Course
DVT Treatment
Course Highlights
- In this DVT Treatment course, we will learn about the etiology and pathophysiology of DVT.
- You’ll also learn the medications that are used in the treatment and management of DVT.
- You’ll leave this course with a broader understanding of the pharmacokinetics of anticoagulant medications.
About
Pharmacology Contact Hours Awarded: 1
Course By:
Elaine Enright
BSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
A DVT is a blood clot that develops in the deep venous system, most often in the lower extremities, but can also occur in the cerebral and mesenteric veins as well as the upper limbs. (1)
DVT represents the third most common cause of death, after Myocardial Infarction (MI) and stroke. (1) The rate of DVTs is 1.6 per 1000 patients annually with numbers of involvement depending on the location. Of those numbers, distal veins are most affected at 40%, popliteal veins are at 16%, femoral at 20%, common femoral is at 20% and iliac veins are at 4% (1).
DVTs are caused by anything that obstructs the vessel. This obstruction could be a post-operative inflammation, a damaged vessel from injury or infection, or anything else obstructing the vessel. DVT is in itself not dangerous, but the clot or piece of the clot breaks off (thrombus) and makes its way to the lungs (thrombosis) causing a pulmonary embolism (PE) or block a vessel causing MI or stroke. At this point, it becomes dangerous and requires medical treatment immediately. (3)
Risk factors for DVTs include genetics, limited blood flow to the vessel, sedentary lifestyles, during pregnancy or post-partum, over 40 years of age, autoimmune diseases, smoking, varicose veins, birth control medication or hormone replacement therapy in menopausal women, a central venous catheter in place and having Covid 19. (3)
Symptoms of DVTs include swelling, warmth to the part of the body affected, pain when standing and walking if in the lower limbs, severe headache, and redness to the area. Additionally, the limb may be larger than usual near the surface of the skin, pain may be felt in the abdomen or pelvis when the DVT is in the mesentery vessel, and/or seizure activity may occur when in the brain. (3)

Self-Quiz
Ask Yourself...
- Are you aware of the Homan’s sign-in DVTs?
- What is the mechanism of a blood clot?
- What type of surgery do you see as having the greatest risk of a clot forming?
Pharmacokinetics
There are several different medications to treat DVT. The goal of these medications is to dissolve the clot, prevent PE, prevent post-thrombotic syndrome, and reduce morbidity. (1) If you have ever cared for a patient with DVT you may know that anticoagulant medications are first-line treatment. (1)
The dosage depends on lab values of INR, prothrombin time (PT), partial prothrombin time, PTT, and the overall health of the patient. For instance, cancer patients with DVT would receive a lower dose of anticoagulant than a healthy patient presenting with DVT.
We will now review drugs used to treat DVT.
Coumadin, Jantoven
- Generic Name (warfarin)
- Drug class: Coumadin and Indandiones
- Uses: In the prevention of blood clots
(6)
Mechanism of Action
Warfarin inhibits vitamin K epoxide reductase. This is an enzyme that reduces the availability of Vitamin K, so the clotting mechanisms for factors II, IX, and X are decreased allowing for thinner blood to pass through the vessels. (6)
Side effects
- Allergy to warfarin. i.e. hives, shortness of breath, facial, lip, tongue, or throat edema.
- Acute bleeding that will not stop
- Increased bruising
- Heavy menstrual or vaginal bleeding
- Nosebleed or bleeding gums
- Weakness or dizziness
- Hematuria or hematochezia (bloody, black, or tarry stools)
- Bruising or bleeding in a breastfed baby
(6)
Warnings
Coumadin should not be taken with any NSAIDs such as aspirin, ibuprofen, naproxen, celecoxib diclofenac, indomethacin, and meloxicam as these drugs can also thin the blood.
Alcohol, grapefruit, pomegranate, and noni juice should be eliminated as they can interact with coumadin, leading to side effects.
Foods that contain Vitamin K should be avoided as they can lower the action of coumadin. Vitamin K is an antagonist which can block the action of coumadin. Foods to avoid or lessen are green leafy vegetables and vegetable oils. Taking too much coumadin can increase bleeding.
Patients should alert their doctor if they have hypertension, kidney or liver disease, cancer or low blood cell counts, a stroke, diabetes, CHF, GI bleeding, or serious heart disease. Coughing up blood or coffee ground vomitus.
Other drugs that affect coumadin’s mechanism of action are antibiotics or antifungal medications, vitamin K supplements, herbal remedies such as echinacea, garlic ginkgo biloba, coenzyme Q10, St. John’s Wart, ginseng, and goldenseal.
**It is not known if warfarin crosses the blood barrier in a pregnant or breastfeeding mother, so it is best if it is not used in these patients. (5)


Self-Quiz
Ask Yourself...
- Does Coumadin have any other names?
- How would you stop an active bleed in a patient on heparin?
- Where can you find which supplements can interact with Coumadin?
Heparins
Heparin medications are anticoagulants in the “heterogeneous group of straight-chain anionic mucopolysaccharides, called glycosaminoglycans”. (6) These glycosaminoglycans have anticoagulant properties that keep blood thin and prevent clots. This group activates antithrombin III, inhibiting factor Xa, and thrombin as the anticoagulant in the blood.
Heparin has two classes known for different types, high molecular weight (heparin) or low molecular weight such as Lovenox. Heparins are used for patients who have atrial fibrillation MI, DVT, and certain orthopedic surgeries. (7)
Lab values for this high molecular weight heparin must be tested daily or as prescribed by the ordering provider to determine a therapeutic level of the drug in the blood. It is available in vials of 1000, 5000, 10000, and 20000, USP, and the IV doses are diluted in 40 or 80 mg of sodium chloride. (6)
Heparins are used as a single dose and the vial should be discarded if a lower dose is indicated. (6) If Benzyl Alcohol is used as a preservative in the vial, it should NOT be used in neonates, infants, and/or nursing mothers. (6)
The dosage of Heparins used depends on the problem and can change throughout treatment.
Drug Class
Heparins fall under the drug class, “Anticoagulants, Cardiovascular, antimicrobials, adjunct, antidotes, Other” (6).
Uses
Heparin is used as a subcutaneous injection or in a diluted IV drip. It is primarily used for venous thromboembolism, in certain orthopedic procedures (total joint replacement), for PE, atrial fibrillation (A fib), disseminated intravascular coagulation, (DIC) clotting prevention in cardiac and arterial surgeries, and to treat and prevent arterial embolism in the periphery. (6)
IV heparin should always be used in an IV pump for accuracy.

Self-Quiz
Ask Yourself...
- How often do you see heparin being used in the hospital?
- Are other drugs being used in the place of heparin for traditional heparin use? 
Low Molecular Weight Heparin (LMWH)
Low Molecular weight heparins (LMWHs) are used for the prevention of DVT or as a treatment for DVT, thromboembolism in pregnant women, and PE in high-risk patients or to prevent recurrence in women, and treatment of ST elevated MI whether the patient is stented. (8).
They are also used for unstable angina, and extracorporeal circuits, which is the procedure when blood is removed from a patient either during a procedure such as cardiac surgery (cardiac bypass) or hemodialysis before returning the blood to the patient. (9) Some LMWHs we are familiar with are Lovenox, known as generic enoxaparin, and Fragmin, generic name Dalteparin.
LMWHs have also been used to assist the body in healing from critical infections, acute respiratory distress syndrome (ARDS), and during the COVID-19 pandemic. (8)
Mechanism of Action
LMWHs act by inhibiting the final pathway of the coagulation cascade (clot-making). This final pathway converts fibrinogen into fibrin using thrombin as the catalyst. LMWHs inhibit factor Xa, (which we will discuss later in this course) to fibrin from being converted. (8) LMWHs have a slower reaction than heparin. (8)
Side effects
As with any anticoagulant excessive bleeding is the major side effect. Other side effects include thrombocytopenia, osteoporosis, hypoaldosteronism, fractures without an injury, and hypersensitivity to the drug. (8)
Contraindications
Patients who have had trauma, bleeding disorders, recent cerebral hemorrhage, peptic ulcers, severe hypertension, recent eye or nervous system surgery, and epidural half-life should not receive any heparins. The risks of bleeding with heparin outweigh the benefits it may give. (8)

Self-Quiz
Ask Yourself...
- Which LMWHs have you used or seen used most often?
- How would you teach a patient to self-inject a LMWH?
- What does thrombocytopenia mean?
Heparin
Heparin is classified as high molecular weight. Heparin requires daily or interval monitoring of aPTT for therapeutic effect. As with LMWHs, heparin injection is used to treat or prevent blood clots from forming. (7) Major uses for heparin are for patients with a high risk of blood clots and thromboembolism.
It is used in cardiac concerns such as Atrial Fibrillation with embolization, and cardiac and arterial surgeries. It also is used in DIC, MI, DVT, knee and hip surgery prevention and treatment for peripheral arterial embolism, blood transfusions, and as previously stated extracorporeal circulation and hemodialysis. (7)
Side effects
Heparin has the same side effects as LMWHs but also includes (see above), however it can cause more serious side effects. Some major issues are chest pain, palpitations or arrhythmias, dyspnea, symptoms of anxiety, sweating, dizziness, nosebleed, hematuria, or black stool(melena), loss of appetite, vomiting or coughing up what looks like coffee grounds, tiredness, fever, chills, easy bruising and prolonged bleeding, thrombocytopenia, and sudden numbness or weakness. (6)
It can also cause heparin-induced thrombocytopenia (HIT) 1 which will cause a slight decrease in platelets and is common in approximately 10% of patients. (11) The second type of HIT or HIT 2 can cause a chain reaction of clotting. (11). This is very dangerous but is rare (1% of patients). (11)
Warnings
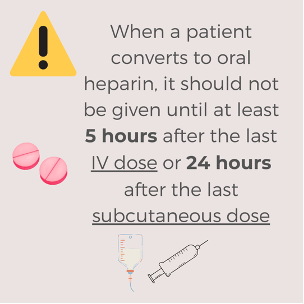
When a patient converts to oral heparin, it should not be given until at least 5 hours after the last IV dose or 24 hours after the last subcutaneous dose. (6)
Nurses must be aware of this dosing as fatal medication errors have occurred.
Major contradictions for heparin use are:
- History of Heparin-Induced thrombocytopenia and thrombosis (HITT)
- Hypersensitivity to heparin or pork products
- Hemorrhage in the gastrointestinal or urinary tract.
- An adrenal hemorrhage causes adrenal insufficiency, ovarian hemorrhage in childbearing-aged women, and retroperitoneal bleeding.
- Osteoporosis in long-term heparin patients
- Increase in lab values of aspartate aminotransferase (AST) and alanine aminotransferase (ALT). (6)
Non-steroidal anti-inflammatories (NSAIDS) should not be taken with heparin as they alone can cause bleeding. Other drug interactions are IV nitroglycerin, digitalis, tetracyclines, antihistamines, and nicotine.

Self-Quiz
Ask Yourself...
- How can you learn more about heparins and their side effects?
- Do you know how to counteract too much heparin in the blood?
- What other lab tests are used for a patient on heparin?
Thrombin inhibitors
Newer medications called thrombin inhibitors are being used more and more frequently in certain circumstances. They do not require lab testing as with coumadin or heparin. Again, they are used in place of heparin for certain conditions like DVT, PE, MI, and stroke. They can also be used for post-surgical in orthopedic patients.
Mechanism of Action
These medications act by inhibiting the activity of thrombin by binding to thrombin as well as free thrombins to prevent the blood from clotting.
Some of these medications are Pradaxa (generic name dagibatran), Angiomax (generic name bivalirudin), and Iprivask (generic name desirudin). (10)
Thrombin inhibitors are used for the prevention of and treatment of DVTs and in AFIB to prevent thromboembolism and do not need lab testing.
Side Effects
As always, the most common side effect is bleeding, however, each of the thrombin inhibitors can cause severe liver problems, and moderate to severe kidney issues. (11) They can also cause indigestion, hypotension, abdominal pain, cardiac arrest, and sepsis if there is an infection.
Warnings
Warnings for these medications are the same for the other anticoagulants, excessive bleeding, or blood clots. So again, it is important to watch for black tarry stools, dizziness, excessive bruising, bleeding gums, and prolonged bleeding. (11)

Self-Quiz
Ask Yourself...
- Where can you find the most common side effects of each thrombin inhibitor?
- What are the most common prothrombin inhibitors used in your practice?
- Have you experienced these side effects in any of your patients?
Factor Xa inhibitors
These inhibitors work by “selectively and reversibly blocking the activity of clotting factor Xa” which will prevent clots from forming. Xa factor acts as a catalyst in activating prothrombin to thrombin. (12) This factor does not require lab monitoring as they have predictable anticoagulant effects. (12).
Some of these Xa factors are:
- Xarelto (rivaroxaban)
- Eliquis (apixaban)
- Arixtra (fondaparinux)
- Savaysa (edoxaban)
- Bevyxxa (betrixaban)
Side effects
The side effects of these medications are like all other anticoagulants. Excessive bleeding, bruising, etc. Other things to be aware of are headaches, dizziness pain or swelling, and/or drainage from wound sites. (12)
Warnings
Some medications should not be taken with anticoagulants. These include some.
antifungals and antibiotics, some statins, and SSRIs. (15) As nurses and pharmacists, we also know that NSAIDS should not be used with anticoagulants.

Self-Quiz
Ask Yourself...
- Can you find the reason for neurological monitoring in factor Xa?
- What condition(s) have you seen that uses the factor Xa?
Nursing Considerations in DVT
Nursing Assessment
As part of the plan for DVT and anticoagulants, nurses must be aware of several things. On assessment, the nurse should be watching for any signs and symptoms of atrial fibrillation and check the patient’s history for bleeding disorders as well as any medications that may interfere with the anticoagulant being prescribed. Allergy status is also important as is pregnancy and lactating in women for up to 3 months post-partum. (2)
Nurses should also know what medications and herbal supplements the patient is taking to avoid interactions. (13) Once it is clear the patient may take anticoagulants and in the case of heparin, blood samples must be taken to measure platelet counts as well as INR, PT and PTT. (14) The timing of these tests will depend on the prescriber, but it is usually before and after the dose if it is heparin.
Evaluation
Monitoring side effects is imperative as is the patient’s understanding and ability to give back all instructions given to them. In older adults, kidney and liver functions should be observed as this group of patients could become toxic if on long-term medication. Finally, cardiovascular and neurological systems should be evaluated and monitored for any arrhythmia or adverse effects. (15)

Self-Quiz
Ask Yourself...
- Does your workplace have an educational program for patients new to anticoagulants?
- How would you instruct a patient on how many green leafy vegetables they can consume?
Research
Ongoing research on anticoagulants focuses on developing them with an improved safety profile. (14). Several promising approaches to reduce the bleeding risk target the contact activation pathway of coagulation. (14)
The ultimate goal of these medications is the prevention of thrombosis without impairing hemostasis. Based on epidemiological data on hereditary factor deficiencies and preclinical studies, factor XI (FXI) emerged as the most promising candidate target. (14)

Self-Quiz
Ask Yourself...
- Where can you find more information on the research into Factor XI?
- Can you find information on how research will change the use of anticoagulants?
Conclusion
As we have reviewed this class of medications and their use, we are reminded of what disorders they are used for and what the different types of anticoagulants are. We have looked at side effects, warnings, and interactions as well as what type of testing needs to be done for these medications. We have also seen the newer medications such as thrombin inhibitors and factor Xa which are being used in a variety of cases. Researchers are now looking at ways to anti–coagulate the blood while maintaining homeostasis. I suspect we will hear more about these new drugs soon.
References + Disclaimer
- Sheikh. M. Waheed; Pujitha Kudaravalli; David T. Hotwagner (2023). National Library of Medicine, Deep Vein Thrombosis. Stat Perls Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK507708/
- Mayo Clinic (2022). Deep Vein Thrombosis. Retrieved from: https://www.mayoclinic.org/diseases-conditions/deep-vein-thrombosis/symptoms-causes/syc-20352557.
- Cleveland Clinic (2022). Deep Vein Thrombosis (DVT) Retrieved from https://www..clevelandclinic.org/health/diseases/16911-deep-vein-thrombosis-dvt
- CDC. What is Venous Thromboembolism? Retrieved from: https://www.cdc.gov/ncbddd/dvt/facts.html#:~:text=Venous%20thromboembolism%20%28VTE
- Drugs.com (2024). Coumadin. Retrieved from: https://www.drugs.com/coumadin.html
- Drugs.com (2022). Heparin. Retrieved from: https://www.rxlist.com/heparin-drug.htm
- Drugs.com (2024). What are Heparins? Retrieved from:https://drugs.com/drug-class/heparins.html
- Solari, Francesca, Varacallo, Matthew (2023) Low molecular weight heparin Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK525957/
- Mayo Clinic (2022). Extra Corporeal Membrane Oxygenation Retrieved from: https://www.mayoclinic.org/tests-procedures/ecmo/about/pac-20484615
- Drugs.com (2024) What are Thrombin inhibitors? Retrieved from https://drugs.com/drug-class/thrombin-inhibitors.html.
- Cleveland Clinic (2024). Anticoagulants. Retrieved from https://my.clevelandclinic.org/health/treatments/22288-anticoagulants
- Drugs.com (2024). Factor Xa inhibitors. Retrieved from https://www.drugs.com/drug-class/factor-xa-inhibitors.html
- Cleveland Clinic. What to avoid when taking a blood thinner. Retrieved from health.clevelandclinic.org/what-to-avoid-when-taking-blood-thinners. 
- Factor XI Inhibitors for Prevention and Treatment of Venous Thromboembolism: A Review on the Rationale and Update on Current Evidence. National Library of Medicine. Retrieved from: https://pubmed.ncbi.nlm.nih.gov/35647061/
- Johns Hopkins Nursing. Anticoagulation Drugs, What Nurses Need to Know. Retrieved from: https://magazine.nursing.jhu.edu/2011/07/anticoagulation-drugs-what-nurses-need-to-know/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
