Moisture Associated Skin Damage
Contact Hours: 1
Author(s):
Elaine Enright, RN, BS
Course Highlights
- In this Moisture Associated Skin Damage (MASD) course, we will learn about identifying when the client has MASD.
- You’ll also learn the etiology of MASD.
- You’ll leave this course with a broader understanding of how research is studying the best methods of healing.
Introduction
While skin is exposed to various challenges, such as weather, pathogens, trauma, incontinence, and excessive fluids, it acts as a natural barrier, protecting the body against these problems. In some cases, such as minor cuts, it can heal itself. However, when the skin has been exposed to copious amounts of fluid or a wound drains large amounts of exudate, another type of issue occurs and must be cared for correctly.
MASD is a serious condition that can affect several body areas. Good examples are diabetic foot wounds, decubitus that drains, incontinence, and napkin dermatitis (diaper rash) in babies. (1) This prolonged exposure to fluids damages the skin and can cause infections, including sepsis.
There is controversy about how to care for these wounds and which dressings are best. Research and studies are ongoing to discover the most effective treatment, and nurses need to understand the mechanisms and prevention of these wounds. They also need to know the type of care used in their place of work, how it is used and when, and how to educate the client and family on excellent hygiene and products to perform the care at home.
Ask yourself...
- Have you seen MASD in your practice?
- Can you recall the layers of the skin?
- Do you know of an area in your facility or town specializing in skin disease?
- What are the best practices for skin care where you work?
Epidemiology
Some of the most common diseases in the world are skin-related. These diseases are not usually fatal; however, they are very costly to society and clients. (2) Skin diseases are the 4th leading cause of non-fatal diseases, and 1/3 of the global population has some skin disorder. (2) These diseases cause much time lost from work and school, with 40% of these clients having a skin disorder, usually psoriasis. Skin disorders may manifest early systemic disease when clients have two or more comorbidities. Costs are incredibly high, with psoriasis alone estimated to be between $51.7 and $63.2 billion annually in the U.S. alone. Studies also reveal that groups of clients with skin diseases have similar comorbidities. (2) Hispanics and African Americans have a lower number of skin diseases, while those of European descent and women tend to have a higher prevalence of disease. These numbers include all skin diseases, including acne, psoriasis, eczema, vitiligo, and rosacea.
An assessment of clients in a midwestern teaching hospital was published in the Journal of Wound Ostomy and Continence Nursing on MASD. (4) The assessments showed 62 out of 1427 hospital clients, or 4.34%, had MASD, and the prevalence of incontinence-associated MASD was 22 out of 1427 clients, or 1.54%. (4) A Global Burden of Disease study (7) revealed that disability-adjusted life years (DALYs) for skin injuries, especially skin cancers, were higher among those who can travel to a sunny climate.
This study (7) suggests that the population of those clients in this category has higher incomes. The study also states that Daly’s in this research only reflects symptoms and appearance without any comorbidities or complications. (7)
Ask yourself...
- Where can you find more information on the burden of MASD?
- What types of skin disorders come to mind when you think of MASD?
- Can you determine which countries have the highest rates of this skin issue?
- How do you think the sun causes MASD?

Etiology
MASD is caused by various inflammatory and erosion injuries that damage the epithelium and change the skin’s pH from acidic 4-6 to a more alkaline pH, thereby increasing the chances of skin breakdown. It is a type of “irritant contact dermatitis” (1) with four distinct categories. (5) This skin disorder has become increasingly common as the population ages, as some elderly clients are either immobile or living alone.
Clients with MASD will experience pain, burning, and pruritus, especially if the wound has involved partial thickness damage. (1) Maceration, which can signal that MASD may occur, is described as the skin beginning to break down and appears soft, sponge-like, and white because of excessive fluid or exudate. It enhances the possibility of infection as microorganisms may enter the wound more easily. (5)
Prevention is critical in averting maceration by minimizing exudate, urine, feces, and other damaging fluids from the skin wound. (5) Once the skin is macerated, healing is prolonged, and infection can occur. (5) The epidermis layer of skin has several stratified epithelial cells that replenish over time. (6) When a wound occurs, the epithelial cells travel to the dermis to aid in healing. When excessive fluids or infection are present, it impairs the healing process. (1,5)
Healing comprises “the coordination and interaction of blood cells, various enzymes, growth factors, and extracellular matrix.” (6) The differing stages of healing are inflammatory when a clot forms, releasing cells of immunity that travel to the wound site, proliferative when keratinocytes from dermis and epidermis travel to the wound and maturational is the restoration of extracellular matrix. (6)
The four types of MASD are as follows:
- Incontinence-associated dermatitis occurs when urine or stool is on the client’s skin. It causes an alkaline environment that “disrupts skin acid mantle (8), allowing unwanted enzymes and pathogens to invade the skin, creating inflammation and erythema. This environment can mean a breakdown in the skin, which can lead to decubiti and infection if not treated early and appropriately. (8 ) This type of MASD is found mainly in older people. (1)
- Intertriginous Dermatitis (ITD) occurs when areas of skin touch each other, such as the underarms, belly folds, creases in the neck, and between toes. The client is at risk for ITD, which can develop through sweat and friction (3). It is often seen in obese clients; however, anyone who has exerted themselves in a hot climate or engaged in any activity that increases core body temperature for an extended period is prone to this issue.
- Clients with hyperhidrosis (excessive perspiration), diabetic feet, and toes are also at risk for ITD, as well as anyone with symptoms who does not receive care. Another interesting fact is that excessive lip licking or cheilitis can cause ITD, as saliva contains chemicals that irritate the lips and the outside corners of the mouth. (3)
- Case study: A client who works out 3-4 times a week and does not remove workout gear immediately post-exercise developed a rash under the breast and in the perineum. The client was initially treated with an antifungal ointment that did not work. Instead, the nurses at the provider’s office suggested using a skin barrier after changing clothes and practicing good hygiene, which helped heal the areas by protecting the skin from sweat. (3,5)
- In other situations, even a minor injury, laceration, or skin tear with excessive exudate can cause Intertriginous dermatitis.
- Peri-wound Skin Damage: Since we know that excessive wound exudate damages the skin. Peri-wound is, as it sounds, the area surrounding a wound that is also affected by excessive fluids, possibly due to increased fluids if an infection is present. (1) It presents erythema that causes pain and may affect the upper migration of skin cells from the outer edges of the wound to its base, which will delay the healing of the wound. (1)
- Although there is no agreed-upon distinct size, some scientists state that up to 1.5 inches of erythema and maceration usually surround a wound.
- Peristomal MASD: When a client has a stoma or fistula that comes through the skin, there is a chance that MASD could occur. With a tracheostomy, respiratory fluids may leak around the stoma, causing skin breakdown. Respiratory secretions are damaging to the skin if left untreated. (1,3) A study conducted by a group of wound and ostomy nurses (3) found that 10% of clients intubated and ventilated for 24 hours required tracheostomy, adding more susceptibility to MASD. (3)
- Like the tracheostomy, the skin around a gastrostomy is at risk, especially if the client has diarrhea or a fistula with an opening to the epidermis. Fecal matter is very caustic to the skin, causing erosion and maceration. (1) The biggest hurdle in caring for this MASD is keeping the skin cleansed and dry. The adhesive around a stoma may cause leakage as it becomes more saturated with fluids. (3) Also, obesity, which causes skin folds around the neck, under the breasts, and abdomen, can increase the chances of skin damage.
Ask yourself...
- Where can you find the content of different bodily fluids that damage skin?
- What type of skincare do you use at your workplace?
- Why do you think the skin began to break down in the case study?
- How can someone with hyperhidrosis care for their skin?

Management and Nursing Considerations
So, how do we manage this problem? Nurses must know how to care for a wound depending on the type and location of skin damage. The most important care is prevention. As a nurse, it is part of our assessment to do a full-body skin check on each client, especially one who is immobile or incontinent. Inspection is essential while turning the client if urine or feces are present on the skin and checking the amount of exudate around a stoma while providing care for the client. Turning the client often, especially those who cannot, and using proper hygiene, dressings, and barriers are preventive measures. With MASD, the skin may appear to have diffuse erythema, edema, papules, or scaling that contains any serous fluid. (8) Once the skin opens, bacteria and a secondary infection, such as candida (a fungus), and other pathogens may grow, complicating the healing process. (8)
An observational study of critically ill patients with fecal incontinence assessed potential risk factors. It identified factors such as liquid stool, diabetes, advanced age, smoking, non-use of diapers, fever, and low oxygen saturation as independent risks for incontinence-associated dermatitis (IAD). (9) The source of excess exudate should be determined to manage peri-wound maceration effectively. Any strategy to manage this issue must address the reasons contributing to high exudate levels that may damage the peri-wound area while also controlling the volume of exudate. (9)
Nurses are usually the first staff members to visualize skin irritation or breakdown. Since the skin’s pH is higher than normal in MASD and becomes alkaline, it is essential to use a gentle cleanser and dry the area softly and thoroughly. (1,3,8) If the skin is cleansed with an alkaline treatment, it creates more of an atmosphere for bacteria to grow. A water-insoluble or surfactant cleanser is recommended. (1,8) Skin should not be rubbed as friction is one mechanism that causes breakdown. (1,8) This cleanser eliminates bacteria on the surface and in the wound bed. After the wound is dry, the nurse should use a barrier cream (not lotion) to keep the skin from excessive fluids. (3) A moisture-absorbing dressing should be used if the wound has copious amounts of exudate. (1,3) It is also essential to use adhesives that will not stick to the wound or surrounding skin. Dressing changes must be contingent on the amount of fluid in the wound and if the client is incontinent.
An ostomy skin tool (1) was developed to assist nurses in determining the extent of damage in the client with a stoma. (1) The tool helps nurses determine a damage grade using discoloration, erosion, and tissue overgrowth. Interviewing the client to establish how the skin broke down is also helpful. (1) The Journal of Wound Ostomy and Continence Nursing (3) suggests that nurses follow a structured skin care regimen using algorithms or best practice guidelines and using the most appropriate management and products. (3)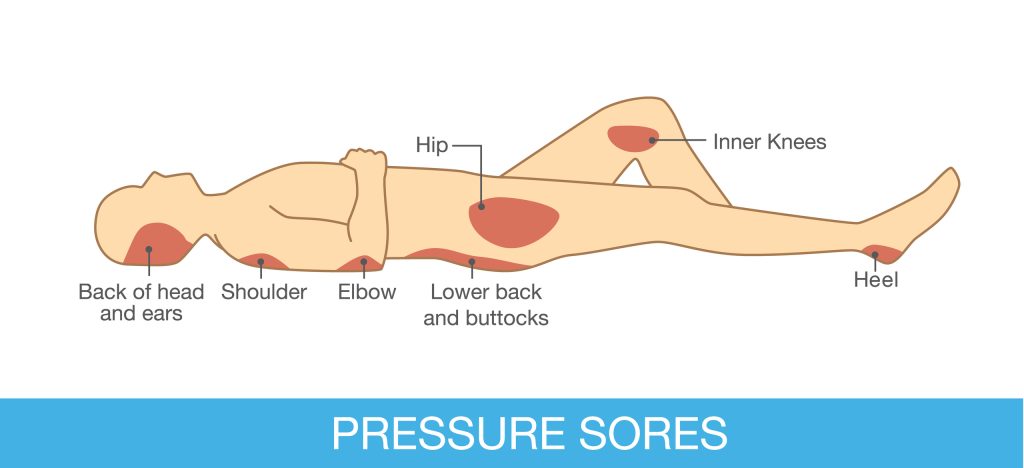
Ask yourself...
- What types of skin barriers should be utilized in MASD?
- Can you determine the types of absorbent dressings?
- Does your place of work have guidelines or algorithms for skin care?
- How can you dress a wound without adhesive bandages?
Research
Since maceration can cause pain and discomfort, research must focus on the early stages of the problem to assist nurses and other providers in preventing it. (9) Further investigation is required to assess the effectiveness of products that shield the skin from moisture, irritants, and friction. (8)
Improved consistency in documentation practices is often needed in various aspects of Moisture-Associated Skin Damage (MASD). Establishing standardization and comprehensive documentation is essential for data collection and guiding future care and research initiatives.
Additional studies are needed to validate existing and emerging technologies for managing MASD in various clinical settings and patient populations. (8)
Ask yourself...
- Can you find more ongoing research for MASD?
- How adequate is documentation on MASD in your workplace?
- Can you observe and identify the differing types of MASD?
- Have you ever cared for a patient with MASD?
Conclusion
In this course, we have examined the etiology of MASD and its four categories. We have briefly touched on the layers of skin affected and the stages of skin breakdown. Excessive exudate can destroy the epidermis and block a wound’s healing stages. Prevention is also key in caring for clients at risk for MASD by observing and determining the most effective dressings and products to use on a MASD wound. The course also discussed the maceration of the skin, what it looks like, and the associated risks that can lead to MASD. Some of these risks are diabetes, autoimmunity diseases, psoriasis, immobility, and incontinence, as well as respiratory illness needing a tracheostomy. The different types, causes, and categories of MASD were discussed.
Research is ongoing to determine the most effective skin barriers and what algorithms would help the nurse document MASD and its progression or healing. Remember to document clearly and concisely and report findings to the next nurse caring for the patient and the provider.
Ask yourself...
- What, if anything, has impressed you most about this subject?
- Will you feel able to discuss MASD confidentially with your colleagues?
- Can you find other reasons MASD may occur?
References + Disclaimer
- Woo KY, Beeckman D, Chakravarthy D. Management of Moisture-Associated Skin Damage: A Scoping Review. Adv Skin Wound Care. 2017 Nov;30(11):494-501. https://doi.org/10.1097/01.asw.0000525627.54569.da
- Li, Q., Patrick, M. T., Sreeskandarajan, S., Kang, J., Kahlenberg, J. M., Gudjonsson, J. E., He, Z., & Tsoi, L. C. (2024). Large-scale epidemiological analysis of common skin diseases to identify shared and unique comorbidities and demographic factors. Frontiers in Immunology, 14, 1309549. https://doi.org/10.3389/fimmu.2023.1309549
- Gray, Mikel; Bliss, Donna Z.; McNichol, Laurie. Moisture-Associated Skin Damage: Expanding and Updating Practice Based on the Newest ICD-10-CM Codes. Journal of Wound, Ostomy and Continence Nursing 49(2):p 143-151, March/April 2022. | https://doi.org/10.1097/won.0000000000000865
- Werth, Sherry Lynn; Justice, Rachel. Prevalence of Moisture-Associated Skin Damage in an Acute Care Setting: Outcomes From a Quality Improvement Project. Journal of Wound, Ostomy and Continence Nursing 46(1):p 51-54, January/February 2019. | https://doi.org/10.1097/won.0000000000000499
- Haryanto H, Arisandi D, Suriadi S, Imran I, Ogai K, Sanada H, Okuwa M, Sugama J. Relationship between maceration and wound healing on diabetic foot ulcers in Indonesia: a prospective study. Int Wound J. 2017 Jun;14(3):516-522. https://doi.org/10.1111/iwj.12638
- Sukmafwat, Tansil Tan et al. Lessons From Epithelialization: The Reason Behind Moist Wound Environment. The Open Dermatology Journal 31 Jul 2019 Review Article (2017) http://dx.doi.org/10.2174/1874372201913010034
- Giesey RL, Mehrmal S, Uppal P, Delost ME, Delost GR. Dermatoses of the world: Burden of skin disease and associated socioeconomic status in the world. J Am Acad Dermatol. 2021 Feb;84(2):556-559. doi: https://doi.org/10.1016/j.jaad.2020.05.157
- Fletcher J, Beeckman D, Boyles A et al (2020) International Best Practice Recommendations: Prevention and management of moisture-associated skin damage (MASD). Wounds International. Retrieved from https://woundsinternational.com/wp-content/uploads/2023/02/77ece7a46c5c084762956b97f9096e53.pdf
- Trudy Young, Director of Education and Training. Welsh Wound Innovation Center, Ynsmaerdy, Rhondda Cynon Taff, Wales. Back to basics: understanding moisture-associated skin damage Retrieved:https://www.wwic.wales/uploads/files/documents/Professionals/New%20Articles/MASD.pdf.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
