Course
New Jersey Renewal Bundle
Course Highlights
In this course we will cover a variety of nursing topics pertinent in the state of New Jersey, which are listed in the course outline below. This course is appropriate for RNs and LPNs. Upon completion of this single module you will receive a certificate for 30 contact hours.
About
Contact Hours Awarded: 30
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
New Jersey Implicit and Explicit Bias
Introduction
In OB-GYN care, biases—both implicit and explicit—can affect pain management during labor, the interpretation of patient concerns, and treatment decisions based on factors such as race, ethnicity, weight, age, or sexual orientation [1]. These biases contribute to disparities in care and can result in negative health outcomes [1]. Implicit bias stems from unconscious stereotypes, while explicit bias involves expressed discriminatory attitudes [2].
The presence of both explicit and implicit biases among maternity care providers plays a significant role in creating disparities in person-centered maternity care (PCMC) [3]. These biases can influence providers' perceptions and behaviors, leading to unequal treatment of pregnant persons during childbirth. Individuals of lower socioeconomic status (SES) often experience less dignified, less responsive care compared to those of higher SES, perpetuating healthcare inequalities [4]. Understanding the impact of these biases is crucial for addressing disparities in PCMC and ensuring that all pregnant persons receive respectful, responsive care regardless of their socioeconomic background. Implicit bias often leads to associating high socioeconomic status (SES) with positive patient traits and low SES with negative ones, contributing to inequities in the quality of care provided [5].
PCMC, defined as respectful and responsive care that honors the preferences, needs, and values of pregnant person during childbirth, has gained prominence in global health discussions [6]. Despite this focus, PCMC remains suboptimal, with significant disparities based on SES. Pregnant persons of lower SES tend to experience poorer PCMC, characterized by less dignified treatment, ineffective communication, and diminished respect for autonomy, compared to pregnant person of higher SES [7]. Disrespectful and non-responsive care, common in facility-based childbirth, deters pregnant persons from seeking institutional care, which can affect maternal and neonatal health outcomes.
Positive PCMC experiences lead to improved outcomes, including increased patient engagement, trust, satisfaction, and stronger psychosocial health [8]. Studies have demonstrated that essential components of PCMC, including birth companionship and respectful communication, are associated with favorable clinical outcomes like shorter labor duration and lower rates of cesarean deliveries [9]. Disrespectful treatment and assumptions about the cognitive abilities or cooperation of low SES pregnant person perpetuate negative healthcare experiences and reinforce community mistrust of facility-based childbirth services [3].
Both explicit and implicit biases shape these care disparities. Explicit bias reflects conscious negative attitudes or beliefs toward certain groups [2]. Implicit bias influences behavior through quick, automatic associations triggered by characteristics like appearance or SES [2].
While much of the research on healthcare provider bias has focused on racial disparities, SES bias is relevant in contexts where racial distinctions are less pronounced. In the United States, many perceive low-SES patients as less intelligent, compliant, or engaged in their health, leading to poorer care, shorter consultations, and fewer diagnostic tests [4][10]. Patients report feeling the impact of SES bias through perceived discrimination and lower quality interactions with healthcare professionals, contributing to mistrust and poorer health outcomes over time [1][4].
These outcomes emphasize the need to address both forms of bias through targeted interventions aimed at improving PCMC is those with a lower SES. Improving provider awareness and enhancing communication, respect, and responsiveness in care delivery are critical steps in reducing disparities and improving health outcomes for all pregnant persons [11].

Self Quiz
Ask yourself...
- How might implicit and explicit biases influence the perceptions and behaviors of maternity care providers toward pregnant persons of different socioeconomic statuses?
- In what ways can biases based on socioeconomic status contribute to disparities in person-centered maternity care and affect maternal and neonatal health outcomes?
- Why is it important to address both implicit and explicit biases when aiming to improve respectful and responsive care for all pregnant persons?
- How can understanding the role of socioeconomic status in healthcare biases help in developing interventions to reduce disparities in maternity care?
Bias and Stereotyping in Healthcare
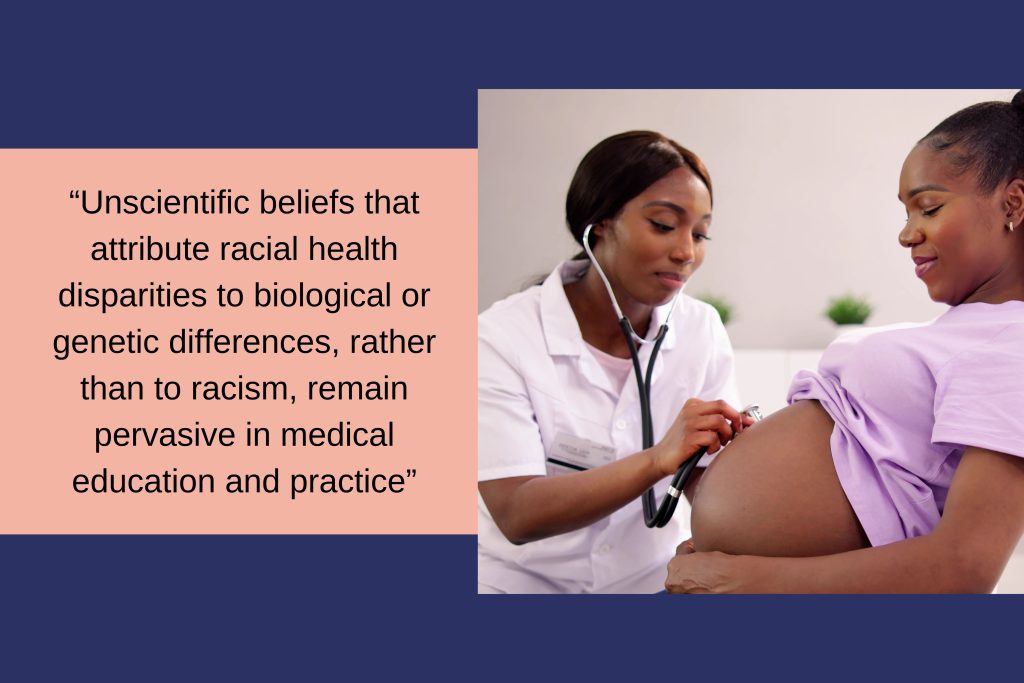
Unscientific beliefs that attribute racial health disparities to biological or genetic differences, rather than to racism, remain pervasive in medical education and practice [12]. These misconceptions, often left unchallenged at the institutional level, infiltrates treatment decisions involving race, and this harms outcomes. For instance, medical students and residents who held explicit stereotypes about Black individuals being of biological difference made less accurate pain management decisions for Black patients [13].
Within the field of obstetrics and gynecology there are significant and perpetuating such stereotypes. The unethical experiments conducted by early gynecologists like J. Marion Sims and François Marie Prevost on enslaved women, including Anarcha, Lucy, and Betsy, while resulting in advances such as vesicovaginal fistula repair and cesarean delivery, contributed to harmful racial stereotypes [14]. These experiments fostered the false belief that Black pregnant persons have a higher tolerance for pain, a stereotype that persists today and may explain why Black pregnant persons may receive epidural analgesia at a reduced rate during labor or postpartum opioids, even when pain levels are comparable [14].
This belief continues to influence modern obstetric tools and decision-making processes. The Vaginal Birth After Cesarean (VBAC) success calculator is a tool to estimate the likelihood of a successful vaginal delivery after a previous cesarean section [15]. The calculator incorporates several factors, including maternal age, body mass index (BMI), prior vaginal delivery, and notably, race or ethnicity. As a result, well-meaning clinicians practicing evidence-based medicine may provide differing counseling to White and Black patients. For instance, the calculator might predict a 66.1% chance of successful VBAC for a White woman but only 49.9% for a Black woman with identical clinical characteristics [12]. This race-based counseling can lead to different decisions—where a White woman may pursue a trial of labor, a Black woman may opt for cesarean delivery, thus contributing to unnecessary maternal morbidity and exacerbating racial disparities in healthcare.

Self Quiz
Ask yourself...
- What might be the underlying reasons that unscientific beliefs attributing racial health disparities to biological differences persist in medical education and practice?
- In what ways have historical unethical medical practices on enslaved women influenced current stereotypes and treatment approaches in obstetrics and gynecology?
- How does the use of race or ethnicity in tools like the VBAC success calculator affect clinical counseling, and what are the potential implications for racial disparities in healthcare outcomes?
Transformations in Care Delivery
The use of standardized protocols can enhance outcomes and address disparities [16]. In California, hospitals implemented a hemorrhage quality improvement collaborative that reduced Black–White disparities in severe maternal morbidity [17]. A labor induction protocol reduced racial disparities in cesarean deliveries and neonatal morbidity [28]. However, standardized protocols may also contribute to disparities. A California hospital implemented a prenatal substance use reporting protocol to child protective services, causing reports of Black mothers to occur five times more often than reports of White mothers during the study period [12]. This outcome resulted from the policy. Standardized quality improvement protocols can worsen disparities across care settings because health systems serving vulnerable populations lack sufficient resources to implement these initiatives [29].
It is important to invest in initiatives aimed at reducing Black–White maternal health disparities and to pilot test them before wide-scale implementation to prevent exacerbating inequalities. The American College of Obstetricians and Gynecologists' support of the Black Maternal Health Momnibus Act of 2021 shows how medical professionals can direct resources to underfunded healthcare systems that serve Black women, ensuring they have the necessary tools to implement and monitor quality improvements [18].
Furthermore, patients of all backgrounds should receive care based on clinical guidelines supported by reliable data. Such care can reduce or even eliminate racial disparities in certain health outcomes, as seen in ovarian cancer survival rates [19]. The Research Working Group of the Black Mamas Matter Alliance developed a research framework to ensure that Black pregnant persons participate in research teams and studies [20].

Self Quiz
Ask yourself...
- How might standardized protocols both reduce and contribute to healthcare disparities in maternal health?
- What factors and practices prevent standardized initiatives from exacerbating inequalities in vulnerable populations?
- Why is it important to pilot test health interventions before implementing them on a wide scale, especially concerning racial disparities?
- How does involving Black pregnant persons in research teams and studies contribute to more equitable healthcare outcomes?
Framework for Addressing Implicit and Explicit Bias in Maternity Care
Curriculum Design with Antiracism and Social Justice Foundations
Develop an educational framework rooted in antiracism and social justice theories. This equips learners to recognize and challenge practices within the field of care.
Bias Awareness and Management Training
Incorporate training on recognizing and managing bias throughout the curriculum. This training should focus on both implicit and explicit biases, helping healthcare providers understand their impact on patient care and outcomes.
Removal of Stereotypical Patient Descriptions
Eliminate stereotypical patient descriptions from all syllabi, case studies, and examination materials. This prevents the reinforcement of harmful biases in the learning environment and promotes equitable care for all patients.
Critical Analysis of Epidemiology and Evidence-Based Medicine
Encourage critical review of epidemiology and evidence-based medicine to identify and address assumptions rooted in discriminatory practices or structural racism. This ensures that medical knowledge does not unintentionally perpetuate stereotypes and biases.
Competency-Based Education and Holistic Evaluations
Adopt competency-based medical education and holistic evaluation methods to reduce bias in the assessment of learners. This approach emphasizes skills and knowledge over factors that bias may influence, promoting fairness in evaluation and advancement.

Self Quiz
Ask yourself...
- How can integrating antiracism and social justice theories into medical education help learners recognize and challenge existing practices in healthcare?
- What effects might removing stereotypical patient descriptions from educational materials have on the delivery of equitable patient care?
Strategies for Addressing Implicit Bias in Healthcare
To address health inequities, many U.S. states have considered or enacted laws requiring implicit bias training (IBT) for healthcare providers. California's "Dignity in Pregnancy and Childbirth Act" mandates that hospitals and birth centers offer IBT to perinatal clinicians to improve outcomes for Black pregnant persons and birthing people [21]. Gathering insights from IBT stakeholders is essential for shaping policy, developing curricula, and guiding implementation efforts.
Education on implicit bias and strategies for managing its impact should be a core component of broader health system efforts to standardize knowledge on recognizing and addressing bias. Research conducted by the Center for Health Workforce Studies at the University of Washington School of Medicine evaluated the effectiveness of a brief online course on implicit bias in clinical and educational settings. The study found that the course increased bias awareness among a national sample of academic clinicians, regardless of their personal characteristics, practice setting, or the level of their implicit racial and gender-based biases [22].
Public policy plays a key role in addressing bias in medical care and promoting racial diversity in the perinatal workforce. The federal government also plays a crucial role in addressing discrimination in healthcare. The Office of Civil Rights conducts Title VI investigations into allegations of discrimination within organizations receiving funding [23]. Legal and healthcare experts have suggested reforms to Title VI to extend these investigations to include all physician-provided services. This helps increase trust among patients, promotes diligence among physicians, and works to reduce disparities in treatment.
Beyond raising awareness, clinicians can take concrete steps to manage the impact of implicit bias in patient care. Act by engaging in role modeling; participate in training to address and interrupt microaggressions and behaviors; and undergo training to eliminate descriptions in notes and communications. Teaching faculty at academic medical centers can contribute by developing inclusive curricular materials that feature diverse imagery and examples, and by consistently using inclusive language in all forms of communication.
At the organizational level, the foundation of bias-management efforts should be a comprehensive, ongoing diversity, equity, and inclusion (DEI) education program [24]. This program should focus on interactive, skill-building education that addresses implicit bias recognition and management and should involve all employees and trainees across the healthcare system. Organizations should also collect data to track equity and monitor progress and adopt best practices for increasing workforce diversity and integrate antibias education and practices into their professionalism policies. Policies for hiring, performance review, and promotion should also give weight to candidates’ DEI contributions.
Reporting systems can further institutional efforts to manage bias. Incident-response teams can review incidents, gather information, and either refer the matter to a department, such as human resources, or conduct further investigation. Transparency is key to the process, and reporting on bias incidents, detailing affected groups, locations, and common themes. The four high-priority areas for intervention: bias in pain management, responses to microaggressions and implicit bias, biased behaviors from patients toward medical staff, and opportunities for enhancing institutional inclusivity [25]. By implementing similar strategies, both individuals and organizations can take meaningful steps toward reducing bias and promoting equity in healthcare settings.
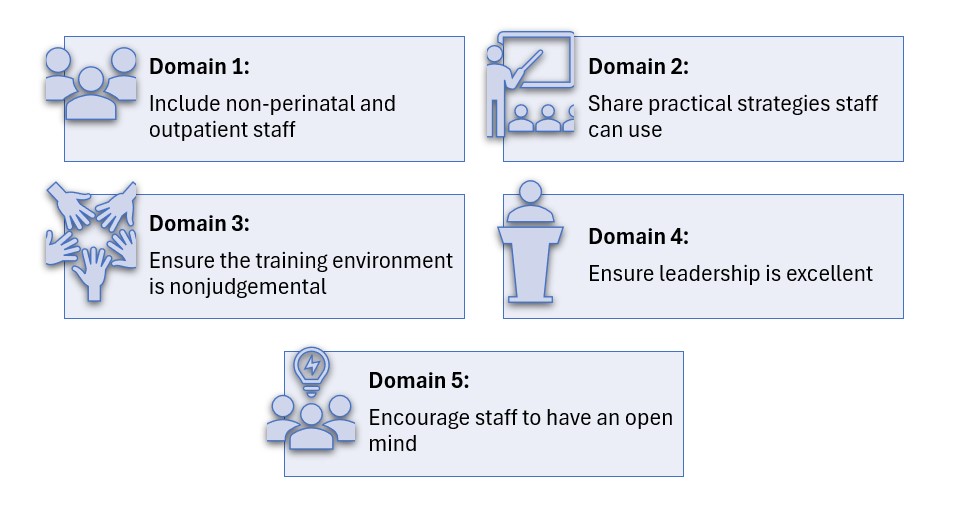
Implicit Bias Training (IBT) is a vital tool for reducing disparities in healthcare and improving patient outcomes in maternity care [26]. Effective IBT helps healthcare providers recognize and address their unconscious biases, leading to more equitable and compassionate care. The following domains outline key areas for enhancing IBT, offering practical strategies for its expansion, effectiveness, implementation, cultural integration within healthcare facilities, and fostering provider engagement.

Self Quiz
Ask yourself...
- How does mandatory implicit bias training, as required by laws like California's "Dignity in Pregnancy and Childbirth Act," impact the outcomes for Black pregnant persons and birthing people?
- Why is it crucial for healthcare providers to engage in education on implicit bias, and what effects might this have on their clinical practice and patient interactions?
- In what ways can public policy and federal initiatives, such as Title VI investigations, play a role in addressing discrimination and promoting diversity within the healthcare system?
- How can healthcare organizations implement comprehensive strategies—including diversity, equity, and inclusion programs and transparent reporting systems to manage and reduce implicit bias among clinicians and staff?
Implicit Bias Training Domains
Domain 1: Scope and Requirements of Implicit Bias Training (IBT)
Instructive Summary: To improve IBT, expand the scope to include non-perinatal and outpatient healthcare providers. Set clear guidelines on training frequency and duration, and establish accountability measures, such as penalties and standards linked to bias performance.
Domain 2: Effectiveness and Structure of IBT
Instructive Summary: For IBT to be effective, it must address systemic biases and provide practical strategies for clinicians. Use real patient stories and case studies to foster reflection and offer actionable insights for managing bias in clinical situations.
Domain 3: Implementing IBT in Healthcare Settings
Instructive Summary: Ensure successful IBT implementation by selecting credible trainers, including community members where possible, and creating safe, nonjudgmental training environments. Provide protected time, continuing education credits, and use data to assess the training's impact on clinical outcomes.
Domain 4: Healthcare Facility Culture and IBT
Instructive Summary: Leadership must demonstrate commitment to reducing bias, fostering trust, and encouraging open dialogue among staff. Implement accountability measures, such as tracking IBT participation and monitoring care quality, to ensure progress in addressing bias.
Domain 5: Provider Engagement and IBT
Instructive Summary: Providers must approach IBT with an open mind and work to recognize their own biases. Focus on engagement to prevent reactions, while understanding that even changes in behavior can improve outcomes.

Self Quiz
Ask yourself...
- How could expanding implicit bias training to include non-perinatal and outpatient providers, along with clear guidelines and accountability measures, impact the overall quality of healthcare delivery?
- In what ways might the commitment of healthcare leadership and the engagement of providers influence the success of implicit bias training in reducing disparities and improving patient outcomes?
- How do both conscious and unconscious biases among healthcare providers contribute to disparities in OB-GYN care affect treatment and outcomes for patients from lower socioeconomic backgrounds?
Conclusion
Biases contribute to disparities in healthcare [27]. Biases include attitudes and assumptions individuals recognize and report, leading to actions based on race, gender, and sexual orientation. Other biases involve attitudes related to characteristics like race, ethnicity, age, and gender, influencing judgments and behaviors without awareness. These biases operate within systems like racism and sexism, affecting patient care, medical training, workforce diversity, and career advancement [25]. Addressing both types of bias is important for achieving equity and improving outcomes.
In OB-GYN care, biases around factors like race, socioeconomic status (SES), weight, and sexual orientation impact pain management, interpretation of patient concerns, and treatment decisions. Individuals from lower SES backgrounds often receive less care, reinforcing inequalities [1]. Providers may associate high SES with certain traits and low SES with others, affecting the quality of care they provide [4]. This occurs in maternity care, where biases can lead to issues in treatment, communication, and autonomy for patients from lower SES backgrounds, affecting health outcomes [4]. Interventions that address these biases, empower patients, and hold providers accountable are important for improving maternal care and reducing disparities in outcomes.
Opioid Abuse
130 Americans die every day due to opiate overdoses. These occur from both illicit and prescribed users of opiates. In recent years, the opiate epidemic has become a mainstream health issue, and opioid abuse was brought to center stage when the President of the United States declared the opioid abuse crisis a public health emergency.
The current crisis is a combination of both licit and prescribed users, but the root of the issue remains an ease-of-access for opiate drugs and synthetics. Nurses can play a pivotal role in curbing the epidemic by being knowledgeable about opiate use disorders, the risks of opiates, and alternatives for pain control. Nurses can use the knowledge in this course help change the course of patients and reduce the risk of opioid abuse.
What are Opiates?
Opiates are powerful substances which are commonly used to alleviate both acute and chronic pain. The history of opioid abuse goes back many thousands of years. The first recorded reference is from 3,400 B.C. when opium was cultivated in southwest Asia. There were even wars fought over the previous flow in the mid 1800s (1). Perhaps the most famous historical event related to opium was the advent of “opium dens”. These were underground “dens” where opium was bought, sold, and utilized; this was a very early but concerning form of opioid abuse (1). Much like today, the addictive properties of opium overcame many individuals and caused great harm to the world and communities as a whole. Indeed, the opiate epidemic of the 2000s is not the first in modern history, though it is much different and more severe than previous epidemics.
Today, opiates are used for both acute and chronic pain. The ability to quickly, reliably, and (when used appropriately) safely reduce pain is what makes the drug class so valuable. Many common drugs are opiate derivatives or synthetics, including morphine, codeine, oxycodone, heroin, hydromorphone, and fentanyl.
In the United States, opiates are considered controlled substances and the majority of them are classified as schedule II (with heroin classified as schedule I) (2). Opiates will always have a place in medicine and treatment of pain and are incredibly useful; however, the current opiate epidemic in America makes evident the potential consequences of opiate abuse.

Self Quiz
Ask yourself...
- What prior knowledge do you have concerning opiates, and their use/misuse?
Preventing Opioid Abuse, Misuse, and Harm
Every day 190 Americans die of opiate overdose (3). Additionally, there are 4.3 million Americans each month who engage in the non-medical (non-prescribed or illicit) use of opiates (5). However, it is key to remember that opioid abuse or opiate-related deaths are not the only negative consequences. There are many overdoses which do not end in death, and on the other end of the spectrum, many negative effects do not cause death. Addiction can cause losses of employment, damage to relationships, psychological distress, homelessness, and many more negative side effects.
So, how do healthcare professionals help reduce the impact of opiate addiction and misuse? The approach must be multi-modal - aimed at primary, secondary, and tertiary prevention.
- Primary prevention includes appropriate opiate prescribing, risk stratification with patients, and generally preventing opiate addiction.
- Secondary prevention is aimed at mitigating the effects of opiate addiction. This includes rehabilitation and cessation of opiates in addicted individuals, ideally in favor of non-opiate treatment options.
- Tertiary prevention is the reduction in harm from opiate addiction and overdose. This includes resuscitation of overdose patients and helping patients recover from the effects of opiate addiction.

Self Quiz
Ask yourself...
- How do healthcare professionals help reduce the impact of opioid abuse and addiction?
Appropriate Prescribing
The Centers for Disease Control and Prevention (CDC) offers excellent guidance on how to appropriately prescribe opiates, though it will continue to require a great deal of knowledge and effort from individual prescribers and managers of chronic pain. For the purpose of this article, we will focus on CDC recommendations. Below we will discuss the 12 key points of opiate management, per the CDC.
Opioids Are Not First-Line Therapy
“Nonpharmacologic therapy and nonopioid pharmacologic therapy are preferred for chronic pain. Clinicians should consider opioid therapy only if expected benefits for both pain and function are anticipated to outweigh risks to the patient. If opioids are used, they should be combined with nonpharmacologic therapy and nonopioid pharmacologic therapy, as appropriate“ (5).
Author’s Input
Many patients experience pain. Pain is indeed one of the most common complaints in primary care offices. When dealing with chronic pain, we should consider ALL non-opiate therapies for patients prior to prescribing opiates. This can include physical therapy, meditation, exercise / movement, treatment of underlying depression and/or psychiatric issues, meditation, modification of aggravating factors, and many more interventions. In some cases, none of these alone or combined will be enough to provide satisfactory relief, but we must utilize non-opiate and non-pharmacological solutions as much as possible to reduce opioid abuse, and dose (if opiates are necessary).
Establish Goals for Pain and Function
“Before starting opioid therapy for chronic pain, clinicians should establish treatment goals with all patients, including realistic goals for pain and function, and should consider how opioid therapy will be discontinued if benefits do not outweigh risks. Clinicians should continue opioid therapy only if there is clinically meaningful improvement in pain and function that outweighs risks to patient safety“ (5).
Author’s Input
Many patients erroneously believe that cessation of pain is the goal of therapy. This is not based on fact nor is it reasonable, as many patients (even with opiate therapy) will not have complete remission of pain. The goal of the clinician should be to work with the patient to provide minimal risk intervention that will provide acceptable pain control.
Discuss Risks and Benefits
“Before starting and periodically during opioid therapy, clinicians should discuss with patients known risks and realistic benefits of opioid therapy and patient and clinician responsibilities for managing therapy” (5).
Author's Input
A prescription for an opiate should never be written to a patient without a thorough discussion of risks and benefits. The clinician must first be convinced that the risk to benefit favors prescribing an opiate. Then, the clinician must discuss rationale with the patient. An individual assessment regarding the risks should be provided to each and every patient.
Prescribe Immediate-Release Opioids First
“When starting opioid therapy for chronic pain, clinicians should prescribe immediate-release opioids instead of extended-release/ long-acting (ER/LA) opioids” (5).
Author's Input
Extended-release opioids have been associated with higher rates of overdose and higher potential for opioid abuse. Immediate-release opioids should be utilized first, whenever possible.
Use the Lowest Effective Dose
"When opioids are started, clinicians should prescribe the lowest effective dosage. Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual benefits and risks when considering increasing dosage to >90 MME/day, and should avoid increasing dosage >90 MME/day or carefully justify a decision to titrate dosage to >90 MME/day." (5).
Author’s Input
The clinician must keep in mind that the “minimum required dose” may change over time. As a patient implements more non-pharmacologic interventions, the required dose may decrease. Conversely, there can be some degree of tachyphylaxis with opiates and the required dose may therefore increase. Dose titration requires careful judgement on the part of the prescribing clinician.
Prescribe Short Durations for Acute Pain
"Long-term opioid use often begins with treatment of acute pain. When opioids are used for acute pain, clinicians should prescribe the lowest effective dose of immediate-release opioids and should prescribe no greater quantity than needed for the expected duration of pain severe enough to require opioids. Three days or less will often be sufficient; more than seven days will rarely be needed” (5).
Author's Input
It is well established that chronic opioid therapy is not the most effective therapy for pain management. Clinicians should consider adjuncts for ongoing or chronic pain patients.
Evaluate Benefits and Harms Frequently
“Clinicians should evaluate benefits and harms with patients within 1 to 4 weeks of starting opioid therapy for chronic pain or of dose escalation. Clinicians should evaluate benefits and harms of continued therapy with patients every 3 months or more frequently. If benefits do not outweigh harms of continued opioid therapy, clinicians should optimize other therapies and work with patients to taper opioids to lower dosages or to taper and discontinue opioids” (5).
Author’s Input
Is it important that clinicians consider changing circumstances. A patient’s health status or life circumstances may change such that opiate therapy benefits no longer outweigh the harm, or vice-versa.
Use Strategies to Mitigate Risk
"Before starting and periodically during continuation of opioid therapy, clinicians should evaluate risk factors for opioid-related harms. Clinicians should incorporate into the management plan strategies to mitigate risk, including considering offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, higher opioid dosages (≥50 MME/day)” (5).
Author's Input
Naloxone therapy should be considered for all patients who are at high risk of opioid overdose.
Review Prescription Drug Monitoring Program Data
“Clinicians should review the patient’s history of controlled substance prescriptions using state prescription drug monitoring program (PDMP) data to determine whether the patient is receiving opioid dosages or dangerous combinations that put him or her at high risk for overdose. Clinicians should review PDMP data when starting opioid therapy for chronic pain and periodically during opioid therapy for chronic pain, ranging from every prescription to every 3 months” (5).
Author's Input
Each state has robust data regarding prescription medication; utilizing this data can help reduce opioid misappropriation and concurrent prescriptions ("doctor shopping").
Use Urine Drug Testing
"When prescribing opioids for chronic pain, clinicians should use urine drug testing before starting opioid therapy and consider urine drug testing at least annually to assess for prescribed medications as well as other controlled prescription drugs and illicit drugs.” (5).
Author’s Input
The author recommends that clinicians take great care in this area. Indeed, drug testing can help identify those who are already abusing other substances, but it can also harm the trusting relationship developed between a patient and clinician. The patient should be re-assured that the testing is performed for their own good and out of concern for their own health, rather than punitively or because the clinician “mistrusts” them, as these may be the default thoughts of many patients.
Avoid Concurrent Opioid and Benzodiazepine Prescribing
"Clinicians should avoid prescribing opioid pain medication and benzodiazepines concurrently 'whenever possible' "(5).
Author's Input
The highest risk of overdose of opioid abuse is commonly seen when opiates and benzodizepine (or any combination of sedating medications) are prescribed concurrently, especially in conjunction with alcohol. For this reason, clinicians should strongly consider avoiding such risks and only prescribe this combination when absolutely necessary.
Offer Treatment for Opioid Abuse Disorder (OAD)
"Clinicians should offer or arrange evidence-based treatment (usually medication-assisted treatment with buprenorphine or methadone in combination with behavioral therapies) for patients with opioid abuse disorder” (5).
Author's Input
In acute cares settings, clinicians often view OAD as a secondary illness and frequently leave it unaddressed. However, there are now effective treatments for OAD. Given the significant morbidity, mortality, and associated quality of life issues arising, patients with OAD should be offered treatment, even if it not the primary reason for treatment.
Nurses' Responsibility
As a nurse treating patients, it is your responsibility to advocate for the patient’s best interests. Nurses can intervene at any juncture in a patient’s care to advocate for appropriately prescribed opiates.

Self Quiz
Ask yourself...
- What are the risks of using drug testing when assessing whether or not opioid abuse is occurring?
Risk Factors for Opioid Abuse, Opiate Harm or Misuse
The risk to benefit has been discussed many times previously and is frequently referenced by the CDC. The benefits of opiate therapy are typically obvious (reduced pain, increased quality of life, etc.), but the risks are less often discussed. So how do nurses know who is at higher risk of the negative effects of opiates?
According to the CDC, the major risk factors are:
- Illegal drug use; prescription drug use for non-medical reasons.
- History of substance use disorder or overdose.
- Mental health conditions (ergo depression, or anxiety).
- Sleep-disordered breathing.
- Concurrent benzodiazepine use (6).
Mortality rates from opioid abuse are highest in those who are middle-aged, have psychiatric conditions, and/or have previously abused substances (7). It is important that clinicians utilize this information when considering risks and benefits associated with opiate therapy. (See the CDC's Drug Overdose Deaths page for current mortality rates).

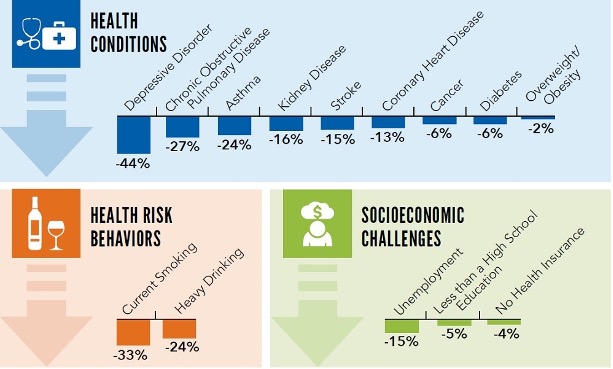
Image source: CDC

Image source: CDC

Self Quiz
Ask yourself...
- Analyzing the graphic data included in this course, how has opioid abuse changed over time?
- Why do you think that deaths have been trending downward?
- In what ways does community nursing play a part in reducing the number of opioid overdoses?
Signs of Opioid Abuse, Diversion, and Addiction
Clinicians should remain vigilant for signs of opioid abuse disorder, as it can occur in any patient (even those not prescribed opiates). Opiate use disorder is characterized in the DSM-5 as a desire to utilize opiates despite social and professional consequences (12). It includes dependence and addiction, with addiction being on the severe end of the spectrum (12). Opiate use disorder can be diagnosed when at least two of the following are observed in a 12-month period:
- Opioids are often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control opioid abuse.
- A great deal of time is spent in activities necessary to obtain the opioid, use the opioid, or recover from its effects.
- Craving, a strong desire, or urge to abuse opioids.
- Recurrent opioid use resulting in a failure to fulfill major role obligations at work, school, or home.
- Continued opioid abuse despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of opioids.
- Important social, occupational, or recreational activities given up or reduced because of opioid use.
- Recurrent opioid use in situations in which it is physically hazardous.
- Continued opioid use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance.
- Exhibits tolerance (discussed in the next section).
- Exhibits withdrawal (discussed in the next section) (13).
Urine drug screening can be useful in patients with suspected opiate abuse disorder as it may identify concurrently abused substances. If a patient is identified as having opiate abuse disorder the “risk” side of the “risk-to-benefit” equation is now shifted, and the continued use should be carefully weighed against the potential for negative effects, including addiction. Addiction is defined as continued substance use despite adverse events or consequences (12).
For those prescribed opiates, clinicians should have candid conversations about the risks of continued use for those with OAD. The CDC offers some creative examples of how to discuss the condition with patients, which nurses may find helpful in their interactions. (Below are only examples; the wording depends on the exemplifying patient's specific scenario and needs):
"Trouble controlling the use of opioid medication makes it unsafe, and long-term risk over time is substantial."
"The medicine has become a problem in itself. You have developed a known complication of therapy that we should not ignore."
"Continuing the current medication is not a reasonable option due to the risks, but there are options for treating what we call opioid use disorder, also known as OUD."
"It seems as if you are running out of your medication more quickly than anticipated."
"Sometimes people become too comfortable with the medications and start to take them for reasons other than pain."
"You meet the criteria for opioid use disorder, also known as OUD. It's helpful to put a name on it because it opens up a variety of approaches to help with your specific circumstance." (All derived from source 13).
Once a nurse identifies a patient with OAD, what should be done? At this point, as above, a candid conversation with the patient must occur. Then, a treatment plan should be formulated, which would include a careful consideration for discontinuing the opiate (if feasible). This provides an excellent transition into our next section, opiate alternatives.

Self Quiz
Ask yourself...
- Once a patient is identified with opioid abuse disorder (OAD), what are the next steps?
- What is your facility’s policy if you suspect a nurse of diversion?
- Have you ever had to report someone for concerns of diversion? If so reflect on your experience.
Opiate Alternatives
Opiate alternatives can be broadly classified as pharmacologic and non-pharmacologic. We will first discuss pharmacologic alternatives.
Pharmacologic
Acetaminophen
Commonly known as Tylenol™. Tylenol™ is an over-the-counter drug and has a very favorable safety profile when utilized correctly. Acetaminophen is considered first-line therapy in any pain management regimen (9).
NSAIDS
NSAIDS can be very powerful in pain management, as many pain conditions are related to inflammation. However, patient tolerance can be an issue with chronic NSAID exposure. Indeed, many clinicians shy away from NSAIDS due to the perceived risk profile (9).
Tricyclic Antidepressants (TCAs)
Tricyclic Antidepressants (TCAs) provide significant pain relief to many patients, as they have the unique ability to modify the perceptions of pain (5). However, tricyclics have many side effects of their own and thus have been generally phased-out in lieu of newer antidepressants. Thus, in the pain realm, they should be considered for certain patients - particularly those with concurrent untreated depression.
SSRI Antidepressants
SSRIs are typically tolerated better than tricyclics (9) but again are not recommend for first-line analgesia. SSRIs are typically reserved for those with concurrent psychiatric illness which may benefit from the overall effect of the drug, and on a case-by-case basis for select patients.
Muscle Relaxants
Medications such as gabapentin can be very useful especially in pain originating from musculoskeletal causes. However, the mechanism of action is poorly understood (9) and side effects can be troublesome. In one study, approximately 25% of patients taking muscle relaxants for chronic pain discontinued the agents due to adverse effects.
Topicals
Many topical agents now exist, including NSAIDS (9). Topicals are typically considered analgesic-sparing rather than standalone treatment (9). The American College of Rheumatology has excellent and detailed guidance on how to utilize topicals, which deserve a course of their own.
Corticosteroids
Corticosteroids have very potent anti-inflammatory effects (9) and have a proven role in pain management. Short-term therapy is typically favored over long-term therapy due to the potential issues of long-term systemic therapy (osteoporosis, immunosuppression, risk of serious or fatal infections, weight gain, muscle weakness, diabetes, Cushing’s syndrome, hypertension, glaucoma and cataracts). Though some serious adverse events can occur with short-term therapy (psychosis, anxiety, avascular necrosis, etc.) (9). Corticosteroids can be beneficial for patients with acute pain. Perhaps the best use of these agents is in targeted (injectable) delivery.
Non-Pharmacologic
These therapies will be discussed less in depth, as they typically require referrals for treatment. However, it is important that nurses are aware of the existence of these therapies, and are able to make appropriate referrals and recommendations. Physical therapy consults are invaluable as they often utilize many of the tools below and offer more knowledge about non-pharmacologic therapies in general:
- Psychological interventions (including distraction, stress management, hypnosis, and other cognitive-behavioral interventions),
- Acupuncture and acupressure,
- Transcutaneous electrical nerve stimulation,
- Physical therapies (including massage, heat/cold, physiotherapy, osteopathy, and chiropractic). (10).
Use of these methods could help reduce opioid abuse.

Self Quiz
Ask yourself...
- What key things can you take away from this article that can help you address opioid abuse in our nation?
- What are 3 interventions that you can assist in the prevention of opioid abuse?
- Have you used any of these alternatives when preparing care for clients with chronic pain?
- What kinds of documentation do you utilize when administering alternative options for the management of pain?
- Have you seen an increased use of non-pharmacological pain interventions or a decrease in your facility?
Conclusion
Nurses should view non-pharmacologic therapies as “tools” available to help patients dealing with acute and chronic pain. Though opiate therapy is a valuable tool as well, its potential negative effects are often under-considered, and the rate of opiate prescription currently is excessive, which can lead to opioid abuse (10).
When evaluating patients with pain, nurses should work with patients and providers to ensure that the patient is on an optimal pain regimen, which ideally should include both pharmacologic and non-pharmacologic therapies. Seeking referral and consultation from relevant professionals can also be very powerful in pain management (physical therapists, chiropractors, psychiatrists, etc.).
Organ and Tissue Donation
Introduction
Doctor Joseph Edward Murray performed the first successful human kidney transplant on December 23, 1954, in Boston, Massachusetts [1]. This groundbreaking procedure took place between identical twins, and it enabled the recipient twin to live an additional eight years. Over the years, transplant milestones have included the first simultaneous kidney/pancreas transplant in 1966, the first liver transplant in 1967, and the first heart and lung transplants in 1981 [2].
According to the United Network for Organ Sharing (UNOS), the U.S. achieved over 42,800 transplants in 2022 alone, marking 1 million total transplants as of September 2022 [3]. There are over 103,924 individuals waiting for transplants, with kidneys being the most needed organ [4]. Each day, 20 people die waiting for a transplant with a single donor having the capacity to save up to eight lives and affect over 50 more by donating organs and tissues [4].
In the United States various regulations and guidelines govern organ donation. The National Organ Transplant Act (NOTA) of 1984 established the Organ Procurement and Transplantation Network (OPTN), managed by UNOS under federal contract [5]. This organization oversees organ allocation policies, data collection, and educates both the public and healthcare professionals.
The Centers for Medicare and Medicaid Services (CMS) ensure hospital compliance with U.S. donation programs, while The Joint Commission requires hospitals to maintain agreements with organ procurement organizations and follow specific donation procedures [6].
UNOS also coordinates the matching of donors with recipients, prioritizing based on medical urgency, tissue compatibility, waiting times, and geographical factors, with special consideration for pediatric patients and previous living donors who are experiencing organ failure [7].


Self Quiz
Ask yourself...
- Considering the historical advancements in organ transplantation since the first successful kidney transplant in 1954, how do you think the ethical considerations surrounding organ donation have evolved in response to technological advancements and increasing demand for organs?
- Given the strict regulations established by the National Organ Transplant Act and the critical role of the Organ Procurement and Transplantation Network (OPTN) in managing organ allocations, what are the potential ethical dilemmas that might arise from prioritizing organ recipients based on medical urgency, tissue compatibility, waiting times, and geographical factors?
Becoming a Donor
Organ transplantation is a critical medical procedure that transfers a healthy organ from one individual to another and can occur either during the donor's lifetime or after their death. The collections of organs from deceased donors occurs after the declaration of brain-death—a permanent cessation of all brain activity—or following cardiac death, when heart and respiratory functions stop due to severe cardiac issues [9].
In 2019, the American Academy of Neurology (AAN) supported this by affirming that brain death constitutes the irreversible loss of all functions of the entire brain and is equivalent to circulatory death [10].
Individuals interested in becoming organ donors can register through online platforms, local Department of Motor Vehicles (DMV) offices, or via voter registration cards, as state regulations allow. This registration serves as legal consent for organ donation, followed by a medical evaluation to ensure the suitability of the donor’s organs for transplantation.
Donatable organs and tissues include the heart, heart valves, kidneys, liver, lungs, pancreas, intestines, corneas, skin, veins, bone, and bone marrow. Living donors can donate kidneys, parts of their liver, lungs, intestines, or bone marrow [4]. According to the Health Resources & Services Administration (HRSA), kidneys are the most transplanted organ [4].

Self Quiz
Ask yourself...
- How does the concept of brain death, as supported by the American Academy of Neurology, influence the ethical justification for organ transplantation from deceased donors?
- Given the various avenues for registering as an organ donor—such as through DMV offices, online platforms, or voter registration cards—what are the potential ethical and privacy concerns that might emerge from these methods?
- Considering that kidneys are the most transplanted organ, what factors might contribute to the high demand for kidney transplants compared to other organs?
Determination of Brain Death/Death by Neurologic Criteria
The process to determine Brain Death or Death by Neurologic Criteria (BD/DNC) requires a thorough clinical examination that verifies the absence of neurological function, evidenced by coma, brainstem areflexia, and apnea. The specific clinical indicators include: (1) no arousal or awareness in response to strong external stimuli such as visual, auditory, or tactile pain; (2) pupils that are midsize or dilated and do not respond to light; (3) no corneal, oculocephalic, or oculovestibular reflexes; (4) lack of facial movement in reaction to painful stimuli; (5) no gag reflex upon stimulation of the back of the throat; (6) absence of a cough reflex when performing deep tracheal suctioning; (7) absence of brain-mediated motor responses to painful stimulation of the limbs; and (8) no spontaneous breathing when apnea testing results in a pH below 7.30 and a Paco2 of 60 mm Hg or more [11].
Healthcare professionals and nurses give special considerations to certain groups including children, individuals undergoing extracorporeal membrane oxygenation, patients experiencing therapeutic hypothermia, and factors related to religious, societal, and cultural norms [11].

Self Quiz
Ask yourself...
- Considering the stringent criteria required to determine Brain Death or Death by Neurologic Criteria (BD/DNC), what are the ethical implications of misdiagnosing brain death due to the subtleties or variations in these clinical indicators?
- Given the special considerations required for certain groups like children, individuals on extracorporeal membrane oxygenation, and patients under therapeutic hypothermia, how should healthcare professionals balance the urgency of organ procurement with the need to ensure comprehensive and individualized patient care?
The Nurse's Role in Organ and Tissue Donation
Nurses are a foundational component of the organ and tissue donation process. Their roles extend beyond clinical duties to encompass emotional support, educational advocacy, and participation in multidisciplinary teams [12]. Their involvement is critical at every stage, ensuring that they oversee both the technical and human aspects of the donation process with care and expertise.
A significant part of a nurse's role involves ensuring that the family is well-informed about the brain death diagnosis, what it means, and the processes involved in organ donation [14]. This role is crucial as it often helps families understand and accept their loved one's condition, facilitating their decision about organ donation.
Nurses are vital in guiding patients and their families through this complex journey by providing detailed education on what to expect before, during, and after the surgery [14]. They explain the surgical procedures, potential risks, and complications, and address any concerns the patient or their family might have, including dispelling myths about the extensive recovery process.
Nurses also advocate for better educational programs to inform both the healthcare team and the public about the importance of organ donation. They work towards enhancing the understanding of organ donation's impact, thereby increasing participation in donation programs. This advocacy is crucial for shifting public perceptions and improving the rates of organ donations [13].
Nurses are key connectors between hospitals, organ procurement organizations, physicians, and families of potential donors. Their attitudes and knowledge impact the success of the donation process [13][15]. Along with other healthcare providers, Nurses help identify patients who are brain dead or nearing brain death due to severe medical conditions and in order of frequency: cardiopulmonary arrest, traumatic brain injury, subarachnoid hemorrhage, and intracerebral hemorrhage [16].
Nurses are responsible for informing the Organ Procurement Organization (OPO) about all potential donors, and it is the OPO's duty to assess whether these individuals qualify as potential donors [17]. Organ Procurement Organizations (OPOs) are vital not-for-profit entities in the U.S., tasked with the recovery of organs from deceased donors for transplantation. The U.S. has 56 federally mandated OPOs, each responsible for a specific donation service area [23].
Their main functions include assessing donor potential, gathering and providing accurate clinical information, and adhering to national policies for organ offerings [23]. While OPOs manage the initial stages of organ procurement and work with the families of potential donors to facilitate the donation process, transplant hospitals are responsible for reviewing and accepting organ offers [17][23]. OPOs play a crucial role in the authorization, testing, recovery, and delivery of donor organs to transplant hospitals, ensuring that each step of the process supports the life-saving mission of organ transplantation.
The presumption is that a registered donor has consented to organ donation, and this decision is often final and not reversible by the family. If the donor has not registered, the nurse must facilitate obtaining consent from an authorized party according to the Uniform Anatomical Gift Act, which governs organ and tissue donation in the U.S. [18].
In an ideal setting, organ recipients benefit from the care of a dedicated transplant nurse, supported by a multidisciplinary team. Transplant nurses assist the patient and their family throughout the transplant process—before, during, and after surgery—managing critical tasks such as fluid and blood replacement and monitoring for potential complications. The process from obtaining consent to organ recovery takes 48 to 72 hours [17]. During this period, the nurse and coordinator collaborate to manage the donor and provide ongoing support to the family, ensuring successful organ recovery and helping to save the lives of recipients.
However, the organ donation journey can be challenging. Recipients may experience desperation while waiting for a suitable organ match or face difficulties during their recovery post-transplantation.

Self Quiz
Ask yourself...
- How do nurses navigate the ethical complexities involved in informing families about brain death and organ donation in situations where the family's beliefs may oppose the concept of donation?
- Given the critical role nurses play in educating families and facilitating their decision-making during the organ donation process, what strategies can be employed to enhance nurse training in communication and cultural competency to better support diverse patient populations?
- Considering the pressure and emotional toll on families during the organ donation process, how do nurses balance providing factual, medical information with offering emotional support without overstepping professional boundaries?
- In cases where a potential donor has not registered their consent for organ donation, how do nurses facilitate the conversation to obtain consent from authorized parties, and what challenges might arise during this sensitive discussion?
Ethical Considerations
Ethical considerations are paramount in the transplant process, often leading care teams to seek third-party ethical consultations. The American Nurses Association’s Code of Ethics offers guidance to nurses, including those involved in transplantation [19].
Key among these is ensuring that the perception of hastening of a donor's death for organ procurement does not exist, and that decisions of the individual's donor status are independent decisions and with prioritization of the patient's wishes. Another important consideration is ensuring that transplant patients, both donors and recipients, have adequate support systems in place after discharge. This support is often critical for their long-term care and is something confirmed during the pre-screening process.
The motivations behind an individual's decision to donate organs are complex and require private discussions during pre-screening. Reasons including expected rewards, feelings of obligation, or the fear of losing a loved one can influence a decision to donate. By advocating for their patients, nurses play a crucial role in preserving patient autonomy and respecting their decisions about life and the meaningful impact of their potential organ donation.


Self Quiz
Ask yourself...
- How do ethical guidelines, such as those outlined by the American Nurses Association's Code of Ethics, influence the decision-making process in organ transplantation in cases where there may be a perceived urgency to procure organs?
- Considering the complexities and emotional intensity around organ donation, how can nurses conduct discussions about donation in a way that respects and preserves the autonomy of the donor or the donor's family under the pressures of an acute medical crisis?
- What measures can ensure that nurses and healthcare professionals understand and respect a patient’s motivations to donate, and these motivations are not compromised by external pressures or misconceptions about the benefits of donation to others?
Medical Management of Potential Donors Before Brain Death
Patients with devastating brain injuries (DBI) require aggressive resuscitation and full support to achieve physiological stability, which is crucial both for their immediate health and their potential as organ donors [20]. This includes maintaining hemodynamic stability, ensuring end-organ perfusion, and achieving euvolemia. Hormone Replacement Therapy HRT plays a significant role in managing patients with DBI before brain death, promoting hemodynamic stability, enhancing organ recovery rates, and improving graft function and survival [17][21][22].
HRT involving thyroid hormones, corticosteroids, insulin, and vasopressin is a key part of this management strategy, though the effects of early HRT still require further study [21][22]. However, the routine use of corticosteroids in patients with severe TBI is controversial due to associations with poorer outcomes [1].
In managing potential donors who have not entered the donation process, it is vital to continue aggressive care unless there are directives from a Legally Authorized Representative (LAR) or explicit advanced directives restricting treatment [17]. This approach helps optimize perfusion, stabilize physiological parameters, and sets the necessary conditions for a formal brain death examination.
Integrating donor-specific management strategies, such as invasive monitoring or renal replacement therapy, must align with the overall goals of care, respecting the patient’s health status and the expectations of families or LARs. This comprehensive approach emphasizes the complexity of managing potential donors and the necessity for tailored medical interventions that respect the patient’s medical needs and their potential to contribute to life-saving organ donations.

Self Quiz
Ask yourself...
- How can healthcare teams balance the ethical considerations of using aggressive resuscitation and Hormone Replacement Therapy (HRT) for patients with devastating brain injuries (DBI) to improve their chances of survival and maintain their viability as organ donors?
- Given the controversy surrounding the use of corticosteroids in patients with severe traumatic brain injury (TBI) and its potential negative outcomes, how should medical professionals approach the decision to use such treatments in the context of preparing patients as potential organ donors?
- In situations where there is no explicit directive from a Legally Authorized Representative (LAR) or advanced directives, how should healthcare providers determine the extent of treatment for potential organ donors when considering invasive procedures like renal replacement therapy or extensive monitoring that may alter the course of end-of-life care?
Conclusion
Dr. Joseph Edward Murray pioneered the first successful human kidney transplant in 1954, marking the beginning of a series of advancements in organ transplantation [1]. With decades of considerable progress, including the introduction of multi-organ transplants and increases in transplant numbers, with over 42,800 transplants recorded in 2022 alone in the U.S. [3]. Today, the demand for organs outweighs supply, as evidenced by over 103,924 individuals waiting for transplants, highlighting the critical need for more donors [4].
The governance of organ donation process is a stringent and regulated process, with the National Organ Transplant Act (NOTA) and organizations like the United Network for Organ Sharing (UNOS) playing key roles in managing and overseeing organ allocation and transplantation guidelines [5][7].
Nurses are instrumental throughout the organ donation process, bridging the gap between potential donors, healthcare facilities, and organ procurement organizations. Their roles encompass clinical duties, educational advocacy, and providing emotional support to donors' families, which is crucial in navigating the complex process of organ donation.
Nurses ensure thorough communication and understanding between all parties involved, including educating families about brain death and the significance of organ donation. Nurses are also pivotal in managing the medical care of potential donors to maintain organ viability, further underscoring their essential role in the success of transplant outcomes and rate of organ donations.

Self Quiz
Ask yourself...
- Considering Dr. Joseph Edward Murray's pioneering work in kidney transplantation and the subsequent advancements in multi-organ transplants, how might future innovations in medical technology further impact the balance between the supply of and demand for organ transplants?
- Given the critical role of nurses in the organ donation process, from clinical responsibilities to providing emotional support, how might the training and education of nurses evolve to enhance their effectiveness in these diverse roles in the context of increasing transplant numbers and complex cases?
- With the rigorous guidelines overseen by the National Organ Transplant Act and the involvement of organizations like UNOS in overseeing organ allocation, what ethical challenges arise in ensuring equitable organ distribution, and how can healthcare professional address these challenges to maintain public trust in the organ donation system?
Conclusion
BODY TEXT
Flap Surgery: The Basics
Introduction
Flap surgeries can be a critical treatment for various wounds to provide bulk tissue. It is a tad more detailed than skin grafts, as it involves a circulatory supply from a donor site to a recipient site. It is important to recognize what flap surgery entails, the indications, and types of flap surgeries. Nurses should be knowledgeable on care plans and assessment for flap surgery, positioning techniques, patient education topics, and how to identify possible complications such as infection or flap dehiscence. Are you ready to dive into the interesting course topic of flap surgery?
Flap Surgery: What is it?
Flap surgery involves removing healthy, live tissue from one location of the body and transporting it to another area that needs it for healing purposes. Flap surgeries are commonly used to transfer this healthy tissue to areas of lost skin, fat, muscle movement, and/or skeletal support (9). A tissue flap has its own system for vascularization and does not depend on the recipient’s wound bed to perfuse the donor tissue, which differs from non-vascularized skin grafts (8). Essentially, a flap is tissue with a substantiated blood supply that is transferred from a donor site to a recipient site. If the flap surgery was a party, the damaged host site would send out an invite saying “BYOB- Bring Your Own Blood-Supply!”
The flap continues to be fed by the same blood supply from where it was taken, until new blood vessels grow from the recipient site and the wound heals completely. The recipient site is called the primary defect and the wound that is created by cutting, lifting, or sliding the flap to fill the primary defect is called the secondary defect (8). The base, or pedicle, of the flap is the tissue that remains attached to the skin adjacent to the defect, it contains the vascular supply required for initial flap survival (8).
Surgeons have used skin flaps to repair wounds and tissue damage for centuries. The term “flap” was derived from the Dutch word “flappe” during the 16th century (8). Around 700 B.C., the Sushruta Samhita (an ancient text on surgery and medicine) first documented a technique of reconstructing a large nasal tip defect with a flap of cheek tissue (8). New techniques are constantly being developed to meet various needs. Flap surgeries are used for a variety of wounds from pressure ulcers to breast reconstruction following mastectomy.

Self Quiz
Ask yourself...
- Have you ever cared for a patient following a flap surgery?
- Do you recognize the difference between flap surgery and skin grafting?
- Are you familiar with the vascular structure at deeper skin levels?
- Can you discuss how significant improvements could have been made over the past hundreds of years?
Types of Flap Surgeries
Flap surgeries are classified in the following ways: (9)
- Blood supply
- Type/composition of tissue
- Distance of the healthy site from the recipient tissue
- Locations of donor and recipient tissue
- Movement
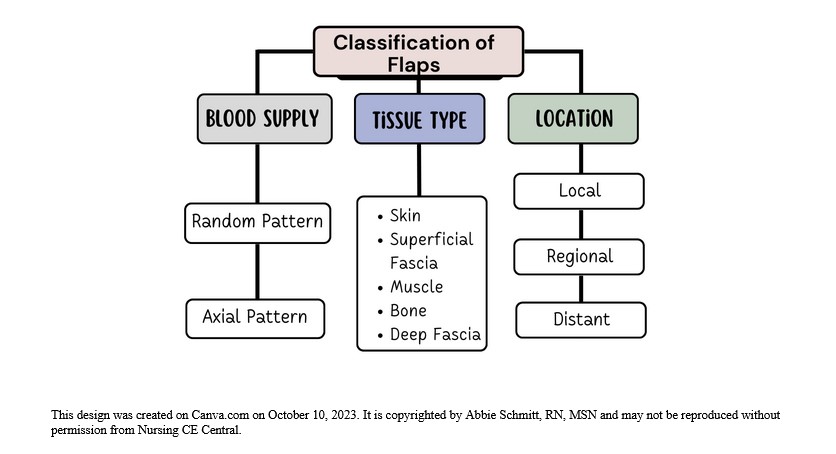
Figure 1: Classification of Flaps
Classification by Blood Supply
Flaps can be named based on the supply of blood. The understanding of the circulation of blood to the donor tissue is critical when describing the type of flap. The terms random and axial are used to categorize the blood supply.
- Random Flaps
- Not based on a specific vessel
- Uses subdermal plexuss (network of blood vessels between the deep reticular portion of the dermis and subcutaneous fat tissue beneath it) (7)
- Axial Flaps
- Single, direct cutaneous artery in the axis of the flap
- Named according to the pathway
Classification by Tissue Type
Flaps can be named according to their composition. The tissue composition may be skin, fascia, muscle, bone, nerve, cartilage, or a combination. Fascia is the thin lining of connective tissue that surrounds and holds each blood vessel, bone, nerve fiber, and muscle in place (7). Cutaneous refers to the layers of skin. Pedicle flaps are those that are still attached to the original site and the other end is moved to cover the recipient area; a free flap is an area of tissue completely removed from one part of the body and surgically placed in another area (8).
Common flaps: (5)
- Skin Flap: Skin and superficial fascia
- Fascio-cutaneous Flap: Skin and deeper layer of deep fascia
- Fascial Flap: Deep fascia only
- Muscle Flap: Muscle only
- Myo-cutaneous Flap: Muscle and skin
- Osteomyocutaneous Flap: Muscle, bone, and skin
- Bone Flaps: Bone (vascularized)
- Innervated Flaps: Flaps that contain a motor or sensory nerve and function
Fascio-cutaneous Flap
This flap includes the skin, subcutaneous tissue, and the underlying deep fascia (5). The musculocutaneous perforators or direct septocutaneous branches of major arteries act as vascular supply (5). Perforator flaps are named based on their location, arterial supply, or the muscle of origin. The indications for fasciocutaneous flaps are based on its advantages of being more simple, reliable, thin, and easily mobilized (8). These flaps can come from many potential donor sites (8).
Muscle Flap
Muscle tissue can be used as donor tissue in flap surgery. Surgeons may utilize the benefits of flap surgery in wound closure following major surgeries. For example, median sternotomy (vertical inline incision through the sternum of the chest) is the most commonly used approach for cardiac surgery (6). Cardiac surgeons face the risk of deep sternal wound infections following surgery, which is associated with significant morbidity and mortality rates. The use of soft tissue flaps for sternal closure is helpful for patients with extensive tissue deficits after debridement (6). It can be used for immediate or delayed closure. Options for donor tissue for sternal flap closure include the pectoralis major, rectus abdominis, and latissimus dorsi muscles, or an omental flap (6).
Remember, flaps are transplanted with blood supply intact, so it’s important to know the supply. For instance, if tissue from the pectoralis major muscle is used, the nurse must recognize that this muscle’s primary and secondary blood supply is the thoracoacromial artery and perforators from the internal mammary artery (6).
Musculocutaneous Flap
This type of flap, which includes muscle and skin layers, is often used when the area to be covered needs more bulk and an increased blood supply. Musculocutaneous flap surgery is frequently used to rebuild a breast after a mastectomy (5).
Bone Flap
A bone flap is comprised of bone with a vascular supply. An example of this flap surgery is for a surgical site infection (SSI) following a craniotomy; in this procedure, operative debridement occurs, and the bone flap is removed, cleaned, and replaced (4). An alternate therapy for this is titanium cranioplasty (implant instead of native bone flap), which has similar outcomes.
Classification by Location and Movement
- Local flap: Donor tissue is located next to the area receiving the tissue; the skin remains attached at one end to allow the blood supply to be left intact (5).
- Regional flap: Donor tissue is a section that is attached by a specific blood vessel.
- Distant flap: Donor and recipient tissues are distally located from each other. This flap surgery involves detaching and reattaching skin and blood vessels from one site of the body to another site; microsurgery is used to connect the blood vessels (5).
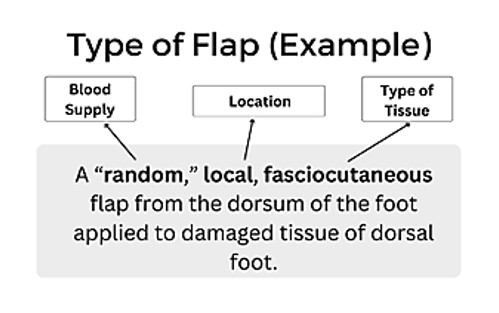
Figure 2: Example of Flap Type
The movement of the flap is also used to describe flap surgery. You may hear terms such as advancement, sliding, rotation, and pivotal. Sliding flaps is when the tissue is moved or "slid" directly into the adjacent defect without "jumping" over other tissue (5). Advancement flaps are considered simple movements for local flaps and fall within the group of sliding flaps. Pivotal (geometric) flaps include rotation, transposition, and interpolation (5). Local, random pattern flaps are common for the reconstruction of cutaneous defects.
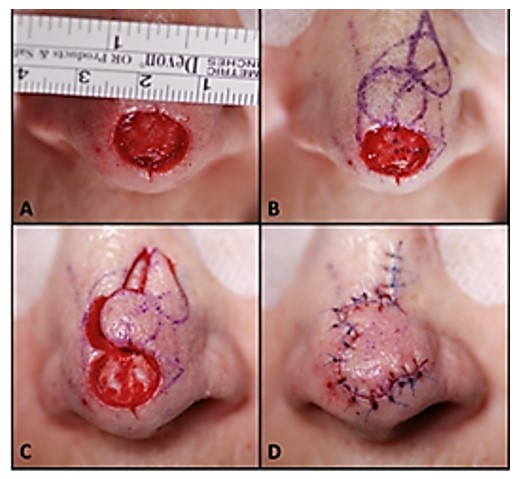
Image 1: Image of a local flap surgical procedure to cover nasal tip defect/wound (9)

Self Quiz
Ask yourself...
- Are you familiar with the differences in skin, muscular, bone, and nerve tissue?
- Can you think of benefits of using a local, pedicle flap over a free flap?
- Can you discuss how fasciocutaneous flaps may have more advantages and more potential donor sites?
- Are you able to recognize the general location and complexity of a surgical note that says “local, random, skin flap with pivotal manipulation at midline of forehead”?
Indications for Surgery
There is an incredible breadth of possibilities for flap reconstructive surgery, from small, skin-only defects to large, multi-tissue defects. There is a wide range of etiologies, such as traumatic, oncological, and congenital (9). The transferred tissue flap can contain multiple types of tissue, including skin, muscle, nerve, fascia, and bone (9). The larger the volume of tissue transferred, the greater the need for perfusion. A common indication is the need for a large bulk of tissue. Flaps are helpful when wounds are large, complex, or need large amounts of tissue for closure.
General Indications:
- Protection of the greater vessels
- Correction of congenital defect
- Abdominal wall reconstruction
- Deep, gaping wounds
- Reconstruction after tumor excision
- Trauma
- Debridement procedure to remove infected or necrotic tissue
- Venous ulcers (non-healing)
- Pressure ulcers (non-healing)
- Breast reconstruction
- Rhinoplasty
- Scar Revision
- Skin Cancer
- Burns
Each type of wound has unique indications. Commonly, skin flap surgery is required when a wound is too big for the edges to be brought together directly, so the flap covers the area and depth of the wound (10).

Self Quiz
Ask yourself...
- Do you have experience in caring for a patient with a deep, healing wound?
- Have you ever cared for a patient following a tumor removal?
- Can you discuss why debridement of the recipient site is essential prior to flap placement?
- Can you name various methods of wound closure? (ex: sutures)
Risks versus Benefits
Flap survival depends on factors of blood flow, angiogenesis (formation of new blood cells), vascularization, edema, wound closure tension, postoperative complications (hematoma/seromas) and infection (8). Before the initial incision, the flap is fully vascularized and viable, but once the flap is raised, it is immediately ischemic. The tissue can survive up to 12 to 13 hours of avascularity at 37°F and many research studies have proven it is viable even longer (8). This time is invaluable to preserve the tissue. Sufficient blood flow through attachment of the base of the flap is essential in the initial 24 to 48 hours after surgery (8). There is a risk for loss of tissue with no meaningful contribution to the needed area, along with a new wound. This risk reminds me of a neighbor who once removed carpet from a closet to patch carpet in a bedroom, only to find the cutting was too small and they were left with two gaping carpet holes.
There is also risk for bleeding, infection, or necrosis at both sites. A recent study found that more than 27% of patients will experience a minor complication (wound dehiscence, infection, fistula, and donor-site problems) after surgery, and 6% of patients will suffer a major complication (flap failure, pneumonia, and cerebrovascular accidents) following surgery (11). Chronic flap complications can also be aesthetic in nature; include scarring, contracture, color/texture mismatch, and lack of hair growth. Patients may experience pain or numbness at the sites on a chronic basis as well (9).
Most flap surgeries are considered safe with a low complication rate, and surgeons report that flap surgery is not avoidable in certain circumstances. However, the surgery preparation itself and anesthesia presents considerations for elderly patients or those with heart disease, uncontrolled diabetes, smokers, or bleeding disorders (2). Nutrition is a key factor in these surgical procedures. Poor nutritional status has been linked with a greater incident of negative outcomes (11). The healthier the patient is before surgery increases, the chances of reduced complications, so glucose control and weight management are examples of risk reduction strategies.

Self Quiz
Ask yourself...
- Do you feel confident with patient education methods for explaining risks versus benefits?
- Can you name reasons informed consent for flap procedures is not only required, but ethical?
- Do you have experience in educating patients on diabetes and the importance of glucose control in wound healing?
- Are you familiar with your facility’s medical literature database?
Preparing for Surgery
Patients undergoing flap surgery need an abundance of education on what to expect throughout this procedure. There are many opportunities to optimize patient outcomes before going to the operating room. Preoperative education, for example, has been suggested to have an important, positive effect on clinical outcomes (11). Many patients are also experiencing other issues, such as cancer diagnoses, poor circulation, comorbidities, bed sores, among others. Taking time to holistically prepare each patient is essential.
Addressing Comorbidities and Other Conditions
Multiple studies have found an increased surgical complication rate in patients with diabetes mellitus, older age, female gender, malnutrition, anemia, and nicotine intake (11). Prior to surgery, the goal is to improve and optimize the modifiable conditions as much as possible, for instance, reduction in nicotine or improvement in glucose control and anemia. Further, patients with advanced cancer can have hypothyroidism affecting postoperative healing if left uncorrected (11). Non-modifiable factors such as a history of radiotherapy, age, advanced cancer stage, or chronic kidney disease, cannot be altered prior to surgery, but can guide care planning and education following the surgery.
Adequate nutrition before and after flap surgery has been demonstrated in numerous studies to improve outcomes. An estimated 35% of patients with head and neck cancers present in a state of malnutrition, and the Enhanced Recovery After Surgery (ERAS) Society recommends that all patients undergo a comprehensive preoperative nutritional assessment and consult with nutritionist (11). Improved nutrition status can hopefully yield enhanced wound healing problems and reduction in risk of infection.
Lab assessment is key to preparation before flap surgery. An example is assessment for anemia prior to surgery. Patients who are anemic at the time of free flap surgery have been found to have poor outcomes (11). Remember, hemoglobin transporting the oxygen to the sites of flap insertion and removal is vital to the survival of the flap. Preoperative hemoglobin values below 10 g/dL have historically been a significant predictor of flap failure and thrombosis (11). A hematocrit level of 30 to 40% with normovolemic hemodilution is ideal to optimize patient outcomes.
Blood transfusions during or following surgery impacts flap success as well. Transfusion can increase blood viscosity and immunosuppression, thus leading to decreased blood flow and flap compromise from poor perfusion (11). Studies also show a link between blood transfusions and increased wound infections (11). Steps and treatments should be taken prior to surgery to improve anemia or blood component abnormalities to give these patients a greater chance for successful flap surgery.
Preoperative considerations should include: (9)
- Patient age
- Diabetes status
- Smoking history
- Atherosclerosis
- Peripheral vascular disease
- Steroid use
- Previous surgeries
- The extent and location of the defect
Providing Preoperative Instructions
A lack of education, difficulty in understanding complex medical information, fear and anxiety about the surgery, and language barriers are some of the challenges a patient for surgery may have. Patients may also have limited access to reliable health resources or be unable to recall important information due to stress or preoperative medications. As a result, they may not be fully informed about the surgical process, potential risks, and postoperative care.
Preoperative education list:
- Assess the patient’s level of understanding.
- Each facility should have a preoperative teaching program with specific content on surgery, but you must assess if the patient understands this information.
- Review specific pathology and anticipated surgical procedure.
- Verify that consent has been obtained / signed.
- Informed surgical choices and consent for the procedure is required, not only a signature.
- Use resource teaching materials, and audiovisuals as available on flap surgery and implement an individualized preoperative teaching plan.
- Preoperative or postoperative procedures and expectations, output (urinary and bowel) changes to expect following surgery, dietary considerations, anticipated intravenous (IV) lines and tubes (nasogastric [NG] tubes, drains, and catheters).
- Preoperative instructions: NPO guidance prior to surgery, shower or skin preparation, medications to take and hold, prophylactic antibiotics or anticoagulants, anesthesia premedication.
- Discuss postoperative pain management plan and options.
- Some patients may expect to be pain-free or are hesitant to take narcotic agents.
- Provide education and encourage practice of coughing and deep breathing.
- Confirm and recheck the surgery schedule, patient identification band, chart, and signed operative consent for the surgical procedure.
- Offer pastoral spiritual care or counseling.

Self Quiz
Ask yourself...
- What are some examples of pertinent laboratory values to assess prior to surgery?
- What are normal values of hemoglobin and hematocrit?
- Do you consider pain management a “one size fits all” care plan?
- Are you familiar with pastoral and spiritual counselors and supportive resources within your organization?
Post-Operative Considerations
This section will cover assessment, drains, positioning, and negative pressure wound therapy during the post-operative period.
Assessment
Frequent monitoring of free flaps in the acute postoperative period is important. It is strongly recommended that flap assessments are performed at least hourly for the first 24 hours postoperatively, then continued at a reduced increment for the duration of the patient's hospitalization (11). Each facility should have standing orders for flap assessment based on the directive of the surgeon or regulatory body.
In addition to conventional assessments of flaps (physical exam of flap warmth, turgor, capillary refill, color, and Doppler assessment of the vascular pedicle), many adjuncts have been developed including implantable Dopplers to assess blood flow (11). Assessments should include a head-to-toe physical assessment and a focused wound assessment. A focused cardiovascular (circulation and perfusion) and integumentary assessment is appropriate. Review of lab work indicative of healing status, hemodynamics, and infection should be a priority. Standard post-operative assessments following anesthesia, such as respiratory and orientation, should be performed according to facility protocol.
Assess circulation of the flap:
- Color of the flap (dusky, blue, pink, pale)
- Warmth
- Dry/Intact? Leaking Fluids?
- Changes in size
- Edema
- Indications of hematoma (sutures over the flap pulling apart, or palpable crepitus beneath the skin)
Assess amount and type of exudate (drainage): (3)
- Amount (scant, small/minimal, moderate, or large/copious)
- Color and thickness: (7)
- Sanguineous: fresh bleeding
- Serous: clear, thin, watery plasma
- Serosanguinous: serous drainage with small amounts of blood noted
- Purulent: thick and opaque; color can be tan, yellow, green, or brown (this is an abnormal finding and should be reported to physician or wound care provider)
Use of Doppler to assess deeper circulation of flap: (11)
- Color duplex ultrasound
- Near-infrared spectroscopy
- LASER Doppler flowmetry
- Implantable Doppler (useful for buried flaps)
Assess circulation distal to the flap:
- Capillary refill
- Color
- Temperature
- Pulses
- Edema
Drains
Drains may be used for removal of fluid around both the donor and recipient surgical areas to enhance healing (7).
Patients may have the following drains after flap surgery:
- Jackson Pratt (JP) drains
- JP drains are closed-suction devices that remove fluids from the surgical sites.
- JP drains contain a flexible bulb that has a plug that can be opened to remove collected fluid.
- Each time fluid is removed from the JP drain, the nurse should squeeze the air out of the bulb and replace the plug before releasing the bulb.
- This suction creates a vacuum that pulls fluid into the drainage tubing and bulb.
- Penrose drains:
- A Penrose drain is a soft, flexible tube inserted into the surgical site that drains fluid away from the wound bed (7).
- Nurses should assess the drain and express fluid when appropriate to prevent accumulation.
Positioning
The goal of positioning following flap surgery is to promote and improve tissue perfusion. Positioning and elevation of the flap recipient will promote venous return and reduce fluid accumulation to improve tissue perfusion. Activity, exercise, and repositioning improve tissue perfusion. Massage of the erythematous area is avoided because damage to the capillaries and deep tissue may occur (10). Patients should never lay on the wound and extremities should never “dangle” (if the donor or recipient site is on the extremities). Positioning may require creativity when there are multiple drains, NG tube, wound therapy devices, IV tubes, and multiple dressings. Positioning should be free of restrictive clothing and flap sites should be visible for assessment of dressings. It is imperative for the surrounding skin to be sanitary and free of debris.
Negative Pressure Wound Therapy
Negative pressure wound therapy (NPWT) is typically used for soft-tissue salvage after the development of complications after flap surgery. For example, NPWT may be applied if an infection occurs in the donor or recipient flap. Immediate postoperative application of NPWT over the flap coverage is not as common (2). However, nurses should be aware of this treatment, the application, and its mechanisms of action.
NPWT is also known as a wound vac. NPWT uses sub-atmospheric pressure to help reduce inflammatory exudate and promote granulation tissue in an effort to enhance wound healing (4). The idea of applying negative pressure therapy is that once the pressure is lower around the wound, the gentle vacuum suction can lift fluid and debris away and give the wound a fighting chance to heal naturally. NPWT systems consist of a sterile foam sponge applied to the wound bed, a semi-occlusive adhesive cover, a fluid collection system or cannister, and the suction pump (1). The foam sponge is applied to the wound and covered. A fenestrated tube is embedded in the foam, the wound is sealed with adhesive tape to make it airtight, and the machine delivers continuous or intermittent suction, ranging from 50 to 125 mmHg (1).
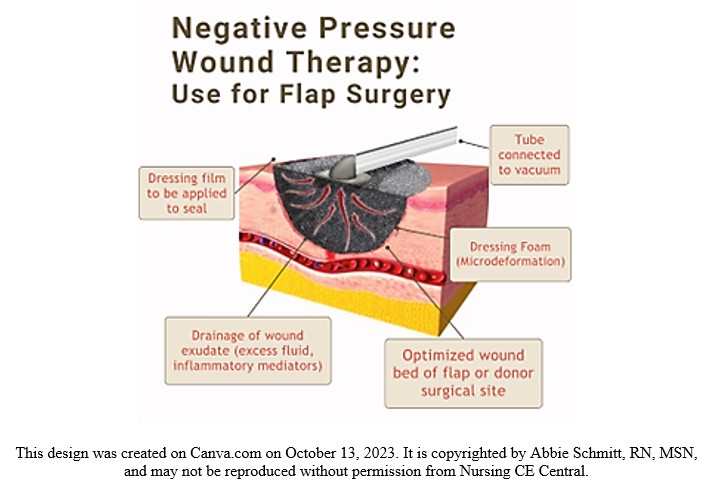
Figure 3. Negative Pressure Wound Therapy Visual

Self Quiz
Ask yourself...
- Have you ever completed a focused wound assessment that resulted in abnormal findings that were anticipated?
- Can you name examples of pertinent laboratory values to assess following general surgery?
- Have you ever used or witnessed the use of a doppler in assessment of proper circulation?
- Can you describe the importance of positioning in tissue perfusion?
Home Care and Patient Education
Educating clients and caregivers about wound care and skin integrity empowers them to actively care for their flap sites. With proper wound cleaning, dressing changes, and preventive measures, individuals can confidently perform their own self-care and enhance the healing process. The use of pamphlets, printouts, websites, and referrals to specialists will give the patients a stronger foundation of knowledge.
- Wound Assessment
- Teach the patient and caregiver about skin and wound assessment, ways to monitor for signs and symptoms of infection, complications, and proper healing.
- Signs of Infection
- Signs of a localized wound infection include redness, warmth, tenderness, and abnormal purulent drainage around the wound.
- Importance of proper nutrition, hydration, and methods to maintain tissue integrity
- Adequate caloric intake and balance of protein and essential vitamins has been shown to improve the healing of flaps (3).
- Dressing changes, wound cleansing, and hand hygiene
- Methods to prevent skin breakdown
- The flap surgery is often for the treatment of a deep pressure wound, so education is needed on impaired skin integrity due to friction.
- Common areas: Sacrum, heels, elbows.
- Avoidance of raising the head of bed often, causing weight to be applied to sacrum.
- Importance of turning, mobility, and ambulation
- Pain management
- Medications
- Heat/cold therapy applications and precautions
- Negative Pressure Wound Therapy devices (wound vac)
- Home healthcare is applicable for these devices and should be changed by a certified individual, but patients should be aware of basic care and troubleshooting.
- Drain maintenance
- Showering restrictions
- Reduction of stress and tension at wound site
- Avoid constipation, strenuous movements, and lifting
- Restrictions vary for location of flaps and per surgeon instructions
- Follow-up appointments

Self Quiz
Ask yourself...
- Can you describe assessment findings that indicate infection after flap surgery?
- Are you familiar with various drains such as JP drains?
- What do you think are some fears among patients going home or to a long-term care facility after flap surgery
Flap Dehiscence or Loss
Flap dehiscence is a complication in which the incision made to either the donor or recipient site reopens. A flap loss refers to the flap not re-establishing blood flow and surviving, leading to necrosis of the tissue. As we mentioned earlier, the survival of the flap is impacted by blood flow, new vascularization and tissue formation, edema, wound closure tension, postoperative complications (hematoma/seromas), and infection (8).
Prevention Strategies
Nurses should apply their basic knowledge on causes of wound dehiscence. Factors that influence dehiscence risk include the ability to synthesize collagen, strength of suture material, closure technique, and stress on the incision, such as coughing, strenuous movement, or obesity (7). Consider areas that have greater stress and tension, such as the abdomen. Dehiscence is most common following abdominal flap surgeries (7). NPWT has been shown to be a great preventative measure for wound dehiscence as studies found a roughly 50% reduction in stress and tension at the incision site with its use (7). This reduction in stress is attributed to the reduction in subcutaneous fluid accumulation and enhanced healing time.
The location of the flap surgical sites will impact prevention. For example, immobilization and stabilization devices are unique to sites such as the abdomen, chest, extremities, and sacral region. Infection prevention measures for wounds are essential for nursing care. Incisions from flap procedures also have a higher chance of opening if the wound becomes infected (7). Prevention of hematomas is also meaningful, including the use of blood thinners. However, the safety precautions for blood thinners is different for each client.
Management and Treatment
It is estimated that 80% of free flaps can be salvaged if dehiscence or compromise is recognized early enough (11). As we mentioned, it is more common for flaps that are removed from (or applied to) the abdomen to open. The following terms describe the depth:
- Superficial dehiscence: the skin wound alone opens, but the rectus sheath remains intact.
- Full thickness dehiscence: the rectus sheath fails to heal and “bursts,” with protrusion of abdominal content.
- This commonly occurs secondarily to intra-abdominal pressure (example: ileus) or poor surgical technique.
The treatments for flap compromise will be determined by the provider once a cause is identified. Treatment may be a return to the operating room for additional surgical intervention or a simple evacuation of hematoma through suctioning.
Recovery
The focus of recovery is the healing and thriving of the flap site and surgical wounds. The time of flap healing varies, and some may heal much quicker than others. There are four phases of wound healing to recognize: hemostasis, inflammatory, proliferative, and maturation (7).
- Hemostasis. This phase begins immediately after surgery when platelets release growth factors that alert various cells to start the repair process.
- Inflammatory. This process involves vasodilation so that white blood cells in the bloodstream can move into the wound to begin cleaning the wound bed. Signs include edema and erythema.
- Proliferative. This phase generally begins a few days after the injury and includes capillary repair and growth, granulation tissue formation, collagen formation, and wound contraction (7).
- Maturation. During this phase, collagen continues to be created to strengthen the wound and fill in the wound gaps.
The healing process can be enhanced in many ways, including nutrition therapy, topical agents, compression therapy, and hyperbaric oxygen therapy (HBOT). The recovery process for flap surgery will include management of pain and discomfort, disturbance of body image, impaired skin integrity, swelling, bruising, and gastrointestinal upset.
Outcomes for recovery should be measurable and achievable. Each patient will have unique recovery goals, integrating comorbidities and psychosocial aspects.
Examples of Patient Outcomes following flap surgery: (3)
- Patient safety: Patient will be able to attain safety by maintaining intra- and extra-cellular environment.
- Healing of wounds: Wounds should heal properly, complications will be prevented or maintained
- Management of pain
- Prevention of further damage or skin breakdown

Self Quiz
Ask yourself...
- How would you describe the process of healing?
- Can you name some underlying causes of flap dehiscence?
- What are some strategies to prevent infection of the surgical site?
Conclusion
As discussed throughout this course on flap surgery, nurses are a key team member in the care and survival of flaps. Hopefully you now understand what flap surgery is, the indications, and types of flap surgeries. Critical knowledge includes pertinent assessment, drain or NPWT management, patient teaching, and prevention and management of possible complications.

Self Quiz
Ask yourself...
- Can you name the various ways to classify flaps?
- Why do you think it’s important to classify flaps according to their blood supply?
- What do you think the reason is for flap surgeries following mastectomies and breast reconstruction?
- Can you name various indications for flap surgery following a burn?
- What are comorbidities that may impact wound healing?
- Can you name common risks of surgeries?
- Can you think of reasons why elderly patients may have poor outcomes following flap surgery?
- Can you identify modifiable and non-modifiable pre-operative considerations?
- What do you think are some common fears and uncertainties among patients prior to flap surgery?
- Can you name teaching topics for a patient who is scheduled for a flap surgery?
Diabetic Ketoacidosis Management
Introduction
Diabetic ketoacidosis is considered one of the most life-threatening complications of diabetes mellitus. More importantly, it is also one of the most preventable complications of diabetes. Through proper education and empowerment of persons with diabetes to self-manage this chronic medication condition, the overall mortality rates associated with this complication have steadily declined in the United States. An interdisciplinary team approach (including medical providers, social workers, case managers, and community resources) has been proven to reduce recurrences of DKA in vulnerable populations. (2)
Definition
DKA, or diabetic ketoacidosis, is defined as the potentially life-threatening medical condition that occurs in people with diabetes. While it usually occurs in persons with type 1 diabetes mellitus, who are dependent on daily insulin injections, it may also occur in individuals with type 2 diabetes for a variety of reasons (underlying physiologic stress, such as an acute infection or trauma, or uncontrolled blood glucose levels and missed routine diabetic medications).
In an acute case of diabetic ketoacidosis, the body is not producing enough insulin to move glucose into the cell for energy, and the liver then begins to break down fat for fuel instead, producing ketones. This buildup of ketones in the body results in ketoacidosis. Left untreated, diabetic ketoacidosis can lead to a diabetic coma and eventual death. (3)


Self Quiz
Ask yourself...
- As you begin this course, think about the diabetic patients you have cared for in your professional career.
- Do you have family or friends in your life that have been diagnosed with diabetes?
- What are your concerns over their self-management ability of this chronic medical condition?
- What areas of diabetes self-management do you consider the highest priority when you are delivering patient discharge instructions?
Epidemiology
Epidemiology is the study of how often a disease process occurs in different populations. By studying the rates of occurrence, epidemiologists are able to evaluate treatment options and develop long term strategies to lower the risk of ongoing or recurrent disease related episodes.
Diabetic ketoacidosis is currently a leading cause of both morbidity and mortality in children with Type 1 diabetes. It usually occurs at the time of the initial diagnosis in as much as 30-40 percent of the children in the United States alone. In children living with a confirmed Type 1 diabetes condition (previously diagnosed), these percentages decrease to average rates of 6-8 percent annually.
The drastic reduction of such occurrences is believed to be directly related to ongoing patient and family education and medication adherence. Diabetic ketoacidosis is potentially life-threatening, but it is for the most part, also preventable. Throughout this educational offering, key components of patient education in diabetic self-management, including reducing the risk of diabetic ketoacidosis, will be discussed (4) (5).
By comparison, other countries, challenged by annual income, healthcare access, cost management, and food insecurity, do not fare so well. Various studies were funded by the Leona M. and Harry B. Helmsley Charitable Trust, and the Juvenile Diabetes Research Foundation Ltd. Several countries included in these studies were deemed “LLMIC” (low and low middle-income countries). Countries, including Haiti, Ethiopia, Senegal, Nepal, and Tanzania, to name a few were found to have inadequate supplies, medications, and equipment to both initially diagnose, and successfully manage diabetes mellitus long term. Critical items necessary for the treatment and stabilization of acute diabetic ketoacidosis were in even shorter supply. These barriers to treatment resulted in delayed or missed diagnosis, increased overall complication rates and premature deaths.
“Evidence from single-center studies suggest that DKA in new-onset T1D is more common in LLMICs compared to upper and upper-middle income countries, with rates ranging from 62.2 to 77.1% in Nigeria, 69.8% in South Africa, and 92.1% in Sudan. In comparison, in upper and upper-middle income countries in North America and Europe the rates range from 14.7% (Denmark) to 42.0% (France”). (6)
Ongoing education of healthcare professionals and patients/families alike, coupled with availability of and easy access to self-management medications, and monitoring equipment, positively affect DKA related health outcomes and quality of health and well-being.
The development of insulin delivery systems (insulin pumps) has further positively impacted the rate of DKA occurrence. Patient comfort, ongoing education, streamlined medication delivery and enhanced monitoring systems have afforded patients with diabetes a better understanding of their condition and empowered them to successfully self-manage their health conditions. While reported rates of DKA in previously diagnosed persons with T1DM were 6.3% in one study, that number decreased to 2.2% at 3 years out.
Ongoing improvements in closed insulin delivery systems medication continues to improve (lower) DKA occurrence rates, when compared to those previously using multiple daily injection therapy. The development of continuous glucose monitoring (CGM) devices, in addition to insulin delivery systems, provides for early detection and treatment of both hypoglycemia and hyperglycemia. The addition of remote app devices further allows constant monitoring and two-way communication between patients, family members, and even healthcare providers.
Sadly, the population identified as being at highest risk for DKA is that of children who are uninsured/underinsured, lacking the insurance coverage for many closed delivery medication systems as well as specialty care (pediatric endocrinology) provider access.
The acute complications associated with DKA account for a high percentage of premature deaths in T1DM patients under the age of 30 years old. (7) Given these statistics of prevalence and incident rates, DKA is an ever-increasing global concern which is best addressed and managed through ongoing, patient specific disease management education.
The prognosis for DKA worsens in the presence of coma, hypotension and in the presence of severe (chronic and acute) comorbidities. Yet, with early identification, ongoing education, and improved glucose monitoring/treatment options, DKA, often life threatening, is also highly preventable. The goal, therefore, is to ensure all patients with diabetes mellitus are given equal opportunity to access both the education and materials necessary to successfully monitor their health condition. (8)
Pathophysiology
Diabetic ketoacidosis occurs when the body is under stress and responds with an increase in catecholamines, cortisol and growth hormones. The release of such hormones decreases the ability of insulin, further increasing insulin resistance and resulting in serum hyperglycemia. Without cellular glucose for energy the body then begins to break down fat and protein for energy, resulting in increased levels of serum ketones. The combination of hyperglycemia and ketosis, as well as dehydration and various electrolyte imbalances, form the basis of diabetic ketoacidosis. (9)
While it is believed that the omission of insulin (nonadherence/ noncompliance, or mechanical failure of insulin delivery systems) accounts for the largest percentage of DKA admissions, other factors may be responsible for the development of this condition. Any disease process that increases insulin resistance, impairs insulin secretion, or interferes with carbohydrate metabolism may contribute to the onset of acute diabetic ketoacidosis in a vulnerable, health compromised patient.
Clinical Signs and Symptoms
Diabetic ketoacidosis is caused by the underlying presence of hyperglycemia, ketoacidosis and ketonuria. Early signs and symptoms may include any of the following:
- Generalized weakness and fatigue.
- Nausea and vomiting
- Diffuse abdominal pain.
- Decreased appetite and anorexia.
- Decreased/ altered levels of consciousness, such as mild disorientation and confusion.
- Dry skin and mucus membranes and decreased perspiration
- Tachycardia (increased heart rate) and tachypnea (increased respiratory rate)
- Acetone/ketone smell on breath
- Significant weight loss (usually a rapid onset in the newly diagnosed Type 1 diabetes mellitus patients)
- A patient history of noncompliance with prescribed insulin therapy (due to coexisting medical issues in which patient may have intentionally stopped insulin due to decreased food/fluid intake), costs factors (unable to afford prescribed therapy) and missed insulin doses (mechanical failure of the patient’s current insulin delivery system).
Additional signs and symptoms may be present, related to the patient’s age. While an adult patient would be able to verbalize symptoms, a child may not be able to do so, especially in cases where the diagnosis of T1DM is done during their initial presentation to an emergency department for suspected DKA.
In all cases, there may be other factors (illness, injury, medication side effects) that cause DKA to occur; thus, thorough examination and diagnostic testing must be done in all cases prior to initiation of treatment. Likewise, discharge planning and ongoing follow-up care must be patient specific to address behaviors and treatments required for optimal health maintenance.
Teens/Young Adults
In the teenager/ young adult population, the following symptoms may occur: (11)
- Increases in urination, thirst, and appetite.
- Unintentional/ unexplained weight loss despite increases in food and fluid intake.
- Changes in energy level (increased fatigue)
- Vision changes
Please note that normal growth and development stages/patterns in a teenager/young adult will influence glucose metabolism (related to hormone levels).
Young Children
In the young children’s population, symptoms usually strike suddenly and, unlike the adult population, are usually not related to a specific lifestyle or dietary practice. Most children present with the following symptoms:
- Increased urination
- Increased thirst
- Fatigue
- Vision problems (blurred vision)
- Acetone/ketone “fruity smell” on breath
- Unexplained weight loss, often despite appearing to eat (and drink) more.
- Changes in mood and behavior
Infants/Toddlers
In the infant/toddler population, symptoms may present as follows:
- Increased food and fluid intake (always appearing thirsty despite normal fluid intake)
- Frequent urination (in the potty-trained child, this may present as a new onset of bed wetting behaviors)
- Increasing fatigue and changes in normal activity levels
- Unexplained weight loss despite increased food and fluid intake
- Increased occurrences in diaper rashes (suspected increase in yeast infection)
- Fruity/acetone smell to breath
- Unusual behavior (child specific)


Self Quiz
Ask yourself...
- Your patient with DKA appears to be “noncompliant” with his prescribed insulin therapy. What factors may be contributing to his failure to take medication as directed?
- What nursing interventions can be done with/for this patient to increase adherence to his current medication regimen?
- Unexplained weight loss in a young adult may indicate diabetes. What other medical conditions could be causing unexplained weight loss in this age group?
- How would you address these concerns with your patient/ their family members?
Etiology
Etiology: Causes of Diabetic Ketoacidosis
Hyperglycemia and low insulin levels lead to diabetic ketoacidosis. Common causes include the following:
- Acute illness, altering a person’s intake of food or drink, makes glucose management more difficult. This is a two-fold situation. The person with diabetes, recognizing the change in their normal food/fluid intake may also choose to intentionally decrease/skip their routine diabetic medications to avoid episodes of hypoglycemia.
- Insufficient levels of insulin due to the demands of normal growth and development patterns in children and young adults.
- Missed insulin doses (intentional decision to take inadequate doses, inadvertently held doses, inaccurate dose amounts, clogged insulin pump tubing).
Other causes of DKA, unrelated to insulin dose administration, are thought to be related to increased stress levels (inflammation/ infection) and normal hormone disruption, physiologic stressors. Persons with Type 2 diabetes may experience DKA due to prolonged, untreated hyperglycemia. (12), (13)
- Myocardial infarction
- Neurological stroke
- Motor vehicle accident with physical injuries (inflammatory response to blunt force/penetrating trauma)
- Abuse of alcohol and illegal drugs
- Medication side effects (diuretic and corticosteroid *use) see below
- Severe or prolonged illness (such as pneumonia and urinary tract infection/ urosepsis/wound infections)

Self Quiz
Ask yourself...
- Why do you think that the number of diabetes cases continues to rise worldwide, despite advances in medication and related treatment options?
- How do you think the healthcare industry can better address diabetic patient education?
- What factors do you think negatively affect the overall health and well-being of persons with diabetes (lack of care, knowledge deficit, health literacy, access to care, costs of care)?
- What can you do as a healthcare professional to improve the health outcomes of patients with diabetes?
Etiology: Precipitating Factors
Common precipitating factors for diabetic ketoacidosis include the following (14):
- Poor compliance with prescribed insulin therapy (intentional, nonintentional)
- Infections (especially T2DM in the elderly/ adult population)
- Newly diagnosed diabetes (especially T1DM in the pediatric/juvenile population)
- Physiologic based stressors, including coronary syndrome, cerebral vascular accidents, ischemic injuries, shock like states, chronic alcoholism, illicit drug use and certain antipsychotic medications.
Etiology: Diabetic Ketoacidosis and Corticosteroid Use
Diabetic ketoacidosis is related to long term corticosteroid usage. yperglycemia has been reported in a large percentage of patients who are using corticosteroids long term, often as high as “64-71%”. The elevated glucose levels combined with the ongoing physiologic stressors warranting use of these medications, increases the risk of DKA. The benefit/risk of using these medications long term must be assessed, especially in patients with pre-existing metabolic risk factors. Ongoing patient monitoring is essential to lower the risk of long-term complications. (15) (16).
Risk factors that “may” increase the likelihood of developing type 2 diabetes after long term steroid usage include the following:
- Overweight (BMI 25.0 -29.9 percent) / obesity (BMI 30 percent or above)
- History of gestational diabetes
- History of polycystic ovarian syndrome
- History of family members with type 2 diabetes

Self Quiz
Ask yourself...
- Your patient, who is recovering from an acute myocardial infarction, has been started on insulin therapy for hyperglycemia. She is adamant that she is “not diabetic” and refuses to take insulin injections. How would you explain to this patient the connection between physiologic stress and hyperglycemia?
- What patient education, regarding insulin and hyperglycemia, would be appropriate for this patient?
- What follow-up care would be appropriate for this patient?
- Would this patient benefit from a referral to a diabetes education/management program at this time?
Treatment
Emergency Treatment
The initial or emergency treatment of diabetic ketoacidosis may require complex, frequent monitoring, often necessitating an intensive care admission. The following generic guidelines refer to intensive care nursing management. Please refer to your specific organization for nursing protocols related to DKA management. Many facilities have strict admission guidelines to ensure the appropriate use of intensive care resources. With respect to patients with DKA, suitable ICU admissions may include the following:
- A newly diagnosed diabetic during an episode of DKA
- Any infectious disease condition that triggers an episode of DKA
- An episode of DKA occurring concurrently with a physiologic stressor event (acute myocardial infarction, cerebrovascular accident/stroke)
The goals of emergency treatment of diabetic ketoacidosis are multifactorial and listed below. Interventions will include, but not be limited to, insulin intravenous infusions, hourly vital sign monitoring (or more frequent), and hourly glucose checks.
- Treatment/correction of dehydration with IV fluids
- Treatment of hyperglycemia with insulin therapy
- Treatment of electrolyte imbalances
- Treatment/correction of acid-base imbalance
Initial/Emergency treatment of DKA includes (20):
- Initial assessment and stabilization ABC airway, breathing and circulation.
- Aggressive fluid therapy to restore circulating volume.
- Isotonic saline IV infusion
- IV with dextrose component once glucose level 200-250mg/dl

Self Quiz
Ask yourself...
- With regards to your current workplace/unit, are there any specific order sets (“standing orders”) for ICU admissions?
- What “standing orders” are currently in place for a suspected diabetic ketoacidosis patient?
- What additional “order sets” would be initiated if a patient with DKA was found to be febrile (102F) with suspected pneumonia?
Laboratory Findings
The following laboratory ranges provide a generic overview of normal ranges and abnormal findings associated with DKA (17) (18) (19). The confirmation of acute diabetic ketoacidosis is dependent on both laboratory findings as well as patient assessment. Please refer to your specific medical organization (unit specific) for further guidance and treatment parameters.
- Serum potassium levels: Normal range (3.5 to 5.0 mEq/L) hyperkalemia range approximately 5.0 to 5.5mEq/L.
- Serum sodium levels: Normal range (137 to 142 mEq/L) severe hyponatremia range approximately 125mEq/L or lower; severe hypernatremia range above 145mE/L
- Serum Amylase level: Normal range (40 to 140 units per liter) (U/L); may be elevated in cases of pancreatitis/ pancreatic inflammation, which may coexist with DKA
- Serum Lipase level: Normal range (0-160 units per liter) (U/L); may be elevated in cases of pancreatitis/ pancreatic inflammation, which may coexist with DKA
- Serum Osmolality level: Normal range 275-295 mOsm/kg: may be elevated to between 300-320 mOsm/kg in DKA
- Arterial blood gas analysis: Arterial ph below 7.3 (normal range 7.35-7.45)
- Anion Gap: Normal 4-12 mEq/L ; levels above > 10 may indicate existing acidosis in DKA
- Serum glucose level (normal fasting below 100mg/dl). Hyperglycemia range above 250mg/dl
- Serum ketone level (normal negative); serum ketones detected in blood; usually greater than 5mEq/L
- Serum bicarbonate level (normal 22-29 mEq/l); usually less than 18mEq/L
- Anion gap level (normal 4-12mmol/L); usually greater than 12 mmol/L)
| Lab Test | Normal Range | DKA | Comment |
| Potassium | 3.5-5.0 mEq/L | >5-5.5 mEq/L and above | |
| Sodium | 137-142mEq/L |
<125mEq/L hyponatremia >145 mEq/L hypernatremia |
|
| Amylase | 40-140 U/L | >140U/L | Elevated with pancreatitis |
| Lipase | 0-160 U/L | >160U/L | Elevated with pancreatitis |
| Arterial PH | 7.35-7.45 | Below 7.3 | |
| Serum Osmolality | 275-295 mOsm/kg | 300-320 mOsm/kg | |
| Anion Gap | 4-12 mEq/L | >10 mEq/L existing DKA |
|
| Glucose | < 100mg/dl | >250mg/dl | |
| Ketone | Negative | >5mEq/L | |
| Bicarbonate | 22-29mEq/L | <18mEq/L | |
| Anion Gap | 4-12mmol/L | >12mmol/L |
To rule out physiologic stressors associated with the development of DKA (systemic infections, acute myocardial infarction, pneumonia, urosepsis), refer to your medical organization (unit specific) guidelines regarding these additional diagnostics:
- Serial blood and wound cultures
- Serial EKG and Troponin levels
- Sputum cultures and sensitivity
- Urinalysis and culture with sensitivity
- Chest Xray
Fluid Resuscitation Guidelines
The American Diabetes Association (ADA) recommends the following initial fluid resuscitation in the adult population; additional boluses may be required after each hourly reassessment: (21). Please refer to your unit specific guidelines regarding fluid boluses, and fluid resuscitation. Caution in use with patients with preexisting heart failure, kidney failure or other medically indicated “fluid restrictions”.
0.9% SC (Sodium Chloride Solution) initially as a 15–20 mL/Kg bolus for hemodynamic resuscitation
- then 250–500 mL/h of fluid until glucose is normalized (usually faster than DKA resolution)
- then 150–250 mL/h until DKA resolution
- For the replenishment, 0.45% SC (Sodium Chloride Solution) unless hyperglycemia-corrected hyponatremia is present.
In the pediatric population, fluid resuscitation boluses are indicated in children who present with the following symptoms: (22)
- Dry mucus membranes
- Poor skin turgor
- Lethargy; altered level of consciousness.
- Nausea and vomiting
- Tachycardia and tachypnea
- Kussmaul type respirations (deep and labored respiratory breathing patterns)
Fluid recommendation: 10–20 mL/kg bolus of isotonic saline given over 30–60 mins.
Insulin Therapy and Acute Diabetic Ketoacidosis
Intravenous use of insulin is preferred in patients with acute diabetic ketoacidosis, as subcutaneous absorption of insulin would most likely be ineffective in light of dehydration.
Intravenous continuous infusion of insulin at a rate of at 0.14 U/kg/hour or
Insulin bolus of 0.1U/kg, followed by insulin continuous infusion at a rate of 0.1U/kg/hour.
Hourly (or more frequent glucose checks) with a decrease in insulin delivery dose when glucose level is 250mg/dl or less. At this time, insulin dose is further decreased to 0.05 or 0.1U/kg hourly until DKA is resolved.
- Patients, once stabilized and deemed able to eat, can be transitioned to subcutaneous insulin administration and routine glucose monitoring (point of care/ POC glucometers)
Laboratory Tests Guidelines Therapy Goals
- Serum glucose levels below 200mg/dl
- Serum bicarbonate level greater than 15mEq/L
- Serum potassium level 4.0 -5.0 mEq/L
- Venous pH greater than 7.30
- Anion gap equal to/less than 12eEq/l. (23)
Electrolyte Imbalance (Hyperkalemia-> Hypokalemia)
Serum potassium levels are usually high/elevated due to the cellular changes occurring as the result of acidosis and decreased insulin. Electrolyte replacement should be monitored very closely in diabetic ketoacidosis. During the rehydration/ volume restoration phase and insulin administration, extracellular potassium shifts back into the intracellular space (causing hypokalemia). In addition, insufficient insulin levels may deplete various serum electrolytes; thus, frequent serum electrolyte levels with appropriate intravenous replacement ensure proper cellular activity.
Treatment-Related Complications
- Hypoglycemia (blood glucose levels below 70mg/dl); treat; accordingly, patient should be transitioned to subcutaneous insulin injections when serum glucose level 200-250mg/dl, and patient is able to tolerate oral intake.
- Hypokalemia (blood potassium levels below 3-3.4 mmol/L); intravenous therapy to include potassium supplements; oral supplements as tolerated once patient transitions to diabetic diet.
- Cerebral edema
Cerebral Edema
Cerebral edema, or brain swelling, occurs for a variety of conditions (brain tumors, blunt trauma, inflammatory conditions, and even infections). Diabetic ketoacidosis and hyponatremia can cause cerebral edema. (24) Cerebral edema is the leading cause of mortality in children. A normal ICP (intracranial pressure) reading is 7-15mmHG; an increased reading in excess of 20-25mmHG, coupled with the following symptoms, may be indicative of cerebral edema.
Initial symptoms of cerebral edema may include the following:
- Headache
- Visual changes (double vision (diplopia) or blurred vision)
- Changes in speech/ ability to talk/ personality.
- Nausea and vomiting
- Changes in level of consciousness (lethargy-> unresponsiveness)
- Changes in respirations/ difficulty breathing
Symptoms that may indicate worsening of cerebral edema.
- decorticate and decerebrate posturing.
- cranial nerve palsies
- fluctuating level of consciousness
- sustained heart rate deceleration,
- increased vomiting, headache, and lethargy
Confirmation Testing:
- CT (Computerized Tomography) scan
- MRI Magnetic Resonance Imaging
Treatment for DKA Related Cerebral Edema
When cerebral edema is confirmed by radiologic testing, the administration of Mannitol (or hypertonic sodium) is recommended as follows (25) (26):
- 0.5-1 g/kg intravenous mannitol may be given over the course of 20 minutes and repeated if no response is seen in 30-120 minutes.
- If no response to mannitol occurs, hypertonic saline (3%) may be given at 5-10 mg/kg over the course of 30 minutes.
- Additional treatments may be warranted, including diuretics, corticosteroids, and possible surgical intervention (to prevent herniation syndrome).

Nursing Care and Management
Nursing Care: Patient Placement
Initial/hourly (or more frequent) assessment to include the following:
Due to the frequency of monitoring and medication administration during the acute phase of DKA, patients are usually placed in the Intensive Care Unit. ICU treatment often includes hourly physical assessments (intake, output, neurological assessment, vital signs; frequent laboratory testing (glucose testing); and rapid identification of complications (cerebral edema, hypoglycemia, hypokalemia).
Transfer to a step-down unit usually occurs when the patient is fully awake, tolerating oral intake (both solid food and liquids), vital signs are stable, and fluid and electrolyte replacements are complete. The average timeline may be 1-2 clinical days. The focus of care now shifts to discharge planning, patient education, and ongoing management.

Self Quiz
Ask yourself...
- What is your current workplace policy of ICU admissions?
- What parameters are used to determine which in-house unit a patient is transferred to?
- Do you feel that patients with acute DKA could be successfully managed on a step-down unit? Why/Why not?
Nursing Care: Acute Phase
- Monitoring of vital signs, level of consciousness/ neurological status, urine output
- Administration of IV fluids as ordered.
- Frequent blood glucose assessment and insulin administration
Nursing Care: Patient Education, Discharge Planning, and Follow-up Care
- Compliance with medications, healthy diet, glucose monitoring, sick day management
- Signs and symptoms of infection
- Importance of follow-up care with primary medical provider/endocrinologist
- Lifestyle behavior changes (smoking cessation, physical activity, healthy diet)
- Medical Alert ID bracelet or wallet insert regarding chronic medical conditions and medication.
- Coordination of follow-up care to ensure ongoing medical support, educational services and financial assistance when appropriate (medical provider, endocrinologist, pharmacist, social worker/ case management services, DSMES classes) (27)
Patient Education
Diabetes Self-Management Education and Support (DSMES)
The Centers for Disease Control and Prevention offer a Diabetes Self-Management Education and Support Toolkit on their website available to the public, designed for various health organizations/ community organizations and others interested in educating persons with diabetes to live a healthier lifestyle. Studies have shown that people who receive such education have better overall health and wellbeing. Despite these studies, a very low percentage of those qualified to receive such services access them. Check out the link below for more information.
- DSMES Program Review: https://www.cdc.gov/diabetes/dsmes/index.html
- DSMES Tooliit: https://www.cdc.gov/diabetes/dsmes-toolkit/index.html
Additional Resources
The following websites are being provided to assist the healthcare professional in accessing appropriate diabetes related information, including insulin coverage, food insecurities, food bank locations, and DSMES information. https://diabetes.org/
The American Diabetes Association provides information on prediabetes, Type 1, and Type 2 diabetes, as well as gestational diabetes. Included on their website are sections on medications, support groups, diet and activity, advocacy efforts, and prevention efforts. https://www.jdrf.org/
The Juvenile Diabetes Research Foundation is a global organization for Type 1 diabetes mellitus. The site offers information on all things T1DM, including sections for those newly diagnosed, those interested in fundraising, research and clinical trials, daily diabetes management, volunteer opportunities, and access to local chapters worldwide. From the healthcare provider perspective, this website offers continuing education programs and pdf downloads for patient specific education. https://getinsulin.org/
The Get Insulin website provides information for persons with diabetes to access affordable insulin coverage. The site also offers information and guidance on health insurance plans, an insulin related newsletter, and external links to food sources (for patients with food insecurity issues) https://www.feedingamerica.org/find-your-local-foodbank
The Feeding America website enables persons with food insecurities to access food banks in their area, according to state location and zip code.

Self Quiz
Ask yourself...
- What community resources are available to your patients, post discharge, regarding access to food and medications?
- If your patient says they simply cannot afford their prescriptions, what is your current facility policy regarding this matter?
- How would you improve your current facility policy regarding patient access to medications for those uninsured/underinsured?
Patient Education and Follow-up Care (DSMES)
DSMES, or Diabetes Self-Management Education and Support, is the gold standard when it comes to patient education on this chronic medical condition. The goal of this education is to educate and empower the patient to successfully manage their medical condition, in efforts to lower the risk of long term, lifetime complications. DSMES is considered an ongoing process, and is recognized as an integral part of patient education at various critical points in their lifetime:
- At time of initial diagnosis
- During all patient medical appointments and routine follow-up care
- At time of onset for newly diagnosed complications
- Anytime a patient expresses concern over current diabetic management challenges.
Medicare and Medicaid
Medicare (Medicare Part B) and Medicaid plans currently offer the following coverage for diabetes related education (28):
- 10 hours of education (combined individual and group training) for an initial diagnosis of diabetes
- 2 hours of follow-up training annually after initial training completion
Qualifying Labs for DSMES
In general, a patient must be diagnosed with type 1, type 2, or gestational diabetes to qualify for DSMES, such as:
- Fasting Blood glucose of 126 mg/dL on 2 separate occasions
- 2-hour Post-Glucose Challenge of ≥200 mg/dL on 2 separate occasions
- Random Glucose Test of >200 mg/dL with symptoms of unmanaged diabetes
DSME Contents Overview
- Diabetes disease process pathophysiology and treatment to increase risk reduction for long term complications.
- Healthy eating includes meal planning, food label reading, carbohydrate counting, and strategies for eating out.
- Physical activity includes the benefits of activity as they related to better weight control, sleep habits and stress reduction.
- Medication usage overview to include medication administration, side effects, storage and cost issues.
- Blood glucose monitoring and management to include proper use of monitoring devices and associated equipment cleaning/repair.
- Prevention of complications (early detection, treatment, acute and chronic complications such as kidney disease and nerve damage; proper foot care)
- Healthy coping strategies to include stress reduction, effective self-management behaviors, and symptom recognition (hypoglycemia/hyperglycemia)
- Sick day management includes intake/output monitoring, over the counter medication usage, carbohydrate counting, ketone assessment, fever control and when to seek emergency services.
- Problem solving to include diabetes management during emergencies (power outages, flooding, tornados, hurricanes)
For more DSMES information visit: https://www.cdc.gov/diabetes/dsmes/dsmes-living-with-diabetes.html


Self Quiz
Ask yourself...
- With respect to DKA, what aspects of DSMES do you think are most important for patient education?
- How do you assess health literacy in your patients?
- What are some nursing interventions that could be done to assess a patient’s ability to correctly use a glucometer (glucose measuring device)?
- What community resources, post hospital discharge, are available for newly diagnosed patients with prediabetes/ type 2 diabetes in your area?
- What aspect of DSMES do you consider most important for ongoing sick day management education for your patients with diabetes?
Safety Considerations (Sick Day Management)
Successful management (prevention) of diabetic ketoacidosis requires patient education and empowerment in managing situations where glucose levels may be elevated and/or insulin levels (doses) are substandard (29).
There are many situations that can put a patient at risk for the development of DKA, including the following (29):
- Illness (acute and chronic), affecting normal food and fluid intake which negatively affects glucose management.
- Missed medication (insulin therapy) due to a clogged insulin pump tubing, a malfunctioning insulin pump, partial doses/skipped doses of insulin (whether related to costs, cognition, or mental health issues {diabetes distress}),
- Medication side effects
- Concurrent use of alcohol or drugs
- Physiologic stress (heart attack, stroke, physical injury)
Patient Education: Sick Day Management
Home treatment/ self-care (30)
The importance of preplanning cannot be understated. All persons with diabetes should have adequate supplies at home, to address an acute illness, including medications to treat basic symptoms before they escalate. These medications may include over the counter medications to treat pain, nausea, vomiting, diarrhea, as well as adequate supplies to manage their diabetes (alcohol prep pads, syringes, prescription medications).
In addition, it is important to stock up on diabetic friendly foods and drinks to maintain nutrition and hydration levels during an acute illness. Such items might include sports drinks, soft drinks, instant cooked cereals, puddings, soups. In the event that a patient cannot eat their regular meals, the goal is to eat or drink 50 grams of carbohydrate every 4 hours to maintain glucose levels.
Sick Day Management Guidelines
- Monitor glucose levels every 4 hours.
- Stay hydrated – 4 to 6 ounces of fluid every ½ hour to prevent dehydration.
- Daily weight
- Temperature checks (rule out underlying infection)
- Current medication compliance- do not stop taking insulin or diabetic oral agents ** notify provider immediately if you choose to stop medications.
Seek emergency care for the following signs/ symptoms:
- Persistent vomiting/diarrhea to the point that you cannot tolerate any food or fluid intake for several hours
- Ongoing glucose levels above 240mg/dl
- The presence of moderate/high levels of ketones in urine
- Unexplained weight loss during an illness
- Any difficulty breathing
- Fruity/acetone smell on breath
- Changes in gait/balance/ vision
Research Findings
Research: Diabetes Distress and Burnout
Diabetes is a 24/7/365 chronic medical condition. Unlike many conditions that are simply managed with lifestyle changes or a single, once a day medication regimen, diabetes mellitus requires lifelong, around the clock commitment. Whether diet, activity, or medication management, a person with diabetes may easily feel overwhelmed by even the basic requirements for self-management. (31)
Ongoing health challenges, comorbid medical conditions, medication and diet cost issues and family dynamics can all affect a person’s ability to successfully manage any health condition. When emotions (sadness, anger, hostility, frustration, and even fear) become overwhelming, diabetic distress (a feeling of defeat) can often occur. Without prompt, patient specific interventions (mental health services, financial assistance, self-management education), these feeling will progress to diabetic burnout, and increase the risk of unhealthy habits (poor medication adherence and overall glycemic control). (32)
Diabetes distress can easily progress to diabetes burnout without appropriate ongoing medical treatment and mental health interventions. When a person with diabetes reaches the point of burnout, they often appear to disconnect from their routine healthcare, exhibiting indifference towards their overall health and well-being. They may become both mentally and physically exhausted from the daily requirements of this chronic medical condition. At this point, it is not uncommon to observe a person’s total disregard for their ongoing medical treatments, daily medications, routine self-care, and more. Missed medications, missed medical appointments, poor dietary intake, and a visible lack of basic hygienic practices are cause for concern.
A multidisciplinary approach to treating suspected diabetic distress and burnout is highly encouraged. From ongoing education, physical and mental health assessments, and enrollment in therapies (individual therapy sessions, and support groups), the person with diabetes needs a supportive environment in which to become empowered in the self-management of their disease progress. In doing so, it is believed that health outcomes are optimal, and the risk of long-term complications is lowered. (33)

Self Quiz
Ask yourself...
- Why do you think diabetes related distress occurs?
- What external factors affect a person’s ability to manage their diabetes successfully?
- What nursing education can you provide to possibly decrease the likelihood of diabetes distress?
- What areas of discharge planning/discharge instructions and follow-up care positively impact a person’s ability to manage their chronic medical condition?
Reserach: Diabulimia
Bulimia nervosa is a potentially life-threatening eating disorder characterized by episodic binge eating of large amounts of food, followed by forced vomiting and possibly laxative use to then “purge” the food. These alternating behaviors are the result of a person fearful of weight gain and willingness to lose weight in unhealthy ways. (34) (35)
Diabulimia is a serious, life threatening eating disorder affecting persons with Type 1 diabetes. Through intentional restricted/ limited use of prescribed insulin, weight loss occurs. This eating disorder is more common in young female adolescents and young adults. (34) (35)
Signs and symptoms may include the following (34) (35):
- Unexplained weight loss
- Hemoglobin A1C > 9
- Multiple episodes of DKA
- Unfilled insulin prescriptions, missed diabetes related medical appointments,
- Expressed fear of insulin related weight gain
- Anxiety related to body image
- Obsessive interest in calories and dieting

Self Quiz
Ask yourself...
- How would you approach patient education with someone you suspect might be suffering from diabulimia?
- What might be some reasons for repeated DKA related incidents, unrelated to intentional restriction of insulin usage?
- How might you encourage a patient to improve compliance with routine medical appointments/ follow-up care?
- How would you respond to a patient’s concerning comment that “insulin is making me gain unwanted weight”?
- What consultations and referrals/resources would be appropriate for discharge planning of patients with suspected diabulimia?

Self Quiz
Ask yourself...
- How would you approach patient education with someone you suspect might be suffering from diabulimia?
- What might be some reasons for repeated DKA related incidents, unrelated to intentional restriction of insulin usage?
- How might you encourage a patient to improve compliance with routine medical appointments/ follow-up care?
- How would you respond to a patient’s concerning comment that “insulin is making me gain unwanted weight”?
- What consultations and referrals/resources would be appropriate for discharge planning of patients with suspected diabulimia?
Research: Insulin Affordability
For many persons with diabetes, the perceived noncompliance with therapy (on behalf of the healthcare professional) is actually that of a cost related issue. Many persons cannot afford ongoing therapies related to management of this chronic medical condition. In attempts to “cut costs”, patients have admitted to skipping certain medications, cutting medications in half, reducing prescribed doses of insulin, and purchasing poorer quality, less expensive foods (that are often lacking in nutritional value). Poorly controlled / uncontrolled diabetes heightens the risk of both acute and chronic complications.
In an attempt to ensure accessibility and affordability of insulin therapy to persons with diabetes, the Inflation Reduction Act of 2022 in part ensures that persons with diabetes on Medicare pay no more than $35 for a month’s supply of insulin product under their prescription drug coverage. Similar drug coverage benefits were also extended to many state-based insurance plans. (36)
In addition, most Medicaid insurance plans, as well as private insurance companies have now enacted reduced insulin costs/ cost sharing programs. Finally, for patients with no insulin costs benefits, many national insurance providers offer free/ reduced cost insulin through their patient assistance program. For a comprehensive list of these resources, please see the following website link (American Diabetes Association): https://diabetes.org/tools-resources/affordable-insulin
Research: Insulin Delivery Systems
With the creation of advanced insulin delivery /monitoring devices (insulin pumps, and continuous glucose monitoring devices), the person with diabetes is afforded a more streamlined process to control their chronic medical condition. Most patients using such devices report better glucose control {“time in range”}, meaning the time their blood glucose levels remained in an acceptable range, ease of portability (of supplies), increased comfort (no more finger sticks), and decreased rates of anxiety, depression and distress.
The following website links represent various insulin delivery devices. Consider making a resource book containing various delivery devices for your specific unit (or hospital organization). Many have 24/7 customer service representatives available if you need to trouble shoot a device suspected of malfunctioning or require additional staff/patient educational resources.
This list contains a variety of websites but is not all inclusive. If you are caring for a patient with an insulin delivery device in place, please contact that specific company for more directions on its usage, removal, replacement parts and more.
Examples of insulin delivery devices:
- Makers of the MiniMed 780G System and the MiniMed 630G system: https://www.medtronic.com/us-en/healthcare-professionals/products/diabetes/insulin-pump-systems.html
- Makers of the Omnipod 5 and the Omnipod DASH Insulin Management System: https://www.omnipod.com/
- Quick overview of various insulin pumps currently on the market: https://consumerguide.diabetes.org/collections/pumps


Self Quiz
Ask yourself...
- What is your facility’s current policy on patient admissions for DKA that want to wear their insulin pumps while in the hospital?
- Would you feel comfortable allowing a Type 1 diabetes patient, admitted for a medical condition unrelated to diabetes, to continue wearing their insulin pump during their hospital stay? Why/Why not?
Case Studies
Case Study #1
A 3-year-old female child is sent, by ambulance, from her local pediatrician’s office with reports of increased lethargy, increased thirst and appetite, and new onset of bedwetting (child had stopped wearing diapers at age 2.5 years). Parents report that the child’s appetite appears increased lately, but pediatrician noted several pounds weight loss since last visit.
- Based on these signs and symptoms alone, what is your initial diagnosis for this child?
- What are your priority nursing interventions for this child?
- How would you assess hydration status on a 3-year-old child?
The child is diagnosed with new onset Type 1 Diabetes and stabilized in the Emergency Department. The parents of this child are visibly distraught over the diagnosis, stating “no one in our family is diabetic; this can’t be happening”.
- What are some of the initial nursing patient/family education areas you could address at this time?
- What are some in hospital consultations that should be considered for this patient and her family?
- What are some community resources you have in your area that you could offer this family?
Case Study #2
A 78-year-old female, with a previous history of CVA, is transferred to your facility from a local nursing home for evaluation of fever and hyperglycemia. The nursing home staff reported the patients’ blood glucose level was 400mg/dl earlier today and her WBC count was 14,500. Upon arrival, the patient is unresponsive, with a temperature 102F , her glucose is 350mg/dl, with +ketones (moderate) and a urinalysis (indwelling catheter) confirms a UTI.
Patient past medical history includes old CVA, T2DM.
- Based on these signs and symptoms alone, what is your initial diagnosis for this patient?
- What diagnostic studies would be warranted in light of hyperglycemia, fever, urinary tract infection, and altered level of consciousness?
- What questions would you ask the nursing home staff, in light of this patient’s initial presentation?
- When this patient is stabilized for transfer back to the nursing home, what information should be included in the discharge instructions/ transfer of care?
Case Study #3
A 60-year-old male present to the Emergency Department with an Acute Myocardial Infarction.
Patient past medical history includes borderline hypertension, and prediabetic HgbA1C 5.8.
The patient was found to have severe coronary artery disease and received Coronary Artery Bypass Graft x 3. During the immediate post operative recovery phase, he receives insulin therapy to control glucose levels >300mg/dl. He is eventually sent home on insulin therapy, pending follow-up with his cardiologist as well as a new consultation for an endocrinologist.
At the time of discharge, the patient is adamant that he was “prediabetic and could easily control my glucose levels with diet alone”; he doesn’t understand how he is now “an insulin diabetic”.
- What are key points in nursing education for this patient, regarding his new “diabetic status”
- How would you explain to the patient the connection between his myocardial infarction, bypass surgery, and currently elevated glucose levels?
- What nursing interventions can you provide PRIOR to discharge to assess his comfort level with insulin injections and glucose monitoring?
- What community resources are available to your patient for a new diagnosis of diabetes?
- The patient wants to know when he can stop the insulin injections. What is your response?
Successful management of acute diabetic ketoacidosis requires resuscitation with intravenous fluids and insulin therapy, replacement of electrolytes and early identification of any events (medical, surgical, and psychological) that contributed to this medical emergency. With the continued increase in diagnosis of diabetes, and ongoing challenges in healthcare costs and coverage, chronic medical conditions will continue to burden the already overwhelmed healthcare arena. By educating and empowering patients to self-manage their disease process, we can lower the risk of long-term complications and improve health outcomes worldwide.
Conclusion
The International Diabetes Federation reports that, in 2021, approximately 10.5 % of the global adult population (ages 20-79 years old) has diabetes, and that nearly 50% of this population are unaware that they are living with this chronic condition. Left untreated, the rates of long-term, nonreversible complications are quite alarming. (37) By the year 2045, it is projected that 1 in every 8 persons (approximately 12.5 %) will be living with diabetes. This will equate to an increase of 46 percent, with nearly 783 million people being affected. This single health condition will represent staggering health expenditures and increased mortality and morbidity associated rates worldwide.
Diabetes ketoacidosis continues to be a potentially life-threatening complication for persons with diabetes. DKA is also, in most cases, a highly preventable condition, with early identification and treatment. The importance of ongoing, patient specific education to address all aspects of diabetes self-management is a key factor in lowering the occurrence of DKA. Dr William Polonsky, a licensed clinical psychologist and certified diabetes educator, is the President of the Behavioral Diabetes Institute in San Diego, California. With regards to the importance of patient education and empowerment, he said the following:
“Well-controlled diabetes is the leading cause of nothing!” Dr William Polonsky. (38)
As healthcare professionals, we have the responsibility to ensure that our patients with diabetes are afforded the education and ongoing support necessary for them to successfully manage their specific disease process. In doing so, we positively impact patient satisfaction, improve medication adherence rates, and lower the risk of long-term complications.

Self Quiz
Ask yourself...
- Why do you think persons with diabetes become “noncompliant” with their diabetes medications?
- What nursing interventions may increase/improve medication compliance rates?
- What community resources are available in your area to assist those who cannot afford their prescribed medications?
- If a patient tells you they simply cannot afford their medications, what resources are available at your place of employment to assist such financial concerns?
- Have you identified any barriers to patient education at your healthcare organization?
- How will your practice change after reading this course?
Heart Disease Prevention & Management
Introduction
Heart disease is an umbrella term encompassing a range of cardiovascular conditions, and stands as the leading cause of death worldwide, claiming millions of lives. Both heart disease and stroke are types of cardiovascular disease. The impact of heart disease transcends individual health, posing a significant economic burden through reduced labor and workforce participation. In 2018, the mean labor income losses were $13,463 for heart disease and $18,716 for stroke. Total labor income losses were estimated at $203.3 billion for heart disease and $63.6 billion for stroke [1].
Heart disease manifests in various forms, each with its unique characteristics and implications. Coronary artery disease, the most common type, arises from the buildup of plaque in the coronary arteries [2]. This narrowing can restrict blood flow to the heart, causing symptoms such as chest pain or shortness of breath [2]. Other prevalent forms include heart failure, rhythm abnormalities, heart valve defects, and congenital heart defects [4]. These conditions can lead to a spectrum of complications, including heart attacks, strokes, and heart failure, significantly impairing quality of life and survival [3]. By understanding the underlying mechanisms, risk factors, and clinical presentations of heart disease, participants will gain a deeper understanding of the disease's impact on the cardiovascular system and overall health.
Prevention, the cornerstone of combating heart disease, will be a central focus. Participants will explore lifestyle modifications that play a pivotal role in reducing the risk of heart disease, including diet, physical activity, weight management, smoking cessation, and stress reduction. Identification and management of risk factors, such as high blood pressure, high cholesterol, and diabetes, is prioritized.

Self Quiz
Ask yourself...
- Why is understanding the underlying mechanisms of heart disease important for prevention and management?
- How can lifestyle modifications, such as diet, physical activity, and stress reduction, play a crucial role in preventing heart disease?
Types of Heart Disease
Heart disease encompasses a spectrum of conditions, each with unique underlying mechanisms and dietary management strategies [5]. Coronary artery disease (CAD), heart failure (HF), hypertensive heart disease (HTN), and arrhythmias constitute a significant portion of these prevalent ailments. Coronary artery disease (CAD) is the most common type of heart disease [6]. The four main types of cardiovascular disease (CVD) include coronary heart disease, stroke, peripheral arterial disease, and aortic disease [7]. Cerebrovascular disease is the second most common type of heart disease [7]. Other forms of heart disease include congenital heart disease, heart valve disease, cardiomyopathy, pericardial disease, arrhythmia, and aortic dissection.
Congenital heart disease (CHD)
Congenital heart disease (CHD) is the most common type of birth defect, affecting about one in 100 babies born in the United States [8]. CHDs can range from mild to severe and can affect the heart's structure, function, or both [8].
Heart Valve Disease
Heart valve disease is a condition in which one or more of the heart valves are damaged or diseased which causes blood to flow backward through the valves, damaging the heart and other organs [9]. Heart valve disease affects 2.5% of the U.S population and can be caused by several factors, including infection, injury, and aging [9].
Heart Failure
Heart failure is a condition in which the heart's weakened pump fails to meet the body's demands for blood and oxygen, leading to a range of debilitating symptoms including fatigue, shortness of breath, swelling, chest pain, palpitations, weight gain, swelling in the ankles, legs, and abdomen, bloated or hard stomach, dry hacking cough, and nausea [10][11]. More than six million adults in the U.S. have heart failure [10].
Cardiomyopathy
Cardiomyopathy represents a collection of diverse conditions of the heart which makes it weaker and less able to pump blood. Cardiomyopathy can be caused by several factors, including infection, toxins, and genetic disorders [12]. Due to the potential for underdiagnosis, estimates of cardiomyopathy prevalence can vary. It is estimated that up to one in 500 adults may be affected by this condition [13].
Pericardial Disease
Pericardial disease is a condition that affects the pericardium, the sac that surrounds the heart [14]. This can cause inflammation, infection, or scarring of the pericardium, which can interfere with the heart's ability to function. Pericardial disease can manifest as acute pericarditis, pericardial effusion, cardiac tamponade, or constrictive pericarditis [14].
Arrhythmia
Arrhythmia is a cardiac disorder characterized by an abnormal heart rhythm, manifesting as tachycardia (excessively rapid heartbeat), bradycardia (abnormally slow heartbeat), or irregular heartbeat patterns [15]. These irregularities can induce symptoms such as palpitations, dizziness, and syncope (fainting episodes) and can arise from various etiologies, including underlying heart conditions, electrolyte imbalances, and adverse effects of certain medications [15].
One in 18 people, or five percent of the U.S. population has an arrhythmia with afib (atrial fibrillation) being the most common [16].
Aortic Dissection
Aortic dissection is a rare, life-threatening condition in which the inner layer of the body’s main artery (aorta), tears [17]. This can cause blood to leak between the layers of the aorta, which can weaken the artery and cause it to rupture. Aortic dissection can be caused by several factors including high blood pressure, atherosclerosis, and connective tissue disorders [17]. Aortic dissection affects about 30 in one million people each year and more than 13,000 die each year [18]. Aortic dissection is most common in individuals over the age of 60 and if not treated, the tear can worsen, ripping the outer layer of the aorta, allowing blood to escape the artery [17] [18]. As many as 40 percent of individuals who suffer from an aortic dissection die, and the risk of death increases by 3-4 percent every hour the condition is left untreated [18].


Self Quiz
Ask yourself...
- Given the diverse range of heart disease conditions, what common underlying mechanisms contribute to their development?
- Considering the various forms of heart disease, what dietary management strategies can be tailored to address specific risk factors and nutritional needs?
- Given the potential for underdiagnosis of certain heart disease conditions, what screening and diagnostic measures can be employed to ensure early detection and intervention?
Epidemiology/Statistical Evidence
Heart disease is a global health crisis, with an estimated 17.9 million deaths attributed to cardiovascular diseases in 2019, representing 32% of all global deaths [19]. This significant number reflects the pervasive nature of heart disease, affecting individuals of all ages, socioeconomic backgrounds, and ethnicities. The distribution and determinants of heart disease plays a pivotal role in understanding the prevalence. Heart disease varies across regions, with higher rates observed in high-income countries compared to low-income countries [20]. However, the burden of heart disease is shifting, with a growing trend in low-income countries due to rapid urbanization, lifestyle changes, and increasing exposure to risk factors [20].
Epidemiology: Modifiable and Non-Modifiable Risk Factors
Epidemiological studies with data from 61 cohort studies, encompassing 12.7 million person-years of follow-up and 56,000 fatalities from coronary heart disease (CHD) and stroke revealed a consistent and graded increase in CVD risk. The risk was associated with higher baseline systolic blood pressure (SBP) and diastolic blood pressure (DBP) levels beyond the usual thresholds of 115 and 75 mmHg. A 20-mmHg elevation in SBP and a 10 mmHg increase in DBP was associated with a two-fold higher risk of CVD [21].
Cardiovascular disease (CVD) is a leading cause of morbidity and mortality in individuals with type 2 diabetes mellitus (T2DM). This increased risk stems from a complex interplay of traditional and non-traditional risk factors that contribute to the initiation and progression of atherosclerosis, a pathological process characterized by the buildup of plaque within artery walls [22].
The epidemiology of heart disease involves recognizing the associated risk factors. These can be categorized into modifiable and non-modifiable factors. Modifiable risk factors include hypertension, high cholesterol, smoking, obesity, diabetes, physical inactivity, and poor diet [23]. Non-modifiable risk factors include age, gender, and family history [23]. According to the American Heart Association (AHA), the likelihood of developing CVD in U.S. men and women is 40% between the ages of 40 and 59, 75% between 60 and 79, and 86% for those over the age of 80 [24].
Statistics on Ethnic/Racial Minorities
Patients from minority groups with acute coronary syndrome (ACS) are at an increased risk of heart attack (MI), readmission to the hospital, and death from ACS [25]. Black/African Americans are at 30% increased risk of heart disease and death from heart disease and double the risk of stroke with a higher risk of developing heart failure [25]. Among Asian Americans /Pacific Islanders, coronary artery disease (CAD) manifests earlier in life and affects a larger proportion of the population compared to other ethnic groups [25]. Overall CVD rates are lower among non-White Hispanic individuals. Among Hispanic subgroups, Puerto Rican Americans exhibit the highest HTN-related death rates [25]. Heart failure incidence among Hispanics falls between that of African Americans and non-Hispanic whites [25].
Epidemiology: Genetic and Environmental Factors
The development of heart disease is influenced by a complex interplay of genetic and environmental factors [26]. Major risk factors include sustained high blood pressure placing excessive strain on the heart, increasing the risk of heart failure, stroke, and other complications [27]. Elevated levels of low-density lipoprotein (LDL) cholesterol can accumulate in arteries, narrowing and reducing blood flow to the heart [28].
Diabetes mellitus, characterized by high blood sugar levels that damage blood vessels and nerves throughout the body, increases the risk of heart disease and stroke [29]. Tobacco contributes to atherosclerosis – the buildup of plaque in arteries – through a cascade of mechanisms that lead to atherosclerosis, including thrombosis, insulin resistance, dyslipidemia, vascular inflammation, abnormal vascular growth, angiogenesis, and impaired endothelial repair and regeneration [30] [50].
Obesity and excess abdominal fat can increase the risk of heart disease by elevating blood pressure, cholesterol levels, and blood sugar levels [27]. A lack of regular physical activity contributes to obesity, high blood pressure, and other risk factors for heart disease [31]. A family history of heart disease increases an individual's risk, indicating a genetic predisposition to the condition [32].

Self Quiz
Ask yourself...
- Despite the global prevalence of heart disease, why do we observe variations in its distribution across different regions?
- How do modifiable and non-modifiable risk factors contribute to the development and progression of heart disease?
- How do socioeconomic disparities and minority status influence the prevalence and outcomes of heart disease?
- How does the interplay of genetic and environmental factors contribute to the development of heart disease?
Prevention Strategies
Prevention for heart disease begins with addressing modifiable risk factors with an emphasis on diet, exercise, smoking cessation, and stress management. Prevention also involves regular health screenings.
Key prevention strategies include:
- Adopting a Heart-Healthy Diet consisting of fruits, vegetables, and whole grains, and limiting saturated and trans fats, sodium, and added sugars [33].
- Maintaining a healthy weight through a balanced diet and regular exercise [23].
- Engaging in regular physical activity for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week [34].
- Participating in smoking cessation, managing high blood pressure, and working with healthcare providers to manage cholesterol levels through lifestyle changes or medication [23].

Self Quiz
Ask yourself...
- Given the emphasis on modifiable risk factors in heart disease prevention, how can individuals make informed and sustainable lifestyle changes to reduce their risk?
- Considering the importance of regular health screenings in heart disease prevention, how can we increase access to and adherence with screening recommendations?
Patient Education for Self-Management
Patient education for self-management plays a vital role in preventing and managing heart disease. Healthcare professionals should begin by conducting a thorough assessment of each patient, considering their unique risk factors, medical history, and lifestyle choices related to heart disease and develop a personalized self-management plan that align with the patient's specific needs and objectives [35].
Provide clear and concise information about heart disease, its risk factors, and prevention strategies, and address individual needs and concerns, with consideration of cultural background, lifestyle, and any underlying health conditions. Effective communication is paramount in this process. Health care professionals should employ strong communication skills to establish a meaningful connection and foster open and honest dialogue, active listening, and demonstration of empathy to gain insight into their preferences [36].
To cater to diverse learning styles, it is essential to offer educational materials in various formats [37]. Tailor the educational approach to each patient's learning style, using plain language, visual aids, and active participation strategies. Involve the patient in setting realistic and achievable self-management goals [38]. These resources may encompass brochures, videos, or online materials. It is imperative that these materials are designed to be comprehensible and sensitive to cultural differences.
Patients must be educated about modifiable risk factors that pertain to heart disease prevention [23]. This includes discussions on dietary choices, physical activity, smoking cessation, and responsible alcohol consumption [23]. Furthermore, healthcare professionals should articulate the significance of adhering to prescribed medications to manage cardiovascular conditions.


Self Quiz
Ask yourself...
- How can healthcare professionals tailor patient education for self-management of heart disease, considering the diverse needs and preferences of their patients?
- How can healthcare professionals communicate the importance of adhering to prescribed medications and lifestyle modifications for managing heart disease and preventing complications?
Medical Management and Treatment
In addition to lifestyle modifications, healthcare providers can prescribe medications to treat heart disease [23]. The common medications used to treat heart disease include antihypertensive medications to lower blood pressure, antihyperlipidemic medications to lower cholesterol levels, and antiplatelet medications to prevent blood clots [40]. Beta-blockers are used to slow the heart rate and lower blood pressure and angiotensin-converting enzyme (ACE) inhibitors are used to lower blood pressure and relax blood vessels. Angiotensin II receptor blockers (ARBs) are prescribed to lower blood pressure and relax blood vessels [41].
In some cases, invasive medical procedures may be required to treat heart disease. The common types of medical procedures used to treat heart disease include coronary angioplasty to open blocked or narrowed coronary arteries, and coronary artery bypass grafting (CABG) to create a new pathway for blood to flow around blocked or narrowed coronary arteries [39][42]. Other common procedures are heart valve surgery to repair or replace damaged heart valves, implantable cardioverter-defibrillators (ICD) to monitor the heart rhythm and deliver electrical shocks to correct abnormal heart rhythms, and implantable pacemakers to help control the heart rhythm [43].

Self Quiz
Ask yourself...
- In what ways do the different pharmacological treatments for heart disease address the underlying mechanisms and risk factors associated with the condition?
- How do invasive medical procedures, such as angioplasty and bypass surgery, address the structural abnormalities and blood flow limitations associated with heart disease?
- What factors are considered when determining whether pharmacological or surgical interventions are the most appropriate treatment approach for heart disease?
Heart Health Resources
Resources for heart disease prevention and management are essential for both healthcare professionals and patients. These resources encompass a wide range of tools, information, and support systems that play a crucial role in reducing the risk and managing heart disease.
Educational Materials/Content
Information is key to prevention and management. Patients and healthcare providers can access pamphlets, brochures, websites, and educational videos that explain the causes, risk factors, symptoms, and treatment options for heart disease [44]. These resources empower individuals to make informed decisions about their heart health. [44].
Patients can benefit from resources that offer guidance on Heart-Healthy diets, including low-sodium meal plans, tips for reducing saturated fats, and strategies for incorporating more fruits and vegetables into their meals.
Published Guidelines
Medical organizations and government health agencies publish guidelines for heart disease prevention. These guidelines provide evidence-based recommendations for diet, exercise, smoking cessation, and medication management, with proper nutrition being a cornerstone of heart disease prevention and management [33].
Support Groups
Support groups provide a platform for individuals with heart disease to connect, share experiences, and receive emotional support [45]. These groups can be in-person or online and offer a sense of community for patients and their families [45].
Technological Advancements
Telehealth has become important in managing chronic conditions such as heart disease [46]. Patients can access virtual consultations with healthcare providers, receive remote monitoring, and access educational materials online. Smartphone apps and wearable devices can help individuals track their health metrics, such as blood pressure, heart rate, and physical activity [47]. Many of these tools provide real-time feedback and reminders to support heart-healthy habits.
Nonprofit Organizations
Nonprofit organizations dedicated to heart health advocacy, such as the American Heart Association, offer a wealth of resources. The American Heart Association (AHA) is a leading organization for heart disease research and education [48]. The National Heart, Lung, and Blood Institute (NHLBI) is a part of the National Institutes of Health (NIH) and offers information on heart disease prevention and management, as well as clinical trials and research studies [49].

Self Quiz
Ask yourself...
- How can healthcare providers utilize available resources to educate and empower patients in making informed decisions about their heart health?
- How can nurses help patients navigate the abundance of resources available and choose those that align with their specific needs and preferences?
Conclusion
Heart disease encompasses a spectrum of conditions with diverse underlying mechanisms and management strategies. Modifiable risk factors, including diet, exercise, smoking cessation, and stress management, play a crucial role in both prevention and management [23]. Resources for heart disease prevention and management empower individuals to take control of their heart health. These resources span from educational materials and support groups to telehealth platforms and smartphone apps, providing comprehensive guidance and support for both patients and healthcare professionals [44][45].

Self Quiz
Ask yourself...
- Why is early detection and intervention crucial for improving outcomes in heart disease?
- How can healthcare professionals advocate for the implementation of preventive measures at the community and population levels to combat the burden of heart disease?
Nutrition for a Healthy Heart
Introduction
Research indicates that a heart-healthy diet is a powerful tool for the prevention and control of cardiovascular disease [1]. A heart-healthy dietary approach to wellness emphasizes the intake of the appropriate proportions of macronutrients, essential vitamins, minerals, and fiber while minimizing the consumption of saturated fats, trans fats, cholesterol, salt (sodium), and the reduction of processed foods, trans-fats, and added sugars [2] [3]. The cornerstone of the diet includes an abundance of fresh fruits and vegetables, whole grains, lean proteins, and healthy fats [2].
For healthcare providers and patients, the goal of adopting a heart-healthy diet is multifaceted. The diet aims for a reduction in overall cardiometabolic risk, improving blood pressure, lowering cholesterol levels, reducing the risk of developing heart disease and stroke, and preserving the overall health of the circulatory system [3].
Nurses play a pivotal role in patient education and promoting heart-healthy lifestyles by empowering patients with knowledge and skills related to nutrition and dietary choices. This course aims to equip nurses with comprehensive knowledge of heart-healthy eating principles, enabling them to guide and educate their patients.
The adoption of healthy lifestyle choices, with nutrition being the most important behavioral factor, is estimated to reduce the risk of myocardial infarction (MI) by 81–94% [5][6][7]. In comparison, treatment with pharmacotherapies alone results in a 20–30% reduction [8].


Self Quiz
Ask yourself...
- Why is nutrition considered the most important behavioral factor in reducing the risk of myocardial infarction (MI) compared to pharmacotherapies alone?
Heart Disease: A Brief Overview
Heart disease remains one of the leading causes of morbidity and mortality worldwide, with diet and nutrition playing a crucial role in both its development and prevention [4]. Cardiovascular diseases, also known as CVDs, are the primary cause of death worldwide, claiming an estimated 17.9 million lives per year [4].
Cardiovascular disorders affect the heart and blood vessels, manifesting in coronary heart disease, cerebrovascular disease, rheumatic heart disease, and others. More than four out of five CVD fatalities stem from heart attacks and strokes, with one-third of these deaths occurring in individuals under the age of 70 [4].
The term "heart disease" encompasses various conditions affecting the heart's structure and function, many of which are influenced by dietary habits [9]. Cardiovascular risk factors, including malnutrition, tobacco and alcohol use, stress, obesity, sedentary lifestyle, hypertension, diabetes, hyperlipidemia, and genetic predisposition, can increase an individual's likelihood of developing cardiovascular diseases [10] [12].
The modifiable risk factors include sedentary lifestyle, smoking, high blood pressure, diabetes, hypercholesterolemia [12]. Almost three quarters of patients (73%) had at least three risk factors compared to 31% of healthy subjects.
Family history of cardiovascular disease (CVD) is a significant independent risk factor for premature coronary heart disease (CHD). The risk of premature CHD increases in a linear fashion as the number of affected family members grows. [11]. Cardiovascular risk factors, including malnutrition, tobacco and alcohol use, stress, obesity, sedentary lifestyle, hypertension, diabetes, hyperlipidemia, and genetic predisposition, can increase an individual's likelihood of developing cardiovascular diseases [10].
The five modifiable risk factors include sedentary lifestyle, smoking, high blood pressure, diabetes, and hypercholesterolemia [10]. A higher proportion of cardiovascular patients (73%) had at least three risk factors compared to healthy individuals, where less than one-third had three or more risk factors [10].

Self Quiz
Ask yourself...
- What are the key dietary factors that contribute to the development of cardiovascular diseases (CVDs)?
- How do modifiable risk factors, such as sedentary lifestyle, smoking, high blood pressure, diabetes, and hypercholesterolemia, increase an individual's likelihood of developing CVDs?
- Why is a family history of CVD considered a significant independent risk factor for premature coronary heart disease (CHD)?
Types of Heart Disease / Statistics
There are multiple types of heart disease, each with distinct mechanisms and implications for dietary management [13]. Coronary artery disease (CAD), heart failure, hypertensive heart disease, and arrhythmias represent a fraction of these conditions. The four main types of CVD include coronary heart disease, stroke, peripheral arterial disease, and aortic disease [15].
Coronary artery disease (CAD) is the most common type of heart disease [14]. Cerebrovascular disease is the second leading cause of heart disease. Other forms of heart disease include congenital heart disease, heart valve disease, cardiomyopathy, pericardial disease, arrhythmia, and aortic dissection.
Congenital heart disease (CHD) is the most common type of birth defect, affecting about 1 in 100 babies born in the United States [16]. CHDs can range from mild to severe and can affect the heart's structure, function, or both [16].
Heart valve disease is a condition in which one or more of the heart valves are damaged or diseased, which causes blood to flow backward through the valves, damaging the heart and other organs [17]. Heart valve disease affects 2.5% of the U.S population and can be caused by several factors, including infection, injury, and aging [17].
Heart failure is the heart's inability to pump blood, leading to symptoms such as fatigue, shortness of breath, swelling, chest pain, palpitations, weight gain, swelling in the ankles, legs, and abdomen, bloated or hard stomach, dry and hacking cough, and nausea [18] [19]. More than 6 million adults in the United States have heart failure [18].
Cardiomyopathy represents a collection of diverse conditions of the heart which makes it weaker and less able to pump blood. Cardiomyopathy can be caused by several factors, including infection, toxins, and genetic disorders [20]. Due to the potential for underdiagnosis, estimates of cardiomyopathy prevalence can vary. It is estimated that up to 1 in 500 adults may be affected by this condition [21].
Pericardial disease is a condition that affects the pericardium, the sac that surrounds the heart [22]. This can cause inflammation, infection, or scarring of the pericardium, which can interfere with the heart's ability to function. Pericardial disease can manifest as acute pericarditis, pericardial effusion, cardiac tamponade, or constrictive pericarditis [22].
Arrhythmia is a cardiac disorder characterized by an abnormal heart rhythm, manifesting as tachycardia (excessively rapid heartbeat), bradycardia (abnormally slow heartbeat), or irregular heartbeat patterns [23]. These irregularities can induce symptoms such as palpitations, dizziness, and syncope (fainting episodes) and can arise from various etiologies, including underlying heart conditions, electrolyte imbalances, and adverse effects of certain medications [23]. One in 18 people, or 5 percent of the U.S. population has an arrhythmia with a-fib (atrial fibrillation) being the most common [24].
Aortic dissection is a rare, life-threatening condition in which the inner layer of the body’s main artery (aorta), tears [25]. This can cause blood to leak between the layers of the aorta, which can weaken the artery and cause it to rupture. Aortic dissection can be caused by several factors, including high blood pressure, atherosclerosis, and connective tissue disorders [25].
Aortic dissection affects about 30 in 1 million people each year and more than 13,000 die each year [26]. Aortic dissection is most common in those individuals over the age of 60 and if not treated, the tear can worsen, ripping the outer layer of the aorta and allowing blood to escape the artery [25] [26]. As many as 40 percent of individuals who suffer from an aortic dissection die, and the risk of death increases by 3-4 percent every hour the condition is left untreated [26].

Self Quiz
Ask yourself...
- What are the distinct mechanisms and implications for dietary management of different types of heart disease?
- How do the etiologies and clinical manifestations of heart valve disease, cardiomyopathy, and pericardial disease differ from each other?
- What are the potential consequences of untreated arrhythmias, and how can lifestyle modifications and pharmacological interventions contribute to their management?
- Why is aortic dissection considered a life-threatening condition, and what are the critical steps involved in its diagnosis and treatment?
Evidence on Diet and Heart Health / Diet Options
When considering the diet options for heart health, the Mediterranean diet, DASH diet, and plant-based diets are among the most researched and recommended. These diets share common elements such as an emphasis on whole foods, minimal intake of red meat, and a high volume of fruits and vegetables. Extensive research has demonstrated that the DASH dietary pattern lowers the risk of cardiovascular disease [37]. Numerous prospective studies have demonstrated the consistent benefits of the Mediterranean diet on cardiovascular health [30].
There is substantial evidence that most vascular events may be prevented by avoiding smoking, participating in regular physical activity, maintaining normal body mass index, and eating a healthy diet [27].
Observational studies have demonstrated that dietary patterns rich in fruits and vegetables, excluding white potatoes, are linked to a lower risk of CVD [28] [29]. Regular consumption of whole grain foods has been linked to a reduced risk of cardiovascular disease (CVD), coronary heart disease (CHD), stroke, metabolic syndrome, and various cardiometabolic risk factors, as evidenced by robust observational studies and clinical trials [28]. Numerous randomized controlled intervention studies have demonstrated that replacing refined grains with whole grains leads to significant improvements in cardiovascular risk factors [28] [31].
Except for a small trial that demonstrated a reduction in arrhythmia recurrences among regular drinkers with atrial fibrillation upon alcohol abstinence, no other studies have reported favorable outcomes associated with alcohol consumption for cardiovascular health [32].
Dietary fiber, abundant in plant-based foods like fruits, vegetables, whole grains, nuts, seeds, beans, and legumes, have shown an inverse association with a lower risk of metabolic syndrome and cardiometabolic risk factors [33].
A systematic review and meta-analysis provided evidence that substituting saturated fat with unsaturated fat can improve cardiovascular outcomes and reduce the risk of CVD [34]. Plant-based diets rich in foods like whole grains, fruits, vegetables, and nuts, have been linked to a reduced risk of cardiovascular events and intermediate risk factors [36].
Current evidence does not support the widespread use of high-dose vitamin and mineral supplements for the prevention of cardiovascular disease (CVD) [28].


Self Quiz
Ask yourself...
- What are the common elements shared by the Mediterranean diet, DASH diet, and plant-based diets that contribute to their positive impact on heart health?
- How does the evidence from observational studies and clinical trials support the link between regular consumption of whole grains and a reduced risk of cardiovascular diseases?
- What are the potential mechanisms by which dietary fiber from plant-based foods exerts its protective effects against metabolic syndrome and cardiometabolic risk factors?
Role of Sodium and Fats
Sodium and fats hold significant impact over heart health. High sodium intake is associated with hypertension, a risk factor for heart disease, while certain types of saturated and trans fats, are linked to an increase in LDL cholesterol and the development of atherosclerosis [28]. A systematic review and meta-analysis revealed the detrimental effects of saturated fat on cardiovascular disease (CVD) outcomes and risk factors compared to unsaturated fat. [36]
A strong body of evidence has documented the adverse effects of trans fatty acids on cardiometabolic risk factors [37]. Adhering to current recommendations to replace saturated fat from meat and dairy with nontropical plant oils also lowers dietary trans fatty acids [38].

Self Quiz
Ask yourself...
- How does the consumption of sodium and certain types of fats contribute to the development of cardiovascular diseases?
- What dietary strategies can be implemented to reduce sodium intake and limit the consumption of saturated and trans fats, thereby promoting heart health?
Healthy Eating Tips and Strategies
Incorporating a heart-healthy diet into a patient’s lifestyle requires practical tips and strategies. First, make gradual changes instead of overhauling the entire diet. Meal planning can help with healthier choices.
Setting realistic goals and collaborating with the patients to set achievable dietary goals. Controlling portion size, using smaller plates and bowls, prioritizing low-calorie, nutrient-rich foods like fruits and vegetables and limit high-calorie, high-sodium foods like refined, processed, or fast foods [39].
Paying attention to the amount of saturated and trans fats, cholesterol, and sodium. Suggest lean protein sources such as fish, poultry, beans, and lentils and limit the intake of unhealthy fats and instead opt for healthy fats like those found in olive oil, avocados, and nuts [39].
Consume at least five servings of fruit and vegetables daily [41]. Choose whole grains over refined grains and limit the intake of added sugars [28]. To have more control over the ingredients, cook and consume meals at home and make gradual changes to diet habits and build on those habits over time.

Self Quiz
Ask yourself...
- How can healthcare providers collaborate with patients to set achievable dietary goals that align with their lifestyle and preferences?
- What are some practical strategies for making gradual changes to a patient's diet, ensuring adherence and long-term success in adopting heart-healthy eating habits?
Patient Education
Nurses are well positioned to provide patient education and counseling on heart-healthy eating. The core of patient education lies in translating knowledge into practice. Nurses must communicate with consideration of cultural, linguistic, and individual patient dietary preferences. Education should be patient-centered, with actionable steps that patients can integrate into their daily lives [40].
Effective patient education strategies can include establishing a rapport, assessing the patient's knowledge, and understanding, tailoring the educational approach, using plain language, incorporating visual aids, encouraging active participation, providing written materials and ongoing support and follow-up, and addressing any barriers and concerns [42].

Self Quiz
Ask yourself...
- How can nurses tailor their patient education strategies to address individual cultural, linguistic, and dietary preferences, ensuring that the information conveyed is relevant, understandable, and actionable for each patient?
Resources
A wealth of resources is available to support nurses in their role as patient educators, from professional organizations like the American Heart Association to local community programs and online platforms [43]. These resources offer educational materials, dietary guidelines, and support tools that nurses can utilize to enhance their teaching.
A heart-healthy diet is one that is low in saturated and trans fats, cholesterol, and sodium. It is also high in fiber, fruits, vegetables, and whole grains [2][3]. Eating a heart-healthy diet can help to lower your blood pressure, cholesterol levels, and risk of heart disease [2].
The National Heart, Lung, and Blood Institute (NHLBI) has a website with information on heart-healthy eating, including recipes, meal plans, and tips for eating out. The American Heart Association (AHA) has a website with information on heart-healthy eating, including recipes, meal plans, and tips for shopping for heart-healthy foods.
The Dietary Approaches to Stop Hypertension (DASH) diet is a heart-healthy eating plan that has been shown to lower blood pressure [45].
The Mediterranean diet is a heart-healthy eating plan that has been shown to have several health benefits, including reducing the risk of heart disease, stroke, and type 2 diabetes [44]. You can find information about the Mediterranean diet on the Mayo Clinic website.
In addition to these websites, there are many cookbooks and other resources available on heart-healthy eating. Patients can also talk to their doctor or a registered dietitian for personalized advice on how to eat a heart-healthy diet.

Self Quiz
Ask yourself...
- How can nurses utilize the wealth of resources available, such as those from professional organizations and online platforms, to enhance their patient education on heart-healthy eating?
- How can nurses convey the key principles of heart-healthy eating, such as limiting saturated and trans fats, cholesterol, and sodium while emphasizing fiber, fruits, vegetables, and whole grains?
- How can nurses guide patients towards reputable and reliable resources, such as those from the National Heart, Lung, and Blood Institute, the American Heart Association, and the Mayo Clinic, to ensure that they have access to accurate and evidence-based information on heart-healthy eating?
Conclusion
In conclusion, adopting a heart-healthy diet is a crucial step towards maintaining cardiovascular well-being and overall health [30]. The nurse's role as a patient educator in promoting a heart-healthy diet is pivotal. By leveraging a position of trust and frequency of contact with patients, nurses can champion dietary choices that can reduce the risk and impact of heart disease.
Research underscores the importance of a balanced intake of nutrients to support the cardiovascular system's health, emphasizing whole foods, lean proteins, healthy fats, and a reduction in sodium, saturated fats, and sugars [3].
Patients adopting a heart healthy diet require a multifaceted approach, combining knowledge with actionable steps that are practical and sustainable. The role of healthcare professional is instrumental in this dietary transition.
A heart-healthy diet offers a multitude of benefits beyond reducing heart disease risk. It can improve blood pressure control, lower cholesterol levels, promote healthy weight management, and enhance overall energy levels [2][3]. A heart-healthy diet can contribute to a stronger immune system, reduced inflammation, and improved mental clarity [46].

Self Quiz
Ask yourself...
- How can nurses bridge the gap between knowledge and practice when educating patients about heart-healthy eating, ensuring that patients understand the rationale behind dietary recommendations and can translate that knowledge into sustainable dietary changes?
- How can nurses emphasize the broader health benefits of a heart-healthy diet beyond reducing heart disease risk, motivating patients to adopt sustainable dietary changes for their overall well-being?
Adverse Childhood Experiences
Introduction
All children should grow and thrive in a caring, nurturing environment that meets their physical, emotional, and social needs. However, many are not so fortunate. Nearly every two in three Americans (64%) have experienced adverse childhood events (ACEs) (1, 2, 4, 5).
ACEs are highly associated with future chronic health conditions, mental illness, premature death, and more (1). In fact, the more ACEs an individual has had, the higher their risk for having poor health outcomes as adults (13).
Fortunately, there are preventive and protective measures that can be taken with the appropriate resources (1). With better awareness of ACEs and the right support in place, healthcare professionals can help improve the quality of life for a myriad of children and the adults they grow up to be.
Definition
Adverse childhood events, or ACEs, can occur from birth until age 18, and are great determinants of future health (1). These are any potentially traumatic events that happened to a child. ACEs are strongly linked to mental and physical disease in adults, contributing to at least half of the leading causes of death in the United States (1).
The ACE score is a 10-item survey to identify any negative occurrences a person had before their 18th birthday (3). The higher a person’s ACE score, the more risk they have for an unhealthy adulthood (1,2).
ACE was a term coined in a large-scale study published in 1998, describing them as childhood abuse and household dysfunction in seven specific areas (1, 2). In subsequent years, three more areas were added (3, 13). Altogether, the ten ACEs are comprised of the following examples of three broad categories:
- Childhood abuse
-
- Psychological
-
- Physical
-
- Sexual
- Household dysfunction
-
- Substance abuse
-
- Mental illness
-
- Parent treated violently.
-
- Family member incarcerated.
- Neglect
-
- Emotional
-
- Physical

Self Quiz
Ask yourself...
- How would you briefly define adverse childhood experiences (ACEs)?
- Would you add or subtract anything from the list above?
- What other examples of ACEs exist?
- Should one’s community and environment factor into ACEs as well? Why or why not?
Statistics and Demographics
The initial adverse childhood experience (ACE) study, conducted in the late 1990s, included over 17,000 adult participants and revealed the following key demographic data (1, 2, 5):
- Nearly 66% of women and 62% of men reported at least one ACE in their lives.
- More than 1 in 6 people (17.3%) said they had experienced four or more types of ACEs.
- Respondents’ races who reported ACEs were: 74.8% white, 11.2% Hispanic, 7.2% Asian/Pacific Islander, 4.5% black, and 2.3% other.
- About 49% of those with college degrees experienced at least one ACE, compared to 44% without a high school diploma.
- The age group who reported the highest incidence of ACEs was those from 35-49, where almost 70% had experienced at least one ACE. The lowest incidence was reported by those aged 65 and older, at 40%.
- Of all women reporting ACEs, 25% said they endured sexual abuse, 30% witnessed substance abuse in the home, and 25% of the respondents’ parents got divorced.
- Of all men reporting ACEs, 30% went through physical abuse, 24% saw substance abuse at home, and 22% of their parents were divorced.
More recent data shows that at least 50% of the top causes of death in the US are associated with ACEs (6). As there is also a high association between ACES and depression, preventing these experiences could reduce adult depression by 44% (6).

Self Quiz
Ask yourself...
- Did any of the statistics surprise you? Why or why not?
- Reflect on your own life. How many of the 10 ACES might you have had, and how might you be able to manage them as an adult?
- What other data gathering might be useful when it comes to identifying and preventing ACEs?
- What would you identify as some of the highest risk factors for the occurrence of ACEs?
Causes and Risk Factors
The causes of adverse childhood events are varied and multifaceted. They can stem from familial or communal challenges, often referred to as social determinants of health. Many of these determinants can cause ACEs, and may include (8):
- Lack of access to healthcare or other resources
- Financial difficulties
- Homelessness or frequent moving
- Discrimination
- Any type of disrupted living situation
As noted earlier, most of the American population has had some sort of adverse childhood experience. However, there are some factors that make it more likely for these to occur. Societal, communal, and familial cultures all play a role in adverse experiences.
The following situations or conditions increase the likelihood of ACEs (7):
Community Risk Factors:
- High rates of poverty, crime, and violence
- Limited educational, economic, and employment opportunities
- Lack of community activities for youth
- Unstable housing and frequent moves by community residents
- Readily accessible alcohol and drugs
- Frequent experiences of food insecurity
Family and Individual Risk Factors:
- Social or developmental disabilities or delays
- Mental or chronic physical illnesses
- A history of abuse experienced by caregivers themselves.
- Youth dating or engaging in sexual activity early.
- Single-parent families, particularly those with young caregivers
- Low income and/or high economic stress
- Low education levels
- Children with few or no friends, or friends who partake in delinquent or aggressive behaviors
- Caregivers with limited understanding of child development
- Use of spanking or other corporal punishment as a form of discipline
- Inconsistent discipline and/or little parental supervision
- Families isolated from extended family, friends, and/or neighbors

Self Quiz
Ask yourself...
- In the community where you live, what might be some factors that contribute to ACEs in those around you?
- What are some ways your community might be able to mitigate some of the risk factors for ACEs?
- Since nearly two in three people have experienced an ACE in their lives, it is likely that you interact with someone affected by this issue. What resources might you recommend to them, and what else might help?
Cultural Considerations
Though many people experience ACEs, some populations are affected disproportionately. This includes women and those in racial or ethnic minorities, who are at greater risk for experiencing 4 or more ACEs (6, 8). Specifically, African Americans, American Indians, and Alaska Natives (AI/AN) are far more likely to have multiple ACEs than any other race or ethnicity (9,10).
The AI/AN community is a relatively young one, with poverty rates up to four times higher than the national average (10). Furthermore, the AI/AN group is often lumped together as “other” as a race category on surveys, making data harder to come by for this population (10).
AI/AN children, when compared to the total US population, are more likely to have:
- Parents who are divorced (33% versus 21%)
- Lived with someone who abused a substance (24% versus 12%)
- Witnessed domestic violence (15% versus 6%)
- Lived with a parent who ultimately died (4% versus 2%)
Lifespan Impact on the Individual
While adverse childhood experiences affect most Americans, having been through four or more puts a person at significantly higher risk of health problems as an adult (1, 2, 9). In general, the more ACEs an individual has experienced, the more likely they will have poor outcomes later in life, with a specifically high correlation to diabetes, heart disease, obesity, depression, substance abuse, smoking, poor academic achievement, and early death (4).
In fact, ACEs can reduce an individual’s life expectancy by as many as 20 years, compared to someone who has had zero ACEs (8).
The original ACEs study was conducted to determine the link between childhood abuse and adult health risk factors (1). The conclusion was overwhelmingly that in the United States, the main causes of morbidity and mortality are related to many of the health behaviors exhibited by those who have experienced ACEs (1). More recent studies find that ACEs contribute significantly to substance abuse, violence, and self-harming behavior (11).
At least 5 of the top 10 leading causes of death in the United States that are strongly related to ACEs include (9,11, 12):
- Heart disease (#1 cause of death)
- Stroke (#5)
- Chronic lower respiratory diseases (#6)
- Diabetes (#8)
- Chronic liver disease and cirrhosis (#9)
As far as mental health goes, the link with ACEs is clear: The higher one’s ACE score, the more likely they are to be depressed, experience impaired work performance, and have suicidal tendencies (13). Harmful behaviors associated with high ACE scores include smoking, drinking, and drug abuse, as these methods are often used to cope with past traumatic experiences (13).

Self Quiz
Ask yourself...
- In light of the correlation between ACEs and some of the top causes of mortality in the US, what interventions could possibly be made in childhood to prevent these deaths from occurring?
- Though the top 10 causes of death in the US have a variety of causes, the link between ACEs has been well-established for nearly three decades. Why do you think more funding and attention aren’t given to this matter?
- What other physical or mental health concerns not listed above might a person with a high ACE score have?
Societal Implications
Adverse childhood events are preventable and have been shown to contribute to at least half of the leading causes of death in the United States (1, 9, 11). Thus, the impact of ACEs on public health is vast. Since the CDC considers ACEs a public health concern, it is of utmost importance to decrease their incidence (1). Through the reduction and prevention of ACEs, general public health would improve markedly, drastically cutting down on healthcare costs and resources (1, 5, 6, 9).
The societal implications for reducing ACEs are manifold:
- Dramatic reduction of preventable causes of death
- Longer lifespans for the general population
- Better mental health
- More cost-effective physical and mental healthcare
- Lower rates of disease and depression in the general population

Self Quiz
Ask yourself...
- What other societal impacts might ACEs have?
- How could you go about preventing some ACEs in your own life or community?
- What are some local, national, or global resources to which you could introduce those in need?
Ways to Mitigate ACEs
Though ACEs are widely pervasive in American society, they need not be so. With proper resources and support systems, many -if not all- ACEs may be eradicated. The best way to mitigate ACEs would be to prevent them in the first place (4). This requires creating safe, stable, nurturing environments for children and their families (9). Furthermore, as ACEs can occur for a wide array of reasons, they need to be addressed at both the family and communal levels.
With individuals, a first step would be prevention of ACEs in the home. This could involve a vast array of mental health, education, and social work services such as: home visits, parenting classes, therapy sessions, and more (8, 9). Different emotion management techniques and child development concepts could be taught to at-risk families, promoting bonding and trust between children and their caregivers.
High-quality childcare and after-school programs with trusted adults can help mitigate ACEs as well (9). Screening for ACEs at regular intervals would also be helpful. This could include annual check-ups at the doctor’s office, visits with the school nurse or counselor, or a consultation with a home health provider. Medical management of physical and mental health conditions would be made available, including routine health screenings and necessary medications (4, 8, 9).
At the community level, prevention could take the form of free education for family members, food and housing assistance, adequate access to healthcare services, and fostering safe neighborhoods (4, 9). Economic support for families could include family-friendly work policies, earned income tax credits, and so forth. Children could partake in community events like after-school clubs and sports, helping them build bonds with trusted and supportive adults.
Three principles are the most helpful preventing long-term effects of ACEs, (4):
- Reducing stress by ensuring basic needs are met, as well as tending to abusive situations, community crime, substance abuse, discrimination, and poverty.
- Strengthening life skills can strengthen the resilience of children and their family members by practicing planning, focus, and self-control.
- Building responsive relationships by having adults listen to their children and respond adequately to their needs, thereby fostering a safe, trusting relationship.

Self Quiz
Ask yourself...
- What specific local resources are available where you live or work that could help prevent ACEs from occurring in the first place?
- What types of secondary and tertiary prevention resources can you identify for ACEs?
- What are other ways ACEs can be mitigated or prevented at the state or federal level?
Reporting ACEs
Considering there are various types of ACEs, they can be difficult to identify and thus report. However, some are clear-cut. In situations where child abuse or neglect is occurring or suspected, a mandated reporter (e.g., nurse, teacher, counselor) would need to report it as soon as possible. If the child is in imminent danger, take them to a safe place and make a report.
To report child abuse in the United States, call or text 1-800-4-A-CHILD (1-800-422-4453). The website is https://www.childhelphotline.org/.
If there is suspicion that a child is being sexually exploited, the phone number to call is 1-800-THE-LOST (1-800-843-5678), and the website is https://report.cybertip.org/.
To report human trafficking, call 1-888-373-7888, use TTY at 711, text BEFREE (233733), or visit the website at https://humantraffickinghotline.org/.
For anyone experiencing feelings of self-harm or suicide, 988 is the national Suicide and Crisis Lifeline that can be called or texted. The website is https://988lifeline.org/.
Support and Additional Resources
While there is no single way to prevent ACEs from occurring, there is a plethora of resources available to help mitigate the effects and to educate others. Visting a healthcare provider can connect a patient to mental health professionals, support groups, or specialty services like social work and support groups (8).
The Substance Abuse and Mental Health Services Administration (SAMHSA) has an abundance of resources on topics like trauma-informed care, early childhood mental health programs, Native Connections for the AI/AN population, school, and campus health, and much more. More information can be found at https://www.samhsa.gov/programs.
Healthy Outcomes from Positive Experiences (HOPE) is a national resource center offering research, training, and technical assistance in order to better the lives of children and their families. Their website is https://positiveexperience.org/.
The Centers for Disease Control and Prevention (CDC) offers ACE-specific information at this website: https://www.cdc.gov/violenceprevention/aces/resources.html.
Conclusion
Adverse childhood events, or ACES, affect the majority of the American population. Strongly correlated with many leading causes of death, ACEs are preventable and warrant attention from healthcare providers and the general public alike. Fortunately, many resources exist at the individual, community, and national levels to provide care and prevention for these experiences.
Though ACEs tend to lead to negative health outcomes, they need not condemn a person to lifelong problems. Through screening tools, community food and housing programs, mental health assistance, education, and adequate medical care, ACEs can be mitigated, well managed, and prevented.
Despite the misfortune in a child’s life, there is still much hope available when they reach adulthood.
Conclusion
Adverse childhood events, or ACES, affect the majority of the American population. Strongly correlated with many leading causes of death, ACEs are preventable and warrant attention from healthcare providers and the general public alike. Fortunately, many resources exist at the individual, community, and national levels to provide care and prevention for these experiences.
Though ACEs tend to lead to negative health outcomes, they need not condemn a person to lifelong problems. Through screening tools, community food and housing programs, mental health assistance, education, and adequate medical care, ACEs can be mitigated, well managed, and prevented.
Despite the misfortune in a child’s life, there is still much hope available when they reach adulthood.
Trauma Informed Care in Nursing
Introduction
As nurses, we have been trained to perform ongoing assessments on patients with every encounter. Many patients have gone through traumatic events that often go undiscovered by the healthcare team.
A trauma informed care approach will help healthcare providers uncover past trauma. This will allow them to tailor a plan of care that helps alleviate patient suffering by decreasing overall stress and anxiety. When the healthcare team is aware of past trauma, they can avoid conversations and situations that could potentially re-traumatize the patient.
Trauma Informed Care
Trauma is a human experience that can affect people from all different backgrounds and walks of life. There is no race, gender, sexual orientation, or social class that is immune to the far-reaching clutches of trauma. A traumatic event is an event that is marked by sexual violence, severe injury and/or death. These events can be first-hand accounts where the people themselves were the victims of the event.
They can also be indirectly experienced by witnessing the event take place on another person. The event can also produce vicarious trauma when it happens to a close friend or loved one. No matter how traumatic an event was experienced, it can have severe and long-lasting effects (1).
Despite the rising accounts of traumatic events, trauma informed care is an underused skill in the healthcare field. Those who support and use trauma informed care understand that there is a large population of people seeking healthcare services who have had past traumatic experiences. They are also aware that just by seeking out care, they have the potential of being re-traumatized.
Empowering the patient to have control over their care through collaboration will help decrease the chances of re-traumatization.
There are six principles of trauma informed care:
- Safety
- Trustworthiness and transparency
- Peer support
- Collaboration and mutual support
- Cultural and historical sensitivity
- Empowerment of voice and choice
Trauma informed care runs parallel to ethics in the healthcare setting. It endeavors to ease the patient’s suffering by preventing re-traumatization and empowering the patient. (3)

Self Quiz
Ask yourself...
- What are two principles of trauma informed care?
- What is a past traumatic event?
- Who is affected by trauma?
Principles of Trauma Informed Care
It is meaningful to explore each of the six principles of trauma informed care
Safety
In trauma informed care, safety pertains to both the psychological and physical safety of the patient and their family throughout their encounter with the healthcare organization. The goal is to prevent any form of re-traumatization. This is accomplished by creating safe spaces, access to services, and engagement between the patient and the healthcare team.
One of the greatest aspects of safety in trauma informed care is environmental. This demands that the healthcare teams create an environment that is both welcoming and accommodating to all patients regardless of their diverse backgrounds. We must understand that patients who have undergone traumatic events can be hypersensitive to their environmental safety.
The trauma informed care plan must be individually tailored and include communication initiatives that promote the patient’s self-identity and how they would like to be addressed (1).

Self Quiz
Ask yourself...
- In trauma informed care, what kind of safety is discussed?
- How does the environment play a part in safety?
Trustworthiness and Transparency
Nursing has long been recognized as the nation’s most trusted profession. This has been accomplished through the intentional focus of patient advocacy. Nation-wide policies and safety goals have promoted diversity, equity, and inclusion. Initiatives to make sure that the patient understands and agrees with their plan of care, such as using their preferred language in plain and clear terms, is an example of how nurses build that trust.
Using the concept of patient-centered care helps demonstrate transparency, which is a way nurses further build trust. True transparency can be accomplished through encouraging patients to be involved in their care. Asking patients if it is acceptable that we document their experiences and even share our notes or computer screens to demonstrate our desire to be transparent.
Educating patients using the teach-back method also indicates our transparency as our knowledge becomes theirs (1).

Self Quiz
Ask yourself...
- How can the healthcare team build trust using trauma informed care?
- How can transparency be accomplished?
Peer Support
Contrary to popular beliefs, the goal of peer support in trauma informed care is not fixing the individual. Rather, the goal is to assist the individual to empower themselves by connecting them with supportive groups of peers that have similar experiences, culture, beliefs, and religion. Empowerment of the patient should be the goal of peer support. Traumatic stress is often accompanied by a re-traumatization cycle that can be interrupted and ultimately stopped through individual empowerment of the patient.
These peer support groups often contain members who themselves have survived traumatic events. To have the best probability of success, the patient should leave behind former friends who enable the re-traumatization cycle and gravitate to the peer support group members. This can leave the patient with further feelings of loss and grief. This has to be considered when developing the plan of care for the patient (1).
Identifying Past Trauma
Trauma informed care does not mean that the care is tailored to a patient’s specific trauma. Nor does it mean that the team endeavors to heal or even address past trauma. Rather, in simple terms, trauma informed care recognizes that the patient has been through a traumatic ordeal and that the plan of care must take that trauma into account in order to properly care for the patient.
The patient’s reaction and compliance may be affected by their past trauma. Past trauma needs to be identified and acknowledged. Past trauma can affect all aspects of a patient’s life. Identifying and acknowledging the trauma and how the patients then needed coping mechanisms may now have become detrimental to their health is important for the overall well-being of the patient.
Through the identification of past trauma, the team can take the opportunity to ensure that the patient does not feel responsible for the life-altering trauma and understands that the trauma was not their fault. Identifying the trauma can lead to the revelation that there is a connection between past trauma and the patient’s current coping and functioning; this can change their overall perspective, thus changing their lives (4).

Self Quiz
Ask yourself...
- What is the goal of peer support in trauma informed care?
- Who is often involved in peer past trauma support groups?
Collaboration and Mutual Support
Collaboration and mutual support demand that the entire healthcare team see the patient as both an equal partner and the expert in their own personal experiences. The patient should be allowed to both identify and prioritize their goals, then the healthcare team can work with the patient to for the plan of care with these goals at the forefront.
Collaboration takes more time than the traditional healthcare “do as I say” method. It helps in the trust-building process and when done properly, it helps the patient to succeed as the goals have come from them. This is something that can also interrupt the re-traumatization cycle. It also increases the probability that the patient will be compliant with the plan of care and any after-care appointments and follow-ups (1,4).


Self Quiz
Ask yourself...
- How is the patient seen through the collaboration lens?
- What destructive cycle can collaboration and peer support interrupt?
Cultural and Historical Sensitivity
The entirety of the patient’s identity is surrounded in cultural and historical sensitivity. Not only does this encompass aspects such as race, gender, age, etc. but it also includes life experiences and relationships right down to the base familial associations.
It also includes beliefs, core values and experiences in open spaces. When seeking healthcare, no matter the reason, all of these aspects of the patient’s identity are brought to the facility and laid in front of the healthcare team (1).
Empowerment of Voice and Choice
As discussed earlier in the peer support principle, empowerment is paramount in trauma informed care. Empowerment of voice and choice is perhaps the chief cornerstone and is present in all the other principles of trauma informed care. Trauma informed care empowers patients by making them feel heard and that their voice is important for their overall well-being.
Though the healthcare team may not always agree, trauma informed care also enforces the concept that the patient’s choices are to be respected. Through the trauma informed care journey, the patient develops their ability to navigate the healthcare setting and becomes familiar with the language of the medical community.
This further empowers the patient as they can understand the plan of care and become an active participant in that plan, as they were involved in both the planning and implementation. Further, trauma informed care creates a safe and supportive environment where the patient is allowed to grow and mature in their knowledge and understanding of themselves and their health (1).

Self Quiz
Ask yourself...
- In what ways does trauma informed care empower patients?
Effects of Traumatic Stress
Traumatic stress has shown to increase chronic illness, mental health issues and early death. When left alone, traumatic stress can morph into enduring stress. Some forms of enduring stress include:
- Chronic stress – this happens when trauma is continuous over a long period of time.
- Toxic stress – this is found in children who experience long-standing and/or frequent trauma such as emotional and physical abuse, neglect, and exposure to violence.
Traumatic stress can have altering effects on multiple brain processes. This includes the neurologic, immunologic, endocrinologic, metabolic, inflammatory, and autonomic processes. Depending on which phase of brain development the patient is in when the trauma occurs, it determines the long-lasting effects.
Repeated trauma can cause a hormonal cascade which can result in the allostatic load phenomenon. This phenomenon distorts the normal stress mediating processes.
Traumatic stress often leads to self-destructive behavior. Drug and alcohol use/addiction, violence and risky behavior often follows those who have had traumatic stress events. There is a fear among traumatic stress victims that they may be judged for their choices and lifestyle (1).


Self Quiz
Ask yourself...
- Can you name a type of enduring stress?
- What is the phenomenon that distorts the normal stress mediating processes of the brain?
- What can traumatic stress lead to?

Self Quiz
Ask yourself...
- What are two things that trauma informed care is not?
- What can be accomplished through identifying trauma?
- What does the healthcare team need to do in connection with the patient’s trauma?
Adverse Childhood Experiences
Nearly 40% of people have been exposed to adverse childhood experiences. Of course, adverse childhood experiences harm the overall health and well-being of the child; they also have a potential great impact on the physical and mental health of the person as they transition into adulthood.
Adverse childhood experiences and childhood trauma have shown to leave the patient with an increased risk for developing leading causes of death and disability. These conditions include heart disease, stroke, cancer, and depression with suicidal ideation. Also, childhood trauma can lead to symptoms of chronic headache and pain as an adult (2).
As most childhood trauma is perpetrated by someone known and close to the child such as a parent, relative or close family friend, the child is often left with an altered expectation of interpersonal relationships. This may lead to severe insecurity and distrust where negative personal perception especially in relation to others may develop.
People who develop physical symptoms of past childhood trauma are often unable to adjust and move on post-trauma. On the other hand, those who are able to form positive relationships tend to have fewer physical symptoms and are more liable to have adjusted to childhood trauma. Childhood trauma can have long-reaching effects on the ability of the adult to form positive relationships and have normal responses to stressful situations (2).

Self Quiz
Ask yourself...
- What percentage of people have had adverse childhood experiences?
- What type of conditions are victims of adverse childhood experiences in danger of developing?
- Can you discuss what adverse childhood experiences can lead to?
Trauma Informed Approach
The trauma informed approach was born out of the research on adverse childhood experiences. The research showed that the more adverse childhood experiences that took place in the patient’s life, the more it affected their mental and physical health; even leading to early death.
Trauma informed approach begins at the organizational level, where the culture must adapt to prevent re-traumatization. There are a few aspects that need to be incorporated into the organization’s training to accomplish the changes needed.
The organization must put on trauma glasses and view the healthcare team through the trauma lens. There is a direct correlation between trauma and mental health; this needs to be acknowledged, accepted, and viewed as part of the care plan.
In order for the trauma informed approach to be effective, the organization must realize that trauma expands beyond Post Traumatic Stress Disorder (PTSD). Rather, trauma incorporates a multitude of differing issues that can include mental, emotional, physical, and other multiple trauma sources.
The healthcare professional who is assessing the patient should be trained in recognizing the signs of trauma and, if disclosed, be able to respond appropriately in the moment. Training needs to be done with all front-line staff who the patient may confide in.
The healthcare team should be aware of resources that are available in the community and be able to refer the patient to those organizations. Being as trauma specific as possible so that the patient can connect in a meaningful way with this new support system. The organization should partner with these support groups to ensure easy transitioning from the institution to the community.
The team should also prioritize the principles of trauma informed care. For instance, to promote trustworthiness and transparency, the team could limit the number of healthcare providers who will ask the patient to repeat the story of their traumatic experience. Turning to more collaborative communication and relationships between the team and the patient; allowing the patient to be actively involved in their plan of care also promotes the trauma informed care principles.
Promoting safety within the organization for both the patient and the healthcare team also helps to change the culture to one of a trauma informed approach. Trauma survivors could be approached and asked to help design, implement, and evaluate the trauma informed approach to be used. What better way to get to know your community resources than to actively partner with them to help meet the needs of the organization’s patients.
It needs to be recognized that not all patients who show similar symptoms to those of past trauma have gone through a traumatic event. There is no cookie-cutter plan of care, and all patients must be properly assessed to determine what their plan of care will be (6).

Self Quiz
Ask yourself...
- How was the trauma informed approach born?
- What must change to prevent patient re-traumatization?
- What are two ways that an organization can change to a trauma informed care culture?
- Should all past trauma survivors be cared for in the same manner?
Impact of Trauma Informed Care
The impact of trauma-informed care on the patient and on the healthcare system as a whole cannot be overstated. By understanding that a great deal of the patients who seek out healthcare services have undergone a traumatic event and tailoring the assessment with that in mind, an organization can minimize the occurrence of re-traumatization.
When we understand how trauma has affected our patients’ lives, how they perceive the healthcare system and what their previous experiences within that system have been like, steps can be taken to ensure better outcomes within this population (1).

Self Quiz
Ask yourself...
- What are healthcare institutions trying to prevent through trauma informed care?
- How can healthcare facilities ensure better outcomes within the past trauma patient?
- What are two ways that nurses can help minimize re-traumatization?
Nursing Implications
In order for trauma informed care to be properly accepted and put into use in the healthcare setting, the culture must be transformed to be a trauma-informed culture. Nursing is with the patient around the clock and nurses have the ability to touch patient’s lives in the most impactful way.
Here are a few considerations that pertain to the healthcare team but when used by nurses have the ability to transform the patient’s environment into a true trauma informed care setting.
Introductions
Even if the nurse believes that the patient knows who they are, it is important for the nurse to reintroduce themselves with every interaction. The patient generally has many different members of the healthcare team entering their space throughout their stay. Team members tend to meld into one anonymous face to the patient; the nurse by introducing and reintroducing themselves and their role to the patient will not only foster an understanding of who does what, but they will empower the patient to be engaged and involved in their plan of care.
Body Language
Body language is important when caring for any patient. When caring for a patient who has experienced trauma, this becomes even more impactful. Open body language sets the stage for trust.
Trauma survivors may often feel a sense of being trapped or confined which may lead to an overall sense of powerlessness. Unintentional threatening body language magnifies these feelings and could bring on a re-traumatization episode. By contrast, non-threatening body language decreases the trauma center and leaves the patient calm and non-triggered.
Trauma informed care body language includes being at the patient’s level; commit to sit or raising the bed so that both patient and nurse are at the same level. Knowing the environment and deescalating trauma by the nurse positioning themselves properly in relation to the patient and the door; allowing for both to access so that the patient does not feel confined.
Anticipatory Guidance
Past trauma may have been unpredictable or an outright surprise. Verbally telling a patient what will be expected during their stay will reassure them even if the coming procedure or test may cause pain. Sharing who will be part of their care during their stay will also set them at ease. Knowing and understanding the expectation further empowers the patient to be involved in their plan of care.
The expectation, when known, decreases those feelings of surprise which could bring them back to that time of trauma.

Self Quiz
Ask yourself...
- Why should the nurse introduce themselves by name and role?
- How can the nurse’s body language affect the past trauma patient?
- What is incorporated in anticipatory guidance?
Permission
Touch can have an incredible impact on the patient who has experienced past trauma. Unwanted or inappropriate touch quite likely may have been a part of their traumatic experience. It can activate those traumatic memories and activate the re-traumatization cycle. Touch is also inevitable when it comes to the nurse/patient relationship.
What the nurse can control is when the touch occurs. Touch should always be preceded by the nurse explaining what they are going to do and asking for the patient’s permission to touch them. Asking permission puts the ball in the patient’s court and empowers them as they are now given a choice and are in control of their body and space.
Permission to touch the patient should never be assumed; permission should be asked every time the nurse needs to touch the patient.
Protect
In many cases, patients who have experienced trauma experienced it at the hand of someone that they know. Many times, the patient will not be alone in their room; family and friends are often present. Patient advocacy has always been the primary role of the nurse.
As part of being an advocate for the patient, the nurse should protect the privacy and safety of the patient. Asking those present in the room to leave prior to discussing the patient’s plan of care is a way to protect both privacy and safety. The patient may not feel safe asking visitors to leave their room especially if they may have been involved in the prior traumatic episode.
By asking visitors to leave, the nurse gives control back to the patient. In private, the nurse can ask who the patient is comfortable with remaining in the room. Once again, the patient is empowered.
Clear and Consistent
Realistic expectations are understood when given in clear and consistent language. This will also foster trust especially if the entire healthcare team is on the same page and vocalizing the same message, consistency. Using language that the patient understands is also paramount. Avoiding medical terminology and acronyms also builds trust as the patient knows that the nurse has made it their priority that the patient understands their plan of care.
Universal Precaution
Finally, trauma informed care needs to be a universal precaution regardless of if the patient’s past trauma history is known or not. By treating all patients as if they had experienced past trauma, those who have will be more apt to share the experience.
Also, nurses will be less likely to start the re-traumatization cycle by inadvertently triggering an episode. It will help treat the patient without relying on the patient to disclose something that they may not yet feel comfortable sharing. (3)

Self Quiz
Ask yourself...
- Why should the nurse ask permission to touch the patient?
- When should the nurse ask permission to touch the patient?
- What does universal precaution in terms of trauma informed care mean?
Resources
It is not easy to become a center where trauma informed care is practiced, it does not happen overnight. Trauma informed care is an intentional shift in culture at the facility and/or system level. Trauma informed training should be implemented, and the staff need to understand the “why” behind the training in order to buy-in.
Trauma informed care not only helps the patient to be empowered and prevent re-traumatization, but staff that have undergone past traumatic experiences can also be helped once a facility adopts this culture. This culture should be at the forefront of both staff and leadership minds. Staff meetings, unit huddles and any other opportunity where leadership actively communicates with staff should incorporate the messaging of trauma informed care.
Facilities should actively be hiring a trauma informed workforce. People from wide varieties of racial and cultural backgrounds should be on the interview panel. Questions pertaining to trauma informed care can and should be asked to pick up on skills and traits that will promote this culture.

A few environmental factors to create the trauma informed culture include keeping doors and common areas well-lit, keeping noise levels low and having warm, cozy colors as decoration in common areas.
Below are some websites that can be visited in order to help kickstart the culture of trauma informed care:
- https://TraumaInformedCare.chcs.org
- https://www.creatingpresence.net/
- https://www.chcs.org/resource/key-ingredients-for-successful-trauma-informed-care-implementation/
- https://store.samhsa.gov/product/SAMHSA-s-Concept-of-Trauma-and-Guidance-for-a-Trauma-Informed-Approach/SMA14-4884
(5)

Self Quiz
Ask yourself...
- What do staff need to understand to be participants in patient informed care?
- When should trauma informed care concepts be communicated to staff?
- How can facilities ensure that new hires are on board with trauma informed care?
- What are some environmental elements that facilities can apply to promote trauma informed care?
Conclusion
Though not a new concept, trauma informed care is essential to help patients who have had traumatic experiences navigate through the healthcare system. Trauma informed care empowers patients to take control of their care in collaboration with the healthcare team. Ultimately, the goal of trauma informed care is to prevent re-traumatization of the patient at the hands of the healthcare team.
The trauma background of any given patient is unknown when they arrive at the facility. It is the responsibility of the nurse to use trauma informed care to both assess the patient and create trust so that they will disclose the trauma. Once known, the team will be able to work together with the patient to prevent further trauma and have positive outcomes.
Conclusion
Though not a new concept, trauma informed care is essential to help patients who have had traumatic experiences navigate through the healthcare system. Trauma informed care empowers patients to take control of their care in collaboration with the healthcare team. Ultimately, the goal of trauma informed care is to prevent re-traumatization of the patient at the hands of the healthcare team.
The trauma background of any given patient is unknown when they arrive at the facility. It is the responsibility of the nurse to use trauma informed care to both assess the patient and create trust so that they will disclose the trauma. Once known, the team will be able to work together with the patient to prevent further trauma and have positive outcomes.
Nursing Care in Lewy Body Dementia
Introduction
Lewy body dementia is one of the more common causes of dementia. Currently it is the second most common dementia disorder following Alzheimer’s disease [2]. This condition is shown to affect more than 1.4 million people in the United States [1] [2]. Of dementia cases in older adults, Lewy body dementia is said to make up 5% of people with dementia [2]. Lewy body dementia is a disorder that progresses over time [1]. The progression of the disease differs between individuals and the severity of the symptoms [1].
On average an individual lives between five to eight years after diagnosis [1]. Currently there is not a cure for this disease [1]. This course will examine the causes of this disease, signs and symptoms patients might experience, diagnostic tests, types of management, and educational resources for family members. This course is designed to inform nurses about this common disease and to use this information in their daily practice to care for their patients.

Self Quiz
Ask yourself...
- What do you think is the most common form of dementia in the United States?
- How common is Lewy body dementia in other parts of the world?
- Is there currently a cure for Lewy body dementia?
- Why do you think Alzheimer’s disease is more common than Lewy body dementia?
Definition
Lewy body is an umbrella term that includes two separate diagnoses: Dementia with Lewy bodies and Parkinson’s disease dementia [5]. As these diseases progress, they develop together and are seen as one entity, not two separate conditions [4]. Lewy body dementia is a condition that involves neurocognitive disorders that include hallucinations, memory loss, behavior changes, and parkinsonism features [2]. This disease can also affect intellectual abilities and cause individuals to act out dreams during REM (rapid eye movement) sleep [2]. REM sleep behavior disorder sometimes may be experienced before any other symptoms are exhibited [2].
Lewy body dementia is known for a buildup of deposits of alpha- synuclein proteins called Lewy bodies [1]. Diagnosing this condition can be difficult because many neurological disorders have similar symptoms. Lewy body dementia and Parkinson disease dementia are very similar. For a diagnosis of Lewy body dementia, there must be a cognitive impairment with motor symptoms occuring in less than 12 months [3]. Parkinson’s disease dementia affects an individual’s movements; cognitive symptoms appear later (greater than one year) [5].
Lewy body dementia is known to affect older adults generally between the ages of 50 and 85 [2]. This disease is said to be underdiagnosed due to a large number of diagnoses occuring post-death during autopsies [4]. Several medications used to treat neurocognitive and behavioral symptoms in other conditions can worsen the symptoms of Lewy body dementia [4]. Therefore, an accurate diagnosis can impact an individual’s quality of life.

Self Quiz
Ask yourself...
- What are the two forms of Lewy body dementia?
- What are the differences between dementia with Lewy bodies and Parkinson’s disease dementia?
- Why is it difficult to diagnose Lewy body dementia?
Epidemiology
Lewy body dementia affects a significant number of individuals in the United States. This condition is found more often in men than women [4]. Age is thought to be the greatest risk factor for an individual developing this disease [4]. An individual who has a family history of Lewy body dementia and Parkinson’s disease is at a higher risk for developing this condition [3].
Lewy Body dementia is more widespread in European, Asian, and African ethnic groups [3]. In individuals with Parkinson’s disease, the incidence of Parkinson’s disease dementia is said to be around 25-30% [4]. The incidence of individuals with Parkinson disease developing this type of dementia after having Parkinson’s for more than 20 years increases to around 83% [4].


Self Quiz
Ask yourself...
- What is the greatest risk factor for developing Lewy body dementia?
- Are there certain ethnic groups that have a higher rate of Lewy body dementia?
- Which gender is Lewy body dementia prominent in?
Pathophysiology
There is a buildup of alpha- synuclein proteins that causes neurons to die in Lewy body dementia [2] [5]. As mentioned above in this course, this buildup of proteins is called Lewy bodies. The death of neurons that produce dopamine result in problems with movement, cognitive impairment, a decline in cognition, and sleep disturbances [4]. In Lewy body dementia there is a deficiency of acetylcholine [3]. There is also a decrease in acetylcholine with Alzheimer’s disease, but the deficiency is greater with Lewy body dementia [3]. The decrease in neurons that produce acetylcholine causes memory loss and learning impairment [4].
The mutation of synuclein alpha and synuclein beta genes can cause dementia with Lewy bodies [2]. Mutations in apolipoprotein E and GBA genes are potential risk factors for developing the disease [2]. There have been cases where a buildup of alpha-synuclein was found during an autopsy, but the individual did not show any clinical signs of Lewy Body dementia when alive [4]. The function of these proteins in this condition is still undetermined [5].

Self Quiz
Ask yourself...
- What are considered Lewy bodies?
- What other disease besides Lewy body dementia has a decrease in acetylcholine?
- What symptoms are a result of destruction of neurons that produce dopamine?
Etiology
The exact cause of Lewy body dementia is still unknown. While research is ongoing and new developments are occuring, the specific cause has not been determined. The accumulation of Lewy bodies cause cell death which causes symptoms, however, the reason for the buildup of Lewy bodies is still under research [5]. As mentioned earlier, there are specific gene mutations that have been shown to increase the likelihood of producing altered alpha- synuclein proteins, in turn causing them to clump together (forming the Lewy bodies) [2].
The mutation of the GBA gene interferes with the function of lysosomes, which can affect the breakdown of the alpha- synuclein proteins, causing the proteins to accumulate [2]. The e4 allele type of the APOE gene has been shown to increase the risk of developing Lewy body dementia [2]. These clumps of Lewy bodies form inside and outside of neurons in different areas of the brain, where they can alter the function of the cell and can cause the cell to die [2].
The neurons that develop the neurotransmitter dopamine are especially impacted by these clumps of Lewy bodies, which was addressed earlier in this course [2]. Further research is required to find out why these Lewy bodies develop in certain individuals. Currently, age, genetics, and environmental factors are some of the greatest risk factors [3].

Self Quiz
Ask yourself...
- What is the cause of Lewy body dementia?
- Why is age a risk factor for developing this disease?
- What does the buildup of Lewy bodies do to cells?
Clinical Signs and Symptoms
Lewy body dementia is a progressive disorder - the signs and symptoms worsen over time. The symptoms that are more common are sleep changes, impaired behavior, movement, and cognition [5]. Research shows that the location of Lewy body accumulation impacts the clinical signs and symptoms the individual experiences [3]. If Lewy bodies develop in the brainstem and cerebral cortex first, the condition is called dementia with Lewy bodies, and the onset of the dementia is early [3]. If Lewy bodies accumulate in the brain stem and then develop into the cerebral cortex as time passes, the onset of dementia appears later, and this condition is called Parkinson’s disease dementia [3].
Rapid Eye Movement Sleep Behavior Disorder
Rapid eye movement (REM) sleep behavior disorder is sometimes the first clinical sign of dementia with Lewy bodies [2]. Individuals with this disorder move and talk while dreaming in their sleep [2]. The movements can be violent and cause the individual to fall out of bed [5]. Individuals may kick, punch, and scream in REM sleep (the second half of their sleep) [4]. REM sleep behavior disorder is seen in 76% of patients with dementia with Lewy bodies [4].
This disorder can cause fractures and contusions in some individuals resulting from falling out of bed [4]. This can not only affect the individual, but also the sleep partner of the patient [4]. In some cases, separate sleeping arrangements are needed for the safety of the individual and their sleeping partner. A questionnaire by the patient and sleep partner is part of the diagnosis of REM sleep behavior disorder [14]. If the individual does sleep next to someone, this questionnaire can be helpful as most of the time the patient cannot recall the events while asleep [14]. Video polysomnography is required for a complete diagnosis of this disorder [14]. These events while asleep must be repeated to meet the diagnostic criteria [14].
Other Sleep Disorders
Other disorders of sleep include sleepiness in the daytime, restless leg syndrome, confusion when awakened, and obstructive sleep apnea [4].
Visual Hallucinations
Visual hallucinations are present in about 80% of individuals with Lewy body dementia [1]. Visual hallucinations are a core clinical symptom of dementia with Lewy bodies [4]. They are more common in women than in men [4]. Individuals are aware of these hallucinations and can tell others what they experienced [4]. Visual hallucinations are vivid to individuals and have been said to range from people walking around the house to seeing people that have died sitting next to them [6]. During the beginning stages of the disease, the hallucinations do not seem to affect the patient as much as when the disease progresses [6]. Patients are said to be afraid of these hallucinations in the later stages of the disease [6]. Nonvisual hallucinations are less common, however can occur in some patients [1]. These hallucinations include smelling or hearing something that is not in their surroundings [1].
Fluctuation in Cognition
Fluctuation in cognition is also a clinical sign that is associated with dementia with Lewy bodies [4]. This symptom includes changes in attention, concentration, and alertness [5]. These changes are random and can differ day-to-day [1]. Symptoms can include delirium, and mimic symptoms that are caused by metabolic diseases, which can further the difficulty with identifying the correct diagnosis [4]. To diagnose dementia with Lewy bodies, one of the episodes must be confirmed [4]. These fluctuations can be present in other forms of dementia in their later stages but when present in earlier stages, they point to dementia with Lewy bodies [4].
Memory loss that impacts activities of daily living can be found in later stages of Lewy body dementia [1]. Memory loss early on is more often a characteristic sign of Alzheimer’s dementia [1]. Confusion about the individual’s whereabouts, and inability to multitask can also occur in dementia with Lewy bodies [4].
Problems with Movement
Problems with movement are signs of Lewy body dementia. Bradykinesia (slow movements) and rigidity occur in about 85% of individuals with dementia with Lewy bodies [4]. Tremor at rest is less common in individuals with this condition [4]. Loss of coordination and difficultly swallowing can occur [1]. Problems with movement greatly increase the risk of falls for these individuals [4]. This can place strain on the individual’s caregivers [4].
Autonomic Dysfunction
Autonomic dysfunction can be present in dementia with Lewy bodies and Parkinson’s disease dementia. This symptom is seen in about 90% of patients with Lewy body dementia [4]. The symptoms that result from autonomic dysfunction can be constipation, urinary incontinence, orthostatic hypotension, erectile dysfunction, and dizziness [1] [4]. Orthostatic hypotension appears as early as five years prior to the diagnosis of Lewy body dementia [4]. Syncope and falls are usually the result of orthostatic hypotension [4]. Constipation can also occur earlier in the disease process [4].


Self Quiz
Ask yourself...
- What is REM sleep behavior disorder?
- Are visual hallucinations common in Lewy body dementia?
- What does cognitive fluctuation mean?
- What are symptoms of autonomic dysfunction seen in dementia with Lewy bodies?
Diagnostic Tests and Evaluations
Throughout this course, it has been mentioned that Lewy body dementia is significantly underdiagnosed. Individuals are usually diagnosed as the disease progresses due to the symptoms that overlap with other forms of dementia and other neurological and psychiatric disorders [3]. An autopsy of the brain after death is one of the only ways to have a conclusive diagnosis of Lewy body dementia [16]. There are certain diagnostic criteria and diagnostic tests that are used to diagnose an individual with Lewy body dementia.
Diagnosis by Symptoms
Lewy body dementia is probable when an individual experiences dementia and two main features of the disease. Lewy body dementia is a potential diagnosis if the individual experiences progressive dementia and one main feature of the disease [3]. As discussed in the clinical signs and symptoms section of this course, key features of Lewy body dementia are cognitive fluctuations, dementia that progresses, problems with movement (signs of parkinsonism), REM sleep behavior disorder, and visual hallucinations [3] [16].
Timing of symptoms is relevant for distinguishing between the two forms of Lewy body dementia [3]. Currently healthcare providers use the time span of one year to distinguish the two forms [3]. If dementia occurs within one year of the appearance of movement problems, then a diagnosis of dementia with Lewy bodies is used [3]. If an individual is diagnosed with Parkinson’s disease and starts experiencing symptoms of dementia more than one year after their Parkinson’s diagnosis, then Parkinson’s disease dementia is used [3]. Some indicative biomarkers in addition to clinical symptoms are used in diagnosis [4]. Some of these biomarkers can be found in cerebral spinal fluid (CSF) and are still under research [4].
Cognitive Tests
Cognitive testing can be used to show the cognitive impairment of patients with Lewy body dementia [3]. The Mini-Mental State Examination can be used as an initial screening test [4]. This exam tests cognitive function by focusing on concentration, orientation, and memory [15]. This test can be limited since symptoms of these patients can fluctuate day to day [3]. Another cognitive function test is the Montreal Cognitive Assessment (MoCA) [15]. Providers do not usually diagnose based on a single test; instead, they use the results to look for other signs and symptoms of Lewy body dementia [4].
Imaging Tests
There are certain imaging tests that can help with diagnosis and distinguishing between other dementia disorders. A single-photon emission computerized tomography (SPECT) scan can help support a diagnosis [16]. This is a nuclear scan that can sense radioactivity [16]. If the SPECT scan shows a reduced dopamine transporter uptake in the basal ganglia, this can be a sign of Lewy body dementia [16]. This will separate the diagnosis between Lewy body dementia and Alzheimer’s disease [4]. Performing this scan alone will not lead to a possible diagnosis of Lewy body dementia; however, in combination with other diagnostic tests, the scan can lead to a more certain diagnosis [4]. Results from these scans can appear normal initially, and the scan may need to be repeated [4].
An iodine- MIBG myocardial scintigraphy can be performed to support Lewy body dementia [16]. This would show decreased communication of cardiac nerves [16]. The results may be skewed by heart disease or certain drugs [4]. A CT or MRI may be used but these imaging tests can present mixed results [4]. With Alzheimer’s disease, significant atrophy is seen in the medial temporal lobes [4]. There is normally minimal atrophy in Lewy body dementia [4].
As mentioned earlier in the course, video polysomnography is needed for the diagnosis of REM sleep behavior disorder [14]. This sleep study without the loss of muscle tone can also point towards a diagnosis of Lewy body dementia as REM sleep behavior disorder has now moved to a key feature of this disease [14].

Self Quiz
Ask yourself...
- What types of imaging tests can be used in the diagnosis of Lewy body dementia?
- Why are cognitive tests used in diagnosis of this disease?
- What criteria are needed for a probable diagnosis of Lewy body dementia?
- Can the cost of diagnostic imaging lead to a reduction in diagnosing Lewy body dementia?
Case Studies
Case Study #1
A 74-year-old male presents to his primary care provider after his wife reports abnormal behavior over the past several months. His wife reports the patient kicks and screams during sleep. The patient reports seeing little people walking around the living room during the day. The wife states the patient some days will fall asleep throughout the day while completing activities. The patient states difficulty walking and muscle stiffness.
The wife states last week the patient was supposed to go to the local grocery store to buy milk. After two hours passed, the wife called her husband as she was worried about him. He states he got lost finding the grocery store and did not know where he was. The wife said she had to drive to find her husband and bring him home. The patient also reports dizziness when standing. After the nurse obtained an orthostatic blood pressure, the patient was positive for orthostatic hypotension.
- Which form of dementia is the patient most likely experiencing?
- What type of symptoms is the patient experiencing that would point to that diagnosis?
- What diagnostic tests or evaluations should the patient undergo?
- What types of supportive treatment should the healthcare provider include in the treatment plan for this patient?
Case Study #2
A 70-year-old female presents to the emergency department via EMS after falling at home. The patient’s daughter called 911 after finding her on the floor when going to visit her. Upon arrival at the emergency department the patient is oriented to self. The patient does not know where she is or what happened to precipitate the fall. The patient has a past medical history of hypertension, diabetes type II, and Parkinson’s disease.
The patient was diagnosed with Parkinson’s disease two years prior. The daughter states the patient has been forgetful lately and not acting like herself. The daughter reports that her mom’s behavior is different from day-to-day. An MRI and the National Institutes of Health Stroke Scale (NIHSS) are used to rule out a cerebrovascular accident. A complete blood count (CBC), a complete metabolic count (CMP), and urinalysis are obtained. The patient suffered a contusion to her right cheek and a right radius fracture. The patient states that she sees figures dancing in the room and smells popcorn. The patient appears to be frightened by the hallucinations. The patient’s daughter states for the last six months the patient has had difficulty swallowing and a reduced appetite.
- Which form of dementia is the patient most likely experiencing?
- What would the MRI of the patient most likely show?
- What clinical signs of dementia is the patient exhibiting?
Management
Currently there is not a cure for Lewy body dementia, only supportive treatment. The management of this disease involves a multifaceted approach, including therapies, pharmacological treatments, and family support.
Therapies
Specific therapies can help with symptom management and help improve the individual’s quality of life. Occupational therapy can help improve a patient’s ability to complete activities of daily living. Speech therapy can help with swallowing coordination and improve the clarity and volume of speech [5]. Physical therapy can aid patients with problems with movement [5]. Mental health counseling can help individuals and their families with managing behaviors and their emotions [5].
Medications
Pharmacotherapy can help with supportive treatment but can also worsen symptoms if certain medications are taken. Below are some examples of medications that are used by patients with Lewy body dementia.
- Cholinesterase Inhibitors are used to help cholinergic activity to improve cognitive function [6].
- Rivastigmine was one of the first of these drugs to be tested [6]. Patients were noted to have improved on their cognitive exams [6]. It is also shown to reduce hallucinations and lessen anxiety [6]. This class of drugs has been said to improve the quality of life for some patients [4].
- Donepezil and Galantamine are also used to reduce dementia symptoms of hallucinations [6]. These drugs were initially targeted for patients with Alzheimer dementia, however, they are effective for individuals with Lewy body dementia as well [3]. A study was done stating even if there is not a sign of cognitive improvement, this should not be the criteria to stop the medication as this medication has been proven to protect the individual from further impairment of cognition [4].
- Atypical Antipsychotics are prescribed to patients that are not seeing a reduction of symptoms while on cholinesterase inhibitors [3]. These types of drugs are seen as controversial due to the many adverse effects that have been seen in patients [4]. Drugs such as haloperidol and olanzapine should be avoided in patients with Lewy body dementia as they can cause neuroleptic malignant syndrome (a life-threatening condition) [5]. Quetiapine, clozapine, pimavanserin, and aripiprazole are atypical antipsychotic drugs that can be used to improve agitation and help prevent cognitive fluctuations [5].
- Carbidopa-Levodopa can be used in patients to manage problems with movement [3]. This medication can cause side effects and can result in hallucinations, delusions, and increase confusion [3]. Providers should begin with low doses of this medication [3].
- Clonazepam is a benzodiazepine that can lessen the REM sleep behavior disorder that patients with dementia with Lewy bodies can experience [5]. Between 33-65% of patients with REM sleep behavior disorder can experience an injury while sleeping [5]. This medication has been proven to decrease injuries that occur during sleep [5]. Clonazepam can adversely affect individuals with gait disorders or sleep apnea [5].
- Melatonin is a hormone that can be used for patients that are affected by REM sleep behavior disorder (5). Studies have shown that the use of melatonin lessened the frequency and the severity of symptoms associated with REM sleep behavior disorder [5]. Melatonin can have side effects such as headaches in the morning, sleepiness during the day, and hallucinations [5].
- Memantine is used to treat dementia symptoms [5]. This medication is an NMDA receptor antagonist that stops effects of glutamate in the brain [5]. Memantine has been shown to improve symptoms of patients early in the disease [5].


Self Quiz
Ask yourself...
- What type of therapies are used in management of Lewy body dementia?
- What class of drugs are used to help improve cognitive function?
- What are some medications that should be avoided in patients with Lewy body dementia?
- Why is melatonin used in patients with Lewy body dementia?
Nursing Care
As mentioned before, there is not a cure for Lewy body dementia. Caring for patients with Lewy body dementia includes supportive treatment. Nurses can play a significant role in caring for these patients and providing the family with support. Home health nurses can help with frequent assessment of the patient and their environment [3]. Environmental changes may be needed to protect the patient from falls and other accidents. Home health nurses can assess the type of assistance the patient would benefit from.
Nurses can aid the family by providing education to assist in how to care for the patient. Family members and caregivers must be aware of the changes in behavior, fluctuations in cognition, and hallucinations that the individual might experience [3]. Nurses must also provide education to the caregiver of the patient on the side effects of certain medications, as they can affect an individual with this disease [7].

Self Quiz
Ask yourself...
- Are there any modifications that nurses must apply to care for patients with Lewy body dementia?
- Whose role is it to educate patients and their family members?
Family Support
Lewy body dementia is growing in recognition; however, many people might not be aware of this condition and the disease process. Family members need support from health care professionals to better care for their loved ones. Support can come in the form of education and preparing the family for the symptoms the individual may experience. The cognitive function of patients with this disease can be very limited [3]. Family members must be educated on monitoring the individual closely to promote safety [3]. These individuals are at a high risk for falling and developing aspiration pneumonia (due to swallowing difficulties) [3]. Family members should be educated in preparing for an emergency.
Individuals with Lewy body dementia may need care and the family needs to know how to inform health care providers of their specific needs. It is important to educate family members that their roles in their past relationship with the patient will likely change due to the disease process. To prevent caregiver burnout, family members must be aware of their limitations and know when they need help [7]. Modifying the patient’s home may be needed for patient safety [3]. Each patient may have specific needs and family members should know what modifications may be necessary [3].

Self Quiz
Ask yourself...
- What type of support do you feel is important to give family members of loved ones with this disease?
- What should nurses include in education for fall risk safety for family members while the individual is at home?
- Can nurses help to prevent caregiver burnout?
Prognosis
The prognosis of Lewy body dementia can be viewed as poor. As mentioned briefly earlier in this course, this disease is progressive and after diagnosis, the life expectancy is five to eight years [3]. The range of expectancy has also been attributed to delay in diagnosis, which can further delay supportive treatment to improve quality of life for the individual [3]. Patients can die from complications from the disease. Complications can include cardiac complications, falls, adverse effects from medications, pneumonia, and suicide [3].
Compared to Alzheimer’s dementia, the risk of hospitalization or death due to respiratory infections is higher in patients with Lewy body dementia [8]. The median age at death is said to be similar between patients with Alzheimer’s dementia and Lewy body dementia [8]. The life expectancy from diagnosis to death is shorter in patients with Lewy body dementia [8]. The patient’s environment has been shown to play a role in the increased risk of mortality [8]. Patients in nursing homes have been shown to have a higher risk of mortality [8]. Caregivers can decrease the risk of complications by educating themselves on this disease and keeping their loved ones safe.

Self Quiz
Ask yourself...
- What are some complications of Lewy body dementia?
- How can the patient’s environment increase the risk of mortality with this disease?
- Why do you think there is delay in diagnosis with Lewy body dementia?
Resources for Family Support
Lewy body dementia is a diagnosis that can affect all aspects of an individual’s life and their family members lives. As nurses we must provide support for family members so they can better care for their loved ones and improve their quality of life. As recognition of this condition grows, family support resources are increasing. The Lewy Body Dementia Association is a nonprofit organization that raises awareness and provides support for families with individuals that suffer from Lewy body dementia [10]. Support groups can be found on their website to help families across the country in their local area [10].
The Lewy Body Dementia Association was started by caregivers of individuals with this condition. They also focus on education and research into the disease. This association is a resource for family members [10].
Another resource for family members is The Lewy Body Dementia Resource Center. This is a nonprofit charitable organization that gives assistance and support to those who care for someone with Lewy body dementia [9]. This organization was founded by caregivers of individuals with Lewy body dementia. They have a support phone line that is available seven days a week to answer questions [9]. They also promote research and early diagnosis of this disease [9].

Self Quiz
Ask yourself...
- How can support of family members improve the quality of life of a patient with Lewy body dementia?
- What are some examples of resources for caregivers of individuals with Lewy body dementia?
- Can providing resources to the community help with early diagnosis of this disease?
Research Programs
Lewy body dementia is the second most common form of dementia in the United States [4]. This illness is thought to be underdiagnosed and commonly mistaken for other neurological disorders [3]. Research on Lewy body dementia can decrease the time it takes to diagnose a patient, and can help with management of the condition.
The National Institute of Neurological Disorders and Stroke provides support for a variety of research endeavors for Lewy body dementia [11]. In 2021 The National Institute of Health spent $93 million dollars on Lewy Body dementia research [11]. One program is the Biomarkers for Lew body dementias program. This program aims to increase clinical data collection from patients with this condition, find biomarkers to expand further research, and allow access to the science community to help with further studies [11]. Another program is the Parkinson’s Disease Biomarkers Program. This program’s purpose is to collectively research with healthcare professionals, patients and family members, and technology professionals to increase biomarker research [11].
Biomarker research has been increasing in Lewy body dementia. A biomarker is a feature that can specifically indicate a certain disease [12]. For quite some time there were not any identified biomarkers for Lewy body dementia. There are certain biomarkers that aid in distinguishing Alzheimer’s disease from Lewy Body dementia [13]. These biomarkers can be assessed through imaging or in cerebral spinal fluid [13]. Currently these biomarkers are only helpful if another disease is doubtful [13].
New biomarkers are needed to separate Alzheimer’s dementia from Lewy Body dementia and other neurological disorders [13]. Biomarkers that can help with early diagnosis would be beneficial for early treatment [13].


Self Quiz
Ask yourself...
- Why is researching biomarkers important for early diagnosis of Lewy body dementia?
- Is there more research conducted on Alzheimer dementia than on Lewy body dementia?
- What are some organizations that promote research for this disease?
Conclusion
Lewy Body dementia affects 1.4 million Americans [2]. The disease is underdiagnosed and often diagnosed incorrectly. Incorrect diagnoses can lead to worsening of symptoms and the administration of drugs that can lead to adverse effects.
Educating healthcare providers and the community about Lewy body dementia can improve quality of life for individuals with the disease. As nurses, we must be informed about this disease to better educate our patients and their caregivers, and to know how to advocate for our patients.
Understanding Lupus Nephritis
Introduction
A lupus diagnosis and the complications that arise can be devastating for patients. Nurses are often looked to for support and answers, so it is important to educate ourselves on these serious conditions. Lupus nephritis (LN) is considered one of the most severe organ manifestations of the autoimmune disease systemic lupus erythematosus (SLE). Essential knowledge on lupus nephritis includes the defining features, epidemiology, pathophysiology of normal kidney function and lupus nephritis, clinical presentation, and treatments.
Lupus Nephritis
Lupus nephritis (LN) is an organ manifestation of the autoimmune disease systemic lupus erythematosus (SLE). The cause of lupus erythematosus is not known. Researchers suggest a genetic predisposition, but a genetic link has not been identified (2). This is a difficult reality, as patients and healthcare providers usually hope for a why. We will discuss the definition, prevalence, pathophysiology, manifestations, clinical diagnosis guidelines, and treatment regimens for LN.
Definition
Lupus nephritis (LN) is considered a condition and a manifestation. LN is one of the most severe organ manifestations of the autoimmune disease systemic lupus erythematosus (SLE). LN is a form of glomerulonephritis, which is inflammation of the glomeruli (the tiny filters within the kidneys). This inflammation causes significant imbalances within the body due to impaired kidney function.
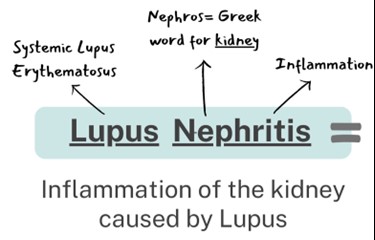
Overview of Systemic Lupus Erythematosus (SLE)
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by a loss of immune tolerance of endogenous nuclear material, which leads to systemic autoimmunity that may cause damage to various tissues and organs (1). Essentially, the damage to DNA structures causes the body’s immune system to be incidentally programmed to attack its own tissue. There are two types of lupus: systemic lupus erythematosus and “discoid” lupus erythematosus. SLE is systemic, meaning it can affect almost any organ system or tissue and presents in different manifestations impacting the skin, joints, kidneys, and brain (2). “Discoid” lupus erythematosus only affects the skin tissue. Our focus will be on systemic lupus erythematosus (SLE) as we gain a deeper understanding of lupus nephritis.
The causes of SLE are unknown but many attribute it to genetic, environmental, and hormonal factors. SLE is hard to diagnose because the symptoms are often mistaken for those of other conditions. There is no cure for SLE, but symptoms can be managed. SLE presentation and prognosis are highly variable, with symptoms ranging from minimal to life-threatening. Patients with lupus may experience periods of exacerbation of symptoms, sometimes called 'flares', as well as periods of remission. SLE is associated with substantial morbidity and mortality, particularly caused by renal and cardiovascular disease and infections. LN is considered one of the most severe manifestations of SLE.
SLE can be compared to a guard dog intended to protect your home. The guard dog (immune system) protects you from unwanted intruders (infection), but also bites friends, family, and the mailman (your own organ tissue)!

Self Quiz
Ask yourself...
- Have you cared for a patient with autoimmune disorders impacting the skin or joints?
- Are you familiar with other autoimmune conditions?
- How are systemic and focal conditions different?
- Can you list the two types of lupus?
Epidemiology and Statistical Evidence of Lupus Nephritis
Systemic lupus erythematosus has an estimated prevalence of about 10–150 per 100,000 persons (2). However, a large number of people could be undiagnosed due to being asymptomatic or the symptoms mistaken for other diseases. An average of 40% of SLE patients develop lupus nephritis (LN). Those diagnosed with SLE at a younger age are at a higher risk of developing LN and other complications (1).
SLE in general is more prevalent in women, especially women of reproductive age, than in men; the ratio is 9:1 (1). Therefore, 90% of SLE cases are women. However, men who have been diagnosed with SLE more commonly develop LN than women with SLE. Numerous studies have also found that the prevalence of LN in patients with SLE is higher in African American, Hispanic, and Asian populations (1). The impact of SLE disproportionately affects children and adults living in poorer geographic areas (8).
Within 10 years of the initial SLE diagnosis, 5–20% of patients with LN develop end-stage kidney disease and the multiple comorbidities associated with immunosuppressive treatment (1). Mortality in LN is quite variable ranging in between 15% and 25% (6). It is important to remember that the treatments are also very risky because it is difficult to balance the risks and benefits of suppressing the immune system. LN is a topic of significant research, so nurses can have a meaningful impact in raising awareness and encouraging hope for more advanced treatment development.

Self Quiz
Ask yourself...
- Can you name the population at greatest risk for developing SLE?
- Do you think all ethnicities are impacted equally?
- Do you think men and women are impacted equally when developing SLE and LN?
- Have you ever cared for a patient with systemic lupus erythematosus? If so, what were specific problems they faced?
Normal Kidney Function
The kidneys have several life-sustaining functions. The kidney serves to maintain fluid and chemical homeostasis and to contribute to hemodynamic stability (3). The renal tubules of the kidneys have unique and vital roles. Daily urine output is about 1–2 L, and over 98% of the glomerular filtrate is reabsorbed by the renal tubules (3).
There is a delicate balance and interdependency between the kidneys and other organs. For example, the kidneys produce hormones that help regulate blood pressure and control calcium metabolism, the kidneys also release a hormone that stimulates red blood cell production. A simple and fun mnemonic formula to help you remember the vital functions: A WET BED.
A WET BED: Functions of the Kidneys
A - controlling ACID-base balance
W - controlling WATER balance
E - maintaining ELECTROLYTE balance
T - removing TOXINS and waste products from the body
B - controlling BLOOD PRESSURE
E - producing the hormone ERYTHROPOIETIN
D - activating vitamin D
Controlling acid-base balance
- Our bodies always have a state of delicate equilibrium among the acids and bases, which has a parameter known as pH.
- The kidneys excrete or retain acids and bases when there is an excess or lack of them.
- The normal pH of the blood is 7.35 to 7.45.
Controlling water balance
The kidneys regulate the volume of urine produced and adapt to one’s hydration level to maintain water balance.
Maintaining electrolyte balance
The kidneys filter specific electrolytes from the blood, return them back into circulation, and excrete excess electrolytes into the urine. Kidneys maintain electrolyte balances like sodium and phosphate.
Removing toxins and waste products from the body
The kidneys remove water-soluble waste products and toxins and excrete them in urine.
Controlling blood pressure
The kidneys produce an enzyme called renin, which converts the angiotensinogen produced in the liver into angiotensin I, that is later converted in the lungs into angiotensin II. Angiotensin II constricts the blood vessels and increases blood pressure. Another way the kidneys help reduce elevated blood pressure is they produce more urine to reduce the volume of liquid circulating in the body to compensate.
Producing the hormone erythropoietin
The kidneys produce a hormone called erythropoietin, which aids in the creation of more red blood cells (erythrocytes), which are vital for the transport of oxygen throughout all the tissues and organs.
Activating vitamin D
The kidneys transform calcifediol into calcitriol, the active form of vitamin D.

Self Quiz
Ask yourself...
- What are ways to help remember the major functions of the kidneys?
- How do the kidneys regulate and maintain electrolyte balance?
- Can you list examples of how electrolyte imbalances affect various organ functions? (example: cardiovascular system)
- What are some ways the kidneys help to regulate blood pressure?
Anatomy and Physiology of the Kidneys
It is important to review the anatomy and physiology of the kidneys. The urinary system as a whole is composed of two kidneys, a pair of ureters, a bladder, and a urethra. The kidneys are located at the back of the abdominal wall and at the beginning of the urinary system. The size of each kidney is dependent on age, sex, and height, but the average length is approximately 10–12 cm, and the right kidney may be slightly smaller than the left kidney (3). The kidneys are made up of nephrons, which are microscopic structures composed of a renal corpuscle and a renal tubule.
The average human kidney is composed of approximately one million individual functioning nephrons, each containing a single glomerulus or filtering unit (3). The function of filtration is accomplished by three major components of nephron activity: (1) glomerular filtration, (2) tubular reabsorption, and (3) tubular secretion. These components respond to factors including renal blood flow, neuroendocrine effects, and the fluid and nutrient supply to the body.
Vascular Structure of the Kidneys
The kidneys are perfused with 1.2 liters of blood per minute, which represents about 25% of the cardiac output (3). From the abdominal aorta, the main renal artery carries blood into the kidney and then branches to segmental arteries, then to interlobar arteries, then branches to arcuate arteries, followed by branching to interlobular arteries, and finally onto afferent arterioles (3). Vascular resistance in the kidney is low when compared to other vascular beds within the body.
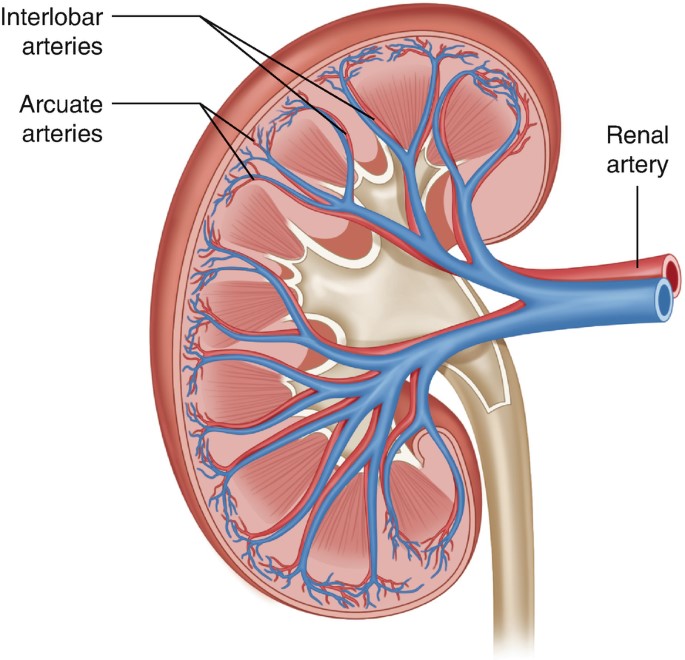
Figure 2. Vascular Structure of the Kidneys (3)

Self Quiz
Ask yourself...
- Can you explain the major functions of the kidneys?
- How would you describe the vascular structure of the kidneys?
- Are you familiar with focused physical assessment techniques for assessing peripheral edema?
- Have you ever cared for a patient with impaired renal function?
Pathophysiology of Lupus Nephritis

Have you ever played dominos? If aligned properly, the domino effect will rapidly cause a consecutive reaction. The immune response can be compared to this domino effect. One cellular action will cause the response and activation of many other cells. A perceived foreign body activates certain immune responses. In most cases, this maintains life. In some cases, it is harmful to vital tissue.
An autoimmune response to the renal system involves the T- and B-cell interactions stimulating interstitial plasma cell generation in the kidney; interstitial tissue leads to restricted autoantibody-producing plasma cells (6). This cascade of inflammatory response is facilitated by the production of interferon-α (IFN-α), which augments autoreactive B-cell activation and its reciprocal interaction in T-cell activation. This prolonged local injury and inflammation attracts neutrophils that try to help alleviate this inflammation, but the sustained local injury leads to neutrophil apoptosis (cell death), which further causes local injury. This injury further augments the inflammatory response by enhancing the intrarenal autoimmunity and inflammation, leading to kidney tissue injury (6).
Lupus nephritis is considered a type-3 hypersensitivity reaction. A hypersensitivity reaction is an inappropriate or overreactive immune response to an antigen. Symptoms typically appear when an individual has had a previous exposure to the antigen. Hypersensitivity reactions can be classified into four types (9).
- Type I - IgE mediated immediate reaction
- Type II - Antibody-mediated cytotoxic reaction (IgG or IgM antibodies)
- Type III - Immune complex-mediated reaction
- Type IV - Cell-mediated, delayed hypersensitivity reaction
In type III hypersensitivity reactions, antigen-antibody aggregates called "immune complexes” are formed. When someone has lupus, a number of DNA are damaged and have cell death, which exposes parts of the nucleus in the cell, and parts of the nucleus are recognized by the immune system as “nuclear antigens.” Remember, the immune system attacks antigens. The antigen-antibody complexes are transported by the blood and are deposited in various tissues, such as the kidneys.
When the complexes are deposited, it initiates the recruitment of inflammatory cells (monocytes and neutrophils) that release lysosomal enzymes and free radicals at the site of immune complexes, causing damage to that tissue (9). Examples of tissues that it may deposit in include skin, joints, blood vessels, or glomeruli. In the case of LN, the site of damage is the glomeruli of the kidneys, and it can have a disastrous impact.

Self Quiz
Ask yourself...
- Can you describe the differences between the types of hypersensitivity reactions?
- How would you describe the composition of the antigen-antibody complexes?
- Can you name types of inflammatory cells?
- Can you think of reasons the glomeruli of the kidneys may be a deposit site for free radicals and antigen-antibody complexes?
Clinical Presentation
The clinical manifestations of LN can be unpredictable and very different among patients. Patients may present with no symptoms at all, while other patients may have significant proteinuria progressing to acute renal failure. Understanding the disease and its progress is vital for nurses to provide optimal care and education to the patient. Remember, these patients may have signs and symptoms from their lupus already, so isolating renal impairment is essential.
Signs and Symptoms
Signs and symptoms of systemic lupus erythematosus depend on the body systems that are affected by the disease. Systemic symptoms include fatigue, malaise, weight loss, anorexia, and fever. The patient may report musculoskeletal symptoms, including joint and muscle pain, joint swelling and tenderness, hand deformities, and skin lesions such as the characteristic “butterfly rash” or maculopapular rash (small, colored area with raised red pimples). Other symptoms stem from the central nervous system (visual problems, memory loss, mild confusion, headache, depression).
It is important for the nurse to establish a history of symptoms related to the hematological system (venous or arterial clotting, bleeding tendencies), cardiopulmonary system (chest pain, shortness of breath, lung congestion), or gastrointestinal system (vomiting, difficulty swallowing, diarrhea, and bloody stools). To differential LN, it is important to focus on specific function impairment and manifestations arising from the kidneys (1).
Nephritic symptoms related to hypertension and poor kidney function:
- Peripheral edema
- Headache and dizziness
- Nausea and vomiting
Nephrotic symptoms related to proteinuria:
- Peripheral or periorbital edema
- Coagulopathy
Patients may report the following:
- Foamy urine
- Blood in the urine
- Dark urine
- Changes in the frequency of urination
- Weight gain and swelling, including the legs and hands
Classifications of Lupus Nephritis
There are six classifications of lupus nephritis:
- Class I: Minimal mesangial
- Prevalence 10-25% of people with lupus (SLE)
- 5% of lupus nephritis cases
- Clinical findings: Kidney biopsy shows build-up of antigen-antibody complex deposits; urinalysis is normal
- Class II: Mesangial proliferative
- Prevalence: 20% of lupus nephritis cases
- Clinical findings: Mesangial hypercellularity of any degree with mesangial immune deposits
- Class III: Focal LN
- Prevalence: 25% of lupus nephritis cases
- Clinical Findings: Active lesions exist in less than half of the glomeruli; hematuria and proteinuria
- Class IV: Diffuse proliferative
- Prevalence: 40% of lupus nephritis cases
- Very severe subtype
- Clinical findings: More than 50% of the glomeruli are affected with active lesions
- Immune complex deposits exist under the endothelial when viewed with an electron microscope
- Hematuria and proteinuria
- Hypertension, elevated serum creatinine, and raises anti-dsDNA (an antibody tested to diagnose lupus)
- Kidney failure is common
- Class V: Membranous
- Prevalence: 10% of lupus nephritis cases
- Clinical findings:
- Hematuria and proteinuria
- Significant systemic edema
- The glomerular capillary wall is thicker in segments
- High risk for renal vein thromboses, pulmonary embolism, or other thrombotic complications; active lesions are present
- Class VI: Advanced sclerotic LN
- Global sclerosis – typically more than 90% of the glomeruli are damaged and have active lesions
- Clinical findings: Progressively worsening kidney function

Self Quiz
Ask yourself...
- What are some differences in clinical manifestations between renal impairment and renal failure?
- Can you name the different classes of LN?
- How are clinical findings of Class I and Class IV different?
- Can you describe the glomerular function impairment in Class IV LN?
Diagnosis
LN is often the presenting manifestation resulting in the diagnosis of SLE (1). SLE is diagnosed clinically and serologically with the presence of certain autoantibodies. Evaluating kidney function in patients diagnosed with SLE is important as timely detection and management of renal impairment has been shown to greatly improve renal outcomes. The clinical presentation and laboratory findings for LN may differ, ranging from normal urinalysis and normal renal function test results to severe proteinuria, nephrotic syndrome, or acute nephritic syndrome, which can result in acute kidney failure (1). Monitoring for the development of lupus nephritis is done by a urinalysis, creatinine, urine albumin-to-creatine ratio, glomerular filtration rate (GFR), and a kidney biopsy.
Laboratory tests for SLE disease activity include the following:
- Antibodies to double-stranded DNA (dsDNA)
- Complement (C3, C4, and CH50)
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (CRP)
Laboratory tests to evaluate kidney function in SLE patients:
- Urinalysis
- Check for protein, red blood cells (RBCs), and cellular casts
- Serum creatinine assessment
- Blood urea nitrogen (BUN) testing
- Spot urine test for creatinine and protein concentration
- 24-hour urine test for creatinine clearance and protein excretion
Urinalysis
A high level of protein or red blood cells in the urine signifies kidney damage. The Systemic Lupus International Collaborating Clinics (SLICC) define renal involvement in lupus as a 24-hour urinary protein excretion of 0.5 g daily or the presence of red blood cell casts in urinary sediment (1). Urinary protein excretion in a 12-hour or 24-hour urine collection provides the best estimate of proteinuria. The most common abnormalities in urinary sediment in patients with LN are leukocyturia, hematuria, and granular casts (1).
Blood Tests
Creatinine is a waste product from the normal breakdown of muscles in your body. Kidneys remove creatinine from the blood. An elevated creatinine reveals damage to the kidneys because it is not functioning as it should. Glomerular filtration rate (GFR) also is an important test to determine how well the kidneys are functioning.
Kidney Biopsy
The next step in diagnosing LN would be a kidney biopsy. Kidney biopsy is currently the gold standard for confirming a diagnosis of LN and characterizing the LN subtype on the basis of histological patterns (1). A kidney biopsy is usually performed as a percutaneous needle biopsy with minimization of risk factors for bleeding complications. The piece of tissue removed is examined under a microscope by a pathologist.
A kidney biopsy can (1):
- Confirm a diagnosis of lupus nephritis
- Help in determining how far the disease has progressed
- Guide treatment

Self Quiz
Ask yourself...
- Can you describe what the glomerular filtration rate (GFR) is important for?
- Can you name components of a urinalysis?
- Have you cared for a patient with hematuria?
- Can you think of reasons a patient may be apprehensive about having a kidney biopsy?
Treatment
Treatment of LN is highly individualized. There is not a specific FDA-approved drug specifically given for the treatment of LN. Treatment cannot be a “one-size fits all” approach, but a plan to target renal impairment and avoid causing further damage. The goal of immunosuppressive therapy is the resolution of inflammatory and immunologic activity. Unfortunately, aggressive treatments can result in additional harm to patients. As the therapy of LN consists of potentially toxic drugs, it may be harmful to begin treatment without a definitive diagnosis (4).
Treatment of LN usually involves immunosuppressive therapy and glucocorticoids. The goals of LN treatment are to achieve rapid remission of active disease, prevent renal flares, prevent progression of chronic kidney disease (CKD), minimize treatment-associated toxicity, and preserve fertility (1). Immunosuppressive therapy is used to treat active focal (class III) or diffuse (class IV) LN or lupus membranous nephropathy (class V); but not usually used to treat minimal mesangial (class I), mesangial proliferative (class II), or advanced sclerosing (class VI) LN.
The treatment of focal or diffuse LN has two main components: initial therapy with anti-inflammatory and immunosuppressive agents to slow kidney injury, followed by long-term subsequent immunosuppressive therapy to control the chronic autoimmune processes of SLE and encourage the repair of damaged nephrons (1).
Treatment Goals
- Reduce inflammation in the kidneys
- Decrease immune system activity by blocking immune cells from attacking the kidneys directly and making antibodies that attack the kidneys
- Treatment of systems (hypertension, fluid retention)
- Support kidney function
Medications
Medications for the treatment of LN include (2):
- Corticosteroid
- Prednisone
- Immunosuppressant
- Cyclophosphamide
- Mycophenolate mofetil
- Hydroxychloroquine (Quinoline drug used to treat or prevent malaria; used for autoimmune response)
Blood pressure control:
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs)
- Diuretics
- Beta blockers
- Calcium channel blockers
| Risk Target and Goals | Interventions |
| Lupus nephritis-related mortality | Chloroquine or hydroxychloroquine |
| Control of blood pressure and hyperlipidemia | |
| SLE and LN activity to avoid ESRD | Immunosuppression no less and no more than necessary |
| Hyperfiltration and proteinuria to avoid end-stage renal disease (ESRD) | Renin-angiotensin-aldosterone system inhibition |
| Avoid drug toxicity | Infections: Reduce or eliminate corticosteroids, PJP prophylaxis, vaccination, personal infection control |
| Malignancy: Avoid cumulative cyclophosphamide of over 30 grams | |
| Fractures: Reduce or eliminate corticosteroids, vitamin D supplementation, bone density monitoring | |
| Symptoms | Improvement or stabilization of the serum |
| Improvement of the urinary sediment | |
| Nephrotic syndrome: loop of Henle diuretics |
Treatment Guidelines
Key points of American College of Rheumatology guidelines for managing lupus nephritis (1):
- Patients with clinical evidence of active and previously untreated lupus nephritis should have a kidney biopsy to classify the disease according to the International Society of Nephrology/Renal Pathology Society (ISN/RPS) criteria.
- Patients with lupus nephritis should receive background therapy with hydroxychloroquine, unless contraindicated.
- Glucocorticoids plus either cyclophosphamide intravenously or mycophenolate mofetil orally should be administered to patients with class III or IV LN.
- Patients with class I/II nephritis do not require immunosuppressive therapy.
- Angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers should be administered if proteinuria reaches or exceeds 0.5 g/day (1).
- Blood pressure should be monitored and maintained at or below 130/80 mm Hg.
- Patients with class V lupus nephritis are generally treated with prednisone for one to three months, followed by tapering for one to two years if a response occurs.
For those who progress to kidney failure, treatment options include dialysis and kidney transplant.

Self Quiz
Ask yourself...
- Can you think of examples of treatments for blood pressure control other than medications?
- Can you think of treatments for LN and the risks of these treatments?
Complications
Complications of LN can be categorized into comorbidities from the actual condition and treatment-associated adverse outcomes. As mentioned, immunosuppressive therapy and glucocorticoids have harmful risks of their own. Comorbidities can include complications of the renal system and cardiovascular system. Treatment-associated complications can include infections, osteoporosis, cardiovascular disease, and reproductive impairment (1).
SLE and treatments, including glucocorticoids and calcineurin inhibitors, can cause hypertension, hyperlipidemia, and nephrotic syndrome (1). Many patients with LN have progressive CKD with associated comorbidities, such as anemia, osteoporosis, and other bone and mineral diseases. These factors contribute to vascular risks of progressive CKD and can lead to cardiovascular disease.
The prevalence of osteopenia and osteoporosis is high in patients with LN taking immunosuppressive therapy. In patients with severe nephrotic syndrome, a loss of plasma proteins, including clotting inhibitors, transferrin, immunoglobulins, and hormone-carrying proteins (such as vitamin D-binding protein), can lead to protein malnutrition, anemia, hormonal and vitamin deficiencies, hyperlipidemia, and increased risk for venous or arterial thrombosis (1). High-dose cyclophosphamide therapy correlates with premature gonadal failure in some cases, which is a complication of male and female reproductive organs (1).
Immunosuppressive agents increase the risk of infection, which can be further increased by disease activity, leukopenia, and CKD-related factors, such as nephrotic syndrome. Patients receiving immunosuppressive treatment can be at risk for poor outcomes with pneumocystis jirovecii pneumonia, herpes, hepatitis B, tuberculosis, influenza, and pneumococcal infection (1).
End-stage renal disease (ESRD) is a major complication of LN. Some 5–20% of patients with LN develop ESRD (1). By definition, all patients with LN have chronic kidney disease (CKD), but not all patients with CKD progress to ESRD. Essentially, ESRD occurs when the kidneys are no longer able to function to maintain life and either dialysis or a kidney transplant is needed.

Figure 4. Complications of Lupus Nephritis

Self Quiz
Ask yourself...
- Can you describe how renal impairment impacts the cardiovascular system?
- Can you name signs and symptoms of renal impairment?
- Have you cared for a patient experiencing adverse reactions to medications for immunosuppression?
- Are you familiar with risk factors for long-term corticosteroid use?
Screening and Prevention of Lupus Nephritis
Screening for LN onset and relapses is important for prompt treatment to improve outcomes. There are many new biomarkers under exploration for predicting and assessing LN (1). Patients with SLE should be screened periodically, even during periods of remission, every six to 12 months, or more frequently when clinically indicated (1). During regular check-ups, screening for LN onset or flares in patients with SLE should include evaluation of volume status, blood pressure measurement, urinalysis, and measurement of serum parameters. Elevation of serum creatinine level, the appearance of dysmorphic erythrocytes, cellular casts and new-onset proteinuria may indicate onset of LN (1). Nurses should encourage patients to regularly attend their appointments.
Patient Education
Patient education must be individualized to each unique patient. Lupus or LN may be a new diagnosis, or the patient may have been diagnosed previously. Teaching topics should include education on the disease process, the purpose of treatment regimens, and the importance of compliance.
Education on medication regimens is essential. Include the purpose, dosage, and possible side effects of all medications. Teach the patient when to seek medical attention. Provide tips such as wearing a medical alert bracelet or lanyard noting the condition and medications so appropriate action can be taken in an emergency. Provide resources on smoking cessation for patients who use tobacco. Teach the female patient the importance of planning pregnancies with medical supervision because pregnancy is likely to cause an exacerbation of the disease and the disease may cause negative pregnancy outcomes.
Discuss all precipitating factors that need to be minimized or avoided, including fatigue, vaccination, infections, stress, surgery, certain drugs, and exposure to ultraviolet light. Teach the patient to avoid strenuous exercise, but instead set goals of steady pace and balance. Describe pain management strategies and the importance of adequate nutrition. The patients may have concerns about skin care products and cosmetics. Teach the patient that these products should be hypoallergenic and approved by a provider prior to use. Encourage the patient to contact appropriate support groups available in the area.
Diet
Education on diet and nutrition for patients with LN can be very helpful in managing this condition. A diet regimen can be challenging because many people with this condition may also experience weight loss or gain, inflammation, osteoporosis, high blood pressure, and atherosclerosis. Recognizing specific nutritional concerns for each condition is important. A registered dietitian would be a meaningful resource for those with LN.
A kidney-healthy diet consists of low salt, low fat, and low cholesterol, with an emphasis on fruits and vegetables. Eating the right foods can help patients manage kidney impairment, maintain a healthy weight, and lower their blood pressure. Steroid medications can cause significant fluctuation in weight and energy.
The provider may advise restrictions on dietary protein intake. According to nephrology research, consuming more than 1.5 g of protein per kilogram per day can overwork the kidney filters, causing hyperfiltration (5). Many proteins are composed of amino acids that are converted to acids that are harmful to the kidney in large amounts; a diet high in animal proteins also contains sulfuric and phosphate acids that promote kidney damage (5). Potassium intake is also an important aspect of diet for those with LN. Potassium is secreted by the kidneys and may rise when kidney function declines; abnormal potassium levels can impact muscle function and increase the risk of hypertension, coronary artery disease, or stroke (5). A balanced diet with special considerations is a key teaching factor. It may be helpful to seek out resources from registered dieticians when needed.
Overview of Teaching Topics
Topics for education:
- Disease process
- Treatment plan
- Diagnostic studies and lab results
- Medications
- Purpose
- Dosage
- Side effects
- Contraindications
- Infection control
- Diet
- Tobacco cessation resources
- Reproductive complications
- Techniques to minimize ultraviolet exposure
Resources
The American College of Rheumatology (ACR) and Lupus Foundation of America (LFA) are excellent resources for patient with lupus that provide education and resources to improve overall well-being. The Lupus Foundation of America has a team of physicians, scientists, health educators, and individuals with lupus who work together to create resources, support groups, awareness initiatives, and programs. Patients can go to the “Ask our Health Educator” portal and get answers to questions they may have.
Conclusion
Nurses need to have a good understanding of lupus nephritis to provide patients with appropriate support and advice about how to maintain wellbeing and lead meaningful active lives. Knowledge on disease pathophysiology, manifestations, treatments, and complications is valuable for this serious condition. Patients often rely on nurses to support and empower them on this pathway.

Self Quiz
Ask yourself...
- How would you describe lupus to a non-medical person?
- Can you describe the difference between normal immune response and autoimmune response?
- Can you name clinical signs and symptoms specific to lupus?
- What is the most reliable diagnostic tool for LN?
- What are some ways the nurse can advocate for a patient having a kidney biopsy?
- How would you empower a patient with a new diagnosis of LN in knowledge of medications and their treatment regimen?
Alcohol Use Disorder: Long Term Effects and Complications
Introduction
Alcohol use disorder (AUD) is one of the most widespread psychiatric disorders and is estimated to affect approximately 29 million individuals aged 12 and older in the United States (9). According to the 2021 National Survey on Drug Use and Health, 28.6 million adults ages 18 and older have AUD and roughly 900,000 adolescents ages 12 to 17 have AUD (7).
Alcohol is the most prevalent misused substance in America with alcohol-related issues causing more than 85,000 deaths annually in the United States and three million deaths a year globally (9, 12). Globally, about 240 million people are affected by AUD, especially in Europe and America (9).
AUD is linked to motor vehicle accidents, dementia, depression, homicide, and suicide (9). The condition can also lead to social complications, such as legal problems, relationship issues, and economic stressors (due to the cost of alcohol, required medical care, missed time at work, and job loss). Individuals with AUD can end up isolating themselves from the individuals who are trying to help them most, including family members and friends.
Moderate alcohol use for most adults—no more than two drinks a day for men and one for women—is relatively harmless. An alcoholic drink includes 12 fluid ounces of regular beer, 10 fluid ounces of malt liquor, five fluid ounces of wine, or 1.5 fluid ounces of 80-proof distilled spirits (3, 4). Heavy alcohol drinking is defined as having four or more drinks per day or eight or more drinks per week for women and five or more drinks per day or 15 or more drinks per week for men (4).
Small amounts of alcohol, in particular red wine, can have beneficial cardiovascular effects, but heavy drinking can lead to serious health issues, such as cancer, cardiovascular disease, liver disease, osteoporosis, and infections (3, 4). Men are more likely than women to develop AUD, but women’s health suffers more than men’s, even at lower levels of consumption (3). Individuals with lower levels of education and of lower income experience AUD more than their counterparts (9).
Drinking can become problematic for those people who have psychological traits of impulsiveness, low self-esteem, and the constant need for attention and approval. Individuals who lack personal insight about drinking can develop AUD. For example, those who use alcohol to emotionally self-medicate (i.e., unwind from a stressful day) can develop alcohol-related issues (3).
Unfortunately, many individuals with AUD deny having a problem with alcohol and therefore do not seek treatment until faced with medical issues or legal complications. Regardless of how severe a patient’s drinking problem may seem, evidence-based treatment that includes medications, behavioral therapies, and support groups can help individuals achieve and maintain recovery.


Self Quiz
Ask yourself...
- How extensive is AUD in the United States and globally?
- How many fluid ounces constitute an alcoholic drink for beer, malt liquor, wine, and distilled spirits?
- To which health risks does heavy drinking contribute?
- Which psychological traits can increase the risk of AUD?
Pathophysiology
Alcohol ethanol or ethyl alcohol is a chemical substance found in alcoholic beverages, such as beer, hard cider, malt liquor, wines, and distilled spirits (liquor). Alcohol is the byproduct of yeast fermentation of sugars and starches. Alcohol is also found in some medicines, mouthwashes, and household products, including vanilla extract and other flavorings (4).
Alcohol use disorder is defined by the National Institute on Alcohol Abuse and Alcoholism as a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences (7). The term alcohol use disorder includes the terms alcohol abuse, alcohol dependence, alcohol addiction, and alcoholism. The condition affects brain function and is classified as mild, moderate, or severe (7).
Several evidence-based theories explain the development of AUD in individuals. These theories are (9):
- Positive-effect regulation: This occurs when people consume alcohol to seek positive rewards like pleasure or euphoria. Alcohol may be consumed to enhance social experiences and positive emotions.
- Negative-effect regulation: Individuals may drink alcohol in response to negative or distressing situations as a means to self-medicate and alleviate feelings of anxiety, depression, or low self-worth.
- Pharmacological vulnerability: This theory explains the differences in how individuals respond to the acute and chronic effects of alcohol. Some individuals are more prone to the rewarding effects of alcohol, or they have a reduced ability to metabolize alcohol, thus increasing their chances of developing AUD.
- Deviance proneness: Individuals with a history of deviant behavior or impaired socialization during childhood are more prone to AUD because these individuals use alcohol to self-medicate to alleviate symptoms of anxiety, depression, or low self-worth.
Cytosolic alcohol dehydrogenase (ADH) is the enzyme that metabolizes alcohol in the liver, and this metabolism process produces acetaldehyde as a byproduct. Acetate is then formed by the metabolism of acetaldehyde by the enzyme aldehyde dehydrogenase (ALDH).
Acetate then enters the body’s various metabolic pathways. Additionally, ADH is present in the gastrointestinal tract as well as the liver, which leads to the initial metabolism of alcohol during its ingestion. This is referred to as first-pass metabolism. The enzyme CYP2E1 of the cytochrome P450 system is upregulated in chronic alcohol users, which leads to an increased rate of alcohol metabolism (9).
Several factors affect the metabolism of alcohol (9):
- Women have a higher initial blood alcohol concentration following consumption because they have a slower first-pass metabolism due to lower levels of ADH; however, women eliminate alcohol consumption faster than males.
- Alcohol elimination declines with age, which is why older adults may experience a lower tolerance to alcohol than when younger, or why they may experience more severe hangover symptoms.
- In pregnancy, the fetal liver has an incomplete expression of enzymes CYP2E1 and ADH, leading to slower alcohol metabolism. This means that the fetus is exposed to the mother’s consumption of alcohol for a prolonged period, increasing the risk of fetal alcohol spectrum disorders.
- Native Americans have been found to metabolize alcohol faster due to the expression of beta-3 Class 1 ADH isoforms than individuals who express only the beta-1 Class 1 ADH isoform.
- When an individual fasts, alcohol metabolism is slowed due to decreased levels of ADH during a fasting state. Alternatively, food intake increases blood flow to the liver and allows fructose and other sugars to speed the metabolism of alcohol.
- The highest rates of alcohol elimination occur in the late evening versus during the daytime hours.
- Medications that have ADH inhibition or H2 receptor-blocking properties decrease the rate of alcohol elimination. This reduces first-pass metabolism in the stomach and increases blood alcohol levels.
- Heavy drinking increases the expression of the CYP2E1 enzyme, which increases alcohol elimination; however, this is eventually slowed in individuals with advanced liver disease.
Alcohol use can permeate every organ and tissue in the body, resulting in systemic dysfunction. The Complications and Long-Term Effects section explores how alcohol use impacts the body.

Self Quiz
Ask yourself...
- Which terms are included in AUD?
- What are the differences between positive-effect regulation and negative-effect regulation theories?
- How does the body’s metabolism process of alcohol work?
- How do pregnancy, fasting, and medications impact the metabolism of alcohol?
Risk Factors
Several factors are believed to contribute to the development of alcohol use disorder, including the home environment, peer interactions, genetic disposition, cognitive functioning, and other mental health disorders, such as schizophrenia, depression, and personality disorders (9).
Risk factors for AUD include (3, 7, 9):
- Genetics and family history. Hereditary factors can influence AUD by as much as 60%. Parents’ drinking habits are directly correlated to the child’s development of AUD. Certain genes have been found to increase an individual’s susceptibility to AUD, including:
- GABRG2 and GABRA2, COMT Val 158Met, DRD2 Taq1A, and KIAA0040.
- Drinking at an early age. Those individuals, especially females, who begin consuming alcohol before age 15 are three times more likely to have AUD. Research indicates that younger people who wait to start consuming alcohol until age 21 are less likely to have AUD.
- Mental health disorders. Psychiatric conditions, such as depression, post-traumatic stress disorder (PTSD), and attention deficit hyperactivity disorder (ADHD) are linked to an increased risk of AUD. Childhood trauma is also strongly correlated with AUD. The presence of both AUDs and psychiatric disorders leads to a worsened prognosis for both disorders.
- Social issues. Poverty and lack of education are significant risk factors for AUD.
Additionally, the risk for developing AUD can depend on how much, how often, and how quickly the individual consumes alcohol. Binge drinking and heavy drinking over time can lead to AUD (7).

Self Quiz
Ask yourself...
- Which mental health disorders can contribute to AUD?
- Which types of drinking can lead to AUD over time?
- Which genes have been found to increase an individual’s susceptibility to AUD?
- Which social factors are significant risk factors for AUD?
Signs and Symptoms
Nurses need to perform a thorough assessment of those individuals suspected of having AUD. The Cut Down, Annoyed, Guilty, and Eye-opener (CAGE) questionnaire is the widely accepted gold-standard assessment tool and is comprised of these questions (2):
1. Have you ever felt that you need to cut down on your drinking?
2. Have people annoyed you by criticizing your drinking?
3. Have you ever felt bad or guilty about your drinking?
4. Have you ever had a drink first thing in the morning to steady your nerves or to get rid of a hangover (eye-opener)?
The scoring for the CAGE includes 0 for “no” answers and 1 for “yes” answers with a total score of two or greater being clinically significant for AUD. However, healthcare providers are encouraged to regard a total score of one or greater as the potential for substance abuse disorder that requires further patient exploration (2).
The Alcohol Use Disorders Identification Test (AUDIT) is a 10-item screening tool created by the World Health Organization (WHO) to assess alcohol-related conditions. There is a patient test that individuals may administer to themselves, and a test designed for healthcare providers to administer to patients. Both tests ask the same questions and use a similar scoring method. The provided answers are 0 for “never”, 1 for “monthly or less”, 2 for “2-4 times a month”, 3 for “2-3 times a week”, and 4 for “4 or more times a week”. A score of 8 or more indicates harmful alcohol use (8, 12).
The AUDIT questions are (8, 12):
- How often do you have a drink containing alcohol?
- How many drinks containing alcohol do you have on a typical day when you are drinking? (The answer options for this question are 0 for “1 or 2”, 1 for “3 or 4”, 2 for “5 or 6”, 3 for “7 to 9”, and 4 for “10 or more”.)
- How often do you have six or more drinks on one occasion?
- How often during the last year have you found that you were not able to stop drinking once you had started?
- How often during the last year have you failed to do what was normally expected to you because of drinking?
- How often during the last year have you needed a first drink in the morning to get yourself going after a heavy drinking session?
- How often during the last year have you had a feeling of guilt or remorse after drinking?
- How often during the last year have you been unable to remember what happened the night before because of your drinking?
- Have you or someone else been injured because of your drinking? (The answer options for this question are “no”, “yes, but not in the last year”, and “yes, during the last year”.)
- Has a relative, friend, doctor, or other healthcare worker been concerned about your drinking or suggested that you cut down? (The answer options for this question are “no”, “yes, but not in the last year”, and “yes, during the last year”.)
Nurses and other healthcare professionals can ask patients the additional questions below about their alcohol use to determine the risk and presence of AUD.
In the past year, have you (7):
- Ended up drinking more or longer than you intended?
- Tried to cut back on drinking, but have been unable to do so?
- Experienced symptoms of illness (hangover) related to your drinking?
- Craved a drink so much that it distracted you from your current activity?
- Found that your drinking has interfered with maintaining your responsibilities and obligations regarding home, family, work, or education?
- Continued to drink despite knowing that it caused problems with family and friends?
- Foregone pleasurable activities (hobbies, etc.) that you enjoy to drink?
- Increased your risk for injury (driving, swimming, using machinery, walking in a dangerous area, engaging in unsafe sexual behavior) due to drinking?
- Continued to drink despite the social, health, or economic problems it causes?
- Experienced feelings of anxiety, depression, or memory blackout due to your drinking?
- Needed to drink more alcohol than in the past to get the same effects?
- Experienced alcohol withdrawal symptoms, such as tremors, restlessness, irritability, nausea and vomiting, sweating, malaise, racing heartbeat, hallucinations, or seizures?
The patient’s positive response to two to three of these criteria indicates mild symptoms, four to five indicates moderate symptoms, and six or more indicates severe symptoms (7).
Patients with AUD often report frequent falls, blackout spells, motor instability and tremors, visual disturbances, hangover symptoms (headache, nausea and vomiting, dry mouth, photophobia), hypertension, heart palpitations, seizures, confusion, mood swings, and sleep disturbances. Social symptoms include school or job instability or loss, relationship separation or divorce, estrangement from family and friends, and homelessness (9). Nurses should also assess patients suspected of AUD for post-traumatic stress disorder, bipolar disorder, panic disorder, anxiety disorder, dysthymic disorder, major depressive disorder, and insomnia (9).
During the assessment of a patient with AUD, nurses may note ataxia, fine motor skill disturbances, mental status changes, mood changes, slurred speech, tachycardia, hypotension, nystagmus, asterixis, ruddy palms, jaundiced coloring, and ascites. Signs of liver disease include hepatomegaly, splenomegaly, cirrhosis, spider angiomata, and liver atrophy (9).

Self Quiz
Ask yourself...
- What are the four CAGE alcohol use screening questions?
- When using the AUDIT screening tool, which score indicates harmful alcohol use?
- Which social symptoms are individuals with AUD likely to experience?
- Which physical symptoms may the nurse observe in patients with AUD?

Prevention
The stage in life when a person is exposed to alcohol is an important predictor for alcohol misuse. Adolescence is a time when many people begin experimenting with drinking, and research indicates that drinking before the brain is fully formed (age 26) can negatively impact brain development and compromise cognitive function. The main goal of preventing AUD is to impede, or at least delay, the onset of drinking in the youth population (6).
Adolescents and young adults seek independence and favor transitioning to adult roles. Most of this population drives automobiles and spends more time with friends than family members, thus making them easily influenced by their peer group. This also means that this population is at high risk for alcohol-related injuries, with 5,000 18- to 24-year-olds dying each year due to alcohol-related incidents (6). This group engages in binge drinking, which can lead to blackouts, alcohol poisoning, sexual assault, sexually transmitted infections, and poor academic performance.
Other factors that influence drinking behaviors that should be considered in prevention interventions are genetics, health status, cultural background, educational background, socioeconomic status, community attitudes toward alcohol use, and exposure to social media. Preventative measures should also be geared toward pregnant women and older adults since these populations have special considerations, such as the risk for fetal alcohol spectrum disorders in pregnant women and the inability to effectively metabolize alcohol in older adults that can lead to injuries (6).
Regular screenings for alcohol misuse are a key prevention strategy, and research shows that most patients do not object to being screened for alcohol use and thus are open to receiving advice about alcohol use (6). Evidence also shows that alcohol-related incidents can be prevented by both individual and environmental interventions. For example, college students who are taught to monitor their drinking and how to effectively refuse alcohol when offered can prevent AUD. College communities that restrict happy hours, enforce the minimum drinking age, and prevent alcohol price promotions can decrease the risk of AUD (6).

Self Quiz
Ask yourself...
- Which factors are predictors of alcohol misuse?
- Which factors put adolescents and young adults at risk for alcohol-related injuries?
- How do most patients react to screenings and advice regarding alcohol use?
- Which measures can college students and college communities implement to prevent AUD?
Diagnostics and Treatment
The preliminary source used to diagnose alcohol use disorder is the Diagnostic and Statistical Manual of Mental Disorders (DSM).
According to the DSM, the criteria for alcohol use disorder include (11):
A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by two or more of the following, occurring at any time in the same 12-month period:
- Alcohol is often taken in larger amounts or over a longer period than was intended.
- There is a persistent desire or unsuccessful efforts to cut down or control alcohol use.
- A great deal of time is spent in activities necessary to obtain alcohol, use alcohol, or recover from its effects.
- Craving, or a strong desire or urge to use alcohol.
- Recurrent alcohol use failing to fulfill major role obligations at work, school, or home.
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol.
- Important social, occupational, or recreational activities are given up or reduced because of alcohol use.
- Recurrent alcohol use in situations in which it is physically hazardous.
- Alcohol use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by alcohol.
- Tolerance, as defined by either of the following:
- A need for markedly increased amounts of alcohol to achieve intoxication or desired effect.
- A markedly diminished effect with continued use of the same amount of alcohol.
- Withdrawal, as manifested by either of the following:
- The characteristic withdrawal syndrome of alcohol
- Alcohol (or a closely related substance, such as a benzodiazepine) is taken to relieve or avoid withdrawal symptoms.
Laboratory testing in patients with AUD can indicate blood disorders; vitamin, mineral, and electrolyte imbalances; cancers; cardiovascular disease; liver disease; and pancreatitis. Alcohol-related organ damage can be determined by biomarkers, such as aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transpeptidase (GGT), phosphatidylethanol (PEth), fatty acid ethyl ester (FAEE), total serum sialic acid (TSA), mean corpuscular volume (MCV), cholesteryl ester transfer protein (CETP), carbohydrate-deficient transferrin (CDT), N-Acetyl-β-Hexosaminidase (Beta-Hex), macrophage migration inhibitory factor (MIF), and D-dopachrome tautomerase (DDT). Biomarkers like alcohol and ethyl glucuronide levels can determine recent alcohol consumption. CDT and PEth levels can help monitor abstinence (1, 9).
Treatment approaches for AUD involve pharmacological and nonpharmacological interventions.
The Federal Drug Administration (FDA) has approved three pharmacological treatments for AUD (9, 10):
- Naltrexone (Vivitrol) is a mu-opioid antagonist that blocks the effects of opioids and is widely used in treating addiction to narcotics. In alcoholism, the medication blocks the effects of naturally occurring opioids, such as endorphins. Therefore, the drinker does not experience any psychological benefits or “high” from the alcohol. Naltrexone also reduces the craving for alcohol leading to improved abstention rates, reduced number of drinking days, and reduced risk of relapse. The potential side effects—nausea, headaches, and fatigue—also work as an alcohol deterrent.
- Acamprosate is a glutamate agonist that promotes a balance of inhibitory and excitatory neurotransmitters in the brain that are disrupted by alcohol abuse. The discontinued brand name is Campral, but the generic equivalent is still available. The medication can cause weight gain and severe depression.
- Disulfiram (Antabuse) is an alcohol antagonist drug that inhibits ALDH, resulting in the accumulation of acetaldehyde in the body. The purpose of disulfiram is to promote fear in the drinker because drinking alcohol in conjunction with taking the medication can result in serious adverse reactions, including flushing, headache, dyspnea, diaphoresis, dizziness, shock, and even death.
- Gabapentin (Neurontin) and topiramate (Topamax) are not yet FDA-approved for AUD, but they are currently being used to treat the disease. Gabapentin, an anticonvulsant used to treat neuropathic pain, corrects dysregulation caused by alcohol use and cessation; it also decreases alcohol cravings. Topiramate, also an anticonvulsant, decreases alcohol cravings.
The most effective non-pharmacological approach to AUD is psychological therapy, including (9):
- Motivational interviewing. This technique is most effective in those patients who are ambivalent about changing their behaviors and quitting alcohol. The approach is client-centered and helps patients recognize and address their issues. It helps them become motivated to make long-lasting, healthy changes.
- Motivational enhancement therapy (MET). MET is a manual-based intervention that includes motivational interviewing and focuses on strengthening the motivation of the patient to change their alcohol use behaviors.
- Cognitive behavioral therapy (CBT). CBT helps individuals explore the connections among their thoughts, emotions, and behaviors. This therapy can increase motivation to stop drinking, identify triggers that prompt alcohol use, and teach effective coping mechanisms to deal with alcohol cravings and alcohol-seeking behaviors. In one study, 58% of patients receiving cognitive-behavioral treatment fared better than those who did not receive this therapy (3).
Other programs that support patients with AUD are residential facilities (in-patient rehabilitation), community programs like Alcoholics Anonymous (AA) or other 12-step programs, and faith-based programs that align with the principles of certain religions.


Self Quiz
Ask yourself...
- How does the DSM define tolerance?
- Which biomarkers can indicate AUD?
- Which three medications has the FDA approved for AUD treatment?
- What are the differences among motivational interviewing, motivational enhancement therapy, and cognitive behavioral therapy?
Complications and Long-Term Effects
AUD impacts each body system and can cause complications that have long-term negative effects. For example, alcohol impairs the brain’s ability to regulate balance, memory, speech, and judgment, which can lead to injuries. With long-term, heavy drinking the neurons reduce in size, the brain’s mass shrinks, and the brain’s inner cavity grows larger.
Alcohol interferes with glutamate action, which inhibits the creation of new memories and leads to blackouts. Alcohol also influences the neurotransmitters dopamine and serotonin, which can cause mood dysregulation, impaired concentration, and decreased motivation. Even though alcohol can cause euphoria at first, it is a depressant that can lead to suicidal ideation, behaviors, and death.
Additionally, excessive alcohol consumption can weaken the immune system, which can lead to increased rates of infection, such as pneumonia (4).
Additional complications of AUD by the organ system are (4, 5, 7):
- Cardiac/Circulatory: Cardiomyopathy, arrythmias, stroke, hypertension, ischemic heart disease, heart failure
- Endocrine: Acute and chronic pancreatitis, pancreatic cancer, diabetes
- Gastrointestinal: Esophageal cancer, oral cavity cancer, larynx cancer, pharynx cancer, gut leakiness, gastritis, ulcers, microbial dysbiosis, colorectal cancer, inflammatory bowel disease (IBD)
- Hepatic: Steatosis, steatohepatitis, fibrosis, cirrhosis, alcohol-associated hepatitis, liver cancer
- Immune/Lymphatic: Infections, such as tuberculosis
- Integumentary: Melanoma
- Neurologic: Ischemic stroke, amyotrophic lateral sclerosis (ALS), Alzheimer’s disease, multiple sclerosis (MS)
- Reproductive: Breast cancer, sexually transmitted infections
- Respiratory: Acute respiratory distress syndrome, alcohol-associated lung disease, pneumonia
- Skeletal: Muscle myopathy, muscle wasting, impaired bone fracture repair, reduced bone density (osteopenia, osteoporosis)
- Urinary: Kidney disease, prostate cancer
Alcohol is a toxic substance that contains carcinogens, such as nitrosamines, asbestos fibers, phenols, and hydrocarbons, which are the cause of 3.5% of cancer deaths in the United States (4).
Some cancers associated with alcohol consumption are (4):
- Head and neck cancer. Drinkers are at increased risk for oral cavity, pharynx, and larynx cancers. The risk increases among those individuals who both drink and use tobacco.
- Esophageal cancer. Esophageal squamous cell carcinoma risk is high in moderate to heavy drinkers.
- Liver cancer. The risk for hepatocellular carcinoma and intrahepatic cholangiocarcinoma doubles in individuals who are heavy drinkers.
- Breast cancer. Light drinkers have a slightly increased risk of breast cancer, whereas moderate to heavy drinkers increase their risk substantially. Tobacco use in conjunction with alcohol use increases the risk of breast cancer.
There are multiple ways in which alcohol can increase the risk of cancer, such as (4):
- Metabolism of ethanol to acetaldehyde, which is a toxic carcinogen, acetaldehyde damages DNA and proteins.
- Oxidation can damage DNA, proteins, and lipids.
- Inability to digest and assimilate vital nutrients that can protect against cancers, such as vitamin A, vitamin B complex, vitamin C, vitamin D, vitamin E, and carotenoids.
- Increasing levels of estrogen can lead to breast cancer.
The prognosis for patients with AUD is very challenging with less than 20% to 30% achieving long-term abstinence and with most acquiring serious to permanent health conditions that are irreversible (9).

Self Quiz
Ask yourself...
- How does alcohol negatively impact the brain?
- How does alcohol affect the gastrointestinal and integumentary systems?
- Why does oxidation increase the risk of cancer?
- What is the prognosis of patients with AUD?
Patient Education
Nurses play a critical role in educating patients with AUD, and they should do so in a non-judgmental and non-confrontational manner.
Educational topics nurses should address with patients include (9, 10):
- Healthy diet. Most patients with AUD suffer from malnourishment, particularly regarding folate. Foods rich in folate include legumes, eggs, leafy greens, citrus fruits, nuts and seeds, and fortified grains. Patients should be taught the importance of maintaining a healthy diet that is rich in protein, complex carbohydrates, fresh fruits and vegetables, healthy fats, and vitamins and minerals.
- Reducing risky behaviors. Individuals with AUD should be taught that alcohol consumption lowers inhibitions, which can lead to risk-taking behaviors, such as driving, swimming, operating heavy machinery, and engaging in unprotected sexual practices.
- Importance of support groups. Patients with AUD are more likely to make progress and stay motivated if they are supported by family, friends, and community resources like Alcoholics Anonymous (AA). Family members should also be encouraged to attend support groups like Al-Anon.
- Maintaining a temptation-free environment. Patients should be encouraged to remove all alcohol from their homes and offices. When traveling, they can request that hotels remove alcohol from the guest room minibar.
- Importance of maintaining health screenings. AUD can lead to other serious health conditions, such as cardiovascular disease, osteoporosis, and various cancers. Patients should be taught the importance of receiving regular medical check-ups and health screenings to maintain optimal health.
Nurses should also ensure that patients can access educational and support resources in their native language, as well as be provided with information about resources available to low-income individuals, if applicable.

Self Quiz
Ask yourself...
- Which foods high in folate should the nurse recommend for patients with AUD?
- Why do individuals with AUD engage in risky behaviors?
- Which serious health conditions are patients with AUD at risk of acquiring?
- How can alcoholics maintain a temptation-free environment at home and when traveling?
Resources
There are many resources available to assist patients with AUD.
- Alcoholics Anonymous: AA is a global fellowship community that helps individuals resolve their issues with alcohol. https://www.aa.org/
- Al-Anon Family Groups: Like AA, Al-Anon is a fellowship community that helps friends and family members of alcoholics gain the support they need. https://al-anon.org/
- Alateen: Alateen is a component of Al-Anon, a fellowship group for adolescents who have been affected by someone else’s drinking. https://al-anon.org/newcomers/teen-corner-alateen/
- Centers for Disease Control and Prevention: The CDC provides resources, such as publications, online tools, and healthcare information related to individual states. https://www.cdc.gov/alcohol/resource-center/index.html
- FindTreatment.gov: This is a national website for locating treatment facilities for mental and substance use disorders. https://findtreatment.gov/locator
- National Association for Children of Addiction (NACoA): This organization provides programs, such as The Clergy Education and Training Project, Celebrating Families, and Children’s Program Kit to support the children of addicted parents. https://nacoa.org/
- Rethinking Drinking: The National Institute on Alcohol Abuse and Alcoholism (NIAAA) website provides evidence-based information for patients and healthcare providers, as well as listings for treatment centers. https://www.rethinkingdrinking.niaaa.nih.gov/

Self Quiz
Ask yourself...
- Which organization assists friends and family members of individuals with AUD?
- Which organization supports teenagers who are affected by someone else’s drinking?
- Which programs by NACoA support the children of addicted parents?
- Which websites provide listings for treatment centers?
Case Study
B.P. is a 32-year-old Caucasian man who presents to the emergency department after a motor vehicle accident during which B.P. lost control of his car and drove it into a roadside ditch. There were no other cars on the road at the time, making the accident a one-person collision. B.P. was brought to the hospital by his girlfriend and presented with superficial lacerations and bruising to his face from deployment of the driver’s side airbag and more serious lacerations to his left forearm that were injured by the breaking glass of the driver’s side window. He states that he thinks he may have hit his head on the automobile’s steering wheel before airbag deployment, but then says, “I’m not completely sure about that little detail.”
B.P.’s vital signs are blood pressure 158/84 mmHg, pulse 78 beats per minute, respirations 16 breaths per minute, and oxygen saturation 95%. His lung fields are clear to auscultation bilaterally, and his cardiovascular exam reveals a regular rate and rhythm without murmurs. Bowel sounds are confirmed in four quadrants via auscultation. Radial, pedal, and dorsal pedal pulses are normal bilaterally. Pupils are sluggish to react to penlight; the patient’s eyes have a glassy appearance. B.P. is oriented to place, but not day or time.
He can state his name and birthdate without hesitation, but he pauses before stating his complete address and incorrectly states his zip code. When speaking, B.P.’s words are slurred, but his hearing bilaterally is intact. During the musculoskeletal and neurological assessments, B.P. is unable to follow all the instructions the nurse provides and at one point he whines, “Can we stop now? This is super hard and I’m so sleepy. I need to go to bed now.” The patient’s left forearm is red and edematous with two lacerations that are both roughly 1.5 inches in length.
There are evident shards of glass present in both lacerations and bleeding has slowed significantly since the patient arrived at the hospital. B.P.’s face has several minor red contusions and a couple of superficial lacerations. The patient denies any reports of pain, headache, nausea, or dizziness, and says that he only feels fatigued.
B.P.’s health history includes chronic hay fever for which he takes over-the-counter antihistamines. He denies any further health issues. The nurse is unable to obtain a detailed social history or family history due to B.P.’s noncompliance.
After B.P.’s face and left arm are cleaned, and the left arm sutured and bandaged, he is taken for a chest x-ray, which is normal, and a computerized tomography (CT) scan of the head, which shows no intracranial hemorrhage, mass, or stroke. Blood test results reveal folate deficiency, and ALT, AST, MCV, GGT, and CETP levels consistent with heavy alcohol use. Intravenous folate and normal saline are administered during the next several hours, and the patient is consistently monitored for pain and alcohol withdrawal symptoms. As B.P. becomes sober, the nurse initiates the AUDIT questionnaire; B.P. scores a 32.
When the nurse explains B.P.’s AUDIT score to him, he states, “Yeah, I’m not surprised. I’ve been drinking since I was 13, and my girlfriend keeps telling me that my drinking is getting worse. I just like to have a few to chill after a hard day at work; my job is super stressful. Maybe she’s right. And after tonight, I should probably look into it. These hospital and car bills aren’t going to be cheap.”
B.P. is discharged with a referral to a psychiatrist for further AUD evaluation and potential treatment. He is also given a couple of brochures about alcohol abuse and in-patient rehabilitation programs. B.P. is encouraged to follow up with his primary care physician for continued care of his injured arm.

Self Quiz
Ask yourself...
- Which social factors about B.P.’s situation put him at risk for AUD?
- Which assessment findings indicate B.P. may have AUD?
- Is B.P.’s AUDIT score concerning? If so, why?
- Which factors indicate it was effective for the nurse to wait to administer the AUDIT to B.P.?
Conclusion
AUD puts individuals at risk for serious health complications, legal problems, and impaired interpersonal relationships. Many alcoholics do not receive appropriate medical care for AUD due to a lack of screening by healthcare providers. Therefore, nurses must use their assessment skills to evaluate patients for AUD and provide them with proper education about the disease, including its long-term effects and complications.
Healthcare screenings for cardiovascular disease and mental health disorders, as well as referrals to community support programs such as Alcoholics Anonymous, help patients take responsibility for their health and recovery.
Bioethics in Nursing
Introduction
Nursing practice is deeply rooted in ethical principles that guide decision-making and client care. Bioethics is a crucial aspect of healthcare that provides a framework for analyzing ethical dilemmas and promoting individualized client-centered care respectfully and compassionately. Nursing ethics involves applying bioethical principles in practice, such as maintaining client confidentiality and respecting autonomy. Nurses face ethical dilemmas regularly. One of the most common is providing care that conflicts with personal beliefs (6).

Self Quiz
Ask yourself...
- How do you think bioethics influences nursing practice
- What are some examples of ethical dilemmas nurses may face?
- Can you describe a situation where a nurse's personal beliefs conflicted with their professional obligations?
- How would you navigate such a scenario?
Definition and Purpose
Bioethics is the study of ethical and moral principles guiding healthcare decisions and practices (10). Its purpose is to ensure that healthcare providers make informed decisions that respect clients' values, beliefs, and rights (5).
Bioethics provides a framework for analyzing ethical issues in healthcare while considering the interests of the clients, their families, and the healthcare providers involved in their care (5). By understanding the definition and purpose of bioethics, nurses can develop a strong foundation for addressing ethical challenges in practice, such as informed consent, client confidentiality, and when it may infringe upon others’ health and proper resource allocation (5,6,10).


Self Quiz
Ask yourself...
- How does the definition of bioethics impact its application in nursing practice?
- What are some potential consequences of ignoring ethical principles?
- Can you think of a situation where a nurse's understanding of bioethics helped them navigate an ethical dilemma?
- What was the outcome?
Principles of Bioethics
The principles of bioethics include autonomy, beneficence, non-maleficence, and justice (5,6,7,9). Autonomy respects clients' decision-making capacity, beneficence promotes a client's well-being, non-maleficence avoids any harm to the client, and justice ensures fairness and equity for all involved in the client’s care (5,6,9).
These principles serve as the guiding force in nursing practice; influencing the decisions related to client care, research, and policy development (1). Autonomy empowers clients to make informed choices about their care (5,6,9). This may include decisions that the client’s family and even healthcare providers may disagree with personally. Beneficence compels nurses to act in the best interests of their clients and advocate for the client’s desires (5,6,9). Non-maleficence reminds nurses to avoid causing harm; this includes not just physical but emotional and mental harm as well (5,6,9).

Self Quiz
Ask yourself...
- How do the principles of bioethics guide nursing practice?
- What are some examples of how these principles are applied in different healthcare settings?
- Can you describe a situation where a nurse had to balance the principles of autonomy and beneficence in their practice?
- How did they navigate this ethical dilemma?
Types of Ethics and Professions
Different professions have specific ethical guidelines, such as the American Nurses Association (ANA) Code of Ethics for nurses (1). Understanding the ethical framework of various professions is essential to the interdisciplinary healthcare approach.
Interdisciplinary collaboration requires an understanding of diverse ethical perspectives and principles, an approach that coincides with an equally diverse client population. Nurses should be aware of the ethical guidelines that govern their practice and be able to apply them in diverse healthcare settings. They must also be aware of their own beliefs and guidelines and how these may affect their decision-making, adversely affecting client care (5,6).

Self Quiz
Ask yourself...
- How do different professional ethical guidelines impact interdisciplinary collaboration?
- What are some potential consequences of ignoring these guidelines?
- Can you describe a situation where a nurse had to navigate an ethical dilemma with an interdisciplinary team?
Ethics in Nursing
Nursing ethics involves applying principles in practice that benefit the client, healthcare providers, and loved ones of the client. Examples include things such as maintaining client confidentiality and respecting autonomy, helping the client make the right decision for themselves, and advocating for those decisions to others (1,5). One of the most difficult decisions nurses face involves those that conflict with their personal belief system (6).
Nurses must be equipped with the knowledge and skills to navigate these ethical challenges and provide care that respects clients' values and beliefs while also nurturing their thoughts and feelings (6). By exploring bioethics in nursing, we can promote a culture of ethical practice that is compassionate and client-centered.
Henrietta Lacks Story
Henrietta Lacks was a Black tobacco farmer who had her cancer cells taken without her knowledge or consent which led to numerous scientific breakthroughs, including the development of the polio vaccine (7,8). Her story raises important questions about medical ethics, racism, and the intersection of science and human compassion.
In 1951, Henrietta Lacks was diagnosed with cervical cancer and began treatment at Johns Hopkins Hospital in Baltimore. During her treatment, a sample collection of her cancer cells was taken by her doctor, Dr. George Gey without her knowledge and or consent (7,8). Dr. Gey discovered that Henrietta's cells were extraordinary in nature and could be of great value for cancer research and future developments as they could survive and thrive in a laboratory setting thus making them ideal for scientific research.
Henrietta's cells, known as HeLa cells, were soon being used in laboratories worldwide, leading to numerous scientific breakthroughs, including the polio vaccine development, in vitro fertilization, and gene mapping (7,8). However, Henrietta's family was never informed or financially compensated for the use of her cells, and her story remained largely unknown until the publication of Rebecca Skloot's book "The Immortal Life of Henrietta Lacks" in 2010 (2).
Henrietta's story highlights the unethical practices that were common in the medical field at the time, particularly in relation to clients that lacked resources, particularly those belonging to minority groups (2). Her cells were taken without her consent, and she was never compensated or acknowledged for her contribution to science. This raised some very important questions about medical ethics, informed consent, and the exploitation of vulnerable populations.
Still, Henrietta's story is a powerful reminder of the intersection of science and the need for personal autonomy. Her cells have been used to advance scientific knowledge, but they also represent a person, a family, and a community. The use of her cells without her consent or compensation is a violation of her humanity and a reminder of the need for ethical considerations in scientific research.

Self Quiz
Ask yourself...
- How do nursing ethics impact patient care?
- What are some potential consequences of ignoring ethical principles in practice?
- Can you describe a situation where a nurse's understanding of ethics helped them provide high-quality care
- What were the benefits for the patient?
Tuskegee Syphilis Experiments
The Tuskegee Syphilis Study was a highly controversial and unethical medical experiment conducted on African American men in Macon County, Alabama between 1932 and 1972 (4,11). The study, led by the Department of U.S. Public Health Services, involved withholding treatment from hundreds of African American men infected with syphilis despite the availability of effective therapies, to study the natural progression of the disease (4,11).
The men, who were mostly illiterate and poor, were not informed that they had syphilis, their partners were not informed of the disease, nor were they given treatment for the disease (4,11). Instead, they were given placebos and misleading information about their condition. The study continued for 40 years, during which time many of the men died from syphilis-related complications, and many others suffered serious health problems which included the spreading of syphilis to unsuspecting sexual partners.
The Tuskegee Syphilis Study is widely regarded as one of the most unethical medical experiments in history. The study was conducted without the men's knowledge or consent, and it violated basic human rights and principles of medical ethics. By way of public outcry and shock, the awareness of these experiments led to major changes in the way human subjects are protected in medical research and a desire for closer oversight by governing groups.
In 1974, a class-action lawsuit was filed on behalf of the men who were involved in the study, resulting in a multimillion-dollar settlement (11). The study also led to the establishment of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, which developed guidelines for the ethical conduct of research involving human subjects (11).
The Tuskegee Syphilis Study has had a lasting impact on the field of medicine and beyond. It highlighted the importance of informed consent and the need for ethical oversight in the field of medical research. It has also led to the increased scrutiny of medical experiments and a greater emphasis on protecting human subjects, their privacy, and most importantly honest care and explanations of medical conditions and treatments.
Today, the Tuskegee Syphilis Study is remembered as a cautionary tale about the dangers of unethical medical research. It serves as a reminder of the importance of prioritizing the well-being and safety of people and the need for ongoing vigilance in ensuring that medical research is conducted ethically and responsibly, and ensuring there are the proper checks and balances in place to provide the oversight needed.
The study also highlighted the need for diversity in medical research and the importance of including diverse populations in clinical trials (11). It led to increased efforts to address health disparities and to ensure that medical research is conducted in a way that is fair and equitable to all.
In addition, the Tuskegee Syphilis Study led to changes in the way that medical research is regulated and overseen (11). It led to the establishment of institutional review boards (IRBs) and independent ethics committees (IECs) which are responsible for reviewing and approving research protocols and ensuring they meet the ethical standards set in place (11).
Transparency and accountability in medical research have also been placed at the forefront of research since these events took place. Highlighting the importance of disclosing potential conflicts of interest and ensuring research is conducted in a way that is transparent and open to scrutiny; there inevitably was major change and growth that came from this huge medical injustice.
The Tuskegee Syphilis Study was a highly unethical and controversial medical experiment that had a profound impact on the field of medicine and beyond. It highlighted the importance of informed consent, ethical oversight, and diversity in medical research, and led to major changes in the way medical research is conducted and regulated. In these ways, it acted as a catalyst of growth and change in the way the U.S. views and treats research participants. It serves as a reminder of the need for ongoing vigilance in ensuring medical research is conducted ethically and responsibly.
The Tuskegee Syphilis Studies and Henrietta Lacks' cases highlight the importance of informed consent in research.
Other examples include: (5,9)
- Abortion and reproductive rights
- Euthanasia and end-of-life care
- Gene editing and genetic research
- Healthcare access and disparities


Self Quiz
Ask yourself...
- How do bioethical issues like informed consent impact healthcare outcomes
- What are some potential consequences of ignoring these issues?
- Can you describe a situation where a bioethical issue like euthanasia sparked a debate?
- How did healthcare professionals navigate this ethical dilemma?
Research in Ethics
Research ethics involves applying bioethical principles in research (3). Obtaining informed consent and ensuring participant confidentiality are two ways in which the provider can best provide ethical care to those that entrust the healthcare system with their voluntary well-being.
Researchers must be aware of ethical principles that guide research and ensure their studies are conducted ethically and responsibly which puts the client first (3).
Ethical Decision-Making
Ethical decision-making involves critical thinking, moral principles, and professional standards. Nurses can use ethical frameworks, such as the MORAL model and Nursing Process model, to guide decision-making (5). Ethical decision-making is a crucial aspect of nursing practice as it enables nurses to navigate complex healthcare issues and promote clients' well-being.

Self Quiz
Ask yourself...
- How do ethical principles guide research?
- What are some potential consequences of ignoring these principles?
- Can you describe a situation where a researcher had to navigate an ethical dilemma in their study?
Conclusion
Bioethics plays a vital role in nursing practice, ensuring that clients receive respectful and compassionate care. Understanding bioethical principles and applications is essential for nurses to provide high-quality care. By applying ethical principles and frameworks, nurses can navigate complex healthcare issues and promote clients' well-being.

Self Quiz
Ask yourself...
- How does the ethical framework guide decision-making in nursing practice and what are some potential consequences of ignoring these frameworks?
- How do personal values and beliefs impact nursing practice what are the implications for patient care?
- How does the principle of autonomy impact informed consent in healthcare?
- What are some potential consequences of prioritizing beneficence over non-maleficence in healthcare, and how can nurses balance these principles?
- How does the concept of justice impact healthcare resource allocation and what are the implications for nurses and patients?
- How do nurses balance the need for patient confidentiality with the need for transparency?
- What are some potential consequences of ignoring the principle of non-maleficence in healthcare, and how can nurses prioritize patient safety?
- How does the principle of autonomy impact patient decision-making?
- How do nurses balance the need for patient education with the need for autonomy?
- Are there any potential consequences for prioritizing patient satisfaction over patient well-being?
- How does the concept of vulnerability impact healthcare ethics?
- How do nurses balance the need for patient advocacy with the need for patient autonomy?
- What are some potential consequences of ignoring the principle of justice in healthcare?
- How does the principle of beneficence impact healthcare resource allocation?
- How do nurses balance the need for patient education with the need for patient confidentiality?
- What are some potential consequences of prioritizing patient well-being over patient autonomy?
- Could the Henrietta Lacks case and the Tuskegee Syphilis cases have an affect the way minorities view medical treatment in the U.S?
Medical Interpreter Use in Healthcare
Introduction
The presence of a medical interpreter can make a significant difference in the care of a patient with limited knowledge of the English language. Their presence is essential for numerous reasons. Along with addressing language barriers and improving communication, they assist in bridging cultural gaps. With the number of those in need of these services increasing, their presence is more important than ever.
Definition
The role of the medical interpreter is a very specialized one. It requires a very distinct set of skills, which includes the ability to speak fluently in several languages and to have an extensive understanding of medical terminology (1). They aim to help non-English speaking people communicate with their healthcare providers and other medical professionals.
The National Council on Interpreting in Health Care (NCIHC) defines a qualified interpreter. "An individual who has been assessed for professional skills demonstrates a high level of proficiency in at least two languages and has the appropriate training and experience to interpret with skill and accuracy while adhering to the National Code of Ethics and Standards of Practice published by the National Council on Interpreting in Health Care" (2).
The terms healthcare interpreter and medical interpreter may be used interchangeably, as they both handle communication in the medical setting (9).

Self Quiz
Ask yourself...
- Can you identify the skills a medical interpreter needs?
- Are you able to define the role of the medical interpreter?
Medical Interpreters
Medical interpreters play a vital role in bridging gaps in healthcare. They promote effective communication between healthcare providers and the individuals who speak different languages, in their care. Most importantly, they address and eliminate language barriers that could result in serious medical errors.
It is common knowledge that language barriers present significant challenges for healthcare providers and medical professionals. Miscommunication between them and their patients can reduce provider and patient satisfaction, decrease the quality of care, and impact patient safety (3).
Medical interpreters promote effective communication by giving the patient a voice. They ensure patients receive the care they are entitled to and assist in avoiding medical errors that could harm the patient. They are essential in advocating for patients experiencing communication barriers (4).
The Importance of Medical Interpreters
As the role of a medical interpreter is to facilitate communication, they are needed in a variety of different situations, which could include (5).
- When a patient needs to provide consent.
- When a healthcare provider is gathering medical history.
- During physical exams.
- When a patient is describing pain or other symptoms.
- When the patient has questions or concerns.
- For treatment discussions and decisions.
- To understand discharge instructions.
These situations can occur in different sites that provide care to patients with language barriers and involve various settings such as (6):
- Hospitals
- Clinics
- Private medical offices
- Rehabilitation centers
- Nursing homes
- Long-term care facilities
- Assisted living facilities
- Mental health facilities
- Forensic services
- Substance abuse clinics
- Domestic violence centers or programs

Differences between the Medical Interpreter and the Medical Translator
It is essential to differentiate between a medical interpreter and a medical translator. While some may use these terms interchangeably, there are significant differences. While a medical interpreter assists in communication between people, a medical translator focuses on written text and content (1).
The interpreter will use spoken words, while the translator will use written words. Therefore, the significant difference is in the way they communicate. Medical interpreters are needed to explain and clarify important events related to healthcare.
Some examples include (1):
- Medical procedures
- Surgical procedures
- Aftercare instructions
- Discharge planning
- Doctor’s explanations and recommendations
Medical translators play an important role in translating written content from one language to another in (1):
- Medical records
- Patient charts
- Patient history
- Family history
- Health issues

Self Quiz
Ask yourself...
- Can you list five situations in which a medical interpreter would be required?
- Explain the role the medical interpreter plays in healthcare.
- What are some settings where a medical interpreter would be employed?
- Identify the differences between a medical interpreter and a medical translator.
Qualifications and Training
The role of the medical interpreter is a very specialized one. They are a crucial healthcare team member, and their services are vital to those they are working with. Therefore, they must possess specific skills, qualifications, training, and credentials.
To start becoming a medical interpreter, the following prerequisites must be met (6):
- Must be 18 years of age.
- General education: Must have proof of a United States high school diploma/GED or equivalent from another country.
- Oral proficiency in the English language.
- Oral proficiency in the target language.
- Medical Interpreter education.
Medical Interpreter education includes training obtained at a college or university and must be at least three credit hours. It may also be obtained through a training course which consists of at least 40 hours (6).

Self Quiz
Ask yourself...
- Can you name the prerequisites needed to begin the process of becoming a medical interpreter?
Certification
The next step is to become a certified medical interpreter. If the above requirements have been met, then certification can be pursued. The benefits of becoming a certified medical interpreter include being on the national registry and the respect that accompanies certification.
In addition, certification identifies the recipient as a competent professional, who understands and follows the standards of practice (9). Certification is becoming important as more employers prefer certified medical interpreters (9).
Two organizations provide professional certification for medical interpreters.
- Certification Commission for Healthcare Interpreters (CCHI) (7).
- National Board of Certification for Medical Interpreters (NBCMI) (8).
Certification Commission for Healthcare Interpreters (CCHI)
The CCHI recognized that certification is fundamental to the medical interpreter's career. The mission of this organization is “to develop and administer a comprehensive national certification program for healthcare interpreters, bringing together representatives from interpreting associations, language companies, community-based organizations, educational institutions, hospitals, health and healthcare providers, and advocates for patients with limited English proficiency (10).
This organization offers three types of national certification (7):
- Core Certification Healthcare Interpreter™ (CoreCHI)
This certification is available to interpreters in all languages and tests the core professional knowledge, critical thinking, ethical decision-making, and cultural responsiveness skills needed to perform duties in healthcare settings (11).
- CoreCHI-Performance™ (CoreCHI-P™)
This is considered the second level of certification for interpreters in all languages. The requirements include meeting the CCHIs language proficiency criteria and passing two tests: The knowledge CoreCHI™ exam and the monolingual performance ETOE™ (English-to-English) exam (11).
- Certified Healthcare Interpreter™ (CHI™)
This language-specific performance certification for Spanish, Arabic, and Mandarin interpreters focuses on interpreting skills and abilities (11).
All three certifications are valid for four years from the issue date. The certification must be renewed at that time to ensure that the medical interpreter remains current and updated in their profession (7).
National Board of Certification for Medical Interpreters (NBCMI)
The NBCMI recognizes that medical interpreters are vital care team members in assisting people with limited English proficiency. They help medical interpreters advance their careers by providing the following.
Hub-CMI Credential
This credential applies to medical interpreters of any language and is a national standard to determine mastery of medical terminology and specialties, cultural competencies, and ethical judgment. This credential is a written exam demonstrating a baseline competency and knowledge level in the medical interpreter profession. This credential must be renewed every four years (14).
CMI Certification
This certification is an oral exam and is offered in six languages, including Cantonese, Korean, Mandarin, Russian, Spanish, and Vietnamese. The candidate must have successfully passed the Hub-CMI (8) to take this exam. CMI certification aims to ensure that candidates meet the standards of the medical interpreter’s profession safely and ethically. This certification must be renewed every five years (15).

Self Quiz
Ask yourself...
- Can you describe the benefits of becoming a certified medical interpreter?
- Identify the two organizations that provide professional certification for medical interpreters.
- How would you compare the different certifications offered?
Nationwide Impact
Statistics
It is estimated that over 25 million Americans have limited English proficiency (LEP), putting them at risk for poor health outcomes due to language barriers (20). Some certain groups and populations have a higher risk for LEP. Those who do not speak English in their homes, immigrants, and those with lower educational levels identify as higher risk (21).
LEP creates barriers to accessing healthcare, understanding health information, and preventative health care. Also, LEP has been linked to chronic health conditions.
LEP patients have (21):
- More extended hospital stays (when interpreters were not used at admission and/or discharge).
- Greater risk for surgical infections.
- Greater risk for falls.
- Greater risk for pressure injuries.
- Greater risk for surgical delays.
- Greater risk for readmission for chronic conditions.
The need for medical interpreters is evident. They are essential for communication between providers and patients with LEP.
Demand
Medical interpreters are in high demand in the healthcare system. The employment of interpreters is projected to grow by four percent from 2022 to 2032 (19). While there are approximately 52,000 interpreters and translators in the United States, it is estimated that there will be 7,200 job openings for interpreters and translators each year in the upcoming decade (19).


Self Quiz
Ask yourself...
- Can you explain why those with LEP are at higher risk for poor health outcomes?
- Are you able to identify why there is an increased need for Medical Interpreters?
Standards of Practice
Medical and healthcare interpreting is a distinct and specialized area of work. Standards of practice guide interpreters in their practice and improve the quality and consistency of interpreting (12).
In the past, interpreters lacked guidance for performance requirements, resulting in the quality of interpreting being inconsistent. This inconsistency led to incomplete and inaccurate communication during interpretation. The development of standards resulted from the need for clarity and consistency at a national level in defining the characteristics and competencies of a qualified healthcare interpreter (12).
Professional organizations such as the National Council on Interpreting in Health Care (NCIHC) and the International Medical Interpreters Association (IMIA) establish these standards. Adherence to these standards is vital for maintaining the integrity of medical interpretation services and promoting positive healthcare outcomes for patients with limited English proficiency.
The NCIHC Standards of Practice
The National Council on Interpreting in Health Care (NCIHC) developed the National Code of Standards for Interpreters in Health Care (16). These standards are used as a reference by interpreters, and those who work with and train the interpreters. They also serve as an important guide to the practice of all interpreters (12).
The standards of practice are used for (12).
- Training
- Hiring
- Performance Monitoring
- Discussion on Certification of Professional Competence
The NCIHC Standards of Practice are organized in nine areas consisting of the following (16).
- Accuracy
- Confidentiality
- Impartiality
- Respect
- Cultural Awareness
- Role Boundaries
- Professionalism
- Professional Development
- Advocacy
The International Medical Interpreters Association (IMIA)
The International Medical Interpreters Association (IMIA) has also developed standards that assist in maintaining the integrity of medical interpretation and promoting positive healthcare outcomes for those with limited English (17).
These standards are used for the following reasons (18).
- Guidance in the development of educational and training programs.
- Evaluation tool.
- Assist healthcare providers in working with interpreters.
- Foundation for certificate examination.
The IMIA Standards of Practice are organized in three major areas.
- Interpretation
- Cultural Interface
- Ethical Behavior

Self Quiz
Ask yourself...
- What are the organizations that developed Standards of Practice for medical interpreters?
- What are Standards of Practice used for?
- Consider how a medical interpreter can promote cultural understanding.
Code of Ethics
Ethical behavior is essential in all professions, and medical interpreters must follow professional codes. Ethics are principles and values which govern the conduct of members of a profession. The NCIHC, IMIA, and the CHIA provide a Code of Ethics for medical interpreters.
They are very similar and address the following areas (22):
- Accuracy
- Confidentiality
- Respect
- Professionalism
- Professional Development
- Role Boundaries
- Impartiality
- Cultural Awareness
- Advocacy
- Communication Flow
- Accepting Gifts

Self Quiz
Ask yourself...
- Define the purpose of the Code of Ethics for the medical interpreter.
- List the organizations that provide a Code of Ethics for medical interpreters.
Policies
As a result of the growing number of LEP patients, and the need to provide equal treatment to these individuals, language service policies addressing communication barriers and language gaps have been established. In addition, policies have been developed to mandate the practice of interpreter services (24). By offering access to medical interpreters, healthcare organizations achieve the goals of delivering culturally competent care and maintaining legal and regulatory compliance.
In the United States, it is a right for all individuals to have access to language services, and no one should be denied care or services because of a language barrier (28).
These rights originate from two laws (13):
- The Civil Rights Act of 1964
- Executive Order 13166
The Civil Rights Act of 1964
In 1964, Title VI of the Civil Rights Act was passed. This gave LEP individuals a legal right to language assistance services and prohibited discrimination (27).
Executive Order 13166
In 2000, the Executive Order (EO) 13166, Improving Access to Services for Persons with Limited English Proficiency, was issued (27). This order mandated laws requiring professional interpreters to be present in healthcare facilities receiving federal funding (28).
Both laws ensure that access to language services is a right and that no one can be denied services based on the language they speak (28).
What Nurses Need to Know
Effective communication is essential in healthcare. With over 25 million people having LEP, many nurses may encounter a patient with communication barriers. These language barriers can affect nursing practice and the care provided by nurses. There is abundant evidence indicating that language barriers impact patient outcomes. Nurses can make a difference by responding to the communication needs of patients with LEP by using a medical interpreter (26).
Nurses can improve health outcomes for LEP patients by effectively working with medical interpreters. To achieve this, nurses should know the standards, guidelines, and policies of working with a medical interpreter.
Some guidance for working effectively with medical interpreters includes these evidence-based interventions (25,26):
- Identify patients needing an interpreter in advance.
- Inform the interpreter of the specific language needed.
- Inform the interpreter how much time the interpretation will take.
- Introduce yourself to the interpreter and provide a report on the work needed.
- Provide a brief patient history.
- Greet the patient and introduce the interpreter.
- Explain to the patient the reason for the interpretation.
- Communicate directly to the patient.
- Have the interpreter sit next to or behind the patient.
- Speak in short sentences.
- If the interpreter appears confused, ask them if they need clarification or rephrasing.
- Do not interrupt the interpreter when they are translating.
- When the session is finished, ask the patient if they need anything else while the interpreter is present.
- After leaving the patient’s room, review the session with the interpreter, as they may have cultural insights helpful to care planning.
Nurses must advocate for their patients by bridging language barriers and providing optimal care. Utilizing medical interpreters and implementing evidence-based strategies can assist nurses in providing quality care by eliminating language barriers (26).
Resources
The U.S. Department of Health and Human Services provides an example of a policy and procedure for giving meaningful communication with persons with limited English proficiency (23).

Self Quiz
Ask yourself...
- Can you discuss how the nurse can improve health outcomes for the LEP patient?
- List ten evidence-based interventions used to work with medical interpreters effectively.
- How can nurses advocate for LEP patients?
- Explain the importance of the Civil Rights Act of 1964.
- Explain the importance of Executive Order 13166.
Conclusion
The role of the medical interpreter is an important one. As the need for professional and certified medical interpreters grows, healthcare organizations must realize this. Medical interpreters are very significant members of the healthcare team. They assist in eliminating one of the most challenging barriers faced by providers: language barriers.
It is common knowledge that language barriers cause miscommunication, resulting in poor outcomes for all. Medical interpreters improve many aspects of healthcare, by assisting in overcoming cultural and language barriers, encouraging effective communication, and improving overall patient safety and satisfaction. As the need for their services grows, so should recognition of the importance of their work.
Nurse Preceptor Training
Introduction
What makes a great nurse preceptor? Nurse preceptors offer much more than extensive professional experience. The nurse preceptor is a valuable asset to both patient-facing nursing and nursing education. Preceptors assist nursing students and new nurses in transitioning to the real world of nursing by serving as trainers, evaluators, and mentors. Many nurse preceptors are chosen based on expertise in the field and leadership skills. However, some are ushered into the role due to staffing shortages.
An ideal nurse preceptor is a nurse who has experience, leadership abilities, and desire to teach or mentor. Amid the ever-present nursing shortage, there remains a high demand for qualified nurse preceptors. Studies show that nurse preceptor development leads to positive patient outcomes and staff retention [14]. Yet many preceptors are provided with little to no training. This course will offer a look into the exciting world of nurse preceptorship and offer tips for nurses who have a desire to transition into this highly esteemed role.
Basics of Nursing Education
Although nurse preceptors may work as staff nurses at hospitals and other clinical facilities, they are often associated with the field of nursing education. It is important to develop a clear understanding of how the field of nursing education works. Nursing education focuses on the training and evaluation of nursing students and professionals. Nurse educators do more than they teach. They test and evaluate if nursing students (or new nurses) understand the material and can practice safely. Many nurse educators serve as mentors and role models, and some even develop course curricula and other student learning materials. Nurse educators work in both clinical and academic settings and fulfill various roles, including facility educators, lecturers, professors, simulation instructors, and clinical instructors.
Clinical Nurse Educator
In clinical settings (hospitals, clinics, nursing homes, etc.), the clinical nurse educator, also termed the “nursing professional development specialist,” is responsible for educating both new and experienced nurses. They keep nurses up to date on current evidence-based practice protocols and guidelines and evaluate role performance ensuring that nurses practice safely and according to evidence. Clinical nurse educators may also have the added responsibility of managing new graduate nurse orientation training programs. Some educators may be responsible for managing several units/departments.
Academic Nurse Educator
In academic settings (colleges, universities, trade schools, etc.), the academic nurse educator is responsible for educating and evaluating nursing students at various levels of study. Evaluation methods include written tests, skills testing, and observation of clinical performance. Academic nurse educators work with nursing students enrolled in practical/vocational nursing programs, undergraduate registered nursing programs, and graduate nursing programs. The academic nurse educator may fulfill several roles in relationship with students, including class lecturer, simulation instructor, and clinical instructor [See Figure 1].
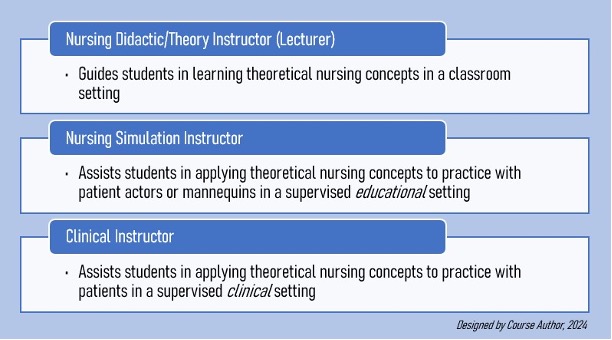
Figure 1: Nurse Educator Roles in Academic Settings
Although nurse preceptors typically do not work for nursing schools, they help by training students during clinical rotations and/or preceptorships at clinical sites, which allows the students to gain supervised clinical hours for educational and professional advancement.

Self Quiz
Ask yourself...
- Have you ever fulfilled the role of a nurse educator, community educator (teaching CPR or other health classes), or teaching assistant?
- Can you think of any other nurse educator positions in either clinical or academic settings?
- What characteristics do you think are most important to possess when training nursing students in particular?
- In your opinion, what is the primary way in which nurse preceptorship relates to nursing education?
Nurse Preceptor: Definition and Characteristics
Nurse preceptors, also called clinical preceptors, are practicing nurses who have the knowledge and experience needed to train nursing professionals. Preceptors train nursing students at clinical sites during their clinical rotations and new nurses at clinical facilities during new graduate nurse orientation programs. They provide one-on-one relationships with preceptees (individuals who receive the training), guiding and validating the knowledge, skills, and attitudes necessary for a smooth transition to a new nursing role [7].
An effective nurse preceptor has certain characteristics that make them best suited for the role. These include: [7][14]
- Nonjudgmental
- Positive demeanor
- Encouraging
- Respectful
- Active listener
- Authentic
- Supportive
- Caring
- Patient
Aside from training nursing students and new nurses, nurse preceptors provide orientation training to nurses transitioning to a new facility, department, or specialty, as well as those re-entering the field after being out of practice for an extended period. Nurse preceptors are critical to the success of a nursing facility/organization. The most effective preceptors help organizations move toward a goal or vision [14]. Goals can include nurse recruitment and retention, and nurse job satisfaction.

Self Quiz
Ask yourself...
- What interests you about fulfilling the role of a nurse preceptor?
- If you have ever fulfilled the role of a nurse preceptor before, what were some challenges you faced?
- In your opinion, what is the most important characteristic a nurse preceptor should possess?
- When you were a nursing student (or new nurse), how was your experience with your assigned nurse preceptor?
Nurse Preceptor Task 1: Build the Relationship
The first step to becoming an effective preceptor is to build a strong trusting relationship with the nursing student (or new nurse). The preceptee should feel a certain level of comfort when interacting with the preceptor. Fostering an environment of trust and safety plays a primary role in eliciting comfort in the relationship.
For example, nurse preceptors can get to know the preceptee by asking questions about their past educational experiences and future goals. Questions to ask may include:
- Is/was nursing school challenging for you?
- What about nursing school do/did you like?
- What do/did you like most about your nursing professors?
- Why did you choose nursing?
- How do/did you balance school and personal life?
- What nursing specialty interests you the most?
- What makes you the most nervous about your first workday on your own?
- Would you like to hear about my first workday as a nurse?
Communication between the nurse preceptor and preceptee should be open, honest, and reciprocal, and should include both formal and informal discussions [14]. Supportive environments allow the preceptee to feel comfortable asking questions [10]. The preceptee should also feel that they can share their fears and weaknesses with the preceptor without feeling judged.
For example, a new nurse may fear being challenged or questioned publicly. This may cause the new nurse to shy away from confrontations that might otherwise be unavoidable in the workplace, for example, when advocating for patients. The nurse preceptor should be aware of these limitations and therefore should provide a safe environment for disclosure.
When nurse preceptors share their past and present fears and weaknesses, preceptees may feel more comfortable opening up, which helps to build trust in the relationship [14]. Nurse preceptors who are emotionally intelligent and respectful in their communication, attitudes, and behaviors are most likely to build trusting relationships with preceptees [14].
Additionally, nurses who have an in-depth understanding of people will likely make great preceptors as people skills are a must [14]. Any nurse who desires to be a preceptor might benefit greatly from engaging in self-development.
Nurse Preceptor versus Clinical Instructor
The role of the nurse preceptor is ever-changing. At times, nursing schools rely on nurse preceptors to fill in when there is a need for clinical nursing faculty [11]. In addition, preceptors fill in the knowledge gap when students graduate without adequate clinical training. This was the case during the COVID-19 pandemic when many students were forced to forego valuable training at clinical facilities, leaving many entering the profession with limited clinical exposure [13].
While nurse preceptors may have the clinical experience necessary to provide training, many have not learned the methods of clinical teaching that would otherwise be required to fulfill the role of a teacher [11][12]. Teaching nursing students or new graduate nurses how to perform certain tasks and skills is only a part of clinical education, and although preceptors may be provided evaluation forms to fill out for each preceptee they train, many may not understand the basics of evaluation, including monitoring progress and providing feedback.
The clinical instructor typically has the knowledge base needed to effectively assess learning styles, apply teaching strategies, and evaluate whether students are understanding the material. This is what differentiates the nurse preceptor from the clinical instructor. In addition, nurse preceptors typically train one student at a time while clinical instructors train several students at once. Nurse preceptors can be prepared for their roles when provided training on basic concepts of clinical education. With this knowledge, nurse preceptors can better understand the teaching goal and collaborate more effectively with the student’s clinical instructor (if training a student) or the clinical nurse educator (if training a newly graduated nurse).


Self Quiz
Ask yourself...
- Did you notice a difference in how your clinical instructors taught you in nursing school and how your nurse preceptor trained you once you became a nurse?
- In your opinion, what is the most important skill a clinical instructor should have?
- How often do you witness clinical instructors teaching students at your facility?
- Do nurse preceptors at your facility also teach at nursing schools?
Skepticism of the Nurse Preceptor Role
Aside from the difficult task of teaching while managing a full patient load, nurse preceptors are responsible for all patients under their care, including those to whom the preceptee is assigned. The responsibility can be heavy for some nurses. Additionally, many nurse preceptors do not receive recognition in their roles. For nurse preceptors who have an interest in filling in as clinical faculty, skepticism about the role may be heightened as incentives are minimal. Many colleges and universities do not pay for clinical preceptors to help train their nursing students.
According to a 2020 Clinical Preceptor Survey report by the American Association of Colleges of Nursing (AACN) and the American Organization for Nursing Leadership (AONL), of 306 nursing schools surveyed, 90% do not pay for clinical preceptors for their students [3]. To make matters worse, more than half of the schools with baccalaureate programs (and two-thirds of those with graduate programs) do not provide additional incentives for nursing preceptors. These include access to an online library, free continuing education opportunities, tuition waivers, recognition certificates and ceremonies, appreciation gifts, and tax credits.
Impact on the Nursing Shortage
A lack of nurse preceptors has been cited as a reason for the growing nursing shortage. Nursing school enrollment is unable to keep up with the demand for nurses in the field [2]. While expanding enrollment would seem to be a plausible solution, there is a shortage of nurse preceptors available to train nursing students.
In 2021, U.S. nursing schools turned away over 90,000 qualified applicants from both baccalaureate and graduate nursing programs for reasons including lack of faculty, clinical sites, classroom space, finances, and clinical preceptors [1]. This number includes nearly 10,000 qualified applicants for master’s programs and approximately 5,000 for doctoral programs.
Nurse preceptors are needed to train both entry-level and graduate-level nursing students. These include students enrolled in any nursing program that requires supervised clinical practice hours. Programs include licensed practical/vocational nursing (LPN/LVN), registered nursing (RN), and advanced practice registered nursing (APRN) (nurse practitioner, clinical nurse specialist, certified midwife, etc.).
A lack of preceptors may also contribute to new nurses leaving the profession early on. Nearly 18% of new graduate nurses leave the profession within the first year for reasons including stressful working conditions and lack of leadership and supervision [4]. Nurse preceptors have the potential to positively influence the job satisfaction of the new nurse [10].
The nursing profession is in dire need of experienced nurses who are willing to serve as preceptors in several settings and at a variety of practice levels.

Self Quiz
Ask yourself...
- During your first year of nursing practice, did you want to leave the profession? If so, what were the reasons?
- What do you think is the primary reason some nurses do not want to fulfill the role of nurse preceptor?
- Does your facility offer any monetary or non-monetary incentives for fulfilling the role of nurse preceptor?
- What do you think facilities and nursing schools should do to help recruit more nurses to become preceptors?

Self Quiz
Ask yourself...
- How often do you see nurse preceptors at your facility engaging with nursing students and new nurses?
- In your opinion, what is the most challenging part of trying to build relationships with nursing students and new nurses at your facility?
- What are some additional questions you could ask the nursing student or new nurse to help build a trusting relationship?
- What are some areas for improvement in your own professional life that may be a barrier to establishing a trusting relationship with a nursing student or new nurse?
Nurse Preceptor Task 2: Assess the Learner
To effectively teach, the nurse preceptor must understand each learner’s learning style. The most effective nurse preceptors understand the importance of assessing the learner and providing teaching that is learner-specific [14]. Assessing the learner means studying the preceptee to see how they learn best. Nurse preceptors can also help preceptees understand their own learning styles. For example, some nursing instructors start class by requiring that new students take a learner assessment quiz.
A great way for the nurse preceptor to assess learning styles is to ask the preceptee how they learn best during school. Do/did they prefer the classroom, skills/simulation laboratory, or clinical activities? Do/did they prefer listening to the material in class and then studying the textbook afterward, or vice versa?
The following are two theories/models that may be helpful in the assessment of nursing students and new nurses.
VARK Learning Style Model
The VARK learning style model is a way that nurse preceptors can discover a preceptee’s learning style. This tool can also be used to help the preceptee learn their own learning style if unaware. VARK stands for Visual, Aural, Reading/writing, and Kinesthetic. The model was originally designed by Roger Flemings in 1987 as a way to differentiate between the various types of learners.
The following four VARK learning styles are described in relationship with students enrolled in health science programs (medical, dental, pharmacy, and nursing students) [6]:
Visual: graphics, maps, diagrams, charts
Auditory: lectures, group discussion, “talking things through”
Read/write: manuals, essays, reports
Kinesthetic: simulations, demonstrations, practical applications
Nurse preceptors should perform regular learning style assessments as styles can overlap and even change over time. One 2020 study found that masters-level nursing students had multimodal (multiple learning styles) and kinesthetic learning styles [6]. The researchers also found that 30% of the nursing students began the study with one preferred learning style but became multimodal later.
Doctor using digital tablet in a hospital corridor
Kolb’s Experimental Learning Theory
Designed by theorist David A. Kolb in 1984, the Experimental Learning Theory suggests that knowledge occurs through experience and is based on how the learner perceives, organizes, processes, and understands information. The theory highlights four stages and four learning styles. Nursing preceptors can use Kolb’s Theory to understand how preceptees learn, therefore, determining the best teaching strategy to employ.
Kolb’s four stages of learning include [7]:
Concrete Experience (CE): learns by feeling and/or being involved
Reflective Observation (RO): learns by observing, reflecting, and/or listening
Abstract Conceptualization (AC): learns through logic, reasoning, and/or creating ideas
Active Experimentation (AE): learns through action and/or decision-making
After determining what stages fit the preceptee, the nurse preceptor assesses which learning style best applies. Each learning style is formed through the combination of two stages. According to the theory, effective learning occurs when learners move through the four learning styles cyclically, typically giving preference to one style.
The four learning styles include:
Diverging (CE and RO): learns by listening, watching, and being involved
Assimilating (RO and AC): learns by listening and watching, and “putting the pieces together”
Converging (AC and AE): learns by “thinking things through” and making decisions
Accommodating (AE and CE): learns by being actively involved and making decisions

Self Quiz
Ask yourself...
- Have you ever assessed your own learning style using a theory or model, and if so, what prompted you to do so?
- What was your preferred learning style in nursing school and what is your preferred learning style now?
- Have you ever asked a nursing student or new nurse about their preferred learning style? If so, what were some answers?
- In your opinion, why might a nurse preceptor avoid assessing a new nurse’s learning style?
Nurse Preceptor Task 3: Tailor Teaching
After discovering a preceptee’s preferred learning style, nurse preceptors should use teaching strategies that would be most appropriate for the learner [14]. Just as care plans should be tailored to each patient, teaching should be tailored to each preceptee. This does not mean to avoid different teaching strategies.
Preceptees still need a variety of teaching strategies to ensure that learning is effective [10]. However, tailoring teaching to the preferred style is beneficial as the preceptee will likely be more engaged, which can lead to an easier learning experience.
For example, if a student learns best through demonstration, try to provide opportunities for the student to practice hands-on skills more often. If a student learns best by hearing a lecture, sit down frequently with the student after patient interactions to verbally go over what was learned during care. If the student learns best when working in groups, consider inviting one or two nurse coworkers to briefly discuss the plan of care for the student’s assigned patient. This way, the student can hear the perspective of multiple nurses and ask questions as needed.
Refer to the following table (Table 1) for ways to prepare the preceptee for tailored learning experiences based on their learning style.
|
If the preceptee learns best when… |
The nurse preceptor should… |
|
Listening to lectures (face-to-face, audio, video) |
Recommend facility-approved videos and/or audio recordings about care topics. Briefly review care topics with preceptee at various intervals throughout shift (can include discussions at the end of shift)
|
|
Reading written materials (textbooks, written presentations) |
Encourage preceptee to bring own learning materials and “cheat sheets.” Refer preceptee to appropriate educational materials about care topics, for example, patient instruction sheets.
|
|
Working in groups |
Arrange brief post-care discussions with preceptee and nursing peers. Arrange for preceptee to attend departmental team huddles/meetings.
|
|
Observing demonstrated skills (on video, or performed by instructor) |
Provide more opportunities for preceptee to observe skills. Recommend facility-approved skills videos about care topics. Ask nursing peers to allow preceptee to observe performed bedside skills.
|
|
Practicing hands-on skills |
Provide frequent opportunities for preceptee to perform supervised bedside skills. Inform nursing peers that preceptee is open to performing skills.
|
|
Studying Alone |
Allow preceptee to take learning breaks to review educational materials alone. Encourage questions afterwards.
|
Table 3: Teaching According to Learning Styles

Self Quiz
Ask yourself...
- What is another way a nurse preceptor can facilitate learning in a nursing student who learns best while working in groups?
- If you have ever had a nursing student or new nurse observe you performing a bedside skill, how was the experience?
- Have you ever asked a coworker to allow a new nurse you were training to perform a bedside skill on their patient?
- What are some other recommendations a nurse preceptor can make to a nursing student who learns best when studying alone?
Nurse Preceptor Task 4: Evaluate Learning
The primary difference between orienting an experienced nurse to a new facility and precepting a new graduate nurse is the process of formal evaluation of clinical competency. Clinical evaluation is the combination of observing clinical performance (skills and professionalism), keeping track of the preceptee’s learning progress, and providing feedback to the preceptee [14].
Observing Skill Performance
Observing the preceptee during skill performance to assess accuracy and safety is likely the most notable part of the evaluation. Once the preceptee has been trained appropriately on a skill, the nurse preceptor should observe the preceptee perform the skill independently, only interrupting if patient safety may be compromised. Nursing students and new nurses must learn how to problem-solve without unnecessary interference from the preceptor. Unknowingly, the nurse preceptor may hinder the development of problem-solving skills in the preceptee when frequently stepping in to “take over” due to time constraints or frustration.
The goal of preceptorship is for the preceptee to be able to provide safe care independently [10]. Therefore, the nurse preceptor should employ the “sink and swim” method (when the nurse preceptor does not help the preceptee during the skill) [10].
This should only occur after the preceptee has been trained in the skill. While it may be challenging to remain inactive while observing, patience is one of the characteristics of an effective nurse preceptor. When the preceptee is allowed to perform the skill on their own in its entirety, only then can the nurse preceptor truly know if the training/teaching was successful.
Observing for Professionalism
Aside from evaluating skill performance, nurse preceptors should observe the level of professionalism the preceptee demonstrates throughout the training experience, for example, remaining punctual, respecting others, and maintaining the confidentiality of patient information. Nurse preceptors should observe the preceptee in daily interactions with patients/families, nursing peers, managers, and other members of the interdisciplinary team, paying attention to the preceptee’s communication and people skills. Nurse preceptors should also be able to identify the cause of a preceptee’s behavior and avoid misinterpreting typical behaviors for lack of professionalism.
Some preceptees (particularly nursing students) may be timid and nervous during training which may lead to errors. For example, a nursing student may fear speaking with a particular physician over the phone, leading to a lack of confidence during the call. This may lead to a transfer of misinformation. In this case, a lack of professionalism is not the problem.
The nurse preceptor should recognize that this behavior is not unusual, and support the student, offering tips to help. Tips can include writing down notes before making the call and keeping the patient’s medical record easily accessible in case the physician has a question. The preceptor can take it a step further and sit down with the student to discuss why they may feel intimidated by the physician. Other reasons why preceptees may struggle during training include knowledge gaps, personal problems, and poor communication skills [10].
Tracking Progress
Some clinical facilities track progress through weekly forms that the preceptor fills out. The forms contain objectives/competencies that must be met by the preceptee before progressing through the various stages of the preceptorship program. Without properly tracking progress, there is a potential that a preceptee will reach the end of the preceptorship without the skills necessary to practice safely or effectively, similar to a student completing an entire four-year nursing program without completing one exam. Keeping track of the preceptee’s progress is a formal way for the nurse preceptor to know that the preceptee truly understands what is being taught at every stage of the clinical training.
Giving Feedback
Providing both positive and constructive feedback is the final piece of evaluation. The nurse preceptor should provide both written and verbal feedback, addressing strengths, areas for improvement, and tips for how to improve. Addressing areas for improvement can be a stressful time for preceptors [10]. Some students may take offense to the negative feedback. However, when preceptees believe that constructive feedback is genuinely intended and not meant to be punitive, it is better received [14].
Feedback should be timely and confidential [10]. Nurse preceptors should remain non-demeaning, use tact and consideration, and allow the preceptee time to ask questions and summarize what was said [14]. The nurse preceptor should inform the preceptee of any progress made as learning is enhanced when learners believe they are making progress [10]. The nurse preceptor can also ask the student to assess their progress in the training program.
Questions to ask the preceptee may include:
- How do you feel like you performed today/this week?
- Was there anything you felt like you missed today/this week?
- What was the most helpful tip you learned today/this week?
- Do you feel like you are progressing at a comfortable speed?
- Do you feel ready for the next training day?
- How can I help you improve for next time?

Self Quiz
Ask yourself...
- Have you ever observed a nursing student or new nurse perform a skill incorrectly? If so, what steps did you take?
- What is your experience with handling unprofessional nursing student behaviors at your facility?
- In ways does your facility track the clinical progress of new graduate nurses?
- Have you ever experienced a nursing student or new nurse challenge you regarding feedback you gave them?
Nurse Preceptor Task 5: Encourage Independence
Along with managing patient care, new nurses (and nursing students) have to learn how to organize their day-to-day activities [12]. One way nurse preceptors can encourage independence in new nurses in particular, is to allow them to develop their own way of organizing their activities, essentially, developing their own practice routines.
While introducing preceptees to the real world of nursing is important, each nurse develops their own routine over time. Nurse preceptors should understand that introducing preceptees to real-life clinical situations has more to do with guiding how to address problems that may arise in the workplace, and less to do with forcing their own personal practice routines on the preceptee. Many nurse preceptors may struggle to find the balance between teaching personal routines and allowing the preceptee to develop their own routines.
Although there may be some routines and tips (that do not compromise patient safety) that can help the preceptee save time, nurse preceptors should make it a priority to teach the standard way of practice (“according to the book”). The rule of thumb is to teach and evaluate the preceptee according to the universal way of practicing (as if they are being observed by a state surveyor) or based on facility culture/practices. Nursing students and new nurses can develop their own unique time-saving routines over time as they get stronger in their practice. Personal time-saving tips should be shared as an optional routine style that the preceptee can adopt at will or as they become more confident in their role as a competent nurse.
The nurse preceptor can demonstrate their own personal routines to the preceptee to show how they may be beneficial in practice. Additionally, it may be helpful for preceptors to share other routine styles. For example, one nurse may choose to perform morning assessments on all of their patients, and then administer morning medications afterward. Another nurse may prefer to perform an assessment on one of their patients, and then administer morning medications to that same patient before moving on to the next patient. Nurse preceptors should consider facility protocols/practices when sharing routines.


Self Quiz
Ask yourself...
- When you first became a nurse, did your preceptor train you according to their own practice routine? If so, what parts did you adopt as your own?
- How long did it take you to develop your own personal practice routine?
- Does your practice routine change when in the presence of a state surveyor or nursing manager/director?
- If you have previously trained a new nurse, what has been the most challenging part of training “by the book”?
Nurse Preceptor Roles and Competencies
Clinical competencies (abilities) are ways by which nursing practice is measured. Nursing students must meet competencies to progress academically. Nurses must meet competencies to continue safely practicing in the field. Nursing educators must meet competencies to teach effectively. Finally, nurse preceptors must also meet competencies to effectively train and mentor nursing students and new nurses. Meeting competencies proves that nurses are “competent” in their role.
The Association for Nursing Professional Development (ANPD) designed a set of 72 clinical competencies that are primarily categorized according to the seven roles (or role domains) of the nurse preceptor [7]. The seven roles include role model, teacher/coach, facilitator, protector, socialization agent, leader/influencer, and evaluator [See Figure 2].
Six of the 72 competencies are considered “core competencies,” meaning, they do not fall under a specific role domain. Core competencies should be met by every nurse preceptor, regardless of the specific role they fulfill.
For example, in basic nursing, some nurses may be required to maintain a sterile environment in their role (like surgical nurses) while others can simply maintain a generally clean environment. However, all nurses, no matter the specialty, must follow basic infection control measures like general handwashing. Core competencies are similar to “general handwashing.” All nurse preceptors must meet core competencies, but others who fulfill certain roles must also meet the competencies of that particular role. As a general rule, all nurse preceptors should aim to fulfill all seven preceptor roles.
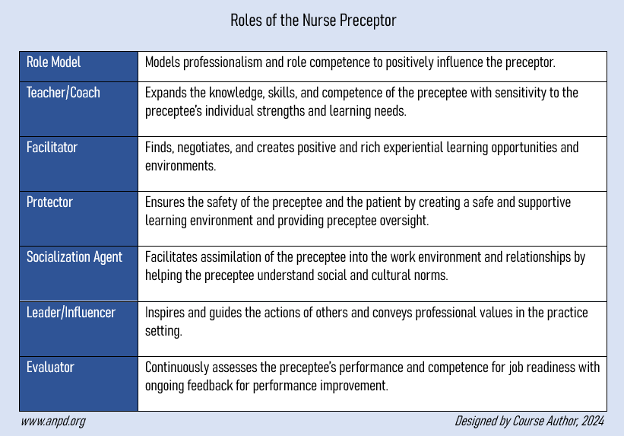
Figure 2: Roles (Role Domains) of the Nurse Preceptor [7]
Core Competencies
To meet core competencies, all nurse preceptors must apply evidence to practice when training preceptees. While preceptors may already engage in evidence-based practice as nurses, they must ensure that all information shared with the preceptee is based on current evidence. This competency requires that nurse preceptors stay up to date on current research. This may be done by regularly attending educational work meetings (like staff meetings and training sessions) and through self-learning, for example, enrolling in professional development courses (i.e., continuing education courses).
Other ways to meet core competencies are by solving problems, maintaining the preceptee’s confidentiality, and respecting diversity and others’ opinions [See Figure 3 below].
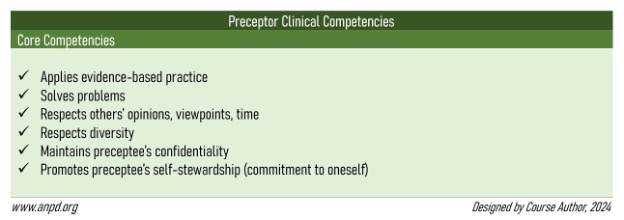
Figure 3: Nurse Preceptor Clinical Competencies Core Competencies [7]

Self Quiz
Ask yourself...
- How do you ensure that you are practicing according to evidence?
- Have you ever witnessed a nurse preceptor disclosing (to other nurses) a new nurse’s challenges and weaknesses?
- What are some ways a nurse preceptor can teach problem-solving skills to a nursing student?
- Have you ever completed a nursing professional development course that was not required to renew your nursing license?
Role Model Competencies
Teaching by example is a way to positively influence the behavior of the preceptee [14]. Many people learn by watching the behavior of others in leadership roles. Modeling professional behavior is one of the primary roles of a preceptor. Nurse preceptors model time management skills, priority setting, critical thinking, problem-solving, and evidence-based practice [14].
To meet competencies for the role model domain, nurse preceptors should be aware of their own attitudes and behaviors as this may impact the preceptee. The preceptor’s behaviors should align with what is being taught to the preceptee as learners are most likely to remember what was done rather than what was said [10].
Personal accountability should be demonstrated by the nurse preceptor when mistakes are made. This way, the preceptee can not only learn the importance of taking accountability for their own actions in the workplace, but they can see what happens as a result (chain of events, rewards, disciplinary action, etc.). Preceptees should understand that disciplinary action is not meant to target the nurse, but to promote positive changes in the workplace. Other competencies include modeling healthy and safe behaviors and demonstrating professional development [See Figure 4 below].

Figure 4: Nurse Preceptor Clinical Competencies for the Role Model Role [7]

Self Quiz
Ask yourself...
- How confident do you feel in your ability to be a good role model to new nurses at your facility?
- If you have previously trained a new nurse, have you ever admitted to the new nurse a mistake that you made during patient care?
- How often do you see new nurses adopting poor practice habits from their preceptors?
Teacher/Coach Competencies
Teaching is the cornerstone of clinical education. The primary goal of clinical education is to prepare the nursing student or new nurse for practice through clinical training and coaching/mentorship. As discussed earlier, effective teaching is learner-specific and tailored to the preceptee’s learning needs. To meet competencies for the teacher/coach role domain, nurse preceptors should incorporate the three domains of learning according to Bloom’s Taxonomy [5][9][13]:
- Cognitive: attainment of knowledge (through written and verbal teaching)
- Psychomotor: development of hands-on skills (through demonstrative teaching)
- Affective: development of skills associated with attitudes, beliefs, values, or feelings (through ethics training, conflict resolution training, etc.)
Instilling critical thinking skills in the preceptee is also a primary goal when fulfilling the role of teacher/coach. Nurse preceptors might consider thinking aloud when observed by the preceptee as this can show critical thinking and decision-making in action [7]. When performing skills or care in the presence of the preceptee, speak aloud what is happening during each step. For example, if an elderly patient who is opioid-sensitive reports pain, review the medical record with the preceptee stating out loud (or to the preceptee) thoughts such as:
“The patient already received a low-dose opioid for pain an hour ago. The patient’s most recent blood pressure is low. Since the patient is elderly, opioid-sensitive, and has low blood pressure, I will give a non-opioid medication for breakthrough pain instead. This way, the patient remains hemodynamically safe.”
The nurse preceptor can encourage the preceptee to ask questions or think aloud while caring for themselves. This way, the preceptor can evaluate the clinical reasoning skills of the preceptee [10]. Other competencies include helping the preceptee recognize errors and near misses, redirecting counterproductive behavior, showing the preceptee how to analyze situations and consider alternatives, and helping them to differentiate between data that is important and unimportant.
[See Figure 5 below].
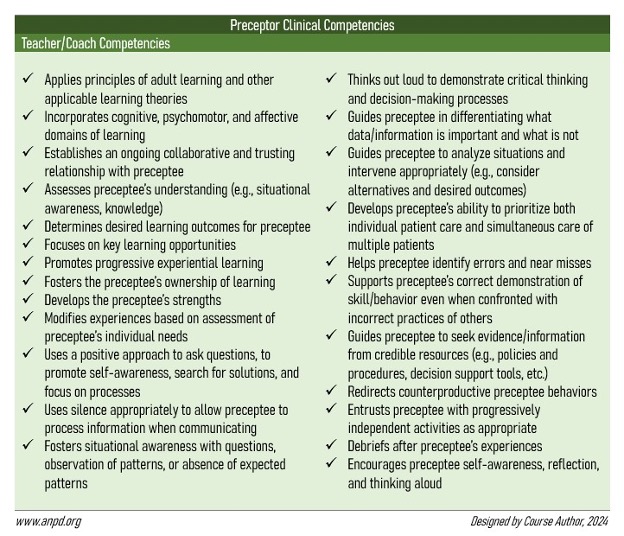
Figure 5: Nurse Preceptor Clinical Competencies for the Teacher/Coach Role [7]

Self Quiz
Ask yourself...
- Have you ever had a coworker confront you about the way you were training a new nurse? If so, how did you address the situation?
- How would you address a nursing student who is frequently engaging in excessive conversations with patients, ultimately disrupting care?
- If you have previously trained a nursing student, have you witnessed the student catch themselves before making an error?
- How else might a nurse preceptor encourage affective learning (learning domain) in a nursing student or new nurse?
Facilitator Competencies
To meet competencies for the facilitator role domain, nurse preceptors must identify learning needs in the preceptee and provide learning opportunities to meet those needs. Although similar to the teaching role, the facilitator makes a concerted effort to make learning easier for the preceptee. As mentioned earlier, nurse preceptors can arrange for the preceptee to observe or practice skills with other nurses within the facility/department. The nurse preceptor should take every opportunity to enhance the learning experiences of the preceptee.
For example, a nurse preceptor at a hospital can request patient assignments that might create optimal learning opportunities for a nursing student. This may include an assignment of patients who need certain skills/tasks performed that day (e.g., enteral feeding, wound care, intravenous insertions, pre-surgical preparation, etc.).
Other competencies include assessing the preceptee’s learning interests and providing resources for support [See Figure 6 below].
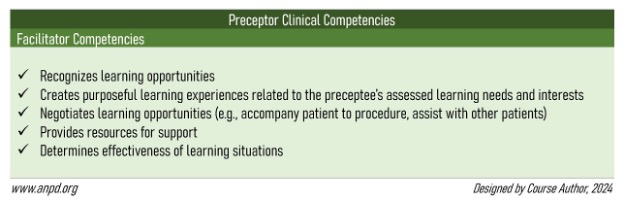
Figure 6: Nurse Preceptor Clinical Competencies for the Facilitator Role [7]

Self Quiz
Ask yourself...
- Is your facility nursing-student-friendly? Do you find that your coworkers generally welcome students from local nursing schools?
- If you work in a hospital, do you find that patient assignments change when there is a nurse preceptor on the floor?
- How open are you to allowing a group of nursing students to observe you perform a bedside skill?
- In what ways have you helped a nursing student gain additional learning opportunities within your department?
Protector Competencies
When training a nursing student, the nurse preceptor is fully responsible for the assigned patients as there is only one nursing license under practice. Although new nurses practice under their own licenses, nurse preceptors still have the responsibility of ensuring that the nurses practice safely. If a new nurse is reprimanded for a mistake made during a preceptorship, the preceptor is likely to be reprimanded as well. In a way, the nurse preceptor is “responsible” for the preceptee and serves as a protector.
To meet competencies for the protector role domain, nurse preceptors must ensure a safe environment for the preceptee. This may include protecting nursing students from physical abuse by teaching them how to properly interact with patients who display aggressive traits or standing up for new nurses to prevent incivility or bullying attempts by nursing peers (for example, when nurses “eat their young”). Other competencies include encouraging preceptees to advocate for themselves and anticipating issues that can cause moral distress to the preceptee [See Figure 7 below].
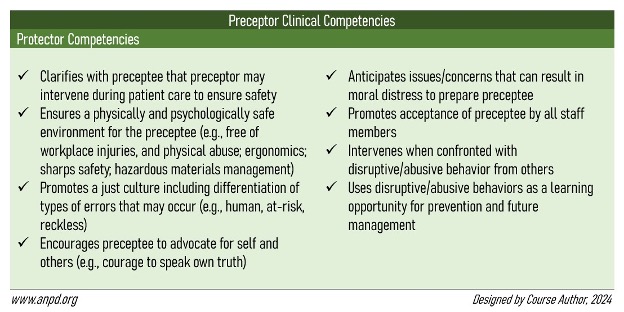
Figure 7: Nurse Preceptor Clinical Competencies for the Protector Role [7]

Self Quiz
Ask yourself...
- Are you most comfortable with the idea of training nursing students or new nurses? What is your reasoning?
- Have you ever been reprimanded for a mistake that a nursing student or new nurse made while under your supervision?
- Can you think of another way a nurse preceptor can protect a nursing student or new nurse from danger in the workplace?
- When you were a nursing student, were you ever bullied by a nurse? Did anyone speak up for you?
Socialization Agent Competencies
Many nursing students and new nurses experience a “reality shock” when entering the real world of nursing [7][12]. While nursing school prepares the preceptee for clinical practice, some situations may arise in the workplace that may be hard to simulate in a controlled educational setting. To meet competencies for the socialization agent role domain, nurse preceptors must introduce preceptees to the unspoken rules and culture of both real-life nursing and the facility itself [7][14].
For example, a new graduate nurse may be unprepared for the many interruptions that often occur when practicing nursing in a clinical setting (e.g., phone calls, physician requests, family visits, and frequent documentation). The new nurse may also be unaware that the department in which they are training schedules interdisciplinary team rounding sessions at a specific time every day, which can make it difficult to establish a solid routine. The nurse preceptor has a responsibility to introduce the preceptee to these types of “real life” situations.
Other competencies include providing the preceptee with opportunities for interprofessional engagement and inclusion in department activities (like work parties) [See Figure 8 below].
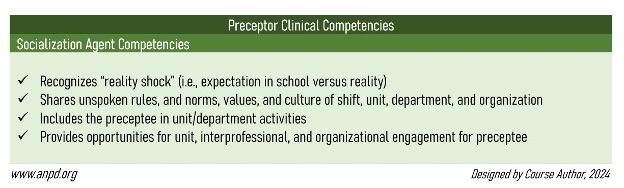
Figure 8: Nurse Preceptor Clinical Competencies for the Socialization Agent Role [7]

Self Quiz
Ask yourself...
- How was your first day as a nurse? Did you experience a reality shock or were you fairly prepared?
- What is something within the culture or practice of your facility that might cause a new nurse to experience a reality shock?
- How does your facility formally introduce new nurses to your department? Email, newsletter, work meeting, quick huddle?
- Have you ever had lunch (at work) with a nursing student or new nurse you were training?
Leader/Influencer Competencies
Leadership skills are vital when training others and serving as a role model. To meet competencies for the leader/influencer role domain, nurse preceptors must demonstrate professionalism and adhere to codes of conduct and regulations. Recognizing the scope of practice of preceptees (nursing students versus new nurses), delegating appropriate tasks, and providing recognition are additional leadership skills the preceptor should possess. Most importantly, the nurse preceptor can demonstrate leadership by advocating for patients.
When nurse preceptors possess excellent leadership skills, they can serve as change agents within the workplace, positively influencing decisions that affect patients, their peers, and the preceptees they train. To be a change agent, nurse preceptors must possess people skills and be able to work effectively in a team (qualities of a leader) [14].
Other competencies include participating in professional activities at the facility, engaging in self-reflection, and helping the preceptee develop a professional role identity [See Figure 9 below].
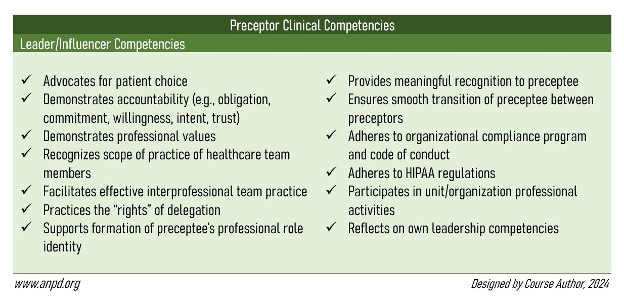
Figure 9: Nurse Preceptor Clinical Competencies for the Leader/Influencer Role [7]

Self Quiz
Ask yourself...
- In what ways do you self-reflect? Do you find that self-reflection contributes to your professional growth?
- Have you ever advocated for a patient in the presence of a nursing student or new nurse?
- Have you ever witnessed a nurse preceptor delegate a task to a nursing student that was out of their scope of practice?
- Think of a nurse within your department who you consider a leader. What sets them apart from other nurses?
Evaluator Competencies
As mentioned earlier, evaluation is the best way for the nurse preceptor to know that the preceptee understands what is being taught. To meet competencies for the evaluator role domain, nurse preceptors must assess preceptee performance and provide accurate, specific, and constructive feedback (both verbal and written). Preceptors must also hold the preceptee accountable for their practice. Other competencies include managing difficult conversations when providing constructive feedback, and informing preceptees of their strengths and areas where improvements are needed [See Figure 10 below].
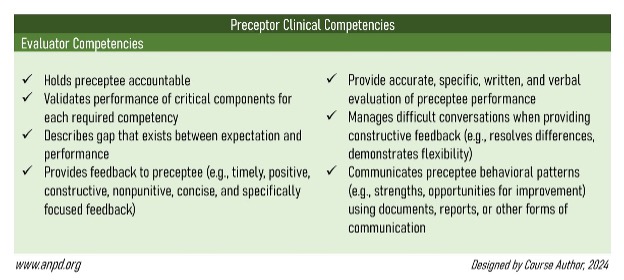
Figure 10: Nurse Preceptor Clinical Competencies for the Evaluator Role [7]

Self Quiz
Ask yourself...
- What was the first compliment you received as a nurse? How important did it make you feel?
- In the past, have you ever felt offended or hurt when a manager gave you constructive feedback? What made you feel that way?
- If you have previously trained a new nurse, did you give written or verbal feedback (or both)?
- With the knowledge from this course, do you feel better prepared to begin your role as a nurse preceptor (or continue doing so)?
Conclusion
Nurse preceptors are a valuable asset to the nursing profession. They assess learners, build trusting relationships, tailor teaching to learning styles, evaluate performance, provide feedback, and encourage independence in the preceptee. Although nurse recruitment and retention are dependent on the availability and service of nurse preceptors, the position has its challenges.
The nurse preceptor role is not always given the recognition it deserves. However, when nurses are adequately prepared for the role, they have the potential to lead positive changes in the workplace, influencing the lives of nursing students and new nurses. Moreover, nurse preceptors can impact the healthcare field by contributing to the future of nursing, ultimately leading to better outcomes for patients.
Orientation of Unlicensed Assistive Personnel
Introduction
Unlicensed assistive personnel (UAP) are valuable members of the healthcare team that can carry out delegated care duties in the assistance of patients including vital signs, personal hygiene, assisting with meals, and toileting. In some cases, UAPs, when additional education is given, may monitor patient’s blood glucose, cognition status, wound care with dressing, and insert foley catheters or intermittent urinary catheters. UAPs come from a variety of different levels of training and are held to different standards based on state law, facility policy, the state’s board of nursing, and the setting that they are employed within. The use of UAPs across the healthcare continuum is advocated by the American Nurses Association and the National Council of State Boards of Nursing to assist with the nursing shortage and ensure that patients receive care that is quality-based and safe.


Self Quiz
Ask yourself...
- If you were a nurse manager, how would you most effectively implement a training program for UAP staff when there are multiple roles hired with differing levels of patient care experience?
- Where would you look to find guidance on the scope of UAP within your state?
- When orienting a new UAP to your unit, what communication style would you use to ensure understanding?
Defining the Role of the UAP
The role of the UAP is varied and broad depending on the setting, needs of the patient, staffing levels, and the level of training provided to the employee. Regardless of the type of facility or practice the UAP is employed in, clear guidelines and barriers must be defined to ensure the UAPs scope is understood by all levels of personnel and management. Leadership must ensure that their policies and procedures align with that state’s nursing practice act (1).
The term UAP can cover many different titles as this is an unregulated position that may cover clinical, administrative, or a blended role of both these areas. As a healthcare paraprofessional, the UAP may be any of the following: nurse aide, ambulatory assistant, clinical unit clerk, nursing assistant, or nurse technician.
The benefits of employing the UAP are to improve staff satisfaction and retention, increase the equity of duty sharing, and lower attrition rates. The balance of duties and responsibilities that may ultimately fall on the nursing staff can be shared. Jobs that do not specifically require nursing knowledge and expertise may be fulfilled by the UAP. This allows nursing staff more time to focus on the clinical aspects of patient care, carry out care plans, and increase the number of hours spent at the bedside (3). The benefits that are reaped by the UAP include gaining employment as a healthcare paraprofessional without having to pursue a degree, opportunities for further responsibility and training to higher level positions, and experience if pursuing a degree in the healthcare field.

Self Quiz
Ask yourself...
- What benefits have you experienced having UAPs to assist with nursing care?
- Have you ever experienced a time where an individual that you delegated to did not complete the tasks? How did you respond?
- Do you find that having additional UAP as opposed to nursing staff increases the amount of time that the nurse can be at the bedside focused on specialized nursing care?
Onboarding
The onboarding and orientation of a UAP should be rigorous in acclimating the new employee to the facility’s culture and team environment. This should include policies and procedures that clearly define the roles, expectations, and assignments that are appropriate to each function. The UAP must understand their role within the nursing care team and the delegating relationships between the RN, LPN/LVN, and UAP roles. The UAP should be provided with a checklist of competencies that explain the skills and assignments that are appropriate to their roles. This training should also encompass the job functions outside of their scope of work to ensure that boundaries are understood.
The UAP must understand the delegation relationship that is a unique part of the nursing/UAP team. Open conversation, collaboration, and shared decision-making promotes work environments that support a culture of safety and healthy relationships (1). A culture of safety has been shown to increase retention rates, increase staff satisfaction, and enhance engagement. All of these contribute to improved patient perception of care, higher scores on quality assessments and publicly reported survey scores (9).
At minimum, orientation should provide the following:
- Introduction to the facility’s mission, vision, and values
- Review of policies and procedures
- Patient-centered care focus
- Individualized topics that relate to work focus
- Communication expectations
- Mindfulness with colleagues, patients, and family members
- Codes of conduct
The American Nurses Association advocates for an orientation that shifts from the previous trend of an in-service layout that introduces an overwhelming amount of new content presented by leaders from across the organization to a toned down, tailored format. The new model is geared towards a multiple day layout where one or two competencies are focused on each day. These competencies are developed from the Quality and Safety Education for nurses’ foundations and cover topics including teamwork and collaboration, patient-centered care, evidence-based practice, quality improvement, informatics, and patient safety (9).

Self Quiz
Ask yourself...
- What ways might be most effective in designing an orientation program that incorporates learning for individuals that have many different levels of experience in patient care?
- What do you believe is the best format to deliver new employee orientation? Remote? Face to face? A blended method?
- Recalling a previous orientation that you have been through, what key points stuck out to you as important information in those beginning days of new employment?
- Have you experienced an orientation that was based on a checklist of competencies? How did this compare or differ to your most recent orientation?
Competency-Based Orientation
A robust education with orientation is essential to the success of the UAP, regardless of their background. As previously discussed, UAP may have varying levels of experience within the healthcare field. There are training certificate programs that provide individuals with basic patient care skills to assist with activities of daily life, obtaining vital signs, and completing simple nursing tasks such as wound care and administering oral medications that are taken on a regular basis. These programs are typically geared towards graduating as a nurse aide or assistant.
While nursing programs embed patient safety education into their programs, the staff that have significant, direct involvement typically have limited training or are new to the healthcare environment. This requires facilities and healthcare organizations to be proactive in determining the role and scope that the UAP will fulfill and ensure that these topics are covered sufficiently for a base understanding. It is important to develop the knowledge, skills, and attitudes that are imperative to carry out evidence-based interventions (2).
A competency-based orientation should be built around a standardized set of best practices that implement and drive forward quality patient care. The minimum time frame to develop these skills that will shape safe patient care and define the responsibilities of the UAP should take approximately six months total. A set of time, typically six to eight weeks, should be scheduled as a preceptorship when the employee begins working on their assigned unit.

Self Quiz
Ask yourself...
- Many nursing programs are now requiring that applicants have previous UAP experience. What are your thoughts on this?
- How long do you think is sufficient to orient and train new UAP staff?
- If a new UAP employee has previous experience in their role or in the healthcare field, is it fair to shorten their orientation?
Preceptor/Preceptee Relationship
When a new hire is onboarded and oriented to their home unit, there is a period of time that is established for training and learning the UAP role. A preceptor is assigned to the new employee for a set period of time, and this is when the new employee starts off shadowing the experienced employee. This relationship may be solely partnered with one preceptor, or there may be many involved depending upon the staffing requirements and needs of the unit, facility, or work environment. Often the preceptor is an experienced team member with the same job title; however, this may not always be the case. The new UAP may also be paired with nursing staff to be acclimated to the workflow, expectations, and to form positive professional relationships with the patient care team. This type of multidisciplinary collaboration early on can limit misunderstandings of practice scopes and role clarification later as time goes on (1, 4, 6).
At this time, the preceptor shows the new employee the skills required to successfully complete delegated tasks and duties. The new employee should be given sufficient time to practice the skills taught and have opportunities to ask questions. It is important to establish a respectful and nurturing relationship where the trainee feels comfortable asking questions (6).
This time is a wonderful opportunity to build healthy working relationships and promote collaboration.

Self Quiz
Ask yourself...
- You have delegated a bed bath and changing linens of a patient to a new UAP. Upon checking progress, you find the UAP texting on their cell phone at the nurse’s station. How would you handle this matter?
- What influence do you believe that UAPs have on the quality of care delivered to patients on a busy unit with high acuity?
- What factors can you think of that may affect the professional relationship between nurses and UAPs?
- What is your personal perception of working with UAPs in your professional healthcare practice?
Patient Care and Responsibilities
The guidelines and standards that determine the scope a UAP can work within are based on tasks that do not require additional formal education or extensive clinical training.
Often UAP are delegated duties that are simple, patient care tasks. These may include any of the following clinical, patient care activities (3, 5):
- Measuring height and weight
- Obtaining and charting vital sign measurements
- Applying cardiac electrodes and recording an electrocardiogram (ECG)
- Collecting urine and performing point-of-care urinalysis
- Assisting with activities of daily care
- Hygiene
- Alarm response and notification to the nurse
- Wound care/dressings
There may be specialized job functions that may be delegated to the UAP after additional education with competency is determined through observation and a verification process. Some job functions that require extra training include (3, 5):
- Insertion and removal of foley catheters
- Removal of intravenous (IV) catheters
- Phlebotomy/venipuncture
- Foot care
- Administration of vaccinations and certain injections
It must always be kept in mind by the delegator that any job that is delegated to the UAP continues to be the responsibility of the professional that has assigned the duty for safety, efficacy, and proper completion.
Delegation Decisions
Delegation is a skill that requires critical thinking, knowledge of the UAPs skills and knowledge levels, and communication to ensure there is clear understanding of responsibilities and closed loop communication. Delegation has been defined by the ANA and NCBSN as the “…transfer of responsibility for the performance of a task from one individual to another while retaining accountability for the outcome” (5).
There are five rights involved with delegation. These include (5):
- Right task
- Right circumstance
- Right person
- Right direction and communication
- Right supervision and evaluation
These principles must be promoted to encourage the delivery of patient care that is safe and retains quality. Focusing on the distribution of tasks that may be delegated to the UAP in order to alleviate the pressure and workload on the nurse is essential to allow RNs to effectively assess, intervene, and evaluate responses to treatment. The healthcare team and healthcare providers rely upon this essential information to guide clinical care. Research has shown that an increase in the hours that an RN spends on direct patient care improves patient outcomes and reduces mortality rates (6).
When the UAP is working on a nursing unit, it is also important to ensure that the nursing staff have the managerial skills and comfort levels to properly delegate. There should be additional education and training in place to teach nursing staff the art of delegation to gain the most benefits from the added responsibility of delegating, monitoring, and ensuring patient care and safety is upheld (1).

Self Quiz
Ask yourself...
- What patient care activities do you believe are beyond the scope of the UAP and should never be considered for delegation?
- You have assessed a UAP for the skills required to change a dressing wound and do not believe they are properly trained. What would you do in this situation?
- In your practice, what difficulties have you experienced in delegating to UAPs?
Policy and Protocols
Executive and unit leadership must ensure that policies are clear in defining the role of the UAP. This will reduce role confusion and prevent close calls and/or adverse events related to the paraprofessionals’ lack of training or inexperience. Ideally, policies and protocols should ensure adequate and appropriate training is afforded to all UAPs that are new to the facility, regardless of their previous experience.
Topics that should be covered in the policies and procedures include (1):
- Nursing and UAP education standards
- Licensing requirements
- Scopes of practice
- Standards of patient care
- Codes of conduct
- Disciplinary action repercussions and actions
- Federal regulations that guide care
- Staffing levels based on acuity
- Facility and unit rules
- Delineating the chain of command to address safety concerns

Conclusion
UAPs are valuable members of the healthcare team that can be trained to provide safe patient care. Many nurses find that having UAP assistance on their unit has changed the flow of patient care and decreased the response time to urgent patient needs. There is a culture change that must occur to clearly establish the rights and responsibilities of delegation between the nurse and UAP.
Lyme Disease and Chronic Fatigue
Introduction
Lyme disease is the most common vector-borne disease in the United States and one of the most frequently diagnosed tick-borne infections globally (1, 11). Each year, approximately 30,000 cases of Lyme disease are reported to the Centers for Disease Control and Prevention (CDC) by state health departments, but this does not reflect all cases. Insurance companies report approximately 480,000 cases of Lyme disease in Americans (1).
Lyme disease is most prevalent in the Northeastern United States, stretching from northeastern Virginia to Maine. Specific states that are affected include Connecticut, Delaware, Maine, Maryland, Massachusetts, Minnesota, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, Vermont, Virginia, and Wisconsin. Some cases have been reported in Northern California, Oregon, and Washington (1, 11).
In the states with the highest reported cases, the incidence is roughly 40 per 100,000 people (11). Most reports of the illness occur during the months when people spend time outdoors: spring, summer, and early fall.
The incidence of Lyme disease is higher in Caucasians than in darker-skinned individuals, but some researchers think this is due to the associated skin lesion being easier to determine in lighter-skinned people (11). The disease affects more women than men and is found in people of all ages. Most cases of Lyme disease have positive outcomes when treated with antibiotics.
Chronic fatigue syndrome, which often accompanies Lyme disease, is a multisystem condition that affects more than two million Americans and is often difficult to diagnose (10). Many healthcare providers do not receive adequate teaching about the syndrome while in school, and thus are not able to effectively diagnose and treat the condition (10). Additionally, many healthcare providers erroneously perceive chronic fatigue syndrome to be a psychological disorder when in reality it is a biological condition with a pathogenesis that is not widely understood (10). To make the situation worse, the medical profession and CDC have been steadfast in denying that Lyme disease can turn chronic until recently (4).
Interestingly, the situation that swayed the CDC’s standing was COVID. Patients with the virus began experiencing long-term symptoms which the medical community called “long COVID.” Two of these long-term symptoms were fatigue and cognitive dysfunction, which are also found in patients with Lyme disease and chronic fatigue syndrome.
The CDC surveyed in 2022 and found that 18 million Americans suffered from long COVID symptoms. These findings prompted the National Academy of Science, Engineering, and Medicine (NASEM) to explore the hypothesis of “infection-associated chronic illness” in June 2023 (4).
Today, the CDC recognizes the following disease agents as being linked to chronic symptoms, including fatigue (4):
- Borrelia burgdorferi (Lyme disease)
- Coxiella burnetti (Q fever)
- Campylobacter
- Chikungunya virus
- Dengue virus
- Ebola virus
- Epstein Barr virus
- Enterovirus
- Poliovirus
- Covid-19 (SARS-CoV-2)
- West Nile Virus
The term “Post Treatment Lyme Disease Syndrome (PTLDS)” is now used to describe the lingering symptoms of fatigue, myalgia, and cognitive disturbances that do not resolve after treatment of Lyme disease with antibiotics (7).

Self Quiz
Ask yourself...
- How prevalent is Lyme disease in the United States and globally?
- Where in the United States are most cases of Lyme disease diagnosed?
- Why has chronic fatigue syndrome been a challenge to diagnose in patients?
- Which situation caused the CDC to reconsider the link between Lyme disease and chronic fatigue syndrome?
Pathophysiology
Lyme disease is caused by the Borrelia burgdorferi bacterium and is transmitted to humans through the bite of infected Ixodes scapularis black-legged ticks. The most common pathology of the disease is the erythema migrans rash that occurs in 70% to 80% of infected persons and appears anywhere on the body. Migrans rash occurs one to two weeks after tick exposure in an endemic area, but it can also be accompanied by tinea and nummular eczema.
The image below is Black-legged tick (Ixodes scapularis):

(1)
The image below is an erythema migrans rash in Lyme disease.

(1)
If left untreated, Lyme disease can cause arthritis in 30% of cases, neurological symptoms in 15% of patients, and cardiac complications in 2% of individuals (1, 11).
Lyme disease is divided into three stages: early localized, early disseminated, and late. The first two stages are signifiers of early infection, and the third stage indicates chronic disease.
Stage 1: Occurs 1 to 28 days following tick bite and includes low-grade fever, myalgia, neck stiffness, headache, and erythema migrans. Erythema migrans may burn, itch, or be warm to the touch, and it spreads gradually with the ability to exceed 12 inches in length. The rash may have the appearance of concentric circles that resemble a target with a bull’s eye, and if left untreated, it will persist for two to three weeks. Roughly 20% of patients experience a recurrent rash while 30% with the initial rash will have no further progression of symptoms (11).
Stage 2: Exists 3 to 12 weeks after tick bite and can last 12 to 20 weeks. This stage includes malaise, fever, dizziness, headache, muscle pain, angina, heart palpitations, dyspnea, diplopia, keratitis, and eye pain. Additional complications can include joint pain (knee, ankle, wrist), encephalopathy, meningitis, cranial nerve neuropathy, and Bell palsy. Encephalopathy symptoms are changes in personality, memory loss, and deficits in cognition, especially concentration. The patient can also experience extreme irritability and depression (11).
Stage 3: This stage can include aseptic meningitis, Bell palsy, arthritis, dysesthesia, radicular pain, and cognitive deficits and can occur as late as many months or years after initial infection. The symptoms are noted to mimic fibromyalgia at this stage. In older women, acrodermatitis chronica atrophicans can appear on the dorsum of the hands and feet. Arrhythmias and heart block can also be present (11).
Chronic fatigue syndrome, also called myalgic encephalomyelitis, causes chronic symptoms of fatigue and malaise that interfere with the patient’s activities of daily living for six months or more. Symptoms can include severe fatigue, cognitive dysfunction, sleep disturbances, autonomic dysfunction, and post-exertional malaise. Chronic fatigue syndrome is now recognized as being a primary set of symptoms that accompany Lyme disease that leads to longer-term post-treatment Lyme disease syndrome (PTLDS) (4). However, the term PTLDS is also used to describe symptoms in patients who do not have diagnostic or clinical evidence of infection with Borrelia burgdorferi (7).
The leading contributors of chronic fatigue syndrome are (10):
- Immune system alterations: Natural killer (NK) cells, interleukins, and T-cell alterations are responsible for the ongoing inflammation and malaise symptoms of chronic fatigue syndrome. The pro-inflammatory state is marked by the activation of glial cells and glial toxins produced by bacteria. Lower levels of immunoglobulins IgG1 and IgG3, and increased levels of IgA and IgM, indicate chronic fatigue syndrome. Autoantibodies against certain neurotransmitters and neurons lead to disrupted sleep patterns and altered cognition associated with chronic fatigue syndrome.
- Increased oxidative stress: An increase in oxidative stress biomarkers like oxidized low-density lipoproteins (LDL) and certain prostaglandins, and an accompanying decrease in antioxidants like glutathione, can lead to chronic fatigue syndrome. The oxidative stress transforms proteins and fatty acids into immunogenic targets. Free radicals damage the electron transport chain, impairing mitochondria and cellular energy production.
- Neuroendocrine system alterations: Excess levels of serotonin and its metabolites in the central nervous system led to decreased motor activity and excessive fatigue. Low cortisol levels due to a malfunctioning hypothalamic-pituitary axis decrease the cortisol awakening response that causes post-exertional malaise in patients with chronic fatigue syndrome.
Additionally, epigenetic modification of deoxyribonucleic acid (DNA) methylation has been shown to lead to the development of chronic fatigue syndrome (10).
It is not clear why some patients experience post-treatment Lyme disease syndrome and others do not. However, the Borrelia burgdorferi bacterium can trigger an autoimmune response that causes symptoms to last well after treatment of the infection.

Self Quiz
Ask yourself...
- Which bacterium causes Lyme disease?
- What occurs in each of the three stages of Lyme disease?
- How long must symptoms persist for the patient to be considered to have chronic fatigue syndrome?
- What are the cellular changes associated with chronic fatigue syndrome in the immune system, neuroendocrine system, and oxidative changes?
Risk Factors
The individuals who are at the highest risk for Lyme disease are those who spend time outdoors in regions where the Ixodes scapularis black-legged tick is common. These can include hikers and other outdoor recreational enthusiasts, hunters, and individuals who have outdoor occupations. Living in wooded or grassy areas and rural communities can increase risk. Being an owner of pets who spends time outdoors can also be a risk factor.
There are no reported cases of Lyme disease transmission from person to person or animal to person. The condition cannot be transmitted sexually, by kissing, or by drinking out of the same glass as someone who has Lyme disease (1).
Chronic fatigue syndrome is higher in individuals aged 40 to 70, and it affects Caucasian women more than men and women of other races. It also affects individuals from lower-income environments than those who come from higher-income and higher-educated cohorts. This indicates that stress can be a major catalyst for the condition (10).


Self Quiz
Ask yourself...
- Which individuals are at the highest risk for Lyme disease?
- Is sexual transmission a concern regarding Lyme disease? Why or why not?
- Which population is most affected by chronic fatigue syndrome?
- Which factor is believed to be a major catalyst for chronic fatigue syndrome?
Signs and Symptoms
Most symptoms of Lyme disease occur within three to 30 days (the average is seven days) after a tick bite (1).
Lyme disease signs and symptoms include (1, 11):
- Fever
- Fatigue
- Arthritis
- Dyspnea
- Dizziness
- Heart block
- Neuropathy
- Encephalitis
- Lymphedema
- Radiculopathy
- Myopericarditis
- Erythema migrans
- Visual disturbances
- Musculoskeletal pain
- Lymphocytic meningitis
- Facial nerve palsy (cranial nerve-VII)
- Headache and neck stiffness
Arthritis occurs in the larger joints, particularly the knees, and can surface months after the tick bite. Muscle, bone, and nerve pain, especially shooting nerve pain and numbness and tingling in the hands and feet can be present (1, 11).
Nurses need to understand that a bite from a tick that does not carry Lyme disease leaves a blemish that resembles a mosquito bite (small, red bump). This goes away in one to two days and is not a sign of Lyme disease. In Southern tick-associated rash illness (STARI), the rash is like erythema migrans, but it is not indicative of Lyme disease. Ticks carry other organisms in addition to Lyme disease, which can cause various types of rashes (1).
The signs and symptoms associated with chronic fatigue syndrome are (2, 10):
- Fatigue that is worsened by exertion and low upright posture that cannot be relieved by rest.
- Malaise and post-exertional malaise follow regular activities of daily living that take a day or more from which to recover.
- Chronic headaches, dizziness, photophobia
- Myalgias, particularly of the joints
- Disturbed sleep patterns that lead to daytime hypersomnolence and nighttime insomnia
- Cognitive decline is marked by slow mental processing speed, impaired learning abilities, memory decline, decreased attention, impaired multitasking abilities, and poor learning ability.
- Sore throat
- Nausea, vomiting
- Night sweats, chills
- Lymphadenopathy
- Intolerance, sensitivities, or allergies to alcohol, medications, foods, odors, and chemicals
- Anxiety, depression, panic attacks, and impaired social functioning
Roughly 20% of individuals who have chronic fatigue syndrome also have an underlying undiagnosed depressive illness (10). Most patients with chronic fatigue syndrome experience relationship challenges and the inability to maintain education or employment responsibilities.
Several tools can be used to determine the presence and severity of the signs and symptoms of post-treatment Lyme disease syndrome, including fatigue, pain, sleep quality, and depression. These tools are the Fatigue Severity Scale (FSS), Short-Form McGill Pain Questionnaire (SF-MPQ), Pittsburgh Sleep Quality Index (PSQI), and Beck Depression Inventory-II (BDI) (9).

Self Quiz
Ask yourself...
- When do the signs and symptoms of Lyme disease occur?
- What are the signs and symptoms of Lyme disease?
- What are the signs and symptoms of chronic fatigue syndrome?
- What other challenges can patients with chronic fatigue syndrome experience?
Prevention
An interdisciplinary approach is most effective for Lyme disease prevention and can include infectious disease, dermatology, and neurology healthcare team members (11).
Individuals should be taught to take the following measures when hiking or working outdoors (1, 11):
- Remove underbrush to reduce tick habitat.
- Apply pesticides to the environment to reduce tick burden.
- Wear long sleeves, long pants, socks, and closed-in shoes.
- Wear insect repellant.
- Remove ticks from the human host promptly and properly.
- Monitor pets for tick exposure and remove ticks promptly and properly.
There is a vaccine available for Lyme disease, but the effects have not proven to be reliable or long-lasting and therefore, it is not a sound measure of prevention (11).
The same preventative measures for Lyme disease apply to post-treatment Lyme disease syndrome and chronic fatigue syndrome. The most crucial factor is for patients to develop rapport with a trusted healthcare provider who can provide care and guidance. Since there is no quick cure for post-treatment Lyme disease syndrome and chronic fatigue syndrome, patients may benefit from the support of mental health providers, community resources, and friends and family (10).

Self Quiz
Ask yourself...
- How can individuals reduce tick habitats and tick burden?
- What attire should individuals wear to prevent tick exposure?
- What Lyme disease prevention measures should be taken regarding pets?
- What measures can patients experiencing chronic fatigue syndrome and post-treatment Lyme disease syndrome take to improve their circumstances?
Diagnostics and Treatment
Lyme disease is diagnosed based on patient symptoms, assessment findings, and the patient’s potential exposure to infected ticks. Early recognition of symptoms, diagnosis, and treatment are critical in preventing late Lyme disease (1). Since serological testing can be insensitive during the first few weeks of infection, patients may be treated based on clinical symptoms (11).
Most Lyme disease tests measure antibodies made by the body in response to infection, but antibodies can take several weeks to develop, so patients may test negative if recently infected. Antibodies persist in the blood for months and years after the infection is gone, so they are not a reliable resource for detecting the patient’s cure rate. Additionally, false positive test results occur in the presence of other diseases besides Lyme disease, which can make the tests unreliable (1).
The past recommendation for diagnosis was to implement a sensitive enzyme immunoassay (EIA) or immunofluorescence assay, followed by a western immunoblot assay for specimens yielding positive or equivocal results. The current recommendation uses a second EIA in place of the western immunoblot assay, the screening tests for serum antibodies to Borrelia burgdorferi (6). Serological diagnosis is greater than 80% for patients who experience neurologic or cardiac manifestations (11).
If a biopsy of erythema migrans is conducted, findings can include cellular infiltration of histiocytes, lymphocytes, and plasma cells, as well as eosinophilic infiltrates and spirochetes. Cerebral spinal fluid analysis is not necessary to diagnose Lyme meningitis, but it can be used to detect potential alternative causes of illness, such as bacterial meningitis. Joint aspiration is only performed if septic arthritis is suspected (11).
Bloodwork can reveal an elevated erythrocyte sedimentation rate (ESR), leukopenia, and thrombocytopenia (11). An electrocardiogram (ECG) can detect atrioventricular block and brain imaging can show abnormalities in 20% of patients with central nervous symptoms, such as punctate lesions of the periventricular white matter (11).
The main treatment for erythema migrans in Lyme disease is the use of antibiotics, and those individuals who utilize the treatment in the early stages of the disease can prevent long-term symptoms. The patient’s age, medical history, current health conditions, pregnancy status, and allergies should be considered before administering antibiotics to patients (1, 11).
The most common antibiotics used to treat erythema migrans and Lyme carditis are (1):
- Doxycycline: 100 milligrams one time per day orally for 10-14 days
- Amoxicillin: 500 milligrams three times per day orally for 14 days
- Cefuroxime: 500 milligrams twice per day orally for 14 days. In cases of severe heart block, two grams of cefuroxime are given intravenously once a day for 14 to 21 days.
Doxycycline 100 milligrams taken twice per day orally is used to treat the neurological symptoms associated with Lyme disease. Lyme meningitis is treated with 200 milligrams of doxycycline per day orally, divided into one or two doses. Ceftriaxone two grams administered once per day intravenously can also be used in severe cases (1).
Lyme arthritis is treated with antibiotics for four weeks and a second course may be needed after the initial treatment. If the patient continues to experience symptoms after two courses of antibiotics, they should be referred to a rheumatologist. If antibiotics are not initiated early on, permanent joint damage can occur. The most common treatment includes (1):
- Doxycycline: 100 milligrams twice per day orally for 28 days
- Amoxicillin: 500 milligrams three times per day orally for 28 days
- Cefuroxime: 500 milligrams twice per day orally for 28 days. In severe cases, two grams of cefuroxime are given intravenously once a day for 14 to 28 days.
The Jarisch-Herxheimer reaction, a cytokine-mediated reaction to the antibiotic destruction of spirochetes, occurs in 5% to 15% of patients and resolves within one day (11).
Individuals with Lyme carditis should be observed until the risk of heart block subsides. For individuals who cannot close one or both eyes due to facial paralysis, an eye patch can be worn, and eye drops are used to prevent irritation. Topical steroids can also be used for ocular pain (1, 11). Treatment is typically curative with 5% of patients experiencing lingering symptoms of myalgia and fatigue for six months or more (11).
The diagnosis of chronic fatigue syndrome is based on clinical findings with the main focus centering on the patient’s fatigue. The fatigue should have a definite beginning, be severe and disabling, and affect the patient’s psychological and physical functioning. The symptoms should be present for at least six months and affect the patient more than 50% of the time. Myalgias, sleep disturbances, and mood changes may also be present. Exclusionary diagnostic criteria are schizophrenia, mania, depression, disordered eating, substance abuse, and organic brain pathology (10).
In 2015, the Institute of Medicine (IOM) released diagnostic criteria for chronic fatigue syndrome.
Three symptoms and at least two additional manifestations are required for diagnosis. The three required symptoms are (2):
- A substantial reduction or impairment in the ability to engage in pre-illness levels of activity (occupational, educational, social, or personal life) that:
- It lasts for more than 6 months.
- Is accompanied by fatigue that is:
- Often profound
- Of new onset (not life-long)
- Not the result of ongoing or unusual excessive exertion
- Not substantially alleviated by rest
- Post-exertional malaise (PEM)—worsening of symptoms after physical, mental, or emotional exertion that would not have caused a problem before the illness. PEM often puts the patient in relapse which may last days, weeks, or even longer. For some patients, sensory overload (light and sound) can induce PEM. The symptoms typically get worse 12 to 48 hours after the activity or exposure and can last for days or even weeks.
- Unrefreshing sleep—patients with chronic fatigue syndrome may not feel better or less tired even after a full night of sleep despite the absence of specific objective sleep alterations.
At least one of the following two additional manifestations must be present (2):
Cognitive impairment—patients have problems with thinking, memory, executive function, and information processing, as well as attention deficit and impaired psychomotor functions. All can be exacerbated by exertion, effort, prolonged upright posture, stress, or time pressure, and may have serious consequences on a patient’s ability to maintain a job or attend school full time.
Orthostatic intolerance—patients develop a worsening of symptoms upon assuming and maintaining an upright posture as measured by objective heart rate and blood pressure abnormalities during standing, bedside orthostatic vital signs, or head-up tilt testing. Orthostatic symptoms including lightheadedness, fainting, increased fatigue, cognitive worsening, headaches, or nausea are worsened with quiet upright posture (either standing or sitting) during day-to-day life and are improved (though not necessarily fully resolved) with lying down. Orthostatic intolerance is often the most bothersome manifestation of chronic fatigue syndrome among adolescents.
The treatment for chronic fatigue syndrome includes both pharmacological and non-pharmacological approaches.
The pharmacological treatments for chronic fatigue syndrome include (10):
- Pain medications: Non-steroidal anti-inflammatory drugs (NSAIDS), including COX-2 inhibitors, can decrease symptoms of pain and inflammation. Opioid medications are avoided due to their addictive properties.
- Tricyclic antidepressants: These medications can improve sleep, pain, and fatigue severity. The dosages used are typically lower than the ones used to treat depression.
- Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs): These medications do not treat the underlying pathophysiology of chronic fatigue syndrome, but they can help reduce the symptoms of anxiety and depression that many patients with chronic diseases experience. SSRIs like fluoxetine, sertraline, and paroxetine can treat psychological symptoms whereas SRNIs can provide neuropathic pain relief in addition to treating anxiety and depression.
- Other medications: Antivirals like acyclovir, valacyclovir, and ganciclovir have been used in conjunction with interferons, but the evidence is inconclusive regarding their benefit. Immunoglobulins and corticosteroids have not been shown to be effective in treating the symptoms of chronic fatigue syndrome.
- Complementary medications: Fatty acids, magnesium, acetyl-1-carnitine, vitamin B12, and antioxidants have been shown to have partial benefit.
Newer treatments like rintatolimod and rituximab have not been shown to have much effectiveness in the treatment of chronic fatigue syndrome (10). However, alterations in gastrointestinal microbiota accompany chronic fatigue syndrome and are believed to be one of the etiologies for the condition. Fecal microbiota transplantation occurs when feces from a healthy donor are transferred to a patient’s gut, and this approach is showing promising results (10).
Non-pharmacological treatments for chronic fatigue syndrome are deep breathing techniques, muscle relaxation, massage, yoga, and tai chi. Cognitive behavioral therapy (CBT) has been shown to improve mood, fatigue, and post-exertional malaise. Graded exercise therapy (GET) is a supervised, gradual increase in the duration and intensity of physical activity, which encourages participants to gradually increase their physical activity until they reach the goal of 30 minutes of light exercise five days a week. Adaptive pacing therapy (APT) teaches the patient how to balance activity and rest sessions to avoid flare-ups (10).


Self Quiz
Ask yourself...
- Why do some individuals test negative for Lyme disease when they have the condition?
- Why are antibodies not a reliable predictor for the patient’s cure rate of Lyme disease?
- Which pharmacological treatments are effective in managing chronic fatigue syndrome?
- Which non-pharmacological treatments are effective in managing chronic fatigue syndrome?
Complications and Long-Term Effects
Lyme carditis occurs when the Borrelia burgdorferi bacteria enters the cardiac tissue and causes arrhythmias and heart block. This complication is present in one out of every 100 individuals with Lyme disease reported to the CDC (1). Symptoms include syncope, vertigo, dyspnea, heart palpitations, and angina. Treatment includes antibiotics and possible pacemakers, and antibiotics should be started immediately without waiting for Lyme disease test results. Patients typically recover in one to six weeks even though 11 patients globally died from Lyme carditis between the years 1985 and 2019 (1).
Lyme carditis requires immediate hospitalization and continued monitoring. Nurses should ask their patients with suspected or diagnosed Lyme disease about cardiac symptoms, such as angina, dyspnea, and vertigo. If patients present with cardiac symptoms for unknown reasons, the nurse should ask about possible exposure to ticks.
Lyme arthritis occurs when the Borrelia burgdorferi bacteria enters the joint tissue and causes inflammation. If the condition is left untreated, permanent damage to the joints can occur. One out of four patients with Lyme disease reports Lyme arthritis to the CDC (1). The knees are affected most often followed by the shoulder, ankle, elbow, jaw, wrist, and hip. Symptoms include warmth to the touch and pain during movement and can move between joints in an exacerbation and remission cycle (1).
Other complications include rheumatoid arthritis, acute memory disorders, ankylosing spondylitis, atrioventricular nodal block, cellulitis, contact dermatitis, gout and pseudogout, granuloma annulare, and prion-related diseases. Long-term Lyme disease triggers an autoimmune response that causes symptoms long after the infection is gone from the body, resulting in post-treatment Lyme disease syndrome. Long-term antibiotics in the treatment of this condition have not been found to improve outcomes (1, 5, 11).
Complications of chronic fatigue syndrome and post-treatment Lyme disease syndrome are anxiety and depression. The unpredictability of experiencing good days and bad days can lead to feelings of stress and hopelessness in these individuals (10).
Patients with post-treatment Lyme disease syndrome suffer a worse quality of life than patients with other chronic conditions, including heart failure, diabetes, multiple sclerosis, and arthritis with over 70% of patients with post-treatment Lyme disease syndrome reporting fair or poor health (5). Over 40% of patients with post-treatment Lyme disease syndrome reported that they are unable to work and 24% of patients admit to receiving disability assistance at some point during their illness (5).
Quality of Life in Patients with Chronic Illness (5):
| Population | Report Health Status as Good or Fair |
| Post-Treatment Lyme Disease Syndrome | 28% |
| Heart Failure | 38% |
| Fibromyalgia | 41% |
| Diabetes | 54% |
| Multiple Sclerosis | 63% |
| Depression | 68% |
| Asthma | 69% |
| General Population | 84% |


Self Quiz
Ask yourself...
- What causes Lyme carditis and what are the symptoms?
- What causes Lyme arthritis and what are the symptoms?
- What are the additional complications of Lyme disease?
- What are the long-term psychological complications of chronic fatigue syndrome and post-treatment Lyme disease syndrome?
Patient Education
All healthcare team members, but especially nurses, should educate patients about measures to prevent tick bites when outdoors and how to effectively remove ticks from the skin and pets. Signs and symptoms of cardiac, neurologic, and immune complications should also be taught, as well as when to seek medical assistance (11).
Patients who are prescribed antibiotics and other medications should be taught the administration, contraindications, and adverse effects. Non-pharmacological measures, such as preventing headache triggers, using over-the-counter medications for pain relief, and getting plenty of rest are also emphasized.
Individuals should also be taught the potential adverse effects of using insect repellants, such as DEET (11).
Most people with chronic fatigue syndrome are healthy before the diagnosis, which makes the decline in the patient’s health difficult to accept (10). These patients should be taught the importance of both pharmacological and nonpharmacological measures for controlling symptoms. Eating a balanced and nutrient-rich diet, drinking plenty of water, and getting fresh air and sunshine can provide health benefits.


Self Quiz
Ask yourself...
- Which factors are most important for nurses to teach patients with Lyme disease?
- Which non-pharmacological measures are important for patients with Lyme disease to understand?
- Why is a diagnosis of chronic fatigue syndrome difficult for patients to accept?
- What lifestyle measures can provide healthful benefits to patients with chronic fatigue syndrome?
Research Findings
Nootkatone is a naturally occurring compound found in grapefruit, Alaska yellow cedar trees, and some herbs, and it can repel and kill ticks. In 2020, the compound was registered with the Environmental Protection Agency (EPA) and is being used in commercial repellant products as of 2022.
Clothing treated with permethrin has been studied by the CDC and universities and is highly irritating to ticks, causing them to drop off and decrease their activity for 24 hours after contact with the chemical (1).
The CDC supports The Tick Project which determines whether neighborhood-based interventions of two tick control methods can reduce the prevalence of Lyme disease. Twenty-four neighborhoods with over 1,000 households are included in the research project (1).
Advanced molecular detection (AMD) methods that sequence the full genome of bacteria have identified Borrelia mayonii as a cause of Lyme disease in upper Midwestern states. The process also identified twelve tickborne species of bacteria, including two not previously associated with human illness (1).
The National Institute of Allergy and Infectious Disease (NIAID) funded three placebo-controlled clinical trials on the effectiveness of prolonged antibiotic therapy in post-treatment Lyme disease syndrome. The first study treated patients with 30 days of intravenous antibiotics followed by 60 days or oral antibiotics and did not find long-term antibiotic therapy effective. In the second study, some patients received 28 days of intravenous antibiotics and another group received a placebo. The study participants who received the antibiotics reported an improvement in fatigue over the placebo group; however, there were no improvements in cognitive function and several of the patients' experienced complications related to the antibiotics for which they were hospitalized. NIAID deduced that the evidence for long-term antibiotic use in post-treatment Lyme disease syndrome was not nonexistent (7).
In a third study conducted with the National Institute of Neurological Disorders and Stroke (NINDS), it was determined that long-term antibiotic use to manage the cognitive symptoms associated with post-treatment Lyme disease syndrome was not effective. Patients were administered intravenous ceftriaxone versus an intravenous placebo for 10 weeks. Adverse effects of ceftriaxone appeared in 26% of patients (7).
In another study conducted in the Netherlands in 2016, researchers concluded that the long-term treatment with antibiotics for post-treatment Lyme disease syndrome did not provide additional benefits compared with shorter-term therapies (7).
Several studies have found that Borrelia burgdorferi persists in mice and nonhuman primates after antibiotic therapy. Research is also emerging that indicates Borrelia burgdorferi can become resistant to medications (7).
Newer research indicates there is a link between gastrointestinal microbiome and chronic fatigue syndrome. Studies, where fecal samples were taken from geographically diverse subjects with chronic fatigue syndrome and those from healthy controls, found key differences in microbiome diversity, quantity, metabolic pathways, and interactions between the species of gut bacteria. This indicates that there is a significant rewiring of bacterial networks in chronic fatigue syndrome (7).
Patients with chronic fatigue syndrome had abnormally low levels of several bacteria compared to the control group, including Faecalibacterium prausnitzii and Eubacterium rectale. These bacteria promote gut health by producing the short-chain fatty acid butyrate. Butyrate is the primary energy source for cells that line the gut, and it supports the gut immune system by providing up to 70% of the cells’ energy requirements and protecting against gastrointestinal diseases. Faecalibacterium prausnitzii overabundance is also linked to fatigue severity in chronic fatigue syndrome. Other bacteria, Enterocloster bolteae and Ruminococcus gnavus, are increased in the presence of chronic fatigue syndrome and lead to inflammatory bowel disease (7).
Additional research shows that patients with long-term chronic fatigue syndrome have a more balanced microbiome but experience more severe clinical symptoms than other groups. Future study findings may inform diagnostic tests, disease classification, and treatments (7).

Self Quiz
Ask yourself...
- What is nootkatone and how is it being used in the fight against Lyme disease?
- Which substance is highly irritating to ticks and how does it affect ticks?
- What are the conclusive findings of the NIAID’s three clinical studies of the effectiveness of prolonged antibiotic therapy in post-treatment Lyme disease syndrome?
- How does the gut microbiome affect chronic fatigue syndrome?
Case Study
T.S. is a 45-year-old Caucasian woman who presents to the emergency outpatient clinic with extreme headache, photophobia, a pain rating of 10 out of 10 for neck stiffness, malaise, excessive fatigue, and a progressive rash on her back. T.S. states, “My head feels like it is going to explode, and my neck is killing me, but I’m so tired that I can’t seem to be able to figure out what to do to make it all better.”
The woman tells the nurse that she went hiking in the woods with her Labrador retriever roughly one week ago in early September while visiting Maine during which she sat on a towel in a clearing and enjoyed a picnic lunch. Upon returning home, she checked herself and her dog for ticks but did not see any. T.S. denies using any insect repellant prior to or after the hike; however, she states that her dog receives a monthly topical dose of flea medication that is also supposed to decrease the incidence of tick involvement.
The patient states that her back had started to itch shortly after the hike, but since she lives alone, she was unable to determine the root cause. She started taking over-the-counter ibuprofen for the headache and neck pain and diphenhydramine for the itching. She has stayed in bed in a dark bedroom due to photophobia and malaise and has not been able to drive, use electronics, or go to work. T.S. called a friend to bring her to the clinic, and this friend observed the rash on the patient’s back and took a photo to share with the patient. T.S. stated to her friend during the car ride to the clinic, “It looks like a red target with a darker bull’s eye. It looks like something bit me because I see a dark scab.”
T.S.’s pertinent past medical history includes seasonal allergies; perimenopausal symptoms of hot flashes, insomnia, and a 10-pound weight gain over the past 12 months; mild asthma; and tonsillectomy at age 10. Medications include over-the-counter antihistamines for allergies, progesterone for menopause symptoms, and a steroid inhaler for asthma symptoms.
T.S.’s family history is that both parents are deceased due to a motor vehicle accident at ages 65 and 68 when T.S. was 35 years old and a younger brother (age 40) with major depressive disorder. The brother is compliant with medication and psychotherapy regimens.
The patient’s assessment findings are temperature 102.5 degrees Fahrenheit, pulse 72 beats per minute, respirations 22 breaths per minute, and oxygen saturation 99% on room air. The bilateral lung sounds are clear to auscultation and the cardiovascular exam reveals a regular rate and rhythm without murmurs and capillary refill of the fingernails is brisk. Radial, pedal, and dorsal pedal pulses are normal bilaterally. Bowel sounds are heard in all four quadrants upon auscultation.
T.S. is oriented to date, place, and time, but she confirms that at times she seems to get a little confused, which is unlike her. The rash on T.S.’s back is red with a bull’s-eye appearance and measures 18 x 22 centimeters in diameter. The palpation of the major joints does not reveal redness or warmth, but T.S. states that her knees and elbows feel tender to the nurse’s touch. Palpation of the patient’s throat and clavicle reveals lymphadenopathy.
The nurse performs a skin assessment to rule out the rash appearing in another location other than T.S.’s back and to assess the skin for any additional evidence of insect bite marks. The findings are negative. Laboratory findings reveal white blood cell count, red blood cell count, hemoglobin, hematocrit, and platelet count all to be within normal ranges. The metabolic panel findings are also within the normal range.
The EIA test for Lyme disease is negative. The patient is prescribed amoxicillin 500 milligrams twice a day to be taken orally for 14 days. She can continue with over-the-counter ibuprofen and diphenhydramine for pain and itching, respectively. T.S. is also advised to eat a well-balanced diet, drink plenty of water, and allow time for rest between activities.
After five days of rest at home, T.S. begins to feel slightly better and returns to work. However, after several weeks, she notices that upon returning home from work each evening, she still goes straight to bed and sleeps all night, waking feeling fatigued and not refreshed. She also continues to experience intermittent headaches, malaise, and some residual neck stiffness and photophobia.
T.S. also notes new symptoms of chronic knee pain, diplopia, dyspnea upon exertion, and tingling in her feet. She calls the nurse at the clinic and receives another amoxicillin prescription 500 milligrams twice a day to be taken orally for 14 days, as well as gabapentin 900 milligrams each evening before bed. The patient is advised to return to the clinic for a follow-up appointment.
During the follow-up appointment, which occurs six weeks after the date of T.S.’s hike, a second EIA test is performed, which shows antibodies positive for the Borrelia burgdorferi bacterium. The rash on T.S.’s back is biopsied and is negative for spirochetes.
T.S. is compliant with her therapy, but a couple of months after her last visit to the clinic, she still experiences symptoms with new ones appearing. Now growing increasingly concerned, she visits her primary care physician who refers her to an infectious disease specialist.
It takes six weeks for T.S. to get an appointment with the specialist. Once at that appointment, she tells the physician, “I have not felt good for six months now. Although some of my symptoms improve at times, they don’t completely go away. My rash is much better, but now I’m experiencing things that are scaring me, like sensitivity to sound, paralysis on the right side of my face, and shortness of breath when doing normal things like laundry. I just don’t understand this. I used to be an avid hiker and now I’m so tired and sick that I can barely fix a bowl of cereal. I’ve had to hire a dog walker because I can no longer walk my dog. What is happening to me? Am I dying?”
T.S. continues to be treated by the infectious disease specialist, but she is also referred to as a rheumatologist for the increasing knee pain and a neurologist for the headaches, photophobia, sound sensitivity, and facial palsy. Several months after visiting with the specialists, T.S.’s symptoms now include those consistent with chronic fatigue syndrome, and she is required to use a cane when walking.

Self Quiz
Ask yourself...
- Why does T.S.’s activity and the location of the activity that she engaged in during early September put her at risk for Lyme disease?
- Which of T.S.’s symptoms are indicative of Lyme disease?
- Does anything in T.S.’s family history increase her risk of Lyme disease? If so, why?
- Which of T.S.’s assessment findings are indicative of Lyme disease?
- Is it unusual for T.S.’s laboratory blood test results to be normal? Why or why not?
- Is it unusual that T.S.’s first EIA test results are negative? Why or why not?
- Which of T.S.’s symptoms are congruent with chronic fatigue syndrome?
- Which stage of Lyme disease is T.S. experiencing when she returns to the clinic for her second visit?
- What explanation can be provided for why T.S.’s first EIA test was negative and the second was positive?
- Which interdisciplinary team member (that is not mentioned in the case study) could T.S. benefit from a referral to?
Conclusion
Most individuals with Lyme disease can expect a full recovery with no residual effects. Only a few patients may develop recurrent infection and even fewer patients can experience serious cardiac, neurological, and immune complications. However, when patients do develop the more serious symptoms associated with post-treatment Lyme disease syndrome, this can be debilitating and lead to relationship stress, school and job disruption, and mental health challenges, such as anxiety and depression.
Research has found that long-term treatment with antibiotics is not effective in the treatment of Lyme disease, but there is a correlation between gut microbiome and some of the symptoms associated with Lyme disease, such as chronic fatigue.

Self Quiz
Ask yourself...
- What time of year is Lyme disease most commonly diagnosed?
- Which gender and race are most affected by Lyme disease?
- How prevalent is the erythema migrans rash?
- Which agents do the CDC recognize as being linked to chronic symptoms?
- In which stage of Lyme disease are cardiac symptoms most prevalent?
- In which stage of Lyme disease do the symptoms mimic those of fibromyalgia?
- Where does Lyme disease arthritis typically occur?
- Which assessment tools help in determining the signs and symptoms of post-treatment Lyme disease syndrome?
- What are the past and current diagnostic recommendations for Lyme disease?
- What are the histological findings of erythema migrans?
- Which bloodwork findings are associated with Lyme disease?
- What is the Jarisch-Herxheimer reaction and how prevalent is it?
- Which are the most common antibiotics used in Lyme disease treatment and what are the recommended lengths of treatment for erythema migrans, neurological symptoms, and Lyme arthritis?
- What is the IOM’s diagnostic criteria for chronic fatigue syndrome?
- What are the differences between graded exercise therapy (GET) and adaptive pacing therapy (APT)?
- What are the additional complications of Lyme disease in addition to Lyme carditis and Lyme arthritis?
- What is post-treatment Lyme disease syndrome and what is the treatment?
- How do patients with post-treatment Lyme disease syndrome compare with patients of other chronic illnesses in regard to quality of life?
- Which bacteria promote gut health by producing the short chain fatty acid butyrate?
- Which bacteria overabundance is linked to fatigue severity in chronic fatigue syndrome?
Respiratory Failure in Chronic COPD
Case Scenario:
BW is a 62-year-old white male seen in the Primary Physician’s office for shortness of breath on exertion, fatigue, and dizziness for the past month. He has been smoking 2 packs per day for 20 years. He works in an auto assembly plant in Kentucky and has hypertension. His vital signs are 148/90, pulse 88, respirations 22, tympanic temperature 98.8, and Sp02 93. He has been on Lisinopril 10 mg tab once daily.
Upon inspection, he is short of breath just walking into the clinic and smells of cigarette smoke. Upon physical exam, his heart sounds are audible without murmurs or dependent edema in his legs. He does have congested and tight lung sounds bilaterally with expiratory crackles. He admits to smoking 2 packs of cigarettes daily. With his smoking history and current clinical symptoms, what is the suspected diagnosis?
As a health care professional, what would you do first? Is this a medical emergency? What diagnostic tests should be completed? What is the probable diagnosis? What were the patient’s risk factors? How common is this? The scenario is unfortunately all too common for people with chronic obstructive pulmonary disease.
Definitions
Chronic Obstructive Pulmonary Disease (COPD) is a chronic and irreversible respiratory disease characterized by airway obstruction or restriction. It is the fourth leading cause of death (1,3). Correct diagnosis and management are important for quality of life and prevention of early death for approximately 16 million patients with COPD in the U.S. and over 65 million worldwide (2, 24).
According to the Centers for Disease Control, more than 143,000 adults die annually from COPD in the U.S. (3). COPD is not contagious or curable, but rather a group of progressive lung diseases characterized by obstructed airflow.
Types of COPD
COPD is characterized by inflammation of the airways and severe air flow restriction both in and out of the lungs. COPD is an umbrella term that includes chronic bronchitis, emphysema, asthma, and COPD. Some people may have combinations of COPD and emphysema or COPD and chronic bronchitis.
It is generally caused by long-term exposure to environmental irritants such as smoke, second-hand smoke, air pollution, fumes, and wood smoke. Although the overall term for each of these diseases is COPD, clinicians refer to COPD as a specific disease process, most seen among long-term cigarette smokers with chronic airway obstruction from inflammation. COPD can also be further described as obstructive or restrictive.
A key characteristic of any type of COPD is limited airflow, which results in hypoxia and carbon dioxide retention. The patient doesn’t have the full ability to exhale as alveoli loses elasticity resulting in poor exchange of oxygen and carbon dioxide. Because of the trapped air, the alveoli often develop air pockets, and the chest becomes expanded with the retention of carbon dioxide (4).
Emphysema is a type of COPD that shares the common clinical symptoms of shortness of breath and airway obstruction. Commonly seen in people with a long-term history of smoking, it is noted uniquely in the clinical presentation as a “pink puffer.” The term comes from the clinical appearance of patients with emphysema who have a pink flushed appearance from the lack of oxygen, poor cardiac output and increased work of breathing. The damage is deep within the lungs from overinflated alveoli where air has become trapped from the inability to exhale out the carbon dioxide.
Chronic smoking damages the flexibility of the alveoli making them stiff and ineffective. Instead of many small air sacs, they become stretched and floppy and less effective in moving oxygen into and out of the capillaries. Often because the work of breathing takes all their energy, they prefer to breathe rather than eat, so they experience weight loss and muscle wasting due to the lack of oxygen. Emphysema has also been called COPD Type A (5).
The prevalence of emphysema indicates that 90% of cases are seen in people over the age of 45 (6). Rates of diagnosis have also been increasing among women showing the similar trends of COPD now equalizing among women and men.
Chronic bronchitis is a type of COPD characterized by inflammation, airway irritation, and mucus buildup in the main bronchus. The clinical diagnosis is defined as a persistent cough that produces phlegm and mucus, for at least three months per year in two consecutive years (6). Symptoms include chronic cough trying to rid the airway of thick mucus and phlegm. There are two types of bronchitis acute and chronic. Acute bronchitis is generally caused by colds and flu. The temporary infection causes inflammation with irritation to the bronchus and bronchioles and results in coughing and shortness of breath.
Women have chronic bronchitis at twice the rate of men (3,7). Age increases the risk factor as people over age 65 have a rate of 64.2 per 1,000 persons compared to the age group of 18-44 the rate drops to 28 per 1,000 (6). Prevalence trends also reveal that non-Hispanic whites have a higher risk than African American blacks and Hispanics.
Chronic bronchitis is also characterized by cough; however, it does not go away with antibiotics or treatment as it is caused by smoking or other environmental pollutants such as dust, air pollution, or unsafe work environments of coal, asbestos, or irritants to delicate respiratory tissues. Although acute bronchitis can be “cured” with pharmacological interventions and time for healing, there is no cure for chronic bronchitis. Treatment is focused on relief from annoying cough symptoms and supporting the airway. Bronchodilators are the mainstay of therapy.
Asthma and COPD may result in the same airflow resistance. Still, as the cause of COPD is generally from smoking, asthma is from other respiratory irritants such as air pollution or environmental triggers like dust, mold, pet dander, and more. Asthma is a form of COPD characterized by spasms of the bronchi in the lungs and is an overreaction and spasm of the bronchial airways (8). Normally the bronchiole tubes can dilate and constrict depending on nervous system messages, however, in asthma the bronchus and bronchiole tubes constrict and overreact to environmental and even emotional triggers causing severe difficulty breathing and airflow.
Asthma is characterized by wheezing from restricted airflow, chest tightness, and increased mucus from the inflamed airways, which worsens the restriction and impedes airflow. Unlike emphysema, which is seen in older patients who have had years of smoking history, asthma is seen in people of all ages and often first manifests during childhood.
When asthma develops in younger children, it may often resolve independently as the child’s respiratory system grows and matures. Other children may continue to suffer from asthma for the rest of their lives and require maintenance medications to keep the airways open. There has been a correlation between asthma and eczema indicating an autoimmune response. Combinations of eczema (atopic dermatitis) and allergic rhinitis indicate a risk of developing other allergies and asthma as immunoglobulins (antibodies) respond to the allergen (8).
A natural body defense against high levels of immunoglobulins is closing the airways to prevent the invading pathogen from further entering the body. In the case of asthma, this natural defense mechanism becomes the problem as airways spasm and even threaten to close.
For many children with asthma, there is a genetic link to a deficiency of a protein in the skin, which normally helps strengthen the skin from pathogens and allergens. Without the protein, the skin is more irritated by environmental allergens and microbes and the body responds quickly with hives, eczema, and the resulting antibodies (8).
Asthma affects 25 million in the United States and is the most common chronic disease of childhood. As high as 95% of patients with asthma also suffer from chronic rhinitis (9).
Case Scenario:
In our earlier scenario, the diagnosis of COPD was determined.
- What symptoms did the patient present with and what were his risk factors?
- What were the triggers that caused COPD?
- What type of COPD does he have?

Self Quiz
Ask yourself...
- What conditions are included in the umbrella term chronic obstructive pulmonary disease (COPD)?
- Compare and contrast COPD with asthma and emphysema.
- How would you explain to a patient what COPD is?
Statistics About COPD
Chronic obstructive pulmonary disease is the third leading cause of death in the United States and is largely irreversible and fatal (3). It is projected that with the increasing prevalence of smoking in developing countries and the aging populations, the prevalence of COPD is expected to rise over the next 30 years. Prevalence indicates how many people currently have the disease and approximately 1 of every 13 Americans aged 18 years and older has COPD.
Data is collected annually from two major surveys including the National Health Interview Survey (NHIS) and the Behavioral Risk Factor Surveillance System (BRFSS). It is the third leading cause of death for people of most racial and ethnic groups in the United States (10). In the United States, COPD is most common among Caucasians and those with a history of smoking. COPD develops over time and is an obstructive or restrictive expiratory airway due to chronic bronchitis, emphysema, or asthma (9).
Approximately 26 million Americans have been diagnosed with COPD and many more yet undiagnosed. It is the third leading cause of death next to cardiovascular disease and cancer. It is seen more in men and women older than 40 years of age, often due to years of chronic smoking.
It is more common in men than women, but rates of COPD among women increase as women smoke. It is estimated from previous studies that 8% of the U.S. population adults have been told by a health-care provider that they have COPD (11, 12, 2).
The incidence and prevalence vary by state and worldwide statistics are unknown as more than 50% of people formally diagnosed with low pulmonary function were not even aware of the diagnosis (13, 14). According to the World Health Organization, approximately 65 million have some form of COPD, however much of the data on morbidity and mortality from COPD comes from first-world countries and is estimated to be approximately 5% of all deaths worldwide (5). In states with higher rates of smokers, there is a direct correlation to a higher incidence of COPD.
Morbidity and Mortality
Morbidity is the term for the cost and consequences of a disease. Illness from COPD has a large impact on the American health system. According to the CDC estimates, COPD costs our country approximately $50 billion annually in both direct and indirect health care (15).
The rates of COPD also correlate with states that have the highest smoking populations, which include the Southeast and Midwest states, such as Alabama and Kentucky. Because COPD is mostly caused by environmental pollutants, of which smoking is the number one cause, other environmental pollutants found in these states are industrial pollutants from factory workers and represent 31% of those who have never smoked (7). In developing countries or poor homes, such rates may also include cooking with fuel instead of electricity.
Female smokers are 13 times more likely to die from COPD than other female non-smokers and male smokers are 12 times more at risk to die from COPD than a counterpart non-smoking male (7). The cost of COPD for people over age 65 also has increased to almost $30 billion in direct healthcare costs and another $20 billion in direct mortality and morbidity costs.
The additional costs include loss of work and ability to function as 51% state their ability to function at work is limited and 70% claim it limits physical ability. Social and family activities are also limited as patients with COPD have difficulty walking, participating in leisure activities they once enjoyed and even performing activities of daily living on their own.
Case Scenario:
Our 62-year-old white male is given the diagnosis of COPD and asks the provider how he developed it, whether is there a cure, and what is his prognosis. The provider tells him that his 20-year history of smoking, which equals 40 pack years (20 years times 2 packs/day 40) is the main cause of his COPD. He has additional risk factors of being a white male and working with industrial pollutants in his job. Unfortunately, there is no cure for him, but he can receive treatment for the symptoms. His prognosis depends on his ability to stop smoking. The reality is that he has increased his morbidity by 12 times by choosing to smoke. The provider then offers him an explanation of the function of his lungs and the treatment options.

Self Quiz
Ask yourself...
- What is the incidence and prevalence of COPD in the US?
- How does COPD compare with worldwide statistics?
- What are the risk factors for COPD?
- What risk factors can contribute to the mortality and morbidity of COPD?
Physiology of Breathing
The internal pressure in the thoracic cavity is negative compared to the positive atmospheric air pressure. When the diaphragm contracts it opens the thoracic cavity allowing air to rush into the bronchioles and fill the alveoli. When the pressure within the lungs exceeds the external pressure by filling with air, the reverse occurs when the diaphragm relaxes, and the air is then pushed out of the bronchioles and lungs to exhale. However, COPD alters this effective function. Because the diaphragm does 80% of breathing, when the alveoli trap air, the diaphragm becomes flattened making complete contraction of the diaphragm ineffective in pulling the thoracic cavity open, which further reduces the airflow coming into the airway.
On the tissue of the bronchiole tubes, the two major receptors for the nervous system are the muscarinic and beta receptors. Muscarinic receptors cause smooth muscle contraction making the lumen of the bronchiole tube smaller. In contrast, the beta receptors will cause relaxation of the muscle causing bronchodilation.
Ideally, the goal for people with COPD is to increase beta receptor activity (dilation of airways) and inhibit muscarinic receptors. The two main classes of medications will act on either of the receptors to open the airways. Because people with COPD also have inflammation of the airways, the third major mechanism to change this vicious cycle of airway over-reactivity is with an anti-inflammatory, such as inhaled corticosteroids (4, 16).
COPD is caused by bronchoconstriction and inflammation making air passage in and out of the lungs more difficult. This reduction in effective airflow creates a state of hypoxia, resulting in hypoxemia. The obstruction can be caused by mucus or narrowing of the bronchus and bronchiole tree creating airway resistance.
Chronic bronchitis is a chronic productive cough lasting three months during two consecutive years. Emphysema is a permanent enlargement of the alveoli, which prevents normal elastic recoil during respiration. People with asthma develop an obstruction of the airway and airflow. Those with asthma who have a reversible airflow obstruction are not considered to have COPD, however, when the airflow remains chronically obstructed, which is not reversible, they are diagnosed with COPD (4, 16).
The lungs become scarred from chronic inflammation and continual irritation from mucus buildup as the lungs attempt to protect themselves from environmental irritants such as smoke. This cycle of irritation, inflammation, and attempts to recover continues until the compensation efforts create disruptive symptoms that often drive the patient to seek medical care. A productive cough with mucus is an effort of the lungs and trachea to rid itself of the irritant, however, the mucus soon becomes a problem, such as seen in chronic bronchitis, and often known as a “smoker’s cough.”
Effects of Smoking
Smoking, as the number one cause of COPD, destroys the fine hairs, or cilia, in the bronchiole tubes and trachea, which are supposed to push up foreign substances and pathogens from the lower airway up into the upper airway to be expelled by a cough. The additional pathology from smoking affects not only the lungs but also the circulatory system (9,17). Nicotine paralyzes the cilia and the tar within cigarettes or cigars further destroys their integrity.
Additionally, the chemicals in cigarette smoke create nicks within the fine endothelial lining of the arteries throughout the body allowing a “shelf” for cholesterol and fat to build up upon. Generally, the public is aware of cigarette smoking as the most common cause of lung cancer, however, most people are unaware of the damage to the circulatory system, which is also the most common cause of atherosclerosis, or narrowing of the arteries.
In addition, nicotine competes with oxygen further stimulating erythropoiesis, or formation of new red blood cells, which can often lead the blood to become thick and sticky. Atherosclerotic plaques narrow an artery and hinder blood flow. The result is the surface of a bulging atherosclerotic plaque sometimes tears, exposing material that stimulates clot formation. Clots and ruptured plaque material can then break away from the wall, be carried by the blood, and clog arteries downstream.
Atherosclerosis can damage tissues throughout the body:
- Blockages in the carotid arteries can reduce or block blood flow to the brain, causing a stroke.
- Obstructions in the peripheral arteries in the legs can cause claudication (pain when walking) gangrene and deep vein thrombosis (DVT).
- Resultant DVTs can travel to the lungs causing a pulmonary embolism and respiratory arrest.
- Atherosclerotic obstructions in the intestines cause ischemic bowel.
- In the coronary arteries, atherosclerotic obstructions cause heart attacks (17).
At the cellular level, DNA is disrupted by nicotine and tars from smoking, which leads to mutations in cellular replication that are out of control, known as cancer. One-third of all cancer deaths are caused by tobacco and smoking. In addition to disruptions in normal DNA creation of proteins, hormones are disrupted affecting lower estrogen and testosterone levels, thyroid problems, and reproduction issues.
Within the blood system itself, white blood cells and red blood cells stay elevated from smoking. High white blood cells indicate to your body they are in a state of infection, which continues the cycle of inflammation and attempts to repair. As formed elements in the blood (RBCs and WBCs) increase, nutrients, minerals, and precious oxygen decrease by sheer volume and availability to be transported by blood.
The image below illustrates a comparison of clear vs congested alveoli from smoking.
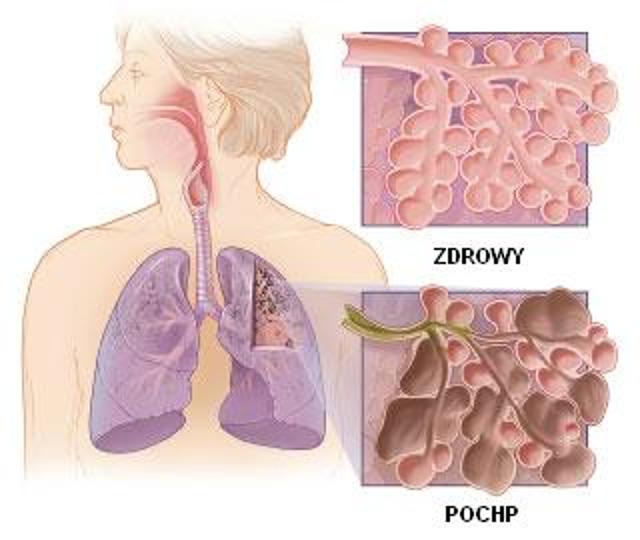
(34)
Case Scenario:
Mr. BW has discovered that the result of 20 years of smoking has compromised his lungs’ ability to inhale and exhale. Unfortunately, his symptoms of shortness of breath and persistent cough were his only indicators. The Provider will order additional diagnostic studies to confirm the diagnosis including spirometry, lab tests to establish a baseline, and a chest x-ray.

Self Quiz
Ask yourself...
- What is the pathology of COPD within the bronchioles?
- What is the pathology of COPD within the alveoli?
- How do the lungs attempt to compensate for congested alveoli?
- What are the results of lab work?
- What resources do you have to teach patients about the effects of smoking on their lungs?
- What other complications for the body does smoking cause?
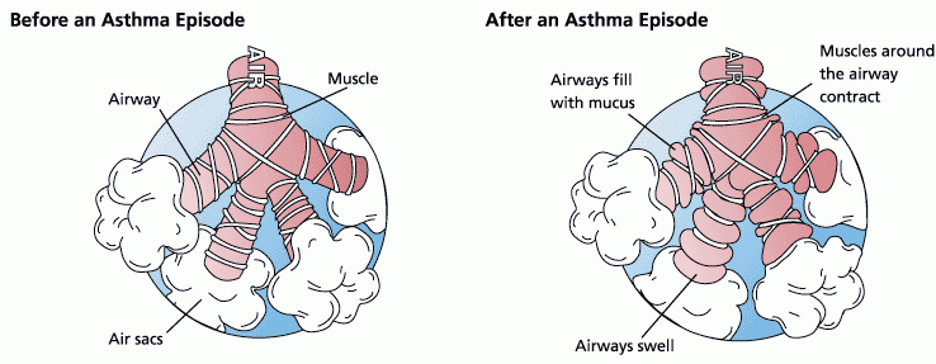
Risk Factors
A valid and costly concern for Health Maintenance Organizations and insurance companies is that numerous patients are hospitalized for acute exacerbations of their COPD, which could have been avoided by careful management by their primary physician.
A hospitalization from a COPD exacerbation can cost thousands of dollars. The national guidelines and the GOLD standard for COPD diagnosis and management were created from numerous clinical research and studies (18). The GOLD standard for COPD has been accepted as a national standard and adopted by HEDIS measures for insurance reimbursement and Center for Medicare Services (CMS).
By surveying and tracking reports of people with COPD across all states, improvements can be made in identifying communities at risk who may benefit from awareness, outreach and public health efforts in prevention, treatment, and control of the disease. Efforts to survey patients with COPD in all states have been made by the Centers for Disease Control using the Behavioral Risk Factor Surveillance System (BRFSS) (12).
Of those who self-identified as COPD, 76% stated they received a diagnostic breathing test, 64% felt the shortness of breath negatively impacted their quality of life, and 55% were taking at least one medication for their COPD (11). Because the spirometry test can be costly, it is not used as a general screening tool for COPD. Currently, there is no public screening tool in use due to cost.
Predisposing factors include environmental pollutants and also include secondhand smoke, genetic factors of Alpha 1-antitrypsin (AAT) deficiency, recurrent or chronic lower respiratory infections or disease, and age over the fifth decade of life.

Self Quiz
Ask yourself...
- Picture your patients who have COPD, emphysema, chronic bronchitis, and asthma.
- How are they the same? How are they different?
- What similarities in medications did they receive?
- What were the interventions applied for each?
Symptoms of COPD
Most symptoms of COPD are due to difficulty breathing and obstruction or restriction to airflow in and out of the lungs (28). Dizziness, fatigue, shortness of breath and even hypertension are all related to hypoxia, a lack of adequate oxygenation to body tissues. As in any condition, a thorough history must be taken to include symptoms and signs visible to the healthcare professional. It is said as much as 90% of diagnoses made can be determined by a good history.
A history of difficulty breathing or shortness of breath after exercise, and exposure to environmental triggers can help identify the development of asthma. Clinical symptoms include wheezing, recurrent cough (worse at night and early morning), recurrent shortness of breath, and chest tightness with moderate activity.
The classic symptom of COPD is shortness of breath. At first, there may be little to no symptoms with COPD, however, because it is a chronic and progressive disease of deteriorating lung capacity and airflow, the symptoms inevitably develop and worsen. Wheezing, shortness of breath, chest tightness, and cough are classic symptoms that also lead to weight loss, muscle loss, and difficulty with daily activities.
Early Symptoms
- Daily morning cough
- Shortness of breath- especially on exertion
- Wheezing
Moderate Symptoms
- Ongoing productive cough
- Chest tightness
- Fatigue
- Loss of appetite if breathing through the mouth
- Sputum- clear and colorless, may be frothy.
- Change in mental alertness.
- Weakness
Late-Stage Severe Symptoms
- Dizziness
- Pallor
- Cyanosis
- Chronic cough-throughout day (smoker’s cough)
- Waking up feeling suffocated
- Blue lips, skin, and nails
- Inability to lie down.
- Irritability and headaches
- Difficulty sleeping
A pneumonic to help you remember the symptoms of COPD is the acrostic “Lung Damage” which stands for:
L-Lack of energy
U-Unable to tolerate activity
N-Nutrition deficit
G-Gas abnormality (respiratory acidosis)
D- Dry or productive cough
A- Accessory muscle use and Abnormal lung sounds
M- Modification of skin color
A- Anterior/Posterior diameter increase
G- Gets in tripod breathing position
E- Extreme dyspnea
Quality: From mild to severe
The quality of shortness of breath varies from mild to severe. Mild is seen in the initial stages of COPD and is common upon exertion, which limits activities of daily living whereas severe shortness of breath and symptoms cause the work of breathing to occupy their entire thoughts and energy. Because asthma is classified in four ways, step 1: mild intermittent, step 2: mild persistent, step 3: moderate persistent, and step 4: severe persistent, the quality of cough and shortness of breath must be determined from mild to severe and quantified by how many days per week the patient is in distress breathing.
Triggers: Exercise
COPD can be triggered by allergies and pollutants. Determining the type of trigger is essential in asthma to teach prevention of acute exacerbations and better preparation.
Occurrence: Predictable or Unpredictable
The use of a home peak flow meter should be used to help identify the current condition of the lungs and airways. Acute exacerbations can be better diagnosed by identifying if the acute event was predictable, such as based on poor weather conditions and air quality, and exercise, or unpredictable without any known trigger (28).
Wheezing
- There are 741 causes of wheezing and COPD is only one cause.
- Identify the characteristics of wheezing.
- Identify the time of day and activities when wheezing starts and stops.
Chronic Cough
- How long have you had the cough?
- How do you describe the cough?
- Is it productive or dry?
- Is it only in the morning or throughout the day?
- When is the cough worse in the day?
- Is the cough related to meals?
- Environmental exposures
Sputum
- What color is the sputum?
- What is the consistency: clear, frothy, pink, thick, thin?
- When is sputum worse during the day?
Breathing Difficulties
- Do you have trouble breathing in or out or both?
- How fast are you breathing?
- Do you use oxygen?
Cyanosis
- What is blue: skin, nails, face, lips?
Irritability/Headache
- What is the nature of the headache?
- What makes the headache worse or better?

Self Quiz
Ask yourself...
- What are the classic clinical symptoms of asthma, chronic bronchitis, and emphysema?
- How are they alike?
- How are they different?
Diagnostic Tests for COPD and Respiratory Failure
Spirometry
Results of extensive quantitative research have concluded that the recommendation for diagnosis of COPD is the use of spirometry (18). The HEDIS measure assesses the percentage of adults over the age of 40 with a diagnosis of COPD who were diagnosed by spirometry. Although the HEDIS measure is to use spirometry for diagnosis, it continues to be underused (19).
Based on the Global Initiative for Chronic Obstructive Lung Disease (20), most patients with COPD have moderate to severe disease due to late or incorrect diagnosis, which increases the overall medical costs and number of exacerbations experienced by the patient. It has been suggested by organizations specializing in respiratory care that the use of spirometry for both diagnosis and management become standardized.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) is the executive summary for diagnosis and management of COPD (20). Ever since 1947, the ratio of vital capacity (FVC) to forced expiratory capacity in 1 second (FEV1) has been the scientific parameter physicians have used to measure lung health (21). The GOLD standard established in 2001 identified the FEV1/FVC < .70 “rule of thumb” to define airflow obstruction.
Other authorities however have proposed other ranges from <.75% by the American Thoracic Society to < 0.75-0.80 by the Global Initiative for Asthma in 2015 (22). These variations have been developed due to the variations among ethnic groups studied in research that determined the values. The differential diagnoses included COPD, asthma, heart failure, bronchiectasis, pulmonary edema, pneumonia, or cancer.
Correct completion of a spirometry test is essential for a valid diagnosis of COPD. Although there are variations with machines, the basic concept is to have the patient breathe deeply and then forcefully exhale for one full minute. The measurements are collected after three separate attempts, which measure the forced expiratory effort (FEV1) in one minute. Remember to identify gender, ethnicity, and height on the machine as each impacts total lung capacity, and the result is calculated based on these factors and performance. Less than 70% of FEV1 may indicate COPD.
Image. Depiction of Spirometry Testing to Diagnose COPD
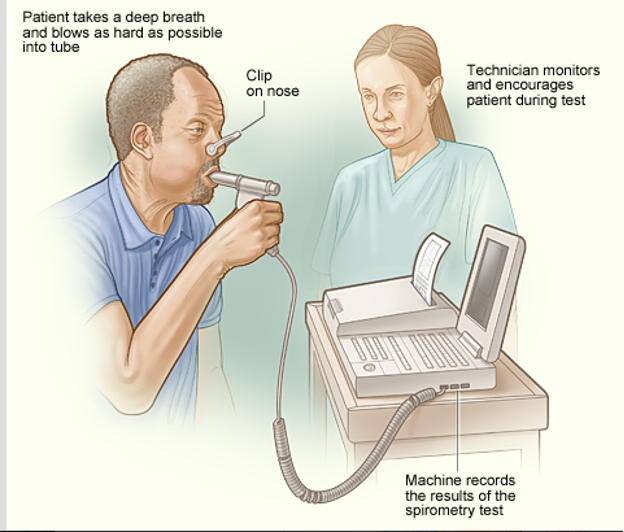
(34)
Classifying COPD
Because treatment for COPD is contingent upon spirometry results, the spirometry needed to be completed to determine the stage of damage to the lungs. The FEV1/FVC ratio for this patient came back to 60% which is below the 70% predicted value and diagnostic for Stage II COPD. A chest X-ray was also ordered to rule out any other diagnosis being considered. It came back negative. ABGs, an EKG, and an echocardiogram could have been completed but were not at this time.
Currently, COPD is classified based on severity by a post-bronchodilator FEV1 score from spirometry. The most recent recommendations also include consideration of both the spirometry results of the FEV1 and the patient’s symptoms to determine the class and severity of COPD. Spirometry confirms the diagnosis, and the pulmonary function test classifies the severity. According to the GOLD standards, which are reviewed annually, the current classes are as follows in the table below:
| STAGE | Symptoms | Post Bronchodilator FEV1 |
| 1 | Mild | >80% |
| 2 | Moderate | 50-80% |
| 3 | Severe | 30-50% |
| 4 | Very severe | < 30% |
Case Scenario:
The patient was tested with spirometry and given a prescription for a short-acting bronchodilator to be used as needed and a daily long-acting bronchodilator. He was encouraged to stop smoking and given smoking cessation resources and options including a group support class, and pharmaceuticals for nicotine replacement for a tapered withdrawal. The patient refused information about smoking cessation.
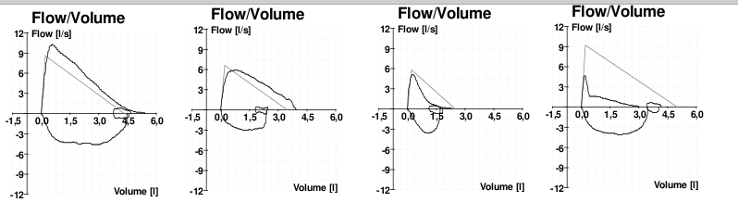
(35)
Medical Management and Treatment of COPD
Unfortunately, there is no cure for COPD. Any damage done to the airways and the lungs is not reversible. Although currently there is no medical cure available for lung tissue damage, adopting regular medical care and consistent lifestyle changes can help slow the progression of the disease.
The major goals of COPD treatment are:
- Relieve symptoms.
- Slow the progression of the disease.
- Improve exercise tolerance.
- Prevent and manage complications.
- Improve overall health.
The current GOLD Standards are established by numerous research studies and the CDC and include the following (20):
- The Global Initiative for Chronic Obstructive Lung Disease (GOLD) is the standard for diagnostic and treatment guidelines.
- General interventions are comfort measures based on the severity of the symptoms and causative factors.
- Smoking cessation should be mandatory as it is the number one causative factor. Smoking cessation should be discussed at every visit.
- The selection of inhalers depends on the age of the person.
- Nutrition management should be included as 25% of COPD patients are malnourished as eating competes with breathing so meals are limited. Encourage higher calorie supplements such as Ensure to deliver needed nutrients.
- Pharmacological therapy is based on spirometry and the stage of disease. For stage 1 short-acting bronchodilators (SABA) are prescribed as needed for shortness of breath. For stage II, a SABA plus a long-acting bronchodilator (LABA) should be prescribed. Stage III should have a SABA, LABA plus an inhaled glucocorticoid if the patient has frequent exacerbations. Stage IV patients need all given to a stage III plus cardiopulmonary rehabilitation and possibly 02 delivery. All patients should receive an annual flu vaccine, once pneumonia vaccine after age 65, and every 5-10 years for high-risk patients
(16)
Oxygen Use
Because the issue with COPD is decreased airflow, the main goal of therapy is to help the patient’s lungs provide sufficient oxygen to the body.
If the patient is short of breath, hypoxemia, or has obvious signs of heart failure, oxygen should be titrated to saturation levels >93% (4).
The concerns are oxygen toxicity and vasoconstriction. Oxygen causes constriction of the coronary, cerebral, renal, and other key vasculatures. If perfusion decreases with blood hyper-oxygenation, the administration of oxygen may place tissues at increased risk of hypoxia. Hyperoxia reduces coronary blood flow by 8% to 29% in normal individuals and in patients with coronary artery disease or chronic heart failure. Although oxygen supplementation is a modality used only in the end stages of COPD it is still a fundamental intervention.
Care must be taken when giving oxygen to patients with COPD as their drive for inhalation is based on carbon dioxide retention, which they become used to. If additional oxygen is given, it may decrease the drive to breathe and further complicate oxygenation.
Patient Education
Patients need to be taught about the possible cause and treatment plan, so they remain a member of the care plan team. Modification of triggers should be taught first if possible, such as smoking, alcohol, and caffeine cessation. Behavior lifestyle changes are ideal including weight loss. Patients should be taught that as a chronic disease, there is no cure.
Advance directives should be taught and put in place. Antibiotics should be given by prescription to fill upon worsening of symptoms after seeing their clinician, according to the GOLD standard. Patients should be taught to conserve their energy and plan for activity. Patients should be taught how to use a peak flow meter at home to measure their breathing ability and alert their provider if they reach the red target zone. They should be taught the COPD action plan, and how to use a home peak flow meter to detect airflow and to become active participants in their care (9,27).
Image. Peak Flow Meter for home use

(36)

Self Quiz
Ask yourself...
- Which tool is used for home use to determine general airflow through the lungs?
- What does pulmonary rehabilitation include?
- What are some general lifestyle recommendations for someone with COPD?
- What patient education can you provide about weight and nutrition for someone with chronic COPD?
Medications
Medications are used to manage all forms of COPD and be used as monotherapy, dual therapy, or multi-drug therapy per the GOLD Guidelines tier algorithm for COPD control and management (25).
The two main categories of medications that open the airways are the beta 2 bronchodilators, which can be remembered with the pneumonic “BAM” that include bronchodilators, anticholinergics such as ipratropium and methylxanthines that stimulate the bronchioles to open such as theophylline.
The second class of medications are the anti-inflammatories that can be remembered by the acronym “SLM,” which includes steroids, leukotrienes, and mast cell stabilizers.
|
Drug Class |
Action |
Brand Names |
|
Bronchodilators:
|
|
|
|
Beta 2 -Short acting (SABA) |
Dilate bronchi |
Albuterol (rescue inhaler) Salbutamol, Terbutaline |
|
Long-Acting Beta Agonists (LABAs) |
Act on Beta 2 receptors bronchodilator |
Advair, Serevent, Foradil, Oxis, Salmeterol, Formeterol |
|
Short Acting Beta Agonists (SABAs) |
Act on Beta 2 receptors to Broncho dilate |
Albuterol, Ventolin, Proventil, Spiriva |
|
Anticholinergics/ Antimuscarinics (LAMA) |
Increase sympathetic system to open airways |
Ipratropium, tiotropium |
|
Methylxanthines |
Beta 2 stimulation to open bronchioles |
Aminophyllin, Theophyllin, Unidur, Theodur |
|
Anti-inflammatories: |
|
|
|
Steroids (Inhaled Corticosteroids) |
Decrease inflammation in the lower airways |
Fluticasone, Advair, Flovent, Pulmicort, Symbicort, Asmanex, Alvesco, mometesone |
|
Steroid (Nasal) |
Decrease inflammation in the upper airways |
Nasonex, Nasacort, Veramyst |
|
Leukotriene Antagonists (LTRAs) |
Non-steroidal anti-inflammatory |
Singulair, Accolate |
|
Allergy Medications |
Antihistamine Anti IgE blockers |
Xolair, Claritin/Clarinex, Allegra, Zyrtec, |
|
Mast Cell Stabilizers |
Decrease release of histamine |
Cromolyn |
|
Phosphodiesterase-4 PDE-4 Inhibitors |
Suppress inflammation |
Roflumilast |
Remembering the physiology of the airways is largely controlled by two main nervous system receptors, the muscarinic and beta receptors, blocking the muscarinic or stimulating the beta receptors will increase the airways. Another way to remember the different kinds of medication used for COPD is to remember the drug name endings. The muscarinic antagonist drugs end in “ium” such as ipratropium, tiotropium, and umeclidinium.
Additionally, a new drug called glycopyrrolate is muscarinic so drugs that end in “ate” will remind you that the drug “ate” the effects of muscarinic receptors. All the respiratory beta-agonist drugs end in “ol” (similar to cardiac beta blockers ending in “ol”). Drugs such as formoterol, salmeterol, and albuterol are beta-agonists and increase the airway diameter. The inhaled corticosteroids end in “one” like fluticasone or mometasone.
A medication grid can help you remember the progression of adjunct medication for both COPD and asthma. Whereas treatment for COPD starts on the left and moves towards the right, asthma begins with an ICS and moves to the left as adjunct medications.
Advancement of treatment also depends on the frequency of the use of the SABA, rescue inhaler. If someone with COPD is using a SABA more than 2x/week then they would advance from a LAMA to adding on an LABA and then later the third class of medication the ICS.
In contrast, someone with asthma who is using the rescue inhaler more than two times/week would have started with only an ICS medication, but now needs to advance to the LABA and then lastly add on the LAMA. If the patient with COPD or asthma is not using the rescue inhaler (SABA) more than two times weekly, then they do not need to advance in medication treatment. For asthma, the first medication is a SABA, then ICS. They will never use a LABA without using the ICS. The last medication to use for asthma is a LAMA.
For COPD, the first class of medication to use after the SABA, is the LAMA, and then advance to the LABA, with the last medication added will be the ICS.
Many pharmaceutical companies will create dual combination therapies for ease of use.
|
COPD |
LAMA |
LABA |
ICS |
ASTHMA |
|
®SABA |
“ium” |
“ol” |
“one” |
¬SABA |
Inhaled Medications
Modes of delivery for each of these drugs can be in inhaled medications such as metered dose, breath-activated, or oral form.
Inhaled medications for COPD use different mechanisms to open the airways. Spacers may be used to help increase drug delivery. Nebulizers can also be used for oxygen or are given through liquid drugs via a face mask. Each medication, many can be given intravenously to critically ill patients.
Each class of medication is described below.
Bronchodilators
Inhaled bronchodilators are the key medications to opening the airways as they act on the beta receptors of the bronchiole tubes to cause bronchodilation.
Bronchodilators relax the smooth muscles around the bronchiole air tubes which dilate the bronchioles allowing more area of air to pass through. Most bronchodilators are taken with inhalers, so the medication goes directly to the airway. Short-acting bronchodilators (SABA) versus long-acting bronchodilators (LABA) work directly on opening the airways.
The short-acting agonists are for an acute exacerbation when the airway closes suddenly, whereas the long-acting bronchodilator agonists (LABAs) are to be taken daily on a regular schedule to maintain the patency of the airways. Generally, SABAs are more expensive than LABAs. Each has a rapid onset of action and can be used symptomatically or before exercise.
Short-acting beta 2 agonists work within several minutes for 3-5 hours, compared to long-acting beta 2 agonists, which last 12 hours. Each includes side effects similar to drugs that mimic the sympathetic system including fine tremors, muscle cramps, nervous tension, palpitations, tachycardia, sleep disturbances, hypokalemia, and occasionally paroxysmal bronchospasm.
Anti-Muscarinic/ Anti-cholinergic
This class of medication causes bronchodilation and reduces mucous secretion by blocking muscarinic receptors in the lung. They have a longer action and greater bronchodilator effect than the B2 agonists and are used in both COPD and asthma. Side effects cause dry mouth, nausea, constipation, and can cause urinary retention so must be used with caution for those patients with bladder problems and glaucoma. Short-acting anti-muscarinic can be inhaled or nebulized and includes ipratropium. The long-acting tiotropium can only be given by an inhaler.
Methylxanthines
This class stimulates the beta 2 receptors in the lungs to allow bronchodilation and includes theophylline. It can be given orally, or by IV. This class works by inhibiting phosphodiesterase or blocking adenosine. This class is often given in acute asthma. Side effects include gastrointestinal upset and cardiac palpitations, tachycardia, arrhythmias, headache, insomnia, and convulsions.
Steroids
Inhaled corticosteroids (ICS) are generally the second adjunct therapy suggested by the GOLD Guidelines and help reduce inflammation in the airways and lungs.
Inhaled steroids should not be used as monotherapy but should be used in combination with a bronchodilator. Because this class is a steroid, it may increase blood sugar levels and complicate control for patients who also have diabetes. This class of medications also may cause oral thrush as the oral inhaler delivers glucocorticoids directly to the mouth. It is recommended that this class of oral inhaler be given last for COPD and then the mouth be rinsed immediately after ingestion. On the contrary, it is often the first class of medications for asthma after short-acting bronchodilators.
They can be given via various routes including inhalation (Beclomethasone and Budesonide), orally in the form of prednisolone, and IV in the form of hydrocortisone.
Systemic side effects of long-term corticosteroids are numerous and affect each body system. Blood sugar levels rise in the endocrine system, the muscular-skeletal system produces myopathy; neurologically growth retardation and psychiatric disturbances, and impaired wound healing, sodium, and water retention for the skin; and glaucoma and central redistribution of fat are some of the common side effects.
Leukotriene Receptor Antagonists
This class is used to block the effects of leukotrienes which would normally stimulate the mast cells to release histamine. When histamines are released, vasodilation and fluid movement to the site are natural reactions of the inflammatory response, which is the cause of many symptoms of COPD.
In blocking this reaction, lungs may have less mucus build up and air can move more easily in ventilation. Omalizumab (Xolair), which costs a lot, is given orally. It is an anti-IgE monoclonal medication and is used in severe cases of asthma.
Side effects include gastrointestinal disturbances, headache, insomnia, arthralgia, myalgias and rare bleeding disorders.
Phosphodiesterase-4 (PDE-4) Inhibitors
If COPD symptoms continue, this class of medication may be added. It is the newest class of medications and suppresses inflammation in the airways.

Self Quiz
Ask yourself...
- What are the common side effects of bronchodilators?
- What patient education needs to be discussed regarding the use of inhalers?
- What class of medications decrease inflammation seen in COPD?
- What class of medications opens the bronchioles?
Case Scenario:
Our patient in the case scenario was given a medication regimen to begin with. Initially, he was referred to a smoking cessation program for behavioral management. The patient thought he could try to quit smoking on his own and did not attend any of the classes or use the resources. He was also inconsistent in the use of his medications due to financial barriers. His symptoms became worse after getting a cold, and he presented again to the emergency department with severe shortness of breath, coughing, weakness, pallor, use of accessory muscles to breathe, and heart palpitations. The Emergency Department physician diagnosed him with respiratory failure.
Complications of COPD
Respiratory failure is an extremely serious complication of uncontrolled COPD. Acute exacerbations need to be treated immediately for airway management. Complications of COPD can become life-threatening beyond just shortness of breath and limitations of activities and include pneumonia, heart disease, hypertension, cardiac arrhythmias, and congestive heart failure.
Although COPD may be controlled, it may also suddenly become worse due to any additional respiratory problem such as a cold or flu. If additional symptoms of fever, difficulty breathing, chest tightness, or increased coughing develop, patients should see their primary care provider immediately for treatment.
In addition to the complications of ineffective breathing, the body is stimulated to make more red blood cells to compensate for hypoxia in the tissues. This results in thickened blood, possible risk for thromboembolism formation, and pulmonary hypertension as the pressure within the lungs increases.
The blood flow from the pulmonary artery backs up into the heart and can eventually lead to left-sided heart failure. If a patient is a smoker, the chronic irritation to the alveoli tissue also stimulates the inflammatory response, which creates vasodilation, release of histamines, and alveolar stiffening. With chronic hypoxia, the patient will also develop chronic hyperventilation as a compensatory mechanism. failure.
Respiratory Failure
The inability to get enough oxygen into the blood can cause respiratory failure, causing a buildup of carbon dioxide, which can damage tissue and organs, and eventually death. Symptoms include shortness of breath, extreme fatigue, tachycardia, pallor, cyanosis of the lips, coughing, and possible collapse.
The inability to sustain adequate breathing may require support from a ventilator (23). High carbon dioxide levels can additionally cause blurred vision, confusion, headache, cyanosis, respiratory acidosis, and damage to the brain and kidneys. Blood pH levels that change from high carbon dioxide will disrupt normal fluid and electrolytes and further damage the entire body.
Diagnosing respiratory failure involves performing many of the same tests used to diagnose COPD including diagnostic imaging like a chest x-ray, bronchoscopy, and lung imaging tests such as computed tomography (CT). Structural abnormalities within the lung tissue or detection of fluid accumulation within it can be identified by CT or magnetic resonance imaging (MRI). It also includes additional blood tests including arterial blood gas (ABG) analysis to determine the severity by measuring oxygen and carbon dioxide levels providing insights into acid-base disturbances.
Blood tests such as a complete blood count (CBC) and basic metabolic panel (BMP) may be performed to assess for signs of infection, electrolyte imbalances or any systemic irregularities that might contribute to respiratory comprise. Additional diagnostic procedures could include collecting cultures of sputum or blood to identify pathogens responsible for infections like pneumonia that may lead to respiratory failure. Electrocardiography (ECG) may also be conducted to evaluate cardiac function and rule out causes that resemble respiratory distress such as heart failure. After determining the root cause of respiratory failure, treatment plans can be customized.
Treatment of Respiratory Failure
In addition to the above-listed medications, oxygen support may be needed. Based on the severity of respiratory failure oxygen support may include a noninvasive positive pressure ventilation such as a nasal cannula or mask (26). More severe respiratory failure may advance to bag-mask ventilation or mechanical ventilator. The most severe may require a tracheostomy to place a breathing tube directly into the trachea to stabilize and support oxygenation (25). Each intervention requires additional careful nursing attention, assessment, and interventions.
The treatment for respiratory failure depends on its source and severity. Relieving airway obstruction, managing exacerbations of chronic lung diseases, or managing fluid overload may be included treatments. Supportive measures, including bronchodilators, corticosteroids or diuretics may be taken as supplements to optimize respiratory function and relieve symptoms.
Close monitoring of vital signs, oxygen saturation levels and arterial blood gases enables clinicians to titrate therapies appropriately while interventions to maintain hemodynamic stability and avoid complications like aspiration or ventilator-associated pneumonia are integral parts of comprehensive care. Collaboration among multidisciplinary teams is vital in creating tailored treatment strategies tailored specifically for individual patient needs and optimizing results in respiratory failure management.
Case Scenario Summary
Because our patient in the evolving scenario presented quickly to the emergency department, he was able to get prompt attention and ventilator support. He remained on a ventilator for five days, received medication for pneumonia, and had a positive outcome.
This time, he was more convinced of the seriousness of his COPD and began a smoking cessation program after discharge. He received financial assistance for his medication, enrolled in a COPD action plan, and followed through with his home health nurse’s recommendations. It was difficult, but with the help of an interdisciplinary team, he extended his life with a chronic condition.
Conclusion
COPD is a chronic and incurable condition that includes three subcategories of chronic respiratory conditions including asthma, chronic bronchitis, and emphysema. Risk factors include smoking and exposure to environmental allergens and pollutants that trigger the lungs and alveoli to become inflamed and produce mucus resulting in narrowed airways. COPD is a condition of restricted airflow and causes complications throughout the body related to chronic hypoxia.
Assessment is based on a history of exposures to allergens, mainly cigarette smoking, symptoms, physical exam, and spirometry test. Clinical symptoms include shortness of breath, coughing, wheezing, and dyspnea. Diagnostic tests include spirometry as the GOLD standard and may include radiography to visualize the size of the lungs.
Treatment includes management of symptoms, medications, lifestyle modifications, and education for pulmonary rehabilitation to avoid acute exacerbations and improve the quality of life. There is no cure but there are many classes of medications to assist with bronchodilation and decrease inflammation of airways and lungs. Respiratory failure is the most severe complication of uncontrolled COPD and requires additional support of oxygenation. Although there is no cure, the prognosis depends on the severity of the condition and the ability to respond to treatment.
Resources
- With information that includes how to stop smoking, the ALA is committed to "Fighting for Air" and publishes a highly informative website about lung diseases and lung disorders.
- This respected U.S. government resource offers information about COPD, including a list of relevant publications and resources for further research.
- A good source for up-to-date developments, this digest is published by the COPD Foundation.
- GOLD works with healthcare professionals and public health officials to raise awareness of COPD and to improve the prevention and treatment of this lung disease for patients around the world. Their website includes information about World COPD Day.
- National Heart, Lung, and Blood Institute:
- A global perspective on COPD, including world statistics and NGO and government-sponsored efforts to combat the disease
References + Disclaimer
- Gopal, D. P., Chetty, U., O’Donnell, P., Gajria, C., & Blackadder-Weinstein, J. (2021). Implicit bias in healthcare: clinical practice, research and decision making. Future Healthcare Journal, 8(1), 40–48. https://doi.org/10.7861/fhj.2020-0233
- Shah, H. S., & Bohlen, J. (2023, March 4). Implicit bias. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK589697/
- Afulani, P. A., Okiring, J., Aborigo, R. A., Nutor, J. J., Kuwolamo, I., Dorzie, J. B. K., Semko, S., Okonofua, J. A., & Mendes, W. B. (2023). Provider implicit and explicit bias in person-centered maternity care: a cross-sectional study with maternity providers in Northern Ghana. BMC Health Services Research, 23(1). https://doi.org/10.1186/s12913-023-09261-6
- McMaughan, D. J., Oloruntoba, O., & Smith, M. L. (2020). Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Frontiers in Public Health, 8. https://doi.org/10.3389/fpubh.2020.00231
- Job, C., Adenipekun, B., Cleves, A., & Samuriwo, R. (2022). Health professional’s implicit bias of adult patients with low socioeconomic status (SES) and its effects on clinical decision-making: a scoping review protocol. BMJ Open, 12(12), e059837. https://doi.org/10.1136/bmjopen-2021-059837
- Tarekegne, A. A., Giru, B. W., & Mekonnen, B. (2022). Person-centered maternity care during childbirth and associated factors at selected public hospitals in Addis Ababa, Ethiopia, 2021: a cross-sectional study. Reproductive Health, 19(1). https://doi.org/10.1186/s12978-022-01503-w
- Afulani, P. A., Sayi, T. S., & Montagu, D. (2018). Predictors of person-centered maternity care: the role of socioeconomic status, empowerment, and facility type. BMC Health Services Research, 18(1). https://doi.org/10.1186/s12913-018-3183-x
- Afulani, P. A., Oboke, E. N., Ogolla, B. A., Getahun, M., Kinyua, J., Oluoch, I., Odour, J., & Ongeri, L. (2022). Caring for providers to improve patient experience (CPIPE): intervention development process. Global Health Action, 16(1). https://doi.org/10.1080/16549716.2022.2147289
- Dubey, K., Sharma, N., Chawla, D., Khaduja, R., & Jain, S. (2023). Impact of birth companionship on maternal and fetal outcomes in primigravida pregnant personin a government tertiary care center. Cureus. https://doi.org/10.7759/cureus.38497
- Arpey, N. C., Gaglioti, A. H., & Rosenbaum, M. E. (2017). How socioeconomic status affects patient perceptions of health care: a Qualitative study. Journal of Primary Care & Community Health, 8(3), 169–175. https://doi.org/10.1177/2150131917697439
- Kwame, A., & Petrucka, P. M. (2021). A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nursing, 20(1). https://doi.org/10.1186/s12912-021-00684-2
- Green, T. L., Zapata, J. Y., Brown, H. W., & Hagiwara, N. (2021). Rethinking bias to achieve maternal health equity. Obstetrics and Gynecology, 137(5), 935–940. https://doi.org/10.1097/aog.0000000000004363
- Meints, S. M., Cortes, A., Morais, C. A., & Edwards, R. R. (2019). Racial and ethnic differences in the experience and treatment of noncancer pain. Pain Management, 9(3), 317–334. https://doi.org/10.2217/pmt-2018-0030
- Reproductive medicine advances linked to slavery. (2022, March 31). NIH Record. https://nihrecord.nih.gov/2022/04/01/reproductive-medicine-advances-linked-slavery
- Thornton, P. D., Liese, K., Adlam, K., Erbe, K., & McFarlin, B. L. (2020). Calculators estimating the likelihood of vaginal birth after cesarean: Uses and perceptions. Journal of Midwifery & Pregnant Women’s Health, 65(5), 621–626. https://doi.org/10.1111/jmwh.13141
- Zhang, X., Hailu, B., Tabor, D. C., Gold, R., Sayre, M. H., Sim, I., Jean-Francois, B., Casnoff, C. A., Cullen, T., Thomas, V. A., Artiles, L., Williams, K., Le, P., Aklin, C. F., & James, R. (2019). Role of health information Technology in addressing health disparities. Medical Care, 57(Suppl 2), S115–S120. https://doi.org/10.1097/mlr.0000000000001092
- Main, E. K., Chang, S., Dhurjati, R., Cape, V., Profit, J., & Gould, J. B. (2020). Reduction in racial disparities in severe maternal morbidity from hemorrhage in a large-scale quality improvement collaborative. American Journal of Obstetrics and Gynecology, 223(1), 123.e1-123.e14. https://doi.org/10.1016/j.ajog.2020.01.026
- The Momnibus Act | Black Maternal Health Caucus. (2024, July 8). Black Maternal Health Caucus. https://blackmaternalhealthcaucus-underwood.house.gov/Momnibus
- Mei, S., Chelmow, D., Gecsi, K., Barkley, J., Barrows, E., Brooks, R., Huber-Keener, K., Jeudy, M., O’Hara, J. S., & Burke, W. (2023). Health disparities in ovarian cancer. Obstetrics and Gynecology, 142(1), 196–210. https://doi.org/10.1097/aog.0000000000005210
- Black Pregnant personScholars and the Research Working Group of the Black Mamas Matter Alliance, Aina, A. D., Asiodu, I. V., Castillo, P., Denson, J., Drayton, C., Aka-James, R., Mahdi, I. K., Mitchell, N., Bella Morgan, I., Robinson, A., Scott, K., Williams, C. R., Aiyepola, A., Arega, H., Chambers, B. D., Crear-Perry, J., Delgado, A., Doll, K., . . . Wolfe, T. (2020). Black Maternal Health Research Re-Envisioned: Best Practices for the conduct of research with, for, and by Black mamas. In Harvard Law & Policy Review (Vol. 14, pp. 394–415). https://journals.law.harvard.edu/lpr/wp-content/uploads/sites/89/2020/11/BMMA-Research-Working-Group.pdf
- California Preterm Birth Initiative. (2019). Policy Report: Legal analysis, stakeholder insights, & policy recommendations for healthcare provider implicit bias training in California. In California Preterm Birth Initiative. https://pretermbirthca.ucsf.edu/sites/g/files/tkssra2851/f/MEND%20Policy%20Report_Final20231118.pdf
- Sabin, J., Guenther, G., Ornelas, I. J., Patterson, D. G., Andrilla, C. H. A., Morales, L., Gujral, K., & Frogner, B. K. (2022). Brief online implicit bias education increases bias awareness among clinical teaching faculty. Medical Education Online, 27(1). https://doi.org/10.1080/10872981.2021.2025307
- Section V – Defining Title VI. (2021, February 3). https://www.justice.gov/crt/fcs/T6manual5
- Lingras, K. A., Alexander, M. E., & Vrieze, D. M. (2021). Diversity, equity, and inclusion efforts at a departmental level: building a committee as a vehicle for advancing progress. Journal of Clinical Psychology in Medical Settings, 30(2), 356–379. https://doi.org/10.1007/s10880-021-09809-w
- Sabin, J. A. (2022). Tackling implicit bias in health care. New England Journal of Medicine, 387(2), 105–107. https://doi.org/10.1056/nejmp2201180
- Garrett, S. B., Jones, L., Montague, A., Fa-Yusuf, H., Harris-Taylor, J., Powell, B., Chan, E., Zamarripa, S., Hooper, S., & Butcher, B. D. C. (2023). Challenges and Opportunities for Clinician Implicit Bias Training: Insights from Perinatal Care Stakeholders. Health Equity, 7(1), 506–519. https://doi.org/10.1089/heq.2023.0126
- Vela, M. B., Erondu, A. I., Smith, N. A., Peek, M. E., Woodruff, J. N., & Chin, M. H. (2022). Eliminating explicit and implicit biases in health care: evidence and research needs. Annual Review of Public Health, 43(1), 477–501. https://doi.org/10.1146/annurev-publhealth-052620-103528
- Hamm, R. F., Srinivas, S. K., & Levine, L. D. (2020). A standardized labor induction protocol: impact on racial disparities in obstetrical outcomes. American Journal of Obstetrics & Gynecology MFM, 2(3), 100148. https://doi.org/10.1016/j.ajogmf.2020.100148
- Hughes, R. G. (2008, April 1). Tools and strategies for quality improvement and patient safety. Patient Safety and Quality – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK2682/
- https://www.deamuseum.org/ccp/opium/history.html
- https://americanaddictioncenters.org/opiates/controlled-substances
- https://www.cdc.gov/injury/features/prescription-drug-overdose/index.html
- https://www.cdc.gov/drugoverdose/prescribing/guideline.html
- https://www.cdc.gov/drugoverdose/pdf/guidelines_at-a-glance-a.pdf
- https://www.cdc.gov/drugoverdose/pdf/pdo_checklist-a.pdf
- APA Webster, Lynn R. MD Risk Factors for Opioid-Use Disorder and Overdose, Anesthesia & Analgesia: November 2017 – Volume 125 – Issue 5 – p 1741-1748 doi: 10.1213/ANE.0000000000002496
- Andrea L. Nicol, Robert W. Hurley, Honorio T. Benzon Anesth Analg. Author manuscript; available in PMC 2018 Nov 1. Published in final edited form as: Anesth Analg. 2017 Nov; 125(5): 1682–1703. doi: 10.1213/ANE.0000000000002426
- Mart van Laar, Joseph V Pergolizzi, Jr, Hans-Ulrich Mellinghoff, Ignacio Morón Merchante, Srinivas Nalamachu, Joanne O’Brien, Serge Perrot, Robert B Raffa
- Open Rheumatol J. 2012; 6: 320–330. Published online 2012 Dec 13. doi: 10.2174/1874312901206010320
- Pak, S. C., Micalos, P. S., Maria, S. J., & Lord, B. (2015). Nonpharmacological interventions for pain management in paramedicine and the emergency setting: a review of the literature. Evidence-based complementary and alternative medicine : eCAM, 2015, 873039. https://doi.org/10.1155/2015/873039
- Safer D. J. (2019). Overprescribed Medications for US Adults: Four Major Examples. Journal of clinical medicine research, 11(9), 617–622. https://doi.org/10.14740/jocmr3906
- Dydyk AM, Jain NK, Gupta M. Opioid Use Disorder. [Updated 2020 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553166/
- https://www.cdc.gov/drugoverdose/training/oud/accessible/index.html
- Tan, S. Y., & Merchant, J. (2019). Joseph Murray (1919–2012): First transplant surgeon. Singapore Medical Journal/Singapore Medical Journal, 60(4), 162–163. https://doi.org/10.11622/smedj.2019032
- The history of organ donation and transplantation | UNOS. (2023, October 11). UNOS. https://unos.org/transplant/history/
- The success of our national organ donation and transplant system – UNOS. (2024, January 23). UNOS. https://unos.org/about/success-of-national-organ-donation-and-transplant-system/
- Organ donation Statistics | Organdonor.gov. (2024, March 1). https://www.organdonor.gov/learn/organ-donation-statistics
- Organ donation legislation and policy | Organdonor.gov. (2021, April 1). https://www.organdonor.gov/about-us/legislation-policy
- The Transplant Eco-System: The Role of Data in CMS Oversight of the Organ Procurement Organizations | CMS. (2023, December 13). https://www.cms.gov/blog/transplant-eco-system-role-data-cms-oversight-organ-procurement-organizations
- How we match organs – UNOS. (2024, February 2). UNOS. https://unos.org/transplant/how-we-match-organs/
- Panna, M. S. A. (2022). Determination of Death: Ethical and Biomedical Update with International Consensus. In IntechOpen eBooks. https://doi.org/10.5772/intechopen.100604
- Spears, W., Mian, A., & Greer, D. M. (2022). Brain death: a clinical overview. Journal of Intensive Care, 10(1). https://doi.org/10.1186/s40560-022-00609-4
- Biel, S., & Durrant, J. (2020). Controversies in Brain Death Declaration: Legal and ethical implications in the ICU. Current Treatment Options in Neurology, 22(4). https://doi.org/10.1007/s11940-020-0618-6
- Greer, D. M., Shemie, S. D., Lewis, A., Torrance, S., Varelas, P. N., Goldenberg, F. D., Bernat, J. L., Souter, M. J., Topçuoğlu, M. A., Alexandrov, A. W., Baldisseri, M. R., Bleck, T. P., Citerio, G., Dawson, R., Hoppe, A., Jacobe, S., Manara, A., Nakagawa, T. A., Pope, T. M., . . . Sung, G. (2020). Determination of brain Death/Death by neurologic criteria. JAMA, 324(11), 1078. https://doi.org/10.1001/jama.2020.11586
- Kleemeier, R. (2020, August 6). Care and collaboration equal successful organ donation. American Nurse. https://www.myamericannurse.com/care-and-collaboration-equal-successful-organ-donation/
- Akbulut, S. (2022). Knowledge levels, attitudes and awareness of nurses toward organ donation. İstanbul Kuzey Klinikleri. https://doi.org/10.14744/nci.2022.24478
- Simonsson, J., Keijzer, K., Södereld, T., & Forsberg, A. (2020). Intensive critical care nurses’ with limited experience: Experiences of caring for an organ donor during the donation process. Journal of Clinical Nursing, 29(9–10), 1614–1622. https://doi.org/10.1111/jocn.15195
- Green, B., Ter Goon, D., Mtise, T., & Oladimeji, O. (2023). A Cross-Sectional study of professional nurses’ knowledge, attitudes, and practices regarding organ donation in critical care units of public and private hospitals in the Eastern Cape, South Africa. Nursing Reports, 13(1), 255–264. https://doi.org/10.3390/nursrep13010024
- Starr, R., Tadi, P., Weisbrod, L. J., Pfleghaar, N., & Sapkota, R. (2024, January 31). Brain death (Nursing). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK568811/
- Seshadri, A., Cuschieri, J., Kaups, K. L., Knowlton, L. M., Kutcher, M., Pathak, A., Rappold, J., Rinderknecht, T. N., Stein, D. M., Young, J., & Michetti, C. P. (2023). Organ donation in the surgical ICU: an American Association for the Surgery of Trauma Critical Care Committee clinical consensus document. Trauma Surgery & Acute Care Open, 8(1), e001107. https://doi.org/10.1136/tsaco-2023-001107
- U.S. Department of Health and Human Services Recommendations 19-28 | HRSA. (2021, June 1). https://www.hrsa.gov/advisory-committees/organ-transplantation/recommendations/19-28
- Code of Ethics for nurses. (2017, October 26). ANA. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/
- Healey, A., Leeies, M., Hrymak, C., Chochinov, A., Grunau, B., Paunovic, B., Teitelbaum, J., Wilson, L., & Shemie, S. D. (2020). CAEP, CCCS, and CNSF Position Statement – Management of devastating brain injuries in the emergency department: Enhancing neuroprognostication and maintaining the opportunity for organ and tissue donation. CJEM. Canadian Journal of Emergency Medical Care/CJEM, 22(5), 658–660. https://doi.org/10.1017/cem.2020.357
- Clarke, C. (2021). Management of the brain-dead organ donor. Indian Journal of Thoracic and Cardiovascular Surgery/Indian Journal of Thoracic and Cardiovascular Surgery, 37(S3), 395–400. https://doi.org/10.1007/s12055-021-01224-y
- Zirpe, K., & Gurav, S. (2019). Brain death and management of potential organ donor: an Indian perspective. Indian Journal of Critical Care Medicine/Indian Journal of Critical Care Medicine, 23(S2), 151–156. https://doi.org/10.5005/jp-journals-10071-23194
- Organ procurement organizations | Increasing organ donations | UNOS. (2024, January 11). UNOS. https://unos.org/transplant/opos-increasing-organ-donation/
- Agarwal, P., Kukrele, R., & Sharma, D. (2019). Vacuum assisted closure (VAC)/ negative pressure wound therapy (NPWT) for difficult wounds: A review. Journal of clinical orthopaedics and trauma, 10(5), 845–848. https://doi.org/10.1016/j.jcot.2019.06.015
- Chen, C. Y., Kuo, S. M., Tarng, Y. W., & Lin, K. C. (2021). Immediate application of negative pressure wound therapy following lower extremity flap reconstruction in sixteen patients. Scientific reports, 11(1), 21158. https://doi.org/10.1038/s41598-021-00369-5
- Doenges, M.E., Moorhouse, M.F., & Alice C. Murr, A.C. (2019). Nursing care plans: guidelines for individualizing client care across the life span: Vol. 10th edition. F.A. Davis.
- Gold, C., Kournoutas, I., Seaman, S. C., & Greenlee, J. (2021). Bone flap management strategies for postcraniotomy surgical site infection. Surgical neurology international, 12, 341. https://doi.org/10.25259/SNI_276_2021
- Hong, J.P., Kwon, J.G. (2022). Flaps in Plastic Surgery. In: Maruccia, M., Giudice, G. (eds) Textbook of Plastic and Reconstructive Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-82335-1_9
- Mazine, A., Hofer, S.O.P., & Yau, T.M. (2021). Infection, sternal debridement and muscle flap. In: Cheng, D.C., Martin, J., David, T. (eds) Evidence-Based Practice in Perioperative Cardiac Anesthesia and Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-47887-2_57
- McNichol, Ratliff, C., & Yates, S. (2021). Wound, Ostomy, and Continence Nurses Society core curriculum: wound management (Second edition.). Wolters Kluwer Health.
- Rohrer, Cook, J. L., & Kaufman, A. J. (Eds.). (2018). Flaps and grafts in dermatologic surgery (Second edition.). Elsevier.
- Saber AY, Hohman MH, Dreyer MA. (2022). Basic flap design. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563252/
- Strauch, B. (2016). Grabb’s encyclopedia of flaps. Volume II, Upper extremities, torso, pelvis, and lower extremities (4th ed.). Wolters Kluwer.
- Vincent, A., Sawhney, R., & Ducic, Y. (2019). Perioperative care of free flap patients. Seminars in plastic surgery, 33(1), 5–12. https://doi.org/10.1055/s-0038-1676824
- World Health Organization: WHO. (2019, May 13). Diabetes. https://www.who.int/health-topics/diabetes#tab=tab_
- Lizzo, J. M., Goyal, A., & Gupta, V. (2023, July 10). Adult diabetic ketoacidosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560723/
- Diabetic ketoacidosis: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000320.htm
- UpToDate. (n.d.). UpToDate. https://www.uptodate.com/contents/diabetic-ketoacidosis-in-children-clinical-features-and-diagnosis/print
- Virdi, N., Poon, Y., Abaniel, R., & Bergenstal, R. M. (2023). Prevalence, cost, and burden of diabetic ketoacidosis. Diabetes Technology & Therapeutics, 25(S3), S-84. https://doi.org/10.1089/dia.2023.0149
- Matthews, S., Coates, M. M., Bukhman, A., & Trujillo, C. (2023). Health system capacity to manage diabetic ketoacidosis in nine low-income and lower-middle income countries: a cross-sectional analysis of nationally representative survey data. eClinical Medicine, 55(101759). https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(22)00488-6/fulltext#%20
- Virdi, N., Poon, Y., Abaniel, R., & Bergenstal, R. M. (2023b). Prevalence, cost, and burden of diabetic ketoacidosis. Diabetes Technology & Therapeutics, 25(S3), S-84. https://doi.org/10.1089/dia.2023.0149
- Lizzo, J. M., Goyal, A., & Gupta, V. (2023b, July 10). Adult diabetic ketoacidosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560723/
- Ghimire, P., & Dhamoon, A. S. (2023, August 8). Ketoacidosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK534848/#:~:text=Introduction-,Ketoacidosis%20is%20a%20metabolic%20state%20associated%20with%20pathologically%20high%20serum,individual%20cells%20in%20the%20body
- Hamdy, O., MD PhD. (n.d.). Diabetic Ketoacidosis (DKA): practice essentials, background, pathophysiology. https://emedicine.medscape.com/article/118361-overview?form=fpf
- JDRF. (2023, February 24). Signs and symptoms of Type 1 diabetes in Children – JDRF. https://www.jdrf.org/t1d-resources/about/symptoms/children/
- Diabetic ketoacidosis: MedlinePlus Medical Encyclopedia. (n.d.-b). https://medlineplus.gov/ency/article/000320.htm#:~:text=People%20with%20type%202%20diabetes,a%20severe%20illness%20or%20infection.
- Diabetic ketoacidosis – Symptoms & causes – Mayo Clinic. (2022, October 6). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/diabetic-ketoacidosis/symptoms-causes/syc-20371551
- Chukwuka, E., Johnson, D., Udoyen, A.-O., Egbunu, E. O., & Ogbuiyi-Chima, I. C. (2023). Comprehensive Review of Diabetic Ketoacidosis: An update. PMC PubMed Central, 85(6), 2802–2807. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10289692/
- Cavataio, M. M., & Packer, C. D. (2022). Steroid-Induced Diabetic Ketoacidosis: A case Report and Review of the literature. Cureus, 14(4), e24372. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9124452/#:~:text=Mechanisms%20for%20steroid%2Dinduced%20diabetes,translocation%20%5B9%2D10%5D.
- Mfa, J. H. M. M. (2021, August 18). What to know about Steroid-Induced Diabetes. Healthline. https://www.healthline.com/health/diabetes/steroid-induced-diabetes
- Professional, C. C. M. (n.d.). Hyperosmolar hyperglycemic state (HHS). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21147-hyperosmolar-hyperglycemic-state
- Ghimire, P., Dhamoon, A. S., & Doerr, C. (2023, August 8). Ketoacidosis (Nursing). StatPearls – NCBI Bookshelf. Retrieved March 22, 2024, from https://www.ncbi.nlm.nih.gov/books/NBK568717/
- Anion gap blood test. (n.d.). https://medlineplus.gov/lab-tests/anion-gap-blood-test/#:~:text=A%20high%20anion%20gap%20test,Dehydration
- Ghimire, P., Dhamoon, A. S., & Doerr, C. (2023b, August 8). Ketoacidosis (Nursing). StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK568717/
- Besen, B. a. M. P., Boer, W., & Honoré, P. M. (2021). Fluid management in diabetic ketoacidosis: new tricks for old dogs? Intensive Care Medicine, 47(11), 1312–1314. https://doi.org/10.1007/s00134-021-06527-7
- Jayashree, M., Williams, V., & Iyer, R. (2019). Fluid therapy for pediatric patients with diabetic ketoacidosis: current perspectives. PMC PubMed Central, 12, 2355–2361. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6858801/
- Lizzo, J. M., Goyal, A., & Gupta, V. (2023c, July 10). Adult diabetic ketoacidosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK560723/
- Professional, C. C. M. (n.d.-a). Cerebral edema (Brain swelling). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/cerebral-edema-brain-swelling
- Hamdy, O., MD PhD. (n.d.-b). Diabetic Ketoacidosis (DKA) treatment & management: approach considerations, correction of fluid loss, insulin therapy. https://emedicine.medscape.com/article/118361-treatment#d13
- Intracranial pressure monitoring. (2024, January 1). PubMed. https://pubmed.ncbi.nlm.nih.gov/31194438/#:~:text=Excerpt,20%20to%2025%20mm%20Hg
- Ahmad, F., & Joshi, S. H. (2023). Self-Care practices and their Role in the control of Diabetes: A Narrative review. PubMed Central Cureus, 15 (7), e41409. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10402910/#:~:text=To%20reduce%20the%20burden%20of,glucose%20levels%20in%20the%20patients.
- Diabetes self-management training. (n.d.). Medicare. https://www.medicare.gov/coverage/diabetes-self-management-training
- Diabetic ketoacidosis. (2021, March 25). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/basics/diabetic-ketoacidosis.html
- Managing sick days | Diabetes | CDC. (n.d.). https://www.cdc.gov/diabetes/managing/flu-sick-days.html
- Mental Health and Diabetes | ADA. (n.d.). https://diabetes.org/health-wellness/mental-health
- Diabetes Distress Assessment & Resource Center. (n.d.). https://diabetesdistress.org/learn-about-dd/
- Dealing with diabetes burnout. (2022, June 20). Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/spotlights/diabetes-burnout.html
- Professional, C. C. M. (n.d.-b). Diabulimia. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/22658-diabulimia
- Bulimia nervosa – Symptoms and causes – Mayo Clinic. (2024, February 29). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/bulimia/symptoms-causes/syc-20353615
- Anniversary of the Inflation Reduction Act: Update on CMS Implementation | CMS. (2023, August 16). https://www.cms.gov/newsroom/fact-sheets/anniversary-inflation-reduction-act-update-cms-implementation#:~:text=Specifically%2C%20the%20Inflation%20Reduction%20Act,Traditional%20Medicare%2C%20or%20Medicare%20Advantage.
- International Diabetes Federation. (2024, February 7). Diabetes Facets and Figures | International Diabetes Federation. https://idf.org/about-diabetes/diabetes-facts-figures/
- Brown, A. (2021, August 14). Diabetes distress: why it’s common and what we can do about it! diaTribe. https://diatribe.org/diabetes-distress-why-it%E2%80%99s-common-and-what-we-can-do-about-it
- Luo, F., Chapel, G., Ye, Z., Jackson, S. L., & Roy, K. (2023). Labor income losses associated with heart disease and stroke from the 2019 panel Study of Income Dynamics. JAMA Network Open, 6(3), e232658. https://doi.org/10.1001/jamanetworkopen.2023.2658
- Coronary artery disease – symptoms and causes | Penn Medicine. (2023). https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/coronary-artery-disease
- Heart disease resources | Cdc.gov. (2023, May 15). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/about.htm
- NHS inform. (2023, November 9). Common heart conditions – Illnesses & conditions | NHS inform. NHS Inform. https://www.nhsinform.scot/illnesses-and-conditions/heart-and-blood-vessels/conditions/common-heart-conditions/
- Casas, R., Castro‐Barquero, S., Estrus, R., & Sacanella, E. (2018). Nutrition and cardiovascular health. International Journal of Molecular Sciences, 19(12), 3988. https://doi.org/10.3390/ijms19123988
- Coronary artery disease – Symptoms and causes – Mayo Clinic. (2022, May 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613
- NHS inform. (2023, November 9). Cardiovascular disease – Illnesses & conditions | NHS inform. NHS Inform. https://www.nhsinform.scot/illnesses-and-conditions/heart-and-blood-vessels/conditions/cardiovascular-disease/
- Data and Statistics on Congenital Heart Defects | CDC. (2023, September 19). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/heartdefects/data.html
- Valvular heart Disease | Cdc.gov. (2019, December 9). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/valvular_disease.htm
- What is heart failure? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/heart-failure
- Heart failure signs and symptoms. (2023, October 18). www.heart.org. https://www.heart.org/en/health-topics/heart-failure/warning-signs-of-heart-failure
- What is cardiomyopathy? | NHLBI, NIH. (2022, April 19). NHLBI, NIH. https://www.nhlbi.nih.gov/health/cardiomyopathy
- Cardiomyopathy | cdc.gov. (2023, February 21). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/cardiomyopathy.htm
- Khandaker, M. H., Espinosa, R. E., Nishimura, R. A., Sinak, L. J., Hayes, S. N., Melduni, R. M., & Oh, J. K. (2010). Pericardial Disease: Diagnosis and management. Mayo Clinic Proceedings, 85(6), 572–593. https://doi.org/10.4065/mcp.2010.0046
- What is an arrhythmia? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/arrhythmias
- Atrial fibrillation | Cdc.gov. (2022, October 14). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
- Harris, C., Croce, B., & Cao, C. (2016). ACS Patient Page Type A aortic dissection. Annals of Cardiothoracic Surgery, 5(4), 256. https://doi.org/10.21037/acs.2016.05.04
- Milner, R., MD. (2022, January 25). What is aortic dissection: What you need to know about the causes, types and more. UChicago Medicine. https://www.uchicagomedicine.org/forefront/heart-and-vascular-articles/silent-killer-everything-you-need-to-know-about-aortic-dissection
- World Health Organization: WHO. (2021, June 11). Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- Gaziano, T. A., Bitton, A., Anand, S., Abrahams‐Gessel, S., & Murphy, A. (2010). Growing epidemic of coronary heart disease in Low- and Middle-Income countries. Current Problems in Cardiology, 35(2), 72–115. https://doi.org/10.1016/j.cpcardiol.2009.10.002
- Fuchs, F. D., & Whelton, P. K. (2020). High blood pressure and cardiovascular disease. Hypertension, 75(2), 285–292. https://doi.org/10.1161/hypertensionaha.119.14240
- Martín-Timón, I., Sevillano-Collantes, C., Segura-Galindo, A., & Del Cañizo-Gómez, F. J. (2014). Type 2 diabetes and cardiovascular disease: Have all risk factors the same strength? World Journal of Diabetes, 5(4), 444. https://doi.org/10.4239/wjd.v5.i4.444
- Hajar, R. (2017). Risk factors for coronary artery disease: Historical perspectives. Heart Views, 18(3), 109. https://doi.org/10.4103/heartviews.heartviews_106_17
- Yazdanyar A., Newman A.B. The burden of cardiovascular disease in the elderly: Morbidity, mortality, and costs. Clin. Geriatr. Med. 2009;25:563–577. doi: 10.1016/j.cger.2009.07.007
- Graham, G. (2015). Disparities in cardiovascular disease risk in the United States. Current Cardiology Reviews, 11(3), 238–245. https://doi.org/10.2174/1573403×11666141122220003
- Multifactorial inheritance and genetic disease | Learn Science at Scitable. (2023). https://www.nature.com/scitable/topicpage/multifactorial-inheritance-and-genetic-disease-919/
- Saheera, S., & Krishnamurthy, P. (2020). Cardiovascular Changes Associated with Hypertensive Heart Disease and Aging. Cell Transplantation, 29, 096368972092083. https://doi.org/10.1177/0963689720920830
- What is Blood Cholesterol? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/blood-cholesterol
- Diabetes, Heart Disease, & Stroke. (2023, June 7). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/heart-disease-stroke
- How smoking affects the heart and blood vessels | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/heart/smoking
- Benefits | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/heart/physical-activity/benefits
- Family Health History of Heart Disease | CDC. (2023). https://www.cdc.gov/genomics/disease/fh/history_heart_disease.htm
- Diab, A., Dastmalchi, L. N., Gulati, M., & Michos, E. D. (2023). A Heart-Healthy Diet for cardiovascular Disease Prevention: Where are we now? Vascular Health and Risk Management, Volume 19, 237–253. https://doi.org/10.2147/vhrm.s379874
- Increase the proportion of adults who do enough aerobic physical activity for substantial health benefits — PA02 – Healthy People 2030 | health.gov. (2023). https://health.gov/healthypeople/objectives-and-data/browse-objectives/physical-activity/increase-proportion-adults-who-do-enough-aerobic-physical-activity-substantial-health-benefits-pa-02
- Dineen-Griffin, S., García-Cárdenas, V., Williams, K., & Benrimoj, S. I. (2019). Helping patients help themselves: A systematic review of self-management support strategies in primary health care practice. PLOS ONE, 14(8), e0220116. https://doi.org/10.1371/journal.pone.0220116
- Moudatsou, M., Stavropoulou, A., Philalithis, Α., & Koukouli, S. (2020). The role of empathy in health and social care professionals. Healthcare, 8(1), 26. https://doi.org/10.3390/healthcare8010026
- Boyde, M., Tuckett, A. G., Peters, R., Thompson, D. R., Turner, C., & Stewart, S. (2009). Learning style and learning needs of heart failure patients (The Need2Know-HF patient study). European Journal of Cardiovascular Nursing, 8(5), 316–322. https://doi.org/10.1016/j.ejcnurse.2009.05.003
- Ricci, L., Villegente, J., Loyal, D., Ayav, C., Kivits, J., & Rat, A. (2021). Tailored patient therapeutic educational interventions: A patient‐centred communication model. Health Expectations, 25(1), 276–289. https://doi.org/10.1111/hex.13377
- Zhou, Q., & Liao, J. K. (2009). Statins and cardiovascular diseases: From cholesterol lowering to pleiotropy. Current Pharmaceutical Design, 15(5), 467–478. https://doi.org/10.2174/138161209787315684
- Medical treatments for carotid artery disease. (2017, September 11). Stanford Health Care. https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/carotid-artery-disease/treatments/medical.html
- Types of blood pressure medications. (2023, June 7). www.heart.org. https://www.heart.org/en/health-topics/high-blood-pressure/changes-you-can-make-to-manage-high-blood-pressure/types-of-blood-pressure-medications
- Coronary artery bypass graft Surgery. (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/coronary-artery-bypass-graft-surgery
- Conditions treated by heart surgery | NHLBI, NIH. (2022, June 1). NHLBI, NIH. https://www.nhlbi.nih.gov/health/heart-surgery/conditions
- Community-based organizations encourage action to prevent heart disease and stroke. (2023). American Heart Association. https://newsroom.heart.org/news/community-based-organizations-encourage-action-to-prevent-heart-disease-and-stroke
- Medina, E. L., Filho, O. L. M., & Mesquita, C. T. (2013). Health Social Networks asOnlineLife Support Groups for Patients With Cardiovascular Diseases. Arquivos Brasileiros De Cardiologia. https://doi.org/10.5935/abc.20130161
- Corbett, J. A., Opladen, J., & Bisognano, J. D. (2020). Telemedicine can revolutionize the treatment of chronic disease. International Journal of Cardiology: Hypertension, 7, 100051. https://doi.org/10.1016/j.ijchy.2020.100051
- Kang, H. S., & Exworthy, M. (2022). Wearing the Future—Wearables to Empower users to take Greater responsibility for their health and care: Scoping review. Jmir Mhealth and Uhealth, 10(7), e35684. https://doi.org/10.2196/35684
- Research at AHA. (2023). https://professional.heart.org/en/research-programs
- National Heart, Lung, and Blood Institute (NHLBI). (2018, June 14). National Institutes of Health (NIH). https://www.nih.gov/about-nih/what-we-do/nih-almanac/national-heart-lung-blood-institute-nhlbi
- Lee, J., & Cooke, J. P. (2011). The role of nicotine in the pathogenesis of atherosclerosis. Atherosclerosis, 215(2), 281–283. https://doi.org/10.1016/j.atherosclerosis.2011.01.003
- Diab, A., Dastmalchi, L. N., Gulati, M., & Michos, E. D. (2023). A Heart-Healthy Diet for cardiovascular Disease Prevention: Where are we now? Vascular Health and Risk Management, Volume 19, 237–253. https://doi.org/10.2147/vhrm.s379874
- Cena, H., & Calder, P. C. (2020). Defining a Healthy Diet: Evidence for the role of contemporary dietary patterns in Health and disease. Nutrients, 12(2), 334. https://doi.org/10.3390/nu12020334
- Diab, A., Dastmalchi, L. N., Gulati, M., & Michos, E. D. (2023). A Heart-Healthy Diet for cardiovascular Disease Prevention: Where are we now? Vascular Health and Risk Management, Volume 19, 237–253. https://doi.org/10.2147/vhrm.s379874
- World Health Organization: WHO. (2019, June 11). Cardiovascular diseases. https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1
- Yusuf S., Hawken S., Ounpuu S., Dans T., Avezum A., Lanas F., McQueen M., Budaj A., Pais P., Varigos J., et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004; 364:937–952. doi: 10.1016/S0140-6736(04)17018-9.
- Akesson A., Weismayer C., Newby P.K., Wolk A. Combined effect of low-risk dietary and lifestyle behaviors in primary prevention of myocardial infarction in women. Arch. Intern. Med. 2007; 167:2122–2127. doi: 10.1001/archinte.167.19.2122
- Ford E.S., Bergmann M.M., Kröger J., Schienkiewitz A., Weikert C., Boeing H. Healthy living is the best revenge: Findings from the European Perspective Investigation into Cancer and Nutrition-Potsdam study. Arch. Intern. Med. 2009; 169:1355–1362. doi: 10.1001/archinternmed.2009.237.
- Chiuve S.E., McCullough M.L., Sacks F.M., Rimm E.B. Healthy lifestyle factors in the primary prevention of coronary heart disease among men: Benefits among users and nonusers of lipid-lowering and antihypertensive medications. Circulation. 2006; 114:160–167. doi: 10.1161/CIRCULATIONAHA.106.621417
- National Library of Medicine. (2022). Heart diseases. https://medlineplus.gov/heartdiseases.html
- Sharifi‐Rad, J., Rodrigues, C. F., Sharopov, F., Docea, A. O., Karaça, A. C., Sharifi‐Rad, M., Karıncaoglu, D. K., Gülseren, G., Şenol, E., Demircan, E., Taheri, Y., Suleria, H. a. R., Özçelik, B., Kasapoğlu, K. N., Gültekin-Özgüven, M., Daşkaya-Dikmen, C., Cho, W. C., Martins, N., & Calina, D. (2020). Diet, Lifestyle and Cardiovascular Diseases: Linking pathophysiology to cardioprotective effects of natural bioactive compounds. International Journal of Environmental Research and Public Health, 17(7), 2326. https://doi.org/10.3390/ijerph17072326
- Chacko, M., Sarma, P. S., Harikrishnan, S., Zachariah, G., & Jeemon, P. (2020). Family history of cardiovascular disease and risk of premature coronary heart disease: A matched case-control study. Welcome Open Research, 5, 70. https://doi.org/10.12688/wellcomeopenres.15829.2
- Holvoet P. Stress in obesity and associated metabolic and cardiovascular disorders. Scientifica. 2012; 2012:205027. doi: 10.6064/2012/205027
- Casas, R., Castro‐Barquero, S., Estruch, R., & Sacanella, E. (2018). Nutrition and cardiovascular health. International Journal of Molecular Sciences, 19(12), 3988. https://doi.org/10.3390/ijms19123988
- Coronary artery disease – Symptoms and causes – Mayo Clinic. (2022, May 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613
- NHS inform. (2023, November 9). Cardiovascular disease – Illnesses & conditions | NHS inform. NHS Inform. https://www.nhsinform.scot/illnesses-and-conditions/heart-and-blood-vessels/conditions/cardiovascular-disease/
- Data and Statistics on Congenital Heart Defects | CDC. (2023, September 19). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/heartdefects/data.html
- Valvular heart Disease | Cdc.gov. (2019, December 9). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/valvular_disease.htm
- What is heart failure? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/heart-failure
- Heart failure signs and symptoms. (2023, October 18). www.heart.org. https://www.heart.org/en/health-topics/heart-failure/warning-signs-of-heart-failure
- What is cardiomyopathy? | NHLBI, NIH. (2022, April 19). NHLBI, NIH. https://www.nhlbi.nih.gov/health/cardiomyopathy
- Cardiomyopathy | cdc.gov. (2023, February 21). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/cardiomyopathy.htm
- Khandaker, M. H., Espinosa, R. E., Nishimura, R. A., Sinak, L. J., Hayes, S. N., Melduni, R. M., & Oh, J. K. (2010). Pericardial Disease: Diagnosis and management. Mayo Clinic Proceedings, 85(6), 572–593. https://doi.org/10.4065/mcp.2010.0046
- What is an arrhythmia? | NHLBI, NIH. (2022, March 24). NHLBI, NIH. https://www.nhlbi.nih.gov/health/arrhythmias
- Atrial fibrillation | Cdc.gov. (2022, October 14). Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/atrial_fibrillation.htm
- Harris, C., Croce, B., & Cao, C. (2016). ACS Patient Page Type A aortic dissection. Annals of Cardiothoracic Surgery, 5(4), 256. https://doi.org/10.21037/acs.2016.05.04
- Milner, R., MD. (2022, January 25). What is aortic dissection: What you need to know about the causes, types and more. UChicago Medicine. https://www.uchicagomedicine.org/forefront/heart-and-vascular-articles/silent-killer-everything-you-need-to-know-about-aortic-dissection
- Yu, E., Rimm, E. B., Qi, L., Rexrode, K. M., Chen, A., Sun, Q., Willett, W. C., Hu, F. B., & Manson, J. E. (2016). Diet, lifestyle, biomarkers, genetic factors, and risk of cardiovascular disease in the nurses’ health studies. American Journal of Public Health, 106(9), 1616–1623. https://doi.org/10.2105/ajph.2016.303316
- Lichtenstein, A. H., Appel, L. J., Vadiveloo, M., Hu, F. B., Kris‐Etherton, P. M., Rebholz, C. M., Sacks, F. M., Thorndike, A. N., Van Horn, L., Wylie‐Rosett, J., & Biology, V. (2021). 2021 Dietary Guidance to Improve Cardiovascular Health: A scientific statement from the American Heart Association. Circulation, 144(23). https://doi.org/10.1161/cir.0000000000001031
- Schwingshackl L, Schwedhelm C, Hoffmann G, Boeing H. Potatoes, and risk of chronic disease: a systematic review and dose-response meta-analysis. Eur J Nutr. 2019; 58:2243–2251. doi: 10.1007/s00394-018-1774-2
- Preventing heart disease. (2023, February 2). The Nutrition Source. https://www.hsph.harvard.edu/nutritionsource/disease-prevention/cardiovascular-disease/preventing-cvd/
- Tosh SM, Bordenave N. Emerging science on benefits of whole grain oat and barley and their soluble dietary fibers for heart health, glycemic response, and gut microbiota. Nutr Rev. 2020; 78(suppl 1):13–20. doi: 10.1093/nutrit/nuz085
- Voskoboinik A, Kalman JM, De Silva A, Nicholls T, Costello B, Nanayakkara S, Prabhu S, Stub D, Azzopardi S, Vizi D, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020; 382:20–28. doi: 10.1056/NEJMoa1817591
- Hardy DS, Garvin JT, Xu H. Carbohydrate quality, glycemic index, glycemic load and cardiometabolic risks in the US, Europe, and Asia: a dose-response meta-analysis. Nutr Metab Cardiovasc Dis. 2020; 30:853–871. doi: 10.1016/j.numecd.2019.12.050
- Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, Miller M, Rimm EB, Rudel LL, Robinson JG, et al; American Heart Association. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017; 136: e1–e23. doi: 10.1161/CIR.0000000000000510
- Chiavaroli, L., Viguiliouk, E., Nishi, S. K., Mejía, S. B., Rahelić, D., Kahleová, H., Salas‐Salvadó, J., Kendall, C. W., & Sievenpiper, J. L. (2019). DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients, 11(2), 338. https://doi.org/10.3390/nu11020338
- Satija, A., & Hu, F. B. (2018). Plant-based diets and cardiovascular health. Trends in Cardiovascular Medicine, 28(7), 437–441. https://doi.org/10.1016/j.tcm.2018.02.004
- Wang DD, Hu FB. Dietary fat and risk of cardiovascular disease: recent controversies and advances. Annu Rev Nutr. 2017; 37:423–446. doi: 10.1146/annurev-nutr-071816-064614
- Eckel RH, Borra S, Lichtenstein AH, Yin-Piazza SY; Trans Fat Conference Planning Group. Understanding the complexity of trans fatty acid reduction in the American diet: American Heart Association Trans Fat Conference 2006: report of the Trans Fat Conference Planning Group. Circulation. 2007; 115:2231–2246. doi: 10.1161/CIRCULATIONAHA.106.181947
- Heart-healthy diet: 8 steps to prevent heart disease. (2022, April 28). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/heart-disease/in-depth/heart-healthy-diet/art-20047702
- Bhattad, P. B., & Pacifico, L. (2022). Empowering patients: Promoting patient education and health literacy. Cureus. https://doi.org/10.7759/cureus.27336
- Pem, D. (2015, October 1). Fruit and Vegetable Intake: Benefits and Progress of Nutrition Education Interventions- Narrative Review article. PubMed Central (PMC). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4644575/
- Marcus, C. (2014). Strategies for improving the quality of verbal patient and family education: a review of the literature and creation of the EDUCATE model. Health Psychology and Behavioral Medicine, 2(1), 482–495. https://doi.org/10.1080/21642850.2014.900450
- Woodgate, R. L., & Sigurdson, C. (2015). Building school-based cardiovascular health promotion capacity in youth: a mixed methods study. BMC Public Health, 15(1). https://doi.org/10.1186/s12889-015-1759-5
- Trichopoulou, A., Martínez‐González, M. A., Tong, T. Y., Forouhi, N. G., Khandelwal, S., Prabhakaran, D., Mozaffarian, D., & De Lorgeril, M. (2014). Definitions and potential health benefits of the Mediterranean diet: views from experts around the world. BMC Medicine, 12(1). https://doi.org/10.1186/1741-7015-12-112
- Challa, H. J. (2023, January 23). DASH Diet to Stop Hypertension. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK482514/
- Childs, C. E., Calder, P. C., & Miles, E. A. (2019). Diet and immune function. Nutrients, 11(8), 1933. https://doi.org/10.3390/nu11081933
- Centers for Disease Control and Prevention (CDC) (2023). Fast Facts: Preventing Adverse Childhood Experiences. https://www.cdc.gov/violenceprevention/aces/fastfact.html
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8.
- Starecheski, L. (2015). Take the ACE quiz—And learn what it does and doesn’t mean. NPR. https://www.npr.org/sections/health-shots/2015/03/02/387007941/take-the-ace-quiz-and-learn-what-it-does-and-doesnt-mean
- Center on the Developing Child at Harvard University (n.d.). What are ACEs? And how do they relate to toxic stress? https://developingchild.harvard.edu/resources/aces-and-toxic-stress-frequently-asked-questions/
- CDC, (2022). About the CDC-Kaiser ACE study. https://www.cdc.gov/violenceprevention/aces/about.html
- CDC. (2021). Preventing adverse childhood experiences. https://www.cdc.gov/vitalsigns/aces/index.html
- CDC (2023). Risk and protective factors. https://www.cdc.gov/violenceprevention/aces/riskprotectivefactors.html
- Cleveland Clinic (2023). Adverse childhood experiences (ACEs) & childhood trauma. (2023). https://my.clevelandclinic.org/health/symptoms/24875-adverse-childhood-experiences-ace
- Merrick, M. T. (2019). Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. Morbidity and Mortality Weekly Report, 68. https://doi.org/10.15585/mmwr.mm6844e1
- Child Trends. (2018). American Indians and Alaska Natives must be included in research on adverse childhood experiences. https://www.childtrends.org/blog/american-indians-alaska-natives-adverse-childhood-experiences
- Hughes, K., Bellis, M.A., Hardcastle, K.A., Sethi, D., Butchart, A., Mikton, C., Jones, L., Dunne, M.P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health; 2(8): e356-e366. doi: 10.1016/S2468-2667(17)30118-4.
- CDC (2023). Leading causes of death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
- Merrick, M. T., Ports, K. A., Ford, D. C., Afifi, T. O., Gershoff, E. T., & Grogan-Kaylor, A. (2017). Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect, 69, 10–19. https://doi.org/10.1016/j.chiabu.2017.03.016
- Center on the Developing Child at Harvard University (n.d.). Take the ACE quiz – And learn what it does and doesn’t mean. https://developingchild.harvard.edu/media-coverage/take-the-ace-quiz-and-learn-what-it-does-and-doesnt-mean/
- National Conference of State Legislatures (2022). Adverse Childhood Experiences. https://www.ncsl.org/health/adverse-childhood-experience
- National Center for Missing & Exploited Children (2023). CyberTipline http://www.missingkids.org/content/ncmec/en/gethelpnow/cybertipline.html
- Dowdell, E. B., & Speck, P. M. (2022). Ce: Trauma-informed care in nursing practice. AJN, American Journal of Nursing, 122(4), 30–38. https://doi.org/10.1097/01.naj.0000827328.25341.1f
- Eilers, H., aan het Rot, M., & Jeronimus, B. F. (2023). Childhood trauma and adult somatic symptoms. Psychosomatic Medicine, 85(5), 408–416. https://doi.org/10.1097/psy.0000000000001208
- Fleishman, J., Kamsky, H., & Sundborg, S. (2019). Trauma-informed nursing practice. OJIN: The Online Journal of Issues in Nursing, 24(2). https://doi.org/10.3912/ojin.vol24no02man03
- Purkey, E., Patel, R., & Phillips, S. P. (2018). Trauma informed care better care for everyone. Canadian Family Physician, 64(3), 170–172.
- Schulman, M., & Menschner, C. (2018, November 9). Laying the groundwork for trauma-informed care [PDF]. Trauma-Informed Care Implementation Resource Center. https://www.traumainformedcare.chcs.org/wp-content/uploads/2018/11/Brief-Laying-the-Groundwork-for-TIC.pdf
- Sweeney, A., & Taggart, D. (2018). (Mis)understanding trauma-informed approaches in mental health. Journal of Mental Health, 27(5), 383–387. https://doi.org/10.1080/09638237.2018.1520973
- National Institute on Aging. (2021) What is Lewy Body Dementia? Causes, Symptoms, and Treatments. Retrieved on December 5, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/what-lewy-body-dementia-causes-symptoms-and-treatments
- Medline Plus [Internet] National Library of Medicine. (2021). Dementia with Lewy Bodies. Retrieved on December 5, 2023, from https://medlineplus.gov/genetics/condition/dementia-with-lewy-bodies/#causes
- Haider, A., Spurlin, B., and Sanchez-Manso, J. (2023). Lewy Body Dementia. In StatPearls. StatPearls [Internet]. Retrieved on December 7, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK482441/
- Prasad, S., Katta, M., Abhishek, S., Sridhar, R., Valisekka, S., Hameed, M., Kaur, J., and Walia, N. (2022). Disease-a-Month. Vol. 69, Issue 5, May 2023, 101441. Retrieved from https://www.sciencedirect.com/science/article/pii/S0011502922001250?via%3Dihub
- Medline Plus [Internet] National Library of Medicine. (2019). Lewy Body Dementia. Retrieved on December 7, 2023, from https://medlineplus.gov/lewybodydementia.html
- Hershey, L. and Coleman-Jackson, R. (2019). Pharmacological Management of Dementia with Lewy Bodies. Drugs Aging. 2019; 36(4) 309-319. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6435621/
- National Institute on Aging. (2018). Caring for a Person with Lewy Body Dementia. Retrieved on December 21, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/caring-person-lewy-body-dementia
- Capouch, S., Farlow, M., and Brosch, J. (2018). A Review of Dementia with Lewy Bodies’ Impact, Diagnostic Criteria and Treatment. Neurology and Therapy. 2018 Dec; 7(2): 249-263. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6283803/
- Lewy Body Dementia Resource Center. (2021) Our Mission & Vision. Retrieved on December 21, 2023, from https://lewybodyresourcecenter.org/about-us/mission/
- Lewy Body Dementia Association. (2023). About LBDA. Retrieved on December 20, 2023 from https://www.lbda.org/about-lbda/
- National Institute of Neurological Disorders and Stroke. (2023) Focus on Lewy BOdy Dementia (LBD). Retrieved on December 20, 2023, from https://www.ninds.nih.gov/current-research/focus-disorders/alzheimers-disease-and-related-dementias/focus-lewy-body-dementia-lbd-research
- National Institute of Neurological Disorders and Stroke. (2018). PDBP About. Retrieved on December 21, 2023, from https://pdbp.ninds.nih.gov/about
- Bousiges, O. and Blanc, F. (2022). Biomarkers of Dementia with Lewy Bodies: Differential Diagnostic with Alzheimer’s Disease. International Journal of Molecular Sciences. 2022 Jun; 23 (12): 6371. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9223587/
- Howell, M. and Schenk, C. Rapid Eye movement sleep behavior disorder. 2023) UpToDate. Retrieved on December 21, 2023 from https://www.uptodate.com/contents/rapid-eye-movement-sleep-behavior-disorder/print#:~:text=INTRODUCTION%20Rapid%20eye%20movement%20(REM,thrashing%2C%20punching%2C%20and%20kicking.
- Arevalo, I., Smailagic, N., Roque I Figuls, M., Ciapponi, A., Sanchez-Perez, E., Giannakou, A., Pedraza, O., Cosp, X., and Cullum, S. (2015). Mini-Mental State Examination (MMSE) FOR THE DETECTION OF Alzheimer’s disease and other dementia in people with milk cognitive impairment (MCI). Cochrane Library. 2015 Mar; 2015(30): CD010783. Retrieved from https://doi.org/10.1002/14651858.CD010783.pub2
- National Institute on Aging. (2021). Diagnosing Lewy Body Dementia: For Professionals. Retrieved on December 22, 2023, from https://www.nia.nih.gov/health/lewy-body-dementia/diagnosing-lewy-body-dementia-professionals
- Anders, H., Ramesh, S., Ming-hui, Z., Ioannis, P., Salmon, J. E., & Mohan, C. (2020). Lupus nephritis (Primer). Nature Reviews: Disease Primers, 6(1). https://doi.org/10.1038/s41572-019-0141-9
- Arnaud, Laurent., & Vollenhoven, R. van. (2018). Advanced handbook of systemic lupus erythematosus. Adis. https://doi.org/10.1007/978-3-319-43035-5
- Hailemariam, F., Falkner, B. (2022). Renal Physiology for Primary Care Clinicians. In: McCauley, J., Hamrahian, S.M., Maarouf, O.H. (eds) Approaches to chronic kidney disease. Springer, Cham. https://doi.org/10.1007/978-3-030-83082-3_1
- Jaryal, A., & Vikrant, S. (2017). Current status of lupus nephritis. The Indian journal of medical research, 145(2), 167–178. https://doi.org/10.4103/ijmr.IJMR_163_16
- Kalantar-Zadeh, K., Mitch, W.E., Fadem, S.Z. (2022). Diet to preserve kidney function. In: Fadem, S.Z. (eds) Staying Healthy with Kidney Disease. Springer, Cham. https://doi.org/10.1007/978-3-030-93528-3_7 Maarouf, O.H. (2022). Lupus nephritis. In: McCauley, J., Hamrahian, S.M., Maarouf, O.H. (eds) Approaches to Chronic Kidney Disease . Springer, Cham. https://doi.org/10.1007/978-3-030-83082-3_10
- Parodis, I., & Sjöwall, C. (Eds.). (2023). Clinical Features and Long-Term Outcomes of Systemic Lupus Erythematosus. MDPI – Multidisciplinary Digital Publishing Institute.
- Pryor, K. P., Barbhaiya, M., Costenbader, K. H., & Feldman, C. H. (2021). Disparities in Lupus and Lupus Nephritis Care and Outcomes Among US Medicaid Beneficiaries. Rheumatic diseases clinics of North America, 47(1), 41–53. https://doi.org/10.1016/j.rdc.2020.09.004
- Usman N, Annamaraju P. (2023). Type III hypersensitivity reaction. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559122/
- Harris, J.C., Leggio, L., Farokhnia, M. (2021). Blood biomarkers of alcohol use: a scoping review. Current Addiction Reports, 8(4), 500-508. https://doi.org/10.1007/s40429-021-00402-7
- Johns Hopkins Medicine. (2023). CAGE substance abuse screening tool. Retrieved from: https://www.hopkinsmedicine.org/-/media/johns-hopkins-health-plans/documents/all_plans/cage-substance-screening-tool.pdf
- Nathan, P.E., Wallace, J., Zweben, J., Horvath, A. T. (2018). Understanding alcohol use disorders and their treatment. Retrieved from: https://www.apa.org/topics/substance-use-abuse-addiction/alcohol-disorders.
- National Cancer Institute. (2021). Alcohol and cancer risk. Retrieved from: https://www.cancer.gov/about-cancer/causes-prevention/risk/alcohol/alcohol-fact-sheet.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Alcohol’s effects on the body. Retrieved from: https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Goal 3: prevention. Retrieved from: https://www.niaaa.nih.gov/strategic-plan/prevention.
- National Institute on Alcohol Abuse and Alcoholism. (2023). Understanding alcohol use disorder. Retrieved from: https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder.
- National Institute on Drug Abuse. (2023). AUDIT. Retrieved from: https://nida.nih.gov/sites/default/files/files/AUDIT.pdf.
- Nehring, S.M., Chen, R. J., Freeman A.M. (2023). Alcohol use disorder. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK436003/.
- Substance Abuse and Mental Health Services Administration, National Institute on Alcohol Abuse and Alcoholism. (2015). Medication for the treatment of alcohol use disorder: a brief guide. Retrieved from: https://store.samhsa.gov/sites/default/files/sma15-4907.pdf.
- Thompson, W., Lande, R. G., Kalapatapu, R.K. (2020). What are the DSM-5 criteria for alcohol use disorder? Retrieved from: https://www.medscape.com/answers/285913-41535/what-are-the-dsm-5-criteria-for-%20alcohol-use-disorder?form=fpf.
- World Health Organization. (2023). AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. Retrieved from: https://www.who.int/publications/i/item/WHO-MSD-MSB-01.6a.
- American Nurses Association (ANA). (2015). Code of ethics with interpretative statements. https://www.nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/
- Baptiste, D. L., Caviness-Ashe, N., Josiah, N., Commodore-Mensah, Y., Arscott, J., Wilson, P. R., & Starks, S. (2022). Henrietta Lacks and America’s dark history of research involving African Americans. Nursing Open, 9(5), 2236–2238. https://doi.org/10.1002/nop2.1257
- Barrow, J. M., Brannan, G. D., & Khandhar, P. B. (2022, September 18). Research ethics. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK459281/
- Centers for Disease Control and Prevention. (2024, September 4). The untreated syphilis study at Tuskegee timeline. https://www.cdc.gov/tuskegee/about/timeline.html
- Christman, E., Christman, T., Demaster, V. Ernstmeyer, K., Kliminski, K., Olson, A., Pomietlo, M., Roesler, A., Stewart, J., Teeter, J., Tyznik, A. & Zwicky, J. (2022). Chapter 6: Ethical practice. In K. Ernstmeyer & E. Christman (Eds.), Nursing management and professional concepts [Internet]. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/nursingmpc/chapter/6-3-ethical-dilemmas/
- Haddad, L. M., & Geiger, R. A. (2023, August 14). Nursing ethical considerations. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. https://www.ncbi.nlm.nih.gov/sites/books/NBK526054/0
- John Hopkins Medicine. (n. d.). The legacy of Henrietta Lacks. https://www.hopkinsmedicine.org/henrietta-lacks
- Office of Science Policy, National Institutes of Health. (2022, October). Significant research advances enabled by HeLa cells. https://osp.od.nih.gov/hela-cells/significant-research-advances-enabled-by-hela-cells/
- Olejarczyk, J. P., & Young, M. (2024, May). Patient rights and ethics. In: StatPearls [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK538279/
- Shea, B. (2023, October 18). Four principles of bioethics. In Ethical explorations: Moral dilemmas in a universe of possibilities. Minnesota Libraries Publishing Project; Rochester, MN. https://mlpp.pressbooks.pub/ethicalexplorations/chapter/chapter-12-bioethics12/
- Tobin, M. J. (2022). Fiftieth anniversary of uncovering the Tuskegee syphilis study: The story and timeless lessons. American Journal of Respiratory and Critical Care Medicine, 205(10), 1145–1158. https://doi.org/10.1164/rccm.202201-0136SO
- Bella. (2023, July 6). The top 10 list of Medical Interpreter Services in the USA – TLD. The Language Doctors. https://thelanguagedoctors.org/list-of-medical-interpreter-services-united-states/
- Niven, A. (n.d.). OD FAQs-translators and interpreters. OD FAQs-Translators and Interpreters. https://www.ncihc.org/faq-translators-and-interpreters#:~:text=A%20healthcare%20interpreter%20is%20one,clinics%2C%20and%20public%20health%20presentations
- Al Shamsi H, Almutairi AG, Al Mashrafi S, Al Kalbani T. Implications of Language Barriers for Healthcare: A Systematic Review. Oman Med J. 2020 Apr 30;35(2): e122. Doi: 10.5001/omj.2020.40. PMID: 32411417; PMCID: PMC7201401.
- Diving into the world of a medical interpreter. The World of a Medical Interpreter | Medical Interpreter Certification | Kent State MCLS. (n.d.). https://www.kent.edu/appling/matranslationonline/blog/world-of-a-medical-interpreter
- Sellers, J. (2023, December 27). How does medical interpreting work? Certified Languages International. https://certifiedlanguages.com/blog/how-does-medical-interpreting-work/
- Certified medical interpreter NBCMI candidate handbook. (n.d.). https://www.certifiedmedicalinterpreters.org/assets/docs/NBCMI_Handbook.pdf?v=20231011
- Certification Commission for healthcare interpreters: National, accredited, inclusive. CCHI. (n.d.). https://cchicertification.org/
- Martinez-Morales, C. (n.d.). Home. THE NATIONAL BOARD OF CERTIFICATION FOR MEDICAL INTERPRETERS. https://www.certifiedmedicalinterpreters.org/
- Antoine, R. (2023, May 18). How to become a Certified Medical Interpreter. InterpreterEd.com. https://interpretered.com/how-to-become-a-certified-medical-interpreter/#:~:text=A%20medical%20interpreter%20handles%20communication,between%20patients%20and%20medical%20staff.
- Fact sheet – cchicertification.org. (n.d.-b). https://cchicertification.org/uploads/CCHI_Factsheet.pdf
- Interpreter certification. CCHI. (n.d.-b). https://cchicertification.org/healthcare-administrators/certification-info/
- Of practice – NCIHC. (n.d.-c). https://www.ncihc.org/assets/z2021Images/NCIHC%20National%20Standards%20of%20Practice.pdf
- medical-interpretation-and-the-law-regulations-in-the-us-ebook.pdf. United Language Group. (n.d.). https://info.unitedlanguagegroup.com/hubfs/-%20ULG%20-%20Aug%202019/Services/Translation/medical-interpretation-and-the-law-regulations-in-the-us-ebook.pdf
- Wild, C. (n.d.). NBCMI programs – hub-CMI. THE NATIONAL BOARD OF CERTIFICATION FOR MEDICAL INTERPRETERS. https://www.certifiedmedicalinterpreters.org/hub-cmi
- Wild, C. (n.d.-a). NBCMI programs – CMI. THE NATIONAL BOARD OF CERTIFICATION FOR MEDICAL INTERPRETERS. https://www.certifiedmedicalinterpreters.org/nbcmi-program-cmi
- Niven, A. (n.d.-a). Ethics and standards of Practice. Ethics and Standards of Practice. https://www.ncihc.org/ethics-and-standards-of-practice
- Who we are. IMIA. (n.d.-b). https://www.imiaweb.org/about-us/who-we-are/
- International Medical Interpreters Association. IMIA. (n.d.-a). https://www.imiaweb.org/standards/standards.asp
- U.S. Bureau of Labor Statistics. (2023, September 6). Interpreters and translators: Occupational outlook handbook. U.S. Bureau of Labor Statistics.https://www.bls.gov/ooh/media-and-communication/interpreters-and-translators.htm
- Schulson, L. B., & Anderson, T. S. (2020, November 2). National estimates of professional interpreter use in the ambulatory setting – Journal of General InternalMedicine. SpringerLink. https://link.springer.com/article/10.1007/s11606-020-06336-6
- Language and literacy. Language and Literacy – Healthy People 2030. (n.d.). https://health.gov/healthypeople/priority-areas/social-determinants-health/literature-summaries/language-and-literacy
- Wu, S. (2013, July 8). Code of ethics for medical interpreters. Their Words. Your Voice. https://shenyunwu.wordpress.com/2011/10/17/code-of-ethics-for-medical-interpreters/
- (OCR), O. for C. R. (2023, December 12). Example of a policy and procedure. HHS.gov. https://www.hhs.gov/civil-rights/for-providers/clearance-medicare-providers/example-policy-procedure-persons-limited-english-proficiency/index.html
- Kwan, M., Jeemi, Z., Norman, R., & Dantas, J. A. R. (2023). Professional Interpreter Services and the Impact on Hospital Care Outcomes: An Integrative Review of Literature. International journal of environmental research and public health, 20(6), 5165. https://doi.org/10.3390/ijerph20065165
- Sindhu, K. (n.d.). Working with medical interpreters. Wolters Kluwer. https://www.wolterskluwer.com/en/expert-insights/working-with-medical-interpreters
- Squires A. (2018). Strategies for overcoming language barriers in healthcare. Nursing management, 49(4), 20–27. https://doi.org/10.1097/01.NUMA.0000531166.24481.15
- Chen, A. H., Youdelman, M. K., & Brooks, J. (2007). The legal framework for language access in healthcare settings: Title VI and beyond. Journal of General Internal Medicine, 22 Suppl 2(Suppl 2), 362–367. https://doi.org/10.1007/s11606-007-0366-2
- Laws requiring interpreters in healthcare – certificate interpreter training programs® – official site. Certificate Interpreter Training Programs® – Official Site – Medical Interpreter Certificate & Legal Interpreter Certificate Training. (2017, July 9). https://interpretertrain.com/laws-requiring-interpreters-in-healthcare/
- American Association of Colleges of Nursing. (2022). Nursing faculty shortage sheet. https://www.aacnnursing.org/news-data/fact-sheets/nursing-faculty-shortage
- American Association of Colleges of Nursing. (2022). Nursing shortage fact sheet. https://www.aacnnursing.org/news-data/fact-sheets/nursing-shortage
- American Association of Colleges of Nursing – American Organization of Nursing Leaders, Advisory Committee. (2020). AACN-AONL clinical preceptor survey summary report. https://www.aacnnursing.org/Portals/0/PDFs/Data/AACN-AONL-Clinical-Preceptor-Survey-May-2020.pdf
- American Nurses Association. (n. d.). Why nurses quit and leave the profession? https://www.nursingworld.org/practice-policy/nurse-staffing/why-nurses-quit/
- Bloom, B. S. (1956). Taxonomy of educational objectives, handbook 1: The cognitive domain. David McKay Co.
- Childs-Kean, L., Edwards, M., & Smith, M. D. (2020). Use of learning style frameworks in health science education. American Journal of Pharmaceutical Education, 84(7), ajpe7885. https://doi.org/10.5688/ajpe7885
- Figueiredo, L. D. F., Silva, N. C. D., & Prado, M. L. D. (2022). Primary care nurses’ learning styles in the light of David Kolb. Brazilian Journal of Nursing, 75(6), e20210986. https://doi.org/10.1590/0034-7167-2021-0986
- Harper, M., Ulrich, B., MacDonald, R., Maloney, P., Warren, J. I., & Whiteside, D. (2023). Summary findings from the 2023 preceptor competency consensus study. Association for Nursing Professional Development. https://www.anpd.org/Portals/0/Files/ANPD_1127571-23_PreceptorCompetencies_Report.pdf
- Krathwohl, D. R., & Bloom, B. S. (1973). Taxonomy of educational objectives, the classification of educational goals, handbook II: Affective domain. David McKay Co.
- Loughran, M. C., & Koharchik, L. (2019). Ensuring a successful preceptorship. American Journal of Nursing 119(5):61-65. https://journals.lww.com/ajnonline/Fulltext/2019/05000/Ensuring_a_Successful_Preceptorship.32.aspx
- National Advisory Council on Nurse Education and Practice. (2021). Preparing nurse faculty and addressing the shortage of nurse faculty and clinical preceptors. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/nursing/reports/nacnep-17report-2021-508.pdf
- Powers, K., Herron, E., & Pagel, J. (2019). Nurse preceptor role in new graduate nurses’ transition to practice. Dimensions of Critical Care Nursing 38(3):131-136. https://journals.lww.com/dccnjournal/fulltext/2019/05000/nurse_preceptor_role_in_new_graduate_nurses_.4.aspx
- Robinson, C. (2022). Are nurse preceptors the new clinical instructors? MEDSURG Nursing, 31(1): 55-56. https://www.proquest.com/openview/5a19002dc1e28d48a357250377696db8/1.pdf?pq-origsite=gscholar&cbl=30764
- Sherrod, D., Holland, C., & Battle, L. (2020). Nurse preceptors: A valuable resource for adapting staff to change. Nursing Management (Springhouse), 51(3): 50-53. https://journals.lww.com/nursingmanagement/fulltext/2020/03000/nurse_preceptors__a_valuable_resource_for_adapting.9.aspx
- Johnson, R. (2024). Enabling registered nurses, licensed practical and vocational nurses, and assistive personnel to practice to their fullest extent. Critical Care Nurse, 44(2), 64-67. Retrieved fromhttps://doi.org/10.4037/ccn2024809
- More, L., & Parsons, L. (2020). Using innovative education to elevate unlicensed assistive personnel practice. Nursing Economic$, 38(2), 86-91.
- Grover, L., & Fritz, E. (2022). Unlicensed assistive personnel in ambulatory care: A systematic integrative review. Nursing Management, 53(10). https://doi.org/ 10.1097/01.NUMA.0000853232.62593.6f
- Fischer, L. (2022). Structured onboarding processes boost employee retention. Oncology Nursing News, 16(4), 16-19. Retrieved April 5, 2024 from https://cdn.sanity.io/files/0vv8moc6/oncnurse/3196d0c4c3d9b61ef4387f04ee2a33e4678a5232.pdf/ONN_AUGUST2022_FINAL.pdf
- Tooman, J. (2024). Maximizing health care efficiency: Unraveling the art of nursing delegation. Urologic Nursing, 44(1), 38-41. https://doi.org/10.7257/2168-4626.2024.44. 1.38
- Hsu, H., Kung, H., Chiang, W., Lee, B., & Wang, R. (2021). A comparison of nurse aides and nurses regarding the work competence of nurse aides in a skill-mixed institution. Healthcare, 9(12), 1-10. Retrieved from https://doi.org/10.3390/healthcare9121725
- Rothwell, C., Kehoe, A., Farook, S., & Illing, J. (2021). Enablers and barriers to effective clinical supervision in the workplace: a rapid evidence review. BMJ, 11(9), 1-10. Retrieved from http://dx.doi.org/10.1136/bmjopen-2021-052929
- Mistri, I., Badge, A., & Shahu, S. (2023). Enhancing patient safety culture in hospitals. Cureus, 15(12), 1-7. Retrieved from https://doi.org/10.7759/cureus.51159
- Centers for Disease Control and Prevention. (2022). Lyme disease. Retrieved from: https://www.cdc.gov/lyme/index.html.
- Centers for Disease Control and Prevention. (2021). Myalgic encephalomyelitis/chronic fatigue syndrome: IOM 2015 diagnostic criteria. Retrieved from: https://www.cdc.gov/me-cfs/healthcare-providers/diagnosis/iom-2015-diagnostic-criteria.html.
- Centers for Disease Control and Prevention. (2023). Post-treatment Lyme disease syndrome. Retrieved from: https://www.cdc.gov/lyme/postlds/index.html.
- Leland, D.K. (2023). Touched by Lyme. Retrieved from: https://www.lymedisease.org/cdc-chronic-lyme-iaccpac/
- LymeDisease.org. (2023). Chronic Lyme disease. Retrieved from: https://www.lymedisease.org/lyme-basics/lyme-disease/chronic-lyme-disease/.
- Mead, P., Petersen, J., Hinckley, A. (2019). Updated CDC recommendation for serologic diagnosis of Lyme disease. Morbidity and Mortality Weekly Report, 68(32), 703. http://dx.doi.org/10.15585/mmwr.mm6832a4external icon
- National Institute of Allergy and Infectious Diseases. (2018). Chronic Lyme disease. Retrieved from: https://www.niaid.nih.gov/diseases-conditions/chronic-lyme-disease
- National Institute of Neurological Disorders and Stroke. (2023). Studies find that microbiome changes may be a signature for ME/CFS. Retrieved from: https://www.ninds.nih.gov/news-events/press-releases/studies-find-microbiome-changes-may-be-signature-mecfs.
- Rebman, A.W., Bechtold, K.T., Yang, T., Mihm, E.A., Soloski M.J., Novak, C.B., Aucott, J.N. (2017). The clinical, symptom, and quality-of-life characterization of a well-defined group of patients with posttreatment Lyme disease syndrome. Frontiers in Medicine, 4, 224. https://doi.org/10.3389/fmed.2017.00224
- Sapra, A., Bhandari, P. (2023). Chronic fatigue syndrome. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK557676/
- Skar, G.L., Simonsen, K.A. (2023). Lyme disease. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK431066/.
- Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2018. NCHS Data Brief, Number 355. Hyattsville, MD: National Center for Health Statistics; 2020.
- Centers for Disease Control and Prevention. National Vital Statistics System detailed mortality data at the Wonder Database website. http://wonder.cdc.gov.
- Centers for Disease Control and Prevention (2023). COPD Prevalence and Incidence. Retrieved from https://www.cdc.gov/copd/data-and-statistics/national-trends.html
- Jarvis, C. (2024). Physical Examination and Health Assessment. 9th ed. Elsevier Publishing.
- World Health Organization (2018). Chronic Respiratory Diseases: Burden of COPD. Retrieved from http://www.who.int/respiratory/copd/burden/en/
- American Lung Association (2024). Trends in COPD (Chronic Bronchitis and Emphysema): Morbidity and Mortality. Retrieved from https://www.lung.org/lung-health-diseases/lung-procedures-and-tests
- Pietrangelo, A. (2015). COPD by the Numbers: Facts, Statistics, and You. Healthline. Retrieved from https://www.healthline.com/health/copd/facts-statistics-infographic
- American Academy of Allergy, Asthma, and Immunology (2016). Immunologic Insights into Triggers of Asthma. Retrieved from https://education.aaaai.org/asthma-education/2016VAM4305
- Glass, C. (2022). Chronic Obstructive Pulmonary Disease (COPD). Family Practice Guidelines, 5th ed. Springer Publisher Co. New York, NY.
- Mozzafarian,D., Benjamin, E., Go, A., Arnett, D., Blaha, M., Cushman, M., de Ferranti, S., Despres, J., Fullerton, H., e al (2015). Heart disease and stroke statistics- 2015 update: a report from the American Heart Association. Circulation Jan 27;131(4): e29-322. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/25520374
- Kosacz, N. (2012). Chronic Obstructive Pulmonary Disease Among Adults-United States, 2011. Morbidity and Mortality Weekly Report. Centers for Disease
- Control and Prevention. Retrieved from https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6146a2.htm
- Centers for Disease Control and Prevention (2013). National Center for Health Statistics. Behavioral Risk Factor Surveillance Survey, 2011. Analysis performed by the American Lung Association Research and Health Education Division using SPSS software. COPD (2017). Right Diagnosis of COPD. Retrieved from http://www.rightdiagnosis.com/c/copd/intro.htm
- Centers for Disease Control and Prevention (CDC). (2016). Overweight and Obesity. Retrieved from https://www.cdc.gov/obesity/
- Halpin, D. M. G., & Criner, G. J. (2020). Global initiative for the diagnosis, management, and prevention of chronic obstructive lung disease. The 2020 GOLD science committee report on COVID-19 and chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine, 202(2), 156-164. https://doi.org/10.1164/rccm.202005-1589ST
- Guarascio, A., Ray, S., Christopher, K., Self, T. (2013). The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clinical Economics and Outcomes Research. 5:235-245. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3694800/
- Grossman, S., & Porth, C. (2014). Porth’s pathophysiology: concepts of altered health states. Ninth Edition. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
- National Heart, Lung, and Blood Institute (2018). COPD Action Plan. Retrieved from
- https://www.nhlbi.nih.gov/health-topics/education-and-awareness/COPD-national-action-plan
- Global Initiative for Chronic Obstructive Lung Disease. (2020). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2020 report. Retrieved from https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf
- NCQA.org (2016). Incorporating HEDIS Measures and Newer Therapies to Improve COPD Treatment Adherence and Outcomes. Retrieved from http://www.ncqa.org/education-events/seminars-and-webinars/live-seminars-webinars/improving-copd-treatment-adherence-and-outcomes
- Global strategy for asthma management and prevention (2015). Global Initiative for Asthma (GINA). Retrieved from: http://www.ginasthma.org/
- Brusasco, V. and Pellegrino, R. (2016). “Spirometry in Chronic Obstructive Pulmonary Disease. From Rule of Thumb to Science”, American Journal of Respiratory and Critical Care Medicine, Vol. 193, No. 7 (2016), pp. 704-706. doi: 10.1164/rccm.201511-2239ED. https://www.cdc.gov/copd/index.html
- U.S. Department of Health and Human Services: Healthy People 2020. U.S. Government Printing Office, Washington, DC, 2020. Retrieved from
- https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Clinical-Preventive-Services
- National Heart, Lung, and Blood Institute. What is Respiratory Failure? Retrieved from https://www.nhlbi.nih.gov/health/respiratory-failure#:~:text=Respiratory%20failure%20is%20a%20serious,made%20in%20the%20body’s%20cells.
- Lopez-Campos, J. L., Tan, W., Soriano, J. B. (2016). Global burden of COPD. Respirology, 21(1), 14-23. https://doi.org/10.1111/resp.12660
- Kory, P., & Pellegrino, E. (2018). Treatment of acute exacerbations of chronic obstructive pulmonary disease. American Family Physician, 98(12), 739-745. https://www.aafp.org/afp/2018/1215/p739.html
- Rochester, C. L., Vogiatzis, I., & Holland, A. E. (2017). An official American Thoracic Society/European Respiratory Society policy statement: Enhancing implementation, use, and delivery of pulmonary rehabilitation. American Journal of Respiratory and Critical Care Medicine, 195(11), 1523-1533. https://doi.org/10.1164/rccm.201704-0785ST
- Criner, G. J., Bourbeau, J., Diekemper, R. L., Ouellette, D. R., Goodridge, D., Hernandez, P., Curren, K., Balter, M. S., Bhutani, M., Camp, P. G., Celli, B. R., Dechman, G., Dransfield, M. T., Fiel, S. B., Foreman, M. G., Hanania, N. A., Ireland, B. K., Marchetti, N., … & Varela, M. V. (2015). Executive summary: Prevention of acute exacerbation of COPD: American College of Chest Physicians and Canadian Thoracic Society guideline. Chest, 147(4), 883-893. https://doi.org/10.1378/chest.14-1677.
- Tan Y, Van den Bergh O, Qiu J, von Leupoldt A. The Impact of Unpredictability on Dyspnea Perception, Anxiety, and Interoceptive Error Processing. Front Physiol. 2019 May 3; 10:535. doi: 10.3389/fphys.2019.00535. PMID: 31130876; PMCID: PMC6509155.
- Wiki Images. (n.d.). COPD. Wikimedia https://commons.wikimedia.org/wiki/File:Copd.JPG
- Wiki Images. (n.d.). Asthma: Before and after. https://commons.wikimedia.org/wiki/File:Asthma_before-after.png#/media/File:Asthma_before-after.png
- Wiki Images. (n.d.) Spirometry NIH. https://commons.wikimedia.org/wiki/File%3ASpirometry_NIH.jpg
- Wiki Images. (n.d.). COPD. Wikimedia. Flow Volume Curve. https://commons.wikimedia.org/wiki/Category:Chronic_obstructive_pulmonary_disease#/media/File:Spirometry.png
- Wiki Images. (n.d.). COPD. Wikimedia. Peak flow meters for home use. https://commons.wikimedia.org/wiki/File%3ATwo_Peak_Flow_Meters.jpg
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate