt.
- Use loosely fitting doorknob covers or safety devices.
- Place STOP, DO NOT ENTER< or CLOSED signs on doors.
- Divert the attention of the person away from using the door.
- Install a door chime that will alert when the door is opened.
- Keep shoes, keys, suitcases, coats, and hats out of sight.
- Make sure not to leave a person who has a history of wandering unattended.

Self Quiz
Ask yourself...
- What are the basic implementations you can make as a caregiver to make handling confusion and aggression easier in a patient with Alzheimer's?
- What are some of the types of medical problems that people with Alzheimer's may face, and how can they be monitored for prevention?
Conclusion
Alzheimer's is a sad, debilitating, progressive disease that robs patients of their lives and dignity. As research continues on the causes, treatment, and prevention of the disease, healthcare workers and caregivers need to know the signs and symptoms of a patient with Alzheimer's disease and potential coping mechanisms and management strategies of the disease. More information on the disease is available through several various resources, including:
Family Caregiver Alliance
800-445-8106
NIA Alzheimer's and Related Dementias Education and Referral Center
800-438-4380
Nursing Care in Lewy Body Dementia
Introduction
Lewy body dementia is one of the more common causes of dementia. Currently it is the second most common dementia disorder following Alzheimer’s disease [2]. This condition is shown to affect more than 1.4 million people in the United States [1] [2]. Of dementia cases in older adults, Lewy body dementia is said to make up 5% of people with dementia [2]. Lewy body dementia is a disorder that progresses over time [1]. The progression of the disease differs between individuals and the severity of the symptoms [1].
On average an individual lives between five to eight years after diagnosis [1]. Currently there is not a cure for this disease [1]. This course will examine the causes of this disease, signs and symptoms patients might experience, diagnostic tests, types of management, and educational resources for family members. This course is designed to inform nurses about this common disease and to use this information in their daily practice to care for their patients.

Self Quiz
Ask yourself...
- What do you think is the most common form of dementia in the United States?
- How common is Lewy body dementia in other parts of the world?
- Is there currently a cure for Lewy body dementia?
- Why do you think Alzheimer’s disease is more common than Lewy body dementia?
Definition
Lewy body is an umbrella term that includes two separate diagnoses: Dementia with Lewy bodies and Parkinson’s disease dementia [5]. As these diseases progress, they develop together and are seen as one entity, not two separate conditions [4]. Lewy body dementia is a condition that involves neurocognitive disorders that include hallucinations, memory loss, behavior changes, and parkinsonism features [2]. This disease can also affect intellectual abilities and cause individuals to act out dreams during REM (rapid eye movement) sleep [2]. REM sleep behavior disorder sometimes may be experienced before any other symptoms are exhibited [2].
Lewy body dementia is known for a buildup of deposits of alpha- synuclein proteins called Lewy bodies [1]. Diagnosing this condition can be difficult because many neurological disorders have similar symptoms. Lewy body dementia and Parkinson disease dementia are very similar. For a diagnosis of Lewy body dementia, there must be a cognitive impairment with motor symptoms occuring in less than 12 months [3]. Parkinson’s disease dementia affects an individual’s movements; cognitive symptoms appear later (greater than one year) [5].
Lewy body dementia is known to affect older adults generally between the ages of 50 and 85 [2]. This disease is said to be underdiagnosed due to a large number of diagnoses occuring post-death during autopsies [4]. Several medications used to treat neurocognitive and behavioral symptoms in other conditions can worsen the symptoms of Lewy body dementia [4]. Therefore, an accurate diagnosis can impact an individual’s quality of life.

Self Quiz
Ask yourself...
- What are the two forms of Lewy body dementia?
- What are the differences between dementia with Lewy bodies and Parkinson’s disease dementia?
- Why is it difficult to diagnose Lewy body dementia?
Epidemiology
Lewy body dementia affects a significant number of individuals in the United States. This condition is found more often in men than women [4]. Age is thought to be the greatest risk factor for an individual developing this disease [4]. An individual who has a family history of Lewy body dementia and Parkinson’s disease is at a higher risk for developing this condition [3].
Lewy Body dementia is more widespread in European, Asian, and African ethnic groups [3]. In individuals with Parkinson’s disease, the incidence of Parkinson’s disease dementia is said to be around 25-30% [4]. The incidence of individuals with Parkinson disease developing this type of dementia after having Parkinson’s for more than 20 years increases to around 83% [4].


Self Quiz
Ask yourself...
- What is the greatest risk factor for developing Lewy body dementia?
- Are there certain ethnic groups that have a higher rate of Lewy body dementia?
- Which gender is Lewy body dementia prominent in?
Pathophysiology
There is a buildup of alpha- synuclein proteins that causes neurons to die in Lewy body dementia [2] [5]. As mentioned above in this course, this buildup of proteins is called Lewy bodies. The death of neurons that produce dopamine result in problems with movement, cognitive impairment, a decline in cognition, and sleep disturbances [4]. In Lewy body dementia there is a deficiency of acetylcholine [3]. There is also a decrease in acetylcholine with Alzheimer’s disease, but the deficiency is greater with Lewy body dementia [3]. The decrease in neurons that produce acetylcholine causes memory loss and learning impairment [4].
The mutation of synuclein alpha and synuclein beta genes can cause dementia with Lewy bodies [2]. Mutations in apolipoprotein E and GBA genes are potential risk factors for developing the disease [2]. There have been cases where a buildup of alpha-synuclein was found during an autopsy, but the individual did not show any clinical signs of Lewy Body dementia when alive [4]. The function of these proteins in this condition is still undetermined [5].

Self Quiz
Ask yourself...
- What are considered Lewy bodies?
- What other disease besides Lewy body dementia has a decrease in acetylcholine?
- What symptoms are a result of destruction of neurons that produce dopamine?
Etiology
The exact cause of Lewy body dementia is still unknown. While research is ongoing and new developments are occuring, the specific cause has not been determined. The accumulation of Lewy bodies cause cell death which causes symptoms, however, the reason for the buildup of Lewy bodies is still under research [5]. As mentioned earlier, there are specific gene mutations that have been shown to increase the likelihood of producing altered alpha- synuclein proteins, in turn causing them to clump together (forming the Lewy bodies) [2].
The mutation of the GBA gene interferes with the function of lysosomes, which can affect the breakdown of the alpha- synuclein proteins, causing the proteins to accumulate [2]. The e4 allele type of the APOE gene has been shown to increase the risk of developing Lewy body dementia [2]. These clumps of Lewy bodies form inside and outside of neurons in different areas of the brain, where they can alter the function of the cell and can cause the cell to die [2].
The neurons that develop the neurotransmitter dopamine are especially impacted by these clumps of Lewy bodies, which was addressed earlier in this course [2]. Further research is required to find out why these Lewy bodies develop in certain individuals. Currently, age, genetics, and environmental factors are some of the greatest risk factors [3].

Self Quiz
Ask yourself...
- What is the cause of Lewy body dementia?
- Why is age a risk factor for developing this disease?
- What does the buildup of Lewy bodies do to cells?
Clinical Signs and Symptoms
Lewy body dementia is a progressive disorder - the signs and symptoms worsen over time. The symptoms that are more common are sleep changes, impaired behavior, movement, and cognition [5]. Research shows that the location of Lewy body accumulation impacts the clinical signs and symptoms the individual experiences [3]. If Lewy bodies develop in the brainstem and cerebral cortex first, the condition is called dementia with Lewy bodies, and the onset of the dementia is early [3]. If Lewy bodies accumulate in the brain stem and then develop into the cerebral cortex as time passes, the onset of dementia appears later, and this condition is called Parkinson’s disease dementia [3].
Rapid Eye Movement Sleep Behavior Disorder
Rapid eye movement (REM) sleep behavior disorder is sometimes the first clinical sign of dementia with Lewy bodies [2]. Individuals with this disorder move and talk while dreaming in their sleep [2]. The movements can be violent and cause the individual to fall out of bed [5]. Individuals may kick, punch, and scream in REM sleep (the second half of their sleep) [4]. REM sleep behavior disorder is seen in 76% of patients with dementia with Lewy bodies [4].
This disorder can cause fractures and contusions in some individuals resulting from falling out of bed [4]. This can not only affect the individual, but also the sleep partner of the patient [4]. In some cases, separate sleeping arrangements are needed for the safety of the individual and their sleeping partner. A questionnaire by the patient and sleep partner is part of the diagnosis of REM sleep behavior disorder [14]. If the individual does sleep next to someone, this questionnaire can be helpful as most of the time the patient cannot recall the events while asleep [14]. Video polysomnography is required for a complete diagnosis of this disorder [14]. These events while asleep must be repeated to meet the diagnostic criteria [14].
Other Sleep Disorders
Other disorders of sleep include sleepiness in the daytime, restless leg syndrome, confusion when awakened, and obstructive sleep apnea [4].
Visual Hallucinations
Visual hallucinations are present in about 80% of individuals with Lewy body dementia [1]. Visual hallucinations are a core clinical symptom of dementia with Lewy bodies [4]. They are more common in women than in men [4]. Individuals are aware of these hallucinations and can tell others what they experienced [4]. Visual hallucinations are vivid to individuals and have been said to range from people walking around the house to seeing people that have died sitting next to them [6]. During the beginning stages of the disease, the hallucinations do not seem to affect the patient as much as when the disease progresses [6]. Patients are said to be afraid of these hallucinations in the later stages of the disease [6]. Nonvisual hallucinations are less common, however can occur in some patients [1]. These hallucinations include smelling or hearing something that is not in their surroundings [1].
Fluctuation in Cognition
Fluctuation in cognition is also a clinical sign that is associated with dementia with Lewy bodies [4]. This symptom includes changes in attention, concentration, and alertness [5]. These changes are random and can differ day-to-day [1]. Symptoms can include delirium, and mimic symptoms that are caused by metabolic diseases, which can further the difficulty with identifying the correct diagnosis [4]. To diagnose dementia with Lewy bodies, one of the episodes must be confirmed [4]. These fluctuations can be present in other forms of dementia in their later stages but when present in earlier stages, they point to dementia with Lewy bodies [4].
Memory loss that impacts activities of daily living can be found in later stages of Lewy body dementia [1]. Memory loss early on is more often a characteristic sign of Alzheimer’s dementia [1]. Confusion about the individual’s whereabouts, and inability to multitask can also occur in dementia with Lewy bodies [4].
Problems with Movement
Problems with movement are signs of Lewy body dementia. Bradykinesia (slow movements) and rigidity occur in about 85% of individuals with dementia with Lewy bodies [4]. Tremor at rest is less common in individuals with this condition [4]. Loss of coordination and difficultly swallowing can occur [1]. Problems with movement greatly increase the risk of falls for these individuals [4]. This can place strain on the individual’s caregivers [4].
Autonomic Dysfunction
Autonomic dysfunction can be present in dementia with Lewy bodies and Parkinson’s disease dementia. This symptom is seen in about 90% of patients with Lewy body dementia [4]. The symptoms that result from autonomic dysfunction can be constipation, urinary incontinence, orthostatic hypotension, erectile dysfunction, and dizziness [1] [4]. Orthostatic hypotension appears as early as five years prior to the diagnosis of Lewy body dementia [4]. Syncope and falls are usually the result of orthostatic hypotension [4]. Constipation can also occur earlier in the disease process [4].


Self Quiz
Ask yourself...
- What is REM sleep behavior disorder?
- Are visual hallucinations common in Lewy body dementia?
- What does cognitive fluctuation mean?
- What are symptoms of autonomic dysfunction seen in dementia with Lewy bodies?
Diagnostic Tests and Evaluations
Throughout this course, it has been mentioned that Lewy body dementia is significantly underdiagnosed. Individuals are usually diagnosed as the disease progresses due to the symptoms that overlap with other forms of dementia and other neurological and psychiatric disorders [3]. An autopsy of the brain after death is one of the only ways to have a conclusive diagnosis of Lewy body dementia [16]. There are certain diagnostic criteria and diagnostic tests that are used to diagnose an individual with Lewy body dementia.
Diagnosis by Symptoms
Lewy body dementia is probable when an individual experiences dementia and two main features of the disease. Lewy body dementia is a potential diagnosis if the individual experiences progressive dementia and one main feature of the disease [3]. As discussed in the clinical signs and symptoms section of this course, key features of Lewy body dementia are cognitive fluctuations, dementia that progresses, problems with movement (signs of parkinsonism), REM sleep behavior disorder, and visual hallucinations [3] [16].
Timing of symptoms is relevant for distinguishing between the two forms of Lewy body dementia [3]. Currently healthcare providers use the time span of one year to distinguish the two forms [3]. If dementia occurs within one year of the appearance of movement problems, then a diagnosis of dementia with Lewy bodies is used [3]. If an individual is diagnosed with Parkinson’s disease and starts experiencing symptoms of dementia more than one year after their Parkinson’s diagnosis, then Parkinson’s disease dementia is used [3]. Some indicative biomarkers in addition to clinical symptoms are used in diagnosis [4]. Some of these biomarkers can be found in cerebral spinal fluid (CSF) and are still under research [4].
Cognitive Tests
Cognitive testing can be used to show the cognitive impairment of patients with Lewy body dementia [3]. The Mini-Mental State Examination can be used as an initial screening test [4]. This exam tests cognitive function by focusing on concentration, orientation, and memory [15]. This test can be limited since symptoms of these patients can fluctuate day to day [3]. Another cognitive function test is the Montreal Cognitive Assessment (MoCA) [15]. Providers do not usually diagnose based on a single test; instead, they use the results to look for other signs and symptoms of Lewy body dementia [4].
Imaging Tests
There are certain imaging tests that can help with diagnosis and distinguishing between other dementia disorders. A single-photon emission computerized tomography (SPECT) scan can help support a diagnosis [16]. This is a nuclear scan that can sense radioactivity [16]. If the SPECT scan shows a reduced dopamine transporter uptake in the basal ganglia, this can be a sign of Lewy body dementia [16]. This will separate the diagnosis between Lewy body dementia and Alzheimer’s disease [4]. Performing this scan alone will not lead to a possible diagnosis of Lewy body dementia; however, in combination with other diagnostic tests, the scan can lead to a more certain diagnosis [4]. Results from these scans can appear normal initially, and the scan may need to be repeated [4].
An iodine- MIBG myocardial scintigraphy can be performed to support Lewy body dementia [16]. This would show decreased communication of cardiac nerves [16]. The results may be skewed by heart disease or certain drugs [4]. A CT or MRI may be used but these imaging tests can present mixed results [4]. With Alzheimer’s disease, significant atrophy is seen in the medial temporal lobes [4]. There is normally minimal atrophy in Lewy body dementia [4].
As mentioned earlier in the course, video polysomnography is needed for the diagnosis of REM sleep behavior disorder [14]. This sleep study without the loss of muscle tone can also point towards a diagnosis of Lewy body dementia as REM sleep behavior disorder has now moved to a key feature of this disease [14].

Self Quiz
Ask yourself...
- What types of imaging tests can be used in the diagnosis of Lewy body dementia?
- Why are cognitive tests used in diagnosis of this disease?
- What criteria are needed for a probable diagnosis of Lewy body dementia?
- Can the cost of diagnostic imaging lead to a reduction in diagnosing Lewy body dementia?
Case Studies
Case Study #1
A 74-year-old male presents to his primary care provider after his wife reports abnormal behavior over the past several months. His wife reports the patient kicks and screams during sleep. The patient reports seeing little people walking around the living room during the day. The wife states the patient some days will fall asleep throughout the day while completing activities. The patient states difficulty walking and muscle stiffness.
The wife states last week the patient was supposed to go to the local grocery store to buy milk. After two hours passed, the wife called her husband as she was worried about him. He states he got lost finding the grocery store and did not know where he was. The wife said she had to drive to find her husband and bring him home. The patient also reports dizziness when standing. After the nurse obtained an orthostatic blood pressure, the patient was positive for orthostatic hypotension.
- Which form of dementia is the patient most likely experiencing?
- What type of symptoms is the patient experiencing that would point to that diagnosis?
- What diagnostic tests or evaluations should the patient undergo?
- What types of supportive treatment should the healthcare provider include in the treatment plan for this patient?
Case Study #2
A 70-year-old female presents to the emergency department via EMS after falling at home. The patient’s daughter called 911 after finding her on the floor when going to visit her. Upon arrival at the emergency department the patient is oriented to self. The patient does not know where she is or what happened to precipitate the fall. The patient has a past medical history of hypertension, diabetes type II, and Parkinson’s disease.
The patient was diagnosed with Parkinson’s disease two years prior. The daughter states the patient has been forgetful lately and not acting like herself. The daughter reports that her mom’s behavior is different from day-to-day. An MRI and the National Institutes of Health Stroke Scale (NIHSS) are used to rule out a cerebrovascular accident. A complete blood count (CBC), a complete metabolic count (CMP), and urinalysis are obtained. The patient suffered a contusion to her right cheek and a right radius fracture. The patient states that she sees figures dancing in the room and smells popcorn. The patient appears to be frightened by the hallucinations. The patient’s daughter states for the last six months the patient has had difficulty swallowing and a reduced appetite.
- Which form of dementia is the patient most likely experiencing?
- What would the MRI of the patient most likely show?
- What clinical signs of dementia is the patient exhibiting?
Management
Currently there is not a cure for Lewy body dementia, only supportive treatment. The management of this disease involves a multifaceted approach, including therapies, pharmacological treatments, and family support.
Therapies
Specific therapies can help with symptom management and help improve the individual’s quality of life. Occupational therapy can help improve a patient’s ability to complete activities of daily living. Speech therapy can help with swallowing coordination and improve the clarity and volume of speech [5]. Physical therapy can aid patients with problems with movement [5]. Mental health counseling can help individuals and their families with managing behaviors and their emotions [5].
Medications
Pharmacotherapy can help with supportive treatment but can also worsen symptoms if certain medications are taken. Below are some examples of medications that are used by patients with Lewy body dementia.
- Cholinesterase Inhibitors are used to help cholinergic activity to improve cognitive function [6].
- Rivastigmine was one of the first of these drugs to be tested [6]. Patients were noted to have improved on their cognitive exams [6]. It is also shown to reduce hallucinations and lessen anxiety [6]. This class of drugs has been said to improve the quality of life for some patients [4].
- Donepezil and Galantamine are also used to reduce dementia symptoms of hallucinations [6]. These drugs were initially targeted for patients with Alzheimer dementia, however, they are effective for individuals with Lewy body dementia as well [3]. A study was done stating even if there is not a sign of cognitive improvement, this should not be the criteria to stop the medication as this medication has been proven to protect the individual from further impairment of cognition [4].
- Atypical Antipsychotics are prescribed to patients that are not seeing a reduction of symptoms while on cholinesterase inhibitors [3]. These types of drugs are seen as controversial due to the many adverse effects that have been seen in patients [4]. Drugs such as haloperidol and olanzapine should be avoided in patients with Lewy body dementia as they can cause neuroleptic malignant syndrome (a life-threatening condition) [5]. Quetiapine, clozapine, pimavanserin, and aripiprazole are atypical antipsychotic drugs that can be used to improve agitation and help prevent cognitive fluctuations [5].
- Carbidopa-Levodopa can be used in patients to manage problems with movement [3]. This medication can cause side effects and can result in hallucinations, delusions, and increase confusion [3]. Providers should begin with low doses of this medication [3].
- Clonazepam is a benzodiazepine that can lessen the REM sleep behavior disorder that patients with dementia with Lewy bodies can experience [5]. Between 33-65% of patients with REM sleep behavior disorder can experience an injury while sleeping [5]. This medication has been proven to decrease injuries that occur during sleep [5]. Clonazepam can adversely affect individuals with gait disorders or sleep apnea [5].
- Melatonin is a hormone that can be used for patients that are affected by REM sleep behavior disorder (5). Studies have shown that the use of melatonin lessened the frequency and the severity of symptoms associated with REM sleep behavior disorder [5]. Melatonin can have side effects such as headaches in the morning, sleepiness during the day, and hallucinations [5].
- Memantine is used to treat dementia symptoms [5]. This medication is an NMDA receptor antagonist that stops effects of glutamate in the brain [5]. Memantine has been shown to improve symptoms of patients early in the disease [5].


Self Quiz
Ask yourself...
- What type of therapies are used in management of Lewy body dementia?
- What class of drugs are used to help improve cognitive function?
- What are some medications that should be avoided in patients with Lewy body dementia?
- Why is melatonin used in patients with Lewy body dementia?
Nursing Care
As mentioned before, there is not a cure for Lewy body dementia. Caring for patients with Lewy body dementia includes supportive treatment. Nurses can play a significant role in caring for these patients and providing the family with support. Home health nurses can help with frequent assessment of the patient and their environment [3]. Environmental changes may be needed to protect the patient from falls and other accidents. Home health nurses can assess the type of assistance the patient would benefit from.
Nurses can aid the family by providing education to assist in how to care for the patient. Family members and caregivers must be aware of the changes in behavior, fluctuations in cognition, and hallucinations that the individual might experience [3]. Nurses must also provide education to the caregiver of the patient on the side effects of certain medications, as they can affect an individual with this disease [7].

Self Quiz
Ask yourself...
- Are there any modifications that nurses must apply to care for patients with Lewy body dementia?
- Whose role is it to educate patients and their family members?
Family Support
Lewy body dementia is growing in recognition; however, many people might not be aware of this condition and the disease process. Family members need support from health care professionals to better care for their loved ones. Support can come in the form of education and preparing the family for the symptoms the individual may experience. The cognitive function of patients with this disease can be very limited [3]. Family members must be educated on monitoring the individual closely to promote safety [3]. These individuals are at a high risk for falling and developing aspiration pneumonia (due to swallowing difficulties) [3]. Family members should be educated in preparing for an emergency.
Individuals with Lewy body dementia may need care and the family needs to know how to inform health care providers of their specific needs. It is important to educate family members that their roles in their past relationship with the patient will likely change due to the disease process. To prevent caregiver burnout, family members must be aware of their limitations and know when they need help [7]. Modifying the patient’s home may be needed for patient safety [3]. Each patient may have specific needs and family members should know what modifications may be necessary [3].

Self Quiz
Ask yourself...
- What type of support do you feel is important to give family members of loved ones with this disease?
- What should nurses include in education for fall risk safety for family members while the individual is at home?
- Can nurses help to prevent caregiver burnout?
Prognosis
The prognosis of Lewy body dementia can be viewed as poor. As mentioned briefly earlier in this course, this disease is progressive and after diagnosis, the life expectancy is five to eight years [3]. The range of expectancy has also been attributed to delay in diagnosis, which can further delay supportive treatment to improve quality of life for the individual [3]. Patients can die from complications from the disease. Complications can include cardiac complications, falls, adverse effects from medications, pneumonia, and suicide [3].
Compared to Alzheimer’s dementia, the risk of hospitalization or death due to respiratory infections is higher in patients with Lewy body dementia [8]. The median age at death is said to be similar between patients with Alzheimer’s dementia and Lewy body dementia [8]. The life expectancy from diagnosis to death is shorter in patients with Lewy body dementia [8]. The patient’s environment has been shown to play a role in the increased risk of mortality [8]. Patients in nursing homes have been shown to have a higher risk of mortality [8]. Caregivers can decrease the risk of complications by educating themselves on this disease and keeping their loved ones safe.

Self Quiz
Ask yourself...
- What are some complications of Lewy body dementia?
- How can the patient’s environment increase the risk of mortality with this disease?
- Why do you think there is delay in diagnosis with Lewy body dementia?
Resources for Family Support
Lewy body dementia is a diagnosis that can affect all aspects of an individual’s life and their family members lives. As nurses we must provide support for family members so they can better care for their loved ones and improve their quality of life. As recognition of this condition grows, family support resources are increasing. The Lewy Body Dementia Association is a nonprofit organization that raises awareness and provides support for families with individuals that suffer from Lewy body dementia [10]. Support groups can be found on their website to help families across the country in their local area [10].
The Lewy Body Dementia Association was started by caregivers of individuals with this condition. They also focus on education and research into the disease. This association is a resource for family members [10].
Another resource for family members is The Lewy Body Dementia Resource Center. This is a nonprofit charitable organization that gives assistance and support to those who care for someone with Lewy body dementia [9]. This organization was founded by caregivers of individuals with Lewy body dementia. They have a support phone line that is available seven days a week to answer questions [9]. They also promote research and early diagnosis of this disease [9].

Self Quiz
Ask yourself...
- How can support of family members improve the quality of life of a patient with Lewy body dementia?
- What are some examples of resources for caregivers of individuals with Lewy body dementia?
- Can providing resources to the community help with early diagnosis of this disease?
Research Programs
Lewy body dementia is the second most common form of dementia in the United States [4]. This illness is thought to be underdiagnosed and commonly mistaken for other neurological disorders [3]. Research on Lewy body dementia can decrease the time it takes to diagnose a patient, and can help with management of the condition.
The National Institute of Neurological Disorders and Stroke provides support for a variety of research endeavors for Lewy body dementia [11]. In 2021 The National Institute of Health spent $93 million dollars on Lewy Body dementia research [11]. One program is the Biomarkers for Lew body dementias program. This program aims to increase clinical data collection from patients with this condition, find biomarkers to expand further research, and allow access to the science community to help with further studies [11]. Another program is the Parkinson’s Disease Biomarkers Program. This program’s purpose is to collectively research with healthcare professionals, patients and family members, and technology professionals to increase biomarker research [11].
Biomarker research has been increasing in Lewy body dementia. A biomarker is a feature that can specifically indicate a certain disease [12]. For quite some time there were not any identified biomarkers for Lewy body dementia. There are certain biomarkers that aid in distinguishing Alzheimer’s disease from Lewy Body dementia [13]. These biomarkers can be assessed through imaging or in cerebral spinal fluid [13]. Currently these biomarkers are only helpful if another disease is doubtful [13].
New biomarkers are needed to separate Alzheimer’s dementia from Lewy Body dementia and other neurological disorders [13]. Biomarkers that can help with early diagnosis would be beneficial for early treatment [13].


Self Quiz
Ask yourself...
- Why is researching biomarkers important for early diagnosis of Lewy body dementia?
- Is there more research conducted on Alzheimer dementia than on Lewy body dementia?
- What are some organizations that promote research for this disease?
Conclusion
Lewy Body dementia affects 1.4 million Americans [2]. The disease is underdiagnosed and often diagnosed incorrectly. Incorrect diagnoses can lead to worsening of symptoms and the administration of drugs that can lead to adverse effects.
Educating healthcare providers and the community about Lewy body dementia can improve quality of life for individuals with the disease. As nurses, we must be informed about this disease to better educate our patients and their caregivers, and to know how to advocate for our patients.
Connecticut Domestic and Sexual Violence
Introduction
Each year, more than 10 million men and women in the United States experience physical abuse from an intimate partner. One in three women and one in four men have experienced some form of physical violence from an intimate partner in their lifetime and one in 10 women has been raped by an intimate partner (18). Such experiences have a lasting impact on physical and mental wellbeing, employment and economic status, effects on children who may witness such abuse, and, in severe cases, may even result in death.
Healthcare professionals are on the front lines of screening and prevention for domestic and sexual abuse and may be able to recognize early signs of abusive relationships, improve client connections to resources, and reduce the overall incidence of acute and long-term injury from abuse. This course aims to educate healthcare professionals on risk factors, signs of abuse, characteristics of abusers, and the role of healthcare in interrupting the abuse cycle.
Defining Domestic Abuse
The Department of Justice defines domestic violence, or intimate partner violence, as “a pattern of abusive behavior in any relationship that is used by one partner to gain or maintain power and control over another intimate partner.” Violence involving intimate partners accounts for 15% of all crime (18). There are various categories of abuse.
- Physical
Physically harming a partner by any manner, including hitting, slapping, shoving, etc. Can also involve denying medical care to someone in need as well as forcing drugs or alcohol use upon someone so as to alter their cognition.
- Sexual
Attempted or successful coercion to participate in sexual contact without consent. Includes rape (including within marriage), sexually demeaning, harming genitals, or forcing sexual acts after physical violence.
- Emotional
Patterns of chronic criticism, name-calling, or demeaning behaviors that damage a person’s self-worth.
- Economic
Use of coercion, fraud, or manipulation to restrict a person’s access to money, assets, or financial information. Or unethically acquiring and/or using someone’s economic resources through exploitation or improper conducting of power of attorney, guardianship, or conservatorship roles.
- Psychological
Threats or intimidation, forced isolation, destruction of property.
- Technological
Use of technology, such as online platforms, computers, mobile phones, cameras, apps, etc. to threaten, harm, control, harass, stalk, impersonate, or monitor another person (22).
Each of these categories has its own nuances and examples, but all consist of acts or threats that influence the weaker or subordinate partner. For the purpose of this course, we will mostly cover physical and sexual abuse, but all forms of abuse are valid and many times overlap with each other. Abusers use tactics such as (22):
- Intimidation
- Manipulation
- Humiliation
- Isolation
- Fear
- Coercion
- Blame
- Injuries/pain
Further information about the epidemiology of domestic violence will be covered below, but it is important to note that anyone can become a victim of domestic violence, including people of all races, ages, sexual orientations, and gender identities. People of all socioeconomic and education levels can be affected, and all types of relationships can be involved; including couples who are opposite-sex, same-sex, married, dating, co-parenting, or living together.
Affected individuals include not only the abused, but also family members (particularly children), coworkers, friends, and other members of the abused person’s community. Frequently witnessing domestic violence as a child increases the risk of becoming a victim of domestic abuse or an abuser in adulthood by demonstrating this as a “normal” way of life (22).


Self Quiz
Ask yourself...
- Which types of abuse do you think may be the most obvious or easy to identify?
- Which types are more subtle or difficult to identify?
- Before reviewing the epidemiology information in the following section, are there particular groups of people or characteristics that you think would be most susceptible to each type of abuse?
- What preconceived notions do you think might contribute to those opinions?
Epidemiology of Abuse
As discussed above, anyone can be a victim of domestic violence, however there are particular populations who are at an increased risk and more likely to be victimized. Awareness of these demographics is useful for healthcare professionals when trying to detect situations where abuse may be more likely. An overview of domestic violence prevalence for at-risk populations is discussed below.
Gender
Women are much more likely to be affected by domestic violence than men.
- 1 in 3 women has experienced some form of physical violence form an intimate partner, though the severity varies widely.
- 1 in 4 women has experienced severe intimate partner violence either of a physical or sexual nature, compared to 1 in 9 men.
- 1 in 7 women have experienced a physical injury from an intimate partner, as opposed to 1 in 25 men.
- 1 in 7 women has been stalked by a partner to a point where they feared harm; conversely 1 in 18 men have had this experience.
- 1 in 10 women have been raped by an intimate partner.
- 72% of all murder-suicides involve intimate partners and 94% of the victims of murder-suicides are women (18).
- Women are at risk for contraception coercion, where a partner pressures them to become pregnant or tampers with contraception to cause pregnancy (1).
Pregnant Women
Pregnant women are particularly vulnerable, and their risk of abuse is higher during this time, further complicating the health risks of abuse.
- 1 in 6 abused women is first abused during pregnancy
- Over 320,000 women experience domestic violence during pregnancy annually (14)
Ethnicity/Race
Minority race groups are more at risk for experiencing domestic violence. Department of Justice (DOJ) survey data indicates that 51.3% and 17.7% of white women report having experienced physical and sexual violence respectively, while non-white women report experiencing these at 54% and 19.8% respectively (26).
Among minorities, American Indian and Alaskan Natives are among the most at risk. This group experiences high poverty rates, particularly on reservations, increased drug and alcohol use, and minimal resources for Natives seeking culturally specific shelter or safety from abuse, all of which increases the risk and prevalence of domestic violence, particularly among Native women (26)
- Over 84% of Native women experience some form of violence during their life
- American Indians are 3 times more likely to be a victim of sexual violence than all other ethnic groups
- 55.5% of Native women experience domestic violence in their lifetime
- 66.6% experience psychological abuse from a partner
- Over half have experienced sexual assault (26)
For the Black community, factors like racist societal and legal structures have created gaps in economic opportunities, education, access to healthcare, and access to safety/resources that puts Black men and women at higher risk of domestic violence than their white peers. Due to stereotypes and inconsistent cultural competence among law enforcement, jurors, and judges, Black victims of abuse are more likely to be arrested and less likely to be believed by the legal system than white victims (13).
- 45.1% of Black women and 40.1% of Black men experience domestic violence of a physical or sexual nature in their lifetimes
- 53.8% of Black women and 56.1% of Black men have been victims of psychological abuse in their lifetime
- 8.8% of Black women have been raped by a partner in their lifetime
- Homicide involving domestic partners was highest among Black women in 2017, at 2.5 per 100,000 (16)
Age
Opposing ends of the age spectrum are both at increased risk of victimization, with teens and young adults as well as elderly people being at higher risk than the rest of the population.
Teens are at an increased risk due to their inexperience with dating and relationships and susceptibility to peer pressure. They may also feel hesitant to tell an adult about abuse for fear of consequences or punishment. They may not recognize behaviors as abusive right away and may perceive controlling or jealous behaviors as signs of love. Teens who have witnessed repeated domestic violence among parents or other family members may also believe that this is how normal relationships function.
According to 2023 data, one in 12 high school students report physical violence and one in 12 report sexual violence in a dating relationship (5).
- 1.5 million high school students are abused in a dating relationship annually (only 33% ever tell anyone about it)
- 26% of teens are victims of cyber dating abuse; female teens were twice as likely to experience this as male teens
- 57% of teens report knowing someone who has been physically, sexually, or verbally abused in a relationship (19)
Older adults are also at an increased risk, often due to impaired physical or cognitive abilities that require them to rely on a caretaker. They may be isolated, with limited social support or without the ability to tell someone what is happening to them.
- It is estimated more than 10% of older adults who live in communities experience physical, psychological, sexual, or financial abuse from a caretaker
- Only about 1 in 14 of these incidents are reported
- A spouse or intimate partner is the perpetrator in 57% of physical abuse, 87% of psychological abuse, and 40% of sexual abuse cases
- 39% of firearm homicides involving older adults were committed by a domestic partner (21)

Self Quiz
Ask yourself...
- Why do you think pregnancy puts women at an increased risk of being a victim of domestic violence?
- Think of an elderly client you have cared for before. How easy do you think it would be for a caregiver to take advantage of them?
- Are there other clients of the same age who might be more or less susceptible to this risk?
- What factors do you think affect the level of risk for elderly clients?
LGBTQ Community
Though it is well-known that members of the Lesbian, Gay, Bisexual, Transgender, Queer (LGBTQ) community are at increased risk of violence or harm. In the general population, awareness of domestic violence rates for the LGBTQ community is just beginning to rise, as most existing data is based on heterosexual relationships. Emerging data is revealing that people in the LGBTQ community experience domestic violence at equal or greater rates than their straight and cis-gender peers (20).
*Note: A basic understanding of sex, gender, and sexual orientation is necessary when caring for members of the LGTBQ community so as to offer comprehensive and competent care. These common terms and their definitions are included below for anyone needing clarification.
Quick Terminology Lesson
Sex: A label, typically of male or female, assigned at birth, based on the genitals or chromosomes of a person. Sometimes the label is “intersex” when genitals or chromosomes do not fit into the typical categories of male and female. This is static throughout life, though surgery or medications can attempt to alter physical characteristics related to sex.
Gender: Gender is more nuanced than sex and is related to socially constructed expectations about appearance, behavior, characteristics based on gender. Gender identity is how a person feels about themselves internally and how this matches (or does not match) the sex they were assigned at birth. Gender identity is not related to who a person finds physically or sexually attractive. Gender identity is on a spectrum and does not have to be purely feminine or masculine and can also be fluid and change throughout a person's life.
- Cis-gender: When a person identifies with the sex they were assigned at birth and feels innately feminine or masculine.
- Transgender: When a person identifies with the opposite sex they were assigned at birth. This can lead to gender dysphoria or feeling distressed and uncomfortable when conforming with expected gender appearances, roles, or behaviors.
- Nonbinary: When a person does not feel innately or overwhelming feminine or masculine. A nonbinary person can identify with some aspects of both male and female genders or reject both entirely.
Sexual orientation: A person’s identity in relation to who they are attracted to romantically, physically, and/or sexually. This can be fluid and change over time, so do not assume a client has always or will always identify with the same sexual orientation throughout their life.
Types of sexual orientation include:
- -Heterosexual/Straight: Being attracted to the opposite sex or gender as oneself
- -Homosexual/Gay/Lesbian: Being attracted to the same sex or gender as oneself.
- -Bisexual: Being attracted to both the same and opposite sex or gender as oneself
- -Pansexual: Being attracted to any person across the gender spectrum, including non-binary people
(11)
There are elements of domestic violence that are specific to the LGBTQ community. One example is “outing” or threatening to disclose a person’s sexual orientation or gender identity without their consent. Threatening to out someone can be used as leverage or a power dynamic in psychological abuse, and actually outing someone can lead to an increased risk of rejection and physical or sexual harm depending on who the information is revealed to.
Additionally, members of the LGBTQ community may be afraid to seek help in abusive situations or may even experience discrimination when they do seek help, putting them at greater risk of significant harm. Poorly trained staff, implicit biases of staff, and even gender-specific resources such as women’s shelters can be difficult to navigate for LGBTQ victims (20). Statistics about domestic violence in LBGTQ relationships include the following:
- 61.1% of bisexual women and 43.8% of lesbian women report experiencing rape, physical violence, or stalking by a domestic partner at some point in their life; compared to 35% of heterosexual women
- 37.3% of bisexual men and 26% of gay men report experiencing rape, physical violence, or stalking by a domestic partner at some point in their life; compared to 29% of heterosexual men
- 26% reported experiences of near-lethal violence in male-male relationships
- Fewer than 5% of all LGBTQ domestic violence victims seek orders of protection
- Transgender people are more likely to experience domestic violence in a public setting compared to cis-gender individuals
- Transgender individuals experience unique forms of psychological/emotional abuse such as being called “it” or being ridiculed for physical appearance
- Bisexual individuals are more likely to experience sexual violence than other sexual orientations
- Black LGBTQ individuals are more likely to experience physical violence from a partner than other races
- White LGBTQ individuals are more likely to experience sexual violence from a partner than other races (20)
Disabled Populations
Nearly a quarter of all U.S. adults have some type of physical, cognitive, or emotional disability. People with disabilities are particularly vulnerable to domestic violence.
- Nearly 70% of people who have a disability experience domestic abuse
- People who have a disability are three times as likely to be sexually assaulted than their non-disabled peers (23)
People with disabilities relying at least partially on others to function in their daily life are particularly vulnerable to being intimidated, isolated, or controlled by someone they trust (power imbalance). Some 75% to 80% of domestic abuse of people with a physical disability and 95% of abuse of those with a cognitive disability goes unreported. The types of abuse are often unique to the disability as well, including:
- Invalidation or minimization of disability
- Shaming or ridiculing for disability
- Refusal to help with daily tasks such as bathing, dressing, or eating
- Over or under medicating
- Sexual acts without consent
- Denying access to healthcare services/appointments or medications
- Limiting access to mobility devices such as walkers, wheelchairs, or prosthetics
- Withholding finances
- Threatening abandonment (23)
Certain populations with disabilities are more at risk than others.
- Women who have a disability:
-
- 80% of women who have a disability report sexual assault
- 40% higher rates of domestic abuse
- Violence experienced by women with disabilities may be more frequent or of greater severity
- More likely to experience reproductive coercion, stalking, or psychological abuse
- People in the LGBTQ community who have a disability:
-
- LGBTQ facilities may not be accessible for those with disabilities
- Disability services may not be competent with issues of the LGBTQ community
- Black, Indigenous, People of Color (BIPOC) with disabilities:
-
- Increased risk for police brutality
- Half of Black people with disabilities have been arrested at least once by age 28
- Half of people killed by law enforcement have disabilities (23)
Geographic Location
A person’s location also plays a role in the risk of domestic violence, with rural locations and homelessness increasing the risk.
Twenty percent of U.S. residents live in a rural location (17). Unique characteristics of rural living increase the prevalence and severity of domestic violence in the following three ways.
Geographic Isolation
- 80% of rural counties do not have a domestic violence program
- >25% of rural communities are more than 40 miles from the nearest domestic violence program
- Rural communities lack robust public transportation, and many people are without a car
- Decreased likelihood that a neighbor or community member will see or hear abuse occurring
- Significantly increased time needed for first responders to arrive after an emergency call
- Scarcity of housing options, especially of lower cost, make it difficult to leave (17)
Social/Cultural Barriers
- Rural regions are often more conservative with traditional gender roles (physical or sexual violence against women may be viewed as “normal”)
- Physical and sexual violence or assault may be viewed as private matters not to be discussed outside of the home
- Friends or family may encourage victims to stay in abusive relationships to avoid divorce or for children
- Women may be shamed or not believed for reporting abuse
- Small-town gossip or lack of anonymity may keep victims from pressing charges or seeking assistive services
- Women may be less likely to have a job or financial independence from their partners (17)
Poor or Impartial Criminal Justice Response
- Domestic violence may be seen as commonplace and low priority among law enforcement
- Law enforcement, prosecutors, or judges may have relationships with perpetrators or their families that impede their ability to be impartial
- Law enforcement may hold a patriarchal sense of loyalty to other men and put that above the safety of women in the community (“Good ol’ boys club” attitude) (17)
Due to geographic isolation and lack of resources, as well as potential lack of income or financial independence, many victims in rural locations wind up homeless if they leave an abusive relationship. This comes with its own significant struggles and risks and is often not sustainable, leading the victims back to live with their perpetrators rather than continue being homeless, essentially creating a vicious cycle between homelessness and abuse.
- A 2003 survey revealed 46% of homeless women reported being a victim of physical or sexual abuse in the last year.
- In 2005, 50% of U.S. cities cited domestic violence as a leading cause of homelessness.
- Some landlords have a zero-tolerance policy for domestic violence and will either evict or refuse to rent in the first place to victims of domestic violence. This was as high as 28% in a survey in New York City (27)

Self Quiz
Ask yourself...
- Think of the type of geographic area you work in. What types of resources are available and how long would it take to get there?
- Is public transportation available to take clients there?
- If you had a client who was physically assaulted, how likely would neighbors be to hear or see the incident?
- How long would it take emergency services to get there if your client called 911?
- Now think about how those factors might differ in a location very different from your own
Socioeconomic Status and Education Level
Though people of any socioeconomic status are susceptible to domestic abuse, those with a low socioeconomic status or education level are at an increased risk. This is in part due to the increased isolation and lack of available resources to people in poverty or with low education. Particularly, women who do not work outside of the home or do not have any professional skills with which to get a job are at risk of being more easily isolated or kept from utilizing resources. Those with lower education levels are also more likely to view physical or sexual violence within a relationship as “normal” and tolerate the abuse without attempting to leave.
Women with household incomes below $75,000 annually are seven times more likely to experience physical or sexual violence than women whose household incomes are above $75,000 (27).
There is also a circular relationship between low socioeconomic status and domestic violence, as victims of abuse are both more likely to be poor and also more likely to experience economic loss or financial insecurity due to the abuse. Access to money or work can also be restricted by the abuse as part of the attempt to maintain power and control.
- Between 21-60% of abuse victims lose their jobs from abuse-related reasons (missing work, distracted or poor job performance, etc.)
- Domestic abuse victims lose a combined eight million days of paid work annually due to injuries or home conflict (18).
Immigrants, in particular, may be affected by this as they may be of lower education (or at least unable to fluently speak the language of the new country), often poor or without any assets, and may be unable to work or earn money. They may rely on an abusive partner for money, a place to live, and even communication, keeping them isolated in a relationship that feeds on control/power (25).


Self Quiz
Ask yourself...
- Are there any of the above statistics or risk factors that surprised you?
- Do you think any of the above information might change your awareness of potential abuse situations?
- Think of a time when you cared for someone at an increased risk of abuse. Do you think you were aware of the risk or were you on the lookout for signs of abuse?
- If you have cared for known victims of abuse, what risk factors did they have?
Health Implications of Abuse
There are many health implications for people in abusive relationships. Acute or short-term injuries are typically physical in nature and include things like (9):
- Cuts
- Bruises
- Broken bones
- Concussions
- Burns
Additionally, only 34% of people who sustained a physical injury from domestic violence sought medical care for those injuries, meaning many may have poorly healed injuries or long-term sequelae from lack of proper treatment (18).
There are also long-term consequences or chronic health conditions that result from domestic violence, including:
- HIV or other sexually transmitted infections (STIs) from sexual abuse
- Bladder and kidney infections
- Circulatory/cardiovascular conditions
- Asthma
- Unintended pregnancy, including teenage pregnancy
- Chronic pain
- Arthritis or joint disorders
- Gastrointestinal disorders or nutritional deficiencies
- Neurological disorders including migraines and neuropathy
- Sexual dysfunction (9)
Mental health effects are also significant with victims experiencing increased rates of:
- Anxiety
- Depression
- Post-traumatic stress disorder (PTSD)
- Suicidal thoughts and attempts
- Addiction to drugs or alcohol (9)
Certain populations, such as individuals in the LGBTQ community, are already at an increased risk for mental health issues and suicidal ideations. Therefore, abused members of this population are at a further increased risk.
Additionally, victims of abuse may experience social or economic consequences that in turn worsen their overall health through poorer living conditions, nutrition, and access to healthcare. Economic consequences include (9):
- Interrupted or lost educational opportunities
- Lost professional opportunities
- Damage or destruction to property or items of value
- Medical or legal debt
Health implications may be dependent on age or situation as well. Among the unique risks are pregnant, very young, and very old victims.
Abuse during pregnancy can result in intrauterine hemorrhage, preterm labor, or miscarriage. Chronic stress during pregnancy, lack of prenatal care, or trauma to the fetus can lead to long-term health effects of the infant once born (14). Some women may also be victims of contraceptive or reproductive coercion, where an abuser pressures them to become pregnant or tampers with their contraception to cause pregnancy. Unwanted pregnancy puts these women into a more vulnerable position to be victims of abuse and the above complications (1).
Surveys of youth show that 50% of teens and young adults who have experienced dating violence or rape have also attempted suicide compared to 12.5% of youths without a history of abuse (19). Domestic violence also increases the risk of pregnancy and STIs which can have a more extreme and lasting impact on teens, affecting reproductive or sexual health for the rest of their lives.
For older adults, the risks are increased as well, with elderly victims of abuse having a shorter lifespan than their peers who are not abused. Mental health effects such as depression, anxiety, fear, isolation, loss of self-esteem, and feelings of shame, powerlessness, and hopelessness may be exacerbated because people in this age group are already struggling with a lack of independence or isolation from a social network. Overall, this can reduce quality of life and dignity in an already difficult period of decline (21).
Exposure to domestic violence, even when not directly victimized, also has a lasting impact on health. Children are particularly vulnerable to witnessing or being exposed to abuse:
- 1 in 15 children are a witness to domestic violence during childhood (of those, nearly 60% experience maltreatment themselves).
- Homes with both child maltreatment and intimate partner violence often have more severe levels of abuse.
- 1 in 5 child homicides between ages 2-14 are related to domestic violence cases (15).
Children who are exposed to domestic violence may experience acute symptoms such as:
- Anxiety
- Aggression
- Sleep disruption
- Nightmares
- Bedwetting
- Concentration deficits or poor school performance
Over time, children who are exposed to domestic violence are:
- 3 times as likely to engage in violent behavior as their peers
- More likely to be either perpetrators or victims in their own future relationships
- At greater risk of health conditions like obesity, cancer, cardiovascular disease, substance abuse, depression, and unintentional pregnancy (15)


Self Quiz
Ask yourself...
- Have you ever cared for an acute victim of physical or sexual violence?
- What types of injuries did they have and how might those injuries have healed differently if the client had not sought care?
- To your knowledge, have you cared for any clients with long-term sequelae of abuse?
- How do you think coping with a chronic illness sustained from violence might be different from coping with a chronic illness not sustained from violence?
Perpetrators of Abuse
It is important for healthcare professionals to not only recognize risk factors for victims of abuse, but also risks for becoming a perpetrator of abuse. Truly mitigating risks and reducing the prevalence of domestic abuse requires recognizing and offering services to victims, but also identifying potential abusers and providing interventions to stop abuse at the source.
Risk Factors
The conditions that lead to perpetrators becoming abusers are nuanced and multifaceted, involving individual experiences, past relationships, attitudes of the person’s community, and societal implications (4).
Individual
Individual risk factors are based on lived experiences, existing mental health conditions, and individual stressors. Individual risk factors include:
- Poor self esteem
- Low education level
- Young age
- Problem behaviors in youth
- Drug or alcohol abuse
- Depression or anxiety
- Poor coping or problem-solving skills
- Poor impulse control
- Personality disorders
- Isolation or few friends, small support network
- Economic stress such as unemployment or low income
- Hostile/misogynistic attitudes towards women and strict gender role of male dominance
- Being physically or emotionally abused as a child
Relationship
Relationship risk factors are based on the characteristics of the people involved in the relationship and their attitudes and behaviors within the relationship. Relationship risk factors include:
- Relationships with frequent jealousy, possessiveness, tension, or divorces and separation
- One partner with clear dominance or control the majority of the time
- Families undergoing economic stress or low income
- Network of peers in aggressive or violent relationships
- Parents with low education levels
- Witnessing violence between parents during childhood
Community
Community risk factors are based on the attitudes and social norms of people in the neighborhoods, workplace, or schools a person is involved in. Community risk factors include:
- High poverty and low education rates
- High unemployment rates
- High crime/violence rates
- High drug use
- Low sense of community among neighbors
Societal
Societal risk factors are based on the attitudes and political policies where a person lives on a broader scale, including city and state level. Societal risk factors include (4):
- Emphasis on traditional gender roles (women at home/unemployed/submissive, men work and make family decisions)
- Cultural norms of aggression
- Weak education, health, and social policies or support
Protective Factors
There are some factors that are protective against becoming a perpetrator of abuse, even for people who may have grown up around domestic abuse. Protective factors include (4):
- A strong social support network
- Exposure to strong, positive relationships
- An involved and neighborly community
- Available services and resources within a person’s community
- Access to stable and safe housing
- Access to medical and mental health care
The Cycle of Abuse
In addition to recognizing who may become or be an abuser, it is important to understand and recognize the pattern or cycle of abuse and how perpetrators maintain control in the relationship. While each abuse scenario is unique, the overall patterns are the same and exist in a cycle which may progress quickly or over longer stretches of time. The four main stages are tension, incident, reconciliation, and calm (10).
Tension Phase
During the tension phase, there is a slow increase in the frequency and intensity of irritability, short temper, emotional outbursts, and impatience. There may be external factors such as life stressors, financial strain, work struggles, etc. that make the abuser feel out of control, adding to this rising tension. Victims may report “walking on eggshells” during this time, as they feel the tension build (10).
Incident Phase
Once the tension builds to a breaking point, one or more abusive incidents will occur. Abuse perpetrators do not have an “anger problem” as they are able to control their emotions in places like work, school, or in public. The anger and aggression displayed by a perpetrator is an intentional use of power to regain or maintain control over the weaker partner in the relationship. Incidents can look like (10):
- Intimidation
- Threats
- Physical violence
- Sexual violence
- Verbal violence (insults, name calling)
- Shaming/humiliation
- Blaming
- Social isolation
- Manipulation
- Financial abuse
- Emotional abandonment
Abusers can use many methods of violence and a variety of tactics within each of those methods. The ultimate goal of all behaviors is to maintain control over the victim and remain in a position of power. Figure 1 below provides examples of specific behaviors within each type of violence.
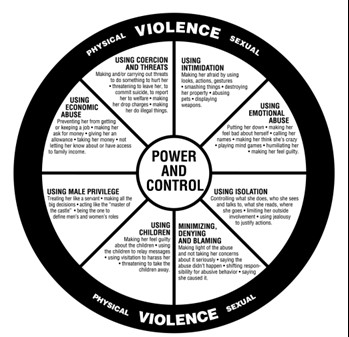
Figure 1. Domestic Abuse Intervention Programs (3)
Reconciliation Phase
Once the incident is over, the perpetrator feels a relief of tension, though the victim likely is at peak anxiety. The abuser may seem to show remorse in the form of apologies, affection, or promises to never become violent again. Victims are often willing to give abusers another chance during this stage because they seem to show genuine remorse or intent to reform (10).
Calm Phase
Next the relationship moves into a calm phase where the perpetrator’s remorse dissipates, and they may begin to dismiss the incident by shifting blame or saying things like “it wasn’t really that bad.” For the victim, this can be confusing or feel like a letdown when the abuser’s previous intent to make changes fades. This eventually shifts back into rising tension and the cycle repeats itself (10).

Self Quiz
Ask yourself...
- Think about the population you work with. Consider who might be at risk for being a victim of abuse but also think about what risk factors you’ve encountered for your clients becoming a perpetrator of abuse.
- What are the community or societal factors in your region that might increase the risk of becoming a perpetrator?
- Think about the abuse cycle and consider why victims may choose to stay in a violent relationship.
- At what point in the abuse cycle do you think healthcare professionals are most likely to encounter victims of abuse or pick up on abuse red flags?
Role of the Healthcare Professional in Abuse
Given all of this knowledge about who is at risk and what goes on in an abusive relationship, you may be wondering how healthcare professionals can help or what your role entails. The responsibility of the healthcare professional lies in a few main areas of identifying and handling abuse situations.
Risk Identification
One of the first steps in disrupting the abuse cycle is identifying those most at risk. Part of this is through knowledge of risk factors and vulnerable populations and signs of abuse, as already covered in this course. Another means of identification is through routine screening of certain populations. Unfortunately, there is a limited number of screening tools available, and tools are almost exclusively targeted at women of reproductive age. Available tools assess for domestic abuse within the last year; there is no recommended appropriate interval to administer screening and it is at the provider’s discretion, though at least annually is typical (24). Some examples of available screening tools include:
- HARK (Humiliation, Afraid, Rape, Kick): A four-question tool that assesses emotional and physical violence
- HITS (Hurt, Insult, Threaten, Scream): A four-item tool that assesses the frequency of domestic violence
- E-HITS (Extended version of HITS): Includes an additional question to assess the frequency of sexual violence
- PVS (Partner Violence Screen): A three-item tool that assesses physical abuse and safety
- WAST (Women Abuse Screening Tool): An eight-item tool that assesses physical and emotional abuse from domestic partner (24)
The above screening tools are well studied in women and have been shown to be effective. Currently, there is a lack of studied and effective domestic violence screening tools in the primary care setting, especially for teens, men, clients in the LGBTQ community, and the elderly. More work is needed in this area. Even for women, screening is not often conducted outside of the obstetrics/gynecology (OB/GYN) setting (24).
Simply asking “Do you feel safe at home?” or “Is there any history of violence in your home?” is also a basic way to cast a wide net among large volumes of patients and reduce the chance of domestic violence going unnoticed. Asking questions like these on admission in the emergency department (ED) or hospital, or during the intake process for office visits can easily be implemented as part of facility policy. Many offices or hospitals will also have signs up in bathrooms, changing areas, or exam rooms that encourage clients to disclose abuse in a confidential and safe way during their visit (24).
Screenings of any kind are most effective when the client is separated from their partner, even briefly. If the abuser is with them, they can be asked to step into the waiting room or, if it is necessary to be more subtle, clients can be asked to leave the room for something inconspicuous, like providing a urine sample, and then lead to a separate room for further, private discussion (24).
Appropriate Response
Timely referral to appropriate ongoing services has been shown to reduce physical and mental harm from violence and abuse. When domestic violence has been disclosed or a screening has come back positive, the attitudes and behaviors of the healthcare professional are important and can have a big impact on the client’s feelings about their care. Appropriate and sensitive behaviors include:
- Listening to clients actively and objectively
- Believing the client
- Validating the client’s feelings and fears
- Avoiding asking “why” questions or placing blame like “Why didn’t you call the police?” or “Why do you stay?”
- Respecting a client’s decision to stay or leave
Plan of Action
Interventions and next steps include (6):
Gathering Additional Information
- Getting a detailed history
- Assessing symptoms
- Taking photographs if necessary (bruise patterns, burns, cuts, etc.)
Assessing Safety
- Verbal/physical threats
- Weapons in the home
- Frequency of violence
- Children or others in the home
Develop a safety plan together with client
- Signs of rising tension
- Who to call or where to go
- Available resources in community
Provide referrals as desired by client
- Police (for order of protection or to press charges)
- Hotlines
- Shelters
- Counseling
Documentation and Reporting
Appropriate documentation of abuse, including detailed history, exam, and any pictures, as well as a safety plan and any resource connection should be included in the client’s chart. Laws about mandated reporting vary by state and healthcare professionals may need to report the documented abuse to authorities.
In Connecticut, there is no requirement to report domestic violence or abuse. Mandated reporting is reserved for abuse of children, disabled people, residents of long term care facilities, the elderly, and healthcare professionals who are impaired or negligent (8).
For situations which must be reported, the report must be made within 12 hours of when a clinician first suspects abuse or becomes aware of an abuse situation. Reports may be made through the Connecticut State Department of Public Health which has various resources and care lines depending on the type of suspected abuse being reported. Examples can be found in the table below (8).
|
Category of Abuse Victim |
Resource for Reporting |
|
Children |
Department of Children and Families (DCF) Child Abuse and Neglect Careline |
|
Disabled person |
Office of Protection and Advocacy for Persons with Disabilities |
|
Residents of long term care facilities |
Commissioner of Social Services |
|
Elderly |
Commissioner of Social Services |
|
Impaired clinicians |
Connecticut Department of Public Health |
If you are required to report an incident, it is best to notify the client prior to reporting so that they are aware and prepared and can utilize their safety plan if they feel this will anger the perpetrator (6).
Counseling/Therapy
When considering counseling, individual therapy is always recommended and beneficial, but it is important to note couples therapy may be contraindicated. If the goal is to maintain the relationship and address abuse cycles, couples therapy should be approached cautiously as this type of treatment may increase the abusive behaviors. Couples therapy may elicit a different viewpoint or information about the relationship that threatens the abuser's desire for control and may increase anger, minimization of abuse, or victim blaming as the abuser now has to work harder to maintain control. This can increase abusive behaviors outside of therapy sessions and put the victim at greater risk.
There is some evidence to suggest couples therapy can be helpful in breaking abuse cycles, but it should only be undergone with an experienced therapist with special knowledge of how to identify and address abuse in a manner that does not exacerbate the abuse (12 ).
Follow Up
Often domestic violence reoccurs and increases in frequency or intensity over time. Up to 75% of clients reporting domestic violence will continue to experience abuse. This can be frustrating for healthcare professionals, but it is important to remember that your role is to document the abuse, provide resources to clients, report when required, and not judge or verbalize opinions on what clients should do (2).
Appropriate follow up for healing wounds or injuries should be scheduled. Information about local domestic violence resources should be provided at each visit with clients. If a client does leave an abusive relationship, it is important to continue screening for violence as they may return to the relationship and are at an increased risk of entering new relationships that are also abusive (2).
Community Outreach
Healthcare professionals can have an impact on domestic violence in broader ways that direct client interactions as well. Advocacy on a community level can help increase awareness, shift harmful societal views on domestic violence, and create more robust community resources. Places where healthcare voices can help shift the narrative on domestic violence include (6):
- Parent Teacher Association (PTA) members
- Church members
- Community leadership positions
- Social clubs
- Political/voter groups
- Connecticut Coalition Against Domestic Violence (CCADV)
Nursing Education
RNs with a Connecticut license must apply for renewal every 6 years. They are not required to obtain CEUs specific to domestic or sexual violence for license renewal, though the topic is strongly recommended as these issues can impact clients across a variety of demographics and in many different healthcare settings. Required topics for license renewal include screening for PTSD, depression, and risk of suicide, and training for suicide prevention (7).
Connecticut APRNs must complete 50 hours of continuing education every 2 years and are required to complete at least 1 hour each on the topics of sexual assault and domestic violence. Having compassionate, knowledgeable, and competently prepared providers in delicate situations such as abuse, or violence can increase client safety and improve overall health outcomes (7).

Self Quiz
Ask yourself...
- What tools or processes does your current facility use to screen for abuse?
- How could your facility improve on those screening practices?
- If your facility does encounter someone who discloses abuse, what processes are in place for next steps of reporting and connecting with resources?
Case Studies
Kimari’s Case
Kimari is a Black, 22-year-old pregnant woman who presents to the OB clinic for a second trimester visit with complaints of abdominal pain. Kimari’s partner accompanies her to the visit today and the nurse notes that Kimari is unusually quiet and withdrawn compared to her previous visits. Her partner is answering most of the nurse’s questions for her. The nurse asks him to step into the waiting room so Kimari can change into a gown. Once he is gone, the nurse administers the HITS screening tool and opens a discussion with the client. Kimari reveals that her partner had been emotionally abusive in the past but never physically. However, since she has become pregnant, the abuse has worsened and has started to include forced sexual activity and physical violence. She admits her abdominal pain today is due to him shoving her down the stairs in the house the day before.
The nurse sits with Kimari and listens to her description of the events of the last few weeks. At this time, she wants to stay in the relationship as she does not have anywhere else to go and also has a two-year-old at home to think about. She is interested in individual counseling and develops a safety plan with the nurse which includes hotlines and local resources, as well as a plan to go to her sister’s house if tension seems to be rising again.
A physical exam reveals a healthy pregnancy with normally developing fetus and no complications from the fall down the stairs. The information from today’s visit is documented in her record and a follow-up appointment is scheduled for the following month.


Self Quiz
Ask yourself...
- What risk factors does this client have for being a victim of abuse?
- What potential complications can occur during pregnancy due to physical violence?
- What interventions did the nurse utilize appropriately when handling Kimari’s case?
- How do you feel about the outcome of this case? Do you have preconceived ideas about how this case should be handled that you would need to adjust in order to provide sensitive care like this nurse did?
Kevin’s Case
Kevin is a 28-year-old gay man presenting to the family practice clinic for an annual wellness visit. Kevin’s provider conducts a thorough physical assessment, orders labs, and administers screening tools for anxiety and depression. Kevin is found to be in good health but does score moderately high on his depression screening. The provider caring for him recommends individual counseling and offers an antidepressant which Kevin accepts. He is scheduled for a follow up in one month and the visit concludes.
Kevin returns home where he lives with an emotionally abusive husband. When Kevin reveals that he was given a prescription for an antidepressant, his husband ridicules him and calls him “crazy” and “weak.” They get into an argument and Kevin’s husband slaps him.
Later that evening, Kevin’s husband finds him unresponsive but still breathing in the bathroom with what appears to be an attempted overdose. He calls 911.


Self Quiz
Ask yourself...
- What risk factors does this client have for being a victim of abuse?
- What risk factors does this client have for suicidal thoughts or actions?
- How could this case have been handled differently?
- Without standard screening tools for domestic violence in LGBTQ relationships, how could Kevin’s provider have assessed for safety within his relationship?
Conclusion
Domestic violence, particularly physical and sexual abuse, is a problem with far-reaching consequences that affects people of all demographics. Identification of those most at risk, early intervention, and connection to resources, as well as prompt treatment of acute injuries and health implications are all important components in reducing the tragic impact of domestic violence. Healthcare professionals in all settings may encounter abuse situations and should be up to date on best practices for screening and management of these cases. Hopefully upon completion of this course, healthcare professionals will feel confident in their role in supporting victims.

Self Quiz
Ask yourself...
- Have you ever reported an abuse situation? If so, what was the process like? Did you find it effective or have concerns?
- What community involvement opportunities exist in your community that can have an impact on domestic violence resources?
➀ Read and Learn
The following course content
HIV/AIDS
Introduction and Objectives
An estimated 1.2 million Americans are living with HIV. As many as 1 in 7 of them do not even know they are infected. The others utilize the healthcare system in a variety of ways, from testing and treatment regimens to hospitalizations for symptoms and opportunistic infections. Healthcare professionals in nearly every setting have the potential to encounter patients with HIV as the disease can affect patients of any age or stage of life (4). Proper understanding of HIV is important in order to provide high–quality and holistic care to these patients.
Upon completion of this course, the learner will:
- Have an increased understanding of the history of HIV and how stigma around the disease developed and is being combated today.
- Demonstrate an understanding of how a person is infected with HIV and the various stages of the disease.
- Demonstrate understanding of transmission modalities and appropriate infection control measures.
- Have a basic knowledge of treatment approaches, common side effects, and barriers to proper treatment.
- Understand comorbidities and coinfections common with HIV.
- Understand ethical issues and confidentiality surrounding the care of HIV patients.
Epidemiology
In the early 1980s, a series of unusual and aggressive illnesses began popping up in clusters across the United States, affecting previously healthy men. Illnesses such as pneumocystis pneumonia, Kaposi‘s sarcoma, and severe wasting, all related to unexplained immunodeficiency, were suddenly rapidly increasing in prevalence, and the only common link seemed to be that it was occurring in gay men. By 1982, the term Acquired Immune Deficiency Syndrome (AIDS) was being used to describe a “moderately predictive…defect in cell–mediated immunity,“ but the details of disease trajectory and how men were contracting it were still foggy (2).
Over the next several years, cases continued to rise, and women and children began presenting with the disease, bringing scientists to the realization that it could be contracted through more ways than just homosexual sex. Amid the social panic, the retrovirus responsible was identified and named Human Immunodeficiency Virus, more reliable testing developed, and various other modes of transmission (like needle sharing, contaminated blood products, childbirth, and breastfeeding) were recognized. By 1989, less than a decade after the first cases were garnering attention, 142,000 cases were reported by 145 countries worldwide (2).
Over the next several decades, more and more information was discovered about HIV and AIDS, and scientists and legislators worked hard to understand and reduce transmission, increase quality and duration of life for those already infected, and fight the stigma and discrimination that had developed during the 1980s (2).
Today, approximately 1.2 million people in the United States are living with HIV, though 1 in 7 people don‘t know it. Rates of infection are not equal across demographic groups, and certain factors may increase a person‘s risk (10). Patient information to consider when determining someone‘s risk includes:
- Age: As of 2018, the age group with the highest incidence of new HIV diagnoses is 25-34 years or approximately 36% of new infections. Ages 13-24 are next, though the numbers in this age range are coming down in recent years. From there, the risk seems to decrease as people age, with the 55 years and older group accounting for only around 10% of new diagnoses each year (10).
- Race/Ethnicity: Currently, the highest rate of new infections is in African Americans, at approximately 45%. This is incredibly high when you consider that African Americans only make up 13% of the general population. This is followed by Hispanic/Latinos at 22% of new infections and people of multiple races at 19% (7).
- Gender: Men are disproportionately affected by HIV, accounting for five times the amount of new infections as females each year. This data refers to the sex of someone at birth. When looking at the transgender population, there is a nearly equal rate of new infections among those who have transitioned male-to-female and female-to-male. Together, transgender people account for 2% of new cases in 2018 (7).
- Sexual orientation: Gay and bisexual men remain the population most at risk of HIV, accounting for around 69% of all new infections in 2018 and 86% of all males diagnosed. Similar racial and ethnic disparities affecting all people with HIV still existed among gay and bisexual men (7).
- Location: Different areas of the country are affected at different rates for a variety of factors, including population density, racial distribution, and access to healthcare. The southern states are unmistakably more affected than other regions, with anywhere from 13-45 people per 100,000 having a diagnosis of HIV. California, Nevada, New York, and D.C. all having similar rates of infection as the southern states and are among the highest in the country. The Midwest and Pacific Northwest are next most affected, with 9-13 people per 100,000. The Northeast and Northwest have the lowest rates nationally at just up to 5 people per 100,000 (7).
While the effects of HIV and AIDS have resulted in a staggering 32 million deaths worldwide since the start of the epidemic, global and national numbers indicate that it peaked around 2005. Numbers of infections and deaths have been on a slow decline since then, mostly due to earlier and more accurate diagnosis, increased knowledge of how to prevent transmission, and effective and accessible treatments. An estimated 65% of Americans currently diagnosed with HIV are considered “virally suppressed,“ demonstrating that adherence to treatment guidelines means most infected people have virtually no risk of transmitting the virus to their partners and have a life expectancy nearly the same as non-infected people (6).
HIV/AIDS’s financial impact is also significant, with an estimated $380,000 spent throughout an individual‘s lifetime with the disease. In 2009, it was estimated that $16.6 billion was spent on HIV treatment in the U.S. alone. However, federal prevention programs do more than improve health outcomes and decrease the number of new infections; they also claim financial benefits and saved approximately $129 billion in the last two decades by averting new infections.
The Ryan White Program is notable and has been in place since 1990. It is a significant source of expanded coverage and funding for patients living with HIV who cannot afford health insurance or proper treatment. This safety net program is federally funded and named after a teenager who died from AIDS after receiving an HIV–contaminated blood transfusion. Ryan‘s story was also a turning point in the public perception of the disease, and the program helps fight the stigma surrounding HIV today (5).

Self-Quiz
Ask Yourself...
- Has the info about HIV/AIDs changed since you first learned it?
- Think about nurses who are from a different generation. How does their experience with this disease differ?
- How might your patients’ experiences or views of this illness be different from yours?
- Why is understanding the complicated history of this illness and its social stigma an important part of providing compassionate care?
- Is access to health insurance and quality healthcare more difficult for those with higher risk to obtain?
- What factors might make one area of the country more at risk than another?
Etiology and Pathogenesis
So just what is this virus that can cause so much devastation but took scientists years to understand? HIV is a type of retrovirus known as lentiviruses; these viruses have long incubation periods and lead to chronic and deadly infections in mammals. Studies indicate that the virus may have first infected humans hunting and eating the meat of infected chimpanzees in central Africa as early as the late 1800s. Once the virus jumped to humans, it spread slowly over many decades and across countries before picking up steam and attracting attention in the United States in the 1980s (7).
Once a host has been infected, the virus seeks out, attaches to, and enters CD4-T cells, immune cells largely responsible for attacking and clearing pathogens in the body. Once inside the cell, viral mRNA (or genetic code) directs the cell to become a factory of more HIV virions, which are then released through a process known as budding. Those virions travel through the body, enter other CD4-T cells, and produce more viruses in a slow but deadly cascade. As part of the body‘s defense against such pathogens, CD4-T cells are programmed for apoptosis (cell death) upon being taken over by a host. Others will experience cell death due to close proximity to infected cells. Still, others will be killed by other types of immune cells. While HIV ravages the body and continues to rise in viral load, the number of CD4-T cells will drop lower and lower until, eventually, the body‘s cell-mediated immunity is no longer viable. Without cell-mediated immunity, opportunistic infections and cancers can take over, and the infected person progresses from HIV infection to full–fledged AIDS (12).
Typically, the disease progresses in 3 stages.
- Stage 1 is acute HIV infection. The virus is reproducing rapidly, and affected individuals may experience flu–like symptoms, including fever, chills, headache, and fatigue. Not everyone experiences symptoms during Stage 1, but all are highly contagious during this period.
- Stage 2 is Chronic HIV infection; viral replication slows, and this stage can last for many years. A person in this stage is still contagious, but they may have no symptoms. Proper use of medication treatment may mean an infected person never moves past this stage.
- And finally, if the viral load continues to increase and the CD4-T cell count gets below 200 cells/mm, the illness transitions to Stage 3, AIDS. In this stage, even minor opportunistic pathogens can make a person very ill due to the lack of a properly functioning immune system. Symptoms and infections such as thrush, pneumonia, peripheral neuropathy, and Kaposi sarcoma are common. Stage 3 is very contagious and life expectancy is about 3 years if left untreated (7).

Self-Quiz
Ask Yourself...
- HIV is unique in that it primarily targets CD4-T cells inside the host. How does this directly contribute to symptoms and affect the trajectory of the disease?
- How does the body‘s natural defenses against such an invasion affect disease trajectory?
- Which stage do you think a person is most likely to be unknowingly transmitting the virus to others?
- Which stage do you think someone not undergoing routine testing is most likely to find out about their illness?
- What about someone who gets routine or yearly testing?
Transmissibility
Perhaps the most elusive part of this virus for many years was how it spreads. We now know that HIV is spread only through certain bodily fluids. An accurate understanding of HIV transmission is important for healthcare professionals to provide proper education to their patients, reduce misconceptions and stigmas, and prevent transmission and protect themselves and other patients (11).
Bodily fluids that can transmit the virus include:
- Blood
- Semen and pre-seminal fluid
- Rectal fluid
- Vaginal fluid
- Breastmilk
- Fluids that may contain blood such as amniotic fluid, pleural fluid, pericardial fluid, and cerebrospinal fluid
If one of these fluids comes in contact with a mucous membrane such as the mouth, vagina, rectum, etc., or damaged tissue such as open wounds, or is directly injected into the bloodstream, then transmission of HIV is possible (11).
Scenarios where transmission is possible include:
- Vaginal or anal sex with someone who has HIV (condoms and appropriate treatment with antivirals reduce this risk)
- Sharing needles or syringes with someone who has HIV
- Mother-to-child transmission during pregnancy, delivery, or breastfeeding (appropriate treatment during pregnancy, c-section delivery, and alternative feeding methods reduce this risk)
- Receiving a transfusion of infected blood or blood products (this is very rare now because of screening processes for blood donations)
- Oral sex with someone who has HIV (though this is very rare)
- A healthcare worker receiving a needle stick with a dirty sharp (risk of transmission is very low in this scenario)
HIV cannot be transmitted via:
- Saliva
- Sputum
- Feces
- Urine
- Vomit
- Sweat
- Mucous
- Kissing
- Sharing food or drink

Self-Quiz
Ask Yourself...
- What sort of PPE do you need to wear when helping an HIV+ patient use a bedpan?
- What about assisting with a procedure where blood splatter may occur?
- What factors about childbirth make this event particularly risky for transmission?
- What interventions might help reduce that risk?
- Think about the population you work with. What methods of transmission are they most at risk from?
- How might this differ among different populations or work settings?
Reducing Transmission
Patient education about risk and protection against HIV, testing, and what to do if exposed should be standard practice for healthcare professionals in nearly all healthcare settings. Primary care should include risk screenings and patient education routinely to ideally help prevent infections from even occurring or catch those that have occurred early on in the disease process (11).
Strategies include:
- Identifying those most at risk, incredibly gay or bisexual men, minority patients, and those using drugs by injection
- Ensure patients are aware of and have access to protective measures such as condoms and clean needle exchange programs
- Provide routine screening blood work for anyone with risk factors or desiring testing
- Providing access to PrEP medications where indicated (discussed further below)
- Staying up to date on current CDC recommendations and HIV developments
- Maintaining a nonjudgmental demeanor when discussing HIV with patients to welcome open discussion (11)
For patients with a repeated or frequent high risk of HIV exposure, such as those with an HIV+ partner or those routinely using IV drugs, pre-exposure prophylaxis (PrEP) may be a good choice to reduce the risk of them contracting the virus. When used correctly, PrEP is 99% effective at preventing infection from high–risk sexual activity and 74% effective at preventing infection from injectable drug use. Depending on the type of exposure risk (anal sex, vaginal sex, needle sharing, etc.), PrEP needs to be taken anywhere from 7-21 days before it reaches its maximum effectiveness. Most insurances, including Medicaid programs, cover PrEP at least in part. There are also federal and state assistance programs available to make PrEP available to as many people who need it as possible. Some side effects are commonly reported, primarily G.I. symptoms, headaches, and fatigue (11).
For those who have a confirmed diagnosis of HIV/AIDS, the focus should be promoting interventions that will prevent further transmission. One of the biggest determinants for transmission is the infected person’s viral load. Individuals being treated for HIV can have their viral load measured to ensure viral replication is being controlled as intended. A viral load lower than 20-40 copies per milliliter of blood is considered undetectable, meaning the virus is not transmissible to others. Even for those not receiving treatment, there are methods to reduce transmission (11).
Important considerations for transmission in patients who are HIV+ include:
- Referral for treatment and educating on the importance of treatment compliance in order to keep the viral load as low as possible
- Education on the importance (and possible legal consequences) of proper disclosure to any sexual or needle–sharing partners who may be at risk of exposure
- Encouraging and assisting with access to condom use and clean needle programs
- Providing information to HIV+ pregnant women about how interventions such as proper treatment during pregnancy, c-section delivery, and formula feeding can keep the risk of transmission as low as 1% (11)
Methods of infection control for healthcare professionals include:
- Universal precautions when handling any bodily fluids
- Eyewear when at risk for fluid splashing
- Careful and proper handling of sharps
- Facilities having a standard plan in place for potential exposures
If exposure or needlestick do occur for healthcare professionals, the patient would ideally submit to testing for HIV to determine if the staff member is even at any risk. If the HIV status of the patient is unknown or confirmed to be positive, four weeks of post–exposure prophylaxis (PEP) may be advised within 72 hours of exposure (11).
PEP is meant for emergency use only, such as for healthcare workers with a potential exposure or patients with an exposure that is not expected to become routine. PEP is not meant to replace the use of PrEP or other preventative measures. In order to be effective, PEP must be started within 72 hours of the potential exposure and must be taken for a 28–day course of treatment. When used correctly, it is highly effective and typically well–tolerated, with nausea being the most common side effect. For healthcare professionals taking it due to workplace exposure, your facility should cover the cost. For patients in the general population, insurance will usually cover it, or there are assistance programs available to make it affordable for everyone (11).

Self-Quiz
Ask Yourself...
- What screening questions or protocols are in place where you work to detect those most at risk of contracting HIV?
- In what ways, if any, could your facility improve its screening protocol to identify more at–risk patients?
- What information should be given to a pregnant woman with HIV who is asking about different infant feeding methods?
- Do you know what your facility‘s blood–borne pathogen protocol is?
- What steps are in place to help you if you get a dirty needle stick?
- Think about the population you work with. Are there any patients that might benefit from routine use of PrEP?
- What sorts of scenarios might indicate the need for the use of PEP?
Treatment Considerations
When HIV is appropriately treated, advancement from HIV to AIDS can be significantly reduced, and quality and longevity of life maximized. In 2018, the CDC estimated around 65% of all U.S. citizens living with HIV were virally suppressed, and 85% of those receiving regular HIV–related care were considered virally suppressed. However, an estimated13% of all HIV cases do not know they are infected. Appropriate medical care and keeping viral loads undetectable is one of the single most effective methods of preventing transmission (4, 6).
For those receiving treatment, a multifaceted and individualized approach can reduce a person‘s viral load, reduce the risk of transmission, reduce the likelihood of developing AIDS, and preserve the immune system. Regardless of how early someone receives treatment, there is no cure for HIV, and an infected person will be infected for life. All individuals diagnosed with HIV (even asymptomatic people, infants, and children) should receive antiretroviral therapy or ART as quickly as possible after a diagnosis of HIV is made. There are seven different classes of antiretroviral medications that disrupt various points in the viral replication process. Most treatment regimens use several of these medications combined with the most effective results; some combination pills are also available for administration ease. Medication regimens are chosen based on a patient‘s health status and history, tolerance or sensitivity to medication, and stage and severity of HIV infection. Patient condition and viral load should be monitored closely, and changes or inadequate response to treatment may indicate the need for a change in medication regimen at any time (1).
The classes and available medications for ART include (1):
Nucleoside reverse transcriptase inhibitors (NRTIs): these inhibit the transcription of viral RNA to DNA
- Abacavir (Ziagen)
- Emtricitabine (Emtriva)
- Lamivudine (Epivir)
- Tenofovir disoproxil fumerate (Viread)
- Zidovudine (Retrovir)
Non-nucleoside reverse transcriptase inhibitors (NNRTIs): these inhibit the transcription of viral RNA to DNA
- Doravirine (Pifeltro)
- Efavirenz (Sustiva)
- Etravirine (Intelence)
- Nevirapine (Viramune, Viramune XR)
- Rilpivirine (Edurant)
Protease inhibitors: inhibit the final step of viral budding
- Atazanavir (Reyataz)
- Darunavir (Prezista)
- Fosamprenavir (Lexiva)
- Ritonavir (Norvir)
- Saquinavir (Invirase)
- Tipranavir (Apitvus)
Fusion inhibitors: prevent the virus from fusing with CD4-T cells
- Enfuvirtide (Fuzeon)
Integrase strand transfer inhibitors (INSTIs): these stop HIV from inserting its DNA into cells
- Dolutegravir (Tivicay)
- Raltegravir (Isentress, Isentress HD)
Chemokine receptor antagonists (CCR5 antagonists): prevent the virus from binding to CD4-T cells
- Maraviroc (Selzentry)
Entry inhibitors: prevent the virus from binding to and entering cells
- Ibalizumab-uiyk (Trogarzo) (1)
These types of medication do not come without side effects or complications. Most side effects fit into a few major groups and may be bothersome but are not life–threatening or serious. More Serious or worrisome adverse effects may occur, and a patient‘s current health status, as well as medical history or existing conditions, should be carefully considered (3). The common categories of adverse medication reactions include:
- Gastrointestinal: Nausea, vomiting, diarrhea, decrease in appetite, reflux, constipation, damage to liver or pancreas
- CNS: Headache, dizziness, sleep disturbance, neuropathy, memory problems, hearing impairment or tinnitus
- Hematological: Anemia, hematuria, hyperbilirubinemia
- Psychological: Mood swings, anxiety, depression, confusion, nightmares/vivid dreams
- Dermatological: Rash, face discoloration, pruritus
- Musculoskeletal: Body aches, abnormal fat distribution
- GU: Menstrual cycle disruption
Due to the need to take medications for the rest of one‘s life and the long list of potentially bothersome side effects, medication adherence is a common issue in treating HIV appropriately (3).
There are several scenarios that increase the likelihood of poor compliance, including:
- Asymptomatic patients, since side effects of medications, maybe unpleasant and they are in a latent phase of disease without symptoms
- Young patients, including children or teenagers who may not understand the necessity of taking daily medications and face a lifetime of treatment
- Patients with substance abuse or mental health issues, as they may be in and out of cognitive and psychiatric crises
- Poor literacy or education level, as these patients may be easily confused by a complicated medication regimen or simply not understand the importance of lifelong therapy, especially if they are feeling well
- Social stigma, which may lead people to try and hide medications or not want their diagnosis to be discovered (3)

Self-Quiz
Ask Yourself...
- Why might it be important to take several medications that interrupt the viral replication process at different points?
- Think about the population you work with. What potential barriers to proper treatment are there?
- Think about the potential side effects of medications for HIV. How difficult do you think it would be to keep taking a medication like that, even if you understood why you needed it?
- Do you think it would be difficult to take daily medication if you had no symptoms and felt well?
Care Considerations for Comorbidities and Coinfections
Caring for patients with HIV or AIDS is a complicated task requiring compassion, patience, and understanding the many potential complications and ways that various body systems are affected. Many infections and comorbidities commonly present alongside HIV/AIDS, particularly as patients age, immune function declines, and effects of long-term medication use develop. The social stigma and psychological impact of such a devastating disease must also be considered to provide holistic care to these patients (9). Common coinfections/comorbidities include:
Tuberculosis
T.B. is a highly contagious airborne illness that affects the respiratory system. It is an opportunistic infection that frequently affects people with weakened immune systems, like those with AIDS. The bacteria can live in the body without causing symptoms in a latent phase for long periods. As the immune system in HIV weakens, a latent T.B. infection may become active, causing symptoms and deteriorating health. Most common symptoms include cough, hemoptysis, fever, fatigue, night sweats, or poor appetite, and weight loss. Seriously immunocompromised people may even experience disseminated T.B. where the infection affects more than the lungs and can even lead to septic shock and death. Annual PPD tests for T.B., or chest X-ray for anyone with a history of positive PPD, should be conducted on patients with HIV (9).
Hepatitis
About 1 in 10 people affected by HIV will also have viral hepatitis, as the diseases are spread in much the same way, particularly needle sharing and sexually and vertically (mother to fetus). Hepatitis infections progress quickly in immunocompromised patients and can greatly reduce liver function, which complicates the use of ART medications and can result in poor clearance from the body. All new HIV diagnoses should be screened for Hepatitis A, B, and C, and Hep A and B vaccines should be encouraged in unvaccinated patients (9).
STIs
Because HIV can be acquired via high–risk sexual activity, infection with other STIs is common. Sometimes, other STIs may even increase the risk of contracting HIV as they result in open sores or breaks in the skin where HIV can more easily enter. Bacterial STIs can typically be cured with antibiotics, but other viral STIs like Herpes and HPV do not have a cure. Routine screening for patients engaging in high–risk sexual activity or those already infected with HIV should be a typical part of care (9).
Cardiovascular Disease
Studies show that patients with HIV also increase inflammation of the arteries and plaque formations throughout the body due to a complicated effect on macrophages. Some of the ART medications also increase the risk of heart attack or stroke. Concurrent infection with hepatitis can increase cholesterol, which further deteriorates cardiovascular health and increases MI or stroke risk. Patients with HIV should be screened for family history and current heart health, and their plan of care should incorporate ways to reduce risks, including a focus on diet and activity level (9)l.
Osteoporosis
Bone density has been shown to decrease faster than normal in patients receiving ART medications, and it is recommended that patients over age 50 have annual bone density scans to estimate fracture risk. Treatment for osteoporosis should be added to the plan of care as needed (9).
Cancer
As science has become better equipped to detect and treat HIV and concomitant infection, cancer has remained a leading cause of death for HIV patients and is a considerable risk for those living with the disease. Most commonly, cancers of the head and neck, anus, lungs, liver, and lymph system occur. Smoking cessation, regular pap tests for women, HPV vaccines, and routine screenings like colonoscopies after a certain age should be heavily counseled in HIV patients to reduce their risk further. Earlier and consistent ART has been shown to reduce the risk of developing cancer (9).
Mental Health Issues
When considering the long–term and eventually fatal nature of this disease, along with the social stigma and complicated and expensive treatment regimens, it is no surprise that mental health disorders such as anxiety and depression are common for patients with HIV. Upwards of 22% of patients with HIV will suffer from depression, likely higher when you account for substance abuse disorders. In addition to assessing and treating body systems affected by the virus, it is important to screen patients for psychiatric disorders and be aware of the negative effects the diagnosis may be having on mental health. Medication treatment and therapy should be included in care where appropriate (9).

Self-Quiz
Ask Yourself...
- Think of the common health concerns in the population you work with, particularly when age and family history are factored in. How would a diagnosis of HIV affect those risks and health considerations?
- Consider what it would feel like to have a diagnosis of HIV and then be given a diagnosis of cancer or T.B. How do you think you would feel?
- How do you think your mental health would be affected?
- What other potential screenings or lifestyle changes would be a good idea for someone with HIV?
Ethical Concerns
Maintaining confidentiality under HIPAA laws is essential in the care of patients with any diagnosis, but the social stigma attached to HIV infection–in addition to the frequency and intensity of medical care needed and the responsibility to notify partners and prevent further spread–makes confidentiality particularly challenging with many ethical considerations to navigate.
The first issue with maintaining confidentiality occurs with testing itself. HIV is considered a reportable disease. Any positive results must be reported to a local health department and then on to the CDC for local and national statistics and to initiate follow–up with the positive person and provide education on the next steps. Patient names and identifying information are included with the positive result when reported to local and state health departments but is removed before it is reported to the CDC. There is an option for anonymous testing where patients are given a special identification number, and their names and identifying information are not included. These are often self–administered tests and are not available everywhere (8).
Testing for HIV requires informed consent, meaning healthcare professionals must discuss the risks, benefits, and potential consequences of testing for HIV and cannot test someone for HIV without their consent. Minors’ ability to get testing and treatment for HIV without a parent or guardian’s consent varies from state to state (8).
Once someone tests positive for HIV, the issue of disclosure presents itself. Patients need to inform their past and future sexual partners or anyone they share needles with of their HIV status. Health departments will help contact tracing and notifying past partners and help those potentially exposed with their testing and prophylactic treatment options. In some states, it is considered a criminal offense to withhold a positive infection status when a person may be exposing others. However, the responsibility to disclose falls on the patient, and healthcare professionals may not notify potential contacts without a patient‘s consent. Infected persons are not required to inform friends, family, employers, or others who are not at risk of contracting the disease (8).
Employers who provide health insurance for their employees may be given information about the costs and benefits of disclosing an HIV diagnosis indirectly. So while insurance companies cannot directly tell an employer about an HIV diagnosis, employees should be aware the information may come out indirectly. However, all workers with HIV are protected under the Americans with Disabilities Act. As long as they can complete their job duties, employers may not discriminate against them (8).
Finally, and of particular importance for healthcare professionals, is navigating the stigma or negative stereotypes that often accompany an HIV diagnosis. There are some societal misconceptions that HIV infections only occur as a result of immoral or taboo behavior or that those infected should be treated differently or avoided. People with HIV may have internalized these harmful stereotypes and feel a sense of shame around their diagnosis. It is important for healthcare professionals to understand that these stereotypes are untrue and harmful, but to provide non–judgemental and compassion that preserves dignity and views the patient as more than their diagnosis.

Self-Quiz
Ask Yourself...
- Why do you think there are laws in place requiring people to disclose their HIV status to potential sexual partners?
- Can you think of any other illnesses where your disclosure is as important as with this disease? Why or why not?
- Why is reporting data about new HIV infections to the CDC important?
- Think about your own internalized thoughts on HIV. Do you have any stereotypes or other negative views that might subconsciously affect your ability to provide non-judgmental care?
Conclusion
Professionals in any healthcare setting may encounter patients with HIV or AIDS. A basic understanding of this disease’s many considerations is fundamental to ensure that quality and compassionate care is being provided. Understanding the disease, treatments, and the unique struggles of these patients can significantly impact their healthcare experiences and promote quality of life.
PrEP: HIV Prevention and Education
Introduction
To understand how Pre-exposure prophylaxis (PrEP) works in preventing Human Immunodeficiency Virus (HIV), it is important that we have some background information on HIV and how it affects the human body. HIV is a virus that attacks the human immune system, making it susceptible to opportunistic infections.
There are two classifications of HIV, and these are HIV -1, which is the most commonly diagnosed infection globally; and HIV-2, which is rare and predominantly occurs in West Africa. If left untreated, HIV can lead to what is known as acquired immunodeficiency syndrome (AIDS) [4][6].
It is crucial for nurses to understand what PrEP is, types of PrEP, indications for use, and patient education topics to advocate for patients at high risk.
Statistical Evidence
Despite advances in medicine, HIV continues to be a persistent public health concern in the United States (US) and worldwide, therefore is still considered an epidemic. As of 2022, there are 39 million people living with HIV globally [7]. According to the World Health Organization (WHO), HIV has claimed over 40 million lives worldwide [12]. In the US, there are approximately 1.2 million people who are currently living with HIV. Of those, 13% do not know that they carry the virus [1] [3].
Furthermore, in 2021, there were an estimated 32,000 new HIV infections in the US. Of those 86% of infections were among all men. From those newly reported HIV infections, the highest subpopulation was among gay, bisexual, and male-to-male sexual contacts who accounted for 22, 400 (70%), followed by 7,100 heterosexual infections (22%) and 2, 500 (8%) infections among drug users [3][9].
Studies have shown that HIV has a disproportionate impact on racial and ethnic minorities. As of 2021, the most affected racial and ethnic group are the black/African Americans who accounted for 40% (14, 383), followed by the Hispanic/Latinos who accounted for 29% [3].
Geographic location and identity also play a role in the rate of HIV infections. The regions that are most affected are the metropolitan cities with over 500, 000 or more people and the southern part of the US has the highest number of people living with HIV [9].
There is no cure for HIV-AIDS, but recent estimates indicate that the rate of HIV infections has reduced by 12% from 2017 to 2021 because of the use of Pre-exposure prophylaxis (PrEP) drugs [3].
Risk Factors and Causes
HIV can occur in three stages in the human body, which are acute HIV infection, chronic HIV infection, and AIDS (late stage).
During the acute HIV stage, most people develop flu-like symptoms which last between 2 - 4 weeks. It is during this stage that the HIV virus levels are high in the blood [9]. As a result, this causes the HIV virus to spread rapidly in the body and intrudes into the immune system by attacking the CD4 T lymphocytes (CD4 cells). The CD4 cells are the white blood cells that help the body fight infections [6].
The late stage is when the HIV infection is most severe because the body can no longer fight opportunistic infections due to a weakened immune system and an increase in viral load. Therefore, the acute and last HIV phase increases one’s risk of contracting the virus due to increased levels in the blood [6]. Also, a recent diagnosis with a sexually transmitted infection (STI) in the past 6 months is a risk factor of acquiring HIV [1].
The two most common ways in which HIV is spread are through unprotected sex (anal or vaginal) and sharing of needles by use of illicit drugs. HIV can be found in the bloodstream, saliva, vaginal fluid, and breast milk of those who are infected [13]. Risk factors can be attributed to substance use and engagement in unsafe behaviors from having sexual intercourse with a partner that is infected with HIV. Also, alcohol and drug use can hinder people from having protected sex [13].
Other risk factors include perinatal infections (mother-to-child transmission) and sexually transmitted diseases (STIs), blood transfusions, transplant tissue, and accidental needle sticks [13].
Prevention Strategies
Ending the HIV epidemic in the U.S (EHE) is a collaborative initiative amongst several federal agencies and organizations whose goal is to reduce the rate of HIV infections to 75% by 2025, and 90% by 2023 (CDC, 2023) [2]. One of the main strategies is through the implementation of PrEP drugs. PrEP has been proven to reduce HIV infections by 99% from sex and 74% from injection transmission when combined with sex education, linkage to care, and evidence-based practice interventions (LGBQT and POC empowerment) [6].
Treatments
HIV is usually treated using highly active antiretroviral drugs (HAART), a potent combination of antiretroviral drugs. HAART assists by slowing the progression of the virus [5]. Pharmacotherapy for HIV/AIDS-related illnesses has led to new drug discoveries such as Pre-exposure prophylaxis (PrEP), that are currently being used to combat the HIV/AIDS epidemic.

Self Quiz
Ask yourself...
- Which subpopulation is known to have the highest rates of HIV infections from recently reported estimated numbers?
- What is a contributing factor that has led to the decrease in the number of HIV infections?
- What are the two HIV stages that pose higher risks for transmission of HIV?
- Name the two most common ways in which HIV is transmitted.
(8)
What is Pre-exposure Prophylaxis (PREP)?
PrEP is a prescribed medication that is recommended to prevent the transmission of HIV in anyone who is at risk of acquiring the HIV infection when exposed [6].
It is worth noting that PrEP prevents the transmission of HIV but not STIs or other viruses. Currently, there is no cure for HIV. However, studies have shown the use of PrEP along with improved testing and treatment is effective in reducing HIV when used as prescribed [6].
Also, clinical guidelines support the use of PrEP when incorporated as part of a comprehensive prevention program which should include safe sexual practices and adherence to treatment. Emphasis must be placed on those using PrEP on adherence to therapy [5].
Types of PrEP Medications
There are three types of PrEP medications that are currently approved for use by the Food and Drug Administration (FDA): Truvada®: Emtricitabine/tenofovir disoproxil fumarate (F/TDF) Descovy®: Emtricitabine/tenofovir and aladenamide (F/TAF) and Apretude®: (Carbotegrovir) long-acting injection (HIV) [10] [11] [12].
Indications of Use for PrEP
- F/TDF and Carbotegrovir are indicated to reduce the transmission of HIV-1 infections in at-risk adults and adolescents who weigh at least 35kgs (77lbs) [1] [5].
- F/TAF is indicated to reduce the transmission of HIV-1 infections in at-risk adults and adolescents who weigh at least 35kgs (77lbs), except for transgender women who were assigned male sex at birth [5].
- One must be HIV - 1 negative prior to starting PrEP [1] [5].
Oral medications
Truvada® (F/TDF) and Descovy® (F/TAF) are fixed-dose oral combination drugs. Although the two medications have some similarities, it is important to differentiate what they are [11] [12].
F/TDF was the first FDA-approved PrEP drug and is the most prescribed drug. Both F/TDF and F/TAF medications are available in pill form and must be taken once daily with or without food.
The kidneys excrete F/TDF and, therefore can cause damage in those with renal impairment which is also linked to loss of bone mineral density. This makes F/TDF more favorable in patients who have osteoporosis and renal impairment.
F/TDF was found to be safe for use in pregnant women [11] [12].
Common side effects – Include fatigue, headache, nausea, and abdominal discomfort also known as ‘Start up Syndrome” which usually lasts for the first month of taking the medication. Increased weight gain and Low-Density Lipoprotein (LDL) seen in F/TAF compared to F/TDF.
Severe side-effects - Clinicians must monitor for the development of the following potential severe or life-threatening effects:
- Lactic acidosis: Not easily identifiable. Signs to look out for include weakness or tiredness, unusual muscle pain, difficulty breathing, stomach pain, nausea, and vomiting.
- Immune reconstitution: flare-up of infections such as tuberculosis or autoimmune disorders and autoimmune Hepatitis.
- Hepatomegaly with steatosis: jaundice, fever, and pain in right abdominal quadrant.
- Renal impairment and bone problems (susceptible to bone fractures): more at risk with F/TDF.
- FDA black box warnings: Severe Hepatitis B exacerbation.
Injectable PrEP Medication
- Apretude® (Cabotegravir): First FDA-approved long-acting intramuscular injectable PrEP.
- The first two doses need to be administered one month apart.
- Cabotegravir is recommended to be administered in the ventrogluteal or upper outer quadrant of the dorsogluteal muscle.
- Cabotegravir is a good alternative for patients who have trouble taking pills or are concerned about the stigma of taking pills.
Side effects - Include stomach pain, nausea, vomiting, loss of appetite, diarrhea, irritation at injection site, flatus, and tiredness.
Severe Side Effects – Include hepatotoxicity, Depressive disorder, mood swings, insomnia, suicidal ideation, muscle pain, fatigue.

Self Quiz
Ask yourself...
- What is the most important blood test result you would check for before you send a patient to get their initial F/TDF or F/TAF from the pharmacy?
- Patient reports that their urine has been very dark in color since they started taking Truvada® (F/TDF) 3 months ago. What serious side effects would you be concerned about?
- Which PrEP medication would be most likely to cause weight gain and increased LDL in a patient?
- The patient requests that you administer their cabotegravir dose in the deltoid muscle. Which are the preferred sites that you would recommend to the patient?
Mechanism of Action
PrEP helps to stop HIV from acting as a catalyst by helping the body to produce antibodies that can block the enzyme needed by the HIV-1 virus to replicate and spread throughout the body [5].
Contraindications
- Unknown HIV-1 status or HIV-1 positive status [5].
- Acute Hepatitis B and Hepatitis C infections.
- Drug-to-drug interactions.
- Previous hypersensitivity with Cabotegravir.
- F/TDF is contraindicated for transgender women who were assigned male sex at birth [1].
- Oral PrEP: Creatinine clearance (CrCL) < 60/ ml per minute for F/TDF and CrCl < 30ml/min for F/TDF for patients with ESRD who are not receiving dialysis [5].
Clinical recommendations for prescribing PrEP
The following recommendations were issued by the CDC for the prevention of HIV using PrEP [1][5].
- Providers must inform their adult and adolescent clients that are sexually active about PrEP.
- Documented HIV-test results taken within a week of starting PrEP medications and periodically while on the medication. The HIV- 1 test must be confirmed through a blood serum test, approved FDA Point of Care test and antigen-antibody fingerstick test.
- The patient must have no signs or symptoms of acute HIV infection.
Drug-to-drug interactions
- F/TDF affects the absorption of the following antiretrovirals: Didanosine, atazanavir, lopinavir/ritonavir. When used with Nonsteroidal anti-inflammatory (NDAIDS) drugs can cause nephrotoxicity [5][11].
- F/TAF and cabotegravir are both known to interfere with: Anticonvulsants i.e., carbamazepine, oxcarbazepine, phenobarbital, phenytoin, antimycobacterial i.e., Rifampin and rifabutin [9] [10].
- F/TAF is decreased when used with Antiretrovirals: Ritonavir and tipranavir [10]
- Cabotegravir interferes with Methadone by decreasing its levels in the body [5].

Self Quiz
Ask yourself...
- How often are the first two doses of Cabotegravir administered?
- You’re attending to a patient during their 3-month revisit. They report that in the last few days, they have been feeling extremely weak and have increased shortness of breath. What would you be concerned about as their nurse?
- What medication would be suitable for a woman who is at high risk for HIV infection and is currently expecting a child?
- Which type of PrEP medication would be suitable for a patient who reports that they’ll have a hard time remembering to take pills?
Required Testing and Monitoring
- Per CDC PrEP guidelines, it is required that health providers have documented HIV negative test results taken within a week prior to initiating PrEP. Thereafter, it is recommended that an HIV test is done every three months while on oral PrEP therapy and every two months for those prescribed the injection [5][9].
- Testing of STI’s i.e., syphilis, gonorrhea & chlamydia prior to initiating PrEP.
- Assess for kidney function i.e., creatinine every six months for those aged 50 or > and with creatinine clearance of < 60ml/min [5].
- Hepatitis B serology testing screening prior to and whilst on F/TDF or F/TD.
- Assess for symptoms of acute HIV infections.
- Monitor lipid profile for patients on F/TAF
- Monitor liver enzymes: indication for acute or chronic viral hepatitis infection [1] [5].
Effectiveness
PrEP is safe and highly effective when taken consistently with a prescribed regimen. PrEP is effective in preventing HIV infections from sex by 99% and 74% among drug users. No reports on significant health effects in those who have taken PrEP for up to 5 years and are HIV negative [6].

Common misconceptions
Two main misconceptions: PrEP is only used in gay men and the use of PrEP encourages risky sexual behaviors [5].

Self Quiz
Ask yourself...
- Which health history reported by a patient would be the most concerning for a patient getting ready to be prescribed Cabotegravir? i.e., psychiatric condition.
- List 3 classes of medications that may affect how PrEP is absorbed in the body?
- List 4 contraindications for PrEP medications.
- What medication should be avoided in transgender women who were not assigned male sex at birth?
Patient Education:
Comprehensive prevention strategies such as counseling, safer sex practices and adherence to medication must be incorporated with the use of PrEP.
- HIV transmission education should be reviewed with patients regularly and must include assessment of high-risk behaviors and appropriate interventions such as regular testing of HIV-1 status.
- Encourage patients to disclose HIV status to sex and needle-sharing partners. Also, they should know their partner's HIV status.
- Educate patients on how to monitor for signs and symptoms of hypersensitivity i.e., muscle pain and fatigue.
- Encourage regular follow-up visits every 3 months.
- Educate patients to recognize and report the important symptoms: change in condition. Instruct patients not to stop taking the medication without consulting their provider.
- Instruct patients to take the medication as scheduled.
- Instruct patients to medication in its original container /blister pack.
- Educate patients that PrEP does not prevent the spread of STIs.
- If patients on dialysis teach them to take medication after dialysis treatment.

Self Quiz
Ask yourself...
- What are some of the components you would include when providing patient education on PrEP? Include at least 5 or more topics you would discuss. \
- How often must/ the HIV test be performed on a patient taking F/TDF or F/TAF?
- What are the two most common misconceptions about PrEP?
Core drug knowledge
- PrEP has proven to be safe and effective in preventing transmission of HIV-1 infections and has become part of the
- F/TAF is not recommended in transgender women or individuals at risk with receptive vaginal sex.
- Adherence to PrEP regimen is the most important factor in maintaining efficacy.
- Risk assessment and baseline labs must be obtained prior to initiating PrEP.
- Renal function should be monitored every 6 to 12 months in patients taking F/TDF or F/TAF based on age and CrCl levels.
- PrEP medications should not be stopped without a patient consulting provider. This should include a repeat HIV test and documentation for discontinuing medication [5].

Self Quiz
Ask yourself...
- What is the most important factor needed to maintain efficacy whilst taking PrEP?
Cost-Reducing Programs:
- The Affordable Care Act allows for all insurance health plans to provide PrEP for free.
- A program known as Ready, Set, PrEP provides free PrEP medications to those who qualify.
- Drug manufacturing assistant programs such as ViiVconnect aids with PrEP injections for those who qualify.
Conclusion
PrEP has become part of a worldwide comprehensive program that is aimed at eliminating the HIV epidemic. The benefits of PrEP can be achieved through identifying those at risk for acquiring HIV, counseling on medication adherence, encouraging safer sex practices and through regular testing and monitoring for HIV using the recommended guidelines.
Risk Management in Nursing
Introduction
Risk management involves the methodical identification, assessment, and evaluation of risks [1]. In healthcare, risk management involves the strategies and actions used to identify, reduce, and prevent hazards within healthcare settings [2]. The necessity of risk management stems from the frequent risks encountered by patients, staff, and the organizations themselves. Establishing a comprehensive risk management plan is vital, as it identifies potential risks and outlines measures to address and minimize them. Risk identification is essential for enhancing patient safety, preserving an organization's reputation, achieving accreditation, securing reimbursements, and becoming a preferred provider [3].
Risk, defined as any factor that could lead to unexpected outcomes or losses, is inherent in all industries. Risk encompasses a range of issues from equipment failures to workplace hazards and medical errors. It may not be possible to eliminate all risks in healthcare, but the management of risk is a critical component of patient safety. Healthcare risk management focuses on evaluating and improving organizational processes to identify existing risks and develop strategies to manage and prevent them, aiming to reduce patient harm and financial losses [2].
The inevitability of risk and uncertainty in nursing, due to human factors, increased complexity of care, and the intricate healthcare system, demands effective risk management tools. The drive for risk management intensified following the 1997 Institute of Medicine (IOM) report, which highlighted the alarming number of deaths due to medical errors, prompting a shift from a culture of blame to one emphasizing safety, system improvement, and trust [4].
Risk management practices in healthcare are a response to the Institute of Medicine’s (IOM's) “To Err is Human: Building a Safer Health System” report, leading to the implementation of the Patient Safety and Quality Improvement Act of 2005 [3]. This act focuses on enhancing patient safety through confidential reporting of adverse events, leading to a collective effort to prevent medical errors and improve safety. Legal experts have outlined the act's key aspects, including the establishment of Patient Safety Organizations, the creation of a patient safety database, and support for state-level error reporting systems, aiming to foster a safer healthcare environment through better error reporting and prevention strategies.
From the onset, risk management focused on utilizing insurance as a protective measure for individuals and corporations against accident-related losses. At its core, risk management theory evolves from three primary concepts: utility, regression, and diversification [5].

Self Quiz
Ask yourself...
- Regarding the inevitability of risk in healthcare, how do you reconcile the goal of maximizing patient safety with the understanding that the elimination of all risks is not possible?
- In light of the Institute of Medicine's report and the subsequent shift from a culture of blame to one emphasizing safety and trust, how might healthcare professionals change their approach to reporting and addressing medical errors?
- Considering the foundational concepts of risk management (utility, regression, and diversification), how can we apply these principles in a healthcare setting to improve patient outcomes and organizational resilience?
Overview of Risk Management
The process of Risk Management involves a systematic approach to identifying, assessing, and mitigating potential risks that could lead to adverse outcomes for patients, staff, and the institution as a whole. The evolution of risk management, from its initial focus on using insurance as a means of protection against losses to its current comprehensive framework, underscores the critical role of risk management in the healthcare sector. This framework now addresses the unique challenges and priorities of healthcare delivery.
The Institute of Medicine's (IOM) 1997 report, which shed light on the alarming rates of medical error, introduced more structured and intensive risk management practices in healthcare [4]. This report led to a paradigm shift from a blame-centric culture to one prioritizing safety, system improvement, and trust. Additional legislative acts, including the Patient Safety and Quality Improvement Act of 2005, further reinforced the commitment to enhancing patient safety through confidential reporting and initiative-taking prevention of medical errors [3].
As the complexity of nursing and healthcare evolves, the role of risk management and nursing expands, focusing on creating resilient systems and processes that mitigate risks but also promote a culture of safety and continuous improvement. This evolution highlights the transition of healthcare risk management from a reactive to an initiative-taking discipline, emphasizing the strategic management of risks to improve patient care and organizational sustainability.
Evolution of Risk Management
Daniel Bernoulli introduced the utility method in 1738, emphasizing a decision-making approach that prioritizes the magnitude of the outcomes' effects, guiding individuals to weigh the impact of various results [5].
The evolution of risk management principles into healthcare risk management illustrates the adaptation of foundational economic and financial theories to address the unique challenges and priorities of the healthcare sector. The core principles of utility, regression, and diversification, rooted in financial decision-making, focus on patient safety, quality care, and organizational sustainability in healthcare [6].
Utilitarian principles in healthcare risk management emphasize the decision-making process based on the magnitude of outcomes' effects, which is central to healthcare risk management [7]. In this context, utility maximizes patient outcomes and minimizes harm [7]. Healthcare providers assess the benefits and risks of treatments, procedures, and care paths, aiming for the greatest good for the patient. Practical decisions about resource allocation, treatment options, and even end-of-life care prioritize the patient's welfare and the utility of health outcomes [8].
Regression in healthcare risk management is a statistical machine learning tool for identifying the relationships between variables, predicting patient outcomes, understanding risk factors, and improving the quality of care [9]. By analyzing historical data on patient outcomes, healthcare providers can identify trends, risks, and potential interventions. This aids in developing preventive measures, improving patient care protocols, and managing the risks associated with different patient demographics, conditions, or treatments.
Diversification in Healthcare Risk Management is a strategy to reduce risk by allocating investments across various financial instruments, industries, and other categories [10]. In healthcare, diversification translates into a broad strategy that includes expanding treatment options, healthcare services, and even investment in research and development. It means having a variety of tools, approaches, and strategies to manage health risks, prevent disease, and treat patients. Diversification also involves spreading operational risks by having multiple suppliers, a mix of income sources, and a variety of service lines to mitigate the impact of any single failure or external threat [10][11].
Over time, healthcare risk management has grown to encompass comprehensive frameworks that include these foundational principles but also regulatory compliance, ethical considerations, and the integration of technology. It focuses on creating systems and processes to identify, assess, and mitigate risks to patients, staff, and organizations. This evolution reflects the increasing complexity of healthcare delivery, the high stakes of patient safety, and the need for an organized approach to managing the inherent uncertainties and risks of providing care.

Self Quiz
Ask yourself...
- How do the principles of utility, as introduced by Daniel Bernoulli, apply to modern healthcare decisions when considering the ethical implications of prioritizing treatments or interventions for patients?
- Considering the role of regression analysis in healthcare risk management, how can healthcare organizations leverage statistical machine-learning tools to predict patient outcomes and tailor interventions?
- What are the obstacles and benefits encountered by healthcare organizations when adopting a varied approach to health risk management, and in what ways does this strategy enhance the resilience of healthcare systems?
Medical Malpractice Case Study: Nurse Practitioner Oversight
Case Overview:
A 52-year-old Hispanic male presented to the local clinic with symptoms of rectal bleeding and discomfort. He sought medical attention from a nurse practitioner. Over several months, the patient continued to experience symptoms without any new or escalated efforts to diagnose his condition.
At the six-month mark, and a significant delay in diagnosing and referring the patient for further gastrological (GI) assessment, the patient received a diagnosis of colon adenocarcinoma. The lack of action, poor documentation, and follow-up resulted in the cancer advancing to a metastatic stage. The patient passed away from metastatic colon cancer one year after his initial clinic presentation.
Patient Background:
The patient's history included depression, anxiety, substance use, hypertension, and a family history of colon cancer and heart disease. Even though the physical examination and the preliminary diagnosis indicated internal hemorrhoids, the patient was reluctant to proceed with the critical step of a colonoscopy or colon cancer screening.
Clinical Encounters:
Over 6 months, the patient had multiple visits to the clinic for various issues including continued rectal bleeding and pain. The nurse practitioner did not revisit the discussion about a colonoscopy for a more definitive diagnosis and limited documentation existed in the EMR. After significant insistence by the patients, a colonoscopy conducted by a gastroenterologist revealed a significant tumor, leading to a late-stage cancer diagnosis.
Legal and Risk Management Findings:
The failure to address continued patient complaints was a significant oversight. The nurse practitioner cited time constraints, frequent presentations, and the patient’s underlying anxiety as reasons for the lack of further testing. The Nurse Practitioner omitted the patient's expressed discomfort with discussing his symptoms with a female practitioner and the prevailing language barrier.
Resolution:
After presentation, expert opinions condemned the nurse practitioner's follow-through and documentation, mediation settled and awarded the defendant over $740,000.
Risk Management Recommendations:
In the unfortunate case of a 52-year-old Hispanic male who succumbed to metastatic colon cancer, fundamental lessons emerge, underscoring the importance of diligent patient follow-up, competent cultural care, and rigorous diagnostic protocols. This case illustrates a series of systemic failures that commenced with an initial underestimation of severe symptoms and culminated in a delayed cancer diagnosis.
Despite presenting with rectal bleeding and discomfort—symptoms warranting direct and thorough investigation—there were no further diagnostic steps taken. Over six months, despite repeated clinic visits, the patient's escalation did not receive an appropriate response, resulting in a significant oversight of colon adenocarcinoma progression to a metastatic stage.
To prevent such outcomes, it is imperative to implement robust risk management strategies focused on these actions:
- Adhere to the scope and standard of care, ensuring safe and appropriate management of clinical symptoms.
- Obtain and document patient and family medical histories.
- Document all patient discussions, consultations, clinical information, and actions, including treatment orders and patient noncompliance.
- Use written communication to inform patients of the risks of noncompliance with treatment recommendations.
This risk management case underscores the critical importance of comprehensive documentation, patient communication, and adherence to screening recommendations in preventing adverse outcomes.


Self Quiz
Ask yourself...
- How might healthcare providers balance the respect for patient autonomy with the imperative to take decisive action when a patient hesitates to undergo recommended diagnostic procedures, as seen in the case where the patient's hesitancy led to a delayed cancer diagnosis?
- In what ways can healthcare systems improve to ensure that cultural sensitivity and language barriers do not impede patient care and communication, as illustrated by the patient's discomfort with discussing symptoms with a female practitioner and potential language barriers?
- Considering the missed opportunities for early diagnosis in this case, are there systemic changes that can enhance documentation and follow-up processes for symptoms that may indicate serious conditions like cancer?
The Five Basic Techniques for Handling Risk
Handling risk within healthcare is an essential aspect of maintaining patient safety, protecting healthcare resources, and ensuring continuity of care.
The five methods of handling risk— Control, Avoidance, Retention, Non-Insurance Transfer, and Buying Insurance—have unique applications in healthcare [30].
Control: In healthcare, controlling risks often involves implementing safety protocols, rigorous hygiene practices, and safety measures to prevent accidents and infections [30] [31]. For example, hospitals use hand hygiene protocols and personal protective equipment (PPE) to reduce the risk of hospital-acquired infections (HAIs) [31]. Regular maintenance of medical equipment and facilities helps mitigate risks related to equipment failure or environmental hazards.
Avoidance: Avoidance in healthcare may involve not engaging in high-risk procedures or treatments without adequate preparation or safeguards [18]. For example, a healthcare provider may defer high-risk services if they lack the necessary expertise.
Retention: In the healthcare context, retention might involve facilities choosing to bear certain risks themselves, such as opting to self-insure for specific types of losses or legal claims [32] [33]. Retention requires careful assessment to ensure the organization can cover potential losses without jeopardizing financial stability or patient care standards.
Non-Insurance Transfer: Healthcare organizations often use non-insurance transfers by shifting certain risks to other parties through contracts. For example, a hospital might have contracts with its suppliers that include provisions requiring the supplier to assume responsibility for any defects in the medical supplies or equipment provided [33].
Buying Insurance: Insurance is a critical component of risk management in healthcare [34]. Facilities purchase insurance coverage, including malpractice insurance, general liability insurance, property insurance, and cyber liability insurance.

Self Quiz
Ask yourself...
- How can healthcare facilities balance the use of control measures including safety protocols and hygiene practices, with the need to provide comprehensive care, when such measures may restrict certain treatments or procedures?
- In what ways might the strategy of risk avoidance impact the innovation and adoption of new medical treatments or technologies in healthcare settings?
- Considering the option of retention in healthcare risk management, how can organizations determine the appropriate level of risk to retain without compromising their financial stability or the quality of patient care?
- How do healthcare organizations navigate the complexities of non-insurance transfer agreements to ensure they mitigate risk without displacing responsibility in a way that could impact patient care?
The Value of Risk Management in Nursing
Deployment of healthcare risk management has focused on the key role of patient safety and the reduction of medical errors that jeopardize an organization’s ability to achieve its mission and protect against financial liability. However, with the expanding role of healthcare technologies, increased cybersecurity concerns, the fast pace of medical science, and the industry’s ever-changing regulatory, legal, political, and reimbursement climate, healthcare risk management has become more complex over time.
With the value-based care movement and today’s risk-bearing models such as bundled payments and CMS’s pay-for-performance programs, financial risk is shifting from payers to providers and requires a broader view of risk management [35]. Hospitals are expanding their risk management programs from reactive initiatives that promote patient safety and prevent legal exposure, to programs that are proactive and view risk through the much broader lens of the entire healthcare ecosystem.
The holistic approach, Enterprise Risk Management (ERM), includes traditional aspects of risk management (patient safety and medical liability) and expands them with a “big picture” approach to risk across the organization [36].


Self Quiz
Ask yourself...
- How does the shift towards value-based care and risk-bearing models influence the strategic priorities of healthcare organizations in terms of risk management considering the balance between financial risk and patient safety?
- Considering the holistic approach of Enterprise Risk Management (ERM), how can healthcare organizations integrate traditional risk management practices with the broader view required to address the complexities of modern healthcare, including technology and cybersecurity concerns?
The Eight Domains of Enterprise Risk Management (ERM)
Enterprise Risk Management (ERM) holds critical importance in the healthcare sector, covering a spectrum that includes everything from patient care to the broader aspects of operational and strategic oversight. The American Society for Healthcare Risk Management (ASHRM) defines ERM in healthcare as a comprehensive approach to decision-making that enhances value preservation and creation by adeptly managing risks and uncertainties, along with their impact on overall value [36].
ERM emphasizes leveraging technology to streamline risk management processes throughout the organization, thereby eliminating the risks that come from isolated departments or units [36]. Through the integration of data analytics, ERM supports informed decision-making, fosters unity among departments, prioritizes risks, and efficiently allocates resources. Analytics play a pivotal role in tracking performance indicators, demonstrating the financial benefits (cost savings) of ERM efforts.
Implementing ERM in healthcare involves a comprehensive approach to managing these risks across eight domains:
Operational Risks involve the day-to-day functions necessary for healthcare organizations to operate [3]. This includes risks associated with supply chain management (e.g., availability of medications and medical supplies), facility management, and internal processes that could impact patient care delivery. Managing these risks involves optimizing operational processes, ensuring redundancy in critical services, and developing contingency plans for operational disruptions.
Clinical & Patient Safety Risks are related to the provision of care. This domain focuses on risks that could result in harm to patients, including medical errors, healthcare-associated infections, and patient falls [37]. Effective ERM strategies in this area involve implementing evidence-based practices, enhancing patient safety culture through training and education, engaging in continuous quality improvement initiatives, and using data analytics to identify and mitigate potential safety issues.
Strategic Risks involve external and internal factors that could affect the organization's ability to achieve its goals. This includes changes in healthcare policy, shifts in market dynamics, competitor actions, and the ability to adapt to changing patient needs [38]. Healthcare organizations address these risks by developing flexible strategic plans, conducting regular market and policy analyses, and engaging in strategic partnerships and collaborations [38].
Financial Risks in healthcare encompass fluctuations in revenue due to changes in payer mix or reimbursement rates, increasing costs of care delivery, and investments in infrastructure or technology that may not yield expected returns [15]. Financial risk management strategies include thorough financial planning and analysis, diversifying revenue streams, implementing cost control measures, and investing carefully in growth opportunities.
Human Capital Risks relate to the management of healthcare personnel, including recruitment, retention, training, and development of staff [17]. Strategies for managing these risks include developing robust workforce planning, fostering a positive organizational culture, investing in staff development, and implementing programs to enhance employee satisfaction and reduce turnover [17].
Legal & Regulatory Risks involve compliance with a complex array of healthcare laws and regulations, including patient privacy laws, licensing requirements, and accreditation standards [13]. Non-compliance can result in significant legal penalties, loss of accreditation, and damage to reputation. Healthcare organizations manage these risks by maintaining robust compliance programs, conducting regular audits and risk assessments, and engaging in ongoing staff education on legal and regulatory obligations [13].
Technological Risks encompass issues related to the adoption, implementation, and use of healthcare information technology (IT), cybersecurity threats, and the reliability of medical equipment [29]. Comprehensive IT security measures, regular technology assessments and upgrades, and appropriate training and support for users of healthcare technologies address these risks [29].
Environmental and Infrastructure Based Hazards include risks from natural disasters, facility-related issues (e.g., fire, water damage), and environmental health risks (e.g., poor air quality) [39]. Managing these risks involves comprehensive emergency preparedness planning, investing in infrastructure resilience, and implementing environmental health and safety programs [39].
In each of these domains, healthcare organizations use a variety of tools and strategies to identify, assess, mitigate, and monitor risks. By integrating ERM into their organizational culture, healthcare providers can navigate the complexities of the healthcare environment but also improve patient outcomes, enhance operational efficiency, and achieve strategic objectives.

Self Quiz
Ask yourself...
- How can healthcare organizations integrate data analytics into their Enterprise Risk Management (ERM) strategies to enhance decision-making and identify emerging risks across the eight domains?
- In the context of ERM, how do healthcare organizations navigate the balance between implementing robust cybersecurity measures and ensuring the seamless use of healthcare IT systems by staff without compromising patient care?
- Considering the wide range of risks covered by the eight domains of ERM, how can healthcare leaders prioritize addressing risks with limited resources?
- How do changes in healthcare policy and the legal landscape influence the strategic and operational decisions made by healthcare organizations under the ERM framework?
Why Is Risk Management Important to Clinical Nursing Practice?
The healthcare system operates with a collection of individual contributors who ensure patient care and safety through collective efforts. When medical errors occur, it is the responsibility of the healthcare institution to address, learn from, and prevent future incidents [18]. This approach emphasizes modifications in systemic policies over scrutinizing individual actions for improvement.
For example, imagine an emergency department that categorizes patients' urgency levels using color-coded wristbands during periods of excessive overflow. A red wristband indicates a need for immediate attention, while a white one suggests less urgency.
Consider a scenario where a 65-year-old attending a crowded real estate conference downtown—marked by a purple wristband for event identification—experiences severe chest pain and rushes to a nearby hospital. He arrives at the hospital on a busy Friday. After triage, the nurse places the patient on a hallway stretcher and portable monitor. At some point during his stay, the patient develops a significant arrhythmia. Observing the purple wristband, the hallway nurse assumes the wristband signifies a Do Not Resuscitate (DNR) order. Before attending to the patient, she accesses the patient's EMR to find emergency contact information to update the family on the patient’s declining status. During the delay to update the family, the patient expires.
This hypothetical error underscores the important opportunity for systemic improvements in healthcare. What if part of the emergency department's intake process included verifying any existing wristbands or bracelets to prevent such confusion? While medical errors can occur, implementing redundant, system-wide safety protocols can help mitigate errors.
The issue of medical errors has been significant since the U.S. Institute of Medicine's landmark report in 1999, which estimated that preventable medical errors result in the deaths of between 44,000 and 98,000 patients per year [40]. Despite efforts to quantify these errors and their impact, accurate data remains elusive due to underreporting and the voluntary nature of reporting to oversight bodies like the Joint Commission [40].

Self Quiz
Ask yourself...
- How can nursing practices evolve to prioritize system-wide safety protocols without diminishing the value of individual accountability in clinical settings?
- Considering the substantial number of deaths attributed to preventable medical errors, what strategies can be employed by clinical nursing staff to improve the accuracy and willingness to report incidents, thereby contributing to a culture of safety and continuous improvement?
Key Components of Performing Risk Management in Nursing
In healthcare, managing risk is analogous to navigating a shifting landscape. By leveraging data, tapping into both institutional and industry-wide knowledge, and fostering active engagement among all stakeholders—including patients, employees, administrators, and payers—healthcare risk managers can begin to unearth and address threats and compensatory events that might otherwise remain hidden.
Risk management has moved towards the quantification and prioritization of these identified risks [3]. This involves a meticulous process of scoring, ranking, and prioritizing each risk based on the probability and impact of the occurrence. This structured approach facilitates the effective allocation of resources and the assignment of responsibilities but also employs tools like risk matrices and heat maps to aid in the visualization of risks.
The pathway of risk management further extends into the realms of investigating and reporting sentinel events, ensuring compliance, capturing learnings from near misses and good catches, diving deep to uncover latent failures, applying proven analysis models for thorough investigation, optimizing risk management information systems, and finding the optimal balance in risk financing, transfer, and retention.
Each of these steps embodies a critical component of a holistic Enterprise Risk Management strategy in healthcare, aimed at not just mitigating risk but also enhancing overall organizational resilience and patient safety.

Self Quiz
Ask yourself...
- How can the integration of data analytics and institutional knowledge enhance the identification and prioritization of risks in nursing practice and transform patient care outcomes?
- Considering the role of sentinel event investigation in risk management, how can nursing professionals contribute to a culture that supports learning from these events without fostering a blame-oriented environment?
Identifying Risks
By leveraging data analytics, drawing upon both institutional and industry-wide expertise, and involving stakeholders at all levels—from patients and employees to administrators and insurers—healthcare risk managers can detect potential threats and opportunities for mitigation that might otherwise go unnoticed.
Quantifying and Prioritizing Risks
The process of identifying risks, assessing, scoring, and prioritizing risks based on their probability and potential impact is fundamental [1]. This process involves utilizing tools such as risk matrices and heat maps to organize risks, thereby facilitating better communication and collaborative decision-making regarding where to direct resources and efforts.
Investigating and Reporting Sentinel Events
Defined by the Joint Commission as unexpected occurrences resulting in death or significant harm not attributable to the natural progression of a patient's condition, sentinel events necessitate immediate and comprehensive investigation [27]. Establishing a protocol for such events fosters a systematic, composed approach to addressing patient safety and reducing future risks, emphasizing the need for a culture of openness and mutual respect between staff and leadership for effective resolution.
Ensuring Compliance Through Reporting
Regulatory bodies at various hospital administration levels require the documentation and reporting of specific incidents, including sentinel events and issues involving medication or medical devices [18]. For example, it is essential for the accurate reporting of incidents including surgical errors or workplace injuries to enhance patient safety.
Learning from Near Misses and Good Catches
In circumstances where a potential error occurs, known as “near misses” or “good catches,” provide valuable insights for preempting risks [41]. Cultivating an environment that encourages the reporting of these incidents can lead to the development of preventive strategies and the reinforcement of best practices.
Exploring Beyond Obvious Errors to Uncover Hidden Failures
While direct errors are apparent, latent failures require deeper analysis to identify. Organizations should consider other factors such as environmental conditions or systemic pressures that contribute to mistakes to understand and address the root causes of adverse events [18].
Applying Rigorous Analysis for Incident Investigation
To dissect complex incidents and uncover underlying issues, healthcare risk management employs various analytical models, including the Failure Mode and Effects Analysis (FMEA) and Root Cause Analysis (RCA) [42][43].
These methodologies facilitate a comprehensive examination of incidents, helping to identify both direct and contributory factors.
Leveraging Technology with Risk Management Information Systems (RMIS)
Advanced RMIS platforms offer a suite of tools for incident documentation, risk tracking, and data analysis [3]. These systems streamline risk management processes and contribute to cost efficiency by automating standard operations and facilitating detailed reporting and comparison.
Balancing Risk Financing, Transfer, and Retention
Effective risk management in healthcare involves strategic financial planning to address potential losses. This includes determining the optimal mix of risk transfer mechanisms, such as insurance, and risk retention strategies, ensuring financial stability in the face of unforeseen events.

Self Quiz
Ask yourself...
- How can healthcare organizations balance the use of data analytics and stakeholder input to identify and address potential risks without overwhelming the decision-making process with too much information?
- In what ways can the prioritization of risks through scoring and ranking improve resource allocation in healthcare settings, and what challenges might arise in achieving consensus on these priorities among different stakeholders?
- Considering the importance of learning from near misses and good catches, how can healthcare institutions develop a culture that encourages the reporting of these incidents and utilizes this information to prevent future errors?
- Given the complexity of healthcare delivery, how can rigorous analytical models like FMEA and RCA be adapted to address the unique challenges of healthcare risk management in terms of uncovering and addressing latent failures?
The Evolution of Risk Management in Healthcare
The American Society for Healthcare Risk Management (ASHRM) defines Enterprise Risk Management (ERM) in healthcare as a holistic framework designed to optimize decision-making through the effective management of risk, uncertainty, and their impact on value [36].
This approach aims to safeguard and enhance the value by ensuring a coherent strategy across the entire healthcare organization, thereby eliminating risks tied to departmental siloes. It leverages technology and embeds data analytics to bolster decision-making, foster unity across departments, prioritize risks effectively, and optimize resource distribution. These analytics play a crucial role in setting benchmarks and demonstrating the financial savings achieved through ERM initiatives, all resting on a governance structure that synchronizes the organization’s operations with its risk management endeavors.
The evolution of healthcare risk management has seen the healthcare risk manager's role expand within this new governance framework, focusing on proactive risk identification, assessment of potential impacts, and the formulation of preemptive action plans [1]. The task of risk managers includes crafting and implementing strategies to limit the fallout from unexpected adverse events.
The revolution of the risk manager reflects the dynamic and complex nature of healthcare risk management, incorporating responsibilities like stakeholder communication, risk documentation and reporting, and the development of processes and policies for managing uncertainty [1]. The healthcare risk landscape is ever-changing, necessitating constant vigilance and adaptation from risk managers.
In the past, healthcare risk management was a reactive field, addressing problems as they occurred, with a focus on patient safety and minimizing medical errors. This approach began to shift in the wake of the medical malpractice crisis of the 1970s. Today's healthcare risk management encompasses a wide array of concerns, from emerging technologies and cybersecurity to the intricacies of regulatory, legal, and reimbursement changes [44]. The transition towards value-based care, including bundled payments and performance-based incentives, illustrates a significant shift of financial risk from payers to providers, urging a more expansive view of risk management [46].
A 2017 report by Moody's Investor Services highlighted the critical link between risk management and a hospital's financial performance, noting that high clinical quality is increasingly vital for financial health and brand integrity as the industry moves away from fee-for-service models towards value-based reimbursement [45]. This evolution signifies a paradigm shift in healthcare organizations' risk management strategies—from reactive measures centered on patient safety and legal compliance to proactive, comprehensive approaches that consider the broader healthcare ecosystem.


Self Quiz
Ask yourself...
- How has the role of technology and data analytics transformed the approach to Enterprise Risk Management (ERM) in healthcare in terms of decision-making and risk prioritization?
- Considering the expanded role of healthcare risk managers in the modern ERM framework, how can these professionals navigate the challenges of integrating proactive risk management strategies across diverse departments within a healthcare organization?
- In light of the shift from a reactive to a proactive approach in healthcare risk management, what are the key factors that have driven this evolution, and how do they impact the day-to-day responsibilities of risk managers?
- Given the significant shift of financial risk from payers to providers as part of the move towards value-based care, how can healthcare organizations adapt their risk management strategies to address this new landscape and maintain financial stability while ensuring high clinical quality?
The Role of the Risk Manager
As the governance structure within healthcare evolves, so has the role of the healthcare risk manager, adapting to oversee and facilitate the Enterprise Risk Management (ERM) framework. Risk managers are at the forefront of identifying potential risks, assessing their impacts and benefits, and crafting preemptive strategies to address them. Risk managers implement and oversee containment strategies to minimize harm and organizational exposure when unexpected challenges arise.
The healthcare risk manager's role is inherently dynamic and multifaceted, reflecting the complex nature of healthcare risk management. Their responsibilities extend across various domains, including effective communication with stakeholders, the meticulous documentation and reporting of risks and adverse events, and the development of robust processes, policies, and procedures tailored to manage risk and uncertainty. Staying abreast of the changing risk landscape in healthcare and necessitating ongoing adaptation and responsiveness requires constant vigilance.
A key aspect of risk management is the cultivation of a preventive mindset not just within the risk management team but throughout the entire healthcare organization [3]. This involves ensuring the training of all personnel, understanding how to implement risk mitigation strategies, and preparing to respond to unforeseen incidents. For instance, it is crucial that a registered nurse can recognize a potential medication contraindication and know the proper channels for reporting such findings to the risk management department.

Self Quiz
Ask yourself...
- How can healthcare risk managers foster a culture of proactive risk management across all levels of a healthcare organization, ensuring that every employee feels responsible for and capable of contributing to the safety and well-being of patients?
- Given the dynamic and ever-changing landscape of healthcare, what approaches can risk managers take to ensure their strategies remain effective and responsive to new challenges in areas like technology adoption and regulatory compliance?
Evaluating Organizational Risk
The development of a risk management strategy requires risk managers and involved stakeholders to foresee and assess all conceivable outcomes that could impact an organization’s patients and staff, alongside devising strategies to address or diminish any emerging concerns [3]. Several fundamental aspects and critical areas of focus underpin the risk management process in healthcare, essential for formulating a comprehensive medical risk management plan.
These aspects include [3]:
- Enhancing patient safety and quality of care
- Compliance with compulsory federal regulations
- Management of potential medical errors
- Navigation of existing and forthcoming legal frameworks
- Elevating care and minimizing risks
- Mitigating financial and compliance-related risks
- Safeguarding data security
For healthcare institutions, it is impractical to anticipate every potential incident. The task of organizations is recognizing the most probable risks and formulating strategies to manage adverse events should they occur.
The process of conducting a risk assessment might encompass inquiries such as:
- What types of adverse incidents could occur?
- What is the likelihood of these scenarios unfolding?
- What would be the consequences should these events materialize?
- How can we minimize the probability of such incidents?
- In cases where prevention is not feasible, what strategies can be employed to mitigate the impact?
- What are the unavoidable consequences should these events transpire?

Self Quiz
Ask yourself...
- How can healthcare organizations balance the need for comprehensive risk management strategies that address a wide range of concerns—from patient safety to data security—without diverting focus and resources away from their primary mission of providing care?
- Given the inevitability of unforeseen events in healthcare, what approaches can be employed to enhance the agility and resilience of healthcare organizations, enabling them to adapt to emerging risks not identified in their risk management plans?
Creating a Healthcare Risk Management Plan
There are at least five necessary components to consider when creating a risk management framework. They include risk identification; risk measurement and assessment; risk mitigation; risk reporting and monitoring; and risk governance [20]. A risk management plan serves as the foundation for identifying, managing, and reducing risks within the organization. It is essential to involve hospital leadership and department heads in the creation and continual reassessment of the risk management strategy.
The design of the risk management plan includes an outline of the mission, scope, and goals of the organization's risk management efforts, specifying the duties and responsibilities of the risk manager and team members dedicated to risk reduction [3]. After their development and thorough testing, these risk management strategies should serve as a cornerstone for the training of physicians and healthcare providers. Leaders should share risk management plans with all team members, review, and update as necessary to guarantee their effectiveness and success in safeguarding patient welfare.
The structure of a Risk Management Plan can differ across organizations, depending on the evaluation of current systems, analysis of historical data, and the distinct nature of each healthcare facility [1].
However, certain key elements are essential in all healthcare risk management plans:
- Education & Training
- The plan should specify the training regimen for employees, covering orientations for new hires, continuous and as-needed training sessions, annual assessments to confirm skills, and training tailored to specific events.
- Patient & Family Grievances
- Procedures should exist for recording and addressing grievances from patients and their families including a process to enhance patient satisfaction and minimize the risk of legal actions. This includes defining response times, designated responsibilities, and prescribed procedures.
- Purpose, Goals, & Metrics
- The plan must articulate the aim and advantages of implementing a risk management strategy. It should set specific objectives for lowering liability claims, sentinel events, near misses, and overall risk-related costs, with a focus on measurable and actionable data reporting.
- Communication Plan
- To foster an open dialogue within the risk management team the plan must outline communication protocols, and follow-up procedures, and ensure reports reach all relevant departments and executive leadership.
- Contingency Plans
- Preparations for managing systemic failures and emergencies, such as EHR system malfunctions, security breaches, cyber-attacks, disease outbreaks, power outages, and acts of terror or mass violence, should be comprehensive and clearly detailed.
- Reporting Protocols
- The organization must adopt an efficient system for logging, categorizing, and monitoring potential risks and incidents, including mandatory reporting mechanisms.
- Response & Mitigation
- Plans should establish collaborative approaches for addressing and managing reported risks and incidents, encompassing immediate action, follow-up, documentation, and strategies to prevent recurrence.

Self Quiz
Ask yourself...
- How can healthcare organizations ensure that their risk assessment processes are comprehensive enough to identify all potential adverse incidents, given the vast and complex nature of healthcare delivery?
- What role does continuous education and training play in strengthening a healthcare organization's risk management plan, and how can leaders tailor to address the specific needs of different departments?
- In developing a healthcare risk management plan, how can hospital leadership engage all stakeholders, including patients and their families, to ensure the plan is responsive to the needs and concerns of those it aims to protect?
- Given the inevitability of unforeseen events, how can healthcare organizations' design contingency plans be flexible and robust enough to manage a wide array of emergencies, from technological failures to natural disasters?
Patient-Specific Risk Management Strategies
As the field of healthcare risk management continues to expand, considering the vast ecosystem of healthcare, the emphasis on enhancing patient safety and minimizing harm remains at the forefront of risk management initiatives [47].
Addressing patient safety involves implementing tailored risk management strategies, which can include actions like:
- Avoiding the dispensation of expired prescriptions
- Ensuring follow-ups on unreported test results
- Monitoring and addressing missed patient appointments.
- Engaging in effective communication with patients
- Implementing measures to prevent falls and promote mobility.
- Maintaining thorough and sufficient patient records


Self Quiz
Ask yourself...
- How can healthcare providers integrate patient-specific risk management strategies into daily clinical practices to address individual patient needs and prevent potential harm?
- What mechanisms can ensure continuous and effective communication between healthcare providers and patients for managing the risks related to unreported test results and missed appointments?
How Incident Reporting Improves Risk Management
For an organization to prevent incidents, it is critical to identify, assess, and manage risks. The healthcare sector benefits from a wealth of information and data sources that illuminate common risks, including those previously discussed. Organizations need to analyze their own incident data to enhance their risk management strategies, offering invaluable insights into prevalent risks and inefficiencies.
Advancements in healthcare risk management technology, including incident reporting software, empower organizations to document hazards, near misses, and adverse events. Analyzing this data facilitates the identification of risk-prone areas, paving the way for the development of strategies aimed at minimizing exposure and reducing potential harm. A direct relationship exists between the implementation of a centralized incident reporting system within a healthcare setting and the overall safety of patients.
Such reporting systems simplify the process for staff to document incidents, ensuring swift communication with the risk management team and providing immediate data that helps pinpoint fundamental problems to prevent recurrence. Therefore, the adoption of an incident reporting system can lead to a reduction in risks, a decrease in costs, and an enhancement in process efficiency [48].

Self Quiz
Ask yourself...
- How can healthcare organizations encourage a culture where staff feel empowered and obligated to report incidents, including near misses, to enhance the effectiveness of risk management strategies?
- Given the potential for incident reporting systems to reduce risks and costs, what barriers might healthcare organizations face in implementing these systems, and how can organizations overcome these barriers to ensure the systems' effectiveness and sustainability?
Sentinel Events
Preventing sentinel events is a collective endeavor that demands the participation of every team member within the healthcare setting, from physicians and nurses to hospital support staff and even patients and their families [49]. Research has highlighted the importance of fostering a culture where everyone, irrespective of their role or seniority, feels empowered to voice concerns about patient safety [49]. This approach ensures the valuation of unique perspectives and insights of each individual involved in patient care, enhancing the ability to detect and prevent sentinel events.
To foster an inclusive environment, it is essential to cultivate a culture of open communication and empowerment right from the start. This means integrating patient safety-focused training from day one of onboarding and consistently reinforcing it throughout an employee's tenure. Hospitals employ various strategies to promote this team-based approach to patient safety, but the core principle revolves around empowering everyone within the healthcare ecosystem to play an active role in maintaining safety.
Understanding what constitutes a sentinel event is critical for effective prevention. As defined by The Joint Commission, a sentinel event is a significant patient safety incident resulting in death, permanent harm, or severe temporary harm [49]. This classification underscores the need for acute awareness and vigilance in everyday medical practices to prevent such outcomes.
The potential triggers for sentinel events include surgical verifications, medication administration, equipment use, infection control, staffing levels, and diagnostic accuracy, among others [49]. These areas highlight the inherent risks present in medical care, as underscored by the seminal report “To Err is Human: Building a Safer Health System” by the US Institute of Medicine in 1999 [40]. This groundbreaking work shifted the focus from individual blame to systemic improvements, acknowledging that mistakes are often the result of flawed systems, not flawed individuals.

Self Quiz
Ask yourself...
- How can healthcare organizations identify and address the systemic flaws that contribute to sentinel events, rather than focusing on individual accountability?
- What role do patients and their families play in the prevention of sentinel events, and how can healthcare providers better engage them in safety protocols and decision-making processes?
- Considering the various potential triggers for sentinel events identified, what specific measures can healthcare organizations implement to mitigate these risks across different areas of care delivery?
Response To a Sentinel Event
Following a sentinel event, a healthcare organization must conduct a thorough investigation into the underlying causes through a root cause analysis (RCA) [25]. The objective of RCA is to devise a corrective action plan aimed at addressing the immediate issue but also at instituting systemic changes to avert similar incidents in the future [25]. This approach shifts the focus from individual mistakes to the broader system or policy failures that may have facilitated the event.
Root cause analysis is valuable for examining patterns across multiple lower-risk incidents [25]. For instance, a study in Denmark involving 40 community pharmacies used root cause analysis to explore over 400 medical errors, pinpointing primary causes such as illegible prescriptions, confusing medication packaging, and distractions leading to a lack of concentration [50].
Since 1997, the Joint Commission has offered resources to help accredited organizations formulate sentinel event policies and conduct root cause analyses [3]. This involves addressing three core questions: What happened? Why did it happen? What are the latent conditions?
Latent conditions refer to the systemic aspects that can either precipitate or prevent errors and sentinel events, encompassing areas like provider familiarity, procedural risks, medical product complexity, environmental factors, patient interactions, and policy adequacy [51].
In response to feedback on the implementation challenges of RCA outcomes, the National Patient Safety Foundation revised the definition of RCA to emphasize action in preventing patient harm [52]. Recommendations include assembling a diverse team after recognizing the need for an RCA and ensuring the interviewing of those involved to prioritize impactful outcomes [52].
The development of a detailed corrective action plan should follow the conducting of an RCA and identifying the factors that contributed to the sentinel event. An effective plan, as outlined by the Joint Commission, should specify corrective actions to address identified system vulnerabilities, assign implementation responsibilities, set timelines, and outline methods to assess and sustain the improvements made [52]. The Joint Commission reviews these plans, which also evaluates the effectiveness of the actions taken and the potential impact on the organization's accreditation.

Self Quiz
Ask yourself...
- How can a healthcare organization ensure that the implementation of a corrective action plan developed after a root cause analysis (RCA) of a sentinel event is effective in preventing future incidents?
- In what ways can the involvement of a diverse team from different departments and disciplines in the RCA process contribute to more comprehensive and effective solutions for preventing sentinel events?
- Considering the potential impact of latent conditions on the occurrence of sentinel events, how can healthcare organizations identify and address these conditions before they contribute to adverse incidents?
- What role does continuous feedback and evaluation play in the success of a corrective action plan following a sentinel event, and how can organizations integrate lessons learned into their risk management practices?
Patient Handoff
Numerous hospitals have implemented standardized protocols for handoffs between healthcare providers, a critical juncture known for its significant risk of contributing to medical errors and compromising patient safety. A prime example of such a standardized protocol is the Team STEPPS Curriculum, developed through a collaboration between the Department of Defense (DOD) and the Agency for Healthcare Research and Quality (AHRQ) in 2008 [53].
This curriculum introduced the “I-PASS” method, a structured framework designed to ensure the seamless transfer of essential patient information during provider transitions [3].
The "I-PASS" mnemonic stands for:
- I - Illness Severity: categorized as “stable,” “watcher,” or “unstable.”
- P - Patient Summary: a brief overview of the patient's condition
- A - Action List: a checklist of tasks and a timeline for completion
- S - Situation Awareness and Contingency Planning: preparation for potential developments
- S - Synthesis by the Receiver: the incoming provider confirms understanding by summarizing the information and repeating the action list
The implementation of the I-PASS handoff system across various levels of healthcare professionals, including physicians and nurses, has been associated with enhanced patient safety and a reduction in medical errors in both adult and pediatric care settings [54].


Self Quiz
Ask yourself...
- How does the implementation of structured communication protocols like the I-PASS method impact the dynamics of teamwork and collaboration among healthcare professionals during patient handoffs?
- Given the success of the I-PASS method in reducing medical errors, what challenges might healthcare organizations face in adopting such standardized handoff protocols, and how can we overcome these challenges to ensure widespread implementation?
Wrong-Site/Wrong-Patient Procedures
The landmark report "To Err is Human" highlighted wrong-site and wrong-patient surgeries as catastrophic instances of medical errors, sparking significant efforts to bolster safety within surgical settings [40]. In response to these concerns, the World Health Organization (WHO) led the charge in 2009 by introducing a surgical safety checklist [55]. Nurses can use this tool before, during, and after surgery, prioritizes patient safety in the operating room through a series of essential checks.
The checklist encompasses various critical verifications such as:
- Confirming the patient's identity
- Marking the intended site of surgery
- Ensuring the functionality of cardiopulmonary monitors and anesthesia equipment
- Reviewing patient allergies
- Assessing the patient's airway
- Clarifying the roles of all surgical team members
- Estimating potential blood loss
- Administering prophylactic antibiotics when necessary
- Confirming the planned surgical procedure
- Discussing potential postoperative concerns
Since its introduction, the WHO Surgical Safety Checklist has undergone numerous adaptations and refinements by healthcare systems worldwide and by authoritative bodies such as the Association of Perioperative Registered Nurses (AORN), the American Academy of Orthopedic Surgeons (AAOS), the American Society of Anesthesiologists (ASA), and the American College of Surgeons (ACS), among others.
The implementation of this checklist has become a cornerstone of contemporary surgical practice, recognized as one of the most effective strategies for enhancing patient safety in the surgical setting [55].

Self Quiz
Ask yourself...
- How can organizations ensure the consistent use of the WHO Surgical Safety Checklist in surgical settings considering the variations in resources, staff training, and organizational cultures?
- In what ways might the surgical safety checklist need to be adapted or expanded to address emerging surgical technologies and techniques, ensuring its continued relevance and effectiveness in enhancing patient safety?
- Given the proven effectiveness of the surgical safety checklist in reducing medical errors, what barriers to its adoption and consistent application might exist within surgical teams, and how can we overcome these barriers?
Medication Errors
Medication errors, encompassing wrong medication administration, incorrect dosages, and giving medications that patients are allergic to, have been a significant concern in patient safety [56]. Although individuals bear the responsibility to ensure the accuracy of medications, dosages, and awareness of patient allergies before prescribing and administering drugs, “To Err is Human” highlighted medication safety as an area needing systemic improvements [40].
The integration of Electronic Medical Records (EMRs) has been crucial in introducing safeguards against medication errors [56]. EMRs offer functionalities like verifying appropriate dosages based on patient weight, checking dosing schedules, and alerting healthcare providers about potential allergic reactions when prescribing [56]. These features are an initial line of defense at the point of prescription. For nursing staff, many hospitals have adopted barcode scanning systems, where nurses scan the patient's identification wristband before medication administration to ensure the correct patient receives the right medication.
Further enhancing medication safety in healthcare settings has elevated the role of pharmacists. Methods implemented include providing 24/7 pharmacist consultations, requiring pharmacists to review and approve medication orders, and ensuring the presence of clinical pharmacists in high-risk areas like the ICU and emergency departments. These systemic safeguards aim to minimize human error by establishing a comprehensive safety net around both healthcare providers and patients.
The essence of preventing sentinel events lies in recognizing the inevitability of human error and shifting from attributing blame to individuals to fostering a protective system and culture around healthcare providers and patients. Successful strategies in this direction have included the standardization of patient handoffs, the implementation of surgical safety checklists, the adoption of EMRs for medication verification, and enhancing the role of pharmacists within the care team. The hallmark of hospitals excelling in patient safety is a positive, supportive, and collaborative culture that invites active participation from everyone involved in patient care, including healthcare workers, patients, and their families.

Self Quiz
Ask yourself...
- How do Electronic Medical Records (EMRs) and barcode scanning systems complement each other in minimizing medication errors, and what additional steps can an organization take to further reduce the likelihood of such errors?
- Considering the expanded role of pharmacists in medication safety, how can organizations optimize the collaboration between pharmacists, nurses, and physicians to ensure the highest standards of medication safety across all stages of patient care?
- In shifting the focus from individual blame to systemic improvements for preventing medication errors, what cultural or organizational changes are necessary within healthcare institutions to support this transition?
Conclusion
Risk management in nursing is a fundamental aspect of healthcare that focuses on the systematic identification, assessment, and mitigation of risks to ensure patient safety and minimize financial losses. It emerged from the foundational need to address frequent risks encountered by patients, staff, and healthcare organizations, with the primary goal of reducing patient harm through effective management of potential hazards.
The principles of risk management have evolved from basic insurance mechanisms to encompass comprehensive strategies that integrate regulatory compliance, ethical considerations, and technology utilization [3]. The 1997 Institute of Medicine (IOM) report, which called for a shift towards a culture emphasizing safety, system improvement, and trust highlighted the urgency for robust risk management practices [3]. This led to the Patient Safety and Quality Improvement Act of 2005, focusing on enhancing patient safety through confidential reporting and prevention of medical errors [57].
Risk management in healthcare relies on utilitarian principles to maximize patient outcomes, employs statistical tools like regression to predict outcomes and improve care, and embraces diversification strategies to mitigate risks across various fronts.
In clinical nursing practice, risk management is pivotal for maintaining patient safety and enhancing care quality. By focusing on system-wide safety protocols, rather than individual errors, nursing professionals can contribute to minimizing medical errors and improving healthcare outcomes [18]. The role of risk managers has expanded to include proactive identification, assessment, and formulation of strategies to mitigate risks, reflecting the evolving nature of healthcare risk management [58].
This comprehensive approach, from patient-specific strategies to organizational risk evaluation, underlines the significance of risk management in enhancing patient safety, operational efficiency, and achieving strategic healthcare objectives [58].

Self Quiz
Ask yourself...
- How can organizations balance the principles of utilitarianism, which aim to maximize patient outcomes, with the ethical duty to treat each patient as an individual, in complex cases where resource allocation may favor broader population outcomes over individual patient needs?
- Given the expanded role of risk managers in healthcare, what specific skills and knowledge are essential for risk managers to lead proactive risk identification and mitigation efforts in today's evolving healthcare landscape?
Suicide Risk ER Admission
Introduction
This continuing education will help you answer those questions about suicide risk and admission to the ER.
Case Scenario
Chad, a 27-year-old male, is brought into the emergency department (ER) by paramedics after a suicide attempt. His wife found him unconscious in their apartment after overdosing on medication. He is conscious but visibly distressed and angry as he is wheeled into the ER.

Self Quiz
Ask yourself...
- As an emergency department nurse, do you know what to do?
- What labs should be ordered?
- How would you approach your patient and his wife?
- What resources do you have at your work to help him in the short and long term?
- What are the policies and procedures for admitting him?
Suicide in the United States
Having a background knowledge of the risks and statistics of suicide in America is important for ER nurses to have an appreciation of the severity and factors related to suicide.
Prevalence, Incidence, Demographics, and Statistics
One suicide is one too many. Suicide is a tragic event and affects the lives of more than the person who took their own life. It impacts family, friends, associates, and others interacting with the individual. Suicide is beyond a cry for help, as the person believes taking their own life is the only solution to their pain and suffering.
Suicide is the ninth leading cause of death in the United States according to the American Foundation for Suicide Prevention costing $69 billion and the loss of approximately 48,344 lives in 2022 (1). Suicide rates are estimated to be approximately 14.5 per 100,000 individuals (2). From 1999 to 2016, American suicide rates increased by nearly 30%. Risk factors appear to be multifactorial and not always due to a mental health disorder.
Suicide in the United States has been ranked as one of the highest rates among developed nations and increased by 30% between 2000 and 2020, from 10.4 to 13.5 suicides per 100,000 individuals (3). In the top nine leading causes of death among those ages 10-64, there were almost 46,000 deaths in the United States from suicide in 2020, which is approximately one death every 11 minutes (4).
The rate of those who think about suicide is higher than those who carry it out. In 2020, 12.2 million Americans admitted to seriously thinking about killing themselves, 3.2 million planned a suicide attempt, and 1.2 million attempted a suicide, not resulting in death (5, 75). During the COVID-19 worldwide pandemic, depression rates increased three-fold, leading to an increase in suicide rates in the U.S., especially for men of color (6). Mental health became a publicly discussed health issue more than ever during the pandemic.
According to the CDC, firearms account for 50% of suicides in the United States, followed by suffocation (28%), drug poisoning (11%), and non-drug poisoning (3%) (3).
There has been a steady increase in both completed suicide and suicidal ideation in the past decade, possibly due to the increase in the availability of firearms, but also complicated by the stressful lifestyle of modern society. Interestingly, more suicides occur in rural areas than suburban areas, again possibly due to the availability of firearms (74).
The American Psychiatric Association Assessment and Management of Risk for Suicide Working Group explains the risk of suicide increases with the following conditions (35):
- Psychiatric diagnoses: especially mood disorders, psychotic disorders, anxiety disorders, posttraumatic stress disorder, substance use disorders, and disorders associated with impulsivity.
- Medical conditions: particularly those that are chronic, debilitating, disfiguring, or painful.

Self Quiz
Ask yourself...
- What is the prevalence of suicide in the United States?
- What is the difference between the incidence and prevalence of suicide?
- What are the most common methods of suicide in the US?
- Why is it important for an ER nurse to know about the risk factors of suicide?
Definition of Terms
Defining terms related to suicide is important to understand what suicide is, versus suicide attempt and the terms related to self-inflicted death.
Suicide is defined by the Centers for Disease Control and Prevention and accepted as a standard definition as “death caused by injury to oneself with the intent to die” (3).
A suicide attempt is the action of self-harm with the intent to cause death without resultant death.
Suicidal ideation is the continual thinking of self-harm and death but is a broad term describing wishes and preoccupations of death and suicide. Because there is no standard definition for suicidal ideation, it becomes difficult for clinicians, researchers, and educators to identify and even code for it as a diagnosis (7).
Research indicates those with a mental health disorder are at higher risk for both suicidal ideation and eventual suicide, however, one study collected by the Centers for Disease Control revealed that as high as 50% of those who committed suicide had no known mental health disorder (7). Whether those deceased had a mental illness that was not yet diagnosed or not is unknown.
A study in the United Kingdom found that as high as 90% of those who successfully committed suicide had disclosed their suicidal ideation to their primary practitioner and 44% within the month of suicide. This points to the standard policy that a suicide threat should always be taken seriously (8).
The study found that only 22% of those primary care providers believed the threat and suicidal ideation to be a concern as they thought the person would never actually carry out the threat. For all healthcare professionals, this is a huge message and reminder to always take seriously any suicidal ideation of a client.
Imminent harm: An immediate and impending action that will cause bodily harm to self or others is imminent harm. When a client is assessed to be in imminent harm to themself, such as in an emergency department, an emergency legal code may be initiated to legally restrain the person to keep them safe. Each state may have a different code. The factors to consider include the duration of the risk, the nature of the potential injury, and the timeframe before the potential harm would occur.
Lethal: An action that is considered lethal, is sufficient to cause death. When discussing suicide, a legal action would cause the end of life of that person.
Homicide: The deliberate and unlawful killing of another person and is also called murder. Suicide is killing oneself and contrasts with homicide, which is taking the life of another person.
Classifying Levels of Risk
Identifying risk factors for suicide is valuable for suicide prevention. Recognizing which factors lead to suicide helps healthcare professionals classify the level of risk to know which level of action is necessary.

Self Quiz
Ask yourself...
- Identify the definition of suicidal ideation.
- Compare and contrast the definition of suicidal attempt and completed suicide.
- What is imminent harm?
- What are methods to determine lethality and suicide risk?
Suicide Risk Factors
Because suicide is multifactorial there are many issues to consider for those that may increase the risk for suicide. There are also protective factors within each category to consider and encourage that may help a person avoid suicidal ideation and behaviors.
Cultural Factors
Culture is defined as the customs, beliefs, behaviors, art, communication style, and dietary habits of a particular group based on ethnicity, race, religion, or even social group (10).
Cultural norms throughout history have had a powerful impact on the individual’s definitions of life, death, wellness, and disease. Historically, in some cultures, self-sacrifice by death could be considered honorable such as the Japanese belief in hari-kari death by disembowelment as a form of seppuku, a ritual suicide.
Suicide by ethnic groups varies with white European Americans having the highest rates, and American Indians and Native Alaskans the highest of ethnic groups (11).
Research also reveals that motivations towards suicide vary among different ethnicities. Latinx or Hispanic individuals were more likely to commit suicide for external stressors such as job loss, divorce, abuse, or discrimination, compared to their white counterparts who cite internal feelings of hopelessness and worthlessness (12). Ethnic minorities often demonstrate more feelings of hopelessness due to discrimination and racism, which puts them at risk for suicidal ideation and suicide (13).
Within culture there is a religious influence among people for their interpretation of the act of suicide. In Christian groups, suicide is considered one of the highest acts against God and is a sin. Other religions may consider suicide as the passing of this one life with a negative consequence for the reincarnation of the next life. Inherent in most cultures however is the sanctity of life and abhorrence of suicide, which in Hindu is termed soul-murder.
Culturally sanctioned doctor-assisted euthanasia is found in some European cultures and is acceptable only for terminal illnesses (13). Interviews with women after a suicide attempt reveal their feelings of not belonging to either culture as their adolescent experience is vastly different from their parents in the country of origin and they feel neither their parents nor peers understood them.
This research revealed that depression may not be the only emotion before a suicide attempt but additionally feelings of anger. Whereas the typical white male will commit suicide with firearms, and have access to them, a younger ethnically diverse population may attempt suicide with hanging or over-the-counter medication overdose demonstrating anger turned within.
Healthcare professionals need to recognize the impact and influence of culture and religion on an individual’s mental health and behaviors, which may either increase or protect against suicidal ideation and behaviors. Application for clinicians is to consider cultural implications along with the generic suicide risk tool that is being used.
Recognizing that Asian and Latinx Americans are generally motivated by external factors and white European Americans may be more motivated by internal factors can help guide the clinician to inquire about life factors that may impact depression, mental health, anxiety, and suicidal ideation.
Sometimes the culture itself may create feelings of shame such as the Asian culture of “saving face” versus the shame of letting parents or the general culture down. Some Asian cultures place great emphasis on excelling academically and if a child chooses not to study the topic directed by the parents, or doesn’t have the academic interest or aptitude, the child may experience deep shame and stress (15).
Protective factors within culture for an individual include feeling a sense of community within their culture. Following cultural norms and expectations appears to be protective as those who commit suicide are described as living without the boundaries of the culture such as being isolated and deviant.
Protective factors for any culture appear to be a sense of connectedness and purpose in life. Some people who still experience feelings of worthlessness or hopelessness may still find protection from feeling connected to their culture, family, an individual, or divine responsibility to honor the sanctity of life (13). Teaching traditional values and spirituality within the culture is a protective factor for youth (16).
Geographic Factors
Research shows geographic factors that matter in the incidence and prevalence of suicide.
Those in rural areas, including Veterans, have a higher incidence of suicide, which may be due to the availability of firearms (17). The only exception to that locality factor is African American males who have an increase in suicide in urban areas.
Living in rural areas may also promote social isolation, barriers to access to medical care for counseling and mental health treatment, and dangerous work conditions such as in farming communities. In addition to living in isolated areas, such as rural communities, geographic factors include living in negative and dangerous or disturbing neighborhoods in urban areas.
Protective factors include programs that help recognize people in isolated rural communities. Veteran programs can be helpful to those in rural areas who choose more isolated areas but can still promote a sense of community and belonging.
Telemedicine has been extremely helpful during the COVID-19 pandemic in delivering mental health and general medical care to people in isolation even in urban areas and can be used more in rural settings. The trend of embracing telemedicine during and after the pandemic has helped improve access to healthcare despite poor or no insurance. Sometimes people who have used telemedicine and screened positive for suicide risk are directed to an emergency department, where ER nurses can continue the screening and crisis management.
Economic Factors
External environmental factors such as unemployment and poverty play a role in despair. Areas with people below the poverty line and those who are unemployed do have an increased rate of suicide (18). Eviction and home foreclosure also increase the risk of suicide. Interestingly, a significant worsening of financial status was more significant as a risk towards suicidal ideation than chronic poverty (19).
Poor economic status also contributes to the lack of resources for mental health counseling and medications. The application for healthcare professionals is to assess the individual’s ability to afford psychiatric medications including simple SSRIs.
Protective factors could include robust financial resources, but suicide occurs even among wealthy or economically stable individuals.
Home and Family Factors
Family dynamics and a sense of belonging are key factors that can be either contributors to suicidal risk or protective factors (20). Even when a person may have a sense of family, they may still have a belief that they don’t want to be a burden, which can outweigh the home and family support, as seen in elderly suicide or those with terminal illnesses.
Studies reveal that the perception of a hostile home environment, criticism, invalidation, and lack of support for life choices increases suicidal ideation and behaviors of not just youth but adults (21, 22). Because suicide attempts are 20 times greater than completed suicide, interviews from persons who attempted suicide reveal family disharmony, parental divorce or arguments, sibling conflicts, and lack of support as factors that contributed to their sense of urgency to disappear from life.
Family factors also include a family history of suicide. Physical and genetic predispositions to mental health may be involved, but also important are the pattern of poor stress management and dysfunctional interpersonal dynamics. A history of physical, emotional, or sexual abuse, including incest, is a sign of dysfunctional family dynamics. A recent family loss and difficulty grieving can also be a risk factor.
Adverse childhood events (ACEs) accelerate mental health disorders and despair and create negative health outcomes in adulthood (23). The key message for healthcare professionals is to consider family dynamics beyond the individual at risk for suicide. Family intervention and group counseling and support may be needed in addition to the individual attention given for more effective risk management.
Protective factors for home and family include the strength and support a person may feel within a family unit. A sense of validation for their existence by loving family members is powerful. If an individual has mental health disorders or chooses an alternative lifestyle, support and understanding are protective against feelings of isolation and hopelessness.

Mental and Emotional Health
Studies reveal that although mental health disorders are found in approximately 50% of those who commit suicide, it is not a consistent factor for all cases of suicide. The more specific mental health issues include intrapersonal thoughts of a persistent sense of hopelessness, worthlessness, shame, guilt, meaninglessness, and a feeling trapped with no way out (24). Those with a sense of loneliness, separation, isolation, and feeling unloved, or rejected have an increased risk of suicidal ideation and behaviors (24).
In completing suicide screening tools, researchers have noticed that some people will skip the question of previous suicide attempts leading to a false conclusion of lower risk. Significance for clinical personnel is to review the entire instrument for completion before scoring.
Although depression is a recognized precursor to suicide it is not the only factor and is not always present. (23). Screening for depression in all individuals ideally should be done but screening is not adequate if there are no solutions or resources for the person, which could make the depression worse by creating a sense of hopelessness.
It is estimated that up to 18 million adults and 7% of the adult population have depression at any time (25). According to the American Society on Aging, up to two-thirds of elder suicides were related to untreated or undiagnosed depression. Not everyone who has depression should be placed in restraints and confinement for protection. Some screening instruments have fallen out of use after not being able to demonstrate valid and reliable identification of risk factors, such as the SAD screening tool (9).
Protective factors include strong mental and emotional health, but that is difficult for anyone to stay consistent all the time. Life itself is inherently difficult but the concept of resilience is key. Can you bounce back from a bad day within a short period, or do you linger in a state of despair or negative emotions? The ability to be resilient through life’s difficulties is key.
Mental health status and emotional strength can either increase suicide risk or add protection.
Depression
Depression is unfortunately a common emotion and is seen in at least 10% of adults at any time in the United States. Depression is a condition that follows and is interlaced with other health conditions such as the following (36). Depression is the most common mental health disorder as the issues of perceived isolation, hopelessness and lack of purpose are reported for those with suicide attempts and completed suicide.
Conditions that often correlate with depression:
- Cancer: 25% of cancer patients experience depression.
- Stroke: Up to 27% of post-stroke patients (more than 1/4 of all stroke patients) experience depression.
- Heart attack: 1 in 3 attack survivors experience depression.
- HIV: Depression is the second most common mental health condition of those with HIV.
- Parkinson’s Disease: 50% experience depression.
- Eating Disorders: approximately 33-50% of clients with anorexia have a comorbid mood disorder, such as depression (37).
- Substance Use Disorder: Over 20% of Americans with a mood disorder, including anxiety or depression have an alcohol or substance use disorder.
- Diabetes Mellitus: approximately 1/3 of all people with diabetes experience depression (Holt, et al, 2014).
- Polycystic ovary syndrome (PCOS): 20% of women with PCOS experience depression. (38).
Each of these conditions creates an additional risk of dissatisfaction with life and self-harm. Recognizing the prevalence of depression in the adult population is a call for healthcare professionals to screen all patients with simple questions for suicidal ideation.
Physical Factors
There are interesting theories based on physical factors that may impact the brain’s ability to think clearly and avoid self-harm. One theory proposes that low cortisol levels are seen in people who commit suicide, which may represent a lack of natural fight-or-flight response to stress. Low cortisol levels were found in the family history of suicide or suicide attempt. Lower than normal cortisol levels were also found in those who reported suicidal ideation. (26).
Another physiologic-based theory shows that microglial cells, found in activation of inflammation and stress are found concentrated in the prefrontal cortex of those who committed suicide. Excess microglial cells affect the concentration of neurotoxic waste products compared to neuroprotective metabolites (27).
Glutamine is a dietary amino acid related to mood and sense of well-being and inflammation may also cause alterations that may contribute to a lack of cognitive flexibility, increased impulsivity, poor memory, depressed mood, and suicidality (28).
There is emerging interest in identifying any genetic mutations that may increase the risk of suicidal ideation. Several studies have identified that gene mutations in families of those with increased incidence of depression include variants of the FKBP5 gene (29).
Risks for suicide are multifactorial and the research continues as suicide for any person and family is devastating.
Social Factors
Social isolation, feelings of not being socially accepted, or socially significant such as immigrants or ethnic minorities, are at risk for suicidal ideation and behaviors. The social construct is also related to culture as it involves interpersonal relationships.
Evidence shows that education, social status, and employment play an important role in suicidal ideation and behavior. Social factors include being male, unemployed, a lone person in a household, and divorced, widowed, or separated are strongly associated with death by suicide (30).
Protective social factors involve positive interpersonal relationships. Healthcare primary care providers, such as nurse practitioners, can refer individuals at risk for individual and group counseling and resources to develop improved emotional intelligence and interpersonal skills.

Self Quiz
Ask yourself...
- Identify at least 5 risk factors for suicide.
- Compare the statistics of suicide in the U.S. to world incidence and prevalence.
- Compare and contrast the risk factors with protective factors for suicide.
- What would you do if you recognized the behaviors of a colleague that may indicate high suicide risk?
At-Risk Populations
Identifying at-risk populations comes from demographic information about the incidence and prevalence of suicide in the United States. Statistics reveal important information about the increased risk for some individuals, which is worth recognizing. Health departments and national organizations can better create prevention and education programs based on this data.
For example, knowing that Veterans in rural areas are at increased risk of suicide due to isolation and poor access to mental health resources allows Veteran agencies to better accommodate those needs, which has been helpful. As noted in the above-listed risk factors several population groups have been recognized to be at greater risk.
Gender
There is a higher incidence of suicide among males worldwide compared to females. Studies reveal that although the incidence of suicide is low in white males over age 75, those men who do attempt suicide have higher success rates. It is estimated 40 per 100,000 men over age 75 will commit suicide. Gender makes a difference as to the means of committing suicide.
When men attempt suicide, it is with more lethal and violent means such as with guns and ropes. Women over age 75 have much lower rates of 4 per 100,000 and are often less successful with suicide efforts and commonly use less lethal methods such as drug overdose attempts. Women are twice as likely to attempt suicide but when men have greater completion rates than women.
Age
The risk of suicide affects people differently in different age groups. There are two age groups with an increased incidence of suicide which include young adults from 25-34, and again a surge in reported attempts and completed acts in the elderly from age 75-84.
Adolescents with any of the above risk factors of depression, mental health disorders, race, dysfunctional family situation and substance use are at greater risk of suicide.
“During 2019, approximately one in five (18.8%) youths had seriously considered attempting suicide, one in six (15.7%) had made a suicide plan, one in 11 (8.9%) had made an attempt, and one in 40 (2.5%) had made a suicide attempt requiring medical treatment” (31).
According to the Suicide Prevention Center, suicide was the second leading cause of death for youth ages 10 to 14, and adults ages 25 to 34 in 2020. Suicide was the third leading cause of death for people ages 15 to 24, the fourth leading cause of death for ages 35 to 44, and the seventh leading cause of death for ages 55 to 64 (32).
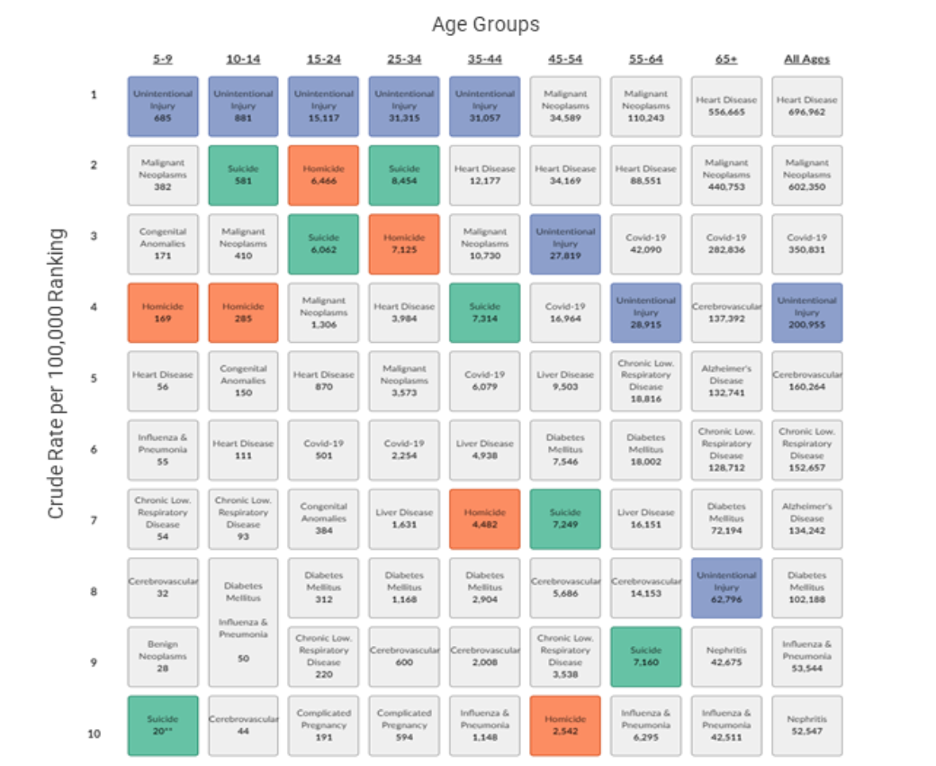
Image Source: CDC, 2021
Race
Ethnic groups with the highest rates of suicide and suicidal attempts are people of color, non-Hispanic whites, and native American Indians. Race, ethnicity, and culture were discussed earlier.
Diagnosis of Substance Use Disorder
Individuals with substance use disorders (SUD) are at a significantly greater risk of suicide for both males and females than those who don’t partake of addictive substances (72). Most research connecting substance use disorders with suicidal ideation and behaviors was conducted with Veterans, but another study examined the general population and found similar results (72). Using multiple substances is extra risky. Alcohol substance use disorder was the most common substance in the historical use of suicide attempts and completed suicide.
It is acknowledged that SUD and mental health disorders often are seen together. It is understood that the SUD condition is often an effort to deal with difficult mental health issues, family, and social issues and even loneliness and despair. When the combination of SUD and mental health disorders is not treated effectively, individuals often see suicide as a viable way to “make it all go away.”
The key message for healthcare professionals is to increase screening for substance use disorders. Using the Substance Use Brief Intervention and Referral to Treatment (SBIRT) method of asking simple screening questions should be done at each client interaction.
Military and Veterans
According to the National Veteran Suicide Prevention Annual Report, there are approximately 6000 veteran suicides annually, and 22 veteran suicides each day. The rate of suicides among this unique population is 1.5 times greater than the rate of non-military and veterans (33).
The Veterans Affairs Department (VA) recognizes the incidence of post-traumatic stress disorder (PTSD) among veterans who have served in the military and offers free services and education for prevention. Online website training, smartphone apps, and free counseling are available for veterans, healthcare professionals, and families.
In examining factors that contribute to the increase in suicide among our veterans several contributors have been identified. Transitioning out of the military and into civilian life is the most delicate time as military personnel often struggle to find their new routine and job, culture, new interpersonal relationships, often physical pain from injury, and new purpose (33 The first year of transition has been called “the deadly gap.”
Studies confirm that human beings crave a sense of belonging, which many veterans identify with in their military service. Once they leave that association, they often find a culture gap and few people understand what they may have experienced in war and military service. Veteran suicides represent almost 14% of all suicides even though their population as a group only represents 8% of the adult population (34).
Substance Use Disorder is also a contributor to the veterans’ population which compounds their risk for suicidal ideation and possible suicide (72). Many contributors to this increased risk have been explored such as risk-taking behavior personality that may have drawn them into the military initially, the use of substances to deal with traumatic military experiences, and the skill of firearms. The following diagram depicts these factors for our veterans.
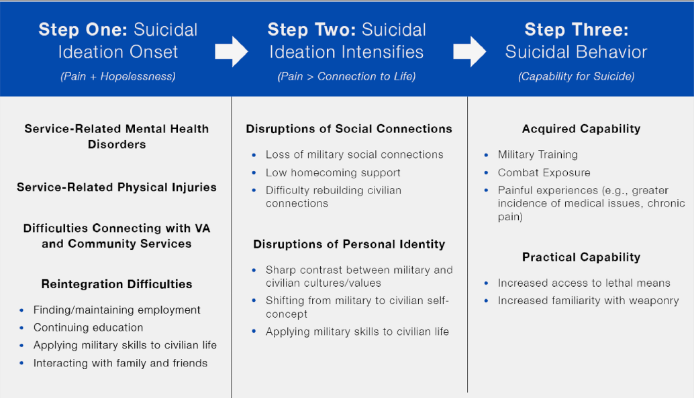
(33)
Our veterans deserve the best medical and psychological care for their service to our country. The role of healthcare professionals, especially primary care providers, is to offer effective screening and education of resources that are available. A challenge is the limited knowledge many medical professionals have about veterans’ resources, which can be difficult to navigate.
Diagnosis of Mental Illness and PTSD
Although it has been assumed all those who commit suicide have a mental health disorder, statistics show only 50% of those who commit suicide had a diagnosed mental health disorder at the time. In contrast, according to the Psychiatric Association Practice Guidelines for Psychiatric Evaluation of Adults, as high as 90% of people who commit suicide meet the diagnostic criteria for one or more mental health illnesses (35).
Healthcare Providers
A unique population at risk for suicidal ideation and behaviors are the very professionals the general population relies on for healthcare when they are in a suicidal crisis. The emotional and often physical stress of the healthcare job itself can place workers at risk.
Healthcare workers face a unique set of obstacles that increase the risk of suicide. Their demanding nature, long hours, high-stress levels, and exposure to trauma all combine to exacerbate vulnerability, increasing suicide risks. Healthcare providers also endure emotional strain when managing patient suffering and ethical dilemmas while striving to provide optimal care within resource-constrained settings.
As mental illness is still perceived with great stigma in healthcare communities, individuals seeking help for mental health problems might avoid seeking assistance altogether, leading to underreporting and untreated issues of this nature. These factors combine to put healthcare professionals at an increased risk for suicide compared to the general population.
A study in the Journal of American Medical Association revealed physicians to have significantly higher suicide rates compared to general populations, underscoring the critical need for targeted interventions and support systems in healthcare industries to combat this significant threat (77).
Suicide among nurses was publicized more during the worldwide COVID-19 pandemic when nurses and healthcare workers functioned with little sleep between shifts, managed without adequate personal protective equipment, and stood by the bedsides of dying patients on ventilators that couldn’t survive the initial onslaught of the mysterious virus and worked despite fears of exposing their own family and loved ones.
The PTSD they experienced was influenced by feelings of hopelessness when no matter what they did could not stop the fatal power of the virus. Tragically the caregivers in trauma and critical care units often experience PTSD themselves, which we know is a risk factor to suicidal ideation.
Nurses are in a unique position to add mental health screening questions to the intake form of their patients. Likewise, taking time for self-care has become not only acceptable but a popular statement of permission to do what we should have been doing all along: healing the healers.
LGBTQIAS2+ Population
This unique population has been at increased risk for suicide due to the essential elements found in those with suicidal ideation and behaviors such as hopelessness for acceptance, often lack of family support, and lack of customized health resources.

Self Quiz
Ask yourself...
- Who are at-risk populations?
- What are the conditions that create the increased risk for people who identify as LGBTQIAS2+?
Special Populations at Risk
Youth and Suicide
Suicide in youth most occurs between the ages 13-21 (69). Suicide by gender also reveals that teen girls from 12-19 are the highest incidence. Thankfully, suicide under the age of 5 is difficult to find in research and statistics. Risk factors include the lack of support and resources, or perceived by the teen, to help them address life’s challenges of critical decisions, high expectations at home, school, athletics, or anything of a competitive nature.
Mental health disorders are found in 90% of teen suicides. The most common disorder is depression. Other common disorders include anxiety and eating disorders that create distress for the individual. About 33% of suicides were proceeded by a suicide attempt or call for help.
As high as 50% of teens who committed suicide had a family member with a mental health disorder. It is supposed that the youth was modeling the maladaptive behaviors seen in the home. Divorce, violence in the home, and negative interpersonal relationships outside the home, such as a romantic breakup, have a great impact on young minds and can become fatal when they are not taught problem-solving skills.
Veterans and Military Personnel
A unique population at risk are our veterans and military personnel due to the added violence they have been exposed to and access to lethal means. Screening should be done by primary care providers, but that means the provider must be aware of their military history and service. Veterans Affairs has created extra programs after recognizing their unique added risk.

Suicide and the COVID-19 Pandemic
Not only did the coronavirus, known as Covid-19, cause the death of millions worldwide, but it created a never-before seen burden on healthcare workers who were exposed to the virus themselves, as they cared for dying patients. The rates of mental health distress, depression and anxiety soared among healthcare workers, which led some to suicide in an often-hopeless environment without adequate personal protective equipment and effective therapies.
It is estimated that in 2020 Covid-19 affected 213, 237, 126 individuals worldwide pending adequate reporting, and result in 4,452,903 deaths including some healthcare professionals.
(70). Those numbers continue to change and still increase each month.
As the burden of new mutations of Covid, including the BA.5 subvariant, take their toll on our vulnerable populations, the nursing shortage has worsened across America. A projected shortfall of 44,500 nurses is estimated by 2030 based on the current workforce and estimated need in hospitals. In the past two years exhausted nurses have left the bedside leaving gaps in direct patient care and facility administrators scrambling for compassionate and competent healthcare workers. Even nurses loyal to the profession have changed their bedside role.
A silver lining through the Covid-19 pandemic has been the new awareness of mental health challenges and stress among healthcare workers. Because of devasting suicides among “our own” more attention to the emotional resilience and well-being of our workers began. Hospitals and administrators began offering counseling, services, and screening.
Much is still needed but at least we as professionals have begun to recognize the healing of our professionals. Just as nurses are taught the risk factors and signs for suicide risk in the general population, we are now being taught to recognize those same signs in our colleagues including irritability, depression, truancy on shifts, appearance of disinterest and just going through the motions at work. Healthcare workers are also at greater risk for substance use disorders due to the increased stress of work and accessibility to medications and mind-altering substances.
Elderly and Suicide
Worldwide suicide rates show that increasing in age increases the risk of suicide, especially of those with chronic disease, or living alone. In the United States, assisted suicide is not a legal option, yet those who experience loneliness after a spouse dies, or have no family members to rely on are at increased risk for self-harm to end it all.
Primary care providers can follow up with care screening questions to identify risk factors. The challenge is always having the time in the insurance reimbursement squeeze of time. Offering seniors access to community services to prevent loneliness such as interest groups or those offered through accountable care organizations in your community can be helpful. Case managers have a unique role as well in being able to make routine phone calls to assess for risk and provide resources.

Self Quiz
Ask yourself...
- What screening tools are available for these populations of risk?
- What is a strategy to help family and friends recognize the risk for suicide among their loved ones?
- Why are healthcare professionals, including nurses, at risk of suicide?
- What are you doing now to prevent suicidal thoughts yourself?
ER Suicide Screening and Assessment
Generally, the first medical professional in the hospital the individual will encounter after a suicide attempt is an ER nurse. The ER nurse is in a unique position to approach the person with compassionate and competent care.
Nurses deliver unconditional care and compassion for patients who are hurting both physically and emotionally. It is often the nurse who serves as the advocate for the patient by providing resources and communication with the family. A careful screening and assessment of all patients for suicide risk is important, especially in the ER as ER nurses encounter a large cross-section of individuals needing immediate help.
The Interview Process and Asking about Safety
Nurses, nurse practitioners, and healthcare workers can improve the ability to identify those at risk for suicidal ideation and behaviors with appropriate and effective screening questions. Often when a provider is unsure about a suspicion for the client’s risk of suicide, completing an objective screening tool can help clarify the risk factors and client’s mental state.
Just by taking this continuing education course, the topic of suicide and recognition of those at increased risk hopefully becomes forefront in your mind. A screening tool beyond a checklist is more valuable and allowing privacy for a client to complete the assessment is also valuable to get genuine responses. This assessment can be completed ideally in an emergency department by the nursing staff.
Screening Tools
The Joint Commission's NPSG 15.01.01 now requires healthcare professionals to use a validated tool to assess suicidal risk for all patients with reasons for seeking healthcare is the treatment or evaluation of a behavioral health condition (40).
When using a suicide risk tool in an emergency department, those patients who were ambivalent about living had a double increased risk of suicide and those with active suicidal ideation who had active thoughts and plans of suicide had a three-fold increase in probability of suicide within 30 days (41, 73).
Various screening tools and instruments exist and may be used differently in a primary care office setting versus an emergency department.
The most common screening tools used in office settings are:
- P4 Screener: a 4-question screening tool that asks the “4 P’s” of past suicide attempts, a plan, probability of suicide, and preventive factors (42).
- PHQ-2 Patient Health Questionnaire 2: this is a simplified 2-question screening for those at risk for harm to themselves or others. (43).
- PHQ-9 Patient Health Questionnaire 2: this is the 9-question version of the PHQ-2.
- Columbia-Suicide Severity Rating Scale (C-SSRS): questionnaire to assess suicidal behavior and reveal suicidal ideation for pediatrics to adults (44).
The most common suicide risk screening tools used in emergency departments with strong validity and reliability include:
- Ask Suicide-Screening Questions (ASQ): a 4-question screening tool for pediatric & young adults who present with medical complaints. It is recommended to administer without the parent/guardian being present.
- Manchester Self-Harm Rule (MSHR): uses 4 questions to identify the ED patient's risk of suicide or repeating self-harm based on their history.
- Risk of Suicide Questionnaire (RSQ): a 4-question screening tool suitable for 8 years through adult; it takes 90 seconds to complete.
The Joint Commission has approved these additional screening instruments as valid and reliable:
- Beck Hopelessness Scale (BHS): a 20-item questionnaire measuring pessimism and hopelessness (7).
- Beck Scale for Suicide Ideation (BSI): a 21-item self-report instrument for detecting and measuring the current intensity of the patients’ specific attitudes, behaviors, and plans to commit suicide during the past week. The first 5 questions can be used as a screening tool (50).
- Scale for Suicide Ideation-Worst (SSI-W): a 19-item rating scale that measures the intensity of patients’ specific attitudes, behaviors, and plans to commit suicide at the period when they were the most suicidal. It takes 10 minutes to complete (7).
- Death/Suicide Implicit Association Test (IAT): developed by Harvard to test implicit thoughts towards death and suicide.
- Geriatric Suicide Ideation Scale (GSIS): a 30-item questionnaire assessing suicidal ideation on a Likert scale and customized for ages 65+ (45).
- Nurses Global Assessment of Suicide Risk (NGASR): useful for new nurses in completing a clinical assessment.
- Scale for Suicidal Ideation (SSI): a classic 19-item questionnaire for clinicians or self-ratings (paper or computer-based).

Self Quiz
Ask yourself...
- Name at least 3 screening tools that can be used in the emergency department.
- How would you describe the SBIRT tool to other colleagues you work with?
Recognition of Warning Signs
Unfortunately, despite decades of research to identify possible risk factors of suicide, there is no one clear profile person or set of behaviors that reliably identify a suicidal personality. The conclusion from numerous studies is that suicidal thoughts and behaviors are due to a complex interaction of psychological, biological, environmental, interpersonal, and cultural factors. (46)
Unlike physical conditions that be assessed and identified visibly or with diagnostic instruments, the emotional components of suicidal ideation are complex and there is no one single screening instrument that is always reliable. What research does conclude is that by using any screening tool, and with the genuine sincerity of the practitioner, someone at risk may feel safe enough to open up.
The approachability and authentic compassion of the provider is a key factor in a client honestly expressing suicidal thoughts. Unfortunately, many healthcare providers are working with tight time constraints and limited client interaction, especially in urgent care settings. Practitioners working in a primary care office setting may also not even consider a client is at risk for suicide when the primary chief complaint is something common or mundane.
In one study, five categories of identifying factors should be assessed to identify those at risk for suicidal ideation or behaviors.
Effective suicide screening instruments should assess these components (47).
- Internal psychopathology (e.g., anxiety disorders; mood disorders; hopelessness; emotion dysregulation; sleep disturbances)
- Demographic factors (e.g., age; education; employment; ethnicity; gender; marital status; religion; socioeconomic status)
- Prior suicidal thoughts and behaviors (e.g., prior deliberate self-harm, non-suicidal self-injury, suicide attempt, suicide ideation)
- External psychopathology (e.g., aggressive behaviors; impulsivity; incarceration history; antisocial behaviors; substance abuse)
- Social factors (e.g., abuse history; family problems; isolation; peer problems; stressful life events)
Studies have identified common thought patterns of those who begin to entertain suicidal thoughts as when people perceive themselves to be a burden and don’t have a sense of belonging. These negative thought patterns begin to overcome the instinct of fear of death (48). When a person’s negative thought processes dwell on non-existence, it is said they develop the capability to die.
Repeated exposure to negative events and thoughts perpetuates the feelings of being burdensome and not belonging. If emotional pain is greater than connectedness and purpose the risk of suicide becomes greater.
The feeling of hopelessness was key, and an important concept for healthcare professionals to assess. Using standardized tools to assess for the lack of purpose, belonging, and hope are the critical concepts to assess and screen for.
The concern is that there is no one perfect screening tool, and results vary based on the provider’s personal prejudices, time constraints by the provider and the medical team to assess and address risk factors, cultural considerations of the client, cognition of the client, and current management of mental health disorders (49).

Self Quiz
Ask yourself...
- What are the warning signs of suicidal ideation?
- What should effective suicidal screening tests inquire about?
- What is the Nurse Practitioner’s responsibility for a suicidal client?
Assessing Lethality
After recognizing risk factors and warning signs, a nurse should assess the lethality and possibility of fatal actions by the client. Some warning signs may actually be indicative of depression and not a true risk for self-harm, however other behaviors may be indicative of a fatal act.
Death or survival depends on various risk factors that affect the degree of lethality. When completing a lethality assessment, three parts should be considered including 1) the degree of planning for suicide, 2) the potential of perceived lethality by the person, and 3) the accessibility to the means to carry out the desired action (51).
A suicide inquiry examines the ideation, plan, behavior, and intent of the client. Assessment tools ideally should be culturally appropriate and continue to be developed yet take time. Although many people have suicidal thoughts, not all will move forward to lethal actions.
It is important to recognize that suicidal thoughts can also move across a spectrum so the client with same risk factors may be at higher risk pending environmental and mental health triggers. Recognizing which risk factors can be modified is also important for a provider when making interventions and recommendations.
Identifying protective factors have not been as researched as risk factors but according to the National Center for Injury Prevention and Control, Division of Violence Prevention has identified the following such as effective clinical care, access to healthcare and interventions, support from medical professionals and family members, problem solving skills, and cultural and religious beliefs that discourage suicide (52).
Levels of Risk
Completing the screening survey is just one step, however, the practitioner needs to identify the score and level of risk. Just documenting the risk assessment score is not adequate. A meta-analysis study revealed that despite recognizing of warning signs and clear risk factors on an assessment, 95% of those did not commit suicide however 50% of those who did were in the low-risk categories (53). Perhaps less important than a score is to truly assess the client’s physical behaviors and emotional affect, and then take appropriate actions.
It is important to distinguish between active and passive suicidal ideation. Active suicidal ideation is when a person has a conscious desire for self-harm and death as a result. The means of inflicting death should not be the key focus, but rather the thought process and person’s expectation that their attempt could be fatal is the primary concern (54).
An example of an active suicidal ideation assessment item is the Modified Suicidal Ideation Scale (Miller et al, 1991) which asks questions such as:
- "Over the past day or two, when you have thought about suicide, did you want to kill yourself? How often? A little? Quite often? A lot? Do you want to kill yourself now?"
Examples of passive suicidal ideation assessment items include:
Scale for Suicidal Ideation (SSI) with questions to measure "passive suicidal desire.”
- 0 = Would take measures to save [one's own] life
- 1 = Would leave life/death to chance
- 2 = Would avoid steps necessary to save or maintain life
European Depression Scale (55) that asks:
- "In the past month, have you ever wished you were dead?"
Documenting Suicide Risk
Documenting suicide risk must be done as always after a provider’s visit, as in any documentation of a visit. The name of the risk screening tool and score should be included in the notes, along with interventions for safety and client/family education.

Self Quiz
Ask yourself...
- What are methods to determine lethality and suicide risk?
- How should suicide risk be documented in your department?
- Explain the levels of risk scale for suicide.
Healthcare Provider Training
Due to the continual high rates of suicide and suicide attempts, more effective suicide prevention strategies are needed. Ideally, if we knew exactly how to prevent suicide, there would be no more suicides, however the reality is much more complicated. Several ideas have been proposed including better training for practitioners to screen and interview effectively, and to reduce access to firearms (56).
The Joint Commission has issued recommendations for healthcare professionals and primary care providers to do the following before a client leaves an appointment or the ER:
- Review each patient’s personal and family medical history for suicide risk factors.
- Screen all patients for suicide ideation using a brief, standardized, evidence-based screening tool.
- Review screening questionnaires before the patient leaves the appointment or is discharged.
- Act based on the assessment results to inform the level of interventions needed (40).
Teaching family members and friends to support someone in a suicide crisis requires clear guidance (75).
Healthcare professionals can begin the public awareness of how to help such as the following actions:
- Talk openly and honestly. Don’t be afraid to ask questions like: “Do you have a plan for how you would kill yourself?”
- Remove means such as guns, knives, or stockpiled pills.
- Calmly ask simple and direct questions, like “Can I help you call your psychiatrist or counselor?”
- If there are multiple people around, have one person speak at a time.
- Express support and concern
- Don’t argue, threaten, or raise your voice.
- Don’t debate whether suicide is right or wrong.
- Try to model calmness in your own body.
- Be patient with the person.
- Use the phrase “It’s safe for you to share your feelings with me because I care about you.”
- Let the person know there are healthcare professionals who can help them with their thoughts.
Recognition of Warning Signs
According to the National Alliance on Mental Illness, recognizing warning signs and behaviors of someone about to commit suicide include the following:
- Increased alcohol and drug use
- Aggressive behavior
- Withdrawal from friends, family, and community
- Dramatic mood swings
- Impulsive or reckless behavior
- Collecting and saving pills or buying a weapon
- Giving away possessions
- Tying up loose ends, like organizing personal papers or paying off debts
- Saying goodbye to friends and family


Self Quiz
Ask yourself...
- What is a strategy to help family and friends recognize the risk of suicide among their loved ones?
- How can you support the family of an individual who has attempted to commit suicide?
- What phrases should you never use to an individual who has attempted suicide?
Treatment and Management of Clients at Risk
Treatment and management of clients at risk for suicide is based on the unique risk factors and needs of the individual client. Several strategies including different therapies have been studied and are available.
Medical Management of Mental Illness
According to the National Institute of Mental Health (NIMH) as high as 46% of those who committed suicide had a mental illness (2). Management of clients with mental illness is one important treatment strategy. When clients with mental illness are not treated appropriately with effective pharmacological management or counseling, the risk of suicidal ideation increases.
The concerning mental health issues include intrapersonal thoughts of a persistent sense of hopelessness, worthlessness, shame, guilt, meaninglessness, and a feeling trapped with no way out (12). A combination of depression, anxiety, or psychological disorders can compound the feelings of hopelessness. Research shows that both pharmacological treatment and cognitive behavior therapy for mood disorders including depression and bipolar disorder, which are among the most common disorders in the world, have better outcomes than either strategy alone (61).
Currently, antidepressant medications used for mood disorders include monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants. In the past two decades, the more commonly prescribed agents that block the reuptake of serotonin, norepinephrine, or dopamine known as selective serotonin reuptake inhibitors (SSRIs) and serotonin/noradrenaline-reuptake inhibitors (SNRIs) (62).
Cognitive Behavior Therapy (CBT) has been the most researched therapy for the treatment of mood disorders and shows statistically significant improvements in mood for participants. ER nurses can also help patients obtain access to mental health services in their community. Knowing and sharing which mental health services are available is a way of advocating for patients experiencing depression and stress.
Management of Substance Abuse
As substance use disorder is associated with an increase in suicide risk, the ER nurse should screen for substance use. Screening, Brief Intervention, and Referral to Treatment (SBIRT) is an evidence-based practice used to identify, reduce, and prevent problematic use, abuse, and dependence on alcohol and illicit drugs (5). The SBIRT model is the practice of having healthcare professionals, from physicians, nurses, nursing assistants, medical assistants and any medical person who interacts with patients, screen for substance use and abuse. If the patient’ screen is positive, the healthcare professional refers them to available programs and community resources. SBIRT is an early and brief intervention of screening questions and takes less than 5 minutes. An additional history, physical exam, and clinical diagnosis of substance abuse disorder take an additional 10-20 minutes. The time for asking screening questions and offering resources is billable to Medicare/Medicaid. The screening and referral to treatment includes a patient encounter, history, physical exam, clinical diagnosis, and plan for care specific to the concern of substance abuse.
A key aspect of SBIRT is the integration and coordination of screening, early intervention, and treatment components into a system of care. The link between substance uses and suicidal ideation has been documented (5).
It is estimated that a person with a substance abuse addiction must be asked at least 10 times by a healthcare professional before they even move towards contemplation in the behavior change process. You may be person #2 or #10 but it takes screening without judgment, in the spirit of help and coaching to move a person forward to begin to consider substance use. Many people in a substance abuse pattern want to stop but don’t know how or what their resources are.
Simple questions to begin with include “Do you smoke?” If yes, then ask about the frequency of daily consumption and years smoked to calculate pack years. The next important question is simply to ask if they have a desire to stop smoking. If the answer is yes, then you can offer programs and resources. If the answer is no, then let them know you are concerned about their health and you are available with resources when they’re ready to stop.
Each time you have a patient encounter, simply go through the same questions and eventually the person may begin to be in the contemplative stage of change. For alcohol and illicit drug use using the CAGE format is an acronym to help you remember to ask certain questions.
Many people with a substance use disorder may feel like they are in a CAGE and just need help to get out.
C: Have you ever felt you needed to Cut down on your drinking? ...
A: Have people Annoyed you by criticizing your drinking? ...
G: Have you ever felt Guilty about drinking? ...
E: Have you ever felt you needed a drink first thing in the morning (Eye-opener) to steady your nerves or to get rid of a hangover?
Learning how to become comfortable with asking the screening questions takes practice and you can overcome any hesitation you may feel that you are prying into their personal life by practicing simple questions. Asking the screening questions is a strong start and then referring clients to effective resources for cessation and recovery is the next important component of SBIRT.
You need to learn what resources are available in your community such as free Alcoholics Anonymous meetings and groups, and more. A simple Google search is a good place to start. There are also many free national resources such as the 1-800-quit-now phone lines that will offer resources to individuals seeking help.

Self Quiz
Ask yourself...
- What screening tools do you currently use in your ER for suicidal ideation?
- What screening tools do you want to learn more about?
- After the acute stage of a suicide attempt, what are the treatment strategies for a patient?
- What is the role of the nurse in helping with the transition from the acute crisis stage to admission?
Suicidal ER Admission
ER nurses play a strong role in caring for a patient being admitted after a suicide attempt, one who verbalizes a high threat of suicide, and those who screen at risk for suicide.
When patients who have attempted suicide arrive at an ER for evaluation and admission, several critical steps must be followed to ensure their safety and provide appropriate care. Initial assessment takes place in the triage area where a nurse assesses and prioritizes care based on the severity of injuries sustained and mental health status.
Nurses working in triage play an invaluable role in quickly recognizing patients in need of immediate medical assistance, particularly those at risk of further harm or worsening health conditions.
After receiving reports from paramedics regarding any attempted suicide attempts and methods used in attempts, as well as interventions taken en route to hospital care, the nurse gathers pertinent details to share with the provider.
This report aids emergency room physicians and clinicians with their evaluation and treatment plan. Following triage and initial assessment, the nurse conducts a full physical exam on the patient to assess physical health issues because of attempted suicide as well as any injuries from the attempt (78).
This assessment includes vital signs monitoring, wound examination, and neurological testing to detect trauma or intoxication symptoms. Nurses conduct mental health evaluations to detect any psychiatric conditions or risks and assess an attempter's suicide risk.
Safety must always come first when caring for such individuals. Nurses work closely with hospital security to create an atmosphere conducive to patient safety and staff wellbeing. Security measures implemented may include continuous observation of patients and removal of potentially hazardous objects from the area near them; in addition to maintaining a calm, supportive atmosphere in the emergency department (ER).
Working closely together between nurses and security staff is vital to effectively address safety concerns and avoid additional injury. Security staff may assist in de-escalating volatile situations and assuring physical safety for both patients and others in the emergency setting.
Together with nurses and security personnel, nurses and security personnel can manage admission processes for those who have attempted suicide efficiently and compassionately while offering comprehensive emergency care in this setting.
Labs and Diagnostic Tests
Healthcare providers assessing suicidal patients in medical settings typically order laboratory and diagnostic examinations to evaluate physical health issues, identify any underlying medical conditions, and assess any self-inflicted injuries sustained during evaluation. These tests may differ based on an individual patient's presentation, medical history, and clinical judgment.
Some common lab and diagnostic tests that might be done for someone post-suicide attempt or in an acute suicide crisis include (80):
- Full Blood Count (CBC): This provides detailed information regarding red and white blood cell counts, platelet count, and hemoglobin levels of an individual patient. Abnormalities in these parameters could indicate serious medical conditions like infection, anemia, and other blood disorders.
- A Comprehensive Metabolic Panel (CMP) measures various organ function markers including electrolyte levels, kidney, and liver enzyme levels such as creatinine urea nitrogen ratios as well as liver enzyme activity including Alanine Amitransferase, Aspartate Amitransferase levels as well as glucose concentration levels.
- Urinalysis: Urinalysis evaluates both physical and chemical characteristics of urine samples to detect metabolic imbalances or organ dysfunction, including any trace amounts of blood, proteins, glucose, or abnormal cells present. Urinary tract infections, kidney dysfunction, or metabolic disorders may all be detected using simple labs and then a simple ultrasound.
- Drug Screening: Toxicology screening may also be conducted if substance abuse or overdose is suspected. This process typically includes clinical interviews, standardized assessment tools, and collaboration between mental health providers.

Self Quiz
Ask yourself...
- What lab tests may be taken on someone who has attempted suicide and why are they done?
- What is the relationship between suicidal ideations and possible physical disorders?
Legal and Ethical Issues with Suicide
Even with the best intentions to help people at risk for suicide, there are legal and ethical issues to consider. Privacy and the right to choose are still key concepts in our society. ER nurses are the frontrunners in seeing the legal side of protecting patients often against their will. When a patient is brought into the ER after a suicide attempt or threat of suicide, the admitting provider may write an order for a 72-hour emergency hold. This is about the legal statute that a person may be held against their will if they are deemed a threat to themselves or others.
Ideally ER admission for suicide should include a safe and compassionate environment, however, most emergency departments (EDs) lack the facilities, staff or expertise required to respond appropriately when dealing with mental health emergencies. Furthermore, most EDs tend to be noisy and disorganized environments unsuitable for de-escalating behavioral health crises. Retrofitting emergency departments to handle behavioral health and suicidal patients is expensive for many hospitals.
Even with adequate funding in place, psychiatric patients frequently experience more stigma and bias when receiving emergency care, including being made to undress without privacy as they may be placed in a hallway for easier monitoring, prolonged boarding times, and minimal therapeutic support during that period (79). ED patients generally don't benefit from much therapeutic assistance during that time. Basic needs like showering, brushing teeth, using the phone, and eating can be extremely challenging for psychiatric patients in ER settings.
An emergency department mental health evaluation does not aim to initiate or provide even short-term mental healthcare but to assess an individual's risk of self-harm (80). Such assessments only consider admission or discharge requirements without providing recommendations for actual treatments or recommendations to manage conditions that have arisen during evaluations.
As part of an overall suicide risk screening in an emergency department (ED), brief screening for suicide risk has limited sensitivity in identifying which patients pose the highest risk. However, low-risk patients can still be identified, and those in which psychiatric holds and real-time psychiatric consultation while in the ED may no longer be necessary allowing more expeditious discharge from the ED.
The role of the ER nurse in admitting a suicidal patient is a careful and delicate one due to the potentially lethal outcomes if a patient is discharged unsafely. Suicidal patients may be admitted into a psychiatric unit where security is provided at a higher level and psychiatric consultations are given. Ideally, the patient will be able to receive further assessments and referrals for appropriate services. Unfortunately, an ER nurse may never know the outcome of their careful attention to the suicidal patient, but knowing the nurse did all possible within their scope can still help. ER nurses can make a difference by becoming more active in public legislation for safe facilities for mental health patients, improvements in hospital policy development and staffing, and effective use of existing screening tools.

Self Quiz
Ask yourself...
- What are ethical issues to consider for an ER nurse about admitting a patient without adequate safety measures?
- What is the role of the nurse in the transition process from the ER to admission?
Case Study Continues
Due to careful and compassionate care from an emergency room nurse, Chad, the 27-year-old male who was brought into the ER after a suicide attempt was admitted and provided with appropriate psychological evaluation and referral for counseling services. After arriving at the emergency department following an attempted suicide attempt, he was met with kindness from a dedicated nurse.
Recognizing how urgent his condition was, she swiftly coordinated his admission process, so he received immediate medical care. With compassion and professionalism, the nurse conducted a detailed assessment, covering both physical and mental aspects of her patient's illness. Once stable, he continued receiving support from the nurse as his condition stabilized over time.
Recognizing the necessity for psychological evaluation and counseling services, the nurse collaborated closely with the healthcare team to facilitate the transition of the patient to appropriate mental health resources. The nurse advocated on behalf of his patient's needs, making certain he received follow-up care and support to address mental health concerns and reduce future self-harm risk. Through careful intervention and a compassionate approach by this ER nurse, the patient felt heard, understood, and supported during a vulnerable moment in his life.
With access to comprehensive mental health services as well as ongoing support services available at his disposal, his journey toward recovery was enabled thanks to a compassionate ER nurse who made such a significant difference when needed the most.
Resources
* Call the National Suicide Prevention Lifeline1-800-273-TALK (8255). Here is a list of international suicide hotlines.
* Text TALK to 741741 for 24/7, anonymous, free counseling.
* Call the SAMHSA Treatment Referral Hotline, 1-800-662-HELP (4357), for free, confidential support for substance abuse treatment.
* Call the RAINN National Sexual Assault Hotline, 1-800-656-HOPE (4673), for confidential crisis support.
* Call Trevor Lifeline, 1-866-488-7386, a free and confidential suicide hotline for LGBT youth.
* 7 Cups and IMAlive are free, anonymous online text chat services with trained listeners, online therapists, and counselors.
Veterans Crisis Line 1-800-273-8255 or text 838255 or go to veterancrisisline.net
Conclusion
Suicide remains one of the leading causes of death in the United States. Risk factors have been identified and solutions proposed. Various prevention strategies include mental health awareness, public awareness for suicide prevention and detection, addressing limited access to lethal weapons, addressing unique concerns for high-risk sub-groups such as offering school-based resources for youth, educating healthcare primary care providers as the gatekeepers, staffing crisis hotlines, and promoting more free counseling services with legislation and tax funds.
Suicide is a complex issue and there are no single solutions. It will continue to require a multifactorial approach that addresses the cultural, economic, political, social, and religious factors. Every effort as a Nurse Practitioner to truly connect with your patients, provide screening, and offer real resources, is a life that may be saved.
References + Disclaimer
- Association of American Medical Colleges. (2019). Diversity in medicine: facts and figures 2019. AAMC. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018
- Buchmueller, T. C. and Levy, H. G. (2020). The ACA’s Impact on racial and ethnic disparities in health insurance coverage and access to care. Health Affairs, 39(3). https://doi.org/10.1377/hlthaff.2019.01394
- Cardiology Magazine. (August 14, 2020). Cardiovascular care of women. Understanding the disparities. American College of Cardiology. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018
- Centers for Disease Control and Prevention. (June 19, 2020). Veterans health statistics survey. CDC. https://www.cdc.gov/nchs/nhis/veterans_health_statistics/tables.htm
- Centers for Disease Control and Prevention. (September 23, 2021). Data and statistics about ADHD. CDC.https://www.cdc.gov/ncbddd/adhd/data.html#:~:text=Boys%20are%20more%20likely%20to,12.9%25%20compared%20to%205.6%25).
- Centers for Disease Control and Prevention. (2024). Disability impacts us all. CDC. https://www.cdc.gov/ncbddd/disabilityandhealth/infographic-disability-impacts-all.html
- CHADD. (n.d.). How the gender gap leaves girls and women undertreated for ADHD. Children and Adults with Attention Deficit Hyperactivity Disorder. https://chadd.org/adhd-news/adhd-news-caregivers/how-the-gender-gap-leaves-girls-and-women-undertreated-for-adhd/
- Diaz, M. (2023). Veteran homelessness increased by 7.4% in 2023. VA News. https://news.va.gov/126913/veteran-homelessness-increased-by-7-4-in-2023/.
- Guevara, J. P., Wade, R., and Aysola, J. (2021). Racial and ethnic diversity in medical schools- why aren’t we there yet? The New England Journal of Medicine, 385(1732-1734) DOI: 10.1056/NEJMp2105578
- Healthy People 2020. (2020a). Disability and health. HealthyPeople.gov. https://www.healthypeople.gov/2020/topics-objectives/topic/disability-and-health
- Healthy People 2020. (2020b). Data 2020. HealthyPeople.gov https://www.healthypeople.gov/2020/data-search/
- Healthy People 2020. (2020c). Lesbian, gay, bisexual, and transgender health. HealthyPeople.gov https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health
- Lee, B., Wang, Y., Carlson, S.A., et al. (2020). National, State-Level, and County-Level Prevalence Estimates of Adults Aged ≥18 Years Self-Reporting a Lifetime Diagnosis of Depression — United States, 2020. MMWR Morb Mortal Wkly Rep 2023;72:644–650. DOI: http://dx.doi.org/10.15585/mmwr.mm7224a1
- Levine DA, Gross AL, Briceño EM, et al. (2020). Association between blood pressure and later-life cognition among black and white individuals. JAMA Neurology, 7(7):810–819. doi:10.1001/jamaneurol.2020.0568
- Liese, K., Stewart, K., Pearson, P., Lofton, S., Mbande, T., Patil, C., Liu, L., & Geller, S. (2022). Melanated Group Midwifery Care: Centering the Voices of the Black Birthing Community. Journal of midwifery & women’s health, 67(6), 696–700. https://doi.org/10.1111/jmwh.13438
- Lillard, J. W., Jr, Moses, K. A., Mahal, B. A., & George, D. J. (2022). Racial disparities in Black men with prostate cancer: A literature review. Cancer, 128(21), 3787–3795. https://doi.org/10.1002/cncr.34433
- Mitra, M., Long-Bellil, L., Moura, I., Miles, A., and Kaye, H. S. (2022). Advancing health equity and reducing health disparities for people with disabilities in the United States. Health Affairs; 41, (10). https://doi.org/10.1377/hlthaff.2022.00499
- Mude, W., Oguoma, V. M., Nyanhanda, T., Mwanri, L., & Njue, C. (2021). Racial disparities in COVID-19 pandemic cases, hospitalizations, and deaths: A systematic review and meta-analysis. Journal of global health, 11, 05015. https://doi.org/10.7189/jogh.11.05015
- Nair, S., Sawant, N., Thippeswamy, H., Desai, G. (2021). Gender Issues in the Care of Elderly: A Narrative Review. Indian Journal of Psychological Medicine. 2021;43(5_suppl):S48-S52. doi:10.1177/02537176211021530
- National Coalition Against Domestic Violence. (n.d.). Statistics. NCADV. https://ncadv.org/STATISTICS#:~:text=1%20in%203%20women%20and,be%20considered%20%22domestic%20violence.%22&text=1%20in%207%20women%20and,injured%20by%20an%20intimate%20partner.
- National Council for Mental Wellbeing. (n.d.). Veterans. National Council for Mental Wellbeing. https://www.thenationalcouncil.org/topics/veterans/
- National Institute of Health. (2024). HIV in gay and bisexual men. HIVinfo.NIH.gov. https://hivinfo.nih.gov/understanding-hiv/fact-sheets/hiv-and-gay-and-bisexual-men
- Pennic, J. (2024). The report finds that 64% of women want to talk more about their health. https://hitconsultant.net/2024/05/09/64-of-women-want-to-talk-more-about-their-health-report-finds/
- Rasmussen, P., & Farmer, C. M. (2023). The Promise and Challenges of VA Community Care: Veterans’ Issues in Focus. Rand Health Quarterly, 10(3), 9.
- Regis College. (n.d.). Why ageism in healthcare is a growing concern. Regis College. https://online.regiscollege.edu/blog/why-ageism-in-health-care-is-a-growing-concern/
- Shetty, Siddharth, A., Chandini, S., Fernandes, Sharol, Lionel, Safeekh, A. T. (2020). Hysteria: a historical perspective. Archives of Medicine and Health Sciences 8(2):p 312-315, DOI: 10.4103/AMHS.amhs_220_20
- Streed C. G., Jr (2022). Health Communication and Sexual Orientation, Gender Identity, and Expression. The Medical Clinics of North America, 106(4), 589–600. https://doi.org/10.1016/j.mcna.2021.12.005
- Swihart, D.L., Yarrarapu, S. N. S., Martin, R. L. (August 31, 2021). Cultural religious competence in clinical practice. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK493216/
- Yu, H., Flores, D.D., Bonett, S. et al. (2023). LGBTQ + cultural competency training for health professionals: a systematic review. BMC Med Educ 23, 558. https://doi.org/10.1186/s12909-023-04373-3
- Arif, S. A., & Schlotfeldt, J. (2021). Gaps in Measuring and Mitigating Implicit Bias in Healthcare. Frontiers in pharmacology, 12, 633565. https://doi.org/10.3389/fphar.2021.633565
- American Academy of Pediatrics. (2015). Recommendations for preventative pediatric health care. Bright Futures. Retrieved from: http://www.advocaresocietyhillpeds.com/getattachment/Office-Info/Well-Child-Visits/AAP-Health-Maintenance-Chart.pdf.aspx
- American Foundation for Suicide Prevention. (n.d.). Risk factors, protective factors, and warning signs. AFSP. Retrieved from: https://afsp.org/risk-factors-protective-factors-and-warning-signs
- Al-Asadi AM, Klein B, Meyer D. (2015). Multiple comorbidities of 21 psychological disorders and relationships with psychosocial variables: a study of the online assessment and diagnostic system within a web-based population. Journal of Medical Internet Research, 26;17(2):e55. doi: 10.2196/jmir.4143. PMID: 25803420; PMCID: PMC4392551.
- Jacobsen, J.C., Zhang, B., Block, S.D., Maciejewski, P.K., Prigerson, H.G. (2010). Distinguishing symptoms of grief and depression in a cohort of advanced cancer patients. Death Studies, 34(3):257-73. doi: 10.1080/07481180903559303. PMID: 20953316; PMCID: PMC2953955.
- National Health Alliance on Mental Illness. (n.d). Mental health screening. NAMI. Retrieved from: https://www.nami.org/Advocacy/Policy-Priorities/Improving-Health/Mental-Health-Screening
- National Health Alliance on Mental Illness. (2022). Mental health by the numbers. NAMI. Retrieved from: https://nami.org/mhstats?gclid=Cj0KCQiAiJSeBhCCARIsAHnAzT8YJyMwaR4nXArETaLvF6OceJ3q4QTHQXR9lbSLAyH6zitldFr5orUaAra4EALw_wcB
- National Health Alliance on Mental Illness. (2022). Risk of suicide. NAMI. Retrieved from: https://www.nami.org/About-Mental-Illness/Common-with-Mental-Illness/Risk-of-Suicide?gclid=CjwKCAiA2rOeBhAsEiwA2Pl7Q6jzFsuqcxXhnVdejzjVIQtowvJCpfwxB-GqWBYI5F5A053PseeV4RoCvuYQAvD_BwE
- National Institute of Mental Health. (2022). Anxiety disorders. NIH. Retrieved from: https://www.nimh.nih.gov/health/topics/anxiety-disorders
- National Institute of Mental Health. (2022). Depression. NIH. Retrieved from: https://www.nimh.nih.gov/health/topics/depression
- National Institute of Mental Health. (2022). Mental illness. NIH. Retrieved from: https://www.nimh.nih.gov/health/statistics/mental-illness
- National Institute of Mental Health. (2022). Post traumatic stress disorder. NIH. Retrieved from: https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd
- National Institute of Mental Health. (2022). Suicide. NIH. Retrieved from: https://www.nimh.nih.gov/health/statistics/suicide/
- University of Queensland. (2019). Risk for developing more than one mental health disorder revealed. Science Daily. Retrieved from: https://www.sciencedaily.com/releases/2019/01/190117090515.htm#:~:text=%22In%20the%20first%20six%20months,months%20since%20diagnosis%2C%22%20Professor%20McGrath
- Alzheimer’s disease fact sheet. (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet
- Preventing Alzheimer’s disease: What do we know? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/preventing-alzheimers-disease-what-do-we-know
- How is Alzheimer’s disease treated? (n.d.). Retrieved February 10, 2021, from https://www.nia.nih.gov/health/how-alzheimers-disease-treated
- Castro-Aldrete, L., Moser, M. V., Putignano, G., Ferretti, M. T., Diemch, A. S., and Chadha, A. S. (2023). Sex and gender considerations in Alzheimer’s disease: The Women’s Brain Project contribution. Frontiers in Aging Neuroscience, 15, 1-11. https://doi.org/10.3389/fnagi.2023.1105620
- Carrarini, C., Russo, M., Dono, F., Barbone, F., Rispoli, M. G., Ferri, L., Di Pietro, M., Digiovanni, A., Ajdinaj, P., Speranza, R., Granzotto, A., Frazzini, V., Thomas, A., Pilotto, A., Padovani, A., Onofrj, M., Sensi, S. L., & Bonanni, L. (2021). Agitation and Dementia: Prevention and Treatment Strategies in Acute and Chronic Conditions. Frontiers in neurology, 12, 644317. https://doi.org/10.3389/fneur.2021.644317
- Alzhimer’s Disease: Common Medical Problems. (n.d.). Retrieved January 9, 2024, 10, 2021, from https://www.nia.nih.gov/health/alzheimers-caregiving/alzheimers-disease-common-medical-problems #7 Wandering and Alzhimer’s Diease. (n.d.). Retrieved January 9, 2024, from https://www.nia.nih.gov/health/alzheimers-changes-behavior-and-communication/wandering-and-alzheimers-disease
- National Institute on Aging. (2021) What is Lewy Body Dementia? Causes, Symptoms, and Treatments. Retrieved on December 5, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/what-lewy-body-dementia-causes-symptoms-and-treatments
- Medline Plus [Internet] National Library of Medicine. (2021). Dementia with Lewy Bodies. Retrieved on December 5, 2023, from https://medlineplus.gov/genetics/condition/dementia-with-lewy-bodies/#causes
- Haider, A., Spurlin, B., and Sanchez-Manso, J. (2023). Lewy Body Dementia. In StatPearls. StatPearls [Internet]. Retrieved on December 7, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK482441/
- Prasad, S., Katta, M., Abhishek, S., Sridhar, R., Valisekka, S., Hameed, M., Kaur, J., and Walia, N. (2022). Disease-a-Month. Vol. 69, Issue 5, May 2023, 101441. Retrieved from https://www.sciencedirect.com/science/article/pii/S0011502922001250?via%3Dihub
- Medline Plus [Internet] National Library of Medicine. (2019). Lewy Body Dementia. Retrieved on December 7, 2023, from https://medlineplus.gov/lewybodydementia.html
- Hershey, L. and Coleman-Jackson, R. (2019). Pharmacological Management of Dementia with Lewy Bodies. Drugs Aging. 2019; 36(4) 309-319. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6435621/
- National Institute on Aging. (2018). Caring for a Person with Lewy Body Dementia. Retrieved on December 21, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/caring-person-lewy-body-dementia
- Capouch, S., Farlow, M., and Brosch, J. (2018). A Review of Dementia with Lewy Bodies’ Impact, Diagnostic Criteria and Treatment. Neurology and Therapy. 2018 Dec; 7(2): 249-263. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6283803/
- Lewy Body Dementia Resource Center. (2021) Our Mission & Vision. Retrieved on December 21, 2023, from https://lewybodyresourcecenter.org/about-us/mission/
- Lewy Body Dementia Association. (2023). About LBDA. Retrieved on December 20, 2023 from https://www.lbda.org/about-lbda/
- National Institute of Neurological Disorders and Stroke. (2023) Focus on Lewy BOdy Dementia (LBD). Retrieved on December 20, 2023, from https://www.ninds.nih.gov/current-research/focus-disorders/alzheimers-disease-and-related-dementias/focus-lewy-body-dementia-lbd-research
- National Institute of Neurological Disorders and Stroke. (2018). PDBP About. Retrieved on December 21, 2023, from https://pdbp.ninds.nih.gov/about
- Bousiges, O. and Blanc, F. (2022). Biomarkers of Dementia with Lewy Bodies: Differential Diagnostic with Alzheimer’s Disease. International Journal of Molecular Sciences. 2022 Jun; 23 (12): 6371. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9223587/
- Howell, M. and Schenk, C. Rapid Eye movement sleep behavior disorder. 2023) UpToDate. Retrieved on December 21, 2023 from https://www.uptodate.com/contents/rapid-eye-movement-sleep-behavior-disorder/print#:~:text=INTRODUCTION%20Rapid%20eye%20movement%20(REM,thrashing%2C%20punching%2C%20and%20kicking.
- Arevalo, I., Smailagic, N., Roque I Figuls, M., Ciapponi, A., Sanchez-Perez, E., Giannakou, A., Pedraza, O., Cosp, X., and Cullum, S. (2015). Mini-Mental State Examination (MMSE) FOR THE DETECTION OF Alzheimer’s disease and other dementia in people with milk cognitive impairment (MCI). Cochrane Library. 2015 Mar; 2015(30): CD010783. Retrieved from https://doi.org/10.1002/14651858.CD010783.pub2
- National Institute on Aging. (2021). Diagnosing Lewy Body Dementia: For Professionals. Retrieved on December 22, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/diagnosing-lewy-body-dementia-professionals
- American College of Obstetrics and Gynecology. (2022). Reproductive and sexual coercion. Retrieved from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2013/02/reproductive-and-sexual-coercion#:~:text=Reproductive%20coercion%20is%20related%20to,pregnancy%20coercion%2C%20and%20pregnancy%20pressure.
- Burnett, L. B. (2018, July). Domestic violence follow up. Emergency Medicine. Retrieved from: https://emedicine.medscape.com/article/805546-overview?form=fpf
- Domestic Abuse Intervention Programs. (n.d.). Power and control wheel. NCADV. Retrieved from: https://www.theduluthmodel.org/wp-content/uploads/2017/03/PowerandControl.pdf
- Centers for Disease Control and Prevention. (2021, November). Risk and protective factors for perpetration. Retrieved from: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/riskprotectivefactors.html
- Centers for Disease Control and Prevention. (2023, January). Fast fact: preventing teen dating violence. Retrieved from: https://www.cdc.gov/violenceprevention/intimatepartnerviolence/teendatingviolence/fastfact.html
- Connecticut Coalition Against Domestic Violence. (2024). https://www.ctcadv.org/
- Connecticut State Department of Public Health. (n.d.). Continuing education. DPH. https://portal.ct.gov/DPH/Practitioner-Licensing–Investigations/Registered-Nurse/Continuing-Education
- Connecticut State Department of Public Health. (n.d.). Mandatory reporters of abuse, neglect, exploitation, and impaired practitioners. DPH. https://portal.ct.gov/DPH/Practitioner-Licensing–Investigations/PLIS/Mandatory-Reporters-of-Abuse-Neglect-Exploitation-and-Impaired-Practitioners
- Connections for Abused Women and Their Children. (2023, February). The impact of domestic violence. Retrieved from: https://www.cawc.org/news/the-impact-of-domestic-violence/?gclid=Cj0KCQjwiIOmBhDjARIsAP6YhSWPF8eUFB4f_OF2oy4w6YdyGheawOkX8Heh_hvOCPT-Wg3vp9bICeIaAkH5EALw_wcB
- Gillette, H. (2022). The 4 stages of the cycle of abuse: from tension to calm and back. Retrieved from: https://psychcentral.com/health/cycle-of-abuse
- GLAAD. N.d. Glossary of terms: LGBTQ. Retrieved from: https://www.glaad.org/reference/terms
- Karakurt, G., Whiting, K., van Esch, C., Bolen, S. D., & Calabrese, J. R. (2016). Couples Therapy for Intimate Partner Violence: A Systematic Review and Meta-Analysis. Journal of marital and family therapy, 42(4), 567–583. https://doi.org/10.1111/jmft.12178
- Lantz, B., Wenger, M. R., & Craig, C. J. (2023). What If They Were White? The Differential Arrest Consequences of Victim Characteristics for Black and White Co-offenders. Social problems, 70(2), 297–320. https://doi.org/10.1093/socpro/spab043
- March of Dimes. (n.d.). Abuse during pregnancy. Retrieved from: https://www.marchofdimes.org/find-support/topics/pregnancy/abuse-during-pregnancy#:~:text=Unfortunately%2C%20some%20women%20experience%20abuse,is%20first%20abused%20during%20pregnancy.
- National Coalition Against Domestic Violence. (n.d.). Domestic violence and children. NCADV. Retrieved from: https://assets.speakcdn.com/assets/2497/dv_and_children.pdf
- National Coalition Against Domestic Violence (n.d.a,). Domestic violence and the black community. NCADV. Retrieved from: https://assets.speakcdn.com/assets/2497/dv_in_the_black_community.pdf
- National Coalition Against Domestic Violence (n.d.). Gender based violence in rural communities. NCADV. Retrieved from: https://assets.speakcdn.com/assets/2497/ncadv_fact_sheet_-_gbv_in_rural_communities.pdf
- National Coalition Against Domestic Violence. (n.d.b.). National statistics. NCADV. Retrieved from: https://ncadv.org/STATISTICS
- National Coalition Against Domestic Violence. (n.d.c.). Teen, campus, and dating violence. NCADV. Retrieved from:https://assets.speakcdn.com/assets/2497/dating_abuse_and_teen_violence_ncadv.pdf
- National Coalition Against Domestic Violence. (2018). Domestic violence and the LGBTQ community. NCADV. Retrieved from: https://ncadv.org/blog/posts/domestic-violence-and-the-lgbtq-community
- National Coalition Against Domestic Violence. (2022). Abuse in later life. NCADV. Retrieved from: https://assets.speakcdn.com/assets/2497/abuse_in_later_life.pdf
- Office of Violence Against Women (OVW). (2023, March). What is domestic violence? Department of Justice. Retrieved from: https://www.justice.gov/ovw/domestic-violence
- Sanctuary for Families. (2022, July). The link between disability and domestic violence. Retrieved from: https://sanctuaryforfamilies.org/disability-domestic-violence/
- Screening for Intimate Partner Violence, Elder Abuse, and Abuse of Vulnerable Adults: Recommendation Statement. (2019). American family physician, 99(10), .
- Taylor, V. (2022). When immigration becomes a tool in intimate partner violence. Retrieved from: https://bwjp.org/when-immigration-becomes-a-tool-in-intimate-partner-violence/?gclid=CjwKCAjwq4imBhBQEiwA9Nx1BjBxfxvBc9Mei36iutSPnSVwzwBynoEOQ5BDngmoCCcNu-pF7qY2xxoC2vkQAvD_BwE
- United States Department of Justice. (2000). Full Report of the Prevalence, Incidence, and Consequences of Violence Against Women. Retrieved from: https://www.ncjrs.gov/pdffiles1/nij/183781.pdf
- Women’s Rights Project. (n.d.). Domestic violence and homelessness. American Civil Liberties Union. Retrieved from: https://www.aclu.org/sites/default/files/pdfs/dvhomelessness032106.pdf
- Avert. (2019). History of HIV and AIDS overview. Retrieved from: https://www.avert.org/professionals/history-hiv-aids/overview
- Bhatti, A. B., Usman, M., & Kandi, V. (2016). Current Scenario of HIV/AIDS, Treatment Options, and Major Challenges with Compliance to Antiretroviral Therapy. Cureus, 8(3), e515. https://doi.org/10.7759/cureus.515
- Centers for Disease Control. (2016). Today‘s HIV/AIDS epidemic. Retrieved from: https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf
- Centers for Disease Control. (2019). HIV cost effectiveness. Retrieved from: https://www.cdc.gov/hiv/programresources/guidance/costeffectiveness/index.html.
- Centers for Disease Control. (2020). Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV. Retrieved from: https://www.cdc.gov/hiv/pdf/risk/art/cdc-hiv-art-viral-suppression.pdf
- Centers for Disease Control. (2020). HIV. Retrieved from: https://www.cdc.gov/hiv/basics/whatishiv.html
- Centers for Disease Control. (2020). Sharing your test results. Retrieved from: https://www.cdc.gov/hiv/basics/hiv-testing/sharing-test-results.html/
- Currier, J. S., & Havlir, D. V. (2017). CROI 2017: Complications and Comorbidities of HIV Disease and Its Treatment. Topics in antiviral medicine, 25(2), 77–83.
- HIV.gov. (2020). U.S. statistics. Retrieved from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
- Nursing Times. (2020). HIV: epidemiology, pathophysiology, and transmission. Retrieved from: https://www.nursingtimes.net/clinical-archive/immunology/hiv-1-epidemiology-pathophysiology-and-transmission-15-06-2020/
- Vaillant, A. J. and Guilick, P. G. (2020). HIV disease current practice. Statpearls. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK534860/.
- Barry, M. J., Nicholson, W. K., Silverstein, M., Chelmow, D., Coker, T. R., Davis, E. M., … & US Preventive Services Task Force. (2023). Preexposure prophylaxis to prevent acquisition of HIV: US preventive services task force recommendation statement. JAMA, 330(8), 736-745.
- Centers for Disease Control and Prevention. (2023). Ending the HIV Epidemic in the U.S. (EHE). (https://www.cdc.gov/endhiv/index.html)
- Centers for Disease Control and Prevention. (2023). Estimated HIV incidence and prevalence in the United States, 2017–2021. HIV Surveillance Supplemental Report, 2023; 28 (No.3). http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2023. Accessed [11/05/2023].
- Center for Disease Control and Prevention (2019). HIV risk behaviors. HIV risk and prevention. https://www.cdc.gov/hiv/risk/estimates/riskbehaviors.html
- Centers for Disease Control and Prevention, & US Public Health Service. (2021). Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 Update: a clinical practice guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
- National Institute of Health. (2021). Preexposure prophylaxis. HIV prevention. https://hivinfo.nih.gov/understanding-hiv/fact-sheets/pre-exposure-prophylaxis-prep
- UNAIDS. (2023). Global HIV and AIDS statistics – Fact Sheet. https://www.unaids.org/en/resources/fact-sheet
- US Department of Health and Human Services. (2022). What is Ending the HIV Epidemic in the US? About Ending the HIV Epidemic in the US.
- US Department of Health & Human Services. U.S. Statistics (2022). Data and trends. https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics/
- US Food and Drug Administration. (2021). Apretude ® (Cabotegravir extended-release injection suspension) prescribing information 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/215499s000lbl.pdf
- US Food and Drug Administration. (2020). Descovy® (emtricitabine and tenofovir alafenamide) prescribing information 2019.
- US Food and Drug Administration. (2020). Truvada® (emtricitabine/tenofovir disoproxil fumarate) prescribing information. 2020.
- World Health Organization. (2023). HIV and AIDS. https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
- Pascarella, G., Rossi, M., Montella, E., Capasso, A., De Feo, G., Botti, G., Nardone, A., Montuori, P., Triassi, M., D’Auria, S., & Morabito, A. (2021). Risk analysis in healthcare organizations: Methodological framework and critical variables. Risk Management and Healthcare Policy, Volume 14, 2897–2911. https://doi.org/10.2147/rmhp.s309098
- Schreck, N. (2023, July 27). The Purpose of Risk Management in Healthcare | The Univ. of Scranton. The University of Scranton. https://elearning.scranton.edu/resources/article/purpose-of-risk-management-in-healthcare/
- McGowan, J., Wojahn, A., & Nicolini, J. R. (2023, August 23). Risk management event evaluation and responsibilities. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK559326/
- Haskins, J. (2022, June 29). 20 years of patient safety. AAMC. https://www.aamc.org/news/20-years-patient-safety
- Craig, M. (2024, March 29). Unraveling the theoretical concepts of risk: foundations and approaches. IIENSTITU. https://www.iienstitu.com/en/blog/unraveling-the-theoretical-concepts-of-risk-foundations-and-approaches
- The Joint Commission. (2024, February 2). The Joint Commission announces Sustainable Healthcare Certification for U.S. hospitals. The Joint Commission. https://www.jointcommission.org/resources/news-and-multimedia/news/2023/09/sustainable-healthcare-certification-for-us-hospitals/
- Vearrier, L., & Henderson, C. M. (2021). Utilitarian principlism as a framework for crisis healthcare ethics. HEC Forum (Print), 33(1–2), 45–60. https://doi.org/10.1007/s10730-020-09431-7
- Seixas, B. V., Dionne, F., & Mitton, C. (2021). Practices of decision making in priority setting and resource allocation: a scoping review and narrative synthesis of existing frameworks. Health Economics Review (Heidelberg), 11(1). https://doi.org/10.1186/s13561-020-00300-0
- Javaid, M., Haleem, A., Singh, R. P., Suman, R., & Rab, S. (2022). Significance of machine learning in healthcare: Features, pillars and applications. International Journal of Intelligent Networks, 3, 58–73. https://doi.org/10.1016/j.ijin.2022.05.002
- Reddy, P., Kurdziel, A., & Sanfilippo, L. (2019, August 9). Transformative healthcare growth through diversification. McKinsey & Company. https://www.mckinsey.com/industries/healthcare/our-insights/transformative-healthcare-growth-through-diversification
- Gurtu, A., & Johny, J. (2021). Supply Chain Risk Management: Literature Review. Risks, 9(1), 16. https://doi.org/10.3390/risks9010016
- Skelly, C. L., Cassagnol, M., & Munakomi, S. (2023, August 13). Adverse events. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK558963/
- Compliancy Group. (2023, September 18). The Cost of Non-Compliance in Healthcare: A Deep Dive into the Consequences. https://compliancy-group.com/the-cost-of-non-compliance-in-healthcare/
- Kadaei, M. (2024, February 23). Which of the following are internal factors that affect patient safety – Ambula Healthcare. Ambula Healthcare. https://www.ambula.io/which-of-the-following-are-internal-factors-that-affect-patient-safety/
- Healthcare financial risk factors and how to mitigate them. (2023, October 20). BDO. https://www.bdo.com/insights/industries/healthcare/healthcare-under-pressure-financial-risk-factors-and-steps-for-mitigating-them
- Safety Management – Hazard Identification and Assessment | Occupational Safety and Health Administration. (2023). https://www.osha.gov/safety-management/hazard-Identification
- Human Capital Risk Assessment: How to assess and manage the risks of your human resources – FasterCapital. (2023). FasterCapital. https://fastercapital.com/content/Human-Capital-Risk-Assessment–How-to-Assess-and-Manage-the-Risks-of-Your-Human-Resources.html
- Rodziewicz, T. L., Houseman, B., & Hipskind, J. E. (2023, May 2). Medical error reduction and Prevention. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK499956/
- Adverse events, near misses, and errors. (2022, March 30). PSNet. https://psnet.ahrq.gov/primer/adverse-events-near-misses-and-errors
- Operational Risk Management: Overview and Guide | AuditBoard. (2024). AuditBoard. https://www.auditboard.com/blog/operational-risk-management/
- Patient Safety Incident Response Framework – Leeds Teaching Hospitals NHS Trust. (2024, March 25). Leeds Teaching Hospitals NHS Trust. https://www.leedsth.nhs.uk/patients/support/patient-safety-incident-response-framework/
- Whistlehub. (2023, June 22). Reputational risk in healthcare. Whistlehub. https://whistlehub.com/blog/reputational-risk-in-healthcare
- Risk Retention Strategies: When Transfer Isn t the Answer – FasterCapital. (2023). FasterCapital. https://fastercapital.com/content/Risk-Retention-Strategies–When-Transfer-Isn-t-the-Answer.html
- Alder, S. (2024, February 19). What is Risk Management in Healthcare? HIPAA Journal. https://www.hipaajournal.com/risk-management-in-healthcare/
- Singh, G., Patel, R. H., & Boster, J. (2023, May 30). Root cause analysis and medical error prevention. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK570638/
- Addressing workplace violence and creating a safer workplace. (2023, October 31). PSNet. https://psnet.ahrq.gov/perspective/addressing-workplace-violence-and-creating-safer-workplace
- Sentinel event. (2024). The Joint Commission. https://www.jointcommission.org/resources/sentinel-event/
- Massachusetts Medical Society. (2018). What is risk management in healthcare? NEJM Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0197
- Alanazi, A. (2023). Clinicians’ perspectives on healthcare cybersecurity and cyber threats. Curēus. https://doi.org/10.7759/cureus.47026
- What are the Essential Techniques of Risk Management – Human Resources, Diversity and Inclusion | CSUF. (2024). https://hr.fullerton.edu/risk-management/information-and-document-requests/information-management/essential-techniques-of-risk-management.php
- Alhumaid, S., Mutair, A. A., Alawi, Z. A., Alsuliman, M., Ahmed, G. Y., Rabaan, A. A., Al‐Tawfiq, J. A., & Al‐Omari, A. (2021). Knowledge of infection prevention and control among healthcare workers and factors influencing compliance: a systematic review. Antimicrobial Resistance and Infection Control, 10(1). https://doi.org/10.1186/s13756-021-00957-0
- Policy approaches to reduce what commercial insurers pay for hospitals’ and physicians’ services. (2022, September 1). Congressional Budget Office. https://www.cbo.gov/publication/58541
- Young, M., & Smith, M. A. (2022, December 13). Standards and Evaluation of Healthcare Quality, Safety, and Person-Centered Care. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK576432/
- Lim, S. (2023, December 19). The importance of cyber liability insurance for healthcare providers — Malpractice insurance brokers | Medical professionals in California. Malpractice Insurance Brokers | Medical Professionals in California. https://calattendingphysicians.com/blog/the-importance-of-cyber-liability-insurance-for-healthcare-providers
- Leao, D. L. L., Cremers, H., Van Veghel, D., Pavlova, M., & Groot, W. (2023). The Impact of Value-Based Payment Models for Networks of Care and Transmural Care: A Systematic Literature review. Applied Health Economics and Health Policy. https://doi.org/10.1007/s40258-023-00790-z
- Da Silva Etges, A. P. B., Grenon, V., Lu, M., Cardoso, R. B., De Souza, J. S., Neto, F. J. K., & Félix, E. A. (2018). Development of an enterprise risk inventory for healthcare. BMC Health Services Research (Online), 18(1). https://doi.org/10.1186/s12913-018-3400-7
- World Health Organization: WHO. (2023, September 11). Patient safety. https://www.who.int/news-room/fact-sheets/detail/patient-safety
- Hüebner, C., & Fleßa, S. (2022). Strategic Management in Healthcare: a call for Long-Term and Systems-Thinking in an uncertain system. International Journal of Environmental Research and Public Health (Online), 19(14), 8617. https://doi.org/10.3390/ijerph19148617
- Salam, A., Awuah, W. A., Jiffry, R., Ng, J. C., Patel, H., Zahid, M. J., Mehta, A., Huang, H., Abdul‐Rahman, T., & Işık, A. (2023). The impact of natural disasters on healthcare and surgical services in low- and middle-income countries. Annals of Medicine and Surgery (London), 85(8), 3774–3777. https://doi.org/10.1097/ms9.0000000000001041
- Estimates of preventable hospital deaths are too high, new study shows. (2021, November 18). YaleNews. https://news.yale.edu/2020/01/28/estimates-preventable-hospital-deaths-are-too-high-new-study-shows
- Haas, E. J., Demich, B., & McGuire, J. W. (2020). Learning from Workers’ Near-miss Reports to Improve Organizational Management. Mining, Metallurgy & Exploration, 37(3), 873–885. https://doi.org/10.1007/s42461-020-00206-9
- Hankin, S. (2022, December 5). QIPS Terminology: Failure Mode and Effects Analysis (FMEA) vs. Root Cause Analysis (RCA). Newsroom. https://www.unmc.edu/newsroom/2022/12/05/qips-terminology-failure-mode-and-effects-analysis-fmea-vs-root-cause-analysis-rca/
- El-Awady, S. M. M. (2023). Overview of Failure Mode and Effects Analysis (FMEA): a patient safety tool. Global Journal on Quality and Safety in Healthcare, 6(1), 24–26. https://doi.org/10.36401/jqsh-23-x2
- Javaid, M., Haleem, A., Singh, R. P., & Suman, R. (2023). Towards insighting cybersecurity for healthcare domains: A comprehensive review of recent practices and trends. Cyber Security and Applications, 1, 100016. https://doi.org/10.1016/j.csa.2023.100016
- Enumah, S., Resnick, A. S., & Chang, D. C. (2022). Association of measured quality with financial health among U.S. hospitals. PloS One, 17(4), e0266696. https://doi.org/10.1371/journal.pone.0266696
- Akinleye, D. D., McNutt, L., Lazariu, V., & McLaughlin, C. C. (2019). Correlation between hospital finances and quality and safety of patient care. PloS One, 14(8), e0219124. https://doi.org/10.1371/journal.pone.0219124
- Vaismoradi, M., Tella, S., Logan, P., Khakurel, J., & Vizcaya-Moreno, M. F. (2020). Nurses’ Adherence to Patient Safety Principles: A Systematic review. International Journal of Environmental Research and Public Health (Online), 17(6), 2028. https://doi.org/10.3390/ijerph17062028
- Ramírez, E., Martín, A. L., Villán, Y., Lorente, M., Ojeda, J. T., Moro, M., Vara, C., Avenza, M., Domingo, M. J., Ávila, P., Asensio, M., Blázquez, J., Hernández, R., Frías, J., & Frank, A. (2018). Effectiveness and limitations of an incident-reporting system analyzed by local clinical safety leaders in a tertiary hospital. Medicine (Baltimore, Md.), 97(38), e12509. https://doi.org/10.1097/md.0000000000012509
- Patra, K. P., & De Jesus, O. (2023, March 29). Sentinel event. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK564388/
- Knudsen, P., Herborg, H., Mortensen, A. R., Knudsen, M., & Hellebek, A. (2007, August 29). Preventing medication errors in community pharmacy: root-cause analysis of transcription errors. PSNet. https://psnet.ahrq.gov/issue/preventing-medication-errors-community-pharmacy-root-cause-analysis-transcription-errors
- Jhugursing, M., Dimmock, V., & Mulchandani, H. (2017). Error and root cause analysis. BJA Education (Print), 17(10), 323–333. https://doi.org/10.1093/bjaed/mkx019
- Mardawi, G., & Rajendram, R. (2021). Investigation of medication safety incidents using root cause analysis and action. Global Journal on Quality and Safety in Healthcare (Online), 4(1), 50–52. https://doi.org/10.36401/jqsh-20-x9
- Revising TeamSTEPPS: The Evolution of Patient Safety Teamwork training. (2024, February 28). PSNet. https://psnet.ahrq.gov/perspective/revising-teamstepps-evolution-patient-safety-teamwork-training
- Blazin, L., Sitthi‐Amorn, J., Hoffman, J. M., & Burlison, J. D. (2020). Improving Patient Handoffs and Transitions through Adaptation and Implementation of I-PASS Across Multiple Handoff Settings. Pediatric Quality & Safety, 5(4), e323. https://doi.org/10.1097/pq9.0000000000000323
- Willassen, E. T., Jacobsen, I. L. S., & Tveiten, S. (2018). Safe Surgery Checklist, Patient Safety, Teamwork, and Responsibility—Coequal Demands? A focus group study. Global Qualitative Nursing Research, 5, 233339361876407. https://doi.org/10.1177/2333393618764070
- Lin, H., Wu, D., Cheng, S., Chen, C., Wang, M., & Cheng, C. (2020). Association between Electronic Medical Records and Healthcare Quality. Medicine, 99(31), e21182. https://doi.org/10.1097/md.0000000000021182
- Rights, O. F. C. (2022, December 23). Patient Safety and Quality Improvement Act of 2005 Statute and Rule. HHS.gov. https://www.hhs.gov/hipaa/for-professionals/patient-safety/statute-and-rule/index.html
- Ferdosi, M., Rezayatmand, R., & Taleghani, Y. M. (2020). Risk Management in Executive Levels of Healthcare Organizations: Insights from a Scoping Review (2018) Risk Management and Healthcare Policy, Volume 13, 215–243. https://doi.org/10.2147/rmhp.s231712
- Centers for Disease Control and Prevention (CDC) (2022a). Suicide data and Statistics. NCHS Data Brief. Number 433, March 2022. Retrieved from https://www.cdc.gov/suicide/suicide-data-statistics.html
- National Institute of Mental Health (NIMH): https://www.nimh.nih.gov
- Centers for Disease Control and Prevention (2022b). Facts about Suicide. Retrieved from https://www.cdc.gov/suicide/facts/index.html#:~:text=Suicide%20is%20death%20caused%20by,suicide%20or%20protect%20against%20it.
- National Vital Statistics System. NVSS Vital Statistics Rapid Release: Provisional Numbers and Rates of Suicide by Month and Demographic Characteristics: United States, 2020.
- Substance Abuse and Mental Health Services Administration. SAMHSA (2021). Key substance uses and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/report/suicidal-thoughts-and-behavior-33-metropolitan-statistical-areas-update-2013-2015
- Nevada Coalition for the Prevention of Suicide (2020). Suicide Facts and Figures. Retrieved from https://nvsuicideprevention.org/facts-about-suicide/
- Harmer B, Lee S, Duong TVH, Saadabadi A. Suicidal Ideation. 2022 May 18. In: StatPearls Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33351435.
- Stene-Larsen K, Reneflot A. Contact with primary and mental health care prior to suicide: A systematic review of the literature from 2000 to 2017. Scand J Public Health. 2019 Feb;47(1):9-17.
- Warden S, Spiwak R, Sareen J, Bolton JM. The SAD PERSONS scale for suicide risk assessment: a systematic review. Arch Suicide Res. 2014;18(4):313-26.
- Merriam-Webster dictionary. nd. Culture defined. Retrieved from https://www.merriam-webster.com/dictionary/culture
- Clay, R. (2018). The cultural distinctions in whether, when, and how people engage in suicidal behavior. American Psychology Today. Vol 49, No. 6, p. 28. Retrieved from https://www.apa.org/monitor/2018/06/ce-corner#:~:text=While%20Asian%2D%20and%20Pacific%20Islander,groups%20as%20well%2C%20Odafe%20adds.
- Chu, J., Khoury, O., Johnson, M. Bahn, F., Bongar, B., and Goldblum, P. (2017). An Empirical Model and Ethnic Differences in Cultural Meanings Via Motives for Suicide. Journal of Clinical Psychology. Vol 73, Issue 10, pp. 1343-1359. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/jclp.22425
- Pierre JM. Culturally sanctioned suicide: Euthanasia, seppuku, and terrorist martyrdom. World J Psychiatry. 2015 Mar 22;5(1):4-14. doi: 10.5498/wjp. v5. i1.4. PMID: 25815251; PMCID: PMC4369548.
- Simes, D., Ian Shochet, Kate Murray, Isobel G. Sands. (2022) A Systematic Review of Qualitative Research of the Experiences of Young People and their Caregivers Affected by Suicidality and Self-harm: Implications for Family-Based Treatment. Adolescent Research Review 7:2, pages 211-233. Retrieved from https://www.tandfonline.com/doi/citedby/10.1080/13811118.2017.1304305?scroll=top&needAccess=true
- Tran, K., Joel, Y., Wong, K., Oakley, O., Brownson, C., Drum, D., Awad, G., and Wang, M. (2015) Suicidal Asian American College Students’ Perceptions of Protective Factors: A Qualitative Study, Death Studies, 39:8, 500-507. Retrieved from https://www.tandfonline.com/doi/full/10.1080/07481187.2014.970299
- LaFromboise, T., Malik, D., Saima, S. Zane, N., Guillermo, B., Leong, F. (2016). Evidence-based psychological practice with ethnic minorities: Culturally informed research and clinical strategies., (pp. 223-245). Washington, DC, US: American Psychological Association, xvi, pp. 330.
- Ivey-Stephenson, A. Z., Crosby, A. E., Jack, S. P. D., Haileyesus, T., & Kresnow-Sedacca, M. (2017). Suicide trends among and within urbanization levels by sex, race/ethnicity, age group, and mechanism of death – United States, 2001-2015. MMWR Surveillance Summaries, 66(18), 1–9.
- Rehkopf, D. H. & Buka, S. L. (2006). The association between suicide and the socioeconomic characteristics of geographical areas: A systematic review. Psychological Medicine, 36, 145–57.
- Turvey, C., Stromquist, A., Kelly, K., Zwerling, C., & Merchant, J. (2002). Financial loss and suicidal ideation in a rural community sample. Acta Psychiatrica Scandinavica, 106(5), 373–80.
- Mathew A, Saradamma R, Krishnapillai V, Muthubeevi SB. Exploring the Family factors associated with Suicide Attempts among Adolescents and Young Adults: A Qualitative Study. Indian J Psychol Med. 2021 Mar;43(2):113-118. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8313455/#bibr10-0253717620957113
- Lasrado RA, Chantler K, Jasani R, et al. Structuring roles, and gender identities within families explaining suicidal behavior in South India. Crisis, 2016; 37(3): 205–211.
- Macalli M, Tournier M, Galéra C, et al. Perceived parental support in childhood and adolescence and suicidal ideation in young adults: a cross-sectional analysis of the I-Share study. BMC Psychiatry, 2018; 18(1): 373.
- Brådvik L. Suicide Risk and Mental Disorders. Int J Environ Res Public Health. 2018 Sep 17;15(9):2028. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6165520/
- Chu, J., Khoury, O., Johnson, M. Bahn, F., Bongar, B., and Goldblum, P. (2017). An Empirical Model and Ethnic Differences in Cultural Meanings Via Motives for Suicide. Journal of Clinical Psychology. Vol 73, Issue 10, pp. 1343-1359.
- Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/jclp.22425
- National Institute of Mental Health “Major Depression”, 2017. Retrieved from https://www.dbsalliance.org/education/depression/statistics/
- O’Connor DB, Green JA, Ferguson E, O’Carroll RE, O’Connor RC. Cortisol reactivity and suicidal behavior: Investigating the role of hypothalamic-pituitary-adrenal axis responses to stress in suicide attempters and ideators. Psych neuroendocrinology. 2017 Jan; 75:183-191.
- Suzuki H, Ohgidani M, Kuwano N, Chrétien F, Lorin de la Grandmaison G, Onaya M, Tominaga I, Setoyama D, Kang D, Mimura M, Kanba S, Kato TA. Suicide and Microglia: Recent Findings and Future Perspectives Based on Human Studies. Front Cell Neurosci. 2019; 13:31.
- De Berardis D, Fornaro M, Valchera A, Cavuto M, Perna G, Di Nicola M, Serafini G, Carano A, Pompili M, Vellante F, Orsolini L, Fiengo A, Ventriglio A, Yong-Ku K, Martinotti G, Di Giannantonio M, Tomasetti C. Eradicating Suicide at Its Roots: Preclinical Bases and Clinical Evidence of the Efficacy of Ketamine in the Treatment of Suicidal Behaviors. Int J Mol Sci. 2018 Sep 23;19(10)
- Hernández-Díaz Y, González-Castro TB, Tovilla-Zárate CA, Juárez-Rojop IE, López-Narváez ML, Pérez-Hernández N, Rodríguez-Pérez JM, Genis-Mendoza AD. Association between FKBP5 polymorphisms and depressive disorders or suicidal behavior: A systematic review and meta-analysis study. Psychiatry Res. 2019 Jan; 271:658-668.
- Biddle, N. Ellen, L, Reddy, K. (2020). Suicide and Self-harm monitoring. Australian Institute of Health and Welfare. Retrieved from https://www.aihw.gov.au/suicide-self-harm-monitoring/research-information/releases
- Ivey-Stephenson A, Demissie Z, Crosby A, et al. (2020) Suicidal Ideation and Behaviors Among High School Students — Youth Risk Behavior Survey, United States, 2019. MMWR Suppl; 69(Suppl-1): 47–55. Retrieved from https://www.cdc.gov/mmwr/volumes/69/su/su6901a6.htm?s_cid=su6901a6_w
- Centers for Disease Control and Prevention (2022c), National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System. Feb 2022. Retrieved from http://wonder.cdc.gov/ucd-icd10.html
- Yosef Sokol, Molly Gromatsky, Emily R. Edwards, Ashley L. Greene, Joseph C. Geraci, Rachel E. Harris, Marianne Goodman (2021). The deadly gap: Understanding suicide among veterans transitioning out of the military,Psychiatry Research, vol 300. Retrieved from https://www.sciencedirect.com/science/article/pii/S0165178121001724
- Veterans Affairs. (nd). From Science to Practice: Understanding the Role of Geography in Suicide Risk. Retrieved from https://www.mentalhealth.va.gov/suicide_prevention/docs/Literature_Review_FSTP_Geography_FINAL_508_8-19-2019.pdf
- American Psychiatric Association Assessment and Management of Risk for Suicide Working Group (2013). Practice Guidelines, American Journal of Psychiatry. 2013 p. 22. Retrieved from https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2015.1720501
- National Alliance on Mental Illness (2020). Risk of Suicide. Retrieved from https://www.nami.org/About-Mental-Illness/Common-with-Mental-Illness/Risk-of-Suicide
- Ulfvebrand, S., Norring, A., Hogdahl, L. & von Hausswolff-Juhlin, Y. (2015). Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Research, 230(2), 294-299.
- Damone, A. L., Joham, A. E., Loxton, D., Earnest, A., Teede, H. J., & Moran, L. J. (2018). Depression, anxiety, and perceived stress in women with and without PCOS: A community-based study. Psychological Medicine, 49(09), 1510-1520. doi:10.1017/s0033291718002076
- U.S. Department of Veterans Affairs. Mental Health Report. (2020). Retrieved from https://www.mentalhealth.va.gov/suicide_prevention/data.asp
- Joint Commission on Accreditation. Sentinel Event New Alert Focuses on Suicide Ideation. Jt Comm Perspect. 2016 Apr;36(4):12-17.
- Naherniak B, Bhaskaran J, Sareen J, Wang Y, Bolton JM. Ambivalence About Living and the Risk for Future Suicide Attempts: A Longitudinal Analysis. Prim Care Companion CNS Disord. 2019 Mar 07;21(2)
- Dube P, Kurt K, Bair MJ, Theobald D, Williams LS. The p4 screener: evaluation of a brief measure for assessing potential suicide risk in 2 randomized effectiveness trials of primary care and oncology patients. Prim Care Companion J Clin Psychiatry. 2010;12(6): PCC.10m00978. doi: 10.4088/PCC.10m00978blu. PMID: 21494337; PMCID: PMC3067996. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3067996/#:~:text=The%20P4%20screener%20assesses%20suicide,completing%20suicide%2C%20and%20preventive%20factors.
- Simon, G., Rutter, C., Peterson, D. Oliver, M., Whiteside, U., Operskalski, B., and Ludman, E. (2013). Does Response on the PHQ–9 Depression Questionnaire Predict Subsequent Suicide Attempt or Suicide Death? Retrieved from http://ps.psychiatryonline.org/doi/pdf/10.1176/appi.ps.201200587.
- Posner, K., Brent, D., Lucas, C., gould, M., Stanley, B., Brown, G., Fisher, P., Zelazny, J., Burke, A., Oquendo, M., and Mann, J. (2010). Columbia-Suicide Severity Rating Scale. 2010.
- Retrieved from https://cssrs.columbia.edu/wp-content/uploads/C-SSRS_Pediatric-SLC_11.14.16.pdf
- Heisel MJ, Flett GL. Investigating the psychometric properties of the Geriatric Suicide Ideation Scale (GSIS) among community-residing older adults. Aging Ment Health. 2016;20(2):208-21.
- Buchman-Schmitt JM, Chu C, Michaels MS, Hames JL, Silva C, Hagan CR, Ribeiro JD, Selby EA, Joiner TE. The role of stressful life events preceding death by suicide: Evidence from two samples of suicide decedents. Psychiatry Res. 2017 Oct; 256:345-352.
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. 2017 Feb;143(2):187-232.
- Klonsky ED, May AM, Saffer BY. Suicide, Suicide Attempts, and Suicidal Ideation. Annu Rev Clin Psychol. 2016; 12:307-30.
- Chappell PB, Stewart M, Alphs L, DiCesare F, DuBrava S, Harkavy-Friedman J, Lim P, Ratcliffe S, Silverman MM, Targum SD, Marder SR. Assessment of Suicidal Ideation and Behavior: Report of the International Society for CNS Clinical Trials and Methodology Consensus Meeting. J Clin Psychiatry. 2017 Jun;78(6): e638-e647.
- de Beurs DP, Fokkema M, de Groot MH, de Keijser J, Kerkhof AJ. Longitudinal measurement invariance of the Beck Scale for Suicide Ideation. Psychiatry Res. 2015 Feb 28;225(3):368-73.
- Harris KM, Lello OD, Willcox CH (March 2017). “Reevaluating suicidal behaviors: Comparing assessment methods to improve risk evaluations”. Journal of Psychopathology and Behavioral Assessment. 39: 128–139.
- MN Department of Health. Suicidal Ideation Risk Assessment (2019). Retrieved from https://www.health.state.mn.us/people/syringe/suicide.pdf
- Murray D. “Suicide Risk Assessment Doesn’t Work”. www.scientificamerican.com. Retrieved from https://www.scientificamerican.com/article/suicide-risk-assessment-doesnt-work/
- McCullumsmith C. Laying the groundwork for standardized assessment of suicidal behavior. J Clin Psychiatry. 2015 Oct;76(10): e1333-5.
- Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, Keyes KM, Hasin DS, Grant BF, Blanco C. Estimating risk for suicide attempt: are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. J Affect Disord. 2011 Nov;134(1-3):327-32.
- Dueweke AR, Bridges AJ. Suicide interventions in primary care: A selective review of the evidence. Fam Syst Health. 2018 Sep;36(3):289-302.
- O’Brien KHM, Fuxman S, Humm L, Tirone N, Pires WJ, Cole A, Goldstein Grumet J. Suicide risk assessment training using an online virtual patient simulation. Mhealth. 2019 Aug 28; 5:31.
- Mospan CM, Hess R, Blackwelder R, Grover S, Dula C. A two-year review of suicide ideation assessments among medical, nursing, and pharmacy students. J Interprof Care. 2017 Jul;31(4):537-539.
- Berman AL. Risk Factors Proximate to Suicide and Suicide Risk Assessment in the Context of Denied Suicide Ideation. Suicide Life Threat Behav. 2018 Jun;48(3):340-352.
- Kee, C. (2018). Here’s what happens when you call into a Suicide Prevention Hotline” BuzzFeed. Retrieved from https://www.buzzfeednews.com/article/carolinekee/what-happens-when-you-call-suicide-hotline
- Vasile C. CBT and medication in depression (Review). Exp Ther Med. 2020 Oct;20(4):3513-3516. doi: 10.3892/etm.2020.9014. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7464866/
- American Psychiatric Association Assessment and Management of Risk for Suicide Working Group (2013). Practice Guidelines, American Journal of Psychiatry. 2013 p. 22. Retrieved from https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2015.1720501
- Becker Bogusz, G. (2020). Health Insurers Still Don’t Cover Mental Health Treatment. NAMI.
- Retrieved from https://www.nami.org/blogs/nami-blog/march-2020/health-insurers-still-don-t-adequately-cover-mental-health-treatment
- Robins, C., Chapman, A., (2004). Dialetical Behavior Therapy Current Status. Journal of Personality Disorders. Retrieved from https://d1wqtxts1xzle7.cloudfront.net/79041854/Dialectical_Behavior_Therapy_Current_Sta20220118-23522-g6mlka-with-cover-page-v2.pdf?Expires=1665525856&Signature=PR0ww~eUf-4JhVlnDmyCYrkAJAmM3CeoHT58qhcxvnbnqKAmsaXPyHltoYe0pw1UgoTUFziOmJMbRLw-Gj2bHp~Xuvrdm2iEqa8XjuQPhvauIxaDJ1i5OVRuWM5GxOQT4EROOUGEHP9c~nG9OR2Akf7a28RfsMKES7Fer7k43WI2ds07DfC-TQpxHoILV4S6CFqXEtzG4YE9D3NotN2W59iKLaFvdj5Ebqr9joqX5vwdrBxkSJrMn-GFnqJsGGW5Q6fze1mnm0CJgAvb6aiDUSnRrrJctNOjCzyY4NpEh6p7fOsAGM88eyJjDMbaayF-MGWlZ6IWdinvZkjKe042Nw__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA
- Kavisto AJ, Magee, L., and Phalen, P. Firearm ownership and domestic versus nondomestic homicide in the U.S. Am J Prev Med. 2019; 57(3):311–20.
- Schaeffer KK. (2021). Facts about Americans and guns. Pew Research Center. Available from: https://www.pewresearch.org/fact-tank/2021/09/13/key-facts-about-americans-and-guns.
- Barry CL, Stone, E., and Crifasi, C., (2019). Trends in public opinion on US gun laws: Majorities of gun owners and non-gun owners support a range of measures. Health Aff (Millwood); 38(10):1727–34.
- Pisani, A. and Hinkson, J. (2020). More than Referrals: The Role of Primary Care in Suicide Prevention. American Foundation of Suicide Prevention. Retrieved from https://afsp.org/story/more-than-referrals-the-role-of-primary-care-in-suicide-prevention
- Bilsen J. Suicide and Youth: Risk Factors. Front Psychiatry. 2018 Oct 30; 9:540. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6218408/
- Dong, E., Du, H, and Gardner, L., (2020). An interactive web-based dashboard to track COVID-19 in real time. Lancet Infectious Disease. 20:533-4.
- Torchinsky, R. (2022). Nearly half of LGBTQ youth seriously considered suicide, survey finds. NPR News. Retrieved from https://www.npr.org/2022/05/05/1096920693/lgbtq-youth-thoughts-of-suicide-trevor-project-survey
- Lynch, F.L., Peterson, E.L., Lu, C.Y. (2020). Substance use disorders and risk of suicide in a general US population: a case control study. Addict Sci Clin Pract 15, 14 (2020). Retrieved from https://doi.org/10.1186/s13722-020-0181-1
- McCullumsmith C. Laying the groundwork for standardized assessment of suicidal behavior. J Clin Psychiatry. 2015 Oct;76(10): e1333-5.
- Clay, R. (2018). The cultural distinctions in whether, when, and how people engage in suicidal behavior. American Psychology Today. Vol 49, No. 6, p. 28. Retrieved from https://www.apa.org/monitor/2018/06/ce-corner#:~:text=While%20Asian%2D%20and%20Pacific%20Islander,groups%20as%20well%2C%20Odafe%20adds
- Vibrant Health (2021). 988 and the National Suicide Prevention Lifeline. Retrieved from https://www.vibrant.org/wp-content/uploads/2020/07/988_two_pager_2021-2.pdf
- Commonwealth Fund (2020). New International Report on Healthcare: US Suicide Rate Highest Among Wealthy Nations. Retrieved from https://www.commonwealthfund.org/press-release/2020/new-international-report-health-care-us-suicide-rate-highest-among-wealthy
- Awan S, Diwan MN, Aamir A, Allahuddin Z, Irfan M, Carano A, Vellante F, Ventriglio A, Fornaro M, Valchera A, Pettorruso M, Martinotti G, Di Giannantonio M, Ullah I, De Berardis D. Suicide in Healthcare Workers: Determinants, Challenges, and the Impact of COVID-19. Front Psychiatry. 2022 Feb 3;12:792925. doi: 10.3389/fpsyt.2021.792925. PMID: 35185638; PMCID: PMC8850721.
- Gursahani K, Char D, Wilson MP, Poirier RF. Emergency Department Management of Suicidal Ideation: Challenges, Misperceptions, and Hope. Mo Med. 2022 Sep-Oct;119(5):437-443. PMID: 36337996; PMCID: PMC9616452.Nordstrom K, Berlin JS,
- Nash SS, Shah SB, Schmelzer NA, Worley LLM. Boarding of Mentally Ill Patients in Emergency Departments: American Psychiatric Association Resource Document. West J Emerg Med. 2019;20(5):690–695. Published 2019 Jul 22.
- Wiler JL, Brown NA, Chanmugam AS, Enguidanos ER, Farley HL, Greenberg RD, et al. Care of the Psychiatric Patient in the Emergency Department-A Review of the Literature. American College of Emergency Physicians website. https://www.acep.org/globalassets/uploads/uploaded-files/acep/clinical-and-practice-management/resources/mental-health-and-substance-abuse/psychiatric-patient-carein-the-ed-2014.pdf.
- Centers for Disease Control and Prevention (CDC) (2022a). Suicide data and Statistics. NCHS Data Brief. Number 433, March 2022. Retrieved from https://www.cdc.gov/suicide/suicide-data-statistics.html
- National Institute of Mental Health (NIMH): https://www.nimh.nih.gov
- Centers for Disease Control and Prevention (2022b). Facts about Suicide. Retrieved from https://www.cdc.gov/suicide/facts/index.html#:~:text=Suicide%20is%20death%20caused%20by,suicide%20or%20protect%20against%20it.
- National Vital Statistics System. NVSS Vital Statistics Rapid Release: Provisional Numbers and Rates of Suicide by Month and Demographic Characteristics: United States, 2020.
- Substance Abuse and Mental Health Services Administration. SAMHSA (2021). Key substance uses and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/report/suicidal-thoughts-and-behavior-33-metropolitan-statistical-areas-update-2013-2015
- Nevada Coalition for the Prevention of Suicide (2020). Suicide Facts and Figures. Retrieved from https://nvsuicideprevention.org/facts-about-suicide/
- Harmer B, Lee S, Duong TVH, Saadabadi A. Suicidal Ideation. 2022 May 18. In: StatPearls Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33351435.
- Stene-Larsen K, Reneflot A. Contact with primary and mental health care prior to suicide: A systematic review of the literature from 2000 to 2017. Scand J Public Health. 2019 Feb;47(1):9-17.
- Warden S, Spiwak R, Sareen J, Bolton JM. The SAD PERSONS scale for suicide risk assessment: a systematic review. Arch Suicide Res. 2014;18(4):313-26.
- Merriam-Webster dictionary. nd. Culture defined. Retrieved from https://www.merriam-webster.com/dictionary/culture
- Clay, R. (2018). The cultural distinctions in whether, when, and how people engage in suicidal behavior. American Psychology Today. Vol 49, No. 6, p. 28. Retrieved from https://www.apa.org/monitor/2018/06/ce-corner#:~:text=While%20Asian%2D%20and%20Pacific%20Islander,groups%20as%20well%2C%20Odafe%20adds.
- Chu, J., Khoury, O., Johnson, M. Bahn, F., Bongar, B., and Goldblum, P. (2017). An Empirical Model and Ethnic Differences in Cultural Meanings Via Motives for Suicide. Journal of Clinical Psychology. Vol 73, Issue 10, pp. 1343-1359. Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/jclp.22425
- Pierre JM. Culturally sanctioned suicide: Euthanasia, seppuku, and terrorist martyrdom. World J Psychiatry. 2015 Mar 22;5(1):4-14. doi: 10.5498/wjp. v5. i1.4. PMID: 25815251; PMCID: PMC4369548.
- Simes, D., Ian Shochet, Kate Murray, Isobel G. Sands. (2022) A Systematic Review of Qualitative Research of the Experiences of Young People and their Caregivers Affected by Suicidality and Self-harm: Implications for Family-Based Treatment. Adolescent Research Review 7:2, pages 211-233. Retrieved from https://www.tandfonline.com/doi/citedby/10.1080/13811118.2017.1304305?scroll=top&needAccess=true
- Tran, K., Joel, Y., Wong, K., Oakley, O., Brownson, C., Drum, D., Awad, G., and Wang, M. (2015) Suicidal Asian American College Students’ Perceptions of Protective Factors: A Qualitative Study, Death Studies, 39:8, 500-507. Retrieved from https://www.tandfonline.com/doi/full/10.1080/07481187.2014.970299
- LaFromboise, T., Malik, D., Saima, S. Zane, N., Guillermo, B., Leong, F. (2016). Evidence-based psychological practice with ethnic minorities: Culturally informed research and clinical strategies., (pp. 223-245). Washington, DC, US: American Psychological Association, xvi, pp. 330.
- Ivey-Stephenson, A. Z., Crosby, A. E., Jack, S. P. D., Haileyesus, T., & Kresnow-Sedacca, M. (2017). Suicide trends among and within urbanization levels by sex, race/ethnicity, age group, and mechanism of death – United States, 2001-2015. MMWR Surveillance Summaries, 66(18), 1–9.
- Rehkopf, D. H. & Buka, S. L. (2006). The association between suicide and the socioeconomic characteristics of geographical areas: A systematic review. Psychological Medicine, 36, 145–57.
- Turvey, C., Stromquist, A., Kelly, K., Zwerling, C., & Merchant, J. (2002). Financial loss and suicidal ideation in a rural community sample. Acta Psychiatrica Scandinavica, 106(5), 373–80.
- Mathew A, Saradamma R, Krishnapillai V, Muthubeevi SB. Exploring the Family factors associated with Suicide Attempts among Adolescents and Young Adults: A Qualitative Study. Indian J Psychol Med. 2021 Mar;43(2):113-118. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8313455/#bibr10-0253717620957113
- Lasrado RA, Chantler K, Jasani R, et al. Structuring roles, and gender identities within families explaining suicidal behavior in South India. Crisis, 2016; 37(3): 205–211.
- Macalli M, Tournier M, Galéra C, et al. Perceived parental support in childhood and adolescence and suicidal ideation in young adults: a cross-sectional analysis of the I-Share study. BMC Psychiatry, 2018; 18(1): 373.
- Brådvik L. Suicide Risk and Mental Disorders. Int J Environ Res Public Health. 2018 Sep 17;15(9):2028. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6165520/
- Chu, J., Khoury, O., Johnson, M. Bahn, F., Bongar, B., and Goldblum, P. (2017). An Empirical Model and Ethnic Differences in Cultural Meanings Via Motives for Suicide. Journal of Clinical Psychology. Vol 73, Issue 10, pp. 1343-1359.
- Retrieved from https://onlinelibrary.wiley.com/doi/full/10.1002/jclp.22425
- National Institute of Mental Health “Major Depression”, 2017. Retrieved from https://www.dbsalliance.org/education/depression/statistics/
- O’Connor DB, Green JA, Ferguson E, O’Carroll RE, O’Connor RC. Cortisol reactivity and suicidal behavior: Investigating the role of hypothalamic-pituitary-adrenal axis responses to stress in suicide attempters and ideators. Psych neuroendocrinology. 2017 Jan; 75:183-191.
- Suzuki H, Ohgidani M, Kuwano N, Chrétien F, Lorin de la Grandmaison G, Onaya M, Tominaga I, Setoyama D, Kang D, Mimura M, Kanba S, Kato TA. Suicide and Microglia: Recent Findings and Future Perspectives Based on Human Studies. Front Cell Neurosci. 2019; 13:31.
- De Berardis D, Fornaro M, Valchera A, Cavuto M, Perna G, Di Nicola M, Serafini G, Carano A, Pompili M, Vellante F, Orsolini L, Fiengo A, Ventriglio A, Yong-Ku K, Martinotti G, Di Giannantonio M, Tomasetti C. Eradicating Suicide at Its Roots: Preclinical Bases and Clinical Evidence of the Efficacy of Ketamine in the Treatment of Suicidal Behaviors. Int J Mol Sci. 2018 Sep 23;19(10)
- Hernández-Díaz Y, González-Castro TB, Tovilla-Zárate CA, Juárez-Rojop IE, López-Narváez ML, Pérez-Hernández N, Rodríguez-Pérez JM, Genis-Mendoza AD. Association between FKBP5 polymorphisms and depressive disorders or suicidal behavior: A systematic review and meta-analysis study. Psychiatry Res. 2019 Jan; 271:658-668.
- Biddle, N. Ellen, L, Reddy, K. (2020). Suicide and Self-harm monitoring. Australian Institute of Health and Welfare. Retrieved from https://www.aihw.gov.au/suicide-self-harm-monitoring/research-information/releases
- Ivey-Stephenson A, Demissie Z, Crosby A, et al. (2020) Suicidal Ideation and Behaviors Among High School Students — Youth Risk Behavior Survey, United States, 2019. MMWR Suppl; 69(Suppl-1): 47–55. Retrieved from https://www.cdc.gov/mmwr/volumes/69/su/su6901a6.htm?s_cid=su6901a6_w
- Centers for Disease Control and Prevention (2022c), National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System. Feb 2022. Retrieved from http://wonder.cdc.gov/ucd-icd10.html
- Yosef Sokol, Molly Gromatsky, Emily R. Edwards, Ashley L. Greene, Joseph C. Geraci, Rachel E. Harris, Marianne Goodman (2021). The deadly gap: Understanding suicide among veterans transitioning out of the military,Psychiatry Research, vol 300. Retrieved from https://www.sciencedirect.com/science/article/pii/S0165178121001724
- Veterans Affairs. (nd). From Science to Practice: Understanding the Role of Geography in Suicide Risk. Retrieved from https://www.mentalhealth.va.gov/suicide_prevention/docs/Literature_Review_FSTP_Geography_FINAL_508_8-19-2019.pdf
- American Psychiatric Association Assessment and Management of Risk for Suicide Working Group (2013). Practice Guidelines, American Journal of Psychiatry. 2013 p. 22. Retrieved from https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2015.1720501
- National Alliance on Mental Illness (2020). Risk of Suicide. Retrieved from https://www.nami.org/About-Mental-Illness/Common-with-Mental-Illness/Risk-of-Suicide
- Ulfvebrand, S., Norring, A., Hogdahl, L. & von Hausswolff-Juhlin, Y. (2015). Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Research, 230(2), 294-299.
- Damone, A. L., Joham, A. E., Loxton, D., Earnest, A., Teede, H. J., & Moran, L. J. (2018). Depression, anxiety, and perceived stress in women with and without PCOS: A community-based study. Psychological Medicine, 49(09), 1510-1520. doi:10.1017/s0033291718002076
- U.S. Department of Veterans Affairs. Mental Health Report. (2020). Retrieved from https://www.mentalhealth.va.gov/suicide_prevention/data.asp
- Joint Commission on Accreditation. Sentinel Event New Alert Focuses on Suicide Ideation. Jt Comm Perspect. 2016 Apr;36(4):12-17.
- Naherniak B, Bhaskaran J, Sareen J, Wang Y, Bolton JM. Ambivalence About Living and the Risk for Future Suicide Attempts: A Longitudinal Analysis. Prim Care Companion CNS Disord. 2019 Mar 07;21(2)
- Dube P, Kurt K, Bair MJ, Theobald D, Williams LS. The p4 screener: evaluation of a brief measure for assessing potential suicide risk in 2 randomized effectiveness trials of primary care and oncology patients. Prim Care Companion J Clin Psychiatry. 2010;12(6): PCC.10m00978. doi: 10.4088/PCC.10m00978blu. PMID: 21494337; PMCID: PMC3067996. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3067996/#:~:text=The%20P4%20screener%20assesses%20suicide,completing%20suicide%2C%20and%20preventive%20factors.
- Simon, G., Rutter, C., Peterson, D. Oliver, M., Whiteside, U., Operskalski, B., and Ludman, E. (2013). Does Response on the PHQ–9 Depression Questionnaire Predict Subsequent Suicide Attempt or Suicide Death? Retrieved from http://ps.psychiatryonline.org/doi/pdf/10.1176/appi.ps.201200587.
- Posner, K., Brent, D., Lucas, C., gould, M., Stanley, B., Brown, G., Fisher, P., Zelazny, J., Burke, A., Oquendo, M., and Mann, J. (2010). Columbia-Suicide Severity Rating Scale. 2010.
- Retrieved from https://cssrs.columbia.edu/wp-content/uploads/C-SSRS_Pediatric-SLC_11.14.16.pdf
- Heisel MJ, Flett GL. Investigating the psychometric properties of the Geriatric Suicide Ideation Scale (GSIS) among community-residing older adults. Aging Ment Health. 2016;20(2):208-21.
- Buchman-Schmitt JM, Chu C, Michaels MS, Hames JL, Silva C, Hagan CR, Ribeiro JD, Selby EA, Joiner TE. The role of stressful life events preceding death by suicide: Evidence from two samples of suicide decedents. Psychiatry Res. 2017 Oct; 256:345-352.
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. 2017 Feb;143(2):187-232.
- Klonsky ED, May AM, Saffer BY. Suicide, Suicide Attempts, and Suicidal Ideation. Annu Rev Clin Psychol. 2016; 12:307-30.
- Chappell PB, Stewart M, Alphs L, DiCesare F, DuBrava S, Harkavy-Friedman J, Lim P, Ratcliffe S, Silverman MM, Targum SD, Marder SR. Assessment of Suicidal Ideation and Behavior: Report of the International Society for CNS Clinical Trials and Methodology Consensus Meeting. J Clin Psychiatry. 2017 Jun;78(6): e638-e647.
- de Beurs DP, Fokkema M, de Groot MH, de Keijser J, Kerkhof AJ. Longitudinal measurement invariance of the Beck Scale for Suicide Ideation. Psychiatry Res. 2015 Feb 28;225(3):368-73.
- Harris KM, Lello OD, Willcox CH (March 2017). “Reevaluating suicidal behaviors: Comparing assessment methods to improve risk evaluations”. Journal of Psychopathology and Behavioral Assessment. 39: 128–139.
- MN Department of Health. Suicidal Ideation Risk Assessment (2019). Retrieved from https://www.health.state.mn.us/people/syringe/suicide.pdf
- Murray D. “Suicide Risk Assessment Doesn’t Work”. www.scientificamerican.com. Retrieved from https://www.scientificamerican.com/article/suicide-risk-assessment-doesnt-work/
- McCullumsmith C. Laying the groundwork for standardized assessment of suicidal behavior. J Clin Psychiatry. 2015 Oct;76(10): e1333-5.
- Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, Keyes KM, Hasin DS, Grant BF, Blanco C. Estimating risk for suicide attempt: are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. J Affect Disord. 2011 Nov;134(1-3):327-32.
- Dueweke AR, Bridges AJ. Suicide interventions in primary care: A selective review of the evidence. Fam Syst Health. 2018 Sep;36(3):289-302.
- O’Brien KHM, Fuxman S, Humm L, Tirone N, Pires WJ, Cole A, Goldstein Grumet J. Suicide risk assessment training using an online virtual patient simulation. Mhealth. 2019 Aug 28; 5:31.
- Mospan CM, Hess R, Blackwelder R, Grover S, Dula C. A two-year review of suicide ideation assessments among medical, nursing, and pharmacy students. J Interprof Care. 2017 Jul;31(4):537-539.
- Berman AL. Risk Factors Proximate to Suicide and Suicide Risk Assessment in the Context of Denied Suicide Ideation. Suicide Life Threat Behav. 2018 Jun;48(3):340-352.
- Kee, C. (2018). Here’s what happens when you call into a Suicide Prevention Hotline” BuzzFeed. Retrieved from https://www.buzzfeednews.com/article/carolinekee/what-happens-when-you-call-suicide-hotline
- Vasile C. CBT and medication in depression (Review). Exp Ther Med. 2020 Oct;20(4):3513-3516. doi: 10.3892/etm.2020.9014. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7464866/
- American Psychiatric Association Assessment and Management of Risk for Suicide Working Group (2013). Practice Guidelines, American Journal of Psychiatry. 2013 p. 22. Retrieved from https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2015.1720501
- Becker Bogusz, G. (2020). Health Insurers Still Don’t Cover Mental Health Treatment. NAMI.
- Retrieved from https://www.nami.org/blogs/nami-blog/march-2020/health-insurers-still-don-t-adequately-cover-mental-health-treatment
- Robins, C., Chapman, A., (2004). Dialetical Behavior Therapy Current Status. Journal of Personality Disorders. Retrieved from https://d1wqtxts1xzle7.cloudfront.net/79041854/Dialectical_Behavior_Therapy_Current_Sta20220118-23522-g6mlka-with-cover-page-v2.pdf?Expires=1665525856&Signature=PR0ww~eUf-4JhVlnDmyCYrkAJAmM3CeoHT58qhcxvnbnqKAmsaXPyHltoYe0pw1UgoTUFziOmJMbRLw-Gj2bHp~Xuvrdm2iEqa8XjuQPhvauIxaDJ1i5OVRuWM5GxOQT4EROOUGEHP9c~nG9OR2Akf7a28RfsMKES7Fer7k43WI2ds07DfC-TQpxHoILV4S6CFqXEtzG4YE9D3NotN2W59iKLaFvdj5Ebqr9joqX5vwdrBxkSJrMn-GFnqJsGGW5Q6fze1mnm0CJgAvb6aiDUSnRrrJctNOjCzyY4NpEh6p7fOsAGM88eyJjDMbaayF-MGWlZ6IWdinvZkjKe042Nw__&Key-Pair-Id=APKAJLOHF5GGSLRBV4ZA
- Kavisto AJ, Magee, L., and Phalen, P. Firearm ownership and domestic versus nondomestic homicide in the U.S. Am J Prev Med. 2019; 57(3):311–20.
- Schaeffer KK. (2021). Facts about Americans and guns. Pew Research Center. Available from: https://www.pewresearch.org/fact-tank/2021/09/13/key-facts-about-americans-and-guns.
- Barry CL, Stone, E., and Crifasi, C., (2019). Trends in public opinion on US gun laws: Majorities of gun owners and non-gun owners support a range of measures. Health Aff (Millwood); 38(10):1727–34.
- Pisani, A. and Hinkson, J. (2020). More than Referrals: The Role of Primary Care in Suicide Prevention. American Foundation of Suicide Prevention. Retrieved from https://afsp.org/story/more-than-referrals-the-role-of-primary-care-in-suicide-prevention
- Bilsen J. Suicide and Youth: Risk Factors. Front Psychiatry. 2018 Oct 30; 9:540. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6218408/
- Dong, E., Du, H, and Gardner, L., (2020). An interactive web-based dashboard to track COVID-19 in real time. Lancet Infectious Disease. 20:533-4.
- Torchinsky, R. (2022). Nearly half of LGBTQ youth seriously considered suicide, survey finds. NPR News. Retrieved from https://www.npr.org/2022/05/05/1096920693/lgbtq-youth-thoughts-of-suicide-trevor-project-survey
- Lynch, F.L., Peterson, E.L., Lu, C.Y. (2020). Substance use disorders and risk of suicide in a general US population: a case control study. Addict Sci Clin Pract 15, 14 (2020). Retrieved from https://doi.org/10.1186/s13722-020-0181-1
- McCullumsmith C. Laying the groundwork for standardized assessment of suicidal behavior. J Clin Psychiatry. 2015 Oct;76(10): e1333-5.
- Clay, R. (2018). The cultural distinctions in whether, when, and how people engage in suicidal behavior. American Psychology Today. Vol 49, No. 6, p. 28. Retrieved from https://www.apa.org/monitor/2018/06/ce-corner#:~:text=While%20Asian%2D%20and%20Pacific%20Islander,groups%20as%20well%2C%20Odafe%20adds
- Vibrant Health (2021). 988 and the National Suicide Prevention Lifeline. Retrieved from https://www.vibrant.org/wp-content/uploads/2020/07/988_two_pager_2021-2.pdf
- Commonwealth Fund (2020). New International Report on Healthcare: US Suicide Rate Highest Among Wealthy Nations. Retrieved from https://www.commonwealthfund.org/press-release/2020/new-international-report-health-care-us-suicide-rate-highest-among-wealthy
- Awan S, Diwan MN, Aamir A, Allahuddin Z, Irfan M, Carano A, Vellante F, Ventriglio A, Fornaro M, Valchera A, Pettorruso M, Martinotti G, Di Giannantonio M, Ullah I, De Berardis D. Suicide in Healthcare Workers: Determinants, Challenges, and the Impact of COVID-19. Front Psychiatry. 2022 Feb 3;12:792925. doi: 10.3389/fpsyt.2021.792925. PMID: 35185638; PMCID: PMC8850721.
- Gursahani K, Char D, Wilson MP, Poirier RF. Emergency Department Management of Suicidal Ideation: Challenges, Misperceptions, and Hope. Mo Med. 2022 Sep-Oct;119(5):437-443. PMID: 36337996; PMCID: PMC9616452.Nordstrom K, Berlin JS,
- Nash SS, Shah SB, Schmelzer NA, Worley LLM. Boarding of Mentally Ill Patients in Emergency Departments: American Psychiatric Association Resource Document. West J Emerg Med. 2019;20(5):690–695. Published 2019 Jul 22.
- Wiler JL, Brown NA, Chanmugam AS, Enguidanos ER, Farley HL, Greenberg RD, et al. Care of the Psychiatric Patient in the Emergency Department-A Review of the Literature. American College of Emergency Physicians website. https://www.acep.org/globalassets/uploads/uploaded-files/acep/clinical-and-practice-management/resources/mental-health-and-substance-abuse/psychiatric-patient-carein-the-ed-2014.pdf.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
