HELLP Syndrome
Contact Hours: 2
Author(s):
Abbie Schmitt, MSN-Ed, RN
Course Highlights
- In this HELLP Syndrome course, we will learn about he pathophysiology behind HELLP syndrome, including its impact on the liver, hematologic system, and vascular function.
- You’ll also learn the clinical presentation and early signs of HELLP syndrome.
- You’ll leave this course with a broader understanding of individualized care plans for client education and postpartum follow-up.
Introduction
HELLP syndrome is a life-threatening pregnancy complication that impacts both the mother and fetus, often emerging in the third trimester or shortly after delivery. The syndrome is characterized by Hemolysis, Elevated Liver enzymes, and Low Platelet count, and it is considered a severe form of preeclampsia, although it can also occur in the absence of high blood pressure. Nurses play a critical role in the early identification and management of HELLP syndrome.
This course is designed to equip nurses with a comprehensive understanding of the best practices in clinical management of HELLP syndrome. Learners will learn to recognize early warning signs, perform appropriate interventions, and provide ongoing care to both mother and baby.
Definition
When you think of “HELLP syndrome,” think of hemolysis, elevated liver enzymes, and low platelet count syndrome. HELLP is an acronym for this rare, life-threatening condition that affects pregnant and postpartum women. HELLP syndrome is a complication of preeclampsia or eclampsia. It is important to review these conditions to gain a strong foundation for HELLP syndrome.
Preeclampsia or eclampsia are considered hypertensive disorders of pregnancy. Hypertensive disorders are some of the most common medical complications during pregnancy, labor, birth, and the postpartum period (9).

Preeclampsia
Preeclampsia is a condition characterized by a new onset of hypertension (with blood pressure greater than or equal to 140 mm Hg systolic or greater than or equal to 90 mm Hg diastolic) on two occasions at least 4 hours apart in previously normotensive women and proteinuria (≥300 mg in a 24-hour urine collection). However, proteinuria is not required for the diagnosis to be made.
It often occurs alongside liver enzyme abnormalities. In the absence of proteinuria, the client must meet blood pressure parameters and have any one or more of the following to meet preeclampsia diagnostic criteria:
- Platelets <100,000 µL
- Serum creatinine >1.1 or doubling of serum creatinine in the absence of renal disease
- Elevated concentrations of blood liver transaminases to at least twice normal level
- Pulmonary edema
- New onset of cerebral or visual disturbances
Preeclampsia typically occurs after the 20th week of pregnancy. It is often accompanied by signs of damage to other organs, most often the liver and kidneys, and may involve swelling in the hands, feet, or face.
Symptoms can include headaches, vision changes, upper abdominal pain, and shortness of breath. Left untreated, preeclampsia can cause serious, even fatal, complications for both mother and baby, such as placental abruption, growth restriction, or premature birth.
The only definitive cure for preeclampsia is the delivery of the baby, so if it develops earlier in pregnancy, management focuses on controlling blood pressure and preventing complications until the baby can be delivered safely.
There are several subtypes of preeclampsia. Most commonly, these subtypes are associated with their timing of onset within pregnancy or in the postpartum period.
- Early onset preeclampsia – Occurs before 34 weeks of gestation
- Late-onset preeclampsia – Occurs on or after 34 weeks of gestation
- Postpartum preeclampsia – Can occur up to 6 weeks postpartum
If signs and symptoms of preeclampsia or eclampsia occur in women with chronic hypertension, the diagnosis of chronic hypertension with superimposed preeclampsia or eclampsia is appropriate.
Eclampsia
Eclampsia is characterized by the onset of seizures in a client with preeclampsia and no history of preexisting neurologic pathology or other identifiable cause of the seizure activity (9). Eclampsia occurs in 0.5% of clients with mild preeclampsia and 2% to 3% of those with severe preeclampsia (4).
Eclamptic seizures are a life-threatening emergency and can occur in antepartum, intrapartum, or postpartum periods of pregnancy.
Eclampsia often precedes nervous system symptoms such as headache and visual changes. Eclamptic seizures are usually generalized tonic-clonic, 60- to 90-second seizures. Postictal confusion, agitation, or combativeness are common after the seizure occurs (4). It is recommended to screen all women with hypertension during pregnancy for proteinuria.
Early detection of preeclampsia is the primary prevention tool for predicting the development of eclampsia; there is currently no specific testing or lab work to detect eclampsia.
Epidemiology
HELLP occurs in 0.2–0.8% of pregnancies and exclusively occurs in the third trimester to the postpartum period (10). This condition is considered a severe complication of pregnancy that coexists in 70–80% of cases with preeclampsia (5). The maternal mortality associated with HELLP syndrome is 1.1–2.0% of cases, and perinatal mortality is as high as 33% (10).
Misdiagnosis and delayed recognition of HELLP syndrome are very common due to vague and varying presentations (7). Although eclampsia is uncommon in developed countries, it is still a major cause of maternal morbidity and mortality worldwide (4).
Ask yourself...
- Why is HELLP syndrome considered a complication of preeclampsia?
- What percentage of women diagnosed with preeclampsia develop HELLP syndrome?
- Is the mortality rate higher during the pregnancy or perinatal period?
- In which trimester is HELLP syndrome typically evaluated and diagnosed?
- How often do you see HELLP syndrome in your practice? Do you feel that this has been increasing or decreasing?
Pathophysiology
Preeclampsia has been called the “disease of theories.” The disease is heterogeneous, and each subtype of preeclampsia may have varying pathophysiology. Research studies are consistently conducted to identify the pathophysiology and genetic, immunologic, biologic, and pathophysiologic causes.
Although the exact mechanism is unknown, preeclampsia is believed to result from a complex combination of maternal and fetal factors. Recent models suggest that factors (immune, genetic, and biological) before pregnancy may cause the condition’s onset very early after conception.
Normal physiologic adaptations to pregnancy include the following (9):
- An increase in plasma volume
- Vasodilation of the vascular bed
- Decreased systemic vascular resistance
- Increased cardiac output
- Increased prostacyclin production
Dilutional anemia, lower systemic blood pressures, a mild increase in heart rate, and peripheral edema are physical assessment findings consistent with these changes (9).
In preeclampsia, these normal adaptations are different. Instead of a plasma volume increase, there is a decrease in circulating plasma volume (9). In cases of preeclampsia, average plasma volume is usually around 9% below average progression of the disease and up to 40% below normal with severe disease (9).
The volume depletion may increase blood viscosity, leading to a decrease in maternal organ perfusion. Vasoconstriction and increased vascular tone are also a result. Vasoconstriction is due to increased systemic vascular resistance and hypertension.
Reduced intravascular volume and vasoconstriction cause decreased organ perfusion, and as the condition progresses, red blood cell hemolysis may further impair tissue oxygenation. As we mentioned, during normal pregnancy adaptation, cardiac output should increase to adapt to the new needs that impact blood pressure.
The pathophysiology of HELLP syndrome is believed to be the result of an enhanced inflammatory state where maternal immune and endothelial cells react to syncytiotrophoblast cells. The syncytiotrophoblast membrane separates maternal and fetal blood (10).
In HELLP, placental protein (PP13) is abnormally incorporated into the membrane, and there is a shift toward soluble FMS-like tyrosine kinase 1 (sFLT1) protein, which favors an overall more antiangiogenic environment (10). A decrease in the placental growth factor (PlGF) levels has been noted in both preeclampsia and HELLP (10). This change is thought to induce maternal vascular endothelial dysfunction, which causes arterial hypertension and a dramatic inflammatory response (10).
As HELLP syndrome progresses closer to term, abnormal reactions lead to thrombotic microangiopathy and hemolysis. The liver damage that occurs in HELLP is caused by soluble CD95L (sCD95L), which has been noted at increased levels in maternal blood in HELLP and causes liver cell apoptosis (10). This leads to an increase in enzymes in the bloodstream.
Ask yourself...
- How does normal pathophysiology in pregnancy differ from the pathophysiology of HELLP syndrome development?
- In what ways can volume depletion impact overall organ perfusion?
- How would you describe HELLP to a patient who was just diagnosed?
Risk Factors
The exact cause of HELLP syndrome is not fully understood. There are theories that it results from genetic mutation and inflammatory origin (5). HELLP syndrome implies impaired placentation during the early stages of pregnancy, associated with hepatic and coagulation cascade (9).
Female relatives, including the mothers of clients with preeclampsia, often have a history of the disorder (3). There is evidence that connects inheritance as either an autosomal recessive trait or an autosomal dominant trait with variable penetrance (3). Women with a hypercoagulable condition (e.g., with factor V Leiden or anticardiolipin antibodies) are at risk for developing early and severe preeclampsia
A genetic analysis of the inheritability predisposition of HELLP syndrome in pregnancy has been explored. Results revealed both genetic and immunological factors that play a role in pathogenesis.
Risk Factors for the Development of Preeclampsia (9):
- First pregnancy (nulliparity)
- Pregnancy through artificial reproductive technology
- Older maternal age
- African American
- Personal or family history of preeclampsia
- Obesity
- Preexisting or gestational diabetes
- Preexisting collagen vascular disease (systemic lupus erythematosus)
- Preexisting chronic hypertension
- Renal disease
- Antiphospholipid antibody syndrome
- Hydatidiform mole
- Periodontal disease
- Thrombophilic disorders

Ask yourself...
- Can you discuss the risk factors for HELLP syndrome?
- Why is a thorough personal and family history important for these clients?
- How can conditions that cause increased coagulability impact the development of HELLP syndrome?
- Is HELLP syndrome more or less common in first pregnancies?
- What education can you provide to patients to help reduce the risk of HELLP?
Case Study: Monique
Monique is a 33-year-old African American client, G1P0 (first pregnancy), at 34 weeks gestation. She has no significant medical history and had a normal, healthy pregnancy until the third trimester.
Monique arrived at the emergency department with complaints of persistent upper right abdominal pain, nausea, headaches, and swelling in her legs. She is also worried because she has not felt her baby move very much over the past 24 hours.
Upon arrival, the following assessments were completed:
- Blood pressure: 170/100 mm Hg
- Heart rate: 94 bpm
- Respiratory rate: 20 breaths per minute
- Physical examination: Generalized edema, especially in the legs and face, tenderness upon palpation in the right upper quadrant of the abdomen.
- Fetal monitoring: Mild fetal heart rate decelerations and decreased variability.
Monique was admitted to the hospital for further evaluation due to her concerning symptoms.
Ask yourself...
- Does Monique have any risk factors that increase the likelihood of HELLP syndrome?
- Do you note any abnormal findings in the initial assessment?
- What interventions would you anticipate doing to assist this patient?
Assessment
Review of Health History
- Assess for general symptoms of preeclampsia
- Hypertension, proteinuria, and edema are the classic triad symptoms of preeclampsia.
- Also, ask about abdominal pain, frequent, severe headaches, vision abnormalities, and shortness of breath.
- Review medications
- Preeclampsia development may be increased by using certain medications during pregnancy
Physical Assessment
- Monitor vital signs closely
- Assess the respiratory status
- Auscultation of the lungs checks for pulmonary abnormalities if the client complains of shortness of breath.
- Palpate the abdomen
- Palpate the right upper quadrant and the epigastric region to check for tenderness.
- Assess for edema
- While swelling in pregnancy is normal, monitor closely for a rapid onset of dependent edema in the lower extremities or edema in the hands or face.
- Monitor fetal growth
- Obtain weight at regular intervals
- Monitor intake and output
- Decreased urine output may indicate impaired kidney function due to low blood volume in circulation.
Diagnostic Procedures
- Collect samples for urine tests and monitor for the following abnormal findings:
- Urine dipstick result of 1+ or greater
- 24-hour urine collection with 300 mg of protein
- Urine protein to creatinine ratio > 0.3
- Laboratory tests are needed to establish the diagnosis of HELLP syndrome:
- Complete blood count
- Peripheral smear
- Liver function tests: aspartate aminotransferase (AST), alanine aminotransferase
- (ALT), and bilirubin
- Creatinine
- Fetal assessment includes:
- Non-stress tests and biophysical profile
- Ultrasound of the amniotic fluid index
- Estimated fetal weight
- CT scans or MRIs may be utilized to assess for intracranial abnormalities if the client displays severe headaches, neurological deficits, and seizures (8).
Hemolysis may also present with jaundice or hematuria; if hemolysis is longer, lymphadenopathy, hepatosplenomegaly, and cholestasis may be noted.
Results that will help confirm hemolysis include:
- Elevated reticulocyte count
- Increased lactate dehydrogenase (LDH)
- LDH is found intracellularly, therefore when RBCs rupture, this value increases.
- Elevated unconjugated bilirubin
- Unconjugated bilirubin is higher because the destruction of RBCs causes the body to be unable to eliminate it as quickly.
- Decreased Haptoglobin.
- Haptoglobin binds free hemoglobin, so when this protein binds to hemoglobin, it will decrease overall Haptoglobin levels.
Hemoglobin concentration can indicate the extent of hemolysis but cannot specifically indicate hemolysis related to HELLP syndrome.
Ask yourself...
- Why is it important to monitor strict intake and output?
- What lab values are critical in the assessment for HELLP syndrome?
- What lab work is specific to confirming hemolysis?
- Are you familiar with prenatal and perinatal physical assessments?
Clinical Presentation and Diagnosis
In addition to hemolysis, elevated serum aminotransferase levels, and thrombocytopenia, along with hypertension and proteinuria, clients with HELLP syndrome commonly complain of chest, epigastric, and RUQ abdominal pain. Other common symptoms include nausea, vomiting, headache, and blurred vision in varying degrees and combinations. In roughly 90% of cases, the primary symptoms are right upper quadrant pain and generalized malaise (1).
HELLP syndrome may have an insidious and atypical onset, with up to 15% of the clients without hypertension or proteinuria (1).
Some pregnant clients may be asymptomatic, but their platelet count abnormality reveals preeclampsia. Malaise is often mistaken for a viral syndrome or fatigue common among pregnant women, so remember to further question reports of fatigue and abnormal malaise in pregnant clients.
Diagnosis of preeclampsia requires a systolic BP of at least 140 mm Hg or a diastolic BP of at least 90 mm Hg on at least two occasions, taken at least four hours apart, plus new-onset proteinuria or a severe new finding.
A single severe feature, in combination with hypertension, is sufficient for the diagnosis. Proteinuria is not essential for diagnosis if a severe feature is present. Severe features of preeclampsia include a systolic blood pressure of at least 160 mm Hg or diastolic blood pressure of at least 110 mm Hg; platelet counts less than 100 × 10^3 per microL; liver transaminase levels two times the upper limit of normal, serum creatinine level two times greater than normal or a level greater than 1.1 mg per dL; additional features include severe right upper quadrant pain, pulmonary edema, or new-onset visual changes (4).
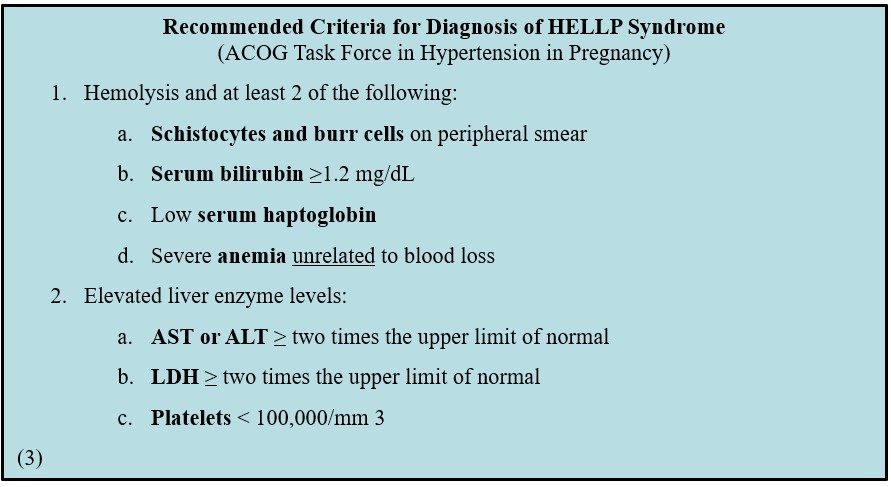
The diagnostic criteria for HELLP syndrome have been developed by the American College of Obstetricians and Gynecologists Task Force in Hypertension in Pregnancy (3).
Most of these individuals seek treatment after week 27 of gestation, but up to 11% may do so earlier. Delayed presentation of HELLP syndrome after delivery occurs in up to 30% of cases.
Ask yourself...
- What organization has developed guidelines for diagnostic criteria in HELLP syndrome?
- What is the relationship between liver function and liver enzyme levels (AST and ALT)?
- Can you describe the process and findings of red blood cell destruction?
- Can you explain the symptoms that commonly accompany hypertension?
- What is the diagnosis of preeclampsia based upon?
Management
The International Society for the Study of Hypertension in Pregnancy (ISSHP) and the American College of Obstetricians and Gynecologists (ACOG) have issued revised guidelines regarding the classification, diagnosis, and management of the hypertensive disorders of pregnancy.
Due to the severity of this complication, women with HELLP syndrome often require immediate treatment, urgent delivery, and transport to a tertiary care facility.
The management of clients with HELLP syndrome requires neonatal and obstetric intensive care units (1).
Anti-inflammatory and immunosuppressive effects of corticosteroids are used to attempt to modify the inflammatory response of preeclampsia with severe features. Many randomized controlled trials of high-dose corticosteroid treatment for antepartum or postpartum stabilization of HELLP syndrome found improved platelet count.
Very close monitoring is required in HELLP syndrome until delivery and in the postpartum period, with laboratory testing at least at 12-hour intervals.
In the natural history of HELLP syndrome, there is an inverse relationship between the trends in platelet values and liver enzyme levels. During the aggravation slope in the disease evolution, platelet count usually decreases at an average rate of approximately 40% per day, whereas liver enzyme values tend to increase.
The drug of choice for the prevention and management of eclampsia is magnesium sulfate (4). This drug reduces the risk of seizures in clients with severe preeclampsia and reduces the rate of eclampsia developing intrapartum and immediately postpartum.
The goal of treatment is to prevent significant cerebrovascular and cardiovascular events in the mother without compromising fetal well-being. If a client is at greater than 34 weeks’ gestation and develops severe preeclampsia, delivery is the treatment of choice. However, mild preeclampsia can be managed without delivery. If the client is 36 weeks’ gestation or further along, the induction of labor should be pursued.
The overall management of preeclampsia includes supportive treatment with:
- Antihypertensives – First-line antihypertensives include hydralazine, labetalol, and nicardipine (4).
- Hydralazine: The recommended dose of hydralazine hydrochloride is 5-10 mg (IV/IM) given every 15 minutes up to 20 mg IV (or 30 mg IM). If pressure does not change after 20 minutes, consider another agent.
- Labetalol: The recommended initial dose of labetalol hydrochloride is 20 mg. A slow injection should be administered this. This drug is often preferred because it has less reflex tachycardia and hypotension (if pushed slowly) or increased intracranial pressure. Caution should be given to clients with a history of previous myocardial disease, congestive heart failure, or asthma (4).
- Nicardipine: The recommended initial rate is 5mg/hour and can be adjusted by 2.5 mg/hour every 5 minutes until the reduction of MAP of 15% is achieved or a maximum dose of 15 mg/hour has been reached (4).
- Anti-epileptics
- Seizures are treated with IV magnesium as a loading dose of 4 g over 5 to 10 minutes, followed by an infusion of 1g/hr maintained for 24 hours after the last seizure.
- Lorazepam and phenytoin can be used as second-line agents but are avoided due to fetal effects.
- Corticosteroids – Used to modulate inflammation and accelerate fetal lung maturity
- Other supportive measures include diuretics (used sparingly) and fluid restriction to avoid pulmonary and cerebral edema.
Clients should be monitored closely with antenatal testing twice a week. If severe features are present, induction is considered as early as 34 weeks, although the benefits must outweigh the risks of preterm delivery. Clients with severe features should be considered to be admitted and/or monitored on bed rest until delivery.
Ask yourself...
- Why is the drug of choice for the prevention and management of eclampsia?
- What are the first-line antihypertensive drugs for the management of preeclampsia?
- How can the appropriate management of preeclampsia impact the overall outcomes of HELLP syndrome?
- Why would corticosteroids be administered if early delivery is anticipated?
- At what point in pregnancy should labor be pursued in a patient who develops preeclampsia?
Complications and Prognosis
Preeclampsia and HELLP syndrome are associated with an elevated risk of cardiovascular disease (hypertension, myocardial infarction, congestive heart failure), cerebrovascular events (stroke), peripheral arterial disease, and cardiovascular mortality in the following years (1). There is a relationship between the severity of preeclampsia or eclampsia and the risk of cardiac disease.
Potential Maternal and Fetal Complications (1, 2, 4):
- Cardiovascular
- Hypoperfusion
- Severe hypertension
- Hypertensive crisis
- Pulmonary edema
- Future cardiac dysfunction
- Renal impairment
- Impaired drug metabolism and excretion
- Hematologic disorders
- Decreased oxygen-carrying capacity
- Thrombocytopenia
- Coagulation defects, including disseminated intravascular coagulation
- Anemia
- Neurologic impairment
- Eclampsia
- Cerebral edema and/or cerebral hemorrhage
- Hepatic impairment
- Hypoglycemia
- Coagulation defects
- Impaired drug metabolism and excretion
- Uteroplacental
- Abruptio placentae
- Decreased uteroplacental perfusion
Fetal Complications (1, 4):
- Impaired intrauterine growth
- Intrauterine fetal demise
- Fetal intolerance to labor
- Preterm birth
- Low birth weight
- Poor fetal lung development
- Decreased oxygenation
Women with HELLP syndrome have a greater risk of pulmonary edema, acute respiratory distress syndrome, and renal failure. Aspartate aminotransferase levels of more than 2,000 IU/L or LDH levels of more than 3,000 IU/L suggest an increased mortality risk.
Case Study: Monique
Monique’s initial blood tests showed:
- Elevated liver enzymes: ALT = 130 U/L, AST = 150 U/L
- Low platelet count: 85,000/µL (thrombocytopenia)
- Peripheral blood smear showed fragmented red blood cells (schistocytes), which is consistent with hemolysis.
Based on these findings, Monique was diagnosed with HELLP syndrome (Hemolysis, Elevated Liver enzymes, Low Platelet count).
Monique was quickly moved to an intensive care unit with higher acuity and was followed by an obstetrics provider with specialized training in obstetric emergencies. She was placed on magnesium sulfate to prevent seizures based on the increased risk of progressing to eclampsia. Labetalol was ordered to manage her high blood pressure. A corticosteroid, betamethasone, was ordered and administered promptly.
Interventions and monitoring include:
- Continuous fetal heart rate monitoring to assess for any signs of fetal distress.
- Ongoing assessment of Monique’s blood pressure, urine output, and oxygen saturation.
- Laboratory tests are repeated every 6 hours to monitor platelet counts, liver function, and renal function.
- Discuss delivery options.
Ask yourself...
- Why were antihypertensives and corticosteroids administered to Monique?
- Why is magnesium sulfate a crucial part of managing clients with HELLP syndrome?
- How would you explain delivery options to Monique to emphasize risks vs benefits?
- Are you familiar with the signs of fetal distress?
Nursing Interventions
Nursing interventions for clients with HELLP syndrome focus on early recognition, stabilization, and prevention of complications to protect both the mother and fetus.
Here are some key interventions:
- Closely monitor vital signs
- Nurses should frequently assess blood pressure, as hypertension is a critical component of HELLP syndrome.
- Collect blood and urine for testing
- Monitor lab work
- Regular assessment of blood tests, including liver enzymes, platelet count, and labs related to hemolysis (such as decreased red blood cells), is crucial.
- Administer ordered medications
- Ensure the client receives the prescribed medications on time and monitor for potential side effects or adverse reactions.
- Monitor the reflexes of clients on magnesium sulfate.
- Fluid management
- Careful management of fluids is crucial to prevent complications like pulmonary edema and to assess kidney function and fluid balance.
- Strict input and output monitoring should be maintained.
- Fetal Monitoring
- The placental function may be compromised, leading to reduced fetal oxygenation or growth restriction. Continuous fetal monitoring is essential to assess fetal well-being.
- Nurses should use continuous electronic fetal monitoring to assess fetal heart rate patterns and identify signs of distress.
- Perform neurologic checks regularly and implement seizure precautions if indicated.
- Prepare for delivery (if indicated)
- In many cases, the definitive treatment for HELLP syndrome is the delivery of the baby.
- Nurses should be prepared to assist in emergencies if the client’s condition deteriorates.
- Client education and support
- Provide education and materials on the physiology of preeclampsia and HELLP syndrome.
- Explain that it is a condition involving high blood pressure during pregnancy, often accompanied by protein in the urine and potential damage to organs like the liver and kidneys. It’s important to explain that preeclampsia can progress to more severe complications if not monitored closely.
- Teach clients that HELLP is a more severe form of preeclampsia, and the condition requires immediate attention and often involves early delivery of the baby.
- Provide education on warning signs and symptoms:
- Explain the importance of regular blood pressure checks at home or in the clinic.
- Emphasize adequate hydration, but discuss fluid restriction if there is any risk of fluid overload.
- Provide education on medications and treatments.
- Emphasize the importance of regular fetal monitoring to ensure the baby’s well-being, especially in cases of preterm labor.
- Explain any procedures or tests that might be required to monitor the baby’s growth and development, such as ultrasounds or non-stress tests.
- Stress the importance of postpartum care, as preeclampsia and HELLP syndrome can still occur or worsen after delivery.
- Encourage clients to seek counseling or join support groups for women with similar experiences.
- Inform these clients that preeclampsia and HELLP syndrome may increase the risk of cardiovascular issues and other complications later in life.
- Postpartum management
- After delivery, clients with HELLP syndrome remain at risk for complications such as bleeding, kidney failure, or seizures.
- Assessment of postpartum bleeding amount, liver and kidney function, and neurologic signs is critical until their condition is stabilized.

Ask yourself...
- Why is fluid management a crucial part of nursing interventions for clients with HELLP syndrome?
- Why is it imperative to provide client education on preeclampsia?
- How can nurses emotionally support clients facing difficult decisions about the induction of labor?
- Why are neurological assessments important following a diagnosis of eclampsia or HELLP syndrome?
Case Study: Monique
Monique’s laboratory results showed a further decline in organ function; the decision was made to induce labor. The provider recognized that the risks of continuing the pregnancy outweighed the benefits of waiting for further fetal development. Despite attempts to induce labor, Monique did not progress, and the fetal heart rate showed further decelerations. The healthcare team and Monique decided to proceed with an emergency Cesarean section.
Monique delivered a healthy but preterm baby boy weighing 5 pounds, 2 ounces, and he was admitted to the neonatal intensive care unit (NICU) for monitoring.
Monique continued to be monitored for postpartum hemorrhage and worsening symptoms of HELLP syndrome. She remained on magnesium sulfate for 24 hours after delivery to prevent seizures. Her platelet count remained low, which was managed with platelet transfusions.
Over the following three days, Monique’s blood pressure stabilized, her liver enzymes began to normalize, and her platelet count gradually increased. Five days postpartum, she was discharged with instructions for blood pressure monitoring and a follow-up appointment with her obstetrician and a maternal-fetal medicine specialist.
Ask yourself...
- Can you discuss the different management pathways for a 37-week-old and a 28-week-old client?
- What education topics would be meaningful to provide to Monique before discharge?
Prevention Strategies
Physical Activity and Exercise
In a healthy pregnancy, there is significant cardiovascular adaptation, including increased blood volume, blood vessel remodeling, arterial compliance, vasodilation, and enhanced endothelial function (9). Regular physical activity can further enhance positive cardiovascular adaptation.
A systematic review of the literature was performed in 2017, which included 17 randomized control trials and 5,075 women, to evaluate the effect of exercise during pregnancy on the risk of gestational hypertensive disorders.
Several studies in the review found that women who performed regular (30 to 60 minutes two to seven times per week) moderate-intensity prenatal exercise (e.g., 140 minutes per week of brisk walking) had significantly lower incidences of gestational hypertensive disorders.
Remember – exercise is currently contraindicated once preeclampsia is diagnosed.
Low-Dose Aspirin Therapy
The ACOG Task Force on Hypertension in Pregnancy initially recommended the use of low-dose aspirin for the prevention of preeclampsia, and the U.S. Preventive Services Task Force expanded this recommendation and included low-dose aspirin (81 mg/day) prophylaxis for women at high risk for preeclampsia. The use of low-dose aspirin during pregnancy is considered safe (9). Poor placental perfusion can lead to ischemia, which results in systemic inflammation and oxidative stress. The therapeutic properties of low-dose aspirin may reduce inflammation, promote normal blood vessel formation and function, and prevent blood clot formation, which promotes normal fetal growth.
Aspirin prophylaxis should be initiated early in gestation, between 12-16 weeks gestation, and should be continued daily until birth (9). Research supports that low-dose aspirin therapy started earlier in pregnancy (<16 weeks) is more effective in reducing fetal growth restriction and preeclampsia. Specifically, ACOG advises that in women with a history of early-onset preeclampsia or preeclampsia in more than one pregnancy, low-dose aspirin should be initiated in the first trimester (9).
Research has shown there is not an increased risk of maternal hemorrhagic complications, such as placental abruption or postpartum hemorrhage, or an increased risk of intracranial hemorrhage in neonates for those taking low-dose aspirin therapy (9).
Dietary Supplementation
Calcium supplementation may effectively reduce the risk of preeclampsia due to its ability to decrease smooth muscle contractility and increase vasodilation (9). For women with low dietary calcium intake, supplementation may decrease the severity of the disease. However, calcium supplementation is not universally recommended to women at risk for preeclampsia in the U.S. Each clinician must examine risk factors, calcium intake, and possible benefits from this supplementation.
Ask yourself...
- Is low-dose aspirin therapy generally considered safe in pregnancy?
- What are complications that can occur with the use of low-dose aspirin therapy?
Research
Significant research is currently being conducted on the relationship between endothelial dysfunction and alterations in the immune response to the development of preeclampsia (9). Vascular endothelial cells impact vascular smooth muscle contractility activity and regulation of blood flow, so the receptors within the endothelial cells respond to vasodilators and vasoconstrictors while producing vasoactive substances such as hormones and cytokines. Endothelial dysfunction and increased capillary permeability can lead to poor organ perfusion.
The underlying functions are not fully understood, but women diagnosed with preeclampsia exhibit histologic evidence of increased circulating markers of endothelial activation (9); so research on this process is meaningful to understanding, preventing, and managing preeclampsia and ultimately HELLP syndrome.
Conclusion
As we conclude this course on HELLP syndrome, learners are now equipped with the critical knowledge and skills to recognize, manage, and intervene in one of the most serious obstetric emergencies. Though rare, HELLP syndrome demands a high level of urgency. Through this course, hopefully, you have gained a deeper understanding of the pathophysiology, the importance of early detection, and evidence-based interventions.
References + Disclaimer
- American College of Obstetricians and Gynecologists. (2020). ACOG Practice Bulletin No. 222: Gestational hypertension and preeclampsia. Obstetrics & Gynecology, 135(6), e237–e260. https://doi.org/10.1097/AOG.0000000000003891
- Beniwal-Patel, P., & Shaker, R. (2019). Gastrointestinal and liver disorders in women’s health : a point of care clinical guide. Springer. https://doi.org/10.1007/978-3-030-25626-5
- Feldman, M., Friedman, L. S. (Lawrence S., & Brandt, L. J. (Eds.). (2021). Sleisenger and Fordtran’s gastrointestinal and liver disease. Pathophysiology/diagnosis/management (11th edition.). Elsevier.
- Magley M, Hinson MR, Haddad LM. Eclampsia (Nursing) [Updated 2024 Oct 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK570548/
- Petca, A., Miron, B. C., Pacu, I., Dumitrașcu, M. C., Mehedințu, C., Șandru, F., Petca, R. C., & Rotar, I. C. (2022). HELLP Syndrome-Holistic Insight into Pathophysiology. Medicina (Kaunas, Lithuania), 58(2), 326. https://doi.org/10.3390/medicina58020326
- Jarvis, C., Eckhardt, A., & Jarvis, C. (2020). Pocket companion for physical examination & health assessment (Eighth edition.). Elsevier.
- Jayawardena, L., & Mcnamara, E. (2020). Diagnosis and management of pregnancies complicated by haemolysis, elevated liver enzymes and low platelets syndrome in the tertiary setting. Internal Medicine Journal, 50(3), 342–349. https://doi.org/10.1111/imj.14337
- Khalid F, Mahendraker N, Tonismae T. HELLP Syndrome. [Updated 2023 Jul 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560615/
- Simpson, K. R., & Creehan, P. A. (2020). Perinatal nursing /. Wolters Kluwer,.
- Singh, A. (2019). Pregnancy-Specific Liver Disorders: Preeclampsia and HELLP Syndrome. In: Beniwal-Patel, P., Shaker, R. (eds) Gastrointestinal and Liver Disorders in Women’s Health . Springer, Cham. https://doi.org/10.1007/978-3-030-25626-5_18
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
