Course
Emergency Severity Index
About
Contact Hours Awarded: 1
Course By:
Kasee Wiesen
DNP, APRM, FNP-C
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
In this course, learners will be able to define the Emergency Severity Index (ESI), including why it is used. They will gain an understanding of the ESI algorithm, including how levels are assigned to patients, what is considered life-threatening, and who is considered high-risk. They will also understand how the predicted number of resources needed to care for a patient determines ESI Levels 3, 4, and 5. The information in this course will serve as a valuable resource to nurses working in the emergency department.
Introduction
The number of people seeking healthcare in emergency departments is significant. In 2021, 139.8 million sought out care in an emergency department in the United States. Of those visits, 18.3 million, or 13.1%, required hospital admission, and 2.8 million were admitted to a critical care unit (2).
With the significant number of people seeking care in emergency departments across the United States, the importance of standardized protocols cannot be overstated. The Emergency Severity Index (ESI) plays a crucial role in this, ensuring all patients are evaluated and treated equally. The ESI, created in 1998, assists triage nurses in determining patient acuity based on the patient’s presentation. This easy-to-follow algorithm is a cornerstone of patient management in almost every emergency department in the United States, helping to manage the increasing patient load effectively (4).
Below, you will learn more about the ESI, including a more in-depth look at the algorithm and the patient criteria for each level. Based on their presentation, I will also provide additional information on determining the anticipated number of resources needed for a patient.
Definition
What is Triage?
Triage is the rapid assessment and evaluation of a patient to determine their acuity, establishing the order and possible location the patient should be seen by an emergency department provider (emergency physician, physician assistant or nurse practitioner). This process should include focused questions to obtain information pertinent to the patient’s problem and should not lead to a delay in patient care (1).
What is the Emergency Severity Index?
The Emergency Severity Index (ESI) is a standardized tool for triaging patients. It utilizes an algorithm to group patients into five levels, with Level 1 being the most urgent and requiring life-saving intervention and Level 5 being the least urgent. This algorithm categorizes patients by acuity while also considering resources needed for stable, less urgent patients (4).
This process is often completed by a registered nurse (RN) who has received specific training related to the ESI, but the emergency department physician, PA, or NP could also triage a patient if they have received the appropriate training (1).

Self-Quiz
Ask Yourself...
- What is triage?
- What is the purpose of the ESI?
- How does the triage nurse use the ESI?
Emergency Severity Index Algorithm
Algorithms provide a step-by-step guide to clinical decision-making that healthcare providers can apply to one’s daily practice. They are used frequently in healthcare to help standardize the care provided by healthcare professionals, and the ESI algorithm provides a step-by-step guide to triaging patients. This tool was not developed to update or communicate changes in a patient’s condition while in the emergency department (3).
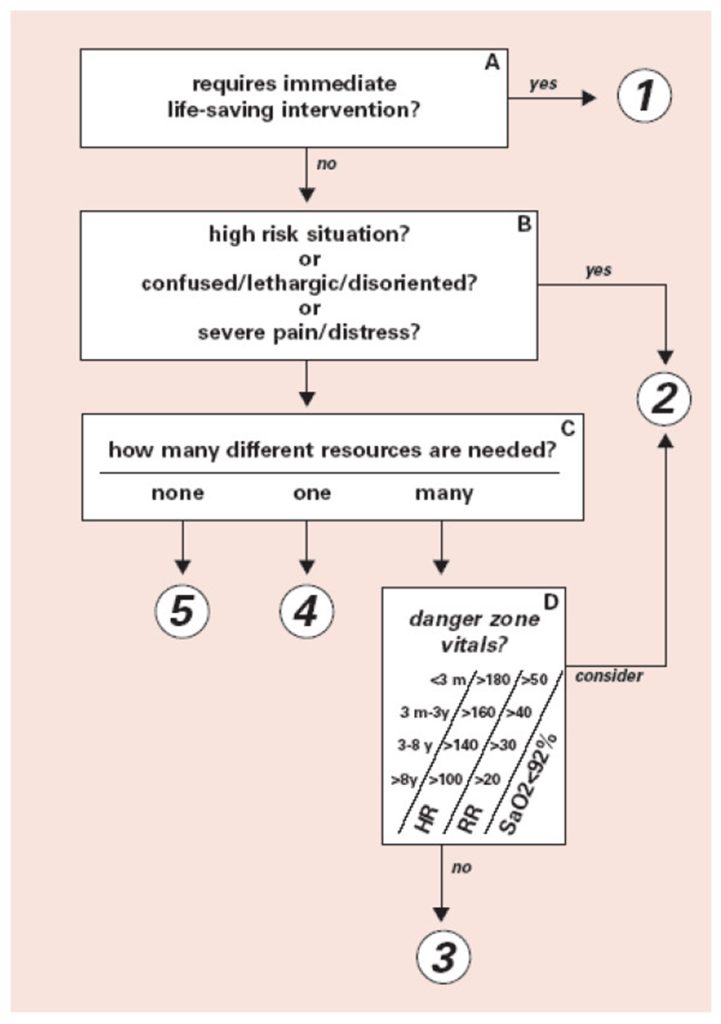
The ESI algorithm is primarily used by experienced emergency department nurses who have received specialized training specific to the ESI. The algorithm has a maximum of four decision points. However, higher acuity patients may only require one or two decisions before an acuity level is assigned. The nurse’s assessment is a key factor in this process, highlighting the value of their expertise (3).
When utilizing the ESI algorithm, the nurse’s expertise comes into play as they determine the patient’s stability. If the nurse deems the patient unstable, the patient is assigned either a Level 1 or Level 2. The triage nurse’s responsibility then extends to considering the number of resources needed to care for the patient, including lab work, diagnostic imaging, EKGs, etc (3).
The acuity of a patient is initially based on the assessment of physiological or psychological stability and if the patient needs life-threatening intervention. If the patient needs immediate life-saving intervention, such as cardiopulmonary resuscitation (CPR), only decision point A is needed as the patient is considered Level 1.
Suppose the patient does not require immediate life-saving intervention. In that case, you move to decision point B, which determines whether the patient will likely deteriorate and/or need more immediate care based on their presentation and risk factors. These patients are considered a Level 2. To make either of these decisions, the patient must have a full set of vital signs and a focused assessment before assigning an ESI level. If a patient does not meet the criteria to be assigned a Level 1 or 2 and is considered stable with a low risk of deterioration, then decision point C is considered.
The triage nurse must now consider how many resources will be utilized during the ER visit based on previous patients with similar presentations. This is the point of the algorithm when you determine if a patient is a Level 3, 4, or 5. Lastly, decision point D considered vital signs to identify more subtle high-risk patients or those requiring life-saving interventions (3).
Ultimately, the ESI algorithm includes four questions the triage nurse must consider before assigning a patient an ESI level (3).
- Is the patient unstable or requires immediate life-saving intervention?
- Is the patient considered high-risk?
- How many resources are needed to care for the patient?
- Do the patient’s vital signs support changing their acuity?

Self-Quiz
Ask Yourself...
- How many decision points are part of the ESI algorithm?
- What does it mean if a nurse considers a patient a Level 1 or 2?
- If a patient is not considered a Level 1 or 2, what now must be considered before assigning an ESI level?
- What is the acuity of the patient initially based on?
What is considered Life-saving Intervention?
Decision point A of the ESI algorithm requires the triage nurse to determine if immediate life-saving interventions are needed. Patient findings that indicate instability may include:
- Unresponsiveness
- Active seizure
- Airway obstruction
- Ineffective gas exchange
- Ineffective/decreased perfusion
Life-saving interventions that may be needed include:
- Intubation with assisted breathing
- Defibrillation
- External Pacing
- Blood administration
- Medications such as dopamine, epinephrine and naloxone
It is important to note that a patient may be discharged home from the emergency department despite being classified as a Level 1 on the ESI scale. There are reversible causes for a patient’s change in level of consciousness or abnormal vital signs such as seizure, anaphylactic reaction to a bee sting, alcohol overdose, or hypoglycemic event. The likelihood of discharge does not have an impact on assigning ESI 1 (3).

Self-Quiz
Ask Yourself...
- What are two patient findings that may indicate a patient is unstable?
- What are two life saving interventions a patient may need?
Who is considered High Risk
If the triage nurse determines the patient does not meet the criteria to be a Level 1 on the ESI, they move to the next decision point. At decision point B, the nurse assesses whether this patient is high-risk or likely to deteriorate. The triage nurse’s understanding of the criteria to be a Level 2 is crucial in preventing under triage, a situation that puts patients at greater risk of poor outcomes. Research has shown that the nurse’s accuracy at triaging a patient at Level 2 is about 43%, which is especially true for patients 65 years of age and older (3).
The nurse should use these questions to help determine whether a patient is a Level 2 on the ESI (3).
- Is the situation high-risk?
- Is the patient likely to deteriorate?
- Does the patient have an acute change in mental status?
- Is the patient in severe pain or distress (physiological or psychological)?
Is the situation high risk?
High-risk patients can be identified through a patient interview and objective data such as vital signs. The high-risk patient is one whose condition could easily deteriorate or who presents with symptoms suggestive of a condition requiring time-sensitive treatment. This may include patients with a threat to a limb, altered mental status, cardiac symptoms, or a threat to their own. Vital signs must also be considered because abnormal respiratory rates, tachycardia, blood pressure readings, and decreased oxygen saturation have been linked to adverse events or signs of possible patient deterioration. Not recognizing or managing these abnormal vital signs has been associated with higher mortality rates, indicating the significance of monitoring vital signs to identify the deterioration of the patient’s condition (3).
The triage nurse must also factor in age when triaging the patient as this can greatly impact the patient’s overall condition and ESI Level based on their complaint and vital signs (3).
Examples of high-risk patients include (3):
- Active chest pain, suspicious for acute coronary syndrome, but does not require an immediate lifesaving intervention.
- Signs of a stroke but do not meet level-1 criteria.
- A patient on chemotherapy, and therefore immunocompromised, with a fever.
- Actively suicidal or homicidal patient
- A needle stick in a health care worker (time-sensitive to postexposure prophylaxis treatment)
It is important to remember that ESI Level 2 patients are still considered high priority, and treatment/interventions should be initiated quickly due to the patient’s risk of deterioration. Missing a high-risk situation may lead to a delay in care, increasing the chance of morbidity and mortality (3).

Self-Quiz
Ask Yourself...
- What four questions should the triage nurse ask before assigning a patient an ESI Level 2?
- What criteria considers a patient high risk or an ESI Level 2?
- What are two examples of high-risk patients?
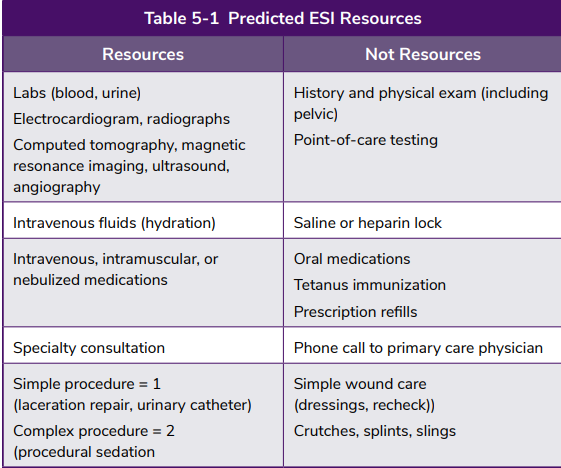
Resources and Vital Signs
Once a patient is not considered an ESI Level 1 or 2, the patient is considered stable, and the nurse moves to decision point 3. At this decision point, the triage nurse considers the resources needed to care for the patient. If two or more resources are required, a Level 3 is assigned; if one resource is required, a Level 4 is assigned; and if no resources are needed, a Level 5 is assigned. To determine the number of resources required, the nurse must be experienced and familiar with general ED standards of care and draw on past experiences when caring for patients with similar symptoms/complaints. The number of resources used is independent of the hospital type and location; in other words, a patient with abdominal pain should require the same general resources in one ED as in any other ED (3).
Many nurses and emergency department providers question what is considered a resource. Table 5-1 from the Emergency Severity Index Handbook from the Emergency Nursing Association identifies what is regarded as a resource and what is not (3).
When a patient does not meet the criteria for an ESI Level 1 or 2, the triage nurse must complete a full set of vital signs before assigning an ESI Level. This is crucial as it allows the nurse to identify potentially unstable patients, even if they appear well. It significantly reduces the risk of undertriaging a patient, especially when their initial presentation suggests a lower acuity. The nurse’s ability to recognize abnormal vital signs and respond appropriately is key to preventing adverse patient outcomes (3).
Vital signs explicitly included in the ESI algorithm include heart rate, respiratory rate, and oxygen saturation (for patients with potential respiratory compromise). It is important to note that the triage nurse must factor in the medications the patient is prescribed and the impact of these medications on their vital signs. For example, if a patient presents with bradycardia but is on a beta blocker, that needs to be accounted for. The nurse must use their clinical decision-making skills and understanding that the patients may present with medication-mediated “normal” vital signs but could still be very sick (3).

Self-Quiz
Ask Yourself...
- How many resources are needed for an ESI Level 5?
- How does the triage nurse determine the number of resources needed to care for a patient?
- What is considered a resource?
- How does obtaining vital signs help minimize the chance of undertriaging a patient?
- What vital signs are included as part of the ESI algorithm?
Case Study:
Using the Emergency Severity Index (ESI)
Patient Information:
- Name: John Doe
- Age: 45 years old
- Sex: Male
- Presenting Complaint: Chest pain, shortness of breath, and dizziness
John Doe presented to the emergency department due to experiencing shortness of breath and chest pain that started 1 hour ago. He has been feeling dizzy since he woke up this morning. The nurse took him back to the triage room to gather additional data, including vital signs, a more in-depth discussion of his current symptoms, and personal and family medical history.
- Vitals:
- Heart rate: 120 bpm (tachycardia)
- Blood pressure: 145/90 mmHg
- Respiratory rate: 24 breaths per minute (slightly elevated)
- Oxygen saturation: 94% on room air
- Temperature: 98.6°F (normal)
- Symptoms:
- Chest pain radiating to the left arm
- Shortness of breath
- Dizziness
- Mild sweating
- History:
- John is a 45-year-old male with a history of hypertension and smoking since 20 years of age.
- Reports that chest pain started suddenly 1 hour ago while walking up a flight of stairs.
- He reports no history of heart disease but a family history of myocardial infarction (MI) in his father at age 50.
Applying the ESI System
- What level would you assign John from the ESI?
- Which resources do you expect to use?
Level 2: John Doe presents with symptoms of chest pain, which is a common symptom of acute coronary syndrome (ACS), and his heart rate and blood pressure are abnormal. Given his risk factors (history of smoking, hypertension, family history of MI), this is a high-risk situation. Chest pain with potential heart problems falls under the high-risk category, and immediate assessment and intervention are necessary to rule out a myocardial infarction (heart attack).
Resources: electrocardiogram (ECG), blood tests (CBC, CMP, troponin, BNPEP), and imaging such as chest x-rays. He will likely need to be monitored closely in the emergency department.
- Why does he not meet the criteria for the other ESI levels?
- Level 1: This level is for patients requiring immediate life-saving interventions, such as those in cardiac arrest, respiratory failure, or major trauma. John does not appear to be in immediate distress or requiring resuscitation, so he does not qualify for this level.
- Level 3: This level is for patients who require multiple resources for diagnosis and treatment but are not in immediate life-threatening conditions. Although John is at high risk, he needs quick interventions rather than multiple resources. Level 3 would apply to less urgent cases like complex fractures or severe infections that require diagnostic imaging and laboratory tests but where the situation is not life-threatening.
- Level 4: This level is for patients requiring only one resource (e.g., a single blood test or a simple X-ray). John’s symptoms support possible cardiac problems, making him more urgent than a Level 4.
- Level 5: This level is for patients requiring no resources and presenting with mild complaints like minor injuries, colds, or routine follow-up care. John’s symptoms are serious and will require multiple resources and close monitoring.
John Doe is assigned an ESI Level 2 and is seen by a physician promptly. Diagnostic tests are ordered, and depending on the test results, the care team may take the following actions:
If John Doe is diagnosed with a myocardial infarction (MI), immediate intervention such as thrombolysis or catheterization may be required. He may also be admitted to the hospital for further evaluation by cardiology to determine the best treatment plan for John Doe.
If the diagnosis is non-cardiac, John Doe may be treated for another condition (e.g., a musculoskeletal injury or acid reflux) but will still require close monitoring.
This case study is an example of the importance of using the ESI to prioritize patients based on their condition’s severity correctly. This helps ensure that the most critical and urgent patients receive immediate care, leading to the best possible outcomes.
Conclusion
The Emergency Severity Index is essential in emergency departments as it provides an algorithm for triage nurses to assist them in assigning acuity to their patients. It helps prevent undertriaging, ensuring those critically ill or at higher risk of deteriorating will see an emergency department provider before a patient with a less urgent or minor problem. The ESI optimizes patient flow through the emergency department and aims to improve patient outcomes.
References + Disclaimer
- American College of Emergency Physicians. (2024, June). Emergency Department Triage. https://www.acep.org/patient-care/policy-statements/emergency-department-triage
- Centers for Disease Control and Prevention. (2024, October 25). Emergency Department Visits. https://www.cdc.gov/nchs/fastats/emergency-department.htm
- Emergency Nurses Association. (2023). Emergency Severity Index 5th Edition. Emergency_Severity_Index_Handbook.pdf
- Emergency Nurses Association. (2023, March 29). ENA Updates Emergency Severity Index Resources to Improve Patient Triage. https://www.ena.org/press-room/2023/04/25/ena-updates-emergency-severity-index-resources-to-improve-patient-triage
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
