Course
Florida APRN Bundle
Course Highlights
- In this course, we will learn about domestic violence, and why it is important for medical professionals to be aware of signs.
- You’ll also learn the Florida HIV/AIDS requirements, the importance of infection reporting, and the basics of treatment as required by the Florida Board of Nursing.
- You’ll leave this course with a broader understanding of the Differentiate between uncomplicated and complicated UTI and summarize key considerations when prescribing antibiotics for UTI.
About
Contact Hours Awarded: 29
Including 18 Pharmacology contact hours
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
Florida Domestic Violence
This fulfills the continuing education requirement of Domestic Violence for the state of Florida.
Florida domestic violence is defined as violent or aggressive behavior occurring within the home and usually involves the abuse of a spouse or partner. In the United States alone, it is estimated that more than 10 million adults have been subjected to domestic violence during the course of a year. This statistic translates to an incident of domestic violence occurring every 3 seconds. Due to the increasing prevalence of domestic violence in society, there is a high probability that all healthcare professionals will evaluate and treat a victim (and quite possibly a perpetrator as well) of domestic violence at some time during their healthcare career. The importance of ongoing education and global awareness cannot be understated.
Introduction
Domestic violence is defined as violent or aggressive behavior occurring within the home and usually involves the abuse of a spouse or partner. In the United States alone, it is estimated that more than 10 million adults have been subjected to domestic violence during the course of a year. This statistic translates to an incident of domestic violence occurring every three seconds. The National Coalition Against Domestic Violence reports some daunting statistics [1][6]:
- 1 in 3 women and 1 in 4 men have experienced some form of physical violence by an intimate partner.
- 1 in 4 women and 1 in 7 men have been victims of severe physical violence (such as beating, burning, strangling) by an intimate partner in their lifetime.
- On average, more than 20,000 phone calls placed to domestic violence hotlines nationwide.
- The presence of a gun in a domestic violence situation increases the risk of homicide by 500%; 19% of domestic violence involves a weapon; Most intimate partner homicides are committed with firearms.
- 1 in 15 children are exposed to intimate partner violence each year, and 90% of these children are eyewitnesses to this violence.
- From 2016 through 2018, the number of intimate partner violence victimizations in the United States increased 42%.
Due to the increasing prevalence of domestic violence in society, there is a high probability that all healthcare professionals will evaluate and treat a victim (and quite possibly a perpetrator as well) of domestic violence at some time during their healthcare career. The importance of ongoing education and global awareness cannot be understated.
In 2020, the COVID-19 pandemics’ stay at home/shelter in place orders resulted in spikes in calls to domestic violence hotlines. From layoffs and loss of income to decreased availability of shelters and backlogged courtrooms, fewer resources were made available to victims of domestic violence. These measures resulted in increases in both the incidence and severity of domestic violence. Sadly, the effects of this pandemic, especially on this issue, continue well into today [2].
Forms of Domestic Violence
Domestic violence may encompass physical abuse, sexual abuse, emotional and verbal abuse, and spiritual and economic abuse. Defined as a pattern of behavior used to gain power or control over an intimate partner, a domestic violence abuser may use tactics that frighten, intimidate, hurt, blame, or injure a person. These behaviors often escalate over time in intensity and have resulted, at times, in life-threatening injuries or death of a victim [3].
Intimate partner violence (IPV) is abuse or aggression that occurs in a romantic relationship. The term “intimate partner” refers to both current and former spouses and dating partners, including heterosexual and same-sex couples. The Centers for Disease Control and Prevention (CDC) further delineates IPV into four separate groups: physical violence, sexual violence, stalking, and psychological aggression [4].
- Physical violence may include hitting, kicking, and punching someone.
- Sexual violence may include using force to get a partner to partake in a sexual act.
- Stalking may include unwanted and threatening phone calls or text messages.
- Psychological aggression may include insults, threats, name-calling, or belittling a partner.
Teen Dating Violence (TDV) is defined as dating violence affecting millions of teenagers annually [5]. In addition to the threats from physical and sexual violence and other forms of aggression, TDV is often done electronically through repeated texting and placing sexual pictures of a person online without permission.
The CDC statistics on teen dating violence report:
- Nearly 1 in 11 female and about 1 in 15 male high school students report having experienced physical dating violence in the last year.
- About 1 in 9 female and 1 in 36 male high school students report having experienced sexual dating violence in the last year.
- 26% of women and 15% of men who were victims of contact sexual violence, physical violence, and/or stalking by an intimate partner in their lifetime first experienced these or other forms of violence by that partner before age 18.
Domestic violence transects every community and affects all people, regardless of age, socio-economic status, race, religion, gender, or nationality [6]. Whether the violence results in physical or psychological injury, the effects can last a lifetime and affect multiple generations.
Healthcare professionals are in a pivotal position to impact the lives of those affected by domestic violence positively. Oftentimes, they may be the first person to encounter a victim of domestic violence. Their ability to effectively evaluate the situation and provide time-sensitive, patient-centered care (including but not limited to treatment interventions, appropriate referrals, and follow-up care) can enhance immediate victim safety and reduce further injury, and improve the home front circumstances, moving forward.
Healthcare professionals must be able to identify and assess all patients for suspected abuse, and be able to offer treatment, counseling, education, and referrals, as appropriate. These referrals may extend out to shelter options, advocacy groups, child protection services and legal assistance [7].
Profiles of Victims and Abusers
Anyone can become a victim of domestic violence. Victims of domestic violence come from all walks of life, all age groups, all socio-economic groups, all religions, and all nationalities [8]. Violence can occur in any relationship when one person feels they are entitled to control another person through whatever means of abuse possible. This abuse is cyclical and usually increases in frequency and intensity. Victims of such violence report feelings of isolation, helplessness, guilt, anxiety, and embarrassment. They may become suicidal, start abusing drugs and alcohol, and feel that they have no one to turn to for help.
Although there isn’t a specific set of factors that result in “being a victim,” there are many thoughts as to what might affect a person’s active willingness to remain in a violent relationship. The following lists serve only as general guidance to inform the healthcare professional of possible underlying causes. Again, anyone can become a victim of domestic violence.
Victims of Domestic Abuse
There is no single “characteristic” or risk factor that automatically causes a person to become a victim of domestic violence. Instead, it may be a series of events that cause a person to become more vulnerable and enter and remain within an abusive relationship [9].
Domestic violence victims may have experienced violence during childhood, experienced total financial dependence on another person, or lacked basic social support (family and friends). These factors affect both the physical and psychological make-up of a person. Without intervention, these victims can develop personal esteem and confidence issues, further social isolation, economic dependency, and general feelings of insecurity. These effects may negatively affect the decision to stay in an abusive relationship.
Researchers have found the following factors may place a person at a higher risk of becoming a victim of domestic violence, including (but not limited to) [10]:
- Poor self-image/ low self-esteem
- Financial dependence on the abuser
- Feeling powerless to stop the violence or leave the relationship
- Personal belief that jealousy is an expression of love
Common characteristics of victims of domestic violence include, but are not limited to:
- A history of abuse
- A history of alcohol or substance abuse (for themselves or their partners)
- Financial and family stressors- low income, limited family/friends contact, poverty status
- A member of an ethnic minority/ immigrant group; Limited English vocabulary
- Holds traditional beliefs that they should be submissive in a relationship
Reasons a victim may choose to stay in the relationship:
- A desire to end the abuse but not necessarily the relationship; they do love their abuser
- Feelings of isolation and helplessness
- Fear of judgment if they reveal the abuse by seeking help
- Feelings that they may not be able to support themselves if they leave their abuser
- Fears for the safety of children involved in the relationship
- Fear of backlash from community or family and friends/lack of knowledge of services available
- Strong religious/cultural belief system that reinforces staying in a relationship at all costs
Abusers/Perpetrators of Domestic Violence
As with the DV victim, there is no one set of traits to identify a domestic violence abuser/perpetrator correctly. There are, however, some signs that may raise the red flag of suspicion when observed in a suspected domestic violence case.
The National Coalition on Domestic Abuse has created a list of “red flag” indicators, including but not limited to the following [11]:
- Extreme jealousy and possessiveness
- Verbally abusive
- Extremely controlling behavior
- Blaming the victim for anything bad that happens
- Control over all the finances in the relationship
- Demeaning the victim publicly or privately
- Humiliating or embarrassing the victim in front of other people
- Control over what the victim wears
- Abuse of other family members, including children (and even pets)
The following is a general list of indicators that “may” help identify an abuser [12].
- History of abuse within one’s family
- History of personal physical or sexual abuse
- A lack of appropriate coping skills
- Low self-esteem
- Codependent behavior
- Untreated mental illness
- Drug or alcohol abuse
- Socio-economic pressures related to the lower income status
- Prior criminal history


Self Quiz
Ask yourself…
- What are interventions/resources currently available at your facility to assist a victim of domestic violence?
- What resources are currently available for domestic abuse perpetrators?
Screening for Domestic Violence
Screening rates are as low as 1.5% to 13% among emergency and primary care physicians. The Academy of Medicine recommendation suggested that all women should be screened for sexual violence. Research found that healthcare providers working in emergency departments only screened 20–25% of their encounters. As a result, this decreased opportunities for intervention, increased safety, and prevention of future violence [13].
Domestic violence (including Intimate partner violence) is an unfortunate cycle that may not be broken with a single emergency department visit; however, identifying and providing resources is necessary to make a difference, increase confidence and safety, and improve the overall health outcome for patients.
Initial Interaction
Compassionate, nonjudgmental screening by healthcare professionals affords the best opportunity for domestic violence victims to disclose their abuse. By recognizing signs of abuse and inquiring further, the nurse validates that the victim is worthy of care and confirms that the violence is a legitimate concern [14].
The screening for domestic abuse should be done in a private environment. Language interpreters, not family and friends, should be utilized if needed. Universal screening should be used; therefore, preventing any victim from being “singled out” and ensuring all potential victims are screened appropriately. All healthcare professionals should remain nonjudgmental and compassionate during the screening process [15].
During the interview process, assure the victim that all patients are screened for domestic violence. Also, inform the victim that DV affects many families, and that services are available to everyone who may be concerned about violence in their home.
Screening Tools
Examples of the following four screening tools can be found in the CDC’s Intimate Partner Violence and Sexual Violence Victimization Assessment Instruments for Use in Healthcare Settings.
Hurt, Insult, Threaten and Scream (HITS)
5-question screening tool assessing physical and verbal interactions with the partner; scores rank 1 (never) -5 (frequently); a score of 10 is considered positive.
- Physically hurt you?
- Insult or talk down to you?
- Threaten you with harm?
- Scream or curse at you?
- Force you to do sexual acts that you are not comfortable with?
http://www.ctcadv.org/files/4615/6657/9227/HPO_HITS_Screening_Tool_8.19.pdf
Woman Abuse Screening Tool (WAST)
8-question screening tool assessing physical, emotional, and sexual intimate partner violence.
http://womanabuse.webcanvas.ca/documents/wast.pdf
Partner Violence Screen (PVS)
3-question screening tool for interpersonal violence
- Have you been hit, kicked, punched, or otherwise hurt by someone within the past year? If so, by whom?
- Do you feel safe in your current relationship?
- Is there a partner from a previous relationship who is making you feel unsafe now?
http://www.nnepqin.org/wp-content/uploads/2018/08/Screening-Tools-Partner-Violence-Screen-PVS.pdf
Abuse Assessment Screen (AAS)
A multiple section assessment tool for sexual and physical violence, including body maps for documentation of injuries.
https://idph.iowa.gov/Portals/1/Files/FamilyHealth/abuse_assessment_tool.pdf
Potential Signs of Domestic Violence
The Crisis Prevention Institute (CPI) encourages to always be aware of physical signs and injuries that could be related to domestic violence, including but not limited to the following [16]:
- Bruising in the chest and abdomen
- Multiple injuries
- Minor lacerations
- Ruptured eardrums
- Delay in seeking medical attention
- Patterns of repeated injury
- Injuries inconsistent with the presenting complaints
Oftentimes, a domestic violence victim may seek medical attention for issues unrelated to a physical injury, such as:
- A stress-related illness
- Anxiety, panic attacks, stress, and/or depression
- Chronic headaches, asthma, vague aches, and pains
- Abdominal pain, chronic pelvic pain
- Vaginal discharge and other gynecological problems
- Joint pain, muscle pain
- Suicide attempts, psychiatric illness
Other observations that may indicate a suspected domestic violence situation include:
- Appear nervous, ashamed, or evasive
- Seem uncomfortable or anxious when around their partner
- Accompanied by their partner, who controls the conversation
- Reluctant to follow advice
As you continue to assess the patient, encourage them to talk and then listen carefully. Only upon listening will you have a better understanding of the patient’s current state and provide the necessary resources and referrals for them to find safety. Above all else, maintain open lines of communication in a safe, accepting environment and assure the victim that they do not deserve the abuse.

Self Quiz
Ask yourself…
- What screening tools are currently available at your facility to assess for possible domestic abuse? Do you feel that they are effective?
- Domestic abuse victims may seek medical attention for issues unrelated to abuse (chronic headache, vague aches, and pain, anxiety, or depression). What further assessments can be done to assess for domestic violence?
Importance of Trauma-Informed Care
While nurses play a critical role in recognizing suspected domestic abuse victims, they often do not feel confident in their role or the screening process itself. This may be due to a lack of communication skills, ongoing training on domestic violence or simple confusion over what victim assistance programs and resources are available [17].
Facility-wide education on domestic violence should be ongoing. Policies and procedures should be on file, and collateral relationships should be in place with the local community and national resources. Finally, nurses should be trained in the delivery of trauma-informed care to ensure the highest quality of interaction with victims of domestic violence, much less all victims of trauma.
Trauma-informed care has been defined as the patient-centered approach that encourages healthcare professionals to provide care that does not retraumatize the patient and the staff [18]. Trauma-informed care ensures that policies and practices in the healthcare setting are not only safe but non-threatening to the physical and mental well-being of those involved. Perceived threats can cause a “flight or fright” mentality that impacts both the ability to administer care and receive immediate care and follow-up recommendations.
The experience of seeking medical care, whether in an emergency department setting or a clinic, can in and of itself bring another source of trauma. Trauma-informed care aims at reducing the impact of trauma on both the patient and provider by focusing on various checkpoints overseeing all interactions: safety, trustworthiness, empowerment, and respect.
The following examples are practical tips that encourage trauma-focused care, ensuring the delivery of care in the least threatening manner to a suspected human trafficking victim (as well as each patient you may intersect with).
- Always introduce yourself and your role within the patient’s care with every interaction.
- Use open body language (direct eye contact, avoid standing “over” the patient as it may be perceived as threatening).
- Explain procedures and timelines for results (“wait times”) to give patients a sense of control. Keep them informed of any changes/delays in their care.
- Always ask before you touch a patient. This is a sign of respect and gives the patient a sense of control over their own bodies.
- Protect patient privacy. Ask them who they would like present during their care; limit visitors if requested; close room doors (with their permission).
During the interview and intervention process, it is also equally important that some things not be said to a suspected victim of domestic violence, such as negating, challenging, or doubting the victim. Examples include:
- Why haven’t you called the police before now?
- Some level of fighting occurs in all relationships.
- Maybe you’re both going through a phase; it will probably stop on its own.
- You wouldn’t stay in this situation if you really care about yourself/ your kids.
- What did you do to make them get so angry?
- Why didn’t you leave the first time you were hurt?
By applying trauma-informed care to all your patients, you lower the risk of perceiving any (nursing and medical) interventions being perceived as a threat. This ensures a higher level of trust and respect, and safety for all patients (and staff) across the care spectrum.

Self Quiz
Ask yourself…
- What are some possible consequences of doubting a victim of domestic violence?
- What can you do as a healthcare professional to ensure all patients are screened for domestic violence?
Legal Issues: Florida Mandatory Reporting Laws
The United States Department of Justice, defines domestic violence to include felony or misdemeanor crimes of violence committed by [19]:
- a current of former spouse or intimate partner of the victim,
- by a person with whom the victim shares a child in common,
- by a person cohabitating with or has cohabitated with the victim as a spouse or intimate partner,
- by a person similarly situated to a spouse of the victim under the domestic or family violence laws of the jurisdiction receiving grant monies,
- by any other person against an adult or youth protected from that person’s acts under the jurisdiction’s domestic or family violence laws.
The Florida Department of Children and Families defines domestic violence as patterns of actions or behaviors that adults or adolescents use against their partners or former partners to establish power and control. It can potentially include physical abuse, sexual abuse, emotional abuse, and economic abuse. It may also include threats, isolation, pet abuse, using children, and a variety of other behaviors used to maintain fear, intimidation, and power over one’s partner (19).” [28].
Under Florida law [21], Domestic Battery is classified as a first-degree misdemeanor, with penalties including up to one year in jail or twelve months’ probation and a $1,000 fine [21][29][30]. In addition, the accused may face additional penalties of a mandated Batterer Intervention Program [31].
RAINN (Rape, Abuse, and Incest National Network) is the nation’s largest anti-sexual violence organization [22]. Under the “Laws of your state” section, they outline the mandatory reporting laws for Floridaall states. Florida’s mandated reporting law can be viewed there or on the Florida Courts website.
Mandatory Reporting Requirements on Children
Children are defined as any unmarried person under the age of 18 years who has not been emancipated by court order.
Who is required to report (from a healthcare professional standpoint):
- Physicians
- Osteopathics physicians
- Medical examiners
- Chiropractors
- Nurses
- Some hospital personnel
- Nursing Home and assisted living facility staff
- Health or mental health professionals
- Social workers
- Paramedics
- Emergency medical technicians
When is a report required:
- When any person knows or has cause to suspect that a child is abused, abandoned, or neglected by a parent, legal custodian, caregiver, or another person responsible for the child’s welfare, or that a child is in need of supervision and care and has no one to provide care.
- When any person knows or has cause to suspect that a child is abused by an adult other than a parent, legal custodian, or another person responsible for the child’s welfare.
- When any person knows or has cause to suspect that the child is a victim of childhood sexual abuse or the victim of a known or suspected juvenile sexual offender.
Reports can be made to the Department of Children and Families abuse hotline at 1-800-96-ABUSE (1-800-962-2873) or at Florida DCF Reporter Portal.


Self Quiz
Ask yourself…
- What policies and protocols are in place at your facility regarding mandatory reporting?
- Who can initiate a report?
- What departments are notified, at your facility, if a report is made?
Elements of a Safety Plan (Escape Plan)
Abusers may go to extremes to prevent a victim from leaving. This may result in the decision to escape an abusive relationship – one of the most dangerous times for the victim of domestic violence. The creation of a safety plan can assist in enhancing the safety of a victim during all phases of a relationship and during the planning phase of actually leaving the abuser.
Knowledge of the various elements of a safety plan will enable the healthcare professional to initiate dialogue with a victim and guide them in the development of a personalized plan of safety moving forward. Discussion of safety plans/escape plans can be very difficult during the limited interactions of an emergency room or clinic visit; therefore, familiarity with the key elements of a plan will help navigate the victim to the most appropriate resources for their situation.
The following overviews of a safety plan are from Safe Horizon and the National Domestic Violence Hotline [23][24]. The Safe Horizon is a victim assistance nonprofit for victims of violence and abuse in New York City since 1978. The following outline provides a detailed overview of the many aspects to consider when formulating a safety plan. Review the entire plan outlined on their website Safe Horizon. Consider creating a template handout for your facility to distribute to domestic violence victims.
A safety plan is an outline that includes ways to remain safe while in a relationship, planning to leave, or after you leave [23]. A personalized safety plan assists in coping with emotions, telling friends and family about the abuse, and the steps to be taken in the event of necessary legal action. An effective safety plan should have specific details tailored to your unique situation.
Considerations in creating your safety plan:
- Do you have a trusted confidant – a friend, family member, or neighbor?
- What are some areas in your neighborhood you could go to in an emergency?
- Are there phone numbers you need to memorize in the event of an emergency?
- Do you have children that need to be part of your safety plan? Where would your children go if they witnessed violence?
- Do you need a safety plan for work or school?
- Where can you safely store your safety plan? Computer? Phone?
Before Leaving
The decision to leave an abusive relationship requires courage and preplanning. Consider these measures before leaving to reduce the risk of violence [23]:
- Record evidence of physical abuse
- Plan with children and identify a safe place where they can go during moments of crisis. Reassure them that their job is to stay safe, not to protect you.
- Call ahead to see what the shelter’s policies are. They can provide information on how they can help and secure a space when it is time to leave.
- Try to set money aside or ask trusted friends or family members to hold money for you.
When Leaving
The following list of items serves as a guide for what to take [23]:
Identification
- Driver’s license or state I.D. card, social security card
- Birth certificate and children’s birth certificates
- Money and/or credit cards
- Checking and/or savings account books
Legal papers
- A protective order, if applicable
- Health and life insurance papers
- Legal documents, including divorce and custody papers
- Marriage license
Emergency numbers
- Local domestic violence program or shelter
- Trusted friends and family members
- The Hotline
Other items to keep in mind:
- Medications and refills (if possible)
- Emergency items, like food, bottles of water, and a first aid kit
- Multiple changes of clothes
- Emergency money
- Address book
- Safe cell phone, if possible
After Leaving
The safety plan should always include ways to ensure your continued safety after leaving an abusive relationship. Here are some precautions to consider [23]:
- Change locks and phone numbers if possible.
- If possible, change work hours and the typical route.
- Alert school authorities of the situation.
- If a protection order is present, keep a certified copy present at all times, and inform friends, neighbors, and employers that you have a protection order in effect.
- Consider renting a post office box or using a trusted friend’s address for mail (remember that addresses are used for restraining orders and police reports)
- Use different stores and frequent different social spots.
- Alert neighbors and work colleagues about how and when to seek help.
If comfortable, tell people who can take care of your children or transport them to/from school and activities.
Again, these suggestions provide an extensive overview of an escape plan. They are meant to assist a victim in the required methodical preplanning of a safety plan that reduces the threat of violence. Not all sections will apply to every victim, but healthcare professionals should be comfortable in discussing any aspects of a safety plan specific to the individual victim.
The Effects of COVID-19 on Domestic Violence
As discussed at the beginning of this course, the COVID-19 pandemic has negatively affected domestic violence incidence. Stay at home /shelter in place orders, job losses, mounting financial concerns, and lack of available shelters in many areas became the norm. Domestic violence victims were met with further hurdles to their safety and well-being, as they found themselves sheltering in place with their abuser, along with fewer resources available to them in their time of crisis.
Domestic violence hotlines prepared for an increase in calls. However, many organizations found the opposite occurring. Calls to hotlines dropped, in some places greater than 50 percent. Victims were not able to safely connect with necessary services [25].
Due to the restrictions of movement (curfews, travel bans, 14-day quarantine advisories), not only was it more difficult to escape, but injury from abuse may have gone unnoticed by family and friends as face-to-face interactions had been sidelined. In addition to job losses and financial insecurities, this isolation may have forced a victim to become even more dependent on their abuser [26].
In March 2020, U.S. police departments reported an increase in domestic violence calls as high as 27% after stay-at-home orders were implemented. The number of Google searches for family violence-related help during the outbreak had been substantial. This increase in domestic violence had not only affected the United States. In the United Kingdom, calls to the Domestic Violence Helpline increased by 25% in the first week after implementing lockdown measures. Furthermore, in China, domestic violence had reportedly increased three times in Hubei Province during the lockdown [27]. The importance of ongoing domestic violence education and awareness cannot be overstated.
In review, healthcare staff often treat victims of domestic violence. Trauma-informed care that is patient-focused affords both the staff and patient (victim) the best outcome in terms of successfully navigating the challenges of domestic violence and mandatory reporting laws.
Facility-wide protocols should be in place regarding all aspects of patient care for suspected victims of domestic violence, including national hotline numbers, community resources, scene safety protocols, and house-wide education. Staff should be regularly educated on interviewing techniques, suspected DV victim indicators, and ongoing community collateral relationships. Improved recognition of these victims and knowledge on how to proceed with specific treatment protocols will lead to a higher level of positive outcomes for domestic violence victims and other forms of abuse.
Time is of the essence when dealing with victims of DV. There may be a small window of opportunity to help these victims when they come to your facility. There may be numerous needs identified quickly (transportation, housing, interpretation services, crisis intervention, case management, safety planning, transitional shelter, and protective orders, to name a few). Staff must feel confident in their abilities to identify possible victims, guide them through the process of seeking help, and advocate for their safety and well-being. Knowledge of their facility protocols and community, state, and national resources will afford them the opportunity to deliver optimal care.


Self Quiz
Ask yourself…
- Can you give examples of what your facility is doing to address the issue of domestic violence?
- How had COVID-19 affected your facility in terms of the availability of community resources for victims of domestic violence?
- What improvements can be made at your facility regarding domestic violence education and awareness?
Case Study
Mary, 26 years old, presents to the emergency department with complaints of abdominal pain, vague body aches, and a headache. During the triage screening, Mary has minimal eye contact with the nurse and appears inadequately dressed for the cold weather, arriving in only jeans, a t-shirt, gym shoes, and a light sweater. While the nurse helps Mary change into a hospital gown in a private examination room, she notices various bruises on Mary’s lower back, arms, and legs, all varying size and color. Mary states she slipped and fell recently at home. You observe that Mary is now avoiding all eye contact, staring down at the ground. She keeps looking at the door, and wall clock, mumbling, “He can’t know I’m here.”
- What are your initial thoughts about Mary’s physical appearance?
- What can you do to make Mary feel more relaxed, comfortable, and safe during her emergency room visit?
Mary lives with her boyfriend, Bill. He works part-time; she is currently unemployed. She admits to the occasional use of alcohol and recreational use of marijuana “to help me relax. My anxiety is very bad lately.” She mentions that her anxiety has increased because “Bill’s hours at work have been cut due to COVID-19 and we’re strapped for money. He is under a lot of pressure.”
On further examination and laboratory testing, including a pelvic examination, it is confirmed that Mary is approximately six weeks pregnant and has a suspected sexually transmitted infection. Mary bursts into tears and says, “He is going to kill me. We can’t afford a baby. What am I going to do?!”
- What are your concerns about this scenario? How will you address these concerns with your patient Mary?
- Why might healthcare professionals, in general, feel uncomfortable speaking with Mary?
- What are the top priorities of Mary’s care at this time?
- What information would you document in the patient record during this visit?
Mary begins to feel comfortable speaking to you about her situation. She reluctantly tells you that Bill pushed her down the back stairs yesterday after an argument but quickly apologized afterward. On another occasion, Bill “beat me up” when he ran out of beer before payday. She states he has been really angry lately over his hours being cut at work and is looking for another job. “A baby now,” Mary confides, “would be a terrible thing for Bill, but I want it. It’s my first, and I want it. Please help me.” Mary gives consent for you to contact your department social worker for additional guidance but does not want law enforcement notified.
- What other key staff members need to be part of the care team for Mary?
- What local and national resources can you refer Mary to at this time?
- How would your plan of care change if Mary did not give consent for the social worker to be notified?
Mary wants to “go back home” tonight so as not to upset Bill when he returns later this evening. “It will be better this way.” She promises to leave him tomorrow and follow-up with the community referrals you gave her. Knowing that these plans may change, you advise Mary to create a safe escape plan “just in case.”
- What items should be part of a safe escape plan?
- How safe is it for Mary to return home?
- What are your legal obligations to Mary regarding Florida’s mandatory reporting laws?
As you are getting ready to leave at the end of your shift hours later, you see Mary arrive by ambulance. She is visibly injured with a broken nose and bloody lip. The emergency medical response team stated the neighbors called 911 when they heard Mary screaming in her apartment next door. No one else was in the apartment when they entered, and Mary would not tell them who injured her. You escort them to a private examination room. Mary sees you and yells, “He’s coming after me. Help me. He is going to kill me.”
- What are your top priorities for Mary and the staff at this time?
- What other hospital departments need to be notified?
Mary’s boyfriend shows up, intoxicated, at the triage window, demanding to see Mary. He threatens to kick in the door to the main examination room if he cannot see Mary immediately. He is pacing back and forth in the triage area and refuses to sit down.
- What additional security measures need to be in place upon the boyfriend’s arrival?
Mary’s boyfriend is removed from the premises by local law enforcement. Mary is given the national hotline number and is contacting the local shelter at this time. Upon discharge, she is escorted by security personnel to the exit and leaves the facility with a shelter representative.

Florida-Specific Domestic Violence Resources
Community Legal Services of Mid-Florida
A full service civil legal aid law firm that promotes equal access to justice, providing professional legal aid on domestic violence to help low-income people protect their health, and their families.
https://www.clsmf.org/violence-protection/
Coast to Coast Legal Aid of South Florida
The Family Law Unit primarily focuses on representing victims of domestic violence in family law matters, such as obtaining an injunction (restraining order), dissolution of marriage cases (divorce), and custody litigation.
https://www.coasttocoastlegalaid.org/
Domestic Shelters.org
Overview of 58 Florida based organizations offering domestic violence services in 47 different cities.
https://www.domesticshelters.org/help/fl.florida
Florida Department of Children and Families
Florida Family Policy Council
Resources to assist victims (and family members) to find help, safe shelter, legal aid, transitional services, and counseling.
https://www.flfamily.org/get-help/domestic-violence
Florida Department of Children and Families:
Child Protective Services:
https://www.myflfamilies.com/service-programs/abuse-hotline/
Florida Abuse Hotline:
The Florida Abuse Hotline accepts reports 24 hours a day and 7 days a week of known or suspected child abuse, neglect, or abandonment and reports of known or suspected abuse, neglect, or exploitation of a vulnerable adult.
1-800-96-ABUSE (1-800-962-2873)
TTY: 1-800-955-8771
https://reportabuse.dcf.state.fl.us/
MyFlFamilies.com
These services include emergency shelter, counseling, safety planning, case management, child assessments, information, and much more.
These shelters may be viewed on the MyFlFamilies.com website. Healthcare professionals should be familiar with shelters available in their surrounding area.
Domestic Violence Hotline: 1-800-500-1119
Harbor House of Central Florida
Offering housing placements service, legal aid, safety planning, support groups, and crisis intervention.
(407) 886-2856
https://www.harborhousefl.com/get-help/safety/
The 15th Judicial Circuit of Florida Batterers Intervention Program (BIP)
The Florida BIP is a 6-month intensive program to address root causes of domestic violence; it is at least 26 weeks of group counseling sessions. A list of statewide providers is available on this site.
https://www.15thcircuit.com/program-page/bip
The Salvation Army
Offering emergency and transitional housing, as well as counseling and rehabilitation services.
National Domestic Violence Resources
Amend, Inc.
AMEND is a nonprofit organization working to end domestic violence by providing counseling to men who have been abusive, advocacy and support to their partners and children, and education to the community. Based in Colorado.
Emerge
Emerge is a Massachusetts Certified Batterer Intervention Program & Training Site, offering abuser education groups and batterer intervention. Based in Massachusetts.
617-547-9879
National Domestic Violence Hotline
1-800-799-SAFE (7233)
Domestic Violence Prevention, Inc
501C3 nonprofit offering education, counseling, and support services to domestic violence clients in multiple counties in Texas and Arkansas.
903-793-HELP (4357)
National Center on Domestic Violence, Trauma and Mental Health
Offering direct website links to multiple national organizations working with domestic violence cases.
http://www.nationalcenterdvtraumamh.org/resources/national-domestic-violence-organizations/
National Network to End Domestic Violence
Offers a range of programs and initiatives to address the complex causes and far-reaching consequences of domestic violence.
New York Model for Batterer Programs National Organization for Men Against Sexism (NOMAS) Model for DV Offender Accountability
Court-ordered program for batterer education, which includes a court-imposed consequence if the offender does not attend. Based in New York. Formerly known as the New York Model for Batterer Programs.
845-842-9125
https://www.nymbp.org/ https://nomas.org/
Women’s Law
Providing state-specific legal information and resources for survivors of domestic violence.
Conclusion
Domestic violence is a national crisis that can lead to poor outcomes for victims. Nurses have the responsibility to ensure that victims are properly screened, provided appropriate education, and supported with resources for safety. Creating a safe space for victims to share concerns, helping them to create escape plans, and respecting their decision to stay or leave the relationship is all a part of providing the best care possible.
Florida HIV/AIDS
This fulfills the continuing education requirement of Florida HIV/AIDS for the state of Florida.
An estimated 1.2 million Americans are living with HIV. As many as 1 in 7 of them do not even know they are infected. The others utilize the healthcare system in a variety of ways, from testing and treatment regimens to hospitalizations for symptoms and opportunistic infections. Healthcare professionals in nearly every setting have the potential to encounter patients with HIV as the disease can affect patients of any age or stage of life (4). Proper understanding of HIV is important in order to provide high-quality and holistic care to these patients. For nurses practicing in the state of Florida, it is also important to understand the laws, statutes, and regulations regarding testing, treatment, reporting, and confidentiality related to Florida HIV and AIDS within the state.
Introduction
An estimated 1.2 million Americans are living with human immunodeficiency virus (HIV). As many as 1 in 8 do not even know they are infected (7). The others utilize the healthcare system in a variety of ways, from testing and treatment regimens to hospitalizations for symptoms and opportunistic infections.
Healthcare professionals in nearly every setting have the potential to encounter patients with HIV as the disease can affect patients of any age or stage of life. Proper understanding of HIV is important in order to provide high-quality and holistic care to these patients. For nurses practicing in the state of Florida, it is also important to understand the laws, statutes, and regulations regarding testing, treatment, reporting, and confidentiality related to HIV and AIDS within the state.
Statistics
Rates of infection are not equal across demographic groups, and certain factors may increase a person's risk. Patient information to consider when determining someone's risk includes:
Age
As of 2021, the age group with the highest incidence of new HIV diagnoses is 13-34 years, approximately 58% of new infections (7). Cases are down 18% in this age group from 2017.
Race/Ethnicity
African Americans had the highest number of new HIV cases in 2021, at approximately 40% (7). This is followed by Hispanic/Latinos at 29%, and whites at 26%.
Gender
Males are disproportionately affected by HIV, accounting for 81% of new cases in 2021 (7). Females accounted for 24% of new cases. This data refers to the sex of someone at birth. When looking at the transgender population, those who have transitioned male-to-female were 2% of new cases and female-to-male, less than 1% (7).
Sexual Orientation
Men who have sex with men (MSM) remain the population most at risk of HIV, accounting for around 70% of all new infections in 2021 (7). Cases are down 13.5% in this group from 2017.
Location
Different areas of the country are affected at different rates for a variety of factors, including population density, racial distribution, and access to healthcare. The southern states are unmistakably more affected than other regions, and accounted for 52% of new cases in 2021 (7). Western states account for 21%, Midwest 14%, and Northeast 14% (7).

Transmission
Perhaps the most elusive part of this virus for many years was how it spreads. We now know that HIV is spread only through certain bodily fluids. An accurate understanding of HIV transmission is important for healthcare professionals to provide proper education to their patients, reduce misconceptions and stigmas, and prevent transmission and protect themselves and other patients (8).
Bodily Fluids
Bodily fluids that can transmit the virus include (9):
- Blood
- Semen and pre-seminal fluid
- Rectal fluid
- Vaginal fluid
- Breastmilk
- Fluids that may contain blood such as amniotic fluid, pleural fluid, pericardial fluid, and cerebrospinal fluid
If one of these fluids comes into contact with a mucous membrane such as the mouth, vagina, rectum, etc., or damaged tissue such as open wounds, or is directly injected into the bloodstream, then transmission of HIV is possible (8).
Ways of Transmission
Scenarios where transmission is possible include:
- Vaginal or anal sex with someone who has HIV (condoms and appropriate treatment with antivirals reduce this risk)
- Sharing needles or syringes with someone who has HIV
- Mother-to-child transmission during pregnancy, delivery, or breastfeeding (appropriate treatment during pregnancy, c-section delivery, and alternative feeding methods reduce this risk)
- Receiving a transfusion of infected blood or blood products (this is very rare now because of screening processes for blood donations)
- Oral sex with someone who has HIV (though this is very rare)
- A healthcare worker receiving a sharps injury with a dirty needle (risk of transmission is very low in this scenario)
HIV cannot be transmitted via:
- Saliva
- Sputum
- Feces
- Urine
- Vomit
- Sweat
- Mucous
- Kissing
- Sharing food or drink
- Ticks or mosquitos
Reducing Transmission & Infection Control
Patient education about risk and protection against HIV, testing, and what to do if exposed should be standard practice for healthcare professionals in nearly all healthcare settings. Ideally, primary care should include risk screenings and routine patient education to help prevent infections from occurring (or preventing worsening of infections that have already occurred) (8).
Prevention Strategies
Strategies to help prevent the spread of HIV include (8):
- Identifying those most at risk, particularly MSM, minorities, and those who use drugs by injection
- Ensure patients are aware of and have access to protective measures such as condoms and clean needle exchange programs
- Provide routine screening blood work for anyone with risk factors or desiring testing
- Providing access to PrEP medications where indicated (discussed further below)
- Staying up to date on current recommendations by the U.S. Centers for Disease Control and Prevention (CDC), and HIV developments
- Maintaining a nonjudgmental demeanor when discussing HIV with patients, to welcome open discussion
Pre-Exposure Prophylaxis
For patients with a repeated or frequent high risk of HIV exposure, such as those with an HIV+ partner or those routinely using needles for drugs, pre-exposure prophylaxis (PrEP) may be a good choice to reduce the risk of contracting the virus. When used correctly, PrEP is 99% effective at preventing infection from high-risk sexual activity and 74% effective at preventing infection from injectable drug use (10).
Depending on the type of exposure risk (anal sex, vaginal sex, needle sharing, etc.), PrEP needs to be taken anywhere from 7-21 days before it reaches its maximum effectiveness (10). Most insurances, including Medicaid programs, cover PrEP at least in part (10). There are also federal and state assistance programs available to make PrEP available to as many people who need it as possible. Some side effects are commonly reported, primarily gastrointestinal symptoms, headaches, and fatigue (10).
Viral Load
For those who have a confirmed diagnosis of HIV/AIDS, the focus should be promoting interventions that will prevent further transmission. One of the biggest determinants for transmission is the infected person's viral load. Individuals being treated for HIV can have their viral load measured to ensure viral replication is being controlled as intended. A viral load lower than 200 copies of HIV per milliliter of blood is considered undetectable, meaning the virus is not transmissible to others (4). Even for those not receiving treatment, there are methods to reduce transmission (11).
Infection Control Methods
Methods of infection control for healthcare professionals include (3):
- Universal precautions when handling any bodily fluids
- Eyewear when at risk for fluid splashing
- Careful and proper handling of sharps
- Facilities having a standard plan in place for potential exposures
If an exposure or needlestick does occur, the patient would ideally submit to testing for HIV to determine if the staff member is at risk. If the HIV status of the patient is unknown or confirmed to be positive, post-exposure prophylaxis (PEP) may be advised to start within 72 hours of exposure (12).

Self Quiz
Ask yourself...
- What are some strategies to reduce Florida HIV/AIDS transmission?
- Have you or any of your coworkers ever had a needlestick occur?
- How did you handle that situation?
Florida HIV/AIDS Treatment
When HIV is appropriately treated, advancement from HIV to AIDS can be significantly reduced, and quality and longevity of life maximized. In 2018, the CDC estimated around 65% of all US citizens living with HIV were virally suppressed, and 85% of those receiving regular HIV-related care were considered virally suppressed at their last test (5). However, as mentioned earlier, an estimated 13% of all HIV cases do not know they are infected. Appropriate medical care and keeping viral loads undetectable is one of the single most effective methods of preventing transmission (4, 5).
For those receiving treatment, a multifaceted and individualized approach can reduce a person's viral load, reduce the risk of transmission, reduce the likelihood of developing AIDS, and preserve the immune system. Regardless of how early someone receives treatment, there is no cure for HIV, and an infected person will be infected for life. All individuals diagnosed with HIV (even asymptomatic people, infants, and children) should receive antiretroviral therapy or ART as quickly as possible after a diagnosis of HIV is made. The classes and available medications for ART include the following (1). There are many other combination formula HIV medications, for example emtricitabine/tenofovir (brand name, Truvada), although not listed here.
Nucleoside Reverse Transcriptase Inhibitors (NRTIs)
Nucleoside reverse transcriptase inhibitors (NRTIs) inhibit the transcription of viral RNA to DNA blocking reverse transcriptase (an enzyme needed for HIV replication).
- Abacavir
- Emtricitabine
- Lamivudine
- Tenofovir disoproxil fumerate
- Zidovudine
Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs)
Non-nucleoside reverse transcriptase inhibitors (NNRTIs) inhibit the transcription of viral RNA to DNA by binding to and altering reverse transcriptase. As mentioned above, transcriptase is an enzyme HIV needs to make copies of itself.
- Doravirine
- Efavirenz
- Etravirine
- Nevirapine
- Rilpivirine
Protease Inhibitors
Protease inhibitors block HIV protease (another enzyme needed for HIV replication).
- Atazanavir
- Darunavir
- Fosamprenavir
- Ritonavir
- Saquinavir
- Tipranavir
Fusion Inhibitors
Fusion inhibitors prevent the virus from entering the CD4-T lymphocyte cells (CD4 cells) of the immune system.
- Enfuvirtide
Integrase Strand Transfer Inhibitors (INSTIs)
Integrase strand transfer inhibitors (INSTIs) block HIV integrase (an enzyme needed for HIV replication).
- Cabotegrevir
- Dolutegravir
- Raltegravir
Attachment Inhibitors
Attachment inhibitors prevent HIV from entering CD4 cells by binding to the gp120 protein on the surface of the virus’ cell.
- Fostemsavir
Post Attachment Inhibitors
Post attachment inhibitors prevent the virus from binding to and entering CD4 cells by block the CD4 receptors on the surface of some immune cells. HIV needs these receptors to enter the cells.
- Ibalizumab-uiyk
Capsid Inhibitors
Capsid inhibitors interfere with the HIV capsid (a protein shell that protects the enzymes HIV needs for replication).
- Lenacapavir
Pharmacokinetic Enhancers
Pharmacokinetic enhancers increase the effectiveness of HIV medications.
- Cobicistat


Self Quiz
Ask yourself...
- How do fusion inhibitors work against HIV?
- How do entry inhibitors work against HIV?
- How soon after diagnosis should patients receive antiretroviral therapy?
- Make a mental list of treatments available for patients of Florida HIV/AIDS.
Florida HIV/AIDS Laws
The Omnibus AIDS Act is based on the premise that illness can be best controlled through public knowledge. If the public is aware of potential illness, and ways to avoid contracting and transmitting illness, that is the best method of prevention and further spread (2). The state of Florida became one of the first states with high rates of HIV infection within their population to enact legislation surrounding the AIDS epidemic. Transmission of HIV, as aforementioned, occurs through direct contact with virus-containing body fluids. Activities by which transmission involves such as sexual activity, needle stick, blood transfusion, or mother-to-baby, the government cannot regulate. Therefore, the governmental response to a disease epidemic must rely primarily upon the education of the public and its cooperation with their educational efforts and recommendations (2).
Informed Consent
The following are regulations surrounding informed consent and HIV testing in the state of Florida (2).
Information Requirements
Healthcare providers performing HIV tests must have advanced procedures in place regarding patient consent, testing samples, and informing patients of their results (2). “Since the 1998 amendments to the Act, health care providers must, as a matter of law, convey three pieces of information, all essentially involving the choice of a testing site, as part of the process of obtaining informed consent:
- Disclose that the provider is required by law to report the test subject’s name to the local county health department if the HIV test results are positive;
- Alert the patient that as an alternative, the patient may secure the HIV test at a site that tests anonymously, the locations of which the provider must make available; and
- Relate the extent of the confidentiality rights that adhere to the test results in the provider's patient records.”
Minors
“The general rule that parental consent is required prior to medical diagnosis or treatment of a minor does not apply when sexually transmitted diseases such as HIV infection are involved. Indeed, Florida specifically forbids telling parents the fact of the minor's consultation, examination or treatment for a sexually transmissible disease, such as HIV infection, either directly or indirectly (such as by billing a parent or their insurer for an HIV test without the child's permission).”
“Infants and young children are treated as unable to make an informed decision and consent of their parents or legal guardian is required. For older children (such as teenagers), however, the provider must make an individual judgment whether the child, as phrased in Department of Health rules, ‘demonstrates sufficient knowledge and maturity to make an informed judgment,’ meaning, whether the child has the cognitive and emotional capacity to understand the risks and benefits of the test or treatment to which the child is being asked to consent.”
Documentation
“As with other medical procedures requiring informed consent, informed consent for HIV testing does not necessarily mean written consent. Except for donations of blood and other tissues and to obtain health or life insurance, Florida does not require providers to have the test subject sign a document authorizing the test. The health care provider need only enter a note in the medical record that the test was explained and consent was obtained.”
Exceptions
Exceptions to informed consent requirements by health care providers (2):
Pregnancy
“Following federal legislation and recommendations from CDC, Florida law in 1996 first imposed “mandatory offering” of HIV tests for all pregnancies upon presentation. In 2005, the statute was further amended to establish the present system of “opt out” testing, in which pregnant women are advised that the health care provider attending them will conduct an HIV test but that they have the right to refuse. The pregnant woman’s objection is required in writing, which must be placed in her medical record” (§384.31, F.S.)
Emergencies
“A provider may test without consent in "bona fide medical emergencies," but only if the provider documents in the medical record that the test results are medically necessary to provide appropriate emergency care or treatment to the test subject and the test subject is unable to consent” (§381.004(2)(h)3, F.S.).
Therapeutic Privilege
“The Act allows a "therapeutic privilege" that bypasses informed consent requirements when the provider's medical record documents that obtaining informed consent would be detrimental to the health of a patient suffering from an acute illness and that the test results are necessary for medical diagnostic purposes to provide appropriate care or treatment to the patient. This same privilege applies to all medical procedures for which informed consent is required. The statute emphasizes that this provision provides no basis for routinely testing patients for HIV without their informed consent” (§381.004(2)(h)4, F.S.).
Sexually Transmissible Diseases
“State laws permit HIV testing for sexually transmissible diseases on certain subjects, such as convicted prostitutes (§796.08, F.S.), inmates prior to release (§945.355, F.S.), and cadavers over which a medical examiner has asserted authority §381.004(2)(h)1.c., without the consent of the test subject. This exception includes exempting pregnancy “opt out” testing from informed consent requirements discussed above.”
Criminal Acts
“Victims of criminal offenses that involve transmission of body fluids may require the person charged with or convicted of the offenses to be tested for HIV infection by requesting a court to order the test” (§960.003(2), F.S.). “Similarly, when a defendant, prosecuted for certain offenses in which transmission might have occurred, has been ordered to or has voluntarily given a blood sample, the victim may request the sample be tested for evidence of HIV without the consent of the defendant” (§381.004(2)(h)6, F.S.).
Organ and Tissue Donations
“Various statutory provisions permit testing without informed consent in specifically identified specialty areas: certain blood and tissue donations; corneal removals and eye enucleation that Florida allows by law to be done without consent; autopsies to which consent to perform the autopsy was obtained” (§§381.004(2)(h)2, 5 and 9, F.S.).
Research
“Established epidemiologic research methods that ensure test subject anonymity is expected from informed consent” (§381.004(3)(h)8, FS)
Abandoned Infants
“When a licensed physician determines that it is medically indicated that a hospitalized infant have an HIV test, but the infant's parent(s) or legal guardian cannot be located after reasonable attempts, the test may be performed without consent. The reason why consent could not be obtained must be documented in the medical record and the test result must be provided to the parent(s) or guardian once they are located” (§381.004(2)(h)13, F.S.).
Significant Exposure
“The blood of the source of significant exposure to medical personnel or to others who render emergency medical assistance may be tested without informed consent” (§381.004(3)(h)10-12, FS).
Repeat HIV Testing
“Renewed consents are not required for repeat HIV testing either to monitor the clinical progress of a previously diagnosed HIV-positive patient or for conversion from a significant exposure” (§§381.004(2)(h)14 and 15, F.S.).
Judicial Authority
“A court may order an HIV test to be performed without the individual's consent” (§381.004(3)(h)7, FS).

Self Quiz
Ask yourself...
- What groups of individuals are exceptions to informed consent requirements when it comes to Florida HIV/AIDS?
Florida HIV/AIDS Confidentiality
The following are regulations surrounding confidentiality of HIV testing in the state of Florida (2).
Not every piece of medical information about a person who has been tested for HIV or assessed for AIDS is protected. “Only the fact that an HIV test was performed on an identifiable individual and any ‘HIV test result’ (negative as well as positive) are specially protected” (§381.004(2)(e), F.S.).
The statute definitions (11):
- HIV test: “test ordered after July 6, 1988, to determine the presence of the antibody or antigen to human immunodeficiency virus or the presence of human immunodeficiency virus infection” (§§381.004(1)(b), F.S.)
- HIV test result: “laboratory report of a human immunodeficiency virus test result entered into a medical record on or after July 6, 1988, or any report or notation in a medical record of a laboratory report of a human immunodeficiency virus test” (§§381.004(1)(c), F.S.)
“Only a laboratory report of an HIV test result entered in a medical record on or after July 6, 1988 (the effective date of the Omnibus AIDS Act), or any report or notation in a medical record of a laboratory report of an HIV test, falls within their scope.”
“Explicitly excluded from the definition of an HIV test result are reports from patients of their HIV status to health care providers. Consequently, patient reports of their HIV test status from Department of Health anonymous testing sites, from home access HIV test kits or from any other sources do not constitute ‘HIV test results’ unless separately confirmed by the provider through a laboratory report or a medical record containing a laboratory report. Patient disclosures of an HIV test or infection to persons other than health care providers caring for the patient under the provisions of the Act also do not fall within the statute's special confidentiality protections.”
Voluntary Partner Notification
The following are regulations surrounding voluntary partner notification of HIV exposure in the state of Florida (2).
“The person ordering the HIV test (or that person’s designee), although under no liability exposure to the sexual or needle-sharing partners of their HIV-positive patients, is required to advise their patients with HIV-positive test results of the importance of notifying partners who may have been exposed” (§381.004(2)(c), F.S.). Practitioners are well advised also to tell the patient of the availability of voluntary partner notification services provided by the Department of Health. Under the authority provided in §384.26, F.S., county health department staff offers voluntary and confidential partner notification and referral services to persons infected with HIV. When notifying partners, county health department staff are required not to reveal the identity of the original client.”
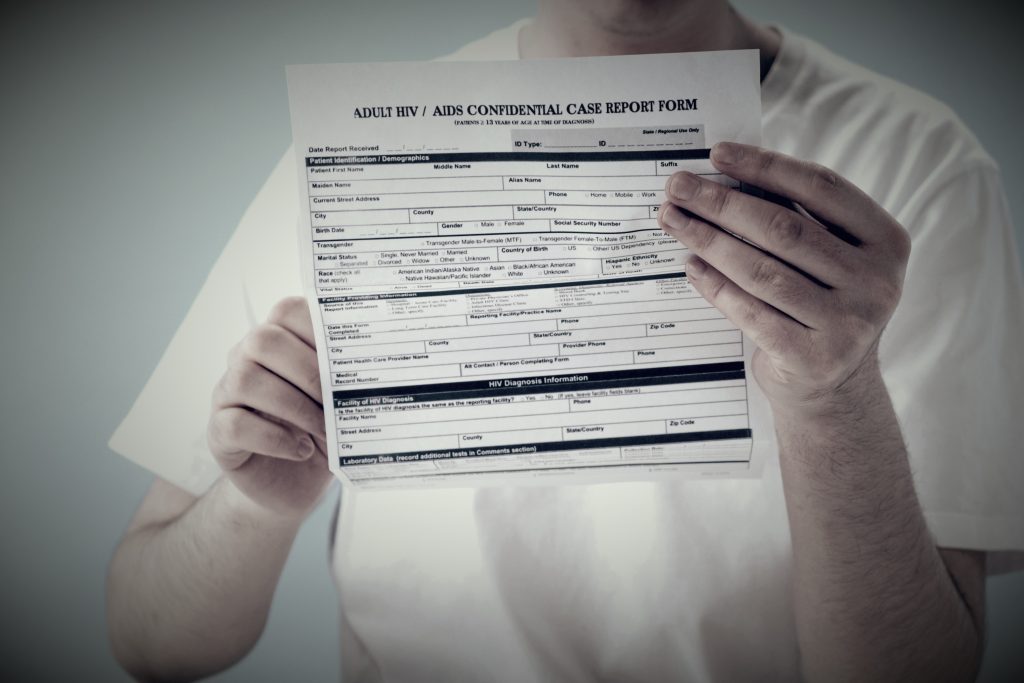
Florida HIV/AIDS Infection Reporting
The following are regulations surrounding HIV infection reporting in the state of Florida (2).
“In 1996, Florida became one of the first states with a high incidence of AIDS to authorize regulatory procedures requiring physicians and laboratories to report to local health authorities HIV-positive test results with patient identifiers” (§384.25, F.S.). “Practitioners and clinical laboratories that fail to report HIV-positive test results are subject to a $500 fine and disciplinary action by their licensing boards” (§384.25(4), F.S.).
“This change was spurred in part by the Ryan White CARE Act. Enacted in 1990 and reauthorized in 2009 as the Ryan White HIV/AIDS Treatment Extension Act, this federal legislation now provides funding to urban areas, states and localities to improve the availability of care for low-income, uninsured and under-insured AIDS and HIV-infected patients and their families.”
“Florida’s HIV infection-reporting requirements increases available Ryan White funding for persons with the illness and enables the Department of Health to link them to medical and support services earlier in the process of infection.” Under the rules by the Department of Health of Florida:
- “Practitioners must report to their local county health department within two weeks of the HIV-positive diagnosis of all persons, EXCEPT infants born to HIV-positive women, which must be reported the next business day” (Rule 64D-3.029, FAC and Rule 64D-3.030(5), FAC).
- “Clinical laboratories must report to the local health department HIV test results from blood specimens within three days of diagnosis” (Rule 64D-3.029, FAC).
Florida Laws and Regulations
The following course content
Introduction
The state of Florida has several statutes that govern the practice of nurses. These statutes consist of Chapters 456 and 464 in Title XXXII Regulation of Professions and Occupations. The Florida Administrative Code is where Division 64B9 is located.
Chapter 464, often called the Nurse Practice Act, is separated into two parts. Part I discusses the advanced practiced registered nurse, registered nurse, and licensed practical nurse. This statute ensures that every nurse practicing in Florida is held to and meets the same minimum standards for safe practice.
Because of this, nurses who do not meet the minimum requirements or display harm to society are not allowed to practice nursing in the state of Florida. The Board of Nursing is the governing body for the Nurse Practice Act and deals with matters such as providing licensure, creating rules, and managing disciplinary actions. Part II of chapter 464 focuses on the certified nursing assistant.
Chapter 456 is a statute directed at all healthcare providers and professions. This statute lists the provisions that Chapter 464 is built on.
Division 64B9 is part of the Florida Administrative Code that provides specific rules that pertain to nurses and how the profession is regulated in terms of eligibility to take the examination of selected practice, set standards for nursing education curriculum and institutions, continuing education requirements, license renewal; rules for impairment of the nurse in the workplace and more.
This course is designed to meet the requirements of Division 64B9-5 as it pertains to two continuing educational hours about Florida’s laws and regulations of nursing practice.

Definitions (3, 4, 5)
Advanced or specialized nursing practice — completion of post-basic specialized training, experience, and education that are appropriately performed by an advanced practice registered nurse. The advanced-level nurse can “perform acts of medical diagnosis and treatment, prescription, and operation” under the authorization of a protocol with the supervision of a physician.
Advanced practice registered nurse (APRN) — any individual who is licensed in this state to practice professional nursing as defined above and holds a license in advanced nursing practice, including:
- Certified Nurse Midwives (CNM or nurse midwife)
- Able to perform superficial or minor surgical procedures as defined by a protocol and approved by the employing medical facility or with a backup physician in the case of a home birth.
- Start and perform approved anesthetic procedures.
- Order appropriate medications based on patient and condition.
- Manage care of the normal obstetrics patient and the newborn patient.
- Certified Nurse Practitioners (CNP)
- Able to manage some medical issues guided by facility or supervising provider protocols.
- Manage and monitor patients who have stable, chronic illnesses.
- Start, monitor, and adjust therapies for select, uncomplicated illnesses.
- Order occupational and physical therapy based on patient needs.
- Certified Registered Nurse Anesthetists (CRNA)
- Able to order pre-anesthetic medications as stated and approved by facility protocols and staff.
- Determine and consult with the supervising anesthesiologist about the proper anesthesia for patients based on labs, history, and physical and patient conditions.
- Assist with managing the patient in the post-anesthesia care unit.
- Clinical Nurse Specialists (CNS)
- A nurse prepared in a CNS-focused program that meets the requirements of a typical APRN program. Additionally, they are trained in the area of expertise that pertains to the advanced practice of nurses.
- Psychiatric Nurse
- Has a master’s or doctoral degree in psychiatric nursing and has a national advanced practice certification as a psychiatric mental health advanced practice nurse.
- has two years of post-master's clinical experience under the supervision of a physician.
- They can prescribe psychotropic controlled substances for the treatment of mental health disorders.
Board — the Board of Nursing.
Licensed Practical Nurse (LPN) — any person licensed in this state or holding an active multistate license under s. 464.0095 to practice practical nursing as defined below.
Practice of practical nursing — the performance of select actions, including the management of specific treatments and medications, while taking care of the ill, injured, or infirm; prevention of illness, promotion of wellness, and health maintenance in others under the direction of a registered nurse, or a licensed provider: physician, osteopathic physician, podiatric physician, or dentist; and the teaching of general health principles and wellness to the public and students other than nursing students. A practical nurse is responsible and accountable for making decisions based on their educational preparation and experience in the profession.
Practice of professional nursing — the performance of actions requiring substantial specialized knowledge, judgment, and nursing skill based on applied principles of physical, psychological, social, and biological sciences, which shall include, but are not limited to:
- The nursing process consists of assessment, nursing diagnosis, planning, intervention, and evaluation of care; teaching and counseling of the ill, injured, or infirm in matters of health; prevention of illness, promotion of wellness, and maintenance of the health of others.
- The administration of medications and treatments as prescribed or authorized by a duly licensed practitioner as they are authorized to do so by the laws of this state to prescribe such medications and treatments.
- The management and education of other individuals, such as nursing students, in the theory and performance of any of the acts described above.
A professional nurse is responsible and accountable for making decisions based on the individual's educational preparation and experience.
Registered nurse (RN) — means any person licensed in this state or holding an active multistate license under s. 464.0095 to practice professional nursing as defined above.
A registered nurse first assistant (RNFA) — is a registered nurse who assists in surgery while in the hospital setting under a physician. They help maintain cost-effective and quality surgery for patients in Florida. They must be certified in perioperative nursing via a core curriculum approved by the Association of Operating Room Nurses, Inc.

Self Quiz
Ask yourself...
- What license or licenses do you currently hold? Have you held another permit in the past?
- What other licensed nursing providers do you work with at your facility?
- What type of APRN license listed in the above definitions surprised you the most? Why?
- Do you agree with the definitions of practical nursing and professional nursing? What is your rationale?
Board of Nursing: Members and Headquarters Location
Florida’s Board of Nursing has 13 unique members that Florida's governor appoints. To maintain diversity and representation of the entire nursing profession, the following criteria must be met (5):
- Seven members must be RNs with a minimum of four years of experience in practice.
- One must be an APRN
- One must be a nurse educator
- One must be a nurse executive
- Three members must be LPNs with a minimum of four years of experience in practice.
- The final three members have no connection to the nursing profession or affiliation or contract with a healthcare agency.
- One member must be over the age of 60
- All members must be residents of the state of Florida
Membership terms last for four years; however, if the governor does not have a successor to appoint, the members can serve for another four years. The Board of Nursing's headquarters is in Tallahassee per Florida statute (5).
The members of the Board have several roles and responsibilities while serving. Their primary job is to ensure that nurses practicing in Florida are doing so safely. To do this, the Board members can create and implement rules or provisions to add to the Nurse Practice Act.
They can approve educational programs for institutions wishing to teach nursing. They can take disciplinary action against a nurse for violating the Nurse Practice Act or other Florida laws. Disciplinary actions can consist of citations, fines, or disciplinary guidelines based on the nurse in question, previous offenses, and the severity of the violation. (5).
Licensure by Examination and Endorsement
Initial licensure requires an individual to examine their desired profession: NCLEX-RN, NCLEX-LPN, and either the American Nurses Credentialing Center (ANCC) or the American Association of Nurse Practitioners (AANP) version for those wishing to become an APRN. In order for the Board of Nursing to approve an individual to sit for their desired examination, a list of requirements must be met in total (5):
- You must correctly complete an application for the desired examination and submit a fee set by the Board.
- Submit to a background check conducted by the Department of Law Enforcement.
- Must be in good physical and mental health and receive a high school diploma or equivalent.
- Has completed the following requirements:
- Graduate from an approved program on or after July 1, 2009, OR
- Graduate from a prelicensure nursing education program that has been determined to be equivalent to an approved program by the Board before July 1, 2009
- Must have the ability to communicate effectively in English as determined by the Department of Health through another examination as indicated.
It is important to note that there is a section dedicated to the scenario of an individual failing the examination or needing to take it within six months of graduating.
Candidates can take the test up to three times if they fail it. Suppose an individual needs to pass their examination of choice after three attempts. In that case, they must take a Board-approved remediation course before they can sit for the examination again. From there, they are given three more chances to take and pass the test before they must remediate again. Reexamination must occur within six months of the approved remediation course (5).
If an individual fails to take their examination within six months of graduation, they must take an exam preparation course approved by the Board. It is to be advised that the individual must pay for the course without using federal or state financial aid (5).
Courses completed in a professional nursing education program that are at least equivalent to a practical nursing education program may be used to satisfy the education requirements for licensure as a licensed practical nurse. This means a registered nursing program student could take the licensure for an LPN license once the courses they have taken meet the LPN licensure requirements (5).
If a nurse holds licensure in another state or US territory and decides to obtain Florida licensure, theycan do so through endorsement. Florida requires those who apply to submit a nonrefundable fee, complete the application, and provide fingerprints for a criminal background check. The Florida Board of Nursing will not issue a license to an individual under investigation when applying (5).
Military Spouses
Applying for a license through endorsement is a route that can be used for nurses who are traveling with military spouses on official military orders. Nurses must have actively practiced nursing for two of the three years before applying for a license. Military spouses also have the option of obtaining a 12-month temporary Florida license if they meet the requirements (4):
- Holds a valid nursing license in another state
- Has a negative criminal background check
- Has not failed their licensure exam
- Has not had any disciplinary action taken against them in another state
Licensure by Compact
Over 40 states in the United States have created legislation to allow nurses to work under one multistate license (2). This means a nurse originally licensed in Florida could work in any other state that participates in the Nurse Licensure Compact without obtaining licensure for each state they wish to work in if they have a multistate license. This has proven especially useful over the years due to the growing nursing shortage and global pandemic.
Many states like Florida are offering to provide multistate licenses to nurses during their initial examination. If a nurse does not obtain a multistate license initially, they can do so later. They must pay a fee and submit fingerprints for a background check. Nurses must also meet any other requirements set by the state of Florida (2).
It is important to note that in Florida, the nurse who holds the compact license must claim residency in the state. If the nurse were to claim residency in another state, they would no longer have a multistate license issued by Florida. If the state they move to is part of the Nurse Licensure Compact, they might be eligible to obtain a compact license in their new home state (2, 5).
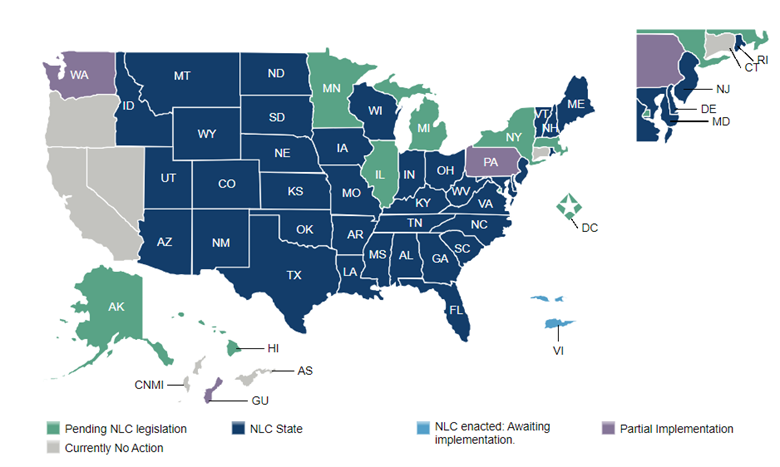
(2)

Self-Quiz
Ask Yourself...
- Do you feel as though Florida’s Board of Nursing has a diverse nursing population?
- Who should appoint members to the Board?
- What information were you required to provide to the Board of Nursing when you applied to take your licensure exam?
- Have you obtained licensure through endorsement, whether in Florida or another state?
- When do you anticipate nurses being able to practice in all 50 states and US territories? Will this be beneficial to healthcare? Why or why not?
Delegation to the Unlicensed Assistive Personnel (UAP) or Unlicensed Personnel (UP)
The Nurse Practice Act defines delegation as transferring a task or activity during a specific situation by a qualified nurse, through licensure and experience in the task, to a competent individual. Different facilities may have several ways of determining the competence of the individuals they employ, but ultimately, the decision rests with the RN or LPN.
The licensed provider must evaluate the task’s difficulty, the potential for predictable or unpredictable harm or rapid change in the patient’s condition, and the level of communication required with the patient. They must also consider the resources available and skills the UAP can do at their facility (4).
When delegating, it is essential to assess the UAP’s skill set through validation or verification. The nurse should communicate clearly regarding the delegated task and explain the desired outcomes. They should also explain what undesired outcomes could occur, what should be done if an undesired outcome does happen when the task should be completed, and if supervision by the nurse is required.
The nurse should follow up to ensure the task was done correctly and within the set time frame. The nurse should be aware that the delegated task and any outcomes are the nurse’s responsibility, and they are ultimately held accountable for it. So, if it is an important task, it may be in the best interest of the nurse to delegate another task to the UAP and perform the critical task themselves (4).
There are a few skills that cannot be delegated to the UAP:
- A skill that is not within the delegating nurse’s scope of practice
- Activities require using the nursing process or specific education, judgment, training, or skills.
- Initial assessments and progress evaluations relate to the patient’s plan of care.
- Skills that a UAP needs to display competence.
IV Administration by LPNs
As mentioned above, LPNs and RNs have a few variations in their scope of practice. LPNs can administer and perform some parts of IV medication therapy instead of the RN, who can do all. IV therapy administration is the infusion or injection of a medication via the intravenous system.
This method involves several aspects, including evaluating, observing, monitoring, discontinuing, titrating, managing, planning, documenting, and intervening during administration. RNs do not always have to be onsite when delegating IV administration to an LPN, but knowing policies and when an RN must be on site is essential (4).
LPNs cannot do any of the following (4):
- Initiate blood or blood products or plasma extenders.
- Mix IV solutions.
- Administer or initiate cancer treatments such as chemotherapy or investigational medications.
- IV pushes, except for heparin or saline flushes.
LPNs may care for patients receiving these therapies, such as actively receiving a blood transfusion, but they cannot do the above.
LPNs can (4):
- Calculate and adjust flow rates.
- Observe and report any signs of adverse effects of IV medications.
- Assess IV insertion sites and change dressings as needed and as educated.
- Remove IV catheters or needles from peripheral veins.
- Hang IV hydrating fluids.
In order for an LPN to administer IV medications through a central line, they must do so under the direction of an RN and have four hours of IV therapy education on central lines. This four-hour requirement can be applied to the 30 total hours LPNs must do on IV therapy (4).
LPN Supervision in Nursing Homes
According to Florida law, LPNs can supervise other LPNs, certified nursing assistants (CNAs), or UAPs in the nursing home setting. To be considered for a supervisory position, the LPN must have completed 30 hours of board-approved, post-basic education courses under the supervision of an RN.
The LPN must also have at least six months of full-time clinical experience either in a hospital or nursing home setting. If the LPN takes a course outside of the Board’s approval courses, the provider of said course must test the LPN and provide attestation of the LPN’s competency (4).
The supervisory LPN’s role is to provide other LPNs, CNAs, and UPAs with guidance and inspection of their completed task per their appropriate scope of practice. The LPN can only delegate tasks within their scope of practice and be assured that the one they are delegating to demonstrates competency (4).
Certified Nursing Assistant (CNA)
The certified nursing assistant is similar to the UAP. Still, to be certified, they must have completed a background check conducted by the Board of Nursing, prove they can read and write, and pass the nursing assistant examination. Once the criteria listed have been met, CNAs can provide general care and assist with activities of daily living under the direction of an RN or LPN. They can also participate in postmortem care and perform CPR (4).

Self-Quiz
Ask Yourself...
- Think of your facility or organization: what types of UAPs do you have? CNAs, Patient Care Technicians (PCTs), emergency service technicians?
- Are you aware of what you can and can’t delegate to them?
- Are there any LPNs where you work?
- What can they do, and what types of patients can they care for?
- Some acute care facilities have started to wean out the LPN role while others are hiring them to address short-staffing needs within their organizations. What do you think of these decisions and which do you prefer?
Maintaining Medical Records
For RNs and APRNs in private practice, the Florida Nurse Practice Act has two rules regarding maintaining medical records. The first applies to the death of the nurse. Whoever legally represents the RN or APRN must post a notification in the county newspaper stating where the medical records are being stored and who to contact if an individual wants to obtain the records. The documents must be stored for a minimum of two years after the death of the nurse (4).
At the 24-month mark, several notices must be posted in the county newspaper, one notification for four consecutive weeks, that the medical records will be destroyed four weeks after the last day of the fourth week that the notice was published (4).
The second rule pertains to an RN or APRN who has terminated or relocated their practice. The rule states that the RN or APRN maintains and holds onto the medical records for at least two years. They must let those who were patients know about the date of termination or relocation and where the medical records can be retrieved.
The notice must be made public, such as in a newspaper, with a minimum appearance of four times over four weeks. A sign must be placed at the location of the business about the termination or relocation until the termination or relocation happens. This sign must tell patients about the opportunity to obtain their medical records (4).
Continuing Education (CE) Requirements
Florida law requires that for renewal of a nursing license, the nurse seeking renewal must complete a set amount of CE hours. Over the two years, 24 hours must be completed, one for each month. Two of those hours must be about the Florida Nurse Practice Act and the other laws that pertain to the nursing profession.
Two hours are required to investigate medication errors and how to prevent them. A one-hour HIV/AIDS is necessary for initial renewal but does not have to be repeated. There must be a two-hour course on domestic violence done every third renewal. As of August 2017, a two-hour course on recognizing impairment in the workplace is required with each renewal (4).
In Florida, completed CE courses are automatically reported to a tracking system created by the Department of Health’s Division of Medical Quality and Assurance (MQA) or manually by the individual. Those who attend CE courses will obtain a certificate of attendance. The attendee is advised to maintain a copy of those certificates for at least four years.
For Florida, the provider of the course, the individual or company that is offering the training, has 90 days (about 3 months) to report to the tracking system, so if the nurse’s date of renewal is less than 90 days, it is suggested that the course be manually reported by the nurse (4).
If a nurse has two licenses, such as RN and LPN or APRN and RN, they may be able to comply with both license requirements through one set of CE requirements. For example, an RN with an LPN license can meet all the CE requirements of the LPN license by completing the RN requirements (4).
Nurses who serve as expert witnesses and provide expert opinions in writing can obtain 2.5 hours for each case. The case must cite at least two current articles of reference being reviewed regarding the Nurse Practice Act (4).
There are a few exemptions to completing the CE renewal requirements. It is advised that the nurse contact the Board of Nursing with specific questions or concerns regarding renewal and CE requirements (4):
- If the nurse is on active duty for the US military within six months of the renewal date.
- This does not apply to short periods of active duty, such as summer or weekend drills.
- This does not apply to those on duty in the US Public Health Service.
- If the nurse’s spouse is a member of the US military and the nurse was absent from the state of Florida because of military duty.
- The nurse must provide adequate proof of the spouse’s absence and military status.

Self-Quiz
Ask Yourself...
- What types of classes do you take to complete your continuing education? Online, in-person, webinar? Which one do you like the best?
- What Florida-mandated classes do you have the most challenging time finding and completing?
- Do you hold licenses in two aspects of nursing, such as LPN and RN, or RN and APRN? If so, how do you complete both your continuing education requirements?
- Do you use a CE tracking site to ensure you are compliant with your CEs? What are the pros and cons of using it?
Disciplinary Action
As mentioned above, the Florida Board of Nursing, as outlined in the Nurse Practice Act, can discipline nurses as they see fit regarding all violations of Florida rules and laws. The Board created a variety of ways a nurse can be punished, ranging from probable-cause panels to citations to disciplinary hearings to loss of nursing license. The severity of the violation reflects on which method the Board of Nursing may take (5).
There are three probable-cause panels in Florida: North Florida, Central Florida, and South Florida. The purpose of these panels is to determine if there was “probable cause” or reasonable ground for the reported case. They decide if a case needs action taken. The panel members review each case and compare it to others of a similar nature, how the Board has treated those cases in the past and what the Board’s guidelines entail. The panel can recommend and consider rules regarding procedures, penalties, and disciplinary actions (5)
Citations can be given in lieu of other forms of discipline. The citation is issued within six months of a complaint being filed and contains the request for the recipient to fix the violation within a specified time frame. These violations are usually classified as “minor” in nature, such as false advertising, falsely using a nursing title, or failure to report the change of address or updates of information required by the Board.
Other reasons a citation can be issued include failing to report a misdemeanor within 30 days of a ruling or failing to utilize the law-required prescription drug monitoring system. Each of these citations can come with a fine, usually ranging from $100 to $250 in amount; however, if a nurse is found guilty of sharing passwords, codes, keys, or other forms of entry to a secure medication administration device or information technology system a fine of $1,500 can be given. In addition, the nurse would have to take a two-hour CE course on legal nursing aspects within 60 days of the citation being issued (5).
The Board of Nursing has the power to take any of the below appropriate actions against nurses who have violated parts of the Nurse Practice Act. It is important to note that any of the actions can be combined, depending on the severity of the violation and the action taken by the nurse after the violation was committed (5):
- Probation, suspension, or revocation of a license
- It can be emergently done depending on the situation.
- Require CE course(s) to be done
- Letter of concern
- Reprimand
- Administer a fine
- A personal appearance is required before the Board of Nursing to monitor compliance.
- Restrict or limit a nurse’s scope of practice.
- Example: prohibiting a nurse from administering any narcotics after they are participating in drug diversion
- Referral to the Intervention Project for Nurses (IPN)
The Board of Nursing has also created an extensive, but not all-encompassing list of reasons why a nurse can be disciplined (5):
- Sexual misconduct
- Unprofessional conduct
- Participating in crime related to healthcare fraud
- Making or filing a false report to appease state or federal law
- Willfully hindering another individual in filing a report that is required by state or federal law
- Testing positive on any drug screen when the individual has no medical/other reason for using the drug
- Inability to practice nursing with satisfactory skill and provide safe patient care due to the use of narcotics, drugs, alcohol, chemicals, or other substances that may impair an individual
- Inability to practice nursing with satisfactory skill and provide safe patient care due to an illness, physical or mental condition
- Failing to meet minimal standards of acceptable nursing practice
- Accepting and performing professional responsibilities the nurse knows or has reason to know they are not skilled to perform
- Delegating or contracting for the performance of professional duties by a person who the nurse knows or has reason to know is not qualified by training, experience, and authorization required to perform
- Failing to identify the type of license the nurse is practicing under through written (can include a nametag) or oral notice to a patient
- Performing or attempting to perform healthcare services on the wrong site or the wrong procedure on the wrong patient includes unauthorized procedures
- Performing or attempting to perform healthcare services that are medically unnecessary or otherwise not related to the patient’s diagnosis or medical condition(s)
- Being convicted or found guilty of or pleading nolo contendere (no contest) to a crime in any jurisdiction that directly relates to the practice of nursing or the ability to practice nursing
- Being convicted of or found guilty of, or pleading nolo contendere to misdemeanors related to failure to protect an adult from abuse, neglect, and exploitation; fraudulent practices; theft and robbery; or having committed an act of domestic violence or child abuse
- Defaulting on a student loan that has been issued or guaranteed by the state or federal government
As with everything in life, the Board of Nursing has created guidelines for imposing discipline. They have a set minimum and maximum amount when it comes to fines. They have time frames for probation or supervision, conditions regarding probation, or the reinstatement of a license. What route they decide to take depends upon the specific case being presented to them. Sometimes, the circumstances presented to the Board are enough to elicit decisions outside the general guidelines. Some of these circumstances are (5):
- Length of time a nurse has practiced
- Presents a danger to the public
- Any visible effort at rehabilitation
- Treatment and disciplinary hearing costs
- Actual physical or other forms of damage caused by the nurse
- Financial hardships
The Board has a timeframe in which a complaint must be filed. Most of the time, it is within a six-year window from the time the incident occurred. However, in certain circumstances—criminal actions, sexual misconduct, impairment of the nurse, or usage/diversion of controlled medications—the Board may allow the complaint’s time frame to extend beyond the six-year timeframe.
Suppose action such as fraud, intentional misrepresentation, or concealment is utilized to hide the violation during the six years. In that case, the timeframe to file a complaint can be extended to 12 years from when the incident occurred (5).
If the Board of Nursing suspends a nurse’s license or agrees to have the license suspended to avoid further action against them, the nurse can possibly file a petition to have their license reinstated. Any final orders or terms issued during the initial suspension must be met as a whole, and the nurse must be able to demonstrate the ability to perform nursing practice safely.
Sometimes, a time frame is set for when a nurse can file a petition; sometimes, there is not. If this is the case, a nurse can appeal as soon as they can after meeting the terms and conditions given to them by the Board (5).
The Board will determine what a nurse must do to demonstrate safe practice. This is based on the violation. For example, a nurse who is working while under the influence of medications or alcohol may be ordered to attend a treatment program with proof of sobriety, references, and completion of any court-mandated sanctions. Nurses must often present to the Board of Nursing in person and speak on their ability to practice nursing (5) safely.
The three-strike policy is utilized when it comes to reinstating a license. Suppose a nurse has been found guilty on three separate occasions of a complaint about drug/narcotic usage or the diversion of medications from patients to the nurse for personal use or to sell. In that case, the Board will not reinstate the license (5).
Relicensing a nurse who has had their license revoked is similar to what happens when a license is suspended. However, the nurse must reapply for the permit and meet all conditions set by the Board. Nurses may have to sit for another examination or take board-approved continuing education if the nurse has been out of practice for an extended period of time. They may require a nurse to participate in Florida’s Intervention Project for Nurses (IPN) program or at least be evaluated for it (5).
Nurses are held accountable for reporting the actions of other nurses and any misconduct to the Board of Nursing. They must report sexual misconduct or healthcare fraud. If they know or have reason to believe that another nurse is not practicing safely or is practicing under the influence of alcohol or medications, they are required to report it (5).

Self-Quiz
Ask Yourself...
- Do you know anyone who has had action taken against them regarding the Nurse Practice Act?
- If so, what was the outcome?
- What other actions do you think could violate the Nurse Practice Act? What other actions outside the Nurse Practice Act should the Board of Nursing address?
- What do you think is the most severe violation listed above?
- Is the Board of Nursing’s list of potential actions that could be taken against a nurse’s license fair?
- If you were on the Board, what types of disciplinary action would you recommend?
Florida’s Intervention Project for Nurses (IPN)
Created in 1983 under the authority of the Nurse Practice Act, IPN was designed to protect the public by monitoring nurses whose skills have been compromised due to improper use of medications or alcohol or the impairment of mental or physical health. IPN is not a treatment center.
Instead, they provide nurses with access to Board-approved practitioners who specialize in addiction, mental health, and other medical conditions to assist the nurses in restoring themselves to a level of safe practice. They also conduct monitoring after a nurse has been discharged from treatment, interventional training, consultations, and advocacy for those who participate (1).
As mentioned above, nurses have an obligation to report themselves or nurses who are, or they have reason to believe, unsafely practicing nursing while under the influence of alcohol or medications. The report is confidential if a nurse self-reports or is reported to the IPN only and they complete treatment and five years of monitoring. If the Board of Nursing becomes involved, either through a failure to report or complete treatment, disciplinary action may be taken (1).
In the beginning, nurses are not able to practice during the initial evaluation period or when the treatment is being determined. After a treatment plan is made, it is up to the discretion of the IPN and the providers involved in the treatment to say if the nurse is able to continue working as a nurse. Restrictions on a nurse’s practice are often implemented during the beginning phase of treatment(1).
To be determined “fit to practice,” the nurse must meet all requirements set by their providers and the IPN. They must sign an advocacy contract, submit to random drug tests, verbalize their understanding of practice restrictions, and participate in a weekly support group for nurses (1).

Self-Quiz
Ask Yourself...
- Should the IPN be a treatment center as opposed to a resource center? Should they offer both?
- Should the status of a nurse who has enrolled in this program, willingly or not, be confidential, even if they do not meet the requirements?
- Should a nurse be allowed to practice nursing with set limitations while being involved with an IPN? Why or why not?
- Do you know anyone who was involved in IPN? What were their limitations of practice? Were they successful or not?
Conclusion
Despite the extensive outline of the Nurse Practice Act and other state rules in this course, it only briefly narrates all Florida laws pertaining to nurses. In addition to this course, nurses must stay on top of new legislation being proposed and implemented regarding their profession and continually review the content in the state laws. Nurses who travel to other states to practice their profession should be educated on each state’s rules regarding nursing practice, as they can differ from state to state. A conscious effort must be made to follow the laws set in place to practice nursing safely and legally in the state of Florida.
Florida Medical Errors
This fulfills the continuing education requirement for Medication Errors Prevention for the state of Florida.
For as long as there have been medical professionals, there have been medical errors. Medical errors can be small and seemingly insignificant to a catastrophic sentinel event.
The Joint Commission (TJC) is a healthcare accrediting agency that sets the standard for patient safety. Each year, TJC publishes a list of national patient safety goals. These goals are focused on the prevention of medical errors. In 2019, the World Health Organization (WHO) found that medical errors harmed up to 40% of patients within the global healthcare system. These medical errors not only cause harm to millions of people worldwide, but they also cost billions of dollars on an annual basis (8).
There are many different types of medical errors. They include, but are not limited to: medication errors, healthcare-acquired infections, surgical errors, lab errors, falls, documentation issues, and omitted care. Healthcare workers must be aware of the possible harm that can be caused by medical errors and the ways in which they can be prevented.
Introduction
For as long as there have been medical professionals, there have been medical errors. Medical errors can be small and seemingly insignificant to a catastrophic sentinel event.
The Joint Commission (TJC) is a healthcare accrediting agency that sets the standard for patient safety. Each year, TJC publishes a list of national patient safety goals. These goals are focused on the prevention of medical errors. In 2019, the World Health Organization (WHO) found that medical errors harmed up to 40% of patients within the global healthcare system. These medical errors not only cause harm to millions of people worldwide, but they also cost billions of dollars on an annual basis (8).
There are many different types of medical errors. They include, but are not limited to: medication errors, healthcare-acquired infections, surgical errors, lab errors, falls, documentation issues, and omitted care. Healthcare workers must know the possible harm caused by medical errors and how they can be prevented.

Self Quiz
Ask yourself...
- What prior knowledge do you have concerning errors in the medical field?
Factors That Impact the Occurrence of Medical Errors
There are multiple factors that can increase the probability of a medical error occurring. Healthcare worker behaviors and attitudes, staffing, and communication are among those that have the most significant impact on medical errors.
In healthcare, a risky behavior is an action that may lead to a compromise in patient safety. Why would any healthcare worker engage in at-risk behaviors? Healthcare workers, especially nurses, are generally compassionate and are ultimately looking out for the patients' welfare in their care. Risky behaviors produce a quick, positive reward without any perceived risk of patient harm. These risky behaviors can range from a simple short-cut like not checking two patient identifiers to a blatant disregard for hospital/facility policy. In all instances, the risk for patient harm is real and will eventually occur (13).
Understaffing in the hospital setting continues to be a factor contributing to medical errors. Poor nurse-to-patient ratios can lead to a variety of medical errors. Ordered patient care may go undone, leading to further medical errors adverse patient outcomes (7). Understaffing leads to fatigue and burnout. A nurse in this state of mind is prone to committing medical errors.
Miscommunication between healthcare professionals and patients and miscommunication between healthcare professionals also contribute to the occurrence of medical errors. As part of their national patient safety goals, TJC has had a communication component almost every year. They have recognized that effective communication is paramount in the prevention of medical errors. A lack of effective communication can be a leading cause of every type of medical error.
In an effort to decrease communication errors, TJC has taken measures to ensure that effective communication is promoted in a variety of different situations. TJC has instituted a list of unacceptable medical abbreviations. This list will decrease medication errors by removing confusion when medications are ordered (11). They also developed a handoff communication protocol for facilities to implement. The handoff communication occurs anytime that care is passed from one caregiver to another. In Florida medical errors prevention, this communication protocol is used to ensure that all pertinent patient information is passed on to the next healthcare worker rendering care to the patient. By using effective handoff communication, all information should be passed on, and mistakes should be avoided (10).

Self Quiz
Ask yourself...
- Have I ever participated in at-risk behavior at my facility?
- Did this contribute to the occurrence of a medical error?
- Is my unit staffed appropriately?
- Do healthcare professionals in my facility use an appropriate hand-off communication tool?
- In Florida medical errors prevention, what communication tool can be used between healthcare professionals?
Recognizing Error-Prone Situations
Studies have shown that the majority of medical errors occur in the inpatient setting. The most common areas for medical errors are the operating room (OR), the emergency room (ER), the intensive care unit (ICU), and the medical/surgical floors (1).
What is it about the inpatient setting that makes it such an error-prone area? More specifically, why do medical errors occur in the ICU, OR, and ER? These are all high-stress areas where effective communication between all parties is vital. Breakdown in communication in these areas will lead to catastrophic medical errors. When the stress level rises, the probability of medical errors occurring also rises. These are also fast-paced areas where the condition can change in the blink of an eye. When we work in such a busy area, we can forget important details. Effective communication is a big part of Florida medical errors prevention. Miscommunication in these environments is a recipe for medical errors.
As the most common type of medical errors is medication errors, we do need to talk about medication administration. Nurses are taught the five rights of medication administration in nursing school:
- Right drug.
- Right patient.
- Right dose.
- Right route.
- Right time.
When working in a busy inpatient setting, nurses may fail to perform the five rights in order to save time (5). Neglecting any one of the five rights of medication administration can cause a medical error.

Self Quiz
Ask yourself...
- Do I work in an error-prone environment?
- What makes the area error-prone?
- Why is communication so integral to Florida medical errors prevention?
- What can I do to decrease stress levels on the job?
Processes to Improve Patient Outcomes
In the technological age in which we live, it is more important than ever before that healthcare facilities consistently demonstrate good patient outcomes. The Centers for Medicare & Medicaid Services (CMS) places great importance on the patient experience and their perception of their healthcare experience quality. Every patient who experiences a hospital stay may be asked to complete a Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. The survey results are published quarterly on the CMS Hospital Compare website. There, patients can compare the hospital's results and choose a hospital where they would like to have their care rendered (4). A medical error could very well cause a patient to give a facility a poor rating on the HCAHPS survey. That is why we must take Florida medical errors prevention seriously.
When medical errors have occurred, they will often result in a risk management response to investigate why the error has happened and how it can be prevented in the future – a root cause analysis (RCA). An RCA will often lead to department-driven performance improvement projects (PIP) to eradicate the problem and improve patient outcomes. A proactive facility trying to minimize medical errors will have multiple department and facility-wide PIP.
As previously stated, each year TJC publishes a list of patient safety goals. These goals will often guide a facility on specific patient outcomes that have required attention for improvement on a national level. They focus on the prevention of medical errors, and as such, they can steer PIP. Accreditation hinges on the ability of a facility to improve and consistently deliver positive patient outcomes. Below is the current list of TJC's patient Safety Goals:
1. Identify patients correctly.
Use at least two ways to identify patients. For example, use the patient's name and date of birth. This is done to make sure that each patient gets the correct medicine and treatment.
2. Improve staff communication.
Get important test results to the right staff person on time.
3. Use medicines safely.
Before a procedure, label medicines that are not labeled. For example, medicines in syringes, cups, and basins. Do this in the area where medicines and supplies are set up.
Take extra care with patients who take medicines to thin their blood.
Record and pass along correct information about a patient's medicines.
Find out what medicines the patient is taking. Compare those medicines to new medicines given to the patient.
Give the patient written information about the medicines they need to take. Tell the patient it is important to bring their up-to-date list of medicines every time they visit a doctor.
4. Use alarms safely.
Make improvements to ensure that alarms on medical equipment are heard and responded to on time.
5. Prevent infection.
Use the hand cleaning guidelines from the Centers for Disease Control and Prevention or the World Health Organization. Set goals for improving hand cleaning. Use the goals to improve hand cleaning.
6. Identify patient safety risks.
Reduce the risk for suicide.
7. Prevent mistakes in surgery.
Make sure that the correct surgery is done on the correct patient and at the correct place on the patient's body.
Mark the correct place on the patient's body where the surgery is to be done.
Pause before the surgery to make sure that a mistake is not being made.
(12)

Self Quiz
Ask yourself...
- What are some PIP in my department?
- What are some PIP in my facility?
- What are some overal PIP in Florida medical errors prevention, that affect all state level facilities?
- What are the current JCM National Patient Safety Goals?
Responsibilities for Reporting as a Part of Florida Medical Errors Prevention
Each individual facility across the nation may have different policies and procedures for the reporting of medical errors within their facilities. There is, however, a growing trend throughout the healthcare industry of creating a culture of safety. The culture of safety promotes the reporting of medical errors and "near misses" in an open, transparent and non-punitive manner. Facilities are taking a stand to ensure patient and staff safety over other competing goals within their system (14). Near miss reporting allows for issues to be addressed and corrected before an actual error occurs. Taking a non-punitive approach to self-reporting of medical errors promotes accurate reporting and allows for a true picture of what is happening in the facility.
The State of Florida has mandated that all licensed healthcare facilities implement an internal risk management program. In Florida medical errors prevention, it is the responsibility of the risk management team to:
- Investigate and analyze the frequency and cause of general and specific types of patient adverse incidents.
- Develop measures to minimize the risk of adverse incidents.
- Analyze patient grievances that relate to care and quality of services.
- The development and implementation of an incident reporting system.
State law further requires that the Agency for Healthcare Administration (AHCA) post quarterly reports on adverse incidents (9).

Self Quiz
Ask yourself...
- How do I report a medical error in my facility?
- Who is the Risk Manager in my facility?
- Do I work in a culture of safety?
- How do I play a role in Florida medical errors prevention?
Safety Needs of Special Populations
There are certain groups of people that are especially vulnerable to experience a medical error.
Elderly
The elderly are especially susceptible to medical errors. Generally, as we get older, we tend to start taking more medications. Complex medication regimens offer a greater opportunity for medication errors. Many medications require close monitoring of vital signs and/or blood levels. Drug-related issues are a major driving force for both ER visits and nursing home admissions among the elderly (3). Declining cognition, poor vision, and increased forgetfulness associated with aging can also play a part in medication errors. Education with frequent reinforcement and the use of support people are crucial to help prevent medication errors.
The elderly are also at a higher risk for falls. Falls within a medical facility can lead to further medical complications, increased length of stay, and serious injury. Patients at risk for falls need to be identified and place on a fall prevention protocol.
Children
Children are on the other side of the spectrum and are also another group that are at higher risk for medical errors. Younger children may be unable to accurately voice exactly their problem is, or what symptoms they are experiencing. They must rely on both parents and other caregivers for the coordination of their care. Though a parent may know their child well, they may not be able to properly convey their child's issues to the healthcare professional. It is also important to realize that children are not little adults. Care plans must be catered to their specific phase of life.
Limited Health Literacy/Education
Another population that is vulnerable to medical errors are patients with limited health care literacy or education. These patients may have difficulty obtaining, retaining, and implementing health information to make proper decisions for their healthcare needs. Populations within this group may include the elderly, low-income populations, immigrants, and minorities. There is also a strong correlation between limited health literacy and the uninsured, undereducated, and unemployed populations. It is important that information be presented to this group at a level that they can understand. The use of interpreters can also be helpful if the patient does not have a good grasp of the English language (6).

Self Quiz
Ask yourself...
- What is the level of health literacy in the community where I live?
- What population to I work with on a daily basis?
- Do I present information to them at a level that they can understand?
Public Education
Now, more than ever before, the general public has greater access to information of all sorts. This includes access to health information, specifically, patient outcomes. The public is able to make informed decisions on where they would like to be cared for by comparing healthcare facilities.
The public is seeking information not only on which facility is the safest with the best outcomes but also on ways that they can actively prevent medical errors from happening to them. There are many resources that patients can find online to help them recognize scenarios that may place them at risk for the occurrence of medical errors. The Agency for Healthcare Research and Quality (AHRQ) has published a list of 20 tips patients can use to help prevent medical errors:
Medicines
1. Make sure that all of your doctors know about every medicine you are taking.
This includes prescription and over-the-counter medicines and dietary supplements, such as vitamins and herbs.
2. Bring all of your medicines and supplements to your doctor visits.
"Brown bagging" your medicines can help you and your doctor talk about them and find out if there are any problems. It can also help your doctor keep your records up to date and help you get better quality care.
3. Make sure your doctor knows about any allergies and adverse reactions you have had to medicines.
This can help you to avoid getting a medicine that could harm you.
4. When your doctor writes a prescription for you, make sure you can read it.
If you cannot read your doctor's handwriting, your pharmacist might not be able to either.
5. Ask for information about your medicines in terms you can understand—both when your medicines are prescribed and when you get them:
- What is the medicine for?
- How am I supposed to take it, and for how long?
- What side effects are likely? What do I do if they occur?
- Is this medicine safe to take with other medicines or dietary supplements I am taking?
- What food, drink, or activities should I avoid while taking this medicine?
6. When you pick up your medicine from the pharmacy, ask: Is this the medicine that my doctor prescribed?
7. If you have any questions about the directions on your medicine labels, ask.
Medicine labels can be hard to understand. For example, ask if "four times daily" means taking a dose every 6 hours around the clock or just during regular waking hours.
8. Ask your pharmacist for the best device to measure your liquid medicine.
For example, many people use household teaspoons, which often do not hold a true teaspoon of liquid. Special devices, like marked syringes, help people measure the right dose.
9. Ask for written information about the side effects your medicine could cause.
If you know what might happen, you will be better prepared if it does or if something unexpected happens.
Hospital Stays
10. If you are in a hospital, consider asking all health care workers who will touch you whether they have washed their hands.
Handwashing can prevent the spread of infections in hospitals.
11. When you are being discharged from the hospital, ask your doctor to explain the treatment plan you will follow at home.
This includes learning about your new medicines, making sure you know when to schedule follow-up appointments, and finding out when you can get back to your regular activities.
It is important to know whether or not you should keep taking the medicines you were taking before your hospital stay. Getting clear instructions may help prevent an unexpected return trip to the hospital.
Surgery
12. If you are having surgery, make sure that you, your doctor, and your surgeon all agree on exactly what will be done.
Having surgery at the wrong site (for example, operating on the left knee instead of the right) is rare. But even once is too often. The good news is that wrong-site surgery is 100 percent preventable. Surgeons are expected to sign their initials directly on the site to be operated on before the surgery.
13. If you have a choice, choose a hospital where many patients have had the procedure or surgery you need.
Research shows that patients tend to have better results when they are treated in hospitals that have a great deal of experience with their condition.
Other Steps in Florida Medical Errors Prevention
14. Speak up if you have questions or concerns.
You have a right to question anyone who is involved with your care.
15. Make sure that someone, such as your primary care doctor, coordinates your care.
This is especially important if you have any health problems or are in the hospital.
16. Make sure that all your doctors have your important health information.
Do not assume that everyone has all the information they need.
17. Ask a family member or friend to go to appointments with you.
Even if you do not need help now, you might need it later.
18. Know that "more" is not always better.
It is a good idea to find out why a test or treatment is needed and how it can help you. You could be better off without it.
19. If you have a test, do not assume that no news is good news.
Ask how and when you will get the results.
20. Learn about your condition and treatments by asking your doctor and nurse and by using other reliable sources.
For example, treatment options based on the latest scientific evidence are available from the Effective Health Care Web site. Ask your doctor if your treatment is based on the latest evidence (2).

Self Quiz
Ask yourself...
- What education do I provide to my patients vis a vis medical errors?
- Have I ever researched a facility prior to using their services?
Case Studies
Mr. Smith is a 68-year-old male with diabetes type 2, hypertension, and chronic renal failure stage 4. He takes both long-acting and short-acting insulin for his diabetes and a beta-blocker for his high blood pressure. He is also taking a diuretic to help regulate his fluids. Mr. Smith was recently admitted to the hospital for a hypoglycemic event. Once in the hospital, Mr. Smith expressed to his nurse that he has been having difficulty reading his medication labels. He also confided that he feels dizzy when he stands up and has fallen back onto his bed on more than 1 occasion.
After two days, Mr. Smith was ready to be discharged. The diabetic educator brought him some pamphlets and educated him on proper blood glucose monitoring and insulin administration. His blood pressure medicines were also changed, and Mr. Smith was given a new prescription to be filled once he left the hospital. He was alone when discharge instructions were given, and his current medications were not removed from his medicine bag.
Two days later, Mr. Smith was readmitted to the hospital with hypoglycemia and hypotension (BP 87/52).
Exercise
-
What are some factors that lead to the occurrence of medical errors with Mr. Smith?
-
What are the medical errors that occurred?
-
What could the nurse/educator have done differently to prevent further medical errors, using steps addressed in this Florida medical errors prevention course?
Bernice is a staff nurse working in a busy ICU. Due to the COVID-19 pandemic, the unit has been short-staffed, with each nurse taking care of 3-4 patients. This is Bernice's fifth day in a row, working fourteen plus hours. There have been multiple "code blue" situations in the ICU over the course of Bernice's workweek, some involving her patients. She was only able to have a full lunch hour on her second day, and she has not been able to sleep much during the night.
One of her patients was having severe abdominal pain, 9/10 on the pain scale. Bernice went in to administer the ordered narcotic and injected the wrong patient.
Exercise
-
What factors lead to Bernice's medical error?
-
What could have been done to prevent the error?
-
Is this a situation that could happen in a unit where you work?

Self Quiz
Ask yourself...
- What can you take away from these case studies?
Conclusion
Medical errors are an ongoing problem in the healthcare setting. They affect patients in all phases of life and come with a large price tag of both money and medical resources. It is everyone's responsibility to help prevent the occurrence of medical errors. Though we may not be able to totally eradicate them, we can all play a big part in Florida medical errors prevention by learning from previous mistakes and taking measures to ensure that they do not happen again.
Florida Recognizing Impairment in the Workplace
This fulfills the continuing education requirement of 2 contact hours on Recognizing Impairment in the Workplace for the state of Florida.
Up to 20% of nurses in the United States are chemically dependent. Substance use disorders, addictions, drug diversions, and other related impairment processes present a threat to the health and safety of those around them. Increasing in concern are overdoses and deaths that are on the rise due to substance abuse and addiction. Early identification of the signs and symptoms of a substance abuse disorder in the workplace contributes to reducing the risk and harm to patients and other healthcare team members. Co-workers play a crucial role in recognizing and reporting suspicious behaviors to their supervisors or appropriate personnel.
Introduction – Florida Recognizing Impairment in the Workplace
Impairment within the workplace of a healthcare environment is, unfortunately, more common than one may realize. Impairment results when a healthcare professional cannot provide competent and safe patient care because they may be impaired by alcohol, prescription, or non-prescription drugs, or other mind-altering substances (2). Impairments can also result from a psychological or neurological condition that may affect a person’s judgment. Because of impairment, the healthcare professional is unable to perform duties essential to their profession safely.

Self-Quiz
Ask Yourself...
- What prior knowledge do you have about impairments in the workplace?
- Take a moment to think about your experiences with individuals with impairments. How did you respond?
Acknowledging the Problem
Ideally, from a professional standpoint, healthcare personnel should acknowledge their condition and seek help voluntarily without requiring intervention; however, this is often not the case. Co-workers play an important role in helping the impaired person get treatment. Often, the abuser has denial with the condition, the social stigma, or fear of potential job loss. Colleagues are often reluctant to report their co-workers because they feel it is not their responsibility. They feel like the individual they are reporting may be punished excessively. They may believe that someone else has already addressed the issue or fear the loss of their colleague’s job or license. Despite these potential reasons, colleagues may have certain legal responsibilities in identifying and reporting. States may have specific reporting laws that could hold colleagues responsible for harm to patients if they fail to report.

Self-Quiz
Ask Yourself...
- Why might someone refuse report an impairment?
Definitions
Substance Use Disorder : a disease of the brain characterized by the recurrent use of substances such as alcohol and drugs that cause clinical and functional impairment such as health problems, disability, and failure to meet responsibilities at work or school.
The disease involves reward, withdrawal, memory, and motivation and can be classified as mild, moderate or severe depending on the level of impairment (1).
Addiction: the most severe, chronic stage of substance use disorder. There is a substantial loss of self-control, indicated by compulsive substance use despite the desire to stop using (1).
Drug Diversion: is the transfer of any substance from the purpose for which it was intended for any illicit use, such as personal use or sale (1).
Impairment: is the inability or impending inability to engage safely in professional and daily life activities as a result of physical, mental, or behavior disorders such as substance use, abuse, or addiction (1).

Self-Quiz
Ask Yourself...
- Have you experienced a co-worker with impairment in the workplace?
- Have you known of someone you currently work with or have worked with in the past that has had an issue with drug diversion or addiction related to their profession? Was there legal action taken?
- What is the difference between addiction and drug diversion?
- What are different ways that drug diversion can be used for?
- Can you as a healthcare worker be held responsible for failure to report impairment of a co-worker in the workplace?
Impairment Behaviors in the Workplace
Some behaviors are associated with emotional problems but are specific to alcohol or other drug abuse. Some signs common to alcohol and other drugs may also be signs of psychological or psychiatric conditions (2). Each situation is individualistic to the person. Health care professionals must be educated appropriately regarding the signs and symptoms of chemical dependence. The workplace is often the last place that addiction may manifest; disruptions in family, personal health, and social life can happen while the workplace remains unaffected.
Behaviors Associated with Substance Abuse
- Severe mood swings/personality changes
- Frequent or unexplained tardiness, work absence, illness, or physical complaint
- Elaborate excuses
- Under-performance
- Difficulty with authority
- Poorly explained errors, accident, or injury
- Confusion, memory loss, difficulty concentrating
- Visibly intoxicated
- Refuses drug testing
Signs Associated with Substance Abuse
- Unreliability in keeping appointments and meetings
- Trouble with relationships (professional familial, marital)
- Physical indications such as track marks or bloodshot eyes
- Signs indicative of drug diversion
- Deterioration in personal appearance
- Significant weight loss or gain
- Discovered comatose or dead
Signs and Behaviors Associated to Drug Diversion Specific to Anesthesia Personnel (1)
- Consistently uses more drugs for cases than colleagues.
- Frequent volunteering to administer narcotics, relieve colleagues for casework
- Heavy wastage of drugs
- Frequent trips to the restroom or breaks
- Drugs and syringes in pockets
- Anesthesia record does not match up with drug dispensed and administered to patient
- Patient has unusually significant or uncontrolled pain after anesthesia.
- The patient has a higher pain score as compared to other anesthesia providers.
- Times of cases do not correlate when provider dispenses drug from automated dispenser
- Inappropriate drug choices and doses for patients are made by the provider
- Missing medications or prescription pads
Substances such as opioids (e.g., morphine and fentanyl), inhalational anesthetics and volatile agents (e.g., sevoflurane, nitrous oxide), and intravenous anesthetic agents (e.g., propofol) are readily available to many healthcare providers (1). Despite medication dispensing and audit controls in place, drugs can be diverted for misuse. This may happen through the procurement of medicines directly from the pharmacy, automated dispensing units, retrieval from sharps containers of medication remaining in syringes, directly from patient medications, or indirectly through dilution of a medication that appears that nothing is missing from the container (1).
Regardless of the substance being abused, impairment in the workplace can negatively impact patient and provider safety. Facilities should have policies and education addressing symptom awareness, prevention, and reporting to help minimize the risk of diversion and adverse outcomes. Studies have shown that substance use disorder is a disease of the brain (1). As a responsible healthcare provider, by arming yourself with knowledge and the signs and behaviors of impairment in the workplace, it will prevent further harm.
Healthcare providers are usually successful at disguising their issues or potential signs are ignored because they are respected or an intelligent member of the healthcare team. Significant changes in behavior in the workplace may various many causes. If signs of substance abuse and drug diversion are left unrecognized or reported, the user may be placed in danger and patient safety compromised. Impaired health professionals sometimes develop coping mechanisms that allow them to cover up their diminished capacity to provide safe and efficient patient care. Eventually, mistakes are made, including medication and procedural errors that become apparent to their co-workers (3).

Self-Quiz
Ask Yourself...
- What are some of the signs and behaviors associated with substance abuse?
- What are some examples of substances that can be misused in the healthcare workspace?
- Are you familiar with the systems in place in your institution related to substance abuse, reporting, and addiction?
Consequences of Drug Diversion and Substance Use in the Workplace
Healthcare providers are responsible for their patients’ safety, including their duty to deliver safe and competent care without impairment. Impairment in the workplace can create a disorganized environment (1). The consequences to associate with substance use and drug diversion in the workplace may cause the following consequences for the patient themselves, their colleagues, and the facility in which they are employed.
Patient
- Pain, anxiety, and side effects from improper dosing
- Allergic reaction to wrongly substituted drug
- Victim of medical errors
Loss of trust in the healthcare system
Communicable infection from a contaminated needle (1)
Impaired Professional
- Adverse health effects related to abuse
- Chronic health problems (heart disease, liver impairment)
- Familial and financial difficulties
- Loss of social status
- Felony prosecution, incarceration, and civil malpractice
- Actions against a professional license
- Accidents resulting from physical harm (1)
Colleagues
- Injury or infection from blood-borne pathogens from improperly stored equipment
- At risk for shared-patient care responsibilities with an impaired professional resulting in adverse patient outcomes
- The stress of increased workload from an impaired healthcare team member
- Disciplinary action for false witness of leftover medication, improper disposal, or failure to report (1)
Facility
- Costly investigation
- Civil liability for patient harm
- Damaged reputation due to public knowledge of mandatory reporting or drug diversion instances, especially those that led to patient harm
- Poor work quality
- Loss of revenue from diverted drugs or reimbursement from adverse events due to impaired provider (1)
The use of addictive substances over time may result in the deterioration of the healthcare professional’s overall health. For example, the use of stimulants may result in cardiovascular problems such as angina, hypertension, and Myocardial Infarction. Alcohol can lead to liver disease, such as cirrhosis. Depression, suicide, and anxiety are mental health disorders that are often coexisting problems with substance abuse. The healthcare workers’ impairment can also lead to traumatic injuries such as falls, fractures, and head injuries (1).

Self-Quiz
Ask Yourself...
- What are some of the adverse health affects that substance abuse can have on a user?
- What are potential detrimental effects that substance abuse of a healthcare professional can have on a patient? Have you experienced any of these in your workplace?
Florida Rules and Regulations
Many states have rules and regulations regarding the use of alcohol and controlled substances that include disciplinary action. Drug diversion is a significant offense that is taken very seriously. Almost every state requires the reporting of a health practitioner who is suspected of impairment in the workplace. The penalties associated with this vary state by state. Florida requires that all nurses take a Florida Recognizing Impairment in the Workplace CE course every other renewal to improve the recognition and outcomes of workplace impairment.
The state of Florida has an efficient reporting system. Nurses report to the Florida Department of Health or Intervention Project for Nurses (IPN). The IPN’s mission is to enhance public safety by assisting nurses and other nursing related personnel whose practice may have been impaired by substance abuse (4). Their call of the acknowledgment of impairment remains confidential. The Intervention Project for Nurses in Florida allows for an opportunity for intervention and the monitoring of nurses that are using alcohol or controlled substances (4).
The IPN after receiving a referral of impairment will:
- Initiate a consultation
- Provide an intervention
- The nurse will be required to stop practicing within 1-3 days-the entire process may take up to 12 months
- Assist the person in obtaining the appropriate treatment needed
- Evaluate the progress of the person and the adherence to their treatment plan
- Continuously monitor the person for 2-5 years

Self-Quiz
Ask Yourself...
- What does the state of Florida require for impairment reporting?
- After receiving an impairment referral, what steps will the IPN take to address the referral?
Reporting and Intervention
Once a nurse or other employee has determined that there is an issue with a coworker regarding impairment in the workplace, an intervention must occur to prevent further harm from happening to patients, themselves, or other co-workers. According to the Intervention Project For Nurses, the co-worker determines that there is sufficient evidence and documentation to support their concerns of the impairment of a health professional, an intervention should be planned (4). The planning and participation related to such intervention is usually the responsibility of the employee’s nursing manager.
- Intervention process steps: (4)
- Prepare a plan
- Review documentation
- Request help from others
- Ask the person to listen to what is said before allowing them to respond
- Stick to their job performance
- Have evaluator options ready
- Expect denial
- Report as necessary to the Board

Self-Quiz
Ask Yourself...
- What are the steps to report impairment in the work place?
Return to Practice
A recovering nurse’s return to practice requires planning and oversight by a nursing manager. Once a nurse has been determined that they are safe to return to practice, several things must fall into place. These things include developing a return to practice guidelines for that specific employee, such as returning to work agreement. Experts must also advocate for the employees to return to work, provide support, review expectations, monitor requirements, and answer questions (4).

Self-Quiz
Ask Yourself...
- Who supervises a nurse’s return to work when they are recovering?
Considerations Of Relapse
Substance use is a chronic illness that comes unfortunately with periods of remission and exacerbation. The rate of relapse among nurses is lower than the general population (4). This is due to several factors, such as support programs and stringent state monitoring programs. Despite the fact, some nurses relapse. Knowledge of the management of relapse in the workplace is a crucial part of impairment in the workplace and plays a significant role in the safety of patients and other employees (4).

Self-Quiz
Ask Yourself...
- In the state of Florida, who do nurses report impairment to?
- What are some things the Intervention Project for Nurses will do once they have received a referral?
- Can a nurse return to practice after disciplinary action for substance abuse?
Conclusion – Florida Recognizing Impairment in the Workplace
Substance abuse is a chronic and progressive disease. Being able to recognize impairment in the workplace is imperative for the safety of patients, the impaired person, and other co-workers. Impairment can come in many forms. Being knowledgeable of the signs and symptoms as well as reporting responsibilities and policies will not only improve safety but also improve the overall practice environment. Nurses can be very good at picking up subtle clues as to another individual’s impairment. Be aware, be knowledgeable, and be supportive.
Florida Human Trafficking
This course meets the Florida Human Trafficking requirement for nurses in the state of Florida.
Human trafficking is a significant humanitarian issue in the United States and the world that has continued to grow in the past several years despite government and public efforts to combat it. With increasing news coverage of high-profile human and sex trafficking cases, the problem was recently brought into the American public’s eye. However, the results published by the Polaris Project make it evident that human trafficking is not just a problem of the elite or occurring in poorer areas. It is within our own neighborhoods, workplaces, and throughout the State of Florida.
For healthcare workers in Florida, human trafficking can be prevented through gaining the knowledge to recognize the warning signs and specific characteristics of a potential trafficking victim; the most effective ways to intervene, which will enable the victims to gain access to help; and where to garner additional support in addressing the issue.
Prevalence and Definitions
The Polaris Project estimates that collectively there are over 25 million victims of human trafficking worldwide. These are individuals that have been forced into sexual or labor servitude. Of those, several hundred thousand are estimated to be in the United States (1). It is very difficult to estimate accurately as so often this is a crime that is unseen and hidden from the public eye. Since 2007, there were 20,415 contacts made concerning human trafficking reported within Florida to the National Human Trafficking Hotline via telephone calls, texts, or online submissions. Of those, there were 6,168 cases of human trafficking with 15,063 victims being identified.These numbers exemplify the number of potential victims that are not reaching out for help.
Often, when human trafficking is discussed, a common misconception is that it is simply the transporting of humans. Human trafficking covers a much broader scope than this. It is this a modern age form of slavery and involves the exploitation of individuals for monetary or sexual gain. As stated by the Department of Homeland Security, “Human trafficking involves the use of force, fraud, or coercion to obtain some type of labor or commercial sex act” (3).
As defined by U.S. law, there are three categories of human trafficking (all from 1):
- Children under the age of 18 induced into commercial sex
- Adults (age 18 or over) induced into commercial sex through force, fraud, or coercion
- Children and adults induced to perform labor or services through force, fraud, or coercion
The majority of trafficking in the United States involves sex crimes, followed by labor. An increase of rates with 16% for sexual exploitation and 25% for labor was noted in North America during Covid-19 restrictions (4). These crimes may be occurring simultaneously to the same victim. Types of trafficking can include forced prostitution, pornography, strip dancing, criminal enterprise and bonded labor in domestic servitude or migrant work. Outside of street prostitution, sex trafficking is most likely to be occurring in venues such as strip clubs, massage parlors, or other fictitious business fronts for prostitution. A major difference with sex trafficking of minors is that, unlike adults, force, coercion, or fraud does not need to be present for prosecution (6). As there are a number of different avenues for and types of human trafficking, recognition can be challenging.
Risk Factors
The profile of the human trafficking victim is not easy to define. Victims of human trafficking come from varied backgrounds that may or may not be what is expected or stereotypical. Victims may come from any race, socioeconomic status, color, religion, age, gender, sexual orientation or gender identity, and on. The main commonality is that there is a layer of deception whereby the human trafficker is targeting a vulnerability in the victim. As stated by the Department of Justice, trafficking victims are deceived with “... false promises of love, a good job, or a stable life and are lured into situations where they are made to work in deplorable conditions with little or no pay” (5). There are some trends noted that do make certain populations more at risk, but keep in mind that this does not encompass all potential victims and vigilance should be taken to avoid assumptions.
The risk factors for human trafficking are just as varied and dependent upon the type of trafficking and method by which the abuser is able to hold the victim indentured or captive. This figurative prison may be physically, emotionally, or monetarily induced. The Center for Disease Control and Prevention (CDC) lists the following characteristics and factors:
- Many victims are women and girls, though men and boys are also impacted.
- Victims include all races, ethnicities, sexual orientations, gender identifies, citizens, non-citizens, and income levels.
- Victims are trapped and controlled through assault, threat, false promises, perceived sense of protection, isolation, shaming, and debt.
Several higher risk populations have been identified through the data gathered from the Polaris Project. It was found that children who were or had been within the foster care system or runaway homeless youth were more likely to encounter sexual victimization. Other factors include substance abuse, recent relocation or migration, unstable housing situations, and underlying mental health disorders (7).
As a population that is often overlooked, shamed, or lacks resources, members of the lesbian, gay, bisexual, transgender, queer, or questions (LGBTQ) community are more vulnerable to being subject to human trafficking. Up to 40% of homeless youth are part of the LGBTQ community and may not seek assistance for fear of being shunned (8).
Illegal and sponsored immigration remains at a higher risk of trafficking and exploitation. The NHRTC reports a significant number of calls that reference foreign nationals (2). Individuals wishing to become American citizens are lured with the promise of freedom in exchange for large fees that are made impossible to be worked off. While there are laws in place to prevent, this type of servant bondage is forced upon the victims who are in a new country and often lack resources or are unable to seek assistance due to cultural, language, and accessibility barriers. Further, cases have been reported where the employer or trafficker withhold visas or identification barriers in order promote compliance and essentially are holding the victim hostage (9).

Self Quiz
Ask yourself...
- What percentage of homeless youth are a part of the LGBTQ+ community?
- What are some of the risk factors for human trafficking?
- Can boys and/or men be victims of human trafficking?
- What are the different methods that perpetrators use to control victims?
Recruitment Techniques
A major tactic of the perpetrators of these crimes is to prey on vulnerable individuals with a lack of resources. Thus, a primary ploy used is a layer of deception whereby the human trafficker is targeting the needs or wants of the victim.
Traffickers are often individuals that the victim has come to trust. This may be a girlfriend or boyfriend, spouse, or other family member. Victims are also commonly sold to outside parties.
In cases of sexual trafficking, typically young women and men are groomed and given preferential treatment, gifts, and drugs until they become reliant upon the “John”. In other cases, individuals are tempted with the promise of a better life, or in the case of immigration, the sponsorship for a visa (9).

Self Quiz
Ask yourself...
- What ploys do perpetrators use to deceive and lead their victims into sex trafficking?
- In Florida, human trafficking victims are commonly immigrants. What is a common promise that perpetrators make to these victims?
Florida Human Trafficking & Mandatory Reporting
Mandatory reporting of human trafficking by health care professionals is incorporated into the law in a growing number of locations in the United States. Health care professionals are already mandated reporters through previous existing laws that require reporting of child abuse, domestic violence, as well as knife and gunshot wounds (10).
The following states the criminal and civil liability of failing to follow the law as a mandatory reporter in some states:
In a civil action, the mandated reporter may be held liable for all damages that any person suffers due to the mandated reporters’ failure to file a report. In a criminal action, the mandated reporter may be found guilty of a misdemeanor punishable by imprisonment for up to 93 days and a fine of $500.
Reporting of suspected adult human trafficking is not as clear in regard to mandatory reporting. However, vulnerable adults suspected of being abused, exploited, or victimized fall under the same guidelines and are reported to CI in the same manner as above.

Self Quiz
Ask yourself...
- Who can be held liable if they fail to report any act of human trafficking?
- In Florida, human trafficking must be reported immediately by which healthcare workers?
Federal Laws
Today, there are 39 states that have committed to the crusade of establishing a statute banning human trafficking.
A specific U.S. Federal law addressing trafficking crimes was first enacted with the Trafficking Victims Protection Act of 2000. The bill has since been revised several times; however, the fundamental of it is to provide guidance and authorization for their “three-pronged approach that includes prevention, protection, and prosecution” and covers both sex and labor trafficking (11).
Preventing Sex Trafficking and Strengthening Families Act of 2014 and The Justice for Victims of Trafficking Act of 2015 are both aimed at providing victims increased protection for exploitation and increased resources specifically aimed at prevention and support for child and youth sex trafficking crimes (11).
The Customs and Facilitations and Trade Enforcement Reauthorization Act of 2009 is aimed towards prohibiting the importation of goods made by the benefit of human trafficking (11).
Recognizing Signs of Human Trafficking
According to the Department of Health and Human Services, close to 90% of human trafficking victims visit a health care facility at least once while in servitude and are not identified as such by health care providers (14). This is due to a lack of education, lack of consistent use of identification and screening tools, and time constraints within the current health care system. As a mandatory reporter and healthcare team member, it is imperative to use best practice in recognizing the signs and symptoms as well as the tools that are available.
Signs and Symptoms
Human trafficking victims may present to a healthcare setting with primary or underlying signs that may be related to physical or mental abuse. These signs and symptoms may be related to the reason that they are seeking treatment or may be identified by the healthcare provider during a thorough assessment. The following physical and psychological sequelae may be noted during an assessment as potential evidence of victimization (all derived from 9, 15):
Physical
- Unexplained or implausible injuries
- Bruising
- Wounds and Cuts
- Missing or broken teeth
- Closed head injuries
- Blunt force trauma
Neurological
- Headaches
- Migraines
- Memory loss or difficulty concentrating
- Vertigo
- Insomnia
- Brain trauma
Gastrointestinal
- Diarrhea
- Constipation
Dietary
- Malnutrition
- Anorexia
- Severe weight loss
Cardiovascular and Respiratory
- Tachyarrhythmias
- Hypertension
- Respiratory Distress
Reproductive System
- Sexually transmitted disease
- Vaginal and/or anal fissures
- Previous Abortions
Psychological
- Depression
- Suicidal Ideation
- Anxiety
- Self-harm including cutting or branding
- Drug and alcohol abuse
- PTSD symptoms
- Regression
- Anger
- Dissociative and depersonalization tendencies
Red Flags and Indicators
There are several characteristics that should be kept in mind as red flags during the interview and assessment that may indicate potential trafficking. These include, but are not limited to (all derived from 9, 15, 14):
- Tattoos that indicate ownership, a number, or tracking system or are out of character/obscene
- Inappropriate clothing for climate
- Workplace violence or abuse
- Unsanitary living conditions
- Multiple families or people sharing a living space that is too small
- Shares living space with employer
- Is not in control of financial assets
- Refusal to speak alone with health professionals
- Accompanied by individual that refuses to allow patient to speak for themselves or be alone
- Sex work under age 18
- Answers are scripted
- Answers are implausible or contraindicate
- Appears younger or older than stated age

Self Quiz
Ask yourself...
- What red flags really stand out to you?
- Have you seen any of these in your practice?
- What are some of the signs and symptoms that victims of human trafficking may present with?
- What are a few red flags or indicators that someone may be a victim of human trafficking?
Interview Tools and Techniques
Check with your facilities protocol for specific guidance on assessment and examination protocols for suspected abuse victims. There are also many scripted interviewing tools available online that assist with asking targeted questions. First and foremost, it is important to establish the patient’s safety and to gain trust.
Gaining trust can be difficult and conducting assessments and interviews should be completed in a non-threatening environment with an unbiased and non-judgmental tone. Creating a space that is quiet and will not be interrupted is important. This will ensure that the potential victim feels safe communicating and is not concerned that she or he will be overheard. Present your demeanor in a non-threatening manner, at eye level, and focus on being attentive with observant listening. Maintain respectful eye contact to convey interest and reflective listening. If taking notes during the interview is required, explain to the patient what will be documented and what it will be utilized for (15).
The National Human Trafficking Resource Center (NHTRC) offers a plethora of resources and scripted questions. The following are general questions on assessing if the individual is being forced into a situation and can be applied to any of the specific types of human trafficking (all from 15):
“Did someone control, supervise or monitor your work/your actions?”
“Was your communication ever restricted or monitored?”
“Were you able to access medical care?”
“Were you ever allowed to leave the place that you were living/working? Under what conditions?”
“Was your movement outside of your residence/workplace ever monitored or controlled?”
“What did you think would have happened if you left the situation?"
"Was there ever a time when you wanted to leave, but felt that you couldn’t?"
"What do you think would have happened if you left without telling anyone?”
“Did you feel that it was your only option to stay in the situation?”
“Did anyone ever force you to do something physically or sexually that you didn’t feel comfortable doing?”
“Were you ever physically abused (shoved, slapped, hit, kicked, scratched, punched, burned, etc.) by anyone?”
“Were you ever sexually abused (sexual assault/unwanted touching, rape, sexual exploitation, etc.) by anyone?”
“Did anyone ever introduce you to drugs or medications as a method of control?”
While screening tools provide a base for asking difficult questions, the NHTRC advises “Before screening, users should also be prepared to draw upon the expertise of local legal and medical staff and to refer identified trafficking victims to appropriate housing, health, and social services in their area . . . the tool is a complement to, not a substitute for, specialized training in human trafficking, good professional practice and victim-centered service” (15).
The NHTRC also provides a 24-hour national hotline that is able to guide health professionals through completing assessments and determining the next best steps to intervene or offer the victim assistance.

Self Quiz
Ask yourself...
- How would you approach and interview a patient victim of human trafficking?
- Are there any additional questions that you would ask them other than tools learned within this course?
Interventions and Collaboration
When presented with a suspected human trafficking victim, it is likely that the individual will not be alone. Maintaining safety and support for the patient may require separation from the suspected trafficker. While this may not be possible, an attempt should be made to bring the patient to a room or examination area unaccompanied.
Be conscious of any cultural preferences that may affect the patient. If there are language barriers preventing meaningful communication, enlist the assistance of a professional interpreter. This is especially vital in cases where the accompanying visitor or family is attempting to interpret for the patient and may be filtering the victim’s responses.
For patients that seek healthcare related to sexual abuse, a SANE assessment and rape kit should be obtained per facility protocol. With permission, patients should be tested for sexually transmitted infections including HIV, gonorrhea, UTIs, syphilis, and pubic lice, as well as a pregnancy test for females. Forced and coerced abortions are frequent among minor females in the sex industry (16).
Thorough documentation of the patient’s reported reason for visit, physical and neurological assessment including any trauma, bruising, wounds, affect, and pertinent statements should be noted in the patient’s electronic medical record.
Educate yourself on local resources and be able to provide assistance with finding access to healthcare, mental health, and rehabilitative resources that are available in the community. Victims may not want to take pamphlets with them that may be found, so providing locations or addresses of shelters or clinics with operating times may be a safer option.
Collaborate with the healthcare team, law enforcement, and social work for suspected child or vulnerable adult trafficking.
Mandatory reporting of suspected cases of child abuse or trafficking is not encumbered by HIPAA disclosure when reporting to authorities; however, when reporting suspected adult trafficking, disclosure and permission must be granted unless there is an imminent threat to the safety of the patient, or the patient has been identified as a vulnerable population. Thoroughly assess if the individual meets criteria as a vulnerable adult and proceed accordingly. If the adult does not meet criteria, permission must be gained to report.
If a competent adult does disclose that they are a trafficking victim, determine if the patient is in immediate, life-threatening danger. If so, follow facility protocol and encourage and support the patient in reporting to a law enforcement agency. If there is no immediate danger, supportive care and assistance should be provided. The patient should be informed of the options available for social services, reporting, and resources. The creation of a safety plan is highly recommended (13).
Prevention
Prevention of human trafficking requires public education, awareness, and knowing how to properly respond when faced with suspicions. The Blue Campaign is a strategy from the Department of Homeland Security to bring national awareness to the issue and provide specialized training to law enforcement and federal employees. Blue Campaign pamphlets and other materials are available at their website, www.dhs.gov/blue-campaign, for distribution.
The Center for Disease Control takes the stance that sex trafficking is preventable via community awareness and acknowledging exploitation when it does occur. They state “Strategies based on the best available evidence exist to prevent related forms of violence, and they may also reduce sex trafficking. States and communities can implement and evaluate efforts that:
- Encourage health behaviors in relationships
- Foster safe homes and neighborhoods
- Identify and address vulnerabilities during health care visits
- Reduce demand for commercial sex
- End business profits from trafficking-related transactions” (6).
One of the largest barriers to prevention in the healthcare system is the inability to recognize signs and symptoms. As cited above, a significant number of human trafficking victims have filtered in and out of healthcare systems without being recognized. This misses the opportunity to connect, provide resources, and offer further assistance. The NHTRC provides many resources for training within healthcare facilities and standardized forms and interviewing questions that may be tailored to individual situations and facility needs.
Patient Education
UNICEF provides excellent resources for human trafficking prevention. Below is an excerpt from UNICEF, with “key messages” for children, which can help prevent trafficking.
- Educate yourself on the issue, and learn the signs of a trafficked victim.
- Don’t accept friend requests from people you don’t know on social media. Traffickers commonly use sites like Twitter, Facebook, and Instagram to lure their victims.
- Be aware of how traffickers recruit people, and pay attention to your surroundings.
- Don’t reveal too much about yourself (i.e. your full name, address, school, or living situation) to people you don’t know, whether on your social media sites or in person, no matter how friendly the person may be.
- Never agree to meet someone you don’t know without first consulting a trusted adult (i.e. parent, teacher, guidance counselor).
- If you feel uncomfortable or are hesitant about a situation, confide in an adult who you can help you make the best choices.
- Making a decision to leave a situation or relationship where you feel unsafe or are being harmed or threatened can be hard and scary. If possible, talk to someone you trust, like a friend, family member, counselor, or youth worker.
- If you are in immediate danger or are being physically harmed, call 911 for help.
- If running away from home, try to find a safe place to go or call the runaway switchboard at 1-800-Runaway.
- If you suspect you or a friend are at risk trafficking, call the National Human Trafficking Hotline at 888-3737-888 or text “BeFree” (233733)
Resources - How to Help
Children and adults can be victims of human trafficking.
“If you see something, say something.”
- Contact the Florida Abuse Hotline 1-800-96-ABUSE (1-800-962-2873) to report known or suspected child abuse, neglect, or abandonment; and known or suspected abuse, neglect, or exploitation of a vulnerable adult.
- For help,contact the National Human Trafficking Hotline 1-888-373-7888.
- Text HELP to 233733 (BEFREE): To get help for victims and surviviors of human trafficking or to connect with local services.
- Visit the National Human Trafficking Hotline online at: https://humantraffickinghotline.org.

Self Quiz
Ask yourself...
- Who might you call within the community as a resource if you suspect a child or vulnerable adult is a victim of human trafficking?
- In Florida, human trafficking is an ongoing problem. What state and national hotlines can you call if you suspect that someone is in danger?
Course
Florida APRN Bundle
Course Highlights
- In this course on safely prescribing opioids, you’ll be able to describe factors when prescribing opioids, their indications, and their effects.
- You’ll also be able to explain new CDC guidelines for opioid prescribing.
- you’ll also be able to identify appropriate teaching elements for patients when prescribed opioids.
About
Pharmacology Hours Awarded: 29
Course By:
Jillian Hay-Roe, RNC-NIC, BSN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
For centuries, humans have been using, developing, and synthesizing opioid compounds for pain relief. Opioids are essential for treating patients who are experiencing severe and sometimes even moderate pain. Chronic pain can negatively affect our lives. In 2011, the cost of chronic pain ranged from $560 to $635 billion in direct medical expenses, lost productivity, and disability. An estimated one in five U.S. adults had chronic pain (11).

Introduction of opioid drug class, indications for use, most prescribed opioids, and their effects.
Opioids usually bind to mu-opioid receptor sites, where they have agonist effects, providing pain relief, sedation, and sometimes feelings of euphoria. Opiates refer only to natural opioids derived from the poppy plant. The term "opioids" includes all-natural, semi-synthetic, and synthetic opioids.
Opioids are classified into several categories based on their origin and chemical structure:
- Natural Opioids (Opiates): These come from the opium poppy plant. Examples include morphine and codeine.
- Semi-Synthetic Opioids: These are natural opioids that are chemically modified. Examples include drugs like oxycodone, hydrocodone, oxymorphone, and hydromorphone.
- Synthetic Opioids: These opioids are entirely synthesized in a laboratory and do not have a natural source. Examples include fentanyl, tramadol, and methadone (4).
Providers must always caution patients about the benefits and risks. The main advantage of opioid medication is that it will reduce pain and improve physical function. A provider may use a 3-item Pain, Enjoyment of Life, and General Activity (PEG) Assessment Scale:
- What number best describes your pain on average in the past week?
- What number best describes how, during the past week, pain has interfered with your enjoyment of life?
- What number best describes how, during the past week, pain has interfered with your general activity?
The desired goal is a 30% improvement overall with opioid treatment. (Centers for Disease and Control)
Providers must also go over potential side effects and warnings. Side effects include sedation, dizziness, confusion, nausea, vomiting, constipation, itching, pupillary constriction, and respiratory depression. Providers should discuss the importance of taking medication as prescribed. Taking opioids in larger than prescribed dosage, or in addition to alcohol, other illicit substances, or prescription drugs, can lead to severe respiratory depression and death. Individuals should not drive when taking opioids due to the sedating effects and decreased reaction times.
There are now thousands of different Food and Drug Administration (FDA) approved opioids available for providers to prescribe. They can be administered via other routes and come in various potencies. The strength of morphine is the "gold standard" used when comparing opioids. A morphine milligram equivalent (MME) is the degree of µ-receptor agonist activity. The following is a sample of some of the most prescribed opioids and their MME:
| Opioid | Conversion factor | Opioid | Conversion factor |
| Codeine | 0.15 | Morphine | 1.0 |
| Fentanyl transdermal (in mcg/hr) | 2.4 | Oxycodone | 1.5 |
| Hydrocodone | 1.0 | Oxymorphone | 3.0 |
| Hydromorphone | 5.0 | Tapentadol† | 0.4 |
| Methadone | 4.7 | Tramadol§ | 0.2 |
To utilize this information, multiply the dose for each opioid by the conversion factor to determine the quantity in MMEs. For example, tablets containing hydrocodone 5 mg and acetaminophen 325 mg taken four times a day would include a total of 20 mg of hydrocodone daily, equivalent to 20 MME (11).

Self Quiz
Ask yourself...
- How often do you prescribe opioids to your patients? If so, which ones and what dosages?
- If you do not prescribe opioids, do you treat patients taking them?
- Have you ever felt hesitant about prescribing opioids? What were the reasons?
- What topics do you routinely cover when you discuss opioid prescriptions with your patients?
- Do you know how to determine if a patient is engaging in opioid-seeking behaviors?
A history of opioids leading to the current epidemic
While the current opioid epidemic has caused devastating effects in recent years, destruction from opioids has been going on for centuries. In the early 1800s, physicians and scientists became aware of the addictive qualities of opium. This finding encouraged research to develop safer ways to deliver opioids for pain relief and cough suppression, which led to the development of morphine. By the mid-1800s, with commercial production and the invention of the hypodermic needle, morphine became easier to administer.
During the Civil War (1861 to 1865), injured soldiers were sometimes treated with morphine, and some developed lifelong addictions after the war. Without other options for pain relief, physicians kept giving patients morphine as treatment. Early indicators that morphine should be used cautiously were largely ignored. Between 1870 and 1880, the use of morphine tripled. Even with the problems associated with opioids, they continued to serve a vital part in the pain treatment of patients, and their use and development continued (6).
Opioid prescribing increased fourfold during 1999–2010. Along with the increase in opioid prescriptions during this time, how they were prescribed also changed; opioids were increasingly prescribed at higher dosages and for longer durations. The number of people who reported using OxyContin for non-medical purposes increased from 400,000 in 1999 to 1.9 million in 2002 and to 2.8 million in 2003. This was accompanied by an approximately fourfold increase in overdose deaths involving prescription opioids (8).
In 2020, approximately 1.4 million people were diagnosed with opioid use disorder (OUD), of those associated with opioid painkillers, as opposed to 438,000 who have heroin-related OUD (1, 4). Over 100,000 people died of a drug overdose, with 85% involved in an opioid (1, 4).
Widespread efforts were made to combat this growing issue. The prescribing rate peaked and leveled off from 2010-2012 and has been declining since 2012. In 2021, an estimated 2.5 million adults had been diagnosed with OUD. However, the amount of MME of opioids prescribed per person is still around three times higher than in 1999 (5).
Controlled Substances
On July 1, 1973, the Drug Enforcement Administration (DEA) was established in the United States. The Diversion Control Division oversees pharmaceuticals. Within this Division are five levels of controlled substances, which classify illicit and medicinal drugs (7).
Schedule I Controlled Substances
No medical use, lack of accepted safety for use under medical supervision, and high abuse potential.
Examples of Schedule I substances are heroin, lysergic acid diethylamide (LSD), and marijuana (cannabis).
Schedule II/IIN Controlled Substances (2/2N)
High potential for abuse, which can lead to severe dependence.
Examples include hydromorphone, methadone, meperidine, oxycodone, and fentanyl. Other narcotics in this class include morphine, opium, codeine, and hydrocodone.
Some examples of Schedule IIN stimulants include amphetamine, methamphetamine, and methylphenidate.
Other substances include amobarbital, glutethimide, and pentobarbital.
Schedule III/IIIN Controlled Substances (3/3N)
Less potential for abuse than substances in Schedules I or II, and abuse may lead to moderate or low physical dependence or high psychological dependence.
Include drugs containing not more than 90 milligrams of codeine per dosage unit like Acetaminophen with Codeine and buprenorphine.
Schedule IN non-narcotics includes benzphetamine, phendimetrazine, ketamine, and anabolic steroids such as Depo®-Testosterone.
Schedule IV Controlled Substances
Have a low potential for abuse relative to substances in Schedule III.
Examples include alprazolam, carisoprodol, clonazepam, clorazepate, diazepam, lorazepam, midazolam, temazepam, and triazolam, Tramadol.
Schedule V Controlled Substances
Low potential for abuse relative to Schedule IV and primarily consist of medications that have small quantities of narcotics.
Examples include cough preparations containing not more than 200 milligrams of codeine per 100 milliliters or per 100 grams and ezogabine (10).

Self Quiz
Ask yourself...
- How have your prescribing practices of opioids changed in response to the epidemic over time?
- What trends have you noticed in overall inpatient treatment plans regarding opioid prescribing trends (e.g., dose changes? or increase in opioid alternative therapies?)
- Do you think there is a stigma surrounding patients who are currently using opioids?
Explore behaviors that indicate opioid seeking, misuse, or addiction in patients.
Opioid use disorder (OUD) causes significant impairment or distress. Diagnosis is based on the following criteria: unsuccessful efforts to reduce or control use or use that leads to social problems and a failure to fulfill obligations at work, school, or home. The term Opioid Use Disorder is the preferred term; "opioid abuse or dependence" or "opioid addiction" have negative connotations and should be avoided. (3).
OUD occurs after a person has developed tolerance and dependence, resulting in a physical challenge to stop opioid use and increasing the risk of withdrawal. Tolerance happens over time when a person experiences a reduced response to medication, requiring a larger amount to experience the same effect. Opioid dependence occurs when the body adjusts to regular opioid use. Unpleasant physical symptoms of withdrawal occur when medication is stopped. Symptoms of withdrawal include anxiety, insomnia, abdominal pain, vomiting, diarrhea, etc. (5).
Patients who have OUD may or may not have practiced drug misuse. Drug misuse, the preferred term for "substance abuse," is the use of illegal drugs and the use of prescribed drugs other than as directed by a doctor, such as using more amounts, more often, or longer than recommended or using someone else's prescription (3).
Some indications that a patient may be starting to have unintended consequences with their opioid prescription may include the following symptoms: craving, wanting to take opioids in higher quantities or more frequently, difficulty controlling use, or work, social, or family issues. If providers suspect OUD, they should discuss their concerns with their patients nonjudgmentally and allow the patient to disclose related concerns or issues. Providers should assess the presence of OUD using the DSM-5 criteria.
Providers can use validated screening tools such as:
- Urine and oral fluid toxicology testing
- Drug Abuse Screening Test (DAST)
- Tobacco, Alcohol, and/or other Substance use Tools (TAPS)
- A three-question version of the Alcohol Use Disorders Identification Test (AUDIT-C)
The following patients are at higher risk for OUD or overdose:
- History of depression or other mental health conditions
- History of a substance use disorder
- History of overdose
- Taking 50 or greater MME/day or taking other central nervous system depressants with opioids


Self Quiz
Ask yourself…
- How often do you have patients exhibiting symptoms of OUD in your practice setting?
- What would your next steps be if you identify a patient with potential OUD (e.g., additional screening, referral, or treatment plans)?
- Have you noticed any trends in patients presenting with OUD? Such as socioeconomic status, occupation, gender, race, and medical diagnosis.
The 12 components of the CDC’s recent guidelines for opioid prescribing.
In 2022, the CDC updated the 2016 guidelines to help prescribers navigate prescribing opioids amid an epidemic. These guidelines are directed toward prescribing medications to adults to be taken in the outpatient setting, for example, primary care clinics, surgery centers, urgent cares, and dental offices. These do not apply to providers caring for individuals with sickle-cell disease, cancer, those receiving inpatient care, or end-of-life or palliative care. They are also intended to serve as a guideline, and each treatment plan should be specific to the unique patient and circumstances.
Some of the Goals of the guidelines are to:
- Improve communication between providers and patients about treatment options and discuss the benefits and risks before initiating opioid therapy.
- Improve the effectiveness and safety of treatment to improve quality of life.
- Reduce risks associated with opioid treatment, including opioid use disorder (OUD), overdose, and death.
Recommendation #1: Determining when it is appropriate to initiate opioids for pain.
An essential part of the prescribing process is determining the anticipated pain severity and duration based on the patient’s diagnosis. Pain severity can be classified into three categories when measured using the standard 1-10 numeric scale. Pain scores 1-4 are considered mild, 5-6 are moderate, and 7-10 severe. Opioids are typically used for moderate to severe pain.
The patient’s diagnosis will allow the provider to determine if pain initially falls into one of the following three categories of anticipated duration: acute, subacute, and chronic. Acute pain is expected to last for one month or less. Acute pain often is caused by injury, trauma, or medical treatments such as surgery. Unresolved acute pain may develop into subacute pain if not resolved in 1 month. If pain exceeds three months, it is classified as chronic. Pain persisting longer than three months is chronic. It can result from underlying medical conditions, injury, medical treatment, inflammation, or unknown cause.
The CDC guidelines state that non-pharmacologic and non-invasive methods are the preferred first-line method of analgesia, such as heat/cold therapy, physical therapy, massage, rest, or exercises, etc. Despite evidence supporting their use, these therapies are only sometimes covered by insurance, and access and cost can be barriers, particularly for uninsured persons who have limited resources, no reliable transportation, or live in rural areas where treatments are not available.
When this is insufficient, non-opioid medications, such as Gabapentin, acetaminophen, or nonsteroidal anti-inflammatory drugs (NSAID), should be considered next. Selective antidepressants and anticonvulsant medications may also be effective. Some examples of when these drugs may be appropriate include neuropathic pain, lower back pain, musculoskeletal injuries (including minor pain related to fractures, sprains, strains, tendonitis, and bursitis), dental pain, postoperative pain, and kidney stone pain.
Providers, however, must also consider the risks and benefits of long-term NSAID use because it may also negatively affect a patient’s gastrointestinal and cardiovascular system. Depending on the diagnosis, a patient may also require an invasive or surgical intervention to treat the underlying cause to alleviate pain.
If the patient has pain that does not sufficiently improve with these initial therapy regimens, at that point, opioids will be the next option to be considered.
It does not mean that patients should be required to sequentially “fail” nonpharmacologic and non-opioid pharmacologic therapy or use any specific treatment before proceeding to opioid therapy. Example: A patient for whom NSAIDs are contraindicated has recently sustained a rotator cuff injury and is experiencing moderate pain to the point at which it is disturbing their sleep, and it will be several weeks before they can have surgery.
Recommendation #2: Discuss with the patient realistic treatment goals for pain and overall function.
Ideally, goals include improving quality of life and function, including social, emotional, and physical dimensions. The provider should help guide these patients to realistic expectations based on their diagnosis. This may mean that the patient may anticipate reduced pain levels but not complete elimination of pain. The provider should discuss the expected or typical timeframe where they may need medications.
If medications are anticipated for acute or subacute pain, a discussion about the expected timeframe for pain should be highlighted in the debate. The patient may then better understand if their recovery is progressing. For chronic conditions, the conversation will focus on or may emphasize the overall risks of beginning long-term medication therapy. They may also advise patients, particularly those with irreversible impairment injuries, that they may experience reduced pain but will not regain function. A withdrawal plan will be discussed if opioid therapy is unsuccessful or the risk vs. benefit ratio is no longer balanced.
The second section of recommendations covers the selection of opioids and dosages.
Recommendation #3: Prescribe immediate-release (I.R.) opioids instead of extended-release and long-acting (ER/LA) opioids when starting opioid therapy.
Immediate-release opioids have faster-acting medication with a shorter duration of pain-relieving action. ER/LA opioids should only be used in patients who have received specific dosages of immediate-release opioids daily for at least one week. Providers should reserve ER/LA opioids for severe, continuous pain, for example, individuals with cancer. ER/LA opioids should not be for PRN use. The reason for this recommendation is to reduce the risk of overdose. A patient who does not feel adequate relief or relief fast enough from the ER/LA dose may be more inclined to take additional amounts sooner than recommended, leading to a potential overdose.
Recommendation #4: Prescribe the lowest effective dose.
Dosing strategies include prescribing low doses and increasing doses in small increments. Prescribe the lowest dose for opioid patients. Carefully consider risk vs. benefits when increasing amounts for individuals with subacute and chronic pain who have developed tolerance. Providers should continue to optimize non-opioid therapies while continuing opioid therapy. It may include recommendations for taking non-opioid medications in addition to opioids and non-pharmacologic methods.
Providers should use caution and increase the dosage by the smallest practical amount, especially before increasing the total opioid dosage to 50 or greater morphine milligram equivalent (MME) daily. Increases beyond 50 MME/day are less likely to provide additional pain relief benefits. The greater the dosage increases, the tendency for risk also increases. Some states require providers to implement clinical protocols at specific dosage levels.
Recommendation #5: Tapering opioids includes weighing the benefits and risks when changing the opioid dosage.
Providers should consider tapering to a reduced dosage or tapering and discontinuing therapy and discuss these approaches before initiating changes when:
- The patient requests dosage reduction or discontinuation,
- Pain improves and might indicate the resolution of an underlying cause,
- Therapy has not reduced pain or improved function,
- Treated with opioids for a long time (e.g., years), and the benefit-risk balance is not clear.
- Receiving higher opioid dosages without evidence of improvement.
- Side effects that diminish the quality of life or cause impairment.
- Opioid misuse
- The patient experiences an overdose or severe event.
- Receiving medications or having a condition that may increase the risk of an adverse event.
Opioid therapy should not be discontinued abruptly unless there is a threat of a severe event, and providers should not rapidly reduce opioid dosages from higher dosages.
Patient agreement and interest in tapering will be key components of successful tapers. Integrating behavioral and non-opioid treatment and interventions for comorbid mental health conditions before/during a taper can help manage pain, strengthen the therapeutic relationship between the provider and patient, and improve the likelihood of positive tapering outcomes. When dosages are reduced or discontinued, a taper slow enough to reduce symptoms and withdrawal should be used. Patients should receive education on possible withdrawal symptoms and when to contact the provider.
For those taking opioids for a shorter duration, a 10% decrease of the original dose per week or slower until close to 30% of the initial amount is reached, followed by a weekly reduction of roughly 10% of the remaining dose) is less likely to trigger withdrawal. Tapers of 10% per month or less are better tolerated than rapidly tapering off when patients have been taking opioids for a longer duration (e.g., for a year or longer). Significant opioid withdrawal symptoms can indicate the need to slow the taper rate further. Short-term medications might also help manage withdrawal symptoms. Providers should follow up frequently (at least monthly) with patients engaging in opioid tapering.
Close monitoring is required for patients who cannot taper and who continue on high doses or otherwise high-risk opioid regimens and should collaborate with patients to mitigate overdose risk. Some patients with unanticipated challenges to tapering may need to be evaluated for OUD.
The third section focuses on the duration of opioid therapy and routine patient follow-up.
Recommendation #6: Prescribing no greater quantity than needed for the expected duration of severe pain requiring opioids.
A few days or less is often enough when opioids are used for common causes of nonsurgical acute pain. Many states have passed legislation that limits initial opioid prescriptions for acute pain to less than seven days. Many insurers and pharmacies have enacted similar policies. Providers should avoid prescribing additional opioids to patients if pain continues longer than expected.
Providers should prescribe and advise opioid use only as needed rather than on a scheduled basis (e.g., one tablet every 4 hours). Limiting the duration of therapy can decrease the need to taper. However, tapering may need to be considered if patients take these medications around the clock for more than a few days.
Longer durations of therapy may be needed when the injury is expected to result in prolonged severe pain (e.g., greater than seven days for severe traumatic injuries). Patients should be evaluated at least every two weeks if they are receiving opioids for acute pain. Suppose opioids are continued for a month or longer. In that case, providers should address potentially reversible causes of chronic pain so that the length of therapy does not continue to extend.
Recommendation #7: Evaluate the benefits and harms of opioid therapy regularly.
The benefits and risks for Evaluating benefits and risks within 1-4 weeks of starting long-term opioid therapy for subacute and chronic pain should be evaluated within 1-4 weeks of initiating therapy and after dosage increases.
The evaluation should include patient perspectives on progress and challenges in moving toward treatment goals, including sustained improvement in pain and function. The Three-item Pain, Enjoyment of Life, and General Activity (PEG) assessment scale could be utilized to help determine patient progress.
Providers should also ask patients about common adverse effects, such as constipation and drowsiness, and assess for outcomes that might be early warning signs for more serious problems such as overdose or OUD.
Patient re-evaluation should occur after therapy begins (about two weeks) when ER/LA opioids are prescribed if the total daily opioid dosage is greater than or equal to 50 MME/day or if there is a concurrent benzodiazepine prescription. These individuals are at a higher risk for overdose. Follow-up for individuals starting or increasing the dosage of methadone is recommended every 2-3 days for the first week. Providers should reassess all patients receiving long-term opioid therapy at least every three months.
The last section of recommendations covers patients at risk for OUD and overdose.
Recommendation #8: Use strategies to mitigate risk by evaluating risk for opioid-related harms, discussing risk with patients, and incorporating risk reduction strategies into the treatment plan.
The patient’s habits (including alcohol and illicit drug use) and behavioral and mental health must be considered. Patients with a history of substance use disorders, depression, and/or mental health disorders have a higher risk of overdose and OUD. Even though the dangers of opioid therapy are higher with these patients, they may still require opioid treatment for pain management.
Psychological distress can interfere with the improvement of pain and/or function in patients experiencing chronic pain; using tools like the Generalized Anxiety Disorder (GAD)-7 and the Patient Health Questionnaire (PHQ-9 or PHQ-4) to assess for anxiety, post-traumatic stress disorder (PTSD), and depression might help providers improve overall pain treatment outcomes. They should also ensure that treatment for depression and other mental health conditions is effective, consulting with behavioral health specialists when needed.
Additionally, providers should:
- Educate on the risks of overdose when opioids are combined with other drugs or alcohol.
- Use caution when prescribing opioids for people with sleep-disordered breathing due to their increased risk for respiratory depression. The provider may ascertain if a patient is compliant with prescribed CPAP.
- Use caution and increased monitoring for patients with renal or hepatic insufficiency.
- Use caution and increased monitoring for patients aged 65 years or older.
- Offering naloxone when prescribing opioids, particularly to patients at increased risk for overdose.
If patients experience a nonfatal opioid overdose, providers should evaluate for OUD. Providers should reduce opioid dosage, discontinue opioids when indicated, continue monitoring, and support for patients prescribed or not prescribed opioids.
Recommendation #9: Reviewing prescription drug monitoring program (PDMP) data.
Providers should review PDMP data specifically for prescription opioids, benzodiazepines, and other controlled medications patients have received from additional prescribers to determine all the opioids the patient could potentially receive. Patients with multiple prescriptions and from various providers are at an increased risk for overdose or OUD. PDMP data should be reviewed before initial drugs for subacute or chronic pain and at least every three months during long-term opioid therapy.
Recommendation # 10: Considering the benefits and risks of [urine] toxicology testing.
Toxicology testing should be used to inform and improve patient care. Providers, practices, and health systems should minimize bias in testing and not test based on assumptions about different patients.
Recommendation # 11: Use caution when prescribing opioid pain medication and other medications concurrently.
Benzodiazepines and opioids can cause CNS depression and potentiate opioid-induced decreases in respiratory drive. Because other CNS depressants can potentiate respiratory depression associated with opioids, benefits vs. risks should be considered.
Recommendation # 12: Offering or arranging treatment for OUD if needed.
Includes referring a patient to a specific treatment center where behavior therapy and medications may be prescribed.

Self Quiz
Ask yourself...
- Do you plan to update your prescribing practices with these new guidelines?
- How often do you assess your patients who require subacute or chronic opioid treatment for their response to treatment?
- How often do you suggest tapering or adjusting opioid dosages?
- Do you routinely screen patients for OUD who are receiving chronic therapy?
- What do you tell patients who would significantly benefit from opioid therapy (e.g., post-operative patients) who are afraid to take them due to adverse side effects?
Prescription Drug Monitoring Programs (PDMP) and Electronic Prescribing.
Prescription Drug Monitoring Programs (PDMP) is a database that keeps track of controlled substance prescriptions. It helps to improve opioid prescribing, inform clinical practice, and protect at-risk patients. A pharmacist must enter controlled substances into the state PDMP when dispensing them. When the pharmacist enters this data, it may occur at various intervals, from one month, daily, or even "real-time." However, a PDMP is only helpful if providers check the system before prescribing (10).
Some states have implemented legislation that requires providers to check a state PDMP before prescribing certain controlled substances and in certain circumstances. Most current mandates require that all prescribers query PDMPs when prescribing any opioid. Some states require prescribers to query PDMPs every time a controlled substance is prescribed, while others require a query only for the initial prescription. Subsequent checks of PDMPs also vary from every time a drug is issued to specific intervals (e.g., every 90 days, twice a year, annually) should prescribing continue.
Some mandates have categorical requirements; e.g., a query must be made if the prescription is over a three-day or seven-day supply or if a certain prescribed level of MME is exceeded. Other states' mandates are based on subjective criteria, e.g., a prescriber's judgment of possible inappropriate use or the prescriber's discretion regarding whether to query the PDMP. Finally, some states mandate that only prescribers in opioid treatment programs, workers' compensation programs, or pain clinics must query PDMPs (10, 11).
In addition to PDMPs, there has been an increase in requirements for providers to utilize Electronic Prescribing for Controlled Substances (ECPS). Electronic prescribing programs for both providers and pharmacies must meet DEA requirements. The DEA's March 31, 2010, conditions were updated on July 27, 2023 (12).
On January 1, 2023, the Centers for Medicare and Medicaid Services (CMS) implemented additional requirements for controlled substances for recipients of Medicare Part D. There are over 51 million U.S. people enrolled in Medicare Part D (Center for Medicare Advocacy, 2023). In addition to state laws, these rules require that prescribers e-prescribe at least 70 percent of controlled substances for patients that have Medicare Part D. A waiver may be approved if the prescriber cannot conduct electronic prescribing due to circumstances beyond the provider's control (12).
Starting June 27, 2023, the 'Consolidated Appropriations Act of 2023' requires new or renewing Drug Enforcement Administration (DEA) registrants, to have at least one of the following:
- A total of eight hours of training from specific organizations on opioid or other substance use disorders
- Board certification in addiction medicine or addiction psychiatry from the American Board of Medical Specialties, American Board of Addiction Medicine, or the American Osteopathic Association
- Graduation within five years and status in good standing from medical, advanced practice nursing, or physician assistant school in the U.S. that included an opioid or other substance use disorder curriculum of at least eight hours (11, 12).
Providers must follow either state law or DEA/CMS regulations, whichever is more stringent. The following map indicates various rules in each state, which will continue to change when new legislation is enacted (11, 12).


Self Quiz
Ask yourself...
- What are the laws in your state about PDMP and E-Prescribing?
- What references can you refer to find out prescribing laws in your state?
- Is the use of PDMP a common practice in your workplace?
Important teaching points about opioid storage and disposal.
Safe Storage
Patients should understand that prescription opioids need to be stored securely (i.e., keeping them in a locked area). This is especially true if children, teens, and other visitors in the house may be aware of their presence. Teens and young adults are the biggest misusers of prescription pain medication. In 2018, over 695,000 youths ages 12–17 and 1.9 million young adults ages 18–25 reported misusing prescription pain medication in the past year. Young people may misuse prescription opioids for many reasons, including curiosity, peer pressure, and wanting to fit in. Another reason teens and young adults may decide to take prescription opioids is because they can be easier to get than other drugs. Studies show that 53% percent of people over 12 who obtained prescription pain medication for non-medical use received them from a friend or relative (13).
Safe Disposal
Patients should be advised on how to get rid of unused or expired medications. The best option is to immediately take them to a drug take-back site, location, or program. These sites or programs can be found online, or the pharmacist may have information. If it is not feasible for the patient to get rid of the drug using a take-back program, the patient should be advised to check if it is on the FDA flush list. If it is, the medication should be flushed down the toilet. Again, the list of drugs is available on the FDA website. If it is not on that list, it should be discarded in the trash at home.
Patients should follow these disposal instructions: Mix medicines (liquid or pills; do not crush tablets or capsules) with an unappealing substance such as dirt, cat litter, or used coffee grounds. Next, place the mixture in a container such as a sealed plastic bag; then throw away the container in your trash at home. Last, the patient should remove or permanently cover all personal information on the prescription label of empty medicine bottles or packaging, then trash or recycle the open container (14).

Self Quiz
Ask yourself...
- Do you often teach your patients about the safe storage and disposal of opioids? If not, what are some barriers to providing this education? How could you overcome these barriers?
- Your patient asks if they can give the leftover pills to their spouse, who has back pain; what would be an appropriate response?
- The patient replies that it is the same medication their spouse has been prescribed and does not understand why they cannot share it; what education will you provide?
OUD treatment, including medications.
Treatment for OUD is multi-faceted and typically includes both mental health components and FDA-approved OUD treatment medications. Mental health components may consist of counseling or a structured treatment program. Cognitive behavioral therapy (CBT) may also be beneficial. A potential barrier to OUD treatment, on the provider's and patient's behalf, is the perception that patients must engage in counseling to start or continue receiving OUD treatment medication. While the mental health components are essential, there may be barriers for patients to begin mental health treatment programs, which include expense, travel, and available openings within the programs. Medication therapy may be a helpful start for these patients (9).
FDA-approved medications indicated for the treatment of OUD include methadone, buprenorphine, and naltrexone. Suboxone is a combination drug composed of buprenorphine and naltrexone.
Medication has several advantages as part of the OUD treatment plan.
- Help the individual to remain safe and comfortable during detox.
- Reduce or eliminate cravings for opioids
- Minimize relapse since the individual is not experiencing uncomfortable withdrawal symptoms
- Allow the individual to focus on therapy without being distracted by withdrawal symptoms and cravings
- Increase safety in cases of overdose
Methadone
Methadone is a full agonist opioid and is a Schedule II controlled medication. Methadone can be prescribed purely for the treatment of pain, as well as for OUD. Methadone treatment for OUD can only be provided through a Substance Abuse and Mental Health Services (SAMHSA)-certified opioid treatment program. Patients taking methadone to treat OUD must receive the medication under the supervision of a clinician. After consistent compliance, patients may take methadone at home between program visits. The length of methadone treatment should be a minimum of 12 months. Methadone doses are often adjusted and readjusted. Methadone is slowly excreted, and there is overdose potential if not taken as prescribed (9).
Buprenorphine
Buprenorphine is a partial agonist opioid. Buprenorphine can be prescribed by any provider with a current, standard DEA registration as a Schedule III Controlled Substance. Like opioids, it produces effects such as euphoria or respiratory depression. With buprenorphine, however, these effects are weaker than those of full opioids such as heroin and methadone. It also has unique pharmacological properties that help lower the potential for misuse and diminish the effects of physical dependency opioids, such as withdrawal symptoms and cravings (9). Subutex was a brand-name version of buprenorphine, discontinued in 2011 after new formulations that were less likely to be misused were developed.
Naltrexone
Naltrexone is an opioid antagonist, not addictive, and does not cause withdrawal symptoms. It blocks the euphoric and sedative effects of opioids by binding and blocking opioid receptors and reduces and suppresses opioid cravings. There is no potential for misuse and diversion. Naltrexone can be prescribed in any setting and can be taken as a pill or once monthly extended-release intramuscular injection (9).
It was estimated 2021 that of the 2.5 million people with OUD, only 36% received any treatment, and only 22% received medications. A part of the July 27, 2023, Consolidated Appropriations Act amended the Controlled Substances Act to eliminate the requirement that providers obtain a specific waiver (a DATA waiver) to prescribe buprenorphine (including Suboxone) to treat opioid use disorder, known as the X-waiver. Additionally, there are no longer any caps on the number of patients a practitioner can treat. This, however, does not change the requirements for methadone treatment (15).


Self Quiz
Ask yourself...
- What are some problems that can occur if opioid medications are not managing pain adequately?
- What are some possible ways you can obtain a detailed, patient-centric health history?
- What are some possible ways APRNs can educate patients on pain and opioid medication options?
Case Study #1
Patient Name: John Henderson,
Gender: Male
Age: 60
Height: 6' 1"
Weight: 190 lbs.
He is employed as a grocery store manager. Reports not using tobacco; drinks alcohol occasionally and has no illicit drug use. He has hypertension and high cholesterol and takes Losartan 50mg daily and Atorvastatin 20 mg daily.
This patient presents to a primary care office with pain and stiffness in the shoulder joint, which has progressively worsened for six months following rotator cuff surgery. He states his pain is unchanged, and he has a limited range of motion. It has been interfering with his ability to do his job. He said he went to physical therapy for a few weeks after his surgery but admitted he did not often complete the home exercise program regimen. An MRI was obtained and showed he had adhesive capsulitis. What are treatment options to consider for "frozen shoulder"?
Given the patient's diagnosis, non-opioid therapy options include nonsteroidal anti-inflammatory drugs, intraarticular glucocorticoid injections, steroid injections into the shoulder joint, range of motion exercises, physical therapy, and consulting with an orthopedic specialist who may recommend a joint manipulation under anesthesia. Each of these should be considered before opioid therapy.
Nursing Considerations
Nurses remain the most trusted profession for a reason, and advanced practice registered nurses (APRNs) are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there are no specific guidelines for the nurse’s role in opioid education and management, here are some suggestions to provide quality care for patients currently taking opioid medications.
Obtain a Detailed Health History
Often times, pain and mental health can be dismissed and overlooked in health care settings. If a patient is complaining of symptoms that could be related to pain, inquire more about that complaint. Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities. A detailed pain assessment and history can provide context for opioid pain management and a patient's plan of care. When taking a health history, ask about any prior surgeries, major life stressors in the past year, or any prior opioid usage.
Review the Medication History
Often times, in busy clinical settings, reviewing health records can be overwhelming. Many people take pain medications, including opioids, for various reasons. Ask patients how they are feeling on the medication, if their symptoms are improving, if there are any changes to medication history, and if they use any other substances other than prescribed medications, such as alcohol, tobacco, or other drugs. Remember, prescription medications are not the only medications people take. Confirm medication route, dosage, frequency, and all the details to make sure you and the patient are on the same page and to avoid medication errors and complications. Medication history should be reviewed at every encounter.
Avoid Making Judgements
Society often stigmatizes open discussions of prescription medication and pain. Patients may avoid asking for pain medication for fear of being perceived as a "drug seeker." Other times, patients may have OUD and continuously ask for an increased number of opioid medications. Be willing to be honest with yourself about your comfort level discussing topics and providing education on opioid medications, drug interactions, and pain management. Be willing to address any questions/concerns the patients may have without making judgements.
Communicate the Plan of Care
Communicate the plan of care to other staff involved for continuity of care. For several patients, especially for patients with chronic pain or who use opioids long-term, care often involves a team of mental health professionals, physical therapists, nurses, specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care and to reduce the incidence of opioid medication errors.
Engage in Self Learning
Stay up to date on continuing education related to opioid medications, pain management, and prescribing regulations. Evidence-based information and scope of practice is always evolving and changing. You can then present your new learning and findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on pain management medications, non-pharmacological pain management options, and opioids by following updates from evidence-based organizations, such as the CDC or your local health department.
Perform Pain Assessments
As we know, it is not possible to look at someone with the naked eye and determine if they are in pain. Sometimes, it may be obvious when a patient is in pain (e.g., visible lacerations) and need pain management options, such as opioids. Other times, pain management is addressed as a result of taking a complete health history, listening to patient's concerns, completing a pain assessment, and offering testing to determine the cause of pain.
Assess for Opioid Use Disorder
While it is not possible to look at someone and determine if they have OUD, APRNs should pay attention to certain behaviors, for example, when a patient continually asks for more opioid medications or mentions that they are experiencing many symptoms common to those of OUD. OUD may be diagnosed as a result of completing a health history, listening to patient's concerns, and offering testing to determine the cause of pain. Remember, anyone can have OUD, and no two OUD patients appear the same.
Provide Patient Teaching
Patients should know that anyone has the possibility of experiencing side effects of opioid medications, just like with any medication. Patients should be aware that if they notice any changes in their breathing, changes in their heart rate, or feel like something is a concern, they should seek medical care. Because of social stigma associated with opioids and pain management, people may be hesitant to seek medical care because of fear, shame, and embarrassment. However, as more research and social movements discuss opioid use, there is more space and awareness for opioid education and opioid overdose prevention.
Nurses should also teach patients to advocate for their own health in order to avoid possible opioid complications and poor pain management.
Here are important tips for patient education in the inpatient or outpatient setting.
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors)
- Tell the health care provider of any existing lifestyle concerns, such as alcohol use, other drug use, sleeping habits, diet, menstrual cycle changes (need to identify lifestyle factors that can influence opioid use and pain management)
- Tell the health care provider of any prior experiences with opioid medication (if applicable) and any medication reactions or side effects (need to identify risk factors, address pain management appropriately, identify any allergies, and avoid possible opioid overdose symptoms)
- Tell the health care provider if you have any changes in your breathing, bodily functions, or heart rate (potential opioid overdose symptoms)
- Tell the nurse or health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your pain, overall health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality and public safety concerns)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries
- Tell the health care provider if you notice any changes while taking medications or other treatments to manage your pain (potential worsening or improving health situation)

Self Quiz
Ask yourself...
- What are some problems that can occur if opioid medications are not managing pain adequately?
- What are some possible ways you can obtain a detailed, patient-centric health history?
- What are some possible ways APRNs can educate patients on pain and opioid medication options?
Research
There is extensive publicly available literature on opioids medications. These can be found via the National Institutes of Health website and other evidence-based journals. As research is dependent upon the available of study participants, there are several ways people who take opioids can become part of research. If a patient is interested in participating in clinical trial research, APRNs can encourage them to seek more information on clinical trials from local universities and health care organizations.
Case Study #2
- Patient: Pilar
- Age: 40
- Height: 5' 1"
- Weight: 135 lbs.
Pilar presents to the urgent care clinic today complaining of a severe migraine, which started yesterday. Her history includes a hip injury following a car accident three years ago in which she developed chronic post-traumatic arthritis in the hip. After a total hip arthroplasty, she was diagnosed with heterotopic ossification (bone grows in tissue where it shouldn’t). For the past year, she has been taking 20 mg of oxycodone twice daily to manage chronic hip pain after unsuccessful non-opioid therapies. She has three children with no known pregnancy or postpartum complications. She previously worked part-time as an administrative assistant but has been off work since the car accident. She has post-traumatic stress disorder (PTSD) related to the accident. She has been prescribed Xanax 0.5mg up to three times daily for anxiety. She does not smoke, drink alcohol, or take illicit substances.
- What are some specific questions you'd want to ask about the hip arthritis?
- What are some health history questions you'd want to highlight?
- What lab work or testing would you suggest to perform?
For her migraine, Pilar stated she needed to take more of her oxycodone to deal with the pain and because she could not sleep last night. She is concerned because she is running out of pills. She said her primary care doctor's office was closed, so she came to the urgent care.
- What are some non-pharmacological interventions you can do for Pilar's pain?
- What are some questions you'd want to ask about her migraine?
- What are side effects of opioids would you discuss with her?
Here are some things to consider for Case Study #2.
- Discuss concerns with the patient. This includes taking the opioid more often than prescribed, potential problems with respiratory depression, and overdose.
- Recommend trying eletriptan or dihydroergotamine nasal spray first rather than additional opioids.
- Review the PDMP to see the prescription history for this patient. Attempt to contact the primary care provider to develop a plan of care.
- Consider conducting toxicology testing
- Consider offering naloxone
- Use the DSM-5 criteria to assess the presence (and severity) of OUD or arrange an assessment with a substance use disorder specialist. Offer treatment for OUD if it is confirmed.
Case Study #3
Sabrina is a 16-year-old Black high school student working as a waitress at a local restaurant. She arrives to the local pediatric emergency room after her shift with her mom because she thinks she is experiencing a sickle cell crisis. Sabrina reports that she has these crises every few months, and this is probably the third time she's been in this much pain. She reports being at this same ER last year for something similar. Her mother is completing paperwork and would like Sabrina to get some pain medication as well.
- What are some specific questions you'd want to ask about her health?
- What are some health history questions you'd want to highlight?
- What lab work or testing would you suggest to perform?
- What pain assessments would you perform on Sabrina?
Sabrina agrees to provide bloodwork, complete imaging, and be admitted. She said that no health care provider talked to her about how painful sickle cell crises can be, and she doesn't routinely take pain medication because she "doesn't want to be addicted." Sabrina and her mom heard about pain management options for these extremely painful episodes from social media and the internet and would like Sabrina to get her pain controlled. Sabrina said that she had some opioids last time she was in the ER, but she doesn't remember the name. Her mom doesn't remember the name either, but she remembers it was in an IV medication.
- How would you discuss Sabrina's pain management concerns?
- Given Sabrina's age, medical history, and prior history of opioid use, what medication options would be appropriate for a sickle cell crisis in an adolescent?
Sabrina has been in the pediatric ER for over a day receiving IV hydromorphone. She reports some relief, but Sabrina and her mom are concerned. Sabrina wants to live her life like a normal teenager without being in the hospital every few months for pain. Her mom asks if there is a way to have pain medication at home. Both Sabrina and her mom would like to know if there is anything that can be done to help with the pain outside of medications as well. Sabrina doesn't want to use pain medications daily but wants to have them at home just in case she can't get to the hospital.
- Knowing Sabrina's concerns, what are some possible non-pharmacological pain management options?
- Knowing Sabrina's health history, what would be some patient education talking points about at-home opioid medications and possible side effects?
- What are some possible consequences of leaving pain improperly managed?

Final Reflection Questions
- Are you familiar with any current research on opioid use?
- What are some reasons someone would want to enroll in clinical trials?
- How can nurses make a contribution to research?
- Do you plan to update your prescribing practices to reflect the new CDC guidelines?
Conclusion
Even providers who do not prescribe opioids should be familiar with the effects of opioids and OUD due to its high prevalence in the United States. Understanding the types of pain, how pain occurs, and how it impacts a person's quality of life is especially important. There is still an associated stigma among patients who use Opioids to treat chronic pain conditions. It is essential to recognize that there are times when opioid use is appropriate, as long as the provider practices the recommended guidelines and sound clinical judgment.
Tirzepatide for Type 2 Diabetes and Weight Management
Introduction
The emergence of the drug tirzepatide is becoming more popular and widespread and is being utilized among those with diabetes and also those who desire to lose weight. It is one of the newest diabetic drugs given by injection that also triggers dramatic weight loss in those who use the injections.
The U.S. Food and Drug Administration (FDA) approved tirzepatide in 2022 for individuals with diabetes, particularly Type 2 Diabetes. The FDA officials have not approved tirzepatide yet for weight loss, but they are currently tracking the medication and may have a recommendation for its approval by the end of this year. Clinical trials have shown that individuals with an elevated body mass index (BMI) and who did not have diabetes lost a considerable amount of weight when they received tirzepatide (1).
Advanced Practice Registered Nurses (APRNs) need to understand how to safely prescribe tirzepatide and the reasoning as to why it causes weight loss for specific individuals.
Drug Classification
Tirzepatide is part of a class of medications called glucose-dependent insulin tropic polypeptide (GIP) receptor and glucagon-like peptide-1 (GLP-1) receptor agonists. It comprises a 39 amino acid linear synthetic peptide conjugate to selective receptor agonists in preclinical and clinical trials.
Tirzepatide is used for treating Type II diabetes in adults as an adjunct to diet and exercise. It is also used for weight loss in some individuals and has gained increased attention as a new therapeutic agent for glycemic and weight control.
Social media has had a significant influence and increased the desire to use tirzepatide, and while individual results vary, the weight loss in adults ranged from 12 – 25 pounds.
Online pharmacies, diet clinics, and medical spas are implementing thousands of ads on social media to capitalize on a surge of interest in the drug.

Self-Quiz
Ask Yourself...
- Why has there seemed to be an increase in patients requesting this medication? What other medicines intended for type 2 diabetes are also being used for weight loss management?
- What are the ethical considerations regarding marketing this drug for weight loss when its primary use is for type 2 diabetes? Could this impact supply and costs?
Indications of Usage
The use of tirzepatide is being used for both Type II diabetes and weight control in certain patients. It has been a game changer for people living with Type II diabetes. The drug’s primary use is as an adjunct to diet and exercise to improve glycemic control in adults with diabetes.
The drug has also proven beneficial for weight loss in patients experiencing obesity, and those who are taking the highest dosage have shared a body weight reduction of 15.7% (2). Tirzepatide is an injectable prescription medication used together with diet and exercise, and it is not yet known if it can be used safely with patients who have had pancreatitis.
It is important to remember that it is not to be used for patients with Type I diabetes, but it is safe for Type II diabetic patients. Also, the safety of tirzepatide has yet to be discovered for children and those under 18; therefore, the medication should not be used for this age group.
In studies conducted with or without diabetic medicines, 75% – 90% of patients taking tirzepatide reached an overall A1C of less than 7% with an average starting A1C of 7.9 – 8.6% across the following dosages – 5mg, 10mg, and 15mg. The study results were measured at weeks 40 and 52 (3).

Self-Quiz
Ask Yourself...
- What dietary and activity recommendations can you provide to patients using tirzepatide for weight loss?
- Is this drug intended for those who want to lose 5-10 pounds?
Use of Tirzepatide with Diabetic Patients
Tirzepatide can be used for patients with Type II diabetes in combination with a diabetic-friendly diet and exercise. The drug works by lowering the patient’s overall blood sugar and also improves the A1C results of patients over some time. The injection has been approved by the FDA to treat Type II diabetes and is administered once weekly (4).
It is considered the first in a new class of medications – a dual glucose-dependent insulin tropic polypeptide (GIP) and glucagon-like-peptide-1 (GLP-1) receptor antagonist. The mechanism of how it works mimics two gut hormones (GIP and GLP-1). These hormones are essential in how patients digest food and regulate blood glucose after meals. The hormones also play a role in making individuals feel fuller and curb specific food cravings.
The provider can prescribe tirzepatide before attempting other diabetic medications if a patient has a BMI of 30 or greater or 27 or greater with weight-related conditions and if the drug is combined with a personalized weight loss plan that addresses physical activity, nutrition, and lifestyle changes.
However, due to the cost and some insurance companies not covering the injection unless the patient has both diabetes and obesity, the provider must carefully consider prescribing this medication.

Case Study
The patient states this ‘miracle drug’ is worth paying for out of pocket!
Jeff Capron, a 53-year-old Boonville, New York, web developer, started taking tirzepatide in December 2022. His friend had reported good results with the medication, so Jeff looked into the research studies behind it and then spoke with his primary physician.
The physician said, “Yeah, let’s give it a shot,” even though he did not have much experience with it. The physician did not have an opinion one way or the other than looking at the data set and seeing no reason why they could not try it.
Jeff’s hemoglobin A1C went from 10.1% to 6% in 3 months, which was very promising. “I never had that kind of experience with any medication for diabetes.” There is a range in how much A1C reduction people experience with tirzepatide, but many people taking it can get their A1C under 7% — an ideal goal for people with Type 2 diabetes.
Jeff experienced constipation and a little trouble sleeping early, but both issues disappeared quickly. He says, “I wake up in the morning, and my fasting blood sugars are normal.”
The medication took effect, he says, within 12 hours. He compared the feeling to having a gastric bypass.
“You cannot overeat food. As soon as you overeat, you almost feel ill.” While it generally takes a few months to notice effects like A1C reduction and significant weight loss, side effects such as lower appetite may be felt immediately.
Weight loss was not his primary goal, but he lost about 35 pounds on the medication in the first five months. He also lost his sweet tooth. “I can maybe count three sweet things I have eaten since December.”
Jeff found that his appetite slowly recovered days after taking tirzepatide. “You take the shot every Sunday, and by Saturday, you start to get a lot of appetite,” he says. “It does not seem to affect your weight. If I eat a little bit more on Saturday night, on Sunday, the scale will not move one way or the other.”
Jeff is allergic to hornets, so he already carries an auto-injector. He was not worried about using another drug delivered through a needle. “It’s just a push button,” he says. It also helped that his wife is a nurse. “So, I had her with me the first time to ensure I was doing it right. I didn’t even feel it.”
When Jeff was first prescribed tirzepatide, his insurance covered it. The company has since removed that benefit. He has filed an appeal but pays about $1,000 monthly out of pocket for his weekly injections. He plans to keep paying as long as necessary.
He considers the financial burden well worth it. “I have never had a medication that worked as well before for chronic conditions,” Jeff says. “I’ve been blown away by it. For me, it’s a miracle drug. It got rid of my diabetes” (4).

Self Quiz
Ask yourself…
- Can a provider willfully choose to prescribe tirzepatide before other diabetic medications are attempted?
- Would that impact his insurance coverage if Jeff did not meet the clinical criteria for using tirzepatide?
Use of Tirzepatide for Weight Loss Management
As mentioned, this medication is indicated for patients with a BMI of >30 or a BMI of >27 with qualifying comorbidities. Obesity can become a chronic lifetime disease, and for conditions such as these, the patient needs to implement therapy for the lifetime of the disease.
In a study conducted for tirzepatide, there was a dramatic increase in effectiveness compared to traditional nonsurgical interventions such as diet, exercise, and lifestyle changes. However, it has been noted that taking tirzepatide on an ongoing basis is recommended and necessary to maintain any weight loss achieved from the medication.
If a patient stops taking the drug, likely, it will no longer work (5).
Public health officials have expressed concerns about using the drug long-term. Still, data is currently lacking regarding long-term effectiveness, treatment duration, and maintaining weight reduction once the therapy is discontinued.
A recent trial consisted of 783 participants with a BMI greater than 30, and these participants agreed to take either a 10mg or 15mg dose of tirzepatide over 36 weeks. The injection is given once weekly, so this would equal a total of 36 injections.
By the end of 36 weeks, participants lost more than 21% of their body weight. After 36 weeks, participants continued on tirzepatide or received placebo treatment for the following year. The patients needed to be made aware of which treatment they were receiving.
Those still taking tirzepatide injections weekly after 88 weeks lost an additional 7% of their body weight, and those taking the placebo regained 15% at the end of 88 weeks (5).

Self Quiz
Ask yourself…
- What is the minimum BMI needed to qualify to receive this drug for weight loss management?
- Is this medication indicated for long-term use for patients with a high BMI?
Common Side Effects and Contraindications
Side Effects
Patients vary immensely with different experiences and side effects related to tirzepatide; however, the following are the most common side effects experienced by those taking the medication:
- Nausea
- Decreased appetite
- Vomiting
- Diarrhea
- Indigestion
- Constipation
- Stomach Pain
Tirzepatide usually does not cause fatigue, leaving one feeling weak, tired, and low energy. However, fatigue can be a common side effect of Type II diabetes.
It is important to note that most individuals who experience nausea, vomiting, and diarrhea episodes do so while the dosage increases, and typically, the symptoms decrease over time. G.I. effects were more prominent in those taking tirzepatide than those taking the placebo. The individuals not in the placebo group were more likely to stop treatment due to the unpleasant side effects (3).


Self Quiz
Ask yourself...
- Does tirzepatide cause fatigue in patients who use it?
Contraindications
Tirzepatide may cause thyroid tumors, including thyroid cancer, and it is essential to watch for possible symptoms, such as swelling or a lump in the neck, hoarseness, shortness of breath, or trouble swallowing.
Tirzepatide should also not be prescribed to any patient with Type 1 Diabetes.
One of the main ways that tirzepatide works is by stimulating the release of insulin from the pancreas, and due to this fact, there have not been many studies and clinical trials that include those with Type I diabetes.
However, this is not to say that prescribers have never ordered tirzepatide for those with Type I diabetes. Still, it is essential to note that if prescribed, it would be in addition to traditional insulin therapy.
- Personal or family history of a type of thyroid cancer known as medullary thyroid carcinoma (MTC).
- Any history of Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
- Patients who are allergic to the actual medication or any of its ingredients.
- Younger than 18 years of age


Self Quiz
Ask yourself...
- What is the reason that tripeptide is contraindicated in those with Type I diabetes?
- Why is there a risk with patients who have a thyroid disorder?
Safe Prescribing Practices, Guidelines, and Considerations for Providers
Safe Prescribing Practices
As with all prescribed medications, safe standards of care must be implemented and followed to ensure patient safety is maintained. The same applies to providers considering prescribing tirzepatide, and specific criteria must be met beforehand. The following information discusses guidelines involving exclusion and inclusion criteria for providers to prescribe tirzepatide (6) accurately.
Guidelines
Exclusion Criteria – If present, the following indicates that the patient should not receive tirzepatide:
- Diagnosis of Type I diabetes
- Personal or family history of medullary thyroid carcinoma or with Multiple Endocrine Neoplasia syndrome type 2
- Severe gastrointestinal dysmotility
- History of pancreatitis
- Pregnancy
- Proliferative Diabetic Retinopathy (PDR), severe Nonproliferative Diabetic Retinopathy (NDR), clinically significant myalgic encephalomyelitis (M.E.), or diabetic macular edema (DME) unless the risks/benefits have been discussed with the patient and are documented in the patient's health record along with monitoring plans and follow-up with an eye specialist who is informed at the time of initiation.
Inclusion Criteria – All of the following must be met for tirzepatide to be prescribed:
- Diagnosis of Type II diabetes
- A BMI of 25 or greater
- Inadequate glycemic control on at least 1mg of semaglutide injection plus two or more glucose-lowering drugs
- Change needed to achieve goal A1C is less than 1%.
- Goal A1C should be based on those recommended in the Diabetic Guidelines.
- Adherence to current diabetic medications as evidenced by a review of the prescription refill history during the six months.
Additional Inclusion Criteria – All of the following must be met for tirzepatide to be prescribed:
- Patients with atherosclerotic cardiovascular disease or chronic kidney disease
- Patients of childbearing potential who are using oral contraceptives
Inclusion Criteria for Weight Loss
- BMI of >30 or >27 with patient weight conditions.

Self Quiz
Ask yourself...
- Would a patient with a BMI of 23 with no comorbidities qualify to use tirzepatide to lose 5-10% of their body weight? Why not?
- What impact can tirzepatide have on a person with a healthy weight and BMI of <25?
Considerations for Providers
There are specific considerations that prescribers must be aware of when contemplating if a patient should receive the medication tirzepatide. The following is imperative and must be considered each time the medication is prescribed to a patient:
- Clinical Indications – indicated for treating adults with insufficiently controlled diabetes mellitus as an add-on therapy to diet and exercise; as monotherapy when metformin is considered inappropriate due to contraindications or intolerance; and other medicinal products for treating Type II diabetes.
- Monitoring of medication – routine monitoring of serum calcitonin or thyroid ultrasound is of uncertain value but is recommended for early detection of Medullary Thyroid Cancer (MTC).
- Cost – the average price for tirzepatide ranges from $1,071-$1,351 without any coupons or insurance. Savings Card – manufacturer provided; patients can pay as little as $25 monthly for up to 12 injections. Savings Card – manufacturer provided; patients can pay as little as $25 monthly for up to 12 injections.
- Benefits and Risks – One must evaluate the effectiveness of diabetes and the weight loss experienced. Some of the risks must be evaluated, such as increased cost of medication, unpleasant gastrointestinal side effects, poor insurance coverage, and drug shortages. The FDA has warned that the medicine can cause thyroid C-cell tumors in rats, and it is not sure whether tirzepatide causes similar tumors.
How long does it take for tirzepatide to begin working?
Tirzepatide will start to lower one's blood sugar levels immediately, but it can take 8 to 12 weeks to reach one's target A1C goal.
Compared to other diabetic treatments, studies have shown that it can take eight weeks to reach an A1C target of less than or equal to 7% and 12 weeks to get an A1C of less than or equal to 6.5%. Significant weight loss can occur as early as 28 weeks.
Safe Administration
It is essential to follow the correct steps for safe administration of tirzepatide as listed below:
- The recommended starting dosage is 2.5mg, injected subcutaneously once weekly. The 2.5mg dosage is for treatment initiation and not for glycemic control.
- After four weeks, increase the dosage to 5mg, injected subcutaneously once weekly.
- If additional glycemic control is needed, increase the dosage in 2.5mg increments after at least four weeks on the current dose.
- The maximum dosage is 15mg, injected subcutaneously once weekly.
- If a dose is missed, instruct patients to administer it as soon as possible, within four days (96 hours) after the missed dose. If more than four days have passed, skip the missed dose, and administer the next dose on the regularly scheduled day. In each case, patients can then resume their regular once-weekly dosing schedule.
- The day of weekly Administration can be changed, if necessary, as long as the time between the two doses is at least three days (72 hours).
- Before initiation, train patients and caregivers on proper injection techniques.
- Instruct patients using the single-dose vial to use a syringe appropriate for dose administration (e.g., a 1ml syringe capable of measuring a 0.5 mL dose).
- Administer the medication once weekly, any time of day.
- Inject the medication subcutaneously in the abdomen, thigh, or upper arm.
- Rotate injection sites with each dose.
- Inspect the medication visually before use. It should appear clear and colorless to slightly yellow. Do not use the medicine if particulate matter or discoloration is seen.
- When using the medication with insulin, administer it as separate injections and never mix. It is acceptable to inject tirzepatide and insulin in the same body region, but the injections should not be adjacent.
Does the tirzepatide injection hurt when administered?
Pain from the injection site has not been reported as a common side effect, but it may occur.
Due to the injection being given subcutaneously, slight pain or discomfort can occur.


Self Quiz
Ask yourself...
- The patient asks you," How long will this take to work?" How will you respond?
- The patient reports they have never used an injection before; what methods can you use to teach your patient how to administer this medication safely?
Alternatives to Tirzepatide for Weight Loss Management
In some instances, patients need to be aware of alternatives to tirzepatide in case they cannot take the actual injection for whatever reason. In cases such as these, there are alternative supplements that can be purchased over the counter, and they include the following (7):
- PhenQ – top OTC choice – comprehensive weight loss solution that targets specific body regions, facilitates prompt fat loss, and expedites the weight loss journey.
- PhenGold – the most potent OTC weight loss alternative – one of the top weight loss supplements that boost metabolism, making one less hungry, less tired, and an overall improved feeling.
- Capsiplex BURN – the best choice for men – helps to burn fat faster and keep blood sugar levels in check. It helps to keep one's muscles, curbs hunger, gives one more energy, and torches stubborn fats.
- Trimtone – the best choice for women – helps women to lose weight, eat less, increase metabolism, burn extra calories, and boost energy.
- Prime Shred – best fat burner for men – boosts metabolism, keeps muscles intact, increases energy, and helps maintain focus.
The advanced practicing nurse or prescriber needs to inform patients about alternative options such as these in an effort for individuals to understand that other choices are available and can be used. Many individuals need to be more knowledgeable about alternatives besides tirzepatide due to the extra hype from social media sources that promote advertisements related to tirzepatide only but do not mention the other options.
Why does social media influence and encourage patients to take tirzepatide?
Social media trends can be helpful but can also become harmful by setting unrealistic expectations and promoting a diet culture mentality. They can create an unhealthy obsession with "clean" eating, especially in the younger populations.
Due to this, many individuals take the medication despite any occurrence or history of Type II diabetes, and the drug can ultimately become misused.
It has been noted that there is an influx of patients requesting this medication for weight loss instead of the intended purpose, which is to help control Type II diabetes.
Tirzepatide represents one of the most recent non-medical treatments aimed at managing the symptoms of Type II diabetes. While it is not indicated for weight management, diabetic patients who receive it frequently report a significant reduction in body weight.
Empirical evidence suggests the efficacy of tirzepatide in weight management, and certain physicians currently endorse the Administration of the medication as a therapeutic and effective means to overcome obesity.
What are some severe side effects of tirzepatide that can impact patient safety?
The Administration of tirzepatide can benefit many individuals, but some severe side effects must be mentioned.
These include thyroid tumors, thyroid cancer, pancreatitis, hypoglycemia, serious allergic reactions, kidney issues, severe stomach problems, vision changes, and gallbladder issues. All these side effects must be taken seriously and reported, as they can lead to life-threatening

Self Quiz
Ask yourself...
- With what you have learned in this course, what education will you provide to patients requesting this medication for weight loss?
- Have you seen increased demand for this medication in your current practice?
- If you Google tirzepatide, your results will likely include links to telehealth services promoting this weight-loss medication. To determine eligibility, what special considerations need to be taken to assess a telehealth patient?
Conclusion
Medications like tirzepatide are game changers for those patients with type 2 diabetes that have failed other medications. Unfortunately, several companies seek to profit from its weight-loss benefits through aggressive marketing campaigns that limit the available supply and increase the costs for those who need it. As healthcare providers, we need to use sound clinical judgment and follow the exclusion/inclusion criteria and other guidelines before prescribing this medication, so we do not unintentionally cause harm while looking to appease our patients who request this.
Semaglutide and Type 2 Diabetes
Introduction
In 2017, the FDA approved the semaglutide injectable (Ozempic) for treating type 2 diabetes. The drug has experienced widespread acceptance due to its positive effects on weight loss and lowering of chronic health risks. The drug has risen in popularity over the past few years, as many well-known actors/actresses/songwriters, and more came forward, publicly sharing their weight loss journey.
This rise in popularity has also resulted in significant shortages of this medication, negatively impacting the lives of the diabetic community, local pharmacies, and healthcare providers. The goal of this continuing education course is to educate and empower the healthcare provider in all aspects of this drug regimen: clinical indications, patient education, cost options, and benefit/risk analysis.
Diabetes Overview
Diabetes is a chronic medical condition. Despite advances in diet, medications, and monitoring devices, diabetes diagnoses continue to grow at staggering rates. The Institute for Health Metrics and Evaluation (IHME) reports that over 529 million people worldwide are currently living with diabetes, and that number is expected to grow to 1.3 billion in only 30 years. While the risk factors for diabetes are vast in number (poor diet, inadequate activity, obesity, sedentary lifestyles, daily stressors, and more), the sad reality is that this chronic medical condition will most likely linger on for generations to come despite our efforts to contain this health epidemic (1).
According to the latest research on diabetes, there are over 37 million people in the United States alone with diabetes as of 2022. Statistically, approximately 28 million of them have a confirmed diagnosis, while another estimated 8 million are experiencing symptoms, without an official diagnosis. Diabetes currently ranks as the 7th leading cause of death in the United States (2).

Self Quiz
Ask yourself...
- As a healthcare provider, what has been your experience with treating chronic medical conditions?
- Why do you think there is a continued increase in diabetes, despite advances in medication and monitoring devices to treat this condition?
- Are you currently offering comprehensive care to your patients, including medication, diet, and activity counseling for their chronic health conditions?
Types of Diabetes
In basic terms, diabetes is an impairment in one’s ability to either adequately produce or utilize insulin, which results in elevated levels of circulating glucose. Chronically elevated glucose levels affect blood vessels at every level, causing chronic inflammation and raising the risk of heart disease, stroke, blindness, and atraumatic amputations.
There are three main types of diabetes:
Type 1 diabetes is thought to be an autoimmune disease. Approximately 5-10 percent of people with diabetes are diagnosed with type 1 diabetes. The diagnosis usually occurs in early childhood, and results in a lifetime use of insulin to regulate blood glucose levels.
Type 2 diabetes is thought to be related to dietary and lifestyle choices. It accounts for nearly 90-95 percent of diabetes diagnoses. Usually occurring later in life (adult-elderly population), it is believed to be related to factors such as diet, activity, weight gain, and related factors. Type 2 diabetes is usually controlled by diet and exercise, in addition to oral medications, although injectable insulin may be included in the treatment plan.
Gestational diabetes refers to elevated glucose levels occurring during pregnancy for patients who are not diabetic at the onset of pregnancy. This version of diabetes usually resolves itself post-partum, although a woman may develop type 2 diabetes later in life, unrelated to pregnancy.
Type 2 diabetes in children: no longer a “later in life diagnosis”
Children are now being diagnosed with type 2 diabetes at an alarming rate. Despite widespread education and an increased awareness of diabetes, our up-and-coming generation is unhealthier than ever. Many families lack access to healthy food for their families, due to both general socioeconomic challenges and an increased rate of food insecurity. (19)
The CDC recommends care providers have resources for diabetic patients and their families, such as food and nutrition programs, budget-friendly diabetes meal plans, how to save money on diabetes care, and coping strategies for diabetes. (19)


Self Quiz
Ask yourself...
- Are you able to articulate the different types of diabetes to patients?
- What resources can you offer to the families of children with type 2 diabetes?
Diabetes Signs and Symptoms, Diagnostic Testing
There are various ways to test for diabetes. The fasting blood sugar (FBS)/ fasting glucose level is a simple way to test for diabetes.
The normal fasting glucose level is below 100mg/dl. The fasting glucose result of 100-125mg/dl indicates prediabetes and results above 126mg/dl indicate diabetes.
The hemoglobin A1C blood test is another test used to confirm the diagnosis of diabetes. The patient does not need to be fasting for this test; thus, it is easier to order this test regardless of the time of day. This blood test reflects the average glucose level over the period of 2-3 months.
The normal A1C level is below 5.7%. Test results between 5.7%- 6.4% indicate prediabetes. Test results above 6.5% indicate diabetes.
A random glucose reading above 200mg/dl, done at any time of day, indicates diabetes.
The diagnosis of diabetes is by blood tests, and for improved accuracy, should be based on two separate readings, done (at least) a day apart. In the case of fasting and random blood tests, dietary intake (large amounts of carbohydrates in a single meal) may adversely affect test results. This is not the case when using A1C testing for a confirmation diagnosis, as the results are the average of a 2–3-month span.
Target blood levels for a person with diabetes (3).
Target blood glucose levels for people with diabetes are as follows:
- Fasting glucose 80-130mg/dl.
- Postprandial blood glucose level- less than 180mg/dl
- A1C level 7-8%.
These target ranges are general guidelines. Patient-specific ranges will be dependent on a variety of factors, including preexisting comorbidities, overall health status, age, and activity levels.

The hallmark signs/symptoms of diabetes
- Polyuria- increased urination
- Polydipsia- increased thirst
- Polyphagia-increased hunger/appetite
The truth is, as healthcare providers, you will have patients who have no hallmark signs and symptoms of diabetes; the diagnosis will be found during annual preventive examinations often unrelated to any chronic disease. For this reason, many insurance companies now cover numerous preventive screenings, including diabetes screenings, as part of their wellness and prevention initiatives. These tests are often approved based on a patient's age, or preexisting conditions, rather than outright signs and symptoms.

Self Quiz
Ask yourself...
- What are the typical glucose levels for non-diabetic versus diabetic patients?
- What are the hallmark symptoms you can identify when treating a potentially diabetic patient?
Lifestyle Interventions and the Diabetes Prevention Program
The initial diagnosis of diabetes can be managed in a variety of ways, depending on the severity of the illness at the time of diagnosis. Lifestyle interventions (behavior modification education) are of utmost importance in the care and management of people with diabetes. Research over the past few decades has consistently shown that such interventions have immense positive effects on the successful long-term management of diabetes.
The official Diabetes Prevention Program was created in 2010 (4) and confirmed the effects of lifestyle interventions in the management of diabetes: Lifestyle interventions decreased the incidence of type 2 diabetes by 58% compared with 31% in the metformin-treated group. Thus, these findings now serve as the blueprint, if you will, for all-inclusive, patient-specific disease management guidelines. These lifestyle interventions will be discussed in detail later in the program.
Additional Resources on Diabetes Prevention

Self Quiz
Ask yourself...
- How do lifestyle interventions compare to other kinds of treatment for patients with type 2 diabetes?
Semaglutide
Semaglutide is an injectable drug used in the treatment of type 2 diabetes. It was approved by the FDA in May of 2017.
It is a once-a-week injectable and belongs to the drug class known as glucagon-like peptide-1 receptor agonists (GLP-1RAs) (5). It has been referred to as a “miracle weight loss drug” among those who are living with obesity, despite frequent side effects, unusually high out-of-pocket costs, drug shortages, and weight regain when attempting to stop using the medication.
GLP-1 receptor agonist: Hormone Review
GLP-1 RAs are a class of medications used to treat Type 2 diabetes, and in some cases, obesity treatment. They are also known as GLP-1 receptor agonists, incretin mimetics, and GLP-1 analogs.
Ghrelin and Leptin (6)
Ghrelin and Leptin are two hormones that greatly influence appetite and the sensation of fullness. Often referred to as the “hunger hormone.” Ghrelin is responsible for many functions, including playing a key role in metabolism through glucose and insulin regulation.
Ghrelin, produced in your stomach, signals your brain when you are hungry, and results in increased food intake.
Leptin, conversely, is produced in your fat cells, and signals to the brain when you have eaten enough (by a decrease in appetite).
Glucagon-like peptide-1 receptors
Known as GLP1 receptors, Glucagon-like peptide-1 receptor proteins are located in the beta cells of the pancreas as well as in the neurons in the brain. GLP-1 receptors are involved in the regulation of blood glucose levels and affect the secretion of insulin. These cells encourage the release of insulin from the pancreas, increase the volume of beta cells, and reduce the release of glucagon. In doing so, they increase the feeling of fullness during and between meals, suppressing the appetite and slowing gastric emptying.

Self Quiz
Ask yourself...
- What are some problems patients might face if they choose to take semaglutide?
- How do Ghrelin and Leptin relate to a patient's appetite?
What is meant by receptor agonist and antagonist?
The term agonist refers to any substance that mimics the actions of a hormone in producing a specific response: a receptor antagonist blocks a response from occurring.
Opioids are examples of receptor agonists in that they produce responses such as analgesia.
Naloxone/Narcan is an example of a receptor antagonist, in that it binds to a receptor site and decreases/blocks a response from occurring.
Semaglutide mechanism of action (7)
GLP-1 agonists work in several ways to positively affect glucose levels. Their mechanism of action includes the following:
- Increasing (stimulating) insulin secretion by the pancreatic beta cells.
- Decreasing the production of glucagon, a hormone that raises blood glucose levels
- Decreasing (slowing) gastric emptying
- Decreasing appetite (and thereby reducing food intake) by creating a sensation of stomach fullness
Through these mechanisms of action, semaglutide results in a lowering of serum glucose/A1C levels, which lowers the risk of cardiovascular events. Studies have also shown that semaglutide resulted in weight loss (approximately 8-14 pounds on average {dose dependent results}.

Self Quiz
Ask yourself...
- What is the difference between an agonist and antagonist substance?
- How much weight do patients lose, on average, when taking semaglutide?
Side Effects of Semaglutide
Common side effects of semaglutide (8)
Common side effects may include any of the following:
- Nausea and vomiting
- Headache
- Diarrhea and stomach pain
- Upset stomach, indigestion, constipation, flatulence
These side effects usually subside within a few weeks, as the patient becomes acclimated to the medication.
Serious side effects of semaglutide
- Hypoglycemia- enhanced/worsened when used in combination with other diabetes medication. Symptoms may include drowsiness, confusion, weakness, irritability, and headache.
- Symptoms may include abdominal pain and distension, nausea and vomiting, fever, and back pain.
- Diabetic retinopathy. Symptoms may include blurred vision, vision loss, and diminished night vision.
- Kidney damage/injury/failure. Symptoms may include fatigue, nausea, diminished urine output, confusion, and edema of extremities.
- Gallbladder disease. Symptoms may include gallstones, abdominal pain, nausea and vomiting, and poor appetite.
Black Box Warning (9)
Semaglutide has a Black Box Warning for thyroid cancer. This is the most serious warning from the Food and Drug Administration (FDA) and is intended to alert consumers to the potential risks of a medication. This black box warning was issued when research found that the drug increased the risk of thyroid tumors in animals.
It is not known if semaglutide actually causes tumors in humans.
Contraindications
- Semaglutide is contraindicated in people with a personal or family history of MTC (medullary thyroid cancer) or in patients with multiple endocrine neoplasia syndrome type 2.
- Known hypersensitivity to semaglutide or any of the product components
Cautions
As noted under “serious side effects”, there have been reports of new illnesses or worsening of existing health conditions occurring “post-marketing”. Thus, healthcare providers are strongly encouraged to continue ongoing surveillance of any patients on semaglutide therapy. In addition, there is insufficient data available regarding the use of semaglutide by pregnant women. Women are therefore highly encouraged to stop any treatment with semaglutide for at least 2 months prior to a planned pregnancy.

Self Quiz
Ask yourself...
- Can you name the 4 common side effects of semaglutide?
- What is the most severe warning associated with semaglutide?
Dosing
Semaglutide is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM). It is looked upon favorably to reduce the risk of cardiovascular events in adults with T2DM and a preexisting history of cardiovascular disease. This drug is FDA-approved for use in people with diabetes, with a BMI of 27% or higher (a BMI of 25-29.9% is considered overweight).
Semaglutide (Ozempic) is available as an injectable prescription medication. Doses include 0.5mg, 1mg, or 2 mg, once weekly.
The injection should be administered subcutaneously to the abdomen, thigh, or upper arm. Injection sites should be rotated, and given as a single injection.
Start at 0.25 mg once weekly. After 4 weeks, increase the dose to 0.5 mg once weekly.
- If additional glycemic control is needed, increase the dose to 1 mg once weekly after at least 4 weeks on the 0.5 mg dose.
- If additional glycemic control is needed, increase the dose to 2 mg once weekly after at least 4 weeks on the 1 mg dose
Administer once weekly at any time of day, with or without meals. The maximum dose recommendation is 2mg/weekly once weekly.
Note: The initial 0.25-mg dose is intended for treatment initiation and is not effective for glycemic control
Missing Dose Guidelines
- If the missed dose is ≤5 days: Administer dose as soon as possible
- If missed dose >5 days: Skip the missed dose and administer the next dose on the regularly scheduled day; patients can then resume their regular once-weekly dosing schedule
Administration Day Guidelines (10).
The administration day each week can be changed, if necessary, as long as the time between 2 doses is at least 2 days (>48 hours)
Dose Availability (packaging)
- 2mg/1.5mL (1.34mg/mL); delivers doses of 0.25mg or 0.5mg per injection or four to eight doses per injection pen
- 4mg/3mL (1.34mg/mL); delivers 1mg per injection or 4 doses per injection pen
- 8mg/3mL (2.68 mg/mL); delivers 2mg per injection or 4 doses per injection pen
Treatment Goals- Effects on A1C and Weight (11)
A majority of adults who were placed on injectable semaglutide for diabetes management achieved a target A1C under 7% and were able to maintain it.
- Dose specific effects on A1C were as follows:
- 0.5mg dose injection yielded a 1.4% decrease
- 1.0mg dose injection yielded a 1.6% decrease
- 2.0 mg dose injection, in combination with diabetes pills, yielded a 2.1% decrease in A1C.
Adults taking semifluid injectables for diabetes management also noted weight loss.
- 8-pound weight loss reported with 0.5mg dose injection
- 10 pounds weight loss reported with 1.0mg dose injection
- Up to 14 pounds of weight loss reported with a 2.0mg dose injection


Self Quiz
Ask yourself...
- What should you tell a patient if they miss their injection by more than 5 days? What if it has been less than five days?
Prescribing insights: Long-Term therapy for a chronic condition?
Semaglutide is viewed favorably as a treatment option for Type 2 diabetes. It appears to lower A1C levels and body weight in the majority of patients, lowering their risk of future cardiovascular events.
The question of long-term medication use, for a chronic health condition, is being heavily discussed in the media. While a percentage of people can decrease or eliminate the need for chronic medications through significant lifestyle changes, there have been reports of weight gain in those who stopped taking this injectable medication.
Without intense lifestyle behavior modification education, there is a heightened risk of weight regain in the absence of such medications. Leaders in the treatment of obesity and related illnesses have commented that this drug is intended for long-term use.
Examples of this include the following:
“GLP-1 medications [like Ozempic] are designed to be taken long-term... They are chronic medications for the treatment of chronic conditions (both diabetes and obesity) (12)". - Christopher McGowan, M.D., a gastroenterologist specializing in obesity medicine and endobariatrics
“As with many chronic conditions, most people who use the drugs for diabetes or weight loss will need to keep taking them to keep benefiting from them. Depending on your individual situation, and without sustained lifestyle changes, it is likely you would need to be on these medications indefinitely to maintain weight loss (13)." - Dr. Cecilia Low Wang, a UCHealth expert in endocrinology, diabetes and metabolism.

Self Quiz
Ask yourself...
- Is semaglutide considered to be a long-term treatment for type 2 diabetes?
Cost Concerns
At this time, injectable semaglutide, FDA-approved for the treatment of Type 2 diabetes, has a self-pay price tag of $935.77 per month (4 injections). With FDA approval, many people with diabetes, insured under commercial plans, receive the drug for the cost of their copay. Those patients without coverage may use pharmacy discount cards that reduce the price, on average, to $814.55/month.
The following links are available to familiarize yourself with patient assistance programs related to semaglutide injectables.
Semaglutide Cost Savings Programs
The following links are provided to explore various semaglutide cost savings programs.

Self Quiz
Ask yourself...
- What resources can you offer patients who are struggling to pay for semaglutide?
Emerging Concerns: Semaglutide and gastroparesis
In August 2023, a first-of-its-kind lawsuit was filed in Louisiana, against the makers of semaglutide. The lawsuit states the makers of this injectable drug did not adequately warn patients about the risk of severe gastrointestinal issues/possible gastroparesis.
The plaintiff in this case had used both Ozempic and Mounjaro and experienced repeated episodes of severe gastrointestinal events, warranting trips to the emergency room and additional medications to alleviate her symptoms (14). While this lawsuit is in the developing stages, it bears mentioning in terms of concerns over long-term usage of the drug and possible complications.
While the drug labeling for semaglutide (Ozempic) does not specifically mention gastroparesis, the semaglutide/Mounjaro drug label does state that the drug has not been studied in patients with severe gastrointestinal disease and is therefore not recommended in these patients.
Up to 50% of people with diabetes have some degree of delayed gastric emptying, but most have no digestive symptoms or have only mild symptoms. For some people with diabetes, problems managing blood glucose levels may be a sign of delayed gastric emptying (15).
Healthcare providers should evaluate all patients with diabetes for possible symptoms of underlying gastroparesis, such as the feeling of fullness shortly after beginning a meal, or the inability to finish a regular meal. Other symptoms of gastroparesis may include abdominal pain, nausea, bloating, vomiting, and anorexia.
Diabetes and gastroparesis
Uncontrolled or poorly controlled diabetes can affect nerve endings systemwide. Diabetes is a very common cause of gastroparesis. Although the condition is rare it occurs more often in people with chronic conditions such as diabetes, autoimmune diseases, and nervous system disorders. Nerve endings are injured or damaged, cease to function properly, and result in delayed gastric emptying. The delay in gastric emptying can cause various symptoms, such as nausea, vomiting, bloating and distension, abdominal pain, and poor appetite.
In addition to underlying medical conditions, some medications may cause symptoms of gastroparesis (delays in gastric emptying and overall gastric motility. These medications include narcotics, antidepressants, and anticholinergics.
Left untreated, diabetic gastroparesis may lead to malnutrition, electrolyte imbalances, and poor glucose management and control.

Self Quiz
Ask yourself...
- Why should nurses prescribing semaglutide watch out for symptoms of gastroparesis?
- What do you think are some ethical issues with semaglutide use for weight loss?
Diabetes Lifestyle changes: Patient education (16)
- Weight Management
- Healthy Eating
- Physical Activity
- Smoking Cessation
- Stress Management
The importance of patient education regarding lifestyle changes is a priority. As with any chronic medication condition, the patient and their family/support system must be given every opportunity to educate and empower themselves on self-management of their disease process. Patients must be given the benefit of the doubt that they can indeed embrace their health and well-being and work with their healthcare provider in maximizing their health outcomes.
For diabetes mellitus, numerous lifestyle behaviors should be addressed and actively worked on, so that the patient receives the maximum health benefits. The following lifestyle behaviors are in no particular order; they all warrant discussion at every office visit.
Diet
A person with diabetes should be educated on the effects of food and nutrition on their glucose level. Referrals to a dietitian/nutritionist or Certified Diabetes Care Education Specialist (CDCES) should be considered a top priority. Well-balanced nutritional intake, appropriate carbohydrate awareness, calorie monitoring if weight loss is appropriate to your specific patient) and medication/food interactions are all essential aspects of dietary lifestyle education. Many commercial insurance plans, as well as hospital community outreach programs, offer diabetes self-management classes.

Activity (17)
The CDC recommends a target goal of 150 minutes weekly, Patients should be educated on the positive effects of daily activity on overall health and well-being, stress management, and metabolism. Patients should find activities they are genuinely interested in, involve family and friends, and slowly build greater endurance through increased intervals of longer duration.
Sleep hygiene (18)
Patients should be educated on the positive effects of a good night’s sleep. The aim should be approximately 7-8 hours of restful sleep. Electronics should be powered down and (optimally) removed from the bedroom. A dark, well-vented, cool room temperature is encouraged, and large meals and late-evening caffeine should be avoided.
Medication adherence/ literacy
Medication education is critical to the health and well-being of a patient. Routine education of the patient, and family members or support systems when available, should be supportive and patient-specific. Patients should be assessed on language barriers, literacy issues, and related comprehension concerns. Medication education should include effects, side effects, treatment goals, and sick day management. Emergency care issues should also be discussed. Any monitoring equipment (continuous glucose monitors, accuchecks, lancets) should be reviewed with patients and confirmed with return verbalization and demonstration.
As discussed in this course, patients with chronic diseases must learn self-management techniques to optimize their health and well-being. They must become confident in their understanding of their disease process and take ownership of their health. In doing so, they minimize the risk of long-term complications, improve their self-worth, and actively invest (both time and money) in their future.

Self Quiz
Ask yourself...
- How does sleep, diet, and activity level affect the treatment of type 2 diabetes?
Ozempic Case Study
- 52-year-old female
- Height 67 inches
- Weight 225 pounds
- B/P 138/84, Heart rate 76 NSR
- BMI 35.2%
- Nonsmoker, occasional social drinker
- Multiple attempts at dieting without success.
- Diagnosed T2DM approx. 6 months ago current A1C 7.5%; initial medication Metformin 500mg BID tablets; tolerated well. No GI upsets.
Today’s appointment is for evaluation and additional medication consideration (the patient requested this appointment)
The patient was diagnosed with T2DM approximately 6 months ago. Initial A1C 8.0%. Current A1C 7.7%
Despite an improved diet and adherence to the medication regimen, the patient voiced frustration at the lack of weight loss. Requesting additional medication. Has a neighbor friend who began injectable Ozempic and is having “really great results with it. I want to start on it as well”.
- What are your thoughts on prescribing semaglutide injectable for this patient?
- What objective health data points should be taken into consideration regarding prescribing semaglutide for this patient?
The patient has expressed frustration that despite taking her medications and adjusting her diet, she has not lost any weight in the past 6 months. She has “heard from her neighbor friend that the weight just melts off immediately” and she is ready to start this medication.
- What concerns do you know about this patient's understanding of weight loss as it relates to semaglutide?
- What prescribing information, specific to semaglutide and weight loss, could you share with your patient regarding realistic weight loss targets?
- In addition to teaching your patient proper injection technique for the use of semaglutide, what other lifestyle education behaviors should you discuss at this point?
- What information should you share with your patient regarding the long-term use of semaglutide and the potential risks of stopping this medication (as it relates to weight regain)?
Your patient decides to go ahead with the semaglutide regimen.
- What are some patient education guidelines regarding common side effects of this medication?
- How often is the dose increased? What is the maximum dose this patient can receive weekly?
Your patient wants to know how long she will be taking this medication.
- What talking points will you cover regarding the long-term use of this medication?
- How do you best prepare this patient for long-term success with this medication?
- What lifestyle behavior modification education would you discuss with your patient, to give her the best chance at successfully managing her diabetes?
Medication Assisted Treatment
Introduction
Medication Assisted Treatment (MAT) is a treatment modality for substance use disorders. It combines counseling and behavioral therapies for addiction with medications used carefully to reduce the physical symptoms of cravings and withdrawal and assist clients in the recovery process. With half of people 12 and older reporting use of an illicit substance at least once and 21 million Americans experiencing addiction, this is an important and relevant topic (4).
Historically, an intense stigma is attached to both addiction and some of the medications used to treat addiction. A thorough understanding of substance use disorders, available MAT therapies, and care of affecting clients are essential topics for nurses to be familiar with, particularly those working in psychiatry, pain management, or addiction medicine.
Overview of Addiction and Substance Abuse:
Drug and alcohol abuse and addiction are chronic, complicated issues involving persistent changes to the brain. There is a stigma or misunderstanding that people with substance abuse disorders can stop any time they want to or lack the willpower or moral fortitude to stop using. This is entirely untrue, and even people who are "recovering" and have not had any drugs or alcohol in years can easily relapse into addiction once those brain changes have occurred (5).
When a person uses drugs or alcohol, the brain's reward center is flooded with dopamine. This provides a "buzz" or pleasurable sensation that may create the desire to use more of the same substance. Over time, and with regular use of the substance, the brain becomes accustomed to the flooding of dopamine and reduces the reward response, a process known as tolerance.
It will now take the same person a more significant amount of the substance to achieve the same "buzz" or "high" they used to feel. This process can also dull the pleasure response to activities not involving substance use, such as food, socialization, or sexual activity. Over time, the chemical changes in the brain can progress to include decreased functioning of learning, decision-making, judgment, response to stress, memory, and behavior (5).
To understand substance abuse disorders, it is first essential to understand some basic definitions. These terms are sometimes used interchangeably, but they mean different things and represent different stages of disease.
Definitions
Substance Use: Substance use is any consumption of drugs or alcohol, regardless of frequency or amount. An occasional glass of wine or taking an edible at a party is an example of substance use. Substance use does not cause problems or dependency in many people (5).
Substance Abuse: Substance abuse is the continued use of drugs or alcohol, even when they do cause problems. Conflict or problems at home, school, work, or legal issues related to the use of drugs or alcohol are signs of abuse. For example, being sent home from school for smoking in the bathroom or failing a drug test at work (5).
Substance Dependence or Addiction: Dependence and addiction can be used interchangeably or is sometimes called substance use disorder. Addiction occurs when a person cannot stop drinking or using drugs despite creating problems in their life. People who are addicted may experience cravings until they use a specific substance, or they may experience uncomfortable physical symptoms, known as withdrawal if they do stop (5).
The American Psychiatric Association (APA) utilizes the following criteria to diagnose clients who suffer from addiction. The more criteria a client answers yes to, the greater their problem with substance use.
Six or more positive criteria are indicative of addiction.
- Using substance in more significant amounts or for more extended periods than intended
- Trying to stop using but being unable to
- Increased amounts of time getting, using, or recovering from use of the substance
- Experiencing cravings or urges to use.
- Continuing to use the substance despite problems with relationships or social situations.
- Missing work, social, or recreational obligations or activities because of substance use
- Participating in risky behavior because of substance use
- Continuing to use the substance despite psychological or physical health problems.
- Needing to use more substance over time to achieve the desired effect.
- Experiencing withdrawal symptoms when stopping the substance (1).


Self Quiz
Ask yourself...
- Do you know anyone who suffers from a substance use disorder?
- Think about your biases (thoughts, opinions, attitudes) about addiction. Does any of the information above conflict with those biases?
Substance Abuse Statistics
Many factors go into gathering data on substance abuse disorders, from underreporting, the nuance between use, abuse, and addiction, and the large variety of substances available, with the legality of some substances varying by state or age.
The statistics below from 2020 are not meant to be an exhaustive list of substance use disorders in this country but rather an overview of some of the more prevalent addiction-related issues.
- 50% of people 12 years and older have used an illicit substance at least once.
- 5% of Americans 12 years and older have used drugs within the last month.
- This is a 3.8% increase from the previous year.
- About 50% of Americans 12 and over drink alcohol
- 4% of those people have an alcohol use disorder.
- About 20% of Americans use tobacco products or vape
- 18% of Americans over 18 used marijuana in the last 12 months
- 30% of those have some level of misuse or addiction.
- Marijuana is commonly involved in polysubstance use, paired with alcohol or other drugs.
- 7% of Americans over 12 misused opioids in the last 12 months
- 96% of those used prescription pain relievers
- Opioid prescriptions peaked in 2012, with 81.3 prescriptions per 100 people.
- The rate has declined recently due to increased attention to this crisis.
- In 2018, the rate was down to 51 prescriptions for every 100 people
- Fentanyl is now rising as a new and deadly concern.
- 5 million prescriptions were written for fentanyl in 2015.
- Fentanyl is involved in 53% of overdose deaths.
- 7% of all Americans misuse a prescription drug.
- 1% of those misuse stimulants
- 2% of those misuse sedatives
- 5% misuse painkillers
- Over 70,000 drug overdose deaths occur annually in the United States (4)
Risk Factors
A combination of factors is involved in the risk of addiction, and no one factor can determine if someone will develop addiction or after how many uses this will occur.
The addiction process does occur more easily or progresses more rapidly for people with certain risk factors, including:
Genetics
There is a strong genetic correlation with addiction, indicating that biology plays a significant role in the disorder. Family history of addiction, gender, ethnicity, and comorbid mental health conditions can all influence the risk of addiction. (5)
- Children of addicts are eight times more likely to develop an addiction at some point.
- In 2020, among those using illicit or misusing prescription drugs, 22% were male and 17% female.
- Only 20% of users in drug treatment programs are women.
- 9% of people with substance abuse disorders also have at least one mental health disorder (4)
Environment/Non-Genetic Demographics
The attitudes about drugs and alcohol from those in a person's network and life experiences play a role in the risk of addiction. Substance use among friends, family, or coworkers increases the risk that a person will also use substances. Exposure to substance use from a young age relaxed parental attitudes about substance use, and peer pressure from friends can increase the risk. Certain stressful life circumstances such as veteran status, history of sexual or physical assault, or being part of the LGBTQ community can also increase risk. (5)
- 20% of people in urban areas used illegal drugs in 2020 compared to 5% in rural locations.
- 51% of Americans with an illegal pain relief medication obtained it from a friend or relative.
- 7% of LGBTQ Americans abuse illicit drugs.
- 2% of LGBTQ Americans abuse alcohol.
- 7% of Veterans abuse illicit drugs.
- 80% of Veterans abuse alcohol (4)
Developmental Stage
Substance use at any age can lead to addiction, but children and teens are at particular risk due to their underdeveloped brains. The parts of the brain responsible for decision-making, risk assessment, and self-control do not fully develop until the early 20's, putting teenagers at increased risk of dangerous behaviors. In addition, the effects of drugs and alcohol on the developing brain may mean that those parts of the brain never fully develop at all for teens with substance abuse disorders. (5)
- 70% of users who try an illegal substance before age 13 will develop a substance use disorder within the next seven years.
- This is for only 27% of people who first try an illegal substance after age 17.
- 47% of youths report trying an illegal substance by the time they graduate high school (4)

Self Quiz
Ask yourself...
- Why do you think medication alone is not an adequate treatment for substance abuse disorders?
- Is MAT something you have heard of before? Why do you think it is relatively uncommon despite being around for decades?
Overview of Medication Assisted Treatment (MAT)
Treatment of substance abuse disorders is a complex and often tumultuous process. The nature of the brain changes that occur during addiction means that a person is never entirely "cured" but will always be considered "recovering" as the risk for relapse is always present. Effective treatment must be multifaceted and often involves removing triggers (such as people, places, and stressors) that may prompt a person to use again behavioral therapy, and medications to curb withdrawal symptoms and reduce cravings.
Medication Assisted Treatment (MAT) is a treatment that involves FDA-approved medications, in combination with behavioral therapy, in the recovery process for substance abuse disorders. Several medications are available for MAT, and evidence continues to emerge that the treatment is highly effective if used correctly.
However, it is a vastly underused and understudied treatment modality. MAT has been available in some form for over 50 years but is just starting to gain traction among the medical community (and policymakers) in recent years, with the federal government calling for more research and increased accessibility for the treatment (8).
The height of the opioid crisis in the last several years has highlighted the magnitude of drug addiction and deaths in the United States, bringing renewed attention to MAT as a treatment option. So, how does MAT work? Prescription medication is given to both stimulate the receptors seeking the abused substance and block the drug's euphoric effects.
Over time, this normalizes brain chemistry and helps the person break the habit of using without the discomfort of cravings and withdrawal symptoms. Gradually, the prescription medication dosage is reduced, all the while in conjunction with behavioral therapy and lifestyle changes, and eventually, the client should be able to stop the medication altogether, often within 1-3 months (8).
MAT does require close supervision by a trained medical professional and an appropriate facility for treatment. It can be done on an inpatient, partial inpatient, or outpatient basis. There may be side effects to the medication, and there is a risk of misusing or developing addiction to the new drug, though the successful outcomes often outweigh this risk. Clients must also participate in behavioral therapy for a comprehensive and effective treatment plan. As with any treatment regimen, careful consideration of the client's history and circumstances is essential (8).


Self Quiz
Ask yourself...
- Why do you think medication alone is not an adequate treatment for substance abuse disorders?
- Is Medication Assisted Treatment (MAT) something you have heard of before? Why do you think it is relatively uncommon despite being around for decades?
Pharmacokinetics
Currently, there are three medications with FDA approval for MAT: buprenorphine, methadone, and naltrexone. Each will be discussed in depth below.
Buprenorphine
Mechanism of Action and Metabolism
Buprenorphine is an opioid partial agonist, acting on the same receptors as other opioids but with weaker effects. It can be used for the treatment of misuse of opioids, including:
- Heroin
- Fentanyl
- Oxycodone
- Hydrocodone
- Morphine
- Methadone (3)
Opiate receptors are G-protein coupled receptors (GPCRs) with four major types: Mu, Delta, Kappa, and opioid receptor like-1 (ORL1). Stimulation of these receptors results in varying levels of the following effects:
- Euphoria
- Relaxation
- Pain relief
- Sleepiness
- Sweating
- Constipation
- Impaired concentration
- Reduced sex drive (3)
Buprenorphine has a high affinity to the Mu-opioid receptor and is a partial agonist at this site, causing reduced opioid effects with a plateau or ceiling at higher doses. This limits dangerous effects and makes overdose unlikely. It also has slow dissociation from the site, allowing milder and more easily tolerated withdrawal effects compared to full agonists like morphine and fentanyl. Buprenorphine is also a weak kappa receptor antagonist and delta receptor agonist, reducing the craving sensation and improving tolerance to stress (3).
Buprenorphine has poor bioavailability when given orally due to the first-pass effect, where most of the drug is broken down in the liver and intestines. Because of this, sublingual or buccal are the preferred routes of administration and the most common forms in which the drug is manufactured. Transdermal patches and IV and IM forms exist, though not for use in MAT (3).
CYP34A enzymes break down buprenorphine, so other drugs, such as ketoconazole, may inhibit metabolism and increase available levels of buprenorphine. CYP34A inducers such as carbamazepine, topiramate, phenytoin, and barbiturates may speed metabolism and lower available levels. Once broken down, the med takes the form of norbuprenorphine and is excreted in the feces (3).
Available Forms
Buprenorphine is available by itself and with naloxone (in a 4 to 1 ratio). However, in oral form, naloxone is not readily absorbed, and buprenorphine is the only genuinely active ingredient. This combination is beneficial should clients try to inject their buprenorphine to get high; naloxone is a fast-acting opioid antagonist that is active when used intravenously and would block the opioid effect of buprenorphine, rendering it useless for recreational use and ensuring it has no street value.
The currently available preparations of buprenorphine for MAT include:
- Generic Buprenorphine/naloxone sublingual tablets
- Subutex - Buprenorphine sublingual tablets
- Suboxone - Buprenorphine/naloxone sublingual films
- Zubsolv - Buprenorphine/naloxone sublingual tablets
- Bunavail - Buprenorphine/naloxone buccal film (3)
Sublingual products dissolve within 2-10 minutes. Bloodstream absorption begins quickly, bypassing the first pass effect. Buprenorphine has a slow onset of action, peaking about 3-4 hours later. Metabolism is also slow, with the half-life lasting anywhere from 25 to 70 hours (an average of about 38 hours). This long half-life means the drug can be spaced out to every other day administration once weaning begins (3).
Dosing and Monitoring
Clients prescribed buprenorphine must stop using opioids for at least 12 to 24 hours before the first dose; this varies depending on which opioid they are stopping. For short-acting opioids like heroin and oxycodone, buprenorphine may be started 6-12 hours after the last dose. With longer-acting opioids such as morphine or extended-release preparations of oxycodone, buprenorphine should be delayed for about 24 hours. For the longest action opioids, fentanyl patch, 48 -72 hours must be between the last dose and buprenorphine initiation (3).
This initiation schedule means clients will be in the early stages of discomfort and withdrawal. Administration of buprenorphine when clients still have opioids in their bloodstream will lead to competition for receptor sites, rapidly replacing the opioid with buprenorphine and causing acute and more severe withdrawal symptoms.
Depending on the severity of a client's addiction, they may complete the first step of abstaining and withdrawal in an inpatient setting. Once the initial withdrawal symptoms have passed and the initial dose of buprenorphine has been given, the client may be discharged home to continue buprenorphine initiation on an outpatient basis (3).
Initial doses are typically 2-4mg, with up to 4mg given to clients used to higher potency or larger doses of opioids. The dose is gradually increased to meet the client's individual needs, with a maximum dosage of 24mg per day. The average client requires 8-12 mg per day and can reach this dose within the first 2-4 days. It is recommended that doses be supervised by a pharmacist at the dispensing pharmacy for the first two months of treatment to ensure compliance and clients are less likely to relapse (3).
The length of treatment with buprenorphine depends on each client's case and, for some, may be indefinite. Clients who do wish to wean off buprenorphine can begin the process once they are stable and experiencing few or no cravings, and a minimum of 8 weeks from treatment initiation. Doses are moved to alternating days and eventually discontinued altogether (3).
Side Effects and Contraindications:
As with any medication, there are potential side effects, including:
Common Side Effects
- Nausea
- Vomiting
- Drowsiness
- Dizziness
- Headache
- Memory loss
- Sweating
- Dry mouth
- Miosis
- Postural hypotension
- Sexual dysfunction
- Urinary retention
Serious side effects
- CNS depression
- QT prolongation
- Reduced seizure threshold
- Potential for abuse or overdose (3)
Buprenorphine is contraindicated for clients with a past hypersensitive reaction to it. It should be used cautiously for clients with respiratory suppression, older adults, or for those with liver pathologies. Regular monitoring of liver enzymes via lab work is essential (3).
It is a Category C medication for pregnancy, and the risks versus benefits should be carefully weighed. Buprenorphine does cross the placenta and increases the risk of withdrawal symptoms and neonatal abstinence syndrome (NAS) after delivery. However, for pregnant clients with the highest risk of relapse and abuse of opioids, evidence does support that continuation of buprenorphine during pregnancy may improve maternal and fetal outcomes (3).
Buprenorphine may be abused by crushing tablets, snorting the powder, or dissolving it into an injectable solution. Safety measures against this include supervised administration by a pharmacist and the addition of naloxone, which blocks the buprenorphine effects. While the effect ceiling of buprenorphine makes overdose difficult, combining the drug with benzodiazepines, alcohol, or other drugs can compound the CNS depressant effects and increase the risk of overdose (3).
Clinicians need to have a comprehensive health history of clients before initiating buprenorphine so that all risks and potential interactions can be addressed appropriately.
Role of the Pharmacist
Pharmacists play a significant role in the success of MAT involving buprenorphine. Outpatient doses are monitored by the dispensing pharmacist daily, with at-home quantities being allowed on a limited basis (such as weekends or travel) and only for the most motivated and compliant clients. Vital signs are collected before each dosage, with careful monitoring for hypotension or bradypnea. The dose may be skipped for clients who experience excessive side effects, and the client can return the next day for their dose.
Clients presenting with signs of overdose (usually to the ED) may receive naloxone, which will reverse overdose symptoms within 1 hour. Overdose symptoms include dizziness, pinpoint pupils, hypotension, bradypnea, hallucinations, seizure, or unconscious state.
If a client misses a dose, does not show up for it, or is experiencing significant side effects from buprenorphine, the prescribing clinician should be notified so that the treatment plan can be revisited and revised if needed (3).
Considerations for the Prescriber
When considering which medication to prescribe for MAT, prescribers should understand that buprenorphine offers advantages over methadone.
- Lower risk of abuse
- Safer, including at higher doses.
- Therapeutic dose achieved quickly.
- Easier to taper.
- Can be obtained from any provider rather than a methadone clinic.
- Less stigma
The cost of a 30-day supply is around $300. Buprenorphine/naloxone combinations are a little more expensive at $400/month. While prior authorization is usually required, most commercial insurance and state Medicaid programs will cover the medication.
Buprenorphine is a Schedule III Controlled Substance; however, recent federal regulations have been aimed at approving access to MAT, and any provider with an active DEA license may prescribe buprenorphine as allowed by state regulations. Specialized clinics are not required (as they are with methadone), and it is dispensed at regular pharmacies.
Prescribers are encouraged to participate in additional training about MAT with buprenorphine, but it is not required. Detailed documentation must be completed, including the reason for prescribing, start and end dates of treatment, the pharmacy used, the credentials of who will supervise administration, and frequency of follow-up and compliance monitoring. The sublingual and buccal routes are the only forms of medication used for MAT; patches, IM, and IV preparations are not routinely used for MAT.
The success of buprenorphine treatment depends on the client's education. Addiction potential, risk of combination with other CNS depressants, and side effects vs. signs of overdose should all be discussed with clients and their support system (3).

Self Quiz
Ask yourself...
- Given the nature of substance abuse disorders, why do you think including an opioid antagonist like naloxone in preparations of buprenorphine is necessary for safety and compliance?
- What challenges do you see with a medication needing to be administered daily with pharmacist supervision?
- What are the risks of buprenorphine being given without this supervision?
- Consider the possible pros and cons of taking a medication like buprenorphine during pregnancy. Also, consider the risks of NOT taking the drug during pregnancy when a substance use disorder is present.
Methadone
Mechanism of Action and Metabolism
Methadone is a synthetic opioid and a full agonist of the Mu-receptor site, stimulating the same effects as opioids.
- Euphoria
- Analgesia
- Sedation
It can be used as a potent analgesic for pain not responding to traditional medications, such as in clients with cancer or terminal illness, as well as for MAT and neonatal abstinence syndrome (NAS).
For this course, it will be discussed as a MAT agent, used in treatment for clients addicted to opioids such as:
- Heroin
- Fentanyl
- Oxycodone
- Hydrocodone
- Morphine
- Hydromorphone (2)
Methadone is a full agonist at the Mu-receptor, meaning it is a more potent and more easily addictive medication than partial agonists like buprenorphine. Methadone has a long half-life (8-60 hours), occupying the Mu-receptors and blocking short-acting opioids from making a client high. The longer half-life also leads to less severe cravings and withdrawal symptoms. Methadone is also an antagonist to the N-methyl-d-aspartate (NMDA) receptor, which adds to its pain relief action (2).
It has high oral bioavailability, is active in the bloodstream within 30 minutes of ingestion and remains elevated for around 24 hours. It is broken down via CYP3A4 and CYP2B6 enzymes and metabolized through the liver, making it a good option for clients with renal problems.
Medications such as ciprofloxacin, benzodiazepines, fluconazole, cimetidine, and fluoxetine may slow methadone metabolism, increasing the available drug and the side effects of overdose risk. Other medications may speed metabolism and decrease the effects of methadone, including phenobarbital, phenytoin, rifampin, ritonavir, and carbamazepine (2).
Available Forms
Methadone is available in many forms, including oral, IM, subcutaneous, IV, and intrathecal, though only the oral is typically used for MAT.
- Methadone - tablets
- DISKETS - dispersible/dissolvable tablet
- Methadone HCL Intensol - 10mg/ml suspension
- Methadone - dispersible tablet (2)
Dosing and Monitoring
Oral dosing is initiated at 30-40 mg/day with a slow titration of 10-20 mg/week until the optimal dosage is reached. The optimal dosage varies by client and depends on the drug they are replacing, tolerance to opioids, and side effects experienced. A dosage between 80- 150 mg/day is the typical goal. (2)
If parenteral methadone is given, it is usually 50%-80% of the oral dosage.
Blood sugar, EKG, and methadone blood levels should be checked regularly, every week for higher-risk patients, and every 3-6 months for those in good health and compliance. The target methadone blood level is around 400 ug/ml (2).
Side Effects and Contraindications
Potential side effects are directly related to stimulation of the opioid receptors and include:
- Diaphoresis
- Flushing
- Pruritus
- Nausea
- Dry mouth
- Constipation
- Sedation
- Lethargy
- Respiratory Depression
- QT prolongation
- Hypoglycemia (2)
Methadone should be considered with a comprehensive view of a client's health history and other medications. Clients with CNS-related disease processes (trauma, increased ICP, dementia, or delirium) must be monitored closely or have other medication considered.
Methadone should not be used simultaneously as other opioids, benzodiazepines, alcohol, or antipsychotics due to increased CNS effects. Methadone is a Pregnancy Category C medication, and risks versus benefits should be weighed carefully. Infants exposed to methadone in utero are at increased risk of NAS after delivery (2).
Overdose can occur, and clients and support systems should be educated on signs of overdose.
- Lethargy
- Somnolence
- Stupor
- Coma
- Miosis
- Bradycardia
- Hypotension
- Respiratory sedation
- Cardiac arrest
Naloxone is used to reverse overdose (2).
Considerations for Prescribers and Clinics
Methadone is a Schedule II Controlled Substance, meaning it has a high abuse potential and must be carefully monitored. The Prescription Drug Monitoring Program (PDMP) is an electronic database used nationwide to register the distribution of controlled substances so that clients do not seek care at multiple clinics or pharmacies to obtain more of a controlled substance.
When prescribing methadone, providers should check the PDMP for both methadone and other prescription opioids so that they are fully aware of other medications clients may be receiving from other places. Regular urine drug screening should be performed to make sure clients are not using other substances not obtained by prescription and that they are testing positive for methadone, meaning they are genuinely taking it if administration is not observed (2).
At the beginning of treatment, methadone is given in the office under a nurse's supervision, and then clients are monitored for adverse effects. Some take-home doses (up to 7 in the first two weeks) may be arranged for weekends or during travel, but this possibility is limited during the first few weeks of treatment. As treatment progresses and compliance is demonstrated, clients may self-administer more doses at home (up to 28 doses per month) and go longer between visits to the clinic. The total length of treatment varies but is often 1-2 years and can even be indefinite (7).
There are methadone clinics that work entirely in the scope of addiction management, but primary care providers may prescribe methadone as well. Prescribers must have an active DEA license and comply with state-based controlled substance regulations (2).


Self Quiz
Ask yourself...
- Why do you think methadone is a Schedule II Controlled Substance while buprenorphine is only a Schedule III?
- What are the benefits of checking the serum level of methadone?
- What might the clinical presentation be for someone overdosing on methadone?
- Have you ever used the PDMP database before? What are the benefits of accessing this database?
Naltrexone
Mechanism of Action and Metabolism
Naltrexone has been in use since the 1960s and is an opioid antagonist. It competes primarily with the mu-receptor but also serves as an antagonist at the kappa and delta receptors. As an antagonist, it competes with agonists such as opioids and alcohol and blocks the effects of agonists at those sites.
- Prevents euphoria.
- Prevents intoxication.
- Reduces tolerance (6)
Naltrexone also acts on the hypothalamic-pituitary-adrenal axis, modifying it to reduce cravings and suppress alcohol consumption.
It is FDA-approved for use in clinical practice for the treatment of:
- Alcohol use disorder
- Opioid use disorder (prescription and non)
Naltrexone is absorbed orally and undergoes extensive metabolism via the first-pass effect. However, this does not affect its potency as naltrexone's active metabolite, 6β-naltrexone, acts as a potent opioid antagonist. The medication's half-life is around 4 hours but can last up to 24 hours. If administered parenterally, it bypasses the first pass and is even longer acting, with a half-life of 5-10 days. Naltrexone is excreted by the kidneys (6).
Available Forms
Naltrexone is available in an oral tablet and IM injection. Available preparations include:
- Generic naltrexone tablets
- Revia (oral tablet)
- Depade (oral tablet)
- Vivitrol (solution for IM injection, extended-release) (6)
Dosing and Monitoring
Since naltrexone will compete for and block all opioid receptor sites, the risk for withdrawal symptoms is high, and clients must stop the use of alcohol or opioids for 7-10 days before beginning treatment to lessen the risk of withdrawal symptoms. A naltrexone challenge is recommended at the start of therapy.
This consists of administering small amounts of naltrexone subcutaneously or via IV and monitoring the client and their vital signs for signs of withdrawal, such as:
- Nausea
- Vomiting
- Diaphoresis
- BP changes
- Tachycardia
- Rhinorrhea
- Agitation
- Tremors
- Abdominal pain
- Pupillary dilation (6)
If a client fails the naltrexone challenge and has not been long enough since their last use of alcohol or opioids, the naltrexone initiation should be delayed, and the test should be repeated in 24 hours. If clients tolerate the naltrexone test and the negative result, they may begin naltrexone treatment (6).
For oral tablets, dosing usually starts at 25 mg for the first dose. Clients are observed for withdrawal symptoms and side effects; an additional 25 mg is given 1 hour later. After that, clients take 50 mg per day. Clients may continue with 50mg daily or take 100 mg every other day or 150 mg every 3rd day (6).
Alternatively, naltrexone may be given via IM injection for more extended action, improving compliance and reducing relapse. Particularly for alcohol or heroin dependence, data indicates that the IM route has much higher success rates than the oral route. If a client receives the IM injection, 380 mg is given to the gluteal muscle every four weeks (6).
Side Effects and Contraindications
Most common side effects of naltrexone include:
- GI irritation
- Diarrhea
- Abdominal cramps
- Nausea
- Vomiting
- Hypertension
- Headache
- Anxiety
- Low energy
- Joint or muscle pain
- Nervousness
- Sleep disruption
Less commonly, clients report:
- Loss of appetite
- Constipation
- Dizziness
- Irritability
- Depression
- Rash
- Chills (6)
Caution should be used for clients with liver function issues and renal impairment. It is Category C for use during pregnancy, and the risks versus benefits of use in pregnancy must be carefully considered. It also crosses into breast milk and must be considered carefully.
There is limited data about the overdose of naltrexone, and there may be very few symptoms if an overdose occurs. Clients should be monitored for signs of liver dysfunction, seizures, depression, and suicidal ideations. No antidote for naltrexone is currently available.
Naltrexone is contraindicated for clients who failed a naltrexone challenge, test positive for opioids or alcohol on drug screening, have a history of seizures, or have experienced a past hypersensitivity reaction to naltrexone.
Clients may switch from buprenorphine or methadone to naltrexone at some point in treatment. Both medications are agonists at the opioid receptor sites, so changing to naltrexone (an antagonist) may increase the risk of withdrawal symptoms for the first two weeks of treatment (6).
Considerations for Prescribers
Because naltrexone does not cause any euphoria or "high," the abuse potential is non-existent. It is not a controlled substance and can be prescribed by any clinician with prescriptive authority. However, its use is typically only by those who work in mental health or addiction medicine. Clients can take the medication at home or go to the clinic for IM injections.
Many considerations for naltrexone use center around monitoring for side effects and treatment compliance. Baseline and periodic drug screening and liver function tests are prudent. Clients' support persons should be educated on compliance and signs of relapse. The IM formulation should be considered for those with poor compliance or most at risk for relapse (6).

Self Quiz
Ask yourself...
- Why might a client benefit from the IM formulation of naltrexone instead of the oral preparation?
- Why might compliance with an opioid antagonist be more complex than an opioid agonist like methadone or buprenorphine?
- How do side effects differ between naltrexone and the agonist medications like methadone?
- What does it mean if a client fails a "naltrexone challenge," and how does this delay their care?
Nursing Considerations
Nurses will encounter clients with addiction and even those receiving MAT in a variety of settings, including:
- Outpatient clinics for routine care of any health issues
- ED admission for acute problems not related to addiction.
- Inpatient hospitalization related to other health problems.
- Outpatient setting for participation in MAT or addiction management.
- ED admission for acute problems related to substance abuse or toxicity of MAT medication.
- Inpatient mental health admission for mental health and addiction issues
Regardless of the setting and if the client is being seen for an addiction issue or something else, it is crucial for nurses to be familiar with MAT medications and how they work to provide safe and competent care. Nurses may need to:
- Administer medication.
- Monitor lab results.
- Observe for side effects, toxicity, or withdrawal symptoms.
- Coordinate care within a multidisciplinary team
- Communicate with therapeutic and nonjudgmental techniques.


Self Quiz
Ask yourself...
- Have you ever cared for a client in a non-addiction setting who had a MAT medication on their drug list?
- Did you have any biases or preconceived ideas about what this medication meant?
- Is there anything you have learned throughout this course that will change your care the next time you encounter a client receiving MAT?
Case Study
Justin is a 32-year-old male who presents to the ED with nausea, lethargy, and confusion worsening over the last 24 hours. Upon exam, the nurse notes diaphoresis, slurred speech, and pinpoint pupils. His vitals are RR 10, HR 54, BP 82/58, SPO2 97%, Temp 99.0.
He reports taking Wellbutrin 150mg daily for depression and smoking cessation, methadone 100mg daily for history of oxycodone abuse, and was started on ciprofloxacin 250mg BID for a UTI 2 days ago at urgent care.
His labs are significant for a WBC of 15,000 but otherwise regular. He tests positive for methadone, which is expected, but not for other substances. He reports being compliant with MAT and avoiding opioid use for nine months.
It is determined that Justin is experiencing methadone toxicity due to the slowed metabolism of the drug from the combination of methadone and ciprofloxacin. He is given naloxone in the ED, and within an hour, his symptoms have improved significantly, and his vital signs are typical. His antibiotic is switched to cefdinir, and he is discharged home in stable condition with instructions to follow up with his PCP within 1-2 days.

Self Quiz
Ask yourself...
- Given Justin's presentation, how could you differentiate between methadone toxicity and relapse?
- How might Justin's condition have progressed if he had not sought emergency care?
- How would Justin's case have been different if he had not tested positive for methadone?
- In what ways could Justin's care before his ED visit have been improved to avoid this complication?
Conclusion
Substance use disorders are a long-standing and dangerous pathology experienced by millions of people each year. At the same time, the stigma of seeking help for such disorders has been eroding in recent years; there has also been a renewed push by the federal government to address the issue in evidence-based and meaningful ways, with access to effective treatment being at the top of the priority list.
Addiction treatment programs utilizing MAT will likely become much more popular in the coming years, and nurses will be on the front lines of this therapy. For nurses to provide competent and comprehensive care to this client population, up-to-date and accurate knowledge is necessary.
Hypertensive Agents
Definitions
Hypertension – high blood pressure above normal. Normal is considered anything less than 120/80 mmHg [7].
Antihypertensives – medications used to control hypertension and lower blood pressure [7].
Hypertensive crisis – severely elevated blood pressure of either:
- Systolic greater than 180 mmHg
- Diastolic greater than 120 mmHg [19].
Hypertensive emergency – acutely elevated blood pressure with signs of target organ damage [2].
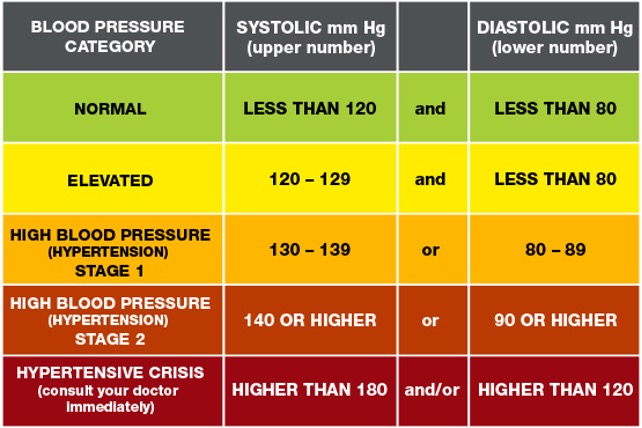

Self-Quiz
Ask Yourself...
- What is hypertension?
- What are antihypertensives?
- What is a hypertensive crisis?
- What is a hypertensive emergency?
Medications Overview
Antihypertensive medications are used for the treatment of hypertension and are used in both inpatient, outpatient, and emergency settings.
Some of the major antihypertensive medication classes include:
- Diuretics
- Beta-blockers
- Angiotensin-converting enzyme inhibitors
- Angiotensin II receptor blockers
- Calcium channel blockers
- Selective alpha-1 blockers
- Alpha-2 Receptor Agonists
- Vasodilators [3].
Different medical organizations have varying recommendations and hypertension treatment guidelines. Hypertension treatment clinical practice guidelines are available from organizations like the American Heart Association, the American College of Cardiology, and the European Society of Cardiology to name a few [21]. Healthcare providers should be aware of their healthcare institution’s recommendations for clinical practice guidelines and organizations.
All organizational guidelines share the same recommended treatment of starting antihypertensives immediately when:
- Blood pressure is greater than 140/90 mmHg for patients with a history of ischemic heart disease, heart failure, or cerebrovascular disease.
- Blood pressure is greater than 160/100 mmHg regardless of underlying medical conditions [21].
Again, healthcare providers should follow current and evidence-based clinical guidelines for initiating or titrating antihypertensive medications.
While most antihypertensives are prescribed in an outpatient setting, certain antihypertensives are indicated during hypertensive or medical emergencies. For example, intravenous (IV) vasodilators, like nitroprusside and nitroglycerin, and calcium channel blockers, like nicardipine, are used during hypertensive emergencies and crises.


Self-Quiz
Ask Yourself...
- In what settings are antihypertensives used?
- What are the clinical guidelines for initiating hypertensive medications?
- Which medications are commonly used to treat hypertensive emergencies?
Pharmacokinetics
Diuretics
Diuretics are a class of drugs that help control blood pressure by removing excess sodium and water from the body through the kidneys. There are several varying types of diuretics, some including thiazide, potassium-sparing, and loop, and all work to lower blood pressure differently [3].
Thiazide Diuretics
Thiazide diuretics remove excess sodium and water from the body by blocking the sodium-chloride (Na-Cl) channels in the kidneys’ distal convoluted tubule. As the Na-Cl channel becomes blocked, this inhibits the reabsorption of sodium and water into the kidneys. Concurrently, this causes a loss of potassium and calcium ions through the sodium-calcium channels and sodium-potassium pump [1].
Thiazide diuretics are approved by the Food and Drug Administration (FDA) for controlling primary hypertension and are available via oral route. Some common thiazide diuretics are hydrochlorothiazide, chlorthalidone, and metolazone [3].
When initiating this medication, the healthcare provider should start with the lowest dose, which is usually 25mg daily, and then increase accordingly to aid with blood pressure control or if the patient has excess fluid retention, usually as evidenced by leg swelling or edema [1].
Common side effects of thiazide diuretics include:
- Increased urination
- Diarrhea
- Headache
- Stomach and muscle aches [16].
As thiazide diuretics interfere with Na-Cl, Na-Ca, and Na-K channels, there is an increased potential for adverse effects, including:
- Hypotension
- Hypokalemia
- Hyponatremia
- Hypercalcemia
- Hyperglycemia
- Hyperlipidemia
- Hyperuricemia
- Acute pancreatitis
When prescribing thiazide diuretics, healthcare providers should avoid prescribing thiazide diuretics to patients with a sulfonamide allergy, since thiazides are sulfa-containing medications. Also, they should avoid prescribing these to patients with a history of gout [1].
Additionally, patients can experience a thiazide overdose if they take more than the amount prescribed. Patients with a suspected overdose may experience confusion, dizziness, hypotension, and other symptoms. These patients must seek emergency care and poison control must be alerted [16].
Potassium-Sparing Diuretics
Potassium-sparing diuretics remove excess sodium and water from the body without causing loss of potassium. Depending on the type, they interrupt sodium reabsorption by either binding to epithelial sodium channels or inhibiting aldosterone receptors. When catatonic sodium is reabsorbed, this creates a negative gradient causing the reabsorption of potassium ions through the mineralocorticoid receptor [5].
Potassium-sparing diuretics are approved for controlling hypertension and are usually combined with other diuretics, like thiazide or loop diuretics since they have a weak antihypertensive effect.
Common names of potassium-sparing diuretics are amiloride, triamterene, and spironolactone. These medications are available by either intravenous or oral routes. Spironolactone is commonly used for treating primary aldosteronism and heart failure [5]. Patients should be started on the lowest dose when first prescribing this class of medications.
Common side effects can include:
- Increased urination
- Hyperkalemia
- Metabolic acidosis
- Nausea
[4]
Healthcare providers should avoid prescribing this class of medications to patients with hyperkalemia or chronic kidney disease. They should also be avoided during pregnancy or in patients who are taking digoxin. Since potassium-sparing medications can cause hyperkalemia, periodic monitoring for electrolyte imbalances and potassium levels is necessary [4].
Loop Diuretics
Loop diuretics inhibit sodium and chloride reabsorption by competing with chloride binding in the Na-K-2Cl (NKCC2) cotransporter. Potassium is not reabsorbed by the kidney, which causes additional calcium and magnesium ion loss.
Loop diuretics are FDA-approved for the treatment of hypertension but are not considered first-line treatment. They can also be used for treating fluid overload in conditions like heart failure or nephrotic syndrome [12].
Loop diuretics are available via oral or IV routes and furosemide, torsemide, and bumetanide are common forms [3].
Bioavailability and dosage differ for each type and route of loop diuretics. The bioavailability of furosemide is 50%, with a half-life of around 2 hours for patients with normal kidney function, and dosages start at 8mg for oral medication. Torsemide has a bioavailability of about 80%, a half-life of about 3 to 4 hours, and oral dosages start at 5mg [12].
Common side effects can include:
- Dizziness
- Increased urination
- Headache
- Stomach upset
- Hyponatremia
- Hypokalemia [13].
Loop diuretics can lead to several adverse effects, including toxicity, electrolyte imbalances, hyperglycemia, and ototoxicity. They have a black box warning stating that high dosages can cause severe diuresis. Therefore, electrolytes, BUN, and creatinine values should be monitored closely by a healthcare provider.
People with a sulfonamide allergy may also be allergic to loop diuretics, so this should be avoided if the patient is allergic. Loop diuretics also interfere with digoxin and therefore should be avoided. Other contraindications include anuria, hepatic impairments, and use during severe electrolyte disturbances [12].


Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of thiazide diuretics?
- What is the pharmacokinetics of loop diuretics?
- What is the pharmacokinetics of potassium-sparing diuretics?
- What are common side effects and contraindications for each type of diuretic?
Beta-Blockers
Beta-blockers work by reducing the body’s heart rate and thus, lowering cardiac output resulting in lowered blood pressure [3]. The mechanism of action for beta-blockers varies, depending on the receptor type it blocks, and are classified as either non-selective or beta-1 (B1) selective.
Non-selective beta-blockers bind to the B1 and B2 receptors, blocking epinephrine and norepinephrine, causing a slowed heart rate. Propranolol, labetalol, and carvedilol are common non-selective beta-blockers.
Alternatively, beta-1 selective blockers only bind to the B1 receptors of the heart, so they are considered cardio-selective. Some examples include atenolol, metoprolol, and bisoprolol. Sotalol is a type of beta-blocker that also blocks potassium channels and is, therefore, a class III antiarrhythmic [8].
Beta-blockers are not primarily used for the initial treatment of hypertension but can be prescribed for conditions like tachycardia, myocardial infarction, congestive heart failure, and cardiac arrhythmias. It’s also approved for use in conditions such as essential tremors, hyperthyroidism, glaucoma, and prevention of migraines.
Beta-blockers are available in many forms, including oral, IV, intramuscular injection, and ophthalmic drops. Starting dosage and route are determined by the health condition being treated [8].
Common side effects of beta-blockers include:
- Bradycardia
- Hypotension
- Dizziness
- Feeling tired
- Nausea
- Dry mouth
- Sexual Dysfunction
[17]
This class of medications can also lead to more severe adverse effects such as orthostatic hypotension, bronchospasm, shortness of breath, hyperglycemia, and increased risk of QT prolongation, torsades de pointes, and heart block [8]. Healthcare providers should avoid prescribing non-selective beta-blockers to patients with asthma. Instead, they can prescribe cardio-selective beta-blockers for patients with asthma.
Additionally, the use of beta-blockers is contraindicated in patients with a history of bradycardia, hypotension, Raynaud disease, QT prolongation, or torsades de pointes. Healthcare providers must encourage patients to monitor their heart rate and blood pressure and follow administration parameters before taking beta-blockers daily since it decreases their heart rate.
Overdose of beta-blockers is life-threatening and healthcare providers must discuss the symptoms of an overdose and the need for emergency care [8].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of beta-blockers?
- What are the common side effects and contraindications of beta-blockers?
Angiotensin-converting Enzyme Inhibitors
Angiotensin-converting enzyme (ACE) inhibitors prevent the body from producing angiotensin, a hormone that causes vasoconstriction. As angiotensin production is reduced, this allows the blood vessels to dilate and therefore lowers blood pressure [3].
Moreover, ACE inhibitors act specifically on the renin-angiotensin-aldosterone system (RAAS) by preventing the conversion of angiotensin I to angiotensin II. It also works to decrease aldosterone, which in turn, decreases sodium and water reabsorption [9].
ACE inhibitors usually end in the suffix -pril and some common examples include lisinopril, benazepril, enalapril, and captopril, and they usually end in the suffix [3].
While ACE inhibitors are approved for treating hypertension, they are also FDA-approved for other uses or combination therapies for medical conditions such as:
- Systolic heart failure
- Chronic kidney disease
- ST-elevated myocardial infarction
One non-approved FDA use is treatment of diabetic nephropathy [9]. This class of medication is available in oral, and IV forms, and dosages are dependent on clinical guidelines, underlying medical conditions, and route.
ACE inhibitors have common side effects, with some including:
- Dry cough
- Dizziness
- Hypotension [9].
This medication can also lead to adverse effects, such as syncope, angioedema, and hyperkalemia [9]. As angioedema is an adverse effect, healthcare providers should understand this class of medications is contraindicated in patients with a history of hypersensitivity to ACE inhibitors.
Additionally, ACE inhibitors are contraindicated in patients with aortic valve stenosis, hypovolemia, and during pregnancy. Individuals with abnormal kidney function should have renal function and electrolyte values monitored. If a patient develops a chronic dry cough, then the healthcare provider should consider another antihypertensive medication class by following current guidelines [9].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of angiotensin-converting enzyme inhibitors?
- What are common side effects and contraindications of angiotensin-converting enzyme inhibitors?
Angiotensin II Receptor Blockers
Similar to ACE inhibitors, Angiotensin II Receptor Blockers (ARBs) act on the RAAS by binding to angiotensin II receptors and thus block and reduce the action of angiotensin II. Again, this reduces blood pressure by causing blood vessel dilation and decreasing sodium and water reabsorption [11]. ARBs typically end in the suffix -artan and common names are losartan, valsartan, and Olmesartan [3]. Oral and IV routes of the medication are available and again, dosages are dependent on the medication specifically and form [11].
All ARBs are FDA-approved for the treatment of hypertension, but a select few are approved for treating other medical conditions, such as:
- Candesartan for heart failure
- Irbesartan for diabetic nephropathy
- Losartan for proteinuria and diabetic nephropathy
- Telmisartan for stroke and myocardial infarction prevention
- Valsartan for heart failure and reduction of mortality in patients with left ventricular dysfunction [11].
Although not as common as ACE inhibitors, two side effects of ARBs are dry cough and angioedema.
Other common side effects include:
- Dizziness
- Hypotension
- Hyperkalemia
[11]
Contraindications for use are if the patient is pregnant or has renal impairment or failure. If a patient is on an ARB, the healthcare provider should closely monitor lab values for electrolyte imbalances and kidney function.
Additionally, if a patient is taking lithium, ARBs can increase lithium concentration and therefore, lithium blood concentration should be frequently checked [11].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of angiotensin II receptor blockers?
- What are common side effects and contraindications of angiotensin II receptor blockers?
Calcium Channel Blockers
Calcium channel blockers (CCBs), also known as calcium channel antagonists, act by preventing calcium from entering the smooth vascular and heart muscles. In turn, this reduces heart rate and causes vasodilation [3].
They are further divided into two major categories, non-dihydropyridines and dihydropyridines, where there are differences in the mechanism of action. Non-dihydropyridines inhibit calcium from entering the heart’s sinoatrial and atrioventricular nodes and thus cause a cardiac conduction delay and reduce cardiac contractility.
Alternatively, dihydropyridines do not directly affect the heart but do act as a peripheral vasodilator leading to lowered blood pressure. Both categories are metabolized by the CYP3A4 pathway [15].
Names of non-dihydropyridine CCBs are verapamil and diltiazem. Dihydropyridine CCBs typically end in the suffix -pine and common names are amlodipine and nicardipine. Both categories are available via oral and IV routes for administration. Oral dosages of non-dihydropyridine CCBs start at 30mg daily and dihydropyridine CCBs start at 30mg daily for immediate release [15].
Calcium channel blockers can be used to treat other medical conditions in addition to hypertension and include:
- Coronary spasm
- Angina pectoris
- Supraventricular dysrhythmias
- Pulmonary hypertension
- Hypertrophic cardiomyopathy
Non-dihydropyridine CCBs can cause side effects like bradycardia, and constipation, while dihydropyridine CCBs can cause:
- Headaches
- Feeling lightheaded
- Leg swelling [15].
Both categories pose the risk of potential hypotension and bradycardia, so healthcare providers should closely monitor the patient’s blood pressure and heart rate when initiating or titrating the dosage.
Also, an overdose of this medication can lead to cardiac conduction delays, complete heart block, and cardiovascular collapse. Patients with possible symptoms of overdose should be sent to the emergency room immediately.
Additionally, healthcare providers should avoid prescribing CCBs to people with heart failure and sick sinus syndrome [15].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of calcium channel blockers?
- What are the common side effects and contraindications of calcium channel blockers?
Selective Alpha-1 Blockers
Selective alpha-1 blockers act on the body’s sympathetic nervous system to lower blood pressure. They prevent norepinephrine from binding to the alpha-1 receptors of the sympathetic nervous system, causing smooth muscle relaxation and vasodilation which leads to lowered blood pressure [18].
Selective alpha-1 blockers are available via the oral route, end in the suffix -osin and examples are doxazosin, terazosin, and prazosin [3]. They are FDA-approved for the treatment of hypertension but are not considered first-line therapy. Additionally, this class of medications may be used to treat benign prostatic hyperplasia. Dosages can start as low as 1mg daily depending on the drug selected.
Common side effects include:
- Hypotension
- Tachycardia
- Dizziness
- Headache
- Weakness [18].
As selective alpha-1 blockers can lead to orthostatic hypotension, the healthcare provider should instruct the patient to take this medication at night. They should also avoid prescribing to the elderly population when able because of hypotension and increased fall risk [18].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of alpha-1 blockers?
- What are the common side effects and contraindications of alpha-1 blockers?
Alpha-2 Receptor Agonists
Alpha-2 receptor agonists work by decreasing the activity of the sympathetic nervous system to lower blood pressure. It inhibits adenylyl cyclase and decreases the formation of cyclic adenosine monophosphate (cAMP). Alpha-2 agonists also cause vasodilation by reducing the amount of available cytoplasmic calcium [20].
This class of medications is typically administered via oral route but is also available in intravenous and transdermal forms. Two FDA-approved alpha-2 agonists for hypertension treatment are methyldopa and clonidine and dosages are dependent on the name and route.
Methyldopa is commonly prescribed to patients with hypertension and who are pregnant since it’s safe [20].
Common side effects of alpha-2 receptor agonists are:
- Dry mouth
- Drowsiness
- Fatigue
- Headache
- Sexual dysfunction [3].
Contraindications for use are orthostatic hypotension and autonomic disorders. Healthcare providers must avoid prescribing alpha-2 receptor agonists to individuals taking phosphodiesterase inhibitors [20].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of alpha-2 receptor agonists?
- What are common side effects and contraindications of alpha-2 receptor agonists?
Vasodilators
Vasodilators lower blood pressure by dilating the body’s blood vessels. It binds to the receptors of the blood vessel’s endothelial cells, releasing calcium. Calcium stimulates nitric oxide synthase (NO synthase), eventually converting to L-arginine to nitric oxide. As nitric oxide is available, this allows for GTP to convert to cGMP, and causes dephosphorylation of the myosin and actin filaments. As this occurs, the blood vessels’ smooth muscles relax, leading to vasodilation and lowered blood pressure.
Common vasodilators that act via this pathway are nitrates and minoxidil. Hydralazine is another vasodilator, but the mechanism of action is unknown [10].
Available forms of vasodilators are sublingual, oral, and intravenous. Similar to other classes of antihypertensives, vasodilator dosages depend on the form and treatment setting [10].
Nitrovasodilators like nitroprusside and nitroglycerin are used during hypertensive emergencies. Hydralazine is used for severe hypertension for the prevention of eclampsia or intracranial hemorrhage and minoxidil for resistant hypertension [10] [3].
Side effects for each will vary, but nitrates commonly cause:
- Reflex tachycardia
- Headache
- Orthostatic hypotension
[10]
Common side effects of hydralazine are headaches, heart palpitations, and myalgias. Minoxidil causes excessive hair growth, weight gain, and fluid retention [3]. Additionally, nitroprusside can potentially cause cyanide toxicity.
Vasodilators have varying degrees of contraindications, such as nitrates are avoided in patients with an inferior myocardial infarction. Hydralazine should not be given to patients with coronary artery disease, angina, or rheumatic heart disease. Healthcare providers should be aware of contraindications and monitor patients’ blood pressure and potential side effects [10].

Self-Quiz
Ask Yourself...
- What is the pharmacokinetics of vasodilators?
- What are the common side effects and contraindications of vasodilators?
Combination Antihypertensives
Many antihypertensive medications come in combined forms, such as ACE inhibitors and thiazide diuretics, beta-blockers and diuretics, or calcium channel blockers and ACE inhibitors. The mechanism of action for combination antihypertensives depends on the blend of medications [3].
Considerations for Prescribers
This section reviews potential considerations when prescribing antihypertensives.
When prescribing antihypertensive medications, there are several factors that healthcare providers must consider. The route is typically determined by the healthcare setting and dosage by the underlying treatment goals. Again, healthcare providers should follow current guidelines when initiating or titrating antihypertensive medications.
Healthcare providers must complete a thorough health history, and review lab values, and contraindications as mentioned above. Monitoring kidney function and electrolyte values is imperative while any patient is taking antihypertensive medications.
While a single antihypertensive medication is recommended for initial treatment, there are some scenarios where combination therapy or combination antihypertensives are recommended [14].
Healthcare providers should also discuss the potential side effects of antihypertensives with patients and what to do if they are experiencing symptoms. For instance, if a patient reports syncope, they should be advised to go to the emergency room or be seen immediately for further evaluation. Also, healthcare providers must encourage patients to monitor their heart rate and blood pressure at home and abide by administration parameters.
For example, instruct patients who are taking beta-blockers to measure their blood pressure and heart rate before taking their medication. If their heart rate is below 60 beats per minute, then they should not take the medication [14].
If a patient is experiencing side effects from an antihypertensive medication, then another alternative should be selected.


Self-Quiz
Ask Yourself...
- What factors should healthcare providers consider when prescribing antihypertensives?
Upcoming Research
This section reviews upcoming research and medications for hypertension treatment.
Research on antihypertensive medications has slowed throughout the years. Some clinical trials were performed on the potential of endothelin receptor antagonists to reduce hypertension. However, some studies found several unwanted side effects, and thus clinical use was stopped for safety reasons.
An endothelin-A and endothelin-B receptor blocker, called aprocinentan, has shown promise for the treatment of resistant hypertension by lowering blood pressure and decreasing vascular resistance.
Research on sodium-glucose transport protein (SGLT2) inhibitors, which are typically used for the treatment of type II diabetes mellitus, is also ongoing. SGLT2 inhibitors may promote blood pressure reduction through diuresis and reduce sympathetic tone [21].

Self-Quiz
Ask Yourself...
- What new research is there about antihypertensives?
Conclusion
If hypertension is left untreated, it can lead to serious health complications, including death. When selecting antihypertensive treatment, healthcare providers should understand the pharmacokinetics of each drug class along with potential side effects and contraindications. They should also follow current clinical guidelines for an evidence-based approach.
Final Reflection Questions
- Which antihypertensive medication is often prescribed during pregnancy?
- Which lab values are important when monitoring patients on each antihypertensive medication?
- Which antihypertensive medications cause hypokalemia?
- Which antihypertensive medications cause hyperkalemia?
Migraine Management

Self Quiz
Ask yourself...
- How might a comprehensive knowledge of migraine medications, including their mechanisms of action, enhance the ability of healthcare professionals to address the specific needs of patients experiencing migraines?
- In what ways can recognizing warnings related to migraine medications contribute to ensuring patient safety?
Definition
Migraines are recurrent, pulsating headaches often accompanied by other symptoms such as nausea, sensitivity to light, and sensitivity to sound. According to recent studies by (17), migraines are recognized as a complex neurological disorder involving abnormal brain activity and a cascade of events leading to pain and associated symptoms.
The impact of migraines extends beyond physical pain, influencing various aspects of life, and recent literature by (14) highlights the profound effect on the quality of life, with disruptions in daily activities, work, and social interactions. For example, a professional experiencing frequent migraines might struggle to meet work deadlines and engage in social events. Recent advancements in diagnostic criteria by (15) emphasize the importance of a precise definition to ensure appropriate treatment strategies. Therefore, understanding the definition is crucial for accurate diagnosis and effective communication between healthcare providers and patients.


Self Quiz
Ask yourself...
- What distinguishes migraines from common headaches, and how does understanding this difference impact the approach to their management?
- In what ways do migraines extend beyond physical pain, and how might this impact influence an individual's overall quality of life?
- How can a precise definition of migraines contribute to accurate diagnosis, and why is accurate diagnosis essential for effective treatment planning?
- How does understanding the definition of migraines facilitate effective communication between healthcare professionals and patients?
Migraine Medications
Understanding the various classes of migraine medications is like having a diverse toolkit to address the complexities of this neurological disorder. By exploring the different classes of medications, healthcare professionals can tailor their approach and make informed decisions based on individual patient profiles and specific migraine characteristics (20).
It is crucial to recognize that migraine medications are not one-size-fits-all. Each patient is unique, and their response to medications may vary. Recent literature by (12) emphasizes the importance of an individualized approach when considering the best medication for each patient. Here’s a list of migraine medications in addition to important details to consider:
Triptans
Triptans are a class of medications specifically designed for the acute treatment of migraines. According to (39), they are not meant for preventive use but are highly effective in providing relief during an ongoing migraine attack. They work by narrowing blood vessels and inhibiting the release of certain chemicals in the brain associated with migraine symptoms (39). Let’s see more details below as described by (7), (39), (29).
Drug Class
Belonging to the serotonin (5-HT) receptor agonists class, Triptans modulate the effects of serotonin receptors in the brain. The various types of Triptans include Sumatriptan, Rizatriptan, Eletriptan, and others. Each Triptan has unique characteristics, such as the onset of action and duration, allowing healthcare professionals to tailor prescriptions based on individual patient needs.
Benefits
Triptans offer several benefits in the management of migraines. One of the primary advantages is their ability to provide rapid and effective relief from migraine symptoms, including headache pain, nausea, and sensitivity to light and sound. The prompt onset of action is particularly valuable for individuals aiming to resume their daily activities quickly. Triptans are available in various formulations, including oral tablets, nasal sprays, and injectables, allowing for flexibility in administration.
Side Effects
While generally well-tolerated, Triptans may cause side effects. Common side effects include mild sensations of warmth or tingling, dizziness, and tightness or pressure in the chest. It is crucial for healthcare professionals to consider the patient's medical history and potential contraindications, such as cardiovascular issues, before prescribing Triptans. In rare cases, more severe side effects like chest pain and changes in heart rate may occur, necessitating immediate medical attention.
Clinical Effects
The clinical effects of Triptans are profound, offering relief to individuals experiencing acute migraine attacks. The primary outcomes include:
- Pain Relief: Triptans are highly effective in reducing the intensity of migraine-associated pain. By targeting the vascular and neuronal components of migraines, these drugs provide rapid relief, allowing patients to resume their normal activities.
- Relief of Associated Symptoms: Beyond pain relief, Triptans address accompanying symptoms such as nausea, photophobia, and phonophobia. This comprehensive effect enhances the overall patient experience during a migraine episode.
- Prevention of Migraine Progression: Triptans, when administered early in the migraine attack, can prevent the progression of the headache phase to more severe stages. This early intervention is crucial for optimizing outcomes and minimizing the impact of migraines on daily life.
- Improvement in Functional Impairment: Migraines often result in functional impairment, limiting individuals' ability to perform daily tasks. Triptans restore functional capacity, allowing patients to regain control over their activities.
Nonsteroidal Anti-Inflammatory Drugs (NSAIDSs)
Nonsteroidal anti-inflammatory drugs, commonly known as NSAIDs, constitute a class of medications used in the treatment of migraines. According to (6), these drugs are characterized by their anti-inflammatory, analgesic, and antipyretic properties. NSAIDs are versatile, as they are not exclusively used for migraines but are also used for various other pain and inflammatory conditions (6). Let’s see more details below as described by (25), (40), (6) and (28).
Drug Class
NSAIDs encompass a broad class of medications, including well-known examples such as ibuprofen, naproxen, and aspirin. They function by inhibiting enzymes called cyclooxygenases (COX), thereby reducing the production of inflammatory prostaglandins. This mechanism provides relief from pain and mitigates inflammation associated with migraines.
Benefits
The primary benefit of NSAIDs in migraine management lies in their ability to alleviate pain and reduce inflammation. They are particularly effective for individuals experiencing mild to moderate migraines. NSAIDs offer a rapid onset of action, making them suitable for individuals seeking prompt relief. Additionally, these medications are available over-the-counter in many formulations, providing accessibility for patients.
Side Effects
While NSAIDs are generally well-tolerated, they may cause side effects, especially with prolonged or excessive use. Common side effects include gastrointestinal issues such as stomach upset or ulcers. Healthcare professionals need to consider a patient's medical history, including conditions like gastric ulcers, before prescribing NSAIDs. In rare cases, more severe side effects like cardiovascular events may occur, emphasizing the importance of cautious use.
Clinical Effects
The clinical effects of NSAIDs in migraine management encompass various aspects. Here’s a list of some of them.
- Pain Relief: NSAIDs are effective in providing pain relief during acute migraine attacks. By reducing prostaglandin levels, they alleviate headache symptoms and contribute to the overall comfort of individuals experiencing migraines.
- Inhibition of Inflammatory Responses: The anti-inflammatory properties of NSAIDs are particularly beneficial when migraines are associated with inflammatory processes. NSAIDs help mitigate inflammation, reducing the severity and duration of migraine attacks.
- Improvement in Associated Symptoms: Beyond pain relief, NSAIDs address associated symptoms such as nausea and photophobia, enhancing the overall patient experience during a migraine episode.
- Prevention of Migraine Progression: When administered early in the migraine attack, NSAIDs can prevent the progression of headaches to more severe stages. This early intervention is critical for optimizing outcomes and minimizing the impact of migraines on daily life.
Calcitonin Gene-Related Peptide (CGRP) Inhibitors
Calcitonin gene-related peptide (CGRP) inhibitors represent a modern class of medications revolutionizing the landscape of migraine management. According to (11), these drugs specifically target CGRP, a neuropeptide involved in dilating blood vessels and transmitting pain signals. By inhibiting CGRP, these inhibitors aim to modulate migraine pathways and reduce the frequency and severity of attacks (11). Let’s see more details below as described by (23) and (11).
Drug Class
CGRP inhibitors belong to a unique drug class designed explicitly for migraine prevention. Examples of CGRP inhibitors include Erenumab, Fremanezumab, and Galcanezumab. These medications are administered via subcutaneous injections, typically monthly or quarterly. The focus on preventive therapy distinguishes CGRP inhibitors from acute treatment options like Triptans.
Benefits
The primary benefit of CGRP inhibitors lies in their efficacy in preventing migraines. Clinical trials have demonstrated a significant reduction in the frequency of monthly migraine attacks among individuals using CGRP inhibitors. This preventive approach is especially valuable for those with frequent and debilitating migraines, offering a chance to enhance their quality of life.
Moreover, CGRP inhibitors are well-tolerated with fewer side effects than other preventive medications. They provide a targeted and specific intervention, addressing the underlying mechanisms of migraines without causing widespread effects on other bodily functions.
Side Effects
While generally well-tolerated, CGRP inhibitors may have some side effects. Local injection site reactions, such as redness or swelling, are common but typically mild. It is crucial for healthcare professionals to monitor and address any adverse effects promptly. Additionally, ongoing research is essential to further understand the long-term safety profile of these medications.
Clinical Effects
The clinical effects of CGRP inhibitors are transformative in the realm of migraine management, offering a novel approach to prevention. Primary clinical effects include the following:
- Reduction in Migraine Frequency: One of the hallmark effects of CGRP inhibitors is a significant reduction in the frequency of migraine attacks. By consistently blocking CGRP receptors, these medications disrupt the migraine cascade, leading to a sustained preventive effect.
- Improvement in Migraine Severity: CGRP inhibitors not only reduce the frequency but also contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall quality of life for individuals suffering from chronic migraines.
- Enhanced Functional Capacity: Migraines often result in functional impairment, limiting individuals' ability to perform daily tasks. CGRP inhibitors restore functional capacity, allowing patients to regain control over their activities and participate more fully in their daily lives.
- Well-Tolerated Profile: CGRP inhibitors are generally well-tolerated, with a favorable side effect profile. This characteristic enhances patient adherence to preventive treatment, a critical factor in long-term migraine management.
Beta-Blockers
Beta-blockers are a class of medications that have found a significant place in migraine management. Initially developed for cardiovascular conditions, beta-blockers have demonstrated efficacy in preventing migraines by reducing the frequency and severity of attacks (32). According to (32), these medications work by blocking the effects of adrenaline, leading to reduced heart rate and blood pressure. Let’s see more details below as described by (32) and (27).
Drug Class
Beta-blockers encompass various medications, with examples such as propranolol, metoprolol, and timolol commonly prescribed for migraine prevention. These drugs fall into the broader category of antihypertensive medications but are repurposed for their preventive benefits in migraine care. Unlike acute treatments, which provide relief during an ongoing attack, beta-blockers are taken regularly to reduce the overall occurrence of migraines.
Benefits
The primary benefit of beta-blockers in migraine management is their preventive action. Clinical studies have shown that beta-blockers can significantly reduce the frequency of migraines, making them particularly suitable for individuals with chronic or frequent attacks. This preventive approach aims to enhance the overall quality of life for those who experience migraines regularly.
Beta-blockers are especially beneficial for individuals with comorbid conditions such as hypertension or heart disease. By addressing both cardiovascular concerns and migraines, these medications offer a comprehensive therapeutic approach.
Side Effects
While generally well-tolerated, beta-blockers may cause side effects that individuals need to be aware of. Common side effects include fatigue, dizziness, and changes in sleep patterns. Healthcare professionals need to monitor patients regularly and adjust the dosage or consider alternative medications if side effects become problematic. Beta-blockers are typically avoided in individuals with certain heart conditions, emphasizing the importance of an individualized approach.
Clinical Effects
The clinical effects of beta-blockers in migraine management encompass various dimensions. See some examples below:
- Reduction in Migraine Frequency: Beta-blockers are known for their ability to reduce the frequency of migraine attacks significantly. This preventive effect is especially valuable for individuals experiencing chronic migraines, enhancing their overall quality of life.
- Alleviation of Migraine Severity: Beyond frequency reduction, beta-blockers contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall comfort of individuals during migraine episodes.
- Improvement in Associated Symptoms: Beta-blockers have been shown to address associated symptoms such as nausea and sensitivity to light. By modulating the autonomic nervous system, these medications offer a holistic approach to migraine management.
- Cardiovascular Benefits: Beta-blockers provide additional benefits for individuals with comorbidities due to their primary use in cardiovascular conditions. This dual action allows for comprehensive management of both migraine and cardiovascular health.
Anticonvulsants
Anticonvulsants, originally developed to control seizures in epilepsy, have emerged as a valuable class of medications in the preventive management of migraines (9). According to (9), these drugs, also known as antiepileptic drugs (AEDs), work by stabilizing electrical activity in the brain and reducing the frequency and severity of migraine attacks. Let’s see more details below as described by (32) and (9).
Drug Class
Anticonvulsants comprise a diverse class of medications, including Topiramate, Valproic acid, and Gabapentin. While their primary use may be in epilepsy, the preventive benefits of certain anticonvulsants extend to migraines. These medications are taken regularly to provide ongoing protection against migraines.
Benefits
The primary benefit of anticonvulsants in migraine management is their preventive action. Clinical trials have demonstrated the efficacy of certain anticonvulsants, such as topiramate, in significantly reducing the frequency of migraines. This preventative approach is particularly suitable for individuals with chronic or frequent attacks, aiming to improve overall quality of life.
Anticonvulsants are especially valuable for individuals who may not find relief or experience intolerable side effects with other preventive medications. The versatility of this drug class allows healthcare professionals to tailor treatment plans based on individual patient characteristics and responses.
Side Effects
While generally well-tolerated, anticonvulsants may cause side effects that individuals need to be aware of. Common side effects include drowsiness, dizziness, and gastrointestinal disturbances. It is crucial for healthcare professionals to monitor patients regularly and adjust the dosage or consider alternative medications if side effects become problematic. Additionally, certain anticonvulsants may have specific considerations, such as the need to regularly monitor liver function in individuals taking Valproic acid.
Clinical Effects
The clinical effects of anticonvulsants in migraine management encompass the following dimensions:
- Reduction in Migraine Frequency: Anticonvulsants are known for their ability to significantly reduce the frequency of migraine attacks. This preventive effect is particularly valuable for individuals experiencing chronic migraines, substantially improving their overall quality of life.
- Alleviation of Migraine Severity: Beyond frequency reduction, anticonvulsants contribute to a decrease in the severity of migraine attacks. This comprehensive effect enhances the overall comfort of individuals during migraine episodes.
- Improvement in Associated Symptoms: By modulating neurotransmission and neuronal excitability, Anticonvulsants address associated symptoms such as nausea and sensitivity to light. This holistic approach contributes to a more comprehensive management of migraines.
- Beneficial in Comorbid Conditions: Anticonvulsants, due to their broader neurological effects, can be helpful for individuals with comorbid conditions such as epilepsy or mood disorders. This dual benefit allows for comprehensive management and improves overall well-being.

Self Quiz
Ask yourself...
- How do Triptans contribute to migraine management, and in what scenarios might healthcare professionals prioritize their use during acute migraine attacks?
- Can you differentiate the mechanisms of action between NSAIDs and Triptans in migraine management, and how might this understanding influence the choice of medication for a specific patient?
- What roles do CGRP inhibitors play in migraine pharmacotherapy?
- Consider a scenario where a patient experiences migraines with comorbid cardiovascular issues. How might the choice of medication be influenced by the need to prioritize both migraine relief and cardiovascular safety?
Clinical Criteria for Prescribing
In migraine management, prescribing medications involves a comprehensive understanding of clinical criteria to tailor interventions effectively. This section explores the clinical factors guiding the prescription of migraine medications and the decision-making process for healthcare providers. Here are some of the factors.
Frequency and Severity of Migraine Attacks
An essential consideration in prescribing migraine medications is the frequency and severity of migraine attacks experienced by the patient. For instance, a patient suffering from frequent and severe attacks may benefit from preventive medications to reduce the overall frequency and intensity of migraines (31).
Individual Response to Pain and Associated Symptoms
The subjective experience of pain and associated symptoms during migraines varies among individuals. A patient who experiences intense nausea and vomiting may require medications with rapid onset and alternative formulations, such as nasal sprays or injectables, to address these specific symptoms effectively (8).
Impact on Daily Functioning and Quality of Life
Prescribing migraine medications involves considering the impact of migraines on a patient's daily functioning and overall quality of life (24). For example, a working professional with migraines that significantly impede productivity may require acute medications with fast-acting formulations for quick relief during work hours.
Comorbid Conditions and Patient Preferences
Comorbid conditions and patient preferences are pivotal factors in prescribing migraine medications. A patient with comorbid cardiovascular issues may require careful consideration of medication options to mitigate potential risks (2).

Self Quiz
Ask yourself...
- How does a patient's medical history, especially factors like cardiovascular health, influence the clinical criteria for prescribing migraine medications?
- Why is it essential for healthcare professionals to assess the frequency and severity of migraine attacks when determining the clinical criteria for prescribing medications?
- How do patient preferences contribute to the clinical criteria for prescribing migraine medications?
Pharmacokinetics
Understanding the pharmacokinetics of migraine management medications enables healthcare professionals to tailor treatment plans based on individual patient characteristics, ensuring maximum therapeutic benefit. Let’s get into more details for each of the medications listed above:
Triptans
Absorption
Triptans exhibit distinct pharmacokinetic properties that influence their efficacy and onset of action. Following oral administration, Triptans are absorbed through the gastrointestinal tract and the rate of absorption varies among different Triptans, contributing to differences in their clinical profiles. (39)
Distribution
Upon absorption, Triptans undergo distribution to reach target sites in the body, primarily the central nervous system. Their lipophilic nature allows them to penetrate the blood-brain barrier, enabling interaction with serotonin receptors implicated in migraine pathophysiology. The distribution of Triptans influences their ability to exert effects centrally and peripherally. (39)
Metabolism
Metabolism is a crucial aspect of triptan pharmacokinetics, occurring predominantly in the liver. The enzyme responsible for triptan metabolism is monoamine oxidase-A (MAO-A). (39)
Excretion
The final phase in the pharmacokinetic journey of Triptans is excretion, primarily through renal and biliary routes. Renal excretion eliminates the unchanged drug and its metabolites, while biliary excretion expels metabolites via the bile into the gastrointestinal tract. The interplay between metabolism and excretion contributes to the overall pharmacokinetic profile of Triptans. Variations in renal function may influence the elimination of the half-life of certain Triptans, impacting the duration of their therapeutic effect. (39)
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
Absorption
Following oral administration, NSAIDs are absorbed in the gastrointestinal tract, with the rate and extent varying among different agents. For instance, ibuprofen exhibits rapid absorption, making it suitable for prompt relief during acute migraine attacks. On the other hand, naproxen has a longer duration of action due to slower absorption, making it well-suited for sustained pain relief. (28)
Distribution
Upon absorption, NSAIDs embark on a journey of distribution throughout the body. Their lipophilic nature allows for penetration into various tissues, including inflamed areas. The distribution influences the drug's ability to reach target sites, such as the central nervous system, where NSAIDs exert their analgesic and anti-inflammatory effects. This property is particularly relevant in the context of migraines, where the inflammatory component contributes to pain. (28)
Metabolism
Metabolism plays a role in shaping the pharmacokinetic profile of NSAIDs, occurring primarily in the liver. Enzymes such as cytochrome P450 contribute to the biotransformation of NSAIDs into metabolites. The metabolism of NSAIDs can vary among individuals, impacting factors such as drug efficacy and potential side effects. For example, the metabolism of certain NSAIDs, like diclofenac, can be influenced by genetic polymorphisms, contributing to interindividual variability in drug response. (21)
Excretion
The final phase of the NSAID journey involves excretion, predominantly through the kidneys. Unchanged NSAIDs and their metabolites are eliminated via urine. Considerations of renal function are crucial in the context of NSAID use, as impaired kidney function can lead to prolonged drug half-life and increased risk of adverse effects. Regular monitoring of renal function is essential, especially in individuals with conditions that may affect kidney health. (21)
Calcitonin Gene-Related Peptide (CGRP)
Absorption
Administered via subcutaneous injections, CGRP inhibitors such as Erenumab and Fremanezumab enter the bloodstream directly, allowing for precise control over drug levels. This mode of administration ensures a reliable and consistent absorption rate, contributing to the predictability of therapeutic outcomes. (11)
Distribution
Following absorption, CGRP inhibitors are distributed throughout the body, focusing on target sites implicated in migraine pathophysiology, like the central nervous system. (11)
Metabolism
Unlike many traditional medications, CGRP inhibitors follow a different path in terms of metabolism. Due to their biotechnological origin as monoclonal antibodies, these drugs do not undergo significant hepatic metabolism. Instead, proteolytic enzymes break them down into smaller peptides and amino acids, which occur systemically. This unique metabolic pathway aligns with the specificity of CGRP inhibitors, minimizing interactions with hepatic enzymes and potential drug-drug interactions. (37)
Excretion
The final phase of the CGRP inhibitor journey involves excretion, primarily through the kidneys via renal clearance. This aspect is particularly relevant when considering individual patient factors such as renal function, as impaired kidney function can affect the clearance of CGRP inhibitors and influence their duration of action. (37)
Beta-Blockers
Absorption
Administered orally, beta-blockers like propranolol and metoprolol are absorbed through the gastrointestinal tract. Depending on the condition of the gastrointestinal tract, the rate and extent of absorption can vary, impacting the time it takes for these medications to reach therapeutic levels in the bloodstream. (27)
Distribution
Once absorbed, beta-blockers embark on distribution throughout the body. Their lipophilic nature enables penetration through cell membranes, allowing them to reach target tissues, including the heart and blood vessels. In the context of migraine management, the distribution properties of beta-blockers are crucial for their ability to modulate the autonomic nervous system centrally and peripherally, leading to the desired preventive effects against migraines. (27)
Metabolism
The metabolism of beta-blockers occurs primarily in the liver, where enzymes play a role in their biotransformation. Genetic polymorphisms in these enzymes can contribute to interindividual variability in drug metabolism. (27)
Excretion
The final phase of the beta-blocker journey involves excretion, predominantly through the kidneys, where unchanged beta-blockers and their metabolites are eliminated via urine. The renal excretion of these drugs is relevant when considering individual patient factors, such as renal function, as impaired kidney function can affect the clearance of beta-blockers and influence their duration of action. (27)
Anticonvulsants
Absorption
Typically administered orally, anticonvulsants like topiramate and valproic acid are absorbed through the gastrointestinal tract. The rate and extent of absorption play a crucial role in determining the onset of action and overall effectiveness. (9)
Distribution
Following absorption, anticonvulsants undergo distribution throughout the body. Their lipophilic nature allows them to penetrate the blood-brain barrier, reaching target sites in the central nervous system relevant to migraine pathophysiology. The distribution properties of anticonvulsants contribute to their ability to modulate neuronal excitability centrally and exert preventive effects against migraines. (9)
Metabolism
Metabolism is a crucial aspect of anticonvulsant pharmacokinetics. This occurs predominantly in the liver and enzymes play an important role in the biotransformation of anticonvulsants into metabolites. The metabolism of anticonvulsants can vary among individuals, impacting factors such as drug efficacy and potential side effects. For example, valproic acid undergoes extensive hepatic metabolism, and variations in enzyme activity can lead to interindividual variability in drug response. (30)
Excretion
The final phase in the anticonvulsant journey involves excretion, primarily through the kidneys. Unchanged anticonvulsants and their metabolites are eliminated via urine. This renal excretion is relevant when considering individual patient factors such as renal function, as impaired kidney function can affect the clearance of anticonvulsants and influence their duration of action. (30)

Self Quiz
Ask yourself...
- How do the pharmacokinetics of Triptans, specifically their absorption and distribution, contribute to their efficacy in managing acute migraine attacks?
- Can you explain the key pharmacokinetic parameters of nonsteroidal anti-inflammatory drugs (NSAIDs) used in migraine management and how they influence drug effectiveness?
- What role do pharmacokinetic factors play in the onset and duration of action of calcitonin gene-related peptide (CGRP) inhibitors?
- In the context of migraine medications, how does the pharmacokinetics of beta-blockers influence their absorption, distribution, metabolism, and excretion in the body?
Warnings Related to Migraine Medications
Understanding potential warnings related to migraine medications is essential for healthcare professionals to ensure safe and effective treatment. Here are some factors to consider.
Medication Safety
Migraine medications, whether preventive or acute, come with specific warnings that need careful attention. For instance, some medications may have contraindications for individuals with certain medical conditions or those taking specific medications concurrently. According to (34), healthcare providers must be vigilant in assessing patient medical histories to identify potential contraindications.
Addressing Cardiovascular Risks
Certain migraine medications, such as Triptans, may pose cardiovascular risks, especially in individuals with pre-existing cardiovascular conditions (35). Therefore, it is crucial for healthcare providers to assess patients' cardiovascular health and consider alternative medications or dose adjustments for those at higher risk. For example, a patient with a history of myocardial infarction may be advised to avoid Triptans, and a different class of medication, like NSAIDs, may be recommended.
Pregnancy and Lactation Considerations
Warnings related to pregnancy and lactation are paramount. Some migraine medications may have potential risks during pregnancy, and healthcare providers must carefully weigh the benefits and risks when prescribing for pregnant or lactating individuals. For instance, valproic acid is associated with an increased risk of congenital disabilities, and alternative medications with a safer profile may be preferred for pregnant individuals seeking migraine relief (1).
Managing Medication Overuse Headaches (MOH)
A significant warning associated with migraine medications is the risk of medication overuse headaches (34). To prevent this problem, healthcare providers need to educate patients about the importance of adhering to prescribed dosages and avoiding excessive use of acute medications. Offering alternative strategies, such as lifestyle modifications and preventive medications, can be crucial in managing and preventing MOH.


Self Quiz
Ask yourself...
- What are some common warnings associated with the use of Triptans in migraine management, and how should healthcare providers address these warnings?
- Can you identify specific cardiovascular risks associated with certain migraine medications, and what should be considered when prescribing these medications to patients with pre-existing cardiovascular conditions?
- What warnings are typically associated with the use of valproic acid in migraine management, particularly concerning specific patient populations such as pregnant individuals?
- How do healthcare providers manage and educate patients about the risk of medication overuse headaches associated with certain migraine medications, and what preventive measures can be implemented to minimize this risk?
Alternatives to Migraine Medications
According to (5), integrating alternative methods provides additional tools for healthcare professionals and empowers individuals seeking a more comprehensive and personalized approach to migraine care. Here are some alternative approaches:
Holistic Lifestyle Modifications
Holistic management of migraines involves lifestyle modifications that can significantly impact the frequency and severity of attacks. For instance, incorporating regular physical activity, maintaining a consistent sleep schedule, and managing stress through practices like mindfulness and yoga have shown promise in reducing migraine occurrence (5). Educating patients about these lifestyle changes empowers them to actively participate in their migraine management.
Biofeedback and Relaxation Techniques
Biofeedback and relaxation techniques offer non-pharmacological interventions that enhance self-awareness and control over physiological responses (22). These approaches teach individuals to recognize and manage stress triggers, ultimately reducing the frequency of migraines. For example, biofeedback training that monitors muscle tension and provides real-time feedback can effectively prevent migraines (22).
Acupuncture and Acupressure
According to (22), traditional Chinese medicine practices like acupuncture and acupressure have gained recognition for their potential in migraine management. Acupuncture involves the insertion of thin needles into specific points on the body, while acupressure applies pressure to these points. Research suggests that these methods reduce the frequency and intensity of migraines, providing an alternative avenue for individuals seeking non-pharmacological options (22).
Nutritional Approaches
Dietary modifications and nutritional approaches also play a role in holistic migraine management. For example, identifying and avoiding potential trigger foods, such as those containing tyramine or artificial additives, can be beneficial (10). Additionally, ensuring adequate hydration and incorporating anti-inflammatory foods into the diet may contribute to overall well-being and migraine prevention (10).

Self Quiz
Ask yourself...
- What benefits do biofeedback and relaxation techniques offer in reducing the frequency and intensity of migraines?
- How can biofeedback and relaxation techniques be integrated into a comprehensive migraine management plan?
- What role do dietary modifications and nutritional approaches play in the holistic management of migraines?
- How can healthcare professionals guide patients in identifying trigger foods and making informed nutritional choices?
Nursing Considerations
Nurses play a pivotal role in the holistic care of individuals with migraines, contributing to both the preventive and acute aspects of management through various considerations. Here are some important considerations.
Assessment and Patient Education
A thorough assessment includes evaluating the frequency, duration, and severity of migraines and identifying triggers and associated symptoms (3). Additionally, nurses play a key role in patient education, ensuring individuals clearly understand their migraine condition, the prescribed medications, and potential side effects. For instance, educating a patient about the importance of early intervention with acute medications during a migraine attack empowers them to take timely action.
Monitoring and Adverse Event Management
Nurses actively monitor individuals undergoing migraine treatment, monitoring the response to medications and any potential adverse events. Regular monitoring includes assessing the effectiveness of preventive measures, tracking the frequency of migraine attacks, and identifying patterns that may require adjustments in the treatment plan (34). If adverse events or side effects occur, nurses are instrumental in managing them promptly, collaborating with healthcare providers to ensure the safety and well-being of individuals.
Supportive Care and Holistic Approach
Nursing considerations extend beyond medication management to supportive care and a holistic approach. Nurses provide emotional support, helping individuals cope with the impact of migraines on their daily lives. Moreover, they collaborate with other healthcare professionals to integrate holistic approaches such as lifestyle modifications, stress management, and alternative therapies into the overall care plan. According to (34), this collaborative and patient-centered approach enhances the effectiveness of migraine management.
Documentation and Communication
Accurate and thorough documentation of relevant patient information, medication administration details, and responses to treatment is a fundamental nursing responsibility in migraine management (34). In addition to that, clear and concise communication between nursing staff, healthcare providers, and other healthcare team members ensures continuity of care (34).

Self Quiz
Ask yourself...
- How can a thorough patient assessment contribute to the safe and effective administration of migraine medications?
- How do nursing responsibilities extend beyond medication administration to encompass patient education?
- When monitoring individuals undergoing migraine treatment, what are the essential aspects that nurses should observe?
- How does the collaborative communication between nursing staff, healthcare providers, and other team members contribute to the continuity of care in migraine management?
Upcoming Research
Staying ahead of the curve is essential for healthcare professionals to provide cutting-edge care and optimize outcomes for individuals with migraines. Upcoming research include the following:
Advancements in Targeted Therapies
Recent research has unveiled promising advancements in targeted therapies for migraine management. For example, research about monoclonal antibodies targeting the calcitonin gene-related peptide (CGRP) pathway is proving to be effective in preventing migraines (12).
Digital Health and Telemedicine in Migraine Care
Integrating digital health technologies and telemedicine is a burgeoning trend in migraine management research. Smartphone applications for tracking migraine patterns, wearable devices for monitoring physiological parameters, and virtual consultations enable a more comprehensive and patient-centric approach (12). This shift toward digital solutions enhances data collection and facilitates remote monitoring and timely interventions, particularly in scenarios where in-person visits may be challenging (12).
Genetic and Personalized Medicine Approaches
Advancements in genetic research are paving the way for personalized medicine in migraine care. Understanding the genetic underpinnings of migraines can guide the development of targeted interventions tailored to an individual's unique genetic profile. This personalized approach could revolutionize treatment strategies, allowing for more precise and effective interventions based on the genetic factors contributing to a person's migraines (13).
Exploration of Lifestyle and Environmental Influences
Upcoming research increasingly focuses on the intricate interplay between lifestyle, environmental factors, and migraines; and studies examining the impact of factors such as diet, sleep patterns, and environmental triggers contribute valuable insights (13). For instance, research may reveal specific dietary components that act as triggers or protective factors for migraines, allowing healthcare professionals to offer targeted lifestyle recommendations.

Self Quiz
Ask yourself...
- What recent research findings have emerged regarding migraine prevention?
- How are digital health technologies and telemedicine being incorporated into upcoming research on migraine management?
- In personalized medicine, how is genetic research influencing upcoming approaches to migraine care?
- How can consideration of lifestyle factors and environmental influences contribute to a more holistic approach of migraine management?
Conclusion
In conclusion, this course focused on empowering learners not only with knowledge about migraine management, but with the practical insights and skills crucial for excellence in migraine care. The journey doesn’t end here; it extends into the realm of compassionate practice, where the combination of scientific understanding and safety measures transforms care providers into formidable advocates for those navigating the complexities of migraines.
Asthma Treatment and Monitoring
Introduction
When hearing the phrase asthma, what comes to mind? If you're an advanced practice registered nurse (APRN) with prescriptive authority, you've definitely heard of asthma before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and respiratory health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management and respiratory health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds, to learn more about medications that can treat and manage asthma.
Defining Asthma
What Is Asthma?
Asthma is a non-communicable chronic health condition that affects the airways of the lungs and affects millions of people nationwide. Asthma is often diagnosed in childhood and can resolve in adulthood or continue for the rest of a patient's life. Several studies postulate the cause of asthma, but there is no definitive cause.
Genetics, age, environmental exposures, smoking, and a history of allergies are thought to play a role in asthma severity and development. Clinical presentation of asthma often includes trouble breathing, chronic airway inflammation, and airway hyperresponsiveness. Assessment for asthma often includes patient history, clinical presentation, spirometry testing, and pulmonary function tests (PFTs).
What Are the Stages of Asthma?
Since asthma is a chronic condition, several established guidelines can be used to determine the severity of asthma and explore possible medication options. Depending on the stage of asthma and patient response to existing therapy, treatment and management vary.
The four stages of asthma include intermittent, mild, moderate, and severe. Based on the 2020 National Asthma Education and Prevention Program (NAEPP) guidelines, here is the standard criteria for what constitutes each stage of asthma (2).
Intermittent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness <2 times a week
- Asthmatic flare-ups are short-lived with varying intensity
- Symptoms at night are <2 a month
- No asthmatic symptoms between flare-ups
- Lung function test FEV 1 at >80% above normal values
- Peak flow has <20% variability am-to-am or am-to-pm, day-to-day
Mild persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness 3-6 times a week
- Asthmatic flare-ups may affect activity level and can vary in intensity
- Symptoms at night are 3-4 times a month
- Lung function test FEV1 is >80% above normal values
- Peak flow has less than 20-30% variability
Moderate persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness daily
- Asthmatic flare-ups may affect activity level and can vary in intensity
- Symptoms at night are >5 times a month
- Lung function test FEV1 is 60%-80% of normal values
- Peak flow has more than 30% variability
Severe persistent asthma is characterized with the following clinical presentation and assessment (2):
- Patient history of respiratory symptoms, such as cough, trouble breathing, wheezing, or chest tightness continuously
- Asthmatic flare-ups affect activity level and often vary in intensity
- Asthmatic symptoms at night are constant
- Lung function test FEV1 is <60% of normal values
- Peak flow has more than 30% variability
Based on patient history, clinical presentation, and these criteria, treatment can be administered to decrease the symptoms of the patient. If a patient presents with symptoms that are outside of your scope of work or understanding, you can always refer patients to a pulmonologist or asthma specialist.
Often times, more severe cases of asthma and asthma emergencies require increased frequency and dosing of asthma-related medications. Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history, pulmonary function, and health history prior to prescribing asthma medications (1).
What Are Asthmatic Emergencies?
Asthmatic emergencies are if a patient has asthma symptoms that are beyond what they typically experience and are unable to function without immediate medical intervention. Asthma emergencies can occur as a result of a patient being unable to access their asthmatic medications, being exposed to a possible allergen, or being under increased stress on the body.
Asthmatic emergencies often require collaborative medical intervention, increased dosages of medications discussed below, and patient education to prevent future asthmatic emergencies (1).
What If Asthma Is Left Untreated?
Depending on the clinical presentation and severity of asthma, asthma can cause several long-term complications if left untreated. If asthma is not properly managed, several complications, such as chronic obstructive pulmonary disease (COPD), decreased lung function, permanent changes to the lungs' airways, and death can occur (1, 2).
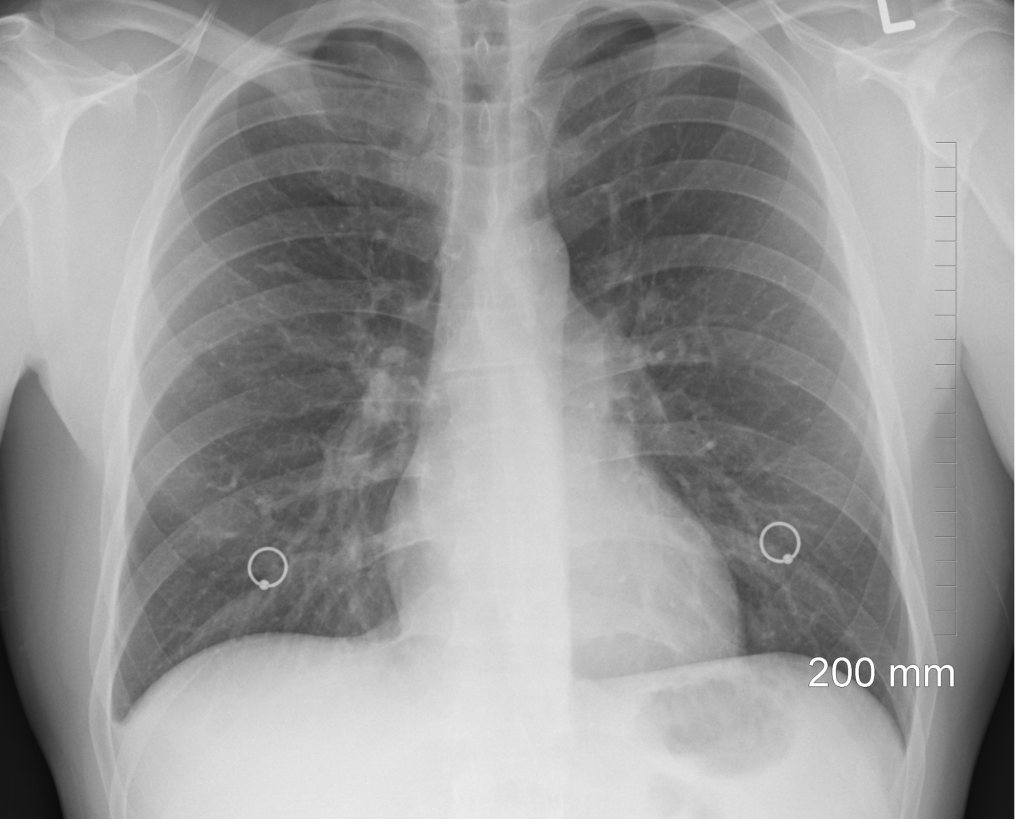
Defining Asthma Medications
What Are Commonly Used Medications to Manage Asthma?
Commonly used medications to manage asthma include inhaled corticosteroids, oral corticosteroids, short-acting beta agonists (SABAs), long-acting beta agonists (LABAs), long-acting muscarinic antagonists (LABAs), adenosine receptor antagonists, leukotriene modifiers, mast cell stabilizers, and monoclonal antibodies. The dosage, frequency, amount of asthma management medications, and medication administration route can all vary depending on clinical presentation, patient health history, and more.
How and Where are Asthma Medications Used?
Asthma medications can be used routinely or as needed for management of asthma symptoms depending on the patient. Asthma medications can be used at home, in public, and in health care facilities. Depending on the specific asthma medication and dosage, these medications can be taken by mouth, by an external device, such as an inhaler, via subcutaneous injection, or via intravenous solution (1).
What Are the Clinical Criteria for Prescribing Asthma Medication?
Clinical criteria for prescribing asthma medication can depend on the clinical presentation of a patient. Assessment of lung health and patient history are essential to determining the dosage and medications needed for adequate asthmatic symptom control.
Clinical guidelines from reputable organizations, such as the National Asthma Education and Prevention Program (NAEPP), the National Institutes of Health (NIH), the Global Initiative for Asthma (GINA), and the American Academy of Family Physicians (AAFP) can provide insight into the latest recommendations for asthma management (1, 2). In addition, local laws or health departments might have recommendations for asthma medication guidelines.
What Is the Average Cost for Asthma Medications?
Cost for asthma medications can significantly vary depending on the type of medication, insurance, dosage, frequency, medication administration route, and other factors. Cost is among a leading reason why many patients cannot maintain their medication regime (3). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost effective solutions for your patients.


Self Quiz
Ask yourself...
- What are some common signs of asthma?
- What are some common medications that can be prescribed to manage asthma?
- What are some factors that can influence asthma development and severity?
Inhaled Corticosteroids Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Inhaled Corticosteroids
Commercially available inhaled corticosteroids include: ciclesonide (Alvesco HFA), fluticasone propionate (Flovent Diskus, Flovent HFA, Armon Digihaler), budesonide (Pulmicort Flexhaler), beclomethasone dipropionate (QVAR RediHaler), fluticasone furoate (Arnuity Ellipta), and mometasone furoate (Asmanex HFA, Asmanex Twisthaler).
Clinical criteria for prescribing an inhaled corticosteroid includes adherence to the latest clinical guidelines, patient medical history, patient clinical presentation, and drug availability (4).
Inhaled Corticosteroids Method of Action
Inhaled corticosteroids have an intricate mechanism of action involving several responses to the immune system. Inhaled corticosteroids decrease the existing initial inflammatory response by decreasing the creation and slowing the release of inflammatory mediators. Common inflammatory mediators include histamine, cytokines, eicosanoids, and leukotrienes. Inhaled corticosteroids can also induce vasoconstrictive mechanisms, which, as a result, can lead to less blood flow, resulting in less discomfort and edema (4).
In addition to anti-inflammatory properties, inhaled corticosteroids can create a localized immunosuppressive state that limits the airways' hypersensitivity reaction, which is thought to reduce bronchospasms and other asthma-associated symptoms. It is important to note that inhaled corticosteroids often do not produce therapeutic effects immediately, as many patients may not see a change in their asthma symptoms for at least a week after beginning inhaled corticosteroid therapy (4).
Inhaled Corticosteroids Side Effects
Every medication has the possibility of side effects, and inhaled corticosteroids are no exception. Common side effects of inhaled corticosteroids include oral candidiasis (thrush), throat irritation, headache, and cough.
Patient education about rinsing their mouth and oral hygiene after use is essential to avoid the possibility of thrush and other oral infections and irritations. More severe side effects can include prolonged immunosuppression, reduction in bone density, and adrenal dysfunction (4).
Inhaled Corticosteroids Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with inhaled corticosteroids, so additional medication, increased dosage, a change in frequency, or a new medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of inhaled corticosteroids?
- What are some patient considerations to keep in mind when prescribing inhaled corticosteroids?
Oral Corticosteroids Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Oral Corticosteroids
Commercially available oral corticosteroids include methylprednisolone, prednisolone, and prednisone. Clinical criteria for prescribing an oral corticosteroid includes adherence to the latest clinical guidelines, patient medical history, patient clinical presentation, and drug availability (4).
Oral Corticosteroids Method of Action
Methylprednisolone and prednisolone have a method of action as intermediate, long-lasting, synthetic glucocorticoids, have COX-2 inhibitory properties, and inhibit the creation of inflammatory cytokines (5).
Prednisone is a prodrug to prednisolone and has anti-inflammatory and immunomodulating glucocorticoid properties. Prednisone has a method of decreasing inflammation by reversing increased capillary permeability and suppressing the movement of certain leukocytes (6).
Oral Corticosteroids Side Effects
Every medication has the possibility of side effects, and oral corticosteroids are no exception. Methylprednisolone and prednisolone have possible side effects of skin changes, weight gain, increased intraocular pressure, neuropsychiatric events, neutrophilia, immunocompromised state, fluid retention, and GI upset.
Consider monitoring symptoms and overall health of patients on systemic corticosteroids to assess for long-term side effects (5). Prednisone has possible side effects of changes in blood glucose, changes in sleep habits, changes in appetite, increased bone loss, an immunocompromised state, changes in adrenal function, and changes in blood pressure (6).
Oral Corticosteroids Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with oral corticosteroids, so additional medication, increased dosage, a change in frequency, or a new medication class might need to be considered (6).

Self Quiz
Ask yourself...
- What are some possible side effects of oral corticosteroids?
- What are some patient considerations to keep in mind when prescribing oral corticosteroids versus inhaled corticosteroids?
Short-Acting Beta Agonists (SABAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – SABAs
Common commercially available SABAs include albuterol sulfate (ProAir HFA, Proventil HFA, Ventolin HFA), albuterol sulfate inhalation powder (ProAir RespiClick, ProAir Digihaler), levalbuterol tartrate (Xopenex HFA), and levalbuterol hydrochloride (Xopenex) (4).
SABAs Method of Action
Short-acting beta-agonists (SABAs) have a rapid onset as broncho-dilating medications. SABAs, especially albuterol in emergent situations, are used often to quickly relax bronchial smooth muscle from the trachea to the bronchioles through action on the β2-receptors.
While SABAs are effective bronchodilators in the short term for asthma symptoms, SABAs do not affect the underlying mechanism of inflammation. As a result, SABAs are often used for short-acting intervals, such as few hours, and have limited capabilities to prevent asthma exacerbations alone (4). SABAs can be administered via meter-dosed inhalers, intravenous, dry powder inhalers, orally, subcutaneously, or via nebulizer.
SABAs Side Effects
Every medication has the possibility of side effects, and SABAs are no exception. Because of the beta receptor agonisms, possible SABA side effects include increased heart rate, chest pain, chest palpitations, body tremors, and nervousness (4). Because of the short half-life of SABAs, chronic side effects are not typically observed.
SABAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with SABAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of short-acting beta agonists?
- What are some patient considerations to keep in mind when prescribing SABAs?
Long-Acting Beta Agonists (LABAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – LABAs
Common commercially available LABAs are salmeterol and formoterol (7).
LABAs Method of Action
Long-acting beta-agonists (LABAs) have a rapid onset like SABAs, but also have a longer half-life. LABAs are used often as asthma maintenance medications to relax bronchial smooth muscle from the trachea to the bronchioles through action on the β2-receptors. While SABAs are effective bronchodilators in the short term for asthma symptoms, LABAs are effective bronchodilators in the long term for asthma symptoms.
Like SABAs, LABAs do not affect the underlying mechanism of inflammation. LABAs can be administered via meter-dosed inhalers, intravenous, dry powder inhalers, orally, subcutaneously, or via nebulizer. LABAs are often effective for 12-hour durations (7).
LABAs Side Effects
Every medication has the possibility of side effects, and LABAs are no exception. Like SABAs, because of the beta receptor agonisms, possible LABA side effects include increased heart rate, chest pain, chest palpitations, body tremors, and nervousness (7). Other more prolonged side effects can include changes in blood glucose levels and changes in potassium levels with prolonged LABA use (7).
LABAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with LABAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).
In addition, there are combination inhaled corticosteroid/LABA medications that can be considered, such as fluticasone propionate and salmeterol (Advair Diskus, Advair HFA, AirDuo Digihaler, AirDuo RespiClick, Wixela Inhub), fluticasone furoate and vilanterol (Breo Ellipta), mometasone furoate and formoterol fumarate dihydrate (Dulera), and budesonide and formoterol fumarate dihydrate (Symbicort) (4).

Self Quiz
Ask yourself...
- What are some possible side effects of LABAs?
- What are some patient considerations to keep in mind when prescribing SABAs compared to LABAs?
Long-Acting Muscarinic Antagonists (LAMAs)
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – LAMAs
Common commercially available LAMAs include two inhalation powders via inhalers known as tiotropium bromide (Spiriva Respimat) and fluticasone furoate, umeclidinium, and vilanterol (Trelegy Ellipta) (4).
LAMAs Method of Action
Both drugs mentioned above are long-acting muscarinic antagonists (LAMAs). LAMAs work to alleviate asthmatic symptoms by antagonizing the type 3 muscarinic receptors in bronchial smooth muscles, resulting in relaxation of muscles in the airway (4). Because LAMAs are long-acting, they are not recommended for cases of acute asthma exacerbations or asthmatic emergencies (4).
LAMAs Side Effects
Possible LAMA side effects include urinary retention, dry mouth, constipation, and glaucoma (4).
LAMAs Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with LAMAs, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of LAMAs?
- What are some patient considerations to keep in mind when prescribing LAMAs?
Adenosine Receptor Antagonists Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Adenosine Receptor Antagonists
The commercially available adenosine receptor antagonist for asthma management is theophylline as a pill or intravenous (8).
Adenosine Receptor Antagonists Method of Action
The method of action for theophylline is acting as a nonselective adenosine receptor antagonist, acting as a competitive, nonselective phosphodiesterase inhibitor, and reducing airway responsiveness to histamine, allergens, and methacholine (8).
Adenosine Receptor Antagonists Side Effects
Common side effects of theophylline include GI upset, headache, dizziness, irritability, and arrythmias (8).
Adenosine Receptor Antagonists Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with theophylline, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of adenosine receptor antagonists?
- What are some patient considerations to keep in mind when prescribing adenosine receptor antagonists?

Leukotriene Modifiers Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Leukotriene Modifiers
Commercially available leukotriene modifiers include montelukast (Singular) and zafirlukast (Accolate) as oral pills taken once a day. Zileuton (Zyflo CR) is a 5-lipoxygenase inhibitor that also modifies leukotriene activity (4).
Leukotriene Modifiers Method of Action
Montelukast and zafirlukast work to control asthma-related symptoms by targeting leukotrienes, which are eicosanoid inflammatory markers. Montelukast works in particular by blocking leukotriene D4 receptors in the lungs, thus allowing decreased inflammation in the lungs and increased relaxation of lung smooth muscle (9).
Zafirlukast works by being a competitive antagonist at the cysteinyl leukotriene-1 receptor (CYSLTR1) (10). Zileuton is a 5-lipoxygenase inhibitor, in which 5-lipoxygenase is needed for leukotriene creation. Blocking 5-lipoxygenase decreases the formation of leukotrienes at several receptors. As a result of decreased leukotriene production, there is decreased inflammation, decreased mucus secretion, decreased bronchoconstriction (11).
Leukotriene Modifiers Side Effects
Possible side effects of montelukast include headaches, GI upset, and upset. Neuropsychiatric events, such as nightmares, changes in sleep, depression, and suicidal ideation are more severe side effects associated with montelukast.
Possible side effects of zafirlukast include headache, GI upset, and hepatic dysfunction (9).
Possible side effects of zileuton include hepatic dysfunction, changes in sleep, changes in mood, headaches, and GI upset. When the leukotriene modifiers, neuropsychiatric side effects are to be monitored for in particular, especially for suicidal ideation (9,10,11).
Leukotriene Modifiers Alternatives
Some patients might not report their symptoms alleviating with leukotriene modifiers, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of leukotriene modifiers?
- What are some patient considerations to keep in mind when prescribing leukotriene modifiers?
Mast Cell Stabilizer Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Mast Cell Stabilizer
A commercially available mast cell stabilizer is cromolyn available via metered-dose inhaler and nebulizer solution (12).
Mast Cell Stabilizer Method of Action
Cromolyn has a method of action in which it inhibits the release of inflammatory mediators from cells, such as the release of histamine and leukotrienes (12).
Mast Cell Stabilizer Side Effects
Every medication has the possibility of side effects, and cromolyn is no exception. Common side effects of cromolyn include dry throat, throat irritation, drowsiness, dizziness, cough, headache, and GI upset (12).
Mast Cell Stabilizer Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with mast cell stabilizers, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of mast cell stabilizers?
- What are some patient considerations to keep in mind when prescribing mast cell stabilizers?
Monoclonal Antibody Pharmacokinetics
Health care provider professional discretion and patient condition should guide therapy. Consider reviewing a patient's medication history and health history prior to prescribing asthma medications.
Drug Class – Monoclonal Antibody
Commercially available monoclonal antibodies include Omalizumab (Xolair), mepolizumab (Nucala), reslizumab (Cinqair), benralizumab (Fasenra), dupilumab (Dupixent), and tezepelumab-ekko (Tezspire). Omalizumab, mepolizumab, benralizumab, dupilumab, and texepelumab-ekko are available via subcutaneous injection. Reslizumab is available via intravenous solution (4).
Monoclonal Antibody Method of Action
Omalizumab is an anti-IgE monoclonal antibody that works by inhibiting the binding of IgE to mast cells and basophils. As a result of decreased bound IgE, activation and release of mediators, such as histamine, in the allergic response are decreased (13).
Mepolizumab, reslizumab, and benralizumab are interleukin (IL)-5 antagonists. These IL-5 antagonists inhibit IL-5 signaling, allowing for a decrease in the creation and survival of eosinophils. However, the full method of action for IL-5 antagonists is still unknown, as more evidence-based research is needed (4, 15).
Dupilumab is an IgG4 antibody that inhibits IL-4 and IL-13 signaling by binding to the IL-4Rα subunit. This inhibition of the IL-4Rα subunit allows for the decrease of IL-4 and IL-13 cytokine-induced inflammatory responses (14).
Tezepelumab-ekko is an IgG antibody that binds to the thymic stromal lymphopoietin (TSLP) and prevents TSLP from interacting with the TSLP receptor. Blocking TSLP decreases biomarkers and cytokines associated with inflammation. Knowing this, the full method of action for Tezepelumab-ekko is still unknown, as more evidence-based research is needed4,15.
Monoclonal Antibody Side Effects
Possible side effects of omalizumab include injection site reactions, fracture, anaphylaxis, headache, and sore throat (13). Possible side effects of mepolizumab, reslizumab, and benralizumab include injection site reactions, headache, and hypersensitivity reactions (4). Possible side effects of dupilumab include joint aches, injection site reactions, and headache (14). Possible side effects of tezepelumab-ekko include injection site reactions and headache (14).
Monoclonal Antibody Alternatives
While there are clinical criteria for asthma medications, everyone can respond to medications differently. Some patients might not report their symptoms alleviating with monoclonal antibodies, so additional medication, increased dosage, a change in frequency, or an additional medication class might need to be considered (4).

Self Quiz
Ask yourself...
- What are some possible side effects of monoclonal antibodies?
- What are some patient considerations to keep in mind when prescribing monoclonal antibodies?
Nursing Considerations
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for the nurses' role in asthma education and management, here are some suggestions to provide quality care for patients currently taking medications to manage asthma or concerned about possibly having asthma.
- Take a detailed health history. Often times, respiratory symptoms, such as a cough or trouble breathing, are often dismissed in health care settings, or seen as "common symptoms with everyone." If a patient is complaining of symptoms that could be related to asthma, inquire more about that complaint.
Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. Millions of people take asthma medications at varying dosages, frequencies, and times of day. Many people with asthma take more than one medication to manage their symptoms.
Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Be willing to answer questions about asthma, respiratory health, and medication options. Society stigmatizes open discussions of prescription medication and can minimize symptoms of asthma, such as a chronic cough.
There are many people who do not know about medication options or the long-term effects of undiagnosed or poorly managed asthma. Be willing to be honest with yourself about your comfort level discussing topics and providing education on asthma medications and asthma clinical assessment options.
- Inquire about a patient's life outside of medications, such as their occupation, living situation, and smoking habits. Household exposures, such as carpets or pets, can trigger asthma. Occupations with high exposure to smoke can also trigger asthmatic symptoms. Smoking, living with someone who smokes, or residing in an area with high levels of pollution can also influence asthma symptoms.
Discuss possible solutions to help with symptoms, such as improving ventilation, increasing air quality, and mask wearing when possible.
- Communicate the care plan to other staff involved for continuity of care. For several patients, especially for patients with severe asthma, care often involves a team of nurses, specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to asthma medications, as evidence-based information is always evolving and changing. You can then present your new learnings and findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on asthma and asthma-related medications by following updates from evidence-based organizations.
How can nurses identify if someone has asthma?
Unfortunately, it is not always possible to look at someone with the naked eye and determine if they have asthma. While some people might have visible asthmatic symptoms, such as wheezing or trouble breathing, asthmatic clinical presentation can significantly vary from person to person.
APRNs can identify and diagnose if someone has asthma by taking a complete health history, listening to patient's concerns, and offering pulmonary function testing.
What should patients know about asthma medications?
Patients should know that anyone has the possibility of experiencing side effects medications for asthma management, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care.
Nurses should also teach patients to advocate for their own health in order to avoid untreated or undetected asthma and possible chronic complications from asthma or asthma-related medications.
Here are important tips for patient education in the inpatient or outpatient setting:
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors).
- Tell the health care provider of any existing lifestyle concerns, such as tobacco use, other drug use, sleeping habits, occupation, diet, menstrual cycle changes (need to identify lifestyle factors that can influence asthmatic medication use, asthma severity, and asthma management).
- Tell the health care provider if you have any changes in your breathing, such as pain with deep breathing or persistent coughing (potential asthma exacerbation symptoms or possibility of asthma medications not being as effective for treatment).
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life.
- Keep track of your health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes).
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for montelukast use).
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries.
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage asthma (potential worsening or improving health situation).

Self Quiz
Ask yourself...
- What are some problems that can occur if medications are not asthma properly?
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on asthma and air quality?
Research Findings
What Research on Asthma Medication Exists Presently?
There is extensive publicly available literature on asthma and asthma-related medications via the National Institutes of Health and other evidence-based journals (1,2,4).
What are some ways for people who take asthma medications to become a part of research?
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.

Self Quiz
Ask yourself...
- What are some reasons someone would want to enroll in clinical trials?
Conclusion
Asthma is a chronic condition that affects many people from their childhood to their aging years. As more medications for asthma come onto the market and more evidence-based approaches to asthma and lung care emerge, APRNs will be at the forefront of primary care and asthma care across the lifespan.
Case Study #1
Susie is a mom to a 15-year-old named Jill. She arrives at the pediatric asthma and allergy specialist practice for a new patient visit. Susie reports that she notices Jill is having trouble sleeping at night and coughing more during the day for the past month. Jill plays soccer with her school, but her mom is concerned about coughing and trouble sleeping interfering with her sports.
Susie knows that her dad has asthma, and Jill spends a lot of time with her aunt who smokes cigarettes. Jill has a history of generalized anxiety disorder and reports no smoking, no drinking, and no recreational drugs. Jill also wants to learn more about her lung health, as she wants to play soccer professionally one day.
- What are some specific questions you’d want to ask about Jill’s coughing and respiratory health?
- What are health history questions you would want to highlight?
- What are some tests or lab work would you suggest performing?

Case Study #2 (Continued)
Susie also shares that she is dating a new partner who vapes in the home, and they recently got a pet puppy in the home. She states that Jill had trouble sleeping at night and coughing a lot when she was younger, but Susie thought Jill grew out of it. Susie wants to learn more about if Jill has asthma like her grandfather, if there are any ways to manage this cough, and if there are any tests that can determine Jill’s lung health in the office today.
- What sort of tests can be done in-office to assess pulmonary function?
- What sort of environmental exposures can trigger respiratory conditions?
Susie agrees to have Jill do allergy testing and to do an in-office pulmonary function test for teenagers. Jill also wants to learn more about spirometry that you mentioned earlier and how to monitor her health outside of the office since she’s busy with school and soccer and doesn’t want to come to the office every time there’s a problem.
Susie is open to medication options for Jill but doesn’t want anything that will interfere too much with Jill’s social time with her friends. Susie and Jill also want to know if this is a health condition that Jill will have forever or if Jill will grow out of this.
- Knowing Susie’s concerns and Jill’s age, what are some talking points about reducing possible asthma triggers?
- How would you explain asthma as a chronic health condition to an adolescent patient?
- Given Jill and Susie’s concerns about medications, what would be some possible medication options to consider after reviewing Jill’s pulmonary function test results and patient history?
SSRI Use in Major Depressive Disorder
Introduction
When hearing the phrase selective serotonin reuptake inhibitors, what comes to mind? If you're an advanced practice registered nurse (APRN) with prescriptive authority, you've heard of SSRIs before. Even as a nurse or maybe before nursing school, conversations about prescription drug use and mental health existed every so often.
Presently, patients seek guidance and information on various health topics from APRNs, including medication management, women's health, and mental health. The information in this course will serve as a valuable resource for APRNs with prescriptive authority of all specialties, education levels, and backgrounds to learn more about SSRIs and major depressive disorder (MDD).
Defining SSRIs
What Are SSRIs?
Selective serotonin reuptake inhibitors, known as SSRIs, are a type of pharmacological drug class. SSRIs have existed for the past several decades as a class of prescription medications that can manage major depressive disorder (MDD) and other mental health conditions (1).
While this course focuses explicitly on SSRI use in MDD management, SSRIs are also Food and Drug Administration (FDA) approved to manage obsessive-compulsive disorder (OCD), panic disorder (PD), post-traumatic stress disorder (PTSD), and social anxiety disorder (SAD). In addition, several off-label uses for SSRI include management for binge eating disorder and menopausal vasomotor symptoms.
How and Where Are SSRIs Used?
SSRIs are commonly prescribed to manage MDD and other mood disorders in the U.S. and around the world in pediatric, adult, and geriatric populations (1, 2). SSRIs can be taken by mouth as a pill, capsule, or liquid oral solution. Presently, SSRIs cannot be offered via intravenous, rectal, buccal, or injection routes.
What Is the Clinical Criteria for Prescribing SSRIs?
Clinical criteria for prescribing SSRIs can vary depending on the intention for the SSRI. In the case of MDD, several factors can play a role in the clinical criteria for prescribing SSRIs. A patient's adherence to swallowing a pill daily, dosage given the patient's weight, medical history, and MDD concerns, and prior experience with other medications can influence prescribing SSRIs. When considering prescribing SSRIs for MDD management, consider assessing the patient for MDD first, taking a detailed health history, and discussing the risk versus benefits of starting SSRIs for this patient (1, 3).
What Is the Average Cost for SSRIs?
Cost for SSRIs can significantly vary depending on the type of SSRI, insurance, dosage, frequency, and other factors. Cost is among leading reasons why many patients cannot maintain their medication regime (4). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost-effective solutions for your patients.
What Is Major Depressive Disorder (MDD)?
Major depressive disorder (MDD) is a mental health condition in which a person has consistent appetite changes, sleep changes, psychomotor changes, decreased interest in activities, negative thoughts, suicidal thoughts, and depressed mood that interfere with a person's quality of life (5). According to the Diagnostic and Statistical Manual of Mental Health Disorders, a patient must have at least five persistent mood related symptoms, including depression or anhedonia (loss of interest in activities once enjoyed), that interferes with a person's quality of life to be formally diagnosed with MDD. Note that MDD does not include a history of manic episodes, and pediatric populations can present with more variable MDD symptoms (5). As an APRN, you can assess for MDD by doing a detailed patient health history or having a patient complete the Patient Health Questionnaire-9 (PHQ-9) - a depression assessment tool (5).


Self Quiz
Ask yourself...
- What are some medication administration options for SSRIs?
- What populations can be prescribed SSRIs?
SSRI Pharmacokinetics
Drug Class SSRIs
Selective serotonin reuptake inhibitors, known as SSRIs, are a type of pharmacological drug class part of the antidepressant drug class. They can be prescribed at various dosages depending on the patient history, severity of major depressive disorder (MDD), other medication use, and other factors based on patient-centered decision making. Currently, SSRIs that are FDA approved for MDD management include paroxetine, sertraline, citalopram, escitalopram, vilazodone, and fluoxetine. SSRIs can be prescribed for the oral route and are available via capsule, tablet, or liquid suspension/solution. SSRIs can be taken at any time of day. They can be taken with or without food, though vilazodone in particular is recommended with food. SSRIs are often prescribed to be taken once a day, sometimes twice a day, depending on the severity of MDD. Health care provider professional discretion and patient condition should guide therapy (1).
SSRIs are metabolized by and known to affect the cytochrome P450 system. CYP2D6 inhibitors include escitalopram, citalopram, sertraline, paroxetine, and fluoxetine. Fluoxetine and fluvoxamine are inhibitors of CYP2C19. Fluvoxamine is an inhibitor of CYP1A2. Consider reviewing a patient's medication history and health history prior to prescribing SSRIs (1).
SSRIs Method of Action
SSRI method of action has been subject to several studies, especially in the last few years. Serotonin is a neurotransmitter that plays a role in mood and other bodily functions. It can be measured in plasma, blood, urine, and CSF (6). It is important to note that serotonin is rapidly metabolized to 5-hydroxyindoleacetic acid (5-HIAA) (6). SSRIs work by inhibiting the reuptake of serotonin at certain chemical receptors, thereby increasing serotonin activity and concentration (1). SSRIs inhibit the serotonin transporter (SERT) at the presynaptic axon terminal.
By obstructing the SERT, a higher amount of serotonin (5-hydroxytryptamine or 5HT) remains in synaptic clefts. This higher amount of serotonin can then stimulate postsynaptic receptors for a more extended period (1). While SSRIs can increase serotonin activity, there is some evidence that suggests the possibility of long-term SSRI use reducing serotonin concentration (6). In addition, the clinical response to SSRIs in patients with MDD can take anywhere from a few to several weeks to emerge (7). While some research suggests that there are initial improvements in mood, evidence remains inconclusive as to the exact time SSRIs can take to provide a therapeutic response for patients (7). Also, while research suggests that SSRIs can increase serotonin levels, there is still mixed evidence on the exact method of action for SSRIs (7).
As a result, it is important to counsel patients that SSRIs can take a few weeks to provide a therapeutic response and to monitor mood and symptoms while taking SSRIs.
SSRI Side Effects
Every medication has the possibility of side effects, and SSRIs are no exception. Fortunately, SSRIs are known to have less side effects than other drug classes of antidepressants, such as monoamine oxidase inhibitors (MAOIs) or tricyclic antidepressants (TCAs). The most commonly known side effects of SSRIs include weight gain, sleep changes, headache, gastrointestinal issues, drowsiness, orthostatic hypotension, and sexual function changes (1).
Sleep changes can include an increased desire to sleep, increase in the amount of time sleeping, or insomnia. Gastrointestinal issues can include an upset stomach, nausea, or dry mouth. Mood changes, such as anxiety, are possible side effects as well. Sexual function changes can include erectile dysfunction, libido changes, impaired orgasmic response, and vaginal dryness (1, 8).
There are more serious possible side effects of SSRIs as well. For instance, SSRIs have the possible side effect of QT prolongation, which if left untreated or undiagnosed, can lead to fatal cardiac arrythmias (1, 8). In particular, the SSRI citalopram has been shown to have more of a risk for QT prolongation compared to other SSRIs. Also, like any other medication that can possibly increase levels of serotonin in the body, there is a possibility of serotonin syndrome as a complication of SSRI use. Possible serotonin syndrome clinical manifestations include increased blood pressure, increased sweating, increased reflex ability, and increased dry eyes (8). Due to the wide varied range of side effects, patient counseling, monitoring, and education is essential when prescribing SSRIs.
SSRI Black Box Warning
In 2004, the FDA issued a black box warning for SSRIs and other antidepressant medications due to the possible increased risk of suicidality in pediatric and young adult populations (up to age 25). When considering SSRI use in patients under 25 and knowing MDD is a risk factor for suicidality, having a conversation with the patient about risks versus benefits must be considered. However, in the past several years since the FDA's warning, there is no clear evidence showing a correlation between SSRIs and the increased risk of suicidality (1, 8). Health care provider professional discretion and patient condition should guide therapy.
SSRI Alternatives
MDD can be a complex, chronic condition to manage with varying clinical presentation and influence on a patient's quality of life. There are several alternatives to SSRI use, such as: (1, 9)
- Other prescription drugs
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Commonly known SNRIs include milnacipran, venlafaxine, desvenlafaxine, duloxetine, and levomilnacipran.
- Atypical antidepressants. Commonly known atypical antidepressants include bupropion and mirtazapine.
- Tricyclic antidepressants (TCAs). Commonly known TCAs include amitriptyline, desipramine, imipramine, clomipramine, doxepin, and nortriptyline.
- Monoamine oxidase inhibitors (MAOIs). Commonly known MAOIs include phenelzine, tranylcypromine, isocarboxazid, and selegiline.
- Psychotherapy, such as cognitive behavioral therapy (CBT) or interpersonal therapy
- Electroconvulsive therapy (ECT)
- Vagus Nerve Stimulation (VNS)
- Transcranial Magnetic Stimulation (TMS)

Self Quiz
Ask yourself...
- What are some possible side effects of SSRIs?
- What are some pharmacological alternatives to SSRIs?
Nursing Considerations
Nurse’s Role
What Is the Nurses' Role in SSRI Patient Education and Management?
Nurses remain the most trusted profession for a reason, and APRNs are often pillars of patient care in several health care settings. Patients turn to nurses for guidance, education, and support. While there is no specific guideline for the nurses' role in SSRI education and management, here are some suggestions to provide quality care for patients interested in or currently taking SSRIs to manage current or suspected major depressive disorder (MDD).
- Take a detailed health history. Often times, mental health symptoms, such as depressive thoughts or anxiety, are often dismissed in health care settings, even in mental health settings. If a patient is complaining of symptoms that could be related to major depressive disorder, inquire more about that complaint. Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other health care professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Often times, in busy clinical settings, reviewing health records can be overwhelming. While a vast number of people take SSRIs, many are no longer benefiting from the medication. Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history.
- Ask about family history. If someone is complaining of symptoms that could be related to MDD, ask if anyone in their immediate family, such as their parent or sibling, experienced similar conditions.
- Be willing to answer questions about mental health and SSRIs. Society can often stigmatize open discussions of prescription medication and mental health. SSRIs are no exception. There are many people who do not know about the benefits and risks of SSRIs, the long-term effects of unmanaged MDD, or possible treatment options. Be willing to be honest with yourself about your comfort level discussing topics and providing education on SSRIs and MDD.
- Communicate the care plan to other staff involved for continuity of care. For several patients, MDD management often involves a team of mental health professionals, nurses, primary care specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to SSRIs and mental health conditions, as evidence-based information is always evolving and changing. You can then present your new findings to other health care professionals and educate your patients with the latest information. You can learn more about the latest research on SSRIs and mental health by following updates from evidence-based organizations.
Identifying Major Depressive Disorder
How can nurses identify if someone has major depressive disorder?
Unfortunately, it is not possible to look at someone with the naked eye and determine if they have MDD. APRNs can identify and diagnose if someone has MDD by taking a complete health history, listening to patient's concerns, having patients complete the PHQ-9 questionnaire and communicating any concerns to other health care professionals (9).
Patient Education
What should patients know about SSRIs?
Patients should know that anyone has the possibility of experiencing side effects of SSRIs, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care. Due to social stigma associated with mental health and SSRI use, people may be hesitant to seek medical care for fear of being dismissed by health care professionals (1, 6). In addition, side effects (that interfere with the quality of life) are often normalized (1, 6). However, as more research and social movements discuss mental health and SSRI use more openly, there is more space and awareness for SSRI use and mental health.
Nurses should also teach patients to advocate for their own health in order to avoid progression of MDD and possible unwanted side effects of SSRIs. Here are important tips for patient education in the inpatient or outpatient setting.
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors)
- Tell the health care provider of any existing lifestyle concerns, such as alcohol use, other drug use, sleeping habits, diet, menstrual cycle changes (need to identify lifestyle factors that can influence SSRI use and MDD)
- Tell the health care provider if you notice any changes in your mood, behavior, sleep, sexual health (including vaginal dryness or erectile dysfunction), or weight (possible changes that could hint at more chronic side effects of SSRIs)
- Tell the health care provider if you have any changes in urinary or bowel habits, such as increased or decreased urination or defecation (potential risk for SSRI malabsorption or possible unwanted side effects)
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your mental health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for SSRI use)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage your MDD (potential worsening or improving mental health situation)


Self Quiz
Ask yourself...
- What are some possible ways you can obtain a detailed, patient centric health history?
- What are some possible ways APRNs can educate patients on SSRIs and major depressive disorder?
Research Findings
What Research on SSRIs exists presently?
There is extensive publicly available literature on SSRIs via the National Institutes of Health and other evidence-based journals.
What are some ways for people who take SSRIs to become a part of research?
If a patient is interested in participating in clinical trial research, they can seek more information on clinical trials from local universities and health care organizations.

Self Quiz
Ask yourself...
- What are some problems that can occur if SSRIs are not managing major depressive disorder symptoms adequately?
- What are some reasons someone might want to enroll in SSRI clinical trials?
Case Study
Case Study Part 1
Susan is a 22-year-old Black woman working as a teacher. She arrives for her annual exam at the local health department next to her place of work. She reports nothing new in her health, but she says she's been feeling more tired over the past few months. Susan reports having some trouble sleeping and trouble eating but doesn't feel too stressed overall. She heard one of her friends talking about SSRIs and wants to try them, but she's never taken prescription medications long-term before. She also thinks she might have some depression because she looked at some forums online and resonated with a lot of people's comments.

Self Quiz
Ask yourself...
- What are some specific questions you'd want to ask about her mental health?
- What are some health history questions you'd want to highlight?
- What lab work would you suggest performing?
Case Study Part 2
Susan agrees to complete bloodwork later this week and thinks she might have a family history of depression. She said that no one in her family talks about mental health, but she heard about depression from her friends recently and family a long time ago. She's back in the office a few weeks later, and her labs are within normal limits. Susan states she's still feeling fatigued and feeling a bit more hopeless these days. She denies thinking about hurting herself or others.

Self Quiz
Ask yourself...
- How would you discuss Susan's mental health concerns?
- How would you explain to Susan the influence of lifestyle, such as sleep, diet, and environment, on mood?
Case Study Part 3
Susan completed the PHQ-9 questionnaire and had a high score. After discussing her responses with her, you diagnose her with MDD. Susan admits that she is open to trying SSRIs. She is also open to seeing a therapist, as she states that she's never been to therapy. She would like resources on any therapy services, medication options, and non-pharmacological options to help her manage her condition.

Self Quiz
Ask yourself...
- Knowing Susan's concerns, what are some possible non-pharmacological management options for her MDD?
- What are some major SSRI side effects to educate Susan on?
Antibiotic Use for UTI
Introduction
A urinary tract infection (UTI) can develop in anyone but is more common in females than males. Approximately 40% of American women will develop a urinary tract infection in their lives [2]. Many UTIs can lead to serious health complications, including sepsis and sometimes patient mortality.
Thus, healthcare providers must be knowledgeable of the signs and symptoms of UTIs, the available antibiotics, and UTI treatment guidelines. Understanding the different pharmacokinetics of antibiotics used to treat UTIs is essential during drug selection. This course outlines UTI antibiotic pharmacology and addresses pharmacokinetics, including mechanism of action, side effects, usage, and contraindications.
Definitions
This section covers the definitions related to UTI treatment and management.
Urinary Tract Infection
Bacterial infection of the lower urinary tract (usually confined to the bladder). This is also sometimes called cystitis and is primarily caused by the bacteria E. coli [2].
Asymptomatic Bacteremia
A urine specimen is collected on a patient and shows the presence of bacteria, but they do not have any UTI symptoms [5].
Pyelonephritis
Bacterial infection of the upper urinary tract (i.e. kidneys) [6].
Urosepsis
When a urinary tract infection causes a systemic infection, also known as sepsis [6].

Self Quiz
Ask yourself...
- What is a urinary tract infection?
- What is asymptomatic bacteremia?
- What is pyelonephritis?
- What is urosepsis?
Medications Overview
This section briefly reviews UTI antibiotic classes and medical indications.
Certain antibiotics are used to prevent or treat urinary tract infections and are used in both inpatient and outpatient settings. Healthcare providers should follow current guidelines regarding UTI treatment, which depends on the patient and type of urinary tract infection. UTI treatment algorithms are further divided into:
- Uncomplicated UTIs
- Complicated UTIs
- Prophylactic treatment for recurrent UTIs [6]
What constitutes uncomplicated UTIs are patients who have urinary symptoms, but do not have signs of systemic infections, like fever, flank pain, costovertebral angle (CVA) tenderness, etc. Patients can be male or female, unlike previous guidelines that categorized all males as complicated UTIs. Also, patients with uncomplicated UTIs usually have no underlying health conditions or risk factors that may affect treatment [6].
Conversely, complicated UTIs occur when patients have systemic symptoms. Patients who are pregnant, have a history of UTIs, or who are considered elderly also fall under complicated UTIs. Patients with pyelonephritis are automatically considered as having complicated UTIs as well. Patients with recurrent UTIs may be prescribed certain low-dose antibiotics for prevention [6].
Regardless of the UTI type, below are some of the common antibiotics prescribed:
- Trimethoprim-sulfamethoxazole
- Nitrofurantoin
- Fluoroquinolones
- Ciprofloxacin
- Levofloxacin
- Beta-lactams
- Cephalexin
- Amoxicillin-clavulanate
- Ceftriaxone
- Cefdinir
- Piperacillin-tazobactam
- Meropenem
- Fosfomycin
- Pivmecillinam


Self Quiz
Ask yourself...
- What are some factors that classify an uncomplicated UTI?
- What are some factors that classify a complicated UTI?
- What are the different names and types of antibiotics used to treat UTI?
Pharmacokinetics
This section discusses the pharmacokinetics of each antibiotic medication used to treat UTIs.
Trimethoprim-sulfamethoxazole
Sulfonamides, also called sulfa drugs, are a class of medications commonly used to treat bacterial infections, including UTIs. A common sulfonamide medication used to treat UTIs is sulfamethoxazole formulated with trimethoprim which is sometimes abbreviated as TMP-SMX, TMP-sulfa, or TMP-SMZ [22]. Trimethoprim-sulfamethoxazole is also approved by the Federal Drug Administration (FDA) to treat chronic bronchitis exacerbations, otitis media in children, and shigellosis.
This medication is also used for prevention and treatment of traveler’s diarrhea, toxoplasmosis, and Pneumocystis jirovecci and Pneumocystis carinii pneumonia. Some other off-label or non-FDA-approved uses are tuberculosis, malaria, listeria, pertussis, and community-acquired pneumonia [10].
Since this a combination medication, TMP-SMX works by two different mechanisms of action. Trimethoprim competes with the enzyme dihydrofolate reductase and subsequently stops the production of tetrahydrofolate from converting to folate.
Sulfamethoxazole, a CYP2CP inhibitor, competes with p-aminobenzoic acid during dihydrofolate synthesis. These two medications combined work against folate production and block bacterial biosynthesis of nucleic acids and proteins. Both medications are metabolized by the liver [10].
TMP-SMX is available via oral and intravenous (IV) forms. Adult TMP-SMX oral dosages are typically 160mg/800mg for the treatment of UTI, respectively, and dosages for children under 40 kilograms are weight-based. This medicaiton is best absorbed orally when taken with at least eight ounces of water. Intravenous TMP-SMX is given to hospitalized patients and dosages will vary. Some common side effects of trimethoprim-sulfamethoxazole include:
- Nausea and/or vomiting
- Rash and photosensitivity
- Dizziness
- Fatigue
- Loss of appetite and anorexia [10]
As this medication’s mechanism of action interferes with folate production, folate deficiency is also common. More severe side effects may include Stevens-Johnson syndrome, anemia, and Clostridioides difficile (C. diff) diarrhea. This medication should not be prescribed to patients with a sulfa allergy since it can cause anaphylaxis [10].
Before prescribing this medication, healthcare providers should also be aware of the precautions and contraindications. Healthcare providers should be cautious when prescribing this medication to patients with decreased kidney function, as it can lead to toxicity and high potassium levels. Therefore, baseline and frequent monitoring of blood urea nitrogen (BUN), creatinine, and potassium levels are helpful.
Other contraindications include patients with liver failure, hematological disorders, or who are pregnant. TMP-SMX interferes with several medications, including phenytoin, digoxin, diuretics, and rifampin. Many of these medication interactions increase the risk for potential hyperkalemia, medication toxicity, and QT prolongation [10].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of trimethoprim-sulfamethoxazole?
- What are the common side effects of trimethoprim-sulfamethoxazole?
- What are some contraindications of trimethoprim-sulfamethoxazole?
Nitrofurantoin
Nitrofurantoin is another antibiotic commonly prescribed to treat urinary tract infections. This medication has been FDA-approved since 1953 to treat and prevent lower UTIs and is commonly considered a first-line treatment. Currently, nitrofurantoin has no other approved or off-label uses. It comes in two different forms, which are monohydrate and macrocrystalline [16].
The mechanism of action for nitrofurantoin is not completely understood. However, it is thought to be absorbed by bacterial flavoproteins in the gastrointestinal tract and then further prevents bacterial enzymes from synthesizing DNA, RNA, and cell wall proteins [16].
Nitrofurantoin is only available via the oral route. The dosage is usually 100 mg twice daily for UTI treatment and for UTI prophylaxis is 50mg to 100mg once daily. Common medication side effects include:
- Nausea and/or vomiting
- Diarrhea
- Loss of appetite [16]
Severe reactions, although rare, are pulmonary toxicity where patients may present with fever, chills, cough, and dyspnea. It may also cause liver toxicity, liver failure, and peripheral neuropathy. This medication is contraindicated in patients with a creatinine clearance of less than 60 mL/minute, hemolysis, or who have glucose-6-phosphate dehydrogenase (G6PD) deficiency [16].
Healthcare providers should also be aware of considerations when prescribing nitrofurantoin. They must understand that nitrofurantoin should not be prescribed to patients with suspected or confirmed pyelonephritis, since it is only used to treat lower UTIs.
Nitrofurantoin should not be prescribed to people who are pregnant, especially between 38 to 42 weeks gestation, and neonates. It is also not recommended to give to patients who are 65 years or older due to increased potential adverse effects. For patients who take nitrofurantoin long-term for prophylactic use, liver function tests should be routinely completed and monitoring of pulmonary function [16].


Self Quiz
Ask yourself...
- What is the pharmacokinetics of nitrofurantoin?
- What are the common side effects of nitrofurantoin?
- What are some contraindications of nitrofurantoin?
Fluoroquinolones
Fluoroquinolones are a class of antibiotics used to treat UTIs and other bacterial conditions. Examples of common fluoroquinolones include ciprofloxacin, moxifloxacin, and levofloxacin. However, ciprofloxacin is more commonly used to treat UTIs than the others and therefore, will be the medication reviewed in this section [19].
In addition to urinary tract infections, ciprofloxacin is FDA-approved to treat various health conditions. Some common health conditions treated are gonorrhea, chancroids, joint infections, prostatitis, and some gastrointestinal infections. Ophthalmic forms are used to treat corneal ulcers and conjunctivitis, while otic forms may be used in otitis externa [17].
Ciprofloxacin’s mechanism of action is considered bactericidal since it works by inhibiting bacterial DNA replication. It acts against DNA topoisomerase and DNA gyrase to hinder DNA replication. Ciprofloxacin is most effective against gram-negative bacteria, but also some gram-positive bacteria. Due to mutations in the DNA gyrase, ciprofloxacin and other fluoroquinolones have begun to show bacterial resistance over the past several years [17].
Ciprofloxacin comes in many forms, including oral, IV, ophthalmic, and otic. For the treatment of UTI, this medication is available via oral and IV forms. Recommended dosages are dependent on the severity of UTI and route. Oral dosages for UTI treatment range from 250mg to 500mg twice daily, while IV dosages can range from 200mg to 400mg twice daily to upwards of 400mg every eight hours. Regardless of the administration route, common side effects are nausea and diarrhea. Some serious adverse effects include:
- QT prolongation
- Hypoglycemia
- Hyperglycemia
- Photosensitivity [17]
Ciprofloxacin has an FDA black box warning of tendinitis and tendon rupture, peripheral neuropathy, and myasthenia gravis exacerbation. Due to the effects this medication has on tendons, Achilles tendon rupture, aortic aneurysm, and aortic dissection are also serious adverse effects. If the healthcare provider suspects any adverse effects, including mild tendonitis, the medication should be discontinued immediately.
Furthermore, when prescribing ciprofloxacin, there are additional considerations and contraindications. As with all medications, ciprofloxacin should not be prescribed to patients with a known allergy to this medication.
Ciprofloxacin should not be prescribed along with tizanidine, theophylline, or cyclosporine due to interactions. Antacids can also interfere with the absorption of ciprofloxacin and ciprofloxacin toxicity is more likely in older adults. Healthcare providers should encourage patients with diabetes to closely monitor their blood glucose levels at home since this medication can cause hypo- or hyperglycemia [17].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of ciprofloxacin?
- What are the common side effects of ciprofloxacin?
- What are some contraindications of ciprofloxacin?
- What is the black box warning of ciprofloxacin?
Beta-lactams
Beta-lactams are a class of antibiotics used to treat various bacterial conditions, including UTIs. The three main beta-lactams covered below are those commonly used to treat UTI and include cephalexin, amoxicillin-clavulanate, and ceftriaxone. Other beta-lactams that are approved for UTI treatment are cefpodoxime, cefdinir, and cefadroxil, and work similarly to others in this medication family.
Cephalexin
Cephalexin is a beta-lactam antibiotic that is classified as a first-generation cephalosporin. It was initially approved by the FDA in 1970 and is widely used throughout healthcare settings. In addition to acute and chronic UTIs, cephalexin is approved to treat upper and lower respiratory infections, bone infections, and otitis media. It is also used to treat surgical site, skin, and soft tissue infections [8].
Cephalexin falls under the beta-lactam class since its structure has a beta-lactam ring. This ring inhibits the synthesis of peptidoglycan which further disrupts the bacterial cell wall. More specifically, the beta-lactam ring binds to the penicillin-binding proteins during peptidoglycan synthesis, causing the disruption of the bacterial cell wall and viability [8].
Cephalexin is only available via oral route and can be prescribed in tablet, capsule, and suspension forms. Daily dosages from 1000mg to 4000mg for adults and for children, are weight-based and range from 25mg to 100mg per kilogram per day. Some side effects of cephalexin include:
- Abdominal pain
- Diarrhea
- Nausea and/or vomiting
- Rash
- Candidiasis [8]
Other reactions may include increased liver enzymes, C. diff colitis, and hemolytic anemia. Although cross-reactivity with penicillin is somewhat uncommon, healthcare providers should use caution when prescribing this medication to patients who are allergic to penicillin. Furthermore, it should not be prescribed to patients with a cephalosporin allergy. Cephalexin also interacts with metformin, causing decreased clearance of metformin from the body.
If a patient is taking metformin, they should be advised to closely monitor their blood glucose levels since the risk for hypoglycemia is increased. Healthcare providers should also be cautious when prescribing this medication to patients who are taking probenecid. Cephalexin can also increase prothrombin time, which typically requires monitoring, especially for those undergoing anticoagulant treatment [8].


Self Quiz
Ask yourself...
- What is the pharmacokinetics of cephalexin?
- What are the common side effects of cephalexin?
- What are some contraindications of cephalexin?
Amoxicillin-clavulanate
As its name implies, amoxicillin-clavulanate is a combination medication of amoxicillin and clavulanic acid. In addition to treating UTIs, this medication is FDA-approved to treat rhinosinusitis, acute otitis media, skin infections, and aspiration and community-acquired pneumonia. Other non FDA-approved uses are impetigo, chronic obstructive pulmonary disease exacerbations, diabetic foot infections, and human and animal bites [4].
Amoxicillin-clavulanate works via two different mechanisms of action since it is a combination medication. The amoxicillin component is a beta-lactam antibiotic and works via the same mechanism as cephalexin described above. Clavulanic acid is a beta-lactamase inhibitor, which prevents bacteria from destroying beta-lactam antibiotics. Thus, the reason why clavulanic acid is often combined with amoxicillin [4].
This medication is only available via oral forms, such as suspensions, chewable, immediate-release, or extended-release tablets. Dosages are dependent on the underlying condition being treated, medication form (i.e. immediate- versus extended-release), and the patient’s age. Regardless of dosage, amoxicillin-clavulanate can lead to common gastrointestinal side effects, such as:
- Diarrhea
- Nausea
- Vomiting
- Loose stools [4]
Vaginal candidiasis is another common side effect of amoxicillin-clavulanate. For patients who are breastfeeding, this medication may cause hypersensitivity reactions in infants since it is excreted in breast milk. Additionally, amoxicillin-clavulanate has several drug interactions with medications, including probenecid, oral anticoagulants, allopurinol, and oral contraceptives. For patients on hemodialysis or with severe renal impairment, usually where their creatinine clearance is less than 30 mL/min, dose adjustments are recommended.
Healthcare providers should monitor patients’ liver enzymes for possible hepatic impairment, and if hepatic injury occurs, stop the medication immediately and follow treatment recommendations accordingly. Since amoxicillin is a penicillin derivative, it should not be prescribed to individuals with a penicillin allergy [4].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of amoxicillin-clavulanate?
- What are the common side effects of amoxicillin-clavulanate?
- What are some contraindications of amoxicillin-clavulanate?
Ceftriaxone
Ceftriaxone is another beta-lactam antibiotic used to treat UTIs and is usually an adjunct medication. It is a third-generation cephalosporin that is also used to treat gonorrhea, pelvic inflammatory disease, meningitis, and certain abdominal, respiratory, and joint infections. Additionally, ceftriaxone treats bacteremia, sepsis, and infective endocarditis. Since ceftriaxone belongs to the beta-lactam class, its mechanism of action is the same as previously described cephalexin [18].
Ceftriaxone comes in both intravenous and intramuscular (IM) forms since it is not absorbed through the gastrointestinal tract. For UTI treatment, the dosage for adults is 1 to 2 grams IV or IM every 24 hours. In an outpatient setting, ceftriaxone is often given as a single IM dose to patients with pyelonephritis who are not hospitalized. Again, this medication is used as an adjunct medication, so it is given as a single IM dose, followed by another oral antibiotic for UTI treatment. Dosages for children range from 50mg to 75mg per kilogram per day for both IM and IV forms [18]. Some common side effects of ceftriaxone are:
- Diarrhea
- Nausea
- Vomiting
- Dysgeusia (metallic or foul taste in the mouth)
- Injection site reaction, especially for IM [18]
Other adverse effects associated with ceftriaxone are hemolytic anemias, neutropenia, and thrombocytosis. It should also be noted that this medication can cause neurological symptoms, cholelithiasis, jaundice, elevated liver enzymes, and pancreatitis [18].
Healthcare providers should also review ceftriaxone’s precautions and contraindications. This medication is cross-reactive with penicillin and can cause a hypersensitivity reaction. Furthermore, it should not be prescribed to patients with a cephalosporin allergy. If ceftriaxone is administered through an IV, it must not be mixed with calcium-containing IV solutions or products. Other possible medication interactions are estradiol, cyclosporine, and bumetanide. For patients with liver or kidney impairment, dosages must be adjusted and should not exceed 2 grams per day [18].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of ceftriaxone?
- What are the common side effects of ceftriaxone?
- What are some contraindications of ceftriaxone?
Cefdinir
Cefdinir is another beta-lactam antibiotic used to treat UTIs and is also a third-generation cephalosporin. In addition to UTI treatment, cefdinir is approved for the treatment of pneumonia, bacterial infections involving the skin, and respiratory infections of the ears, throat, and sinuses. As cefdinir is a third-generation cephalosporin, its mechanism of action is the same as previously described ceftriaxone. Thus, it interferes with bacterial cell wall synthesis [13].
Cefdinir is only available via oral route by either capsule or liquid suspension. Treatment dosages and duration are dependent on the underlying condition it is being used to treat [13]. For UTI, this medication is usually prescribed at 300mg twice daily for 5 to 7 days. However, this course may be extended for patients with pyelonephritis or complicated UTIs. Some common side effects of this medication include:
- Nausea and vomiting
- Diarrhea
- Vaginal itching
- Red-tinged stools [13]
Other more serious side effects may include rash, hives, facial swelling, and difficulty breathing or swallowing. As with all medications, healthcare providers should be aware of this medication’s precautions and contraindications. Cefdinir should not be prescribed to patients with a cephalosporin allergy or who are taking probenecid. It should also be avoided in patients with gastrointestinal diseases, like colitis, and kidney disease. This medication should be taken at least two hours apart from any aluminum, magnesium, or iron supplement. Additionally, healthcare providers should avoid prescribing the oral suspension form to patients with diabetes, since it contains high amounts of sucrose and can potentially raise blood sugar levels [13].


Self Quiz
Ask yourself...
- What is the pharmacokinetics of cefdinir?
- What are the common side effects of cefdinir?
- What are some contraindications of cefdinir?
Other Antibiotics Used to Treat UTI
This section reviews other antibiotics used to treat urinary tract infections. Two common additional antibiotics administered in an inpatient setting include piperacillin-tazobactam and antipseudomonal carbapenems, such as imipenem or meropenem. These are usually reserved for patients with at least one risk factor for multidrug-resistant gram-negative organisms [7]. Drug information about meropenem will be discussed in greater detail below. Other less common antibiotics available in the outpatient are fosfomycin and pivmecillinam. Although these medicatios are used less commonly, it is still important to understand their pharmacokinetics.
Piperacillin-tazobactam
As mentioned, piperacillin-tazobactam is used to treat multidrug-resistant gram-negative UTIs in an inpatient setting. In addition to treating UTIs, it is approved for the treatment of skin, gynecological, and certain abdominal infections. This medication is a combination of piperacillin (a penicillin antibiotic) and tazobactam (a beta-lactamase inhibitor). Therefore, its mechanism of action is that of both the penicillin and beta-lactam classes as previously described [15].
Piperacillin-tazobactam is available in IV form and the dosage is usually 3.375 grams every six hours [7]. Like many antibiotics, some common side effects include:
- Diarrhea
- Nausea and/or vomiting
- Stomach pain [15]
This medication can also cause mouth sores, sleeping difficulties, and in more severe cases, itching, difficulty swallowing, and wheezing. Piperacillin-tazobactam should not be prescribed to patients who are taking other penicillin or beta-lactam antibiotics or who have an allergy. It interferes with certain medications including, aminoglycosides, anticoagulants, methotrexate, and vancomycin. Additionally, for patients with diabetes, this medication can cause false results with certain glucose tests [15].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of piperacillin-tazobactam?
- What are common side effects of piperacillin-tazobactam?
- What are some contraindications of piperacillin-tazobactam?
Meropenem
An antipseudomonal carbapenem, meropenem, is used to treat inpatient multidrug-resistant gram-negative UTIs. Meropenem is also approved for the treatment of pneumonia, intra-abdominal infections, peritonitis, and meningitis [21].
This medication’s mechanism of action is similar to beta-lactams, as it falls under the same family of antibiotics. It binds to penicillin-binding proteins and inhibits bacterial cell wall synthesis by inhibiting peptidoglycan [21].
Meropenem is only available in IV form and dosages are dependent on the condition being treated. For UTIs, 1 gram is administered every 8 hours. Gastrointestinal side effects are common for this medication and include symptoms like diarrhea, nausea, vomiting, and constipation. Additional adverse effects may include:
- Drowsiness
- Headache
- Insomnia
- Depression [21]
Seizures are also a potential adverse effect, and therefore, healthcare providers must monitor patients for neurological symptoms. Agranulocytosis, thrombocytopenia, gastrointestinal bleeding, and hemolytic anemia are other conditions which have been reported when taking this medication. For patients with renal impairment, the dosage will need to be adjusted. Meropenem also has many medication interactions, with some major ones including afatinib, atogepant, cariprazine, and colchicine [21].

Self Quiz
Ask yourself...
- What is the pharmacokinetics of meropenem?
- What are the common side effects of meropenem?
- What are some contraindications of meropenem?
Fosfomycin
Fosfomycin is an antibiotic that is FDA-approved to treat uncomplicated urinary tract infections and is considered a first-line treatment option. In the United States, fosfomycin is only available in oral, powder which is mixed and dissolved in liquid. Furthermore, although this medication is a first-line UTI treatment option, it is not widely available in the United States [20].
This medication’s mechanism of action works by interfering with the formation of peptidoglycan precursor UDP N-acetylmuramic acid, also known as UDP-MurNAc. As it acts one step prior to the beta-lactam antibiotic family, Fosfomycin enters the bacteria through the transporter systems L-alpha-glycerophosphate and hexose-6-phosphate. This medication also reduces the ability of bacteria to adhere to the epithelial cells of the urinary tract [9].
To treat UTI, a single dose of 3 grams of fosfomycin is given, which is added to about 3 to 4 ounces of cold water to dissolve the medication. Common side effects may include:
- Nausea
- Diarrhea
- Headache
- Back pain [14]
Other serious side effects are joint pain, rash, facial or oral swelling, and jaundice. Healthcare providers should review this medication’s interactions and contraindications. Fosfomycin interacts with medications like cisapride, metoclopramide, and certain vitamins. Healthcare providers should use caution when prescribing to patients with a history of asthma, liver disease, or who are pregnant or breastfeeding [14].

Self Quiz
Ask yourself...
- What is the mechanism of action for fosfomycin?
- What are some common side effects of fosfomycin?
- What are some contraindications of fosfomycin?
Pivmecillinam
Pivmecillinam is another antibiotic used to treat lower urinary tract infections and is part of the UTI treatment algorithm. However, the FDA has not approved this medication for use in the United States [11]. Therefore, most of the specific drug information is not available.

Considerations for Prescribers
This section reviews potential considerations when prescribing antibiotics for UTIs.
Healthcare providers must consider and review several factors when prescribing antibiotics for UTI treatment. First, the medication’s route, dosage, and treatment duration are usually determined by the setting (inpatient versus outpatient), the type of UTI (e.g. empirical, asymptomatic bacteremia, uncomplicated, complicated, or prophylaxis), and the patient’s underlying medical conditions and risk factors. Furthermore, healthcare providers should strive to follow current treatment guidelines, approved uses, and their organization’s protocols when initiating or adjusting these medications. Healthcare providers must review the patient’s medical history, recent lab values, contraindications, and potential side effects.
Patient Population
Certain classes of antibiotics should be avoided in specific individuals or patient populations, and thus, healthcare providers must be aware of these precautions, contraindications, and black box warnings. Ciprofloxacin can lead to medication toxicity and hypoglycemia in older adults and must be avoided in this patient population when able [17]. Additionally, prescribing medications, such as TMP-SMZ and cephalexin, should be cautioned in patients with renal impairment [8, 10]. Prescribing nitrofurantoin, TMP-SMZ, cephalexin, and ceftriaxone should be cautioned in patients with liver failure or elevated liver enzymes. Healthcare providers should routinely monitor the patient’s liver enzymes and function tests [8, 10, 16, 18].
The patient’s gender at birth plays another large factor in antibiotic selection since treatment for males is considered a complicated UTI and antibiotic duration is extended. Furthermore, in patients who are pregnant or breastfeeding, certain antibiotics should not be prescribed, with some including TMP-SMZ and fluoroquinolones. Alternative treatments for patients who are pregnant are amoxicillin-clavulanate or [6]. For patients with chronic UTIs, initial prophylactic treatment should be started for 3 months and then reevaluated thereafter for prevention. Typical low-dose prophylactic antibiotics are TMP-SMX and nitrofurantoin. However, the healthcare provider should strongly consider medication compliance and potential antibiotic resistance [1].
Allergies
Healthcare providers should also review the patient’s allergies and cross-reactivity of certain antibiotics. Trimethoprim-sulfamethoxazole should not be prescribed to individuals with a sulfa allergy. Furthermore, healthcare providers should not prescribe patients with a penicillin allergy amoxicillin-clavulanate and should use caution when prescribing these individuals beta-lactams or cephalosporins due to their potential cross-reactivity, although the percentage is low [8, 10].
Medication History
As discussed, certain antibiotics interact with specific medications. Healthcare providers must review the patient’s medication list prior to prescribing antibiotics. For instance, amoxicillin-clavulanate interacts with allopurinol and lessens the effectiveness of oral contraceptives. Patients on oral contraceptives should be instructed to use backup birth control methods while on the antibiotic [4]. Additionally, while interactions may exist medication timing plays an important role. For example, medications such as ciprofloxacin and TMP-SMZ interact with antacids. However, if the antibiotic is taken two hours before or six hours after the antacid, a potential medication interaction is less likely [17]. Cephalexin is better absorbed on an empty stomach while other antibiotics are recommended to be taken with food [8].
Bacterial Sensitivity
Some antibiotics do not treat certain strains of bacteria and thus, healthcare providers must be judicious about initial antibiotic selection and following up with the patient about their urine culture results. For example, bacterial growth on the urine culture might not be sensitive to the initial antibiotic prescribed and may be resistant. Therefore, the antibiotic may need to be changed or dual therapy may be needed.
Also, patients with recurrent UTIs sometimes develop antibiotic resistance to first-line medications for the treatment of UTI, so an alternative medication should be initially prescribed, and a urine culture sent. If the patient is treated frequently for UTIs, then a referral to urology is warranted for further evaluation [6]. In some patients, asymptomatic bacteremia is found on a routine urinalysis completed during an annual comprehensive exam. Healthcare providers should review the current screening and treatment guidelines on asymptomatic bacteria in adults. For most patients, a urine culture should be sent for further evaluation, and antibiotic administration delayed until the culture has resulted [5].
Patient Education
Patients should be instructed on potential medication side effects and signs of adverse reactions. In an outpatient setting, healthcare providers must instruct patients on worsening symptoms and when to seek immediate or emergent treatment. Oftentimes, urinary tract infections move upstream into the kidneys and cause pyelonephritis or urosepsis [6].

Self Quiz
Ask yourself...
- What factors should healthcare providers consider when prescribing antibiotics?
- Which antibiotic can be prescribed during pregnancy?
- Which steps should be taken for patients with recurrent UTIs?
- What health conditions and lab values are important when selecting UTI antibiotics?
Upcoming Research
This section reviews upcoming research and medications for UTI treatment.
The bacteria strain, E. coli, is typically responsible for urinary tract infections. However, this is not the case for all UTIs, and some patients have developed multiple drug-resistant organisms due to recurrent infections. Therefore, there is much research needed on UTI antibiotic treatment to eradicate these organisms. Recent development of immunomodulatory therapy has been considered as well as medications that inhibit bacterial adhesions to the epithelial cells of the urinary tract. Vaccinations against UTI have also shown recent promise, but further research is still needed [3]. Other non-antibiotic therapies are also being researched, like Lactobacillus-containing products (i.e. probiotics) and cranberry supplements [12].


Self Quiz
Ask yourself...
- Which bacteria commonly causes urinary tract infections?
- What new research is there about antibiotics for UTI treatment?
- Which types of new products are being researched about UTI treatment?
Conclusion
As discussed, antibiotic selection for the treatment of urinary tract infections depends on a variety of factors. Healthcare providers should understand the pharmacokinetics, potential side effects, interactions, and contraindications when selecting an antibiotic. They should also follow current clinical guidelines and their facility’s protocols for a more evidence-based approach. Furthermore, ordering a urine culture or referring a patient to a urologist is warranted for patients with recurrent urinary tract infections.

Self Quiz
Ask yourself...
Final Reflection Questions
- What differentiates a lower versus upper UTI?
- What are the different names of beta-lactam antibiotics used to treat UTIs?
- Which antibiotics are commonly prescribed for UTI prophylaxis?
- Which antibiotics are not commonly prescribed or available in the United States?
- Which antibiotics are commonly used to treat multi-drug resistant organisms?
- Which antibiotics can be used in outpatient versus inpatient settings?
- What are the two types of fluoroquinolones used to treat UTIs?
- What are some other antibiotics used to treat UTIs?
References + Disclaimer
- National Statistics. (n.d.). National Coalition Against Domestic Violence. Retrieved February 7, 2021, from https://ncadv.org
- Sharma, A., & Borha, S. (2020, July 28). Covid-19 and Domestic Violence: An Indirect Path to Social and Economic Crisis. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7386835/
- What is domestic abuse? (n.d.). Https://Www.Un.Org/En/Coronavirus/What-Is-Domestic-Abuse. Retrieved February 8, 2021, from https://www.un.org/en/coronavirus/what-is-domestic-abuse
- Centers for Disease Control and Prevention. (2020, October 9). Intimate Partner Violence. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/violenceprevention/intimatepartnerviolence
- Centers for Disease Control and Prevention. (2020a, March 9). Preventing Teen Dating Violence. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/injury/features/dating-violence
- National Coalition Against Domestic Violence (2020). Domestic violence. Retrieved from https://assets.speakcdn.com/assets/2497/domestic_violence-2020080709350855.pdf?1596811079991
- Yousefnia, N., Nekuei, N., & Farajzadegan, Z. (2018, July 10). Injury and Violence. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6101232/
- National Coalition Against Domestic Violence. (n.d.). Dynamics of Abuse. National Coalition Against Domestic Violence (NCADV). Retrieved February 9, 2021, from https://ncadv.org/dynamics-of-abuse
- Pereira, M., Azeredo, A., Moreira, D., Brandão, I., & Almeida, F. (2020, May). Personality characteristics of victims of intimate partner violence: A systematic review. Science Direct. https://www.sciencedirect.com/science/article/abs/pii/S1359178919302642
- Axelrod, J. (2016, May 17). Who Are the Victims of Domestic Violence? PsychCentral. https://psychcentral.com/lib/who-are-the-victims-of-domestic-violence#1
- National Coalition Against Domestic Violence. (n.d.-b). Signs of Abuse. Retrieved February 9, 2021, from https://ncadv.org/signs-of-abuse
- Domestic Shelters (2014, July 1). Profile of an Abuser. Domestic Shelters. https://www.domesticshelters.org/articles/identifying-abuse/profile-of-an-abuser
- Emergency Nurses Association. (2018). Intimate Partner Violence. Emergency Nurses Association (ENA). https://www.ena.org/docs/default-source/resource-library/practice-resources/position-statements/joint-statements/intimatepartnerviolence.pdf?sfvrsn=4cdd3d4d_8
- Bettencourt, E. (2019, October 4). Domestic Violence and How Nurses Can Help Victims. Diversity Nursing. http://blog.diversitynursing.com/blog/domestic-violence-and-how-nurses-can-help-victims
- Stanford Medicine. (2020). How to Ask. https://domesticabuse.stanford.edu/screening/how.html
- Power, C. (n.d.). Domestic Violence: What Can Nurses Do? Crisis Prevention Institute (CPI). Retrieved February 11, 2021, from https://www.crisisprevention.com/Blog/Domestic-Violence-What-Can-Nurses-Do
- Alshammari, K., McGarry, J., & Higginbottom, G. (2018, July 5). Nurse education and understanding related to domestic violence and abuse against women: An integrative review of the literature. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6056448/
- Fleishman, J., Kamsky, H., & Sundborg, S. (2019, May). Trauma-Informed Nursing Practice. The Online Journals of Issues in Nursing (OJIN). https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol-24-2019/No2-May-2019/Trauma-Informed-Nursing-Practice.html
- The United States Department of Justice. (n.d.). Domestic Violence. U.S. Department of Justice. Retrieved February 9, 2021, from https://www.justice.gov/ovw/domestic-violence
- Houseman, B., & Semien, G. (2020, October 17). Florida Domestic Violence. National Center for Biotechnology Information (NCBI). https://www.ncbi.nlm.nih.gov/books/NBK493194/
- Domestic Battery under Florida Law. (2019). Hussein and Webber, PL. http://www.husseinandwebber.com/crimes/violent-crimes/domestic-violence-battery/
- Rape, Abuse, and Incest National Network (RAINN). (n.d.). The laws in your state: Florida. Retrieved February 14, 2021, from https://apps.rainn.org/policy/?&_ga=2.161880060.1354221772.1613679799-1191886798.1613418373#report-generator
- Safe Horizon. (n.d.). Safety Plan for Domestic Violence Survivors. Retrieved February 9, 2021, from https://www.safehorizon.org/our-services/safety-plan/?gclid=Cj0KCQiApY6BBhCsARIsAOI_GjYsM6rkXLswOpzipsjGADI_JOewgRMdKX39WcUjaB14uFcYieLmM5saAmFREALw_wcB
- National Domestic Violence Hotline. (n.d.). Create a safety plan. Retrieved February 12, 2021, from https://www.thehotline.org/create-a-safety-plan/
- Evans, M. L., Lindauer, M., & Farrell, M. E. (2020). A Pandemic within a Pandemic — Intimate Partner Violence during Covid-19. New England Journal of Medicine, 383(24), 2302–2304. https://doi.org/10.1056/nejmp2024046
- Wallace, A. (2020, November 4). 11 Things to Know About Domestic Violence During COVID-19 and Beyond. Healthline. https://www.healthline.com/health/things-to-know-about-domestic-violence
- Xue, J., Chen, J., Chen, C., Hu, R., & Zhu, T. (2020). The Hidden Pandemic of Family Violence During COVID-19: Unsupervised Learning of Tweets. Journal of Medical Internet Research, 22(11), e24361. https://doi.org/10.2196/24361
- Arts, E. J., & Hazuda, D. J. (2012). HIV-1 antiretroviral drug therapy. Cold Spring Harbor perspectives in medicine, 2(4), a007161. https://doi.org/10.1101/cshperspect.a007161
- Hartog, J., & Robinson, G. (2013, August). Florida’s Omnibus Act: A brief legal guide for healthcare professionals. Retrieved February 25, 2021, from http://www.floridahealth.gov/diseases-and-conditions/aids/administration/_documents/Omnibus-booklet-update-2013.pdf
- Hartog, J., & Robinson, G. (2013, August). Florida’s Omnibus Act: A brief legal guide for healthcare professionals. Retrieved February 25, 2021, from http://www.floridahealth.gov/diseases-and-conditions/aids/administration/_documents/Omnibus-booklet-update-2013.pdf
- Centers for Disease Control. (2016). Today’s HIV/AIDS epidemic. Retrieved from: https://www.cdc.gov/nchhstp/newsroom/docs/factsheets/todaysepidemic-508.pdf
- Centers for Disease Control. (2020). Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV. Retrieved from: https://www.cdc.gov/hiv/pdf/risk/art/cdc-hiv-art-viral-suppression.pdf
- Centers for Disease Control. (2020). HIV. Retrieved from: https://www.cdc.gov/hiv/basics/whatishiv.html
- HIV.gov. (2020). US statistics. Retrieved from: https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
- Nursing Times. (2020). HIV: epidemiology, pathophysiology, and transmission. Retrieved from: https://www.nursingtimes.net/clinical-archive/immunology/hiv-1-epidemiology-pathophysiology-and-transmission-15-06-2020/
- Intervention Project for Nurses. (2024). About. Intervention Project for Nurses. https://www.ipnfl.org/about/
- National Council of State Boards of Nursing. (2024). Participating jurisdictions. NURSECOMPACT. https://www.nursecompact.com/
- The Florida Senate. (2023a). Chapter 394, section 455. Www.flsenate.gov. https://www.flsenate.gov/Laws/Statutes/2023/394.455
- The Florida Senate. (2023b). Chapter 456. Www.flsenate.gov. https://www.flsenate.gov/Laws/Statutes/2023/Chapter456/All
- The Florida Senate. (2023c). Chapter 464. Www.flsenate.gov. https://www.flsenate.gov/Laws/Statutes/2023/Chapter464/PART_I
- Ahmed, Z., Saada, M., Jones, A. M., & Al-Hamid, A. M. (2019, 05 22). Medical errors: Healthcare professional’s perspective at a tertiary hospital in Kuwait. PLoS ONE, 14(5), 1-14. doi: 10.1371/journal.pone.0217023
- AHRQ. (2020, 11 01). 20 Tips to Help Prevent Medical Errors: Patient Fact Sheet. Retrieved from AHRQ Agency for Healthcare Research and Quality: https://www.ahrq.gov/questions/resources/20-tips.html
- CDC. (2017, 10 11). Medication Safety Program. Retrieved from cdc.gov: cdc.gov/medicationsafety/adult_adversedrugevents.html
- CMS. (2020, 11 19). Hospital CAHPS (HCAHPS). Retrieved from CMS.gov: https:www.cms.gov/Research-Statistics-Data-and-Systems/Research/CAHPS/HCAHPS1
- Federico, F. (2021). Improvement Stories. Retrieved from ihi.org: https://www.ihi.org/resources/Pages/ImprovementStories/FiveRightsofMedicationAdministration.aspx
- MRMC. (2018). Community Health Needs Assessment 2018. Mission, TX. Retrieved from https://missionrmc.org/documents/Mission-Regional-Medical-Center-2018-CHNA.Final-Draft.pdf
- Reducing Medication Errors Associated with At-risk Behaviors by Healthcare Professionals. (2014, 8 30). Retrieved from NCCMERP: https://www.nccmerp.org/reducing-medication-errors-associated-risk-behaviors-healthcare-professionals
- Senek, M., Robertson, S., Ryan, T., King, r., Wood, E., & Tod, A. (2020, 7 10). The association between care left undone and temporary Nursing staff ratios in acute settings: a cross-sectional survey of registered nurses. BMC Health services Research, 20(1), 1-8. doi:10.1186/s12913-020-05493-y
- Sutcliffe, K. (2019, 11 25). How to Reduce Medical Errors. TIME Magazine, 194(22/23), 25-26.
- The 2020 Florida Statutes. (2020). Retrieved from www.leg.stste.fl.us/Statutes/index.cfm?App_mode=Display_Statute&Search_String=&URL=0300-399/0395/Sections/0395.0197.html
- TJC. (2017, 09 12). Inadequate handoff communication. Sentinel Event Alert (58), 1-5.
- TJC. (2020, 08 01). Official “Do Not Use” List. Retrieved from jointcommission.org: https://www.jointcommission.org/-/media/tjc/documents/fact-sheets/do-not-use-list-8-3-20.pdf?db=web&hash=2489CB1616A30CFFBDAAD1FB3F8021A5
- TJC. (2021). 2021 Hospital National Patient Safety Goals. Retrieved from www.jointcommission.org: https://www.jointcommission.org/-/media/tjc/documents/standards/national-patient-safety-goals/2021/simplified-2021-hap-npsg-goals-final-11420.pdf
- Trossman, S. (2016, May/June). ANA calls for a culture of safety in all health care settings. American Nurse, 48(3), 3.
- American Association of Nurse Anesthetists. (n.d.). Addressing Substance Use Disorder for Anesthesia Professionals. Retrieved February 01, 2021, from https://cms.aana.com/docs/default-source/practice-aana-com-web-documents-(all)/professional-practice-manual/addressing-substance-use-disorder-for-anesthesia-professionals.pdf?sfvrsn=ff0049b1_4
- Washington Health Professional Services. (2016, March). A Guide for Assisting Colleagues Who Demonstrate Impairment in the Workplace. Retrieved February 03, 2021, from https://www.doh.wa.gov/portals/1/Documents/Pubs/600006.pdf
- Toney-Butler TJ, Siela D. Recognizing Alcohol and Drug Impairment in the Workplace in Florida. [Updated 2020 Dec 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507774/
- Employer Information. (n.d.). Retrieved February 03, 2021, from https://www.ipnfl.org/employer-information/#sec1
- https://polarisproject.org
- https://humantraffickinghotline.org/en/statistics/florida#year-2021
- https://www.dhs.gov/blue-campaign/what-human-trafficking
- United Nations Office on Drugs and Crime. (2022). Global report on trafficking in persons, 2022. New York, NY: United Nations. Retrieved from https://www.unodc.org/documents/data-and-analysis/glotip/2022/GLOTiP_2022_web.pdf
- https://www.justice.gov/humantrafficking/what-is-human-trafficking
- https://www.cdc.gov/violenceprevention/sexualviolence/trafficking.html
- https://polarisproject.org/2019-us-national-human-trafficking-hotline-statistics/
- https://polarisproject.org/wp-content/uploads/2019/09/LGBTQ-Sex-Trafficking.pdf
- Hachey, L., & Phillippi, J. (2017). Identification and management of human trafficking victims in the emergency department. Advanced Emergency Nursing Journal, 39(1), 31–51.doi: 10.1097/TME.0000000000000138
- English, A. (2017). Mandatory Reporting of Human Trafficking: Potential Benefits and Risks of Harm. AMA Journal of Ethics. https://journalofethics.ama-assn.org/article/mandatory-reporting-human-trafficking-potential-benefits-and-risks-harm/2017-01
- https://humantraffickinghotline.org/what-human-trafficking/federal-law
- Update: Identifying human trafficking patients alert. Patient Safety Monitor Journal. 2018;19(9):6. Accessed October 31, 2020. http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=131246408&site=eds-live
- Identifying Victims of Human Trafficking: What to Look for in a Healthcare Setting. Journal of Legal Nurse Consulting. 2020;31(3):30-33. Accessed October 31, 2020. http://search.ebscohost.com/login.aspx?direct=true&db=ccm&AN=145452392&site=eds-live
- https://www.state.gov/identify-and-assist-a-trafficking-victim/
- National Human Trafficking Hotline. Comprehensive human trafficking assessment tool. Retrieved from https://humantraffickinghotline.org/sites/default/files/Comprehensive%20Trafficking%20Assessment.pdf
- https://www.hhs.gov/guidance/sites/default/files/hhs-guidance-documents//fact_sheet_human_trafficking_fy18.pdf
- Dowell, D, et al. (2022). CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022. MMWR, 71(3):1-95. Retrieved from https://www.cdc.gov/mmwr/volumes/71/rr/rr7103a1.htm
- Bhatnagar, P. (2022, September 12). Opioid Equivalency. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK535402/
- Puntillo, K., & Naidu, R. K. (2018). Measurement of Chronic Pain and Opioid Use Evaluation in Community-Based Persons with Serious Illnesses. Journal of palliative medicine, 21(S2), S43–S51. https://doi.org/10.1089/jpm.2017.0457
- Grewal, N. and Heucker, M. R. (2023). Opioid Prescribing. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551720/
- US Department of Health and Human Services (HHS). (2020, Jan. 1). Opioid Oral Morphine Milligram Equivalent (MME) Conversion Factors table for prescription drug coverage. Retrieved from https://www.hhs.gov/guidance/document/opioid-oral-morphine-milligram-equivalent-mme-conversion-factors-0
- Geyer, D. H. (2023, January 17). A brief history of morphine use. Retrieved from Mayo Clinic Press: https://mcpress.mayoclinic.org/opioids/history-of-morphine/#:~:text=1803%3A%20Morphine%20is%20discovered&text=After%20conducting%20several%20years%20of,because%20it%20made%20people%20sleepy.
- Preuss, et al. (2023, April 29). Prescription of Controlled Substances: Benefits and Risks. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537318/
- Center for Disease Control. (2019, August 13). Prescribing Practices. Retrieved from CDC: https://www.cdc.gov/drugoverdose/deaths/prescription/practices.html
- Dydyk, A.M, et al. (2024, Jan. 17). Opioid Use Disorder. StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK553166/
- Center for Disease Control. (2021, May 19). PDMPS: What States Need to Know. Retrieved from CDC Drug Overdose: https://www.cdc.gov/drugoverdose/pdmp/index.html
- DrFirst. (n.d.). State Mandates Driving EPCS and PDMP Utilization. Retrieved from DrFirst: https://drfirst.com/resources/regulatory-mandates/
- Centers for Medicare and Medicaid Services. (2023). E-Prescribing Standards and Requirements. Retrieved from https://www.cms.gov/medicare/regulations-guidance/electronic-prescribing/adopted-standard-and-transactions
- SAMHSA. (n.d.). Talking with Your Teen About Opioids. Retrieved from Substance Abuse and Mendal Health Services Administration: https://www.samhsa.gov/sites/default/files/TTHY-Opioid-Broch-2020.pdf
- Food and Drug Administration. (2020, October 1). Safe Disposal of Medications. Retrieved from FDA: https://www.fda.gov/drugs/safe-disposal-medicines/disposal-unused-medicines-what-you-should-know
- National Institute on Drug Abuse. (2023, August 7). Only 1 in 5 US adults with opioid use disorder received medications to treat it in 2021. Retrieved from National Institutes of Health: https://nida.nih.gov/news-events/news-releases/2023/08/only-1-in-5-us-adults-with-opioid-use-disorder-received-medications-to-treat-it-in-2021
- Katie Kerwin McCrimmon, Uch. (2023, May 15). What is Mounjaro? and does it work better for weight loss than Ozempic and Wegovy?. UCHealth Today. https://www.uchealth.org/today/what-is-mounjaro-and-how-does-it-work-for-weight-loss/
- National Institutes of Health. (2023, July 28). DailyMed – mounjaro- tirzepatide injection, solution. U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d2d7da5d-ad07-4228-955f-cf7e355c8cc0
- Type 2 Diabetes Treatment to Lower A1C | Mounjaro® (tirzepatide). (2023). https://www.mounjaro.com/?utm_id=go_cmp-16966473997_adg-133042365262_ad-626584063672_kwd-1651326559888_dev-c_ext-_prd-_mca-_sig-EAIaIQobChMIxcXZqYeHgQMVhDjUAR2Lvw5CEAAYASAAEgIMkfD_BwE&utm_source=google&utm_medium=ppc&campaign=16966473997&adgroup=133042365262&ad=626584063672&utm_keyword=kwd-1651326559888&gclid=EAIaIQobChMIxcXZqYeHgQMVhDjUAR2Lvw5CEAAYASAAEgIMkfD_BwE
- GoodRX – error. (2023, July 14). https://www.goodrx.com/mounjaro/how-make-you-feel
- Chen, S. (2023, July 28). Diabetes drug Mounjaro shown to have extraordinary weight loss for people without diabetes. diaTribe. https://diatribe.org/diabetes-drug-mounjaro-shown-have-extraordinary-weight-loss-people-without-diabetes
- VA Pharmacy Benefits Management Services. (2022, August). Tirzepatide Injection Criteria for Use. https://www.va.gov/formularyadvisor/DOC_PDF/CFU_Tirzepatide_MOUNJARO_Criteria_Aug_2022.pdf.
- Allied PR. (2023 B.C.E., May 6). Mounjaro Weight Loss: Newly Launch Over The Counter Alternative Pills To Tirzepatide & Mounjaro Weight Loss. https://newsdirect.com/news/mounjaro-weight-loss-newly-launch-over-the-counter-alternative-pills-to-tirzepatide-and-mounjaro-weight-loss-300908569. Retrieved August 30, 2023, from https://newsdirect.com/news/mounjaro-weight-loss-newly-launch-over-the-counter-alternative-pills-to-tirzepatide-and-mounjaro-weight-loss-300908569
- Mounjaro (2023). Savings and support for Mounjaro. Retrieved on August 31st 2023 from https://www.mounjaro.com/savings-resources?gclid=Cj0KCQjw9MCnBhCYARIsAB1WQVWAcINPKFwiHl4SbZQiGC8E_o9wHVOkDJDDUuphW3OlsKBagVTF1rQaApLJEALw_wcB
- Global diabetes cases to soar from 529 million to 1.3 billion by 2050. (n.d.). The Institute for Health Metrics and Evaluation. https://www.healthdata.org/news-events/newsroom/news-releases/global-diabetes-cases-soar-529-million-13-billion-2050.
- Diabetes Research Institute Foundation. (2023, March 31). Diabetes Statistics – DRIF. DRIF. https://diabetesresearch.org/diabetes-statistics/#:~:text=37.3%20million%20people%2C%20or%2011.3,yet%20been%20diagnosed%20(2022)
- Manage blood sugar. (2021, April 28). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/managing/manage-blood-sugar.html
- About the National Diabetes Prevention Program | CDC. (n.d.). https://www.cdc.gov/diabetes/prevention/about.htm#:~:text=The%20National%20Diabetes%20Prevention%20Program%E2%80%94or%20National%20DPP%E2%80%94was%20created,diabetes%20in%20
- Ms, M. G. R. (2023, February 16). All about Ozempic. Healthline. https://www.healthline.com/health/drugs/ozempic#_noHeaderPrefixedContent
- Professional, C. C. M. (n.d.). Ghrelin. Cleveland Clinic. https://my.clevelandclinic.org/health/body/22804-ghrelin#:~:text=Ghrelin%20and%20leptin%20are%20two,brain%20when%20you’re%20hungry
- Prelipcean, M., MD. (2020, June 22). Behind the counter: Glucagon-like peptide-1 receptor agonists for type 2 diabetes. https://www.medicalnewstoday.com/articles/glp-1-receptor-agonists-type-2-diabetes
- Mba, A. B. P. (2023, May 1). Ozempic side effects: What you should know. https://www.medicalnewstoday.com/articles/drugs-ozempic-side-effects
- Delong, C. (2023, February 11). Black box warning. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538521/
- MNT Medical Network. (2023, February 16). Ozempic (semaglutide). https://www.medicalnewstoday.com/articles/326252
- Ozempic® vs. Other Type 2 Diabetes Treatments | Ozempic® (semaglutide) injection 0.5 mg or 1 mg. (n.d.). https://www.ozempic.com/why-ozempic/diabetes-medicines-comparison.html
- Northrop, A. (2023, August 3). Ozempic For Weight Loss: Side Effects, Risks And More. Forbes Health. https://www.forbes.com/health/body/ozempic-for-weight-loss/%20)
- Kerwin McCrimmon, UCHealth, K. (2023, April 5). Wegovy vs. Ozempic: The truth about new ‘weight-loss’ drugs. Uchealth. https://www.uchealth.org/today/wegovy-vs-ozempic-the-truth-about-new-weight-loss-drugs/#:~:text=If%20you%20take%20Wegovy%20or,to%20keep%20benefiting%20from%20them
- Stott, R. (2023, August 4). Lawsuit claims Ozempic, Mounjaro labels ‘downplayed severity’ of gastroparesis. Healio Gastroenterology. Retrieved August 11, 2023, from https://www.healio.com/news/gastroenterology/20230804/lawsuit-claims-ozempic-mounjaro-labels-downplayed-severity-of-gastroparesis#:~:text=While%20the%20drug%20label%20for,not%20recommended%20in%20these%20patients.%E2%80%9D
- How Does Gastroparesis Affect People with Diabetes? (2022, August 30). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/professionals/diabetes-discoveries-practice/how-gastroparesis-affect-people-with-diabetes
- Living Healthy with Diabetes. (2023, March 29). www.heart.org. https://www.heart.org/en/health-topics/diabetes/prevention–treatment-of-diabetes/living-healthy-with-diabetes
- Move more; sit less. (2023, June 22). Centers for Disease Control and Prevention. https://www.cdc.gov/physicalactivity/basics/adults/index.htm#:~:text=Each%20week%20adults%20need%20150,Physical%20Activity%20Guidelines%20for%20Americans.&text=We%20know%20150%20minutes%20of,do%20it%20all%20at%20once
- Good sleep habits. (2022, September 13). Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/about_sleep/sleep_hygiene.html
- Centers for Disease Control and Prevention. (2022, August 1). Food and nutrition insecurity and diabetes. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes-and-food-insecurity.htm
- American Psychiatric Association. (2020, December). What is a substance use disorder? https://www.psychiatry.org/patients-families/addiction-substance-use-disorders/what-is-a-substance-use-disorder
- Durrani M, Bansal K. Methadone. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562216/
- Kumar R, Viswanath O, Saadabadi A. Buprenorphine. [Updated 2023 Apr 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459126/
- National Center for Drug Abuse Statistics. (2023). Drug abuse statistics. https://drugabusestatistics.org/
- National Institute of Health. (2018, June). Understanding drug use and addiction. https://nida.nih.gov/publications/drugfacts/understanding-drug-use-addiction
- Singh D, Saadabadi A. Naltrexone. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534811/
- Substance Abuse and Mental Health Services Administration. (2023, August). Methadone take-home flexibilities extension guidance. https://www.samhsa.gov/medications-substance-use-disorders/statutes-regulations-guidelines/methadone-guidance#:~:text=In%20treatment%200%2D14%20days,be%20provided%20to%20the%20patient
- S. Food and Drug Administration. (2023, May). Information about medication assisted treatment (MAT). https://www.fda.gov/drugs/information-drug-class/information-about-medication-assisted-treatment-mat
- Akbari, P., Khorasani-Zadeh, A. (Updated 2023, January 23). Thiazide Diuretics. In Stat Pearls. Stat Pearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532918/
- Alley, W.D., & Schick, M.A. (Updated 2023, July 24). Hypertensive Emergency. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470371/
- American Heart Association. (2023 June 7). Types of Blood Pressure Medications. Retrieved from https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Arumugham, V.B., & Shahin, M.H. (Updated 2023, May 29). Therapeutic Uses of Diuretic Agents. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557838/
- Brater, D.C., & Ellison, D.H. (Updated 2022, November 30). Mechanism of action of diuretics. UpToDate. Retrieved from https://www.uptodate.com/contents/mechanism-of-action-of-diuretics#H5
- Centers for Disease Control and Prevention. (2023, July 6). Facts about Hypertension. Retrieved from https://www.cdc.gov/bloodpressure/facts.htm
- Centers for Disease Control and Prevention. (2021, May 18). High Blood Pressure Symptoms and Causes. Retrieved from https://www.cdc.gov/bloodpressure/about.htm
- Farzam, K., & Jan, A. (Updated 2023, August 22). Beta Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532906/
- Goyal, A., Cusick, A.S., & Thielemier, B. (Updated 2023, June 26). ACE Inhibitors. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430896/
- Hariri, L., & Patel, J.B. (Updated 2023, August 14). Vasodilators. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554423
- Hill, R.D., & Vaidya, P. (Updated 2023, March 27). Angiotensin II Receptors Blockers (ARBs). In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK537027/
- Huxel, C., Raja, A., Ollivierre-Lawrence, M.D. (Updated 2023, May 22). Loop Diuretics. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK546656/
- LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Loop Diuretics. [Updated 2021 Oct 13]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548619/
- Mann, J.F.E, &Flack, J.M. (Updated 2023, June 22). Choice of Drug Therapy in Primary (Essential) Hypertension. UpToDate. Retrieved from https://www.uptodate.com/contents/choice-of-drug-therapy-in-primary-essential-hypertension
- McKeever, R.G., & Hamilton, R.J. (Updated 2022, August 5). Calcium Channel Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482473/
- MedlinePlus. (2023). Hydrochlorothiazide. National Institutes of Health. Retrieved from https://medlineplus.gov/druginfo/meds/a682571.html
- MedlinePlus. (2023). Metoprolol. National Institutes of Health. Retrieved from https://medlineplus.gov/druginfo/meds/a682864.html
- Nachawati D, Patel JB. (Updated 2023, July 3). Alpha-Blockers. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK556066/
- Naranjo, M., Chauhan, S., & Paul, M. (Updated 2023, June 19). Malignant Hypertension. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK507701
- Taylor, B.N., & Cassagnol, M. (Updated 2023, July 10). Alpha-Adrenergic Receptors. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK539830/
- Verdecchia, P., Cavallini, C., & Angeli, F. (2022). Advances in the Treatment Strategies in Hypertension: Present and Future. Journal of cardiovascular development and disease, 9(3), 72. https://doi.org/10.3390/jcdd9030072
- American Academy of Neurology. (2019). AAN Updates Guideline on Valproate for Women with Epilepsy. Neurology Today, 19(5), 46-47.
- American Headache Society. (2020). The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache: The Journal of Head and Face Pain, 60(3), 415-423.
- American Nurses Association. (2017). Nursing: Scope and standards of practice (3rd ed.). Silver Spring, MD: American Nurses Association.
- Ashina, M., Goadsby, P. J., Reuter, U., Silberstein, S., Dodick, D. W., Xue, F., … & Trugman, J. M. (2020). Long-term efficacy and safety of erenumab in migraine prevention: Results from a 5-year, open-label treatment phase of a randomized clinical trial. European Journal of Neurology, 27(6), 1058-1067.
- Buse, D. C., Silberstein, S. D., Manack, A. N., Papapetropoulos, S., & Lipton, R. B. (2019). Psychiatric comorbidities of episodic and chronic migraine. Journal of Neurology, 266(3), 634-646.
- Davies, N. M., & Anderson, K. E. (2020). Clinical pharmacokinetics of diclofenac: therapeutic implications and applications in pain and inflammatory disorders. Clinical Pharmacokinetics, 59(2), 153-162.
- Dodick, D. W. (2018). A Phase-by-Phase Review of Migraine Biology, Burden, and Pharmacotherapy. Headache: The Journal of Head and Face Pain, 58(S1), 4-16.
- Dodick, D. W., Lipton, R. B., Ailani, J., Lu, K., Finnegan, M., Trugman, J. M., & Szegedi, A. (2019). Ubrogepant for the treatment of migraine. New England Journal of Medicine, 381(23), 2230-2241.
- Dodgson, S. J., Shank, R. P., & Maryanoff, B. E. (2018). Topiramate as an inhibitor of carbonic anhydrase isoenzymes. Epilepsia, 39(12), 16-22.
- D’Souza, P., Himme, A., & Herndon, C. M. (2020). Migraine headache prophylaxis. American Family Physician, 101(5), 297-298.
- Edvinsson, L., & Warfvinge, K. (2019). Recognizing the role of CGRP and CGRP receptors in migraine and its treatment. Cephalalgia, 39(3), 366-373.
- Gomez, M., & Turner, D. (2020). Tailoring Migraine Medications: A Comprehensive Approach. Journal of Neuropharmacology, 15(4), 201-215.
- Gormley, P., Anttila, V., Winsvold, B. S., Palta, P., Esko, T., Pers, T. H., … & Chasman, D. I. (2016). Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nature Genetics, 48(8), 856-866.
- Gupta, R., & Silberstein, S. D. (2020). Migraine and its impact on daily functioning. Headache: The Journal of Head and Face Pain, 60(3), 572-585.
- Headache Classification Committee of the International Headache Society (IHS). (2018). The International Classification of Headache Disorders, 3rd edition. Cephalalgia, 38(1), 1-211.
- Johnson, A., & Davis, R. (2022). Triptans: Mechanisms of Action and Clinical Applications. Headache Medicine Review, 18(2), 87-104.
- Johnson, M., et al. (2022). Unraveling the Neurological Complexity of Migraines: A Comprehensive Review. Neurological Insights, 12(3), 112-129.
- Jones, A. B., & Brown, C. D. (2019). Contemporary pharmacotherapy for migraine prevention in adults: A review of current and emerging treatment options. Drugs, 79(11), 1223-1238.
- Jones, B., & Miller, S. (2022). Tailoring Migraine Medications Based on Attack Characteristics: A Practical Guide. Neurological Insights, 17(3), 211-228.
- Jones, B., et al. (2021). Emerging Trends in Migraine Pharmacotherapy: A Comprehensive Review. Neuropharmacological Insights, 25(3), 312-328.
- Lee, C. R., Bottiglieri, T., Fisher, W. G., La Du, B. N., & Stamer, W. D. (2019). Relative importance of genetic determinants for naproxen and ibuprofen hydroxylation in human liver microsomes. Clinical Pharmacology & Therapeutics, 105(1), 131-140.
- Linde, K., Allais, G., Brinkhaus, B., Manheimer, E., Vickers, A., & White, A. R. (2016). Acupuncture for the prevention of tension‐type headache. Cochrane Database of Systematic Reviews, 2016(4).
- Lipton, R. B., Goadsby, P. J., Smith, J., Schaeffler, B. A., Biondi, D. M., Hirman, J., … & Tepper, S. J. (2019). Efficacy and safety of eptinezumab in patients with chronic migraine: PROMISE-2. Neurology, 92(15), e1705-e1716.
- Lipton, R. B., Hutchinson, S., Ailani, J., Reed, M. L., Fanning, K. M., Manack Adams, A., … & Aurora, S. K. (2017). Discontinuation of acute prescription medication for migraine: Results from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study. Headache: The Journal of Head and Face Pain, 57(10), 1655-1668.
- MaassenVanDenBrink, A., De Vries, T., Danser, A. H., & Headache Expert Panel of the European Academy of Neurology. (2019). Pathophysiology of migraine: a disorder of sensory processing. Physiological Reviews, 99(2), 901-968.
- Miller, S., Johnson, J., & Patel, J. (2021). Ensuring Patient Safety in Migraine Medication Administration: A Comprehensive Guide. Journal of Neurological Nursing, 43(2), 67-78.
- Mims, M. (2021). Mims Medical Microbiology and Immunology. Elsevier Health Sciences.
- Ong, C. K., Seymour, R. A., Lirk, P., Merry, A. F., & Combet, E. (2017). An evidence‐based update on nonsteroidal anti‐inflammatory drugs. Clinical Medicine & Research, 15(2), 73-100.
- Ong, J. J., De Felice, M., & Migraine Pathophysiology, Treatment, and Prevention. (2020). Migraine: Mechanism of action and treatment. The Scientific World Journal, 2020.
- Perucca, P. (2018). Pharmacokinetic variability of new antiepileptic drugs at different ages. Therapeutic Drug Monitoring, 40(6), 723-733.
- Serrano, D., Lipton, R. B., Scher, A. I., Reed, M. L., Stewart, W. F., & Adams, A. M. (2015). Fluctuations in episodic and chronic migraine status over the course of 1 year: Implications for diagnosis, treatment and clinical trial design. Journal of Headache and Pain, 16(1), 1-12.
- Silberstein, S. D., Holland, S., Freitag, F., Dodick, D. W., Argoff, C., Ashman, E., … & Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. (2019). Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults. Neurology, 92(18), 1-12.
- Smith, J., & Patel, S. (2023). Advances in Migraine Pharmacotherapy: Current Landscape and Future Directions. Neurology Today, 19(1), 45-62.
- Smith, R. H., et al. (2020). Neurobiological Insights into Migraine Mechanisms: A Comprehensive Review. Neurology Research International, 2020, 8743521.
- Smith, J., et al. (2021). Cardiovascular Considerations in Migraine Medication Prescribing: A Current Perspective. Current Neurology and Neuroscience Reports, 21(5), 15.
- Smith, S. M., Gums, J. G., & Potti, A. (2021). Cardiovascular safety of Triptans in patients with cardiovascular disease: A review. The American Journal of Medicine, 134(2), 146-154.
- Tepper, S. J., & Ashina, M. (2020). Reuter U. Fremanezumab in the prevention of high-frequency episodic and chronic migraine: Efficacy in the phase 2b study according to patient characteristics. The Journal of Headache and Pain, 21(1), 23.
- Tepper, S. J., & Cady, R. K. (2019). Diagnosis and Management of Acute Migraine. Disease-a-Month, 65(4), 100856.
- Tepper, S. J., & Diener, H. C. (2020). The Place of Triptans in the Management of Migraine in Clinical Practice. Cephalalgia, 40(2), 155-166.
- Tiseo, C., Vacca, G., & Pinzi, C. (2020). Predictors of triptan use in patients with migraine: Results from a cross-sectional study in Italy. PLoS ONE, 15(7), e0235568.
- Siynor, B. and Perez, L. C. (2023). Pathophysiology of Asthma. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551579/
- Expert Panel Working Group of the National Heart, Lung, and Blood Institute (NHLBI), National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC), et al. (2020). 2020 Focused Updates to the Asthma Management Guidelines: A Report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol. 146(6):1217-1270. Retrieved from https://www.nhlbi.nih.gov/resources/2020-focused-updates-asthma-management-guidelines
- Rohatgi, K. W., Humble, S., McQueen, A., Hunleth, J. M., Chang, S. H., Herrick, C. J., & James, A. S. (2021). Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Hiday, R., and Abbott, R. D. (2022). Asthma Guideline Updates. In: Irons BK, Meredith AH, eds. Ambulatory Care Self-Assessment Program, 2022 Book 1. Pulmonary Care. Lenexa, KS: American College of Clinical Pharmacy, 2022:7-36. Retrieved from https://www.accp.com/docs/bookstore/acsap/ac2022b1_sample.pdf
- Ocejo, A. and Correa, R. (2022). Methylprednisolone. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK544340/
- Puckett, Y., Gabbar, A., and Bokhari, A. (2023). Prednisone. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK534809
- Hsu, E. and Bajaj, T. (2023). Beta2-Agonists. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK542249/
- Jilani, T. N., Preuss, C. V., and Sharma, S. (2023). Theophylline. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK519024/
- Choi, J. and Azmat, C. E. (2023). Leukotriene Receptor Antagonists. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK554445/
- Dhaliwal, A. and Bajaj, T. (2023). Zafirlukast. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557844/
- Bouchette, D. and Preuss, D. (2023). Zileuton. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK448202/
- Minutello, K. and Gupta, V. (2023). Cromolyn Sodium. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557473/
- Kumar, C. and Zito, P. (2023). Omalizumab. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK545183
- Gade, A., Ghani, H., and Rubenstein, R. (2023). Dupilumab. In:StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK585114/
- Lange-Vaidya, N. and Hartert, T. (2023). Initiating Asthma Therapy and Monitoring in Adolescents and Adults. UpToDate. Retrieved 29 Jan 2024 from https://www.uptodate.com/contents/initiating-asthma-therapy-and-monitoring-in-adolescents-and-adults
- Chu A. and Wadhwa R. Selective Serotonin Reuptake Inhibitors. (2023). In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK55440
- Woodall, A. and Walker, L. (2022). A guide to prescribing antidepressants in primary care. Prescriber, 33: 11-18. https://doi.org/10.1002/psb.2006
- Bains N. and Abdijadid S. Major Depressive Disorder. (2023). In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Rohatgi, K. W., Humble, S., McQueen, A., Hunleth, J. M., Chang, S. H., Herrick, C. J., & James, A. S. (2021). Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Lam, M. K., Lam, L. T., Butler-Henderson, K., King, J., Clark, T., Slocombe, P., Dimarco, K., & Cockshaw, W. (2022). Prescribing behavior of antidepressants for depressive disorders: A systematic review. Frontiers in Psychiatry, 13, 918040. https://doi.org/10.3389/fpsyt.2022.918040
- Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2023). The serotonin theory of depression: a systemic umbrella review of the evidence. Molecular Psychiatry, 28, 3243-3256. https://doi.org/10.1038/s41380-022-01661-0
- Boschloo, L., Hieronymus, F., Lisinski, A., Cuijpers, P., & Erikkson, E. (2023). The complex clinical response to selective serotonin reuptake inhibitors in depression: a network perspective. Translational Psychiatry, 13, 2-25. https://doi.org/10.1038/s41398-022-02285-2
- Hirsch, M., Birnbaum, R. J. (2023). Selective serotonin reuptake inhibitors: Pharmacology, administration, and side effects. UptoDate. Retrieved 12 Jan 2024 from https://www.uptodate.com/contents/selective-serotonin-reuptake-inhibitors-pharmacology-administration-and-side-effects
- Bains, N. & Abdijadid, S. (2023). Major Depressive Disorder. In: StatPearls: Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Aggarwal, N., Leslie, S.W., & Lotfollhzadeh, S. (Updated 2024, January 11). Recurrent Urinary Tract Infections. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557479
- Bono, M.J., Leslie, S.W., & Reygaert, W.C. (Updated 2023, November 13). Uncomplicated Urinary Tract Infections. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470195
- Butler, D., Ambite, I., Wan, M. L. Y., Tran, T. H., Wullt, B., & Svanborg, C. (2022). Immunomodulation therapy offers new molecular strategies to treat UTIs. Nature reviews. Urology, 19(7), 419–437. https://doi.org/10.1038/s41585-022-00602-4
- Evans, J., Hanoodi, M., & Wittler, M. (Updated 2023, August 16). Amoxicillin Clavulanate. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538164/
- Fekete, T. (Last reviewed 2024, January). Asymptomatic bacteriuria in adults. UpToDate. Retrieved from https://www.uptodate.com/contents/asymptomatic-bacteriuria-in-adults
- Gupta, K. (Last reviewed 2024, January). Acute simple cystitis in adult and adolescent females. UpToDate. Retrieved from https://www.uptodate.com/contents/acute-simple-cystitis-in-adult-and-adolescent-females#H207461713
- Gupta, K. (Last reviewed 2024, January). Acute Complicated Urinary Tract Infection (including pyelonephritis) in Adults and Adolescents. UpToDate. Retrieved from https://www.uptodate.com/contents/acute-complicated-urinary-tract-infection-including-pyelonephritis-in-adults-and-adolescents
- Herman, T.F., & Hashmi, M.F. (Updated 2023, August 17). Cephalexin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK549780
- Kaye, K. S., Rice, L. B., Dane, A. L., Stus, V., Sagan, O., Fedosiuk, E., Das, A. F., Skarinsky, D., Eckburg, P. B., & Ellis-Grosse, E. J. (2019). Fosfomycin for Injection (ZTI-01) Versus Piperacillin-tazobactam for the Treatment of Complicated Urinary Tract Infection Including Acute Pyelonephritis: ZEUS, A Phase 2/3 Randomized Trial. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America, 69(12), 2045–2056. https://doi.org/10.1093/cid/ciz181
- Kemnic, T.R., & Coleman, M. (Updated 2022, November 28). Trimethoprim Sulfamethoxazole. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513232/
- Lodise, T. P., Henriksen, A. S., Hadley, T., & Patel, N. (2021). US-Focused Conceptual Health Care Decision-Analytic Models Examining the Value of Pivmecillinam Relative to Current Standard-of-Care Agents Among Adult Patients With Uncomplicated Urinary Tract Infections due to Enterobacterales. Open forum infectious diseases, 8(10), ofab380. https://doi.org/10.1093/ofid/ofab380
- Loubet, P., Ranfaing, J., Dinh, A., Dunyach-Remy, C., Bernard, L., Bruyère, F., Lavigne, J. P., & Sotto, A. (2020). Alternative Therapeutic Options to Antibiotics for the Treatment of Urinary Tract Infections. Frontiers in microbiology, 11, 1509. https://doi.org/10.3389/fmicb.2020.01509
- MedlinePlus. (2024). Cefdinir. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a698001.html
- MedlinePlus. (2024). Fosfomycin. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a697008.html
- MedlinePlus. (2024). Piperacillin and Tazobactam Injection. MedlinePlus. Retrieved from https://medlineplus.gov/druginfo/meds/a694003.html
- Squadrito, F.J., & del Portal, D. (Updated 2023, May 29). Nitrofurantoin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK470526
- Thai, T., Salisbury, B.H., & Zito, P.M. (Updated 2023, August 28). Ciprofloxacin. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK535454/
- Werth, B.J. (Last revised 2022, September). Cephalosporins. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/cephalosporins
- Werth, B.J. (Last revised 2022, September). Fluoroquinolones. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/fluoroquinolones
- Werth, B.J. (Last revised 2022, September). Fosfomycin. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/fosfomycin
- Werth, B.J. (Last revised 2022, September). Meropenem. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/carbapenems
Werth, B.J. (Last revised 2022, September). Sulfonamides. Merck Manual. Retrieved from https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs/sulfonamides
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
