Course
Fall Prevention in Inpatient Settings
Course Highlights
- In this Fall Prevention in Inpatient Settings course, we will learn about three risk factors for falls in the hospital setting.
- You’ll also learn three ways nurses can prevent falls in hospitalized patients.
- You’ll leave this course with a broader understanding of how hospitals can measure the effectiveness of fall prevention practices.
About
Contact Hours Awarded: 3
Course By:
Charmaine Robinson
MSN-Ed, BSN, RN, PHN, CMSRN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
A patient fall is described as an “unplanned descent to the floor with or without injury to the patient” (1). Falls can cause a cascade of poor outcomes, so prevention is a meaningful goal. Nurses should be familiar with the incidence of falls in inpatient settings, types of falls, risk factors, complications, impact on health care, and the nursing role in fall prevention.
Case Study:
Mary is a 76-year-old woman hospitalized with a recent hip fracture related to a fall. She is in the medical unit preparing for surgical repair of the hip fracture. She has a history of high blood pressure, high cholesterol, osteoporosis, and Alzheimer’s dementia.
She currently lives with her daughter. Prior to the fall, Mary had a steady gait and did not use any assistive mobility devices. Mary said that she lost her balance and fell in the kitchen while making breakfast.
In this course, we will follow Mary’s hospital stay until discharge.

Self-Quiz
Ask Yourself...
- Have you ever witnessed a patient fall? If so, what were the contributing factors?
- Have you encountered a case where a fall was preventable?
- Have you encountered a case where a fall was not preventable?
Incidence of Falls in Inpatient Settings
This section will discuss falls in the U.S. and around the world. This section will also compare falls in inpatient versus outpatient settings.
What is happening globally?
Falls are the second leading cause of unintentional injury deaths in the world, after road traffic injuries (2). While falls do not have to lead to severe injury or death, over 35 million falls each year are severe enough to require medical care (2). Women have the highest prevalence of falls around the world (2, 7). Location plays a role as well.
Older Adult Fall prevalence by Country:
- India: 53%
- United States: 30%
- China: 26.4%
- Japan: 13.7%
Approximately 684,000 people die from falls every year (2). Deaths related to falls are most likely to occur in older adults (age 65 and older) (2). Of all fall-related deaths around the world, 80% occur in low- and middle-income countries (2).
What is happening nationally?
Each year, over 800,000 people are hospitalized due to a fall injury in the U.S. (3). Each year, three million older adults are treated in the emergency department for injuries related to falls (3).
Falls are more likely to occur in women and older adults (over age 65), particularly to those over age 85 (4, 8). Among older adults, falls are the leading cause of fatal and nonfatal injuries (3). Over 10,000 people in the U.S. turn 65 every day and falls among this group are expected to increase (9).

While these numbers are high, they do not account for the many falls that go unreported each year. Every year, one in four older adults (over 14 million) report falling and less than half report the fall to their doctor (3).
The fall-related death rate among older adults in the U.S. (number of deaths per 100,000 older adults) has increased 30% in the last decade and is still rising (9). In 2020 alone, over 36,000 older adults died from fall-related injuries (3). The following year, in 2021, an average of 100 older adults died each day due to falls (8). Although fall incidence is highest among women, deaths related to falls are highest among men (2, 8).
Falls by race/ethnicity in the U.S.:
- American Indian/Alaska Native: 32%
- White: 28%
- Hispanic: 28%
- Black: 23%
- Asian/Pacific Islander: 16%
Incidence of Falls within Healthcare Facilities
While there is minimal data on falls that occur in hospitals globally, research shows that in nursing homes around the world, 1.5 falls occur per bed each year (7).
Hospital falls are a common occurrence in the U.S. Anywhere between 700,000 and one million people fall in the hospital each year and 1.3 million in nursing facilities (1). In 2022, falls were the most common sentinel events in hospitals (sentinel events are patient safety events that lead to harm or death) (10). While the numbers are high, falls in the hospital are on the decline.

Self-Quiz
Ask Yourself...
- What was the most common age range of the patients who fell?
- Aside from age-related risk factors, why do you think falls occur more often in nursing homes than in hospitals?
- How often did you see patients admitted to your facility after they sustained a fall?
- Have you ever had a patient tell you they fell, a while after it happened?
Types of Falls
When a patient falls, determining the type of fall that has occurred may reveal how to prevent future falls. There are three types of falls: accidental, anticipated physiological, and unanticipated physiological (1).
Anticipated Physiological
Anticipated physiological falls happen when a person is already at risk for falling. These falls are “predictable” and the reason behind the fall may be easily identifiable. A person who sustains this type of fall may have mobility limitations, altered mentation, and frequent toileting needs. Other reasons can include taking medications that cause drowsiness or confusion.
Most hospital falls can be categorized as anticipated physiological (1).
Unanticipated Physiological
Unanticipated physiological falls happen when a person is at a low risk of falling. These falls are typically unpredictable. The reason for the fall may or may not be easily identifiable. A person who sustains this type of fall may have had a sudden change in condition like a seizure, stroke, or syncopal episode. In the hospital, these falls are hard to prevent, particularly if the patient is generally healthy with no other risk factors.
Accidental
Similar to unanticipated physiological falls, accidental falls happen when a person is at a low risk of falling. These falls are related to environmental hazards. In the hospital, these falls are easily preventable and have nothing to do with the patient who sustained the fall.
Case Study Reflection: Mary is now under your care. The physician asks you to obtain a patient history to discover the type of fall that has occurred. After reviewing Mary’s case,
- What type of fall did she sustain?
- Do you have enough information to make that assessment?
Risk Factors
While age tends to be the most studied risk factor for falls in the U.S., falls can also be associated with occupation, lifestyle, medical conditions, and the environment. Falls can be intrinsic (associated with the body, like medical conditions or mobility problems) or extrinsic (caused by something outside of the body, like cluttered environments).
The following are various risk factors for falls (2,3,4,5)
- Jobs that require working at elevated heights
- Other hazardous working conditions
- Unsafe environments
- Substance or alcohol use
- Medical and other disabling conditions
- Medication side effects
- Incontinence and need for toileting assistance
- Limited mobility
- Deconditioning from physical inactivity
- Cognition problems
- Previous falls
- Older age
In one report, researchers studied U.S. falls in relation to factors including health conditions and functional ability (4). Results showed that depression was the most common medical condition associated with falls. Second was stroke. Other top conditions included arthritis and diabetes.
Results also revealed that people who report difficulty dressing or bathing had the highest number of falls, followed by those who had difficulty doing errands alone and those who had trouble concentrating or making decisions. Those who had difficulty walking or climbing stairs and those who were blind or had difficulty seeing also had high percentages of falls (4).

Self-Quiz
Ask Yourself...
- Was there ever a fall associated with a medication side effect?
- What environmental factors were most associated with the falls?
- Were most of the patients who fell ambulatory?
- What types of medical conditions contributed to the falls?
Case Study Reflection:
Mary denied feeling any dizziness or discomfort before falling. She says, “I was trying to fix breakfast and I lost my balance.” We know that Mary does not have gait problems and does not use any assistive mobility devices.
- What other questions can you ask Mary or her daughter?
Complications of Falls
Fall complications can include injury, disability, social limitations, and death. One out of every five falls result in an injury (3). These injuries may include head trauma, lacerations, hematomas, and fractures (1, 3).
Most research on fall complications are associated with falls among older adults. The most common fall complication among older adults is a fracture. Hip fractures in particular are primarily caused by falling, and over 300,000 older adults are hospitalized for hip fractures every year (3).
Complications from falls may be non-physical as well. Older adults who fall may develop a fear of falling again, which can lead to limitations in mobility, self-care, and household activities (6). One study suggested that fear of falling in older adults is a risk factor that is just as important as having previous multiple falls in terms of limiting daily activities (6). Limited activities in older adults can lead to dependency on others, limited social interactions, and disability (6).
Case Study:
Mary’s daughter says she found her mother on the floor after getting home from running errands. She says that her mother was wearing her favorite rubber-sole slippers when she found her. She denied that there were any nearby rugs or spills. She says, “This time around my mom couldn’t get up so I called emergency right away. My mom just won’t listen to me. I keep telling her to wait until I get home before she starts cooking.”
- Based on this information, is there anything else you need to ask Mary’s daughter?

Self-Quiz
Ask Yourself...
- What was the most common injury that resulted from the falls?
- Were there any falls that resulted in a fracture other than a hip fracture?
- Have you ever cared for a patient who had a fear of falling? If so, how did you calm them?
- Have you ever cared for a patient who had permanent disability that was caused by a fall?
Impact on Healthcare
This section will cover the financial implications of falls.
Falls cost the healthcare system billions each year. The older adult population in the U.S. is expanding and fall costs are projected to increase. Each year, fall-related medical costs among older adults are approximately $50 billion (3). Of that amount, about $754 million is spent on fatal injuries and the rest on non-fatal injuries (3).
Direct costs related to falls
- Hospital care
- Nursing home care
- Doctors’ services
- Other professional services
- Rehabilitation
- Community services
- Medical equipment
- Medications
- Insurance processing
Indirect costs related to falls
- Disability
- Dependency on others
- Loss of work
- Reduced quality of life
Case Study Reflection: There will be costs directly associated with Mary’s fall as well as costs related to the complications she may encounter after she is discharged from the hospital.
- What medical services do you anticipate Mary may need during her hospital stay and after discharge?

Self-Quiz
Ask Yourself...
Think back on your past experiences with patient falls.
- What were some medical services that the patients needed?
- What were some ways the falls reduced the patients’ quality of life?
- Were there any special community services that were needed by the patients or families?
Reimbursement
There are two types of fall-related injuries: fatal and non-fatal. The costs of non-fatal injuries can be covered by Medicare, Medicaid, and private pay (out-of-pocket).
Medicare is a government health insurance plan for people aged 65 and older, and Medicaid is for adults and children with limited income. Each year, Medicare pays $29 billion for non-fatal falls, Medicaid $9 billion, and out-of-pocket $12 million (3).
Payment occurs through reimbursements. For many medical conditions, the Centers for Medicare and Medicaid Services (CMS) – the government entity that oversees federal health insurance plans – provides financial reimbursement to hospitals for the care of patients who are covered through their programs. The hospital pays the initial bill and after a certain amount of time, receives reimbursement.
Hospital-acquired traumatic injuries (which may occur after a fall) were initially eligible for reimbursement until 2008, when the CMS determined that many of these injuries are “preventable” (11). Currently, if a patient falls in a hospital, CMS will not reimburse for the cost of the injury – meaning that the hospital will be responsible for the bill (1).
Case Study Reflection: Mary is over the age of 65 and may already have Medicare coverage. If so, Medicare may help to cover the costs of her fall-related injuries.
- What might you anticipate as a primary goal during Mary’s hospital stay?

Self-Quiz
Ask Yourself...
Think back on your past experiences with patient falls.
- Was there ever a time that a patient did not have insurance to cover a fall cost?
- Who addressed payment/insurance issues for the patients at your facility?
Fall Risk Assessment and Scores
Assessing fall risk factors is one of the primary ways to prevent falls in the hospital. Fall risk assessment tools are helpful in identifying patients at risk for falls and can be used to guide comprehensive assessments.
Identifying fall risks involves gathering the patient’s medical history, performing a physical assessment (for example, to determine mobility), and observing the surrounding environment. The use of fall risk assessment tools should be used upon admission and throughout the patient’s stay.
Fall risk assessments tools help to identify a fall risk diagnosis for the patient (in other words, a “fall score”). These tools are often imbedded within the electronic medical record and may send an alert to the care team should the fall risk score change, particularly if the score indicates an increased risk for falls (12).
While each hospital will adopt its own fall risk assessment tool, there are many other tools available. These tools may also be helpful in some outpatient settings.
The STEADI (Stopping Elderly Accidents, Injury, and Death) Initiative offers a coordinated approach to implementing fall prevention measures.
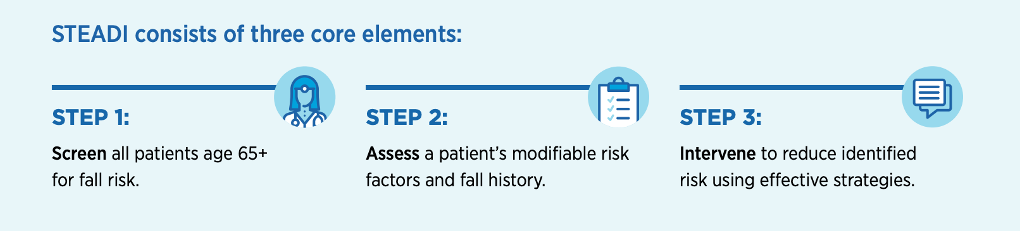
(9)

Self-Quiz
Ask Yourself...
Think back on your past experiences with using fall risk assessment tools.
- How often were you required to document fall risk assessments?
- Was the tool embedded into the electronic medical record?
- What was the protocol if a patient’s fall score increased on your shift?
Henrich II Fall Risk Model ® (HIIFRM)
The HIIFRM is intended for use in adult acute care, ambulatory, assisted living, long-term care, and community health settings. The model incorporates risk factors like medical history, cognition, medications, and mobility. The higher the score, the higher the patient’s risk of falling.
|
Henrich II Fall Risk Model ® |
|
|
Risk Factors |
Risk Points |
|
Confusion/disorientation/impulsivity |
4 |
|
Symptomatic depression |
2 |
|
Altered elimination |
1 |
|
Vertigo/dizziness |
1 |
|
Gender (male) |
1 |
|
Administered antiepileptics (anticonvulsants) |
2 |
|
Administered benzodiazepines |
1 |
|
Get-Up-and-Go-Test: “Rising from a Chair” |
|
|
Ability to rise in a single movement – no loss of balance with steps |
0 |
|
Pushes up, successful in one attempt |
1 |
|
Multiple attempts, but successful |
3 |
|
Unable to rise without assistance during test |
4 |
|
(Total score of 5 or greater = high risk for falls) |
Total Score: |
(12)
Morse Fall Scale (MFS)
The MFS is widely used in acute care settings, both hospitals and long-term care facilities. The scale incorporates risk factors like history of falling, secondary diagnosis, mental status, and whether the patient has intravenous (IV) fluids infusing. The higher the score, the higher the patient’s risk of falling.
|
Morse Fall Scale |
||
|
Item |
Item Score |
Patient Score |
|
History of Falling (immediate or within 3 months) |
No: 0 Yes: 25 |
|
|
Secondary Diagnosis |
No: 0 Yes: 15 |
|
|
Ambulatory Aid
|
0 15 30 |
|
|
IV/Heparin Lock |
No: 0 Yes: 20 |
|
|
Gait/Transferring
|
0 10 20 |
|
|
Mental Status
|
0 15 |
|
|
*Patient clutches onto furniture when ambulating Score: 0: No risk for falls | <25: Low risk | 25-45: Moderate risk | >45: High risk |
Total Score: |
|
(13)
STRATIFY Risk Assessment Tool
The STRATIFY tool is typically used in hospital settings. The scale incorporates risk factors like recent history of falls, visual impairments, frequent toileting, and mobility. The higher the score, the higher the patient’s risk of falling.
|
STRATIFY Risk Assessment Tool |
|||
|
No. |
Question |
Yes/No |
|
|
1 |
Is the patient present to hospital with a fall or has he or she fallen on the ward since admission (recent history of fall)?  |
Yes = 1 |
No = 0 |
|
2 |
Is the patient agitated? |
Yes = 1 |
No = 0 |
|
3 |
Is the patient visually impaired to the extent that everyday function is affected? |
Yes = 1 |
No = 0 |
|
4 |
Is the patient in need of especially frequent toileting? |
Yes = 1 |
No = 0 |
|
5 |
Does the patient have a combined transfer and mobility score of 3 or 4? (Calculate below)
Transfer score: Choose one of the following options which best describes the patient’s level of capability when transferring from a bed to a chair:
0 = Unable 1 = Needs major help 2 = Needs minor help 3 = Independent
Mobility score: Choose one of the following options which best describes the patient’s level of mobility:
0 = Immobile 1 = Independent with the aid of a wheelchair 2 = Uses walking aid or help of one person 3 = Independent
Combined score (transfer + mobility): ____________
|
Yes = 1 |
No = 0 |
|
Score: 0 = Low risk | 1 = Moderate risk | 2 or above = High risk |
Total Score: |
||
(14)
Case Study Reflection: As you do your assessment, Mary’s daughter reveals that her mother has fallen once before (last year) but did not sustain any injuries. She says, “Mom was cooking once again. This time I was asleep. I don’t like her cooking by herself, but she won’t listen to me. She can be forgetful sometimes.”
You perform a new cognitive assessment on Mary. Mary is alert and completely oriented but now she does not remember her fall.
- What can you conclude may be a contributing factor to Mary’s fall?

Self-Quiz
Ask Yourself...
Think back on your past experiences with using fall risk assessment tools.
- Aside from mobility, what were some other sections within tools you have used?
- Did using the tool help to alert you to your patients’ fall risks?
Nursing Implications: Fall Risk Prevention Strategies
This section will cover the assessment, diagnosis, and implementation portion of the nursing process by addressing the nurse’s role in fall risk assessments, interventions, and teaching.
While there are many ways nurses can prevent patient falls in general, there are fall hazards that are primarily present in the inpatient setting, for example, patients attached to IV equipment and supplies (like pumps, poles, and tubing).
In addition, patients in the hospital are admitted for a variety of illnesses and medical conditions that may place them at a high risk for falls when they would not have any risk factors otherwise. After determining a patient’s risk for falls, the nurse should tailor the care plan to address each risk factor.
Although some falls are unpreventable (like unanticipated falls), nurses can prevent accidental and anticipated falls by creating fall prevention care plans that consider the following interventions: environment, gait and mobility, elimination, mentation, and medications (5, 15).

Environment
- Ensure that there is proper lighting in patients’ rooms when assisting with care.
- Keep the halls and rooms free of clutter and walking pathways clear.
- Report any uneven flooring or broken/ineffective equipment to the engineering/maintenance team (through appropriate channels).
- Keep bed wheels locked at all times except during bed transportation.
- Keep the patient’s personal items within reach.
- Keep the patient’s call light/button within reach.
Gait and Mobility
- Ensure that ambulatory patients wear non-slide footwear.
- Encourage use of assistive devices as needed (walkers, canes, patient transfer equipment).
- Assist patients with mobility needs.
- Encourage patients to participate in physical therapy (if ordered).

Elimination
- Check on patient regularly (frequent rounding).
- Set a toileting/continence care schedule.
Mentation
- Check on patients regularly.
- Set an activities schedule.
- Use alarms on beds and chairs as needed.
- Use floor mats near beds and chairs (to prevent injuries should the patient fall).
- Assess alcohol/drug withdrawal and initiate protocol per facility.
- Assess for delirium and initiate protocol per facility.
Medications
- Consult pharmacists about medications as needed.
- Assess for orthostatic hypotension and initiate protocol per facility.

Self-Quiz
Ask Yourself...
Think back on your past experiences with patient falls and facility fall prevention practices.
- What were some environmental hazards that contributed to the falls?
- What types of medications were the patients taking at the time of the falls?
- Was there ever a time a family member contributed to a patient’s fall?
- What did your facility recommend preventing falls associated with IV poles?
- How often were you required to perform rounding on your patients (checking on patients)?
Quality Improvement
This section will cover the evaluation portion of the nursing process by addressing quality improvement practices to prevent hospital falls.
“Quality improvement involves setting goals (or initiatives) and standards of care. The goal of quality improvement is to improve patient outcomes at a systematic level where everyone involved is on the same page. Although possibly unaware, all care team members are involved in quality improvement. Nursing leaders design, manage, and evaluate program initiatives. Staff nurses and other care team members follow protocols that are often developed from these initiatives” (18).

Self-Quiz
Ask Yourself...
Think back on your past experiences with fall prevention practices at a facility.
- What fall prevention practice did your facility stress the most?
- Aside from reducing the number of falls, what were other fall prevention goals at your facility?
- What would happen if your unit did not meet fall prevention goals?
Falls as a Nursing Quality Indicator
The Falls Management Program: A Quality Improvement Initiative for Nursing Facilities is a guide designed by the Agency for Healthcare and Research Quality (AHRQ) – an agency that monitors fall data in the U.S. This guide is designed to help health facilities implement a structured fall prevention initiative based on QI (15).
Nursing QI initiatives are steps that facilities or organizations take to “initiate” change. Fall-related nursing QI initiatives are moves that facilities make to prevent falls. More than eight million falls require medical attention or limit activity for at least a day; however, research shows that one-third of falls are preventable (1, 9).
The 2008 CMS decision to stop reimbursements for hospital fall-related injuries may have led many hospitals to make drastic changes to their fall prevention programs to avoid the high costs (11). While it is clear the impact that falls have on patients, families, and the general healthcare system, healthcare facilities engage in QI to also address the adverse consequences that falls have on the facility itself. Falls can impact facilities in the following ways (15):
- Increased paperwork for staff
- Increased levels of care required for those who fall
- Poor survey results
- Lawsuits
- High insurance premiums
Falls prevention QI initiatives can be aimed at reducing falls, related injuries, and/or associated costs. A 2023 research study highlighted how a particular fall prevention program led to significant cost benefits for a group of health facilities (11).
Researchers evaluated the cost benefits of a fall prevention program implemented across eight facilities in the U.S. over a five-year span. The cost to implement the program was approximately $268,000. The results revealed that out of the 900,635 patients involved in the study, 567 falls were prevented. This intervention saved the facilities about $22 million total. The researchers projected a nationwide savings of $1.82 billion in health care costs with the implementation of their program.
Another research study highlighted how the use of a nurse-led fall prevention tool kit resulted in cost savings for 14 adult medical units in the U.S (19). Researchers studied 37,231 patients over a three-year span. Results revealed an adjusted 15% reduction in falls and an adjusted 35% reduction in injurious falls.
To monitor the falls that occur within a facility, quality indicators (or measures) are used. “Quality measures are tools that measure a system’s health care goals and/or ability to provide high-quality care (20). In simple terms, quality measures are specific ways that systems (governments, states, organizations, etc.) can show how they are making progress in meeting goals” (18).
Case Study Reflection: Mary returns from surgery without complications. Mary has a urinary catheter in place and IV fluids infusing. You medicate her for hip pain with a low-dose opioid pain medication. The surgeon states that Mary will start physical therapy tomorrow. Mary’s daughter says that she has to work tonight and there is no one who is able to stay the night with Mary in the hospital. Mary’s fall score has now increased.
- What new factors contributed to this increase?

Self-Quiz
Ask Yourself...
Think back on your past experiences with fall prevention practices at a facility.
- Were you ever afraid to report a fall due to fear of punishment?
- Were x-rays required after a patient fell at your facility?
- How did you know which patients were at risk for falls in your facility?
- Was the fall incident reporting system at your facility easy to use?
- Was there a difference in the way you were required to report a fall that was witnessed versus one that was unwitnessed?
Nursing Implications
Fall prevention teaching is vital for patient safety. Along with identifying fall risk factors and implementing fall prevention practices, nurses should ensure that patients and families are on board with the fall prevention plan. Fall prevention education may vary depending on if the teaching is provided during the inpatient stay or upon discharge.

Self-Quiz
Ask Yourself...
Think back on your past experiences with fall prevention practices at a facility.
- In what ways could nurses give opinions about ways to prevent falls on your unit?
- Has your falls documentation ever been audited (or have you ever been asked to explain your documentation)?
- Have you ever attended a quality improvement meeting of any kind?
- Were you ever a part of a fall prevention team? If so, what goals did you and your team set?
Inpatient teaching
Inpatient fall prevention teaching focuses on encouraging patients and families to comply with safety protocols that are already in place at the hospital. Patients should be instructed to call for help prior to getting out of bed (as applicable), wear non-slid footwear, and use assistive devices as instructed. Patients should be made aware of the risk factors for falls, how falls can happen in the hospital, and the complications associated with falls. Upon admission to the hospital, patients should be educated on the importance of reporting medical conditions, alcohol or drug use, medications, mobility limitations, and toileting needs, as these will affect the care plan.
Discharge teaching
To prevent falls after discharge from the hospital, the nurse should educate the patient and family on ways to assess the home environment for fall hazards. Older adults in particular, who have had a hospital stay are more likely to fall within the first month after discharge (16). For this reason, discharge teaching on fall prevention for the older adult patient (and family) is imperative. Fall prevention education may be reinforced with written instructions as needed.
The following home fall hazards checklist may be helpful for use during teaching (17).
- Are there objects on the floors/stairs?
-
- Encourage the patient and family to keep the floors clutter-free.
- Do you (or your loved one) have to walk over or around wires or cords?
-
- Encourage the patient and family to coil or tape cords and wires next to the wall.
- When walking through a room, do you (or your loved one) have to walk around furniture?
-
- Encourage the patient and family to get help moving the furniture to make a clear path.
- Are the stairs broken or uneven? Is the carpet on the stairs loose or torn? Are stair handrails loose or broken?
-
- Encourage the patient and family to repair any problems with the stairs, carpeting, or handrails.
- Is the path from the bed to the bathroom dark?
-
- Encourage the patient and family to keep all walking paths visible with proper lighting.
- Do you have rugs on hard flooring?
-
- Encourage the patient and family to use a non-slip backing (or double-sided tape) for the rugs.
- Do you (or your loved one) keep the items used often on high shelves?
-
- Encourage the patient and family to keep items that are used often on lower shelves (waist-high).
- Is there a light near the bed? If so, is the light hard to reach?
-
- Encourage the patient and family to keep a lamp near the bed within an arm’s reach.
- Is the tub/shower floor slippery?
-
- Encourage the patient and family to place a nonstick rubber mat in the tub/shower.
- Do you (or your loved one) need support when getting in and out of the tub/shower?
-
- Encourage the patient and family to get help to install grab bars for the tub.
Case Study Reflection: You talk to the physician about Mary’s memory loss. The physician speaks to Mary and her daughter and determines that the memory loss is mild and is related to her history of dementia. Shortly afterwards, Mary is taken for surgery. You use this time to speak with Mary’s daughter about possible home fall hazards.
- What are some fall prevention strategies you can teach that may be helpful for when Mary returns home after a short stay in a rehabilitation facility?

Self-Quiz
Ask Yourself...
Think back on your past experiences with patient falls.
- How did you handle situations in which patients were resistive to fall prevention education?
- What were some reasons why patients did not press the call light/button even after instruction?
- What types of educational resources did you give patients and families during teaching?
- Did you adjust your teaching based on if the patient was newly admitted versus ready for discharge?
Fall Rates
First and foremost, facilities should know how many patients are falling. Fall rates reveal how often patients are falling and which patients are falling. For this reason, fall reporting is critical. Incident reporting systems can be helpful in gathering fall data. However, facilities must ensure that staff members feel safe when reporting falls (no retaliation for reporting) so that fall rates will be accurate.
How nurses can help:
- Report every fall (witnessed or unwitnessed)
Fall-related Injuries
Facilities should know which falls result in injuries versus not. Falls that result in injuries are most costly. Therefore, in order to make improvements, facilities should keep a record of all injuries that occur after a fall. Incident reporting systems can be helpful in gathering this information. Facilities can use this information to implement a protocol in which all patients who fall and report pain must receive an x-ray.
How nurses can help:
- Report every fall (witnessed or unwitnessed)
- Perform detailed assessments after every fall (like pain and skin assessments)
- Document all assessments accurately and timely
While declining fall rates and fall-related injuries within a facility is a great sign, these rates alone do not necessarily reveal that a fall prevention practice (or program) is the reason why there are less falls (5, 15).
For example, a facility may see an increase in falls during flu season. At the same time, the facility may have implemented a fall prevention program. After flu season is over, the facility may notice that falls have declined.
The decline in falls may not be related to the fall prevention program. The original increase in falls may have been related to an increase in the number of elderly patients admitted to the facility for respiratory illness during flu season.
While it may be unclear if a fall prevention program is the cause of declining fall rates, facilities can use the following two types of quality measures (recommended by the AHRQ) to evaluate if staff members are performing the appropriate safety tasks (15).
Fall risk factor assessment within 24 hours of admission.
Fall risk factor assessments within 24 hours of admission is a quality measure that facilities can use to see if nurses are using fall risk factor tools appropriately early in the admission process (like the Henrich II Fall Risk Model or Morse Fall Scale).
Facilities can also use this quality indicator to evaluate if nurses are using fall risk assessment tools throughout the patient’s entire stay. This data is often gathered through patient chart audits.
How nurses can help:
- Perform fall risk assessments (using tools provided by the facility) in a timely fashion.
- Document fall risk assessments accurately and timely.
Care-planning addresses each risk factor identified.
Facilities can measure if a fall prevention program is working by reviewing patient charts to see if each risk factor that has been identified is being addressed within the patient’s care plan. For example, a nurse may use the Henrich II Fall Risk Model to assess a patient’s risk for falls and document that the patient is confused and has limited mobility. The QI team may perform an audit by reviewing the nurse’s documentation. The team may find that the nurse documented safety interventions that addressed both the patient’s confusion and mobility issues. In this case, the QI team can prove that nurses are effectively addressing a patient’s fall risk factors.
How nurses can help:
- Perform fall risk assessments (using tools provided by the facility) in a timely fashion
- Document fall risk assessments accurately and timely
- Perform interventions that address each fall risk in a timely fashion
- Document interventions performed, accurately and timely
Case Study Reflection: You will care for Mary over the next three days. You are creating a plan of care to address her fall risks. First, you will update her fall score daily.
- Can you think of fall prevention measures that you can include in Mary’s care plan to address each of her risk factors: recent fall, occasional forgetfulness, limited mobility, elimination changes, and opioid use?

Self-Quiz
Ask Yourself...
Think back on your past experiences with fall prevention practices at a facility.
- Was there ever a time where there were many falls occurring on your unit? If so, what do you think was happening?
- How often were you required to update a patient’s fall score at your facility?
- In what ways did you show that you were addressing your patients’ fall risk factors?
- What time frame was required to perform fall risk assessments for newly admitted patients?
- What were some practices you initiated to help reduce your patients’ fall risks?
The Joint Commission Recommendations
This section will cover The Joint Commission’s recommendations for healthcare facilities in preventing falls.
The Joint Commission is an organization that conducts surveys to monitor and evaluate health facilities in the delivery of patient care. The mission of The Joint Commission is to inspire health care organizations to excel in providing safe, effective, and quality care (21). The Joint Commission recommends the following seven actions in the prevention of falls in healthcare facilities (22).
1. Raise Awareness about Fall Prevention
Recommendation: “Lead an effort to raise awareness of the need to prevent falls resulting in injury.”
Healthcare facilities are encouraged to communicate safety information to all staff members and promote the use of fall prevention equipment like bed alarms. Facilities may appoint a fall prevention champion to serve as a liaison.
2. Create a Fall Prevention Leadership Team
Recommendation: “Establish an interdisciplinary falls injury prevention team or evaluate the membership of the team in place to assure organizational infrastructure and capacity to reduce injury risk from falls.”
Healthcare facilities are encouraged to promote interdisciplinary collaborative efforts to reduce falls. Team members may be pulled from various departments including nursing, medicine, pharmacy, environmental services, allied care, and risk management.
3. Use Standardized Fall Risk Screening Tools
Recommendation: “Use a standardized, validated tool to identify risk factors for falls.”
Healthcare facilities are encouraged to use standardized tools to identify risk factors for falls. These tools may include the Hendrich II Fall Risk Model or Morse Fall Scale. Along with tools, comprehensive individualized fall risk assessments should be performed. Assessments should include the patient’s age, gender, cognitive status, and level of function.
4. Create Individualized Care Plans
Recommendation: “Develop an individualized plan of care based on identified fall and injury risks, and implement interventions specific to a patient, population or setting.”
Healthcare facilities are encouraged to create individualized plans of care for each patient based on identified fall risks. These care plans should include interventions to address each risk.
5. Use a Standardized Communication Process
Recommendation: “Standardize and apply a hand-off communication process.”
Healthcare facilities are encouraged to create a process or protocol for caregivers on how to communicate with one another which patients are at risk for falls. Information exchange may occur in verbal or written format (like during shift change reports) and should include areas of risks and ways to address each risk.
6. Provide Fall Prevention Patient Education
Recommendation: “Standardize and apply a one-to-one education of each patient at the bedside.”
Healthcare facilities are encouraged to ensure that caregivers are trained to provide individualized patient education on fall prevention. Educational materials should include information on causes of falls, risks, prevention strategies, and goals and review.
7. Conduct Post-Fall Management
Recommendation: “Conduct post-fall management, which includes: a post-fall huddle; a system of honest, transparent reporting; trending and analysis of falls which can inform improvement efforts; and reassess the patient.”
Healthcare facilities are encouraged to ensure that there is a huddle (or meeting) shortly after every patient falls. Huddle participants should include the patient (if able) and involved staff members at all levels. The huddle should be guided by a post-fall huddle tool or form.
Huddle discussion should include:
- When and where the fall happened
- How and why the fall happened
- Other factors that may have contributed to the fall
- If there were appropriate interventions in place
- Where to adjust the patient’s plan of care
Health facilities are encouraged to ensure that each patient is continually reassessed during the post-fall period. Assessments should include medication changes, cognition, and functional status. Lastly, health facilities are encouraged to continually report and analyze contributing factors (may be done through a designated fall prevention team). The data should be used to modify current fall prevention quality improvement projects or develop new ones.
Case Study Reflection: You have implemented Mary’s care plan over the last three days. The physician has determined that Mary’s fall was related to short-term memory loss secondary to dementia. Mary has been cleared by the physician for transfer to a rehabilitation facility for a few weeks before returning home. Her daughter has received a social services consultation for caregiver support resources and will hire a caregiver to help at home.
Congratulations! Mary did not sustain a hospital fall and remained safe while under your care.

Self-Quiz
Ask Yourself...
Think back on your past experiences with fall prevention practices at a facility.
- What was the protocol when a patient fell on your unit?
- Have you ever attended a post-fall huddle/meeting? If so, what was discussed?
- Have you ever used a bed or chair alarm? If so, was it helpful in preventing falls?
- During nurse shift report, was there a particular way you had to communicate which patients were at risk for falls?
Conclusion
Falls are not only detrimental to patients and families, but they also negatively impact healthcare facilities and are costly to the healthcare system as a whole. Many falls in the hospital are preventable. Through fall risk assessments, safety interventions, patient education, and timely and accurate documentation, nurses can help to prevent patient falls and the associated complications and morbidity.

References + Disclaimer
- Agency for Healthcare Research and Quality. (2013). Preventing falls in hospitals. Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/fall-prevention/toolkit/overview.html
- World Health Organization. (2021). Falls: Key facts. Retrieved from https://www.who.int/news-room/fact-sheets/detail/falls
- Center for Disease Control and Prevention. (2023a). Older adult fall prevention. Retrieved from https://www.cdc.gov/falls/
- Bergen, G., Stevens, M., Kakara, R., & Burns, E. (2019). Understanding modifiable and unmodifiable older adult fall risk factors to create effective prevention strategies. American Journal of Lifestyle Medicine, 15(6):580-589. doi:10.1177/1559827619880529
- Dykes, P., Adelman, J., Adkison, L. et. al. (2018). Preventing falls in hospitalized patients. American Nurses Association. Retrieved from https://www.myamericannurse.com/preventing-falls-hospitalized-patients/
- Liu, M., Hou, T., Li, Y. et al. (2021). Fear of falling is as important as multiple previous falls in terms of limiting daily activities: a longitudinal study. BMC Geriatrics 21(350). https://doi.org/10.1186/s12877-021-02305-8
- Salari, N., Darvishi, N., Ahmadipanah, M. et. al. (2022). Global prevalence of falls in the older adults: a comprehensive systematic review and meta-analysis. Journal of Orthopedic Surgery and Research, 17(334). https://doi.org/10.1186/s13018-022-03222-1
- Centers for Disease Control and Prevention. (2023b). Morbidity and Mortality Weekly Report: Nonfatal and fatal falls among adults aged ≥65 years — United States, 2020–2021. Retrieved from https://www.cdc.gov/mmwr/volumes/72/wr/mm7235a1.htm
- Centers for Disease Control and Prevention. (2020). Older adult falls: A growing problem that can be prevented. Retrieved from https://www.cdc.gov/steadi/pdf/steadi_clinicianfactsheet-a.pdf
- The Joint Commission. (2023a). New sentinel event data available for first 6 months of 2023. Retrieved from https://www.jointcommission.org/resources/news-and-multimedia/newsletters/newsletters/joint-commission-online/oct-18-2023/se-data/
- Dykes, P., Curtin-Bowel, M., & Lipsitz, S. (2023). Cost of inpatient falls and cost-benefit analysis of implementation of an evidence-based fall prevention program. JAMA Health Forum 4(1): e225125. doi:10.1001/jamahealthforum.2022.5125
- Hendrich, A. (2023). Fall risk assessment for adults: The Hendrich II Fall Risk Model ®. Try This ® Issue Number 8. Hartford Institute for Geriatric Nursing. Retrieved from https://hign.org/sites/default/files/2022-11/Hendrich%20II%20Fall%20Risk%20Model.pdf
- Agency for Healthcare Research and Quality. (2023a). Preventing falls in hospitals: Tool 3H: Morse Fall Scale for identifying fall risk factors. Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/fall-prevention/toolkit/morse-fall-scale.html
- Agency for Healthcare Research and Quality. (2023b). Preventing falls in hospitals: Tool 3G: STRATIFY Scale for identifying fall risk factors. Retrieved from https://www.ahrq.gov/patient-safety/settings/hospital/fall-prevention/toolkit/stratify-scale.html
- Agency for Healthcare Research and Quality. (2017). The falls management program: A quality improvement initiative for nursing facilities. Retrieved from https://www.ahrq.gov/patient-safety/settings/long-term-care/resource/injuries/fallspx/man1.html
- Centers for Disease Control and Prevention. (2021). STEADI-older adult fall prevention: Inpatient care. Retrieved from https://www.cdc.gov/steadi/inpatient-care.html
- Centers for Disease Control and Prevention. (2017). Check for safety: A home fall prevention program for older adults. Retrieved from https://www.cdc.gov/steadi/pdf/STEADI-Brochure-CheckForSafety-508.pdf
- Robinson, C. (2023). Pressure injury prevention, staging, and treatment. Nursing CE Central Courses Page. https://www.nursingcecentral.com
- Dykes, P., Burns, Z., Adelman, J. et. al. (2020). Evaluation of a patient-centered fall-prevention tool kit to reduce falls and injuries: A nonrandomized controlled trial. JAMA Network Open, 3(11): e2025889. doi:10.1001/jamanetworkopen.2020.25889
- Centers for Medicare and Medicaid Services. (2023). Quality measures. Retrieved from https://www.cms.gov/medicare/quality/measures
- The Joint Commission. (2023b). Who are we? Retrieved from https://www.jointcommission.org/who-we-are/
- The Joint Commission. (2015). Sentinel alert event: Preventing falls and fall-related injuries in health care facilities. Retrieved from https://www.jointcommission.org/-/media/tjc/newsletters/sea-55-falls-4-26-16-final-2-combined.pdf
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
