Course
Inpatient Management of Psychosis
Course Highlights
- In this Inpatient Management of Psychosis course, we will learn about psychosis.
- You’ll also learn positive and negative symptoms of psychosis.
- You’ll leave this course with a broader understanding of necessary elements of a thorough assessment for psychosis.
About
Contact Hours Awarded: 2
Course By:
Michael York, MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Psychosis is an illness or symptom of illnesses that is often misunderstood. This amalgamation of symptoms will most likely result in the patient’s loss of touch with reality. Care must be taken to properly diagnose and treat both the psychosis and the underlying issue(s) which caused it. The patient may be scared of what others will be thinking as there is a stigma associated with psychosis. The treatment plan must be individualized for the patient, taking into account any other medical problems they may have.
Definition
Psychosis is the result of multiple psychological symptoms that leaves the patient out of touch with reality. These symptoms or mental disorders include hallucinations, delusions, and disorganized thinking and behaviors. Psychosis is particularly common in patients with neurocognitive disorders (NCD) such as dementia, Alzheimer’s disease and Parkinson’s disease (1, 4).
Epidemiology
First-time psychosis has an incidence of approximately 50 in 100000 people. For males, the peak age of onset is from their teenage years to the mid-twenties. Whereas for females, the peak age of onset is from their teenage years to the late twenties. It is rare for children to present with psychosis. It is known that the earlier the onset of psychosis, the poorer the outcome. It should also be noted that the earlier the treatment is initiated, the better the outcome will be (1).
It is more common for males to develop psychosis. Studies have shown that the prevalence of psychosis is fairly stable globally. There are some new studies that are questioning whether this remains true; they are focusing on ethnicity, sex, age, and geographical location when it comes to incidence of psychosis. Still other studies are showing that the incidence of psychosis/schizophrenia is on the rise around the world (8).


Self-Quiz
Ask Yourself...
- What is the definition of psychosis?
- What are two symptoms of psychosis?
- Which population is more prone to experience psychosis?
- When should treatment be started to increase the probability of a better outcome?
- What are newer studies of psychosis focusing on?
Pathophysiology
The neurotransmitter dopamine is most strongly linked to the onset of psychosis. The Dopamine Hypothesis came from the discovery that drugs that increase dopamine activity in the brain can lead to psychosis. On the other hand, drugs that impede dopamine receptors lessen the symptoms of psychosis. The Dopamine Hypothesis states that, in a person without psychosis, when the limbic dopamine system is suppressed, the prefrontal dopamine system takes control. In a person with psychosis, there is a reduction in the dopaminergic neurons in the prefrontal dopamine system, resulting in an overactive limbic dopamine system. When the activity in the prefrontal dopamine system is lessened, this can bring on the negative symptoms of psychosis. When the limbic dopamine system becomes overactive, it can lead to the positive symptoms of psychosis.
Another neurotransmitter, glutamate, has also been shown to contribute to psychosis. Sensory, cognitive, motor, and affective symptoms of psychosis are linked to abnormal glutamate transmission in the brain (5, 8).

Self-Quiz
Ask Yourself...
- What can an increase of dopamine in the brain lead to?
- What does the Dopamine Hypothesis state?
- What leads to the negative symptoms of psychosis?
- What leads to the positive symptoms of psychosis?
- Name two neurotransmitters involved with psychosis.
- Name two symptoms of psychosis linked to glutamate.
Stages
The clinical staging of psychosis was developed to assist providers in diagnosing and treating with greater precision. There are three stages of psychosis: (1) prodrome phase, (2) acute phase, and (3) recovery phase.
Prodrome Phase
The prodromal stage is the first stage of psychosis. This is where behaviors and perceptions may change, indicating that a psychotic event is about to start. As psychosis begins, the patient may show symptoms such as sleep disturbances, difficulty focusing, or feelings of wanting to be alone.
Acute Phase
In the acute phase of psychosis, behaviors such as hallucinations and delusions begin. As these behaviors progress, they can become debilitating and interfere with the patient’s normal life. The length of the acute phase is undetermined and may depend on the cause of the psychosis.
Recovery Phase
The recovery phase is the last stage of psychosis. In this phase, the symptoms of psychosis will decrease, and the patient should be able to return to their normal life routines. This stage is brought on after treatment has started or if the patient stops the substance that may have brought on the psychosis (7).

Self-Quiz
Ask Yourself...
- Name the three stages of psychosis.
- Which is the first stage of psychosis?
- Name a symptom that may be present in the first stage of psychosis.
- Name a symptom that may debilitate a patient in the second stage of psychosis.
- What will determine the length of the second stage of psychosis?
- Name the third stage of psychosis.
- What causes the third stage of psychosis to begin?
Clinical Signs and Symptoms
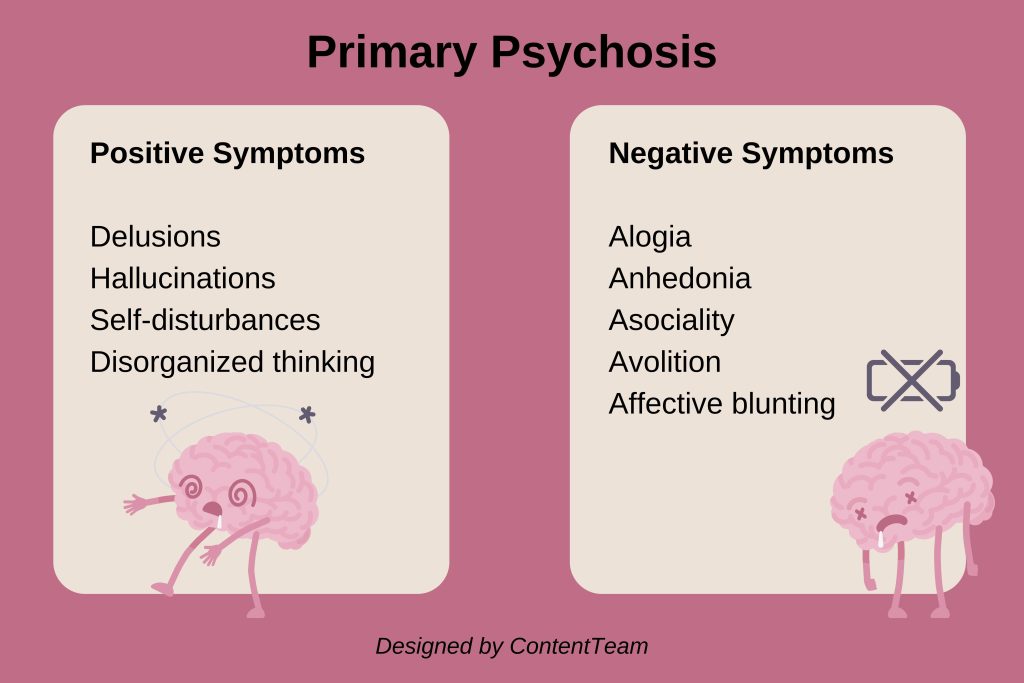
Through every stage of psychosis, patients can present with symptoms. There are two classifications or dimensions of symptoms of primary psychosis: positive and negative.
Positive Dimension of Psychosis
The positive dimension of psychosis has been evolving for decades and is known as the core of primary psychosis. Symptoms include delusions, hallucinations, self-disturbances, and disorganized thinking.
- Delusions: Delusions are continuous false beliefs which are based on flawed reasoning about reality. These beliefs are sustained even though there is evidence they are incorrect and other people do not share them. There are different types of delusions which can manifest. Persecutory delusions are when the patient believes that something/someone is out to get them; these are the most common type of delusions.
Another type of delusion is when the patient has false beliefs about their or another person’s body. This type of delusion is called somatic. When the patient feels that a catastrophe is going to happen, they are experiencing a nihilistic delusion. An erotomanic delusion is when the patient believes that someone is in love with them. A grandiose delusion has the patient believing that they are more important than they really are.
- Hallucinations: Hallucinations are perceived experiences that are untrue though they have the clarity and impact of true perceptions. These experiences happen without the stimulation of the organ needed for the real experience. When speaking about hallucinations, the default thought is auditory. It should be noted that hallucinations can also affect the visual, olfactory, and tactile senses.
- Self-disturbances: These are changes in the sense of self through the patient’s experiences and actions.
- Disorganized thinking: The patient’s speech pattern and overall communication pattern is what gives away disorganized thought. During a psychotic episode, the patient may have sequences of unrelated or very loosely associated ideas. They may be unable to properly answer questions or give long answers with excessive details. The patient may drift from the original topic of conversation, never returning to the initial point. At times, the patient may use a string of incoherent jumble of words. They may also repeat words, phrases, or other statements.
Negative Dimension of Psychosis
Negative symptoms of psychosis have been consistently linked with poor outcomes. As per the National Institute of Mental Health (NIMH), the negative symptoms of psychosis include the domains of alogia, anhedonia, asociality, avolition, and affective blunting. These domains are commonly known as the 5 A’s.
- Alogia: Alogia is when the patient speaks less often than normal and uses less words when they do speak. They also tend to take a long time to talk and are unlikely to initiate conversation. When asking questions, the patient will reply with short responses saying only what is necessary to answer the question.
- Anhedonia: Anhedonia can be thought of as both consummatory and anticipatory. The patient with anhedonia does not feel pleasure when performing acts that should feel pleasurable. They may also not feel the associated pleasure in the anticipation of performing pleasurable acts.
- Asociality: This is a decrease in normal social interactions and in the drive to initiate them. This is due to a disinterest and lack of any desire to interact.
- Avolition: Apathy is another name for avolition. This refers to a lack of involvement in any type of activity. Avolition is due to both a disinterest in activities and a loss in the motivation to perform them.
- Affective blunting: Affective blunting is usually referred to as blunted affect. It is both a decrease in the patient’s expression of emotions and reaction to circumstances (4, 6).

Self-Quiz
Ask Yourself...
- Name two positive symptoms of psychosis.
- What is a delusion?
- Describe disorganized thinking.
- Name three negative symptoms of psychosis.
- Describe anhedonia.
Assessment
As with most disease processes, the first line of treatment is a thorough assessment. The patient interview is perhaps the most important tool in developing an individualized plan of care. The clinician should start by obtaining an accurate history (it should be noted that a patient having a psychotic episode may not be the best historian). The history needs to include certain items:
- Timeline and severity of symptoms. An accurate timeline is important to assess the onset of psychosis. The type and severity of symptoms will also give the provider insight to help formulate the plan of care.
- Previous psychiatric history. Assessing any prior psychiatric history will guide the plan of care. It may also facilitate the diagnosis process.
- Previous medical history. There are medical conditions that are linked to psychosis. Obtaining a proper medical history will give valuable insights and guide the plan of care.
- Medications. An accurate medication reconciliation is important. There are medications that can contribute to psychotic episodes. It is also important to rule out any medication interactions that may present with the treatment of psychosis.
- Substance use. The use of drugs and alcohol can contribute to the onset of psychosis.
- Trauma. Trauma of all types (social, physical, sexual, emotional) can be a major cause of psychosis. Knowledge of the trauma will also guide the plan of care.
- Mental Status Exam. When suspecting any type of psychiatric disorder, the Mental Status Exam (MSE) should be performed. The MSE has the provider take into account the appearance, mood, behavior, speech, and affect of the patient. It should be used with every encounter with the patient. This will help the provider paint a picture of any changes in the mental status of the patient. Looking back, the provider can compare prior assessments and map the course of the psychosis.
A regular work-up should be performed, including a urinary drug screen. This will help rule out any non-psychiatric causes of the psychotic episode. One thing to take note of is that not all substances can be found in routine labs. Once the non-psychiatric causes are ruled out, a psychiatric consultation can be ordered to find the diagnosis and begin treatment tailored to the patient’s case (1).

Self-Quiz
Ask Yourself...
- What is the first line of the treatment of psychosis?
- Name three elements necessary in a thorough patient history when assessing for psychosis.
- What lab test is essential when assessing for psychosis?
Etiology
The cause of psychosis remains unknown. The mechanism by which it develops is also unknown. Though the prevailing thought is that psychosis (and particularly schizophrenia) is mainly a disease of the brain, recent studies point to early development, social and psychological processes, and genetics as playing a role in its onset and development. Issues such as childhood trauma, sexual abuse, drug use/abuse, infectious disease, and pregnancy have all been known to contribute to the onset of psychosis. It is important to take a comprehensive history when assessing a patient with psychosis (1).
Treatment
Currently, the most common approach in the treatment of psychosis is antipsychotic medications. Typically, second-generation antipsychotics are preferred to first generation.
First Generation Antipsychotics
Chlorpromazine and other first generation antipsychotics are all dopamine D2 receptor antagonists. They also share many of the same adverse effects such as parkinsonism, motor restlessness (akathisia), involuntary repetitive movements (tardive dyskinesia), and hyperprolactinemia. In 1990, the drug clozapine was approved by the U.S. Food and Drug Administration (FDA). It is practically free of the adverse effects of increased prolactin and neurologic issues.
Second Generation Antipsychotics
Researchers built on the success of clozapine and developed more drugs with the same or less efficacy. Though all the second-generation medications do not have neurologic adverse effects, they do present with other adverse effects such as weight gain and insulin resistance (3).
Treatment of psychosis should be personalized and based on the clinical presentation of the patient. Cognitive behavioral therapy has proven to be effective yet rarely used worldwide. Other psychosocial interventions are often implemented for patients with psychosis, though the interventions used are rarely validated by any up-to-date research (4).
Quality of Life
Patients suffering from psychosis often have issues with normal life functioning. One of the biggest issues is the stigma associated with mental illness. Both the stigma from others who look down on the patient with psychosis and, perhaps more detrimental, the internal stigma the patient places on themselves. With prolonged psychosis, there is a strong connection with internalized stigma and poor social functioning, and an increase in psychotic symptoms. These affect the patient’s overall functioning and quality of life. It should be noted that when a patient has psychosis, this also puts a strain on their family. Often, it is up to the family members to manage the patient’s treatment and adherence to the plan. They can be greatly affected by the patient’s issue and may, themselves, need counseling. They can also be stigmatized because of their family member’s diagnosis (2).

Self-Quiz
Ask Yourself...
- What is the cause of psychosis?
- Name two elements that can contribute to the onset of psychosis.
- What is the most common treatment of psychosis?
- Name a first generation antipsychotic.
- Name one adverse effect of second generation antipsychotics.
- Aside from medications, name another treatment for psychosis.
- Beside the patient, whose quality of life may be affected by psychosis?
Conclusion
Psychosis is a complex disorder which can affect the patient in many different ways. Patients with psychosis have been known to completely detach themselves from reality. As such, the problem can also greatly affect the family of the patient. The most important aspect, from the nursing point of view, is early detection through an extensive assessment with a comprehensive history. The treatment should be designed with the individual patient in mind.
References + Disclaimer
- Calabrese, J., & Khalili, Y. A. (2023, May 1). Psychosis. Europe PMC. Retrieved March 16, 2024, from https://europepmc.org/article/NBK/nbk546579#impact
- Firmin, R. L., Lysaker, P. H., Luther, L., Yanos, P. T., Leonhardt, B., Breier, A., & Vohs, J. L. (2019). Internalized stigma in adults with early phase versus prolonged psychosis. Early Intervention in Psychiatry, 13(4), 745–751. https://doi.org/10.1111/eip.12553
- Goff, D. C. (2020). The pharmacologic treatment of schizophrenia—2021. JAMA. https://doi.org/10.1001/jama.2020.19048
- Maj, M., van Os, J., De Hert, M., Gaebel, W., Galderisi, S., Green, M. F., Guloksuz, S., Harvey, P. D., Jones, P. B., Malaspina, D., McGorry, P., Miettunen, J., Murray, R. M., Nuechterlein, K. H., Peralta, V., Thornicroft, G., van Winkel, R., & Ventura, J. (2021). The clinical characterization of the patient with primary psychosis aimed at personalization of management. World Psychiatry, 20(1), 4–33. https://doi.org/10.1002/wps.20809
- Novak, G., & Seeman, M. V. (2022). Dopamine, psychosis, and symptom fluctuation: A narrative review. Healthcare, 10(9), 1713. https://doi.org/10.3390/healthcare10091713
- Sauvé, G., Brodeur, M. B., Shah, J. L., & Lepage, M. (2019). The prevalence of negative symptoms across the stages of the psychosis continuum. Harvard Review of Psychiatry, 27(1), 15–32. https://doi.org/10.1097/hrp.0000000000000184
- The Recovery Village. (2023, May 8). How long does psychosis last? stages & types of psychotic episodes (R. Alston, Ed.). The Recovery Village Drug and Alcohol Rehab. Retrieved June 16, 2024, from https://www.therecoveryvillage.com/mental-health/psychosis/how-long-does-psychosis-last/
- Volkan, K. (2020). Schizophrenia: Epidemiology, causes, neurobiology, pathophysiology, and treatment. Journal of Health and Medical Sciences, 3(4), 487–521. https://doi.org/10.31014/aior.1994.03.04.143
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
