Course
Ketamine in Depression Management
Course Highlights
- In this Ketamine in Depression Management course, we will learn about what treatment-resistant depression (TRD) is and how it impacts patients.
- You’ll also learn important drug information about ketamine and esketamine, including mechanism of action, side effects, adverse reactions, and indications for use.
- You’ll leave this course with a broader understanding of nursing interventions for drug administration and monitoring patient condition for ketamine.
About
Contact Hours Awarded: 1
Course By:
Abbie Schmitt, RN, MSN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
There is a light at the end of a very dark tunnel for those suffering with a condition called treatment-resistant depression (TRD). That light came in the form of esketamine, which is a nasal spray form of Ketamine, and was approved for treatment of TRD by the FDA in 2019. The medical community seems to have consensus in positive support for this drug therapy, given that the guidelines are followed in treatment regimens and contraindications are closely reviewed. This course is designed to highlight TRD by explaining the statistics, signs and symptoms, medications, and alternative treatments. We will also dive into the pharmacological aspects of Ketamine, including the drug history, indications, mechanism of action, contraindications, common side effects, and recommended administration.
Treatment-Resistant Depression
Treatment-resistant depression (TRD) is a term to define continued depression for a patient diagnosed with major depressive disorder without an adequate response to multiple treatments (10). Although this disorder is widely recognized, there is currently a need for a comprehensive and streamlined definition for what constitutes both an adequate response and an adequate trial. Researchers and clinicians are trying to establish a more comprehensive guideline for this condition. TRD can be classified as the patient not ever having adequate response to antidepressant treatments or as having relapsed after achieving an adequate response (10). An “adequate response” is typically defined as roughly half or greater reduction in depressive symptoms (10). Depressive symptoms measurements utilize a depression rating scale such as the Hamilton Depression Rating Scale (HAM-D) or Montgomery-Asberg Depression Rating Scale (MADRS) (10).
Depression is highly linked with comorbidities that impact physical decline (5). Factors such as physiological impact of physical illnesses, the use of multiple medications, and the burden of physical disability contribute to the lack of response to depression treatment (5). Research supports that several medical conditions have a strong correlation to TRD. A meta-analysis of long-term longitudinal studies found significantly higher risk of incident diabetes in patients who are depressed. Diabetic patients with depression have been shown to have poor self-management leading to increased risk of complications and mortality (5).
Immune decline has also been linked with TRD (5). Other conditions with a higher correlation with TRD include metabolic syndrome, hypertension, dyslipidemia, and cardiovascular diseases in general (5). Studies show that when TRD is present, management and outcomes of these various diseases decline. With successful treatment of TRD, we could see an improvement among diabetes and heart disease management as well.
Statistics
The World Health Organization (WHO) reports an estimated 4.4% of the global population suffers from depression (5). Studies tell us that roughly 50% of patients with major depressive disorder do not have a significant response to their first antidepressant treatment and 20%–30% do not respond to at least two treatment trials (10). This reality can be discouraging for clinicians and especially patients. Medical providers may continue changing medications, refer to psychotherapy, or both. Unfortunately, relapse rates among individuals requiring three to four trials are reported at approximately 65%–70% (10). Relapse is when a patient reports relief of depressive symptoms after treatment, but then reports this relief is no longer present after a period.
Signs and Symptoms
The foundation of TRD is depression. Depression is a broad term and is unique to every patient. The medical team will heavily rely on subjective data, which focuses on the patient’s expression of feelings, thoughts, or emotions. Objective data will also be present. Let’s take a look at commonly reported signs and symptoms of depression before we move on to specify TRD. A depressive episode is different from mood fluctuations, as episodes are reported to last the majority of the day, almost every day, for at least 2 weeks (7).
Subjective Data of Depressive Episode:
- Verbalized depressed mood (feeling sad, irritable, empty, groggy)
- Loss of pleasure or interest in activities they typically enjoy
- Poor concentration
- Feelings of excessive guilt or low self-worth
- Hopelessness
- Suicidal thoughts
- Poor sleep patterns
- Changes in appetite or weight
- Report of fatigue and low energy
- Poor performance at work and school
Objective Data of Depressive Episode:
- Disorientation
- Drowsiness
- Impaired memory
- Disheveled appearance
- Flat affect
A depressive episode can be categorized as mild, moderate, or severe depending on the severity of symptoms.
There are different patterns of depressive episodes including: (7)
- Single episode depressive disorder (first and only episode)
- Recurrent depressive disorder
- Bipolar disorder (depressive episodes alternate with periods of manic symptoms)
Psychiatric Assessment Tools: (10)
- Patient Health Questionnaires
- Hamilton Rating Scale for Depression (HDRS-17)
- Montgomery-Asberg Depression Rating Scale (MADRS)
- Monitoring for suicidal ideation is of paramount importance.
Medications
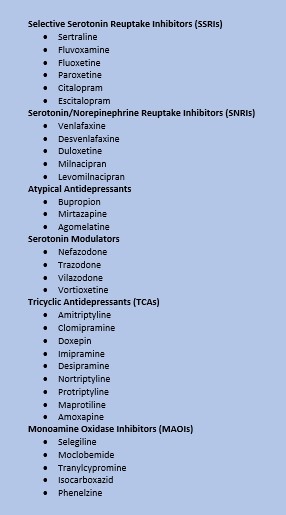
Monotherapy (single medication change) or polytherapy (addition of more medications) treatment options may be considered for TRD. Simply changing to a different type of medication eliminates the risk of adverse drug interactions, while combined therapy may reach better results for reduced depressive symptoms. Clinicians may choose to switch to a different class of antidepressant (e.g., from an SSRI to an SNRI) or switch within the same class (e.g., citalopram to fluoxetine) (10).
Figure 1. List of Antidepressants: Classes and Brands. (8)
Alternative Treatments
Alternative psychological treatments used for depression include:
- Electroconvulsive therapy (ECT): The oldest among the early biological treatments introduced in psychiatry, and the only one still in use (7)
- Behavioral activation (7)
- Cognitive behavioral therapy
- Interpersonal psychotherapy
- Problem-solving therapy
- Magnetic seizure therapy (MST) (7)
- Trigeminal nerve stimulation (TNS)
- Vagus nerve stimulation (VNS) (7)
- Psychedelics (7)

Self-Quiz
Ask Yourself...
- Have you ever cared for a patient experiencing depressive symptoms?
- Can you name the various classes of antidepressants?
- How do you think multiple diagnosis’ impact self-care?
Ketamine
History
Ketamine has been used as an anesthetic agent for more than 50 years (5). It was originally patented for veterinary use in 1963 and then approved for human use as an anesthetic treatment in 1970 (5). It became very popular because the analgesic properties of Ketamine outlast its anesthetic effect (5). Essentially, the pain relief of Ketamine outlasted the sedation effects in patients. Racemic ketamine (typically given IV) and esketamine (intranasal) pharmacokinetics are identical.
Indications
Esketamine is recommended for use by adults with treatment-resistant depression (TRD) or adults with major depressive disorder (MDD) with suicidal thoughts or actions. Although there is a need for specific guidelines for defining treatment-resistant depression (TRD), the basic definition contains the following components:
- TRD is broadly defined as a failure for a patient to achieve an adequate response to an adequate trial of an antidepressant therapy for treatment of a major depressive disorder (10).
- Adequate response is either defined as nearly asymptomatic or a ≥50% decrease in depressive symptoms (measured using an approved depression rating scale).
- An adequate trial must include an approved antidepressant medication taken at a consistent dose for a period deemed adequate to achieve a therapeutic effect (e.g., 12 weeks).
Pharmacokinetics
Ketamine metabolism is characterized by low binding to plasma proteins and has an extensive distribution (4). Plasma protein binding refers to how tightly a medication attaches to blood proteins within the blood plasma, which impacts the drug’s efficacy. The less bound a drug is, the more efficiently it can diffuse through cell membranes (2). Esketamine is primarily metabolized to noresketamine; esketamine’s half-life is biphasic, with an initial decline in concentration within two to four (4). Metabolism occurs in the liver, the kidneys, intestine, and the lungs; then excreted in bile and urine after glucuronoconjugation (4).
Ketamine elimination clearance is considered high (1000–1600 ml/min), which is equal to liver blood flow (4). Elimination clearance describes the rate at which a drug is removed from a patient’s blood plasma. High clearance means it does not linger over a long period of time. Ketamine elimination half‐life is 2–3 h. Ketamine targets the glutamatergic system, specifically the NMDA receptor. Its antagonistic component of GABAergic interneurons results in a glutamatergic surge, causing an increase in brain-derived neurotrophic factors (4).
Important take-away points: Ketamine is metabolized in multiple organs, acts quickly, and is typically cleared quickly. It’s important to remember that various patient factors such as comorbidities and metabolism impact the efficacy of Ketamine.
Mechanism of Action
Ketamine and esketamine are considered to be mainly noncompetitive NMDA receptor antagonists. The drug also interacts with opium receptors, monoaminergic receptors, cholinergic receptors, and Ca2+ channels, according to research studies (3). Research also shows ketamine acts to inhibit the reuptake of dopamine, thus dramatically increasing levels of dopamine (3). Ketamine is unique because it has a combination of these actions. Research proves this uniqueness, as other NMDA receptor antagonists have failed to provide comparable results to Ketamine on depressive symptoms.
For many years our brains were considered to have a static internal environment, it is now understood that brain histology changes and adapts in response to environment changes and injury (2). Basically, the brain and neural function is constantly firing and transferring responses. The dynamic and responsive nature of neuronal function is known as plasticity (2). Poor synaptic communication, sometimes caused by various stressors, is believed to be responsible for depressive symptoms. Studies have shown that ketamine induces brain-derived neurotrophic factor (BDNF) in the brain, which rejuvenates the stress-degraded synapse to its original pre-stress state (2).
If neural plasticity is accepted as a phenomenon, this is helpful in our understanding of the delayed benefits of antidepressant treatments as it takes time to repair neurotransmitters to their original state. Ketamine targets the glutamatergic system, specifically the NMDA receptor. Its antagonistic component of GABAergic interneurons results in a glutamatergic surge, causing an increase in brain-derived neurotrophic factors (4).

Self-Quiz
Ask Yourself...
- Have you cared for a patient who was given ketamine for pain or sedation?
- How do you think the mechanism of action of ketamine compares to other antidepressant medications?
Adverse Effects
Several randomized controlled trials (RCTs) have been done to test the efficacy and safety of esketamine for the treatment of TRD and meaningful data was collected with a meta-analysis. The most frequent adverse effects under treatment with esketamine were nausea, dissociation, dizziness, vertigo, hypoesthesia, sedation, and paresthesia (11). The clinician can mediate these effects and weigh the benefits versus effects with the patient. Patient education and involvement is critical for navigating adverse effects.
Benefits versus Risks
The patient should be the center of this discussion on weighing benefits versus risks. Each patient is unique in their experience. Some patients have fears and aversions of side effects, while some view it as a beneficial trade-off. Informed consent is a critical aspect of patient care, providing patients with education on the drug and potential complications. Studies support the efficacy of ketamine in the treatment of depression and reduction of suicidal thoughts and has been named a ‘breakthrough therapy’ medicine by US FDA (11). However, studies have also revealed relapse in treatment. Statistics support a response lasting at least a day for about 70% of patients and up to three days for 30% of patients (11). Dependance and tolerance are risks that must be addressed with the patient, as well as the possibility of long-term organ (liver, bladder) injury that is lacking in longitudinal studies (3).
Contraindications
Ketamine is contraindicated in the following patients with:
- Elevated Blood Pressure:
- Patients with underlying hypertension should be closely monitored and cardiology should be consulted for patients with cardiovascular disease (due to an increase in heart rate and blood pressure).
- Underlying conditions that raise blood pressure:
- High blood pressure increases the risk of complications such as aortic dissection, uncontrolled hypertension, myocardial infarction, or aneurysms (6).
- Prior hypersensitivity to the drug
- During pregnancy or breastfeeding:
- It is unknown if Ketamine passes into breast milk.
- Intoxicated with ethanol due to additive sedation
- Schizophrenia:
- There is potential for exacerbating the underlying condition.
Common Side Effects
Ketamine can cause an increase in pulse rate and blood pressure, which is suggested to be dose-dependent (5). Another common side effects of ketamine nasal spray include dysgeusia, which is an unpleasant or bitter taste, and is attributed to postnasal dripping of residual spray into the oral cavity contacting the taste buds and triggering the taste receptor cells (3). Another physiological side effect reported mainly with long-term use of ketamine is ulcerative or interstitial cystitis (5). Hallucinations have been reported (11); along with tinnitus (a ringing in the ears), nausea or vomiting, anxiety, and headache (7). These side effects have generally been considered short-lasting following treatment.

Self-Quiz
Ask Yourself...
- Can you prioritize the common side effects based on needed intervention?
- Have you administered a nasal spray before? If so, what were common complaints from the patient?
- Do you recognize any concerning long-term complications with extended use?
- What are some critical interventions for nausea/vomiting of the sedated patient?
FDA Approval
The U.S. Food and Drug Administration approved esketamine nasal spray for the treatment of treatment-resistant depression in 2019 and for treatment in patients with major depression and suicidal ideation or behavior in 2020 (5). There are certain restrictions that fall under a Risk Evaluation and Mitigation Strategy (REMS) – a drug safety program. The restrictions primarily focus on where this drug is administered and who can obtain it. Ketamine and esketamine are Schedule III controlled substances under the US Controlled Substances Act (5). Thus, controlled substances are closely followed and scrutinized regardless of the treatment use.


Self-Quiz
Ask Yourself...
- Are you familiar with the approval process for drugs by the U.S. Food and Drug Administration (FDA)?
- What do you think is required for an approval?
- Are you familiar with the different classes/ schedules of controlled substances?
Administration FAQs
Q: What is the recommended dosage for esketamine?
- A: Dosing may fluctuate based on each provider and the severity of patient’s symptoms. The recommended dosage of a common brand of esketamine for the treatment of depressive symptoms in adults with MDD with acute suicidal ideation or behavior is 84 mg twice per week for 4 weeks (9). Dosage may be reduced to 56 mg twice per week based on tolerability (9).
Q: How is the administration of the nasal spray different from the ketamine infusion?
- A: The nasal spray is inhaled into the respiratory system through the nasal passage, in contrast to the medicine injected into a muscle or blood vessel.
Q: Can patients take esketamine on their own?
- A: No. Administration must be within a controlled on-site healthcare environment.
Q: Can Ketamine interact with other medications?
- A: Patients should alert the healthcare provider of central nervous system (CNS) depressants, psychostimulants, or monoamine oxidase inhibitor (MAOI) medications they take regularly (9). Considering it is a nasally administered medication, other medications given this route, like a nasal steroid or decongestant spray, should not be given within one hour (9).
Q: Is it recommended to eat or drink prior to administration?
- A: It is recommended to avoid eating within two hours or drinking liquids within 30 minutes of administration (9). This is related to side effects of gastrointestinal upset, nausea, and vomiting.
Monitoring
Ketamine administration must be done in an on-site clinic or hospital setting (4). The patient should be observed and monitored for two hours, or longer, under the judgment of the treating physician following administration. As we discussed earlier, it is essential to monitor vital signs and cardiac function. Continuous and time regulated blood pressure, pulse, respiratory rate, and oxygen saturation is crucial when using ketamine. The healthcare team should have the emergency intubation materials prepared when administering ketamine. It is also advised that patients should not drive, use heavy machinery, or perform other potentially hazardous activities for up to 24 hours following ketamine administration (6).
Assessment tools, such as the Montgomery-Asberg Depression Rating Scale or the Hamilton Depression Rating Scale, can assign scores to symptoms and help monitor improvement among patients.

Self-Quiz
Ask Yourself...
- Can you think of patients with certain conditions who should be monitored more closely or longer than others?
- Have you ever cared for a patient that needed continuous vital sign assessment (example, blood administration, anesthesia)?
- What are some examples of tools to help healthcare professionals identify progression or improvement of depression?
Current Research Studies
The research community certainly shows interest in the use of Ketamine for depression. There is a significant need for this because there is a hopeful possibility that this drug may be effective in the treatment of other mental health disorders.
As we consider research studies, it is vital to examine the most meaningful data available, especially when gaining understanding of medications. Research studies are conducted for almost any drug and the results can unfortunately be unreliable. Studies must apply sound research methods and be free of bias. Meta-analysis studies are a terrific resource for nurses when researching topics. Meta-analysis data is the statistical combination of results from two or more separate studies that examine the integrity of each research study.
A major clinically researched topic is the use of Ketamine for TRD with the presence of suicidal ideations and the risk of suicidal behavior. Multiple meta-analysis found positive results, mixed contraindications, and implications for further research. For example, one specific meta-analysis was conducted on 11 studies of single-dose ketamine use in depression and found a significant reduction in suicidal ideation and improvement in depression symptoms (5). There are also many randomized controlled trials (drug vs placebo) which showed reduction in depressive symptoms in the patients administered esketamine, along with a significant reduction of suicidal ideation (4, 5, 10, 11).

Self-Quiz
Ask Yourself...
- Have you noticed opportunities to participate in clinical trials?
- Can you name different research databases that contain reliable, peer-reviewed articles?
- What do you think are some benefits of meta-analysis data?
Conclusion
Hope for patients suffering with treatment-resistant depression (TRD) and suicidal thoughts has possibly come in the form of esketamine, which is a nasal spray form of Ketamine. Following the approval by the FDA in 2019, this drug has had significant positive outcomes. The statistics, signs and symptoms, medications, and alternative treatments for TRD are important to understand when examining the pharmacological actions and effects of Ketamine. Nurses can have a meaningful impact in both the clinical and research environment for the continued understanding and use of this drug for depression.
References + Disclaimer
- Domino, E.F., Domino, S.E., Smith, R.E., Domino, L.E., Goulet, J.R., Domino, K.E. and Zsigmond, E.K. (1984), Ketamine kinetics in unmedicated and diazepam-premedicated subjects. Clinical Pharmacology & Therapeutics, 36: 645-653. https://doi.org/10.1038/clpt.1984.235
- Hood, P. & Khan, E. (Eds.). (2020). Understanding pharmacology in nursing practice. Springer. https://doi.org/10.1007/978-3-030-32004-1
- Kenakin, T.P. (2022). Comprehensive pharmacology. Elsevier.
- Kuntz. (2021). Managing treatment-resistant depression. The Psychiatric Times., 38(9).
- Quevedo, Riva-Posse, P., & Bobo, W. V. (Eds.). (2022). Managing treatment-resistant depression: road to novel therapeutics. Elsevier.
- Rosenbaum SB, Gupta V, Patel P, et al. Ketamine. [Updated 2023 May 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470357/
- Sadek. (2021). Clinician’s guide to psychopharmacology. Springer. https://doi.org/10.1007/978-3-030-60766-1
- Sheffler ZM, Patel P, Abdijadid S. Antidepressants. (2023) In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538182/
- Spravato. (2020) Prescribing information. GlaxoSmithKline. Available from: https://www.janssenlabels.com/package-insert/product-monograph/prescribing- information/SPRAVATO-pi.pdf
- Vaccarino, S. & Kennedy, S. (2021). Chapter 3 – Treatment resistant depression, Editor(s): Gustavo H. Vazquez, Carlos A. Zarate, Elisa M. Brietzke,
- Ketamine for treatment-resistant depression. Academic Press, Pages 33-84, ISBN 9780128210338,
- Yang, S., Wang, J., Li, X., Wang, T., Xu, Z., Xu, X., Zhou, X., & Chen, G. (2022). Adverse Effects of Esketamine for the Treatment of Major Depression Disorder: Findings from Randomized Controlled Trials. The Psychiatric quarterly, 93(1), 81–95. https://doi.org/10.1007/s11126-020-09871-x
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
