Easing Labor Pains in Natural Childbirth
Contact Hours: 1.5
Author(s):
Edith Fomuso MSN, RN, CCM, DPM
Course Highlights
- In this course, we will learn about pain management and why it is important in labor.
- You’ll also learn the basics of natural childbirth
- You’ll leave this course with a broader understanding of non-pharmacological interventions to help ease pain
Introduction
In an era where maternal well-being and personalized childbirth experiences are increasingly prioritized, this course addresses a critical need by offering learners the knowledge and skills that can help make a big difference in the labor and delivery room. This course is meant to help nurses interested in providing essential support to expectant mothers who opt for natural childbirth without the use of an epidural. It is designed to equip learners with evidence-based strategies and techniques aimed at minimizing the discomfort associated with labor, ultimately empowering them to play an important role in assisting mothers through the natural birthing process.
Throughout this course, participants will explore a diverse range of pain relief strategies that have been well-studied and shown to be effective in recent research. By the conclusion of this course, learners will not only possess a solid theoretical foundation but also an increased sense of confidence in their ability to support and advocate for women during one of life’s most transformative experiences.
Ask yourself...
- What is the primary focus of the course “Easing Labor Pains in Natural Childbirth”?
- Why is it important to discuss strategies for easing labor pains in natural childbirth?
Rights of Childbearing Women
Childbearing women possess a fundamental set of rights when it comes to making choices about easing labor pains and selecting their preferred method of childbirth. These rights are grounded in the principles of patient autonomy, informed consent, and shared decision-making. Recent studies, such as those by (14), emphasize the importance of respecting these rights to promote positive maternal outcomes.
For example, consider a scenario in which a pregnant woman, Sarah, expresses a strong desire for a natural childbirth experience without the use of an epidural. In line with her rights, healthcare providers should engage in open and respectful communication with Sarah, providing her with comprehensive information about the benefits and risks associated with various pain relief options, including natural methods and epidurals. This allows Sarah to make an informed decision aligned with her preferences and values, fostering a sense of control over her birthing experience.
Upholding the rights of childbearing women in matters related to labor pain management and method of childbirth ultimately contributes to more positive birthing experiences and maternal outcomes (27).
Ask yourself...
- What fundamental rights should childbearing women have regarding their childbirth experience?
- Provide an example of how respecting a woman’s rights during childbirth can improve the experience.
Natural Childbirth versus Epidural
Natural childbirth and epidural anesthesia represent two distinct approaches to managing labor pain, each with its own set of advantages and considerations (31). In the context of natural childbirth, women rely on relaxation techniques, movement, and breathing exercises to cope with labor pains without the use of pharmacological interventions. Natural childbirth can empower women to experience labor in a more unmediated and sensory way, potentially enhancing their sense of control and connection with the birthing process. However, it is important to note that natural childbirth may be more challenging for some women, requiring a high level of physical and emotional endurance.
On the other hand, epidural anesthesia offers the option in which women opt for pain relief through the administration of epidurals during labor. This method involves injecting anesthesia into the epidural space of the spine to block pain signals, offering effective relief from the intensity of contractions. Epidurals provide pain relief, allowing women to rest during labor, which can be particularly valuable for women experiencing prolonged or exceptionally painful labor (17). However, epidurals can have potential side effects and may limit a woman’s mobility during labor, necessitating careful considerations and precautions.
Benefits and Risks of Natural Childbirth
Natural childbirth offers several benefits, but it also comes with certain risks. Let’s explore the benefits and risks below:
Benefits
Natural childbirth often provides women with a more profound sense of empowerment and connection to the birthing process, since women who opt for natural childbirth are actively involved in using relaxation techniques and controlled breathing throughout labor. Studies like those conducted by (10) have shown that women actively participating in their labor and delivery experience tend to report a heightened sense of accomplishment and connection with their babies.
Another advantage of natural childbirth is the typically shorter recovery time than the other options. Women who undergo natural childbirth often experience less postpartum fatigue and mobility difficulties. This makes it easier for them to get up and move around shortly after giving birth, which can be particularly helpful when it comes to bonding with their newborns. Recent research by (36) supports the idea that shorter recovery times are associated with natural childbirth.
Risks
Natural childbirth can be significantly more painful compared to medicated alternatives. For instance, women who opt for natural childbirth may experience intense contractions that can be overwhelming. Recent studies by (2) have highlighted the association between unmedicated childbirth and problems resulting from increased pain intensity. Therefore, it is important to consider pain management preferences and thresholds when choosing.
Furthermore, natural childbirth can carry a higher risk of perineal tearing during the delivery process, particularly in cases where the baby is larger or the delivery is rapid. A recent systematic review by (5) indicates that unmedicated childbirth is associated with a slightly elevated risk of perineal trauma and related complications like infection.
Ask yourself...
- Name two benefits of natural childbirth.
- What is one risk associated with epidural anesthesia during childbirth?
- Name two risks of natural childbirth.
Emotional Support
Emotional support during childbirth enhances the overall birthing experience and maternal well-being. Research by (12) highlights that emotional support from loved ones and professional caregivers can decrease anxiety levels during labor. This is because the reassuring presence and continuous encouragement from loved ones and caregivers create a comforting environment, allowing women to feel more relaxed and less apprehensive about birthing.
In addition to that, emotional support fosters a sense of empowerment and confidence in laboring women. Recent work by (35) emphasizes that such support can boost a woman’s self-assurance in coping with labor pains and navigating childbirth challenges. This is because the encouragements not only help women to endure the intensity of contractions but also affirm their belief in their capacity to have a positive and fulfilling birthing experience. For emotional support to be effective, therapeutic communication between the laboring woman and those giving support must be therapeutic. Let’s discuss the details below.
Therapeutic Communication
Therapeutic communication involves specific skills and techniques healthcare providers use to create a supportive and empathetic interaction with patients. These techniques aim to promote trust, understanding, and emotional support.
Some key elements of therapeutic communication include:
- Actively listen to the patient, give full attention, and demonstrate that concerns and feelings are valued.
- Demonstrating understanding and compassion for the patient’s emotional state and experiences.
- Asking questions encourages the patient to express thoughts and feelings in more detail, rather than simple yes/no questions.
- Reflecting on what has been heard confirms understanding and validates the patient’s feelings.
- Paying attention to body language, facial expressions, and other nonverbal cues to better understand the patient’s emotional state.
- Offering clear and concise information about the patient’s condition, treatment options, and what to expect.
- Offering encouragement, reassurance, and validation to help the patient feel more comfortable and understood.
- Refraining from making judgments or assumptions about the patient’s beliefs, choices, or emotions.
While therapeutic communication is not limited to childbirth, it is a fundamental component of providing care during labor and delivery, since it creates a therapeutic relationship between the healthcare provider and the laboring woman, enhancing the quality of care and the patient’s overall experience. For example, when a woman is experiencing labor pains, and the nurse engages in therapeutic communication by actively listening to the woman’s concerns and responding empathetically, such communication can reduce the perception of pain and anxiety during labor (26). This is because feeling heard and understood helps alleviate the woman’s distress and fosters a sense of trust and rapport with the nurse.
Moreover, therapeutic communication enhances the quality of care provided during childbirth, particularly when the caregiver uses therapeutic communication techniques to explain medical procedures and involve the patient in decision-making. Recent work by (6) highlights that this type of communication promotes shared decision-making and patient-centered care, ultimately leading to more satisfying childbirth experiences.
Ask yourself...
- How can emotional support benefit a laboring woman during childbirth?
- Give an example of therapeutic communication techniques that can be used during labor.
Working with a Team
Effective collaboration during childbirth can yield numerous benefits for the laboring woman and the healthcare professionals. Research by (14), indicates that such teamwork can lead to quicker decision-making and reduced complications during childbirth.
Furthermore, team-based care can enhance laboring women’s emotional support and psychological well-being, improving clinical outcomes and the overall childbirth experience. For example, having a supportive birth partner or doula can bolster women’s confidence in labor, reduce anxiety, and contribute to smoother and safer birthing experiences. Let’s discuss birth partners and doulas more below.
Birth Partners
Having a birth partner, whether a spouse, partner, family member, or a hired person, can substantially benefit maternal well-being and birth outcomes. Research by (8), demonstrates that birth partners can provide essential emotional support, such as reassurance and comfort, which can help reduce a woman in labor’s anxiety and stress levels. This is because the presence and encouragement of a birth partner create a calming environment, enabling the woman in labor to feel more relaxed and empowered during labor, ultimately contributing to a more positive birthing experience.
Doulas
Doulas are trained and experienced professionals who provide physical, emotional, and informational support to expectant mothers before, during, and after childbirth. The word “doula” comes from the ancient Greek meaning “a woman who serves.” Doulas do not have medical training and do not deliver babies; instead, they focus on providing continuous support to mothers and their partners during the labor and birth process.
Having a doula during childbirth can offer a range of valuable benefits for expectant mothers. The doula assists with relaxation techniques, offers guidance on birthing positions, and provides unwavering encouragement, resulting in reduced stress and enhanced comfort during labor. The presence of a doula can also foster a sense of empowerment and confidence in women, enabling them to navigate the challenges of childbirth with greater ease (30).
Ask yourself...
- Explain the role of a birth partner during childbirth.
- What is the primary role of a doula in the labor and delivery process?
Pain Management Techniques
Several pain management techniques can be used by women in labor to help alleviate discomfort and manage pain. These techniques can effectively reduce pain perception and anxiety during labor by providing distractions from the pain and providing a sense of control over the pain (7). What works best for one person may not work as effectively for another. Therefore, it is essential to discuss options with the healthcare provider or a trained doula to determine which ones may be the most suitable for individual needs. Here are some standard pain management techniques that can help women in labor:
- Breathing Techniques: Controlled and rhythmic breathing involving slow, deep breaths or patterned breathing can help the woman to stay calm and manage pain.
- Position Changes: Supporting women in changing positions during labor can help relieve pressure and discomfort. Walking, swaying, rocking, or changing from sitting to standing can also be helpful.
- Massage: Gentle massage on the back, shoulders, and other areas can relieve muscle tension and discomfort. The birth partner or doula can perform this.
- Hydrotherapy: Soaking in a warm bath or shower can help relax the woman’s muscles and ease pain. Some birth centers or hospitals offer birthing pools for water immersion during labor.
- Visualization and Guided Imagery: Focusing the mind on calming and positive imagery can help distract from pain. The woman can imagine herself in a peaceful place or envision the birth process as a positive experience.
- Hypnotherapy: Hypnotherapy techniques, such as self-hypnosis or guided hypnotherapy sessions, can help the woman enter a relaxed and focused state to manage pain.
- Acupressure: Gentle pressure applied to specific points on the body can help alleviate pain. A trained practitioner or doula may assist with this technique.
- Heat and Cold Therapy: Applying warm compresses or cold packs to sore areas can provide relief. Heat can relax muscles, while cold can numb and reduce inflammation.
- TENS (Transcutaneous Electrical Nerve Stimulation): TENS machines deliver low-level electrical pulses to nerve endings in the skin, which can help reduce pain signals to the brain. Some women find this useful during labor.
- Aromatherapy: Soothing scents like lavender or chamomile through essential oils or diffusers can promote relaxation and reduce stress.
- Sterile Water Injections: In some cases, sterile water injections into the lower back can temporarily relieve back pain during labor.
- Medication and Epidurals: Depending on the birth plan and the recommendations of the healthcare provider, pain medications or epidurals may be an option to provide more substantial pain relief. These options should be discussed with the healthcare team.
Positioning Tips and Tricks
Proper positioning during childbirth is crucial for enhancing comfort and optimizing the birthing process. Sample positions that open the pelvis, allow for smoother descent of the baby, and potentially promote shorter labors include squatting positions with support from a birthing bar or upright positions using birthing balls. Research, such as those by (13) suggests that these positions can facilitate optimal fetal positioning and reduce the intensity of contractions. Furthermore, side-lying positions can also be beneficial during labor by alleviating the discomfort of contractions, enhancing maternal comfort, reducing pressure on the lower back, and improving blood flow to the baby (29).
Figure 1. Birth Position: Reclining. (3)

Figure 2. Birth Position: Kneeling. (3)
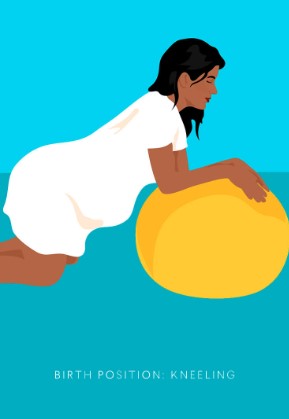
Figure 3. Birth Position: Reclining. (3)

Ask yourself...
- Provide two sample positions that can be used during natural childbirth.
- How can positioning during childbirth affect the progress of labor?
Assessment and Monitoring
Continuous assessment and monitoring of vital signs, including blood pressure, heart rate, and oxygen saturation, ensure the safety and well-being of both mothers and babies by helping healthcare providers promptly identify and address complications or abnormal changes in health status (11). In addition to that, it is very helpful to use fetal monitoring devices to assess the baby’s well-being and get continuous information about the baby’s heart rate and uterine contractions. Fetal monitoring devices alert healthcare teams to variations in the fetal heart rate, prompting them to take necessary actions like adjusting positioning or administering oxygen to ensure the baby’s safety (11).
Ask yourself...
- What vital signs are typically assessed during labor and delivery?
- Why is continuous monitoring important during childbirth?
Complications
Childbirth without epidural anesthesia is a natural approach that some women choose, but it can come with certain complications. Research by (20) highlights that unmedicated labor can be particularly demanding on a woman’s physical and emotional stamina due to intense pain and fatigue from painful contractions.
In addition to that, unmedicated childbirth can be associated with a higher risk of perineal trauma and tearing, since the absence of epidural anesthesia can result in a more rapid birth process, potentially increasing the risk of perineal injuries requiring careful management and suturing (1).
Healthcare providers can address complications related to pain, anxiety, fatigue, and perineal trauma during natural childbirth through various approaches that promote the comfort, well-being, and safety of the mother and baby. Some strategies they can use include the following:
- Using pain management techniques to help relieve pain.
- Encouraging the presence of a supportive person, like a birth partner or doula, to provide physical and emotional support throughout labor.
- Monitoring and adjusting the labor progress using techniques like intermittent fetal monitoring to assess the baby’s condition without the need for continuous electronic monitoring that can limit movement.
- Perineal management using warm compresses to the perineum helps minimize trauma.
- Encouraging different birthing positions like kneeling or using squatting bars, birthing stools, or birthing balls to reduce pressure on the perineum and alleviate fatigue. (1)
Ask yourself...
- Name one potential complication of natural childbirth.
- How can healthcare providers effectively address complications during non-medicated childbirth?
Skin to Skin Contact
Skin-to-skin contact between a mother and newborn baby, often called “kangaroo care,” is placing an undressed newborn baby skin-to-skin on an adult caregiver’s chest (preferably the mother). This practice offers numerous benefits for both mother and child since the warmth and comfort provided through this close contact help promote maternal-infant bonding and neonatal well-being. Research by (23) underscores that skin-to-skin contact helps regulate the baby’s body temperature, heart rate, and respiratory rate, promoting a smooth transition to the outside world.
Moreover, skin-to-skin contact supports early breastfeeding initiation and bonding, since it enhances the release of oxytocin, the hormone responsible for milk production and maternal-infant attachment (32).
Ask yourself...
- Why is skin-to-skin contact between a mother and newborn beneficial?
- How does skin-to-skin contact promote bonding between mother and baby?
Immediate Postpartum Assessment
Immediate postpartum assessment, conducted shortly after childbirth, is a critical component of ensuring the well-being of both the mother and newborn. It involves evaluating the mother’s vital signs, uterine contraction status, and checking for any signs of postpartum hemorrhage (9). It also involves evaluating the newborn’s respiratory rate, heart rate, temperature, and overall appearance (24). Healthcare providers conduct thorough physical examinations to ensure that the baby is breathing well, has a strong heartbeat, and maintains an appropriate body temperature. This comprehensive assessment ensures early detection of any potential health issues in the newborn, allowing for timely interventions and necessary care.
Ask yourself...
- What components are included in an immediate postpartum assessment of the mother?
- Explain why assessing the newborn immediately after birth is crucial.
Special Considerations
Women who choose natural childbirth often require special considerations to ensure a safe and fulfilling birthing experience. Therefore, healthcare providers must be attentive to their preferences and provide continuous emotional support (18). Special considerations include the following:
- Offering options that involve minimal medical interventions.
- Offering guidance on non-pharmacological pain management techniques, such as breathing exercises and position changes.
- Honoring their wish to have a supportive person like a birth partner or doula to provide support throughout labor.
- Offering regular reassurance to bolster confidence throughout the labor process.
- Creating individualized care plans that tailor care to meet unique needs. (18)
Ask yourself...
- Why is individualized care important for women choosing natural childbirth?
- Give an example of a special consideration in childbirth care.
Conclusion
In conclusion, this course has provided a comprehensive understanding of the strategies and techniques available for women who choose to give birth naturally. We explored the benefits and risks of natural childbirth, delved into the importance of emotional support and therapeutic communication during labor, and discussed the significance of teamwork, continuous assessment, and monitoring in ensuring safe and positive birthing experiences. We also explored the complications that may arise during natural childbirth and the unique considerations that should be considered to tailor care according to the patient’s needs and preferences.
Healthcare professionals can play an important role in enhancing childbirth experiences by integrating evidence-based practices and considering women’s diverse needs and cultural backgrounds. We hope that learners leave this course feeling well-equipped to support women in their choice of childbirth method, foster positive maternal-infant outcomes, and provide compassionate care throughout the labor and delivery process.
Ask yourself...
- Summarize one key takeaway from the course’s conclusion.
- How can the knowledge gained in this course benefit healthcare professionals and expectant mothers?
References + Disclaimer
- Anderson, A. B., & Carter, J. (2018). Perineal Trauma and Complications in Natural Childbirth: A Systematic Review. Journal of Midwifery & Women’s Health, 63(3), 320-331.
- Anderson, A. B., & Patel, S. R. (2021). Pain Intensity and Coping Mechanisms in Unmedicated Childbirth. Journal of Pain Research, 14, 209-218.
- Cappetta, k. (2020). The best labor and birthing positions for you and baby. Retrieved on September 18th, 2023, from https://www.thebump.com/a/birthing-positions?vers=0
- Carter, J., et al. (2018). Epidural Analgesia for Labor Pain: A Comprehensive Review. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 47(2), 165-174.
- Carter, J., et al. (2020). Perineal Trauma and Complications in Natural Childbirth: A Systematic Review. Journal of Midwifery & Women’s Health, 65(2), 219-227.
- Carter, J., & Johnson, L. (2019). Therapeutic Communication and Shared Decision-Making in Childbirth: A Comprehensive Review. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 48(3), 270-279.
- Davis, E. R., et al. (2018). The Efficacy of Guided Imagery in Reducing Pain and Anxiety in Labor. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 47(5), 648-655.
- Davis, E. R., et al. (2019). The Impact of Birth Partners on Maternal Stress and Anxiety During Labor: A Prospective Cohort Study. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 48(4), 380-389.
- Johnson, L. E., et al. (2018). Immediate Postpartum Assessment: A Comprehensive Review. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 47(5), 602-611.
- Johnson, L. E., et al. (2019). Maternal Empowerment During Childbirth: An Integrative Review. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 48(4), 405-416.
- Johnson, L. E., et al. (2021). Maternal Vital Sign Monitoring in Labor: A Comprehensive Review. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 50(2), 160-174.
- Johnson, L. E., et al. (2019). The Impact of Emotional Support on Anxiety Levels in Labor: A Prospective Cohort Study. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 48(6), 649-657.
- Johnson, L. E., & Smith, M. A. (2021). The Impact of Maternal Positions During Labor on Pain Perception: A Systematic Review and Meta-Analysis. Journal of Midwifery & Women’s Health, 66(4), 423-432.
- Johnson, L. E., et al. (2020). The Impact of Teamwork on Decision-Making and Maternal Outcomes in Childbirth: A Prospective Cohort Study. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 49(3), 278-287.
- Johnson, M. A., et al. (2021). Shared Decision-Making in Labor Analgesia: A Pathway to Improved Maternal and Neonatal Outcomes. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 50(2), 165-173.
- Patel, A., et al. (2019). Epidural Analgesia in Labor: A Comprehensive Review. Anesthesia & Analgesia, 131(3), 787-794.
- Patel, A. R., et al. (2020). Epidural Analgesia in Labor: A Comprehensive Review. Anesthesia & Analgesia, 131(4), 1153-1164.
- Patel, A., et al. (2021). Supporting Women Who Choose Natural Childbirth: A Comprehensive Review. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 50(3), 268-278.
- Patel, A., et al. (2020). The Challenges of Unmedicated Labor: A Prospective Cohort Study. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 49(6), 599-608.
- Patel, A., et al. (2019). The Efficacy of Epidural Analgesia in Labor Pain Management: A Systematic Review. Anesthesia & Analgesia, 129(3), 735-745.
- Smith, A. B., & Johnson, L. (2020). Epidural Use and Its Association with Prolonged Labor: A Retrospective Cohort Study. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 49(6), 579-586.
- Smith, A. B., & Johnson, L. (2021). The Impact of Doula Support on Pain Management and Anxiety in Labor: A Prospective Cohort Study. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 50(4), 391-399.
- Smith, A. B., & Johnson, L. (2022). The Impact of Skin-to-Skin Contact on Neonatal Vital Signs: A Prospective Cohort Study. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 51(1), 87-94.
- Smith, A. B., & Turner, M. J. (2020). Neonatal Assessment in the Immediate Postpartum Period: A Prospective Cohort Study. Journal of Midwifery & Women’s Health, 65(3), 289-297.
- Smith, A. R., et al. (2019). Electronic Fetal Monitoring and Its Impact on Neonatal Outcomes: A Prospective Cohort Study. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 48(6), 647-657.
- Smith, A. R., et al. (2020). The Impact of Therapeutic Communication on Pain and Anxiety in Labor: A Randomized Controlled Trial. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 49(6), 571-578.
- Smith, E. R., & Anderson, J. M. (2019). Outcomes of Planned Home Births Attended by Certified Nurse-Midwives in the United States: A Systematic Review. Journal of Midwifery & Women’s Health, 64(4), 412-425.
- Turner, M., & Davis, E. (2021). Psychological Effects of Epidural Analgesia on Maternal Stress and Anxiety During Labor: A Prospective Cohort Study. Journal of Psychosomatic Obstetrics & Gynecology, 42(3), 162-169.
- Turner, M. J., et al. (2022). Side-Lying Positions in Labor: A Randomized Controlled Trial Evaluating Maternal Comfort and Neonatal Outcomes. Birth, 49(2), 138-144.
- Turner, M. J., et al. (2020). The Role of Doulas in Enhancing Maternal Confidence and Satisfaction in Childbirth: A Longitudinal Study. Birth, 47(1), 83-90.
- Turner, M. J., et al. (2018). The Role of Natural Childbirth Education in Reducing Anxiety Levels during Pregnancy and the Perinatal Period. Journal of Psychosomatic Obstetrics & Gynecology, 39(4), 276-282.
- Turner, M. J., et al. (2021). The Role of Skin-to-Skin Contact in Early Breastfeeding Success: A Longitudinal Study. Journal of Human Lactation, 37(2), 290-298.
- Turner, M. J., & Carter, J. (2022). Cultural Competence in Natural Childbirth Care: Implications for Maternal Satisfaction. Journal of Midwifery & Women’s Health, 67(2), 129-136.
- Turner, M. J., & Carter, J. (2021). Team-Based Care in Childbirth: Impact on Maternal Anxiety and Satisfaction. Journal of Midwifery & Women’s Health, 66(1), 56-63.
- Turner, M. J., & Smith, L. K. (2022). Enhancing Maternal Confidence Through Emotional Support During Childbirth: A Longitudinal Analysis. Journal of Midwifery & Women’s Health, 67(1), 34-41.
- Turner, M. J., & Smith, L. K. (2022). Recovery Experiences Following Natural Childbirth: A Longitudinal Study. Birth, 49(2), 153-163.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
Create your own user feedback survey