Florida HIV/AIDS
Contact Hours: 1
Author(s):
Morgan Curry BSN, RN
Course Highlights
- In this course, you will cover Florida’s HIV/AIDS requirements and the importance of infection reporting.
- You’ll also learn the basics of Florida HIV/AIDS treatment, as required by the Florida Board of Nursing.
- You’ll leave this course with a broader understanding of reducing HIV transmission and infection control.
Introduction
An estimated 1.2 million Americans are living with human immunodeficiency virus (HIV). As many as 1 in 8 do not even know they are infected (7). The others utilize the healthcare system in various ways, from testing and treatment regimens to hospitalizations for symptoms and opportunistic infections.
Healthcare professionals in nearly every setting have the potential to encounter patients with HIV, as the disease can affect patients of any age or stage of life. A proper understanding of HIV is essential to provide high-quality and holistic care to these patients. For nurses practicing in the state of Florida, it is also essential to understand the laws, statutes, and regulations regarding testing, treatment, reporting, and confidentiality related to HIV and AIDS within the state.
Statistics
Infection rates are unequal across demographic groups, and certain factors may increase a person’s risk. Patient information to consider when determining someone’s risk includes:
Age
As of 2021, the age group with the highest incidence of new HIV diagnoses is 13-34 years, approximately 58% of new infections (7). Cases have been down 18% in this age group since 2017.
Race/Ethnicity
African Americans had the highest number of new HIV cases in 2021, at approximately 40% (7). Hispanics/Latinos follow this at 29%, and whites at 26%.
Gender
Males are disproportionately affected by HIV, accounting for 81% of new cases in 2021 (7). Females accounted for 24% of new cases. This data refers to the sex of someone at birth. When looking at the transgender population, those who have transitioned male-to-female were 2% of new cases, and female-to-male, less than 1% (7).
Sexual Orientation
Men who have sex with men (MSM) remain the population most at risk of HIV, accounting for around 70% of all new infections in 2021 (7). Cases have been down 13.5% in this group since 2017.
Location
Different areas of the country are affected at different rates due to various factors, including population density, racial distribution, and access to healthcare. The southern states are unmistakably more affected than other regions and accounted for 52% of new cases in 2021 (7). Western states account for 21%, the Midwest for 14%, and the Northeast for 14% (7).

Ask yourself...
- Are you surprised by any of these statistics?
- How are the statistics different from what you see in your area of practice?
Transmission
Perhaps the most elusive part of this virus for many years was how it spreads. We now know that HIV is spread only through certain bodily fluids. An accurate understanding of HIV transmission is vital for healthcare professionals to provide proper education to their patients, reduce misconceptions and stigmas, and prevent transmission and protect themselves and other patients (8).
Bodily Fluids
Bodily fluids that can transmit the virus include (9):
- Blood
- Semen and pre-seminal fluid
- Rectal fluid
- Vaginal fluid
- Breastmilk
- Fluids that may contain blood, such as amniotic fluid, pleural fluid, pericardial fluid, and cerebrospinal fluid
Suppose one of these fluids comes into contact with a mucous membrane such as the mouth, vagina, rectum, etc., or damaged tissue such as open wounds, or is directly injected into the bloodstream. In that case, transmission of HIV is possible (8).
Ways of Transmission
Scenarios where transmission is possible include:
- Vaginal or anal sex with someone who has HIV (condoms and appropriate treatment with antivirals reduce this risk)
- Sharing needles or syringes with someone who has HIV
- Mother-to-child transmission during pregnancy, delivery, or breastfeeding (appropriate treatment during pregnancy, c-section delivery, and alternative feeding methods reduce this risk)
- Receiving a transfusion of infected blood or blood products (this is very rare now because of screening processes for blood donations)
- Oral sex with someone who has HIV (though this is very rare)
- A healthcare worker receiving a sharps injury with a dirty needle (risk of transmission is very low in this scenario)
HIV cannot be transmitted via:
- Saliva
- Sputum
- Feces
- Urine
- Vomit
- Sweat
- Mucous
- Kissing
- Sharing food or drink
- Ticks or mosquitoes
Ask yourself...
- What are the routes of transmission?
- How can HIV NOT be transmitted?
Reducing Transmission & Infection Control
Patient education about risk and protection against HIV, testing, and what to do if exposed should be standard practice for healthcare professionals in nearly all healthcare settings. Ideally, primary care should include risk screenings and routine patient education to help prevent infections from occurring (or prevent worsening of infections that have already occurred) (8).
Prevention Strategies
Strategies to help prevent the spread of HIV include (8):
- Identifying those most at risk, particularly MSM, minorities, and those who use drugs by injection
- Ensure patients are aware of and have access to protective measures such as condoms and clean needle exchange programs
- Provide routine screening blood work for anyone with risk factors or desiring testing
- Providing access to PrEP medications where indicated (discussed further below)
- Staying up to date on current recommendations by the U.S. Centers for Disease Control and Prevention (CDC) and HIV developments
- Maintaining a nonjudgmental demeanor when discussing HIV with patients, to welcome open discussion
Pre-Exposure Prophylaxis
For patients with a repeated or frequent high risk of HIV exposure, such as those with an HIV+ partner or those routinely using needles for drugs, pre-exposure prophylaxis (PrEP) may be a good choice to reduce the risk of contracting the virus. When used correctly, PrEP is 99% effective at preventing infection from high-risk sexual activity and 74% effective at preventing infection from injectable drug use (10).
Depending on the type of exposure risk (anal sex, vaginal sex, needle sharing, etc.), PrEP needs to be taken anywhere from 7-21 days before it reaches its maximum effectiveness (10). Most insurances, including Medicaid programs, cover PrEP at least in part (10). Federal and state assistance programs are available to make PrEP available to as many people who need it as possible. Some side effects are commonly reported, primarily gastrointestinal symptoms, headaches, and fatigue (10).
Viral Load
For those who have a confirmed diagnosis of HIV/AIDS, the focus should be on promoting interventions that will prevent further transmission. One of the biggest determinants for transmission is the infected person’s viral load. Individuals being treated for HIV can have their viral load measured to ensure viral replication is being controlled as intended. A viral load lower than 200 copies of HIV per milliliter of blood is considered undetectable, meaning the virus is not transmissible to others (4). Even for those not receiving treatment, there are methods to reduce transmission (11).
Infection Control Methods
Methods of infection control for healthcare professionals include (3):
- Universal precautions when handling any bodily fluids
- Eyewear is at risk of fluid splashing
- Careful and proper handling of sharps
- Facilities have a standard plan in place for potential exposures
If an exposure or needlestick does occur, the patient would ideally submit to testing for HIV to determine if the staff member is at risk. If the HIV status of the patient is unknown or confirmed to be positive, post-exposure prophylaxis (PEP) may be advised to start within 72 hours of exposure (12).
Ask yourself...
- What are some strategies to reduce Florida HIV/AIDS transmission?
- Have you or any of your coworkers ever had a needlestick occur?
- How did you handle that situation?
- What is viral load, and how does it impact the diagnosis of AIDS?
- What comprises pre-exposure prophylaxis?
- What are your facilities’ requirements for standard precautions with patients?
- What exposures have you seen in your practice?
Florida HIV/AIDS Treatment
When HIV is appropriately treated, progression from HIV to AIDS can be significantly reduced, and quality and longevity of life maximized. In 2018, the CDC estimated that around 65% of all US citizens living with HIV were virally suppressed, and 85% of those receiving regular HIV-related care were considered virally suppressed at their last test (5). However, as mentioned earlier, an estimated 13% of all HIV cases do not know they are infected. Appropriate medical care and keeping viral loads undetectable are one of the single most effective methods of preventing transmission (4, 5).
For those receiving treatment, a multifaceted and individualized approach can reduce a person’s viral load, reduce the risk of transmission, reduce the likelihood of developing AIDS, and preserve the immune system. Regardless of how early someone receives treatment, there is no cure for HIV, and an infected person will be infected for life. All individuals diagnosed with HIV (even asymptomatic people, infants, and children) should receive antiretroviral therapy (ART) as quickly as possible after a diagnosis of HIV is made. The classes and available medications for ART include the following (1). There are many other combination formula HIV medications, for example, emtricitabine/tenofovir (brand name, Truvada), although not listed here.
Nucleoside Reverse Transcriptase Inhibitors (NRTIs)
Nucleoside reverse transcriptase inhibitors (NRTIs) inhibit the transcription of viral RNA to DNA , blocking reverse transcriptase (an enzyme needed for HIV replication).
- Abacavir
- Emtricitabine
- Lamivudine
- Tenofovir disoproxil fumerate
- Zidovudine
Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs)
Non-nucleoside reverse transcriptase inhibitors (NNRTIs) inhibit the transcription of viral RNA to DNA by binding to and altering reverse transcriptase. As mentioned above, transcriptase is an enzyme HIV needs to make copies of itself.
- Doravirine
- Efavirenz
- Etravirine
- Nevirapine
- Rilpivirine
Protease Inhibitors
Protease inhibitors block HIV protease (another enzyme needed for HIV replication).
- Atazanavir
- Darunavir
- Fosamprenavir
- Ritonavir
- Saquinavir
- Tipranavir
Fusion Inhibitors
Fusion inhibitors prevent the virus from entering the immune system’s CD4-T lymphocyte cells (CD4 cells).
- Enfuvirtide
Integrase Strand Transfer Inhibitors (INSTIs)
Integrase strand transfer inhibitors (INSTIs) block HIV integrase (an enzyme needed for HIV replication).
- Cabotegrevir
- Dolutegravir
- Raltegravir
Attachment Inhibitors
Attachment inhibitors prevent HIV from entering CD4 cells by binding to the gp120 protein on the virus’s surface.
- Fostemsavir
Post Attachment Inhibitors
Post attachment inhibitors prevent the virus from binding to and entering CD4 cells by blocking the CD4 receptors on the surface of some immune cells. HIV needs these receptors to enter the cells.
- Ibalizumab-quick
Capsid Inhibitors
Capsid inhibitors interfere with the HIV capsid (a protein shell that protects the enzymes HIV needs for replication).
- Lenacapavir
Pharmacokinetic Enhancers
Pharmacokinetic enhancers increase the effectiveness of HIV medications.
- Cobicistat

Ask yourself...
- How do fusion inhibitors work against HIV?
- How do entry inhibitors work against HIV?
- How soon after diagnosis should patients receive antiretroviral therapy?
- Make a mental list of treatments available for patients of Florida HIV/AIDS.
- What are examples of NRTIs?
- Which of these medications have you administered?
- What education do you provide to patients taking these medications?
Florida HIV/AIDS Laws
The Omnibus AIDS Act is based on the premise that public knowledge can best control illness. If the public is aware of potential illness, and ways to avoid contracting and transmitting illness, that is the best prevention method and further spread (2). The state of Florida became one of the first states with high rates of HIV infection within its population to enact legislation surrounding the AIDS epidemic. Transmission of HIV, as aforementioned, occurs through direct contact with virus-containing body fluids. Activities by which transmission involves, such as sexual activity, needle stick, blood transfusion, or mother-to-baby, the government cannot regulate. Therefore, the governmental response to a disease epidemic must rely primarily upon the education of the public and its cooperation with the government’s educational efforts and recommendations (2).
Informed Consent
The following are regulations surrounding informed consent and HIV testing in Florida (2).
Information Requirements
Healthcare providers performing HIV tests must have advanced procedures regarding patient consent, testing samples, and informing patients of their results (2). “Since the 1998 amendments to the Act, health care providers must, as a matter of law, convey three pieces of information, all essentially involving the choice of a testing site, as part of the process of obtaining informed consent:
- Disclose that the provider must report the test subject’s name to the local county health department if the HIV test results are positive.
- Alert the patient that, as an alternative, the patient may secure the HIV test at a site that tests anonymously, the locations of which the provider must make available; and
- Relate the extent of the confidentiality rights that adhere to the test results in the provider’s patient records.”
Minors
“The general rule that parental consent is required before medical diagnosis or treatment of a minor does not apply when sexually transmitted diseases such as HIV infection are involved. Indeed, Florida specifically forbids telling parents the fact of the minor’s consultation, examination, or treatment for a sexually transmissible disease, such as HIV infection, either directly or indirectly (such as by billing a parent or their insurer for an HIV test without the child’s permission).”
“Infants and young children are treated as unable to make an informed decision, and consent of their parents or legal guardians is required. For older children (such as teenagers), however, the provider must make an individual judgment whether the child, as phrased in Department of Health rules, ‘demonstrates sufficient knowledge and maturity to make an informed judgment,’ meaning, whether the child has the cognitive and emotional capacity to understand the risks and benefits of the test or treatment to which the child is being asked to consent.”
Documentation
“As with other medical procedures requiring informed consent, informed consent for HIV testing does not necessarily mean written consent. Except for donations of blood and other tissues and to obtain health or life insurance, Florida does not require providers to have the test subject sign a document authorizing the test. The health care provider must only enter a note in the medical record explaining the test and obtaining consent.”
Exceptions
Exceptions to informed consent requirements by health care providers (2):
Pregnancy
“Following federal legislation and recommendations from CDC, Florida law in 1996 first imposed “mandatory offering” of HIV tests for all pregnancies upon presentation. In 2005, the statute was further amended to establish the present system of “opt out” testing, in which pregnant women are advised that the health care provider attending them will conduct an HIV test but that they have the right to refuse. The pregnant woman’s objection is required in writing, which must be placed in her medical record” (§384.31, F.S.)
Emergencies
“A provider may test without consent in “bona fide medical emergencies,” but only if the provider documents in the medical record that the test results are medically necessary to provide appropriate emergency care or treatment to the test subject and the test subject is unable to consent” (§381.004(2)(h)3, F.S.).
Therapeutic Privilege
“The Act allows a “therapeutic privilege” that bypasses informed consent requirements when the provider’s medical record documents that obtaining informed consent would be detrimental to the health of a patient suffering from an acute illness and that the test results are necessary for medical diagnostic purposes to provide appropriate care or treatment to the patient. This same privilege applies to all medical procedures requiring informed consent. The statute emphasizes that this provision provides no basis for routinely testing patients for HIV without their informed consent” (§381.004(2)(h)4, F.S.).
Sexually Transmissible Diseases
“State laws permit HIV testing for sexually transmissible diseases on certain subjects, such as convicted prostitutes (§796.08, F.S.), inmates before release (§945.355, F.S.), and cadavers over which a medical examiner has asserted authority §381.004(2)(h)1.c., without the consent of the test subject. This exception includes exempting pregnancy “opt out” testing from informed consent requirements discussed above.”
Criminal Acts
“Victims of criminal offenses that involve transmission of body fluids may require the person charged with or convicted of the offenses to be tested for HIV infection by requesting a court to order the test” (§960.003(2), F.S.). “Similarly, when a defendant, prosecuted for certain offenses in which transmission might have occurred, has been ordered to or has voluntarily given a blood sample, the victim may request the sample be tested for evidence of HIV without the consent of the defendant” (§381.004(2)(h)6, F.S.).
Organ and Tissue Donations
“Various statutory provisions permit testing without informed consent in specifically identified specialty areas: certain blood and tissue donations; corneal removals and eye enucleation that Florida allows by law to be done without consent; autopsies to which consent to perform the autopsy was obtained” (§§381.004(2)(h)2, 5 and 9, F.S.).
Research
“Established epidemiologic research methods that ensure test subject anonymity are expected from informed consent” (§381.004(3)(h)8, FS)
Abandoned Infants
“When a licensed physician determines that it is medically indicated that a hospitalized infant have an HIV test, but the infant’s parent(s) or legal guardian cannot be located after reasonable attempts, the test may be performed without consent. The reason why consent could not be obtained must be documented in the medical record, and the test result must be provided to the parent(s) or guardian once they are located” (§381.004(2)(h)13, F.S.).
Significant Exposure
“The blood of the source of significant exposure to medical personnel or to others who render emergency medical assistance may be tested without informed consent” (§381.004(3)(h)10-12, FS).
Repeat HIV Testing
“Renewed consents are not required for repeat HIV testing either to monitor the clinical progress of a previously diagnosed HIV-positive patient or for conversion from a significant exposure” (§§381.004(2)(h)14 and 15, F.S.).
Judicial Authority
“A court may order an HIV test to be performed without the individual’s consent” (§381.004(3)(h)7, FS).
Ask yourself...
- What groups of individuals are exceptions to informed consent requirements when it comes to Florida HIV/AIDS?
- What are the information requirements?
Florida HIV/AIDS Confidentiality
The following are regulations surrounding the confidentiality of HIV testing in the state of Florida (2).
Not every piece of medical information about a person who has been tested for HIV or assessed for AIDS is protected. “Only the fact that an HIV test was performed on an identifiable individual and any ‘HIV test result’ (negative as well as positive) are specially protected” (§381.004(2)(e), F.S.).
The statute definitions (11):
- HIV test: “test ordered after July 6, 1988, to determine the presence of the antibody or antigen to human immunodeficiency virus or the presence of human immunodeficiency virus infection” (§§381.004(1)(b), F.S.)
- HIV test result: “laboratory report of a human immunodeficiency virus test result entered into a medical record on or after July 6, 1988, or any report or notation in a medical record of a laboratory report of a human immunodeficiency virus test” (§§381.004(1)(c), F.S.)
“Only a laboratory report of an HIV test result entered in a medical record on or after July 6, 1988 (the effective date of the Omnibus AIDS Act), or any report or notation in a medical record of a laboratory report of an HIV test, falls within their scope.”
“Explicitly excluded from the definition of an HIV test result are reports from patients of their HIV status to health care providers. Consequently, patient reports of their HIV test status from Department of Health anonymous testing sites, from home access HIV test kits, or from any other sources do not constitute ‘HIV test results’ unless separately confirmed by the provider through a laboratory report or a medical record containing a laboratory report. Patient disclosures of an HIV test or infection to persons other than health care providers caring for the patient under the provisions of the Act also do not fall within the statute’s special confidentiality protections.”
Voluntary Partner Notification
The following are regulations surrounding voluntary partner notification of HIV exposure in the state of Florida (2).
“The person ordering the HIV test (or that person’s designee), although under no liability exposure to the sexual or needle-sharing partners of their HIV-positive patients, is required to advise their patients with HIV-positive test results of the importance of notifying partners who may have been exposed” (§381.004(2)(c), F.S.). Practitioners are also advised to inform patients of the availability of voluntary partner notification services provided by the Department of Health. Under the authority provided in §384.26, F.S., county health department staff offer voluntary and confidential partner notification and referral services to HIV-prone persons. When notifying partners, county health department staff are required not to reveal the identity of the original client.”
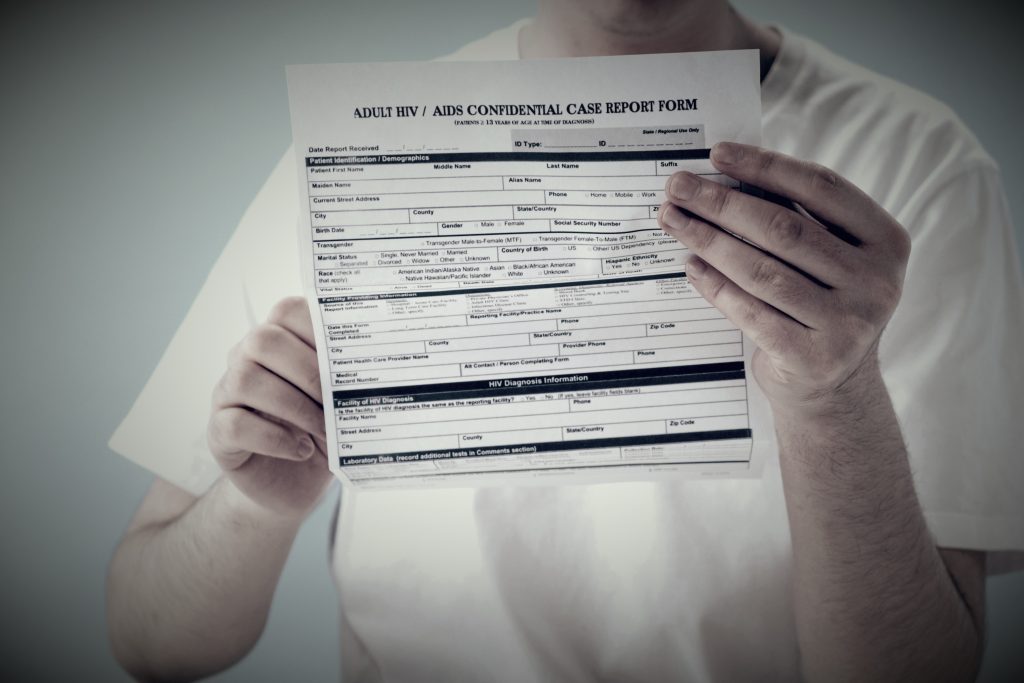
Florida HIV/AIDS Infection Reporting
The following are regulations surrounding HIV infection reporting in Florida (2).
“In 1996, Florida became one of the first states with a high incidence of AIDS to authorize regulatory procedures requiring physicians and laboratories to report to local health authorities HIV-positive test results with patient identifiers” (§384.25, F.S.). “Practitioners and clinical laboratories that fail to report HIV-positive test results are subject to a $500 fine and disciplinary action by their licensing boards” (§384.25(4), F.S.).
“This change was spurred in part by the Ryan White CARE Act. Enacted in 1990 and reauthorized in 2009 as the Ryan White HIV/AIDS Treatment Extension Act, this federal legislation now provides funding to urban areas, states, and localities to improve the availability of care for low-income, uninsured, and under-insured AIDS and HIV-infected patients and their families.”
“Florida’s HIV infection-reporting requirements increase available Ryan White funding for persons with the illness and enable the Department of Health to link them to medical and support services earlier in the process of infection.” Under the rules of the Department of Health of Florida:
- “Practitioners must report to their local county health department within two weeks of the HIV-positive diagnosis of all persons, EXCEPT infants born to HIV-positive women, which must be reported the next business day” (Rule 64D-3.029, FAC and Rule 64D-3.030(5), FAC).
- “Clinical laboratories must report to the local health department HIV test results from blood specimens within three days of diagnosis” (Rule 64D-3.029, FAC).
References + Disclaimer
- U.S. Department of Health and Human Services. (2023, March). FDA-approved HIV medicines. https://hivinfo.nih.gov/understanding-hiv/fact-sheets/fda-approved-hiv-medicines
- Hartog, J., & Robinson, G. (2013, August). Florida’s Omnibus Act: A brief legal guide for healthcare professionals. http://www.floridahealth.gov/diseases-and-conditions/aids/administration/_documents/Omnibus-booklet-update-2013.pdf
- National Center for HIV, Viral Hepatitis, STD, and TB Prevention. (2019, September). HIV and occupational exposure. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/workplace/healthcareworkers.html
- National Center for HIV, Viral Hepatitis, STD, and TB Prevention. (2023, January). Protecting others. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/livingwithhiv/protecting-others.html
- Centers for Disease Control. (2020). Evidence of HIV treatment and viral suppression in preventing the sexual transmission of HIV. https://www.cdc.gov/hiv/risk/art/evidence-of-hiv-treatment.html
- Centers for Disease Control. (2020). HIV. https://www.cdc.gov/hiv/basics/whatishiv.html
- U.S. Department of Health and Human Services. (2023, December). US statistics. https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
- Wilkins, T. (2020) HIV 1: Epidemiology, pathophysiology and transmission. Nursing Times [online], 116(7), 39-41. https://www.nursingtimes.net/clinical-archive/immunology/hiv-1-epidemiology-pathophysiology-and-transmission-15-06-2020/
- U.S. Department of Health and Human Services. (2022, June). How is HIV transmitted? https://www.hiv.gov/hiv-basics/overview/about-hiv-and-aids/how-is-hiv-transmitted/
- National Center for HIV, Viral Hepatitis, STD, and TB Prevention. (2022, June). PrEP (pre-exposure prophylaxis). Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/prep.html
- The Florida Senate. (2023). 2021 Florida statutes (including 2021B session): Chapter 381 Public Health, General Provisions, Section 004 HIV testing. https://www.flsenate.gov/Laws/Statutes/2021/381.004
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
