Course
Geriatric Hip Fracture
Course Highlights
- In this Geriatric Hip Fracture course, we will learn about the anatomical structures involved in the hip joint, including bones, muscles, and ligaments.
- You’ll also learn age-related physiologic changes that contribute to hip fractures.
- You’ll leave this course with a broader understanding of assessment and diagnostic tools for geriatric clients who have suspected hip fractures.
About
Contact Hours Awarded: 1
Course By:
Abbie Schmitt, MSN-Ed, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
A common fear among older adults is falling and breaking their hip – and rightly so. A hip fracture can cause long-term and often lifelong challenges for elderly individuals and their families. Normal physiological changes related to aging make this population especially vulnerable.
Geriatric hip fracture clients require a multidisciplinary team, including the surgeon, primary care provider, nurses, social workers, physical and occupational therapists, rehabilitation center coordinators, and home health and/or long-term care facilities. Each client’s complex journey is unique, but there is hope for all involved. Nurses can change the outcome and empower those impacted by hip fractures. Let’s dive in!
Understanding Geriatric Hip Fractures
Hip fractures are fractures that occur at the proximal femur (10). More than 85% of hip fractures happen to individuals older than 65 (1). According to researchers, approximately one in three women and one in twelve men will have a hip fracture in their lifetime (1). Age-related physical changes in neuromuscular coordination, vision, balance, and medication use are associated with falls and hip fractures.
The hip joint is a complex structure that supports much of the body’s weight during standing, walking, and other activities. It is composed of bones, muscles, ligaments, and cartilage that work together to maintain stability and mobility.
Etiology
Most hip fractures in the elderly population are the result of a fall. Age-related bone fragility from osteoporosis or decreased bone mineral density can make even a simple fall into a disaster. Stress fractures, which are usually caused by repetitive force or overuse, can also occur but are less common.
Risk factors for falls in the elderly population include a history of falls, gait abnormalities, the use of walking aids, vertigo, osteoporosis Parkinson’s disease, and the use of multiple medications (4). Cognitive impairment is also a significant risk factor among the elderly population. Trauma or blunt force can also cause hip fractures. Comorbidities, such as diabetes and cardiovascular disease, increase the likelihood of fractures in the elderly.
Age-Related Physiologic Changes
There are natural biological processes that result in the gradual decline of the body’s systems as we age. The normal aging process affects multiple organ systems, including the cardiovascular, nervous systems, and musculoskeletal systems. This includes structural and functional changes such as reduced cellular function, decreased bone density, slower metabolism, and diminished immune response (3).
Changes in bone density and surrounding supportive tissue make older adults more vulnerable to fractures.
Imagine bones are like a strong, woven basket throughout childhood and adulthood. Each fiber is tightly bound, making the basket sturdy and able to hold heavy items without breaking. Over time, however, some of those fibers begin to wear away, with fewer fibers holding it together, even a lighter load that once posed no problem can cause it to tear or collapse.

Similarly, bones are tightly packed with minerals like calcium, protein, collagen, and phosphorus, making them strong and resilient, much like this sturdy basket. Osteocytes are cells within the bone matrix. Osteocyte viability begins to decline with the aging body. Lack of osteocytes impacts the strength of bones and the ability for bone healing. A minor fall or bump that a young, “woven” bone could easily withstand might now cause a fracture because the bone has become more porous and fragile.
In addition to weakened bones, the bony architecture of the proximal femur is affected by muscular and ligament tissue strength, which also declines with age. Muscle mass diffusely decreases with age (3). Sarcopenia is the term used to describe reduced muscle mass and strength (8).

Self-Quiz
Ask Yourself...
- Can you describe the normal physiological changes of aging?
- How can diabetes and cardiovascular disease increase the risk of falls?
- Can you name safety precautions to prevent falls, both within the home and healthcare environment?
- Can you discuss the reasons why hip fractures are more commonly diagnosed in older adults?
Anatomy and Physiology
It is important to review the anatomy of the hip joint and how aging affects bone density, muscle strength, and balance. We will review the bones, muscles, ligaments, and cartilage of the hip joint.
Bones
The hip joint is a ball-and-socket joint formed by two main bones: the pelvis and the femur (2). The femur is the thigh bone and the longest bone in the body. The top of the femur forms the femoral head, which fits into the acetabulum of the pelvis (2).
The pelvis is made up of the ilium, ischium, and pubis, which fuse together to form the pelvic girdle. The acetabulum forms the socket of the hip joint where the femur head fits to form the ball-and-socket structure. (2) This structure allows movement.
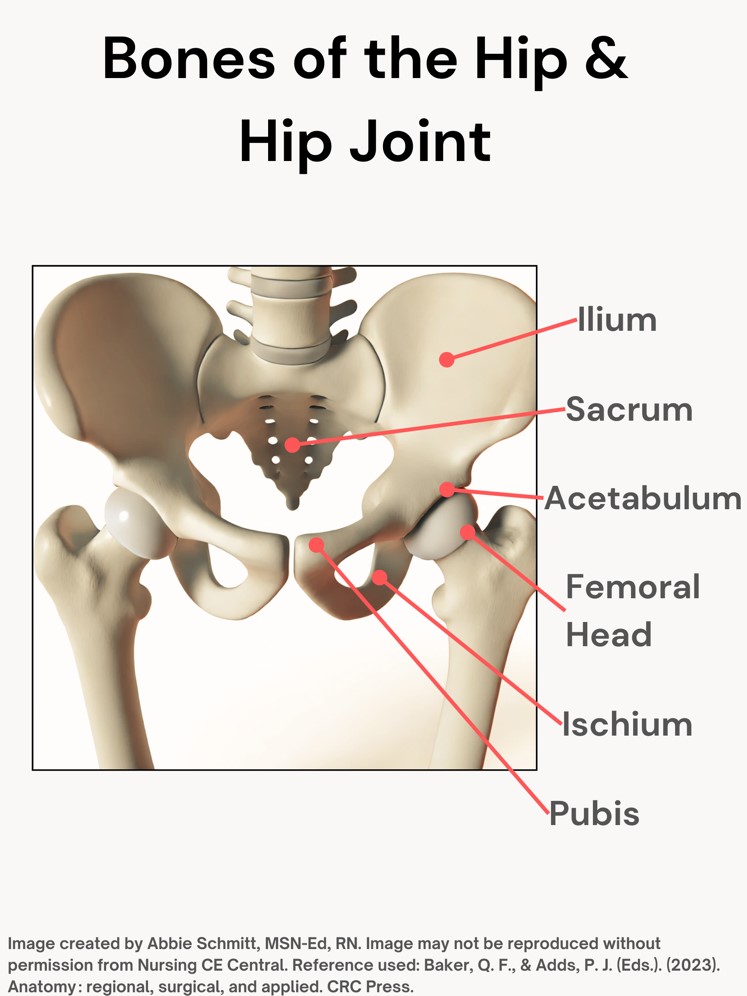 Figure 1. Bones of the Hip and Hip Joint
Figure 1. Bones of the Hip and Hip Joint
Muscles of the Hip Joint:
The muscles around the hip joint provide vital support for movement and stabilization of the joint. They are divided into different groups based on their function:
- Flexors
- Iliopsoas is the strongest hip flexor and allows for lifting the leg toward the body.
- Rectus Femoris is one of the quadriceps muscles and assists in hip flexion.
- Extensors
- Gluteus maximus: Found in the buttocks area, it extends the thigh and straightens the hip.
- Hamstrings: A group of muscles (biceps femoris, semitendinosus, and semimembranosus) that support hip extension.
- Abductors
- Gluteus medius and gluteus minimus are located on the outer surface of the pelvis and move the leg away from the midline of the body (abduction) and stabilize the hip during walking.
- Adductors: A group of muscles located on the inner thigh and are responsible for bringing the legs together (adduction).
- Rotators
- Internal rotators rotate the thigh inward.
- External rotators rotate the thigh outward.
The ligaments of the hip provide stability by connecting bones and limiting excessive, overextending movement.
Articular cartilage covers the femoral head and acetabulum surfaces, allowing smooth movement between the bones and cushioning the joint. The labrum is a ring of cartilage that covers the acetabulum and supports joint stability. (10)

Self-Quiz
Ask Yourself...
- How do muscles, such as flexors, extensors, and abductors, have a part in movement and flexion?
- Can you describe how ligaments protect the hip joint?
- What is the name of the longest bone in the body?
- Why is knowledge of the anatomy of the hip joint important when discussing pain and range of motion (ROM)?
Types of Hip Fractures
Hip fractures can be classified as intracapsular, extracapsular, and subtrochanteric. This is based on the location of the fracture. Intracapsular fractures include fractures of the femoral head and femoral neck. An extracapsular hip fracture occurs below the joint capsule of the hip. Subtrochanteric fractures are below the lesser trochanter, typically within 5 centimeters of the trochanter. (7)
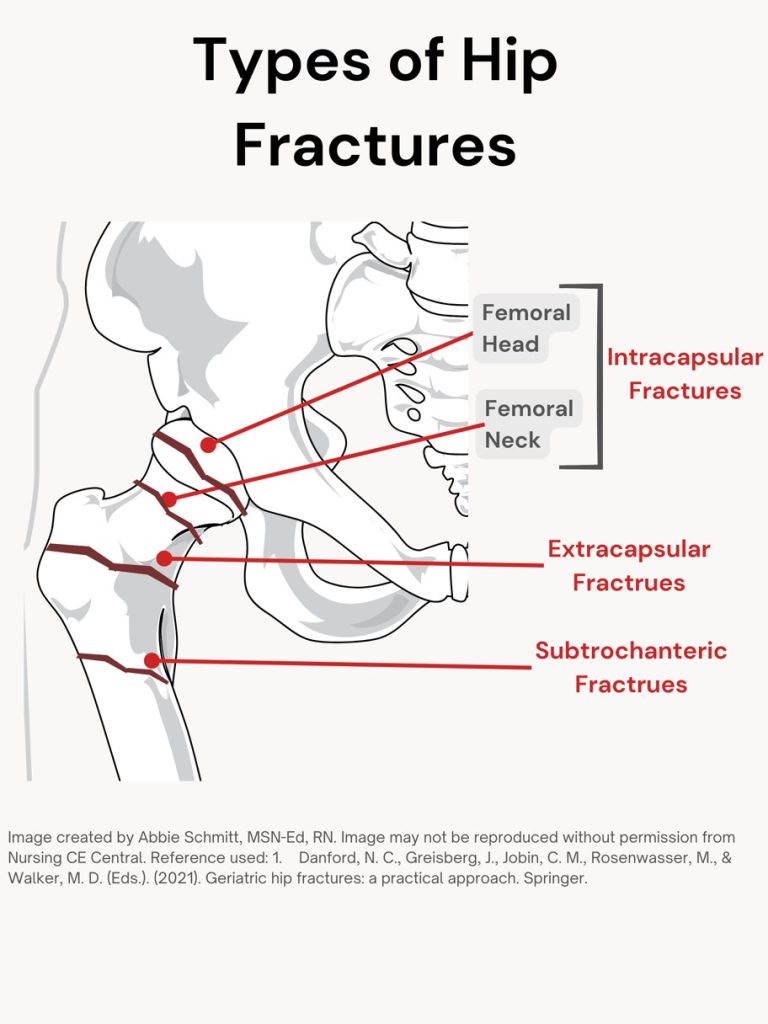
Figure 1. Types of Hip Fractures
A displaced fracture occurs when the bone breaks into two or more parts, and the broken pieces move out of alignment from their normal anatomical position (10).
The most commonly used classification for femoral neck fractures is the Garden classification, which divides femoral neck fractures into four subgroups based on the severity of the fracture and the degree of displacement. (7). The classification system is simple and aims to predict the development of Avascular necrosis of the femoral head.
Garden Classification of Intracapsular Femoral Neck Hip Fractures:
The fractures are graded, depending on the type, pattern, and whether or not there is displacement of the bone: (7)
- Type I: Incomplete fracture or valgus-impacted fracture.
- Type II: Complete fracture without displacement.
- Type III: Complete fracture with partial displacement of fracture fragments.
- Type IV: Complete fracture with total displacement of fracture fragments; the femoral head can be rotated back to its anatomical position within the acetabulum
Fractures of the femoral head are rare and are typically the result of impact or dislocation of the hip. The fracture location and pattern will guide treatment, as well as each client’s unique conditions.

Self-Quiz
Ask Yourself...
- How would an incomplete fracture be categorized using the Garden Classification of Intracapsular Femoral Neck Hip Fractures?
- Can you describe a fracture that is “displaced”?
Assessment and Diagnosis
An initial assessment protocol should ensure timely history and physical assessment, pain management, imaging, and communication with orthopedics.
Many geriatric clients who present with a suspected hip fracture will have comorbidities such as hypertension, heart disease chronic kidney disease, and dementia. Assessment and management of these conditions are essential throughout the process of hip fracture evaluation.
The performance of an electrocardiogram and baseline blood tests (full blood count, urea and electrolytes, and coagulation tests) are meaningful.
A thorough physical examination is important to assess for any additional fractures or injuries, and this is especially important in elderly clients. Assessment of circulation, pain, ability to bear weight, external rotation of the leg, and bruising is critical. Review past medical history and medication regimen.
Pain should be continuously assessed, and appropriate analgesia offered immediately upon arrival to the hospital, even before hip fracture is confirmed; it should be reassessed within 30 minutes of the initial analgesia to assess the effectiveness.
Pain assessments should be individualized, as clients with cognitive impairment may find it difficult to self-report pain or use a numerical rating scale.
Diagnostic imaging is important in recognizing the extent and type of fracture.
- X-rays. Appropriate studies include an anteroposterior (AP) view of the pelvis with a marker ball and full-length femur X-rays including an AP and lateral of the hip.
- Magnetic resonance imaging (MRI) scans. An MRI scan provides images of both soft tissue structures and bone. An MRI can sometimes detect a smaller fracture that cannot be seen on an X-ray.
- Computerized tomography (CT) scans. A CT scan will provide a detailed cross-sectional image of the hip region.
Classifying the fracture allows the surgical team to properly communicate and plan for the procedure and have a more informed preoperative discussion with the client and family members. (7)
Differential Diagnosis
- Osteoarthritis/rheumatoid arthritis of the hip
- Hip dislocation
- Pathologic fracture
- Tendonitis
- Lumbar disk syndrome with radicular pain
- Trochanteric bursitis
- Septic hip joint
- Pelvis fracture
(6)
A client’s cognition should be assessed on admission, as potential cognitive impairment will have consequences for care and treatment. Cognition can be assessed using tools like the Mini Mental State Examination (MMSE) or Montreal Cognitive Assessment (MOCA).
Each client’s capacity to consent to treatment must be formally assessed and documented and then re-evaluated if there is a change in the client’s condition.

Self-Quiz
Ask Yourself...
- What are the diagnostic images that are typically performed to assess for hip fractures?
- Can you discuss the differential diagnoses for hip fracture?
- What are some tools and methods for assessing pain?
- What are some tools and methods for assessing cognitive impairment and orientation?
Complications
Hip fractures in the geriatric population often lead to significant complications due to the aging process causing a reduced ability to heal and manage stress. Hip fractures significantly increase the risk of mortality in the elderly (3).
Common complications include:
- Surgical Site Infections
- Particularly in clients with diabetes or poor wound healing.
- Deep Vein Thrombosis (DVT)
- Prolonged bed rest can lead to blood clots in the legs, which may dislodge and cause a pulmonary embolism.
- Muscle loss and atrophy
- Urinary Tract Infections (UTIs)
- Pneumonia
- Non-healing of the Fracture
- Osteoporosis and poor bone density in older adults can impair the healing process and result in long-term disability or the need for additional surgeries.
- Cognitive Decline
- Surgery and hospitalization correlate with confusion or delirium in older adults, especially those with preexisting cognitive impairments such as dementia.
- There is an association between hip fractures and long-term cognitive decline (3).
- Cardiovascular Complications
- The physical stress of a fracture and subsequent surgery can exacerbate underlying heart conditions, increasing the risk of heart failure or myocardial infarction.
The Nottingham Hip Fracture Score can be used to predict 30-day and one-year mortality and assist with care planning. It helps healthcare professionals assess the likelihood of adverse outcomes and tailor postoperative care based on individual risk factors. The score is calculated by assigning points to several variables based on the client’s condition and demographics.
Variables included in the Nottingham Hip Fracture Score (5):
- Age
- 66-85 years: 3 points
- 85 years: 4 points
- Sex
- Male: 1 point
- Hemoglobin level (g/dL)
- <10 g/dL: 1 point
- Living in a facility (e.g., nursing home)
- Yes: 1 point
- Comorbidities
- Presence of 2 or more comorbid conditions: 1 point
- Mini-Mental Test Score (MMTS)
- MMTS <6 (out of 10): 1 point
- New Mobility Score
- NMS <6: 1 point
Total Score and Interpretation
- Low risk: 0-3 points
- Medium risk: 4-6 points
- High risk: 7-10 points
Surgical and Non-Surgical Treatment Options
Management of elderly clients with hip fractures can be challenging. A multidisciplinary co-management is essential, including input from geriatrics, internal medicine, orthopedic surgery, anesthesiology, and possibly other medical and surgical subspecialties.
Treatment for geriatric hip fractures depends on the type of fracture, the client’s overall health, and their level of mobility before the injury.
The goals of treatment are to manage pain, restore mobility, and prevent complications. Treatment options can be categorized into surgical and non-surgical approaches.
Surgical Treatment Options
Surgery is generally the preferred treatment for hip fractures in older adults, as it allows for faster mobilization, reducing the risk of complications associated with immobility (3, 5).
- Internal Fixation (Hip Pinning)
- This procedure involves metal screws or pins that are inserted to hold the broken bone in place.
- Typically used for non-displaced fractures (the bone fragments are aligned)
- Commonly used for femoral neck fractures
- Bone density and quality are important in this procedure.
- Hemiarthroplasty (Partial Hip Replacement)
- The damaged/ fractured portion of the femoral head is surgically removed and replaced with a metal prosthesis and the acetabulum (hip socket) is left intact.
- Total Hip Arthroplasty (Total Hip Replacement)
- The femoral head and the acetabulum are replaced with prosthetic components.
- Intramedullary Nailing
- This procedure involves a metal rod that is inserted into the bone marrow canal of the femur. The purpose is to stabilize fractures, particularly those in the trochanteric region, just below the femoral neck.
Non-Surgical Treatment
Non-surgical treatment is considered for clients who may not be able to undergo surgery due to significant comorbidities or when the fracture is non-displaced and stable.
Pain medications: Pain relief is typically managed with analgesics (e.g., acetaminophen, opioids) and anti-inflammatory medications. Injections of nerve blocks or epidurals may also be used to control pain in clients who cannot undergo surgery.
Immobilization and traction apply splints or casts, and traction to realign the bone. This option is generally but not preferred for older adults due to the risks associated with prolonged immobility and muscle atrophy. Remember, the aging process already causes deterioration of bone and muscle tissue, so a long period of hardly any movement could lead to poor outcomes.
Physical Therapy – Early mobilization is key to recovery. Physical therapy begins soon after surgery to help restore mobility, strengthen muscles, and improve balance.
Occupational Therapy – Focuses on helping clients regain independence in activities of daily living (ADLs), such as dressing, bathing, and using assistive devices like walkers.
Nutritional Support: Adequate nutrition, particularly protein and calcium, is essential for healing.
As we mentioned, geriatric clients often have comorbidities that need to be managed along with the hip fracture.
These commonly include:
- Anticoagulation therapy
- Breathing exercises or incentive spirometry to prevent pneumonia.
A palliative approach may be meaningful for many clients with hip fractures. This includes aggressive pain management, physical therapy to improve mobility as tolerated, and comfort-focused care to address the client’s quality of life.

Self-Quiz
Ask Yourself...
- Can you discuss the various surgical options for a hip fracture?
- How can nurses provide support before, during, and after PT and OT?
- Can you think of reasons palliative care may be a better option for clients who are not candidates for surgery?
- Why is nutritional support important for aging and wellbeing?
Nursing Care and Rehabilitation
Note on Author Experience: In my experience as a nurse in an Internal Rehabilitation Unit, countless elderly clients noted a hip fracture as the trigger to their health decline. Statements such as “everything went downhill after I broke my hip.” This was one of the most numerous opinions among clients and their families. Hip fractures were seen as a catastrophic event, even for clients who have had a stroke, MI, or kidney failure – they often felt most impacted by a hip fracture.
Nurses have the opportunity to change this narrative – offering new hope and advocacy. It is a holistic, complex process. Education and client involvement are key.
Key nursing interventions and implications for geriatric clients with hip fractures focus on post-operative care, mobility, pain management, caregiver/family support, discharge planning relating to environment, nutrition, and physical and occupational therapy.
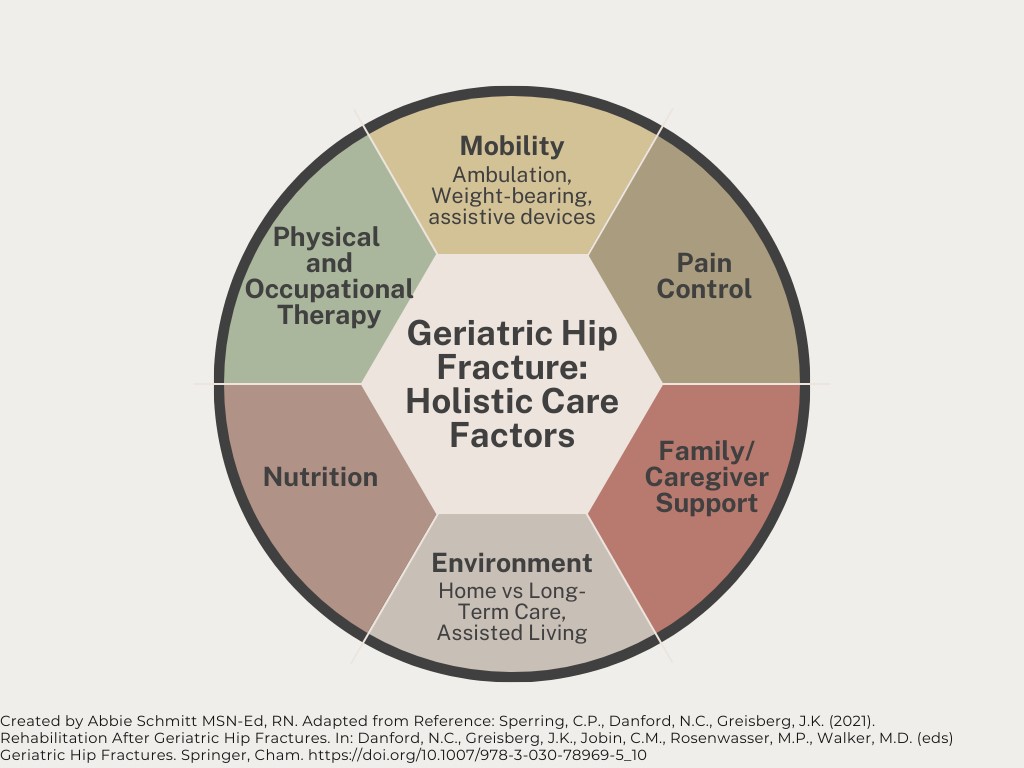 Figure 3. Geriatric Hip Fracture: Holistic Care Factors
Figure 3. Geriatric Hip Fracture: Holistic Care Factors
Mobility
- Encourage early mobilization in collaboration with physical therapy.
- Early mobilization reduces the risk of complications like deep vein thrombosis (DVT), pressure ulcers, and pneumonia, while also aiding in functional recovery.
- Follow guidelines on weight-bearing status and restrictions.
- For clients who undergo non-operative treatment of displaced intracapsular or extracapsular hip fractures, weight bearing as tolerated on the injured extremity is recommended.
- Weight-bearing as tolerated is recommended because it does not restrict the mobility of a client for whom immobilization would be detrimental, both in terms of physical function and in terms of medical complications such as venous thromboembolism.
- For unstable fracture patterns or fixation, the strain of weight bearing would cause significant damage. Partial weight-bearing or non-weight-bearing may be required for these clients. However, weight-restrictions do not mean “bed-bound”.
- Assist the client with safe movement, using assistive devices like walkers or crutches.
- Provide range-of-motion exercises if full mobilization isn’t possible immediately.
- If pain prevents weight bearing, then clients should have assistance for transfer from bed to chair and should engage in passive and active range of motion exercises with physical therapy.
- Patients undergoing closed reduction and internal fixation of intracapsular hip fractures are made “toe touch” or “partial” weight bearing for 6 weeks to protect the fixation and allow time for fracture healing.
- Advocate for communication between the surgeon, physical therapist, care team, and the client so that definitions of restrictions and weight-bearing protocols are clear.
- For example, “toe touch” may be interpreted as more weight placed on the toes than is desirable.
- Range of motion restrictions to prevent dislocation would be determined by the surgeon.
- Ensure safety: Make sure the therapy environment is free of hazards (such as loose rugs or clutter) and ensure proper lighting to reduce the risk of falls or injuries.
(5, 7, 9)
Physical and Occupational Therapy
Patients should be immediately mobilized under the guidance of a physical therapist; If surgery occurs early in the day, physical therapy often begins on the day of surgery. Otherwise, therapy must start the day after surgery, with consideration given to any medical issues.
The physical therapist assists in a variety of exercises, including:
- Passive and active range of motion of both upper and lower extremities
- Strengthening exercises
- Transfers (bed to chair, toilet to wheelchair)
- Ambulation
The occupational therapist assists the client in re-learning activities of daily living in the face of the new injury. These activities include:
- Brushing teeth
- Using the toilet
- Bathing
- Dressing
- Getting into and out of vehicles
Physical therapists and occupational therapists are invaluable in the client’s journey toward recovery, especially for geriatric clients.
Pain Control
Balancing pain control in older adults with managing the risks of opioid use is like walking a tightrope – on a unicycle!
On one side, effective pain relief is essential for promoting mobility and recovery, but on the other, increased use of opioids can lead to dangerous side effects such as respiratory depression, confusion, addiction, and constipation (7).
The following is an example of a multi-modal approach to pain control by a leading expert in this field: (9)
- Neuraxial anesthesia is administered preoperatively by the anesthesiology team.
- Postoperative administration of standing acetaminophen (650 mg every 6 h); low-dose oral oxycodone as needed (starting with 2.5 mg every 6 h for moderate pain and 5 mg every 6 h for severe pain); 0.2 mg of intravenous hydromorphone every 3 h for breakthrough pain.
- Ice and transdermal lidocaine (lidocaine patch) application.
- Based on tolerance and pain assessments; Ibuprofen 600 mg standing every 6 h or its equivalent if there are no contraindications such as renal disease, concomitant administration of aspirin for venous thromboembolism prophylaxis, or history of gastrointestinal bleeding.
This is a sample, and your facility and surgeon will have their protocols and guidelines for pain control. However, nurses are in a unique position to offer advocacy for clients to appropriately address pain while reducing harm.
Environment
Patients may be discharged from the hospital to a rehabilitation center, skilled nursing facility, assisted living facility, or home after surgery. The important differentiator is not the name of the setting, but rather the activities offered at the setting.
Patients who can perform activities of daily living at home and/or have assistance for home living in the form of family or professional aides may be discharged home after surgery for a hip fracture. If they can travel and attend therapy at an outclient center, this would be appropriate. However, if a client cannot or will not travel for therapy, home-based physical therapy is an option (9).
Nutrition
Malnourishment is common among elderly clients with hip fractures (9). Surgery increases the risk for protein catabolism and malnutrition due to increased energy needs, inflammation, and decreased protein intake, especially in older adults (9). Malnutrition compromises bone strength and structure. Malnutrition is also associated with gait impairment, increased mortality, worse mobility, worse physical function, poor cognition, and increased rates of rehospitalization (9).
Research suggests that protein supplementation following hip fracture treatment reduces the chance of complications, prevents muscle atrophy, and decreases the hospital’s length of stay (9). However, this may not be appropriate for all clients based on comorbidities, such as kidney failure.
Nutritional assessment and referral to a nutritionist should be included in care planning in both hospital and post-hospital rehabilitation.
Support
Psychosocial factors and coping strategies are crucial in the rehabilitation of the hip fracture client. Common psychological restrictions include fear of falling or feeling too tired to participate.
Social support through family and/or friends is critical to success. Research shows that greater social support, interaction with others, and meaningful relationships increase clients’ sense of self-efficacy and correlate with better outcomes (9).

Self-Quiz
Ask Yourself...
- What are activities a client will likely perform in physical therapy following a hip fracture and/or surgery?
- Why is early mobilization crucial for these clients?
- How can nurses provide holistic advocacy for pain management?
- Can you describe environmental hazards for falling (e.g. loose rugs, clutter)?
Conclusion
We have explored the critical elements involved in the care of geriatric clients with hip fractures, including early intervention, surgical and non-surgical treatments, and the importance of rehabilitation in promoting recovery and preventing complications. Key areas include physiologic changes of aging, risk factors for hip fractures, effective pain management, early mobilization, and complication management. As healthcare professionals, our role extends beyond physical care to include providing emotional support, educating clients and their families, and coordinating multidisciplinary care to promote independence and improve quality of life.
References + Disclaimer
- Amarilla-Donoso, F. J., López-Espuela, F., Roncero-Martín, R., Leal-Hernandez, O., Puerto-Parejo, L. M., Aliaga-Vera, I., Toribio-Felipe, R., & Lavado-García, J. M. (2020). Quality of life in elderly people after a hip fracture: a prospective study. Health and quality of life outcomes, 18(1), 71. https://doi.org/10.1186/s12955-020-01314-2
- Baker, Q. F., & Adds, P. J. (Eds.). (2023). Anatomy: regional, surgical, and applied. CRC Press. https://doi.org/10.1201/9781003312895
- Danford, N. C., Greisberg, J., Jobin, C. M., Rosenwasser, M., & Walker, M. D. (Eds.). (2021). Geriatric hip fractures: a practical approach. Springer. https://doi.org/10.1007/978-3-030-78969-5
- Emmerson BR, Varacallo M, Inman D. Hip Fracture Overview. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557514/
- Falaschi, P. (2021). Orthogeriatrics: the management of older patients with fragility fractures (P. (Paolo) Falaschi & D. Marsh, Eds.; Second edition.). Springer Nature. https://doi.org/10.1007/978-3-030-48126-1
- Ferri, F. F. (2024). Ferri’s Clinical Advisor 2025: 5 Books in 1. Elsevier.
- Levitsky, M.M., Shah, R.P., Neuwirth, A.L. (2021). Initial Workup, Diagnosis, and Fracture Classification for Geriatric Hip Fractures. In: Danford, N.C., Greisberg, J.K., Jobin, C.M., Rosenwasser, M.P., Walker, M.D. (eds) Geriatric Hip Fractures. Springer, Cham. https://doi.org/10.1007/978-3-030-78969-5_2
- Santy-Tomlinson, J., Hertz, K., Myhre-Jensen, C., & Brent, L. (2021). Nursing in the Orthogeriatric Setting. In: Falaschi, P., Marsh, D. (eds) Orthogeriatrics. Practical Issues in Geriatrics. Springer, Cham. https://doi.org/10.1007/978-3-030-48126-1_17
- Sperring, C.P., Danford, N.C., Greisberg, J.K. (2021). Rehabilitation After Geriatric Hip Fractures. In: Danford, N.C., Greisberg, J.K., Jobin, C.M., Rosenwasser, M.P., Walker, M.D. (eds) Geriatric Hip Fractures. Springer, Cham. https://doi.org/10.1007/978-3-030-78969-5_10
- Standring, S. (2021). Gray’s Anatomy: The Anatomical Basis of Clinical Practice (Forty-second edition.). Elsevier.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
