Course
Management of Digoxin Toxicity
Course Highlights
- In this Management of Digoxin Toxicity course, we will learn about the indications for digoxin and therapeutic digoxin levels.
- You’ll also learn the risk factors for digoxin toxicity.
- You’ll leave this course with a broader understanding of the symptoms of digoxin toxicity.
About
Contact Hours Awarded: 1
Course By:
Keith Wemple, BSN, R.N., CCRN, CMC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Digoxin is one of the oldest cardiac medicines still in use today. It was first derived from the foxglove plant in 1930 – a plant that is famously poisonous (1). Digoxin is a unique medication because it helps control dysrhythmias and is also a positive inotrope. This combination of effects has not been found in any other medicine to date and explains why digoxin continues to be used.
Unfortunately, digoxin also has a higher likelihood of producing toxicity than most medications. Digoxin toxicity (also called digitalis toxicity) can be life-threatening, so it is important to understand how to identify and treat this condition.

Self-Quiz
Ask Yourself...
- How often do you see patients who are prescribed digoxin?
- What do you already know about digoxin toxicity?
Digoxin Pharmacology
It is meaningful to discuss what digoxin does and how it is used. Digoxin is classified as a cardiac glycoside. It works by binding to sodium-potassium pumps in the heart (1). This results in stronger contractions of heart muscle, slower heart rate, and a reduction in AV node conduction.
For patients, this leads to improved cardiac output from stronger contractions and therefore larger stroke volumes. Slowing the heart rate and conduction through the heart also helps control arrhythmias, such as atrial fibrillation. This means that it helps prevent abnormal heart rhythms while increasing the pumping function of the heart. Other antiarrhythmic medications typically decrease cardiac output, making digoxin preferable in patients who cannot tolerate a decrease in cardiac output (2).
Unfortunately, these beneficial effects come with a risk. Digoxin has a narrow therapeutic index, meaning there is only a small margin between a therapeutic dose and a toxic dose. The therapeutic range for digoxin is just 0.8-2.0 nanograms/milliliter of blood (4). This narrow therapeutic index and the fact that digoxin has been shown to improve symptoms but not mortality has led to digoxin losing favor (1, 2).

Self-Quiz
Ask Yourself...
- What factors influence cardiac output?
- Which of these factors does digoxin treat?
- If digoxin slows AV node conduction, which arrhythmias would it not be effective for?
Digoxin Monitoring
The potential for digoxin to create toxicity requires careful monitoring of drug levels during digoxin therapy. Current guidelines recommend patients starting digoxin therapy have serum digoxin levels checked 7-10 days after starting therapy (4). While the therapeutic range of digoxin is 0.8-2.0ng/mL, newer research suggests targeting a therapeutic level of <1.2ng/mL (4).
Once a therapeutic level is established, patients should have their digoxin levels checked every 6-12 months (4). Levels should also be checked if the patient is experiencing symptoms of toxicity, or if they have a change in their renal function (4).
Digoxin undergoes little metabolism and is excreted unchanged in the urine (1). This means a decrease in renal function can easily lead to higher serum levels of digoxin at the same dose. Serial ECGs should be checked annually and when adjusting dosages or new symptoms arise (4).


Self-Quiz
Ask Yourself...
- Does your workplace have specific guidelines for monitoring digoxin therapy?
- How might medication compliance affect digoxin levels?
Risk Factors for Digoxin Toxicity
Several factors can put a person at a higher risk of digoxin toxicity. The two most important risk factors are older age and renal dysfunction. The majority of digoxin toxicity occurs in older patients, especially those with declining renal function (2). Other risk factors include hypokalemia, hypomagnesemia, hypercalcemia, dehydration, hypoxemia, and myocardial ischemia (2). A classic digoxin toxicity patient would be an older, malnourished patient who has had a decline in urine output.
Medications that can increase serum digoxin levels include amiodarone, captopril, gentamicin, erythromycin, itraconzaole, quinidine, ranolazine, telaprevir, tetracycline, and verapamil (5). Rather than trying to remember all those names, just remember that digoxin can be increased by several antibiotics, and some antiarrhythmics and blood pressure medications.

Self-Quiz
Ask Yourself...
- How often have you seen a patient prescribed digoxin and one of these blood pressure medications?
- How often do you see patients that fit the description of the classic digoxin toxicity patient?
Diagnosis of Digoxin Toxicity
A diagnosis of digoxin toxicity is based on clinical suspicion, ECG findings, and serum digoxin levels. Many of the symptoms of digoxin toxicity are vague, so they must be coupled with a thorough history.
Signs of digoxin toxicity can include gastrointestinal, cardiac, or neurological symptoms. The gastrointestinal symptoms include loss of appetite, nausea, vomiting, and diarrhea. Neurological symptoms include headache, confusion, lethargy, and vision changes such as blurred vision or seeing halos. The cardiac symptoms are related to abnormal heart rhythms, commonly bradycardia-dysrhythmias that may progress to ventricular tachycardia. These dysrhythmias affect cardiac output and lead to hypotension and/or cardiogenic shock.
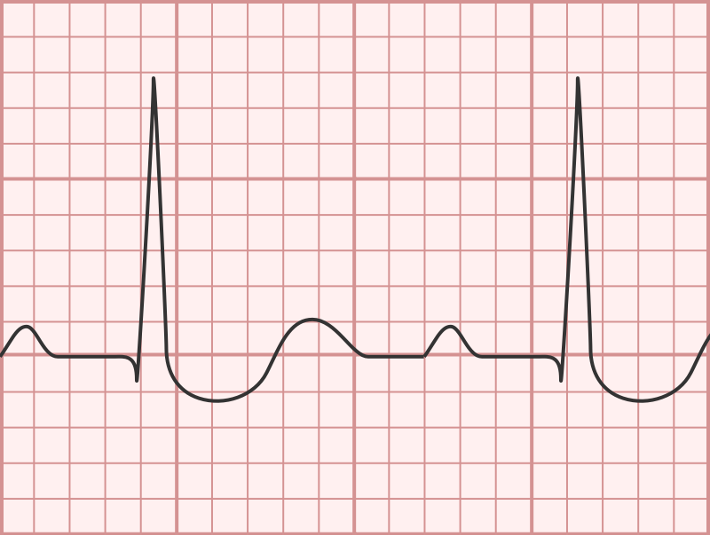
ECG findings suggestive of digoxin toxicity include ST segment depression (especially those with a scooped-out appearance), T wave flattening, U waves, and arrhythmias.
Below you can see examples of what these ECG findings look like (6):

Self-Quiz
Ask Yourself...
- What other conditions could this ECG be mistaken for?
- What other conditions could the symptoms of digoxin toxicity be mistaken for?
Treatment of Digoxin Toxicity
Treatment of digoxin toxicity includes reducing or holding the dose of digoxin, administering digoxin immune antibody fragments, and supportive care.
Reducing or holding the dose of digoxin is appropriate for patients with mild symptoms (2). Digoxin immune antibody fragments, otherwise known as DigiFab or DigiBind, are used in serious or life-threatening digoxin toxicity. DigiFab works by binding to and inactivating the circulating digoxin (3). The recommended dosing for digoxin immune fab is 1 vial (40mg) for every 0.5mg digoxin ingested in acute overdose (3). For chronic overdose, the dose is calculated with the following formula: serum digoxin concentration (ng/mL) * weight (kg)/100 = dose in vials (3). Hypokalemia is common after DigiFab administration. This typically resolves on its own, but potassium levels should be monitored closely (2).
Supportive care depends on the patient’s presentation and their heart rhythm. Unstable patients with a slow heart rate (bradycardia), should be treated with medications to increase their heart rate, such as dopamine, dobutamine, or epinephrine (2).
For patients who devolve into ventricular tachycardia, treat according to ACLS guidelines. Hyperkalemia is common with digoxin toxicity; it can be treated with diuresis, IV insulin with dextrose, and IV calcium administration (2).
While dialysis may seem tempting to treat digoxin toxicity, especially with hyperkalemia, digoxin is not cleared well by dialysis (2). Patients should have continuous ECG monitoring until their toxicity has fully resolved (2).

Self-Quiz
Ask Yourself...
- How would you access digoxin immune fab at your facility?
- How many vials of digoxin immune fab should a 100kg patient with chronic digoxin toxicity and a serum level of 4ng/mL receive?
- What piece of information can you take from this course to your daily practice?
Conclusion
Digoxin is a unique medication that can offer benefits to patients suffering from arrhythmias. However, because of its narrow therapeutic index, it requires careful monitoring. Nurses caring for patients on digoxin therapy should be aware of the signs and symptoms of digoxin toxicity. It is also important to understand the risk factors for toxicity, and the appropriate treatment should toxicity occur. Hopefully, this course has provided you with this knowledge and a new level of confidence in how to identify and manage digoxin toxicity.
References + Disclaimer
- Patocka J, Nepovimova E, Wu W, Kuca K. Digoxin: Pharmacology and toxicology-A review. Environ Toxicol Pharmacol. 2020 Oct; 79:103400. doi: 10.1016/j.etap.2020.103400. Epub 2020 May 7. PMID: 32464466.
- Andrews P, Anseeuw K, Kotecha D, Lapostolle F, Thanacoody R. Diagnosis and practical management of digoxin toxicity: a narrative review and consensus. Eur J Emerg Med. 2023 Dec 1;30(6):395-401. doi: 10.1097/MEJ.0000000000001065. Epub 2023 Aug 25. PMID: 37650725; PMCID: PMC10599802.
- Lavonas EJ, Akpunonu PD, Arens AM, Babu KM, Cao D, Hoffman RS, Hoyte CO, Mazer-Amirshahi ME, Stolbach A, St-Onge M, Thompson TM, Wang GS, Hoover AV, Drennan IR; American Heart Association. 2023 American Heart Association Focused Update on the Management of Patients with Cardiac Arrest or Life-Threatening Toxicity Due to Poisoning: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2023 Oct 17;148(16): e149-e184. doi: 10.1161/CIR.0000000000001161. Epub 2023 Sep 18. PMID: 37721023.
- Gona SR, Rosenberg J, Fyffe-Freil RC, Kozakiewicz JM, Money ME. Review: Failure of current digoxin monitoring for toxicity: new monitoring recommendations to maintain therapeutic levels for efficacy. Front Cardiovasc Med. 2023 Jul 3; 10:1179892. doi: 10.3389/fcvm.2023.1179892. PMID: 37465455; PMCID: PMC10350506.
- Food and Drug Administration, T. (2016, December 1). Lanoxin (digoxin) tablets for oral use. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/020405s013lbl.pdf
- ECG Stampede, T. (2024). Digoxin Toxicity. ECG Stampede. Retrieved April 21, 2024, from https://www.ecgstampede.com/glossary/digoxin-toxicity/.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
