End of Life Care for Patients with Disorders of Consciousness
Contact Hours: 2
Author(s):
Peggy Fossen DNP, RN, CNE
Course Highlights
- In this End of Life Care for Patients with Disorders of Consciousness course, we will learn the differences between the three states of Disorders of Consciousness.
- You’ll also learn the different approaches and treatments used to care for patients with Disorders of Consciousness.
- You’ll leave this course with a broader understanding of key components to include in the education of the family of patients with Disorders of Consciousness.
Introduction
Understanding consciousness is helpful for fully understanding disorders of consciousness. Consciousness is defined as the state of full awareness of oneself and one’s relationship to one’s environment. It requires awareness and wakefulness; in other words, it simply means being awake and aware of one’s surroundings.
Disorder of Consciousness (DoC) occurs when there is a significant change in awareness and wakefulness. This usually occurs because of damage or injury to the brain (1). If the damage or injury is mild, the change in consciousness can be mild. However, if the damage or injury is severe, the level of consciousness could be seriously changed, lasting a longer period or even permanently.
Health outcomes for patients with DoC vary greatly depending on the individuals’ circumstances. Some patients may be permanently unconscious, while some may have severe disabilities and require assistance with their activities of daily living. On the other hand, some may recover and be able to function on their own (20). Regardless of the state of consciousness, the patient’s diagnosis, treatment, and recovery can be a complex and challenging process.
Disorders of Consciousness
Definition
Disorders of Consciousness (DoC) are a specific group of conditions related to difficulty with awareness and wakefulness (8). Three states are included in the DoC.
- Coma
- Vegetative State (VS) or Unresponsive Wakefulness Syndrome
- Minimally Conscious State (MCS)
Coma
While individuals in the state of coma are alive, they are in a deep state of unconsciousness, lacking awareness of their surroundings and are unable to move or respond to their surroundings. Their eyes may open, and they may even cry, laugh, or grimace. However, they have lost the ability to speak or react to commands. The state of coma usually does not extend over two to four weeks (2). It is important to remember that in a coma, there is a loss of both awareness and wakefulness.
Clinical Presentation of Coma
- Depressed brainstem reflexes
- Failure to respond to stimuli
- Irregular breathing
- Absent sleep-wake cycle
- Inability to voluntarily open the eyes
- No voluntary actions
Vegetative State or Unresponsive Wakefulness Syndrome
The vegetative state (VS) is sometimes referred to as unresponsive wakefulness syndrome. Many prefer the terminology of unresponsive wakefulness syndrome due to the negative insinuations associated with vegetative state (1).
Those in a VS have a loss of awareness, wakefulness, and the ability to respond, follow commands, and interact with others. While they may display complex reflexes such as eye movements, yawning, and involuntary movements, they have no awareness of self or environment.
The VS is a chronic condition caused by significant injury or damage to the cortex (3). While the cortex has been severely damaged, the hypothalamic and medullary brain stem functions remain functional. This results in the loss of cognitive functioning, but the cardiorespiratory and autonomic functions are still able to support life.
While any condition that results in brain damage can cause a VS, the most common causes are traumatic brain injury and diffuse cerebral hypoxia (3). A VS can be continuing or permanent. If the condition has lasted longer than four weeks, it is a continuing VS. It is considered a permanent VS if the condition has lasted longer than 6 months, and is caused by a non-traumatic brain injury, or has lasted longer than 12 months and is caused by a traumatic brain injury (15).
Clinical Presentation of Vegetative State
- Eye-opening, reactive pupils and oculocephalic reflex
- Return of Sleep-Wake Cycles
- Yawning, chewing, swallowing, guttural vocalizations, and moaning.
- Arousal and startle reflexes
- Watering and tearing of the eyes
- The appearance of a smile or a frown
- Spontaneous roving eye movements
Minimally Conscious State
This state of consciousness is recognized by minimal or inconsistent awareness and can be temporary or permanent. Like the VS, the minimally conscious state (MCS) is caused by severe damage to the brain (3). As a result, the person could remain in this state, or they could regain full consciousness. It is important to note the length of time the patient has been in the MCS, as the longer they remain in this state, the greater the risk for developing permanent impairments is (3). Someone who has been in a coma or VS could then enter the MCS (5). This state is considered to be permanent if it has lasted for several months with no sign of improvement (15).
Clinical Presentation of Minimal Conscious State
- Eyes will open.
- Remaining awake for longer periods of time
- Ability to track visually
- Will have purposeful interaction with their environment
- Will be able to follow simple instructions.
- May speak some words or phrases
- Ability to answer yes or no questions
- May make automatic movements such as scratching, crossing legs, or gesturing
- May respond to others by crying, smiling, or laughing
- Reaching for or trying to hold objects
Comparison of Disorders of Consciousness States
The following table shows the differences between vegetative state and a minimally conscious state.
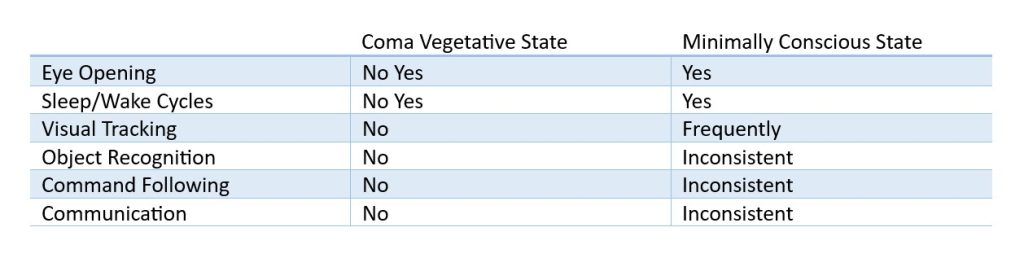
Table 1. Comparison of Disorders of Consciousness States (3)
Ask yourself...
- What is consciousness?
- What are the differences between the vegetative state and minimally conscious state? What are their clinical presentations?
- What are the common causes of vegetative state?
- What are the key characteristics of the state of coma?
Causes
DoC is a result of serious impairment to the brain and its functions. This can be due to several reasons, which are classified into two types: severe brain injury from trauma and severe brain injury from disease or illness. Brain injury from trauma results from physical injury. Meanwhile, brain injury from disease or illness is a result of a health issue affecting significant systems in the body, resulting in damage to the brain (21). Some of those commonly seen are.
Traumatic Brain Injury
Traumatic Brain Injury is caused by:
- Falls
- Car Accidents
- Sports-related head injuries
Acquired Brain Injury
- Anoxia/Hypoxia
- Seizures
- Cardiac arrest
- Stroke
- Infections
- Neurological Diseases
- Chemical exposure
- Developmental or Genetic Disorders
- Metabolic Disorders
- Brain bleed
Ask yourself...
- What is the difference between a traumatic brain injury and an acquired brain injury?
- What are the most common causes of acquired brain injury?
Diagnosis and Assessment
There are no specific laboratory or imaging tests available to diagnose DoC. However, some diagnostic scales and assessments evaluate the patient’s attention, communication, response to stimulation, vision, and ability to follow commands (7).
Healthcare professionals should carry out a thorough examination, which includes extensive testing of the patient’s level of wakefulness and awareness.
To accurately diagnose and treat DoC, a thorough assessment needs to be conducted. There are a variety of screening tools and multi-modal imaging techniques available to aid with this process. These tools assist in differentiating between the states of consciousness and are essential in diagnosing, determining prognosis, and developing a rehabilitation plan.
- Glasgow Coma Scale (GCS).
- Coma Recovery Scale-Revised (CRS-R)
- The Simplified Evaluation of Consciousness Disorders (SECONDS)
- Full Outline of Unresponsiveness (FOUR) Score
- Rancho Los Amigos Levels of Cognitive Functioning Scale (RLA)
- Disability Rating Scale (DRS)
- Nociception Coma Scale-Revised (NCS-R)
- Functional magnetic response scan (fMRI)
- Electroencephalography (EEG)
- Functional near-infrared spectroscopy (fNIRS)
Glasgow Coma Scale (GCS)
The Glasgow Coma Scale (GCS) (4) is the most frequently used tool for measuring decreases in consciousness and coma. The GCS measures the level of consciousness by assigning scores for levels of wakefulness, awareness, and response to basic instructions (4). It can be used for any situation in which there is a decrease in consciousness and is an important part of a neurological exam (4).
Coma Recovery Scale-Revised (CRS-R)
The CRS-R is designed specifically for patients with DoC. It is a standardized neurobehavioral assessment measurement used to assist in determining a diagnosis, predicting outcomes, and assisting in treatment planning (1). The scale consists of 23 items and 6 subscales, which assess auditory, visual, motor, oromotor, communication, and arousal functions (1).
The CRS-R helps differentiate patients in MCS from those in VS (1). While the CRS-R is considered the gold standard for assessing severely brain-injured patients, it does require a significant amount of time to complete.
The Simplified Evaluation of Consciousness Disorders (SECONDS)
SECONDS is a simplified, shorter version of the CRS-R. It is a fast and valid tool used to assess the level of consciousness in patients with severe brain injuries. While it is a shorter scale, it does address the key areas of observation, command-following, visual pursuit, visual fixation, oriented behaviors, arousal, localization of pain, and communication (13). It is considered a good alternative to other scales when time is a consideration.
Full Outline of Unresponsiveness (FOUR) Score
FOUR is another tool used to assess the severity of coma. It is considered to be more accurate for ventilated patients and for those with only brainstem reflexes (1).
Rancho Los Amigos Levels of Cognitive Functioning Scale (RLA)
The RLA is used in the cognitive and behavioral assessment of persons experiencing a TBI. It is a standardized measurement of cognitive and behavioral patterns assessing the state of consciousness and level of assistance required (1). The RLA assesses the patient’s state of consciousness and the level of assistance required to complete physical and cognitive functions (22). It assists the multidisciplinary team in understanding the patient’s current status and enables them to develop an effective treatment plan (22).
Disability Rating Scale (DRS)
The DRS is a concise, comprehensive, and easy-to-use tool that measures impairment, disability, and handicap. This scale determines how long recovery may take and tracks the patient’s progress. It tracks these key aspects, recovery, and progress over time, from coma to community. It is used primarily for patients suffering from moderate to severe Traumatic Brain Injury (TBI) (23).
Nociception Coma Scale-Revised (NCS-R)
The NCS-R is a validated assessment that rates pain in patients with brain injuries related to VS and MCS. As these patients are unable to communicate their feelings and perceptions of pain, it is a valuable tool (1).
Multi-Modal Imaging Techniques
Functional Magnetic Resonance Scan (fMRI)
This method contributes to the assessment of cognitive abilities in chronic DoC, specifically those in a VS. It has proven to be a beneficial diagnostic tool in determining if patients are in a VS or MCS and providing information related to the brain functions in patients with DoC (24).
Electroencephalography (EEG)
This method is easily accessible in many clinical settings, making it perfect for routine and recurring assessments. EEG has helped assess residual cognitive functions in patients with chronic DoC. The evidence indicates that the EEG does assess the dysfunctional brain networks of DoC patients. The benefits of this are more accurate diagnosis, treatment, and prognosis (26).
Functional near-infrared spectroscopy (fNIRS)
This method is a beneficial tool for assessing brain activity. It is a noninvasive optical method that detects neural activity in nonresponsive patients who have suffered an acute brain injury and can play a vital role in assessing awareness (25).
Ask yourself...
- Consider the reasons for the lack of specific laboratory or imaging tests that diagnose Disorders of Consciousness.
- Review the different diagnostic scales and assessments used to evaluate Disorders of Consciousness.
Recovery
Recovery can be a long and challenging journey for the patients and families of those with DoC. While some patients have the potential to recover, some do not. Regaining consciousness may happen at any time during the recovery process. Key components of the recovery process include imaging, electrophysiology, and pharmacological therapies.
Behavioral, imaging, and electrophysiological information should all be integrated into the patient’s recovery from DoC (27).
During the recovery process, the DoC patient may transition to different levels of care and receive care in different healthcare settings. Usually, the care will begin in an acute care hospital and then transition to an acute rehabilitation hospital. Some patients may be transferred directly to a long-term acute care hospital, a skilled nursing facility, or a nursing home. Some patients return home with their families or with the assistance of home health aides (3).
The focus of these settings does differ (3):
Acute care hospital
The focus is on saving the patient’s life and stabilizing the patient. After these needs are met, the focus shifts to restoring function (3).
Acute rehabilitation hospital
This is the setting where high-intensity treatment is provided, such as medical care, physical therapy, occupational therapy, speech therapy, recreational therapy, neuropsychological services, and nursing care (3).
Prognosis
Prognosis and possible recovery depend on the extent of the brain damage and the specific cause of the damage. Rapid treatment with the correct medical interventions and treatments is crucial for the successful recovery of the patient with DoC. The advancement of neuroimaging and electrophysiological techniques has provided insights into the brains of those with DoC, which results in a more accurate prognosis (27).
Patients with disorders of consciousness may transition through the stages of unconsciousness at a faster or slower rate depending upon the severity of their brain injuries. If recovery occurs, patients will usually progress through numerous states, and it is a gradual process.
Ask yourself...
- What are the key components of the Recovery Process?
- What are some factors that impact the prognosis of the patient with Disorders of Consciousness?
Care of the Patient with a Disorder of Consciousness
Patients with DoC require extensive and focused care. The treatment plan should be focused on the individual and their specific needs. The care provided is based on their specific condition, state of consciousness, any underlying conditions, and unique needs. While each plan needs to be individualized, the following areas should be considered in the treatment and care of the patient with DoC.
- Multidisciplinary Team Approach
- Rehabilitation Management
- Stimulation and Sensory Input
- Additional Care
Multidisciplinary Team Approach
The care of DoC patients can be a very complex endeavor. This care requires a multidisciplinary team approach. This would include physicians, nurses, social workers, psychologists, rehabilitation specialists, physical therapy, occupational therapy, speech therapists, dieticians, and spiritual support. The essential role of the multidisciplinary team is the collaboration of a group of healthcare professionals from different areas to develop an individualized treatment plan (17).
Rehabilitation Management
This department is responsible for overseeing medical management related to the prevention and treatment of immobility. It also works to improve consciousness. It will assist in maintaining the patient’s overall general health, which includes skin integrity, range of motion, and bowel and bladder management (18).
Stimulation and Sensory Input
Sensory stimulation is used to increase responsiveness. It stimulates the main senses of vision, hearing, and smell. A trained professional or a family member can perform this technique, which focuses on promoting arousal and behavioral responses by using environmental stimuli (28).
Additional Care
Patients with DoC could require additional care. The care could include the following (3):
- Feeding with a feeding tube
- Turning and positioning to prevent pressure injuries
- Managing and caring for a tracheostomy tube
- Performing Range of Motion exercises
- Using equipment to aid in positioning and the prevention of pressure injuries
- Preventing and treating infections
- Managing pain
- Administering medications
- Managing other health conditions
Interventions
Specific interventions that are considered for patients with DoC should involve multiple procedures that improve the condition of the patient (6).
Interventions used for patients with disorders of consciousness include (6).
- Environmental Stimulation
- Transcranial Magnetic Stimulation (TMS)
- Transcranial Direct Current Stimulation (tDCS)
- Deep Brain Stimulation
Environmental Stimulation
This is a frequently used intervention and involves the presentation of daily stimulus events, such as music (6).
Transcranial Magnetic Stimulation (TCM)
TCM is an intervention that uses magnetic fields to stimulate nerve cells in the brain.
Transcranial Direct Current Stimulation (tDCS)
tDCS is a brain stimulation method that requires the use of a portable wearable device. The device delivers a low electric current to the scalp (10). Evidence has supported the use of tDCS in clinical practice and has determined it may be a beneficial assessment tool in patients with DoCs (10).
Deep Brain Stimulation
This intervention involves implanted electrodes that provide electrical stimulation of the thalamus. The goal is to increase the patient’s alertness, awareness, and responsiveness (6).

Ask yourself...
- Consider the reasons why care should be focused on individualized and the specific needs of the patient with Disorders of Consciousness.
- List the areas that should be included in the care and treatment of the patient with Disorders of Consciousness.
- Why do you think a Multidisciplinary Team Approach is essential for caring for the patient with Disorders of Consciousness?
- How may interventions, such as tDCS, assist in assessing patients with Disorders of Consciousness?
Families of Patients with Disorders of Consciousness
Support
While the care for the patient with DoC is of the utmost importance, the care of the family should not be overlooked. This can be an emotionally draining and very stressful time in their lives. The challenges they face may continue for months or even years and can affect these family members’ mental and physical well-being.
Consideration and support should be provided for the following areas:
- Emotional support
- Social support
- Respite care
- Education
- Routine and structure
- Financial and legal support
- Communication
- Rehabilitation support
- Advance care planning
- Comfort and dignity
Education
Disorders of consciousness are a difficult concept to understand, especially for the families of those patients in this state. It may be difficult for the family to understand why their loved one will not wake up or respond to them. For them to understand what is happening to their family member and why it is happening, they will require assistance and understanding.
Providing education and resources will ensure they have the awareness and knowledge needed to assist them in coping with the family member with DoC. Many family members have limited knowledge related to DoC. While wanting to assist their loved one, they are unsure of what they can do to help.
Educating family members can increase their awareness of the diagnosis, prognosis, care, and treatment of their family member with DoC. It will also help them understand the role of health care providers and caregivers.
This education should include (29):
- Information on specific brain injury.
- Information on what part of the brain is affected.
- Information on how the brain is reacting to injury.
- Provide information on terminology related to DoC.
- Education on what treatments, medications, and interventions are being used.
- Explain the different types of assessment or screening tools that may be used.
- Discuss ways in which families can participate and communicate with patients.
Communication with families should be done in a private location, using clear descriptions and avoiding medical terminology if possible (29). Allow time for questions, and provide illustrations, written information, pamphlets, or fact sheets on DoC (29).
Resources
While patients diagnosed with DoC require extensive care and treatment, their families also require special care and attention. It is important that they are aware of and receive access to available resources and support.
Educational resources that include information on types of brain injury, diagnosis, prognosis, and care should be readily available. The family should be encouraged to increase their awareness and knowledge regarding DoC. This will increase their understanding of what is happening to their loved one and assist in making informed decisions about their care (12).
Resources should be provided on (32):
- Information on sources that increase knowledge about DoC
- Financial issues
- Long-term care
- Discharge planning
- Hands-on training for providing daily care
- Community support groups
- Community services and programs
- Agencies to assist with legal and financial needs
- Assist in awareness of websites providing information, resources, and support related to DoC
Consideration must be given to the families and caregivers as they attempt to understand what is happening to their loved one. In addition, they may be attempting to provide care and manage their own emotional, psychological, social, and financial struggles (33).
Ask yourself...
- What are the key areas to include when supporting the families of patients with Disorders of Consciousness?
- Why do you think providing education and support to the families is an important part of caring for the patient with Disorders of Consciousness?
End-of-Life Care for the Patient with a Disorder of Consciousness
Caring for the patient with DoC can be a complex and challenging task for healthcare providers and families. This is especially true for the end-of-life DoC patient. Patients with DoC present medical and ethical challenges, and difficult decisions must be made at times. Patients at the end of life with DoC will require different levels of medical support to sustain life (31).
A palliative care approach is needed to address the complex issues related to end-of-life care for these patients (31). Palliative care focuses on preventing and managing physical, social, psychological, and spiritual suffering (31).
Palliative care skills should be included:
- Symptom Management
- Communication skills
- Psychosocial Support
- Spiritual Support
- Systems of Care
- End-of-life Care
Symptom Management
This involves recognizing signs of awareness, pain, agitation, and delirium and keeping patients comfortable (31).
Communication Skills
This involves effectively communicating with patients, families, and surrogates. Communication should be empathetic and compassionate, and the patient’s information and goals should be communicated in an easily understandable manner (31).
Psychosocial and Spiritual Support
This involves identifying psychosocial and emotional needs in the patient’s families and caregivers, assisting with providing referrals for psychosocial and spiritual needs, and finding resources to support families and caregivers (31).
Systems of Care
This involves developing treatment and follow-up plans to ensure the patient’s and the caregiver’s needs are met (31).
End-of-Life Care
This involves providing emotional support and guidance during the dying process and also providing and facilitating bereavement support (31).

Ask yourself...
- Identify the purpose of palliative care for the patient with Disorders of Consciousness.
- Why do you think communication skills are important in the end-of-life care for patients with Disorders of Consciousness?
Statistics
According to a recent study, brain injury is a leading cause of disability and mortality in the United States. Over five million people are currently living with a long-term disability resulting from a brain injury (7). A significant number of these will be in a state of DoC.
While most people who experience a brain injury do regain consciousness, the number of those remaining in a state of unconsciousness does vary. The approximate annual incidence of VS in the United States is 4200, while that of MSC is unknown (14).
The collection of statistics related to DoC has been challenging. This could be attributed to underreporting or misdiagnosis. DoCs are very complex and can be caused by a variety of conditions, making diagnosis difficult (16). Even at this time, it is estimated that VS is misdiagnosed approximately 40% of the time (19).
Current Research on Disorders of Consciousness
The treatment of DoC can be very challenging, and in the past, evidence-based treatment options promoting recovery were limited (9). Based on current research, advances have been made in understanding DoC. These advances have provided updated methods to assist in understanding the conditions of DoC and improving diagnostic and treatment strategies.
Pharmacology
Few therapies have been available in the past to promote the recovery of patients with DoC. Recent studies have supported pharmacological therapies in the treatment and recovery of these complex and challenging conditions (31).
While multiple pharmacological therapies are being explored, Amantadine has been strongly associated with the acceleration of consciousness recovery (11).
Apomorphine is another pharmacological therapy gaining attention in the treatment of DoC. It has demonstrated promising behavioral effects and is a promising treatment for DoC (31).
Rehabilitation and Stimulation Therapies
A study conducted by the Coma Science Group focused on the non-invasive brain stimulation technique of transcranial direct current stimulation (tDCS). This therapy promotes brain plasticity using low electrical currents. The results demonstrated an improvement in behavioral responses (9, 10).
Ask yourself...
- Identify the reasons why the collection of statistics for patients with Disorders of Consciousness is challenging.
- Explain the importance of this research in caring for patients with Disorders of Consciousness.
Conclusion
Disorders of Consciousness involve conditions impacting a patient’s awareness and wakefulness. The disorders of coma, vegetative state, and minimally conscious state are results of brain damage or injury. DoCs are very complex, and providing care and treatment for the patient with DoC is a challenging job for all involved. Challenges are presented throughout the entire process, which includes assessment, diagnosis, prognosis, care, and recovery.
A multidisciplinary team is required to collaborate to provide current, relevant, and effective treatments. This must also be accompanied by increasing awareness and education on DoC for those providing care for these patients and their families. It is encouraging that there is an increasing number of studies related to the advancements of neuroimaging technologies and pharmacological therapies related to the DoC.
Ask yourself...
- Disorders of Consciousness include what three states?
- Why would the terminology Unresponsive Wakefulness Syndrome be preferred over Vegetative State?
- Identify the clinical presentation of Coma.
- Identify the clinical presentation of Vegetative State.
- Identify the clinical presentation of the Minimally Conscious State.
- Compare the clinical presentation of the Coma, Vegetative State, and Minimally Conscious State, and identify the key differences.
- List three causes of a Traumatic Brain Injury.
- A thorough examination of the patient with Disorders of Consciousness includes extensive testing of what?
- What does the Glasgow Coma Scale measure?
- Which diagnostic scale is considered the gold standard for assessing severely brain-injured patients?
- Identify the key characteristics of the Simplified Evaluation of Consciousness Disorders scale.
- What diagnostic tool is helpful in determining if a patient is in a Vegetative State or Minimally Conscious State?
- Identify why Functional near-infrared spectroscopy is a beneficial diagnostic tool.
- Which rating scale assists in determining how long recovery may take and tracking progress in patients with Traumatic Brain Injuries?
- Differentiate between an acute care setting and an acute rehabilitation hospital setting.
- What are the benefits of using an EEG in the assessment of patients with Disorders of Consciousness?
- Consider why emotional support is important for family members and how you would provide this type of support.
- Identify the focus of palliative care for the patient with a Disorder of Consciousness.
- List the essential care skills in palliative care of the patient with a Disorder of Consciousness.
- Examine how pharmacological therapies could advance the recovery of patients with Disorders of Consciousness.
References + Disclaimer
- Schnaker, C., & Lauryes, S. (2012). Coma and disorders of consciousness – springer. https://link.springer.com/content/pdf/10.1007/978-1-4471-2440-5.pdf
- U.S. Department of Health and Human Services. (n.d.). Glossary of neurological terms. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/disorders/coma
- Sherer et al. (2020). Facts About the Vegetative and Minimally Conscious States After Severe Brain Injury. MSKTC (Model Systems Knowledge Translation Center) https://msktc.org/tbi/factsheets/facts-about-vegetative-and-minimally-conscious-states-af t er-severe-brain-injury#fsmenu1
- professional, C. C. medical. (n.d.). The Glasgow Coma Scale and how experts use it. Cleveland Clinic. https://my.clevelandclinic.org/health/diagnostics/24848-glasgow-coma-scale-gcs
- Vega, I., & Vega, I. (2023, November 14). Disorders of consciousness (DOC) rehabilitation: Strategies For Success. MedBridge Blog. https://www.medbridge.com/blog/2023/02/disorders-of-consciousness-doc-rehabilitation introductory-strategies-for-success/
- Lancioni, G.E., Bosco, A., O’Reilly, M.F. et al. Assessment and Intervention with Patients with Severe Disorders of Consciousness. Adv Neurodev Disord 1, 196–202 (2017). https://doi.org/10.1007/s41252-017-0025-5
- Tung, J., Speechley, K. N., Gofton, T., Gonzalez-Lara, L. E., Graham, M., Naci, L., Peterson, A. H., Owen, A. M., & Weijer, C. (2020). Towards the assessment of quality of life in patients with disorders of consciousness. Quality of Life Research, 29(5), 1217–1227. https://doi-org.library.capella.edu/10.1007/s11136-019-02390-8
- What part of the brain is damaged in a person with a disorder of consciousness? BrainLine. (2023, December 15). https://www.brainline.org/dchub/what-part-brain-damaged-person-disorder-consciousness
- ScienceDaily. (2023, September 6). Encouraging new prospects for the treatment of consciousness disorders. ScienceDaily. https://www.sciencedaily.com/releases/2023/09/230906112434.htm
- TDCS in patients with disorders of consciousness | neurology. (n.d.-a). https://www.neurology.org/doi/10.1212/WNL.0000000000000260
- Edlow, B. L., Claassen, J., Schiff, N. D., & Greer, D. M. (2021, March). Recovery from disorders of consciousness: Mechanisms, prognosis, and emerging therapies. Nature reviews. Neurology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7734616/
- Wright, J. (2000). The Disability Rating Scale. The Center for Outcome Measurement in Brain Injury. http://www.tbims.org/combi/drs ( accessed December 20, 2023 ).* http://www.tbims.org/combi/drs/
- Sanz LRD;Aubinet C;Cassol H;Bodart O;Wannez S;Bonin EAC;Barra A;Lejeune N;Martial C;Chatelle C;Ledoux D;Laureys S;Thibaut A;Gosseries O; (n.d.). Seconds administration guidelines: A fast tool to assess consciousness in brain-injured patients. Journal of visualized experiments : JoVE. https://pubmed.ncbi.nlm.nih.gov/33616111/
- Knadmin. (2023, May 17). Disorders of consciousness. PM&R KnowledgeNow. https://now.aapmr.org/disorders-of-consciousness/
- NHS. (n.d.-a). NHS choices. https://www.nhs.uk/conditions/disorders-of-consciousness/
- Wang, J., Hu, X., Hu, Z., Sun, Z., Laureys, S., & Di, H. (2020, September 12). The misdiagnosis of prolonged disorders of consciousness by a clinical consensus compared with repeated coma-recovery scale-revised assessment – BMC neurology. BioMed Central. https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-020-01924-9
- Taberna, M., Gil Moncayo, F., Jané-Salas, E., Antonio, M., Arribas, L., Vilajosana, E., Peralvez Torres, E., & Mesía, R. (2020, January 16). The Multidisciplinary Team (MDT) approach and quality of care. Frontiers. https://doi.org/10.3389/fonc.2020.00085
- Disorders of consciousness. www.aapmr.org. (n.d.). https://www.aapmr.org/about-physiatry/conditions-treatments/rehabilitation-of-central-ne r vous-system-disorders/disorders-of-consciousness
- Update on diagnosis in disorders of Consciousness – Taylor & Francis Online. (n.d.). https://www.tandfonline.com/doi/full/10.1080/14737175.2020.1796641
- Practice guideline update recommendations: Disorders of consciousness. (n.d.). https://www.aan.com/Guidelines/Home/GuidelineDetail/926
- NHS. (n.d.). NHS choices. https://www.nhs.uk/conditions/disorders-of-consciousness/causes/
- Rancho Los Amigos level of cognitive functioning scale. Physiopedia. (n.d.). https://www.physiopedia.com/Rancho_Los_Amigos_Level_of_Cognitive_Functioning_S cale
- Disability rating scale. Disability Rating Scale at Centre for Neuro skills. (n.d.). https://www.neuroskills.com/education-and-resources/disability-rating-scale/
- Gębska-Kośla, K., Głąbiński, A., Sabiniewicz, M., Wolak, T., Wachowski, M., Kruczykowska, L., & Majos, A. (2020). The use of functional magnetic resonance imaging techniques in the evaluation of patients with disorders of consciousness: a case report. Polish journal of radiology, 85, e118–e124. https://doi.org/10.5114/pjr.2020.93664
- Androu, A., Milej, D., Norton, L., Debicki, D., & Owen, K. (2021, July 8). The potential role of fNIRS in evaluating levels of consciousness. Frontiers in Human Neuroscience. doi: 10.3389/fnhum.2021.703405
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
