Course
Florida Autonomous NP Bundle
Course Highlights
- In this course, we will learn about the classic and atypical symptoms associated with hypothyroidism.
- You’ll also learn common clinical presentations of depression, including more severe clinical presentations.
- You’ll leave this course with a broader understanding of the alarming rates of diabetes diagnoses in the United States and its effect on chronic disability and premature mortality.
About
Contact Hours Awarded: 10.5
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
Differential Diagnosis of Hypothyroidism
Introduction
As we embark on the journey of differential diagnosis of hypothyroidism, we will examine several medical mysteries. This condition, marked by the thyroid gland's failure to produce sufficient hormones, often disguises itself with a cloak of nonspecific symptoms that could easily be mistaken for other health issues.
A patient could report feeling tired, perhaps having unexplained weight gain, or feeling unusually cold, not realizing that these could be whispers of an underactive thyroid. The challenge for clinicians lies not just in recognizing these whispers among the noise of overlapping symptoms, but in using them to trace the path back to the true culprit.
The process of differential diagnosis for hypothyroidism is a critical exploration—a blend of pathophysiology, etiology, and clinical signs and symptoms of hypothyroidism. By carefully piecing together clues from patient histories, physical exams, and targeted laboratory tests, it is possible to uncover the hidden patterns of this disorder.
Definition
"Differential diagnosis" is a term used to describe the process by which a provider determines which disease or condition most likely explains an individual’s symptoms and signs. The process involves comparing and contrasting various possibilities to arrive at the most likely diagnosis.
Hypothyroidism essentially occurs when the thyroid gland is not able to produce adequate amounts of thyroid hormone. In the context of hypothyroidism, a differential diagnosis means considering and ruling out other conditions that might cause similar symptoms to those of hypothyroidism. These symptoms can include fatigue, weight gain, cold intolerance, dry skin, hair loss, and constipation, among others.
The provider will consider medical history, physical examination, and laboratory tests to narrow down the list of possible diagnoses to the most likely one. For hypothyroidism, measuring levels of thyroid hormones and thyroid-stimulating hormone (TSH) in the blood is key to confirming the diagnosis.
Hypothyroidism can be broken down into two categories, primary and secondary (central) hypothyroidism. Secondary is less common and occurs when the thyroid gland functions normally, but the pituitary gland or hypothalamus do not, which causes thyroid dysfunction.
Epidemiology
Roughly 5% of the U.S. population has a diagnosed thyroid disorder, and the American Association of Clinical Endocrinologists suggests that an additional 5% has undiagnosed thyroid disease (8). In developing countries, where dietary iodine is lacking, thyroid disease is even more prevalent.
Impaired thyroid function is more common in females and individuals greater than 65 years old. Thyroid dysfunction is more prevalent among individuals with autoimmune diseases such as diabetes type I, celiac disease, or autoimmune endocrine disorders. Those with Downs’ or Turners’ syndrome are at higher prevalence as well.
Heredity is a significant contributor to the development of hypothyroidism in individuals who have a history of hypothyroidism in their family; the chances of TSH being transferred from parents to children are 60%, while that of free T4 is 20% to 60% (11).
Causes of Hypothyroidism
The most common cause of primary hypothyroidism across the world is iodine deficiency (6). Within the United States, the most common cause of hypothyroidism is autoimmune thyroid disease, also called Hashimoto thyroiditis. Hypothyroidism may be caused by a defect of the hypothalamic–pituitary–thyroid axis. The following are causes of hypothyroidism (4, 6).
- Autoimmune Thyroiditis (Hashimoto’s Thyroiditis)
- Inflammatory condition in which the immune system mistakenly attacks and damages the thyroid gland, which leads to a gradual decline in thyroid function.
- Iatrogenic Causes
- Examples include the surgical removal of the thyroid gland (thyroidectomy) or radioiodine therapy for hyperthyroidism.
- These interventions may inadvertently cause insufficient thyroid hormone production.
- Congenital Hypothyroidism
- This is hypothyroidism acquired from birth. This can result from genetic factors, abnormal thyroid development, or maternal thyroid dysfunction during pregnancy.
- Medication-Induced Hypothyroidism
- Certain medications can interfere with thyroid hormone production. Close monitoring is essential for patients taking such medications.
- Iodine Deficiency
- Iodine is an essential component for thyroid hormone synthesis. Living in certain regions of the world with iodine insufficiency can increase the risk of inadequate intake of iodine. Iodine deficiency is less common in areas with iodized salt supplementation.
Types of Hypothyroidism
Primary Hypothyroidism
Primary hypothyroidism is due to impaired function of the thyroid gland, resulting in increased thyroid-stimulating hormone (TSH). Primary hypothyroidism causes about 99% of cases and may be accompanied by goiter (5).
Post-therapeutic hypothyroidism is damage to the thyroid function during radioactive iodine therapy or surgical treatment of hyperthyroidism or goiter. The use of radioactive iodine to manage Graves’ disease usually results in permanent hypothyroidism in about 80-90% of those patients. Radiation treatment to the head and neck area can also result in hypothyroidism.
Hypothyroidism can also result from the use of certain medications. These include amiodarone, thalidomide, oral tyrosine kinase inhibitors (sunitinib, imatinib) stavudine, interferon, bexarotene, perchlorate, rifampin, ethionamide, phenobarbital, phenytoin, carbamazepine, interleukin-2, and lithium (5). Research shows that a newer class of cancer medications, such as anti-CTLA-4 and anti-PD-L1/PD-1 therapy, is associated with both primary and/or secondary hypothyroidism.
Postpartum thyroiditis is found in about 10% of women and commonly presents 8-20 weeks after delivery.
Secondary and Tertiary Hypothyroidism
Secondary hypothyroidism, also known as central hypothyroidism, is caused by a defect in the hypothalamic-pituitary axis.
This form of hypothyroidism is related to the following (5):
- Pituitary tumors
- Tumors compressing hypothalamus
- Sheehan syndrome
- This syndrome occurs when significant blood loss results in damage to the anterior pituitary gland.
- Thyrotropin-releasing hormone (TRH) resistance or deficiency
- Thyrotropin-releasing hormone (TRH) is a hormone produced by neurons in the hypothalamus that stimulates the release of thyroid-stimulating hormone (TSH)
- Lymphocytic hypophysis
- Radiation therapy to the brain
- Drugs such as dopamine, prednisone, or opioids

Self Quiz
Ask yourself...
- How are primary and secondary hypothyroidism different?
- What is a common cause of primary hypothyroidism in the United States?
- Can you describe post-therapeutic hypothyroidism and why this occurs?
- What are some other hormones that are impacted by an underactive thyroid?
Pathophysiology
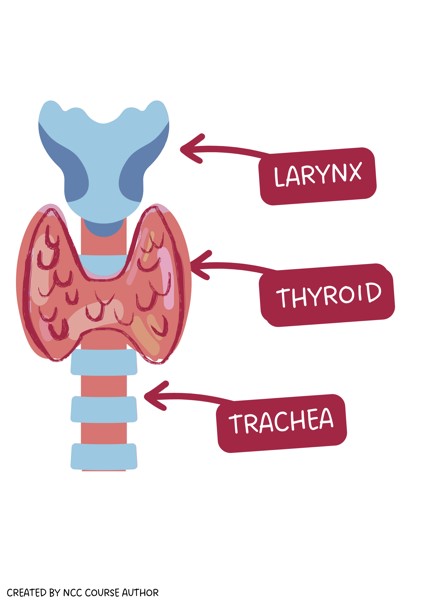
The thyroid gland is located in the neck anterior to the trachea and below the larynx and cricoid cartilage (8). It consists of right and left lobes connected by an isthmus. The thyroid weighs around 15 to 20 g (8).
The thyroid has two essential responsibilities in the endocrine system:
- Maintaining metabolic rate necessary for heat generation.
- Promotes normal growth and development from fetal life into childhood.
Thyroid follicles are the structural and functional units of a thyroid gland. They are spherical-shaped, and the wall is made up of a large number of cuboidal cells, the follicular cells, which are less than 0.5 mm in diameter. These follicular cells are the derivates of the endoderm and secrete thyroid hormone.
Follicles are filled with thyroglobulin, the glycoprotein precursor to thyroid hormone. The pool of thyroglobulin molecules is referred to collectively as a substance called colloid. The follicles are bundled into lobules by connective tissue, nerves (parasympathetic and sympathetic), blood vessels, and lymphatic tissue.

Self Quiz
Ask yourself...
- How would you describe the role of the endocrine system?
- Can you discuss how thyroid functioning impacts other systems in the body?
- If thyroid hormones maintain metabolic rates and heat generation, how would low or high levels be manifested?
- Have you ever cared for a patient with severe and untreated hypothyroidism?
Clinical Findings
Clinicians must ask why a certain sign or symptom is present. It is important to recognize the underlying physiological process.
For individuals with longer-term untreated hypothyroidism, signs and symptoms are more pervasive and involve multiple body symptoms. However, signs and symptoms of primary hypothyroidism are often subtle and less obvious.
As we mentioned, the thyroid's main job is to create the hormones T4 and T3 to control metabolism, which is the process by which food is broken down to produce energy. These hormones regulate how much energy to use. They also regulate body temperature and heart rate.
The amount of thyroid hormones in the bloodstream is controlled by the pituitary gland, which is located in the center of the skull below the brain. When the pituitary gland senses either a lack of thyroid hormone or too much, it adjusts its own hormone, called thyroid stimulating hormone, or TSH, and sends it to the thyroid to balance these levels.
The signs and symptoms can point to the cause. An essential part of differential diagnosis is to evaluate the impact on each system and consider other causative factors.
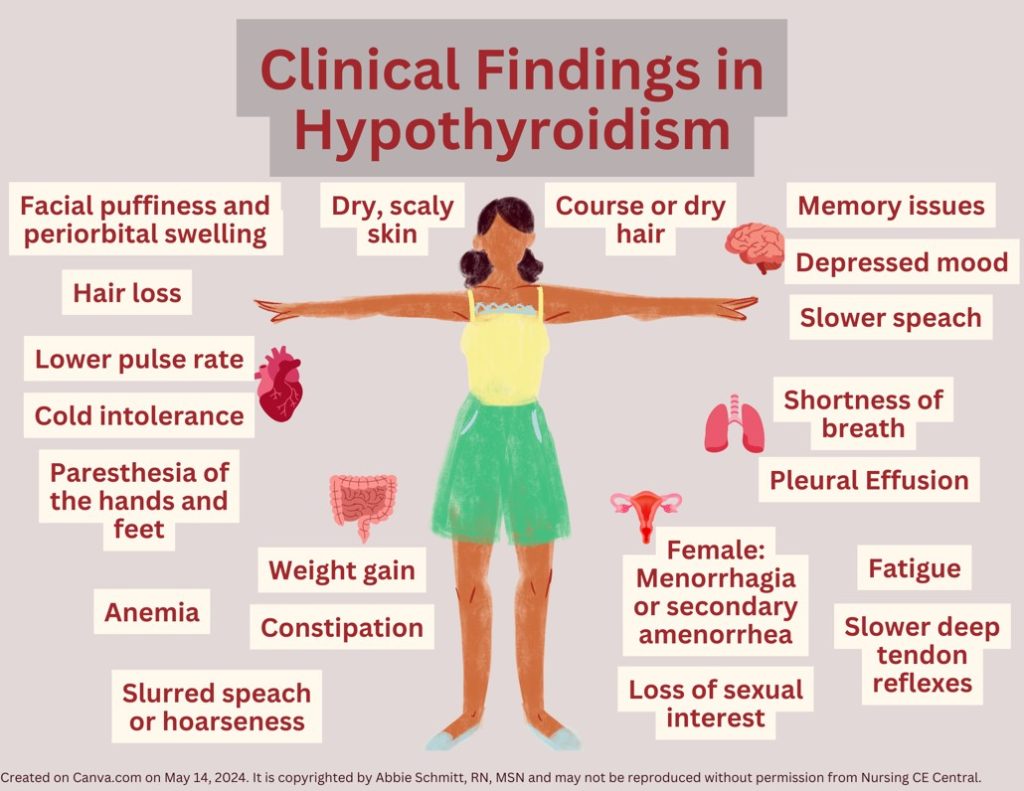
Hypothyroidism affects various organ systems in the body, including the central and peripheral nervous systems, and the cardiovascular, integumentary, gastrointestinal, muscular, reproductive, and hematopoietic systems.
Common symptoms include:
- Integumentary
-
- Myxedema (skin swelling and thickening)
-
- Dry, coarse skin and hair
-
- Hair loss
-
- Puffiness in the eyes and face
-
- Eyelid drooping
- Cardiac
-
- Bradycardia
-
- Diastolic hypertension
-
- Cold intolerance
- Neuromuscular
-
- Numbness and tingling in the hands and feet (paresthesia)
-
- Feeling depressed
-
- Feeling more forgetful or having “brain fog”
- Gastrointestinal
-
- Constipation
-
- Weight gain
- Respiratory system
-
- Shortness of breath
-
- Pleural effusion
- Muscular
-
- Muscle soreness and weakness
- Reproductive
-
- Decrease in sexual interest
-
- Frequent and heavy menstrual periods
- General
-
- Fatigue
-
- Voice may sound lower and hoarser
- Hematopoietic System
-
- Anemia
Myxedema refers to the appearance of the skin and subcutaneous tissues when severe hypothyroidism is present (5). Facial puffiness and periorbital swelling occur because of infiltration with mucopolysaccharides, known as hyaluronic acid and chondroitin sulfate. The eyelids droop due to decreased adrenergic drive (5). Hair may appear and feel coarse, dry, and sparse. The skin is also coarse, dry, scaly, and thickened. Facial expression may be dull. Myxedematous infiltration of the tongue causes thick, slurred speech; and infiltration of the larynx causes hoarseness.
Deficiency in thyroid hormones will also lead to decreased cerebral blood flow. In hypothyroidism, the decreased stroke volume and heart rate result in reduced resting cardiac output (5). These hemodynamic alterations cause pulse pressure to be narrowed, circulation time to be prolonged, and a reduction in blood flow to body tissues. Essentially, there is often a lower pulse rate. Decreased cutaneous circulation causes coolness and pallor of the skin as well as cold sensitivity.
Development of the CNS requires thyroid hormones and a deficiency in fetal life or at birth will lead to impaired neurologic development. Manifestations include hypoplasia of the cortical neurons, slowed myelination, and decreased vascularity (5). When thyroid hormone deficiency occurs in adulthood, manifestations are less severe, and symptoms usually respond easily to hormone therapy. Ongoing deficits lead to intellectual functions slowing down, including speech. Hypothyroidism may manifest with feelings of depression, a loss of initiative to perform tasks, and memory problems. There is prominent lethargy.
Modest weight gain is usually the result of decreased metabolism and fluid retention, caused by the hydrophilic glycoprotein tissue deposits, but usually does not exceed 10% of body weight (5). There is also reduced peristalsis, leading to constipation, contributing to weight gain. Symptoms that mimic mechanical ileus may occur, including gaseous abdominal distention (myxedema ileus), colicky pain, and vomiting.
Hypothyroidism affects the respiratory system and breathing due to the actions upon the central regulation of respiration, the reduced function of respiratory muscles, the upper airways, and the tongue. Generally, lung volumes are normal, but there are reductions in maximal breathing capacity and diffusing capacity. Pleural effusions may be noted. Severe hypothyroidism causes myxedematous changes in respiratory muscles and depression of the hypoxic and hypercapnic ventilatory drives. Hypothyroid patients have an increased likelihood of obstructive sleep apnea (5).
Body movements become slower and clumsier with cerebellar ataxia sometimes occurring. Numbness and tingling in the extremities are common. The relaxation phase of the deep tendon reflexes becomes slowed due to decreased rates of muscle contraction and relaxation. This is not a delay in nerve conduction, which is important when considering neurological conditions.
Females with hypothyroidism may develop menorrhagia or secondary amenorrhea. Another reproductive symptom would include decreased interest or drive for sexual activity.
The thyroid gland has a very important role in hematopoiesis. Thyroid hormones have a direct effect on blood parameters by stimulating erythrocytes precursors and indirectly by enhancing erythropoietin production. Individuals with hypothyroidism commonly have blood disorders. Patients with thyroid abnormalities may have low iron, folate, and B12 levels, which have been detected in up to 25% of patients (1). This will eventually impact the hemoglobin and the red blood cells (RBCs).
A goiter signifies an enlarged thyroid gland. It may be an overall enlargement of the thyroid, or it may be the result of irregular cell growth that forms one or more nodules in the thyroid. A goiter may or may not impact thyroid function.
Myxedema coma is a life-threatening complication of hypothyroidism and typically occurs in patients with a long history of untreated hypothyroidism. The clinical presentation can include a coma with extreme hypothermia, areflexia, seizures, and respiratory depression with carbon dioxide retention (2). Precipitating factors include illness, infection, trauma, medications (or substances that suppress the central nervous system), and exposure to cold.
Rapid diagnosis and treatment of myxedema coma are imperative because death will likely occur without rapid treatment.

Self Quiz
Ask yourself...
- How would you prioritize these symptoms from least to most worrisome?
- Can you think of any medications that have side effects that may mimic these symptoms? For example, certain antidepressants have side effects of weight gain.
- Can you discuss how insufficient thyroid hormone can impact respiration?
- How would you describe myxedema coma?
Advanced Health Assessment
An advanced health assessment for differential diagnosis of hypothyroidism involves a comprehensive evaluation that distinguishes hypothyroidism from other conditions with similar symptoms.
History and Physical
Gathering detailed information about the patient's symptoms, medical history, family history, and any medications or supplements they are taking is vital. These symptoms can be another medication condition or an effect of a medication. Remember, the common symptoms of hypothyroidism (fatigue, weight gain, cold intolerance, constipation, dry skin, hair loss, and depression) can be easily attributable to various diagnoses. Collecting information about physical and psychological symptoms; for example, ask about constipation, dry skin, muscle cramps, cold intolerance, insomnia, menstrual cycle changes, weight gain, anxiety, depression, difficulty focusing, or fatigue.
Ask if there is a family history of thyroid disease and any personal surgical, medication, psychosocial, and reproductive history (e.g., number of pregnancies and live births).
A thorough physical exam can help identify signs of hypothyroidism, such as dry skin, swelling, slowed reflexes, and goiter. Close examination of the neck and throat, palpating the thyroid gland to feel texture and firmness, and looking for skin/hair changes are important.
Vital signs provide valuable insight, including heart rate, blood pressure, temperature, respiratory rate, and pain levels.
Laboratory Tests
The most crucial tests for diagnosing hypothyroidism involve measuring levels of thyroid hormones and thyroid-stimulating hormone (TSH).
- TSH Test: High levels of TSH may indicate hypothyroidism. The pituitary gland produces more TSH to stimulate the underactive thyroid.
- Free T4 and Free T3 Test: Low levels of the thyroid hormone thyroxine (T4) and (T3) can confirm hypothyroidism.
Reference Ranges for Thyroid Function Tests:
The majority of TSH and free T4 assays used in industry are immunoassays, and their reference ranges are based on statistics to be between the 2.5th and 97.5th percentiles in a population with positive health indicators (11). The reference ranges vary according to age, sex, and ethnicity.
Additional Tests: Depending on the suspected cause of hypothyroidism, additional tests may be necessary:
- Thyroid Antibodies Test: This test can detect autoimmune thyroiditis (like Hashimoto's disease), which is a common cause of hypothyroidism.
- Ultrasound of the Thyroid: The structure of the thyroid gland is visualized, which can help identify nodules or abnormalities.
Diagnosis
Primary hypothyroidism is distinguished by (11):
- TSH values higher than the standard reference range (0.5-5 mIU/L)
- Free T4 levels below the patient-specific reference range
- The reference ranges for pregnant women are 0.1-2.5 mIU/L (first trimester), 0.2-3.0 mIU/L (second trimester), and 0.3-3.5 mIU/L (third trimester)
Fluctuation of Hormone Levels
The levels of TSH fluctuate throughout the day, with the peak value being in the late afternoon and evening. Individuals with severe hypothyroidism have very high TSH secretion, which may become erratic (11). Seasonal fluctuation has been noted and concentrations of TSH are higher in winter and spring, while they are lower in autumn and summer.

Self Quiz
Ask yourself...
- Can you explain why TSH would be higher in hypothyroidism?
- What vital sign abnormalities may be present in a patient with hypothyroidism?
- At what time of day do TSH levels peak?
- Are you familiar with performing an assessment and palpation of the thyroid gland?
Differential Diagnosis
The presence of hypothyroidism can be overlooked if the diagnosis is not considered adequately. Severe primary hypothyroidism is often not recognized. It is meaningful to consider other conditions that might mimic the symptoms of hypothyroidism.
Differential diagnosing hypothyroidism involves a systematic approach to rule out other conditions that share similar symptoms. We are going to break down each sign and symptom to expose other conditions with similar presentations.
These conditions may be considered in the differential diagnosis of hypothyroidism:
- Pernicious anemia
- Chronic renal insufficiency
- Depression
- Other hormonal disorders
- Nutritional deficiencies
- Autoimmune disorders
- Heart disease
- Euthyroid sick syndrome
- Goiter
- Myxedema coma
- Riedel thyroiditis
- Subacute thyroiditis
- Thyroid lymphoma
- Iodine deficiency
- Addison disease
- Chronic fatigue syndrome
- Dysmenorrhea
- Erectile dysfunction
- Infertility
Pernicious Anemia
There are several overlapping signs and symptoms of pernicious anemia and hypothyroidism. These symptoms include pallor, fatigue, weakness, and intolerance to cold. Blood tests showing low hemoglobin and hematocrit levels help differentiate anemia from hypothyroidism.
Chronic Renal Insufficiency
Chronic renal insufficiency and hypothyroidism may be suggested by anorexia, periorbital puffiness, torpor, anemia, and a sallow (yellow or grayish) complexion. It may be more difficult to distinguish hypothyroidism from nephrotic states by clinical examination alone.
Edema, pallor (or “waxy” pallor), hypometabolism, and hypercholesterolemia may suggest hypothyroidism. Also, total serum thyroxine concentrations may be decreased when large amounts of thyroid-binding globulin are excreted in the urine, yet the fT4 and TSH would be normal.
Depression
Depression is a mental health disorder that can mimic several symptoms of hypothyroidism, such as fatigue, feelings of sadness or despair, and weight changes. Depression typically lacks specific thyroid-related symptoms like cold intolerance and hair loss.
Adrenal Insufficiency
Fatigue, weight loss (or less commonly, gain), and low blood pressure can overlap in these conditions. Adrenal insufficiency may have symptoms like hyperpigmentation and electrolyte imbalances that are not typically present in hypothyroidism.
Pituitary Disorders
- Overlapping symptoms: May present with symptoms of multiple hormonal imbalances, including hypothyroidism.
- Distinguishing factors: Other hormonal deficiencies, such as in growth hormone or adrenal hormones, alongside imaging tests showing pituitary abnormalities.
Other Hormonal Imbalances
Conditions like Cushing's syndrome or hyperprolactinemia can cause symptoms that overlap with those of hypothyroidism. Low testosterone or adrenal insufficiency could also be considered. Similarly, conditions like hypoparathyroidism can have similar presentations. The distinguishing factors would include specific symptoms and hormonal test results.
Nutritional Deficiencies
Deficiencies in iron or vitamin B12, for example, can cause fatigue and other symptoms similar to hypothyroidism.
Autoimmune Disorders
Other autoimmune conditions like lupus or rheumatoid arthritis might initially present with symptoms that can be confused with hypothyroidism.
Heart Disease
Overlapping symptoms for various heart conditions include fatigue, abnormal pulse rate, and exercise intolerance. Distinguishing factors would include symptoms primarily related to cardiac function, such as chest pain and palpitations are key.
Euthyroid Sick Syndrome
Euthyroid sick syndrome is a condition in which serum levels of thyroid hormones are low in patients who have non-thyroidal systemic illness. Possible underlying system illnesses include starvation, protein-energy undernutrition, severe trauma, myocardial infarction, chronic kidney disease, diabetic ketoacidosis, cirrhosis, thermal injury, drug overdose, and sepsis (3).
Symptoms overlap with severe hypothyroidism, such as hypothermia, hypoventilation, hypotension, lethargy, or coma.
Decreased triiodothyronine (T3) levels are most common, but more severe or prolonged illnesses will result in decreased thyroxine (T4) levels (3). Thyroid-stimulating hormone (TSH) levels may be normal or even low (3).
Pathogenesis is unknown, but suspected to be a result of the following:
- Decreased peripheral conversion of T4 to T3
- Decreased clearance of rT3 generated from T4
- Decreased binding of thyroid hormones to thyroxine-binding globulin (TBG)
Treatment is directed toward the underlying illness and thyroid hormone replacement is not indicated.
Medication Effects
Certain medications can lead to symptoms mimicking hypothyroidism. A thorough review of the patient's medication history may reveal drugs known to affect thyroid function, such as lithium or amiodarone.
Sleep Apnea
Individuals with sleep apnea may have significant fatigue and cognitive impairment. Sleep apnea is characterized by episodes of breathing cessation during sleep, which can also impact heart rate and blood pressure.
Fibromyalgia
Fibromyalgia has classic symptoms of muscle and joint pain, fatigue, and sleep disturbances. Fibromyalgia usually involves widespread pain and tender points throughout the body, which are not specific to hypothyroidism.

Medical History and Demographic Considerations
Clinical diagnosis overlap often happens in older patients. Sometimes, slowed mental and physical activity, dry skin, and hair loss can mimic similar hypothyroidism findings. Older individuals often become hypothermic from cold exposure.
Hypothyroidism can develop from an extrinsic factor, an acquired condition, or due to a congenital defect that impairs TH biosynthesis (5).
About 20% of patients who have a surgical lobectomy develop hypothyroidism (5). There is also increased risk in locations of insufficient iodine or in patients who have anti-TPO (thyroid peroxidase) antibodies.
Hypothyroidism should be considered in the differential diagnosis of ovarian cysts and multi-cystic adnexal masses to avoid inadvertent surgery (9).

Self Quiz
Ask yourself...
- Can you name overlapping symptoms of hypothyroidism and heart disease?
- What are some underlying illnesses that cause euthyroid sick syndrome?
- Can you describe how differential diagnosis for hypothyroidism should be modified for older adults?
- Can you think of conditions that cause muscle soreness and malaise?
Case Study: Gertrude
Gertrude is a 40-year-old female who presented to her general physician for a regular check-up. Past medical history includes fibromyalgia and depression. Gertrude reported a family history of hypertension, Alzheimer’s disease, hypercholesterolemia, and Hashimoto's disease.
Gertrude is currently working as a schoolteacher and lives with her husband and teenage child. She has a sedentary lifestyle and reports occasional non-adherence to her medications due to forgetfulness.
Gertrude’s vital signs are as follows: Blood pressure (BP) 130/80 mmHg, heart rate (HR) 60 beats per minute (BPM), respiratory rate (RR) 18 breaths per minute, and temperature 98.6°F.
She is alert and fully oriented but complains of an intermittent headache. Her skin is warm and dry, and there is no visible edema. Lungs are clear on auscultation and heart sounds are normal rhythm with no murmurs. The abdominal assessment reveals no tenderness or masses. Body mass index (BMI) of 30, which indicates obesity.
Gertrude reports new symptoms that have slowly worsened over the previous 3 months. She reports worsening depression symptoms, changes in her menstrual cycle, hair loss, and intermittent tingling in her toes throughout the day.
- Are there any new symptoms that Gertrude is experiencing that could be attributed to more than one possible condition?
- Should the provider order any lab work or just refer this patient to a mental health provider, neurologist, and gynecologist?
- What are appropriate assessment questions to ask Gertrude?
- What would you focus on during a head-to-toe physical assessment?
Statistical Evidence
Let's incorporate current statistical evidence on the prevalence and risk factors for these conditions in the differential diagnosis of hypothyroidism.
These statistics are from recent studies (5, 9, 10):
- Hypothyroidism
-
- Prevalence: Varies by region but generally around 0.3-0.4% for overt hypothyroidism and 4-5% for subclinical hypothyroidism in the general population.
-
- Risk Factors: Female gender, older age, family history of thyroid disease, history of autoimmune conditions or specific surgeries or radiation therapy.
- Anemia
-
- Prevalence: Depends on the type; for example, iron deficiency anemia is very common worldwide, especially in women of childbearing age.
-
- Risk Factors: Poor diet, chronic bleeding (e.g., from ulcers), genetic conditions.
-
- Depression
-
- Prevalence: Approximately 5% globally in adults.
-
- Risk Factors: Family history of depression, major life changes, trauma, certain medications.
- Adrenal Insufficiency
-
- Prevalence: Primary adrenal insufficiency is rare, about 40-60 cases per million in developed countries.
-
- Risk Factors: Autoimmune disorders, infections, genetic predisposition.
- Sleep Apnea
-
- Prevalence: Estimated to affect about 3-7% of men and 2-5% of women in the general population.
-
- Risk Factors: Obesity, male gender, older age, family history.
- Fibromyalgia
-
- Prevalence: About 2-4% of the population, predominantly in women.
-
- Risk Factors: Female gender, middle age, family history.
- Pituitary Disorders
-
- Prevalence: Rare; specific prevalence depends on the type of pituitary disorder.
-
- Risk Factors: Genetic mutations, brain tumors, radiation treatment.
- Other Hormonal Imbalances
-
- Prevalence and Risk Factors: Vary widely depending on the specific hormonal disorder, such as diabetes, hypoparathyroidism, etc.
- Heart Disease
-
- Prevalence: One of the leading causes of morbidity and mortality worldwide; the prevalence varies by type of heart disease.
-
- Risk Factors: Family history, smoking, high blood pressure, high cholesterol, diabetes, obesity, sedentary lifestyle.

Self Quiz
Ask yourself...
- Can you discuss the prevalence of the above conditions?
- How do overlapping risk factors contribute to the likelihood of comorbidities?
Pharmacological Treatment of Hypothyroidism
The goal of treatment is to return blood levels of thyroid-stimulating hormone (TSH) and thyroxine (T4) to the normal range and to relieve symptoms.
Hypothyroidism is mainly treated with thyroid hormone replacement therapy, which is an oral T4 replacement called "levothyroxine." In most cases, symptoms of hypothyroidism begin to improve within two weeks of starting thyroid replacement therapy. However, people with more severe symptoms, especially muscle pain and weakness, may require several months of treatment before they fully recover.
The majority of individuals with hypothyroidism need to take levothyroxine for the rest of their lives.
The levothyroxine dose is 1.6 mcg/kg per day; however, in patients who are elderly and those who have atrial fibrillation, it is important to reduce the dose (6). Elemental supplements such as calcium and magnesium, to name a few, do affect the absorption of levothyroxine. Proton pump inhibitors also interfere with levothyroxine absorption.
Switching to the intravenous (IV) form in the hospitals is indicated when thyroid replacement orally is not possible or if myxedema coma is suspected; the dose of levothyroxine is reduced to generally 50% of the oral dose (6).

Self Quiz
Ask yourself...
- How would you describe the goal of treatment for hypothyroidism?
- How should levothyroxine dosing be adjusted for older adults or individuals with atrial fibrillation?
Follow Up and Monitoring
Effective treatment helps to achieve a clinical improvement of signs and symptoms and normal TSH (or free T4 levels as applicable). If symptoms persist despite normalization of TSH/free T4 levels, then non-endocrine etiologies should be considered.
Thyroid replacement treatment can exacerbate co-existing adrenal insufficiency. Patients with known or suspected adrenal insufficiency should be tested and treated. Adrenal insufficiency can also be associated with subclinical hypothyroidism that is reversible with treatment of the adrenal insufficiency. It is important to rule out or treat adrenal insufficiency when a patient has severe hypothyroidism, as with myxedema coma.
Patient Education
Patient education should be focused on hypothyroidism and properly taking medication.
Tips include:
- Levothyroxine should be taken once daily on an empty stomach (ideally one hour before eating or 2 to 4 hours after).
- It may be helpful to take the medication upon waking in the morning.
- Foods that are high in fiber, calcium or aluminum-containing antacids, and iron tablets can interfere with the absorption of levothyroxine and should be taken at a different time of day.
- It is preferable to stay on the same manufacturer of levothyroxine, rather than switching between brand name or generic formulations.
- Duration and dose: An initial dose of levothyroxine will be determined by the provider and then the blood level of TSH will be checked in six weeks. The dose can be adjusted at that time if needed. This process may need to be repeated several times before the hormone levels become normal and a therapeutic dose is found.
- Color-coded tablets can help with dose adjustments.
- Never increase or decrease the levothyroxine dose without talking with your healthcare provider.
The dose may need to be decreased with aging, after childbirth, or with weight changes. Most healthcare providers prescribe a lower initial dose of levothyroxine in older adults and those with coronary artery disease.
Over-replacement of T4 can cause mild hyperthyroidism, with the associated risks of atrial fibrillation and osteoporosis.

Case Study: Gertrude
Laboratory results show CBC and differential WBC are normal, serum TSH is 8.0 uIU/ml (reference range: 0.450 to 4.500 uIU/mL)
- Are there any follow-up labs that would be appropriate to collect?
- What education would be appropriate for Gertrude?
- Collaboration with which interdisciplinary team would be appropriate?
- Do you anticipate further studies and evaluation?
Conclusion
The differential diagnosis of hypothyroidism is a critical aspect of clinical practice, requiring meticulous attention to detail. The commonality of its symptoms—such as fatigue, weight gain, and cold intolerance—may overlap with other medical conditions. Differentiating these conditions requires a systematic approach. This process includes a thorough patient history, detailed physical examination, specific laboratory tests, and sometimes, advanced imaging techniques. Each of these components plays a vital role in accurately diagnosing hypothyroidism and ruling out other potential causes of the symptoms, ensuring that the patient receives appropriate treatment. The implications of correctly diagnosing hypothyroidism extend beyond immediate symptom management to long-term health outcomes and quality of life.
Differential Diagnosis of Depression
Introduction
When hearing the phrase depression, what comes to mind? If you're a nurse, you've heard about depression at some point in your nursing studies and career. Maybe even before nursing school, conversations about mental health, depression, and other health conditions existed every so often.
Presently, patients seek guidance and information on various health topics from nurses, including depression and mental health. The information in this course will serve as a valuable resource for nurses of all specialties, education levels, and backgrounds to learn more about depression and differential diagnosis of depression.
Defining Depression
Major depressive disorder (MDD), more commonly known as depression, is one of the most common mental health conditions in the United States, worldwide, and a leading cause of disability.
Depression is often characterized by symptoms of a depressed mood, decreased interest in activities, changes in sleep patterns, thoughts of self-harm, psychomotor changes, and more. Given the prevalence of depression, depression is expected to be the global leading cause of disability by 2030, making depression a concern for social well-being and functioning. (1, 2, 3, 4)
What is the Prevalence of Depression?
The prevalence of depression can vary significantly because of possible underdiagnosis and mistreatment. Present prevalence rates of depression in the United States range from 5-17% with women experiencing depression at twice the rate compared to men.
Studies have suggested that the most common age of onset for depression is 40; however, more studies on adolescent, pediatric, and adult mental health suggest that this common age of onset can be much lower. Early diagnosis, intervention, and assessment are essential for prompt diagnosis and treatment (1).
Depression is also noted to be more common in people who do not have strong social support networks, those who have co-morbid conditions, and those who live in rural communities compared to urban areas (1). While several studies and interventions on depression and mood have focused on adults, pediatric and adolescent populations must also be educated and screened for depression as well (1,2).
What if Depression Is Left Untreated?
If left untreated, depression can lead to further mental health complications, suicide, disability, and further decreased quality of life. For many people with depression, depression can interfere with their abilities to maintain and form social relationships, work, and go to school as well. By leaving depression untreated or not adequately managed, depression can cause further chronic issues to someone's health and livelihood (1).
Depression Pathophysiology
There are several studies, theories, and speculations regarding depression's pathophysiology. One common factor is that depression's pathophysiology is not a one-size-fits-all, and many things can influence depression in people. Genetics, hormonal shifts, pregnancy, stress, brain injuries, side effects of other medications, co-morbid health complications, psychosocial factors, and environmental situations are all suspected to influence depression pathophysiology (1).
While several studies postulate low levels of neurotransmitters, such as serotonin, GABA, dopamine, or norepinephrine, can play a role in suicidal ideation and mental health, low levels of these neurotransmitters are not the single cause of depression. More research is being done to determine the role of neuroregulatory functions, brain functions, and neurotransmitter distribution in depression and mental health overall.
Because further research is needed to determine the exact pathophysiology of depression, it is important to consider many factors that influence depression in people (1).
Depression Etiology
Similar to depression's pathophysiology, the exact etiology and cause of depression is not known. Several studies show the role of genetics, trauma, adverse childhood events (ACEs), stress, pregnancy, and more influencing the etiology of depression. That said, because there are several etiologies of depression with more research needed, it is important to consider several options for depression etiology in direct patient care (1).
Various Types of Depression
While depression is often used as a catch-all phrase for people with a depressed mood, there are several types of depression with distinct clinical presentations, management options, and interventions as well. A common type of depression is postpartum depression, which is the most common postpartum complication in the United States and one of the most common postpartum complications worldwide.
Other types of depression include perinatal depression (depression during pregnancy), seasonal affective disorder (SAD) (depression during winter months), atypical depression, psychotic depression, and more. Because of the wide variety of clinical presentations of depression, adequate assessment, intervention, and treatment are essential for appropriate patient care (1,2).

Self Quiz
Ask yourself...
- What populations can be affected by depression?
- What are some common types of depression?
- How would you explain to a patient what can cause depression?
Differential Diagnosis for Depression
Clinical Criterium for Depression
Major depressive disorder (MDD) is a mental health condition in which a person has consistent, prolonged appetite changes, sleep changes, psychomotor changes, decreased interest in activities, negative thoughts, suicidal thoughts, and depressed mood that interfere with a person's quality of life.
According to the Diagnostic and Statistical Manual of Mental Health Disorders, a patient must have at least five persistent mood-related symptoms, including depression or anhedonia, that interfere with a person's quality of life to be formally diagnosed with MDD. Other depressive states can also be assessed with the PHQ-9. Note that MDD does not include a history of manic episodes, and pediatric populations can present with more variable MDD symptoms. As a nurse, you can assess MDD by doing a detailed patient health history or having a patient complete the Patient Health Questionnaire-9 (PHQ-9) (1,3,4).
The PHQ-9 is a short questionnaire that can be completed in inpatient or outpatient settings, often on an electronic device, with questions about appetite, sleep, concentration, and self-harm. Patients can rate their thoughts on these questions from not at all to nearly daily, indicating the possible severity of depression.
Since depression can also overlap with other mental health conditions, such as anxiety, schizophrenia, and chronic fatigue, it is important to also ask the patient questions about their mood, diet, sleep, and health in addition to having them complete the PHQ-9 (1,3,4).
Advanced Health Assessment Skills
Depression is such a common, chronic health condition affecting millions of people, so it can be under-recognized or misinterpreted as another health condition. When considering a formal diagnosis for depression, it is important to take a detailed patient history and also other conditions that can affect mood, such as thyroid complications, head trauma, nutritional deficiencies, electrolyte imbalances, symptom duration and onset, infection history, chronic health history, substance use, and more (1).
For instance, while a decreased interest in activities or changes in sleep patterns can be signs of depression, those can also be signs of thyroid abnormalities, Vitamin B12 deficiency, or substance use.
In addition, depressive symptoms can also be common side effects of other medications as well, such as hormonal contraception, pain medications, or antipsychotic medications. Furthermore, changes in the ability to concentrate or mood changes could be related to another mental health condition, such as attention-deficit/hyperactivity disorder (ADHD) or bipolar disorder (1).
Key considerations for advanced health assessment skills and performing a differential diagnosis for depression include:
- Obtaining blood work, such as a complete metabolic panel (CMP), complete blood count (CBC), vitamin levels (specifically D and B12), iron and folate levels, and a complete thyroid panel
- Obtaining a detailed, honest patient history of substance use (including marijuana, tobacco, stimulants, and alcohol use), recent and historical trauma (sexual abuse, head trauma, car accidents), and medical history (all current and prior medication use, existing health conditions)
- Obtaining an infectious disease screening panel to include HIV, COVID-19, and syphilis
- Asking questions about mental health in general to screen for other mental health conditions, such as asking if a patient sees or hears hallucinations, has sudden mood changes, or has had any mental health concerns in the past
Upon examination and lab work result completion, it is important to consider a referral to a mental health specialist, such as a psychiatrist, mental health specializing health care provider, or therapist for a consultation. When lab work shows lab values, you can discuss these results with the patient and discuss findings of any possible health concerns (1).
Depression screening needs to be considered for every annual visit (including adult, geriatric, and pediatric patients), every pregnancy visit, and as needed. Oftentimes, in several busy healthcare settings, depression screenings are not completed or performed because of a lack of staff and lack of time. However, this results in missed opportunities for earlier intervention, detection, and management of depression and other health conditions.
If you are not comfortable with diagnosing or screening for depression, you can be honest with your patients and also refer them to specialty care as well (1).
Depression Management Options
Because of the wide clinical presentation of depression and the wide range of age groups affected by depression, there are several depression management options. From medications to therapies and lifestyle interventions, depression is a chronic health condition with several management options and more options being studied. (1, 2, 3, 4)


Self Quiz
Ask yourself...
- What depression screenings do you use presently?
- What are some health conditions that can have similar clinical presentations of depression?
- What are some clinical labs you can use to rule out other possible causes of depressive symptoms?
Depression Recovery Paths
What Are the Options for Depression Recovery?
Depression recovery is often non-linear and complex. Many people with depression consider suicide, develop co-morbid health conditions, and report a decreased quality of life (1). Depression management options include prescription medications, therapy options, lifestyle modifications, and more. Many healthcare providers will recommend an antidepressant medication as a first-line option in addition to a therapy option, such as a referral for psychotherapy. Depending on patient presentation and response to medication, patients might need to return multiple times to manage their medication dosage, frequency, route, or new medication entirely (1,3,4,5).
In addition, medications for depression have a wide range of side effects, which is something to consider as an option for depression recovery. It is also important to educate patients that recovery from depression is often life-long and requires extensive time and effort. Oftentimes, medication alone is not enough to manage depression, and lifestyle modifications and therapies are needed as well (1).
How and Where Are Depressive Management Methods Used?
Medications for depression management are used in America and around the world in pediatric, adult, and geriatric populations. Medications can be taken by mouth as a pill, capsule, or liquid oral solution. Therapies, such as psychotherapy or group therapy, can be done in person or online depending on the mental health provider's ability. The role of telehealth has also increased access to mental health services in rural and underserved areas, making depressive management more accessible in these communities as well (1,3,4).
What Is the Average Cost of Depression Management?
Cost for depression management can significantly vary depending on the type of medications used, insurance, dosage, frequency, and other factors. Cost is among a leading reason why many patients cannot maintain their medication or therapy regime (6). If cost is a concern for your patient, consider reaching out to your local pharmacies or patient care teams to find cost effective solutions for your patients. Consider also looking into telehealth therapy options for your patients or in collaboration with your place of work as well.
Common Depression Medications
Depression has a wide variety of medication management options. Some of the most common medication management options for depression include:
- Selective serotonin reuptake inhibitors (SSRIs). Commonly known SSRIs include sertraline, fluoxetine, fluvoxamine, citalopram, escitalopram, and paroxetine.
- SSRIs are among the first line of depression medication management options and the most widely prescribed antidepressants because of their cost, medication administration route, and side effect profile.
- SSRIs have a method of action of inhibiting the reuptake pumps for serotonin, causing serotonin levels and absorption in the body to vary, causing changes in mood.
(1,3)
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Commonly known SNRIs include milnacipran, venlafaxine, desvenlafaxine, duloxetine, and levomilnacipran.
- SNRIs have a method of action of inhibiting the reuptake pumps for serotonin and norepinephrine, causing serotonin and norepinephrine levels and absorption in the body to vary, causing mood changes.
(1,3)
- Atypical antidepressants. Commonly known atypical antidepressants include bupropion.
- Bupropion has a method of action of inhibiting the reuptake pumps for dopamine and norepinephrine, causing dopamine and norepinephrine levels and absorption in the body to vary, causing mood changes.
(1,3)
- Tricyclic antidepressants (TCAs). Commonly known TCAs include amitriptyline, desipramine, imipramine, mirtazapine, clomipramine, doxepin, and nortriptyline.
- TCAs have a method of action of inhibiting the reuptake pumps for serotonin and norepinephrine, causing serotonin and norepinephrine levels and absorption in the body to vary, causing changes in mood. (1,3)
- Because of TCAs' more serious side effect profile and incidence of toxicity, TCAs are often not a first-line medication prescribed for depression or often prescribed by providers who are not extensively knowledgeable of mental health medications.
(1,3)
- Monoamine oxidase inhibitors (MAOIs). Commonly known MAOIs include phenelzine, tranylcypromine, isocarboxazid, and selegiline.
- MAOIs have a method of action of inhibiting the reuptake pumps for serotonin, dopamine, and norepinephrine, causing serotonin, dopamine, and norepinephrine levels and absorption in the body to vary, causing mood changes. (1,3)
- Because of MAOI’s more serious side effect profile and incidence in toxicity, MAOIs are often not a first-line medication prescribed for depression or often prescribed by providers who are not extensively knowledgeable of mental health medications.
(1,3)
While these are among the most common types of medications for depression, most of these medications also have other indications as well, such as management for anxiety or nerve pain. It is important to consider other possible conditions a patient has that can be affected by these medications, in addition to cost, ease of access, and medication administration route.
While these medications are among the most common for depression management, they also come in various dosages. It is often recommended to start a patient on the lowest dosage possible and monitor the patient for symptom alleviation or changes. Some patients will respond well to the lowest dosage of an SSRI, while others will respond better to a higher dose of an SNRI (1,3,4,5).
When tapering a patient off of a medication to try another medication or discontinue medication therapy entirely, it is recommended to do so slowly. Patients tapering off or switching from one antidepressant to another can have severe side effects, such as serotonin syndrome, psychological changes, and physiological changes (1,3).
Because of the possibility of severe negative side effects when tapering off or stopping antidepressant medications, monitoring is essential. Before prescribing a medication, consider patient preference, other medication use, allergies, medication administration route, possible caregiver and family education, and patient overall health in determining your first possible medication option.
Common Depression Medication Side Effects
All medications have a risk of side effects, and antidepressant medications are no exception. Common medication side effects for medications for depression include weight changes, sleep changes, mood changes, headache, dry mouth, vision changes, rash, tremors, eating habit changes, and GI upset (1,7). Specific side effects of medications for depression include:
- Selective serotonin reuptake inhibitors (SSRIs)
- SSRIs have additional possible side effects of sexual dysfunction (such as vaginal dryness, erectile dysfunction, vaginal pain, decreased ability to orgasm), QTc prolongation, and jaw pain.
- Serotonin-norepinephrine reuptake inhibitors (SNRIs)
- SNRIs have additional possible side effects of increased blood pressure, diaphoresis, and possible bone absorption.
- Atypical antidepressants
- Bupropion has a possible side effect of seizures and has a contraindication for patients with a history of seizures or suspected seizures.
- Tricyclic antidepressants (TCAs)
- TCAs have additional possible side effects of urinary changes (specifically urinary retention), constipation, QRS prolongation, orthostatic hypotension, and seizures.
- It is also recommended to avoid TCAs in patients with a history of cardiovascular complications, such as heart disease, because of the risk of QRS prolongation and orthostatic hypotension.
- Monoamine oxidase inhibitors (MAOIs)
- MAOIs have additional possible side effects of increased potential for serotonin syndrome compared to other antidepressant medications.
In 2004, the Food and Drug Administration (FDA) issued a black box warning for SSRIs and other antidepressant medications because of the possible increased risk of suicidality in pediatric and young adult (up to age 25) populations. When considering SSRI use in patients under 25 and knowing MDD is a risk factor for suicidality, having a conversation with the patient about risks versus benefits must be considered. However, in the past several years since the FDA's warning, there is no clear evidence showing a correlation between SSRIs and the increased risk of suicidality (7). Healthcare providers’ professional discretion and patient condition should guide therapy. Consider your patient's health history and needs before prescribing any medication.
Common Depression Medication Alternatives
While prescription medications are often among the first-line options for depression management, they are often prescribed in conjunction with non-pharmacological management options. Common non-pharmacological management options for depression include psychotherapy, physical exercise, electroconvulsive therapy (ECT), vagus nerve stimulation (VNS), and transcranial magnetic stimulation (TMS). meditation, yoga, mindfulness exercises, over-the-counter supplements, and more (1,3).

Self Quiz
Ask yourself...
- What are some common medications that can be prescribed to help manage depression?
- What is the difference between SSRIs and MAOIs?
- How does cost influence someone's access and ability to manage their depressive symptoms?
Common Non-Pharmacological Depression Management Options
One of the most complementary non-pharmacological management options for depression is psychotherapy, such as cognitive behavioral therapy (CBT) or interpersonal therapy. Given the COVID-19 pandemic, telehealth psychotherapy, also known as virtual therapy, has become increasingly popular, leading to a surge of online therapy options for several age groups and populations typically hard to reach with traditional office visit times.
Patients can opt-in for psychotherapy to meet with a licensed mental health professional, such as a licensed clinical social worker or psychologist, to discuss their depressive symptoms and emotional state. Often, healthcare providers can work with therapists to determine a plan of care and monitor patients' responses to medication therapy.
In addition, while psychotherapy is often prescribed to help people with depression, therapy can also be done for families, couples, friends, and other social settings. Therapy's cost can vary by insurance, location, and provider, so if cost is a concern, that is something to address with a patient.
Physical Exercise and Depression
One of the most complementary non-pharmacological management options for depression is physical exercise, which can include walking, running, doing yoga, and performing mindful exercises. Many times, when patients (and other health care providers) hear of physical exercise, they think of someone running on a treadmill for an hour a day for a few times a week. While that is one way to do physical exercises, there are thousands of ways to do physical exercise and activity. It is important to provide realistic, evidence-based information to patients and realize that not everyone is going to go run on a treadmill for an hour every day.
Educating patients on walking in nature for 5-10 minutes a day, doing some at-home yoga for 15 minutes a few times a week with some free videos online, or taking a class once a week at a local gym are simple, straightforward steps for physical exercise. With the rise of free online fitness videos, there are multiple ways for people who are limited in time, money, or mobility to perform fitness from the comfort of their homes. While some people might enjoy physical exercise in the presence of others, other people might find more ease in fitness and exercise in a more private setting (8).
Many times, people with depression feel that physical exercise is prescribed when they might be experiencing symptoms of trouble eating, trouble concentrating, and sleeping. It is appropriate to use clinical judgment and patient-friendly language when discussing physical exercise as a possible option for helping with depressive symptoms (8).

Other Methods: ECT, VNS, TMS, OTC Supplements and Depression
Less used non-pharmacological methods to help with depression include ECT, VNS, TMS, and OTC supplements. ECT, also known as electroconvulsive therapy, is what it sounds like. ECT involves electric shocks into the brain in a healthcare setting, often in psychiatric institutions. ECT is more commonly used for seizure management but can be used for patients who have not responded to other types of depression management, for patients who are unable to take any medications, or for patients who are experiencing extreme depressive symptoms. VNS, also known as vagus nerve stimulation, is also what it sounds like. Similar to ECT, VNS uses electric shocks to the brain via vagal nerve stimulation. VNS involves electric shocks into the vagal nerve in a health care setting, often in psychiatric institutions (1).
VNS is not often a first-line option for depressive management, but it is a possible option for people who have not responded to other types of depression management, for patients who are unable to take any medications, or for patients who are experiencing extreme depressive symptoms (1).
TMS, also known as transcranial magnetic stimulation, is a type of electrical stimulation using magnets to send electrical currents throughout various parts of the brain. Similar to ECT and VNS, it is not a first-line option and uses electricity to help with brain function. TMS is a possible option for people who have not responded to other types of depression management, for patients who are unable to take any medications, or for patients who are experiencing extreme depressive symptoms. TMS involves electric shocks into the vagal nerve in a healthcare setting, often in psychiatric institutions (1).
Because of the specialized equipment and staff needed for ECT, TMS, and VNS, they are rarely used as first-line options for depressive management and are often used when other options have failed. These options are also often found in specialized psychiatric centers, which are often in major cities, presently a barrier for transportation, cost, and access for those in rural areas or with limited transportation options. Cost for ECT, TMS, and VNS can also vary significantly depending on the number of treatment sessions needed, the duration of sessions, the frequency of sessions, and patient response to these therapies (1,6).
In addition to these mechanical non-pharmacological options, there are several OTC supplements, such as magnesium and serotonin supplements, that patients can try as well. While these medications are not regulated by the FDA, for patients to limited access to health care, these are often their first-line options given their ease of access and affordability. Because of the ease of access to OTC supplements, it is important to obtain a detailed medication history prior to prescribing any medications to avoid possible complications of serotonin syndrome and medication interactions (1,6).

Self Quiz
Ask yourself...
- Why would a patient prefer to use non-pharmacological options instead of pharmacological options for depressive symptom management?
- What is the difference between ECT and VNS?
- What sort of physical exercises can be done to help with depressive symptoms?
Nursing Considerations
Nurses remain the most trusted profession for a reason, and nurses are often pillars of patient care in several healthcare settings. Patients turn to nurses for guidance, education, and support. While there are no specific guidelines for the nurses' role in depression education and management, here are some suggestions to provide quality care for patients with a current or suspected history of depression.
- Take a detailed health history. Oftentimes, mental health, such as depressive thoughts or anxiety, are often dismissed in health care settings, even in mental health settings. If a patient is complaining of symptoms that could be related to depression, inquire more about that complaint. Ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient's complaint is not being taken seriously by other healthcare professionals, advocate for that patient to the best of your abilities.
- Review medication history at every encounter. Sometimes, in busy clinical settings, reviewing health records can be overwhelming. While millions of people take medications, many people take medications and are no longer benefiting from the medication. Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to their medication history. Make sure to specify if the patient is taking any over-the-counter supplements or herbs as well.
- Ask about family history. If someone is complaining of symptoms that could be related to depression, ask if anyone in their immediate family, such as their parent or sibling, experienced similar conditions.
- Be willing to answer questions about mental health and medication use. Society stigmatizes open discussions of prescription medication and mental health. Many people do not know about the benefits and risks of depression-related medications, the long-term effects of unmanaged depression, or possible treatment options. Be willing to be honest with yourself about your comfort level discussing topics and providing education on medication and health conditions. If you are not comfortable discussing something, please refer to another staff member.
- Communicate the care plan to other staff involved for continuity of care. For several patients, depression management often involves a team of mental health professionals, nurses, primary care specialists, pharmacies, and more. Ensure that patients' records are up to date for ease in record sharing and continuity of care.
- Stay up to date on continuing education related to medications and mental health conditions, as evidence-based information is always evolving and changing. You can then present your new learnings and findings to other healthcare professionals and educate your patients with the latest information. You can learn more about the latest research on medications and mental health by following updates from evidence-based organizations.
Unfortunately, it is not possible to look at someone with the naked eye and determine if they have depression. APRNs can identify and diagnose if someone has depression by taking a complete health history, listening to patient's concerns, having patients complete the PHQ-9 questionnaire, and communicating any concerns to other health care professionals (1,3,4).
Nurses can recommend self-monitoring for patients with depression, especially regarding medication side effects. Patients should know that anyone has the possibility of experiencing side effects on antidepressant medications, just like any other medication. Patients should be aware that if they notice any changes in their mood, experience any sharp headaches, or feel like something is a concern, they should seek medical care.
Because of the social stigma associated with mental health and antidepressant use, people are hesitant to seek medical care because society has normalized side effects interfering with quality of life and fear of being dismissed by health care professionals (1,3,5). However, as more research and social movements discuss mental health and mental health medication use more openly, there is more space and awareness for medication use and mental health.
Nurses should also teach patients to advocate for their health to avoid the progression of depression and possible unwanted medication side effects. Here are important tips for patient education in the inpatient or outpatient setting.
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors)
- Tell the health care provider of any existing lifestyle concerns, such as alcohol use, other drug use, sleeping habits, diet changes, menstrual cycle changes (need to identify lifestyle factors that can influence medication use and depression management)
- Tell the health care provider if you notice any changes in your mood, behavior, sleep, sexual health (including vaginal dryness or erectile dysfunction), or weight (possible changes that could hint at more chronic side effects of medication use)
- Tell the health care provider if you have any changes in urinary or bowel habits, such as increased or decreased urination or defecation (potential risk for medication malabsorption or possible unwanted side effects)
- Tell the nurse of health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your mental health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality is a possible side effect for medication use or worsening depressive symptoms)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options or surgeries
- Tell the health care provider if you notice any changes while taking medications or on other treatments to manage your depression (potential worsening or improving mental health situation)
What should families and caregivers know about depression?
Families and caregivers should know that depression is a chronic health condition that can require extensive medical intervention and support. Some people will need more support than others, and everyone will respond to medications differently. Because of the non-linear trajectory of depression, it is important to be realistic of your expectations when caring for someone with depression (1).


Self Quiz
Ask yourself...
- What are some problems that can occur if medications are not managing major depressive disorder symptoms adequately?
- What are some possible ways you can obtain a detailed, patient-centric health history?
- What are some possible ways nurses can educate patients on medication options for depression?
Upcoming Research
There is extensive publicly available literature on depression via the National Institutes of Health and other evidence-based journals. If a patient shows interest in participating in clinical trial research, they can seek more information on clinical trials from local universities and healthcare organizations.

Self Quiz
Ask yourself...
- What are some reasons someone would want to enroll in depression-related clinical trials?
Conclusion
Depression management, treatment, and recovery are complex processes for people. While there are several medical interventions and guidelines, depression can vary in clinical presentation and response to therapies from person to person, making this condition extremely personalized in management, assessment, and care. Depression management is often a lifetime process that involves several medical interventions, assessments, follow-ups, appointments, therapies, medications, and people professionally and within one's social circle. Education and awareness of different management options and different clinical presentations of depression can influence the lives of many people healthily.
Case Study
Stephanie is a 32-year-old woman working as an accountant. She arrives for her annual exam at her primary care next to her place of work. She says she's been feeling more tired over the past few months. Stephanie reports having some trouble sleeping and eating but doesn't feel too stressed overall. She has a history of pre-diabetes before pregnancy, gestational diabetes during pregnancy earlier, and gave birth a few months ago.
She is currently not taking medication but was put on insulin briefly when she was giving birth a few months ago. Stephanie reports taking some over-the-counter magnesium from her local drug store, but that has not helped her sleep. She also thinks she might have some depression because she looked at some forums online and resonated with a lot of people's comments.

Self Quiz
Ask yourself...
- What are some specific questions you'd want to ask about her mental health?
- What are health history questions you'd want to highlight?
- What lab work would you suggest performing?
Stephanie heard one of her friends talk about SSRIs for depression and wants to try them, but she's never taken prescription medications long-term before. She doesn't know if she has postpartum depression or if she's just stressed and tired of being a new mom. She agreed to complete blood work today and scored an average PHQ-9 score. She said that no one in her family talks about mental health, but she heard about depression from her friends recently and family a long time ago.
Before leaving this visit, you prescribe Stephanie sertraline 25mg once a day and want her to follow up in 6 weeks to see how she is doing. You also recommend that she see a therapist, as Stephanie reports she has never been to therapy. She denies thinking about hurting herself or others.

Self Quiz
Ask yourself...
- How would you discuss Stephanie's mental health concerns?
- How would you explain to Susan the influence of lifestyle, such as sleep, diet, postpartum, and environment, on mood?
- What side effects would you educate Stephanie on?
- How would you educate Stephanie on self-monitoring while on a new medication?
Stephanie returns to your office three months later, and she reports that she found a good therapist online who specializes in women's health issues and has availability in the evenings. Her therapist diagnosed her with postpartum depression, and she sees her therapist weekly. Her lab work shows AIC 6 with no other abnormalities, but Stephanie is still reporting trouble sleeping and also reports pain during sex as well. She wants to know if these can be related to the serotonin changes and if there are other options for her depression.

Self Quiz
Ask yourself...
- Knowing Susan's concerns, what are some possible other pharmacological and non-pharmacological management options for her postpartum depression?
- What other specialists would you refer Stephanie to?
Differential Diagnosis of Depression
Introduction
Erectile dysfunction (impotence) is a complex condition affecting males over the age of 40, with its incidence rising worldwide and marked by a persistent or recurrent inability to achieve and maintain an erection sufficient for satisfactory sexual activity [1]. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), defines erectile dysfunction (ED) as a condition that persists for a minimum of six months and specifies that the symptoms must be present in at least 75% of sexual encounters and must cause significant distress to the individual [2][3].
In the U.S., erectile dysfunction (ED) impacts at least 12 million men [4]. Numerous regulatory mechanisms participate in maintaining normal erectile function with disruptions in any of the penile arteries, nerves, hormone levels, smooth muscle tissue, corporal endothelium, or tunica albuginea—alone or in combination—leading to erectile dysfunction (ED) [5]. ED can arise from vascular, neurological, psychological, and hormonal disorders and often associated with health issues including diabetes mellitus, hypertension, hyperlipidemia, obesity, testosterone deficiency, and treatments for prostate cancer [5]. In addition, certain medications and substances can also trigger or exacerbate ED. Identifying the underlying causes is fundamental for effective treatment. The psychological and emotional impacts of ED are significant, affecting both the individual and their partner. If not addressed, ED can lead to anxiety, depression, reduced self-esteem, and strained interpersonal relationships [5].
A wide range of treatment options are available for managing ED. These include oral phosphodiesterase type 5 inhibitors, hormone replacement therapies, external vacuum devices, urethral suppositories, intracavernous injections (in the base of the penis), topical gels, surgical interventions, and sex therapy [5][6]. The evaluation and treatment of ED emphasizes the role of an interprofessional team in managing this condition. The revised five-question International Index of Erectile Function provides a quick clinical tool for assessing ED. The goal of this tool is to facilitate the automated scoring of The International Index of Erectile Function (IIEF), also referred to as the SHIM Questionnaire [7][8].
Differential Diagnosis
Erectile dysfunction (ED) is a complex condition with a variety of underlying causes, necessitating a thorough differential diagnosis to tailor treatment. The initial differential diagnoses for ED would be hypogonadism, loss of libido, depression with low mood, and other psychological conditions [5]. ED may be the first manifestation of diabetes or cardiovascular disease, as well as depression [5][8][9]. Differentiating between true erectile dysfunction and other sexual disorders, such as premature ejaculation, is essential and accomplished by obtaining a good sexual history of the patient.
Differential diagnoses to consider include:
- Abdominal Vascular Injuries
- Cirrhosis Imaging
- Depression
- Hemochromatosis
- Hypertension
- Hypogonadism
- Hypopituitarism (Panhypopituitarism)
- Noncoronary Atherosclerosis
- Peyronie's Disease
- Scleroderma
- Sickle Cell Disease (SCD)
- Type 2 Diabetes Mellitus
Causes of ED can be categorized into several types: psychological (including performance anxiety, stress, and relationship problems), endocrine (such as hypogonadism, hyperprolactinemia, thyroid disorders, and diabetes mellitus), neurogenic (including spinal cord injuries, multiple sclerosis, Parkinson's disease, stroke, and peripheral neuropathy), and vascular (such as atherosclerosis, hypertension, peripheral artery disease, and heart disease) [8][10][11][87].
Anatomical causes can include Peyronie’s disease, characterized by a curvature of the penis due to fibrous scar tissue, and congenital penile abnormalities [12]. Medication-related causes often involve antihypertensives (e.g., beta-blockers), antidepressants (SSRIs), antiandrogens used in prostate cancer therapy, diuretics, and antipsychotics [13] [14]. Lifestyle factors include smoking, excessive alcohol consumption, obesity, and a sedentary lifestyle which can play a significant roles, as do surgical or traumatic causes including trauma to the pelvic region or spinal cord [15]. Conducting a thorough history and physical examination, alongside appropriate laboratory tests, is necessary. This approach helps identify the underlying cause of ED, allowing for the most effective treatment plan, addressing any reversible causes, and enhancing overall health outcomes.

Self Quiz
Ask yourself...
- What are the numerous factors that contribute to erectile dysfunction (ED)?
- How can the process of differentiating erectile dysfunction (ED) from other conditions improve the effectiveness of treatment plans for patients?
- How does understanding the various causes of erectile dysfunction (ED) influence the approach to diagnosis and treatment?
Diagnostic Considerations
In addition to conditions considered in the differential diagnosis, it is essential to evaluate for other significant health issues that might contribute to erectile dysfunction. These include cancer and its treatments, epilepsy, multiple sclerosis, Guillain-Barré syndrome, Alzheimer's disease, epispadias, widower syndrome (e.g. Takotsubo cardiomyopathy (TCM) – broken heart syndrome), performance anxiety, malnutrition, leukemias, and the effects of various medications such as antidepressants, antipsychotics, antihypertensives, antiulcer drugs, and those used to treat hyperlipidemia [15][16][17].
For the diagnosis and management of erectile dysfunction, the Process of Care Model provides a structured approach suitable for primary care and multidisciplinary settings [18][19]. This model includes a rational approach to diagnosis and treatment, emphasizes thorough clinical history taking and a focused physical examination, mandates specialized testing and referrals in specific scenarios, and advocates a stepwise management approach that prioritizes treatment options [19]. It also emphasizes incorporating the needs and preferences of the patient and their partner into the decision-making process. This model encourages patients and their partners to express their preferences for reasonable and appropriate treatment options and collaboratively implement these with their physician. The model is data-driven, evidence-based, and applicable to a wide array of healthcare providers, reflecting contemporary management practices for erectile dysfunction (ED) [19].
The revised model (2018) emphasizes the modification of risk factors and the correction of comorbidities associated with ED as key components of patient management [19], including positive lifestyle changes, dietary improvements, and increasing physical exercise. First-line medical therapies should accompany these lifestyle modifications, including sexual counseling and therapy, which consider patient sexual dynamics, and pharmacotherapy with phosphodiesterase type 5 inhibitors (PDE5Is) [15].
The revised model underscores the essential role of healthcare providers in the assessment and treatment of men presenting with erectile dysfunction. According to the model, the initial assessment should comprise a comprehensive clinical history, a targeted physical examination, and specific laboratory tests. Subsequent management should be goal-oriented, considering the needs and preferences of both the patient and their partner [19]. The stepwise treatment algorithm prioritizes criteria such as ease of administration, reversibility, relative invasiveness, and cost.

Self Quiz
Ask yourself...
- What role do specific medications play in contributing to erective dysfunction (ED)?
- How does the Process of Care Model for diagnosing and managing ED emphasize the importance of incorporating patient and partner preferences?
Medications that Can Cause Erectile Dysfunction
Medications and substances that may cause or contribute to erectile dysfunction include a variety of drug classes and substances. Chronic analgesics such as opiates can affect erectile function [94]. ED can also be caused by anticholinergics, tricyclic antidepressants, and anticonvulsants like phenytoin and phenobarbital [20]. Antidepressants, including lithium, monoamine oxidase inhibitors, selective serotonin reuptake inhibitors, and tricyclic antidepressants, may contribute to ED. Antihistamines, such as dimenhydrinate, diphenhydramine, hydroxyzine, meclizine, and promethazine, are known to have similar effects [20][21].
Antihypertensives, including alpha blockers, beta blockers, calcium channel blockers, clonidine, methyldopa, and reserpine, can contribute to erectile dysfunction [20][21]. Anti-Parkinson agents including bromocriptine, levodopa, and trihexyphenidyl also play a role. Cardiovascular agents such as digoxin, disopyramide, and gemfibrozil, as well as cytotoxic agents like methotrexate [20][21][91]. Diuretics, including spironolactone and thiazides, can affect erectile function [20][21].
Hormonal treatments, including 5-alpha reductase inhibitors, corticosteroids, estrogens, luteinizing hormone-releasing hormone agonists, and progesterone, are also contributing factors [20][21]. Illicit drugs, alcohol, and nicotine, including amphetamines, barbiturates, cocaine, heroin, and marijuana can impact erectile function [22]. Immunomodulators such as interferon-alfa and tranquilizers, including benzodiazepines, butyrophenones, and phenothiazines, are known to contribute to erectile dysfunction [20][21][22][23].

Self Quiz
Ask yourself...
- How do various classes of medications, such as antidepressants, antihypertensives, and antihistamines, contribute to erectile dysfunction?
- How can healthcare providers address the potential impact of medications, substances, and illicit drugs on erectile dysfunction when developing a comprehensive treatment plan for patients?
Medical and Sexual History
A detailed knowledge of the physiological, neurological, and molecular dimensions of ED is vital for devising effective treatments and for further advancements in our understanding of this condition. Gathering a detailed medical and sexual history is an initial step in diagnosing erectile dysfunction (ED). A health care provider should inquire about numerous aspects including a patient’s confidence in achieving and maintaining an erection, the firmness of their erections suitable for intercourse, their ability to maintain an erection throughout sexual activity, and their overall satisfaction with their sexual experiences. Providers should ask about morning erections, level of sexual desire, frequency of climax or orgasm, and any ejaculatory functions [25]. A comprehensive history will help a provider understand the potential underlying factors of an individual’s ED, revealing any related diseases or treatment side effects and diagnosing issues related to sexual desire, erection, climax, or ejaculation.
Information about any surgeries or medical treatments that could have impacted nerve or vascular health near the penis is also fundamental [24]. Providers should gather details about any medications, whether prescription or over the counter, as well as the use of substances like illegal drugs, alcohol, or tobacco [22].
A healthcare professional may also delve into psychological or emotional factors that could contribute to ED by asking personal questions or utilizing a questionnaire. Questions directed to the patient’s sexual partner may help to better understand relationship dynamics that could affect ED.

Self Quiz
Ask yourself...
- How does a detailed understanding of erectile dysfunction (ED) contribute to advancements in managing this condition?
- Why is gathering a comprehensive medical and sexual history essential in diagnosing erectile dysfunction?
Advanced Physical Assessment
A physical examination can identify physical causes of ED. This includes assessing the sensitivity and appearance of the penis, which can indicate nerve or structural issues, such as those caused by Peyronie’s disease [12]. The examination should explore signs of hormonal imbalances including abnormal hair growth or breast enlargement and check vascular health through blood pressure and pulse measurements in your wrists and ankles [26][27]. The patient’s history should focus on gathering relevant information that might indicate prostate cancer or predisposing factors. Advanced nursing health assessment for prostate cancer is a meticulous process that requires a comprehensive evaluation, which encompasses taking a detailed patient history, conducting a thorough physical examination, and utilizing appropriate diagnostic tests [28]. Key areas include urinary symptoms such as difficulty starting urination, weak urine flow, frequent nocturnal urination, pain during urination, presence of blood in urine or semen, painful ejaculation, and pain in the lower back, hips, or thighs [28].
A thorough documentation of any family history of prostate cancer or other cancers, as this can increase risk. The medical history should also note any previous cancers, surgeries, or health conditions that might affect prostate health. Questions about lifestyle factors such as diet, physical activity, smoking, and alcohol use are also important, as these can influence the risk of prostate cancer [28]. A provider should palpate the prostate gland (digital rectal exam) through the rectal wall to check for irregularities in size, shape, or texture [37]. A general assessment of the patient’s overall health should include height, weight, height, body mass index (BMI), and visible signs of distress [28]. This comprehensive approach ensures that providers consider all aspects of the patient's health, leading to a more accurate differential diagnosis and effective treatment planning of ED.
Sexual history questions include inquiries about the quality and duration of erections [29]. Additional questions focus on the duration an erection lasts, whether the penis feels numb or unusual, and if it loses rigidity during foreplay or when attempting vaginal penetration. It is also important to know if the penis stays erect until after penetration, which could indicate anxiety or a venous leak, and if morning erections are still occurring [29]. Questions regarding overnight erections include hardiness and if hardness varies from day to day.
It is also important to determine if there have been times when erections worked better, such as during masturbation or with an alternate partner, and how erectile rigidity compares during masturbation versus intercourse [29]. The history of normal erections and the onset of erectile troubles is critical. A sudden, unexplained onset of erectile dysfunction is often psychogenic [5]. Further questions address significant life changes that coincided with the start of erection trouble, including new relationships or medications. A history of traumatic sexual events, contraception use, previous treatments, and whether ejaculation and orgasm remain normal despite erection issues, including how hard the erection is at ejaculation [5].
Other pertinent information can include the patient’s general interest in sexual activity and how often intercourse would be desired if erectile dysfunction were not an issue. The partner's agreement with the frequency, awareness of the treatment-seeking, and willingness to become involved in treatment are also important. Questions should include the straightness or curvature of erections, problems with libido, interest, ejaculation, or orgasm, and the timeline of these symptoms [30].

Self Quiz
Ask yourself...
- How does a thorough physical examination contribute to identifying the physical causes of erectile dysfunction (ED)?
- Why is it important to gather detailed information about a patient's sexual history, lifestyle factors, and family history when diagnosing erectile dysfunction?
Testing
Laboratory Testing
Blood tests can help identify underlying conditions that might cause ED, such as diabetes, atherosclerosis, chronic kidney disease, or hormonal imbalances [31].
- Complete Blood Count (CBC) - May detect signs of anemia or other blood disorders that might be contributing to ED [35].
- Lipid Profile - Used to assess the risk of cardiovascular disease, which can affect blood flow and contribute to ED [36].
- Blood Glucose Levels - High glucose levels are indicative of diabetes, which is a common cause of ED due to nerve and blood vessel damage [38].
- Serum Creatinine and Kidney Function Tests - These tests evaluate kidney health, which can affect hormonal balances and blood flow, influencing ED.
- Liver Function Tests - Liver issues can affect hormonal balance, including levels of sex hormones, impacting erectile function [33].
- Testosterone Levels - Low testosterone (hypogonadism) can cause or contribute to ED [32].
- Thyroid Function Tests - Thyroid hormones regulate metabolism and can influence sexual function, so abnormalities may contribute to ED [34].
- Prolactin Levels - Elevated prolactin can indicate pituitary disorders that may lead to ED [39].
- PSA (Prostate-Specific Antigen) - Used to screen for prostate issues, including cancer, which can impact sexual function [42].
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH) - These are additional hormones assessed if there is a suspicion of pituitary or hypothalamic disease [40][41].
Imaging Tests
The cause of ED often involves multiple factors, including physiological and psychological issues. Various conditions, such as neurological and endocrine disorders and medication side effects, may contribute to ED. A thorough medical history and physical exam guide the management of ED, while imaging tests can help determine if there is an obvious underlying physiological causes.
A penile doppler ultrasound is a noninvasive test that measures blood flow in and out of the penis using high-frequency sound waves to create real-time images [43]. This test helps diagnose and monitor erectile dysfunction (ED), which can result from insufficient blood flow into the penis (inflow ED) or blood becoming trapped in the penis (outflow ED). A technician uses Doppler ultrasound to create color images that show blood speed and direction with a handheld device [43].
Ultrasonography is an effective imaging technique providing real-time visualization of normal anatomy and significant pathological changes related to erectile dysfunction (ED) [92]. Penile Doppler ultrasonography (PDUS) measures blood flow in the penis during and after an erection, aiding in diagnosing and evaluating ED and distinguishing between vascular and nonvascular causes [92].
Color Doppler ultrasonography (CDUS) can assess functional alterations in penile blood flow, such as those occurring in erectile dysfunction (ED) [43]. Color Doppler ultrasonography (CDUS) of the penis is a valuable tool for identifying vasculogenic ED and may also predict coronary vascular disease [43].

Self Quiz
Ask yourself...
- How can blood tests help in identifying the underlying causes of erectile dysfunction (ED)?
- Why is it important to evaluate kidney, liver, and thyroid function when diagnosing erectile dysfunction (ED)?
- Why is it important to perform a thorough medical history and physical examination in managing ED?
Additional Tests
Nocturnal Penile Tumescence (NPT) Test, although not a blood test, measures erections during sleep and can help distinguish between physical and psychological causes of ED [44][45]. Tumescence refers to the state of being swollen. Nocturnal erection tests involve wearing a device around the penis overnight to monitor erections during sleep, helping to determine any physical or psychological factors for ED [45].
For more detailed assessments, electronic monitoring devices can record erection firmness, number, and duration. The injection test involves administering medication into the penis or into the urethra to induce an erection, assessing the erection’s fullness and duration to help pinpoint the cause of ED [24]. These tests are critical in guiding healthcare professionals in determining the appropriate interventions for managing ED.


Self Quiz
Ask yourself...
- What insights can imaging tests, such as the penile dopper ultraound, provide regarding the vascular and nonvascular causes of ED?
- How can the Nocturnal Penile Tumescence (NPT) test, which measures erections during sleep, help distinguish between physical and psychological causes of erectile dysfunction?
Pathophysiology
Various classification systems for erectile dysfunction (ED) are based on different criteria. Classification of ED can be based on its underlying causes, such as diabetic, iatrogenic (caused by medical treatment), or traumatic origins [5]. Other classifications focus on the neurovascular mechanisms that play a role in the erectile process, dividing ED into categories like failure to initiate (neurogenic), failure to fill (arterial), or failure to store (venous) blood [46].
Hemodynamics and Mechanism of Erection and Detumescence
The smooth muscles within the corpora cavernosa, along with the smooth muscles of arteriolar and arterial walls, play a critical role in the erection process [47]. These muscles remain contracted in a flaccid state, allowing minimal arterial flow for nutritional purposes [47]. Upon sexual arousal, neurotransmitters released from cavernous nerve terminals induce muscle relaxation, resulting in increased arterial blood flow and arteriolar dilation [47]. This influx of blood expands the sinusoids, trapping blood and compressing the venular plexuses, thereby reducing venous outflow [47][48]. The stretching of the tunica albuginea further decreases venous outflow by occluding emissary veins, which increases intracavernous pressure and elevates the penis into an erect position [47][48]. Subsequent muscle contractions may enhance erection rigidity, influenced by the penis's size and anatomical attachments.
The dynamics in the corpus spongiosum and glans penis differ from those in the corpora cavernosa [48]. During erection, these areas experience less venous occlusion due to their thinner tunica coverage, functioning similar to an arteriovenous shunt during peak erection [48]. This mechanism contributes to the engorgement and pressure in the glans and spongiosum.

Self Quiz
Ask yourself...
- How do different classification systems for erectile dysfunction (ED) enhance treatment of the condition?
- How do the dynamics of venous outflow contribute to the process of achieving an erection?
- How do the mechanisms of blood flow and pressure in the corpus spongiosum and glans penis differ from those in the corpora cavernosa during erection?
Neuroanatomy and Neurophysiology of Penile Erection
The triggers of penile erection in humans include auditory, visual, olfactory, tactile, and imaginative stimuli with reflexogenic and psychogenic stimuli acting through the sacral parasympathetic routes [66][67]. Multiple sites within the brain and spinal cord, along with the coordination of somatic and autonomic pathways, make sexual behavior, including erection, vulnerable to neurological injury and disease [66]. The brain and spinal cord work together to process, coordinate, and distribute the neural inputs necessary for sexual behavior, including erection [66]. Activation of neurons in certain regions, either pharmacologic or through electrical stimulation, links to penile tumescence [67].
Peripheral and autonomic pathways innervate the penis, which integrate signals from the spinal cord and peripheral ganglia to regulate neurovascular events during erection and detumescence [47]. Both sympathetic and parasympathetic autonomic nerves, along with somatic sensory and motor nerves, play crucial roles in this regulatory process [47].
In males, physiological sexual arousal begins with an erection, initiated by sensorial signals transmitted by the dorsal nerve of the penis after stimulation of nerve endings along the penis and glans [67]. Penile hemodynamics during erection involve the swelling of the cavernous bodies due to vasodilation, caused by nitric oxide released by the endothelium following parasympathetic stimulation of the pelvic nerves [49][67]. The pelvic, cavernous, and pudendal nerves of the sympathetic nervous system, along with various vasoconstrictor factors mediate detumescence (subsidence of a swelling) [67].
Molecular and Clinical Understanding of Erectile Function
Advances in molecular biology and clinical research have enhanced the understanding of erectile function, emphasizing the role of nitric oxide and the relaxation of intracavernous smooth muscle [49]. This relaxation is important for increasing blood flow and reducing venous outflow, both essential for maintaining an erection [49]. Ongoing research into the pathways regulating smooth muscle relaxation and contraction continues to contribute to the development of therapeutic strategies for treating erectile dysfunction (ED).

Self Quiz
Ask yourself...
- How do various sensory stimuli initiate the process of penile erection?
- How do the sympathetic and parasympathetic autonomic nerves coordinate to regulate the neurovascular events during erection and detumescence?
- How have advances in molecular biology and clinical research improved our understanding of the role of nitric oxide in the relaxation of intracavernous smooth muscle?
Statistical Evidence / Etiology
Erectile dysfunction (ED) often arises from multifactorial causes. It is important to distinguish whether the condition stems from psychological factors or has an organic basis. The 1994 Massachusetts Male Aging Study (MMAS) found that 52% of men experience some degree of ED, with 10% being impotent [50]. Medication-related ED occurs in 25% of cases due to blood pressure medications [14]. Vascular disease is the leading cause of natural ED, with 35% to 75% of men with diabetes also suffering from ED [38]. Up to 40% of men with renal failure and 30% of men with chronic obstructive pulmonary disease (COPD) have ED [51]. Smoking and illicit drug use are more prevalent among younger men with ED [27][30]. Obesity and diabetes account for 8 million cases of ED, and the majority (79%) of men with ED are overweight [52]. 40% of men with ED also have hypertension, and 35% of men with hypertension experience ED [5]. In addition, 42% of men with ED suffer from hyperlipidemia [5].
Undiagnosed diabetes (28%) in three times as common in men with ED when compared to men without ED (10%) [53]. Among men over 50, those with diabetes have twice the risk of ED (46%) compared to those without diabetes (24%), with the risk increasing with the duration and severity of diabetes [52][54]. Furthermore, one-third of diabetic men experience hypogonadism, a condition linked to ED [52][54]. Up to 35% of men with ED also suffer from hypogonadism, and about 6% have abnormal thyroid function [34]. While testosterone deficiency can affect erectile function, vascular disease and diabetes are much more common causes of ED [32][52][54].
Obesity increases ED risk by 50% compared to men of normal weight, and one-third of obese men with ED who join a weight loss program see their symptoms resolve within two years. [15]. Bariatric surgery for obesity can improve sexual performance [58]. Smokers who quit experience a 25% improvement in erectile quality after one year [55]. Heavy alcohol use also increases the risk of ED due to direct toxicity to the corporal endothelium, loss of smooth muscle tissue, and early neuropathy [5].
There is a strong correlation between benign prostatic hyperplasia (BPH) with lower urinary tract symptoms (LUTS) and ED, with up to 72% of men with symptomatic BPH also experiencing ED [56]. Men with depression have a 40% higher chance of having ED, and those with ED have three times the chance of being depressed [57]. In addition, 30% to 60% of men with ED experience premature ejaculation [59].
Worldwide, experts project the prevalence of ED to rise to 322 million men by 2025 [60]. In the United States, about 30 million men experience ED, and estimates show that 1 in 10 men will face ED at some point in their lives [61]. In an international study, the U.S. reported the highest self-reported rate of ED at 22%, while Spain reported the lowest at 10% [62].

Self Quiz
Ask yourself...
- How do multifactorial causes, such as psychological factors, organic bases, and lifestyle choices, contribute to the prevalence of erectile dysfunction (ED)?
- What role do conditions like diabetes, hypertension, obesity, and smoking play in the development of erectile dysfunction (ED)?
Cardiovascular Disease and Erectile Dysfunction
Erectile dysfunction (ED) is an early sign of cardiovascular disease [63]. Therefore, healthcare providers should assess men with ED for cardiovascular risk factors to prevent future major adverse cardiovascular events (MACE) [63]. Studies show that 50% of men with diagnosed coronary artery disease have ED [63]. The similarity in size between coronary and penile cavernosal arteries means that atherosclerosis in the penile arteries precedes coronary artery symptoms, making ED a potential indicator of cardiovascular issues [5]. Patients with ED can exhibit subclinical atherosclerosis for up to a decade before any overt cardiac symptoms [64]. Younger men with unexplained ED have an up to 50-fold increase in cardiovascular risk later in life compared to age-matched controls [65].
Traditional risk factors are not present in all individuals at high cardiovascular risk, as a considerable proportion of MACE occurs in men who appear free of risk factors [68]. In men with ED, it is important to consider both traditional and unconventional risk factors. Several parameters from a thorough clinical assessment of men with ED have proven to be valuable predictors of MACE [65]. These include family history of cardiometabolic events, alcohol abuse, fatherhood, decreased partner’s sexual interest, severe impairment in erection during intercourse or masturbation, impaired fasting glucose, increased triglycerides, obesity even without metabolic complications, decreased penile blood flow, or impaired response to an intra-cavernosal injection test [5][65]. Recognizing these risk factors can help identify men with ED who may benefit from a stricter lifestyle or pharmacological interventions to minimize their cardiovascular risk. Addressing these risk factors in men with ED who face elevated risk reduces cardiovascular risk and improves erectile function.
Impact of Prostate Cancer Treatment on ED
Post-operative ED is common in prostate cancer patients, with different treatments having varying impacts. Up to 85% of patients undergoing radical prostatectomy may experience ED, compared to a 25% rate in those receiving definitive radiation therapy [68]. Since the cavernous nerves responsible for erection can take 18 to 24 months to heal after radical prostatectomy (RP), natural erections through sexual stimulation and nocturnal erections may be absent during this recovery period [68]. Under normal physiologic function, erections pull oxygen-rich blood into the penile tissue, maintaining its health. Men who cannot achieve natural erections post-RP do not oxygenate their penile tissue, which can lead to atrophy and permanent structural changes [69]. This may result in venous leak, which is irreversible and causes erectile dysfunction [69]. Innovations in surgical techniques, such as nerve-sparing procedures, have lowered the incidence of post-operative ED.
Controversial Role of Cycling
The impact of cycling on ED remains debated. Traditional racing bicycle seats may exert considerable pressure on perineal nerves and blood vessels, contributing to ED [70]. A meta-analysis indicated a significantly higher risk of ED among cyclists compared to non-cycling controls [71]. A comprehensive understanding of the multifactorial nature of ED aids clinicians in delivering effective treatment and reassurance to patients, allowing them to address both psychological and organic components.

Self Quiz
Ask yourself...
- How can recognizing erectile dysfunction (ED) as an early indicator of cardiovascular disease influence the approach healthcare providers take in assessing cardiovascular risk factors in men with ED?
- How do different prostate cancer treatments, such as radical prostatectomy and radiation therapy, affect the likelihood of post-operative erectile dysfunction (ED)?
- How does the use of traditional racing bicycle seats contribute to erectile dysfunction (ED) in cyclists?
Pharmacotherapy & Mechanical Treatments
Initial treatment for erectile dysfunction (ED) focuses on enhancing overall health through lifestyle modifications, which not only improve erectile function but also reduce cardiovascular risk. Select each treatment based on its specific applications, benefits, potential side effects, and the patient's needs, preferences, and medical history. Proper education on the use and potential risks of these therapies is crucial to ensure safety and effectiveness.
Lifestyle Changes
Recommended lifestyle changes include increasing physical activity, adopting a Mediterranean diet or seeking nutritional counseling, and quitting smoking, drugs, and excessive alcohol consumption [15]. Healthcare providers should review and adjust the patient’s medication regimen to eliminate or reduce the impact of drugs that may cause or worsen ED.
Supplements
Pharmacological treatments for erectile dysfunction (ED) offer effective options for improving sexual function and quality of life in affected men. L-arginine, an amino acid supplement, is essential for producing nitric oxide synthase, which generates nitric oxide—a key molecule in erectile function. Supplementation with L-arginine (1500 mg to 5000 mg daily) has shown some effectiveness in treating mild to moderate ED by boosting nitric oxide synthase levels [5][49][67].
Topical Gels
Eroxon, a proprietary topical gel, is the only over-the-counter product with FDA endorsement for treating ED. The De Novo medical devices classification approved Eroxon on June 13, 2023 [72]. It is the first over the counter treatment for ED in the U.S. that does not require a doctor's prescription [72]. It contains ingredients such as carbomer, ethanol, glycerin, propylene glycol, and potassium hydroxide. Application of the gel to the glans penis provides a cooling effect that stimulates nerve endings and warms the tissue, thereby enhancing blood flow and relaxing the smooth muscles in the corpora cavernosa. This aids in achieving and maintaining an erection. Eroxon has shown a 60% success rate within 10 minutes of application, increasing to 75% after 20 minutes, which is comparable to the efficacy of prescribed oral agents [5]. Eroxon gel is available in the United Kingdom and Belgium, with its release in the U.S. pending.
Oral Medications
Oral PDE-5 inhibitors, such as sildenafil, tadalafil, vardenafil, and avanafil, are the first-line treatment for ED due to their effectiveness across various causes including cardiovascular disease, diabetes, and hypertension [73]. Tadalafil offers a theoretical benefit over sildenafil due to its longer half-life and pharmacokinetics, but there is insufficient data to make any formal recommendation [5]. These drugs work by enhancing the relaxation of cavernosal smooth muscle through the prolongation of cyclic GMP effects [73]. These medications require sexual stimulation to work. While PDE-5 inhibitors are effective, they can cause side effects such as headaches, nasal congestion, and visual disturbances [73]. Rare but serious side effects include non-arteritic anterior ischemic optic neuropathy (NAION), which can lead to permanent vision loss, and sudden hearing loss [74].
Patients who do not respond to one PDE-5 inhibitor may benefit from trying another, as differences in drug metabolism and patient response can influence effectiveness. For those who fail initial PDE-5 inhibitor therapy and have not had their testosterone levels checked, assessing, and treating hypogonadism with testosterone supplementation may be beneficial in conjunction with continued PDE-5 inhibitor therapy [75].
PDE-5 inhibitors work by enhancing the effects of nitric oxide, a natural chemical produced by your body that relaxes muscles in the penis [5][49][67][75]. This relaxation increases blood flow, enabling you to achieve an erection in response to sexual stimulation. It is important to note that for patients taking a PDE-5 inhibitor; sexual stimulation is necessary to release nitric oxide from your penile nerves. PDE-5 inhibitors amplify signals, facilitating normal penile function in some individuals. The medications differ in dosage, duration of action, and potential side effects. Common side effects include flushing, nasal congestion, headache, visual changes, backache, and stomach upset [76].
External Vacuum Devices
External vacuum devices provide a non-surgical treatment option. These devices use negative pressure to engorge the penis with blood, and a constriction band maintains the erection [77]. They are effective but require practice for optimal use. A penis pump (vacuum erection device) is a hollow tube with a hand-powered or battery-powered pump. Patients place the tube over the penis, then use the pump to remove the air inside the tube. This creates a vacuum that pulls blood into the penis. Once the patient receives an erection, individuals place a tension ring around the base of the penis to hold in the blood and keep it firm. Bruising of the penis may occur, and the band will restrict ejaculation [78].
Intraurethral and Intracavernous Therapies
Intraurethral and intracavernous therapies offer alternatives when oral medications are insufficient. Intraurethral prostaglandin E1 (alprostadil) pellets and intracavernous injections of agents like prostaglandin E1 or combination therapies (TriMix or QuadMix) can induce an erection by enhancing smooth muscle relaxation and blood flow within the penis [79]. This method involves using a fine needle to inject alprostadil (Caverject, Edex) into the base or side of the penis [79]. These combination medications, known as bimix when they include two medications and trimix when they include three, treat ED. Administer each injection to create an erection lasting no longer than an hour. Side effects include mild bleeding from the injection, prolonged erection (priapism), and the formation of fibrous tissue at the injection site [79].
Alprostadil intraurethral therapy involves placing a tiny alprostadil suppository inside your penile urethra [80]. A special applicator inserts the suppository into the urethra. The erection starts within 10 minutes and, when effective, lasts between 30 and 60 minutes. Side effects can include a burning sensation in the penis, minor bleeding in the urethra, and the formation of fibrous tissue inside the penis [80].
Penile Implants
Penile implants involve placing devices into both sides of the penis. These implants consist of either inflatable or malleable (bendable) rods [81]. Inflatable devices allow you to control when and how long you have an erection, while the malleable rods keep your penis firm but bendable. Healthcare professionals should try other methods before considering penile implants [81]. However, implants have a high degree of satisfaction among those who have tried and failed more conservative therapies.
Surgeries
Surgeons perform penile revascularization on a small subgroup of patients, estimated at 5% of all ED cases. [5]. Consideration for this procedure includes younger patients (under 30) with ED following pelvic or perineal trauma that results in an isolated vascular injury [37]. Penile doppler ultrasound and a formal arteriogram must demonstrate arterial insufficiency [5]. The revascularization operation involves anastomosing the inferior epigastric artery to the dorsal artery of the penis or directly to the corpus cavernosum, though long-term results are marginal [5].
Surgeons perform arterial balloon angioplasty for focal arterial stenosis of the pudendal (supply blood to the main organs of the pelvic area) or penile arteries [82]. However, the improvement does not last due to arterial narrowing and restenosis unless using drug-eluting stents [82]. This therapy is not yet the standard of care and is helpful in patients with focal, identifiable arterial stenosis in vessels large enough to accept a stent.
Venous ligation surgery for veno-occlusive dysfunction involves embolizing or ligating the penile veins, such as the deep dorsal vein [83]. Long-term results do not show lasting efficacy [83].
Shockwave Therapy
Low-intensity shockwave therapy has shown efficacy in patients with severe ED not responding to PDE-5 inhibitors [84]. Its presumed mechanism of action includes improved cavernosal hemodynamics, induction of endothelial cell proliferation, and activation of endogenous stem cells, as well as penile revascularization [84][86]. Shockwave therapy increases angiogenic factors that promote neovascularization, restore smooth muscle activity, and attract stem cells [84][85]. This therapy also increases vascular endothelial growth factor, neuronal nitric oxide synthase, and other natural bioactive agents [84][85] [86]. Although the exact mechanism of shockwave therapy remains unclear, its effect is dose-dependent, with 3000 pulses per session yielding better results than 1500 or 2000 pulses [86].
Stem Cells and Plasma
Intracavernous stem cells and platelet-rich plasma therapy are promising but experimental and require more investigation.
Rehabilitation and Combination Therapies
Several studies are examining penile rehabilitation therapy after radical prostatectomy surgery, suggesting a benefit, but there is no consensus on the exact treatment selection, duration, or timing [5][87]. The majority of published studies suggest that a combination of PDE-5 inhibitors with external vacuum device therapy offers the best results, although intraurethral pellet therapy and intracavernous injections have been successful [89]. Patients should begin penile rehabilitation treatment early, continuing for up to one year after surgery, though the exact timing lacks study [90].
The most effective treatment options for erectile dysfunction in spinal cord injury patients are phosphodiesterase 5-inhibitors and intracavernous drug injections [88]. The choice of treatment should consider factors such as residual erectile function, the location of the spinal cord injury, and the patient's comorbidities.


Self Quiz
Ask yourself...
- How do lifestyle modifications impact erectile function and cardiovascular health?
- What are the mechanisms by which oral PDE-5 inhibitors, like sildenafil and tadalafil, improve erectile function?
- What factors should guide the choice of treatment for individual patients with erectile dysfunction (ED)?
Conclusion
Erectile dysfunction (ED) affects men of all ages, with higher prevalence in those over 40 [4]. Men in their 40s have a 40% chance of experiencing ED, and this likelihood increases by about 10% each subsequent decade [93]. The prevalence of ED is rising with at least 12 million men in the U.S. affected [4]. The causes of ED are diverse, encompassing psychological, neurological, hormonal, vascular, and lifestyle factors [8][10][11][87]. Common associated conditions include diabetes mellitus, hypertension, hyperlipidemia, obesity, and testosterone deficiency [5]. Identifying the underlying causes is crucial for effective treatment.
The psychological and emotional impacts of ED are significant, affecting both individuals and their partners [5]. If not addressed, ED can lead to anxiety, depression, reduced self-esteem, and strained interpersonal relationships. Various treatment options are available, ranging from lifestyle modifications and first-line medical therapies, such as PDE-5 inhibitors, to more invasive options like penile implants and intracavernous injections [15][73]. Providers should tailor treatments to the patient's specific needs, preferences, and medical history, with a focus on safety and effectiveness.
The Process of Care Model for ED management underscores the importance of a structured, stepwise approach to diagnosis and treatment. It emphasizes the role of healthcare providers in guiding patients through lifestyle changes, psychosexual counseling, and appropriate pharmacotherapy. By adopting this comprehensive model, healthcare professionals can address both the physiological and psychological aspects of ED, improving overall health outcomes and patient satisfaction.
When evaluating and treating erectile dysfunction (ED), it is important to inquire about sexual health in all adult patients using a non-threatening and non-judgmental approach. Clues to psychological causes of ED include a sudden onset of symptoms, high variability in erectile function, good morning erections, and good erections with masturbation or alternate partners [5]. Refer psychogenic sexual disorders to appropriate mental health providers.
There is no specific testing for ED, but blood panels including morning testosterone level, CBC, CMP, liver and renal function tests, lipid panel, HgbA1c, and TSH are reasonable. A thorough understanding of the multifactorial nature of ED, combined with a structured approach to diagnosis and treatment, can significantly enhance the quality of care for men with ED. This approach not only improves erectile function but also addresses associated comorbidities and psychological impacts, leading to better overall health and quality of life for patients.
Differential Diagnosis of Pneumonia
Introduction
Pneumonia is an acute respiratory disease diagnosed in patients of all ages and populations. Individuals with comorbidities or in specific age groups are at an increased risk of developing pneumonia. There are varying symptoms of pneumonia, including an atypical presentation, which can make diagnosing pneumonia sometimes difficult. Therefore, healthcare providers must understand the typical and atypical symptoms of pneumonia, along with potential differentials and overlapping health conditions. The purpose of this course is to equip learners with the knowledge and expertise related to pneumonia. It reviewed the statistical evidence, pathophysiology, and etiology of pneumonia. Readers will also read about advanced health assessment practices and diagnostics reasoning to help determine the likelihood of possible differential diagnoses. Lastly, pharmacological treatment and follow-up monitoring of patients with pneumonia are discussed.
Definitions
- Community-acquired pneumonia (CAP): Pneumonia developed outside of a hospital. This includes health centers, nursing homes, rehabilitation, assisted living, skilled nursing facilities [8, 11].
- Hospital-acquired pneumonia (HAP): Pneumonia developed within a hospital setting. Diagnosis must be made 48 hours after admission, and symptoms were not present during the time of admission [8].
- Ventilator-associated pneumonia (VAP): Pneumonia that develops after endotracheal intubation within 48 hours [8].
- Atypical pneumonia: Sometimes also called “walking pneumonia,” where symptoms are not typical and tend to be milder. Identified pathogens are not the common causes [8].
Statistical Evidence
Pneumonia impacts individuals of all ages and populations. The World Health Organization reports that pneumonia is the “single largest infectious cause of death in children worldwide.” In 2019, pneumonia accounted for about 14% and 22% of deaths in children under 5 years of age and between 1 and 5 years old, respectively. Additionally, children living in southern Asia or sub-Saharan Africa are more likely to die from pneumonia [15].
The Centers for Disease Control and Prevention (CDC) estimates that around 1.4 million are diagnosed with pneumonia in the U.S. annually, with most visits occurring in the emergency room. Furthermore, just over 41,000 Americans die annually from pneumonia, which equates to about 12.3 deaths per 100,000 people [1].
According to the CDC, influenza and pneumonia were ranked as the 9th and 13th leading causes of death in the United States for 2020 and 2021, respectively [2]. Furthermore, preliminary 2023 estimates for the U.S. show that influenza and pneumonia rank as the 11th leading causes of death, accounting for approximately 13.5% of deaths per 100,000 [3].

Self Quiz
Ask yourself...
- What is the epidemiology of pneumonia in the United States?
- Which age groups is pneumonia more prevalent in?
Pathophysiology
While the respiratory tract's primary responsibility is to exchange oxygen and carbon dioxide, it also helps filter bacteria and other potentially harmful pathogens from entering the body. Similar to other body systems, like the gastrointestinal tract and integumentary system, the respiratory system has a balance of organisms and immune defenses, both innate and acquired. When there’s a breakdown in the body’s natural defenses, pathogens can enter the lung alveoli, and immune macrophages respond and attempt to clear the new pathogen. The macrophages signal to other molecules and cytokines, triggering an inflammatory response. By signaling neutrophils and T cells to respond at the site, capillary permeability is increased, creating inflammation and, thus, causing pneumonia to develop [8].
Risk Factors
Several factors increase the likelihood of certain individuals developing pneumonia. Major risk factors include [10].
- Age, 2 years old or younger
- Age, 65 years or older
- Environmental conditions, like crowded areas or air pollution
- Smoking
- Drug and alcohol use, which weakens the immune system
- Individuals who are immunocompromised, like people with HIV, AIDS, or bone marrow disorders
- People with chronic respiratory conditions, like asthma, COPD, or cystic fibrosis
Certain medical conditions, like diabetes, liver disease, and heart failure, also increase risk. Additionally, people with impaired swallowing ability or those who’ve had a stroke or head injury are also at a higher risk [10].

Self Quiz
Ask yourself...
- What is the pathophysiology of pneumonia?
- What are the risk factors of pneumonia?
Etiology and Classification
Pneumonia has three underlying causes or etiologies: bacteria, viruses, and fungi. The most common cause of pneumonia in adults in the U.S. is bacteria, with Streptococcus pneumoniae being the most common organism, followed by Staphylococcus aureus. Furthermore, different bacteria can cause usual or atypical presentations of pneumonia. For example, the bacteria Mycoplasma pneumonia causes an atypical presentation of pneumonia, also called “walking pneumonia” [8, 10].
Viruses can also contribute to developing pneumonia. In adults, influenza, parainfluenza, and rhinovirus are the top causes, while in children, respiratory syncytial virus (RSV) is the leading cause. The SARS-CoV-2 virus causes COVID-19 disease, which often contributes to developing COVID-19 pneumonia [8, 10].
Lastly, fungi and their spores can contribute to fungal pneumonia. In North America, Histoplasma, Coccidioides, and Blastomyces are common fungi causing pneumonia, while Aspergillus is the common cause of ventilator-associated pneumonia [8, 13]. For immunocompromised individuals, Pneumocystis jirovecii is a common fungal organism that causes pneumonia. Most healthcare providers refer to this type of pneumonia as PJP, formerly known as PCP pneumonia [10].
Many healthcare providers also classify pneumonia based on the clinical setting from which the initial source of infection was acquired. The three main types are ventilator-associated, community-associated, and hospital-acquired. Community-acquired pneumonia (CAP) is acquired from outside a hospital setting. If an individual develops pneumonia in their home or an outpatient facility, like assisted living or rehabilitation, it’s considered community-acquired [8].
Conversely, if a patient acquires pneumonia within a hospital setting 48 hours after admission, it’s considered hospital-acquired pneumonia (HAP). However, to be considered HAP, symptoms or incubation of pneumonia must not have been present during the time of admission. Lastly, ventilator-associated pneumonia (VAP) is like the name implies. VAP is pneumonia that develops 48 hours after endotracheal intubation [8].


Self Quiz
Ask yourself...
- What are the different types of pneumonia?
- What are the different etiologies of pneumonia?
Advanced Health Assessment
History and Physical
No matter the health setting where the diagnosis of pneumonia is made, the provider must complete a thorough history and physical assessment. Common signs and symptoms of pneumonia include:
- Fever or chills
- Lack of appetite or nausea
- Myalgias
- Fatigue or weakness
- Cough, with or without sputum production
- Shortness of breath [8].
Symptoms vary per patient, and some may have an atypical presentation. For example, fever, myalgias, and watery sputum are more correlated with viral pneumonia, while purulent or blood-tinged sputum may indicate bacterial etiology [8].
Conducting a thorough physical examination can aid in diagnosing pneumonia. Physical examination of patients with pneumonia often reveals tachycardia, tachypnea, and the presence of fever. Adventitious lung auscultation findings are typically present, like crackles, rales, or diminished breath sounds. Further lung evaluation may show consolation processes, such as decreased chest expansion, egophony, dullness to percussion, or increased tactile fremitus [8, 11].
Differential Diagnosis
When conducting a history and physical, providers should also formulate potential differential diagnoses. Reviewing the patient’s medications, health history, comorbidities, and family and social history is useful when considering additional differentials. For example, if a patient has a history of deep vein thrombosis, is not taking an antithrombotic, and presents with a cough and shortness of breath, the provider should consider a pulmonary embolism as a differential. Formulating differentials is also based on possible etiologies.
Differential diagnoses of bacterial pneumonia to consider include some of the following:
- Asthma
- Atelectasis
- Bronchitis
- COPD
- Lung abscess
- Respiratory failure
[7,11]
Differential diagnoses of bacterial pneumonia in children are different. The provider should consider diagnoses like asthma, croup, epiglottitis, or bronchiolitis in their differential [7,11]. For viral pneumonia, other differentials to potentially consider are pulmonary hypertension, pulmonary fibrosis, hyperreactive airway disease, and pulmonary edema [6]. For fungal pneumonia, possible differentials may be coal worker’s pneumoconiosis, neurogenic pulmonary edema, tuberculosis, and eosinophilic pneumonia [9]. While this list is not all-inclusive, it does provide valuable insight that providers should consider a vast array of possibilities when formulating possible differential diagnoses.
Diagnostic Tests
Diagnostics tests are useful to help make a diagnosis of pneumonia and can help reduce the likelihood of other health conditions. Initial tests are determined by the initial healthcare setting in which the patient is presenting and their acuity. Diagnostic tests to help make the diagnosis of pneumonia include [6,11].
- Chest X-ray: the appearance of pulmonary infiltrates or opacities helps support a pneumonia diagnosis. Specific lobes or interstitial infiltrates may indicate other disease processes, like heart failure or tuberculosis.
- Complete Blood Count (CBC) with differentials: an elevated white blood cell count (WBC) shows signs of infection. Bacterial pneumonia is correlated more with an elevated WBC than with viral.
- Complete Metabolic Panel (CMP): helps evaluate kidney function and assess for dehydration. Evaluating impaired kidney function is necessary when tailoring treatment plans.
- Inflammatory biomarkers: An increased erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) indicates inflammation. However, these tests can be non-specific [6,11].
While typically, the diagnosis of pneumonia can be initially made by correlating clinical findings with radiological and laboratory results, it can still sometimes be challenging to determine the likely etiology, especially for those with an unclear history. Thus, additional diagnostic tests are considered in the appropriate setting.
Additional tests may include [6,11]:
- Blood cultures: can help determine the presence of bloodstream pathogens, which in turn helps determine the appropriate antibiotics for treating bacterial or fungal pneumonia. However, blood cultures must be collected before any treatment medications are administered.
- Sputum analysis or culture: can also help determine possible etiology. These are especially helpful in an outpatient setting.
- Rapid antigen tests: certain rapid antigen tests can help identify viral pathogens, like RSV, herpes simplex virus, influenza, or coronavirus.
- Viral culture: if viral etiology is suspected, a viral culture may be necessary to identify the pathogen, especially when rapid antigen testing is not available for the specific virus.
- Chest CT: sometimes pneumonia may not be clear on chest X-ray alone, or another differential is highly suspected. A chest CT provides greater detail of lung processes and should be completed when a pneumonia diagnosis is unclear [6,11].

Diagnostic Reasoning and Critical Thinking
When considering the differential diagnoses of pneumonia, the healthcare provider should gather and analyze all of the pertinent data. The history of the present illness can provide valuable insight into the features of pneumonia and, most likely, its etiology. For example, if the patient reports a cough with blood-tinged sputum, myalgias, and a fever, bacterial etiology may be the most likely. However, if the patient lacks a fever and states they have a cough with blood-tinged sputum and shortness of breath, then a pulmonary embolism should also be added to the likely differential. On the other hand, patients with viral etiology, such as influenza, may have an initial sudden onset of symptoms like fever, myalgias, sore throat, fatigue, and nonproductive cough. Their symptoms may persist and develop into viral pneumonia over several days.
Providers should also consider the patient’s risk factors and known exposures. For instance, if the patient has a history of HIV and develops a fever, cough, dyspnea, and lower lung field crackles, then fungal pneumonia (more specifically, PJP pneumonia) should be suspected. Since the patient is immunocompromised, other pneumonia etiologies are still considered, like mycoplasma, tuberculosis, COVID-19, etc. [14]. Another example is a college student who lives in crowded dorms and develops myalgias, fever, and a cough. They are at risk for certain etiologies and types of pneumonia, like tuberculosis, COVID-19, or “walking pneumonia.”
Patient comorbidities should also be considered when determining the differential. For example, if they have a history of asthma and present with a cough and shortness of breath, then asthma should be considered as a lead possibility. Comorbidities, especially for those with CAP, also guide the treatment of pneumonia. For instance, a patient with a history of advanced COPD and a penicillin allergy will likely require fluoroquinolone. When compared to a healthy patient with no comorbidities or penicillin allergy, amoxicillin alone or plus a macrolide can be prescribed, depending on which current guidelines the provider follows [4].
The setting where the patient’s symptoms developed is also imperative when considering differentials. If a patient developed symptoms shortly after being intubated rather than at home, then the most likely etiologies will differ.
Additionally, the setting determines initial diagnostic testing. If a patient is located in an outpatient facility without STAT lab capabilities, an initial diagnostic workup may include a chest X-ray and point-of-care testing. For atypical pneumonia presentation, a sputum culture may be helpful, but the provider should consider if the cough is productive. Alternatively, in an emergency department setting, diagnostic testing may include a chest X-ray, CBC, and CMP.
Regardless of the setting, the provider should assess the patient’s overall condition and vital signs. If a patient’s oxygen saturation is 88% and temperature is 103°F in an outpatient facility, then immediately applying oxygen and transferring the patient to the hospital will be necessary. Once in the emergency department, the provider might consider ordering an arterial blood gas (ABG) and blood cultures along with the additional diagnostics mentioned above.
Whether ordering diagnostic tests in an outpatient or inpatient setting, appropriateness and cost incurred to the patient should also be considered. For example, if an outpatient urgent care provider suspects a healthy patient has CAP, then a chest X-ray may be the only test required for diagnosis. If the provider suspects viral etiology, like COVID-19 or influenza, they may want to order viral point-of-care testing. However, tests and workups may vary depending on the health facility, as some facilities have specific testing protocols.
Once a diagnosis of pneumonia is made, many healthcare providers also use the CURB-65 (confusion, uremia, respiratory rate, blood pressure, age greater than 65) scoring tool to guide the treatment setting. If the patient is confused, uremia symptoms are present or BUN is greater than 20 mg/dL, respiratory rate is greater than 30 breaths/minute, blood pressure is less than 90/60 mmHg, and they are older than 65, one point is given for each positive. For patients with a total score of one or less, they can likely be treated in an outpatient environment, 2 or more require hospitalization, and 3 or more intensive care admission [11].
The SMART-COP score is also useful in determining pneumonia severity in an emergency room or inpatient environment. It scores the patient’s systolic blood pressure, whether multi-lobar infiltrates are present, albumin levels, respiratory rate, presence of tachycardia, new-onset confusion, oxygenation status, and pH [11].

Self Quiz
Ask yourself...
- What are some possible differentials of pneumonia?
- Which tests can confirm pneumonia?
- What are some elements to consider when determining possible differentials?
Pharmacological Treatment
The treatment of pneumonia is determined by etiology and type and is further discussed below. Please note that these are general guidelines, and treatment plans should be tailored to each individual. As guidelines vary per medical organizational approach and are updated frequently, please refer to current practice guidelines.
Bacterial Pneumonia
For the treatment of CAP in a healthy individual who is less than 65 years old in an outpatient setting, amoxicillin monotherapy or amoxicillin plus a macrolide or doxycycline is used. If the patient is allergic to penicillin, a third-generation cephalosporin, like cefpodoxime, plus a macrolide or doxycycline can be prescribed. Or a macrolide or doxycycline alone can be used.
For patients with significant comorbidities, advanced age, and other risk factors that are not penicillin-allergic, prescribing amoxicillin-clavulanate plus a macrolide or doxycycline is recommended. If they are allergic to penicillin, a third-generation cephalosporin plus macrolide or doxycycline is recommended. For patients unable to tolerate penicillin or cephalosporins and with structural lung disease, respiratory fluoroquinolone is recommended. Again, this is determined by the approach and guidelines the provider is following. The provider should also consider local bacterial resistance rates, if any [4].
Treatment widely differs for patients with CAP who require hospital admission. Those without suspicion of methicillin-resistant Staphylococcus aureus (MRSA) or pseudomonas CAP may receive an intravenous (IV) beta-lactam antibiotic regimen or a fluoroquinolone alone. Patients with CAP and MRSA or pseudomonas risk factors may be started on an anti-MRSA medication (vancomycin or linezolid), aztreonam, and an aminoglycoside. Individuals presenting with symptoms of sepsis usually are started on an array of empiric IV antibiotics until the underlying organism is identified. Empiric antibiotic therapy regimens may vary depending on the healthcare facility and protocols [5].
Hospital-acquired or ventilator-associated cases of bacterial pneumonia are also treated with IV antibiotics. Initially, treatment is typically guided by hospital or healthcare facility-specific antibiograms. Once the sputum or blood cultures return, the antimicrobial selection is tailored to the specific bacterial organism causing the infection [12].
Viral Pneumonia
Supportive care is typically the mainstay of treatment of viral pneumonia. Patients should be encouraged to maintain or increase their hydration through oral intake. If they are intubated or unable to tolerate oral intake, IV fluids should be administered. Rest is another factor to promote. If required, oxygen supplementation and mechanical ventilatory support in an inpatient setting may be necessary.
Specific antiviral therapy is determined by the underlying viral etiology. Influenza is typically treated with oseltamivir or zanamivir, while RSV, parainfluenza, and adenovirus are treated with ribavirin. Herpes simplex virus and varicella-zoster virus cases of pneumonia are typically treated with acyclovir [6].
Fungal Pneumonia
Cases of fungal pneumonia are usually treated initially with amphotericin B. However, other antifungals, like fluconazole and ketoconazole, may be administered. In many instances, fungal pneumonia develops as an opportunistic infection. Providers should consider risk factors, such as immunosuppression, chemotherapy, bone marrow transplant, steroid use, and infected catheters, as potential causes of infection [9].
For patients with PJP, treatment options are outlined as outpatient versus inpatient. The first-line outpatient oral antifungal treatment is trimethoprim-sulfamethoxazole (TMP-SMX). For patients with a sulfa allergy, atovaquone alone or trimethoprim plus dapsone can be prescribed as an alternative. More severe cases of PJP require hospitalization with IV antifungals, where again, intravenous TMP-SMX is preferred as initial treatment. Moderate to severe cases may require treatment with pentamidine or primaquine. Corticosteroids are also given in an inpatient setting, especially for patients with HIV [14].


Self Quiz
Ask yourself...
- What are the recommended treatments for the different types of pneumonia?
Monitoring and Follow-up
Pneumonia can lead to a variety of complications. Thus, healthcare providers must monitor the patient’s health status for signs of clinical decompensation or deterioration. Complications to consider may include lung abscess, atelectasis, empyema, sepsis, multisystem organ failure, and acute respiratory failure. Heart complications, such as heart failure and pericarditis, may also develop. Bacteremia and sepsis may also develop, and patient death is another to consider [8,11].
Whether inpatient or outpatient, patients with pneumonia require follow-up. In an outpatient setting, providers should schedule a follow-up appointment within 24 to 48 hours of beginning treatment to assess the patient’s response. Vitals signs and overall patient condition are assessed. A repeat chest X-ray is not required for re-evaluation unless the patient’s condition does not seem to be improving.
Referral to pulmonology should also be considered, especially for patients with chronic lung conditions or resolved symptoms. Sometimes, patients may require additional diagnostic tests or hospitalization if symptoms are not improving with oral treatment [4].
Follow-up and monitoring in an inpatient environment will differ. The patient’s overall condition, including vital signs and hemodynamic stability, will be monitored. Upon diagnosis, the provider should also consider if the patient needs to be placed on isolation precautions, like droplet, airborne, etc. Depending on the patient's overall health condition, consultation with pulmonology, infectious disease, and intensive care is necessary.
Repeat chest X-rays and laboratory tests may be ordered daily as well to assess clinical response to therapy. Once the patient’s pneumonia begins to resolve with treatment, they are weaned from supplemental oxygen, and vital signs stabilize; convert them to oral treatment (if possible). Patient discharge planning should also continue. Upon hospital discharge, the patient should follow up with their primary care provider and pulmonologist within one week. They may also need to follow up with an infectious disease specialist [5].
Patients are also educated on pneumonia prevention strategies, such as receiving COVID-19, influenza, and pneumococcal vaccinations and seeking immediate care when symptoms develop [8,11].


Self Quiz
Ask yourself...
- What elements drive patient monitoring and follow-up?
Conclusion
Pneumonia can lead to serious health complications, especially if left untreated. Healthcare providers should recognize the signs and symptoms of pneumonia and understand the clinical features of each type. If there is clinical suspicion of pneumonia, additional diagnostics can help make the diagnosis. Additional testing may help rule up or down the likely etiology (bacterial versus viral versus fungal) and assess the patient’s overall acuity. Diagnostic reasoning and critical thinking are useful when creating a list of differentials and treatment options. Patient monitoring and follow-up are important aspects to consider as part of the patient’s treatment plan for both inpatient and outpatient environments. Education regarding prevention strategies is also helpful for future prevention.
Differential Diagnosis of Diabetes Mellitus
Introduction
According to the CDC (1), approximately 38.4 million people have diabetes, representing 11.6 percent of the United States population. An additional 97.6 million people over the age of 18 have prediabetes, representing 38% of the United States population. Untreated (or poorly controlled) Diabetes Mellitus has been shown to directly impact all facets of life, from work-related absenteeism and decreased productivity to chronic disability and premature mortality. This chronic medical condition is currently the 8th leading cause of death.
Early detection and appropriate treatment afford persons with diabetes the best health outcomes. While a diagnosis of diabetes may appear straightforward, many medical conditions can also mimic diabetes in terms of signs/ symptoms, and physical assessment findings. Secondary diabetes can also be caused by complications and side effects of other disease processes, including organ injury, hormonal disturbances, tumors, and medication side effects.
The goal of this CE program is to discuss various health conditions that can be misdiagnosed as diabetes, their specific assessment findings, and the necessary differential diagnosis to appropriately treat the actual underlying causes of hyperglycemia and diabetic-like symptoms.

Self Quiz
Ask yourself...
- As you begin this course, why do you think the rate of diabetes continues to rise?
- As a healthcare professional, what do you find most frustrating/ most rewarding in caring for patients with diabetes?
- Do you feel, as a healthcare professional, that people with diabetes are given appropriate education to successfully manage their condition?
- What is your current care plan for newly diagnosed persons with diabetes?
Confirmation Testing to confirm a diagnosis of diabetes (2)
The following laboratory blood tests are used to confirm a diagnosis of prediabetes/ diabetes. These common tests will also be performed in the diagnostic workup for secondary diabetes and hyperglycemia related to other medical conditions.
Glycated Hemoglobin (Hb) A1C/ A1C
- Normal range: less than 5.7%
- Prediabetes range: 5.7%-6.4%
- Diabetes range: 6.5% or higher
Fasting Blood Sugar / Fasting Plasma Glucose
- A blood sample is taken after the person has fasted overnight x 8 hours.
- Normal Range: below 100mg/dl
- Prediabetes Range: 100-125mg/dl
- Diabetes Range: levels greater than 126mg/dl; confirmation testing is done twice, on two separate occasions, especially if the person is asymptomatic. (3)
Two-Hour Oral Glucose Tolerance Test (OGTT)
- Plasma glucose levels are measured before and two hours after the ingestion of 75 grams of glucose.
- Normal Range: less than 140mg/dl
- Prediabetes Range: 140-199 mg/dl
- Diabetes confirmation: 200mg/dl or greater.
- Diabetes is confirmed with a glucose level greater than 200mg/dl.
- *Patients should not take any medications that may impact glucose tolerance, such as steroids, thiazide diuretics, statins, and beta blockers.
Random Plasma Glucose Testing (also known as casual glucose testing)
- Random glucose testing, in patients experiencing symptoms such as polydipsia, polyphagia and polyuria.
- Results plasma glucose levels greater than 200mg/dl are considered sufficient to diagnose diabetes (although many practitioners prefer additional screenings under more controlled circumstances).
Primary Types of Diabetes: Pathophysiology, Etiology, and Health Assessment Findings
Type 1 Diabetes Mellitus
T1DM accounts for approximately 5-10 percent of all diagnosed cases of diabetes mellitus in the United States. It is believed to be autoimmune; there is no direct link to the development of T1DM, and it most often occurs in children (age 4-9 years old) and early puberty (age 10-14 years old). (4), (5).
Symptoms of T1DM may include the following:
- Increased thirst
- Increased urination
- Extreme hunger, nausea, and vomiting
- Unintentional/unexplained weight loss
- Blurred vision
- Fatigue, mood changes and irritability
- Flu-like symptoms.
- Bedwetting in children who are already successfully potty-trained, frequent full diapers in infants.
- Slow healing cuts, sores
- Vaginal yeast infections
Risk factors for the development of T1DM (6)
- Family history of diabetes
- Genetic component
Diagnosis
Antibody testing includes: (7), (8)
One or more of the islet autoantibodies will be present in about 95% of those affected with autoimmune type 1 diabetes at the time of initial diagnosis. With type 2 diabetes, the autoantibodies are typically absent.
Five common diabetes-related autoantibody tests include:
- Islet Cell Cytoplasmic Autoantibodies (ICA)
- Glutamic Acid Decarboxylase Autoantibodies (GADA)
- Insulinoma-Associated-2 Autoantibodies (IA-2A)
- Insulin Autoantibodies (IAA)
- Zinc Transporter-8 Autoantibodies (ZnT8A)
Diabetic Ketoacidosis
DKA can occur as the result of untreated/ undertreated diabetes mellitus. Diabetic ketoacidosis is often the first emergent condition to occur that eventually leads to the confirmation of T1DM.
Symptoms include:
- Fruity-smelling breath; acetone breath.
- Abdominal pain, nausea, and vomiting
- Rapid respirations
- Drowsiness, confusion, altered levels of consciousness.
- Flushing of face
- Dry mucus membranes, dehydration
DKA confirmation
- Serum glucose level > 250mg/dl
- Arterial pH < 7.30
- Serum bicarbonate < 15mEq/l
- Ketonuria +
- Elevated anion gap (normal results 4-10 mEq/l) (9)
T1DM Treatment (10)
Referral to pediatric endocrinologist for long-term follow-up care. Normal growth and development will necessitate medication adjustments through childhood and adolescence.
Insulin therapy options available include the following:
- Multiple daily injections (MDI)
- Insulin pen
- Insulin pump
- Rapid-acting inhaled insulin
Glucose monitoring options available include the following:
- Glucose monitoring through a finger stick
- Continuous glucose monitoring (CGM) devices (skin sensors)
DSMES (Diabetes Self-Management Education and Support) / Carbohydrate counting/ diabetes emergencies and sick day management.
- Extensive individual and family/ family support system education to cover all aspects of diabetes self-management, including Section 504 under the Americans with Disabilities Act, to protect the rights of children with diabetes in the school system. (11), (12).


Self Quiz
Ask yourself...
Your pediatric patient has been admitted to the Emergency Department with newly diagnosed Type 1 diabetes mellitus. The parents are understandably upset and ask you “How did this happen” as there is no family history of diabetes. Consider appropriate family teaching currently.
- How do explain this newly diagnosed condition to the parents?
- What are the appropriate elements of family teaching at this time?
- What medical consultations would you initiate at this time?
- What are some high-priority follow-up appointments that a newly diagnosed diabetic pediatric patient should have?
Type 2 Diabetes Mellitus
According to the CDC (13), approximately 38 million Americans have diabetes and 90%-95% of them have Type 2 diabetes. Although Type 2 diabetes usually occurs in people over the age of 45, this medical condition can now be detected in younger adults, teenagers, and, sometimes, young children. The rates of childhood obesity are rising, and it is thought that the obesity rates (and lifestyle behaviors attributed to childhood obesity) are directly influencing rates of diabetes.
In Type 2 diabetes, insulin resistance is thought to be contributing to the increased development of diabetes. Conversely, Type 1 diabetes is considered an autoimmune disease process.
Risk factors (14)
- Prediabetes
- Overweight
- Are 45 years or older
- Have a parent, brother, or sister with type 2 diabetes
- Physically active less than 3 times a week
- History of gestational diabetes (diabetes during pregnancy) or given birth to a baby who weighed over 9 pounds
- African American, Hispanic, or Latino, American Indian, or Alaska Native person. Some Pacific Islanders and Asian American people are also at higher risk.
Symptoms of Type 2 diabetes (15)
- Increased thirst. (Polydipsia)
- Frequent urination. (Polyuria)
- Increased hunger. (Polyphagia)
- Fatigue.
- Blurred vision.
- Slow-healing sores and/or frequent infections.
- Numbness or tingling in the hands or feet.
- Areas of darkened skin, usually in the armpits and neck (known as acanthosis nigricans). (16)
Treatment (17, 18, 19)
- Lifestyle intervention; behavioral modifications
- Oral medications: Metformin usually first choice, followed by DDP-4 inhibitors, GLP-1, SGLT2 inhibitors, Sulfonylureas, TZDs
- Insulin therapy: for initial A1C greater than 10-12 %, consider insulin replacement therapy; for A1C >/- to 7.0% after 2-3 months of dual oral therapy. The initial prescription for Type 2 diabetes is once-daily basal insulin.
- DSMES patient/family education
- Dietary /nutrition consultation (calorie and/or carbohydrate controlled, depending on BMI and other comorbid conditions)

Self Quiz
Ask yourself...
Your patient has been diagnosed with Type 2 diabetes. He states he does not want to start medication to control his glucose level, preferring to treat his condition with “diet and activity” first.
- What are some recommendations regarding diet and weight loss guidelines for your patient with a BMI of 38%?
- How would these recommendations change if your patient had a BMI of 29%?
- Your newly diagnosed T2DM patient wants to pursue a “low carb lifestyle” to treat his condition, stating he heard “less than 20 grams CHO (carbohydrates) daily is optimal”.
- What dietary consultations do you currently order in your practice setting for newly diagnosed T2DM patients; and what nutritional guidelines would you advise this patient to follow (and to avoid)?
Gestational Diabetes
Pregnant women, with no personal history of diabetes should be tested for GDM at 24 to 28 weeks of gestation. The American Diabetes Association and American College of Obstetrics and Gynecology (ACOG), as well as the United States Preventive Services Task Force, recommend using either a 1-step or 2-step approach for diagnosing GDM. (20)
Testing
One-Step Strategy:
75 gm OGTT oral glucose tolerance testing
- Following an overnight fast.
- Blood samples are collected for 1 hour and 2 hours.
- GDM is diagnosed if fasting glucose meets or exceeds 92 mg/dl (5.1 mmol/l), 1-hour serum glucose of 180 mg/dl (10.0 mmol/l), or 2-hour serum glucose of 153 mg/dl (8.5 mmol/l).
Two-Step Strategy:
- Step one: Perform a 50-gram glucose challenge test irrespective of the last meal.
- If PG plasma glucose level at 1 hour after the load is greater than or equal to 140mg/dl (7.8 mmol/l), proceed to step 2.
- Step 2: 100g glucose OGTT is performed after overnight fasting.
- Cut-off values are fasting PG 95 or 105 mg/dl (5.5/5.8 mmol/l), 1-hour PG of 180 or 190 mg/dl (10.0/10.6 mmol/l), 2-hour PG of 155 or 165 mg/dl (8.6/9.2 mmol/l) or 3-hour PG of 140 or 145 mg/dl (7.8/8.0 mmol/l). GDM is diagnosed if two or more PG levels equal to or exceed these cutoffs.
Treatment
- Lifestyle behavioral changes (diet and physical activity)
- Routine blood glucose testing
- Insulin therapy for glucose regulation
- Frequent monitoring of gestational growth and development
Latent autoimmune diabetes in adults (LADA)
Latent autoimmune diabetes in adults (LADA) is a type of diabetes that develops slowly in adulthood and has signs of both type 1 and type 2 diabetes. LADA is also known as type 1.5 diabetes. (21), (22)
The Immunology for Diabetes Society (https://www.immunologyofdiabetessociety.com/) has specified three criteria for the diagnosis of LADA:
- Age greater than 35 years
- Positive autoantibodies to islet beta cells
- Insulin independence for at least the initial 6 months after initial diagnosis
A diagnostic screening tool with three criteria was used to identify LADA in diabetic patients older than 50 years of age:
- A low or normal BMI.
- Fasting blood glucose 270 mg/dl or higher, HbA1C 10% or greater despite good compliance.
- Loss of weight despite a diet constant in calorie content.
LADA versus Type 2 DM
T2DM has absent autoantibodies to islet cell components and does not need insulin for an extended period. Glucose control is often achieved by eliminating risk factors and dietary improvement. LADA screening should be considered in patients with T2DM who do not achieve adequate glycemic control within a reasonable period despite compliance to therapy, if they are not obese, lack the features of the MetS (metabolic syndrome), and the patient, nor their first-degree relatives, have other preexisting autoimmune disorders.
Symptoms usually start in people who have LADA when they are over 30, typically older than people diagnosed with Type 1 diabetes. In addition, the pancreas is still able to make some insulin at this point, which leads further to a diagnosis of Type 2 diabetes. Persons diagnosed with type 2 diabetes who are lean and physically active, or who have lost weight without effort, could have LADA.
First, LADA may be managed with lifestyle changes such as exercising regularly, losing weight, making healthy diet choices, and quitting smoking. As the body slowly loses its ability to make insulin; though, most persons with LADA eventually need insulin shots.
Maturity Onset Diabetes (MODY)
Also known as Maturity Onset Diabetes of the Young or monogenic diabetes, is a non-insulin dependent version of diabetes mellitus that usually occurs in young adulthood. It is thought to occur due to changes in a genetic mutation and may account for up to 5% of all confirmed cases of diabetes. MODY is often misdiagnosed as either Type 1 or Type 2 diabetes. MODY should be suspected in nonobese persons diagnosed with diabetes at a young age and have a strong familial history of diabetes.
MODY is most often an autosomal dominant disease and is divided into subtypes (MODY1 to MODY14) based on the causative genetic mutation. Subtypes 1 to 3 account for 95% of cases. Patients with MODY have preserved pancreatic beta-cell function three to five years after diagnosis, as evidenced by detectable serum C-peptide levels with a serum glucose level greater than 144 mg per dL and no laboratory evidence of pancreatic beta-cell autoimmunity. (24)
Patients with MODY1 and MODY3 have progressive hyperglycemia and vascular complication rates similar to patients with types 1 and 2 diabetes. Lifestyle modification including a low-carbohydrate diet should be the first-line treatment for MODY1 and MODY3. Sulfonylureas are the preferred pharmacologic therapy. Patients with MODY2 have mild stable fasting hyperglycemia with a low risk of diabetes-related complications and generally do not require treatment, except in pregnancy.
TYPE 2 DIABETES versus MODY
The pathophysiology of MODY involves impaired insulin secretion, whereas type 2 diabetes is characterized by insulin resistance and a progressive loss of beta-cell function.
Persons diagnosed with type 2 diabetes who have MODY may exhibit the following:
- Lack of response to metformin
- Larger drop in serum glucose level with sulfonylureas
- Greater sensitivity to insulin
Maturity-Onset Diabetes of the Young or MODY affects 1-2% of people with diabetes, although it often goes unrecognized. (25) The 3 main features of MODY are:
- Diabetes often develops before the age of 25.
- Diabetes runs in families from one generation to the next
- Diabetes may be treated by diet or tablets and does not always need insulin treatment.

Self Quiz
Ask yourself...
- What are some objective patient findings (such as BMI and age) that might make you consider a diagnosis of LADA versus Type 2 diabetes?
- What are some objective patient findings that might make you consider autoantibody testing for a patient with suspected diabetes?
Differential Diagnosis of DM
The following medical conditions frequently “mimic” diabetes-related symptoms (or cause secondary diabetes) and should be considered in the differential diagnosis of diabetes mellitus.
Metabolic Syndrome
Metabolic syndrome (also known as syndrome X or insulin resistance syndrome) is very common in the United States, with approximately 1 out of every 3 persons having the condition. (26)
Metabolic Syndrome refers to a group of medical conditions, occurring together, that increase a person’s risk for the development of heart disease, stroke, and type 2 diabetes. These five individual conditions include the following:
- Elevated blood pressure
- Elevated serum glucose level
- Excessive body fat accumulation in a person’s waist (abdominal obesity)
- Elevated serum cholesterol levels
- Elevated serum triglyceride levels
Risk factors (27)
- Age
- Ethnicity (increased rates of metabolic syndrome are noted in the female Hispanic population)
- Obesity/overweight
- Family history of type 2 diabetes; personal history of gestational diabetes
- Preexisting medical conditions, including nonalcoholic fatty liver disease, polycystic ovarian syndrome, sleep apnea
Complications (if left untreated):
- Insulin resistance, progressing to type 2 diabetes mellitus.
- Cardiovascular disease, including myocardial infarction and cerebral vascular accidents due to ongoing plaque development and arterial disease.
Diagnostic Criteria
The National Institutes of Health define metabolic syndrome as having three or more of the following conditions, including conditions that are currently being treated with prescription medication. (A patient history of hypertension, even well controlled with medications, would still be considered a positive (+) finding). (28)
| Condition | Female Patient | Male Patient |
| Waistline measurement | >35 inches | > 40 inches |
| Blood pressure reading | >130/85 mm Hg | >130/85 mm Hg |
| Fasting serum glucose level | >100mg/dl | >100 mg/dl |
| Serum HDL Cholesterol level | <50mg/dl | <40mg/dl |
| Serum Triglyceride level | >150mg/dl | >150mg/dl |
Lifestyle Recommendations
- Routine physical activity at least 30 minutes daily
- Weight loss reduces blood pressure and insulin resistance. Aim for 5-7 percent body weight loss.
- Dietary intervention- healthy diet intake with an emphasis on fresh fruits/vegetables, high fiber, lean protein, nutrient-dense foods, and lower sodium intake. Decrease intake of sugary-based foods and drinks, heavily processed or refined foods, and saturated and trans-fat foods. DASH diet or Mediterranean Diet
- Smoking cessation
- Stress management
- Proper sleep hygiene practices
Medication interventions (where applicable)
- Blood pressure medication
- Statin therapy to lower triglycerides and cholesterol levels
- Glucose lowering medications.


Self Quiz
Ask yourself...
- You are currently treating a patient whose fasting glucose level is 124mg/dl, suggestive of prediabetes.
- What patient education and follow-up care, if any, will be provided for this patient?
- How would this patient education change if the fasting glucose level was only two points higher at 126mg/dl, suggestive of diabetes?
Cushing Disease /Cushing Syndrome
Cushing disease is a rare condition in which the pituitary gland specifically makes too much adrenocorticotropic hormone (ACTH). It is typically found in the age group 20-50 years old, with women being diagnosed 3x more so than men. Cushing disease is the most common form of Cushing syndrome (29).
Conversely, Cushing syndrome can occur from excessive (external) cortisol levels related to corticosteroid usage. (30)
Symptoms (31):
- Roundness and redness of face/ facial appearance
- Hump formation on the back of the neck.
- Stretch marks are visible on the abdomen, chest, and armpit areas.
- Excessive facial hair growth
- Excessive bruising is noted on the skin.
- Weight gain, often rapid and unusual, to the abdominal area.
- Elevated blood sugar
- Increased thirst
- Increased urination
- High blood pressure (hypertension)
- Mood changes, anxiety, irritability, headaches
- Depression
- Increased number of infections
- Irregular menstrual periods
Diagnostics:
- Serum ACTH and cortisol level
- Urine cortisol level
- Saliva cortisol level
- MRI/CT to confirm the presence of pituitary adenoma.
Treatment options
- Medications for Cushing disease/syndrome include:
- Central-acting inhibitors of ACTH: Pasireotide (Signifor)
- Adrenal-directed inhibition of steroidogenesis: Medications in this category are used off-label for Cushing disease medications include ketoconazole, metyrapone, mitotane, and etomidate.
- Glucocorticoid receptor blockade: mifepristone (Mifeprex)
- Surgical removal of the tumor
- Targeted Radiation therapy
Corticosteroid-Induced Hyperglycemia
Steroid-induced diabetes (SID) is a unique situation where hyperglycemia occurs secondary to chronic use of steroid medications. As steroids interfere with glucose regulation and insulin metabolism, elevated serum glucose levels occur, often producing the typical diabetes symptoms of polyuria, polydipsia, and polyphagia.
Persons on long-term steroid therapy, as often seen in medical conditions such as COPD, are at an increased risk of developing SID. Studies have found that 86 percent of people on steroid therapy will experience at least one episode of hyperglycemia. (32)


Self Quiz
Ask yourself...
- What additional hyperglycemia surveillance testing/ screenings should be done on patients using long-term corticosteroids?
- Do you routinely check the glucose levels of patients on long-term steroids?
- What patient education should be given to patients on steroids regarding diabetes signs and symptoms?
Neuroleptic-Induced Hyperglycemia
Neuroleptic-induced diabetes, also known as antipsychotic-induced diabetes, may cause type 2 diabetes in people who take antipsychotic medications. Antipsychotic medication side effects include hyperglycemia and obesity, which increase the risk of diabetes. In addition, these medications directly reduce insulin sensitivity and insulin secretory capacity. (33)
As the use of antipsychotics rose, reports of substantial weight gain, diabetes, and dyslipidemia began to emerge. Additional studies further linked the increase in diabetes as being multifactorial. Unhealthy food choices, physical inactivity, and social deprivation all contribute to obesity in people with severe mental illness.
Antipsychotics induce weight gain largely through increased appetite and food intake, in addition to reducing energy expenditure and voluntary movement, in part due to their sedative effects. Although these medications have proven to treat severe mental illness, the risk of diabetes in this population needs to be aggressively monitored with screenings and strategies to ensure early diagnosis and optimal treatment of diabetes to lower the risk of long-term complications.

Self Quiz
Ask yourself...
Your patient, on antipsychotic medications, reports significant weight gain and poor activity levels for the last few months. His recent serum glucose level registered prediabetic at 5.8% mg/dl. He would like to stop taking the prescribed medication, “before I end up on insulin-like my dad”.
- What patient education opportunity exists regarding diet, activity, and medication compliance?
- What additional testing/surveillance should be considered in light of the comment,” …before I end up on insulin like my dad?”
Infection
Hyperglycemia can be a normal part of your body’s response to acute stress. Any accident or condition that deeply stresses your body, including sepsis, can cause non-diabetes-related hyperglycemia. When elevated serum glucose levels are related to an accident, injury, or condition, it’s called stress-induced hyperglycemia (SIH), which is a glucose level greater than 180mg/dl in persons who do not have a history of diabetes. (34)
SIH occurs when counterregulatory hormones (cortisol, glucagon, and catecholamines) disturb the glucose hemostasis. This results in insulin resistance and hyperglycemia. Statistically, hyperglycemia in critically ill patients (ICU-based) is an observed finding evident in the first 48 hours of admission in at least 50% of the patients. (35)
Treatment
- Insulin coverage sliding scale/ insulin infusion per ICU protocol.
- Nutrition consults to ensure diet (if applicable) is optimal to avoid overfeeding/ excessive glucose intake (avoid prolonged fasting state)
- Follow-up with a primary doctor to ensure diabetes screenings/ hyperglycemia surveillance.
- DSMES classes on nutritional therapy, exercise, and smoking cessation to delay onset of prediabetes/ diabetes.

Self Quiz
Ask yourself...
- How would you explain to your patients, with no history of diabetes mellitus, that they are now being suddenly treated for hyperglycemia after a severe motor vehicle accident?
- What hyperglycemia surveillance testing would you recommend after this MVA patient is discharged from the hospital?
Pheochromocytoma
Pheochromocytoma is a rare, catecholamine-secreting tumor that originates from the adrenal medulla and can cause glucose intolerance or diabetes mellitus. This occurs as beta-receptors stimulate gluconeogenesis, while alpha-2 receptors decrease insulin release. 60.78% of patients with pheochromocytoma also have diabetes or glucose intolerance. The increase in catecholamine levels is associated with decreased glucose uptake and increased gluconeogenesis and glycogenolysis. (36)
Persons with a diagnosis of pheochromocytoma should be screened for diabetes, especially if other risk factors are present. The removal of a pheochromocytoma reduces insulin secretion and peripheral insulin resistance, making early diagnosis important.
Symptoms (37, 38)
- Hypertension/ orthostatic hypertension
- Headache
- Irregular heart rates
- Feelings of anxiety
- Nausea/ vomiting/ diarrhea
- Unexplained weight loss
- Glucose intolerance pre-op (due to catecholamine release); severe hypoglycemia post-op tumor removal (due to abrupt tumor removal)
Diagnosis
- 24-hour urine test catecholamine level
- Serum catecholamine level
- CT/ MRI imaging of adrenal glands
Iron Overload (Hemochromatosis)
Iron overload disorder may be caused by genetics or as the result of another disease/ medical condition. Hereditary hemochromatosis is the result of a genetic component; secondary hemochromatosis may result from excessive dietary intake of iron, numerous blood transfusions, and various blood disorders such as sickle cell disease or thalassemia. Left undiagnosed and untreated, excessive accumulation of iron in the pancreas can interfere with insulin production, leading to diabetes mellitus. (39)
Symptoms may include the following:
- Chronic fatigue and weakness
- Abdominal pain, possible pancreatitis
- Joint pain, possible arthritis
- Irregular heart rate, possible heart disease
- Enlargement of liver, possible cirrhosis
Diagnosis
- Blood tests, including ferritin and transferrin saturation levels.
- Liver scans, abdominal scans (CT, MRI)
- Genetic testing when applicable
Treatment
- Phlebotomy is routinely scheduled, to reduce the severity levels of iron overload.
- Chelation therapy
- Hemochromatosis diet to focus on the reduced intake of iron-rich/iron-fortified foods (including dietary supplements)
The Importance of DSMES (Diabetes Self-Management Education and Support)
What next? After a confirmed diagnosis of diabetes mellitus, regardless of the underlying cause, all patients should be referred to a structured diabetes management program. In doing so, you as a healthcare professional will afford your patient the best opportunity to gain the knowledge and skills necessary to effectively manage this chronic medical condition.
DSMES programs, often covered by insurance plans including Medicare (Medicare covers up to 10 hours of diabetes education for people diagnosed in the past year), offer the person with diabetes the practical skills, knowledge, and insights to address all avenues of diabetes. In doing so, they gain self-confidence, lower risk factors and complications, reduce hospitalizations, and improve the quality of their life.
Referrals to DSMES should take place at the time of diagnosis when new health concerns arise, and any time life changes/events interfere with ongoing chronic disease management. By giving your patient, the knowledge, and skills necessary to manage their diabetes, short- and long-term complication risk is lowered, as well as unnecessary trips to the emergency department/hospital. (43)


Self Quiz
Ask yourself...
- Does your hospital/office practice currently offer structured DSMES programs?
- Are these programs open to the public or solely insurance covered by patients?
- What DSMES-type programs are available to your uninsured/ self-paid patients?
Conclusion
As stated in the introduction of this course, cases of diabetes mellitus continue to increase throughout the world. Early stages of this medical condition may not be detected through symptoms alone, yet left untreated, can affect long-term health and well-being. While 38.1 million adults were diagnosed with diabetes in 2021, another 8.7 million adults had diabetes but were undiagnosed.
The argument for annual screenings (routine, preventive) is justified to reduce the worldwide crisis in terms of healthcare dollars spent for direct medical costs as well as reduced productivity due to poor diabetes-related outcomes (long-term disability associated with nontraumatic amputations, as well as kidney and eye disease. (40), (41)
Untreated/ undiagnosed diabetes can wreak havoc on the health and well-being of an individual. Early treatment and intervention afford a person the best chance at achieving optimal glucose levels and lowering the risk of long-term, often life-threatening complications. Annual diabetes screenings, especially in high-risk populations/ persons afford the best opportunity for early detection and treatment.
Consider preventive screenings/ routine diabetes surveillance in the following populations:
- Persons 45 years of age
- Certain races/ethnicities (Native American, African American, Hispanics, or Asian American, Pacific Islander)
- Overweight or obese persons with a BMI greater than or equal to 25 kg/m2 (or 23 kg/m2 in Asian Americans)
- First-degree relative with diabetes mellitus
- History of cardiovascular disease or hypertension
- Low HDL-cholesterol or hypertriglyceridemia
- Women with polycystic ovarian syndrome
- Physical inactivity
- Conditions associated with insulin resistance.
- Women diagnosed with gestational diabetes mellitus (GDM) should have lifelong testing at least every three years. (Approximately 50 % of women diagnosed with GDM will go on to develop Type 2 diabetes within 3-6 years. (42)

Self Quiz
Ask yourself...
- As a healthcare professional, have you identified any other “high-risk” categories that should be screened for diabetes?
- What education do you currently provide for patients with high BMI levels and (self-admitted) reduced physical activity levels?
- Are patients routinely referred to dietitians and nutritionists as part of your chronic disease management program?
References + Disclaimer
- Ahmed, S. S., & Mohammed, A. A. (2020). Effects of thyroid dysfunction on hematological parameters: Case-controlled study. Annals of medicine and surgery, 57, 52–55. https://doi.org/10.1016/j.amsu.2020.07.008
- Boucai, L. (2024). Hypothyroidism. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/thyroid-disorders/hypothyroidism
- Boucai, L. (2024). Euthyroid sick syndrome. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/thyroid-disorders/euthyroid-sick-syndrome
- Kasper, D. L., Fauci, A. S., Hauser, S. L., Longo, D. L., Jameson, J. L., & Loscalzo, J. (2018). Harrison’s principles of internal medicine (20th ed.). McGraw-Hill Education.
- Moini, J., Pereira, K., & Samsam, M. (2020). Epidemiology of thyroid disorders. Elsevier.
- Patil N, Rehman A, Jialal I. Hypothyroidism. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519536/
- Pirahanchi Y, Toro F, Jialal I. Physiology, Thyroid Stimulating Hormone. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): Stat Pearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499850/
- Seifter, J., Sloane, D., & Walsh, E. C. (2022). Integrated physiology and pathophysiology. Elsevier.
- Tresa A, Rema P, Suchetha S, Dinesh D, Sivaranjith J, Nath AG. Hypothyroidism Presenting as Ovarian Cysts-a Case Series. Indian J Surg Oncol. 2021 Dec;12(Suppl 2):343-347. doi: 10.1007/s13193-020-01263-8. Epub 2021 Jan 2. PMID: 35035167; PMCID: PMC8716654.
- World Health Organization. (2021). Global health estimates: Leading causes of DALYs. https://www.who.int/data/global-health-estimates
- Zamwar, U. M., & Muneshwar, K. N. (2023). Epidemiology, Types, Causes, Clinical Presentation, Diagnosis, and Treatment of Hypothyroidism. Cureus, 15(9), e46241. https://doi.org/10.7759/cureus.46241
- Bains N. and Abdijadid S. Major Depressive Disorder. (2023). In: StatPearls. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Batt M, et al. (2020). Is Postpartum Depression Different from Depression Occurring Outside of the Perinatal Period? A Review of the Evidence. Focus, 18(2), 106-119. https://focus.psychiatryonline.org/doi/10.1176/appi.focus.20190045
- Woodall, A. and Walker, L. (2022). A guide to prescribing antidepressants in primary care. Prescriber, 33: 11-18. https://doi.org/10.1002/psb.2006
- Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2023). The serotonin theory of depression: a systemic umbrella review of the evidence. Molecular Psychiatry, 28, 3243-3256. https://doi.org/10.1038/s41380-022-01661-0
- Lam, M. K., Lam, L. T., Butler-Henderson, K., King, J., Clark, T., Slocombe, P., Dimarco, K., & Cockshaw, W. (2022). Prescribing behavior of antidepressants for depressive disorders: A systematic review. Frontiers in Psychiatry, 13, 918040. https://doi.org/10.3389/fpsyt.2022.918040
- Rohatgi, K. W., Humble, S., McQueen, A., Hunleth, J. M., Chang, S. H., Herrick, C. J., & James, A. S. (2021). Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. https://doi.org/10.3122/jabfm.2021.03.200361
- Sheffler ZM, Patel P, Abdijadid S. Antidepressants. 2023. In: StatPearls. Treasure Island (FL): Stat Pearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538182/
- Noetel, M, et al. (2024). Effect of exercise for depression: systematic review and network meta-analysis of randomized controlled trials. BMJ, 384. https://www.bmj.com/content/384/bmj-2023-075847
- Leslie, S. W., & Sooriyamoorthy, T. (2024, January 9). Erectile dysfunction. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK562253/
- Erectile dysfunction. (2024, January 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/32965924/
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
- Erectile dysfunction. (2016, November 15). PubMed. https://pubmed.ncbi.nlm.nih.gov/27929275/
- Leslie, S. W., & Sooriyamoorthy, T. (2024, January 9). Erectile dysfunction. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK562253/
- Carrell, D. T. (2023, November 1). Medical and surgical management of issues of male health. Cambridge Core. https://www.cambridge.org/core/books/abs/mens-reproductive-and-sexual-health-throughout-the-lifespan/medical-and-surgical-management-of-issues-of-male-health/E55912AAD1DC8D035D1331E297700898
- Vickers, A. J., Tin, A. L., Singh, K., Dunn, R. L., & Mulhall, J. (2019). Updating the International Index of Erectile Function: Evaluation of a large clinical data set. The Journal of Sexual Medicine, 17(1), 126–132. https://doi.org/10.1016/j.jsxm.2019.10.020
- Erectile Dysfunction (ED) guideline – American Urological Association. (2024). https://www.auanet.org/guidelines-and-quality/guidelines/erectile-dysfunction-(ed)-guideline
- Nehra, A. (2009). Erectile dysfunction and cardiovascular disease: Efficacy and safety of phosphodiesterase type 5 inhibitors in men with both conditions. Mayo Clinic Proceedings, 84(2), 139–148. https://doi.org/10.4065/84.2.139
- Wyllie, M. G. (2005). The underlying pathophysiology and causes of erectile dysfunction. Clinical Cornerstone, 7(1), 19–26. https://doi.org/10.1016/s1098-3597(05)80045-6
- Yafi, F. A., Jenkins, L., Albersen, M., Corona, G., Isidori, A. M., Goldfarb, S., Maggi, M., Nelson, C. J., Parish, S., Salonia, A., Tan, R., Mulhall, J. P., & Hellstrom, W. J. G. (2016). Erectile dysfunction. Nature Reviews. Disease Primers, 2(1). https://doi.org/10.1038/nrdp.2016.3
- Palumbo, F., Sebastiani, F., Procacci, A., D’Altilia, N., Ricapito, A., & Cormio, L. (2022). Peyronie’s Disease. In Springer eBooks (pp. 61–73). https://doi.org/10.1007/978-3-031-11701-5_6
- Chrysant, S. G. (2015). Antihypertensive therapy causes erectile dysfunction. Current Opinion in Cardiology/Current Opinion in Cardiology, With Evaluated MEDLINE, 30(4), 383–390. https://doi.org/10.1097/hco.0000000000000189
- Harvard Health. (2021, February 15). Some drugs may cause your erectile dysfunction. https://www.health.harvard.edu/mens-health/some-drugs-may-cause-your-erectile-dysfunction
- Santoro, F., Gil, I. J. N., Arcari, L., Vitale, E., Martino, T., El‐Battrawy, I., Guerra, F., Novo, G., Mariano, E., Musumeci, B., Cacciotti, L., Caldarola, P., Montisci, R., Ragnatela, I., Cetera, R., Vedia, O., Blanco, E., Pais, J. L., Martin, A., . . . Brunetti, N. D. (2024). Neurological Disorders in Takotsubo Syndrome: clinical phenotypes and outcomes. Journal of the American Heart Association. Cardiovascular and Cerebrovascular Disease, 13(4). https://doi.org/10.1161/jaha.123.032128
- Zalewska, T., Pawelec, P., Ziabska, K., & Ziemka-Nalecz, M. (2022). Sexual dimorphism in neurodegenerative diseases and in brain ischemia. Biomolecules, 13(1), 26. https://doi.org/10.3390/biom13010026
- Petersen, M., Kristensen, E., Giraldi, L., & Giraldi, A. (2020). Sexual dysfunction and mental health in patients with multiple sclerosis and epilepsy. BMC Neurology, 20(1). https://doi.org/10.1186/s12883-020-1625-7
- Rosen, R. (1999). The process of care model for evaluation and treatment of erectile dysfunction. International Journal of Impotence Research, 11(2), 59–70. https://doi.org/10.1038/sj.ijir.3900411
- Mulhall, J. P., Giraldi, A., Hackett, G., Hellstrom, W. J., Jannini, E. A., Rubio-Aurioles, E., Trost, L., & Hassan, T. A. (2018). The 2018 Revision to the Process of Care Model for Management of Erectile Dysfunction. The Journal of Sexual Medicine, 15(10), 1434–1445. https://doi.org/10.1016/j.jsxm.2018.05.021
- Drugs that may cause erection problems: MedlinePlus Medical Encyclopedia. (2024). https://medlineplus.gov/ency/article/004024.htm
- Kaplan-Marans, E., Sandozi, A., Martinez, M., Lee, J., Schulman, A., & Khurgin, J. (2022). Medications Most Commonly Associated with Erectile Dysfunction: Evaluation of the Food and Drug Administration National Pharmacovigilance Database. Sexual Medicine, 10(5), 100543. https://doi.org/10.1016/j.esxm.2022.100543
- Mohammed, S. A., Abdelhamed, A., & Sayed, R. M. E. (2020). Evaluation of drug abuse in patients with lifelong Premature Ejaculation: A Cross-Sectional Study. Sexual Medicine, 8(4), 608–614. https://doi.org/10.1016/j.esxm.2020.08.008
- Zoroufchi, B. H., Doustmohammadi, H., Mokhtari, T., & Abdollahpour, A. (2021). Benzodiazepines related sexual dysfunctions: A critical review on pharmacology and mechanism of action. Revista Internacional De Andrología, 19(1), 62–68. https://doi.org/10.1016/j.androl.2019.08.003
- Diagnosis of erectile dysfunction. (2022, August 29). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/erectile-dysfunction/diagnosis
- Gahm, E., Peterson, M., & Larsson, K. (2024). Men’s views on causes and consequences of erectile dysfunction or premature ejaculation in a primary care population: a qualitative study. Scandinavian Journal of Primary Health Care, 42(2), 355–364. https://doi.org/10.1080/02813432.2024.2327501
- Miller, K. (2023, September 7). Erectile dysfunction treatment. WebMD. https://www.webmd.com/erectile-dysfunction/erectile-dysfunction-treatment
- Erectile dysfunction (ED): Symptoms, Diagnosis & treatment – Urology Care Foundation. (2024). https://www.urologyhealth.org/urology-a-z/e/erectile-dysfunction-(ed)
- Jain, M. A., Leslie, S. W., & Sapra, A. (2023, October 26). Prostate cancer screening. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK556081/
- Savoy, M., Gurek, D., & Brown-James, A. (2020, March 1). Sexual Health history: Techniques and tips. AAFP. https://www.aafp.org/pubs/afp/issues/2020/0301/p286.html
- Erectile dysfunction – Symptoms and causes – Mayo Clinic. (2022, March 29). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/erectile-dysfunction/symptoms-causes/syc-20355776
- Heitz, D. (2018, May 31). Blood tests for erectile dysfunction. Healthline. https://www.healthline.com/health/erectile-dysfunction/blood-tests
- Hoffman, M., MD. (2023, August 10). Low testosterone and sex drive. WebMD. https://www.webmd.com/men/how-low-testosterone-can-affect-your-sex-drive
- Vaishnav, B., Tambile, R., Minna, K., Addepalli, S., Wadivkar, A., Pailla, R., Thakkar, N., & Balem, S. (2023). Study of gonadal hormones in males with liver cirrhosis and its correlation with Child-Turcotte-Pugh and model for End-Stage liver disease scores. Curēus. https://doi.org/10.7759/cureus.34035
- Gabrielson, A. T., Sartor, R. A., & Hellstrom, W. J. (2019). The impact of thyroid disease on sexual dysfunction in men and women. Sexual Medicine Reviews, 7(1), 57–70. https://doi.org/10.1016/j.sxmr.2018.05.002
- Jewell, T. (2023, December 14). Is there a link between iron deficiency anemia and erectile dysfunction? Healthline. https://www.healthline.com/health/erectile-dysfunction/can-anemia-cause-erectile-dysfunction
- Ma, W., Qin, M., Cui, T., Zhang, X., Ke, Z., Pan, Z., Gao, Y., & Liu, B. (2021). Relationship between the risk factors of cardiovascular disease by testing biochemical markers and young men with erectile dysfunction: a case-control study. Translational Andrology and Urology, 10(2), 724–733. https://doi.org/10.21037/tau-20-1056
- Erectile Dysfunction (ED) guideline – American Urological Association. (2024). https://www.auanet.org/guidelines-and-quality/guidelines/erectile-dysfunction-(ed)-guideline
- Erectile dysfunction and diabetes: Take control today. (2023, February 16). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/erectile-dysfunction/in-depth/erectile-dysfunction/art-20043927
- Prolactin levels. (2024). https://medlineplus.gov/lab-tests/prolactin-levels/
- Luteinizing hormone (LH) levels test. (2024). Https://medlineplus.gov/lab-tests/luteinizing-hormone-lh-levels-test/
- Face, S. a. J. M. F. (2024). Follicle-Stimulating Hormone Abnormalities Clinical presentation: History, physical, causes. https://emedicine.medscape.com/article/118810-clinical?form=fpf&scode=msp&st=fpf&socialSite=google&icd=login_success_gg_match_fpf
- Zapata, D. F., Howard, L. E., Frank, J., Simon, R. M., Hoyo, C., Grant, D. J., Freedland, S. J., & Vidal, A. C. (2017). The association between sexual function and prostate cancer risk in US veterans. Asian Journal of Andrology/Asian Journal of Andrology, 19(2), 191. https://doi.org/10.4103/1008-682x.184869
- Jung, D. C., Park, S. Y., & Lee, J. Y. (2018). Penile Doppler ultrasonography revisited. Ultrasonography, 37(1), 16–24. https://doi.org/10.14366/usg.17022
- Johnson, M., McNeillis, V., Gutbier, J., Eaton, A., Royston, R., Johnson, T., Chiriaco, G., Walkden, M., & Ralph, D. (2021). Differences in polysomnographic, nocturnal penile tumescence and penile doppler ultrasound findings in men with stuttering priapism and sleep-related painful erections. International Journal of Impotence Research, 34(6), 603–609. https://doi.org/10.1038/s41443-021-00462-3
- Singh, N. R., & Sandhu, I. M. (2019). Absence of nocturnal penile tumescence: an earlier sign of erectile dysfunction and its linked comorbid conditions. AMEIS’s Current Trends in Diagnosis & Treatment, 3(2), 72–76. https://doi.org/10.5005/jp-journals-10055-0074
- Ma, M., Yu, B., Qin, F., & Yuan, J. (2020). Current approaches to the diagnosis of vascular erectile dysfunction. Translational Andrology and Urology, 9(2), 709–721. https://doi.org/10.21037/tau.2020.03.10
- Sangiorgi, G., Cereda, A., Benedetto, D., Bonanni, M., Chiricolo, G., Cota, L., Martuscelli, E., & Greco, F. (2021). Anatomy, pathophysiology, molecular mechanisms, and clinical management of erectile dysfunction in patients affected by coronary artery Disease: a review. Biomedicines, 9(4), 432. https://doi.org/10.3390/biomedicines9040432
- Dean, R. C., & Lue, T. F. (2005). Physiology of penile erection and pathophysiology of erectile dysfunction. Urologic Clinics of North America, 32(4), 379–395. https://doi.org/10.1016/j.ucl.2005.08.007
- Adam, D. R., & Alem, M. M. (2022). Erectile Dysfunction: Pharmacological Pathways with Understudied Potentials. Biomedicines, 11(1), 46. https://doi.org/10.3390/biomedicines11010046
- Feldman, H. A., Goldstein, I., Hatzichristou, D. G., Krane, R. J., & McKinlay, J. B. (1994). Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. The Journal of Urology, 151(1), 54–61. https://doi.org/10.1016/s0022-5347(17)34871-1
- Marinelli, L., Lanfranco, F., Motta, G., & Zavattaro, M. (2021). Erectile Dysfunction in Men with Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine, 10(12), 2730. https://doi.org/10.3390/jcm10122730
- Chitaley, K., Kupelian, V., Subak, L., & Wessells, H. (2009). Diabetes, Obesity and Erectile Dysfunction: field Overview and research priorities. The Journal of Urology, 182(6S). https://doi.org/10.1016/j.juro.2009.07.089
- Diabetes and ED Sexual Medicine BUMC. (2003). Copyright (C) Boston University. https://www.bumc.bu.edu/sexualmedicine/patientinformation-physicians/diabetes-and-ed/
- Cayetano‐Alcaraz, A. A., Tharakan, T., Chen, R., Sofikitis, N., & Minhas, S. (2022). The management of erectile dysfunction in men with diabetes mellitus unresponsive to phosphodiesterase type 5 inhibitors. Andrology, 11(2), 257–269. https://doi.org/10.1111/andr.13257
- Allen, M. S., & Tostes, R. C. (2023). Cigarette smoking and erectile dysfunction: an updated review with a focus on pathophysiology, e-cigarettes, and smoking cessation. Sexual Medicine Reviews, 11(1), 61–73. https://doi.org/10.1093/sxmrev/qeac007
- Calogero, A. E., Burgio, G., Condorelli, R. A., Cannarella, R., & La Vignera, S. (2018). Epidemiology and risk factors of lower urinary tract symptoms/benign prostatic hyperplasia and erectile dysfunction. Aging Male The Aging Male, 22(1), 12–19. https://doi.org/10.1080/13685538.2018.1434772
- Xiao, Y., Xie, T., Peng, J., Zhou, X., Long, J., Yang, M., Zhu, H., & Yang, J. (2023). Factors associated with anxiety and depression in patients with erectile dysfunction: a cross-sectional study. BMC Psychology, 11(1). https://doi.org/10.1186/s40359-023-01074-w
- Fahmy, A., Abdeldaiem, H., Abdelsattar, M., Aboyoussif, T., Assem, A., Zahran, A., & Elgebaly, O. (2021). Impact of bariatric surgery on sexual dysfunction in obese men. Sexual Medicine, 9(2), 100322. https://doi.org/10.1016/j.esxm.2021.100322
- Crowdis, M., Leslie, S. W., & Nazir, S. (2023, May 30). Premature ejaculation. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK546701/
- Wang, C., Wu, B., Xiang, P., Xiao, J., & Hu, X. (2023). Management of male erectile dysfunction: From the past to the future. Frontiers in Endocrinology, 14. https://doi.org/10.3389/fendo.2023.1148834
- Definition; Facts for Erectile Dysfunction. (2022, August 29). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/urologic-diseases/erectile-dysfunction/definition-facts
- Rojanasarot, S., Williams, A. O., Edwards, N., & Khera, M. (2023). Quantifying the number of US men with erectile dysfunction who are potential candidates for penile prosthesis implantation. Sexual Medicine, 11(2). https://doi.org/10.1093/sexmed/qfad010
- Kałka, D., Gebala, J., Biernikiewicz, M., Mrozek-Szetela, A., Rożek-Piechura, K., Sobieszczańska, M., Szuster, E., Majchrowska, M., Miętka, A., & Rusiecka, A. (2021). Erectile Dysfunction in Men Burdened with the Familial Occurrence of Coronary Artery Disease. Journal of Clinical Medicine, 10(18), 4046. https://doi.org/10.3390/jcm10184046
- Sayadi, M., Elmafshar, R., Razeghian-Jahromi, I., & Zibaeenezhad, M. J. (2021). Detection of coronary artery disease by an erectile dysfunction questionnaire. Cardiology Research and Practice, 2021, 1–6. https://doi.org/10.1155/2021/6647995
- Yannas, D., Frizza, F., Vignozzi, L., Corona, G., Maggi, M., & Rastrelli, G. (2021). Erectile dysfunction is a hallmark of cardiovascular disease: unavoidable matter of fact or opportunity to improve men’s health? Journal of Clinical Medicine, 10(10), 2221. https://doi.org/10.3390/jcm10102221
- De Groat, W. (2017). Autonomic Nervous System: Central Urogenital Control. In Elsevier eBooks. https://doi.org/10.1016/b978-0-12-809324-5.01816-2
- Calabrò, R. S., Cacciola, A., Bruschetta, D., Milardi, D., Quattrini, F., Sciarrone, F., La Rosa, G., Bramanti, P., & Anastasi, G. (2019). Neuroanatomy and function of human sexual behavior: A neglected or unknown issue? Brain and Behavior, 9(12). https://doi.org/10.1002/brb3.1389
- Emanu, J. C., Avildsen, I. K., & Nelson, C. J. (2016). Erectile dysfunction after radical prostatectomy. Current Opinion in Supportive and Palliative Care, 10(1), 102–107. https://doi.org/10.1097/spc.0000000000000195
- Panchatsharam, P. K., Durland, J., & Zito, P. M. (2023, May 1). Physiology, erection. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK513278/
- Harvard Health. (2021, February 15). Can cycling cause erectile dysfunction? https://www.health.harvard.edu/staying-healthy/can-cycling-cause-erectile-dysfunction
- Gan, Z. S., Ehlers, M. E., Lin, F., Wright, S. T., Figler, B. D., & Coward, R. M. (2021). Systematic Review and Meta-Analysis of cycling and Erectile Dysfunction. Sexual Medicine Reviews, 9(2), 304–311. https://doi.org/10.1016/j.sxmr.2020.01.002
- Solan, M. (2023, September 1). FDA approves new over-the-counter gel for erectile dysfunction. Harvard Health. https://www.health.harvard.edu/mens-health/fda-approves-new-over-the-counter-gel-for-erectile-dysfunction
- Dhaliwal, A., & Gupta, M. (2023, April 10). PDE5 inhibitors. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK549843/
- Salvetat, M. L., Pellegrini, F., Spadea, L., Salati, C., & Zeppieri, M. (2023). Non-Arteritic Anterior Ischemic Optic Neuropathy (NA-AION): A comprehensive overview. Vision, 7(4), 72. https://doi.org/10.3390/vision7040072
- Schardein, J. N., & Hotaling, J. M. (2022). The impact of testosterone on erectile function. Androgens, 3(1), 113–124. https://doi.org/10.1089/andro.2021.0033
- ElHady, A. K., El-Gamil, D. S., Abdel-Halim, M., & Abadi, A. H. (2023). Advancements in Phosphodiesterase 5 Inhibitors: Unveiling present and future perspectives. Pharmaceuticals, 16(9), 1266. https://doi.org/10.3390/ph16091266
- Vacuum erectile devices for erection problems: MedlinePlus Medical Encyclopedia. (2022). https://medlineplus.gov/ency/patientinstructions/000985.htm
- Erectile dysfunction – Diagnosis and treatment – Mayo Clinic. (2022, March 29). https://www.mayoclinic.org/diseases-conditions/erectile-dysfunction/diagnosis-treatment/drc-20355782
- Hew, M. R., & Gerriets, V. (2023, April 3). Prostaglandin E1. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK546629/
- Jain, A., & Iqbal, O. A. (2023, July 17). Alprostadil. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK542217/
- Penile implants – Mayo Clinic. (2024, January 19). https://www.mayoclinic.org/tests-procedures/penile-implants/about/pac-20384916
- Diehm, N., Do, D., Keo, H., Boerlin, J., Regli, C., Schumacher, M., Jungmann, P. M., Raeber, L., & Baumann, F. (2018). Early recoil after balloon angioplasty of Erection-Related Arteries in patients with arteriogenic erectile dysfunction. Journal of Endovascular Therapy, 25(6), 710–715. https://doi.org/10.1177/1526602818807704
- Diehm, N., Pelz, S., Kalka, C., Keo, H. H., Mohan, V., Schumacher, M. C., D, D., DO, & Hoppe, H. (2023). Venous Leak Embolization in Patients with Venogenic Erectile Dysfunction via Deep Dorsal Penile Vein Access: Safety and Early Efficacy. Cardiovascular Radiology/Cardiovascular and Interventional Radiology, 46(5), 610–616. https://doi.org/10.1007/s00270-023-03412-2
- Musa, Z. S., El-Assmy, A., Shokry, A. M., Shokeir, A. A., Zween, T., & Al-Kenawy, M. R. (2019). Long-term effectiveness and predictors of success of low-intensity shockwave therapy in phosphodiesterase type 5 inhibitors non-responders. Arab Journal of Urology, 18(1), 54–58. https://doi.org/10.1080/2090598x.2019.1688072
- Lue, T., Wang, B., Reed-Maldonado, A., Ly, K., & Lin, G. (2022). Potential applications of low-intensity extracorporeal shock-wave therapy in urological diseases via activation of tissue resident stem cells. Urological Science, 33(1), 3. https://doi.org/10.4103/uros.uros_56_21
- Medrano-Sánchez, E. M., Peña-Cantonero, B., Candón-Ballester, P., Blanco-Díaz, M., & Díaz-Mohedo, E. (2024). Effectiveness of Low-Intensity Extracorporeal Shock Wave therapy in Erectile Dysfunction: An Analysis of Sexual Function and Penile Hardness at Erection: An Umbrella review. Journal of Personalized Medicine, 14(2), 177. https://doi.org/10.3390/jpm14020177
- Pérez-Aizpurua, X., Garranzo-Ibarrola, M., Simón-Rodríguez, C., García-Cardoso, J. V., Chávez-Roa, C., López-Martín, L., Jaumot, J. J. T. I., Alonso-Román, J., Maqueda-Arellano, J., Gómez-Jordana, B., De Castroviejo-Blanco, J. R., Osorio-Ospina, F., González-Enguita, C., & García-Arranz, M. (2023). Stem Cell Therapy for Erectile Dysfunction: A Step towards a Future Treatment. Life, 13(2), 502. https://doi.org/10.3390/life13020502
- Afferi, L., Pannek, J., Burnett, A. L., Razaname, C., Tzanoulinou, S., Bobela, W., Da Silva, R. a. F., Sturny, M., Stergiopulos, N., Cornelius, J., Moschini, M., Iselin, C., Salonia, A., Mattei, A., & Mordasini, L. (2020). Performance and safety of treatment options for erectile dysfunction in patients with spinal cord injury: A review of the literature. Andrology, 8(6), 1660–1673. https://doi.org/10.1111/andr.12878
- Argiolas, A., Argiolas, F. M., Argiolas, G., & Melis, M. R. (2023). Erectile dysfunction: Treatments, advances, and new therapeutic strategies. Brain Sciences, 13(5), 802. https://doi.org/10.3390/brainsci13050802
- Thakur, P. S., Gharde, P., Prasad, R., Wanjari, M. B., & Sharma, R. (2023). Restoring Quality of Life: A comprehensive review of penile rehabilitation techniques following prostate surgery. Curēus. https://doi.org/10.7759/cureus.38186
- Kataoka, T., Sanagawa, A., Suzuki, J., Muto, T., Hotta, Y., Kawade, Y., Maeda, Y., Tohkin, M., & Kimura, K. (2021). Influence of anticancer agents on sexual function: An in vivo study based on the US FDA Adverse Event Reporting System. Andrology, 10(1), 166–178. https://doi.org/10.1111/andr.13094
- Jung, D. C., Park, S. Y., & Lee, J. Y. (2018). Penile Doppler ultrasonography revisited. Ultrasonography, 37(1), 16–24. https://doi.org/10.14366/usg.17022
- Ferrini, M. G., Gonzalez-Cadavid, N. F., & Rajfer, J. (2017). Aging related erectile dysfunction—potential mechanism to halt or delay its onset. Translational Andrology and Urology, 6(1), 20–27. https://doi.org/10.21037/tau.2016.11.18
- Ajo, R., Segura, A., Inda, M., Margarit, C., Ballester, P., Martínez, E., Ferrández, G., Sánchez-Barbie, Á., & Peiró, A. M. (2017). Disfunción eréctil en pacientes con dolor crónico tratados con opioides. Medicina Clínica, 149(2), 49–54. https://doi.org/10.1016/j.medcli.2016.12.038
- Centers for Disease Control and Prevention. (2024, April 30). FastStats: Pneumonia. Retrieved from https://www.cdc.gov/nchs/fastats/pneumonia.htm
- Centers for Disease Control and Prevention. (2024, May 2). Leading Causes of Death. Retrieved from https://www.cdc.gov/nchs/data/databriefs/db492-tables.pdf#4
- Centers for Disease Control and Prevention. (2024, January 17). Provisional Mortality Statistics. Retrieved from https://wonder.cdc.gov/controller/datarequest/D176;jsessionid=6D5C5A75890CFBC006123D20DA22
- File, Jr., T.M. (Updated 2023, November 6). Treatment of Community-acquired Pneumonia in Adults in the Outpatient Setting. UpToDate. Retrieved from https://www.uptodate.com/contents/treatment-of-community-acquired-pneumonia-in-adults-in-the-outpatient-setting#H2787226612
- File, Jr., T.M. (Updated 2023, April 13). Treatment of Community-acquired Pneumonia in Adults who Require Hospitalization. UpToDate. Retrieved from https://www.uptodate.com/contents/treatment-of-community-acquired-pneumonia-in-adults-who-require-hospitalization
- Freeman, A. M., & Leigh, Jr., T.R. (Updated 2023, July 4). Viral Pneumonia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513286/
- Gamache, J. (Updated 2024, January 29). Bacterial Pneumonia Differential Diagnoses. Medscape. Retrieved from https://emedicine.medscape.com/article/300157-differential
- Jain, V., Vashisht, R., Yilmaz, G., & Bhardwaj, A. (Updated 2023, July 31). Pneumonia pathology. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK526116/
- Mandanas, R.A. (Updated 2021, October 22). Fungal Pneumonia. Medscape. Retrieved from https://emedicine.medscape.com/article/300341-overview#a7
- National Heart, Lung, and Blood Institute. (2022, March 24). Pneumonia: Causes and Risk Factors. National Institutes of Health. Retrieved from https://www.nhlbi.nih.gov/health/pneumonia/causes
- Sattar, S.B.A., Nguyen, A.D., & Sharma, S. (Updated 2024, February 26). Bacterial Pneumonia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK513321/
- Shetty, K. (Updated 2023, June 2). Hospital-Acquired Pneumonia (Nosocomial Pneumonia) and Ventilator-Associated Pneumonia. Medscape. Retrieved from https://emedicine.medscape.com/article/234753-overview#a14
- Torres, A., & Martin-Loeches, I. (2020). Invasive Pulmonary Aspergillosis in Ventilator-associated Pneumonia: The Hidden Enemy? American journal of respiratory and critical care medicine, 202(8), 1071–1073. https://doi.org/10.1164/rccm.202006-2605ED
- Truong, J., & Ashurst, J.V. (Updated 2023, January 21). Pneumocystis jirovecii Pneumonia. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK482370/
- World Health Organization. (2022, November 11). Pneumonia in Children. Retrieved from https://www.who.int/news-room/fact-sheets/detail/pneumonia
- National Diabetes Statistics Report. (2024, January 8). Diabetes. https://www.cdc.gov/diabetes/php/data-research/?CDC_AAref_Val=https://www.cdc.gov/diabetes/data/statistics-report/index.html
- Diabetes Diagnosis & Tests | ADA. (n.d.). https://diabetes.org/about-diabetes/diagnosis
- Diabetes testing. (2023, March 18). WebMD. https://www.webmd.com/diabetes/diagnosing-type-2-diabetes
- Type 1 diabetes. (2024, April 9). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/type-1-diabetes
- Professional, C. C. M. (n.d.). Type 1 diabetes. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21500-type-1-diabetes
- Type 1 diabetes – Symptoms and causes – Mayo Clinic. (2024, March 27). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/symptoms-causes/syc-20353011
- Testing.com. (2021, November 9). Islet autoantibodies in diabetes – Testing.com. https://www.testing.com/tests/islet-autoantibodies-diabetes/#:~:text=Islet%20autoantibody%20testing%20is%20primarily,caused%20by%20non%2Dautoimmune%20problems
- American Diabetes Association. (2022). Routine Islet Autoantibody Testing in Clinically Diagnosed Adult-Onset Type 1 Diabetes Can Help Identify Misclassification and the Possibility of Successful Insulin Cessation. Diabetes Care, 45(12), 2844–2851. https://diabetesjournals.org/care/article/45/12/2844/147718/Routine-Islet-Autoantibody-Testing-in-Clinically
- Hamdy, O., MD PhD. (2024, March 21). Diabetic Ketoacidosis (DKA) workUp: approach considerations, plasma glucose study, urine dipstick testing. https://emedicine.medscape.com/article/118361-workup#c15?form=fpf
- Professional, C. C. M. (n.d.-b). Type 1 diabetes. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21500-type-1-diabetes
- Safe at School | ADA. (n.d.). https://diabetes.org/advocacy/safe-at-school-state-laws#:~:text=Federal%20law%20gives%20students%20the,manage%20their%20diabetes%20anytime%2C%20anywhere
- Legal Protections | ADA. (n.d.). https://diabetes.org/advocacy/safe-at-school-state-laws/legal-protections
- About Type 2 diabetes. (2023, December 20). Diabetes. https://www.cdc.gov/diabetes/about/about-type-2-diabetes.html?CDC_AAref_Val=https://www.cdc.gov/diabetes/basics/type2.html
- Diabetes risk factors. (2023, December 20). Diabetes. https://www.cdc.gov/diabetes/risk-factors/?CDC_AAref_Val=https://www.cdc.gov/diabetes/basics/risk-factors.html
- Type 2 diabetes – Symptoms and causes – Mayo Clinic. (2023, March 14). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
- Brady, M. F., & Rawla, P. (2023, August 11). Acanthosis nigricans. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK431057/#:~:text=Acanthosis%20nigricans%20is%20most%20commonly,systemic%20glucocorticoids%20and%
- What are my options for type 2 diabetes medications? | ADA. (n.d.). https://diabetes.org/health-wellness/medication/oral-other-injectable-diabetes-medications#:~:text=Thiazolidinediones%20(TZDs)-,Metformin,glucose%
- UpToDate. (2023, February 20). UpToDate. https://www.uptodate.com/contents/type-2-diabetes-insulin-treatment-beyond-the-basics
- Chun, J., Strong, J., & Urquhart, S. (2019). Insulin initiation and titration in patients with type 2 diabetes. Diabetes Spectrum, 32(2), 104–111. https://doi.org/10.2337/ds18-0005
- Gestational diabetes: screening. (2021, August 10). https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/gestational-diabetes-screening
- Rajkumar, V., & Levine, S. N. (2024, March 1). Latent autoimmune diabetes. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK557897/#:~:text=Latent%20autoimmune%20diabetes%20of%20adults,2%20diabetes%20mellitus%20(DM).
- Latent autoimmune diabetes in adults (LADA): What is it? (2023, June 14). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/expert-answers/lada-diabetes/faq-20057880
- Harvard Health. (2023, September 28). Maturity onset diabetes of the young (MODY). https://www.health.harvard.edu/a_to_z/maturity-onset-diabetes-of-the-young-mody-a-to-z
- Kant, R., Davis, A., & Verma, V. (2022, February 15). Maturity-Onset Diabetes of the Young: Rapid Evidence Review. AAFP. https://www.aafp.org/pubs/afp/issues/2022/0200/p162.html
- What is Maturity-Onset Diabetes of the Young? // Diabetes Genes. (n.d.). https://www.diabetesgenes.org/what-is-mody/
- What is metabolic syndrome? | NHLBI, NIH. (2022, May 18). NHLBI, NIH. https://www.nhlbi.nih.gov/health/metabolic-syndrome
- Metabolic syndrome – Symptoms & causes – Mayo Clinic. (2021, May 6). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916
- What is metabolic syndrome? | NHLBI, NIH. (2022b, May 18). NHLBI, NIH. https://www.nhlbi.nih.gov/health/metabolic-syndrome
- Cushing disease: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000348.htm
- Cushing Disease / Cushing Syndrome | Brain Institute | OHSU. (n.d.). https://www.ohsu.edu/brain-institute/cushing-disease-cushing-syndrome
- Kahn, A. (2023, April 7). Cushing Syndrome: Everything you need to know. Healthline. https://www.healthline.com/health/cushings-syndrome
- Mph, A. O. P. (2022, September 9). What is Steroid-Induced Diabetes? Verywell Health. https://www.verywellhealth.com/steroid-induced-diabetes-6501185#:~:text=Yes%2C%20steroid%2Dinduced%20diabetes%20can,and%20exercise%20can%20also%20help.
- I.G. Holt, R. (2019). Association between antipsychotic medication use and diabetes. PubMed Central. https://doi.org/10.1007/s11892-019-1220-8
- Edwards, J. M. (2023, April 11). How does sepsis affect your blood sugar? Healthline. https://www.healthline.com/health/sepsis-hyperglycemia
- Muacevic, A., & R Adler, J. (2022). Stress-Induced Hyperglycemia: Consequences and Management. PubMed Central, 14(7), e26714. https://doi.org/10.7759/cureus.26714
- Derrou, S., Bouziane, T., Salhi, H., & El Ouahabi, H. (2021). Pheochromocytoma and glucoregulation disorders. PubMed Central, 20(1). https://doi.org/10.4103/aam.aam_13_20
- Professional, C. C. M. (n.d.-a). Pheochromocytoma. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/23373-pheochromocytoma
- Abe, I., Islam, F., & King-Yin Lam, A. (2020). Glucose intolerance on Phaeochromocytoma and Paraganglioma—The current understanding and Clinical Perspectives. PubMed Central. https://doi.org/10.3389/fendo.2020.593780
- Brazier, Y. (2023, December 14). Everything to know about hemochromatosis (Iron Overload). https://www.medicalnewstoday.com/articles/166455#overview
- Diabetes Statistics. (2024, March 1). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/health-statistics/diabetes-statistics#:~:text=Estimated%20prevalence%20of%20diabetes%20in,8.9%25%20of%20the%20population
- Vasavada, A., & Taub, L. F. M. (2022, October 31). Diabetes mellitus screening. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK554615/#:~:text=The%20American%20Diabetes%20Association%20recommends,risk%20factors%20regardless%20of%20age
- Adam, S., McIntyre, H. D., Tsoi, K. Y., Kapur, A., C, R., MA, Dias, S., Okong, P., Hod, M., Poon, L. C., Smith, G. N., Bergman, L., Algurjia, E., O’Brien, P., Medina, V. P., Maxwell, C. V., Regan, L., Rosser, M. L., Jacobsson, B., Hanson, M. A., . . . McAuliffe, F. M. (2023). Pregnancy as an opportunity to prevent type 2 diabetes mellitus: FIGO Best Practice Advice. International Journal of Gynaecology and Obstetrics, 160(S1), 56–67. https://doi.org/10.1002/ijgo.14537
- Referring patients to DSMES. (2024, May 15). Diabetes. https://www.cdc.gov/diabetes/hcp/dsmes/?CDC_AAref_Val=https://www.cdc.gov/diabetes/dsmes/dsmes-health-pro.html
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
