High Flow Oxygen Delivery Systems
Contact Hours: 1
Author(s):
Karson Carter BSN, RN, CPN
Course Highlights
- In this High Flow Oxygen Delivery Systems course, we will learn about the differences between high-flow oxygen delivery systems and low-flow oxygen devices.
- You’ll also learn three indications of use for high-flow oxygen therapy.
- You’ll leave this course with a broader understanding of the nursing role when caring for patients requiring high-flow oxygen therapy.
Introduction
Oxygen therapy is a prescribed treatment that is administered to patients who are hypoxic or in respiratory distress. There are several types of delivery devices for high-flow oxygen therapy. A typical device is the high-flow nasal cannula. High-flow nasal cannula oxygen therapy was implemented for premature neonates in the 2000s. This therapy was created to be used as an alternate type of therapy to continuous positive air pressure (CPAP) that was used to help with apnea (2).
High-flow oxygen therapy is now commonly used in pediatrics and even for adult patients. It can be administered through a high-flow nasal cannula, where the oxygen is humidified and heated, making this therapy more tolerable for the patient (2). High-flow oxygen therapy can deliver 2 liters up to 60 liters per minute (1).
This course will explore when high-flow oxygen is necessary for a patient and the nurse’s role in caring for these patients. It will provide nurses with information to use in everyday practice to better educate their patients and families.
Ask yourself...
- Why was high-flow oxygen therapy created?
- How many liters of oxygen can a high-flow nasal cannula administer per minute?
Definition
As stated earlier in this course, high-flow oxygen via a high-flow nasal cannula can deliver between 2 liters and 60 liters per minute of oxygen. The flow nasal cannula can only give up to 4 to 6 liters of oxygen per minute (1). The low-flow cannula is an open system in which there is a significant amount of leaking oxygen when administered. With this therapy, FiO2 is directly related to the oxygen flow rate (1). The flow rate must be increased if the patient requires a higher percentage of FiO2 (1).
The dryness of the oxygen delivered can irritate the patient’s nares and cause bleeding (1). A standard oxygen delivery device, such as a nasal cannula, is not heated or humidified (1). Oxygen flow is cold and dry, which can lead to increased inflammation and airway resistance (1).
High-flow nasal cannulas can administer up to 100% FiO2, which can be increased independently from the flow rate (5). High-flow oxygen delivery devices are heated and humidified (1). Patients tolerate the high-flow nasal cannula, which keeps them more comfortable.
Ask yourself...
- What is the difference between a low-flow cannula and a high-flow cannula?
- How many liters of oxygen can a low-flow cannula administer?
- Which type of oxygen therapy is the FiO2 related to the liter flow?
High-Flow Oxygen Delivery Devices
A Venturi mask is a high-flow oxygen delivery device that allows the provider to administer a specific FiO2. This device is cone-shaped and must have a good seal over the mouth and nose to reduce the retention of CO2 (6,7). It is not meant to help with breathing work and is usually used for adult patients. This device does not produce gastric distention and can be used with any source of O2 (4).
Continuous positive air pressure devices use a facemask to open the upper airway and increase lung volumes. These devices may decrease the need for intubation for some patients. CPAP can use a mask or a different interface to improve lung volume and open the upper airway. Positive end-expiratory pressure (PEEP) can be titrated in adults aged 5 to 15. For pediatric patients, the PEEP is typically 5-10. This type of therapy can prevent atelectasis (4).
Noninvasive positive pressure ventilation applies greater inspiratory pressure than during the exhalation phase. It is also used with a mask. Bilevel positive airway pressure can decrease the work of breathing and add positive end-expiratory pressure (4).
Ask yourself...
- Which type of delivery device does not help with the patient’s work of breathing?
- Does the cost of the device affect the availability for use?
Components of High-Flow Oxygen Nasal Cannula
Specific components make providing high-flow oxygen possible. An air-oxygen blender must be present to increase the FiO2 from 21% to 100% without changing the flow rate. The device also contains a flow generator that administers flow up to 60 liters per minute. A heated humidifier keeps the gas mixture’s temperature between 31 and 37 °C. The tubing used is also heated, which helps minimize condensation (1).
The nasal prongs used are more comprehensive than those from a low-flow cannula. The heating and humidification of the high-flow cannula are thought to increase compliance by increasing patient comfort. As with any therapy, there can be some disadvantages. A high-flow nasal cannula can be more expensive than a low-flow delivery device. This device also requires specialized training and can be complex to set up. A high-flow nasal cannula is more challenging to transfer a patient on than a standard low-flow nasal cannula (1).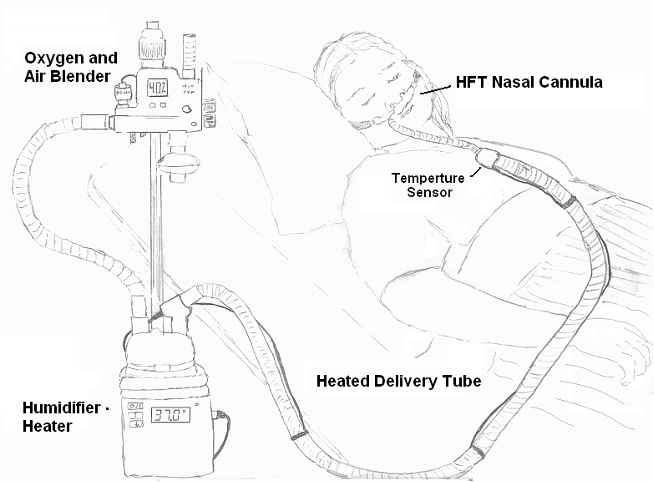
Ask yourself...
- What temperature is the gas mixture kept at for high flow nasal cannula?
- Why is the tubing heated for the high-flow nasal cannula?
- Would this type of oxygen delivery device increase a patient’s compliance?
History and Background
Oxygen therapy is commonly prescribed for patients in respiratory distress or hypoxia. Conventional oxygen therapy, such as a traditional nasal cannula, may not provide the patient with enough support. In this case, noninvasive ventilation may be needed, which can be difficult for patients to tolerate (4).
High-flow nasal cannulas have been on the rise since the early 2000s. In certain instances, patients can eat and speak while on a high-flow nasal cannula, which may not be true with traditional noninvasive ventilation such as CPAP (2).
Indications of Use
High-flow oxygen can help with a patient’s increased work of breathing. Patients experiencing acute respiratory failure can be tachypneic, and the increased flow of oxygen can help them reach their peak inspiratory flows (5). Pediatric patients with acute bronchiolitis and asthma exacerbations can benefit from the use of high-flow nasal cannulas to help decrease their work of breathing (2).
Adult patients with community-acquired pneumonia in respiratory distress would be an indication for the use of a high-flow nasal cannula (5). Because the oxygen is humidified, it allows the secretions to move and either cough or have them suctioned (5).
FiO2 is the fraction of inspired oxygen in a gas mixture (3). These devices can give a more accurate amount of FiO2 than a low-flow device. Certain patients, such as patients with chronic obstructive pulmonary disease, require specific amounts of supplemental oxygen (6).
A high-flow nasal cannula also gives the patient a flow of fresh gas instead of rebreathing excessive amounts of carbon dioxide. Usually, when a patient breathes, it is a mixture of a new gas, 21% FiO2, and gas previously exhaled, which would contain high carbon dioxide and less than 21% oxygen. Because the high flow continuously gives the patient a new mixture of gas. This helps patients with acute respiratory failure not retain increased carbon dioxide. This is called dead space washout (5).
Studies have shown that pre-oxygenating with a high-flow nasal cannula before intubation improves oxygenation during the intubation process as opposed to the nonrebreather mask [1]. This would be appropriate in an alert and awake patient. The high flow and FiO2 would increase the PO2, allowing more intubation time [1]. High-flow nasal cannulas can also be used for post-extubation (1).
Ask yourself...
- What does washout of dead space mean?
- How can high-flow nasal cannulas help with secretion removal?
- What are the indications for high-flow cannula use in pediatric patients?
Case Study #1
A seven-month-old male is brought into the emergency department by the infant’s mother. The mother reports the patient has had a cough and fever for two days. The mom states that the infant appeared to be working hard to breathe when the patient woke up. Upon arrival at the emergency department, the patient was irritable and had a coarse cough. The patient is tachypneic with nasal flaring and moderate subcostal retractions. The patient’s vitals are T 38.4 C, HR 184, RR 75, BP 85/48, and O2 sat 92%. The patient weighs 8kg. The patient tests positive for respiratory syncytial virus (RSV). The provider orders a high-flow nasal cannula for the patient.
Ask yourself...
- Why would this patient benefit from high-flow oxygen therapy?
- What would the nurse need to monitor to assess if the oxygen therapy improves the patient’s respiratory status?
- How would the nurse explain to the patient’s mother why a high-flow nasal cannula is part of the treatment plan for this patient?
Case Study #2
A 70-year-old patient is admitted to a progressive care unit with a diagnosis of community-acquired pneumonia. The patient was initially placed on a 2L nasal cannula. Throughout the day, the patient has increased breathing work and is now on a 4L nasal cannula. The patient’s vitals are T 37.8C, HR 110, RR 28, BP 110/68, O2 sat 88%. The patient has a course cough with thick yellow secretions. The nurse notes that the patient cannot complete sentences due to shortness of breath. The patient cannot transfer to the bedside commode without shortness of breath. The nurse notifies the provider and the respiratory therapist.
Ask yourself...
- What type of increase in respiratory support does this patient require?
- What position should the nurse move this patient to help with the increased work of breathing?
- How would an increase in respiratory support aid in secretion removal?
Nursing Care
A multidisciplinary team is used when caring for all patients. Patients on high-flow oxygen therapy are the same. All oxygen is considered a medication and must be prescribed by a provider.
The bedside nurse caring for that patient must collaborate with the provider and the respiratory therapist to give the patient the highest level of care. The bedside nurse should monitor the patient’s vitals and communicate them to the respiratory therapist and provider to ensure they are on adequate support. The nurse will also assess the patient’s work of breathing while on high-flow oxygen therapy. It is essential to work closely with the respiratory therapist and provider to titrate the flow and FiO2, so the patient is not over-oxygenated or causes barotrauma to the patient (1).
While the respiratory therapist is often in control of the oxygen delivery device, the nurse needs to be familiar with the device. The nurse should complete safety checks to ensure the equipment functions correctly and that all tubing is not kinked or obstructed. The nurse also needs to ensure the patient receives the required FiO2 and flow rate as specified by the provider (6).
The nurse is responsible for positioning the patient to promote chest expansion and improve breathing work. When completing a skin assessment, the nurse should inspect the patient’s skin under the oxygen delivery device for skin breakdown (6).

Ask yourself...
- Whose role is it to manage the high-flow oxygen device?
- How can positioning a patient affect their respiratory effort?
- Does high-flow oxygen need to be prescribed by a provider?
Safety Considerations
As mentioned earlier in this course, the patient should be monitored closely while receiving high-flow oxygen therapy to reduce adverse effects. Patients receiving high-flow oxygen therapy have an increased aspiration risk (1).
Pediatric patients on a flow cannula can commonly only feed by mouth when the flow is at 2 liters per minute due to the risk of aspiration. Over-oxygenation is possible, and with the ability to provide an increased flow, this should be considered when a patient is on high-flow oxygen therapy (1).
While a patient is undergoing oxygen therapy, especially for a considerable amount of time, it is essential to monitor for skin breakdown (6). Security devices should be moved frequently to prevent breakdown, especially with older adults and pediatric patients (7). As discussed earlier, assessing the patient’s bridge of the nose and nares is essential for pressure injury (7).
When using high-flow nasal cannulas with neonates and pediatric patients, specific considerations must be made. The diameter of the prongs should be at most 50% of the diameter of the nares (4). This ensures adequate flow around the cannula to decrease the risk of extra pressure being delivered (4).
The flow is usually titrated by the patient’s weight in neonates and pediatrics [4]. In patients 0-10kg, the flow rate is usually 2L/kg/ minute, with the maximum flow being 8 liters per minute (4,5). The flow rate in patients 10-20kg is usually 1L/kg/ minute [4]. In patients 20-40kg, the flow rate is usually 0.5L/kg/ minute, with a maximum of 30 liters per minute [4]. Patients weighing more than 40kg are the same at 0.5- 1L/kg/ minute flow, with the maximum being 60 liters per minute [4]. These calculations may vary depending on the facility policy.
Patient and Family Education
While caring for patients, patient education is part of the nurse’s role. Nurses should educate their patients and families to understand their disease process better and make informed healthcare decisions. The nurse should explain high-flow oxygen therapy and how it can be used to treat their symptoms or disease process (7). Due to the high liter flow, the patient was informed that there was a risk of nose bleeds and irritation to the nasal passages. While most patients use high-flow oxygen in acute settings, in some instances, patients can be on high-flow oxygen at home (7). Extensive education in at-home use would then be provided to the patient and family.

Ask yourself...
- What are two nursing interventions to prevent skin breakdown?
- Why is there an increased risk for aspiration while on this therapy?
- What are some adverse effects of high-flow oxygen therapy?
Conclusion
High-flow oxygen therapy is a prescribed treatment that delivers oxygen at a high flow rate and FiO2 up to 100%. Different delivery devices can be used to administer this oxygen therapy. This type of oxygen therapy can be used in neonates, pediatric patients, and adults. High-flow nasal cannulas are becoming more present in clinical practice. Research is still being conducted on the effectiveness of this type of oxygen therapy and when to use it. As nurses, it is our role to assess changes in respiratory status, monitor vital signs, and educate patients and their families while caring for patients on high-flow oxygen therapy. As new therapy develops, educating ourselves to provide better care for our patients is essential.
References + Disclaimer
- Sharma, S., Danckers, M., Sanghavi, D., and Chakraborty, R. (2023). High-Flow Nasal Cannula. In: StatPearls. StatPearls [Internet]. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK526071/
- Nolasco, S., Manti, S., Leonardi, S., Vancheri, C., and Spicuzza L. (2022). High-Flow Nasal Cannula Oxygen Therapy: Physiological Mechanisms and Clinical Applications in Children. Frontiers in medicine, 9, 920549. Retrieved from doi: 10.3389/fmed.2022.920549
- Fuentes, S., and Chowdhury, Y. (Updated 2022 Nov 29) Fraction of Inspired Oxygen in StatPearls. Stat Pearls [Internet] Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560867/
- Lipnick, M., Sendagire, C., Kallet, R., Branson, R., and Silvers, S. Overview of Oxygen delivery devices. (2023). OpenCriticalCare. Org. Retrieved on July 16, 2024, from https://opencriticalcare.org/encyclopedia/overview-of-oxygen-delivery-devices/
- Lodesert, F., LettichT., and Rezaie, S. (2018). High-flow Nasal Cannula: Mechanism of Action and Adult and Pediatric Indications. Cureus, 10 (11), e3639. Retrieved from doi: 10.7759/curious.363
- Ernstmeyer, K., and Christman, E. (2021). Chapter 11 Oxygen Therapy. Open Resources for Nursing (Open RN). Nursing Skills [Internet]. Eau Claire (WI): Chippewa Valley Technical College. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK593208/
- Elsevier. (2024) Oxygen Therapy: Nasal Cannula or oxygen Mask- CE/ NCPD. Retrieved from https://elsevier.health/en-US/preview/oxygen-therapy-nasal-cannula-or-oxygen-mask
- [Image]. By Strangecow at English Wikipedia. Artist: Strangecow. Offered for free use into the public domain., CC0, https://commons.wikimedia.org/w/index.php?curid=89284158
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
