Liver Transplant Nursing Care
Contact Hours: 3.5
Author(s):
Chelsea McCracken RN-CCRN
Course Highlights
- In this course you will learn about the stages and causes of liver disease, and why it is important for nurses to recognize these.
- You’ll also learn the basics of liver transplant nursing care.
- You’ll leave this course with a broader understanding of liver transplantation.
Introduction
In 1967, Dr. Thomas Starzl was the first in the realm of liver transplant nursing care to successfully perform an orthotopic liver transplant (OLT) in a hepatoblastoma patient. Although the patient ultimately died 18 months later of metastatic disease, this was the beginning of several major transplant surgery breakthroughs, including the introduction of brain-death criteria in 1968 and the introduction of immunosuppressive medications in 1979 (1).
52 years later, and the process of a liver transplant nursing care is far from a perfect science. Patients require lifelong close follow-up, have frequent infections, and can occasionally need re-transplantation due to graft dysfunction.
Purpose Statement
Liver transplant nursing care patients require meticulous care both pre and post-transplant, and it is paramount that advanced care clinicians in all medical subspecialties are knowledgeable on the basic medical problems and risks of organ transplant.
The purpose of this module is to provide a comprehensive overview of the liver transplant process and an extensive review of the inpatient management of the post-transplant patient. By educating clinicians on the transplant process and the care of the transplant patient, the medical community hopes that the success of liver transplants in nursing care will continue to grow.
Stages of Liver Disease
As most of us know in liver transplant nursing care, there are many liver diseases that can cause organ dysfunction. Despite the long list of liver diseases, they tend to progress in a similar fashion. Here, we will break down the stages of liver disease, from a healthy liver to cirrhosis.
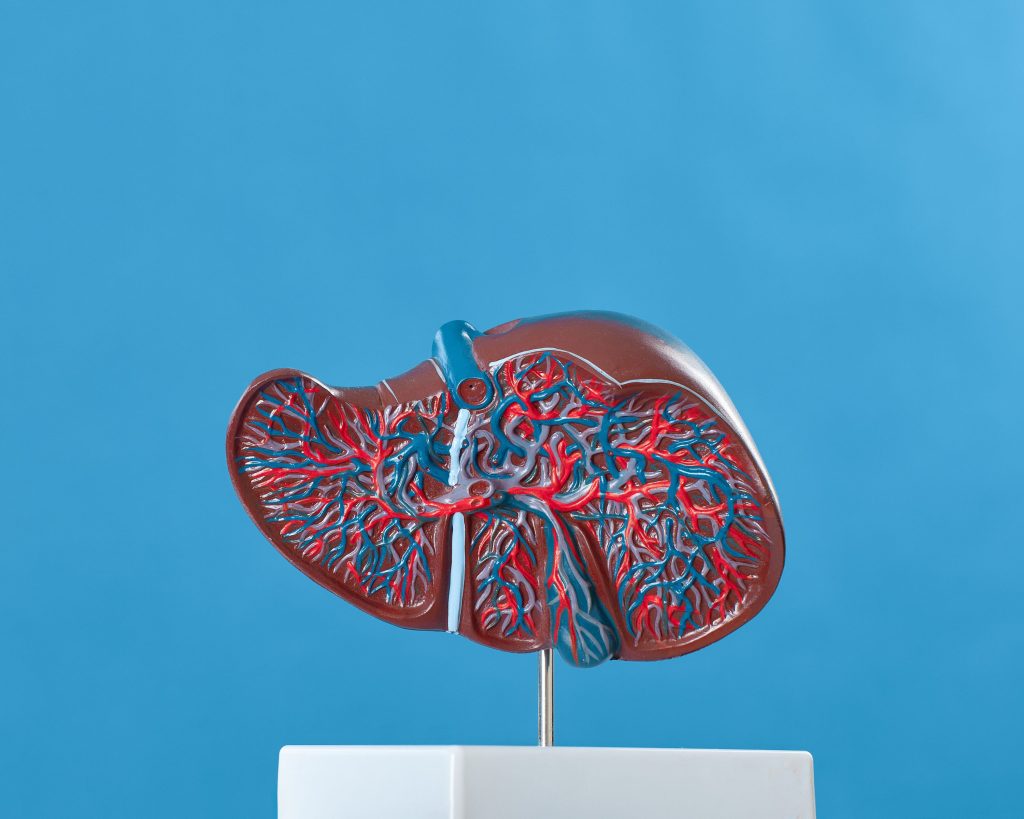
A healthy liver has numerous important functions, including helping to fight infection, cleaning the blood of bacteria, producing coagulation factors, producing bile to digest fat and absorb certain vitamins, metabolizing and removing toxic byproducts of medications, and processing food into storable energy. It can regenerate when injured, but as damage occurs from infection or disease, the liver loses its ability to function fully (2).
The first stage of liver injury is inflammation, which causes the liver to be tender and enlarged (2). This can occur when the immune system is trying to fight off infection and can cause a patient discomfort, or depending on the severity of inflammation, they may be asymptomatic (2).
If the liver dysfunction is left untreated, the liver will begin to develop scar tissue and slowly replace healthy tissue. This process is referred to as fibrosis. As scar tissue replaces healthy tissue, blood flowing through the portal system can be impaired, making it more difficult for the healthy parts to function appropriately. There are numerous scoring systems to grade fibrosis to give an objective trajectory of the degree of liver fibrosis and predict how the fibrosis will progress. A popular scoring system is the METAVIR scoring system, which uses a liver biopsy sample to assign a score for “activity,” or how the fibrosis is projected to progress, and a score for the degree of fibrosis itself (3). The scores range from A0 (no activity) to A3 (severe activity) and F0 (no fibrosis) to F4 (cirrhosis) (3).
As fibrosis progresses, it leads to cirrhosis, which is defined as irreversible scarring of the liver. At this stage of liver disease, the liver cannot heal, but progression of scaring can be prevented. There are four stages of cirrhosis: Stage 1 is considered to be compensated cirrhosis as it involves scaring of the liver but has few symptoms (4). Worsening of portal hypertension and the development of varices characterize stage 2 cirrhosis (4). The new onset of ascites characterizes stage 3 cirrhosis and is the hallmark stage of decompensated cirrhosis (4). Stage 4 cirrhosis is characterized by the development of end-stage liver disease (ESLD) and is fatal without a liver transplant (4).
Ask yourself...
- What prior experiences have you had with liver transplant nursing care?
- How will you explain the stages of liver disease to patients?
- Have you seen an increased or decreased need for liver transplantation in practice?
- What experience do you have with transplants?
- What indicates that a patient has progressed to stage four liver disease?
- What ethical considerations impact transplantation?
- What education can a nurse provide to a patient in the early stages of liver failure that may reduce the risk of further liver failure?
- How would you describe fibrosis?
- Is the treatment after a liver transplant short or long-term? Why?
- What is the role of the liver in the body?
Causes of Liver Disease Necessitating Liver Transplant Nursing Care
Liver disease is the 12th most common cause of death in US adults, resulting in 34,000 deaths annually from cirrhosis alone (5).
A liver transplant is indicated in patients with severely decompensated cirrhosis that has surpassed the limits of medical management or once a patient with cirrhosis has experienced complications such as ascites, hepatic encephalopathy, variceal hemorrhage, or hepatocellular dysfunction and results in a MELD > A/A = A 15 (6). The most common cause of decompensated cirrhosis remains the hepatitis C infection (HCV). The fortunate caveat is that direct-acting antiretroviral agents (DAAs) are becoming more readily available, and the incidence of OLT related to HCV infection is expected to decrease (7).
Due to the high prevalence of HCV in the community and in-patient settings, providers should be aware of the DAA classes and the basic mechanisms of action. DAAs work by directly targeting the hepatitis C virus to prevent viral duplication, offering shorter treatment times, fewer side effects, and higher overall cure rates (8). There are four classes of DAA, and the drug chosen is based on the patient’s specific hepatitis C genotype. Most DAA drugs are combination drugs that combine two separate courses of DAAs to maximize viral replication inhibition. Common combination DAA drugs include Mavyret, which is a combination of two DAA drugs and has an approximate cure rate of 97-100% (9). Treatment is between 8-12 weeks and costs $ 26,400 for 8 weeks of treatment (9).
Common side effects reported in clinical trials include headache, insomnia, nausea, fatigue, and asthenia (9). Another well-known DAA is Harvoni (Ledipasvir and Sofosbuvir), which has a sustained viral response of 93-99% and has varying treatment lengths depending on the patient’s degree of liver disease (10). Treatment length ranges from 8 weeks in patients who are treatment-naïve with no cirrhosis to 24 weeks for patients with previously treated HCV and compensated cirrhosis (10). The cost of a 12-week regimen is averaged at $ 94,500 (10). Most insurance plans offer partial coverage, but even if a patient’s plan does not cover the cost, numerous patient assistance programs can be used to assist with the treatment.
The other main indications for liver transplant in order of decreasing frequency are alcoholic liver disease (18%), idiopathic/autoimmune hepatitis (12%), primary biliary cirrhosis (10%), acute liver failure (7%), hepatitis B virus (6%), metabolic liver disease (3%), cancer (3%), and fulminant hepatic failure (2%) (11)
Less common reasons a patient may qualify for a transplant in the absence of liver failure include treatment of portopulmonary hypertension, hepatopulmonary syndrome, correction of primary hyperoxaluria (done with a simultaneous kidney transplant), and management of cystic fibrosis-induced cirrhosis (10).
Ask yourself...
- What are some modifiable and non-modifiable risk factors for liver disease in liver transplant nursing care?
- How can patients alter their lifestyles to reduce their chances of developing liver disease?
- HCV infection treatment represents an opportunity to reduce the burden of liver disease. What screening and treatment programs are offered to liver transplant nursing care patients?
- What role does the nurse play in preventing liver disease in patients?
- What are three things that are toxic to the liver that a nurse can educate a patient to avoid?
- What is cirrhosis?
- What role do community nursing and education play in preventing liver disease?
- How do healthcare disparities impact the incidence of liver disease?
- Why does hepatitis increase the risk of liver failure and transplant?
- Which laboratory values are important to monitor for patients taking hepatotoxic medications?
Case Study: Meet The Patient
You are an acute care nurse practitioner working in a busy ICU. You begin your shift with a new admission, Ms. Mino. She was an ICU to ICU transfer overnight, and the overnight resident figured you’d do the HPI on pre-rounds because the patient “wanted to sleep”!
Ms. Mino is a 65-year-old woman with a PMH of all the good stuff. HTN, T2DM, hypercholesterolemia, and arthritis. She drinks 1-2 glasses of wine on special occasions and does not smoke.
Ask yourself...
- Which of the above information indicates that the patient may have an increased risk for liver disease?
When Demand Exceeds Supply: How Do We Allocate Livers?
While the best results are achieved in patients who are still relatively healthy, the patients who need a transplant most urgently are those who are critically ill and have acutely decompensated. A model that prioritizes the sickest first was developed to allocate organs properly. The Model for End-Stage Liver Disease (MELD) was originally developed to predict the 3-month mortality of patients who underwent a transjugular intrahepatic portosystemic shunt (TIPS) placement (12). It was adopted by the United Network for Organ Sharing (UNOS) in 2002 as the model for liver allocation in the United States.
The MELD score is the product of an equation using the patient’s bilirubin, INR, and creatinine to produce a number that directly correlates to the patient’s need for a transplant in the next 3 months (9). The equation is as follows: MELDScore = 10 * ((0.957 * log(Creatinine)) + (0.378 * log(Bilirubin)) + (1.12 * log(INR))) + 6.43 (12).
In 2016, UNOS modified the MELD score also to take the patient’s sodium level into account. Hyponatremia is directly correlated with the severity of cirrhosis and independently predicts mortality independently of the MELD score. MELDNa score benefits patients who have a low MELD score but suffer from profound hyponatremia. The equation for MELD-Na is: MELDNa= MELD – Na – [0.025 × MELD × (140 − Na)] + 140 (12).
Additionally, there are certain patient populations, such as those with hepatocellular carcinoma (HCC), Cholangiocarcinoma, or portopulmonary hypertension, that receive MELD exception points to depict their waitlist mortality accurately. The exception to the MELD system is referred to as Status 1A and is reserved for patients who have a sudden and severe onset of liver failure and are expected to live only a matter of hours without a transplant (13).

Ask yourself...
- What are the strengths and weaknesses of our current transplant system?
- How do you think we can improve our current transplant system/
- What barriers in healthcare can cause complications within our transplant system and process?
Case Study: History of Present Illness
During the exam, she was awake, alert, and able to participate in your HPI. Her husband, Jim, is with her and looks concerned. She states that she has been mostly in her normal state of health, minus a chest cold that her grandson gave her last week, but “with some cold medicine, I felt good enough to work on my garden all week! “All the kneeling on the hard ground really hurt my back and knees, though.
Don’t ever get old! It’s all downhill from 40, I swear. I fell just once trying to get up from planting in my flowerbeds the other day. Nothing major. I just toppled over and landed pretty hard on my right knee and side. Can you believe that! I used to be an athlete!”
When asked what originally brought her into the hospital, Jim states that he noticed the whites of her eyes had a strange tint. “Almost yellow-ish,” he says. She replies, “Yes, and my urine has gotten very dark, and I don’t have much urge to urinate, but I probably wasn’t drinking enough when I was out in the yard. This pain in my right side hasn’t really gotten any better either”.
You review her home medications, which are as follows: Glipizide 5mg daily, Amlodipine 10mg daily, and Tylenol for arthritis PRN. She states that due to her fall, she’s been taking a little more than her doctor told her to—3 tablets 3x/day as needed. She’s also been taking NyQuil to help her cough at night—2 tablespoons before bed and 2 tablespoons if she wakes up coughing in the middle of the night.
You do some quick math, and yes- that comes out to about 6,500- 7,150 mg of Tylenol a day. Acute Acetaminophen Toxicity with Acute Liver Failure jumps to the top of your differential. Luckily, she is encephalopathic, but she could become critically ill very quickly. Around this time, her labs come back.
Cr 2.5, Bilirubin 4.8, INR 3.2, Sodium 133. Acetaminophen level: 50
AST 7,377 ALT 3,570 Alk Phos 109
Using the MELD calculator, this MELD score of 35 would be enough to list her as a Status 1A transplant candidate.
Ask yourself...
- What do the lab values indicate is occurring for the patient?
- What additional risk factors does the patient have that increase their risk for liver disease?
- Which medications is the patient taking that are considered hepatotoxic?
- What education should the nurse include about Tylenol and other over-the-counter medications?
- What other assessments do you want to complete for this patient?
Evaluation Process – Liver Transplant Nursing Care
Evaluation for a liver transplant is an extensive and multidisciplinary process that focuses mainly on the allocation of donor organs to recipients with the physical and psychosocial health to withstand a taxing surgery and adopt the new lifestyle that comes with being a transplant recipient. The evaluation process is a multifaceted process involving transplant hepatologists, transplant surgeons, social workers, nutritionists, financial counselors, transplant coordinators, and a psychiatrist.
Patients are expected to abstain from alcohol consumption, tobacco, and illicit drug use, which can pose a challenge if the patient has a prior substance abuse problem. Additionally, patients are educated to avoid NSAIDs and use less than 2,000 mg of acetaminophen daily for pain control. Patients are also educated on adopting healthy eating habits. Transplant medications can increase the risk of developing obesity, heart disease, diabetes, bone loss, and hyperkalemia, and diet modifications can help manage these side effects.
During the evaluation by the hepatology and transplant surgery team, the patient’s history is reviewed with a focus on the duration, severity, complications, and past medical management treatments of the primary liver disease (14). Drug and alcohol dependency issues, current functional level, and level of debility as it relates to liver disease are discussed at length. The physical exam aids in confirming signs of advanced liver disease and identifying exam findings that may impact the success of OLT (cachexia, muscle wasting, overall debility) (14).
This is also when the patient can be assessed for variceal hemorrhage prophylaxis, hepatitis A/B vaccination if applicable, and HCV treatment pre and post-transplant, if applicable (14). The surgical consultation serves as a first-pass education to the patient and family regarding the surgical procedure, donor and graft types, potential complications, rejection rates, and the necessity of lifelong immunosuppression.
During the psychosocial evaluation, social workers and mental health professionals evaluate the potential organ recipient for evidence of compliance with medical directives, adequate support from caregivers, and no psychiatric disorders that may impact compliance post-transplant or include harmful behaviors, such as alcohol, tobacco, or illicit drug use (14). No psychiatric disorder leads to an absolute contraindication to transplant as long as there is adequate preparation, education, and social support (14).
A large part of the psychosocial evaluation is making sure the patient has active insurance that will help to pay for their new lifelong need of medical care and ensuring that the patient has a caregiver identified that will assist them in getting to and from clinic appointments, especially if the patient is under the influence of narcotic pain medication post-operatively (14).
The patient undergoes a battery of laboratory tests to evaluate hepatic function, electrolytes, renal function, viral serologies (to establish Hepatitis A/B/C, CMV, Epstein-Barr virus, and HIV status), tumor markers, ABO-Rh blood typing, and creatinine clearance (14).
The results of the hepatic, chemistry, and electrolytes panels can potentially change the patient’s MELD score, increasing their status on the waitlist. Conversely, if the patient responds to medical management and the lab work improves, their MELD score will reflect improvement in their hepatic function and move them to a lower position on the waitlist.
The renal function and creatinine clearance are crucial to establish a baseline, evaluate the patient for the need for a simultaneous liver-kidney transplant, and dose their medications post-transplant.
The results of viral studies will dictate whether the patient needs treatment pre or post-transplant for a viral illness. There are also programs in place that match HIV + donors to HIV + recipients, and new programs are beginning to emerge that include HCV + recipients with HCV + OR – recipients. As transplant surgery continues to advance, it is very likely that practitioners will be seeing HCV – recipients receiving HCV + organs and undergoing acute HCV treatment post-operatively.
The patient will also undergo ultrasonography to assess the patency of the portal vasculature and triple-phase computed tomography or gadolinium MRI to exclude a complicating hepatocellular carcinoma (HCC). If HCC is identified, attention will be paid to the size and number of lesions in order to direct the next steps in the evaluation process (14). The Milan Criteria uses tumor size, number, and presence of extrahepatic and major vessel involvement to aid in differentiating between patients who should undergo OLT and those who would not be suitable (14).
An important aspect of the transplant evaluation process is cardiac evaluation. As with any surgical procedure, there is a great cardiovascular risk, and the patient must undergo a noninvasive echocardiogram, as well as noninvasive stress testing and a basic cardiovascular exam to rule out a severe cardiovascular disease that would hinder a good long-term outcome (14).
Patients who have advanced liver disease may not be able to achieve the target heart rate during an exercise stress test and may need to undergo a stress test with pharmacological stress test and cardiac catheterization if coronary artery disease cannot be confidently excluded (14).
If >70% coronary artery stenosis is detected, revascularization may be attempted prior to liver transplant, although cardiac surgery in a patient with decompensated cirrhosis carries a risk that does not have documented benefit. In addition to evaluating the patient’s coronary arteries, attention must be paid to assessing valvular heart disease and the presence of ventricular dysfunction.
There is no fast and hard rule when heart function is too poor to undergo transplant surgery. Traditional medical therapies are utilized to optimize the patient’s cardiac function prior to surgery, and they are closely monitored post-transplant to ensure that medical management is sufficiently treating their underlying cardiac disease.

Ask yourself...
- The evaluation process can be difficult for patients and families. How can you help them communicate these emotions?
- It provides an opportunity for hope but, at the same time, may end without a definitive treatment. What additional resources can you utilize to help the family?
- How do liver transplant nursing care professionals explain the process and offer emotional support during the evaluation?
- What education is the priority for a patient scheduled for a liver transplant?
- In what way can collaborative care be beneficial for patients waiting for a liver transplant?
- How can a patient’s psychosocial status impact their transplant outcome and recovery?
- Is there a limit to how long a person can be on the transplant list?
- Why are there so many different members of the treatment team of a patient who needs a liver transplant?
- What role does the nurse play in preparing a patient for a transplant?
- What resources does your facility have to help patients pay for needed surgery such as a transplant?
Case Study: The Workup
After completing your HPI, you go back to the office and call a STAT consult for both hepatology and transplant surgery. You explain the patient’s background, your preliminary data, and your concern for acute decompensation if she remains untreated. The transplant surgery team comes to evaluate the patient, and on their exam, she is lethargic, answers questions, but quickly falls back to sleep.
He noted a flapping tremor when she extended her hand to shake the physician’s hand. Her husband provided her with the details of the HPI. They ask for a full hepatic panel, viral serologies including CMV, EBV, hepatitis panel, and HIV status. They also ask for ABO-Rh blood typing to be done in case the patient needs to be cross-matched with an organ donor. Her standard labs are frequently increased to every 8 hours to assess for metabolic changes, decline in coagulation ability, and trend of liver enzymes.
An MRA abdomen and pelvis are ordered to evaluate her portal vasculature. Cardiology is consulted for pre-surgical cardiac clearance, an EKG is done, and records of her last stress test are requested from her private cardiologist, whom she sees for her hypertension management.
Her viral serologies are all negative, and her abdominal imaging shows no contraindications to liver transplant. She is listed as a Status 1A transplant candidate by the afternoon.
Hepatology recommended initiating an N-acetylcysteine infusion to help medically manage her acetaminophen toxicity and to give Vitamin K 10mg IV to help with her coagulopathy while organ offers are evaluated. Both teams will continue to follow her case closely and update the ICU team and family if an organ becomes available.
Ask yourself...
- What picture are these diagnostic results painting?
- Why is obtaining a current ABO-Rh important for this patient?
- What is a Status 1A transplant candidate?
- What is the purpose of administering an N-acetylcysteine infusion?
- Why did the physician order for the patient to receive Vitamin K?
Living Donor Liver Transplant: The Other Kind of Transplant
Organ transplants have become a victim of their own successes. The number of patients awaiting an organ transplant far exceeds the availability of deceased donor organs. Living donor liver transplantation (LDLT) has expanded the donor pool while also providing patients with a lower MELD score a chance to receive a transplant.
Indications for LDLT vary between the pediatric and adult populations. In adults, the concept of putting a healthy individual at surgical risk poses an ethical dilemma if the organ recipient has an increased risk for mortality post-transplant. Ideal LDLT candidates are separated into two main categories.
First, patients with hepatocellular carcinoma that is confined to the liver and is not associated with liver decompensation (15). This group of patients will not mount a MELD score suitable for a deceased donor liver transplant (DDLT). Still, as their disease progresses and becomes extrahepatic, they will quickly become unsuitable for a transplant altogether.
The second group of patients includes those with disease severity that is not reflected in their MELD scores, such as patients with severe refractory encephalopathy, complicated cholestatic liver disease, ascites, or cachexia (15).
The projected outcome of the transplant recipient is weighed considerably before putting a healthy live donor at surgical risk. In a report by Berg et al. (16), the mortality rate associated with receiving an LDLT was lower than receiving a deceased donor liver transplant, but this depends largely on the severity of illness in the recipient.
As discussed previously, the sicker the patient prior to transplant, the higher their post-operative mortality. Sicker patients with higher MELD scores tend to do poorly with an LDLT because the partial graft is unable to meet the needs of a severely chronically ill patient (15).
Evaluation of the living organ donor is comprehensive and aims to medically and psychologically assess the patient. The medical evaluation begins with a detailed history and physical exam, including assessing the patient’s BMI, as obesity is a risk factor for developing hepatic steatosis.
Patients undergoing the preliminary workup to be live organ donors should be assessed for risk or history of viral hepatitis, non-alcoholic fatty liver disease, cardiovascular disease, malignancy, and bleeding disorders. Further medical workup includes routine blood work, including blood typing, viral serologies (HBV, HCV, HIV, CMV, EBV), autoimmune markers, and coagulation studies (18).
A CT scan or MRI is completed to estimate the volume of the left lateral segment or right lobe to assess whether the mass is appropriate for a particular potential recipient (18). Imaging also allows for identifying any space-occupying lesions or the presence of steatosis. The liver biopsy’s role in the donor depends on the transplant site’s protocol and the patient being evaluated.
A biopsy may be indicated in the potential donor who has elevated liver enzymes, an elevated BMI, or steatosis is suspected (18). The psychological evaluation of the patient centers around ensuring that the potential donor is educated on the procedure and is afforded ample time to make an informed decision about the procedure.
Due to the rigorous process, only a few potential donors are suitable for participating in an LDLT. In the Adult-to-Adult Living Donor Liver Transplantation Cohort (A2ALL), only 40% of donor candidates were accepted for donation (18).
While LDLT has many advantages, it is not without risk to the healthy donor. Farkas et al. (1) report that the donor has a post-surgical morbidity risk of 30% and a mortality risk of 0.8%. The most common cause of morbidity was mild pleural effusions (16.4%), followed by biliary leaks and strictures (15). A significant risk of LDLT for the adult donor is small for size syndrome (SFSS).
This syndrome can occur when there is inaccurate size matching, and the residual hepatic mass is inadequate for the donor’s metabolic needs. SFSS is characterized by prolonged cholestasis with elevated serum bilirubin levels, elevated liver enzymes, coagulopathy, ascites, and, in severe cases, primary non-function with subsequent shock and death (19).
Despite these potentially life-threatening complications, the overall risk for the donor in LDLT is low, and patients are supported medically and psychologically by the medical team throughout their entire transplant process.

Ask yourself...
- What are the advantages and disadvantages of living donor transplants in Liver Transplant Nursing Care?
- What are some ethical complications that may arise when a patient receives a living donor transplant?
- What can cause a person not to be a viable donor to someone?
- What education would the nurse provide to a living donor about the donation process?
- What emotions do you anticipate would coincide with a living donor transplant?
Contraindications of Transplantation
Contraindications to liver transplants can be grouped into two categories: absolute contraindications and relative contraindications. While absolute contraindications depend on the patient’s disease process, relative contraindications rely heavily on the clinical judgment of the medical team. For example, active alcohol abuse is often seen as a relative contraindication depending on the patient’s social support system and desire or willingness to overcome their addiction post-transplant. Absolute contraindications include uncontrolled sepsis, metastatic hepatocellular carcinoma, and uncorrectable cardiopulmonary disease, causing a surgical risk (1).
Traditionally, patients infected with HIV were considered to be unsuitable for transplant due to the concern that immunosuppression post-transplant would accelerate their HIV infection (20). However, due to the use of antiretroviral therapy, the prognosis of HIV patients has improved substantially, and HIV/AIDS without co-infection of hepatitis B or hepatitis C is viewed as a relative contraindication to transplant and is viewed on a case-by-case basis (20).
Relative contraindications include psychosocial conditions, such as poor social support or repetitive noncompliance with medical care (21). Additional relative contraindications include advanced age, severe obesity, severe malnutrition, and other comorbidities that could potentially outweigh the benefit of a transplant.
Ask yourself...
- What is the main difference between absolute and relative contraindications?
- Can an individual with an absolute contraindication still qualify for a liver transplant?
Liver Transplant Nursing Care Complications
Patients recovering from a liver transplant typically spend some time in the intensive care unit. As the practice of liver transplantation has evolved, the length of ICU stay has decreased dramatically, and most patients requiring ICU level of care post-transplant have a 24-hour median length of stay (22). Patients with preexisting conditions, intraoperative events, or postoperative complications may require a prolonged ICU stay and often require the expertise of multiple disciplines to manage their postoperative care.
Infections occurring during liver transplant nursing care are the leading cause of postoperative morbidity and mortality in liver transplants. Razonable et al. (22) estimated that more than half of liver transplant patients will develop an infection in the first year post-transplant.
The risk of developing a postoperative infection is directly related to the patient’s exposure to infectious agents and immunosuppression. Commonly seen infections include urinary tract infections, wound infections, bacteremia, and fungemia.
The causative bacteria are often drug-resistant organisms that require home IV antibiotic administration. Additionally, transplant patients are at higher risk of contracting viral illnesses and frequently get readmitted with enterovirus, adenovirus, or rotavirus.
In the first month postoperatively, patients are most likely to develop infections related to the surgical procedure and hospitalization, such as bacterial and fungal wound infections, urinary tract infections, bloodstream infections, pneumonia, and Clostridium difficile colitis (22).
Patients undergoing liver transplant nursing care should be treated empirically with antibiotic coverage, ideally with a third-generation cephalosporin, preoperatively to decrease the risk of postoperative infectious complications (22). Treatment of bacterial infections involves characterization of the causative organism, source control, and an appropriate antibiotic regimen.
Immunosuppression should be immediately decreased and may need to be temporarily stopped to control a post-operative infection (16) adequately.
Patients are also at risk for specific opportunistic infections in the early postoperative period. Herpes simplex virus (HSV) reactivation disease is the most common opportunistic viral infection and can quickly progress to disseminated multi-organ infection and failure (22). Dissemination of visceral organs is primarily observed in immunocompromised patients. It should be on any practitioner’s differential if a patient is ill and has had previous herpes viral outbreaks, even if no active lesions are present.
Although the incidence of viral sepsis in liver transplant nursing care is somewhere around 1% in developed countries, there is clear documentation of HSV dissemination leading to fulminant hepatitis, pneumonia, encephalitis, and sepsis (12). Treatment of HSV should focus on prophylaxis with antiviral agents, such as acyclovir or ganciclovir.
The donor’s cytomegalovirus (CMV) status, whether positive or negative, must be recorded in the recipient’s chart. CMV affects the recipient’s ability to mount an immune defense and may cause a predisposition for developing postoperative infections (23).
To combat this, patients are started on either a prophylactic or treatment dose of valganciclovir immediately after transplant, depending on their risk of contracting CMV from their donor.
For example, if a recipient is CMV negative pre-operatively but the donor is CMV positive, then this patient will require treatment with valganciclovir and close monitoring of their CMV titers to ensure they don’t contract CMV viremia.
Post-transplant acute kidney injury (AKI) has been reported to occur in 9-78% of cases, with 10% progressing to end-stage renal failure (22). Early identification of potential AKI is crucial to improving patient outcomes, as evidence shows that even small increases in serum creatinine are associated with a decline in overall mortality.
The etiology of post-liver transplant can be related to numerous causes, including sepsis or bacteremia, hemodynamic instability, or hypovolemia. Immunosuppressive agents, such as calcineurin inhibitors (tacrolimus, cyclosporine), are known to cause drug-induced kidney injury. Unfortunately, many OLT patients will end up back on the transplant list for a kidney transplant due to CNI-induced renal failure.
Tacrolimus is the immunosuppressive drug of choice in solid organ transplants, and it is never completely held due to renal dysfunction. If a liver transplant nursing care patient exhibits progressively increasing creatinine, the tacrolimus dose may be decreased and the goal trough lowered to protect renal function. Patients are instructed to increase their oral rehydration and have repeat lab work in 2-3 days to assess changes in their creatinine.
Ask yourself...
- Knowing the potential complications of liver transplants- what physical exam, history, and clinical data will you examine to monitor for these?
- What education would you give a family before a transplant regarding the potential risks of liver transplant nursing care?
- Why do you feel that the length of stays in the ICU has decreased?
- What infections are a patient with a liver transplant at higher risk of getting?
- What education can you provide to the patient about reducing the risk of infection transmission?
- Have you ever seen any of the complications listed above?
- What other complications might you encounter in patients after liver transplant?
Case Study: The Post-Operative Period
Ms. Mino receives an orthotopic liver transplant from a local deceased donor less than 24 hours after transfer to your ICU. You are returning for your 3rd shift in a row, just in time for her to return to your care from the operating room.
You get a sign-out from the transplant surgery fellow. “Yeah, the case went great. For EBL 8.5L, we gave 5 units of PRBC, 3 units of platelets, 3 units of FFP, 6L crystalloid, and 2L albumin. She has 3 JP drains to bulb suction. I wouldn’t start anticoagulation yet. The case was pretty oozy since her INR was >3 at the start of the case. The pressures are a little soft, but we took her off vasopressors before transferring her back here. Okay, thanks. …she’s still intubated but can be extubated at your discretion.”
You assess your patient and find that she has a traditional Mercedes incision with 2 JP drains on the right side and 1 JP drain on the left, all with moderate serosanginuous drainage. Her abdomen is full but soft. She is still sedated from the procedure, but you ask the nurse to titrate the sedation down in hopes of doing a spontaneous breathing trial and extubating in a few hours. Her blood pressure is 110/65 via the arterial line. She is making adequate amounts of clear yellow urine, which will be monitored closely for signs of intravascular depletion or ongoing AKI.
If her SBP drops below 95, you will plan to give her a bolus of albumin and watch for a response. Due to the high EBL of the case, she could need a blood transfusion at some point. Her routine labs are cycled every 6 hours for the first 24 hours. Her first set of post-operative labs show an H/H of 8.5/24, WBC 17, and her liver enzymes are now all under 1,000.
You review her post-operative orders and see that the transplant team entered most of them. Mrs. Mino received induction immunosuppression in the operating room and will begin Tacrolimus, Mycophenolate mofetil, and a Methylprednisolone taper today. Tacrolimus levels will be drawn every morning, and the transplant surgery team will manage the medication dosage. You see that she is on a perioperative antibiotic for five days and prophylactic doses of Bactrim to protect against toxoplasmosis, IV Ganciclovir for CMV prophylaxis, and IV Fluconazole for fungal prophylaxis.
Knowing that her WBC will be elevated due to the surgical stress and high doses of steroids, you will have to remain diligent to assess for additional signs of infection.
Ultimately, Mrs. Mino does well and is extubated 8 hours post-surgery. She is comfortable on a 2L nasal cannula. Her pain is well controlled with IV Dilaudid, which will be transitioned to oral medications once she has returned to bowel function. She was stepped down from the ICU on post-op day 3 and discharged from the hospital on post-op day 7 with close outpatient follow-up.
Ask yourself...
- What assessments are the priority for this patient?
- What lab values will you want to trend for this patient?
- What does bulb action mean for a JP drain?
- What vital signs would indicate that the patient is having post-operative complications?
- What is acute kidney injury, and what are its symptoms?
- What is toxoplasmosis?
- Have you ever managed a patient post-operatively following a transplant? Was their care similar to the scenario above? If not, what did you do differently?
- What education would you provide to Mrs. Mino upon discharge?
- What education would you provide to Mrs. Mino’s family upon discharge?
- What risk does steroid medication play in a patient’s risk for infection?
Post Transplant Management: Immunosuppression, Infection Prevention, and Long Term Outcomes
Management of the post-liver transplant patient requires diligent and comprehensive care.
Liver enzymes, bilirubin, protein synthesis markers, and coagulation factors are monitored frequently to detect early graft dysfunction and the need for aggressive intervention. Enzyme levels are expected to be markedly elevated in the immediate post-operative phase but begin to decrease over the course of several days (23). Persistent elevation in a patient’s liver enzymes may indicate ongoing hepatocellular necrosis (23).
Diligent immunosuppressive therapy is required to prevent rejection, and while immunosuppression pharmacology is always improving, the basic regimens are worth mentioning. In the early postoperative phase, immunosuppressive therapy is complex and must be patient-specific. The most common immunosuppression regimens include calcineurin inhibitors, such as Tacrolimus. Tacrolimus is typically started on post-op day one at a dose of 4mg BID and titrated based on the patient’s goal trough. A goal trough is typically 10-12 ng/mL in the immediate post-transplant phase.
After approximately 4 weeks of initial treatment, the Tacrolimus trough goal will stabilize to a maintenance lifelong goal of 5-8 ng/mL. Corticosteroids play a major role in solid organ transplant immunosuppression and are critical in treating acute organ rejection (23). Typically, patients will begin with high doses of methylprednisolone intraoperatively and transition to prednisone to complete their taper over the course of 3-6 months.
An additional agent, Mycophenolate mofetil, is used to treat acute rejection but is often used as an adjunct to immunosuppressive therapy (23). Due to its adjuvant nature, mycophenolate is the first immunosuppressive drug to be used when there is a concern of infection. Many of these drugs have harsh side effects, making long-term compliance difficult and frustrating.
Most commonly, patients on immunosuppressive medications suffer from diarrhea, headaches, tremors from the neurotoxicity risk of tacrolimus, and insomnia. In cases of neurotoxicity, the tacrolimus trough goal is lowered as much as possible, and other side effects are managed with supportive medications (Imodium, Lomotil, Melatonin). Immunosuppression regimen education is a focus of the post-transplant recovery process and should begin as early as possible.
Long-term patients require close follow-up, including weekly clinic appointments for the first several months after transplant. As they recover from the surgery, clinic appointments become less frequent, but they still require frequent lab work to assess immunosuppressive drug levels.
Ask yourself...
- What education is important to provide patients after transplant regarding their treatment regimen?
- Why are labs so closely monitored after surgery?
- Why is immunosuppressive therapy so important after transplant surgery?
- What resources should you take for patients you provide care for immunosuppressed patients?
- How can you reduce the risk of patient injury through infection control and education in a patient after transplant surgery?
Summary
Liver transplantation has come a long way since the first successful surgery 50 years ago, but patients today are facing new challenges that have yet to become medical triumphs.
The number of transplant organs continues to grow each year. In 2016, a total of 7,841 liver transplants were completed, a 10% increase from 2015 (24). As transplant medicine continues to grow, long-term outcomes improve as well. In 2016, the incidence of graft failure at one year decreased to 9.8% for recipients of deceased donor organs, a 10% reduction from 2015 (24). The three and five-year mortality rates continue to improve, especially in those who received living donor liver transplants (24).
As of June 30, 2016, there were 79,188 liver transplant patients living with a functioning graft (24), making the knowledge and care of a post-transplant patient crucial to both acute care and primary care practicing providers.
Ask yourself...
- After this course, what information have you learned that will improve the care you provide to patients?
- What resources do you have at your facility to help expand your knowledge further?
References + Disclaimer
- Farkas, S., Hackl, C., & Jurgen Schlitt, H. (2014). Overview of the indications and contraindications for liver transplantation [Journal]. Cold Spring Harbor Perspectives in Medicine, 4, 1-12. http://dx.doi.org/10.1101/cshperspect.a015602
- The Stages of Liver Disease. (n.d.). Retrieved February 12, 2019, from https://liverfoundation.org/for-patients/about-the-liver/the-progression-of-liver-disease/#1503432933768-040e8645-d918
- Watson, S. (2017, December 19). Understanding hepatitis C from diagnosis to stage 4. Retrieved February 12, 2019, from https://www.healthline.com/health/stage-4-hepatitis-c#acute-hepatitis-c
- Cunha, J. P. (n.d.). What Is Cirrhosis of the Liver? Symptoms, Treatment & Stages. Retrieved February 12, 2019, from https://www.medicinenet.com/cirrhosis/article.htm
- Martin, P., DeMartini, A., Feng, S., Brown Jr, R., & Fallon, M. (2014). Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation [Practice Guideline]. Clinical Journal of the American Association for the Study of Liver Diseases, 59(3). http://dx.doi.org/10.1002/hep.26972
- Martin, P., DiMartini, A., Feng, S., Brown, R., Jr., & Fallon, M. (2013). Evaluation for liver transplantation in adults: 2013 practice guidelines by the AASLD and the American Society of Transplantation. AASLD Practice Guideline,1-98. Retrieved February 9, 2019, from https://www.aasld.org/sites/default/files/guideline_documents/141020_Guideline_Evaluation_Adult_LT_4UFb_2015.pdf.
- Berg, C. L. (2016). Liver transplantation in 2016: An update [Invited Commentary]. NC Medical Journal, 77(3), 194-197. Retrieved from http://www.ncmedicaljournal.com/
- The Four Classes of Hep C Treatment DAAs. (2017, September 21). Retrieved February 13, 2019, from http://www.hepctip.ca/daas/
- Andrews, M. (2017, October 04). FDA’s Approval Of A Cheaper Drug For Hepatitis C Will Likely Expand Treatment. Retrieved February 13, 2019, from https://www.npr.org/sections/health-shots/2017/10/04/555156577/fdas-approval-of-a-cheaper-drug-for-hepatitis-c-will-likely-expand-treatment
- Harvoni (ledipasvir and sofosbuvir) | Hepatitis C TIP | PHCN. (n.d.). Retrieved February 13, 2019, from http://www.hepctip.ca/harvoni-ledipasvir-and-sofosbuvir/
- Liver transplants. (2016). Retrieved from http://emedicine.medscape.com/article/776313-overview
- Bambha, K., & Kamath, P. S. (2016). Model for end-stage liver disease (MELD). Retrieved from https://www.uptodate.com/contents/model-for-end-stage-liver-disease-meld#H16431598
- Questions and answers for transplant candidates about liver allocation. (2017). Retrieved from http://www.unos.org/wp-content/uploads/unos/Liver_patient.pdf
- Martin, P., DeMartini, A., Feng, S., Brown Jr, R., & Fallon, M. (2014). Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation [Practice Guideline]. Clinical Journal of the American Association for the Study of Liver Diseases, 59(3). http://dx.doi.org/10.1002/hep.26972
- Arvelakis, A., & Shapiro, R. (2013). Living donor hepatectomy. Retrieved from http://emedicine.medscape.com/article/1830182-overview#a4
- Berg, C. L., Gillespie, B., Merion, R. M., Brown, R. S., Abecassis, M. M., Trotter, J. F., … Everhart, J. E. (2007). Improvement in survival associated with adult-to-adult living donor liver transplantation [Entire issue]. Gastroenterology.
- Glass, M., Smola, S., Pfuhl, T., Pokorny, J., Bohle, R. M., Bücker, A., . . . Volk, T. (2012, September 16). Fatal Multiorgan Failure Associated with Disseminated Herpes Simplex Virus-1 Infection: A Case Report. Retrieved February 13, 2019, from https://www.hindawi.com/journals/cricc/2012/359360/
- Cotler, S. J. (2017). Living donor liver transplantation. Retrieved from https://www.uptodate.com/contents/living-donor-liver-transplantation
- Sun, Z., Yu, Z., Yu, S., Chen, J., Wang, J., Yang, C., … Zhang, M. (2015). Post-operative complications in living liver donors: A single-center experience in China. PLoS One, 10(8). http://dx.doi.org/10.1371/journal.pone.0135557
- Tebas, P. (2015). Solid organ transplantation in HIV-infected individuals. Retrieved from https://www.uptodate.com/contents/solid-organ-transplantation-in-hiv-infected-individuals#H1
- Dove, L., & Brown, R. S. (2015). Liver transplantation in adults: Patient selection and pretransplantation evaluation. Retrieved from https://www.uptodate.com/contents/liver-transplantation-in-adults-patient-selection-and-pretransplantation-evaluation?source=see_link§ionName=CONTRAINDICATIONS&anchor=H5#H5
- Razonable, R. R., Findlay, J. Y., O’Riordan, A., Burroughs, S. G., Ghobrial, R. M., Agarwal, B., … Gropper, M. (2011). Critical care issues in patients after liver transplantation [Review]. Liver Transplantation, 17, 511-527. http://dx.doi.org/10.1002/lt
- Feltracco, P., Barbieri, S., Galligioni, H., Michieletto, E., Carollo, C., & Ori, C. (2011). Intensive care management of liver transplanted patients. World Journal of Hepatology, 3, 61-71. http://dx.doi.org/10.4254/wjh.v3.i3.61
- Kim, W. R., Lake, J. R., Smith, J. M., Skeans, M. A., Schladt, D. P., Edwards, E. B., . . . Kasiske, B. L. (2018). OPTN/SRTR 2013 Annual Data Report: Liver. American Journal of Transplantation,15(S2), 1-28. doi:10.1111/ajt.13197
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
