Course
Family Planning and Contraceptive Methods
Course Highlights
- In this Family Planning and Contraceptive Methods course, we will learn about common side effects, including severe possible side effects, of contraception.
- You’ll also learn alternatives hormonal contraception, such as non-hormonal contraception.
- You’ll leave this course with a broader understanding of the clinical criteria for prescribing contraception.
About
Contact Hours Awarded: 3
Course By:
Sadia A., MPH, MSN, WHNP-BC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
When hearing the phrases family planning or contraceptive methods, what comes to mind? If you’re a nurse, you’ve definitely heard of family planning or contraception before. Even as a student nurse or maybe before nursing school, conversations about family planning, pregnancy, and contraception existed every so often. Presently, clients seek guidance and information on various health topics from nurses, including family planning and contraceptive education management during their lifetime. The information in this course will serve as a valuable resource for nurses of all specialties, education levels, and backgrounds to learn more about family planning and contraceptive methods for people.
Defining Family Planning and Contraceptive Methods
Family planning and contraceptive methods are very popular health topics in mainstream media, scientific literature, and social norms. Family planning is often defined as the ability to plan when to or if someone desires to start a family. Contraceptive methods, such as the hormonal contraceptive pill or condom, are options that can assist in pregnancy prevention during instances of vaginal intercourse. With modern advances in the past fifty years, even in the past decade, regarding contraception, and the rise of people wanting to assert more autonomy over their reproductive health, family planning and contraceptive methods are very common topics for nurses to serve as a trusted information source.
Family planning and contraception is not limited to those with a uterus, as several people with a penis have family planning concerns as well. Often times, in many health care settings, family planning and contraceptive method discussions focus on women and clients with a uterus. However, it is important to recognize that people with a penis and sperm have the capacity to get someone pregnant during their lifespan from adolescence to geriatric ages. In addition, once someone with a uterus has their menarche (age of first menstrual cycle) until they have reached menopause (the cessation of menstrual cycles), that person has the capacity to become pregnant. Given the nature of family planning, pregnancy, social norms, health implications, and medication interactions, it is important to be aware of various family planning and contraceptive methods for your clients (1,2,3).

How Prevalent Are Family Planning and Contraceptive Methods?
Family planning and contraceptive methods are extremely prevalent in the United States and around the world. It is estimated that at least 90% of people who engage in vaginal intercourse will use at least one form of contraception in their lifetime. Since there are many family planning methods that do not require a prescription or medical consult, such as the withdrawal method or abstinence, many instances of using contraceptive methods can also be unaccounted for. Regardless, the need for family planning and contraceptive methods will be a continuing concern for all clients of reproductive capacity since pregnancy, birth, and parenting can have significant influences on someone’s health and livelihood.
While some people also use family planning methods for non-pregnancy prevention purposes, such as the use of hormonal contraception to assist with menstrual cramping, many people rely on family planning methods of all sorts to aid in their family planning journey as they see fit. Family planning also is a personal, cultural, and social health paradigm for many people, especially people with a uterus. As a result, culturally sensitive and nuanced conversations can be had regarding contraception to ensure evidence-based, medically accurate care (1,2,3,4).
What Are Some General Family Planning and Contraceptive Considerations?
While many forms of contraception can be obtained over the counter (OTC) without a prescription or initiated without any medical intervention, many people seek guidance from health care professionals regarding contraception. General family planning and contraceptive considerations would be to prioritize the client’s desires regarding their family size, experiences with prior contraception, and interest in any current contraception. Family planning can be considered in client populations who have reproductive capacity, from adolescents to those in perimenopause and those in retirement homes.
Assuming by someone’s age, physical appearance, or health status alone their contraceptive needs does a disservice to a client and can influence their ability to trust in the health care system. In addition, given that hormonal contraception, permanent contraceptive methods, such as surgical interventions, and OTC methods all have possible risks and benefits, a detailed health history of a client is essential for contraceptive counseling. For instance, if a client with a uterus has had a history of a pulmonary embolism, that client would not eligible to be on estrogen-containing hormonal contraception. Yet, this client is eligible for non-hormonal contraception, such as a tubal ligation or cervical cap. Even some forms of hormonal contraception that contain progestin only might be a good fit for a person with a history of a blood clot.
Given the wide range of contraceptive options, the range of health conditions a person can experience, and the many ways contraception is extremely personalized for each client, education and awareness of various methods is essential (1,2,3,4).
What Is Family Planning and Contraceptive Considerations Are Left Unmet?
If family planning and contraceptive considerations are left unmet, a client is at risk for miseducation on pregnancy and could result in an unintended pregnancy. Unintended pregnancies compromise about 50% of pregnancies presently, and they can have life-long lasting consequences on the pregnant person. While some people will terminate a pregnancy, some people are unaware of their pregnancy status, can enter prenatal care late, and can have undetected pregnancy complications. Though many people use the Internet, social media, and social networks to learn about family planning and contraception, not all information is medically accurate, leading someone to become pregnant without their knowledge. As a result, being aware and having conversations about contraceptive needs is essential when working with clients of reproductive potential (1,2,3,4,5).
What Are Family Planning and Contraceptive Options?
There are several prescription, surgical, and OTC options that can be used in family planning and for contraceptive purposes. This course will start by discussing hormonal options, such as the pill, shot, ring, patch, implant, and intrauterine device (IUD), and then discuss the non-hormonal options, such as condoms, surgeries, and abstinence. It is important to note that there is no medication or procedure to 100% prevent pregnancies alone. Even if someone takes a contraceptive pill every single day at the same time, has a vasectomy, or an IUD, if that client has a uterus and eggs and is engaging in vaginal intercourse with someone with a penis that has sperm, they are still at risk of pregnancy.
Family planning and contraceptive options can reduce the risk of pregnancy, but they do not 100% eliminate the risk of pregnancy. The only 100% method to prevent pregnancy is to abstain from vaginal intercourse. It is important to remind clients that no medication or intervention is 100%, and it is still possible to become pregnant when using contraception. Certain contraceptive methods, such as the hormonal contraceptive implant, has a higher rate of pregnancy prevention than the hormonal vaginal ring, but pregnancy is still possible. It is also possible that some people will use multiple forms of contraception at once, such as one partner receiving the hormonal contraceptive shot and the other partner using a condom. Often times, multiple forms of contraception can be used in family planning (1,2,3,4,5,6).
How and Where Are Family Planning and Contraceptive Options Used?
Medications for family planning and contraception are used all over America. From universities to emergency rooms to neurology offices and primary care clinics, family planning and contraceptive methods are among the most popular medications and interventions a nurse can encounter at work. Family planning and contraceptives can be prescribed by any licensed health care provider such prescribing authority, such as an advanced practice registered nurse (APRN), physician assistant, or doctor. In fact, some states and institutions are also permitting pharmacists to write and dispense hormonal contraceptive pills from pharmacies directly. Most pharmacies dispense hormonal contraception, and non-hormonal contraception, such as condoms and spermicide, are readily available at several stores.
Because of the ubiquitous nature of contraception, it is important to ask clients about their medical history. Many people can often forget about their contraceptive choice, especially if it was a surgical intervention, such as a vasectomy or tubal ligation (1,2,3,4,5,6).
What Is the Clinical Criteria for Prescribing Contraceptive Medications?
Clinical criteria for prescribing contraception is often determined by institutional guidelines, contraceptive guidelines, client preference, and health history. Several reproductive health organizations, public health agencies, and institutions often have their own guidelines and parameters for contraceptive prescribing. In addition, because there are hundreds of commercial hormonal contraceptive pills, various contraceptive patches, health conditions, and allergies, clinical criterium is something to be familiar with when discussing contraception. For instance, if someone wants to use condoms, several brands of condoms are made with latex, a top allergen which can trigger severe, life-threatening reactions. Another instance is with smoking and its risk of blood clots in addition to the risk of hormonal contraception as well. Depending on client history and clinical presentation, many options can be considered as well as be severely contraindicated (1,2,3,4,5,6).
What Is the Average Cost for Contraceptive Medications?
Cost for family planning and contraception can significantly vary depending on the type of contraception, insurance, dosage, administration route, frequency, and other factors. Cost is among a leading reason why many clients cannot maintain their medication regime in general. In fact, many people go through various contraceptive means through their lifespan, which can place a significant burden of cost on the client as well. If cost is a concern for your client, consider reaching out to your local pharmacies or client care teams to find cost effective solutions for your clients (7).

Self-Quiz
Ask Yourself...
- What are some possible complications of untreated or unmanaged family planning concerns?
- What are some common medications that can be prescribed to address family planning needs?
- What are some challenges clients may face when trying to receive family planning and contraception care?
- What are some contraceptive trends you have noticed in your place of work among your clients?
- How can cost affect family planning and contraceptive needs?
Contraceptive Medication
Health care provider professional discretion and client condition should guide therapy of hormonal and non-hormonal contraceptives. Consider reviewing a client’s medication history, clinical presentation, and health history prior to prescribing hormonal contraceptive pills. Consider consulting with a contraceptive specialist or other relevant clinical staff regarding medication management. It is also important to note that there are several contraindications for hormonal contraception, such as smoking status, age, or body mass index (BMI), that should be verified and addressed with clinical guidelines and your institution’s policy on contraceptive prescribing. Hormonal contraception that is initiated on the first day of someone’s period is considered effective immediately, whereas hormonal contraception initiated outside of someone’s period can take up to 7 days for effectiveness to reach its peak (1,2,8,9).

Hormonal Contraceptive Pills
Contraceptive Pills Drug Class
The hormonal contraceptive pill is often regarded as one of the greatest inventions and medical interventions of our lifetime. Originally when the hormonal contraceptive pill was introduced on the market, it was a pill that only contained estrogen. As a result of several severe side effects from an estrogen-only pill, such as blood clots and severe mood changes, and severe public health injustices in Puerto Rico, the estrogen-only pill is no longer available in the USA market. That said, presently, in the U.S., there are two main types of hormonal contraceptive pills – those that contain synthetic estrogen and synthetic progesterone and those that contain synthetic progesterone alone. Synthetic estrogen can be ethinyl estradiol or estetrol. Synthetic progesterone can be divided into various progestins, such as norethindrone, norgestrel, levonorgestrel, or drospirenone.
In non-USA countries, there are other synthetic progestins available in hormonal pills, such as dieongest. Combined hormonal contraceptive pills that contain both synthetic estrogen and progestin are among the most widely used form of hormonal contraception and are extensively popular among several people with a uterus of reproductive capacity. Combined hormonal contraceptive pills also come in various dosages, such as a lower-dose estrogen containing pill compared to one with drospirenone or levonorgestrel.
In addition, there are also progestin-only hormonal contraceptive pills available in the USA that contain either norethindrone, norgestrel, or drospirenone alone. The only hormonal contraceptive pill that is available OTC is the norgestrel only pill. All other hormonal contraceptive pills, including the other progestin only pills, need a prescription. All forms of hormonal contraceptive pills need to be taken daily, ideally at the same time, for the most maximum effectiveness for pregnancy prevention. Also, all forms of hormonal contraception, including the pills, containing estrogen poses a risk of increased blood clots because of the nature in which estrogen can affect someone’s clotting factors and clotting cascade.
It is recommended to also evaluate someone’s liver and B12 levels upon administration of hormonal contraceptive pills since pills in general are metabolized by the liver. B12 levels can also be altered by hormonal contraceptive pills in some clients as well. Studies have shown that many hormonal pills are typically 93% effective at pregnancy prevention because of user error, missing a dose, and the like. When taken consistently, hormonal contraceptive pills can be highly effective at pregnancy prevention, up to 99% for some pill combinations (1,2,8,9).
Contraceptive Pill Method of Action
The combined hormonal contraceptive pill has a primarily method of action of ovulation suppression with possible thickened cervical mucus and changes to the endometrial lining. Progestin only pills, such as those only norethindrone or norgestrel have a lower rate of ovulation suppression compared to drospirenone only containing pills alone. While it is possible to experience breakthrough ovulation on the hormonal contraceptive pills, it is also possible to have pregnancy prevented via the thickened cervical mucus or changes to the endometrial lining (1,2,8,9).
Contraceptive Pill Side Effects
Every medication has the possibility of side effects, and hormonal contraceptive pills are no exception. The most commonly reported side effects of hormonal contraceptive pills are irregular bleeding, changes in libido, weight changes, changes in vaginal composition, mood changes, and acne. The most severe of side effects are blood clot related, which often occurs within the first few months of hormonal contraception administration. While reports of hormonal contraceptive pill side effects can vary person to person, it is also important to keep in mind that many people do not report side effects at all for fear of being judged or misunderstood. Because of the varied nature of side effects of hormonal contraceptive pills, it is important to monitor client side effects to determine if risks outweigh the benefits and to adjust the medication regime as needed (1,2,8,9).
Contraceptive Pill Alternatives
Given the nature of hormonal contraceptive pills, a client might try a few various dosages of pills before selecting one that works with their body best. Likewise, a client might try a hormonal contraceptive pill for a few months and request switching to a different method all together. Alternatives to hormonal contraceptive pills include the patch, shot, ring, implant, IUD, or non-hormonal methods as well. It is important to listen to your clients’ needs to help determine what sort of complications they are looking to avoid and what option might be a good fit for them.

Self-Quiz
Ask Yourself...
- What are some possible side effects of hormonal contraceptive pills?
- How would you explain the differences in hormonal contraceptive pill dosages, strengths, and ingredients to a client?
- What are some client considerations to keep in mind when prescribing hormonal contraceptive pills?
- How can you recommend self-monitoring to clients taking hormonal contraceptive pills?
Hormonal Contraceptive Patch
Contraceptive Patch Drug Class
The hormonal contraceptive patch is still widely used as a hormonal contraceptive option, though not as popular as the pill for various reasons. Unlike the hormonal contraceptive pill, the hormonal contraceptive patch has a BMI limit since the patch is known to have less efficacy at BMIs greater than 30. As a result of this and the growing obese population in the U.S., patches have faltered in their use over the past decade. Still, millions of people rely on patches for their family planning needs. Like the hormonal contraceptive pill, there are no estrogen-only containing patches because of the risk of blood clots and severe side effects.
There are a few combinations of synthetic estrogen and progestin patch combinations on the USA market, but there are not hundreds of types of patch dosages compared to the pill. Unlike the hormonal contraceptive pill, the patch is placed onto a client’s skin, typically their abdomen, and left for one week. Clients leave the patch on their skin for a week, place a new patch in a week in a new location, and continue this for as long as they wish to prevent pregnancy. While the patch has its benefit of not taking a pill daily, the patch can also cause adhesive reactions or skin sensitivities. When used consistently and correctly, the patch is considered over 98% effective at pregnancy prevention (1,2,10,11,12).
Contraceptive Patch Method of Action
Hormonal contraceptive patches work to prevent pregnancy by suppressing ovulation. Patches have enough synthetic hormones for a week to work by suppressing ovulation (1,2,10,11,12).
Contraceptive Patch Side Effects
Every medication has the possibility of side effects, and hormonal contraceptive patches are no exception. It is important to monitor side effects to determine if risks outweigh the benefits and to adjust the medication regime as needed. The most commonly reported side effects of hormonal contraceptive patches are changes in bleeding patterns, patch site discomfort or irritation, and mood changes. In addition, the hormonal contraceptive patch does have an increased risk of blood clot formation because of the ways estrogen influences the clotting cascade. Educating clients on early signs and symptoms of blood clots and to be aware of their symptoms is essential to prevent complications (1,2,10,11,12).
Contraceptive Patch Alternatives
Given the nature of the hormonal contraceptive patch, a client might try a few types of patches before selecting one that works with their body best. Likewise, a client might try a hormonal contraceptive patch for a few months and request switching to a different method all together. Alternatives to hormonal contraceptive patches include the pill, shot, ring, implant, IUD, or non-hormonal methods as well. It is important to listen to your clients’ needs to help determine what sort of complications they are looking to avoid and what option might be a good fit for them.


Self-Quiz
Ask Yourself...
- What are some possible side effects of hormonal contraceptive patches?
- What are some contraindications for hormonal contraceptive patch use?
- What are some ways a client can self-monitor their symptoms while using a contraceptive patch?
- When can a contraceptive patch be prescribed?
- What happens if a client’s BMI increases while they are on the patch?
Hormonal Contraceptive Ring
Contraceptive Ring Drug Class
The hormonal contraceptive ring remains a popular choice for many people with a uterus of reproductive potential since it is a ring that sits in the vagina to prevent pregnancy. Unlike the pills, there are not hundreds of types of rings on the market. In fact, there are only two vaginal rings on the USA market, both of which contain synthetic estrogen and progestin. Both are designed to be left in the vagina for three weeks at a time and can be left in the vagina during vaginal intercourse. If needed, the vaginal ring can be taken out for up to three hours and then placed back into the vagina. The rings are designed to be soft, painless, and flexible, and they are compatible with condom use. If a client is considering the ring, it is important to ask the client how comfortable they are touching their vagina and vulva, as they would be the ones inserting the ring on their own at their own pace. When used consistently and correctly, the vaginal ring is considered over 98% effective at pregnancy prevention (1,2,13,14).
Contraceptive Ring Method of Action
Hormonal contraceptive vaginal rings work to prevent pregnancy primarily by suppressing ovulation (1,2,13,14).
Contraceptive Ring Side Effects
Every medication has the possibility of side effects, and hormonal contraceptive vaginal rings are no exception. It is important to monitor client side effects to determine if risks outweigh the benefits and to adjust the medication regime as needed. The most commonly reported side effects of hormonal contraceptive rings are changes in bleeding patterns and vaginal microbiome changes (leading to more yeast infections or bacterial vaginosis). In addition, the hormonal contraceptive ring does have an increased risk of blood clot formation because of the ways estrogen influences the clotting cascade. Educating clients on early signs and symptoms of blood clots and to be aware of their symptoms is essential to prevent complications (1,2,13,14).
Contraceptive Ring Alternatives
Given the nature of the hormonal contraceptive ring, a client might try a ring before selecting one that works with their body best. Alternatives to hormonal contraceptive rings include the pill, shot, patch, implant, IUD, or non-hormonal methods as well. It is important to listen to your clients’ needs to help determine what sort of complications they are looking to avoid and what option might be a good fit for them.

Self-Quiz
Ask Yourself...
- What are some possible reasons a client with family planning needs might be a good candidate for a contraceptive hormonal ring?
- What are some client considerations to consider when prescribing a hormonal contraceptive pill compared to a hormonal contraceptive ring?
- What would be some reasons a client might prefer a contraceptive ring instead of a pill?
- How would you explain to a 16-year-old client how to use a contraceptive vaginal ring compared to a 40-year-old client?
- How would you assess for vaginal conditions, such as a yeast infection, in a client who uses a vaginal contraceptive ring?
Hormonal Contraceptive Injection
Contraceptive Injection Drug Class
The hormonal contraceptive shot, also known as the depot medroxyprogesterone acetate (DMPA) shot, is one of the most popular injection medications in the USA and world. It is often regarded as the progestin only contraceptive shot that works for up to three months at a time at preventing pregnancy 99% when taken regularly. There is no estrogen-containing shot to prevent pregnancy. DMPA is not available in the pill, patch, IUD, or ring as a progestin given its specific progestin properties. Studies have shown great success with starting DMPA immediately postpartum as well.
DMPA can also be administered via the intramuscular (IM) route in a clinic setting or administered subcutaneously (SC) in an outpatient setting as well. With depo, it is important to monitor for bone loss and changes, as DMPA has a severe warning of possible changes to bone formation over time. That said, in the USA, it is recommended to only take Depo for 2 years because of the possible risks of bone loss. However, many people take Depo for longer than 2 years because of their personal preference, health history, and conversations with their health care team. When used consistently and correctly, the shot is considered over 99% effective at pregnancy prevention (1,2,15,16,17).
Contraceptive Injection Method of Action
The hormonal contraceptive shot, DMPA shot, works primarily to prevent pregnancy by suppressing ovulation (1,2,15,16,17).
Contraceptive Injection Side Effects
Every medication has the possibility of side effects, and the depot shot is no exception. Most common side effects of the depo shot include injection site reaction, changes in bleeding patterns, fatigue, mood changes, and bone loss (1,2,15,16,17).
Contraceptive Injection Alternatives
Given the nature of the hormonal contraceptive shot, a client might be on the shot for a few months before trying another option. Alternatives to the hormonal contraceptive shot include the pill, ring, patch, implant, IUD, or non-hormonal methods as well. It is important to listen to your clients’ needs to help determine what sort of complications they are looking to avoid and what option might be a good fit for them.

Self-Quiz
Ask Yourself...
- What are some possible side effects of the hormonal contraceptive shot?
- What are some client considerations to consider when administering the hormonal contraceptive shot during the immediate postpartum?
- What would be some client education points for the hormonal contraceptive shot administered via SubQ compared to IM?
- What are some parameters that need to be monitored if a client is taking the hormonal contraceptive shot?
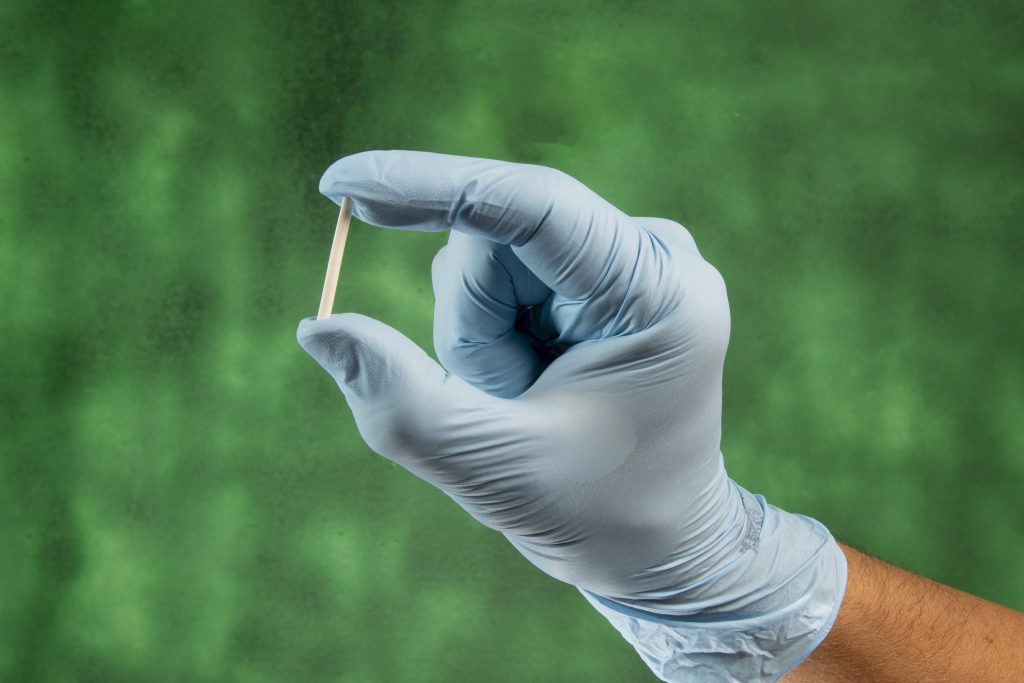
Hormonal Contraceptive Implant
Contraceptive Implant Drug Class
Hormonal contraceptive implants are progestin only rod(s) that are inserted into someone’s arm to prevent pregnancy. In the USA, the progestin only rod is a single rod system that is inserted into someone’s arm and removed by a health care provider. The rod contains etonogestrel, a synthetic type of progestin. The rod is inserted in an office setting and removed in an office setting as well. Some people report removing their implants at home, but that is not recommended for danger of hurting their veins and arm integrity. The implant is effective at pregnancy prevention for three years and can be removed before then if the client wants it removed. Not all health care providers are trained in implant insertion and removal, so it is important to make sure you are aware of which providers can remove and insert and implant. When used consistently and correctly, the implant is considered over 99% effective at pregnancy prevention (1,2,18,19,20).
Contraceptive Implant Method of Action
The hormonal contraceptive implant works to prevent pregnancy primarily by suppressing ovulation (1,2,18,19,20).
Contraceptive Implant Side Effects
Every medication has the possibility of side effects, and the hormonal contraceptive implant is no exception. Most common side effects of the hormonal contraceptive implant include changes to bleeding, mood changes, arm site tenderness, and weight changes (1,2,18,19,20).
Contraceptive Implant Alternatives
Given the nature of the hormonal contraceptive implant, a client might have the implant for a few months or years before trying another option. Alternatives to the hormonal contraceptive shot include the pill, ring, patch, shot, IUD, or non-hormonal methods as well. It is important to listen to your clients’ needs to help determine what sort of complications they are looking to avoid and what option might be a good fit for them.

Self-Quiz
Ask Yourself...
- What are some possible side effects of the hormonal contraceptive implant compared to the hormonal contraceptive patch?
- What sort of client considerations would you take into account for inserting and removing a hormonal contraceptive implant?
- How would you manage a client who states that they are experiencing suicidal thoughts while taking on the hormonal contraceptive implant?
- How would you determine someone’s pregnancy status prior to inserting a hormonal contraceptive implant?
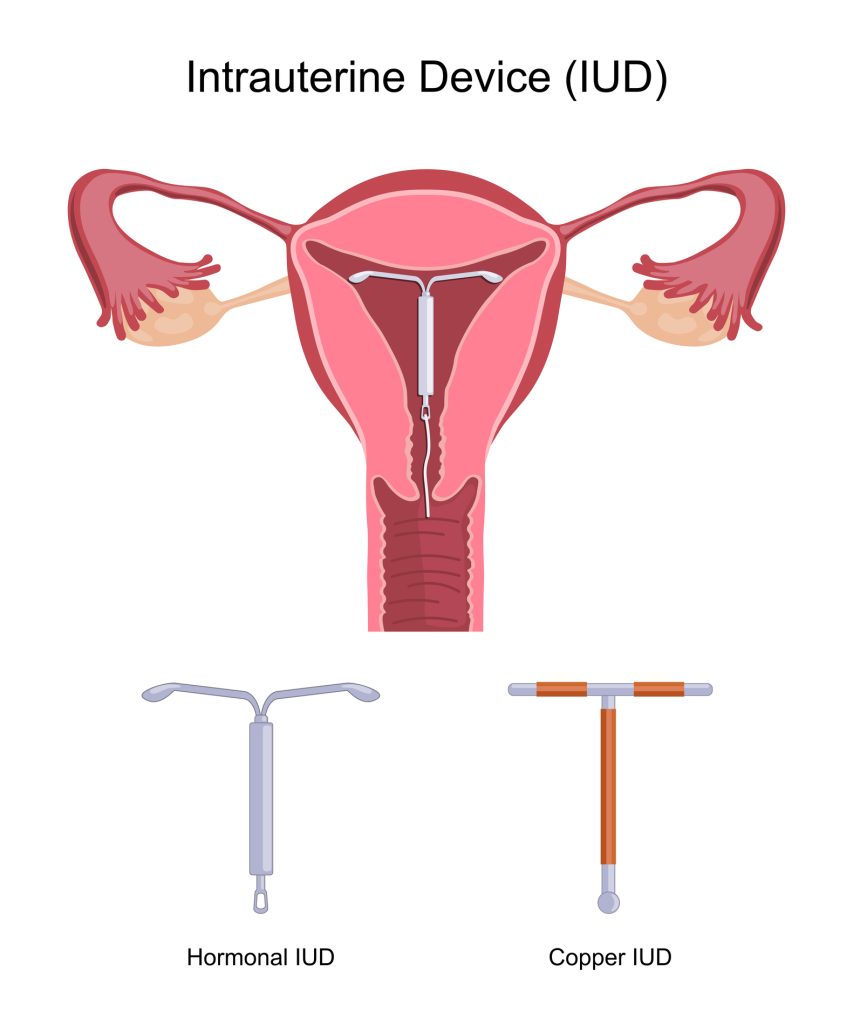
Hormonal Contraceptive Intrauterine Device (IUD)
Hormonal IUD Drug Class
The hormonal contraceptive IUD contains the synthetic progestin levonorgestrel. There are three main hormonal IUDs in the USA and some internationally as well. These IUDs, depending on their dosage, are indicated for pregnancy prevention for 3-5 years. IUDs are inserted by a trained health care provider and can be removed by a trained health care provider as well. Often times, unless there are severe IUD complications, a client can also self-remove an IUD in the comfort of their home or in clinic if possible. There are no estrogen-containing IUDs given the nature of estrogen in the uterus.
Since IUDs are placed directly into the uterus, this insertion is done with the speculum opening up the walls of the vagina, an instrument measuring the length of the uterus, and an inspection of the cervix prior to insertion. Given the rise of social media and people wanting their voices regarding pain management to be heard, more health care institutions are offering pain management regarding IUD insertions. That said, pain management for IUD insertion remains inconclusive, and there is no one set way to provide pain relief during an IUD insertion.
Discussion about realistic pain expectations, timeline for IUD insertion, and removal are essential for IUD discussions. Historically, IUDs were only placed in people who had given birth, but many people can have an IUD inserted, regardless of their age or parity, as long as they have a uterus that can hold an IUD. When used consistently and correctly, the IUD is considered over 98% effective at pregnancy prevention (1,2,21,22,23).
Hormonal IUD Method of Action
The hormonal IUD prevents pregnancy by suppressing ovulation, thickening the cervical mucus, and altering the lining of the endometrium. Hormonal IUDs are not known to suppress ovulation as consistently and strongly as systemic hormonal contraception, such as the pill or patch (1,2, 21,22,23).
Hormonal IUD Side Effects
Every medication has the possibility of side effects, and IUDs are no exception. Most common side effects of hormonal IUDs include painful insertion, changes in bleeding, cervical irritation, and uterine complications (1,2, 21,22,23).
Hormonal IUD Alternatives
Given the nature of the hormonal IUD, a client might have the IUD for a few months or years before trying another option. Alternatives to the hormonal contraceptive shot include the pill, ring, patch, shot, implant, or non-hormonal methods as well. It is important to listen to your clients’ needs to help determine what sort of complications they are looking to avoid and what option might be a good fit for them. It is also important to ensure that a client can remove an IUD when they desire as well.

Self-Quiz
Ask Yourself...
- What are some possible side effects of hormonal contraceptive IUDs?
- What are some possible pain management options for an IUD insertion and removal?
- At what age can a client receive an IUD?
- How can a client self-remove an IUD?
- Which clients are not good candidates for IUDs?
Non-Hormonal Contraceptive Intrauterine Device (IUD)
Non-Hormonal IUD Drug Class
The non-hormonal contraceptive IUD contains copper. There is only one commercially available copper IUD in the USA, but there are several other copper IUDs globally. The copper IUD is intended to prevent pregnancy for 10 years. Like the hormonal IUDs, copper IUDS are inserted by a trained health care provider and can be removed by a trained health care provider as well. Often times, unless there are severe IUD complications, a client can also self-remove an IUD in the comfort of their home or in clinic if possible. Since IUDs are placed directly into the uterus, this insertion is done with the speculum opening up the walls of the vagina, an instrument measuring the length of the uterus, and an inspection of the cervix prior to insertion.
Given the rise of social media and people wanting their voices regarding pain management to be heard, more health care institutions are offering pain management regarding IUD insertions. That said, pain management for IUD insertion remains inconclusive, and there is no one set way to provide pain relief during an IUD insertion. Discussion about realistic pain expectations, timeline for IUD insertion, and removal are essential for IUD discussions. Historically, IUDs were only placed in people who had given birth, but many people can have an IUD inserted, regardless of their age or parity, as long as they have a uterus that can hold an IUD. When used consistently and correctly, the IUD is considered over 99% effective at pregnancy prevention (1,2,24,25,26).
Non-Hormonal IUD Method of Action
The copper IUD has a method of action of copper acting as a spermicide in the uterus (1,2,24,25,26). The copper IUD does not interfere with the menstrual cycle.
Non-Hormonal IUD Side Effects
Every medication has the possibility of side effects, and IUDs are no exception. Most common side effects of copper IUDs include painful insertion, increased bleeding, increased vaginal discharge, cervical irritation, and uterine complications (1,2,24,25,26).
Non-Hormonal IUD Alternatives
Given the nature of the copper IUD, a client might have the IUD for a few months or years before trying another option. It is important to listen to your clients’ needs to help determine what sort of complications they are looking to avoid and what option might be a good fit for them. It is also important to ensure that a client can remove an IUD when they desire as well.

Self-Quiz
Ask Yourself...
- What are some possible reasons why a client would prefer a non-hormonal contraceptive option compared to a hormonal contraceptive option?
- How would you obtain a detailed medication history from a client prior to an IUD insertion?
- What are some contraindications for the non-hormonal IUD?
Family Planning: Condoms
Condoms are among some of the most popular forms of family planning given their ease of access, availability, ability to prevent sexually transmitted infections (STIs), cost, and variety. A male or external condom is a barrier device that is made of latex, polyisoprene, polyurethane, or lamb skin that is placed over the penis to prevent pregnancy. A female or internal condom is a barrier device that is made of nitrile that is placed into the vagina to prevent pregnancy. Male condoms do not need a prescription in the USA, but female condoms do. When used consistently and correctly, condoms can be highly effective at pregnancy prevention and STI transmission. Given the widespread use of condoms, they are popular among several age groups, given out for free from several health departments, and can be easily available in the moment of vaginal intercourse (1,2,26,27,28).
Condoms have a straightforward method of action of collecting the sperm to prevent sperm from travelling to the uterus (1,2,26,27,28).
Every medication has the possibility of side effects, and condoms are no exception. Most common side effects of condoms are skin irritation or allergic reaction, especially to latex (1,2,26,27,28).
Alternatives to condoms include hormonal contraception and other forms of non-hormonal contraception, such as withdrawal or surgical options.

Self-Quiz
Ask Yourself...
- How could condoms affect skin tissues in the vagina, vulva, or on the penis?
- What are some common materials condoms are made of?
- What are some reasons people would use condoms in addition to hormonal contraception for family planning purposes?
- What sort of lubrication can be used with condoms?
Family Planning: Diaphragm and Cervical Cap
A diaphragm or cervical cap are barrier methods that are inserted into the vagina and are used to collect semen. Only a diaphragm or cervical cap can be used at a time, not both together. These require a prescription since they need to be assessed to see if they will fit a client’s body correctly for maximum pregnancy prevention. Like condoms, they are made of various materials that could cause skin sensitivities, can be used in the moment of vaginal intercourse, and do not influence the menstrual cycle (1,2,29,30). Both devices work to prevent pregnancy by collecting the semen to prevent the semen from entering the uterus (1,2,29,30).
Every medication has the possibility of side effects, and the diaphragm and cervical cap are no exception. Most common side effects are skin irritation and discomfort (1,2,29,30).
Alternatives to the diaphragm and cervical cap include hormonal contraception and other forms of non-hormonal contraception, such as withdrawal or surgical options.

Self-Quiz
Ask Yourself...
- What are some client talking points to consider when discussing the diaphragm or cervical cap use?
- How could being postpartum and type of delivery affect the types of cervical cap needed for pregnancy prevention?
Family Planning: Fertility Awareness Method, Withdrawal, Lactation Amenorrhea Method, and Spermicide
The fertility awareness method (FAM) is a readily available method that involves the person with the uterus tracking their cycle using a planner, app, or other device and noting when they are most fertile, such as when they ovulate. This option works best for people who have regular menstrual cycles and who are comfortable tracking their cycles regularly (1,2,29,30).
Withdrawal is a readily available method in which the penis withdraws from the vagina before it ejaculates (1,2).
Lactation Amenorrhea Method (LAM) is very popular among newly postpartum and breastfeeding people, as consistent lactation is known to induce amenorrhea and prevent pregnancy (1,2,29).
Spermicide is an OTC option that can be purchased at stores and is used during vaginal intercourse in which the spermicide is placed into the vagina before ejaculation (1,2).

Self-Quiz
Ask Yourself...
- What are some reasons why a client would prefer to use OTC family planning methods instead of those that require a prescription?
- How would you educate a client on the FAM method?
- What are some current contraceptive and family planning trends you see in your workplace?
Surgical Interventions
A vasectomy is a permanent surgical option that cuts the supply of sperm to the semen in an outpatient procedure. During the vasectomy, two tubes called the vas deferens are cut and sealed. Vasectomies can take up to three months to work, so it is important to understand that is method is not instant. Vasectomies can have surgical complications, such as incision site infections, changes in testosterone levels, and more. Proper post-surgical follow up is recommended (1,32).
A tubal ligation is a permanent surgical option that cuts and ties the fallopian tubes to prevent pregnancy and the person still maintains their menstrual cycle. Tubal ligation is often immediate with pregnancy prevention. Like all surgical procedures, there can be surgical complications, such as incision site infections, hemorrhage, and more (1,32).
A hysterectomy is a permanent surgical option that removes the uterus, leading to immediate pregnancy prevention. Like all surgical procedures, there can be surgical complications, such as incision site infections, anesthesia complications, and more (1,32).
Research Findings
What Family Planning and Contraceptive Medication Research Exists Presently?
There is extensive publicly available literature on medications via the National Institutes of Health and other evidence-based journals.
What are some ways for people who take medications to become a part of research?
If a client is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.


Self-Quiz
Ask Yourself...
- What are some possible surgical complications to be aware of for a vasectomy, tubal ligation, or hysterectomy?
- What are your institution’s policies for surgical procedures?
- What are some possible ways you can obtain a detailed, client centric health history in pediatric populations?
- What are some possible ways you can obtain a detailed, client centric health history in postpartum populations?
- What are some reasons someone would want to enroll in clinical trials?
- What trends in contraceptive technology do you see in your workplace or see in the future of nursing and healthcare?
- How would you discuss the role of social media and misconceptions about hormonal medication to your clients?
- What are some client education points to discuss about typical versus perfect use of contraceptive methods?
- How would you determine drug-drug interactions with hormonal contraception and other medications?
- How would you discuss the influence of hormonal contraception on future fertility?
- How would you discuss the role of non-hormonal contraception on future fertility?
- What are some reasons why a client would prefer a surgical approach to family planning?
- How are some possible ways nurses can educate clients on contraceptive medication options?
- Why is it important for clients to self-monitor themselves for symptoms on contraception, especially hormonal contraception?
- What are some possible risks and benefits of hormonal contraception compared to non-hormonal contraception?
- How does culture factor into family planning and contraception?
Conclusion
Contraceptive methods and family planning is often a lifelong process for millions, if not billions, of people. People have to make various choices regarding their contraceptive autonomy and decisions, and it is up to nurses to provide the best education possible for our clients.
References + Disclaimer
- Cason P, et al. 2023. Contraceptive Technology, 22nd Edition. Jones and Barlett Publishing.
- Nguyen AT, Curtis KM, Tepper NK, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2024. MMWR Recomm Rep 2024;73(No. RR-4):1–126. DOI: http://dx.doi.org/10.15585/mmwr.rr7304a1.
- Patient-Centered Contraceptive Counseling: ACOG Committee Statement Number 1. Obstetrics & Gynecology 139(2), 350-353, February 2022. DOI: 10.1097/AOG.0000000000004659
- Lesnewski R. Initiating Hormonal Contraception. American Family Physician. 2021;103(5):291-300. https://www.aafp.org/pubs/afp/issues/2021/0301/p291.html
- Mauck CK, et al. Contraceptive efficacy should primarily be measured using life table pregnancy rates. Contraception. 2023(127):110140. https://doi.org/10.1016/j.contraception.2023.110140
- Teal S, Edelman A. Contraception Selection, Effectiveness, and Adverse Events. JAMA. 2021;326(24):2507-2518. doi:10.1001/jama.2021.21392
- Rohatgi, KW, et al. 2021. Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Patterson L. The combined oral contraceptive pill. InnovAiT. 2022;15(2):106-112. doi:10.1177/17557380211059847
- Zuniga C, et al. Effectiveness and efficacy rates of progestin-only pills: A comprehensive literature review. Contraception. 2023;119:109925. https://doi.org/10.1016/j.contraception.2022.109925
- Parasrampuria DA, et al. Comparison of a transdermal contraceptive patch with a newly sourced adhesive component versus EVRA patch: A double-blind, randomized, bioequivalence and adhesion study in healthy women. Contraception. 2020;101(4):276-282. https://doi.org/10.1016/j.contraception.2019.12.012
- Sriprasert, I., Archer, D.F. (2020). Transdermal Contraceptive Delivery Systems. In: Shoupe, D. (eds) The Handbook of Contraception. Current Clinical Practice. Humana, Cham. https://doi.org/10.1007/978-3-030-46391-5_4
- Nelson A, et al. Efficacy, safety, and tolerability of a levonorgestrel/ethinyl estradiol transdermal delivery system: Phase 3 clinical trial results. Contraception. 2021;103(3):137-143. https://doi.org/10.1016/j.contraception.2020.11.011
- Al-Haddad S, Branham KKR, Clare CA. Advances in contraception: vaginal contraceptive rings. Therapeutic Advances in Reproductive Health. 2023;17. doi:10.1177/26334941231186733
- Murina, F, et al. The impact of combined contraceptive vaginal ring on vaginal environment: an observational, longitudinal study. The European Journal of Contraception and Reproductive Health Care, 2023;28(4), 234–237. https://doi.org/10.1080/13625187.2023.2228440
- McCullough, D.C., Eraso, K.M., Kaunitz, A.M. (2020). Depot Medroxyprogesterone Acetate. In: Shoupe, D. (eds) The Handbook of Contraception. Current Clinical Practice. Humana, Cham. https://doi.org/10.1007/978-3-030-46391-5_6
- Burlando, AM, et al. The Role of Subcutaneous Depot Medroxyprogesterone Acetate in Equitable Contraceptive Care: A Lesson From the Coronavirus Disease 2019 (COVID-19) Pandemic. Obstetrics & Gynecology. 2021:138(4):574-577. DOI: 10.1097/AOG.0000000000004524
- Gallo MF, et al. Potential effect of immediate postpartum use of injectable contraception on lactogenesis. Contraception. 2024, 110726. https://doi.org/10.1016/j.contraception.2024.110726
- Moray KV, et al. A systematic review on clinical effectiveness, side-effect profile and meta-analysis on continuation rate of etonogestrel contraceptive implant. Reprod Health 18, 4 (2021). https://doi.org/10.1186/s12978-020-01054-y
- Gilbert BG. Contraceptive Implant Insertion and Removal. Primary Care: Clinics in Office Practice. 2021;48(4):545-554. DOI: 10.1016/j.pop.2021.07.002
- Edelman A, et al. Treatment of unfavorable bleeding patterns in contraceptive implant users: a randomized clinical trial of curcumin. American College of Obstetrics and Gynecology. 2023;229(2):141-145. https://doi.org/10.1016/j.ajog.2023.04.028
- Ramanadhan S, et al. Progestin intrauterine devices versus copper intrauterine devices for emergency contraception. Cochrane Database of Systemic Reviews. 2023. https://doi.org/10.1002/14651858.CD013744.pub2
- Buyuk, GN, et al. 2021. Copper and levonorgestrel containing intrauterine devices: comparison of their effect on oxidative stress markers. Gynecological Endocrinology, 37(4), 320–323. https://doi.org/10.1080/09513590.2021.1878132
- Bastianelli, C, et al. 2020. Effects of progestin-only contraceptives on the endometrium. Expert Review of Clinical Pharmacology, 13(10), 1103–1123. https://doi.org/10.1080/17512433.2020.1821649
- Unsal SR, Ustun Y. The Effect of Use of Copper Intrauterine Device for Contraception on Pain and Female Sexual Functions. Reproductive BioMedicine Online. 2023. 47. https://doi.org/10.1016/j.rbmo.2023.103561
- Brown, BP, et al. Copper intrauterine device increases vaginal concentrations of inflammatory anaerobes and depletes lactobacilli compared to hormonal options in a randomized trial. Nat Commun 14, 499 (2023). https://doi.org/10.1038/s41467-023-36002-4
- Steiner RJ, et al. Long-Acting Reversible Contraception, Condom Use, and Sexually Transmitted Infections: A Systematic Review and Meta-analysis. 2021. American Journal of Preventive Medicine. 61(5):750-760. https://doi.org/10.1016/j.amepre.2021.04.032
- Beksinska M, et al. Male and female condoms: Their key role in pregnancy and STI/HIV prevention. Best Practices and Research in Clinical Obstetrics and Gynaecology. 2020. 66:55-67. https://doi.org/10.1016/j.bpobgyn.2019.12.001
- Wiyeh, AB, et al. Effectiveness of the female condom in preventing HIV and sexually transmitted infections: a systematic review and meta-analysis. BMC Public Health 20, 319 (2020). https://doi.org/10.1186/s12889-020-8384-7
- Duane M, et al. Fertility Awareness-Based Methods for Women’s Health and Family Planning. Frontiers in Medicine. 2022. Vol. 9. https://doi.org/10.3389/fmed.2022.858977
- Lindh I, et al. New types of diaphragms and cervical caps versus older types of diaphragms and different gels for contraception: a systematic review. BMJ Sexual and Reproductive Health. 2021;47. https://doi.org/10.1136/bmjsrh-2020-200632
- Schulz AE, et al. Vasectomy and Vasectomy Reversals—a Review of the Current Literature. Curr Sex Health Rep 15, 138–147 (2023). https://doi.org/10.1007/s11930-023-00364-z
- Mills K, et al. Salpingectomy vs tubal ligation for sterilization: a systematic review and meta-analysis. American Journal of Obstetrics and Gynecology. 2021;224(3):258-265. https://doi.org/10.1016/j.ajog.2020.09.011
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
