Course
Guidelines for Outpatient Antibiotic Therapy
Course Highlights
- In this Guidelines for Outpatient Antibiotic Therapy course, we will learn to differentiate between bactericidal and bacteriostatic mechanisms of action
- You’ll also learn antibiotic recommendations for the treatment of at least two common illnesses.
- You’ll leave this course with a broader understanding of patient teaching points surrounding the use of antibiotics.
About
Pharmacology Contact Hours Awarded: 3
Course By:
Charmaine Robinson
MSN-Ed, BSN, RN, PHN, CMSRN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Imagine a world without antibiotics…a world where potentially deadly infections have no cure. This was the case before the discovery of the first antibiotic – a time when developing an infection most likely meant a death sentence. Throughout history, the world has weathered through various pandemics and epidemics that resulted in shortened lifespans and millions of lives lost. Antibiotics, on the other hand, have expanded the human lifespan by 23 years [4]. Surprisingly enough, the first antibiotic was not discovered until the turn of the 20th century.
Today, around 80-90% of antibiotic use occurs in outpatient settings [8]. However, with growing antibiotic use comes suboptimal antibiotic prescribing practices. Many antibiotics are prescribed unnecessarily or inappropriately. National clinical guidelines are in place to help guide clinicians on best practices for prescribing antibiotics to reduce antibiotic resistance and ensure effective treatments.
This course will take learners on a journey from the very first antibiotic discovery in 1910 to current-day best practices for antibiotic use among adults in outpatient settings.
History of Antibiotics
Antibiotic therapy has fairly recent beginnings. In 1900, scientists began studying organisms within the soil and noticed that some organisms released metabolic substances that were harmful to others, a concept known as “antibiosis” [4]. Some 10 years later, to mimic this natural process, the first synthetic antibiotic “Salvarsan” was developed for the treatment of infection, specifically, syphilis [4][15].
Antibiotic discoveries remained underway until 1928, when the infamous Penicillin was incidentally discovered by a physician/microbiologist named Alexander Flemming. Penicillin was unique in that it was not synthetic, like Salvarsan. On the contrary, it was developed from a product of nature – mold. After having been away on vacation, Flemming returned to the laboratory to find mold growing on one of the petri dishes that originally contained solely the growing bacteria he and his team were studying [18]. He noticed that the bacteria were not growing in the area of the mold, which he later found to be “Penicillium notatum” or “Penicillin mold.” From here, Penicillin was developed. Penicillin became the gold standard for antibiotic therapy during its time. Antibiotic use peaked during the 1950s, and today, antibiotics are in regular use.

Self-Quiz
Ask Yourself...
- What role does microbiology play in antibiotic use?
- How often do you prescribe/administer antibiotics in your care setting?
- Are you familiar with any other “naturally occurring” antibiotics?
Statistical Evidence
In response to the many infections rampaging across the U.S., antibiotic prescribing in outpatient settings has become astronomical. In 2022, 709 antibiotic prescriptions were dispensed in U.S. outpatient pharmacies per every 1000 people, equaling a total of 236 million prescriptions in one year. The state with the highest number of prescriptions in 2022 was West Virginia, and the state with the lowest, Alaska [See Figure 1] [2].
The CDC estimates that half of all antibiotic use in outpatient settings is inappropriate in some way [8]. Inappropriate antibiotic use includes unnecessary prescribing, and inappropriate drug selection, dosing, and duration. Nearly 30% of the antibiotics prescribed in outpatient settings are simply unnecessary [8][9]. While drug selection, dosing, and duration may depend on the individual patient, prescribing unnecessary antibiotics poses a greater problem – the potential for antibiotic resistance. In the U.S., over 2.8 million antimicrobial-resistant infections occur every year, resulting in more than 35,000 deaths [10].
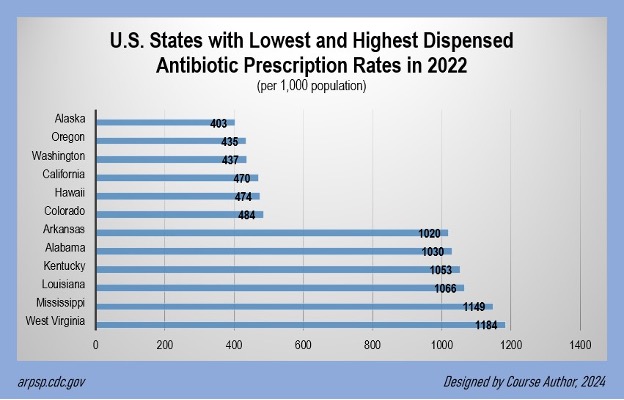
Figure 1. Dispensed Antibiotic Prescriptions in 2022, by State [2]

Self-Quiz
Ask Yourself...
- Which one of the above statistics is most alarming? Why?
- In your opinion, what are some factors that may explain why antibiotics are frequently administered in some states and not others?
- Have you ever prescribed an unnecessary antibiotic (or witnessed a provider/clinician doing so)?
Antibiotics: The Basics
Infections can be caused by bacteria, viruses, parasites, and fungi, and can colonize in multiple regions of the body. Antibiotics, however, are only effective in the treatment of infections caused by bacteria. Antibiotics treat serious bacterial infections and serve as prophylactic treatments for surgical procedures.
Antibiotics are also indicated when patients are at a high risk of developing an infection, for example, those receiving chemotherapy treatments [11]. While some infections do not require treatment with antibiotics, like simple sinus and ear infections, antibiotics are often the gold standard [11].
Antibiotics are classified by their chemical structure and generally work in one of two ways – by killing bacteria (bactericidal) or by inhibiting them from multiplying (bacteriostatic) [7]. This course will cover eight different types of antibiotics (dispensed to patients from community pharmacies in the U.S.) as outlined by the U.S. Centers for Disease Control (CDC) [7].
These include:
- Penicillin
- Macrolides
- Cephalosporins
- Fluroquinolones
- Tetracyclines
- Trimethoprim-Sulfamethoxazole
- Nitrofurantoin
- Clindamycin

Self-Quiz
Ask Yourself...
- Have you experienced patients requesting antibiotics for the common cold?
- How often do you prescribe/administer antibiotics to patients who have cancer?
- How do you distinguish between a simple ear (or sinus) infection and one that requires antibiotics?
- Which of the antibiotic types above are you most familiar with?
Outpatient Antibiotics
Penicillin
Penicillins, the most common class of antibiotics dispensed in outpatient settings, are a group of bactericidal beta-lactam drugs [7][16]. “Beta lactam” refers to the chemical structure of the drugs. Common penicillins include penicillin (PCN) and amoxicillin.
Combination Therapy
Some penicillins are formulated as part of a two-drug combination therapy with another type of medication called “beta lactamase inhibitors” (enzymes that enhance the effectiveness of the penicillins). An example of a drug within this antibiotic class is amoxicillin/clavulanate. The beta-lactamase inhibitor protects the penicillin by preventing it from being destroyed by serine beta-lactamases (enzymes produced by some bacteria) [6].
With amoxicillin/clavulanate, the antibiotic portion (amoxicillin) fights the bacteria. The beta-lactamase inhibitor portion (clavulanate) acts as a “shield,” protecting the antibiotic from potential harm caused by the bacteria, essentially, helping to prevent antibiotic resistance.
Clinicians should review information for these combination drugs separately as this course will focus on penicillins as a stand-alone drug class.
Mechanism of Action
Penicillins work by preventing bacteria from forming cell walls, which ultimately kills them. This is done by binding to penicillin-binding proteins (PBPs) within the bacteria’s cell walls, inhibiting the final stage of the wall’s formation.
Pharmacokinetics
Food may interfere with some penicillins (like penicillin G), and not with others (like amoxicillin). Penicillins are distributed quickly in the extracellular fluid of many tissues, particularly when inflammation is present. At least partially excreted in urine, most penicillins are present in high levels in the urine.
Contraindications
Clinicians should not prescribe/administer penicillins to patients with a PCN allergy.
Pregnancy and Breastfeeding
Although penicillins cross the placenta, they are considered generally safe for use during pregnancy, and although they enter breast milk in small amounts, they are considered compatible with breastfeeding as long as the infant does not have a PCN allergy.
Adverse Effects
The most common allergic reaction caused by penicillins is a rash. Other reactions include nausea, vomiting, and diarrhea. Penicillins (as with any antimicrobial drugs) can cause pseudomembranous colitis or Clostridioides difficile-associated diarrhea by altering the normal flora of the colon, leading to an overgrowth of the C. diff bacteria. Clostridiolides was previously term “Clostridium.” A black hairy tongue is a rare temporary reaction from oral penicillin (caused by keratinization of the superficial layers of the tongue).


Self-Quiz
Ask Yourself...
- Why do you think penicillins are the most commonly prescribed antibiotic in outpatient settings?
- How often do you encounter patients with PCN allergies?
- How comfortable are you with prescribing/administering antibiotics with associated pregnancy risks (when the risks are low, but the drug is deemed safe)?
- Do you find the combination form of penicillin prescribed/administered more frequently than penicillins alone?
Macrolides
Macrolides are the second most common antibiotic dispensed in outpatient settings [7]. This class of antibiotics is generally bacteriostatic but can be bactericidal when administered in high doses [16]. Common macrolides include azithromycin and erythromycin.
Mechanism of Action
Macrolides work by preventing bacteria from making the proteins necessary to multiply. This is done by binding to particular units inside of the cells of bacteria. More specifically, macrolides attach to the ‘50S’ sub-unit of a ribosome within the cytoplasm of the cell, blocking protein synthesis (proteins are made in the ribosomes of cells).
Pharmacokinetics
Food may have an effect on some macrolides (like azithromycin and extended-release clarithromycin), and not on others (like immediate-release clarithromycin). In general, macrolides are not absorbed well orally. However, they diffuse well into body fluids after absorption, with the exception of cerebrospinal fluid. This class of antibiotics is excreted primarily in bile.
Contraindications
Clinicians should not prescribe/administer macrolides to patients who have had an allergic reaction to them. Clarithromycin or erythromycin should not be taken together with astemizole (antihistamine), cisapride (for gastrointestinal mobility), pimozide (for Tourette’s syndrome), or terfenadine (antihistamine) as potentially fatal cardiac arrhythmias can occur.
Pregnancy and Breastfeeding
The safety of macrolide use during pregnancy or breastfeeding depends on the particular drug. Erythromycin is considered safer than azithromycin during pregnancy, although both carry some risks. Clarithromycin should be avoided entirely unless there is no other alternative. The only macrolide with a known compatibility with breastfeeding is erythromycin.
Adverse Effects
Macrolides, more specifically erythromycin, can cause cardiac abnormalities (like QT-interval prolongation and ventricular tachyarrhythmia), nausea, vomiting, abdominal cramps, diarrhea, ringing in the ears, dizziness, and reversible hearing loss. Clarithromycin and azithromycin can also cause QT-interval prolongation but are less likely to cause arrhythmias.

Self-Quiz
Ask Yourself...
- When prescribing/administering antibiotics in the outpatient setting, which is most beneficial for you to obtain – health histories or physical assessments?
- Why is understanding an antibiotic’s mechanism of action important before prescribing/administration?
- For what types of infections do you prescribe/administer azithromycin?
- Do you provide written materials about antibiotics to patients prior to prescribing/administering?
Cephalosporins
Similar to penicillins, cephalosporins are also a group of bactericidal beta-lactam antibiotics [16]. These particular antibiotics are characterized by “generations” (based on their coverage against certain bacteria). Some cephalosporins include cephalexin and cefdinir.
Combination Therapy
As with penicillins, some cephalosporins are formulated as part of a two-drug combination therapy with beta lactamase inhibitors. An example of a drug within this antibiotic class is ceftazidime/avibactam. Ceftazidime (the antibiotic) is protected by avibactam (the beta-lactamase inhibitor). As mentioned earlier, clinicians should review information for each combination drug separately as this section will cover the stand-alone drug class.
Mechanism of Action
Similar to penicillins, cephalosporins work by binding to penicillin-binding proteins (PBPs) within the bacteria’s cell wall to inhibit the final stage of the wall’s formation, ultimately killing the bacteria.
Pharmacokinetics
Like penicillins, cephalosporins diffuse well into most body fluids, as well as the extracellular fluid of most tissues, especially when inflammation is present. However, not all cephalosporins can reach the cerebrospinal fluid in high enough levels to treat illnesses like meningitis.
Those that have this capability include ceftriaxone, cefotaxime, ceftazidime, and cefepime. While the majority of cephalosporins are excreted mostly in urine, cefoperazone and ceftriaxone have significant biliary excretion.
Contraindications
Cephalosporins should not be prescribed/administered to patients who have had a major allergic reaction to other cephalosporins. Additionally, clinicians should take precautions when prescribing/administering cephalosporins to patients with late-onset PCN allergies as cross-sensitivity may occur (although uncommon).
Pregnancy and Breastfeeding
Cephalosporins are considered safe for use during pregnancy. However, breastfeeding is discouraged as these antibiotics can enter the breast milk and alter the infant’s gut flora.
Adverse Effects
The most common adverse effect to cephalosporins is an allergic rash (anaphylaxis is rare). This class of antibiotics, as with many, can cause C. diff-associated diarrhea. Clinicians should also consider laboratory changes associated with cephalosporins, including low white blood cell count, low platelets, increased bleeding times (more specifically with cefotetan), and a positive Coombs test (reveals presence of red blood cell antibodies).

Self-Quiz
Ask Yourself...
- What is the most common cephalosporin you have prescribed/administered?
- Why do you think it is important to know how well an antibiotic diffuses into body tissues?
- What types of antibiotic-associated rashes have been reported by patients in your care setting?
- When prescribing/administering cephalosporins, what do you think is a major teaching point for patients?
Fluroquinolones
Fluroquinolones are a class of antibiotics that are bactericidal (dependent on the concentration) [16]. Common fluroquinolones include ciprofloxacin and levofloxacin.
This class of antibiotics has a black box warning (see below).
Mechanism of Action
Fluroquinolones work by keeping bacteria from making DNA, thus killing them. This is done by inhibiting the activity of two enzymes, “DNA gyrase” and “topoisomerase” (both essential for some bacteria’s DNA replication).
Pharmacokinetics
Fluroquinolones’ absorption in the body can be diminished when given with aluminum, magnesium, calcium, zinc, and iron preparations (e.g., antacids, many vitamins/minerals). This class of antibiotics is distributed in most intra- and extracellular fluids, concentrating in the prostate, lungs, and bile. Fluroquinolones are excreted in urine at high levels, with the exception of moxifloxacin, which is excreted primarily in bile.
Contraindications
Clinicians should not prescribe/administer fluroquinolones to patients who have had an allergic reaction to them, or those who have disorders that predispose them to arrhythmias. These disorders include prolonged QT-interval, uncorrected low electrolyte imbalances (potassium and magnesium), and significant bradycardia.
Fluroquinolones should also be avoided in patients who take medications that cause prolonged QT-interval and significant bradycardia, including metoclopramide (used for nausea and GI motility), cisapride (for GI mobility), erythromycin, clarithromycin, certain antiarrhythmic medications (classes Ia and III), and tricyclic antidepressants.
A black box warning cautions clinicians against prescribing/administering fluroquinolones to patients with central nervous system (CNS) disorders (potential for irreversible CNS damage), and those with myasthenia gravis (potential for muscle weakness exacerbation) (more on Black Box warnings below) [13].
Pregnancy and Breastfeeding
Precautions should be taken with fluroquinolone use during pregnancy as studies show some potential risks. Fluroquinolones enter breastmilk and should therefore be avoided during breastfeeding.
Adverse Effects
Fluroquinolones can cause GI problems like upper GI irritation and C. diff (strong association). Hypoglycemia (especially when coupled with antihyperglycemic drugs), prolonged QT-interval, photosensitivity, and sunburn reactions may occur as well. Although rare, clinicians may note a low white blood cell count and anemia.
Black Box Warnings
The U.S. Food and Drug Administration (FDA) placed black box warnings on Fluroquinolones citing disabling and potentially irreversible severe adverse effects of the tendons, muscles, joints, nerves, and CNS. These adverse effects can occur hours to weeks after exposure to both the oral and parenteral forms of fluroquinolones [13].
Potential adverse effects include: [16]
- Achilles tendon rupture
- Peripheral neuropathy
- Seizures
- Increased intracranial pressure, including pseudotumor cerebri (or “idiopathic intracranial hypertension”)
- Toxic psychosis
- Muscle weakness
- Other CNS symptoms: Nervousness, anxiety, agitation, insomnia, nightmares, dizziness, mood alteration, paranoia, confusion, tremors, hallucinations, and depression.

Self-Quiz
Ask Yourself...
- How are you informed of any new black box warnings for medications in your care setting?
- Why do you think it is important to know in what area of the body an antibiotic is concentrated?
- How often do you order follow up labs for patients after antibiotic therapy (or witnessed a provider/clinician doing so)?
- What was the most severe antibiotic-associated adverse effect reported by a patient under your care?
Tetracyclines
Tetracyclines are a bacteriostatic class of antibiotics frequently dispensed in outpatient settings [16]. Common tetracyclines include tetracycline and doxycycline.
Mechanism of Action
Similar to macrolides, tetracyclines work by preventing bacteria from making the proteins necessary to multiply by binding to units within the bacteria’s cells. While macrolides attach to the ‘50S’ sub-unit of a ribosome within the cytoplasm of the bacteria’s cell, tetracyclines attach to the ribosome’s ‘30S’ sub-unit instead, ultimately serving the same purpose – blocking protein synthesis.
Pharmacokinetics
Pharmacokinetics depends on each individual medication within the drug class. For example, food decreases the absorption of some tetracyclines, but this is not significant for doxycycline in particular. Additionally, only 60-80% of the specific drug “tetracycline” is absorbed after oral use, while more than 90% of doxycycline is absorbed. Tetracyclines’ absorption in the body can be diminished when given with aluminum, magnesium, calcium, zinc, and iron preparations (antacids, many vitamins/minerals).
Tetracyclines penetrate most body tissues and fluids and are concentrated in unobstructed bile. They are primarily excreted in urine with the exception of a few (like doxycycline) which are excreted primarily in the GI tract.
Contraindications
Clinicians should not prescribe/administer tetracyclines to patients who have had an allergic reaction to them.
Pregnancy and Breastfeeding
Clinicians should take precautions when prescribing/administering tetracyclines to patients who are pregnant as they can cross the placenta, enter the fetus’ blood, and accumulate in fetal bones. This class of antibiotics can cause permanent discoloration of the fetus’ teeth if used during the second or third trimester of pregnancy. Breastfeeding is typically discouraged as tetracyclines enter breast milk (though in small amounts).
Adverse Effects
Tetracyclines can cause GI problems including nausea, vomiting, C. diff-associated diarrhea, and fatty degeneration of the liver (particularly during pregnancy). These antibiotics can also cause photosensitivity (sunburn reaction), yeast infections, and esophageal erosions (if not swallowed with water).
Tetracyclines can cause azotemia (buildup of nitrogen and waste products in the blood) and elevated phosphate levels in patients with renal insufficiency (with the exception of doxycycline, which is primarily excreted in the GI tract, as mentioned earlier).

Self-Quiz
Ask Yourself...
- Where in your care setting can you locate drug information?
- Have you ever cared for a patient with an antibiotic-associated yeast infection?
- How do you determine which adverse effects to focus on during patient teaching?
- How often have you consulted with an infectious disease specialist in your care setting (or witnessed a provider/clinician doing so)?

Trimethoprim-Sulfamethoxazole
Trimethoprim-sulfamethoxazole (TMP-SMX) is a bactericidal two-drug combination antibiotic [16]. While this drug is not necessarily a class of antibiotics, it is often dispensed in outpatient settings to treat infections, particularly those related to the urinary tract. The sulfamethoxazole portion of the drug falls under the antibiotic class of sulfonamides.
Mechanism of Action
TMP-SMX keeps bacteria from multiplying. This is done by preventing the bacteria from making folic acid (folic acid is needed to help bacteria make DNA and proteins). Each drug of the combination has its own task in inhibiting certain steps of the folate synthesis process within the bacteria’s cells. TMP binds tightly to dihydrofolate reductase (an enzyme that helps to break down folic acid components) making it difficult for the enzyme to do its job. SMX acts in a similar way by binding to dihydropteroate synthase (another enzyme needed in the process).
Pharmacokinetics
TMP-SMX is absorbed well orally and excreted in the urine. This drug also penetrates well into body tissues and fluids, including cerebrospinal fluid. TMP in particular, is concentrated in prostatic tissue.
Contraindications
TMP-SMX should not be prescribed/administered to patients who have had an allergic reaction to the drug. Clinicians should use precautions when prescribing/administering TMP-SMX to patients with folate deficiency, renal insufficiency, and/or liver dysfunction.
Pregnancy and Breastfeeding
TMP-SMX should be avoided during the first trimester of pregnancy (risk for neural tube defects) and near birth. However, if this medication cannot be avoided, clinicians should co-prescribe/administer folic acid supplements. Clinicians should consider that this antibiotic can increase unconjugated bilirubin blood levels, increasing the risk of kernicterus (bilirubin-induced brain damage) in the fetus/infant. Breastfeeding is typically discouraged as sulfonamides enter breast milk.
Adverse Effects
The most common adverse effects include nausea, vomiting, and rash. Clinicians might expect to see laboratory changes in patients taking this drug, including low folate (leading to macrocytic anemia) and high potassium (up to life-threatening levels). Low white blood cell counts, and low platelets can occur with prolonged use.
TMP in particular, can cause an artificial increase in creatinine level, although more likely in patients with diabetes and renal insufficiency. Renal failure in patients with underlying renal insufficiency may also be noted.

Self-Quiz
Ask Yourself...
- For what types of infection is TMP/SMX typically prescribed/administered in your care setting?
- What are the most common TMP/SMX adverse effects reported in your care setting (if any)?
- In your opinion, why is it important to know how an antibiotic is excreted? What benefit does this information provide?
- How often do you consult with nephrologists (or witness a provider/clinician doing so) when prescribing antibiotics to patients with renal failure?
Nitrofurantoin
Nitrofurantoin, a urinary anti-infective, is a commonly dispensed antibiotic in the outpatient setting. This drug has bactericidal properties particularly when in a patient’s urinary tract at therapeutic doses [16].
Mechanism of Action
While the mechanism of action for nitrofurantoin is considered somewhat unusual and not entirely understood, the drug is known to have two mechanisms – to kill bacteria by preventing its cell wall from forming, and to keep them from multiplying by preventing their ability to make DNA and proteins [1]. This is done by inactivating or altering ribosomal proteins and other macromolecules within the bacteria’s cells.
Pharmacokinetics
Nitrofurantoin can be poorly absorbed when prescribed/administered with antacids containing magnesium trisilicate. This drug does not reach therapeutic levels in the blood, but rather in the patient’s urine.
Contraindications
Nitrofurantoin should not be prescribed/administered to patients who have had an allergic reaction to the drug. Clinicians should not prescribe/administer this drug to patients with renal insufficiency. Additionally, this drug should not be prescribed/administered to pregnant patients who are at term, during labor, or at delivery as it can damage the infant’s red blood cells (hemolytic anemia).
Pregnancy and Breastfeeding
Nitrofurantoin is generally considered safe during all trimesters of pregnancy. However, as mentioned above, this drug should not be prescribed/administered at term, during labor or at delivery. This medication should be avoided in the first month of breastfeeding to reduce the risk of hemolytic anemia (especially in infants with high bilirubin).
Adverse Effects
Paresthesia’s (“pins and needles” skin sensations) can occur, followed by peripheral neuropathies, especially in patients with renal failure. Clinicians may note pulmonary changes like allergic inflammation of the lungs (pneumonitis) and chronic progressive lung fibrosis (usually occurs when drug is used for more than six months). Hemolytic anemia can occur in patients with G6PD deficiency (G6PD is an enzyme that protects red blood cells). Labs can reveal a low white blood cell count.

Self-Quiz
Ask Yourself...
- In your opinion, is there a benefit in knowing if an antibiotic is bactericidal (kills bacteria) or bacteriostatic (prohibits them from multiplying)?
- In your practice, has nitrofurantoin been effective in the treatment of urinary infections?
- Have you ever cared for a patient with permanent sequalae (or disability) caused by an allergic reaction to an antibiotic?
Clindamycin
Commonly used in outpatient settings, clindamycin is part of the class of antibiotics called lincosamides and is primarily bacteriostatic [16]. Clindamycin has a black box warning (see below).
Mechanism of Action
Like macrolides, lincosamides also work by preventing bacteria from making the proteins necessary to multiply through binding to the ‘50S’ sub-unit of a ribosome within the cytoplasm of the bacteria’s cell. This in turn blocks protein synthesis, causing changes in the surface of the cell’s wall, making it more difficult for the bacteria to adhere to host cells [5].
Pharmacokinetics
Not only is clindamycin absorbed well, but it also diffuses well into body fluids, with the exception of cerebral spinal fluid. Clindamycin is excreted in bile and urine.
Contraindications
Clinicians should not prescribe/administer clindamycin to patients who have had an allergic reaction to the drug. Clinicians should use precaution when prescribing/administering clindamycin to patients with a history of Crohn’s disease, ulcerative colitis, or antibiotic-associated colitis (due to the drug’s strong ability to cause a C. diff infection: see black box warning below).
Pregnancy and Breastfeeding
Clindamycin may be used during pregnancy as research trials showed no association with increased birth defects when given during the second and third trimester. Breastfeeding is not recommended as clindamycin enters breast milk.
Adverse Effects
The primary adverse effect of clindamycin is C. diff-associated diarrhea (strong association). Clindamycin can cause allergic skin reactions from as mild as a maculopapular rash to a life-threatening skin condition called toxic epidermal necrolysis (or “TEN”), which causes pain, blisters, and peeling. Other adverse effects include esophagitis (if not swallowed with water), and prolongation of the QT interval (especially in patients already at risk).
Black Box Warnings
The FDA placed a black box warning on clindamycin citing association with severe colitis that can be fatal, more so than with any other antibiotic [14]. The FDA recommends reserving this antibiotic for patients with a PCN allergy or when penicillin is not appropriate. The FDA also recommends this antibiotic for serious infections only or when other less toxic antibiotics are not appropriate. Clinicians are also encouraged to consider the nature of the infection and the susceptible bacteria.

Self-Quiz
Ask Yourself...
- Is there a protocol in place in your care setting that provides guidance on prescribing/administering an antibiotic with a black box warning?
- Have you ever cared for a patient with antibiotic-associated C. diff?
- Has there ever been a time in your practice in which you had no choice but to prescribe/administer an antibiotic to a patient who had a mild non-life-threatening allergic reaction to the drug in the past?
- What are some common labs you order (or witness providers/clinicians ordering) related to antibiotic use?
Antibiotic Guidelines for the Treatment of Common Illnesses
Common illnesses in the community include the common cold (or non-specific upper respiratory infection), acute uncomplicated bronchitis, acute rhinosinusitis, pharyngitis, and acute uncomplicated cystitis (bladder infection). The CDC outlines recommendations for clinicians in the treatment of common illnesses.
Antibiotics are not recommended for common colds as these illnesses are viral. In the past, many cases of uncomplicated bronchitis had been routinely treated with antibiotics (azithromycin or “Z-pack”) as the illness is in fact bacterial. However, new practices discourage the use of antibiotics for this type of bronchitis, instead focusing on symptom management.
The following are the most recent recommendations for antibiotic therapy in the outpatient setting [12].

Acute Rhinosinusitis
Most cases of acute rhinosinusitis cases are viral (98%), but of the bacterial cases, antibiotics are only indicated when signs/symptoms are severe, persistent, and/or worsening. These may include fever up to 39 degrees Celsius (102 degrees Fahrenheit), presence of purulent nasal discharge, or facial pain.
Antibiotic recommendations:
Clinicians can prescribe penicillins, more specifically amoxicillin/clavulanate for the treatment of acute rhinosinusitis. For patients with a PCN allergy, doxycycline, or respiratory fluoroquinolone (levofloxacin or moxifloxacin), may be used as alternatives. Clinicians should note that antibiotics may or may not be effective for acute rhinosinusitis even though the infection may be bacterial.
Pharyngitis
While most cases of pharyngitis are viral, approximately 5-10% are caused by the bacteria Group A streptococcus. The illness is known as Group A Streptococcal pharyngitis (GAS) or by its more common name, “Strep throat.” Clinicians are discouraged from attempting to distinguish between bacterial and viral pharyngitis based on signs/symptoms alone.
Antibiotic therapy is only indicated when bacterial pharyngitis is confirmed by a rapid antigen detection test (RADT).
Antibiotic recommendations:
Clinicians can prescribe penicillins (PCN and Amoxicillin) for the treatment of GAS. For patients with a PCN allergy, cephalexin, cefadroxil, clindamycin, or macrolides are recommended. However, clinicians should note that GAS is becoming increasingly resistant to clindamycin (and azithromycin).
Acute Uncomplicated Cystitis
Most common in women, symptoms of uncomplicated cystitis include frequent voiding, voiding in small amounts each time, and urgency. Pelvic pain and blood in the urine are not common with the uncomplicated type of cystitis. Clinicians should test urine for nitrates and leukocyte esterase to obtain the most accurate diagnosis prior to treatment with antibiotics.
Antibiotic recommendations:
The CDC focuses on treatment in women as the infection is most common in this group. For healthy adult non-pregnant premenopausal women, first-line choice antibiotics include nitrofurantoin, TMP/SMX, and Fosfomycin (a newer antibiotic). Clinicians can prescribe/administer fluoroquinolones, but they should be used only when other antibiotics are not appropriate.

Self-Quiz
Ask Yourself...
- Have you ever prescribed an antibiotic based on symptoms alone (or witnessed a provider/clinician doing so)?
- How often do you prescribe/administer antibiotics for sinus infections?
- When two different antibiotics treat the same infection, what do you think are the primary reasons providers/clinicians choose one antibiotic over the other?
- How often have you discouraged treatment with oral antibiotics, instead recommending a patient to receive inpatient care for intravenous antibiotics (or witnessed a provider/clinician doing so)?
Antibiotic Guidelines for Treatment of Sexually Transmitted Infections
In 2021, the CDC outlined guidelines for the treatment of STIs. Antibiotics should be prescribed after confirming diagnosis with the appropriate tests. Many antibiotic treatments are one-time doses that can be administered in the outpatient setting.
Some require take-home doses for a few days and up to a week. This course will cover the CDC recommendations for chlamydia, gonorrhea, and Mycoplasma Genitalium [17].
Chlamydia
Chlamydia is the most commonly reported bacterial infectious disease in the U.S. (highest among people under age 24) [17].
Antibiotic recommendation:
Oral doxycycline for one week is recommended as a treatment for chlamydia. A one-time oral dose of azithromycin may also be prescribed/administered. A final alternative is oral levofloxacin for one week.
Gonorrhea
Gonorrhea is the second most commonly reported bacterial infectious disease in the U.S. and may be centralized to the throat, genitals, or rectum. [17]. Often asymptomatic in women, gonorrhea can cause a painful or burning sensation during urination in men [3].
Antibiotic recommendation:
- For uncomplicated gonorrhea of the cervix, urethra, or rectum: one dose of intramuscular (IM) ceftriaxone is indicated. If ceftriaxone is not available, one dose of IM gentamicin in combination with one dose of oral azithromycin may be administered. Another alternative is one dose of oral cefixime.
- For uncomplicated gonorrhea of the throat: one dose of IM ceftriaxone is indicated.
Mycoplasma Genitalium
Mycoplasma genitalium is a bacteria associated with urethritis in men and cervicitis and pelvic inflammatory disease (PID) in women. Clinicians should be aware that although azithromycin is used to treat the infection, the bacteria is becoming increasingly resistant to the drug [17].
Antibiotic recommendation:
The type of antibiotic treatment is dependent on if M. gentalium antibiotic resistance testing is available.
- If M. genitalium resistance testing is available and the patient is macrolide-sensitive, oral doxycycline for one week followed by oral azithromycin for three days is indicated.
- If M. genitalium resistance testing is available and the patient is macrolide-resistant, oral doxycycline for one week followed by oral moxifloxacin for seven days is indicated.
- If resistance testing is not available but the bacteria is detected by an FDA-cleared nucleic acid amplification (NAAT) test, oral doxycycline for one week followed by oral moxifloxacin for seven days is indicated.

Self-Quiz
Ask Yourself...
- Throughout your nursing career, how often have you reviewed nationally published clinical practice guidelines on your own?
- Prior to prescribing/administering one-time IM antibiotic doses in the outpatient setting, what type of assessments do you perform? Vital signs? Labs? EKG?
- Have you ever witnessed a patient have an allergic reaction to a one-time IM antibiotic dose in your care setting?
- Do you find it time-consuming to determine which antibiotic is most appropriate for a patient? (Or do you feel that this may be time-consuming for providers/clinicians in your care setting?)
Patient Teaching
To ensure adequate treatment for bacterial infections, clinicians should instruct patients on infection control prevention strategies and antibiotic therapy. Education should include drug indication, dosing, precautions, adverse effects, the benefits of adherence, and the risks of nonadherence.
The following are some key teaching points to include [11].
Infection Prevention
- Wash hands with soap and water for at least 20 seconds (may use hand sanitizer that contains at least 60% alcohol)
Indications
- Antibiotics only treat bacterial infections, not viral infections like the common cold or influenza.
- Antibiotics may not be necessary for the treatment of some uncomplicated infections, like sinus and ear infections.
Prescriptions
- Complete the full antibiotic regimen as prescribed even if feeling better. Not doing so can lead to partial treatment, which may lead to worsening infection.
Adverse Effects
- Antibiotics may cause a bowel infection caused by the organism Clostridioides difficile (C. diff). A C. diff infection causes diarrhea and other bowel symptoms, leading to colon damage and potential death.
- Antibiotics can also cause rash, dizziness, nausea, and yeast infections
- Inform the provider or nurse if you feel worse after taking the antibiotics.


Self-Quiz
Ask Yourself...
- How often have you experienced patients failing to complete the full antibiotic regimen as prescribed?
- Have you ever had a patient return with worsening symptoms after having been prescribed/administered antibiotics in your care setting?
- How often do you think providers/clinicians rely on pharmacists to educate patients about their antibiotic prescriptions?
- On average, how much time do you spend educating patients on antibiotic therapy?
Conclusion
Nurse clinicians working in outpatient settings have the responsibility of keeping the public safe and properly educated on antibiotic use. While some antibiotics may be administered in the clinic or office as one-time doses, many are prescribed to patients to take home and complete the doses on their own.
Better prescribing practices are dependent on staying abreast of national clinical guidelines surrounding antibiotic use. With antibiotic resistance on the rise, appropriate prescribing, safe administration, and effective patient teaching is of upmost importance. Better prescribing practices lead to better patient outcomes.
References + Disclaimer
- Center for Drug Evaluation and Research, U.S. Food and Drug Administration. (2021). Macrobid. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/020064Orig1s029lbl.pdf
- Division of Healthcare Quality Promotion (DHQP), U.S. Centers for Disease Control and Prevention. (n. d.). Antibiotic use & stewardship: All antibiotic classes. https://arpsp.cdc.gov/profile/antibiotic-use/all-classes
- Division of STD Prevention, National Center for HIV, Viral Hepatitis, STD, & TB Prevention, U.S. Centers for Disease Control and Prevention. (2022). Gonorrhea – CDC basic fact sheet. https://www.cdc.gov/std/gonorrhea/stdfact-gonorrhea.htm
- Hutchings, M. I., Truman, A. W., & Wilkinson, B. (2019). Antibiotics: past, present, and future. Current Opinion in Microbiology, 51, 72–80. https://doi.org/10.1016/j.mib.2019.10.008
- Johnson, M. (2023). Clindamycin: Overview. UpToDate. https://www.uptodate.com/contents/clindamycin-an-overview
- Khanna, N.R., Gerriets, V. (2022). Beta-Lactamase Inhibitors. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK557592/
- National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP) U.S. Centers for Disease Control and Prevention. (n. d.). Antibiotic resistance & patient safety portal outpatient antibiotic prescription data: Antibiotic class definitions. https://arpsp.cdc.gov/resources/OAU-Antibiotic-Class-Definitions.pdf
- National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP), U.S. Centers for Disease Control and Prevention. (2022). Measuring outpatient antibiotic prescribing. https://www.cdc.gov/antibiotic-use/data/outpatient-prescribing/index.html
- National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP), U.S. Centers for Disease Control and Prevention. (2023). Antibiotic prescribing and use. https://www.cdc.gov/antibiotic-use/index.html
- National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP), U.S. Centers for Disease Control and Prevention. (2021). Antimicrobial resistance: National infection and death estimates. https://www.cdc.gov/drugresistance/national-estimates.html
- National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP), U.S. Centers for Disease Control and Prevention. (2021). Patient safety: Smart use, best care. https://www.cdc.gov/patientsafety/features/be-antibiotics-aware.html
- National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP), U.S. Centers for Disease Control and Prevention. (2017). Antibiotic prescribing and use: Healthcare professional resources and training: Adult outpatient treatment recommendations. https://www.cdc.gov/antibiotic-use/clinicians/adult-treatment-rec.html
- U.S Food and Drug Administration. (2016). FDA news release: FDA updates warnings for fluoroquinolone antibiotics. https://www.fda.gov/news-events/press-announcements/fda-updates-warnings-fluoroquinolone-antibiotics
- U.S. Food and Drug Administration. (2014). CLEOCIN HCl®: Clindamycin hydrochloride capsules, USP: Reference ID: 3532960 https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/050162s092s093lbl.pdf
- Vernon, G. (2019). Syphilis and Salvarsan. The British Journal of General Practice: The Journal of the Royal College of General Practitioners, 69(682), 246. https://doi.org/10.3399/bjgp19X702533
- Werth, B. J. (2022). Bacterial and antibacterial drugs. Merck Manual Professional Version. https://www.merckmanuals.com/professional/infectious-diseases/bacteria-and-antibacterial-drugs
- Workowski, K.A., Bachmann, L.H., Chan, P.A., Johnston, C.M., Muzny, C.A., Park, I., Reno, H., Zenilman, J.M., & Bolan, G.A. (2023). Sexually transmitted infections treatment guidelines, 2021. MMWR Recommended Report 70(No. RR-4), 1-187. https://www.cdc.gov/mmwr/volumes/70/rr/rr7004a1.htm#chlamydialinfections
- De Simeis, D., & Serra, S. (2021). Actinomycetes: A never-ending source of bioactive compounds-An overview on antibiotics production. Antibiotics (Basel, Switzerland), 10(5), 483. https://doi.org/10.3390/antibiotics10050483
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
