Course
Mild Traumatic Brain Injury or Concussion
Course Highlights
- In this Mild Traumatic Brain Injury or Concussion course, we will learn about signs and symptoms of mild-to-moderate traumatic brain injury.
- You’ll also learn how mild-to-moderate traumatic brain injury is diagnosed.
- You’ll leave this course with a broader understanding of prevention strategies for mild-to-moderate traumatic brain injury.
About
Contact Hours Awarded: 1.5
Course By:
Elaine Enright
BSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
A traumatic brain injury or TBI is considered a major issue in the United States. It can range from a minor concussion to severe and lasting cognitive, sensory, and motor function deficits (1). Although the medical community has made many advances in treatment and prevention, still one in three deaths are caused by TBI in the U.S. (2). In this course, the nurse will gain knowledge on mild-to-moderate TBI, causes, risk factors, prevention, new treatments, and rehabilitation, as well as ongoing research for better outcomes.
Definition
“Traumatic brain injury usually results from a violent blow or jolt to the head or body” (3). A mild TBI can affect the brain by causing physical damage such as bleeding, bruising, or tissue injury (3). The amount of damage is dependent on the type of injury and how hard the blow is to the head. TBIs can range from mild concussion to severe debilitating injury and even death. This course will focus on mild-to-moderate TBI in the U.S.
Epidemiology and Statistics
As of 2010 in the U.S., the costs associated with TBI is estimated at $76.5 billion. Globally, approximately 27 to 69 million people have suffered a TBI. TBI leads to changes in the brain’s function and is caused by an external force (4). There are approximately 190 deaths each day from this injury in the U.S. and more than 214 hospitalizations in 2020 (1). In 2019, about 15% of students who play sports or are recreationally athletic have reported sustaining a sports/recreation-related mild TBI within the preceding year (1).
The highest incidence of hospitalizations for mild concussion was in the age group of 75 years or older. Emergency room (ED) visits were also high in this age group as well as for children up to four years of age (4). Motor vehicle accidents that led to hospitalizations were higher for persons aged 15 – 44 (4). From 2007 to 2013, ED visits for TBI increased by 47% while hospitalization dropped by 2.5%. Death rates also decreased by 5% (5). These lower hospitalizations may be due to better prevention measures such as motorcycle and bicycle helmets, better sport helmets and using gates at the top and bottom of stairs for toddlers (9). For the older adult, it is important to have grab bars in the shower and next to the toilet, and non-slip bathmats in the tub/shower (9).
There is a large proportion of TBIs among American Indian and Alaska Native children due to car accidents, suicides, and the inability to receive appropriate health care (9). African Americans and Hispanics are also less likely to receive rehabilitation after a TBI (9).


Self-Quiz
Ask Yourself...
- Where can you find more information on statistics of TBI?
- Why do you think hospitalizations and death rates are down for TBI?
- Which sports do you think have the highest number of TBIs?
Etiology/Causes
Any injury to the head, neck, or body can potentially cause TBI. There are two types of injury: penetrating and non-penetrating or open and closed injuries. A penetrating injury is caused by any opening in the skull from a gunshot, knife, or other penetrating item/weapon. Non-penetrating (or closed injuries) indicates that there was trauma to the head without an opening to the skull. Motor vehicle accidents, falls, and sports injuries are the cause of most closed head injuries. The force and mechanism of the blow will determine how much damage is done to the brain. The following is a list of injuries that can cause a TBI:
- Falls
- Motor vehicle accidents
- Penetrating head injuries
- Explosive blasts
- Combat injuries
- Boxing injuries
Newborns up to age four, young adults, adults over age 60, and males of all ages are at the greatest risk for TBI. In newborns and adults over sixty, falls are the most common causes of brain injury. Motor vehicle accidents can cause a brain injury because of acceleration and deceleration of the brain within the skull.

Self-Quiz
Ask Yourself...
- Where can you find more information on rates of TBI in your community?
- What may be a secondary reason for TBI in young children?
- What other actions should older people take to reduce the risk of TBI?
Pathophysiology
According to the Monro-Kellie hypothesis, the total volume in the intra-cranium should always remain constant. This includes brain tissue, blood, and cerebrospinal fluid which sits in the skull. The skull is rigid and non-expansive (11). When one of the parts of the intra-cranium is disrupted, another part must reduce its volume to prevent intracranial hypertension (11). A secondary insult to the brain can occur when this disruption takes place as the intracranial pressure (ICP) increases and the cerebral perfusion pressure (CPP) reduces, which can lead to ischemia and infarct to the brain (11).
Mild concussions or TBI occur when there is trauma to the head as in a non-penetrating blow. This typically happens when there is acceleration/deceleration as in a motor vehicle accident or a direct blow to the head (for example, with boxing) (11). If an athlete continues to play after the first mild TBI, they are at greater risk for Chronic Traumatic Encephalopathy, which can lead to “psychiatric disturbances and suicidal behavior, attention deficits and derangements in memory and executive functions” (11).
These TBI fall into several categories ranging from mild concussion to severe and ongoing deficits.

Self-Quiz
Ask Yourself...
- Where can you find more information on the Monroe-Kellie hypothesis?
- What age group is at the highest risk for motor vehicle accidents?
- Where can you find information on the different types of mild concussion?
Signs and Symptoms
In mild-to-moderate TBI, symptoms can be immediate or delayed, as in days or weeks later. The most common physical signs in mild concussion are as follows: (3)
- Headache
- Nausea or vomiting
- Dizziness or loss of balance
- Fatigue or drowsiness
- Problems with speech
There may also be sensory symptoms such as tinnitus, vision blurriness, and changes in taste and smell (3). Some symptoms of cognition, behavior, or lowered mental acuity could be brief. Loss of consciousness or being disoriented and confused can occur. The patient may be unable to concentrate or remember, have changes in their mood, feel sad or frightened, have insomnia, or find themselves sleeping more than usual (3).
In moderate brain injuries, signs and symptoms of mild concussion may be evident but may increase in time with symptoms of vomiting and nausea, loss of consciousness for minutes to hours, or a headache that may persist or worsen (3). There may be seizures, pupil dilatation in one or both eyes, weakness or numbness in extremities, drainage from ears and nose, loss of coordination, and inability to wake up from sleep (11).
In children or infants, symptoms may show up as changes in eating and sleeping habits, seizure activity, drowsiness, low interest in toys, sadness, crying, inability to console, and irritability that is more than usual (3).

Self-Quiz
Ask Yourself...
- Are you able to treat a patient with TBI (or have you ever)?
- What is the first sign/symptom you may assess in a patient presenting to the ER with a potential TBI?
- Where can you find more information on children and infant TBI?
Diagnosis
Initial assessment in TBI is evaluation of four items as listed below: (11)
- Altered mental status
- Level of consciousness
- Post traumatic amnesia
- Glasgow Coma Scale
To assess the degree of injury in a patient, providers use clinical assessment, history, and physical exams. As well, providers may test serum levels of Glial fibrillary acidic protein (GFAP) and Ubiquitin C-terminal hydrolase (UCH-L1) – two proteins that may leak from neurons and astrocytes. GFAP may be in the serum up to seven days after injury (11).
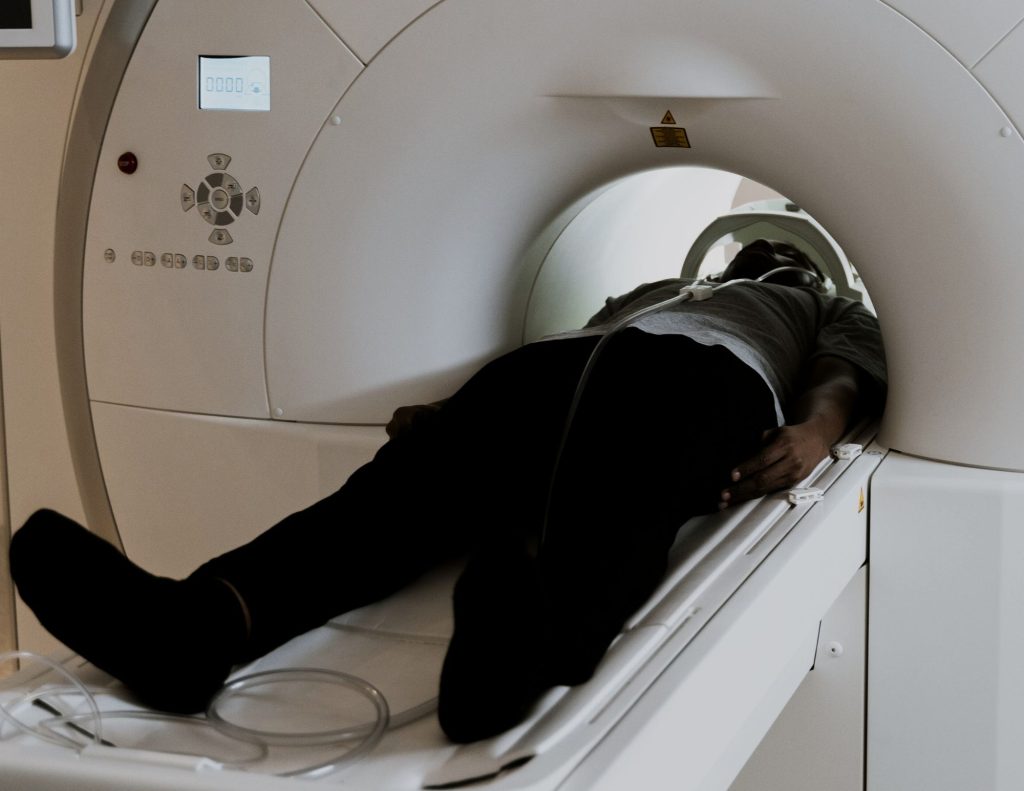
To address any anatomical or physiological changes, a magnetic resonance imaging test (MRI) and computerized tomography (CT) of the head are the first imaging used in TBI. Both are used to check for edema, bleeding, vascular injury, and intracranial pressure. To measure cerebral blood flow and brain activity, a Single Photon Emission Computed Tomography (SPECT) may be used. This imaging may be utilized to distinguish between TBI and Post traumatic Stress Syndrome (PTSD) (11).
TBI can affect the brain in several ways. TBIs may be found in one area of the brain (focal injury) or in many areas (diffuse injury) (11).


Self-Quiz
Ask Yourself...
- What is the Glasgow Coma Scale?
- How would you implement the Glasgow Coma Scale to practice?
- What would be your plan in a patient with mild-to-moderate concussion?
Treatment
There are different treatments for mild-to-moderate TBI based on the location, size of the injury, and severity of symptoms present. Treatments should be based on the individual patient. Some modalities used are physical and occupational therapy, psychological therapy, and pharmacology (9, 11). There are special support groups for patients with TBI that address family issues, financial needs, and legal concerns. Some rehabilitation can include balance training, coordination, and modalities for attention and concentration deficits (1). As a nurse, you may be involved in planning and implementing a program with the patient and family.
Again, taking into consideration symptomatology, certain medications can be used in mild-to-moderate TBI. The following list are some of the medications used: (9)
- Pain medications (over-the-counter or prescribed)
- Anticonvulsants for any seizure activity
- Anticoagulants for prevention of blood clots
- Diuretics to decrease fluid buildup, reducing pressure in the brain
- Stimulants to increase alertness
- Antidepressants and anti-anxiety medications to treat anxiety and depression
Patients with mild concussions should be educated to rest for the first few days. Once they are beginning to feel better, they can gradually begin normal activities, like taking a short walk while avoiding strenuous activities (12). Staying home from work or school may be necessary in the short term. It is important that patients stay in touch with their healthcare providers, especially if symptoms worsen or do not abate. Nurses should be aware of symptoms to assess for and evaluate if amendment of a care plan is needed.

Self-Quiz
Ask Yourself...
- How would you develop a care plan for a patient with mild-to-moderate TBI?
- Why would a patient with TBI need psychological attention?
- How would you educate a patient and/or family member on managing a TBI?
Repeated Concussions
It is well known that athletes tend to be the population that have repeated concussions. Another large group of patients with repeated concussions are military personnel serving during a war. Due to gunshot wounds and loud blast noises, many in this group have developed TBIs. Repeated concussions can cause patients to feel no symptoms. This certainly is a problem. With repeated mild head trauma, there is a chance that recovery will be longer, and the patient may have ongoing problems with concentration, headache, memory, balance, and performance of physical skills (10).
A person who has had repeated head injuries may also be at risk for developing Chronic Traumatic Encephalopathy (CTE). This syndrome can cause problems with thinking, moods, emotions, and lead to suicidal thoughts or behaviors. CTE is typically found during an autopsy of the brain. Other diseases such as Alzheimer’s disease or Parkinson’s disease may also be found. However, researchers are making attempts to diagnose CTE prior to death (10).

Self-Quiz
Ask Yourself...
- As a nurse, how would you educate a patient regarding repeated brain injury?
- Where can you find more information on CTE?
- What would your initial assessment include with multiple head injury?
Recovery
Recovery from mild-to-moderate TBI depends on the mechanism of injury and how severe that injury is. For mild-to-moderate TBI, a patient may rehabilitate in a variety of settings including the home, an outpatient rehabilitation or physical therapy office, or a short stay inpatient rehabilitation center. Each patient’s needs will be different, and the nurse should be involved in developing a plan that is best for that patient (7). The provider and the nurse will determine the discharge needs of the TBI patient. Options may include speech and language therapy, psychiatric care, bowel and bladder retraining, and social support (7).
The patient and family should be educated on instructions at discharge. Frequently, the nurse provides this education. Education should include signs and symptoms to watch for and expect, when to call the provider, how to stay safe, ways to practice self-care, alcohol and drug cessation advice, and community resources available (7).

Self-Quiz
Ask Yourself...
- What setting might be the best rehabilitation for the patient with a mild TBI?
- When would you advise the patient to call their provider?
- If you are following a patient with a mild-to-moderate TBI, how would you assess their progress?
Common Misconceptions
Since TBI is considered a “silent” or “invisible” injury, many misconceptions are circling around online. It is important that nurses demystify some of these ideas. According to an article titled “TBI: Common Myths and Misconceptions” there are at least eight myths (8). The following is a summary of the myths contained in the article.
- Myth: Concussion is not a serious injury.
Nurses know that a concussion may become serious and can in fact have long-term effects.
- Myth: A concussion is not serious if the patient does not have loss of consciousness.
We know that there can be vision changes, dizziness, disorientation, headaches, and nausea.
- Myth: A person must be hit in the head to have a concussion.
As discussed previously in this course, a patient can have an acceleration/deceleration injury in a motor vehicle accident causing the brain to shake within the hard bony skull.
- Myth: Only athletes can sustain a head injury.
TBIs can be caused by car crashes, explosions, blast injuries, domestic violence, falls, gunshot wounds, and any trauma that is physical.
- Myth: Patients with TBIs should not be allowed to go to sleep for 24 hours after the injury.
A doctor should evaluate this concern as rest and sleep are vital for a person with TBI.
- Myth: Imaging is the only way to detect a TBI.
Imaging can detect associated bleeding, fractures, and other acute trauma, but other tests must also be performed to make the diagnosis of TBI.
- Myth: TBI symptoms will worsen over time.
Symptoms are the worst at the time of injury. If symptoms last over a year, other diagnoses should be considered.
- Myth: TBI will change a person’s personality and emotions.
Emotions do not necessarily change, but personality traits remain the same as before the injury.
It is important that nurses address these misconceptions when developing a care plan and educating the patient and family after a TBI (8).

Self-Quiz
Ask Yourself...
- Where do you think these myths and misconceptions arose from?
- What other diagnoses might be present if the patient’s symptoms last longer than expected?
- What other disciplines might be involved in the care of a patient with a TBI?
Patient Education
As in any other disease or injury, patient education is crucial. The most important item to consider in a care plan is prevention. Prevention teaching may be related to general safety or discharge teaching specifically.
General Safety Education
The following are general teaching tips for safety (3):
For infants and small children, specialized car seats are required in most states. Seat belts and airbags should be in good working condition. Gates at the top and bottom of stairwells can help prevent falls in small children.
Everyone should wear helmets when bicycling, skateboarding, skating, skiing, snowboarding, motorcycling, and horseback riding. People should be aware of their surroundings and not use cell phones while walking or driving. Driving under the influence can cause motor vehicle accidents and should be avoided at all costs.
For adults and seniors, there should be handrails and non-slip mats in the bathroom and tub/shower. Area rugs should be discarded, lighting should be improved especially around stairs, and handrails should be installed on both sides of stairs.
Discharge Teaching
Discharge Instructions that should be included in an educational care plan as outlined by the U.S. Centers for Disease Control and Prevention (CDC) include: (13)
A family member or friend should know about the patient’s injury and the types of symptoms to look out for. They may notice symptoms before the patient.
A follow-up appointment with the patient’s regular doctor should be scheduled. Due to the injury, patients may need to take some time off from activities like work or school.
The patient should ask their doctor for written instructions about when they can safely return to work, school, sports, or other activities such as driving a car, riding a bike, or operating heavy equipment.
Symptoms of mild TBI and concussion are different for each person. Most people will have one or more symptoms that affect how they feel, think, act, or sleep. Symptoms may change during recovery. For example, headaches and nausea may occur immediately after the injury. A week or two after the injury, there may be different symptoms like feeling more emotional than usual or having trouble sleeping.
The nurse is most often the person who will educate the family on the signs and symptoms to watch out for and when to call the provider. Evaluation of the plan and changing the care plan may be necessary as the patient progresses.

Self-Quiz
Ask Yourself...
- Where can you find more information on developing a care plan for a patient with a mild-to-moderate TBI?
- Why is it important for a family member or friend to be available for education?
- How would you coach a patient with a TBI on initial recovery?
Conclusion
There is a plethora of information about TBI online. As we have discussed, TBI has a major impact on healthcare costs and society. We learned that some areas in the U.S. are more affected than other regions for various reasons. Patients with TBI require close and careful watching for symptoms to ensure progression towards positive outcomes. Nurses will be at the forefront as the patient recovers. We have also discussed mechanisms of injury from car crashes to falls, the severity and location of the injury in the brain, as well as resulting effects. Most important is prevention of TBI and excellent care planning for recovery.
When managing the care of the patient with TBI, it is important to keep in mind the misconceptions that people may have and educate the patient and family. At this point in time, more research is being conducted to minimize extending trauma, find quicker interventions, and develop new medications for TBI.
References + Disclaimer
- U.S. Centers for Disease Control and Prevention. (2023). Traumatic brain injury and concussion. https://www.cdc.gov/traumaticbraininjury
- U.S. Centers for Disease Control and Prevention. (2018). Reducing severe TBI in the U.S. https://www.cdc.gov/grand-rounds/pp/2011/20110920-brain-injury.html
- Mayo Clinic. (2021). Traumatic brain injury: Symptoms and causes. https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
- Williamson, C., & Venkatakrishna, R. (2023). Traumatic brain injury: Epidemiology, classification, and pathophysiology. https://www.uptodate.com/contents/traumatic-brain-injury-epidemiology-classification-and-pathophysiology
- BrainLine. (2017). Get the Stats on Traumatic Brain Injury in the United States. https://www.brainline.org/article/get-stats-traumatic-brain-injury-united-states
- Xiong, Y., Mahmood, A., & Chopp, M. (2009). Emerging treatments for traumatic brain injury. Expert Opinion on Emerging Drugs, 14(1), 67–84. https://doi.org/10.1517/14728210902769601
- John Hopkins Medicine. (2023). Rehabilitation after traumatic brain injury. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/rehabilitation-after-traumatic-brain-injury
- TBI.com. (2022). Common myths about traumatic brain injury (TBI). https://tbi.com/common-myths-about-traumatic-brain-injuries-tbi/
- U.S. Centers for Disease Control and Prevention. (2023). Health disparities and TBI. https://www.cdc.gov/traumaticbraininjury/health-disparities-tbi.html
- U.S. Centers for Disease Control and Prevention. (2023). Traumatic brain injury and Concussion: Repeated head impacts. https://www.cdc.gov/traumaticbraininjury/concussion/repeated-head-impacts.html
- Georges, A., & Das J. M. (2023). Traumatic brain injury. [Updated 2023 Jan 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459300/
- U.S. Centers for Disease Control and Prevention. (2022). Traumatic brain injury and Concussion: Getting better after a mild TBI or concussion. https://www.cdc.gov/traumaticbraininjury/concussion/getting-better.html
- U.S. Centers for Disease Control and Prevention. (n.d.). Mild traumatic brain injury and concussion: Information for adults. https://www.cdc.gov/traumaticbraininjury/pdf/TBI_Patient_Instructions-a.pdf
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
