Drains: Everything You Need to Know
Contact Hours: 2.5
Author(s):
Charmaine Robinson MSN-Ed, RN
Course Highlights
- In this course you will learn about drains, and why it is important for nurses to know best practices when handling them.
- You’ll also learn the basics of types of drains and drain management.
- You’ll leave this course with a broader understanding of troubleshooting drain problems, and risks associated with drain usage.
Introduction
Picture this: you walk into your hospital unit, fresh off a good night’s sleep. You find your client assignment and head over to get the report. Then, the outgoing nurse says something that makes your heart skip a beat. “This client has an abscess drain. You need to flush it every X hour(s), record the output every X hour(s), call the provider if __ happens…” Before long, your head is spinning, and then you realize you’ve been spelling ‘abscess’ incorrectly for who knows how long!
Drains can be intimidating, especially with little to no prior experience in drain management. They often come with a specific set of instructions that can be confusing. What’s worse, a client may suffer a serious delay in recovery if something goes wrong. Nobody wants to be the one to make that call to the provider about a malfunctioning drain. Fortunately, like anything else, managing drains becomes much easier with experience and a little education.
Types of Drains
A client may require drain placement for several reasons. Often, they are placed at the end of surgery or percutaneously to help eliminate any fluid that may accumulate within the wound [14]. A common type of surgical drain is the bulb drain. Certain organs, such as Foley catheters or nasogastric tubes, may require a drain to remove their contents. Drains may also be placed to help remove fluid or air from body cavities. A chest tube is a good example of this type of drain. Finally, if a client develops an abscess, a drain is often required to help remove the infected fluid more quickly.
Drains serve a particularly important purpose (other than driving the client and their nurses crazy). The accumulation of fluid in the wrong place can have a detrimental effect on the client’s health and healing [14]. Excess fluid in the surgical site can cause significant pain and injury to surrounding tissues and organs. It can also increase the chance of infection.
Medical drains can be divided into multiple categories: active versus passive, open versus closed, and surgical versus percutaneous.
Active vs. Passive Drains
Drains are often described as being active or passive. Passive drainage allows for gravity to help remove excess fluid without the use of pressure [5]. An example of a passive drain would be placing a urinary catheter to gravity or a Penrose drain. A Penrose drain (also called a “straight” or “open” drain) is a flat, ribbon-like tube that creates a passage from a wound to the open air, which allows excess fluid to flow outward (see image below) [5]. The area surrounding the opening is often lightly covered with gauze to collect fluid as it drains and must be changed when saturated.

Image 1. Penrose drain
Active drains use actual pressure, typically negative pressure, to help remove excess fluid from the body. Examples of active drainage systems include:
- Gastric drain: drains stomach acid or bile from the stomach; uses a gastric tube to decompress the stomach when clients have abdominal distention from bile buildup; often indicated for bowel obstruction; pressure is created by connecting one end of a suction hose to the gastric tube and the other end to a vacuum device
- Negative pressure wound vacuum system: drains exudate from wounds to promote wound healing; indicated for complex or non-healing wounds; pressure is created by connecting one end of a suction hose to a special wound dressing and the other end to a vacuum device (more on this later) [20]
- Bulb drain: drains fluid from a body cavity to prevent pooling, which can lead to infection; often placed after surgical procedures to drain blood or fluid, keeping the surgical site clean; pressure is created by removing the stopper from the emptying port, compressing the bulb, then immediately re-plugging the stopper, which creates a low-pressure vacuum that pulls the fluid out of the body (see images below) [1][14]

Image 2. Bulb drain containing bloody fluid

Image 3. Bulb drain containing serous fluid
Open vs. Closed Drains
Drains can also be described as open or closed. An open system means that it is open to air. An example of an open system would be a Penrose drain, as described above. A closed drain, on the other hand, is not open to the environment. Rather, the draining fluid is contained within the system, and the collection bulb or bag is emptied occasionally as needed. A bulb drain or chest tube (see image below) is an example of a closed drain.
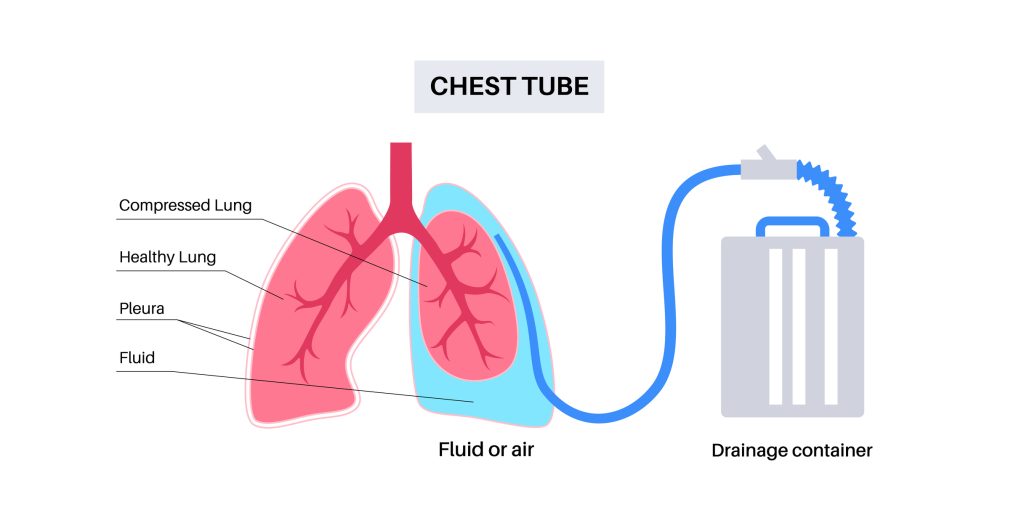
Image 4. Chest Tube Drainage System
Surgical vs. Percutaneous Drains
While not a technical classification, it is interesting to note how the drain is placed. Surgical drains are usually positioned in the operating room or, more rarely, at the bedside by the provider. The bulb drain is an example of a surgical drain. Drains may also be placed percutaneously. Percutaneous is an adjective that means “effected or performed through the skin” [13]. These drains are placed without surgical intervention. Rather, interventional radiologists use imaging, such as CT, ultrasound, or fluoroscopy to guide a needle into a fluid collection [19]. This technique is less invasive than surgery [8].
Examples of percutaneous drains include:
- Pleural catheter: drains fluid from the pleural space, for example, when a client has recurrent pleural effusion (see images below) [17]
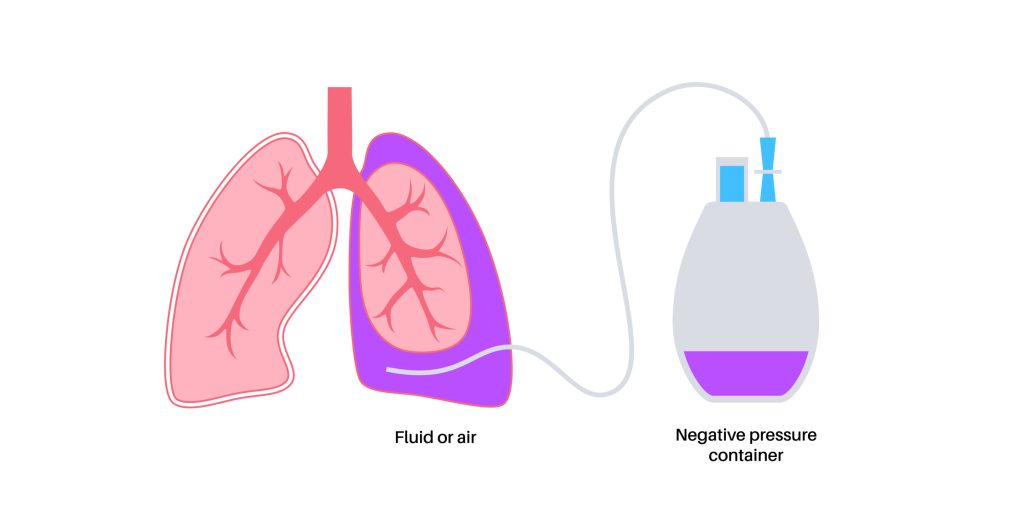
Image 5. Pleural Catheter Drainage System

Image 6. Pleural Catheter/Drain
- Peritoneal catheter: drains fluid from the peritoneal space when a client has recurrent ascites. (see image below) [6]
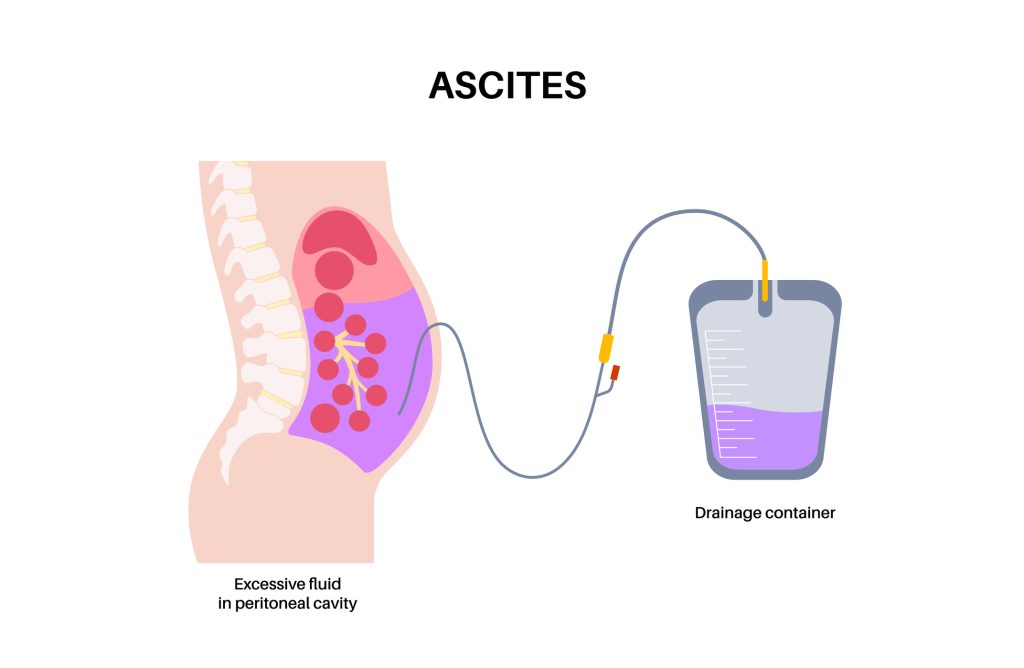
Image 7. Peritoneal Catheter Drainage System
- Abscess/hematoma drain: accordion drain that drains fluid from an abscess or blood from a hematoma (see image below)

Image 8. Accordion Drains
- Biliary drainage catheter: drains bile from the bile ducts, preventing backup to the liver, for example, when a client has a biliary obstruction (i.e., from gallstones or a tumor) [12]
- Nephrostomy tube: drains urine from the kidney, for example, when a client has a urinary obstruction such as a blood clot or kidney stone [4]
Before surgical or percutaneous drain insertion or any procedure, the client’s coagulation status and hemostasis risk must be evaluated [8][10].
Ask yourself...
- What are the advantages of open vs closed drainage systems
- Why might a provider place a passive drain in lieu of an active one?
- Have you encountered another type of percutaneous drain in your practice?
- What risks might be associated with percutaneous placements of drains?
Infections 101: A Brief History of Drains
Before the advent of antibiotics, the development of an abscess or postoperative infection was often a death sentence [15]. Thanks to advances in modern medicine, suffering clients now stand a chance. In certain situations, infections can be treated simply with a course of antibiotics. However, if there is any concern for developing sepsis, further intervention is needed [9].
Until the 1970s, the most effective (and only) way to treat infection and abscess was surgical intervention [15]. Surgeons would attempt to remove the infected material while striving for “directness, simplicity, and above all, avoidance of unnecessary contamination of uninvolved areas” [15]. Unfortunately for these clients, this meant that a second surgery was required to heal them from complications of their first surgery. Even with the addition of antibiotics, these situations were associated with significant morbidity and mortality [9].
Luckily, rapid technological advances allowed for developing a less invasive solution. The advent of fluoroscopy, ultrasounds, and especially CTs gave providers a tool to see inside the body without having to cut someone open. The first studies involving the use of medical imaging for percutaneous drain placement were published in the late 1970s [15]. Over the next several years, multiple studies reported success rates ranging from 60-80% using these new techniques [3].
Providers can drain up to three abscess/infection sites percutaneously [3]. Some studies report technical success of up to 90% with percutaneous drain placement, and it can offer immediate improvement in sepsis, with a return to hemodynamic stability within 1-2 days [11]. CT is considered the imaging modality of choice because of its ability to fully visualize the infection and surrounding structures and provide a pathway from the skin to the destination [11].
Ask yourself...
- What are the advantages of open vs closed drainage systems
- What types of drains are you most familiar with?
- Have you encountered a client with an abscess who needed a drain due to ineffective antibiotic therapy?
- When was the last time you encountered a client who had a surgical drainage of an abscess (incision and drainage)?
Client Considerations for Percutaneous Drain Placement
Not every infection or fluid collection requires percutaneous drain placement or even surgery. Thus, providers need to work together to determine the appropriate treatment for each client individually [14]. When a client is found to have an abscess, multiple providers may get involved, usually either a surgeon or interventional radiologist (sometimes both) and a clinical pharmacist if an infection is suspected or confirmed.
Providers must choose clients carefully, as ineffective or incomplete drainage of the infection can lead to significant morbidity and mortality [3]. For example, percutaneous drainage is sometimes avoided in clients with chest infections, such as empyema, abscess, and pleural effusion, because of the risk of pneumothorax [11]. Additionally, pyogenic and fungal abscesses in the lung parenchyma often resolve with more conservative management, namely through supportive care and antibiotics [11]. Pancreatic abscesses remain at high risk of treatment failure with percutaneous drain placement; thus, surgery is usually still the intervention of choice [11].
Many types of abscesses respond well to percutaneous drainage. Liver abscesses have a very low risk of complications with this type of drain placement, around 1-4% [11]. It is also very effective in managing infections related to visceral perforation, which may result from Crohn’s disease, prior operations, diverticulitis, and appendicitis [11]. Deep pelvic abscesses respond well to percutaneous drainage, although these can be more challenging and require careful planning because of the presence of nearby organs [11]. Percutaneous drainage is often considered for clients who are too ill for surgery, hoping it may improve sepsis and promote increased strength/rest [3]. It is also recommended for clients who have a good response to antibiotics and a low risk of mortality.
Ask yourself...
- Deciding who may benefit from a drain and who needs conservative therapy is difficult and nuanced. Who would you consult with on this subject?
- How has the increased use of medical drains altered the medical care and approach to managing abscesses?
- Do you find that surgeons consult with infectious disease providers for abscess treatment?
- Have you ever encountered a client with more than one drain at a time? How difficult was it to manage each drain?
Image-Guided Drainage: How Does it Work?
When first contemplating percutaneous drainage, providers must first decide which modality to use: fluoroscopy, ultrasound, or CT [8]. As mentioned previously, CT is most often used to guide drain placement because of its superior visualization.
The interventional radiologist will typically review any available imaging beforehand to plan the most appropriate route for drain placement. Care must be taken to avoid major vessels and other important structures [9][14]. To minimize the risk of complications, providers are advised to use the safest, most direct route and attempt placement in the most dependent part of the fluid collection to encourage effective drainage [9].
Once the client is properly positioned on the table, the provider will use the CT, ultrasound, or X-ray to guide the placement of a special needle, taking frequent pictures to monitor its progression from the skin through soft tissue and into the infection [8]. Once the needle is in place, a wire (termed “guide wire”) is passed through the needle into the fluid collection, and then the needle is removed, leaving only the wire in place (see image below).

Image 9. Guidewire for drain placement
Next, a drainage catheter is threaded across the wire to its final resting place. The tip of the catheter rests within the fluid collection. The drainage catheter contains holes to help fluid pass out of the body (see image below). Once the tube is in place, the wire is removed, and a drainage bag is attached. Throughout the procedure, images are taken to ensure correct placement. Clients are often given moderate sedation to make them more comfortable, but not in every case.
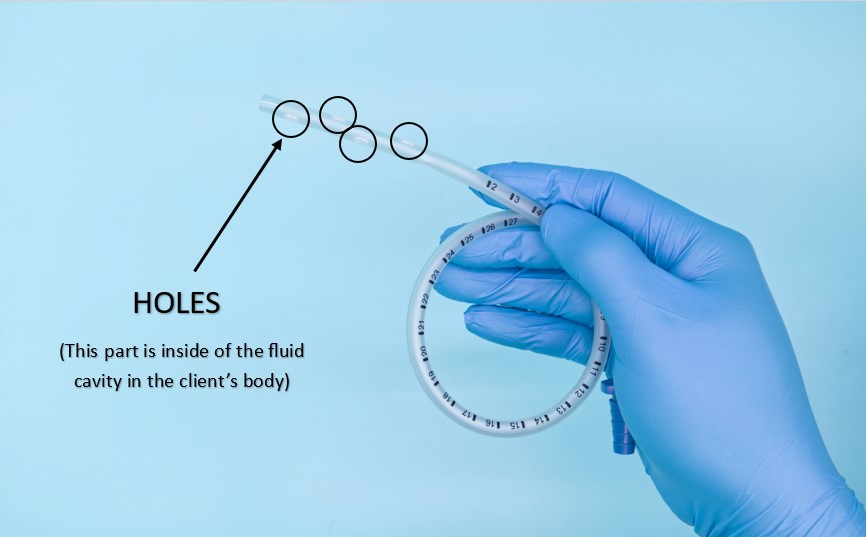
Image 10. Drain Tube
Ask yourself...
- Should medical therapy be initiated while awaiting intervention?
- Image guidance has revolutionized drain placement. In your experience, what is the most common imaging study to accompany drain placements?
- What are the advantages of surgical drains, and what is their current role?
- How might a provider determine which diagnostic scan is most appropriate for drain placement?
Drain Management
Care for the client with a drain can seem intimidating, but it doesn’t have to be. Often, the provider will write orders to guide nursing staff while caring for these clients. Drain management may also differ depending on the type of drain the client has. If there are no orders, it is reasonable to contact the provider who placed the drain for clarification.
Surgical Drains
As mentioned before, the bulb drain is an example of a surgical drain that is an active closed system drain. This means it uses low negative pressure to help remove excess fluid from a surgical wound, all of which is stored within the collection device [14].
When managing bulb drains, it is important to note the color of the drainage fluid. The fluid is typically bloody or purulent at first (see image below), but should gradually lighten to a light pink, clear, or yellow color [1][14]. Indications for removal may vary, but these drains generally remain in place until the daily output decreases to less than 30 ml [14].
Nurses will also be responsible for emptying the drain, observing the site, and documenting findings. The drain should be emptied no later than when it becomes half full, as it will lose suction and become ineffective [14]. Observe the insertion site for drainage and signs of infection. Be sure to keep the skin clean. These drains may also be sutured in place [1]. The drains should be further secured with medical adhesive or pinned to the client’s gown with a safety pin to secure the drains before mobilizing and to avoid accidental removal (more on this later).
Percutaneous Drains
Percutaneous drains usually look a little bit different. The interventional radiologist uses a special type of drainage tube that is also sometimes called a ‘pigtail’. These tubes do not always have to be sutured in place, for they may contain a string that, when pulled, curls the distal end of the tube, making it a bit harder to pull out. They are then usually adhered to the skin with a dressing.
Drains are often used for abscesses or infections, meaning fluid will be purulent and/or bloody. Check for any specific written instructions for drain management. Monitor the drain site regularly for signs of infection or drainage. Empty the drainage bag as directed or as needed and document findings. These drains may also use a collection bag that applies suction through negative pressure.
This is the case with drains like the pleural and peritoneal catheter drainage systems, which activate suction by using high negative pressure through a glass drainage bottle. Like bulb drains, the glass bottles should be emptied when half full [14]. These glass bottles are used for draining large amounts of fluids [18].
Typically, you do not have to empty high-pressure percutaneous drains because the old bottle can be removed and simply replaced with a new one. To change the bottle, start with preparing the new bottle. First, close all clamps on the bottle and its tubing (see images below) to prevent air from entering the system once connected [14].
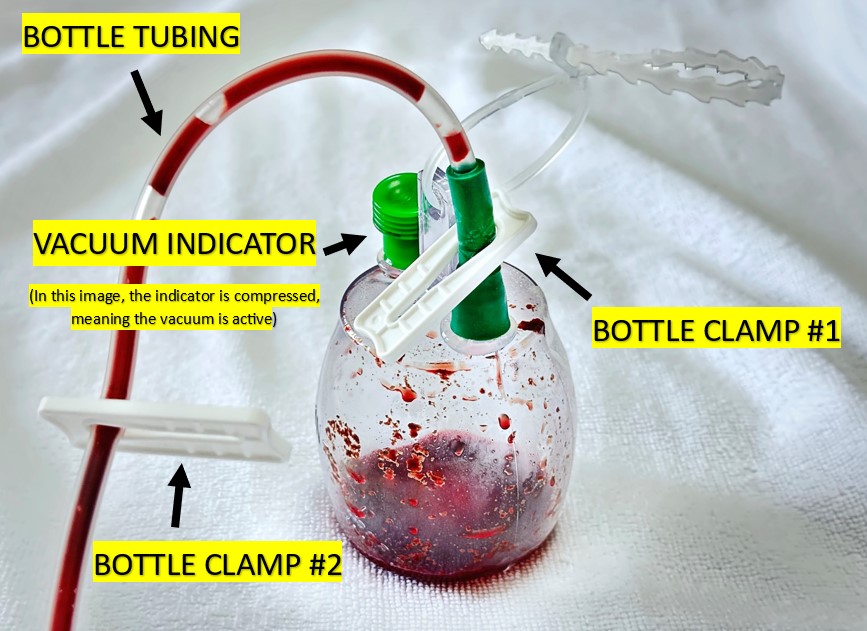
Image 11. High negative pressure glass drainage bottle for pleural and peritoneal catheter drainage systems
Once clamped, remove the old glass bottle by disconnecting the bottle tubing from the end of the client’s drain. A sterile technique is used to clean the end of the drain with an alcohol swab. Then, remove the cap from the new bottle tubing and attach it to the end of the drain [14]. Finally, all clamps on the bottle and its tubing are released [14].
Observe the fluid’s flow. The vacuum indicator (see image above) should be compressed if the suction is active [14][18]. Note fluid characteristics. Dispose of the old bottle per your facility’s protocol.
Some percutaneous drains, like abscess drains, are more likely to require flushing because the purulent drainage can be thick and pose a risk for drain occluding. They may be equipped with a three-way stopcock to allow for easy flushing (more on this later).
The following are colors to expect from the output of some percutaneous drains:
- Gastric drain: Depending on the location from which the fluid originates, fluid from a gastric drain can be in multiple colors. Stomach acid may be dark yellow, while bile is typically green or yellow. [12] If gastric bleeding is present, the fluid may be black.
- Pleural catheter: depending on the nature of the client’s condition, the pleural fluid can be of various colors, including pale, straw-colored, bloody, milky white, green, or even black (in cases of malignancy) [2][16].
- Peritoneal catheter: depending on the nature of the client’s condition, the pleural fluid can be of various colors, including yellow, pink, bloody, or milky white. [6]
- Biliary drain: Because this drain is specifically placed in the bile duct, the output is typically bile-colored (green or yellow) [12]
- Nephrostomy tube: while urine is normally yellow, nephrostomy tube output may also be pink in color, particularly when the tube is initially placed. Urine can also be bloody, but this is cause for concern [4]
Wound Drains
A negative pressure wound vacuum system (or “wound vac”) is used to drain exudate from wounds for optimal healing [20]. The wound vac uses intermittent suction to slowly pull drainage from wounds. The system comprises a vacuum device and a suction hose/catheter. The end of the hose attaches to an airtight sealed dressing placed directly over the client’s wound. The drainage is collected into a drainage canister on the device and emptied regularly. The wound vac system requires the wound dressing to remain intact at all times, as any air opening will inhibit the suctioning action of the device [14][20].
Wound vacs do not have a stopcock and do not require flushing. If a wound requires flushing, this must be performed in between wound vac dressing changes. Wound vac dressings may be changed at least every few days, depending on the provider’s order or facility’s protocol. When applying the wound vac, be sure to set the suction pressure on the device at the appropriate level ordered by the provider, as settings may be specific to each wound type [20].
When removing/changing the wound vac dressing, turn the machine off, and then carefully remove the soiled dressing from the client’s wound. Note the amount, color, consistency, and odor of the drainage, and monitor for signs of infection. Drainage from wound vacs can have a range of colors from milky white to bloody, depending on the wound’s condition. Dispose of the soiled dressing and tubing, and empty/ dispose of the canister as directed. Document findings. Wound vacs are often used for complex wounds, non-healing wounds, and wounds at risk for suboptimal healing, such as highly exudative wounds (or “overly wet” wounds) [20].
Ask yourself...
- You arrive on shift to find the vacuum indicator on a client’s peritoneal drain bottle compressed. What does this mean?
- Why might a nephrostomy tube output be bloody?
- Have you ever changed a wound vac dressing? If so, did you find it challenging to create a vacuum seal?
- Is a wound vac an active or passive drain
How to Flush a Drain Using a Three-way Stopcock
The first step is to review written orders and become familiar with policies regarding drain flushing. You may be required to have a provider’s order before you can flush a drain. If so, obtain the order, then gather some supplies: gloves, an alcohol pad, a “dead end” cap or clave, a clean pad/towel, and saline flush syringes. Prepare by applying gloves and laying out a clean towel or pad underneath to create a workspace and catch any drainage. Flushing a drain is usually painless, but advise clients that they may feel a little discomfort.
Take a look at the figure below. It is an example of a three-way stopcock. It has three different ports and a swivel “off switch.” Whichever direction the off switch is pointing closes that port so fluid cannot flow. In the example below, the switch is closed to the flush port, meaning that fluid cannot pass into the flush port, and the flush port cannot be flushed. An attached saline syringe will not flush, no matter how hard the plunger is pushed.
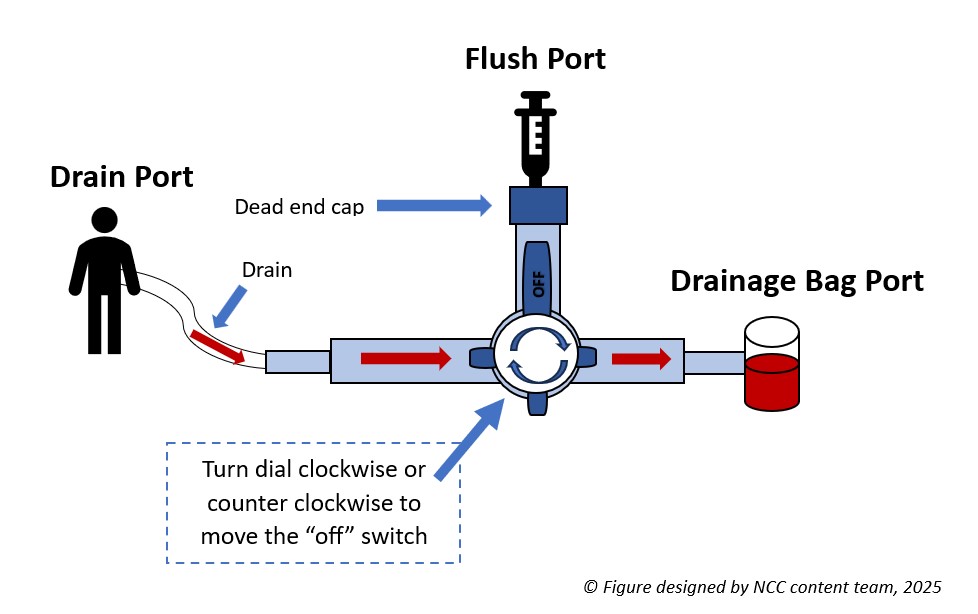
Figure 1. Three-way stopcock on drain
Step 1. Find the Flush Port
To flush the drain, find the flush port located on the stopcock. It should be pretty easy to spot, as it is usually the only port that does not have anything attached to it. The flush port should be capped with either a “dead-end” cap or a clave. If there is a dead-end cap, it will have to be removed. If a clave is present, the saline syringe can be screwed in directly (see images below).
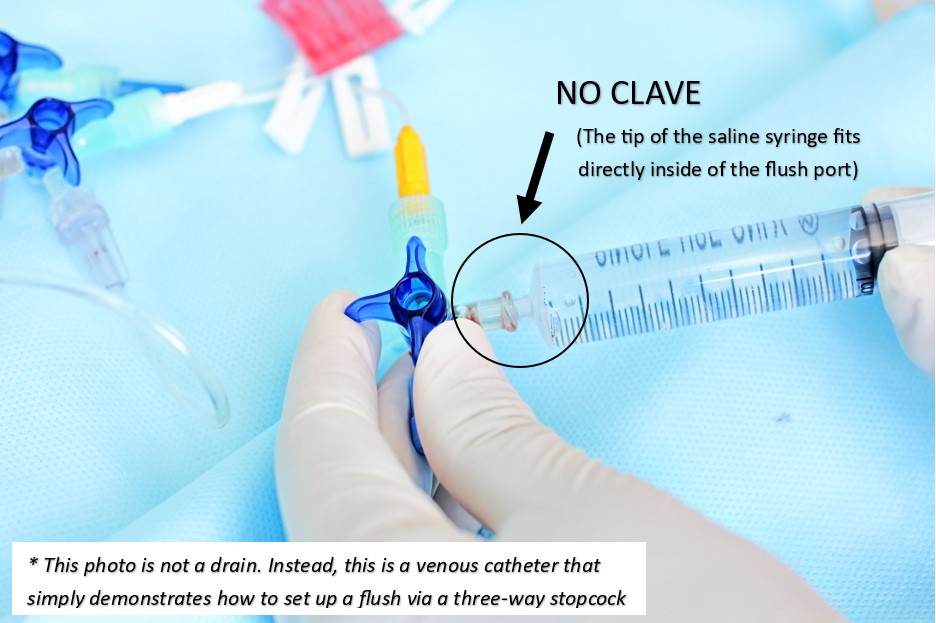
Image 13. Example of a three-way stopcock flush port without a clave
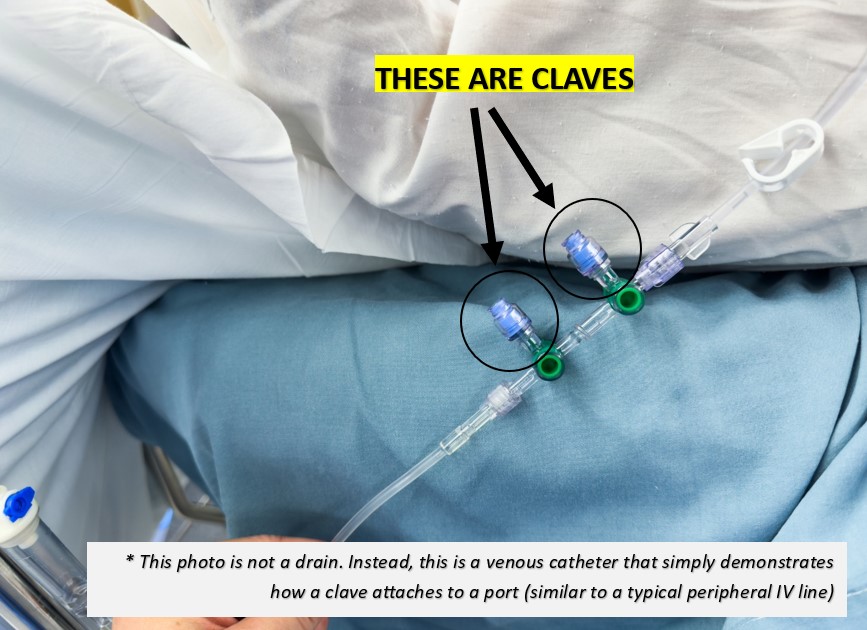
Image 14. Example of flush ports with claves
Step 2. Prepare the Flush Port
Next, if a dead-end cap is present, remove it. Wipe the flush port with an alcohol pad and attach a new, sterile clave, if available. Claves make future flushing much easier because the flush syringe can be attached directly. If a clave is already present, wipe it thoroughly with an alcohol pad before accessing it.
Step 3. Prepare the Saline
Attach a saline syringe to the flush port. 5-8 ml is usually plenty. If the ordering provider gave specific instructions on how much saline to infuse, follow the directions closely. When ready to flush, the off switch must be turned away from the flush port before flushing is possible.
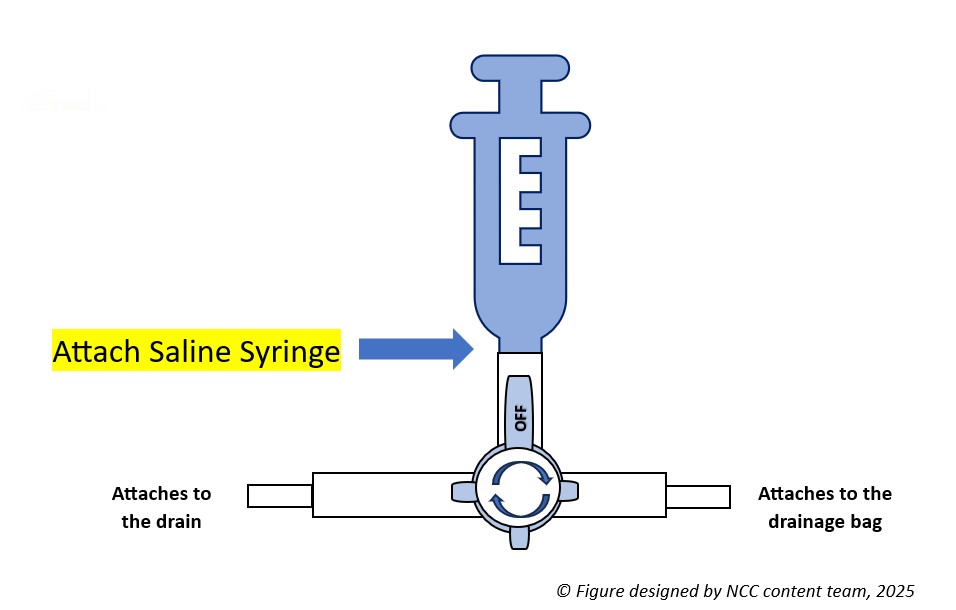
Figure 2. Preparing the saline prior to flushing the drain
Step 4. Flush the Drain
Saline can be flushed either into the drain or into the drainage bag, depending on which way the off switch is turned. To flush the drain, a nurse must direct the saline toward the client. This means the off switch needs to be turned toward the bag. The bag is now “off” and won’t get any flow, allowing saline to travel through the flush port and up the drain into the client.
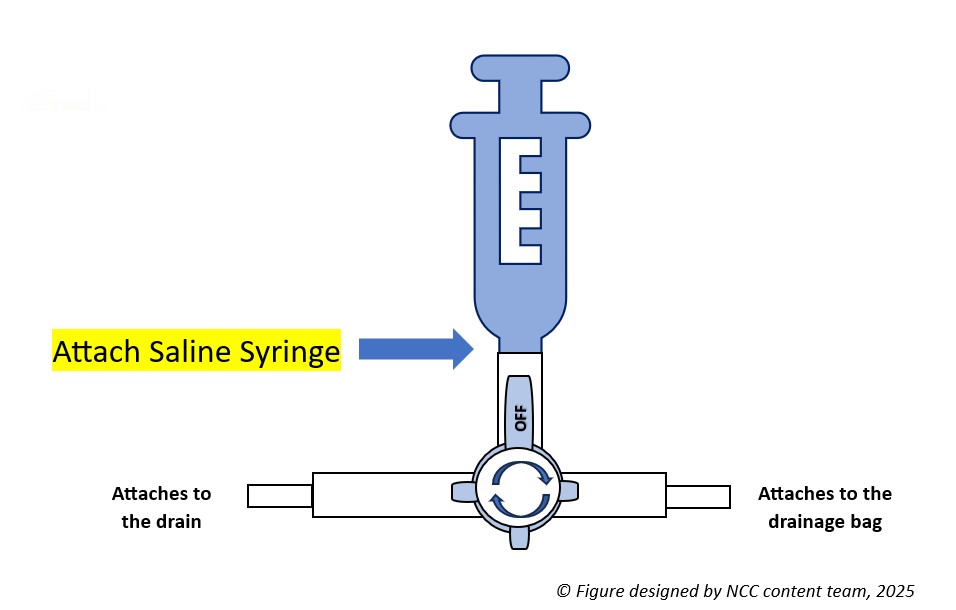
Figure 3. Flushing the drain
Once the saline is flushed, turn the off switch back to the flush port. This will reopen flow into the bag. The saline that was just infused should now travel freely through the drainage tube and into the bag. Observing this allows the nurse to know that the tube is draining correctly.

Figure 4. Allowing the flushed saline to flow into the drainage bag
Sometimes, the contents of an abscess can be thick or contain particles that can clog the tube leading to the bag. Thus, the drainage bag may also need to be flushed. Simply follow the steps listed above; instead of turning the off switch to the bag, it should be turned to the client. This will prevent flow from entering the drainage tube, leaving a pathway from the flush port into the drainage bag. The nurse should be able to see the saline traveling into the bag.
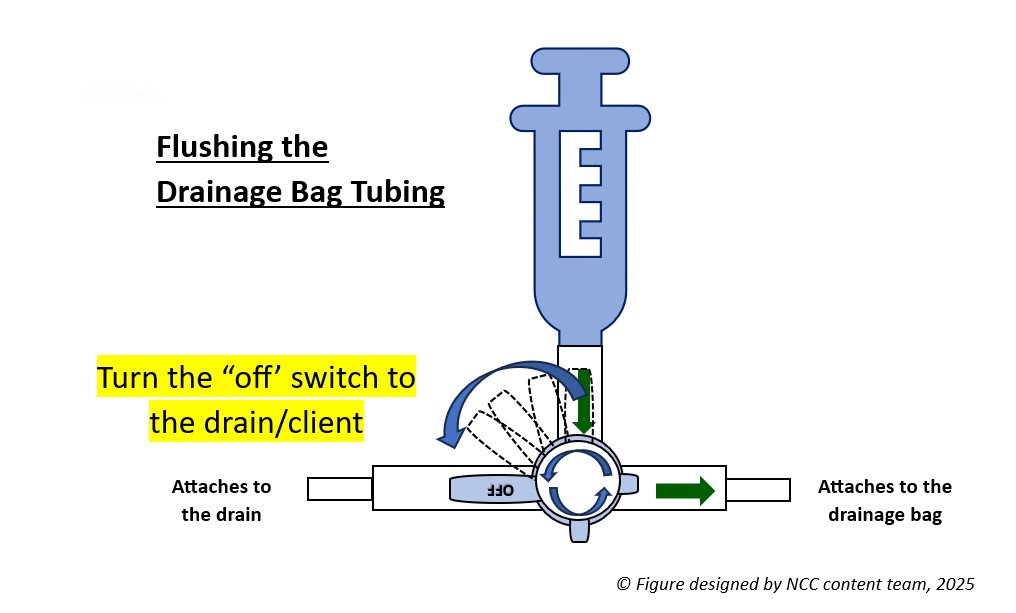
Figure 5. Flushing the drainage bag tubing
Once the bag is flushed, return the off switch to face the flush port. This allows for an open pathway from the drain into the bag.
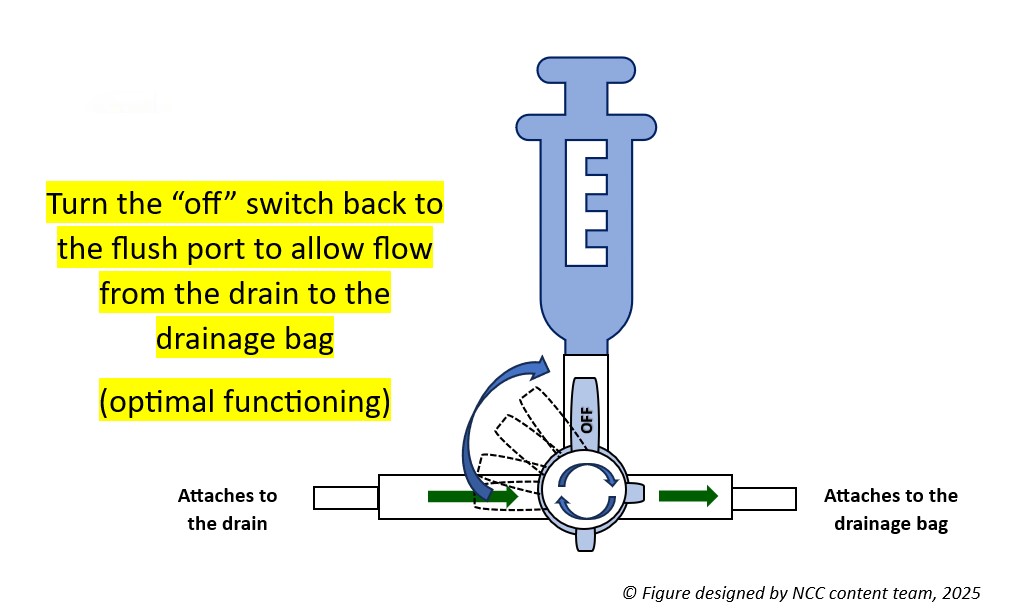
Figure 6. Returning the off switch to the flush port
Step 5. Assess the Drain
After flushing, it is important to note any client discomfort, as well as document how much saline was flushed. Before leaving the bedside, and always when assessing a client’s drain, ensure that the off switch on the stopcock is turned toward the flush port. This will allow drainage to flow seamlessly from the client into the bag.
*Note: Not all drains are meant to be flushed, especially those that do not contain a flush port and/or three-way stopcock. Never flush a drain without a provider’s order. Do not attempt to flush a drain if you suspect it has been pulled away from its original position.
Ask yourself...
- How was your last experience with drain care?
- What is the most common drain output color you witness in your practice?
- The client asks you to flush their drain. What should you confirm first before flushing the drain?
- What would happen if you forget to turn the off switch back to the flush port after flushing a drain with a three-way stopcock?
Properties of a Well-Functioning Drain
Since humans lack X-ray vision, the inner workings of a drain can seem a little mysterious. What is going on in there? How can a nurse know if the drain is doing what it is supposed to do? Repeat imaging (CT, ultrasound, etc.) is the best way to visualize how infections and abscesses change over time. However, it is costly and unnecessary to expose clients to extra radiation as a matter of curiosity.
One has to look at the drain itself to get some idea of how it is functioning. Even though drains may look different, they function in similar ways; thus, these considerations can be applied to both surgical and percutaneous drains.
Output
The hallmark of a well-functioning drain is output. A drain is designed to get fluid out of the body. Therefore, if the collection bag/bulb is capturing drainage fluid, this is a good indication that it is working correctly. Remember that the fluid is often bloody at first but should lighten over time. The drainage from an abscess may also be bloody at first before appearing purulent.
Skin Site Clean/Dry
The skin at the drain site should be kept clean and dry [14]. Minimal amounts of fluid may leak around the tube, causing crusting on the skin or a small amount of visible drainage. Depending on your facility’s protocol, this can be gently wiped away with clean gauze soaked with normal saline or warm, soapy water [14]. If a large amount of drainage is leaking from the skin and around the tube, this is not normal and should be addressed.
Apply a fresh, clean gauze at the site to protect the skin from breakdown [14]. This may be done by using a “drain sponge” (a piece of flat gauze that has a pre-made slit down one side, stopping at the center) (see image below). You can also fold a piece of gauze in half and lay it adjacent to the drain, then fold another piece of gauze and place it adjacent to the opposite side of the drain, then apply tape to the edges [14].
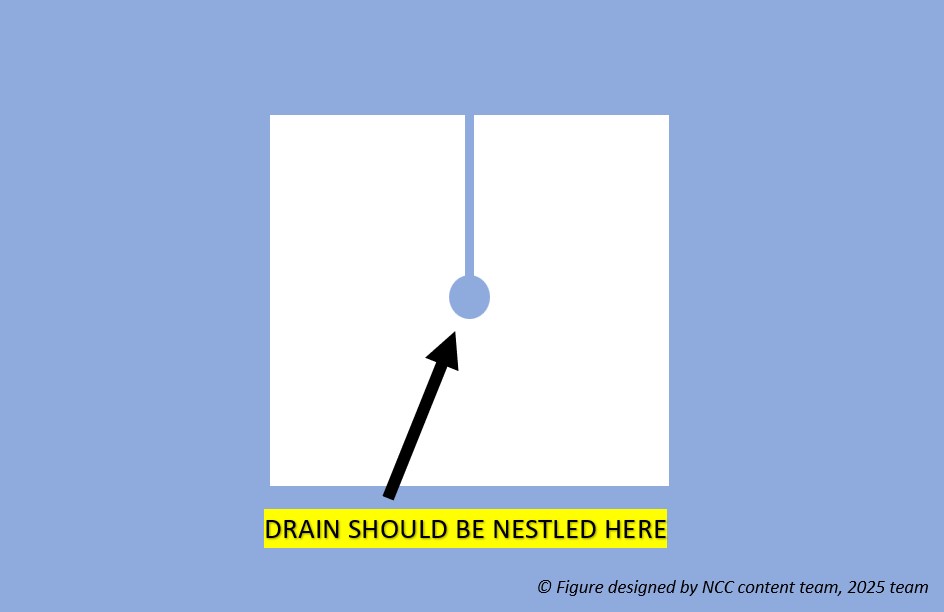
Figure 7. Example of drain sponge
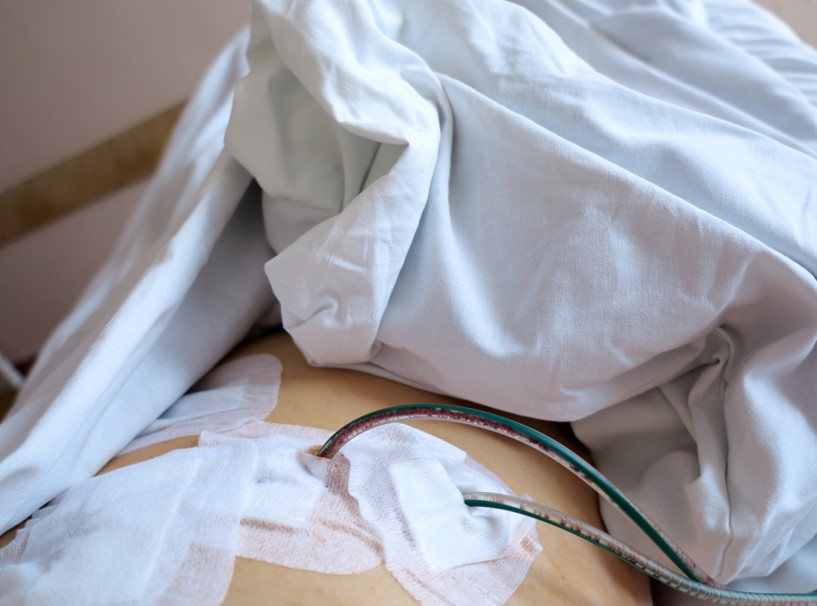
Image 14. Drain sites with dressings in place
Once the drain is removed, apply a piece of 4×4 gauze folded four ways over the puncture site, then apply tape [14]. Change the dressing as instructed.
Stopcock in the Proper Position
Ensuring that the three-way stopcock (if present) is in the proper position is essential for proper function. The off switch should be pointing to the flush port at all times unless the nurse is actively flushing the drain. Turning the off switch to the flush port prevents fluid from draining outside of the system and creates an open pathway from the drain into the drainage bag.
Active Suction
All active drains should be monitored closely to ensure that the bulb or accordion is adequately compressed [14]. Constant negative pressure must be maintained in order for the drain to work. To compress a bulb drain, use the “side-to-side” where the nurse compresses the bulb at its largest diameter (in the middle) with fingers and thumb to compress the bulb (see image below) [14]. The drain should be emptied when it is approximately 50 percent full to maintain the pressure within the bulb [14]. These drains may require frequent assessment and emptying, especially at first.

Image 2. Compressed bulb drain
Ask yourself...
- The client has just had a drain placed for abscess drainage. You notice the drain is emptying a small amount of bloody fluid. What is your next course of action?
- You assess a client’s drain insertion site to find a minimal amount of leakage. What is your next action?
- The surgeon plans to remove the drain. Once the drain is removed, which supplies might you anticipate will be needed at the insertion site?
- You assess a client’s drain to find the off-switch on the three-way stopcock facing towards the drain. The client is reporting pressure to the drain site. What is happening?
Is this Normal? Drain Troubleshooting
Unfortunately, drains can develop complications. Knowing what to look for is essential to identifying potential problems early. As mentioned previously, a delay in reporting or discovering a drain malfunction may cause delays in client healing. Luckily, the problems are fairly easy to spot if you know what to look for.
Bleeding
Some bleeding is normal. The act of placing a drain may cause bleeding from nearby small vessels [8]. This is usually self-limiting, so the nurse may note bleeding early after placement. The drainage should gradually lighten [14]. Prolonged bleeding or developing new bleeding warrants a prompt call to the provider.
Leaking
A leaky drain can be messy. If the source of the leak is not immediately known, the nurse should evaluate the drain, assess the tubing for cracks or holes, and ensure all connections are tight. Sometimes, the drainage bag/bulb may be punctured. If so, it is often easily replaced.
Leaking may occur because the drain is occluded or kinked [14]. Assess the tubing carefully for signs of obstruction. Flushing the drain can help dislodge occlusions. Again, never flush a drain without orders from the provider.
A drain may also leak at the skin. Minimal amounts of leakage can be expected because the drain creates a track for small amounts of fluid to escape. Moderate to severe leakage can cause skin breakdown and is not normal. It suggests that the drain is malfunctioning in some way, often due to an occlusion or displacement of the drain. Fluid travels the path of least resistance. If it can’t pass easily through the tube, it will find another way out. Notify the provider, who may order follow-up imaging, like a CT scan. If a percutaneous drain leaks, the client may have to be sent to interventional radiology for assessment and possible replacement.
No Output
Drain output may cease for two reasons: there is no more fluid, or the fluid cannot get out [14]. It is easy to assume the former. Yet, when faced with a drain without drainage, it is important to use critical thinking and common sense. Drainage usually tapers off, meaning it will drain a little less over time. An abrupt cessation of fluid could indicate a problem. Assess the drain for kinks or obstructions. If the drain is occluded, fluid may begin to leak around the tube at the skin.
Blood clots can obstruct fluid flow in a drain [14]. In this case, the surgeon may request the nurse to ‘milk the tube.’ This action may not be practiced in some facilities, so be sure to follow your facility’s protocol. Milking (also called “stripping”) refers to moving clots through the drain tube into the collection bulb [1]. Similar to squeezing the last bit of toothpaste from a tube of toothpaste, milking is done by holding the tube at the skin insertion site with the non-dominant hand, then using the dominant hand to gently squeeze the tube between the thumb and index finger while moving along the tube towards the collection bulb [14]. The nurse should have a provider’s order before attempting to milk a drain.
Carefully document drain output as dictated by the provider or facility protocol. If a concern arises, the provider should be notified.
Infection
Infection may occur with both surgical and percutaneous drains. It usually forms one of two ways: during initial drain placement or due to continued catheter presence [11]. Infection may form during initial placement if the needle punctures a non-target area (such as the colon) or from prolonged dilation, which is why the procedure should be completed in a timely manner [11]. Infections may also form on the skin if a drain is present for a long time [11].
The nurse should assess the drain site frequently. Signs of skin infection include redness, increased pain, swelling, fever, and purulent drainage [14]. Additionally, sepsis is always a concern for the client with an abscess or catheter/drain [7][8]. A client with sepsis will sicken very quickly, with a rapid increase in fever, chills, and rigors (back and forth between shivering/ feeling cold and feeling very hot due to fever) [7]. Vital sign monitoring is essential. If the nurse suspects a new infection of any kind or deterioration, notify the provider immediately.
Displacement
Living with a drain takes some getting used to. It can be easy for clients to forget it’s there. Sometimes, the tubing can become tangled up in the bed sheets or left behind when a client stands up. Although drains come equipped with reinforcements, such as a suture or dressing, to help keep the tubing in place, it is possible to pull the drain at least partially or sometimes completely out of the body.
If a drain is pulled out entirely, the nurse should cover the site with gauze to catch any drainage [14]. When drains are placed, they form a pathway from the abscess or infection to the skin. The tube’s job is to provide a conduit for the fluid to escape. If the tube is removed abruptly, that pathway still exists temporarily, so fluid will continue to leak out of the body without the tube. Do not attempt to put the tube back in, as it is no longer sterile. Simply notify the provider [14].
If the drain is only partially removed, reinforce the dressing as best as possible to maintain its current position and call the provider. Again, do not attempt to push the tubing back inside the client. The provider may order imaging to assess the drain’s location. Removal and/or replacement may be necessary.
Ask yourself...
- Managing drains can be intimidating at first. How would you troubleshoot the common issues listed here?
- What is one way you can tell a drain is working properly?
- On postoperative day two, your client’s bulb drain suddenly stops draining. What might be happening?
- Your client accidentally pulls their drain out when exiting the bed. Which action do you take first?
Client Education for Home Drain Care
Many drains require management by the clients themselves when discharged home. The surgeon may order the drain to be kept at home until the first post-discharge follow-up visit with the provider, during which the surgeon/provider will remove the drain themselves. While the client wears the drain at home, certain restrictions and precautions should be in place. It is the nurse’s responsibility to ensure the client returns to the provider’s office having followed all orders and directions regarding drain care. The following are educational tips for clients/families who wear drains at home.
Teach home drain care (such as keeping the site clean and dry and bathing restrictions). If possible, demonstrate how to empty the drain (for drains that must be emptied manually, such as bulb drains, pleural catheter drains, urinary catheters, or nephrostomy tubes) and ask the client/family for a returned demonstration.
Educate on infection prevention (such as handwashing before and after drain care), signs of infection, when to report findings to the provider, and what to do if the drain is accidentally pulled out. Inform never to remove sutures (if in place) or pull at the drain. Per your facility’s protocol, provide a drain pouch/bag, clip, ties, or pin to keep the drain in place while the client is at home and instruct on how to wear and protect the drain during movement and away-from-home activities (see images below).

Image 15. Bulb drain attached to client’s shirt with clip

Image 3. Bulb drain attached to client’s pants with a clip

Image 16. Bulb drain attached to client with a drain pouch
Provide a documentation form (per facility protocol) so clients/families can track how much drainage is emptied and how often [1]. The form may include a section for the client’s name, surgery name and date, and a table or list with entries for dates, times, and drainage amounts. Often, surgeons want to see that the client’s drainage is gradually lessening as the days progress, and this will determine when the drain should be removed [1][14].
A sudden decrease or increase in drainage may indicate a complication (such as a clot in the drainage system or bleeding), and clients should be informed to report this information to the provider right away [1][14]. Review the discharge order and confirm the amount that should be reported (for example, 500 ml/cc or more of drainage in 24 hours). Clients should also report any new blood in the drain or purulent or odorous drainage [1].

Image 17. Client emptying a bulb drain
Ask yourself...
- How often do you send clients home with drains?
- What do you suspect might be the most uncomfortable part of home drain management for clients and their families?
- How would you respond to a client who asks, “How long does my drain stay in place?”
- What signs/symptoms should a client report to the provider when managing a drain at home?
Frequently Asked Questions
What is an Accordion Drain?
An accordion drain removes fluid from a wound, abdomen, or lung space. The drain is comprised of a bag and vale that does not allow air or fluid to return back into the open space, wound, or lungs. An accordion drain is considered a closed drainage system, meaning that the drain is formed by tubes draining into a bag.
What is the difference in a Penrose Drain and a bulb drain?
Penrose Drain
A Penrose drain is a flat, ribbon-like tube that creates a passage from a wound. The drain is open to the air, allowing excess fluid to flow outward. The surrounding area on the outside of the body is covered in gauze to collect the fluid as it drains. The gauze must be changed frequently as it becomes saturated.
A Penrose drain is considered a passive and open draining system, meaning that it allows gravity to remove the fluid without the use of pressure.
Part of the Penrose drain is inside of the body cavity, with one or both ends coming out of the incision.
Although they are tubular, most of the drainage occurs outside of the tube, more so around it. It is used more as a “space-holder” to keep the tissue area open, allowing drainage to flow out.
Indications for a Penrose Drain:
- Wounds
- Infected area or abscess
- Underneath of skin graft
- Septic joints
- Tendon sheaths
NOT suitable for the abdominal or thoracic cavity
Bulb Drain
A bulb drain is considered an active and closed drainage system that uses negative pressure to remove excess fluid from the body. The pressure is created by the compression of the collection container (which looks like an egg), creating a low-pressure vacuum pulling fluid from the body. It is closed, meaning it is not open to the external environment; instead, the fluid is contained within a collection bulb.
The drain is sutured in place at the skin at the insertion site to promote stability and prevent wound breakdown and pulling. The drain is left in place until the drainage is minimal. If pulled too early, the client may be at risk of developing a seroma or hematoma.
Indications for a bulb drain:
- Superficial wounds where there is pre-existing or anticipated fluid build-up.
- Surgery if large amounts of drainage is expected, such as:
- plastic surgery
- breast surgery
- orthopedic procedures
- chest surgery or drainage
- infected cysts
- neurosurgery
- biliary surgery
- pancreatic surgery
How do you flush a bulb drain?
You should not flush a bulb drain without a stopcock. There is no indication for doing so, and it will only introduce additional bacteria into the drain.
If you must, and there is a stop-cock present, ensure it is done under sterile conditions with sterile saline.
What is a wound vac?
A wound vac is a negative-pressure wound vacuum system that uses intermittent suction to drain exudate from wounds slowly for optimal healing. The device comprises a vacuum device and a suction hose/catheter, which are attached to an airtight sealed dressing placed directly over the client’s wound. The wound vac system requires the dressing to remain intact at all times, as any air opening will inhibit the suctioning action of the device.
What are the main client teaching points for home drain care?
The main teaching points for drain care include infection prevention (including handwashing), what and when to report to the provider (i.e., signs of infection right way), restrictions and precautions (such as bathing limitations), and emptying of the drain with documentation of output. The goal of drain care is to ensure the client returns to the provider’s office having followed all orders and directions regarding drain care so the drain can be safely removed by the provider/surgeon.
Ask yourself...
- What is the primary difference between a Penrose drain and a bulb drain?
- Is it okay to flush a bulb drain?
- How might you know a drain can be flushed just by looking at it?
- What is one main teaching point for clients managing their drain at home?
Conclusion
This course is designed to help readers become more familiar with drains. They have all sorts of indications: to facilitate healing after surgery or infection, to assist with draining contents from affected organs, or to remove fluids that have accumulated in body cavities.
Drains are classified based on their function: open or closed, passive or active. Familiarity with the different types of drains gives the nurse a basic understanding of how they work- which is important because they can look very different, depending on the manufacturer.
In the old days, surgery and antibiotics were the only way to treat intra-abdominal infections. Significant advances in technology have allowed interventional radiologists to specialize in using medical imaging (CT, ultrasound, X-ray, and MRI) to place drains without making an incision. However, client selection is still very important, and providers must know which clients are good candidates for percutaneous drain placement and which are better off heading to the operating room.
This course is also designed to provide a basic understanding of drain management and troubleshooting. Nursing staff needs to understand how a drain is supposed to behave when it is functioning normally so that potential problems are easier to spot. When in doubt, consult the provider. Always be aware of any prescribing orders or policies that dictate drain management, as practices may vary from place to place.
As with anything else, the best way to become more comfortable with drains is to be around them!
Ask yourself...
- What is the difference between an active and passive drain?
- What differentiates surgical drains from percutaneous drains?
- What criteria must be met before a drain can be flushed?
- How might you know a drain is infected?
- What is one type of drain that uses a high negative-pressure glass drainage bottle?
References + Disclaimer
- American College of Surgeons. (n. d.). After your operation: Your surgical drain. https://www.facs.org/for-patients/the-day-of-your-surgery/breast-cancer-surgery/after-your-operation/your-surgical-drain/
- Bailey, J., & Florence, J. (2020) Cloudy pleural fluid on thoracentesis. Am Fam Physician, 102(5):307-308 https://www.aafp.org/pubs/afp/issues/2020/0901/p307.html
- Cinat, M. E., & Wilson, S. E. (2002). Determinants for successful percutaneous image-guided drainage of intra-abdominal abscess. Arch Surg., 137(7), 845-849. doi:10.1001/archsurg.137.7.845
- Cleveland Clinic. (2023, July 20). Nephrostomy tube. https://my.clevelandclinic.org/health/treatments/25141-nephrostomy-tube
- Cleveland Clinic. (2023, September 19). Penrose drain. https://my.clevelandclinic.org/health/articles/penrose-drain
- Digestive Disease and Surgery Institute, Cleveland Clinic. (n. d.). Cirrhotic ascites: Diagnosis. https://my.clevelandclinic.org/departments/digestive/medical-professionals/hepatology/cirrhosis-ascites#diagnosis-tab
- Fischer, J. (2024, April 2). Sepsis symptoms: Recognizing the need for urgent medical care. Harvard Health. https://www.health.harvard.edu/diseases-and-conditions/sepsis-symptoms-recognizing-the-need-for-urgent-medical-care
- Harclerode, T. P., & Gnugnoli, D. M. (2022, October 17). Percutaneous abscess drainage. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK564356/
- Hearns, W. C. (2012). Abscess drainage. Seminars in Interventional Radiology, 29(4), 325-336. doi 10.1055/s-0032-1330068
- Jover Pinillos, J. L., Ferrandis Comes, R., Zamudio Penko, D., Bermúdez López, M., Basora Macaya, M., & Colomina Soler, M. J. (2024). Preoperative coagulation tests: A narrative review of current guidelines. Revista espanola de anestesiologia y reanimacion, 71(10), 740–747. https://doi.org/10.1016/j.redare.2024.09.005
- Lorenz, J. & Thomas, J. L. (2006). Complications of percutaneous fluid collection. Seminars in Interventional Radiology, 23(2), 194-204. doi: 10.1055/s-2006-941450
- Memorial Sloan Kettering Cancer Center. (2024, February 2). About your biliary drainage catheter. https://www.mskcc.org/cancer-care/patient-education/about-your-biliary-drainage-catheter
- Merriam-Webster Dictionary. (2024, December 21). Percutaneous. https://www.merriam-webster.com/dictionary/percutaneous#medicalDictionary
- Ramesh, B. A., Evans, J. T., & BK, J. Suction drains. (2023 July 4). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557687/
- Rivera-Sanfeliz, G. (2008). Percutaneous abdominal abscess drainage: A historical perspective. American Journal of Roentgenology, 191(3), 642-643. doi: 10.2214/AJR.07.3903
- Shrestha, U., Sarkar, S., Naqvi, F., Alam, A., & Balakrishnan, B. (2023). Why is the pleural fluid green? A review of pleural fluid characterization and analysis. Am, J Respir Crit Care Med, 207, A41009. https://www.atsjournals.org/doi/pdf/10.1164/ajrccm-conference.2023.207.1_MeetingAbstracts.A4109
- Siddiqui, F., Ihle, R. E., & Siddiqui, A. H. (2023, February 8). Intrapleural catheter. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK493229/
- The Royal Children’s Hospital Melbourne. (2023, November). Surgical drains (non cardiac). https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Surgical_Drains_(Non_Cardiac)/#types-of-drains
- UCLA Health. (n. d.) Interventional radiology: Drainage percutaneous. https://www.uclahealth.org/medical-services/radiology/interventional-radiology/treatments-procedures/drainage-percutaneous
- Zaver, V., & Kankanalu, P. (2023, September 4). Negative pressure wound therapy. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK576388/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
