Course
Lymphedema Management
Course Highlights
- In this Lymphedema Management course, we will learn about the pathophysiology and etiology of lymphedema.
- You’ll also learn the common signs and symptoms of lymphedema.
- You’ll leave this course with a broader understanding of appropriate assessment techniques in the evaluation of upper and lower extremity edema.
About
Contact Hours Awarded: 2
Course By:
Abbie Schmitt, MSN-ED, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Imagine the human body as a bustling city, with a complex network of roads and highways. In this city, there is a unique delivery service called the lymphatic system, which is responsible for transporting important packages and keeping the roadways clean.
The lymphatic system consists of a network of vessels, like roads, carrying a clear fluid called lymph. Lymph is like the city’s waste management team, collecting unwanted materials like bacteria, toxins, and excess fluids from the tissues. The lymphatic vessels transport this fluid to the lymph nodes, which are like security checkpoints scattered throughout the city. At these security checkpoints, the lymph nodes filter and inspect the lymph to find harmful invaders like viruses and bacteria. Important structures like the spleen act as a recycling center for old or damaged blood cells, and the thymus, where new immune cells are made.
Lymphedema is a condition in which lymphatic fluid accumulates in tissue, causing swelling. This happens when the lymphatic system is damaged or blocked, preventing the normal drainage of lymphatic fluid. This lymphatic system damage can be caused by various things, including surgery, infection, cancer, trauma, or radiation therapy. This injury to lymph nodes, such as removal or damage, is like closing lanes on the highways, and lymphatic fluid begins to back up and causes swelling in the body parts that those lymph nodes drain fluid from. Lymphedema is essentially like a disastrous traffic jam in our city comparison.
As we explore the complex lymphatic system and the development of lymphedema, we will review the pathophysiology, etiology, assessment, clinical findings, and treatment.

Definition
The lymphatic system is a complex network of lymph nodes, vessels, and organs that collect and carry lymph. This system has vital functions of immune system support, fluid balance, protein transport, absorption, and circulatory support.
Lymphedema is a persistent state of edema characterized by the failure of interstitial fluid to return to normal circulation in vessels, resulting in an accumulation of fluid and fibro-adipose tissue within extravascular spaces (5). Essentially, lymphedema is chronic swelling within soft tissue caused by lymph build-up and stasis.
Lymphedema can be characterized as primary or secondary. Primary lymphedema can be present at birth or appear later in life spontaneously or following a mild injury (e.g., bug bite, sprained wrist, arthroscopic surgery). Secondary lymphedema results from significant direct or indirect injury in a previously healthy lymphatic system

Self-Quiz
Ask Yourself...
- How is lymphedema defined and categorized?
- What are the roles of the lymphatic system in maintaining homeostasis in the body?
- How is the cardiovascular system closely linked with the lymphatic system?
- Would you consider lymphedema as a condition, symptom, or both?
Epidemiology
Lymphedema affects about 250 million people worldwide (2).
Primary lymphedema is rare, affecting about one in 100,000 adults in the United States; secondary lymphedema is more common and affects about one in 1000 adults in the U.S. (8). Older adults are diagnosed with lymphedema at a much higher rate at about five in 1000 adults over the age of 65 living (5).
The prevalence of lymphedema is widely studied in the area of oncology. One in 5 women treated for breast cancer will develop lymphedema (6). In breast cancer–related lymphedema (BCRL), younger African American women have the highest risk and highest prevalence (6).
Lymphatic and soft tissue complications and resulting lymphedema are developed in more than 90% of patients treated for cancer within the head and neck (5).
In a recent study, 37% of women treated for gynecological cancer had measurable evidence of lymphedema within 12 months following treatment. In the gynecologic oncologic population, several risk factors were identified: (1) more extensive lymph node dissection, (2) chemotherapy and radiation therapy, (3) higher body mass index, (4) insufficient levels of physical activity, (5) vulvar/vaginal cancer (5).

Self-Quiz
Ask Yourself...
- How are patients with cancer and/or cancer treatments at a higher risk for developing lymphedema?
- What are the chances a woman treated for breast cancer will develop lymphedema?
- Can you name other risk factors associated with this condition?
- Have you cared for patients with significant edema of an extremity?
Etiology
As we mentioned, primary lymphedema is an inherited or congenital condition causing abnormal structure and function of the lymphatic system, most often because of genetic mutation. Primary lymphedema can be subdivided into these categories: congenital lymphedema (present at birth or recognized within two years of birth), lymphedema praecox (occurring at puberty or the beginning of the third decade), or lymphedema tarda (onset after the age of 35) (8).
Secondary lymphedema results from damage or obstruction to a healthy lymphatic system. The leading cause is malignancy or the related treatment of malignancy (6). This includes surgical excision of lymph nodes, local radiation treatment, or oncological medication therapy. Breast cancer is the most common cancer associated with secondary lymphedema in developed countries.
Globally – lymphatic filariasis (LF), which is a parasitic infestation of lymph nodes by the parasite Wuchereria bancrofti, is the most common cause of secondary lymphedema. LF affects roughly 120 million people, disfiguring about 40 million worldwide. This type of lymphedema is prevalent in parts of India, Africa, and South America in tropical and underdeveloped countries (2). However, in developed countries, most secondary lymphedema cases are due to cancer or related cancer treatment.
Pathophysiology
A thorough understanding of normal lymphatic anatomy and how it changes in lymphoedema is crucial in effectively managing lymphedema.
The Lymphatic System
The lymphatic system is a network of specialized cells, vessels, and organs whose function is to maintain fluid homeostasis, facilitate intestinal fat absorption, and support the immune system (5).
Lymph fluid contains proteins, salts, and water, as well as white blood cells. Lymph vessels or ducts have one-way valves to transport fluid and muscle tissue helps move the fluid through the body.
Lymph nodes are small, bean-sized glands located along the lymph vessels that help filter potentially threatening substances, such as cancer cells and infections. Lymph nodes are found distributed all over the body, including the neck, axillary regions, chest, abdomen, and groin. The tonsils, adenoids, spleen, and thymus are also parts of the lymph system. Lymph tissue is also found in many other parts of the body, including the small intestine. In the average adult, more than 8 liters of lymphatic flow is generated every day (5).
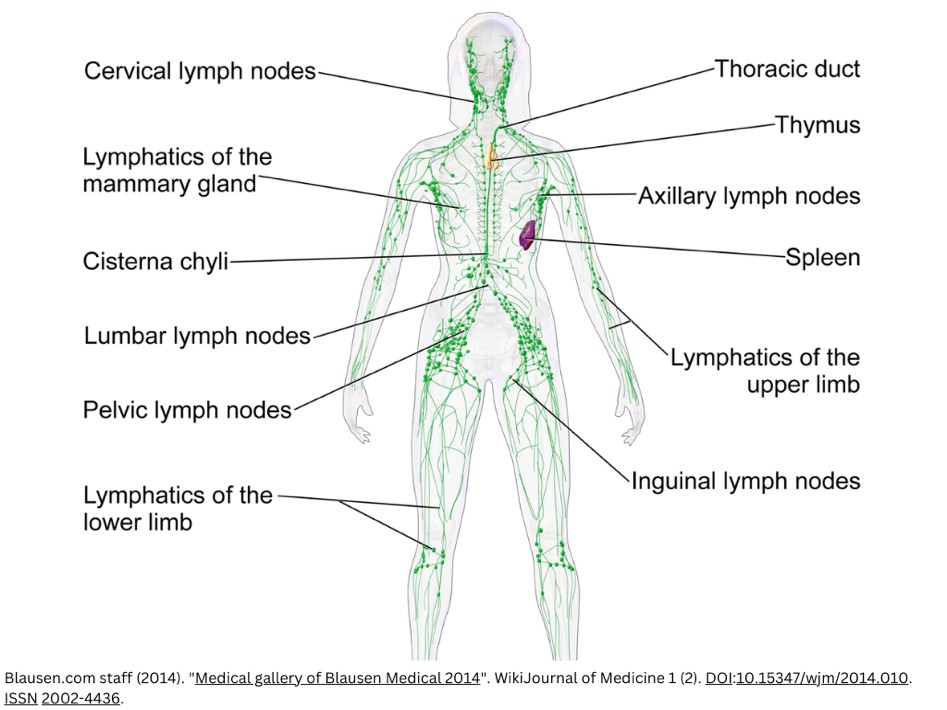
Image 1. The lymphatic system.
The lymphatic pathways are structured in two layers, comprising superficial and deep systems separated by the deep fascia (7) The superficial lymphatic system is vital to understanding the pathology of lymphedema. The superficial lymphatic system involves tiny, thin-walled vessels located just beneath the skin and are primarily responsible for draining the skin and subcutaneous tissues. These vessels absorb excess interstitial fluid, which includes waste products, toxins, and other unwanted materials. The larger vessels transport the absorbed lymph fluid from the capillaries toward regional lymph nodes, and they have one-way valves that prevent backflow and make sure it is traveling in the proper location (7). When the superficial lymphatic vessels are damaged or obstructed, they cannot effectively drain the lymph from the tissues, resulting in swelling.
In primary lymphedema, the lymphatic drainage system does not function properly due to abnormal lymphatic vessels. In secondary lymphedema, the lymphatic system reaches proper maturity; however, a physiologic injury—such as cancer, infection, radiation therapy, or inflammation—causes the dysfunction. Lymphedema can also be present in chronic overload of the lymphatic system, such as the case of phlebo-lymphedema.
Relationship Between the Lymphatic and Circulatory System
The lymphatic and circulatory systems are interdependent, working together to maintain fluid balance, transport nutrients, and support immune function. In some ways, the lymphatic system works similarly to the cardiovascular system, in that both circulate fluid (or blood) through vessels. However, the cardiovascular system has a powerful pump, the heart, that moves blood through the body; the lymphatic system does not have a pump. Instead, it relies on lymph nodes and the movement of muscles to keep fluid moving. This is why the lymph system is more likely to have poor drainage in some places, especially if lymph nodes are damaged or removed.
Considering the close relationship between the circulatory and lymphatic systems, in some patients with chronic venous disease, the lymphatic system is unable to compensate for the excess accumulation of interstitial fluid which results in lymphedema (5).
Fluid Balance. Blood plasma leaks out of the capillaries into the tissues, forming interstitial fluid, which delivers nutrients and removes waste products. The lymphatic system collects the excess interstitial fluid through lymphatic capillaries and turns it into lymph. The lymphatic system then returns this fluid to the circulatory system through the subclavian veins near the heart, which helps to maintain fluid balance.
Immune Function. The circulatory system carries white blood cells and various immune components in the bloodstream, allowing them to quickly reach sites of infection or injury. The lymph nodes filter the lymph and trap pathogens, and immune cells within the lymph nodes monitor and respond to potential threats to initiate an immune response.
The extracellular space comprises fluid rich in protein, cell debris, and immune cells that are expelled during normal vascular flow and reabsorbed by lymphatic capillaries. The reabsorbed fluid travels to lymphatic vessels from these capillaries that lead into lymph nodes. The fluid then travels from the lymph nodes back into the cardiovascular system.
Considering this significant fluid volume and the complex pathway of lymphatic drainage, it is understandable that any lymphatic disruption can lead to poor outcomes. Excess accumulation of lymph in the interstitial space causes an inflammatory cascade and progressive lymphatic dysfunction.
Imbalanced capillary filtration and improper lymphatic drainage lead to a buildup of interstitial fluid in extracellular spaces, causing edema.
Assessment
A comprehensive evaluation of patients presenting with extremity swelling is essential for accurate diagnosis and treatment. A detailed history and physical assessment are supported by multiple metrics to correctly support the diagnosis and staging.
Assessment of the lymphatic system includes inspecting the skin for signs of lymphedema. The most common sign is swelling, but other signs and symptoms may be present when the condition is severe or not well managed.
Lymphedema may be complicated by a complex interplay with insufficiency of the venous system, in particular when affecting the lower extremities, and specific imaging may be indicated for further evaluation. Measurement of the relative lymphatic fluid/adipose tissue composition is important to guide the optimal sequence of lymphedema treatment.
Lymphedema will present as upper or lower extremity edema. The assessment will expand on this finding and explore possible causes and physical abnormalities associated with the edema.
Focused History
- Cancer
- History of surgery/radiation therapy to regional lymph node basin
- Duration; time to onset
- History of cellulitis and the number of episodes.
- Treatment history and exacerbating factors.
- A thorough family history is essential if primary lymphedema is suspected. It is important to evaluate if other family members, usually from an earlier generation, suffer or have suffered from swollen feet, ankles, and legs due to an “unknown cause.”
- Injuries
- Severe burns
Patients with lymphedema will usually report that they are experiencing swelling or that their clothes or jewelry appear to be fitting tighter. This will help you to determine where to begin your assessment. During a general evaluation, observing the face, neck, arms, and legs in a sitting or supine position is appropriate. Observe the bare skin and compare bilaterally.
A focused assessment for lymphedema involves the following steps:
- Inspect for swelling and symmetry over the face, neck, arms, and legs.
- Typically, no swelling is present on the face, neck, arms, and legs, and limb circumference is equal bilaterally.
- Describe edema if present: Location, asymmetrical findings, circumference measurements
- Measure the circumference with a flat/flexible tape measure around the largest area of swelling on the affected area and measure at the same location on the opposite extremity.
- If you note swelling, assess for pitting edema: an indentation that remains after applying pressure over the location [See image 2 below].
- Inspect for skin discoloration, skin breakdown, and ulcers over the face, neck, arms, and legs. Inspect under skin folds and the bottom of the feet.
- Assess and Measure pitting/ non-pitting edema.
- Apply pressure with the pad of your finger on a distal area for about 3-5 seconds and then release.
- If you observe an indentation (a “pit”), note the location and how long the indentation remains.
- Next, repeat this in a proximal area to assess how high the edema goes
- Check with the facility you work on about the scale used to evaluate pitting edema. Scales are used to measure and record the pit depth and rebound time. Often, 1 is classified as mild, 2 as moderate, 3 as severe, and 4 as very severe.
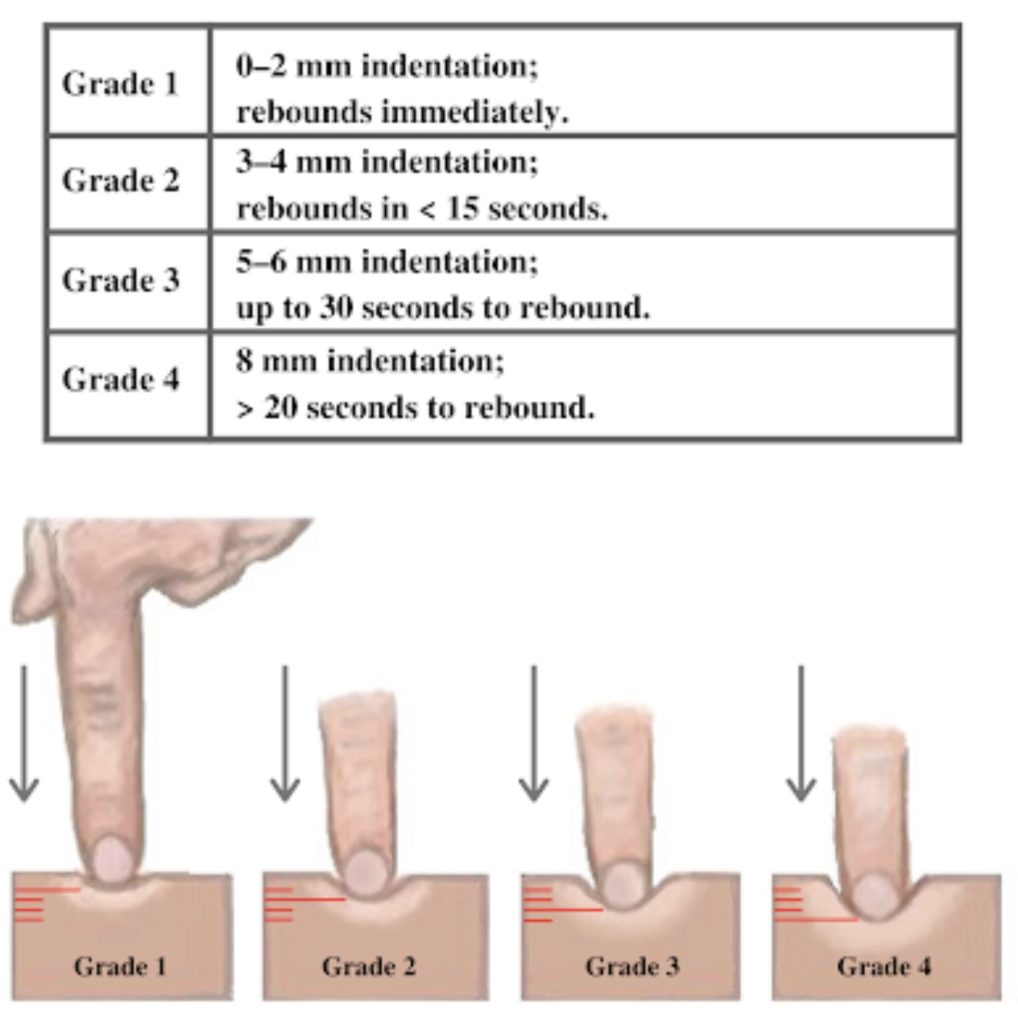
Image 2. Assessment of pitting edema (Attribution: https://wtcs.pressbooks.pub/nursingskills/ CC-BY 4.0).
- Palpate for temperature using the dorsal portion of your hands, beginning at the top of the extremities and going downward.
- Note any asymmetry in temperature or extreme temperatures, and document the location and temperature (i.e., cold or hot).
- Palpate skin texture and consistency with your first two or three fingers and thumb over the area of suspected lymphedema.
- Skin texture is typically smooth and soft with no lumps.
- Describe the quality and note the location of any dry, moist, dimpled, or firm areas on the skin.
- If you suspect lymphedema, assess the client’s mobility of the affected limb and range of motion.
- Note any difficulty moving, limited range of motion, or discomfort.
- Perform pain assessments as necessary.
- Document findings
- Example of normal findings: “No swelling or discoloration present on the face, neck, or upper and lower extremities; limb circumference is equal bilaterally. Skin temperature is warm to touch and equal bilaterally, and skin texture is smooth. No edema present.”
- Example of abnormal findings: “Redness and swelling noted on left UE, left UE circumference 18 inches and forearm circumference 10 inches. Right UE circumference 12 inches and forearm circumference 10 inches. Full range of motion of both arms.”

Self-Quiz
Ask Yourself...
- Can you describe the process of measuring pitting edema?
- Why is it important to inspect before palpation?
- How can nurses provide holistic advocacy to patients with lymphedema and severe pain?
- Why is it important to measure the circumference of both sides and not only the affected area?
Clinical Signs and Symptoms
Clinical manifestations of lymphedema include (8):
- Swelling/edema is the most notable symptom, commonly in an extremity
- Patients commonly report a feeling of “heaviness” or “tightness” in the swollen area.
- Reduced range of motion
- Pain to the affected region
- Changes in the skin
-
- Hyperkeratosis: Skin becomes scaly and thickens
-
- Lymphangioma: Small blisters on the surface of the skin
-
- Lymphorrhea: Lymph fluid leaks from the skin
- Recurrent infections
-
- Cellulitis or lymphangitis occurs due to impaired immune function in the swollen tissues.
Differential Diagnosis
Lymphedema is often misdiagnosed or undiagnosed due to its clinical resemblance to other, more common, edema-causing conditions. The differential diagnosis of lymphedema involves distinguishing it from other conditions that cause peripheral edema.
Common conditions to consider:
- Chronic venous insufficiency
-
- This condition is characterized by lower extremity swelling, varicose veins, skin changes, and ulcers.
-
- The distinguishing factors include improvement with leg elevation, the presence of varicose veins, and hemosiderin staining.
- Deep Vein Thrombosis (DVT)
-
- Signs and symptoms include a sudden onset of swelling, pain, redness, and warmth in the area.
-
- DVT can be confirmed with an ultrasound; risk factors include prolonged immobility or recent surgery.
- Congestive heart failure (CHF)
-
- In addition to extremity swelling, CHF may present with shortness of breath, orthopnea, and fatigue. Clinical evaluation and diagnostic testing can distinguish these conditions.
- Infection or inflammation (Cellulitis, erysipelas)
-
- The area would be red, hot, and painful; fever is common. Distinguishing factors include systemic signs of infection such as fever, increased white blood cell count, and positive blood cultures or wound cultures.
- Nephrotic syndrome
-
- This is related to kidney impairment and the body excreting too much protein in the urine. Generalized swelling is more common, especially in the facial area.
-
- Distinguishing factors include proteinuria, hypoalbuminemia, and hyperlipidemia.
- Drug reactions
-
- Medications can have adverse effects on peripheral edema. Examples include certain corticosteroids, dopamine agonists, antipsychotics, nitrates, nonsteroidal anti-inflammatory (NSAIDs), angiotensin-converting enzyme (ACE) inhibitors, and insulin (9).
Other conditions that may present with peripheral edema:
- Constrictive pericarditis
- Lower limb dependency syndrome
- Lipedema
- Malignancy
- Malignant lymphedema
- Postoperative complications following surgery

Self-Quiz
Ask Yourself...
- How would you describe the initial signs and symptoms of congestive heart failure?
- What are the distinguishing factors between lymphedema and kidney impairment?
- What are examples of infections that can cause swelling to the extremities?
- Are you familiar with medications that have an adverse effect of peripheral edema?
Diagnostic Imaging
Evaluation and diagnosis of edema can be quite challenging. In addition to a careful history and physical examination, imaging can often help distinguish lymphedema-related edema from other etiologies of edema. An objective evaluation of the lymphatic system is often essential to ensure an accurate diagnosis. There are newer diagnostic imaging modalities available to clinicians to help visualize the lymphatic network.
Invasive lymphangiography has been the cornerstone of lymphatic evaluation since the 1950s; however, advances in technology have led to non-invasive methods that are now more widely used (5).
Lymphangioscintigraphy is a study using nuclear medicine, in which patients receive an intradermal injection with a radionuclide isotope called technetium-99 m (5). This substance becomes visible within the lymphatic network using a gamma-ray camera to assess lymph drainage patterns (5). This diagnostic study is considered the preferred imaging modality for the initial assessment of lymphedema.
Other methods of evaluation include computed tomography (CT) or magnetic resonance (MR) lymphangiography, which allow lymph node visualization; however, MR has significant advantages: (1) it allows for the assessment of lymphatic vessels, cisterna chyli, and the thoracic duct, providing a more thorough evaluation, and (2) MR has lower levels of radiation than with CT (5).
More recently, indocyanine green (ICG) lymphography has been developed as a technique to evaluate lymphatic drainage (5). ICG lymphography uses a water-based solution that is injected into the extremity, which is then absorbed by the lymphatic vessels, and observed when infrared light is applied to the surface of the skin.
Lymphedema Staging
Staging lymphedema based on pathological changes of the lymphedematous skin and subcutaneous tissue in the affected area is based on clinical judgments (3). The International Society of Lymphology (ISL) organizes limb swelling into four stages based on skin firmness and response to limb elevation (5).
The four stages are (3):
- Stage 0
-
- “At-risk” for lymphedema due to lymphatic vessel injury, but there are no outward signs of edema.
- Stage I
-
- Mild edema is pitting and may fade with elevation of the extremity.
-
- Increased proliferation of various cell types may also occur.
-
- Reversible
- Stage II
-
- Pitting edema
-
- Edema does not improve with elevation of the extremity
-
- Formation of a large amount of subcutaneous fat and fibrosis may occur, and edema is no longer present as a depression.
- Stage III
-
- Non-pitting edema
-
- Tissue thickening, hardening, and further deposition of subcutaneous fat, and fibrosis.
- Stage IV
-
- Advanced lymphedema
-
- Also known as “elephantiasis”
-
- Diseased soft tissue hypertrophy
-
- Pitting edema
-
- Dry skin, alterations in skin character and thickness, further deposition of fat and fibrosis, and papilloma or overgrowths may be present.
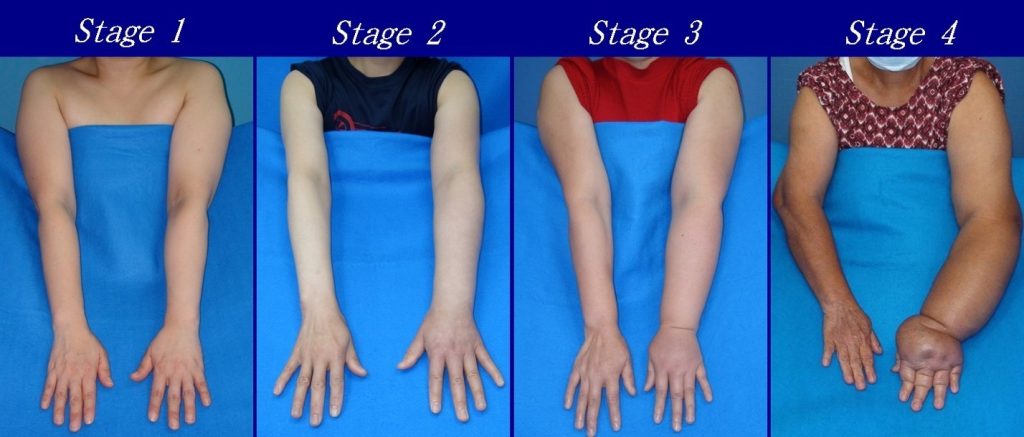 Image 3. Stages of lymphedema in upper extremity. (DocHealer, Upper limb lymphedema, CC BY-SA 4.0) Permission for use obtained.
Image 3. Stages of lymphedema in upper extremity. (DocHealer, Upper limb lymphedema, CC BY-SA 4.0) Permission for use obtained.

Image 4. Severe lymphedema in lower extremity (10)

Self-Quiz
Ask Yourself...
- Will symptoms be present in Stage 0 of lymphedema?
- Why is it important to determine the correct staging of lymphedema when creating a management plan?
- Is a CT or an MR considered to be a better diagnostic tool for visualizing lymphatic dysfunction?
- How can nurses provide patient education on the staging of lymphedema?
Treatment
Once a correct diagnosis is made, there are numerous options available to patients to help alleviate their symptoms. Lymphedema treatment should be highly individualized, considering each patient’s expectations, comorbidities, and lifestyle factors. There is often variability in what patients hope to achieve when seeking care for lymphedema (5). Common treatment goals include decreasing symptoms, finding a clear diagnosis, and preventing the disease from worsening.
Non-Surgical Management
Comprehensive Decongestive Therapy
Comprehensive decongestive therapy (CDT) is considered the standard for lymphedema management worldwide, according to the international guidelines of the International Society of Lymphology (2).
This therapy consists of the following (2):
- Manual Lymphatic Drainage (MLD)
- Skin stretching technique that stimulates the lymphatic system.
- Compression Therapy
- Layered bandaging with foam or fitted garments that support the area to control swelling.
- Exercises
- Unique exercises will help to pump lymph out of the swollen area, designed to be used with compression.
- Skin and Nail Care
- Maintaining hygiene of skin and nails to help prevent infections that often can happen with lymphedema, such as cellulitis or fungal infections.
- Self-Care Training
- Providing teaching to each patient on the management of lymphedema at home including self-bandaging or self-MLD (as needed), a thorough review of infection control practices, applying compression garments, exercises, and the importance of follow-up/review visits.
- Supporting services
- Counseling, physical therapy, and nutrition consult.
Phases of Lymphedema Treatment
- Active Phase (Phase 1)
- Mobilization of fluid.
- The gradual decrease in the proliferated connective tissue.
- The time-frame depends on the amount of swelling and tissue firmness.
- Complete decongestive therapy for one-hour sessions, 4 to 5 days per week.
- Bandages with foam are worn about 23 hours per day and often only removed to shower.
- Maintenance Phase (Phase 2)
- Maintain reduced edema and optimize connective tissue reduction
- Lasts for months or years.
- Compression garments are worn during the day.
- Bandages with foam are worn at night to decrease daily daytime swelling.
- Exercises are done while wearing compression garments.
- Self-manual lymphatic drainage is done for 20 minutes per day
Compression Therapy
A common lymphedema management tool is compression therapy. This method focuses on mobilizing and decreasing fluid accumulation in the affected limb through the application of extrinsic pressure (5).
There are numerous options available to patients. Compression garments are available over the counter or by prescription, but there is a difference in the amount of pressure the garment provides. Medical providers often start with low extrinsic compression and gradually increase strength and fit, adjusting the pressure based on patient comfort, compliance, and tolerance.
The degree of compression is measured by extrinsic pressure, traditionally measured in millimeters of mercury, mmHg. Over-the-counter options are available at less than 20 mmHg, whereas prescription strength options can range anywhere from 20 to 60 + mmHg (5).
In general, it is recommended to start with something simple like a ready-to-wear, circular knit 20–30-mmHg compression garment for mild cases and 30–40 mmHg for patients with more moderate edema. In prescription strength compression garments, custom fitting by a trained professional is vital because inadequate fit or excessive restriction can lead to worsening swelling or additional injury.
Compression garments should be worn during the hours the patient is awake, with removal at night, except custom garments which can be worn throughout the entire day and night. Custom flat-knit garments offer a superior fit and edema control for many patients. Additionally, in upper extremity edema, a gauntlet should be simultaneously worn over the hand to prevent fluid from escaping into non-compressed areas in many patients.
A second form of compression therapy is intermittent pneumatic compression (IPC), which uses a machine with an inflatable sleeve that fits over the affected extremity and delivers greater pressure to accelerate lymphatic drainage (5). It is often used in conjunction with garment-based compression.
Kinesio tape is a flexible, highly elastic adhesive applied to afflicted areas to support and stabilize muscles and joints, thereby stimulating the movement of lymph fluid with skin stretching. Patients have reported Kinesio tape as being more comfortable and convenient to use than compression garments and devices (5). However, guidelines support this is intended to be an adjunctive, not substitutive, therapy in garment-based compression.
Manual Lymphatic Drainage
Manual lymphatic drainage (MLD) can be applied during the first phase of management. Manual lymphatic drainage is a form of massage therapy that mobilizes lymphatic fluid, softens fibrotic tissue, and increases lymph drainage into functioning lymphatic vessels and venous circulation (5). These unique messages can be performed by trained professionals.
The Role of Pharmacotherapy
An important question that arises is, “is there a medication for lymphedema”? The role of effective pharmacotherapy in the management of lymphedema is limited. There is currently no medication that is routinely prescribed for non-infectious lymphedema care, but several drug therapies have been used in attempts to improve patient symptoms.
Diuretics have little role in lymphatic decongestion for primary lymphedema unless there is a comorbid condition, such as congestive heart failure (5).
In cases of infectious lymphedema due to filariasis infection, anti-parasitic agents are appropriate.
Additional Management Therapies
Light to moderate-level exercise and daily basic movement of the extremities can help decrease edema, improve circulation, strengthen muscles, and encourage lymphatic drainage. Physical therapy can also provide support in activity levels. The levels of physical abilities will vary among patients, especially those with comorbidities.
Maintaining skin integrity and hygiene is essential to decrease the chances of developing infection. Patients should be advised to avoid severe temperature extremes or procedures that risk puncturing the skin.
Surgical Management
You may hear the term debulking procedures when discussing lymphedema treatment. Debulking procedures are surgical interventions used to treat severe cases of lymphedema. This intervention is typically used only when other treatments such as compression therapy and manual lymphatic drainage are insufficient. The goal of these procedures is to reduce the volume by removing excess fibrotic and fatty tissue that accumulates due to chronic lymphedema. Liposuction is an example of a debulking procedure. Liposuction is a surgical procedure that uses a suction device to remove subcutaneous fat and fibrotic tissue.
Another type of surgical management is microsurgical procedures. Lymphovenous Anastomosis (LVA) is a microsurgical procedure that involves connecting lymphatic vessels to nearby veins to bypass the damaged lymphatic system and improve fluid drainage.

Self-Quiz
Ask Yourself...
- What therapy is considered the standard for lymphedema management worldwide?
- Can you describe the importance of compression in lymphedema treatment?
- Is there a standard pharmacological treatment for lymphedema?
- Why do you think compression therapy is often not adhered to and followed? (Example: discomfort, lack of understanding, etc.).
Patient Education
Patient education is crucial for managing lymphedema effectively.
These are key topics to provide patient education on:
- Explain what lymphedema is, the difference between primary and secondary lymphedema, and common causes.
- Educate patients on the lymphatic system and how it works.
- Teach early signs of lymphedema, including swelling, heaviness, tightness, and changes in skin texture.
- Explain the purpose and proper use of compression garments, bandages, and pneumatic compression devices.
- Describe the MLD technique, its benefits, and how it should be performed by a trained therapist.
- Provide teaching on the importance of regular physical activity to improve lymphatic flow.
- Explain the importance of maintaining good skin hygiene to prevent infections.
- Discuss the role of a balanced diet and maintaining a healthy weight in managing lymphedema.
- Encourage the support of mental health professionals or support groups.
- Explain the importance of regular follow-up appointments with healthcare providers to monitor the progression or maintenance of lymphedema.
- Educate on recognizing serious complications and when to seek immediate medical attention.

Self-Quiz
Ask Yourself...
- Have you ever placed compression stockings on a patient? If so, describe the challenges with this process.
- Can you describe the importance of infection prevention in the management of lymphedema?
- Can you name serious complications of lymphedema and why it is important to educate patients on this topic?
- Are you familiar with support groups for those with lymphedema in a local or online community?
Research Findings
Although lymphedema is somewhat prevalent and the effects are devastating, there is a lack of research on this condition and treatment options.
Research is currently being developed to evaluate pharmacological options. Animal studies have shown that vascular endothelial growth factors (VEGFs) may promote lymphangiogenesis and support lymphatic function; however, their potential for clinical application is in the early stages and there are major concerns about in-vivo effects (5). Researchers at Stanford University in Stanford, CA are currently conducting studies on a drug therapy for lymphedema (4).
Research on growth factors, anti-inflammatory, and anti-fibrotic agents has made an important expansion in this area; however, there are currently no agents that have been proven effective and safe for the treatment of lymphedema.
The Lymphatic Education and Research Network is an organization that aims to educate the public on lymphatic diseases and promote research on therapies. Several therapies are being proposed concerning inflammation and fibrosis. Surgical procedures are also being investigated for effectiveness. Vascularized Lymph Node Transfer (VLNT) involves transplanting healthy lymph nodes from one part of the body to injured areas to restore lymphatic function. Clinical trials are currently evaluating the long-term efficacy and optimal techniques for this procedure.
Another example is the development of an implantable device for lymphedema treatment. LymphoPilot is an investigational implantable medical device. The device is implanted in the subcutaneous tissue of the arm and drains excess fluids to the supraclavicular subcutaneous tissue where fluids are reabsorbed by the healthy lymphatic and venous system (4).

Self-Quiz
Ask Yourself...
- Why is research such a vital component of evidence-based care?
- How can nurses contribute to research and clinical trials?
- Can you name current studies evaluating new medications for the treatment of lymphedema?
- What are some complications associated with implantable devices?
Conclusion
Lymphedema is a chronic condition characterized by the accumulation of lymphatic fluid that causes swelling, primarily in the arms or legs. Understanding the pathophysiology, etiology, and manifestations of lymphedema is crucial for effective management and prevention of complications. Effective management of lymphedema requires a multifaceted approach involving therapy interventions, lifestyle modifications, and continuous patient education. With holistic and individualized care and support, those with lymphedema can maintain a good quality of life and minimize the risk of complications.
References + Disclaimer
- American Cancer Society. (2024). Lymphedema. https://www.cancer.org/cancer/managing-cancer/side-effects/swelling/lymphedema.html
- Gogia, S.B., Rekha, A. & Sood, S. Chronic Lymphedema Management: Case Series Analysis of 9 Years from a Specialized Clinic in Delhi. Indian J Surg 84, 597–605 (2022). https://doi.org/10.1007/s12262-021-02931-x
- Liu, N. (2021). Stage of Lymphedema. In: Liu, N. (eds) Peripheral Lymphedema. Springer, Singapore. https://doi.org/10.1007/978-981-16-3484-0_8
- Lymphatic Education and Research Network. (2024). Clinical trials and studies. Retrieved from https://lymphaticnetwork.org/treating-lymphedema/clinical-trials/
- Misra, S., Carroll, B.J. (2023). Comprehensive Approach to Management of Lymphedema. Curr Treat Options Cardio Med 25, 245–260. https://doi.org/10.1007/s11936-023-00991-8
- Ren, Y. Kebede, M.A., Ogunleye, A.A., Emerson, M.A., Evenson, K.R., Carey, L.A., Hayes, S.C., Troester, M.A. (2022). Burden of lymphedema in long-term breast cancer survivors by race and age. Cancer: An International Interdisciplinary Journal of the American Cancer Society 128 (23), 4119-4128. https://doi.org/10.1002/cncr.34489
- Schaverien, M. V., & Dayan, J. H. (2022). Multimodal management of upper and lower extremity lymphedema. Springer. https://doi.org/10.1007/978-3-030-93039-4
- Sleigh BC, Manna B. Lymphedema. [Updated 2023 Apr 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537239/
- Sinnathamby, E. S., Urban, B. T., Clark, R. A., Roberts, L. T., De Witt, A. J., Wenger, D. M., Mouhaffel, A., Willett, O., Ahmadzadeh, S., Shekoohi, S., Kaye, A. D., & Varrassi, G. (2024). Etiology of Drug-Induced Edema: A Review of Dihydropyridine, Thiazolidinedione, and Other Medications Causing Edema. Cureus, 16(2), e53400. https://doi.org/10.7759/cureus.53400
- (Image) Medical doctors (https://commons.wikimedia.org/wiki/File:Lymphedema limbs.JPG), https://creativecommons.org/licenses/by-sa/4.0/legalcode.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
