Course
New York APRN Bundle
Course Highlights
- In this New York APRN Bundle, you will learn how to determine if a child shows indicators of maltreatment or abuse, including in a virtual setting.
- You’ll also learn to understand strategies for preventing transmission of pathogenic organisms; and describe how infection control concepts are applied in professional health practice.
- You’ll leave with a better understanding of how to apply state and federal laws on prescribing New York (NY) controlled substances.
About
Contact Hours Awarded:
8
Pharmacology Contact Hours Awarded: 3
Course By:
Various Authors
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
NY Identification and Reporting of Child Abuse
Pre-Evaluation
Please complete the evaluation below prior to reading any of the course material.
Introduction
Child abuse and neglect happen across the country, affecting 1 in 7 children in the United States each year. Among the states with the highest rates of child abuse is New York, with an annual rate of abuse double that of the national average. In addition to this gut-wrenching statistic, the actual occurrence of abuse is believed to be underreported. The purpose of this course is to provide education to mandated reporters about risk factors, recognition, and reporting of abuse and to hopefully increase awareness of this tragic problem and reduce the number of children who are victims of harm.
New York State’s Child Welfare Practice Model
Excerpt from the CPS Manual (12)
“New York State’s Child Welfare Practice Model establishes a consistent and recognizable approach to child welfare practice across New York State. Children, families, and adults are protected and supported to achieve safety, permanency, and well-being.
The Practice Model is founded on these values:
- We believe children and adults have the right to be safe, and to have permanent families and lasting relationships.
- We listen first, then learn and proceed with knowledge, focusing on the individual and family resources and strengths.
- We believe that services for children, families, and adults must be individualized and culturally competent, recognizing, and honoring differences in traditions, heritage, values, and beliefs.
- We approach our work with a sense of urgency and persistence, recognizing and respecting a child and family’s sense of time.
- We believe that high-performing supervisors and caseworkers are key to building and sustaining an effective child welfare system.
- We value interagency collaboration.
- We believe in accountability for action and results.
- We strive for data-informed decision-making.
- We value the principles of partnership:
- Everyone desires respect.
- Everyone needs to be heard.
- Everyone has strengths.
- Judgments can wait.
- Partners share power.
- Partnership is a process.”
Epidemiology- Current Patterns of Abuse in New York
Every year across the United States, nearly 700,000 children are abused or neglected in families of all racial, ethnic, and socioeconomic backgrounds. Abuse and neglect encompass many situations that cause physical, mental, or emotional harm through intentional acts of maltreatment or failing to meet a child’s basic needs to the point of endangering their overall health and well-being (8).
Any person under the age of 18 can be a victim of child abuse, but very young children are most at risk, and abuse commonly occurs during the first 2 years of life when they are not yet highly verbal. Nationally, around 75% of deaths from child abuse occur in children under the age of 3. Children are affected nearly equally across genders. The abuser is a parent or guardian over 78% of the time (1).
Neglect is the most common form of abuse, accounting for 60.8% of confirmed abuse cases nationally. Physical abuse accounts for 10.7% of cases, sexual abuse occurs 7% of the time, and emotional/psychological abuse occurs 2.3% of the time. Often, children experience two or more types of abuse (8).
The occurrence of abuse varies by state, and unfortunately, New York leads by nearly double the national rate of child abuse, with 17 children per 1,000 being the victim of some form of abuse in 2017. Even the New York County with the lowest rate of abuse, Saratoga, with 12.7 children per 1,000 affected, is still over 3 points higher than the national average. The worst county in the state is Montgomery, with a staggering rate of 34.3 children per 1,000 (10).
A 2017 analysis from the Child Welfare League of America identified 156,994 reports of child abuse and neglect in New York and reported that over 20,000 children were living separately from their families due to removal from the home following abuse or neglect (5).
The effects of child abuse are far-reaching; in addition to the obvious physical injuries and health problems, childhood victims of abuse are more likely to suffer from psychological issues such as anxiety, depression, chronic fear, and difficulty forming intimate relationships for the rest of their lives. Behavioral problems such as poor academic achievement, substance abuse, crime, teen pregnancy, and delinquency are increased in abuse victims as well, and the state of New York spends an estimated $2.4 billion per year on child welfare, law enforcement, and healthcare-related costs (9).

Self-Quiz
Ask Yourself...
- Think about the population you work with. Who is most at risk?
- What factors put young children at such a high risk of abuse?
- Consider the long-term effects of abuse on children. Why do you think people who have been victims of abuse as children are more likely to abuse their own children?
Defining Child Abuse and Neglect
To be an effective mandated reporter in the state of New York, you must have a clear understanding of who is involved in a child abuse situation and what is considered abuse or neglect. Abuse and neglect/maltreatment do have differing criteria, but it is up to the caseworker to investigate the report to determine where each situation falls. As a mandated reporter, you just need to know what sorts of scenarios warrant reporting, and the investigators will take care of the rest.
Definitions of particular importance include:
Child
A child is any individual after birth and up to the age of 18. Individuals under age 21 with certain disabilities who live in New York residential care facilities are also considered children under New York law (6).
Perpetrator
A perpetrator is anyone over the age of 18 who has been legally entrusted with the care of a child or children and knowingly causes harm to them through their actions or inactions. Most often, a perpetrator is a parent or legal guardian, but they can also include other relatives who live in the home, regular babysitters or nannies, or foster parents.
Individuals who cause harm to a child but are not legally responsible for their care are liable for different types of criminal charges but cannot be the subjects of a report. In the state of New York, this most often includes people like teachers or church personnel (6).
Abuse
Abuse is when a perpetrator inflicts or knowingly allows another person to inflict physical harm onto a child, causing serious injury or risk of death. This can include but is not limited to injuries such as burns, head trauma, fractures, or internal organ damage. It can also be considered an abusive situation if a person creates an environment that puts the child at great risk of serious injury or death, even if serious injury or death do not occur. Sexual acts are also included, such as rape, forcible touching, genital mutilation, or promoting or forcing sexual performance by a child (6).
Neglect and Maltreatment
Perhaps less immediately or life-threateningly dangerous, but still reportable, are neglect and maltreatment situations, which include:
- Anything that impairs (or risks impairment of) a child’s physical, mental, or emotional wellbeing.
- A failure to provide minimal standards of care such as food, shelter, clothing, medical attention, schooling, or supervision.
- Infliction of corporal punishment
- Creating an environment that is unsafe or unable to meet a child’s needs due to the misuse of drugs or alcohol by the parent or guardian.
- Abandonment (6)
It should be noted that physical discipline is legal in New York and that reports are only required for excessive or corporal punishment. Discipline is considered excessive or corporal punishment if it is severe or brutal, inappropriate for a child’s age/size, degrading to the child, outlasting a child’s endurance, or gratifying a parent’s rage (6).


Self-Quiz
Ask Yourself...
- Have you ever cared for a child who was a victim of abuse or neglect? What category did their situation fall under?
- Why might neglect or maltreatment be less obvious or more difficult to detect than abuse?
Identifying Child Abuse and Neglect
In addition to understanding what constitutes child abuse or neglect, mandated reporters need to be able to identify common signs or indicators that abuse has occurred or is occurring. Sometimes, abuse may be obvious and unquestionable; more often, however, the situation will be more subtle and require you to notice several indicators and combine them with your professional expertise.
There are three main types of indicators to be aware of, discussed below:
Child’s physical indicators
These indicators include bruises, fractures, lacerations, and other injuries to a child’s body that are inconsistent with typical childhood injuries or likely to require intentional force to occur. The location, size, and shape of bruises are important to consider; children commonly have bruises to bony prominences like elbows, knees, and shins from running and playing. Bruises over soft tissue like the buttocks, back, or the face and neck or bruises with clearly outlined shapes of a hand or household object are less common with typical play and are more suspicious. The types and mechanism of injury will vary with age. A child’s development should be considered and compared with the story of how an injury occurred and what types of injuries are likely to be accidental versus intentional. Also, pay close attention to children who have poor hygiene, dirty clothing, are always hungry, or frequently tired (2).
Child’s behavioral indicators
Do not assume that children will tell you if they are in an abusive situation. Often, children are afraid of retaliation from their abusers and will not report abuse to an adult, or they are too young to communicate or don’t even know that they can ask for help. You will need to be in tune with a child’s behavior in relation to their development and understand what behaviors raise suspicion for abuse. Children who are wary of adults (outside of the normal separation anxiety phase around 9-18 months), frequently falling asleep in class, hoarding or stealing food, behavioral regressions (toileting accidents, thumb sucking, etc.), change in sleeping or eating habits, withdrawn or overly quiet, anger or aggressive outbursts, delinquency, and drug abuse are all among behaviors to consider as potential red flags (2).
Virtual Settings
This is specific for providers or teachers that provide services to children through telehealth. Most of the signs will be the same, but you will have to be more intentional in your questioning and use critical thinking since sometimes you may have less one-on-one time with a child than in a face-to-face setting.
Other things to consider:
- Does the child frequently miss class/appointments because of a lack of internet or limited access to technology?
- Are they afraid to speak when their parent/caregiver is around?
- Attempts to reach parent/caregiver go unanswered.
- You hear yelling or screaming in the household.
- There is evidence that there may be illicit drug or alcohol use in the home and that the parents or even child are under the influence, etc. (14).
Perpetrator’s behavioral indicators
Attention must also be given to the behavior of the adult who is suspected of inflicting the abuse. Inconsistent stories or details of how an injury occurred, lack of concern for or delay in seeking care for a child’s injuries, talks negatively about the child (such as bad, mean, evil, etc.) are all suspicious for abuse. Consideration must also be given to a personal history of the parent of mental illness, substance abuse, or being abused as a child themselves. In general, if a story is not very believable or keeps changing, it should be regarded with a high amount of suspicion (2).
In any situation where you notice some of the above indicators or a child or parent gives you suspicious information, or your own clinical judgment raises concern, you have reasonable cause to suspect and are required to make a report. It is important to note that you do not have to have proof and that your own mistrust of a situation is enough to make a report in good faith. Even if you think or know another person has made a report regarding the same scenario, you still need to make your own report. This may not only help build a case against a potential abuser but may also offer a different perspective or additional information that others have not yet reported (9).
Whenever you suspect abuse or neglect, it may often be helpful to have a conversation with the child, if they are old enough, to gather more information. Remember that you are just trying to gather more information to add to your current assessment, but not trying to interrogate the child or investigate beyond the issue in front of you. When talking with children, be open and honest, let them know you are there to help, find a private place for the conversation, and listen while remaining calm. Particularly in the case of sexual abuse, it may be difficult or traumatizing for children to relive the details and so keep your conversation brief and to the point (2).
Case Study
A 6-year-old child is brought to the pediatrician for a wellness check. While the nurse is gathering vitals on the child, the mother apologizes for all of the bruises on the child’s shins and states she doesn’t even know how he got them. The child laughs and says he falls off his bicycle sometimes.

Self-Quiz
Ask Yourself...
- Is this situation presented in the case study concerning abuse? Why or why not?
New York Child Protective Services
New York passed its Child Protective Services Act in 1973 which standardized criteria for the reporting and handling of investigations of child abuse and made these regulations into statewide law (10).
The main regulations outlined by this act include:
- Definition of a mandated reporter, duties of mandated reporters, and a detailed list of professions that fall under this mandate. This list is updated regularly.
- Creation of the State Central Register (SCR), a 24/7 statewide program operated by the New York State Office for Children and Family Services that receives reports of child abuse and neglect and passes them on appropriately.
- Establishment of local Child Protective Service (CPS) departments that receive registered reports from SCR and delegate them to CPS officers who investigate and handle the allegations from there (11).
The purpose of the CPS Act is to create a reliable and smoothly operating process for suspected abuse to be reported, documented, and investigated in the hopes of properly identifying abuse cases and preventing further harm from coming to affected children. It also helps to connect children, abusers, and family units with the resources needed to properly rehabilitate them and minimize long-term healthcare outcomes (11).

Self-Quiz
Ask Yourself...
- Why is a statewide protocol for reporting abuse allegations necessary?
- Additionally, why do you think investigation and action on reports is delegated to the local level?
Role of Mandated Reporters
So, what exactly is a mandated reporter, and who falls under this definition?
Anyone who witnesses or suspects abuse at any time may report it, but there are certain professional capacities that require a person to report any suspected abuse with the goal of keeping children as safe as possible and minimizing overall harm; these are mandated reporters. A comprehensive list is included in section 413 of the Social Services Law and is updated periodically.
In general, professions that are likely to come in contact with children or be at least somewhat responsible for the wellbeing of children, and are therefore mandated reporters, include (9):
- Healthcare workers- doctors, nurses, NPs, PAs, dentists, etc.
- School personnel- teachers, social workers, guidance counselors, administrators, school nurses, etc.
- Childcare or children’s program personnel- Daycare providers, church employees, camp counselors, etc.
Law enforcement and legal professionals- police officers, investigators, attorneys, etc.
When to Call the Statewide Central Register (SCR)
A comprehensive list is included in section 413 of the Social Services Law and is updated periodically. Those professionals who fall under the definition of mandated reporters are required to make a report to SCR any time that they are operating in a professional capacity and encounter a child they have reasonable cause to suspect is being maltreated.
The same requirement also applies any time a mandated reporter encounters someone they believe may be abusing a child or endangering them. Reports should be made immediately once suspicions arise. Mandated reporters are not required to report potential abuse scenarios they encounter when they are not working, though they would still be encouraged to report the incident on a “non-mandated” basis (9).
Case Study
Imagine you are a nurse working in an ED setting. Your patient is a 32-year-old woman who presents with a migraine. She brings her 4-year-old child with her until the child’s father can pick him up. The child is withdrawn, and the mother seems to have a poor attachment to him. She belittles him and tells him she wouldn’t get headaches and have to go to the hospital if he wasn’t such a bad kid. At one point, you note a large fading bruise on the back of his right arm. The father comes to pick up the child, and you continue on with the mother’s care.

Self-Quiz
Ask Yourself...
- Are you required to report the above scenario as potential child abuse?
- Why or why not?
- What about if this scenario had taken place at a playgroup meeting at the park and, instead of caring for this mother as a patient, she was a fellow parent who brought her child to play when you noticed the bruise and their poor relationship?
What to Expect When You Make a Report
For any mandated reporter who needs to call in suspected abuse, there is a specific hotline (1-800-635-1522) that may be called 24/7. There is also a hotline for non-mandated reporters (1-800-342-3720). You should call the line that best describes which capacity you are in when making the report (10). If you believe the child is in imminent danger, call 911.
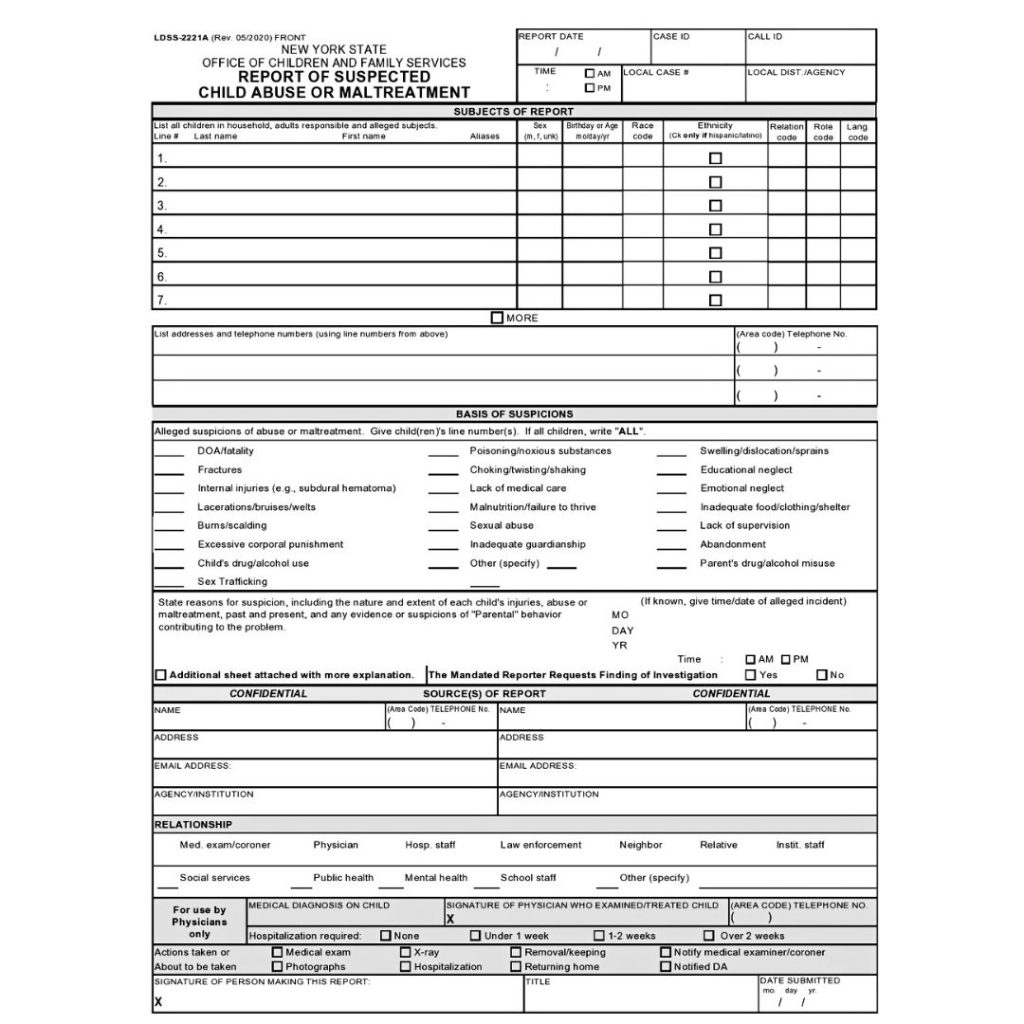
All pertinent information should be gathered and readily available to make the call go as smoothly as possible. A written form (called LDSS-2221A) is available on the New York CPS website that can help gather all the necessary information. This paperwork must also be filled out and submitted within 48 hours of registering a verbal report (11).
Once connected with an agent, you will need to describe the child’s demographics, the scenario, and details that make you suspicious of abuse, the relationship of the person responsible for the suspected abuse, and where the child is now (11).
After information about the incident has been provided, the CPS agent will make one of three actions (11):
Report not registered
If the situation does not qualify for abuse, neglect, or maltreatment, a report may not be registered, and it may be recommended that the reporter connect the family with their local CPS department for services that may benefit them.
Law Enforcement referral
If the situation warrants immediate intervention by the police, such as if a crime is being committed or the child is in imminent danger, then the situation is reported to law enforcement. These situations are not registered as a report.
Report registered
If the situation meets the criteria for abuse, neglect, and maltreatment and does not require emergency action, it is registered as an official report and handed off to the appropriate local CPS agent for further investigation.
Once a report is registered, the local CPS agent will begin an investigation within 24 hours. During the investigation, the CPS agent will determine if the case is founded or unfounded (9).
- Unfounded reports are sealed and remain on record for ten years, after which they are expunged.
- Founded reports have 60 days for a plan of action to be created. CPS agents determine what sort of services, if any, a family should be connected with to improve the safety of the child or if removal from the home is warranted. Monitoring of these cases is ongoing.
Whenever a report is made, the caller is given a call ID number and can track the case’s progress at any time.

Self-Quiz
Ask Yourself...
- What sort of situation do you think would be considered imminent danger?
- Why do you think an imminent danger case gets referred to the police rather than registered as an official report?
- What sort of actions could be included in the plan for a founded report in order to improve the safety of a child’s home?
LDSS-2221A Form
The Report of Suspected Child Abuse or Maltreatment form known as LDSS-2221A, has several important elements that must be completed for the SCR to determine what actions need to be taken.
(12)
Section Breakdown
- List all children in the household, adults responsible, and alleged subjects.
- First and Last Name and known aliases.
- Sex
- Birthday or Age
- Race Code
- Ethnicity
- Relation Code
- Role Code
- Language Code
- List addresses and telephone numbers
- Basis of Suspicions
- The reporter will write the number of the child (from the list above) beside the following alleged suspicions, if all children, write all
- DOA/fatality
- Fractures
- Internal Injuries (e.g., subdural hematoma)
- Lacerations/bruises/welts
- Burns/scalding.
- Excessive corporal punishment
- Child’s drug/alcohol use
- Sex Trafficking
- Poisoning/noxious substances
- Choking/twisting/shaking
- Lack of medical care
- Malnutrition/failure to thrive.
- Sexual abuse
- Inadequate guardianship
- Swelling/dislocation/sprains
- Educational neglect
- Emotional neglect
- Inadequate food/clothing/shelter
- Lack of supervision
- Abandonment
- Parent’s drug/alcohol misuse
- Other (specify)
- State reasons for suspicion, including the nature and extent of each child’s injuries, abuse, or maltreatment, past and present, and any evidence or suspicions of “Parental” behavior contributing to the problem.
- Form provides space here for the reporter to explain, reporters can add an additional sheet with more information if there is not enough room.
- If the incident occurred on a specific date, provide the Month, Date, and Year
- Source(s) of Report
- The reporter will fill out their personal information in this section. Everything in this section will be strictly confidential but is necessary for CPS to obtain in case they need to contact the reporter for additional information regarding the case.
- Relationship
- This section refers to the reporter’s relationship with the child/children
- Medical examiner/coroner
- Physician
- Hospital staff
- Law enforcement
- Neighbor
- Relative
- Institutional staff
- Social services
- Public health
- Mental Health
- School Staff
- Other (specify)
- For use by Physicians only
- Medical diagnosis of child
- Signature of the physician who examined/treated the child.
- Telephone number
- The following are checkboxes:
- Hospitalization required.
- None
- Under 1 week
- 1-2 weeks
- Over 2 weeks
- Actions taken or about to be taken.
- Medical Exam
- Photographs
- X-ray
- Hospitalization
- Removal/keeping.
- Returning home
- Notify the medical examiner/coroner.
- Notified DA (12).
- Hospitalization required.
Page 2 (codes are explained in this section)
Page 3 provides additional space to write an explanation or provide pertinent information.
Legal Considerations
There are several legalities to consider regarding mandated reporters. The law is designed to protect those doing the reporting and encourage them to do so, even penalizing those who knowingly ignore abusive situations.
The main legal considerations for registering an abuse report include:
Immunity
One of the biggest concerns many mandated reporters have is what sort of liability or retaliation they might face after making a report. The law is very specific in that it protects anyone who makes a report in good faith, even if the investigation does not confirm abuse occurred.
In general, mandated reporters are immune from any legal action taken against them by a suspected abuser or employer who may be angered by the report. If an accused person believes a report was made in “bad faith” or as an attempt to knowingly falsify information that would incriminate them, they will have to prove this to be true in order for action to be taken against the mandated reporter.
Healthcare professionals reporting suspected abuse are not considered to be in violation of patient confidentiality laws either and may share patient information when it is done to protect the health and safety of a suspected victim of abuse. Employers may not keep employees from making reports or retaliate against them after a report has been made (9).
Confidentiality
The Office for Children and Family Services and Child Protective Services must keep the mandated reporter’s identity confidential and not release information about who or where a report came from whenever possible. This is intended to protect the mandated reporter from any negative attention, harassment, or social consequences of registering a report.
Mandated reporters are not required to inform parents when they are making a report, though they may choose to. Certain entities, such as police, attorneys, and other court officials, may request and be given information about who initiated a report in qualifying instances. For healthcare professionals who will need to testify in a court case, their identity cannot usually remain confidential (8).
Penalties
In addition to the protections offered to mandated reporters, there are also consequences for not reporting. Failing to report suspected abuse can be considered a Class A Misdemeanor and is punishable with up to 12 months in jail and/or a $1,000 fine. If serious injury or death befalls a child due to a lack of proper reporting, the mandated reporter can also be sued in civil court for damages or wrongful death.
It is important to remember that mandated reporters are only required to report suspected abuse that they encounter within their job duties and not outside of work or in their personal lives, though reporting even then is still encouraged (9).
Additional Information
Record requests may also be made of healthcare professionals who have made reports. Providing further information from a patient’s chart, including progress notes, records, diagnosis and treatment plans, or additional information about a patient is considered to be part of the SCR report and bypasses HIPAA laws. Providing this additional information is protected under the law as detailed above (9).
It is important to note that in order for the above protections to be upheld and to avoid penalties for not reporting, all reports must be made to the SCR and not to local law enforcement agencies or local social service departments. The SCR is used statewide and will contact local agencies, as necessary. Still, it is their responsibility, not the mandated reporters, to handle those resources once a report has been made (9).
Case Study
A 5-year-old patient is brought to the pediatric office with complaints of arm pain x 1 week. The mother states she was not with him but that he fell out of a swing in the backyard, and she assumed he was fine. When he continued to complain she decided to make an appointment a week later but thinks he is dramatic. She also later says he fell off a slide. An x-ray reveals a radial fracture, and the arm is in a cast.
You make a report to the SCR due to delay in seeking treatment, parental lack of concern, and inconsistent story. The investigation reveals no concern for abuse, and the case is closed. However, the mother is angry that a report was made and asked to speak to the supervisor of the department.

Self-Quiz
Ask Yourself...
- Are you liable for disciplinary action since no abuse was found?
- If the mother called CPS to ask who made the report, would they be required to tell her?
Adverse Childhood Experiences
Adverse Childhood Experiences or ACE is an umbrella term to describe events that had a potentially traumatic impact and that occurred before the individual turned 18 (3).
The CDC reports that approximately 64% of adults in the United States have experienced an ACE These experiences can have long-lasting effects on health, overall wellbeing, access to higher education, and job opportunities. The impact reaches far beyond just the individual, it can affect their family dynamics and can have societal implications. This is why preventing childhood abuse and promoting family stability needs to be a community effort and not just the responsibility of a select few (3).
Potential Impact of ACEs:
- Limited opportunities for higher education
- Limited financial resources
- Less access to job opportunities
- Unsafe sex practices – increased exposure to HIV and other STDs
- Substance and alcohol use
- Increased risk of cancer and diabetes
- Unintended pregnancy
- Mental health disorders such as depression, anxiety, PTSD, and suicidal ideation.
- Traumatic Brain Injury
- Fractures
- Burn injuries (3).
Community Strategies to Prevent ACE
- Increasing opportunities for families to have financial stability.
- Providing education on how to prevent violence and how to approach these situations as a person required to report or person encouraged to report.
- Community Youth Activities
- Early Intervention
- Affordable access to high-quality childcare (3).

Self-Quiz
Ask Yourself...
- What other negative impact can ACEs have on an individual?
- Thinking on community strategies, do you know of any opportunities or activities in your community that could help prevent ACE?
- Do you think that people who have experienced ACE are more likely to be perpetrators in the future? Why or why not?
Protective Factors to Prevent Child Abuse/Neglect
-
Nurturing and Attachment
Creating emotional bonds and attachments between parents and children in the early stages of development is very important. Research shows that this helps promote trust, feelings of love, acceptance, and protection. Children who experience consistent nurturing and attachment experiences tend to have more positive outcomes later in their adult lives (4).
-
Knowledge of parenting for child and youth development
Providing children with consistent, reasonable rules, expectations and opportunities leads to healthy child development that will allow them to succeed later in life. Positive parenting that demonstrates respect and love for children, rather than harsh punishments and unreasonable expectations, can be learned and there are many resources available for parents. (4).
-
Parental resilience
Dealing with the everyday stressors of life and being a parent can be very challenging at times. Learning healthy coping skills, developing resilience, strength and having flexibility when things don’t go quite as we expect them to can make a big difference in how we react towards children. Some people really struggle with this and lash out at their family and children, which is why this is included as a protective factor (4).
-
Social Connections
It really does take a village when it comes to raising children, parents can’t do it all alone. Having a strong support system of family, friends, and neighbors that you can turn to when you need advice or tangible help can really help reduce stress and anxiety. Parents with strong support systems are less likely to mistreat their children (4).
-
Concrete support for parents
This can include food assistance, help with childcare, job assistance programs, housing vouchers, and more. It’s important to connect parents who are in need with support networks and resources that will help them provide for their needs and for the needs of their children (4).
-
Social and emotional competence of children
Modeling how to communicate your emotions in a healthy, effective way, regulate your emotions, and nurture friendships and social connections will help develop social-emotional competence in the child (4).

Self-Quiz
Ask Yourself...
- What resources can you think of that can help parents with protective factor #2?
- What community and state-wide support programs can you think of? Do you think there is a need for more funding and support for these programs?
Special Populations
Limited English Proficiency (LEP)
LEP is defined as the limited ability to speak, read, or write English. It is essential to provide appropriate language assistance services to individuals with limited English proficiency. Healthcare institutions and other entities that receive any kind of federal funding are mandated by law to provide these services when indicated (11).
Indian Child Welfare Act
The purpose of this legislation is to support Native American, Indigenous, and First Nations children’s cultural identity when it comes to foster care placement, parental rights termination, emergency removals due to safety concerns, and adoption. CPS will work with the child’s tribe/nation regarding court proceedings and placements (11).
Immigrant Families
Investigations of suspected abuse or maltreatment will be conducted using the same standards as any other report. Not being a documented citizen is not grounds for the removal of the child or children in the household. CPS and mandated reporters should examine their own biases towards individuals who are not documented citizens and not be judgmental in these sensitive situations (11).

Self-Quiz
Ask Yourself...
- Is the use of qualified medical interpreters encouraged at your place of work? Do you know how to access these services to communicate with your patients?
- Immigrant families are treated with the same standards and guidelines as any other families, prior to reading this lesson, did you think otherwise? Why do you think you had that misconception?
Reducing Bias
Implicit bias is a subconscious attitude or opinion about a person or group of people that has the potential to influence the actions and decisions taken when providing care. Explicit bias is a conscious and controllable attitude (using racial slurs, making sexist comments, etc.) (8).
Before making a report, it is helpful to ask yourself these questions:
- Why am I suspecting abuse, neglect, or mistreatment?
- Is there objective evidence that supports my suspicion?
- Are the families’ values, race, cultural identity, or religion affecting how I perceive this situation? Would I feel the same if the family was more like mine? (13).
Research shows that implicit and explicit bias from healthcare providers exists, with Asian and Hispanic children’s cases of abuse being underreported, and cases of Black children being overrepresented in reports (13).
So how can we help mitigate bias in child abuse reporting? The number one thing we can do is to encourage ongoing and consistent evidence-based implicit bias education. Secondly, having standardized tools, protocols, and guidelines can help caseworkers and mandated reporters make sound decisions using critical thinking. Additionally, we must ensure we try to recognize how our own biases can have an impact on our decisions and work on increasing our knowledge (13).
We do not cover implicit bias at length in this course but do encourage you to seek out courses and training on this subject to increase your knowledge.

Self-Quiz
Ask Yourself...
- Does your workplace require implicit bias training?
- Think about the facility where you work and the different types of clients you encounter each day. Are there certain types of people you assume things about just based on the way they look, their gender, or their skin color?
- In what ways do you think these assumptions might affect the way you care for your patients, even if you keep these opinions internal?
- How do you think you could try and re-frame some of these assumptions?
Resources offered by the NY OFCS: excerpt from CPS Manual
OCFS H.E.A.R.S. – Help, Empower, Advocate, Reassure, and Support is a family line that assists families by providing resources and referrals to a variety of services. Families can call their helpline at 888-554-3277.
NY Project Hope provides emotional support for New York State residents.
Emotional Support Helpline (1-844-863-9314),
Online Wellness Groups, and a website filled with supportive resources (NYProjectHope.org).
The New York State Office for the Prevention of Domestic Violence
Prevent Child Abuse New York also has a prevention and parent helpline available for parents and caregivers. Families can call the helpline at 1-800-CHILDREN.
United Way – families can call 2-1-1, operated by the United Way, for health and human services information, referrals, assessments, and crisis support.
NYS Mandated Reporter site has additional resources
Conclusion
Though child abuse is an uncomfortable topic, most people who work in healthcare will encounter a situation sooner or later that raises concern and requires further action to promote young patients’ safety and well-being. With an improved understanding of who is at risk, key indicators to watch for, what sort of situations warrant reporting, and the reporting process itself, the hope is that abuse situations can be recognized and corrected early on, improving the health and safety of New York’s children as much as possible.
NY Infection Control Training for Nurses
Introduction
Healthcare professionals have the responsibility to adhere to scientifically accepted principles and practices of infection control in all healthcare settings and to oversee and monitor those medical and ancillary personnel for whom the professional is responsible.
The following sections explore the sources and definitions of standards of professional conduct as they apply to infection prevention and control.
Element I
Rules of the Board of Regents, Part 29.2 (a)(13)
New York (NY) law clearly defines the responsibilities of health professionals in having access to products, using, and adhering to scientifically approved techniques for “. . . the cleaning and sterilization or disinfection of instruments, devices, materials and work surfaces, utilization of protective garb, use of covers for contamination-prone equipment and the handling of sharp instruments” (1).
These guidelines and rules are laid out within the Rules of the Board of Regents, Part 29.2 (a)(13). It is the responsibility of nursing to review and execute these standards throughout the healthcare continuum as follows (1):
- Wearing appropriate protective gloves at all times when touching blood, saliva, other body fluids or secretions, mucous membranes, non-intact skin, blood-soiled items or bodily fluid-soiled items, contaminated surfaces, and sterile body areas, and during instrument cleaning and decontamination procedures.
- Discarding gloves used following treatment of a patient and changing to new gloves if torn or damaged during treatment of a patient; washing hands and donning new gloves before performing services for another patient; and washing hands and other skin surfaces immediately if contaminated with blood or other body fluids.
- Wearing appropriate masks, gowns or aprons, and protective eyewear or chin-length plastic face shields whenever splashing or spattering of blood or other body fluids is likely to occur.
- Sterilizing equipment and devices that enter the patient’s vascular system or other normally sterile areas of the body.
- Sterilizing equipment and devices that touch intact mucous membranes but do not penetrate the patient’s body or using high-level disinfection for equipment and devices that cannot be sterilized before use for a patient.
- Using appropriate agents, including but not limited to detergents for cleaning all equipment and devices before sterilization or disinfection.
- Cleaning, by the use of appropriate agents, including but not limited to detergents, equipment, and devices that do not touch the patient or that only touch the intact skin of the patient.
- Maintaining equipment and devices used for sterilization according to the manufacturer’s instructions.
- Adequately monitoring the performance of all personnel, licensed or unlicensed, for whom the licensee is responsible regarding infection control techniques.
- Placing disposable used syringes, needles, scalpel blades, and other sharp instruments in appropriate puncture-resistant containers for disposal; and placing reusable needles, scalpel blades, and other sharp instruments in appropriate puncture-resistant containers until appropriately cleaned and sterilized.
- Maintaining appropriate ventilation devices to minimize the need for emergency mouth-to-mouth resuscitation.
- Refraining from all direct patient care and handling of patient care equipment when the health care professional has exudative lesions or weeping dermatitis, and the condition has not been medically evaluated and determined to be safe or capable of being safely protected against in providing direct patient care or in handling patient care equipment; and
- Placing all specimens of blood and body fluids in well-constructed containers with secure lids to prevent leaking, and cleaning any spill of blood or other body fluid with an appropriate detergent and appropriate chemical germicide
- Part 92 of Title 10 (Health) of the Official Compilation of Codes, Rules, and Regulations of New York
Under Part 92 of Title 10, it is the responsibility of healthcare professionals who are in a position of providing direct care or providing supervision over staff providing direct patient care to maintain competency in infection prevention and barrier precautions. The requirement is fulfilled via a New York board-approved coursework or training. Coursework or training must be before initial licensing, subsequently renewed every four years, and maintained for six years after ceasing position or such work (2).
Statements of Relevant Professional and National Organizations
As the largest healthcare workforce in the nation, nurses are in a position to positively affect the rates of infection at the bedside. The Center for Disease Control asserts the minimum accepted practice of preventing infection is with the use of Standard Precautions, with the number one action in prevention being proper hand washing (3).
The American Nurses Association refers to similar basic tenets of infection prevention: thorough hand washing; staying home when ill; ensuring vaccinations are complete and up to date; using appropriate personal protective equipment; and covering the face when coughing or sneezing (4).
In 2017, the CDC, ANA, and 20 other professional nursing organizations collaborated to create the Nursing Infection Control Education (NICE) Network. This team effort is aimed at introducing clear obligations and competencies for nursing and all healthcare providers to stop the spread of microorganisms within healthcare systems. Within these cores is the responsibility of nurses as leaders within healthcare, “To be successful, infection prevention programs require visible and tangible support from all levels of the healthcare facility’s leadership” (5).
Implications of Professional Conduct Standards
As healthcare professionals who participate in and supervise the care of patients, nurses are responsible for being knowledgeable of the guidelines set by State and federal bodies. Several of these will be touched on throughout this course.
The responsibility also applies to delegated activities. The nurse must ensure that the five rights of delegation are considered when assigning a task to unlicensed assistive personnel and that appropriate infection control policies and protocols are being followed appropriately. Always refer to facility policies and procedures to avoid potentially adverse outcomes.
Failure to follow the accepted standards of infection prevention and control may have serious health consequences for patients, as well as healthcare workers. Hospital acquired infections (HAI) have increased overall from 2020 to 2021 in all infections including central line-associated bloodstream infections (CLABSI), catheter-associated urinary tract infections (CAUTI), ventilator-associated infections, and methicillin-resistant staphylococcus aureus (MRSA). Only clostridium difficile (C-Diff) and surgical site infections (SSI) saw rates lower (6).
In cases of nurses observing incompetent care or unprofessional conduct in relation to infection control standards, the chain of command should first be utilized. Taking consideration into the type of misconduct, the infection control violation should be addressed according to facility policy. Charge nurses and managers would be wise to first address the issue with the nurse involved to gather information and address any education deficits.
In cases where clear misconduct is evident, the National Council of State Boards of Nursing provides advice, “A nurse’s practice and behavior is expected to be safe, competent, ethical and in compliance with applicable laws and rules. Any person who has knowledge of conduct by a licensed nurse that may violate a nursing law or rule, or related state or federal law may report the alleged violation to the board of nursing where the conduct occurred” (7).
The New York Board of Nursing can be reached via its website or at (518) 474-3817. The mailing address is Education Bldg., 89 Washington Avenue, 2nd Floor West Wing, Albany, NY 12234.
The consequences of failing to follow accepted standards of infection prevention and control may result in a complaint investigation from New York’s Professional Misconduct Enforcement System. Upon investigation, penalties include but are not limited to reprimand and censure, fines of up to $10,000 per violation, and probationary terms.
Severe misconduct may result in the loss or revocation of a nursing license. Also, in cases where the neglect to follow appropriate conduct has resulted in harm to a patient or co-worker, there is potential for professional liability through a malpractice suit brought against the nurse.
Methods of Compliance
Nurses are responsible for being knowledgeable of the licensure guidelines, renewal CEs, and targeted education in their state of practice. Refer to the NY Board of Nursing for further guidance beyond the above-mentioned licensing requirements.
Education of infection control best practices, complying with state requirements, and following the facility practices and policies will provide the best protection for self, patients, and staff in preventing and controlling infection during patient care.


Self-Quiz
Ask Yourself...
- What are the consequences of a one-size-fits-all method for infection prevention?
Element II
Modes and mechanisms of transmission of pathogenic organisms in the healthcare setting and strategies for prevention control.
Definitions
Pathogen or infectious agent: A biological, physical, or chemical agent capable of causing disease. Biological agents may be bacteria, viruses, fungi, protozoa, helminths, or prions.
Portal of entry: How an infectious agent enters the susceptible host.
Portal of exit: The path by which an infectious agent leaves the reservoir.
Reservoir: A place in which an infectious agent can survive but may or may not multiply or cause disease. Healthcare workers may be a reservoir for a number of nosocomial organisms spread in healthcare settings.
Standard precautions: A group of infection prevention and control measures that combine the major features of Universal Precautions and Body Substance Isolation and are based on the principle that all blood, body fluids, secretions, excretions except sweat, non-intact skin, and mucous membranes may contain transmissible infectious agents.
Susceptible host: A person or animal not possessing sufficient resistance to a particular infectious agent to prevent contracting infection or disease when exposed to the agent.
Transmission: Any mechanism by which a pathogen is spread by a source or reservoir to a person.
Common vehicle: Contaminated material, product, or substance that serves as a means of transmission of an infectious agent from a reservoir to one or more susceptible hosts through a suitable portal of entry.
Component of the Infectious Disease Process
The infectious disease process follows a particular sequence of events that is commonly described as the “Chain of Infection.” Nurses must have a solid understanding of this process in order to identify points in the chain where the spread of infection may be prevented or halted.
The sequence involves six factors: pathogen, reservoir, portal of exit, portal of entry, mode of transmission, and a susceptible host. The cyclical and consistent nature of the chain provides many opportunities to utilize scientific, evidence-based measures in combating infection spread.
Pathogens within healthcare are widespread and plentiful, putting patients and healthcare workers at particular risk for contamination. The manifestation of symptoms and mode of transmission varies depending upon the characteristics of the specific infectious agent.
Healthcare workers are at a considerably higher risk for bloodborne pathogens such as human immunodeficiency virus (HIV), hepatitis B virus, and hepatitis C virus. Influenza, methicillin-resistant Staphylococcus aureus (MRSA), and Tuberculosis (TB) also pose a higher risk (1). Due to the immunocompromised systems of patients, these and many other pathogens cause a considerable risk and can result in HAIs such as Central Line-associated Bloodstream Infection (CLABSI), Catheter-associated Urinary Tract Infections (CAUTI), Surgical Site Infection (SSI), and Ventilator-associated Pneumonia (VAP) (1).
Pathogens require a reservoir, which is typically a human or animal host; however, may also be from the environment, such as standing water or a surface. From the reservoir, the pathogen is spread via a mechanism such as body fluid, blood, and secretions.
Common sites for contact within patient care include the respiratory, genitourinary, and gastrointestinal tracts, as well as skin/mucous membranes, transplacental, or blood. From here, the mechanism must come into contact with another portal of entry.
Transmission may occur through respiratory, genitourinary, and gastrointestinal tracts, skin and/or mucous membranes, and parenteral pathways. Some of these sites may have become compromised during patient care due to percutaneous injury, invasive procedures or devices, or surgical incisions.
In order to acquire a pathogen, a mode of transmission must be provided. These can be from contact, transmission via a common vehicle, or vector-borne.
Contact with a pathogen may be categorized as direct, indirect, droplet, or airborne. Contact transmission is through direct or indirect contact with a patient or objects that have been in contact with the patient. Pathogens related to this include Clostridium difficile and multi-drug resistant organisms such as MRSA.
Droplet transmission occurs when a pathogen is able to infect via droplets through the air by talking, sneezing, coughing, or breathing. The pathogen is able to travel three to six feet from the patient. Airborne transmission occurs when pathogens are 5 micrometers or smaller in size and are capable of being suspended in the air for long periods of time. These types of pathogens include tuberculosis, measles, chickenpox, disseminated herpes zoster, and anthrax (2).
Transmission may also occur through a common vehicle which affects multiple hosts and can come from food, intravenous fluid, medication, biofilms, or equipment that is shared and often leads to widespread outbreaks. Vector-borne pathogens are derived from living vectors such as mosquitoes, fleas, or ticks.
The last factor in the chain of infection is a susceptible host with a mode of entry. This is the reason that patients are at a much higher risk for developing secondary infections while within the healthcare system.
Factors Influencing the Outcome of Exposures
The human body provides several natural defenses against acquiring infection from a pathogen. The most prominent defense is the integumentary system, and the focus should be on maintaining skin integrity to prevent a mode of entry.
Respiratory cilia function to move microbes and debris from the airway. Gastric acid is at a pH that prevents the growth of many pathogens. Bodily secretions provide defense through flushing out and preventing back-flow of potential infectious agent colonization.
The normal flora within the gastrointestinal system also provides a layer of defense that must be protected from the action of antibiotics. Probiotics are commonly administered to patients on antibiotics to prevent a secondary infection due to the normal flora being disrupted (3).
Host immunity is the secondary defense that utilizes the host’s own immune system to target invasive pathogens. There are four types of host immunity (3):
- Inflammatory response is pathogen detection by cells in a compromised area that then elicit an immune response that increases blood flow. This inflammatory provides delivery of phagocytes or white blood cells to the infected site response. Phagocytes are designed to expunge bacteria.
- Cell-mediated immunity uses B-cells and T-cells, specialized phagocytes, are cytotoxic cells that target pathogens.
- Humoral immunity is derived from serum antibodies produced by plasma cells.
- Immune memory is the ability of the immune system to recognize previously encountered antigens of pathogens and effectively initiate a targeted response.
Pathogen or Infection Agent factors
For each type of infectious agent, there are specific factors that determine the risk to the host. Infectivity refers to the number of exposed individuals that become infected. Pathogenicity is the number of infected individuals that develop clinical symptoms and virulence is the mortality rate of those infected. The probability of an infectious agent causing symptoms depends upon the size of the inoculum (amount of exposure), and the route and duration of exposure (4).
The environment is another factor that warrants attention in limiting the probability of exposure in the healthcare setting. Fomites are materials, surfaces, or objects that are capable of harboring or transmitting pathogens. These can be bedside tables, scrubs, gowns, bedding, faucets, and any other number of items that are in contact with patients and healthcare providers (7).
Equipment may factor into the spread of infection, especially portable medical equipment that can come into contact with numerous patients in a day. This can include vitals machines, IV pumps, wheelchairs, and computers on wheels, among numerous other care items frequently used.
Care must be taken to ensure cleaning in between each patient’s use. For patients in isolation precautions, dedicated equipment for that patient should remain in the room for the duration of their stay.
Methods to Prevent the Spread of Pathogenic Organisms
Standard Precautions
Standard precautions are the minimal amount of caution and procedure applied to typical patient care. According to the CDC, standard precautions are to be used in all patient care areas with critical thinking applied to “. . . common sense practices and personal protective equipment use” (5). The primary of these is proper hand hygiene to be exercised by healthcare providers, patients, and visitors. This will be covered in detail further in this course.
Standard precautions provide guidelines for respiratory hygiene and cough etiquette. The CDC recommends that the mouth and nose be covered with a tissue when coughing or sneezing, with appropriate disposal of the tissue in the nearest waste station. Hand hygiene is to be performed after contact with any respiratory secretions or potentially contaminated items (5).
As mentioned, healthcare workers are at a higher risk for bloodborne infections due to the handling of sharps. Approximately 385,000 needle sticks and sharps injuries are reported by healthcare workers in hospital settings each year (5). Standard precautions can be applied to ensure safe injection practices and will be further covered in Element III.
Certain spinal procedures that access the epidural or subdural space provide a means of transmission for infections such as bacterial meningitis. The CDC states (all from 6):
- Face masks should always be used when injecting material or inserting a catheter into the epidural or subdural space.
- Aseptic technique and other safe injection practices (e.g., using a single-dose vial of medication or contrast solution for only one patient) should always be followed for all spinal injection procedures.
For Patients Infected with Organisms Other Than Bloodborne Pathogens
Special considerations must be given to patient populations that are infected with organisms other than bloodborne pathogens. During the triage of a patient entering a facility, a thorough history should be obtained.
This would include exposure to infectious agents, travel to certain countries in the world, and previous infections that are resistant to antibiotics (i.e., MRSA, VRE, or carbapenem-resistant Enterobacteriaceae). Patients who are identified with a risk or history of any of these pathogens may be placed on the appropriate precautions in an isolation room.
Infection prevention and the attending physician should be consulted immediately for further orders and treatment.
Control of Routes of Transmission
Controlling the routes of transmission is a key factor in preventing infection spread. Hand hygiene has been established as the primary prevention method.
Care must be taken to follow guidelines for proper hand washing including:
- Use antibacterial soap and water when hands are visibly soiled or when a Clostridium difficile infection is known or suspected.
- Hands should be lathered ensuring all surfaces, between fingers, and under nails are covered with scrubbing lasting at least 20 seconds.
- Thoroughly rinse the soap from your hands with running water, pat dry with a paper towel, and use a paper towel to turn off the faucet.
- Hand sanitizer that is at least 60% alcohol based may be used in between soap and water use.
- A dime-sized amount of hand sanitizer should be rubbed over the surface of hands and fingers, then allowed to air dry.
Barriers to proper hand hygiene include knowledge gaps and the availability of appropriate supplies. Training programs to educate healthcare providers on proper hand washing should be accompanied with ongoing assessment and feedback to ensure that compliance is met.
Incorporating hand hygiene into the professional development plan of each nurse is also recommended (7). Healthcare facilities should be diligent in ensuring that hand washing stations are located in convenient areas and that hand cleaning product is frequently monitored and refilled (7,8). Signage and educational materials may be posted in high-traffic areas and at hand washing stations to encourage use by healthcare providers, patients, and visitors (7).
Nurses and healthcare personnel must be aware of the potential of hand hygiene materials as being a potential source of contamination or cross-contamination. Hand hygiene dispensers are touched frequently with contaminated hands and must be frequently cleaned. Follow the manufacturer’s recommendations for cleaning.
Hand hygiene systems that allow products to be refilled pose a risk of contaminating the contents. If refilling is a requirement, this should be accomplished using an aseptic technique as much as possible. Facilities should avoid purchasing this type of product and move to pre-filled dispensing units, if possible (10).
Use of Appropriate Barriers
Appropriate barriers are essential in keeping patients and healthcare providers safe from transmitting or contracting pathogens. The type of PPE chosen depends on certain variables such as the patient care being provided, standard precautions, and transmission-based precautions. The minimal amount of PPE recommended are as follows:
Contact precautions require gloves and gowns. If bodily secretions may be contacted, a mask and eye protection are required.
Droplet precautions require a surgical mask.
Airborne precautions require the wearing of gloves and a gown as well as an approved N95 respirator mask that has been fit tested for the individual wearing. Negative pressure rooms that are able to filter 6 to 12 air exchanges per hour are also recommended (1).
Be mindful that these are the minimal recommendations based solely on the identified transmission status of the patient. Selection of PPE should be made using critical thinking to identify potential risks depending on the type of patient care being performed, procedure, behavioral considerations, and other factors that may deviate from the standard.
The following are current recommendations from the CDC for donning and doffing (11):
How to Put On (Don) PPE Gear: More than one donning method may be acceptable. Training and practicing using your healthcare facility’s procedure is critical. Below is one example of donning.
- Identify and gather the proper PPE to wear. Ensure the choice of gown size is correct (based on training).
- Perform hand hygiene using hand sanitizer.
- Put on an isolation gown. Tie all of the ties on the gown. Assistance may be needed by other healthcare personnel.
- Put on NIOSH-approved N95 filtering face-piece respirator or higher (use a facemask if a respirator is not available). If the respirator has a nosepiece, it should be fitted to the nose with both hands, not bent or tented. Do not pinch the nosepiece with one hand. The respirator/facemask should be extended under the chin. Both your mouth and nose should be protected. Do not wear a respirator/facemask under your chin or store it in a scrubs pocket between patients.
- Respirator: Respirator straps should be placed on the crown of the head (top strap) and base of the neck (bottom strap). Perform a user seal check each time you put on the respirator.
- Face mask: Mask ties should be secured on the crown of the head (top tie) and base of the neck (bottom tie). If the mask has loops, hook them appropriately around your ears.
- Put on a face shield or goggles. When wearing an N95 respirator or half face-piece elastomeric respirator, select the proper eye protection to ensure that the respirator does not interfere with the correct positioning of the eye protection and that the eye protection does not affect the fit or seal of the respirator. Face shields provide full face coverage. Goggles also provide excellent protection for eyes, but fogging is common.
- Put on gloves. Gloves should cover the cuff (wrist) of the gown.
- Healthcare personnel may now enter the patient’s room.
How to Take Off (Doff) PPE Gear: More than one doffing method may be acceptable. Training and practicing using your healthcare facility’s procedure is critical. Below is one example of doffing.
- Remove gloves. Ensure glove removal does not cause additional contamination of hands. Gloves can be removed using more than one technique (e.g., glove-in-glove or bird beak).
- Remove gown. Untie all ties (or unsnap all buttons). Some gown ties can be broken rather than untied. Do so in a gentle manner, avoiding forceful movement. Reach up to the shoulders and carefully pull the gown down and away from the body. Rolling the gown down is an acceptable approach. Dispose of in a trash receptacle.
- Healthcare personnel may now exit the patient’s room.
- Perform hand hygiene.
- Remove face shields or goggles. Carefully remove face shields or goggles by grabbing the strap and pulling upwards and away from the head. Do not touch the front of your face shield or goggles.
- Remove and discard the respirator (or face mask if used instead of respirator). Do not touch the front of the respirator or face mask.
- Respirator: Remove the bottom strap by touching only the strap and bring it carefully over the head. Grasp the top strap, bring it carefully over the head, and then pull the respirator away from the face without touching the front of the respirator.
- Face mask: Carefully untie (or unhook from the ears) and pull away from the face without touching the front. Perform hand hygiene after removing the respirator/face mask and before putting it on again if your workplace is practicing reuse.
- Perform hand hygiene after removing the respirator/face mask and before putting it on again if your workplace is practicing reuse.
Appropriate Isolation/Cohorting of Patients with Communicable Diseases
Cohorting patients is a common practice within facilities, especially with limited rooms and an increasing number of patients with MDROs (12). In order to combat these issues, placing patients with the same type of pathogen in one room, when single rooms are not available is an option. The minimal standard for all patients is standard precautions.
The CDC offers guidance for appropriately isolating or cohorting patients based on the type of precaution.
Contact: Patients with a known or suspected pathogen that is transmitted via contact should be placed in a private room, if available. Cohorting can be achieved if the cohorted patients share the same type of pathogen (13).
Droplet: Unless a single patient room is not available, patients in droplet precautions should only be cohorted if neither have an excessive cough or sputum production. The cohorts should be tested to ensure they are infected with the same type of pathogen. Immunocompromised patients are at an increased risk and should not be cohorted. Patients are to be separated at least three feet apart and a privacy curtain should remain drawn between their respective areas. Care providers must don and doff new PPE in between providing care to each respective patient (13).
Airborne: An airborne infection isolation room (AIIR) with negative air pressure that exchanges air at least six to 12 changes per hour is required. The door must remain closed except for entry and exit. Cohorting of patients is not recommended except in the case of an outbreak or a large number of exposed patients (13). In these instances, the CDC recommends the following (13):
- Consult infection control professionals before patient placement to determine the safety of alternative rooms that do not meet engineering requirements for AIIR.
- Place together (cohort) patients who are presumed to have the same infection (based on clinical presentation and diagnosis when known) in areas of the facility that are away from other patients, especially patients who are at an increased risk for infection (e.g., immunocompromised patients).
- Use temporary portable solutions (e.g., exhaust fan) to create a negative pressure environment in the converted area of the facility. Discharge air directly to the outside, away from people and air intakes, or direct all the air through HEPA filters before it is introduced to other air spaces.
Host Support and Protection
Vaccinations to prevent disease are highly recommended by numerous health organizations such as the CDC, the World Healthcare Organization, and the Office of Disease Prevention and Health Promotion. As stated by the U.S. Department of Health and Human Services, “The United States will be a place where vaccine-preventable diseases are eliminated through safe and effective vaccination over the lifespan.” (14).
As healthcare providers, nurses are in a position to review the patient’s history for gaps in appropriate vaccination coverage and offer education to the patient. Additionally, healthcare providers hold an ethical responsibility to maintain current vaccinations and can prevent transmitting known communicable diseases by receiving an influenza vaccination each year.
Pre- and/or post-prophylaxis may be recommended during certain types of exposures or for patients at an increased risk for infection. This is commonly used for emergent or planned procedures and surgeries that access areas that are at higher risk for becoming a portal of entry, such as the respiratory, gastrointestinal, and genitourinary tracts. Antibiotics may be ordered when it is known that the sterile field has been broken during a procedure or there has been a concern of contamination of a wound or incision site.
In cases of exposure to an infectious pathogen, the decision to treat includes factors such as the type of exposure, source of the patient’s symptoms, time frame since exposure, the health status of the individual exposed, as well as the risks and benefits of the treatment. Pre-prophylaxis may be considered in the prevention of HIV for high-risk individuals.
Typically, after exposure, the host’s blood is drawn to determine pathogen risk regardless of if there is a known pathogen. Post-exposure prophylactics are given within a short time frame from the exposure based on results. The individual who is exposed will have baseline testing for HIV, hepatitis B virus, and hepatitis C viral antibodies. Follow-up testing occurs six weeks, three months, and six months after initial exposure.
Maintaining skin and immune system integrity is of the utmost importance to prevent the transmission of infectious pathogens.
Nursing interventions to promote skin and immune system integrity are:
- Perform a thorough skin assessment every shift and with changes in condition
- Accurately document any wounds or incisions
- Use gentle cleansers on the skin and pat dry
- Use moisturizers and barrier creams on dry or tender skin
- Prevent pressure ulcer development by turning and repositioning the patient every 2 hours
- Maintain aseptic technique during wound care, dressing changes, IV manipulation or blood draws, and catheter care
- Use neutropenic guidelines when providing care to immunocompromised patients
- Encourage adequate nutritional intake
Environmental Control Measures
The cleaning, disinfection, and sterilization of patient care equipment should be performed per the recommendations of the manufacturer. Cleaning should be performed between multiple patients.
For equipment that has been used in an isolation room, a terminal clean must be performed before being used in any other patient care. Additional information on this topic will be covered within Element V.
Environmental cleaning personnel must be educated on the appropriate cleaning for all precautionary patient environments. The Material Safety Data Sheets for all chemicals are to be available to all healthcare personnel for reference as to the proper use and storage. These should be referred to in order to ensure that the correct cleaning product is effective in terminally cleaning isolation rooms based on pathogens.
Ventilation should be thoroughly managed and maintained by the environmental operations team. Negative pressure rooms should be consistently monitored, and alarms investigated to ensure proper air exchange. Concerns from nursing regarding ventilation issues should be directed to the environmental team for follow-up.
Regulated medical waste (RMW) within the healthcare system that must follow state guidelines for disposal includes:
- Human pathological waste
- Human blood and blood products
- Needles and syringes (sharps)
- Microbiological materials (cultures and stocks)
- Other infection waste (16)
According to the Department of Environmental Conservation in New York, “In accordance with both federal and state requirements, and to ensure containment, RMW (except medical waste sharps) is required to be placed in plastic bags and then packaged in single-use (e.g., corrugated boxes) or reusable rigid (e.g., plastic) or semi-rigid, leak-proof containers before transport. Once packaged, RMW is either transported to a designated secure storage, a collection area within the facility for third party pick-up, or a generator’s on-site treatment facility” (16).
Bodily fluid (urine, vomit, and feces) may be safely disposed of in any utility sink, drain, toilet, or hopper that drains into a septic tank or sanitary sewer system. Healthcare personnel must don appropriate PPE during disposal.
Linen and laundry management is governed by Title 10: Section 83-1.17 which states (17) shared health facilities shall:
- Provide a sufficient quantity of clean linen to meet the requirements of patients.
- Separately bag or enclose used linens from infectious patients in readily identified containers distinguishable from other laundry.
- Transport and store clean linen in a manner to prevent contamination.
Food services are required to follow stringent standards under the New York State Department of Health’s Bureau of Community Environmental Health and Food Protection to ensure that food service establishments are maintained to reduce the incidence of food-borne illness.
Environment controls include medical devices and systems that are put in place to isolate or remove the blood-borne pathogens hazard from the workplace. These include sharps disposal containers, self-sheathing needles, and safer medical devices, such as sharps with engineered sharps injury protections and needleless systems. Further information will be provided on this subject in Element III.
Per facility specifications, continuous training and education should be provided to healthcare personnel on the various methods and modes of environmental control measures that are put in place to prevent and contain pathogen spread.

Self-Quiz
Ask Yourself...
- In what ways must an organization balance single-use versus reusable portable medical equipment when considering infectious disease spread?
ELEMENT III
Use of engineering and work practice controls to reduce the opportunity for patient and healthcare worker exposure to potentially infectious material in all healthcare settings.
Definitions
Healthcare-associated infections (HAIs): Infections associated with healthcare delivery in any setting (e.g., hospitals, long-term care facilities, ambulatory settings, home care).
Engineering Controls: Controls (e.g., sharps disposal containers, self-sheathing needles, safer medical devices, such as sharps with engineered sharps injury protections and needleless systems) that isolate or remove the bloodborne pathogens hazard from the workplace.
Injection safety (or safe injection practices): A set of measures taken to perform injections in an optimally safe manner for patients, healthcare personnel, and others. A safe injection does not harm the recipient, does not expose the provider to any avoidable risks, and does not result in waste that is dangerous for the community. Injection safety includes practices intended to prevent transmission of blood-borne pathogens between one patient and another, or between a healthcare worker and a patient, and also to prevent harm such as needlestick injuries.
b A bottle of liquid medication that is given to a patient through a needle and syringe. Single-use vials contain only one dose of medication and should only be used once for one patient, using a new sterile needle and a new sterile syringe.
Multi-dose medication vial: a bottle of liquid medication that contains more than one dose of medication and is often used by diabetic patients or for vaccinations.
Work Practice Controls: Controls that reduce the likelihood of exposure to bloodborne pathogens by altering how a task is performed (e.g., prohibiting the recapping of needles by a two-handed technique).
High-risk Practices and Procedures
Percutaneous exposures are a work hazard within the healthcare industry. There are approximately 5.6 million healthcare workers at risk, with nurses ranking number one. Studies have shown that needlestick injuries occur most frequently within a patient room or the operating room (1).
Exposures can occur through not following safe practices. The following practices in handling contaminated needles and other sharp objects, including blades, can increase the risk of percutaneous exposure and should be avoided:
- Manipulating contaminated needles and other sharp objects by hand (e.g., removing scalpel blades from holders, removing needles from syringes)
- Delaying or improperly disposing of sharps (e.g., leaving contaminated needles or sharp objects on counters/workspaces or disposing in non-puncture-resistant receptacles)
- Recapping contaminated needles and other sharp objects using a two-handed technique
- Performing procedures where there is poor visualization, such as:
-
- Blind suturing
- Non-dominant hand opposing or next to a sharp
- Performing procedures where bone spicules or metal fragments are produced
Mucous membrane/non-intact skin exposures occur with direct blood or body fluids contact with the eyes, nose, mouth, or other mucous membranes via:
- Contact with contaminated hands
- Contact with open skin lesions/dermatitis
- Splashes or sprays of blood or body fluids (e.g., during irrigation or suctioning)
Parenteral exposure is the subcutaneous, intramuscular, or intravenous contact with blood or other body fluid. Injection with infectious material may occur during:
- Administration of parenteral medication
- Sharing of blood monitoring devices (e.g., glucometers, hemoglobinometers, lancets, lancet platforms/pens)
- Infusion of contaminated blood products or fluids
- Human bites, abrasions, or cuts
According to the CDC, unsafe injection practices have resulted in more than 50 outbreaks of infectious disease transmission since 2001. As well, since that time over 150,000 patients were potentially exposed to HIV, hepatitis B virus, and hepatitis C virus solely due to unsafe practice (2). These deviations from best practice have resulted in one or more of the following consequences:
- Transmission of blood-borne viruses, including hepatitis B and C viruses to patients
- Notification of thousands of patients of possible exposure to blood-borne pathogens and recommendation that they be tested for hepatitis C virus, hepatitis B virus, and human immunodeficiency virus (HIV)
- Referral of providers to licensing boards for disciplinary action
- Malpractice suits filed by patients
Pathogens including HCV, HBV, and human immunodeficiency virus (HIV) can be present in sufficient quantities to produce infection in the absence of visible blood.
- Bacteria and other microbes can be present without clouding or other visible evidence of contamination.
- The absence of visible blood or signs of contamination in a used syringe, IV tubing, multi- or single-dose medication vial, or blood glucose monitoring device does NOT mean the item is free from potentially infectious agents.
- All used injection supplies and materials are potentially contaminated and should be discarded.
Proper infection control techniques require that healthcare providers follow best practices to prevent injury and pathogen transfer. At all times, aseptic techniques should be used to prepare and administer an injection. The following are best practice guidelines:
- Medications should be drawn up in a designated “clean” medication area that is not adjacent to areas where potentially contaminated items are placed.
- Use a new sterile syringe and needle to draw up medications while preventing contact between the injection materials and the non-sterile environment.
- Ensure proper hand hygiene (i.e., hand sanitizing or hand washing if hands are visibly soiled) before handling medications.
- If a medication vial has already been opened, the rubber septum should be disinfected with alcohol before piercing it.
- Never leave a needle or other device (e.g., “spikes”) inserted into a medication vial septum or IV bag/bottle for multiple uses. This provides a direct route for microorganisms to enter the vial and contaminate the fluid.
- Medication vials should be discarded upon expiration or any time there are concerns regarding the sterility of the medication.
Never administer medications from the same syringe to more than one patient, even if the needle is changed.
Never use the same syringe or needle to administer IV medications to more than one patient, even if the medication is administered into the IV tubing, regardless of the distance from the IV insertion site.
- All of the infusion components from the infusate to the patient’s catheter are a single interconnected unit.
- All of the components are directly or indirectly exposed to the patient’s blood and cannot be used for another patient.
- Syringes and needles that intersect through any port in the IV system also become contaminated and cannot be used for another patient or used to re-enter a non-patient-specific multidose medication vial.
- Separation from the patient’s IV by distance, gravity, and/or positive infusion pressure does not ensure that small amounts of blood are not present in these items.
- Never enter a vial with a syringe or needle that has been used for a patient if the same medication vial might be used for another patient.
Dedicate vials of medication to a single patient, whenever possible.
- Medications packaged as single-use must never be used for more than one patient:
- Never combine leftover contents for later use
- Medications packaged as multi-use should be assigned to a single patient whenever possible.
- Never use bags or bottles of intravenous solution as a common source of supply for more than one patient.
- Never use peripheral capillary blood monitoring devices packaged for single-patient use on more than one patient:
- Restrict the use of peripheral capillary blood sampling devices to individual patients.
- Never reuse lancets. Use single-use lancets that permanently retract upon puncture whenever possible.
Safe injection practices and procedures are designed to prevent disease transmission from patient to healthcare worker. A fact sheet from OHSA can be found here.

Evaluation/Surveillance of Exposure Incidents
A plan to evaluate and follow up on exposure incidents should be put into place at every facility. At a minimum, this plan should include the following elements:
- Identification of who is at risk for exposure
- Identification of what devices cause exposure
- Education for all healthcare employees who use sharps. This would include that ALL sharp devices can cause injury and disease transmission if not used and disposed of properly. Specific focus should be on the devices that are more likely to cause injury such as:
- Devices with higher disease transmission risk (hollow bore), and
- Devices with higher injury rates (“butterfly”-type IV catheters, devices with recoil action),
- Blood glucose monitoring devices (lancet platforms/pens).
- Identification of areas/settings where exposures occur, and
- Circumstances by which exposures occur,
- Post-exposure management (See Element VI).
Engineer Controls
Engineer controls are implemented to provide healthcare workers with the safest equipment to complete their jobs. Safer devices should be identified and integrated into safety protocols whenever possible.
When selecting engineer controls to be aimed at preventing sharps injuries the following should be considered:
- Evaluate and select safer devices
- Passive vs. active safety features
- Mechanisms that provide continuous protection immediately
- Integrated safety equipment vs. accessory devices:
- Properly educate and train all staff on safer devices
- Consider eliminating traditional or non-safety alternatives whenever possible
- Explore engineering controls available for specific areas/settings
- Use puncture-resistant containers for the disposal and transport of needles and other sharp objects:
- Refer to published guidelines for the selection, evaluation, and use (e.g., placement) of sharps disposal containers.
- National Institute for Occupational Safety and Health (NIOSH) Guidelines
- NYSDOH recommendations “Household Sharps-Dispose of Them Safely”
- Use splatter shields on medical equipment associated with risk-prone procedures (e.g., locking centrifuge lids).
Work Practice Controls
- General practices:
- Hand hygiene including the appropriate circumstances in which alcohol-based hand sanitizers and soap and water hand washing should be used (see Element II)
- Proper procedures for cleaning of blood and body fluid spills
- Initial removal of bulk material followed by disinfection with an appropriate disinfectant
- Proper handling/disposal of blood and body fluids, including contaminated patient care items
- Proper selection, donning, doffing, and disposal of personal protective equipment (PPE) as trained (see Element IV)
- Proper protection of work surfaces in direct proximity to patient procedure treatment area with appropriate barriers to prevent instruments from becoming contaminated with blood-borne pathogens
- Preventing percutaneous exposures:
- Avoid unnecessary use of needles and other sharp objects
- Use care in the handling and disposing of needles and other sharp objects:
- Avoid recapping unless medically necessary
- When recapping, use only a one-hand technique or safety device
- Pass sharp instruments by the use of designated “safe zones”
- Disassemble sharp equipment by use of forceps or other devices
- Discard used sharps into a puncture-resistant sharps container immediately after use
Modify Procedures to Avoid Injury:
- Use forceps, suture holders, or other instruments for suturing
- Avoid holding tissue with fingers when suturing or cutting
- Avoid leaving exposed sharps of any kind on patient procedure/treatment work surfaces
- Appropriately use safety devices whenever available:
-
- Always activate safety features
- Never circumvent safety features

Self-Quiz
Ask Yourself...
- What best practices should always be employed when delivering injections and intravenous medications?
ELEMENT IV
Selection and use of barriers and/or personal protective equipment for preventing patient and healthcare worker contact with potentially infectious material.
Definitions
Personal protective equipment (PPE): Specialized clothing or equipment worn by an employee for protection against a hazard.
Barriers: Equipment such as gloves, gowns, aprons, masks, or protective eyewear, which when worn, can reduce the risk of exposure of the health care worker’s skin or mucous membranes to potentially infective materials.
Types of PPE/Barriers and Criteria for Selection
Per OSHA guidelines, employers must provide employees with appropriate PPE that protects them from any potential infectious pathogen exposure (1). PPE includes gloves, cover garb, masks, face shields and eye protection. All PPE is intended to provide a barrier between the healthcare worker and potential contamination, whether from a patient, object, or surface.
Gloves are intended to provide coverage and protection for hands. There are several types of gloves to choose from and the type of patient care or activity should guide choice.
- Sterile – to be utilized when performing sterile procedures and aseptic technique
- Non-sterile – medical grade, non-sterile gloves may be used for general patient care and clean procedures (such as NG tube insertion)
- Utility – not medical grade and should not be used in patient care
Choice of material glove is made from is often dictated by cost and facility preference. When given a choice, considerations should be made as to the types of material being handled.
- Natural rubber latex – rarely used in facilities due to allergen risk
- Vinyl – made from PVC, lower in cost, provides protection in non-hazardous and low-infection environments
- Nitrile – more durable, able to withstand chemical and bio-medical exposure (2)
An appropriately sized glove fits securely to the fingertips and palm without tightness or extra room. If a glove develops a tear or is heavily soiled, it should be replaced immediately.
Cover garb is a protective layer to wear over scrubs or clothes to protect garments and skin. These include laboratory coats, gowns, and aprons. As with gloves, consideration should be given to size, sterility, type of patient care involved, and material characteristics of the gown.
- Fluid impervious – does not allow passage of fluids
- Fluid resistant – resists penetration of fluids, but fluid may seep with pressure
- Permeable – does not offer protection against fluids
Masks are intended to provide protection to the wearer’s mouth and nose, with respirators providing an extra layer of protection to the respiratory tract against airborne infection pathogens (1). Goggles are designed to protect the eyes from splashes and droplet exposure, while face shields offer additional protection to the entire face. It is important to note that face shields are not designed to be a replacement for masks.
The choice of PPE is based on the factors that are reasonably anticipated to occur during the patient care encounter. Potential contact with blood or other potentially infectious material can occur via splashes, respiratory droplets, and/or airborne pathogens.
The type of PPE chosen will be based on standard or transmission-based precaution recommendations. Follow your facility policy and procedures for guidance on the appropriate choice.
The nurse will also need to anticipate whether fluid will be encountered, such as emptying a drain or foley collection device. In situations where a large amount of fluid is likely to be encountered, it would be wise to choose a higher level of protection, such as an impermeable gown, if available, and to wear eye protection to ward off splashes.
Choosing Barriers/PPE Based on Intended Need
Barriers and PPE are aimed at keeping patients and healthcare providers safe. There are certain circumstances where specific PPE is selected based on patient care or circumstances.
Patient Safety
During invasive procedures, such as inserting a central line or during a surgery, staff directly involved in performing the procedure or surgery must maintain sterility. Appropriate sterile PPE will be selected based on the type of procedure and the patient will be draped in a sterile fashion according to recommended guidelines (1).
Patients in droplet precautions pose a significant risk to healthcare workers and visitors. The patient, as well as anyone inside the patient’s room, should wear a mask for the most effective prevention of transmission (1).
Employee Safety
Employees must ensure that they are evaluating the types of exposure that is likely to occur during patient care. Selection of PPE and appropriate barriers should consider the following:
Barriers for contamination prevention: Per the CDC, “use of PPE is recommended based on the anticipated exposure to blood, body fluids, secretions, or excretions” (3). The following are CDC guidelines based on the expected type of exposure or precaution; however, clinical judgment should be used based on the situation (all from 5):
- Standard precautions are to be used with any potential exposure to blood, mucous membranes, compromised skin, contaminated equipment or surfaces, and body fluids. Barriers may include gloves, gowns, and eye and face protection.
- Employees must be judicious in identifying any precautions that are placed on a patient (i.e., Contact, droplet, airborne) and following recommended PPE guidelines for protecting themselves and other patients.
- PPE should be donned prior to going into a patient room and doffed upon exit. PPE must never be worn in the halls or when going from one patient’s room to the next. All gloves must be changed in between use and hands washed or sanitized upon removal of gloves.
- Additionally, whenever possible, social distancing of 6 feet should occur within the work environment. When not possible, adherence to mask guidelines is sufficient.
Masks for prevention of exposure to communicable diseases: With the onset of COVID-19 across the globe, masks are an essential tool in preventing the transmission of communicable diseases. At a minimum, a medical mask is to be donned during all patient care. During procedures or surgery, surgical masks are to be utilized.
N-95 masks are reserved for patient care with known or suspected Covid-19, if airborne precautions are ordered, or during procedures that may aerosolize (such as during intubations and certain endoscopy procedures).
The CDC recommends reserving surgical N-95 masks for healthcare providers “who are working in a sterile field or who may be exposed to high-velocity splashes, sprays, or splatters of blood or body fluids”. Standard N95 respirators are recommended for all other care involving confirmed or suspected Covid-19 patients (5).
Guidance on Proper Utilization of PPE/Barriers
Proper fit is required for PPE to be effective. Gowns and gloves chosen should fit well, allow movement, and neither be too baggy or too tight. For particulate respirators, the CDC recommends the following regarding proper fit and use of particulate respirators:
All workers who are required to wear tight-fitting respirators (e.g., N95 respirators, elastomerics) must have a medical evaluation to determine the worker’s ability to wear a respirator, and if medically cleared, a respirator fit test needs to be performed using the same model available in the workplace (3, 4).
Prior to donning PPE, it should be inspected for any anomalies, tears, or vulnerable spots. PPE that is compromised should be disposed of and a new garment selected. Nurses must consider the selection of PPE to ensure that it is the correct type for the job and anticipate any circumstances where splashes or saturation of fabric is likely to occur.
The PPE provided by the employer may be single-use or reusable. Always verify with the manufacturer’s guidelines and facility policy on the correct usage and processing of worn garments. It is the facility’s responsibility to ensure that re-usable gowns are laundered according to State guidelines.
In order to prevent cross-contamination, OSHA offers the following guidelines:
- Personal protective equipment must be removed prior to leaving a work area
- Garment penetrated by blood or other potentially infectious material must be removed immediately or as soon as possible
- PPE must be discarded in “. . . an appropriately designated area or container for storage, washing, decontamination, or disposal”
- Employers must ensure that proper hand washing is taking place after the removal of PPE
Healthcare facilities have a legal duty to protect their workers. Per OSHA, “One way the employer can protect workers against exposure to bloodborne pathogens, such as hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV), the virus that causes AIDS, is by providing and ensuring they use personal protective equipment or PPE. Wearing appropriate PPE can significantly reduce risk since it acts as a barrier against exposure. Employers are required to provide, clean, repair, and replace this equipment as needed, and at no cost to workers” (5).
Employers and healthcare workers must understand the balance of cost versus benefit ratio in PPE selection and use. While it is important to be good stewards with resources, always erring on the side of caution and choosing PPE based on anticipated exposure risk is the most effective way to protect yourself and your patients.
Selection, donning, doffing, and disposal. See Element II

Self-Quiz
Ask Yourself...
- How would you handle working at an organization that does not provide a sufficient quantity of PPE to protect frontline staff?
- What is an example of an acceptable refusal to don PPE by a healthcare provider
- What do you think causes healthcare providers to forgo established safety measures?
- What other industries are healthcare analogous to when considering the safety of people?
ELEMENT V
Creation and maintenance of a safe environment for patient care in all healthcare settings through the application of infection control principles and practices for cleaning, disinfection, and sterilization.
Definitions
Contamination: The presence of microorganisms on an item or surface.
Cleaning: The process of removing all foreign material (i.e., dirt, body fluids, lubricants) from objects by using water and detergents or soaps and washing or scrubbing the object
Critical device: An item that enters sterile tissue or the vascular system (e.g., intravenous catheters, needles for injections). These must be sterile prior to contact with tissue.
Decontamination: The use of physical or chemical means to remove, inactivate, or destroy blood-borne pathogens on a surface or item to the point where they are no longer capable of transmitting infectious particles.
Disinfection: The use of a chemical procedure that eliminates virtually all recognized pathogenic microorganisms but not necessarily all microbial forms (e.g., bacterial endospores) on inanimate objects.
High-level disinfection: Disinfection that kills all organisms, except high levels of bacterial spores, and is affected with a chemical germicide cleared for marketing as a sterilant by the U.S. Food and Drug Administration (FDA).
Intermediate level disinfection: Disinfection that kills mycobacteria, most viruses, and bacteria with a chemical germicide registered as a “tuberculocide” by the U.S. Environmental Protection Agency (EPA).
Low-level disinfection: Disinfection that kills some viruses and bacteria with a chemical germicide registered as a hospital disinfectant by the EPA.
Non-critical device: An item that contacts intact skin but not mucous membranes (e.g., blood pressure cuffs, oximeters). It requires low-level disinfection.
Semi-critical device: An item that comes in contact with mucous membranes or non-intact skin and minimally requires high-level disinfection (e.g., oral thermometers, vaginal specula).
Sterilization: The use of a physical or chemical procedure to destroy all microbial life, including highly resistant bacterial endospores.
Universal Principles
Instruments, medical devices, and equipment should be managed and reprocessed according to the recommended and appropriate methods regardless of a patient’s diagnosis, except for cases of suspected prion disease.
Due to the infective nature and steam-resistant properties of prion diseases, special procedures are required for handling brain, spinal, or nerve tissue from patients with known or suspected prion disease (e.g., Creutzfeldt-Jakob disease [CJD] or Bovine spongiform encephalopathy [BSE]). Consultation with infection control experts before performing procedures on such patients is warranted.
Industry guidelines as well as equipment and chemical manufacturer recommendations should be used to develop and update reprocessing policies and procedures. Written instructions must be made available for each instrument, medical device, and equipment reprocessed.
The CDC recommends that critical medical and surgical devices and instruments that would be expected to enter a system through which sterile body fluids, blood, or sterile tissue be sterilized prior to use on each patient. (1).
Potential for Contamination
The type of instrument, medical device, equipment, or environmental surface cause variables that are more likely to be a source of contamination. External contamination may be caused by the presence of hinges, crevices, or multiple interconnecting pieces.
If able, these devices should be disassembled. Endoscopes provide a particular challenge for both internal and external contamination, due to their lumens as well as the crevices and joints present.
The disinfectant must reach all surfaces and assurance that there are no air pockets or bubbles to impede penetration (2). As well, these devices may be made of material that is not heat resistant, which prevents the ability to sterilize. In these instances, chemicals must be utilized to provide disinfection.
Once rendered sterile, there are multiple opportunities for potential contamination due to the frequency of hand contact with the device or surface. Packaging may be overhandled and breached, or the item may come into contact with potential contaminants via poor storage, improper opening, or environmental factors.
The efficacy of sterilization and disinfection is dependent upon the number and type of microorganisms present. Several types of pathogens carry an innate resistance, making successful decontamination more challenging (2).
Most infections are caused by bacteria, followed by viruses, fungi, protozoa, and prions (3). Due to the nature of their outer membranes, spores, and gram-negative bacteria have a natural barrier that prevents the absorption of disinfectants.
Bacterial spores are especially resistant to chemical germicides, as are the following pathogenic organism types (all from 2):
- Coccidia – i.e. Cryptosporidium
- Mycobacteria – i.e. M. tuberculosis
- Nonlipid or small viruses – i.e. poliovirus, coxsackievirus
- Fungi – i.e. Aspergillus, Candida
- Vegetative bacteria – i.e. Staphylococcus, Pseudomonas
- Lipid or medium-size viruses – i.e. herpes, HIV
The number of microorganisms that are present on a medical instrument, device or surface affects the time that must be factored into disinfection and sterilization efficacy. As stated by the CDC, “Reducing the number of microorganisms that must be inactivated through meticulous cleaning, increases the margin of safety when the germicide is used according to the labeling and shortens the exposure time required to kill the entire microbial load” (2)
In general, used medical devices are contaminated with a relatively low bioburden of organisms. Inconsistencies or incorrect methods of reprocessing can easily lead to the potential for cross-contamination (1).
Steps of Reprocessing
Reprocessing medical instruments and equipment is completed sequentially depending upon the instrument and the process chosen.
Pre-cleaning is the process of removing soil, debris, and lubricants from internal and external surfaces through mopping, wiping, or soaking. It must be done as soon as possible after use to lower the number of microorganisms present on the object.
Cleaning may be accomplished manually or mechanically. Manual cleaning relies upon friction and fluidics (fluids under pressure) to remove debris and soil from the inner and outer surfaces of the instrument. There are several different machines used in mechanical cleaning including ultrasonic cleaners, washer-disinfectors, washer-sterilizers, and washer-decontaminators. Studies have shown that automated cleaning is more effective than manual; however, the frequency of fluid changes must follow the manufacturer’s guidelines to eliminate the risk of contaminating debris (1).
Disinfection involves the use of disinfectants, either alone or in combination, to reduce the microbial count to near insignificant. Common disinfectants used in the healthcare setting include chlorine and chlorine compounds, hydrogen peroxide, alcohols, iodophors, and quaternary ammonium compounds, among others. These products are formulated and then approved by the Environmental Protection Agency and Food and Drug Administration for specific uses.
Sterilization is used on most medical and surgical devices that are utilized in healthcare facilities. This requires sufficient exposure time to heat, chemicals, or gases to ensure that all microorganisms are destroyed.

Choice/Level of reprocessing sequence
The choice or level of reprocessing is based on the intended use:
- Critical instruments and medical devices require sterilization
- Semi-critical instruments and medical devices minimally require high-level disinfection
- Noncritical instruments and medical devices minimally require cleaning and low-level disinfection
Manufacturer’s recommendations must always be consulted to ensure that appropriate methods, actions, and solutions are used. There is a wide variability of compatibility among equipment components, materials, and chemicals used. Rigorous training is required to appropriately understand the various equipment heat and pressure tolerance as well as the time and temperature requirements for reprocessing.
Failure to follow the manufacturer’s recommendations may lead to equipment damage, elevated microbial counts on instruments after reprocessing, increased risk for infections, and possibly patient death.
Effectiveness of reprocessing instruments, medical devices, and equipment
Pre-cleaning and cleaning before disinfection is one of the most effective ways to reduce the microbial count. This is only effective when completed prior to disinfection.
Disinfection relies upon the action of products to eliminate microbial count. Depending on the medical instrument or device design, the product may only be required to cover the surface. However, due to the lumens of scopes, crevices, or hinges on certain instruments, immersion products and dwell times are required (4).
The presence of organic matter, such as blood, serum, exudate, lubricant, or fecal material can drastically reduce the efficacy of a disinfectant. This may occur due to the presence of organic material acting as a barrier. It may also occur from a chemical reaction between the organic material and the disinfectant being utilized.
Biofilms pose a particular challenge and offer protection from the action of disinfectants. Biofilms are composed of microbes that build adhesive layers onto the inner and outer surfaces of objects, including instruments and medical devices, rendering certain disinfectants ineffective. Chlorine and Monochloramines remain effective against inactivating biofilm bacteria (1).
Per the CDC, “. . . a given product is designed for a specific purpose and is to be used in a certain manner. Therefore, users should read labels carefully to ensure the correct product is selected for the intended use and applied efficiently” (1). The label will indicate sufficient contact time with the chemical solution to achieve adequate disinfection.
After disinfection, staff and management must adopt a system of record keeping and tracking of instrument usage and reprocessing. Reprocessing equipment must be on a schedule to be maintained and regularly cleaned, according to the manufacturer’s guidelines.
There are several methods of sterilization used such as steam sterilization (autoclaves), flash sterilization, and more recently, low-temperature sterilization techniques created for medical devices that are heat sensitive. Selection depends upon the type of instrument, material, ability to withstand heat or humidity, and targeted microbes.
There are several methods of ensuring that sterilized instruments are processed and tracked appropriately. Indicators or monitors are test systems that provide a way of verifying that the sterilization methods were sufficient to eradicate the regulated number of microbes during the process. These safeguards include:
- Biologic monitors
- Process monitors (tape, indicator strips, etc.)
- Physical monitors (pressure, temperature gauges)
- Record keeping and recall/ tracking system for each sterilization processing batch/item
Studies have shown that the best practice of handling and storage of reprocessed medical equipment and instruments uses a system of event-related shelf life, rather than time-related. The rationale for this lies in the theory that the sterile items remain sterile as long as the packaging is not compromised (2).
Factors that are considered event-related include internal or external contamination such as damage to the packaging, humidity, insects, vermin, open shelving, temperature fluctuations, flooding, location, and the composition of packaging material.
Standards for handling must also focus on the protection of workers from health issues.
Recognizing Potential Sources of Cross-Contamination in The Healthcare Environment
- Surfaces or equipment which require cleaning between patient procedures/treatments
- Practices that contribute to hand contamination and the potential for cross-contamination
- Consequences of reuse of single-use/disposable instruments, medical devices, or equipment
Factors That Have Contributed to Contamination in Reported Disease Transmission Cases
At any point in reprocessing or handling, breaks in infection control practices can compromise the integrity of instruments, medical devices, or equipment. Specific factors include:
- Failure to reprocess or dispose of items between patients
- Inadequate cleaning
- Inadequate disinfection or sterilization
- Contamination of disinfectant or rinse solutions
- Improper packaging, storage, and handling
- Inadequate/inaccurate record keeping of reprocessing requirements.
Expectations Regarding Differing Levels of Disinfection and Sterilization Methods
Professionals who practice in settings where handling, cleaning, and reprocessing equipment, instruments, or medical devices is performed elsewhere (e.g., in a dedicated Sterile Processing Department) are responsible for ensuring understanding of the core concepts and principles:
- Standard and Universal Precautions (e.g., wearing of personal protective equipment)
- Cleaning, disinfection, and sterilization (Sections III and IV above)
- Appropriate application of safe practices for handling instruments, medical devices, and equipment in the area of professional practice
- Designation and physical separation of patient care areas from cleaning and reprocessing areas is strongly recommended by NYSDOH.
- Verify with those responsible for reprocessing what steps are necessary prior to submission of pre-cleaning and soaking
Professionals who have primary or supervisory responsibilities for equipment, instruments, or medical device reprocessing (e.g., Sterile Processing Department staff or clinics and physician practices where medical equipment is reprocessed on-site) are responsible for understanding core concepts and principles:
- Standard and Universal Precaution
- Cleaning, disinfection, and sterilization described in Sections III and IV above
- Appropriate application of safe practices for handling instruments, medical devices, and equipment in the area of professional practice
- Designation and physical separation of patient care areas from cleaning and reprocessing areas is strongly recommended by NYSDOH
Facilities must be fastidious in developing appropriate reprocessing practices that follow regulatory guidelines. When selecting appropriate methods, consideration must be given to the antimicrobial efficacy, time constraints, and requirements of these methods, as well as compatibility. Compatibility among equipment/materials includes corrosiveness, penetrability, leaching, disintegration, heat tolerance, and moisture sensitivity.
The toxicity of the products used can pose occupational and environmental hazards to staff and patients. Facilities must adopt procedures and policies to reduce exposure to harmful substances, monitor for harmful exposures, and train staff using reprocessing cleaning and chemicals.
To reduce potential exposure to harmful substances, OSHA mandates that training for workers before use include (all from 5):
- Health and physical hazards of the cleaning chemicals
- Proper handling, use, and storage of all cleaning chemicals being used, including dilution procedures when a cleaning product must be diluted before use
- Proper procedures to follow when a spill occurs
- Personal protective equipment required for using the cleaning product, such as gloves, safety goggles and respirators
- How to obtain and use hazard information, including an explanation of labels and SDSs
Other considerations in developing a safety plan for appropriate reprocessing practices include:
- Potential for patient toxicity/allergy
- Residual effects including antibacterial residual and patient toxicity/allergy
- Ease of use
- Stability of products, including concentration, potency, efficacy of use, and effects of organic material
- Odor
- Cost
- Monitoring requirements and regulations
- Specific labeling requirements for reprocessing single-use devices

Self-Quiz
Ask Yourself...
- You are concerned that the sterilized equipment your co-worker just opened onto a sterile field was compromised. The co-worker assures you it is fine. How would you handle this situation?
- When would it be appropriate for a facility to deviate from the manufacturer’s recommendations in processing medical and surgical equipment?
- Why do you think there is variation in the level of reprocessing of medical instruments?
- How would you verify that sterile instruments are not compromised with a shelf-stable system?
ELEMENT VI
Prevention and control of infectious and communicable diseases in healthcare workers.
Definitions
Infectious Disease: A clinically manifest disease of humans or animals resulting from an infection.
Communicable Disease: An illness due to a specific infectious agent or its toxic products that arises through transmission of that agent from an infected person, animal, or inanimate source to a susceptible host.
Occupational Health Strategies: As applied to infection control, a set of activities intended to assess, prevent, and control infections and communicable diseases in healthcare workers.
Pre-Placement and Periodic Health Assessments
Occupational health strategies are aimed at ensuring employees are healthy and keeping them healthy. Upon hiring, employees should undergo an initial health screening that reviews immunization records.
The CDC suggests that healthcare workers are screened when newly hired and periodically ongoing to (all from 1):
- Ensure sufficient immunity to vaccine-preventable diseases such as measles, mumps, rubella, varicella, hepatitis B, annual influenza and any other recommended or mandated requirements
- Assess for and manage underlying conditions and illnesses that may affect workplace safety
- Prevent, assess, and treat any potential infectious exposures or illnesses that may be acquired or transmitted within the healthcare setting
- Initiate and continue personalized health counseling
- Thorough history and physical
A tuberculosis screening should be completed before a new employee provides patient care and upon possible exposure for an existing employee. A thorough assessment should include an evaluation of the following symptoms:
- Fever
- Cough
- Chest pain, or pain with breathing or coughing
- Night sweats
- Chills
A Mantoux tuberculin skin test (TST) must also be completed. The test is performed by injecting a small amount of tuberculin into the epidermis of the forearm. The test is then evaluated for a reaction in 48 to 72 hours.
If there is no reaction, the test result is negative. If reactive, a scale is used to interpret the measurement of induration and to direct further testing or treatment (2).
When working in healthcare, nursing staff must be healthy to provide optimal care. This is especially true in the care of vulnerable patients who have weakened immune symptoms.
The following symptoms require immediate evaluation by a licensed medical professional:
- Fever
- Cough
- Rash
- Vesicular lesions
- Draining wounds
- Vomiting
- Diarrhea
Upon evaluation, there may be possible restrictions from patient care activities and work clearance must be completed prior to return.
Management Strategies for Potentially Communicable Conditions
Management and the Infection Prevention department should collaborate and strategize to ensure that employees who have had an exposure or possible exposure are protected and have support in seeking treatment without fear of retaliation or job loss (3). Managerial support should prioritize:
- Appropriate evaluation and treatment
- Limiting contact with susceptible patients and staff
- Placement in a non-clinical setting
- Depending on the severity of symptoms or potential transmission, a furlough until no symptoms are present may be necessary
Prevention and Control Strategies for Bloodborne Pathogen Transmission
Robust training and educational programs are essential for the prevention of healthcare worker exposure and transmission. Prevention strategies should include education, training, and availability of the following:
- Information on potential agents such as HBV, HCV, and HIV
- HBV vaccination (including safety, efficacy, components, and recommendations for use)
- Hand hygiene
- Appropriate PPE and barrier precautions (see Element II)
- Sharps safety (see Element III)
- Standard and Universal Precautions
- Education on the availability of confidential and anonymous testing for bloodborne pathogens (4)

Post-Exposure Evaluation and Management.
Each facility must plan for post-exposure evaluation and management in the case that any employee or patient experiences a potential or actual bloodborne exposure. The plan should incorporate the following:
- Prompt evaluation by a licensed medical professional
- Risk assessment in occupational exposures
- Recommendations for approaching source patient and healthcare worker evaluations
- Recommendations for post-exposure prophylaxis emphasizing the most current NYSDOH and CDC guidelines
- Post-exposure management of patients or other healthcare workers when the exposure source is a healthcare worker obligates the patient to be informed of the type of exposure, whether it is the healthcare worker’s blood or other potentially infectious material.
Airborne or droplet pathogens require several special considerations. The above guidelines should be applied appropriately. As well, New York requires mandatory reporting of certain communicable diseases is required, including tuberculosis. The New York State Department of Health (NYSDOH) states:
Reporting of suspected or confirmed communicable diseases is mandated under the New York State Sanitary Code (10NYCRR 2.10,2.14). The primary responsibility for reporting rests with the physician; moreover, laboratories (PHL 2102), school nurses (10NYCRR 2.12), daycare center directors, nursing homes/hospitals (10NYCRR 405.3d), and state institutions (10NYCRR 2.10a) or other locations providing health services (10NYCRR 2.12) are also required to report (5).
NYSDOH follows the CDC’s recommended guidelines when exposure to TB occurs. The HCW should be retested for TB using TST and be monitored for symptoms of disease progression. If found to have a TST reaction of 10 or more millimeters, the patient would be given high priority to receive drug treatment under the criteria of working within a high-risk setting (6). Drug treatment typically consists of 3 months of isoniazid once weekly in addition to rifapentine in adults and children over 2 years old.
Post-exposure of other Airborne pathogens such as varicella, measles, mumps, rubella, and pertussis should be directed toward the most current federal, state, or local requirement for post-exposure evaluation and management. As with tuberculosis, mandatory reporting may be required. The Communicable Disease Reporting Requirements form may be found here.
For additional, up-to-date information and guidance, the New York State Department of Health Bureau of Communicable Disease Control can be reached at (518) 473-4439 or (866) 881-2809 after hours.
All patients and health care workers who have been potentially exposed to any pathogens should be educated and counseled about (all from 7):
- Risk of exposure or illness
- Testing
- Options for and risks and benefits of post-exposure prophylaxis or treatment
- Need for specialty care
- Follow-up testing and treatment
- Work restrictions, if indicated
- Risk of transmitting infections to others and methods to prevent transmission, and
- Signs and symptoms of illness to report after exposure, including side effects such as prophylaxis.
Evaluation of Healthcare Workers Infected with Bloodborne Pathogens
The NYSDOH provides the following rules and recommendations based on scientific evidence-based practice in relation to policies to prevent infected healthcare personnel-related blood-borne pathogen transmission (HIV, HBV, HCV) (all from 4):
- Strict adherence to Standard Precautions
- Voluntary testing without fear of disclosure or discrimination
- Mandatory screening of New York HCW for blood-borne pathogens is not recommended. Such a program would cost millions of dollars and would not produce any appreciable gain in public safety. Negative antibody tests for HIV, HBV, and HCV do not rule out the presence of infection since it can take some time for measurable antibodies to appear.
- Employer notification of a blood-borne pathogen is not a requirement for employment
Criteria must be followed when evaluating infected healthcare workers for the risk of transmission in order to adhere to laws protecting workers from discrimination and disability laws. The following outlines a general assessment to determine the risks posed:
- Nature and scope of professional practice
- Techniques used in the performance of procedures that may pose a transmission risk to patients
- Assessed compliance with infection control standards
- Presence of weeping dermatitis, draining, or open skin wounds
- Ability to carry out duties with Cognitive status examination
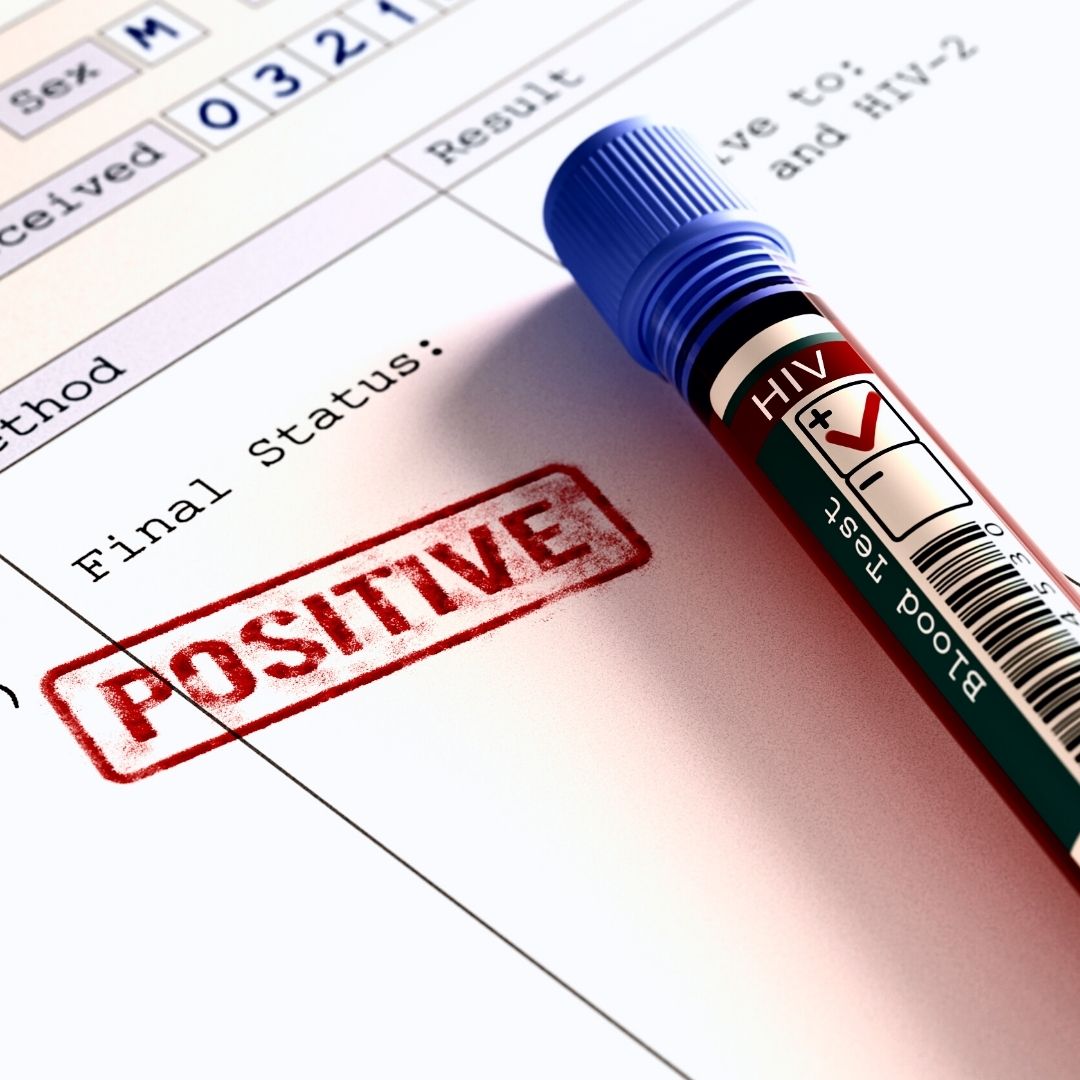
Expert Panels for Evaluating Healthcare Workers Infected with Bloodborne Pathogens
Upon request, a blood-borne pathogen-infected HCW may seek advice from the NYSDOH regarding potential risk during patient care of blood-borne disease transmission. A state advisory panel would convene with, at minimum, representation by a state or local public officer, an epidemiologist, and an infectious disease expert (4).
The purpose of the panel is to provide consultation to the MCW regarding the risk of blood-borne disease transmission related to occupation and to give recommendations on best practices, needs for limitations, modifications, or restrictions if there is an identified risk to patient care. Confidentiality is maintained with the restriction that recommendations are followed, and any restrictions are disclosed to the facilities where the HCW is currently employed or seeks future employment (4)

Self-Quiz
Ask Yourself...
- What are your thoughts on a proposal to test all healthcare workers for bloodborne illness prior to licensing?
- Should nurses who provide care to vulnerable patients require health screenings before performing patient care?
- A colleague confides in you that they are concerned they may have been exposed to hepatitis C but are wary of being tested. What options are available to support the colleague and protect patients?
- Who should be responsible for providing post-exposure prophylaxis to potentially infectious material when the employee is not following regulated guidelines for care delivery?
ELEMENT VII
Sepsis awareness and education
Definitions
Sepsis: Sepsis is a life-threatening condition caused by a host’s extreme response to infection. The Surviving Sepsis Campaign 2016 International Guidelines define sepsis as life-threatening organ dysfunction caused by a dysregulated host response to infection. Earlier definitions defined sepsis as an inflammatory response to infection, while sepsis associated with organ dysfunction was identified as severe sepsis. Septic shock is a subset of sepsis that manifests with circulatory and cellular/metabolic dysfunction; it is associated with a higher mortality risk.
Scope of the Problem
Over 1.7 million Americans are diagnosed with sepsis each year, with the incidence rising by approximately 8% annually. In New York, there are approximately 50,000 patients treated for severe sepsis and septic shock, resulting in just under 30% of patients dying each year (1).
Sepsis is a life-threatening medical emergency that requires early recognition and intervention. Sepsis occurs when the body overcompensates in response to an infection, resulting in multiple organ dysfunction and damage.
Most sepsis cases are community-acquired. Seven in 10 patients with sepsis had recently used healthcare services or had chronic conditions requiring frequent medical care (1). Early recognition and treatment are the most effective ways to combat sepsis.
In 2013, New York State became the first in the U.S. to develop a state mandate that requires all hospitals to develop and adopt sepsis protocols. The mandate is dubbed “Rory’s Regulations,” after Rory Staunton, a 12-year-old boy whose death was attributed to lack of sepsis recognition. These protocols were required to adopt the following practices (2):
- A process for the screening and early recognition of patients with sepsis, severe sepsis, and septic shock.
- A process to identify and document individuals appropriate for treatment through severe sepsis protocols, including explicit criteria defining those patients who should be excluded from the protocols, such as patients with certain clinical conditions or who have elected palliative care.
- Guidelines for hemodynamic support with explicit physiologic and biomarker treatment goals, methodology for invasive or non-invasive hemodynamic monitoring, and time frame goals.
- For infants and children, guidelines for fluid resuscitation with explicit time frames for vascular access and fluid delivery are consistent with current evidence-based guidelines for severe sepsis and septic shock with defined therapeutic goals for children.
- A procedure for identification of infection source and delivery of early antibiotics with time frame goals; and
- Criteria for use, where appropriate, of an invasive protocol and for use of vasoactive agents.
- Medical staff also gained responsibility for the collection, use, and report quality measures and for the mortality data of peers, including national, hospital, and expert stakeholders (2).
This led to The New York State Sepsis Care Improvement Initiative, started in 2014, to increase early recognition of suspected sepsis and competence in implementing the new sepsis protocols by all healthcare professionals.
This was to be achieved through mandatory training or coursework on sepsis (3). The goal was to stress the importance of timely initiation of evidence-based protocols to improve sepsis outcomes.
Causes of Sepsis
As stated by the Sepsis Alliance, “Sepsis is the body’s overwhelming and life-threatening response to infection that can lead to tissue damage, organ failure, and death” (4).
Bacterial infections commonly trigger sepsis, although other microbial infections (e.g., fungal or viral) can also trigger sepsis. The triggering infection most commonly originates from the lungs, urinary tract, skin, and/or gastrointestinal tract.
Certain populations are at an increased risk of developing sepsis including:
- Babies (under 1 year), and individuals 65 years of age and older.
- People with chronic conditions such as diabetes, lung disease, kidney disease, or cancer; and
- People with impaired immune systems.
Early Recognition of Sepsis
- Manifestations of sepsis vary based on the type of infection and host factors.
- Some people may have subtle sepsis presentations.
- Signs and symptoms that may be associated with sepsis in persons with confirmed or suspected infection can include:
- Altered mental state
- shortness of breath
- fever
- clammy or sweaty skin
- extreme pain or discomfort
- high heart rate
Signs and symptoms in children and the elderly may not present the same. In children and the elderly sepsis symptoms may present as above or any of the following: decreased temperature; pallor or bluish tone to skin; non-blanching rash; high respiratory rate; lethargy; and seizure.
Sepsis can progress to more severe forms of sepsis, including septic shock. When septic shock occurs, the body’s inflammatory response causes extensive vasodilation throughout the body. This results in a sudden drop in blood pressure that can quickly lead to organ failure and damage (5).
If a person presents with suspected or confirmed infection, healthcare professionals should assess for signs of, and risk factors for sepsis following facility sepsis protocols.
Principles of Sepsis Treatment
Sepsis treatment starts with prompt recognition and diagnosis. The diagnosis of sepsis starts with the assessment of a patient with a known or suspected infection. For adults, sepsis is defined as having two or more symptoms of systemic inflammatory response syndrome, which includes (6):
- Temperature (>38 o C or <36 o C)
- Elevated heart rate > 90 bpm
- WBC (<4×109/L or >12×109/L)
- Respiratory rate (>20 breaths/min, PACO2<32 mm Hg
Severe sepsis has traditionally been defined as having sepsis plus organ failure, while septic shock involves sepsis along with refractory hypotension after fluid resuscitation or requiring vasopressors to maintain hemodynamics (6). The standard changed in 2016 with the elimination of severe sepsis; however, most facilities still adhere to the above criteria. Follow sepsis protocol and bundles per facility.
With the recognition of sepsis and/or septic shock, previously state law mandated that one- and three-hour care bundles be created. While these may vary slightly per facility, Surviving Sepsis promotes a one-hour bundle that incorporates all the recommendations of the other bundles yet decreases the time to treat (7):
One Hour Bundle
- Obtain lactate level. Reorder if initial lactate is > 2 mmol/L
- Obtain blood cultures before administering antibiotics
- Administer broad-spectrum antibiotics
- Rapidly infuse crystalloids at a rate of 30 mL/kg for hypotension or lactate ≥ 4 mmol/L
- If hypotensive post fluid resuscitation, administer vasopressors to maintain a mean arterial pressure ≥ 65 mm Hg.
In addition to blood cultures, type and screens may be ordered for urine, wound exudate, or respiratory secretions depending upon where the suspected infection originates from. Blood tests may also include a complete blood count and a basic metabolic panel to assess for any damage to the kidneys or liver. Other diagnostic imaging may include chest X-rays, CTs, ultrasounds, and MRIs (8).
Fluid resuscitation and vasopressors, if needed, will continue until the patient is hemodynamically stable. Physicians should be notified when blood cultures result in order to ensure that the ordered antibiotic is effective against the identified organism (8).

Patient Education and Prevention
Patient education should strive to provide memorable and simple ways to stay free of infection. The number one method of preventing infection is adequate hand hygiene. The CDC also suggests that patients keep wounds and cuts clean and covered until healed.
Patients at higher risk should be notified of their risk factors, including (9):
- Adults 65 or older
- People with chronic medical conditions, such as diabetes, lung disease, cancer, and kidney disease
- People with weakened immune systems
- Sepsis survivors
- Children younger than one
Patients should be educated on warning signs and symptoms of sepsis that are easy to remember. The Sepsis Alliance suggests the following acronym and verbiage for seeking immediate care (4):
Patients should be encouraged to give relevant history and information to clinicians, including if they have had a recent infection, sepsis in the past, or are immunocompromised.

Self-Quiz
Ask Yourself...
- A facility has implemented a sepsis screening program, and chart reviews indicate that the order set is not consistently followed. What is the best action for the facility to take to improve compliance?
- What are ways that nursing can promote sepsis screening upon admission?
- A unit-based council is preparing education for the public regarding sepsis recognition and prevention. What methods would be most effective to reach the most vulnerable populations?
- How are sepsis and septic shock interrelated? How does treatment differ for each sequela?
New York Mandatory Prescriber Education
Introduction
Welcome to the transformative journey to enhance your prescribing practices, safeguard your patients, and be a catalyst for positive change in the fight against opioid addiction in New York State. As healthcare providers, it is vital to be equipped with the latest knowledge and skills for safe and effective prescribing of controlled substances, ultimately contributing to the reduction of opioid misuse and improving patient care outcomes in New York State. Familiarity with state and federal regulation of controlled substances as well as recognizing addiction and misuse is imperative. The use of pain assessment tools and potential substance misuse is essential for delivering high-quality, effective, and patient-centered care. Prescribers should also be mindful of palliative and hospice care principles.

State and Federal Laws on Prescribing Controlled Substances
There are state and federal regulations on prescribing controlled substances. A significant factor is if controlled substances are required to be submitted electronically. Not all states currently mandate that controlled substances be prescribed electronically, though a significant majority do. The federal government has mandated electronic prescribing for controlled substances (EPCS) for Medicare Part D, but states have their specific regulations and deadlines. As of recent updates, states have enacted mandates requiring electronic prescriptions for all controlled substances, with some states providing waivers or exceptions under certain conditions. Implementing these requirements can help combat opioid misuse and improve prescription safety.
New York (NY) Controlled Substance Prescribing Laws
The state of New York has implemented numerous laws designed to improve the safety and efficacy of NY controlled substance prescribing, reduce misuse and diversion, and ensure that prescribers have the necessary education to manage these substances responsibly.
Electronic Prescribing (E-Prescribing)
Mandatory E-Prescribing: New York is among the states that require all prescriptions for NY controlled substances to be issued electronically, except under certain circumstances such as technological failure or specific patient scenarios. Prescribers must be familiar with the particular regulations and guidelines governing these exceptions, and document any use of exceptions appropriately.
The following are key exceptions to mandatory electronic prescribing in New York:
- Temporary Technological or Electrical Failure: If a prescriber is experiencing a temporary technological or electrical failure that prevents the use of electronic prescribing systems, they may issue a paper prescription. This situation should be documented, and the prescription must comply with all other applicable regulations.
- Waiver Granted by the Commissioner of Health: Prescribers who have been granted a waiver by the New York State Commissioner of Health due to economic hardship, technological limitations, or other exceptional circumstances can issue non-electronic prescriptions. Waivers are typically granted for a specific period and may require periodic renewal.
- Practitioner Dispenses Directly: If a practitioner dispenses the medication directly to the patient (e.g., samples or medications given in the office), they are not required to issue an electronic prescription.
- Out-of-State Prescriptions: Prescriptions issued by licensed practitioners practicing in another state and who do not regularly practice in New York are exempt from the electronic prescribing requirement.
- Long-Term Care Facilities: In some cases, medications prescribed to patients residing in long-term care facilities may be exempt from electronic prescribing requirements, depending on specific circumstances and regulatory guidelines.
- Emergency Situations: In cases of emergencies medication should be given immediately, and electronic prescribing is not practical, prescribers may issue a paper prescription. Documentation is necessary and the prescription must meet all other regulatory requirements.
- Public Health Emergencies: During public health emergencies or situations where electronic prescribing systems are compromised or unavailable, exceptions may be made to allow for non-electronic prescriptions.
- Complicated Medications with Lengthy Instructions: The use of this exception must meet exception requirements and must be documented properly.
Mainstreaming Addiction Treatment Act
The Mainstreaming Addiction Treatment (MAT) Act is a federal law and became effective in 2022. Important changes resulting from this act, include (12):
- Elimination of the requirement for registration through the federal Drug Enforcement Administration to prescribe or dispense buprenorphine for the treatment of opioid use disorder (OUD).
- Elimination of the limitations on the number of patients a practitioner was permitted to treat with buprenorphine for OUD.
Essentially, prescribers holding a standard DEA registration can prescribe buprenorphine for the treatment of OUD, without limitation to the number of patients or a special waiver or registration through the DEA.
Annual Opioid Antagonist Prescription Requirement
Effective June 2022, the Public Health Law Section 3309(7) requires prescribers to prescribe an opioid antagonist along with the first opioid prescription to specific patients every year when any of the following risk factors are present (12):
- A history of substance use disorder (SUD)
- High-dose or cumulative prescriptions that result in 90 morphine milligram equivalents or higher per day
- Concurrent use of opioids and benzodiazepine or nonbenzodiazepine sedative hypnotics.
This requirement does not apply in the following settings:
- General Hospitals
- Skilled Nursing Facilities
- Mental Health Facilities
- Patients under Hospice Care
Information on this law can be found here: Section 3309 - Opioid overdose prevention.
New York’s 7-Day Rule for Opioid Prescribing
In New York State, the 7-day rule, effective since 2016, limits the initial opioid prescription for acute pain to a 7-day supply (9). This regulation aims to reduce opioid overprescribing and misuse. Providers can prescribe additional supplies of opioid drugs after the initial 7-day period if needed, but they must follow existing rules and regulations for renewals and refills.
Prescription Monitoring Program (PMP) Requirements
The I-STOP Act is a law that mandates that prescribers review the state's PMP registry before prescribing Schedule II, III, and IV controlled substances. The purpose of this initiative is to monitor and prevent prescription drug misuse and diversion.
There are online instructional webinars available that provide education on topics associated with the New York State Prescription Monitoring Program Registry (PMP), including the PMP registry search and use of the PMP Data Collection Tool (12).
Written Treatment Plan for Opioid Prescribing
Effective April 1, 2018, a written treatment plan in the patient’s medical record is required if a practitioner prescribes opioids for pain that has lasted for more than three months or past the time of normal tissue healing (12).
Specific Controlled Substance Regulations
- Schedule II substances require a written or electronic prescription, and refills are not permitted.
- Schedule III-V substances can be prescribed with up to five refills within six months from the date of issue.
Reporting Requirements
- Prescribers must report any dispensed controlled substances to the NYS Department of Health within 24 hours to ensure accurate and up-to-date tracking of NY controlled substances.
Safe Disposal and Prevention Measures
- Drug Take-Back Programs: Prescribers are encouraged to educate patients about proper disposal of unused medications through approved drug take-back programs to prevent misuse.
- Opioid Stewardship Act: Enforces measures for safe opioid prescribing and patient education on the risks of opioid use and misuse.
Title Eight of the Education Law in New York
Title Eight of the Education Law in New York mandates that healthcare professionals with the prescribing authority and who possess a DEA registration number to prescribe NY controlled substances must complete specific educational requirements. This training must incorporate pain management, palliative care, and addiction and should be a minimum of three hours. These requirements must be met every three years.
The training covers eight key areas:
- State and federal laws on prescribing controlled substances
- Pain management
- Appropriate prescribing practices
- Managing acute pain
- Palliative care
- Prevention, screening, and signs of addiction
- Responses to abuse and addiction
- End-of-life care
Upon completion of all required eight (8) training topic areas, practitioners must attest to the completion of this education to the New York State Department of Health (NYSDOH). Documentation of the completion of the course work or training must be maintained by the prescriber for a minimum of six (6) years from the date of the applicable attestation deadline, for audit purposes.
For more information on the mandatory prescriber education requirement, the attestation form, and Frequently Asked Questions, please visit the Department’s Bureau of Narcotic Enforcement website at: http://www.health.ny.gov/professionals/narcotic/.
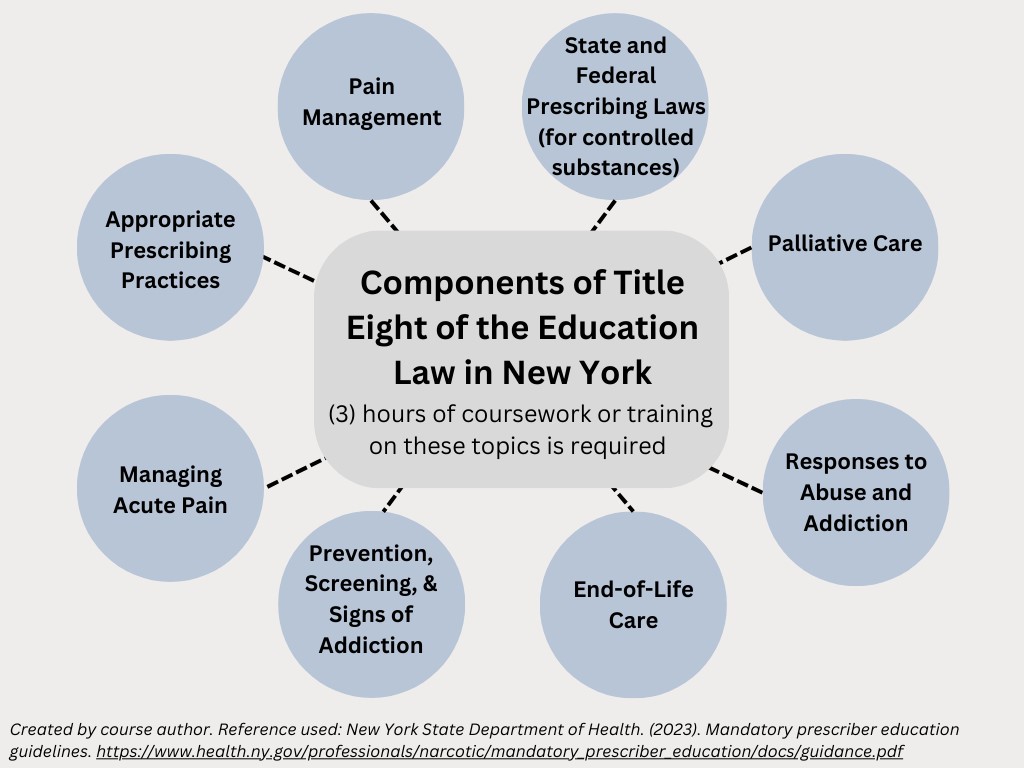

Self Quiz
Ask yourself...
- Can you describe the mandatory E-Prescribing laws in New York?
- What is the I-STOP Act?
- Can you name the components of Title 8 of the Education Law in NY, as it relates to required education for prescribers?
- What is the timeframe allowed for the initial prescribing of narcotics for acute pain management?
Pain Basics
Pain is defined as a subjective experience, which means it cannot be directly observed by those who are not experiencing it. Pain varies greatly from person to person. Pain basics include factors contributing to pain’s subjectivity, pain types, descriptors, and psychological aspects.
Factors Contributing to Pain’s Subjectivity
- Personal Thresholds and Tolerance: Individuals have different pain thresholds and levels of pain tolerance. These thresholds and tolerances can be influenced by genetics, past experiences, and psychological factors.
- Cultural and Social Influences: Cultural background and social conditioning can affect how people perceive and express pain.
- Psychological Factors: Emotions, stress, and mental health conditions can influence the perception of pain. An example is depression, which can exacerbate symptoms of pain.
- Previous Experiences: Past experiences with pain can shape how future pain is perceived. A person who has endured significant pain in the past might react differently to a similar pain compared to someone who has had minimal painful experiences.
- Neurobiological Factors: The neurological system, including how pain signals are processed in the brain, can vary between individuals. Neurological conditions all impact the experience of pain.
Pain cannot be measured objectively in the same way as other physical parameters like temperature or blood pressure. Instead, healthcare providers rely on self-reports from patients and descriptive scales to assess and manage pain.
A meaningful definition of pain was described by McCaffery and Beebe in 1989 as: “Pain is whatever the experiencing person says it is, existing whenever the experiencing person says it does” (14). The exception to this would be individuals with cognitive impairment or inability to verbally communicate their pain.
Pain has been established as the “fifth vital sign” and evaluation of pain is considered as basic as the assessment and management of temperature, blood pressure, respiratory rate, and heart rate.
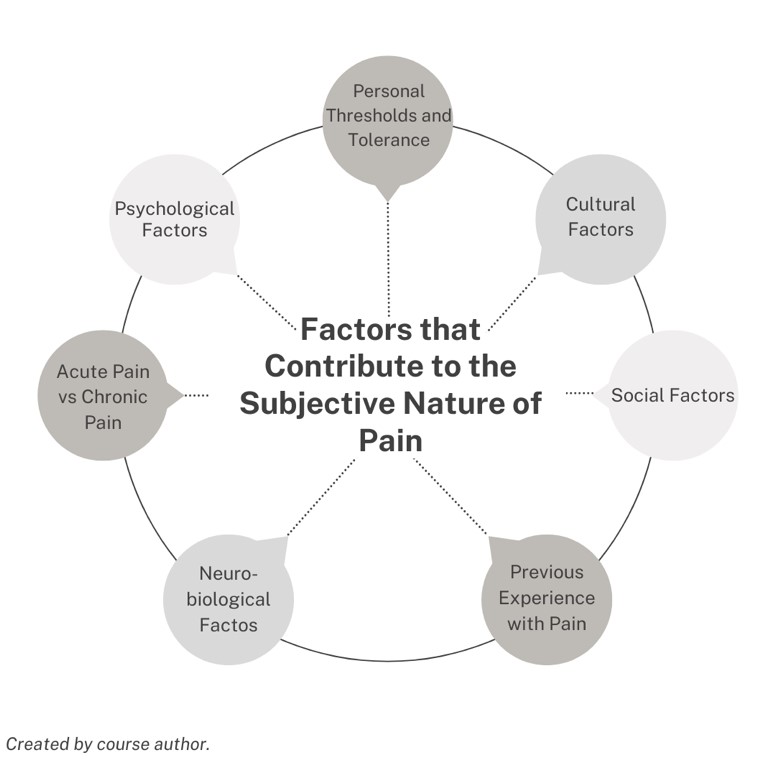
Types of Pain
Pain can be classified as acute or chronic. Acute and chronic pain differ in their duration, causes, and implications for treatment. Understanding these differences helps in the appropriate management of pain, ensuring that those with acute and chronic pain receive the care and support they need.
Acute pain occurs abruptly and often has a specific cause or trigger, such as an injury or illness. Acute pain is short-term, typically lasting less than three months, and usually resolves once the underlying cause is treated or healed.
Common causes of acute pain include:
- Trauma or impact
- Surgery
- Broken bones
- Dental work
- Burns or cuts
- Labor and childbirth
Although uncomfortable for the one experiencing the pain, acute pain has a meaningful purpose and often serves as a warning signal to the body, alerting it to injury or illness that needs attention. Acute pain also triggers protective reflexes, such as pulling your hand away from a hot surface or a sharp object.
Acute pain is usually described as sharp in quality and severe, but it may vary depending on the cause. It often comes on suddenly and is accompanied by visible signs of injury or illness, like swelling, redness, or warmth.
Treatment for acute pain focuses on addressing the underlying cause, such as medication for pain relief, physical therapy, or surgery. It often includes analgesics like NSAIDs or opioids.
Chronic pain persists for longer periods, typically defined as lasting more than three months, and can continue even after the initial injury or illness has healed. It is described as a multidimensional syndrome because the pain can have a profound impact on mental health (anxiety, depression), daily activities (physical, professional, social), and overall quality of life.
In the United States, musculoskeletal pain is increasingly prevalent and is a leading cause of disability (6).
Chronic pain can be more complex to manage and may not have a clear, ongoing cause. Sometimes, chronic pain may occur without any obvious injury or illness. The most common source of chronic pain is musculoskeletal conditions such as back pain or joint pain. It can also result from long-term conditions like arthritis, cancer, neuropathy, or fibromyalgia.
Chronic pain is linked to conditions that include:
- Headache
- Orofacial pain
- Cancer
- Neuropathic pain
- Fibromyalgia
Subsequent manifestations of this pain can include:
- Muscle tension and soreness
- Fatigue
- Decreased energy and motivation
- Loss or change in appetite
- Decreased mobility
- Depression
- Anxiety
Managing chronic pain often requires a multidisciplinary approach, including medications, physical therapy, psychological counseling, dietary changes, and lifestyle changes. Treatment aims to reduce pain, improve function, and enhance the quality of life, rather than eliminate the pain.
Other Descriptors of Pain
Pain can also be characterized as nociceptive, neuropathic, inflammatory, and nociplastic.
- Nociceptive pain is a typical result of excessive stimulation of sensory neuroreceptors that occurs with a normally functioning somatosensory system.
- Inflammatory pain is often of internal origin (e.g. infection, osteoarthritis, digestive pain).
- Neuropathic pain is caused by an abnormality in the peripheral or central somatosensory nervous system. 10% of the United States population complain of neuropathic pain.
- Nociplastic (psychogenic or dysfunctional) pain does not have an origin but is mainly caused by psychological factors.
A sharp or throbbing pain is more likely to be acute nociceptive pain. Pain that is described as burning, shooting, pins, and needles, or electric shock-like points toward a neuropathic origin of pain.
Somatization can be described as a tendency to experience and communicate psychological distress in the form of physical (somatic) symptoms and to seek medical help for them.
Somatosensation encompasses sensations such as touch, pressure, temperature, itch, and pain.
Psychological Aspects of Pain
Chronic pain brings psychological distress, and in return, a cycle of psychological factors can worsen chronic pain. Depression and anxiety can make individuals more susceptible to developing chronic pain conditions. Conversely, chronic pain often leads to increased anxiety and depression, forming a vicious cycle.
Within the biopsychosocial model, negative and discouraging beliefs about pain have a detrimental impact on patients’ overall health, self-efficacy, and function. Thoughts can positively influence beliefs about the pain experience if there is control in managing pain, confidence that harm and disability will not occur, and expectations of recovery.
Cognitive behavioral therapy (CBT) essentially examines an individual’s thoughts and determines if they are accurate and helpful (14). If thoughts are found to be untrue and destructive, mental health professionals can help individuals consider alternate patterns of thinking and beliefs about pain. For example, “I will never enjoy life again with this pain”, or pain catastrophizing, which is the belief that the pain will never go away and will only worsen.

Self Quiz
Ask yourself...
- Do you have experience with patients who have various forms of chronic pain?
- Have you witnessed the psychological impact acute or chronic pain can have on an individual?
- How is therapy altered for acute vs chronic pain?
- What are the differences in duration and pain quality in acute and chronic pain?
Pain Assessment Tools and Techniques
Standardized pain assessment tools are an objective way of monitoring pain levels, quality, aggravating factors, and improvement. The use of pain assessment tools is essential for delivering patient-centered care, ensuring that pain is appropriately recognized and managed.
Using pain assessment tools is crucial to holistic care for several reasons:
- Pain assessment tools provide a standardized way to quantify pain, helping healthcare professionals to assess and compare pain levels more reliably.
- Pain assessment tools enhance communication between patients and healthcare providers as well as ongoing communication between the healthcare team.
- Healthcare providers can appropriately determine the type and dosage of pain relief measures when applying these measurements of pain.
- The regular use of pain assessment tools allows for continuous monitoring of a patient’s pain levels and helps in evaluating the effectiveness of treatments over time.
- Pain assessment tools can aid in identifying changes in a patient's condition.
- Pain assessment tools provide a documented record of a patient’s pain levels and the interventions used. This documentation is meaningful for legal, regulatory, and quality improvement purposes.
- These tools include and empower patients in their treatment plans. This can lead to better adherence to treatment plans and a greater sense of control over their pain management.
Asking the severity of pain on a scale from 0 to 10, with “0” being no pain and “10” being the worst pain imaginable is a common question used to screen patients for pain. This question is acceptable to initially screen a patient for pain, but a thorough pain assessment is required if any pain above 0 is reported.
In this NY Controlled Substance Prescribing course, we will explore the following tools for assessing pain:
- The “PQRSTU” and “OLDCARTES” mnemonics
- Faces Scale
- FLACC Scale
PQRSTU Assessment
The “PQRSTU” assessment mnemonic:
- Provocation/ Palliation: What makes your pain worse? Better?
- Quality: What does the pain feel like? (Ex: “aching,” “stabbing,” or “burning.”)
- Region: Where exactly do you feel the pain? Does it move around or radiate elsewhere?
- Severity: How would you rate your pain on a scale of 0 to 10, with “0” being no pain and “10” being the worst pain you’ve ever experienced?
- Timing/Treatment: When did the pain start? What were you doing when the pain started? Is the pain constant or does it come and go? How long does the pain last?
- Understanding: What do you think is causing the pain?
OLDCARTES Assessment
The “OLDCARTES” assessment mnemonic:
- Onset: When did the pain start? How long does it last?
- Location: Where is the pain?
- Duration: How long has the pain been going on? How long does an episode last?
- Characteristics: What does the pain feel like? Can the pain be described in terms such as stabbing, sharp, dull, aching, piercing, or crushing?
- Aggravating factors: What brings on the pain? What makes the pain worse? Are there triggers such as movement, body position, activity, eating, or the environment?
- Radiating: Does the pain travel to another area of the body, or does it stay in one place?
- Treatment: What has been done to make the pain better and has it been helpful? Examples include medication, position change, rest, and application of hot or cold.
- Effect: What is the effect of the pain on participating in your daily life activities?
- Severity: Rate your pain from 0 to 10.
FACES Scale
The FACES scale is a visual tool for assessing pain in those who cannot quantify the severity of their pain on a scale of 0 to 10. This may include those with cognitive impairment or children.
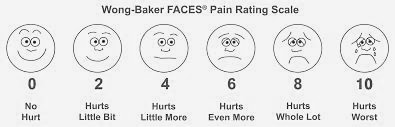
Figure 1. Wong-Baker FACES® Pain Rating Scale (21)
FLACC Scale
The FLACC (Face, Legs, Activity, Cry, Consolability) scale is a measurement used to assess pain for children or individuals who are unable to verbally communicate their pain. The scale is scored in a range of 0–10 with “0” representing no pain.
|
Criteria |
Score 0 |
Score 1 |
Score 2 |
|
Face |
No expression |
Occasional grimace or frown, withdrawn. |
Frequent to constant quivering chin, clenched jaw |
|
Legs |
Normal position or relaxed |
Uneasy, restless, tense |
Kicking, or legs drawn up |
|
Activity |
Lying quietly in a normal position |
Squirming, shifting, back and forth, tense |
Arched, rigid or jerking |
|
Cry |
No cry (awake or asleep) |
Moans or whimpers; occasional complaint |
Crying steadily, frequent screams |
|
Consolability |
Content, relaxed |
Reassured by occasional touching/ distractible |
Difficult to console or comfort |
Table 1. The FLACC Scale (22)

Self Quiz
Ask yourself...
- Are you familiar with these pain assessment tools?
- How is pain assessment modified for individuals with cognitive impairment?
- Why are standardized assessment tools important in managing pain?
- Which of these tools would be more appropriate for a non-verbal patient?
Pain Management
Setting appropriate and achievable goals and expectations of treatment is critical. The goals must be unique to each individual and center around the patient’s activities of daily living and function.
Pain management goals can include the absence of pain; however, absence may not always be possible, and goals should focus on the reduction of pain to a level that the patient can have optimal functioning. Practical, measurable goals should specify an action and frequency.
Components of goals:
- Behavior is within the individual’s control and is practical, being they were able to do this before the pain.
- Goal is measurable
- Not primarily focused on pain reduction (i.e., reduce pain totally or by a specific amount)
Examples of appropriate goals:
- Being able to do one load of laundry once a week.
- Being able to walk to the mailbox each day.
- Take dogs to the park for 30 minutes once per week.
Recent evidence-based clinical practice guidelines from the American College of Physicians strongly recommend that clinicians should initially select nonpharmacologic treatment, including multidisciplinary rehabilitation, exercise, acupuncture, yoga, or mindfulness-based stress reduction. The guidelines also encourage the patient's active involvement in their care planning.
| Non- Pharmacological Pain Therapies | Description |
| Therapies and Rehabilitation |
|
| Self-Care |
|
| Complementary Therapies |
|
| Behavioral And Mental Health Therapies |
Psychiatrists, clinical social workers, and mental health counselors provide therapies that identify and treat mental disorders or substance abuse problems that may serve as barriers to pain management. |
Non-Pharmacological Approaches to Pain Management
Individualized care is a collaborative process among patients and their multidisciplinary care team. Pain management should include the patients, caregivers, and various healthcare providers. Individualized care can improve aspects of physical health, mental health, and the ability to self-manage conditions.
Non-Pharmacological Pain Management: Physical and Occupation Therapy
Physical and occupational therapy are highly effective for pain management, function improvement, strength, and overall well-being. Physical therapy focuses on exercises and activities that enhance mobility, strength, and flexibility, which help reduce pain by alleviating stiffness and strain. Additional techniques include massage, heat/cold therapy, and electrical stimulation to provide direct pain relief and promote healing of injured tissues. Physical therapists provide essential education on body mechanics and posture that further helps to prevent pain and injury. These therapies often help patients avoid addictive pain medications, surgeries, and invasive procedures.
Physical therapy generally leads to improved outcomes and decreased health care costs.
Physical therapy interventions can integrate the following:
- Exercise
- Passive Therapy
- Heat or Ice
- Massage
- Ultrasound
- TENS and Electrical Stimulation
- Dry needling
- Pain Neuroscience Education (PNE)
Pain Neuroscience Education (PNE) is a vital part of the management of acute and chronic pain.
Neuroscience pain experts have found that learning about pain through pain neuroscience education (PNE) can improve symptoms, mobility, and feelings of psychological well-being in those with chronic pain. Essentially, teaching patients about their pain and why it is happening can ultimately lead to better outcomes in PT sessions and long-term goals. Physical therapists may spend time teaching about pain, why the pain may be occurring, and how an individual can take control of pain.
Occupational therapy, on the other hand, helps patients modify their daily activities and environments to reduce pain and prevent injury. By teaching pain management strategies, recommending ergonomic adjustments, and improving strength and endurance, occupational therapists enable patients to perform daily tasks with less discomfort. They also address the psychological aspects of pain, providing support and coping mechanisms.
The use of concurrent physical and occupational therapy offers a holistic and comprehensive approach to pain management. They empower patients to take an active role in their care, improving pain levels, function, and quality of life.
The following are methods of overall reduction in pain and improvement of quality of life:
- Encourage positive health habits, roles, and routines gained in OT and PT.
- Set goals that are client-centered, and occupation-based.
- Encourage proactive problem-solving habits.
- Prevent pain onset by self-management techniques.
- Teach ways to avoid fear-avoidance, avoiding tasks due to fear of pain.
- Educate the client on energy conservation.
- Consider whole-body exercises such as yoga, stretching, and tai-chi.
- Focus on problem-solving and how to live with the pain.
Collaboration among the healthcare team is critical. Medical staff can gain vital insight from therapists on goals and outcomes and in turn relay information about opioid analgesics and other symptom-targeted treatments.
Non-Pharmacological Pain Management: Cold Therapy
Clinicians must recognize the underlying pathophysiology that occurs with the application of ice or heating pads/products. It may seem simple, but there are key indicators that could either improve pain or cause worsening or additional injuries.
The application of cold is better for immediate injuries and heat is typically better for chronic conditions. Patients can implement this therapy on their own, and this independent activity may increase self-efficacy and reduce negative thought patterns. However, safety practices should be taught to patients to avoid injuries from the cold or heat.
Common types of cold therapy:
- Cold packs
- Cold compresses
- Aquathermia pad (attached to a cooling/heating unit): The unit has two hoses and is filled with distilled water to bring it to the desired temperature. The water flows through one of the hoses and into the tubes in the pad.
Cold therapy uses:
- Acute musculoskeletal injuries
- Muscle spasming and contraction
- Post-surgical intervention
Guidelines for using cold therapy include:
- Limit duration of application. Prolonged exposure to the cold application can result in hypoxia and tissue damage, rebound inflammation, and frostbite.
- Monitor patient reaction. Assess the skin appearance. A splotchy, white appearance, or if the patient complains of numbness or burning, could indicate impaired blood flow to the tissue receiving cold application.
- Review provider orders. Typically, cold therapy is executed for 15 to 20 minutes at a time depending on the condition or injury. For an acute musculoskeletal injury, the cold application may be repeated every 2 hours as well.
- Document the type of cold therapy, the duration, the patient’s reaction, and the effect.
Non-Pharmacological Pain Management: Heat Therapy
The application of heat causes blood vessels in the area to dilate; this increase in blood flow brings more oxygen and nutrients to the surrounding tissue for healing. The vasodilation also encourages excess fluid to be removed from the area more effectively.
Heat can help to relieve pain, relax muscles, promote healing, reduce tissue swelling, and decrease joint stiffness. The sensation of heat may decrease the transmission of pain signals to the brain, which can relieve pain and discomfort.
Heat applications are used for chronic, or ongoing, conditions. These include back pain and arthritis; heat may also be used only after the first two to three days following an acute, or sudden, injury (1).
Research studies have found the appropriate heat application is effective in relieving chronic lower back pain and chronic knee pain.
Common types of heat therapy:
- Aquathermia pad
- Hot packs (produces dry heat; used to treat muscle sprains and mild inflammations)
Some hot packs are filled with hot fluid and may be heated in the microwave, in hot water, or by striking or squeezing them to activate chemicals. The water temperature of a hot pack should not exceed 110°F or 43°C.
Guidelines for using heat therapy include:
- Apply for 20 to 30 minutes every 2 to 3 hours
- Leaving heat packs in place longer than 45 minutes can cause a rebound phenomenon (constriction of vessels instead of dilation)
Patient education and empowerment can have a significant impact on pain management.

Self Quiz
Ask yourself...
- What are some safety guidelines for using heat therapy?
- Can you describe injuries and pain that ice and cold therapy would be more appropriate than heat therapy?
- Are you familiar with devices that deliver cold and heat therapy?
- How would you describe the role of physical and occupational therapy in the management of acute and chronic pain?
Non-Pharmacological Pain Management: Cognitive and Behavioral Strategies
Researchers have studied several types of non-pharmaceutical pain management methods that have been proven effective in chronic pain management; these include:
- Cognitive-behavioral therapy (CBT)
- Mindfulness-based therapy
Both strategies have been shown to improve psychological adjustment to pain and coping with it.
Cognitive behavior therapy (CBT) is a type of psychotherapy that focuses on unhelpful or unhealthy ways of thinking, feeling, and behaving.
The goal of CBT in the management of pain is to provide individuals with an active, problem-solving approach to manage and decrease the challenges associated with chronic pain. By applying these helpful strategies, it is possible to change one’s pain experience, physically and emotionally.
Goals of CBT for pain management (14):
- Contradict false and discouraging concepts of pain control and management
- Increase participation in meaningful activities
- Manage pain flare-ups more effectively
- Reduction in worries and anxiety about increased pain or injury
- Improvement of overall quality of life
Mindfulness is practicing a state of awareness and staying present or mindful in daily life, rather than thinking of the past or future. Mindfulness involves various techniques and practices. Being present is an ongoing practice and consistent dedication to actions and thoughts, rather than a single action.
Two major concepts of mindfulness may help reduce various forms of psychological distress:
- Awareness of oneself and immediate surroundings.
- Non-judgmental acknowledgment and acceptance of what is being experienced from moment to moment.
By using certain mental and physical tools, such as mindful breathing, meditation, and body scans, individuals can direct their attention to the present moment, which can help to cultivate everything from inner stillness to self-control.
Research studies reinforce the positive effects of mindfulness, revealing an association with psychological health improvement and differences in brain activity (13). These studies indicate that the practice of mindfulness alters brain pathways and function in areas of the brain, including the medial cortex, default mode network, insula, amygdala, lateral frontal regions, and basal ganglia; these areas in the brain are involved in the transmission of pain sensations as well.
Non-Pharmacological Pain Management: Acupuncture
Acupuncture is a technique in which fine needles are inserted into the skin to treat certain conditions and interrupt pain transmission. The needles may be manipulated manually by a practitioner, or stimulated with small electrical currents, which is called electroacupuncture. According to national survey data, acupuncture is most commonly used for back, joint, or neck pain.
Acupuncture has been practiced for at least 2,500 years and originated from traditional Chinese medicine. According to the World Health Organization, acupuncture is used in 103 of 129 countries that reported data (9).
There has been a rapid rise in the use of this technique in the United States over the past few decades.
Non-Pharmacological Pain Management: Yoga
A systematic review explained by the National Center for Complementary and Integrative Health (2020) notes yoga as an effective tool in the management of specific types of chronic pain.
Studies have found that yoga can be helpful in the following conditions:
- Fibromyalgia
- Low-back pain
- Neck pain
- Arthritis
Non-Pharmacological Pain Management: Nutritional Consult
Adequate nutrition plays a role in inflammatory and metabolic concepts that impact pain management. There is a substantial relationship between nutrition and chronic pain, but not typically integrated into the care plan despite the emerging evidence that poor nutrition and dietary intake play a key role in the development and management of chronic pain (7). Health professionals need to be aware of and understand the role nutrition plays in chronic pain


Self Quiz
Ask yourself...
- What are some goals of cognitive behavior therapy in pain management?
- What are the American College of Physicians’ recommendations in the initial treatment of acute pain?
- How would you describe the role of nutrition and reduced inflammation in the experience of pain? For which conditions is yoga helpful?
Pharmacological Approaches to Pain Management
|
Non-Opioid Drug Class |
Description |
|
Nonsteroidal Anti-Inflammatory Drugs |
|
|
Controlled Substances |
Description |
|
Schedule II & IIN
|
Opioids and Opiates
|
|
Schedule III |
|
|
Schedule IV |
|
|
Adjuvant Medications |
Description |
|
Anticonvulsants |
|
|
Antidepressants |
|
|
Topicals: Medicated Creams, Foams, Gels, Lotions, Ointments, Patches |
|
|
Interventional Pain Management |
|
Pharmacological Pain Management: NSAIDs
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a drug class FDA-approved for use as antipyretic, anti-inflammatory, and analgesic agents. NSAIDs are used for treating muscle pain and strains, dislocations, dysmenorrhea, arthritic conditions, pyrexia, gout, and migraines.
NSAIDs are typically divided into groups based on their chemical structure and selectivity:
- Acetylated Salicylates (Aspirin)
- Non-acetylated Salicylates (Diflunisal, Salsalate)
- Selective COX-2 Inhibitors (Celecoxib, Etoricoxib).
- Propionic Acids (Naproxen, Ibuprofen
- Acetic Acids (Diclofenac, Indomethacin)
- Enolic Acids (Meloxicam, Piroxicam)
- Anthranilic Acids (Meclofenamate, Mefenamic Acid),
- Naphthylalanine (Nabumetone)
Topical NSAIDs are also available for use.
Mechanism of Action of NSAIDs: The primary mechanism of action of NSAIDs is the inhibition of the enzyme cyclooxygenase (COX); this enzyme converts arachidonic acid into thromboxanes, prostaglandins, and prostacyclins (5). Prostaglandins cause vasodilation, help regulate temperature, and play a vital role in anti-nociception of pain; thromboxanes aid in platelet adhesion (5)
There are two cyclooxygenase isoenzymes: COX-1 and COX-2.
- COX-1 impacts gastrointestinal mucosa lining, kidney function, and platelet aggregation.
- COX-2 is expressed during an inflammatory response.
The majority of NSAIDs inhibit both COX-1 and COX-2; except COX-2 selective NSAIDs (ex. celecoxib) only target COX-2. The COX-2 essentially provides anti-inflammatory relief without compromising the gastric mucosa.
NSAIDs are contraindicated in the following patients:
- Those with NSAID hypersensitivity or salicylate hypersensitivity
- Those who have experienced an allergic reaction after taking NSAIDs
- Those who have undergone coronary artery bypass graft surgery
- Patients in the third trimester of pregnancy
Adverse/ Side Effects: NSAIDs have well-established adverse effects affecting the gastric mucosa, renal system, cardiovascular system, hepatic system, and hematologic system (5)
The most frequently reported side effects of NSAIDs are gastrointestinal symptoms, such as:
- Heartburn
- Stomach pain
- Nausea and vomiting
- Diarrhea
- Constipation
Taking NSAIDs with food, milk or antacids may reduce these symptoms.
Additional side effects of NSAIDs include:
- Dizziness.
- Difficulty concentrating
- Mild headaches
Pharmacological Pain Management: Opiates and Opioids
Opiates are chemical compounds that are extracted or refined from natural plant matter (poppy sap and fibers).
Examples of opiates:
- Opium
- Morphine
- Codeine
- Heroin
Opioids are chemical compounds that are generally not derived from natural plant matter. Most opioids are synthesized. Some opioids are partially synthesized from chemical components of opium, while other commonly used opioid molecules are designed and manufactured in laboratories. The pharmaceutical industry has created more than 500 different opioid molecules.
Common opioids used in the United States for pain management:
- Fentanyl/fentanyl
- Dextropropoxyphene
- Hydrocodone
- Oxycodone
- Oxymorphone
- Meperidine
Pharmacological Pain Management: Fentanyl
Fentanyl is a synthetic opioid agonist that is 80-100 times stronger than morphine and is often added to heroin to increase its potency (4). Fentanyl is significantly more potent than other opioids. Fentanyl can cause severe respiratory depression and has high addiction potential.
Fentanyl drug information (15):
Drug Class
- Opioid, narcotic agonist (Schedule II).
Uses
- Pain relief, preop medication; adjunct to general or regional anesthesia. Management of chronic pain (transdermal).
Mechanism of Action
Opioids can be classified according to their effect on opioid receptors and can be considered as agonists, partial agonists, antagonists, and agonist-antagonists.
- Agonists interact with an opioid receptor to produce a maximal response from that receptor.
- Antagonists bind to receptors but produce no functional response, while at the same time preventing an agonist from binding to that receptor (naloxone).
- Partial agonists bind to receptors but elicit only a partial functional response regardless of the amount of drug administered.
- Agonist-antagonists act as agonists to a certain opioid receptor but have antagonist activity to another opioid receptor.
Fentanyl binds to and activates the mu-opioid receptors (MORs) in the brain and spinal cord. These receptors are part of the endogenous opioid system, which regulates pain, reward, and addictive behaviors. Mu-opioid receptors are widely distributed throughout the body and play a crucial role in mediating the effects of opioids. MORs are found in the central nervous system (brain, thalamus, cortex, brainstem, hypothalamus), the spinal cord, peripheral nervous system (nerve endings), gastrointestinal tract, muscle tissue, etc. This wide distribution of MORs in both the central and peripheral nervous systems, as well as in other tissues, explains the broad range of effects opioids have on the body, including analgesia, euphoria, respiratory depression, and gastrointestinal disturbances.
By binding to the mu-opioid receptors, fentanyl inhibits the release of neurotransmitters involved in pain signaling, such as substance P, glutamate, and GABA (15). This interferes with the transmission of pain signals from the peripheral nervous system to the CNS, which essentially reduces the acknowledgment of pain (15).
Fentanyl also increases potassium conduction and decreases calcium influx in neurons, which hyperpolarizes the neuronal membrane and reduces the pain signal transmission. Fentanyl alters the perception of pain by modulating pain pathways at various levels of the CNS, which changes how pain is experienced and processed by the brain.
Fentanyl also produces euphoria and sedation by acting on the reward pathways in the brain, specifically through the mesolimbic dopamine system. This action contributes to its potential for misuse and addiction.
Onset of Action for Adults
- IM: 7 to 8 minutes
- IV: Almost immediate (maximal analgesic and respiratory depressant effects may not be seen for several minutes)
- Transdermal patch (initial placement): 6 hours
- Transmucosal: 5 to 15 minutes
Duration
- IM: 1 to 2 hours
- IV: 0.5 to 1 hour
Protein Binding
- 79% to 87%, primarily to alpha-1 acid glycoprotein; also binds to albumin and erythrocytes.
Metabolism
- Hepatic, primarily via CYP3A4 by N-dealkylation and hydroxylation to other inactive metabolites.
Half-Life Elimination
- IV: Adults: 2 to 4 hours; when administered as a continuous infusion, the half-life prolongs with infusion duration due to the large volume of distribution (Sessler 2008)
- SubQ bolus injection: 10 hours
- Transdermal device: Terminal: ~16 hours
- Transdermal patch: 20 to 27 hours
- Transmucosal products: 3 to 14 hours (dose dependent)
- Intranasal: 15 to 25 hours (based on a multiple-dose pharmacokinetic study when doses are administered in the same nostril and separated by a 1-, 2-, or 4-hour time lapse)
- Buccal film: ~14 hours
- Buccal tablet: 100-200 mcg: 3 to 4 hours; 400 to 800 mcg: 11 to 12 hours
Time to Peak
- Buccal film: 0.75 to 4 hours (median: 1 hour)
- Buccal tablet: 20 to 240 minutes (median: 47 minutes)
- Lozenge: 20 to 480 minutes (median: 20 to 40 minutes)
- Intranasal: Median: 15 to 21 minutes
- SubQ bolus injection: 10 to 30 minutes (median: 15 minutes) (Capper 2010)
- Sublingual spray: 10 to 120 minutes (median: 90 minutes)
- Sublingual tablet: 15 to 240 minutes (median: 30 to 60 minutes)
- Transdermal patch: 20 to 72 hours; steady-state serum concentrations are reached after two sequential 72-hour applications
Excretion
- Urine 75%; feces ~9%
Side Effects
- IV: Postop drowsiness, nausea, vomiting.
- Transdermal: Headache, pruritus, nausea, vomiting, diaphoresis, dyspnea, confusion, dizziness, drowsiness, diarrhea, constipation, decreased appetite.
Adverse Effects
Overdose or too-rapid IV administration may produce severe respiratory depression, skeletal and thoracic muscle rigidity. This muscle rigidity may lead to apnea, laryngospasm, bronchospasm, cold/clammy skin, cyanosis, and coma. Tolerance to analgesic effect may occur with repeated use. The antidote for Fentanyl is naloxone.

Self Quiz
Ask yourself...
- What is the time of onset for the various forms of fentanyl?
- How is the half-life meaningful when prescribing fentanyl?
- What are some common side effects of fentanyl?
- Can you name some management strategies for these side effects?
Nursing Considerations for Fentanyl Administration
Considerations for the nurse administering Fentanyl include (15):
- Prepare: Resuscitative equipment and opiate antagonist (naloxone 0.5 mcg/kg) should be available for initial use.
- Establish baseline blood pressure, pulse rate, and respirations.
- Assess the type, location, intensity, and duration of pain using a standardized assessment tool.
- Assess fall risk and implement appropriate precautions.
- Monitor respiratory rate, B/P, heart rate, oxygen saturation.
- Re-assess for relief of pain.
- Assist with ambulation and encourage the patient to turn, cough, and deep breathe every two hours.
- For patients with prolonged high-dose use, and continuous infusions (critical care, ventilated patients), clinicians should consider weaning drip gradually or transitioning to a fentanyl patch to decrease symptoms of opiate withdrawal.

Self Quiz
Ask yourself...
- How do the mechanisms of action differ between agonists, partial agonists, antagonists, and agonist-antagonists?
- Can you describe how fentanyl prevents the release of pain neurotransmitters?
- Where are MORs located in the body?
- How much more potent is fentanyl than morphine?
Regulation and Schedules of Controlled Substances
The Controlled Substances Act (CSA) requires that all substances must be regulated under existing federal law and categorized into five schedules. The schedule determination is based on the substance’s medical use, potential for abuse, and safety or dependence liability (7).
These factors are listed in Section 201 (c), [21 U.S.C. § 811 (c)] of the CSA as follows (7):
- The actual or relative potential for abuse.
- Scientific evidence of its pharmacological effect, if known.
- The current state of scientific knowledge on the substance or drug.
- The historical pattern of abuse.
- The scope, duration, and significance of abuse.
- Risk to the public health.
- Any psychic or physiological dependence liability.
- If the substance is an immediate precursor of a substance already controlled under this subchapter.
Based upon this law, the United States Drug Enforcement Agency (DEA) maintains a list of controlled medications and illicit substances categorized from Schedule I to V. Schedule I drugs are considered to have the highest risk of abuse and have no recognized medical use in the United States. Schedule V drugs have the lowest potential for abuse among controlled substances.
Description of Schedule I through V drugs (7):
Schedule I
- Examples: Marijuana, heroin, mescaline (peyote), lysergic acid diethylamide (LSD), methylenedioxymethamphetamine (MDMA)
Schedule II
- High abuse potential with severe psychological or physical dependence; however, these drugs have an accepted medical use and may be prescribed, dispensed, or administered.
- Examples: Fentanyl, oxycodone, morphine, hydromorphone
- Schedule II drugs should not have a refill at the pharmacy
Schedule III
- Abuse potential, but considered less than Schedule II
- Examples: Ketamine
Schedule IV
- "Abuse potential less than Schedule II but more than Schedule V medications"
- Examples include diazepam, alprazolam, and tramadol
Schedule V
- The least potential for abuse among the controlled substances.
- Examples: Pregabalin and dextromethorphan

Controlled Substance Addiction
The United States is facing an opioid epidemic with unparalleled impact. Drug overdoses are the leading cause of accidental deaths in the United States (8). Roughly two-thirds of drug overdose deaths were caused by opioids— both legal and illicit (3). There are two intertwined epidemics: the excessive use of opioids for both legal and illicit purposes, and unprecedented levels of consequent opioid use disorder (OUD).
Overview of Addiction Disorders in New York State
New York State has been significantly impacted by addiction disorders, particularly opioid abuse. According to the New York State Department of Health and the Office of Addiction Services and Supports (OASAS), substance use, and related disorders are on the rise. In 2022 approximately 3,030 New Yorkers died of a drug overdose, which is a 12% increase from 2021 (2,696 deaths), and the highest amount since reporting started in 2000. Opioids, particularly fentanyl, were involved in over 84% of these overdose deaths (13).
Commonly Abused Substances
- Opioids
- Stimulants (cocaine and methamphetamine)
- Alcohol
- Cannabis
Substance abuse and overdose are higher among certain demographics of individuals in New York. Overdose fatalities of male New Yorkers were nearly four times as high as the rate among females (13). Blacks have the highest rate, followed by Hispanics/Latino and whites (13). High-poverty neighborhoods had a larger increase in overdose rates in 2022, and these residents in high-poverty neighborhoods had the highest rate of overdose deaths (13).
Opioid Use Disorder
An opioid use disorder (OUD) is defined as a pattern of opioid use that leads to serious impairment or distress (5).
In the late 1990s, prescription opioid use increased in all regions of the United States. Unregulated prescription opioid use was promoted, in large part by the pharmaceutical industry (5). Misuse and diversion of these medications became widespread; by 2017, an estimated 1.7 million people in the United States suffered from substance use disorders related to prescription opioid pain medications (5).
The DSM-5 Criteria is an excellent guide for diagnosing OUD.
To be eligible for methadone treatment, patients must meet DSM-5 criteria for OUD.
DSM-5 Criteria for Opioid Use Disorder:
- Opioids are often taken in larger amounts or over a longer period than was intended
- There is a persistent desire or unsuccessful efforts to cut down or control opioid use.
- A great deal of time is spent in activities necessary to obtain the opioid, use the opioid, or recover from its effects.
- Craving or a strong desire to use opioids.
- Recurrent opioid use causes failure to fulfill major role responsibilities at work, school, or home.
- Continued opioid use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of opioids.
- Important social, occupational, or recreational activities are given up or reduced because of opioid use.
- Recurrent opioid use in situations in which it is physically hazardous.
- Continued use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by opioids.
- Tolerance as defined by either of the following: (1) Need for markedly increased amounts of opioids to achieve intoxication or desired effect or (2) Markedly diminished effect with continued use of the same amount of opioid
- Withdrawal as manifested by either of the following: (1) Characteristic opioid withdrawal syndrome or (2) The same (or a closely related) substance is taken to relieve or avoid withdrawal
The presence of at least 2 of these symptoms indicates an OUD.
The severity of the OUD is defined as:
- MILD: The presence of 2 to 3 symptoms
- MODERATE: The presence of 4 to 5 symptoms
- SEVERE: The presence of 6 or more symptoms
Diagnosing patients can be a controversial practice. However, establishing this diagnosis is required in some work settings and for third-party billing (2). The DSM-5 no longer includes the terms substance abuse, substance dependence, or addiction because of the lack of clarity and stigma.
Two types of substance-related disorders are distinguished in the DSM-5:
- SUDs
- Substance-induced disorders
- Intoxication, withdrawal, and other substance-induced mental disorders.
- All SUDs in the DSM-5 are diagnosed according to severity based on the number of symptoms.
Drug testing is required in some settings because people with active addictions typically minimize, deny, and lie about the extent of their drug use (2).

Self Quiz
Ask yourself...
- How is Opioid Use Disorder (OUD) defined?
- What is the DSM-5 criteria for this diagnosis?
- How can clinicians determine if opioids are having an impact on a patient’s functional level?
- Can you think of reasons it is important to appropriately diagnose the disorder before prescribing medications for the treatment?
Screening and Assessment Tools for Substance Misuse
There are many tools and instruments that can help with OUD assessment. A general history questionnaire is useful for clinicians and counselors, followed by a more specific assessment of substance misuse and addiction.
- The American Psychiatric Association has developed the DSM-5 Self-Rated Level 1 Cross-Cutting Symptom Measures (adult, ages 11– 17, or ages 6– 17) to get a general diagnostic idea of an individual or the specific measure for substance use in each age category. The measures are available from https://www.psychiatry.org/psychiatrists/practice/dsm/educational-resources/assessment-measures
Additional Tools:
- The National Institute on Drug Abuse (NIDA) - provides several evidence-based screening tools and resource materials.
Signs and Symptoms of Substance Misuse and Addiction
Signs of alcohol and drug use include:
General Appearance
- Disheveled appearance
- Hyperactivity
- Hypoactivity
- Wearing long sleeves at inappropriate times
- Weight gain or loss
Neurological
- Constricted pupil
- Dilated pupils
- Diminished alertness
- Sedated
- Sleepiness
- Insomnia
- Poor concentration
- Poor judgement
- Slurred speech
- Tremors
- Unsteady gait
Mood
- Lying
- Mood changes
- Defensiveness/ paranoia
- Denial
Other
- Bloodshot eyes
- Watery eyes
- Frequent accidents
- Frequent pain complaints
- Perforation of the nasal septum
- Runny nose
- Unexplained nausea, vomiting, or diarrhea
- Diaphoresis
Substance Abuse Among Healthcare Professionals
Unfortunately, there is a high prevalence of substance and alcohol use disorders in healthcare settings, which has increased awareness of the issue. When these disorders occur in healthcare settings, the risk of unintended harm to patients makes this an issue of high importance.
Symptoms of alcohol and substance use disorder within the healthcare setting (19):
- Abnormal wasted opioids
- Altered orders
- Arriving to work late
- Difficulty meeting deadlines
- A discrepancy in controlled substance records
- Dishonesty
- Documentation errors
- Excessive sick time
- Frequent mistakes
- Frequent reports of patients not receiving pain relief
- Frequent unexplained absences
- Maximum use of pain medications
- Not performing narcotic counts
- Obsession with opioids
- Offering to medicate patients
- Poor quality work and poor charting
- Rounding at odd hours
Behaviors that are associated with drug diversion (19):
- Altered orders for drugs
- Discrepancies for controlled substances
- Frequent corrections on medication records
- Higher-than-average opioid administration
- Higher-than-average opioid wastage
- Incorrect opioid counts
- Patients complaining of poor pain relief
- Tampering with capsules or vials
- Unexplained disappearances or trips to isolated areas
Responses to Addiction and Controlled Substance Misuse
New York State has a robust system for addressing addiction, overseen by OASAS. This includes a variety of treatment options, such as outpatient programs, inpatient rehabilitation, medication-assisted treatment (MAT), and harm reduction services. NY integrates a data-driven approach to monitor and respond to addiction trends effectively.
Key Initiatives and Programs
- Prevention and Early Intervention: Programs aimed at reducing the onset of substance use, particularly among youth and high-risk populations.
- Treatment Accessibility: Efforts to make treatment services more accessible, including expanding telehealth options and ensuring coverage for addiction services under health insurance plans.
- Harm Reduction: Distribution of naloxone to reverse opioid overdoses, safe consumption spaces, and needle exchange programs to reduce the harms associated with drug use.
- Recovery Support: Providing long-term support for individuals in recovery, including housing assistance, employment services, and peer support networks.
Responses to Addiction and Controlled Substance Abuse
- Medication-Assisted Treatment (MAT)
- Utilizes medications like methadone, buprenorphine, and naltrexone in combination with counseling and behavioral therapies to treat opioid use disorder (OUD).
- MAT has been shown to reduce opioid use, improve retention in treatment, and decrease the risk of overdose Naloxone Distribution
- Counseling and Behavioral Therapies
- Public Education and Prevention Programs
- Policy and Regulatory Measures
- Support Groups and Peer Support
Outside of prison, the most effective treatment for OUD is a combination of Medication-Assisted Treatment (MAT) and mental health counseling and therapies.
Medication-Assisted treatment for Opioid Use Disorder
Medication-assisted treatment (MAT) is the use of medications, in combination with counseling and behavioral therapies, in the treatment of opioid use disorders (OUD). The goal is sustained recovery. Often, individuals have actual, pain, and become dependent on prescription narcotic drugs, then switch to illicit opioids or opiate heroin when the medically supplied narcotics run out.
The U.S. Food and Drug Administration (FDA) requires that prescribing information for medicines intended for use in the outpatient setting include how to safely decrease the dose. Prescribers should not abruptly discontinue opioids in a physically dependent patient, but slowly taper the dose of the opioid and continue to manage pain therapeutically.
The FDA has only approved three MATs for OUD: methadone, buprenorphine, and naltrexone.
Buprenorphine and methadone have been shown to decrease mortality among those with OUD (16). A recent study reported that buprenorphine was associated with a lower risk of overdose during active treatment compared to post-discontinuation.


Self Quiz
Ask yourself...
- Can you name the drugs approved by the FDA for the treatment of OUD?
- How can partnerships between policymakers and healthcare providers enhance MATs?
- How would you describe your experience with addiction treatment programs?
- Have you ever administered methadone in your nursing practice?
Treatment of Opioid Use Disorder: Methadone
Methadone is a medication approved by the FDA to treat OUD and manage chronic pain. Methadone is safe and effective when taken as prescribed. Methadone is a component of a comprehensive treatment plan, which includes counseling and other behavioral health therapies to provide patient-centered care.
Methadone, a long-acting opioid agonist that helps to relieve cravings and withdrawal, while also blocking the effects of opioids (18). Methadone is available in liquid, powder, and diskette forms. Patients taking methadone to treat OUD must receive the medication under the supervision of a medical provider, but after a period of stability and consistent compliance, patients may be allowed to take methadone independently at home between provider visits (18).
Drug information for Methadone includes (12):
Methadone Drug Cass
Opioid agonist (Schedule II)
Methadone Uses
Methadone is a first-line Opioid Addiction Treatment (OAT) option, along with buprenorphine. Methadone may be preferable to buprenorphine for patients who are at high risk of treatment cessation and subsequent fentanyl overdose. It also alters processes affecting analgesia, and emotional responses to pain, and reduces withdrawal symptoms from other opioid drugs (18).

Self Quiz
Ask yourself...
- Can you name the uses of methadone?
- How does the mechanism of action of methadone help to alleviate withdrawal symptoms from opioids?
- Is the half-life of this drug considered long or short?
- Why is it important to recognize that methadone binds to plasma proteins in circulation?
Methadone Pharmacokinetics
Description of methadone pharmacokinetics per route (12):
|
Route |
Onset |
Peak |
Duration |
|
PO |
0.5 – 1 hour |
1.5 – 2 hours |
6 – 8 hours |
|
IM |
10 – 20 mins |
1 – 2 hours |
4 – 5 hours |
|
IV |
n/a |
15 – 20 mins |
|
Methadone is also (18):
- Well-absorbed after IM injection.
- Protein binding: 85%–90%.
- Metabolized in liver. Primarily excreted in urine.
- Not removed by hemodialysis.
- Half-life: 7– 59 hrs.
- Crosses the placenta and is found in breast milk.
Methadone Precautions
Considerations when prescribing methadone (20):
- Respiratory issues may occur in neonates if the mother received opiates during labor.
- Elderly patients are more susceptible to respiratory depressant effects.
- Age-related renal impairment may increase the risk of urinary retention.
- Caution: Renal/ hepatic impairment, elderly/debilitated pts, risk for QT prolongation, medications that prolong QT interval, conduction abnormalities, severe volume depletion, hypokalemia, hypomagnesemia, cardiovascular disease, depression, suicidal tendencies, history of drug misuse, respiratory disease, and biliary tract dysfunction
Side Effects
As with other opioid medications, general side effects of methadone are related to excessive opioid receptor activity, including but not limited to:
- Diaphoresis/flushing
- Pruritis
- Nausea
- Dry mouth
- Constipation
- Sedation
- Lethargy
- Respiratory depression
Warnings
- May prolong the QT interval, which may cause serious arrhythmias.
- May cause serious, life-threatening, or fatal respiratory depression.
- Monitor for signs of misuse, misuse, and addiction.
- Prolonged maternal use may cause neonatal withdrawal syndrome.
- Do not confuse methadone with Mephyton, Metadate CD, Metadate ER, methylphenidate, or morphine
- Serious adverse effects: pancreatitis, hypothyroidism, Addison’s disease, head injury, increased intracranial pressure.
Methadone Dosing and Titration for Prescribers
Information for prescribers in dosing and titrating methadone include (20):
- The clinician should attempt to reach an optimal dose of methadone safely and quickly (3).
- Starting methadone at 30mg is recommended.
- The starting dose of methadone can be increased by 10–15mg every three to five days.
- Slower titration is recommended for patients at higher risk of toxicity (e.g., older age, sedating medications or alcohol, patients new to methadone).
- Patients who have recently been on methadone dosing at higher doses (i.e., in the previous week) can be considered for more rapid dose increases based on their tolerance.
- Once a dose of 75–80mg is reached, the dose can then be increased by 10mg every five to seven days.
- If four consecutive missed doses, the dose of methadone should be reduced by 50% or to 30mg, whichever is higher. If five or more consecutive doses are missed, methadone should be restarted at a maximum of 30mg and titrated according to patient need.
- SROM at a maximum starting dose of 200mg can be added on the day of a restart, as long as the patient has not become completely opioid-abstinent.
- For patients who use fentanyl regularly, methadone doses of 100mg or higher are often appropriate.
- Use prescription practices that promote treatment retention, including phone visits, check-ins, extending prescriptions, or leaving longer-duration methadone prescriptions for 30mg at the pharmacy so patients can restart treatment.
- Be aware of the limitations of urine drug testing.
- Provide treatment for concurrent psychiatric illnesses and substance use disorders.
Methadone and Pregnancy
Opioid withdrawal is associated with a high risk of spontaneous abortion and preterm labor. Pregnant patients with OUD should be started as soon as possible and titrated to avoid withdrawal symptoms (20). The use of opiates during pregnancy produces withdrawal symptoms in neonates, including irritability, excessive crying, tremors, hyperactive reflexes, fever, vomiting, diarrhea, yawning, sneezing, and seizures (20).

Self Quiz
Ask yourself...
- Can you name drugs that should be carefully monitored when prescribed along with methadone?
- What are examples of additional precautions for elderly patients?
- Can you explain the major side effects of methadone?
- Can you describe the recommendations for missed doses of methadone?
- What symptoms might neonates, who were exposed to opiates while in-utero, experience?
- What are some ways to manage the adverse effects of methadone?
Treatment of Opioid Use Disorder: Buprenorphine
Buprenorphine should be used as part of a comprehensive treatment program that includes counseling and psychosocial support.
Buprenorphine is categorized as a Schedule III drug. It is a synthetic opioid developed in the late 1960s and is used to treat OUD. This drug is a synthetic analog of thebaine, which is an alkaloid compound derived from the poppy flower (6).
Buprenorphine is approved by the FDA to treat acute and chronic pain and OUD.
Drug information for buprenorphine include:
Drug Class
- Analgesic, Opioid
- Analgesic, Opioid Partial Agonist
Uses
Buprenorphine is used to treat OUD and pain management in patients for which alternative treatment options (e.g., nonopioid analgesics) are ineffective, not tolerated, or are inadequate to provide sufficient management of pain (16).
Buprenorphine should be used as part of a complete treatment program to include counseling and psychosocial support.
Mechanism of Action
Buprenorphine has an analgesic effect by binding to mu opiate receptors in the CNS; however, it behaves like an antagonist due to it being a partial mu agonist but the analgesic effects plateau at higher doses (16). This is a meaningful attribute, and this plateauing of its analgesic effects at higher doses, causes it to have limited effects on respiratory depression as well (16). This is a positive attribute when considering safety.
Essentially, the benefits of this drug include: (1) higher doses do not lead to greater analgesic effects, thus respiratory depression; and (2) the withdrawal symptoms from buprenorphine are not as intense as full-opioid antagonists.
The extended-release formulation is injected subcutaneously as a liquid (16).
Note on absorption: When administered orally, buprenorphine has poor bioavailability. The preferred route of administration is sublingual, so it can have rapid absorption and circumvents the first-pass effect. Placing the tablet under the tongue results in a slow onset of action, with the peak effect occurring approximately 3 to 4 hours after administration (16).
Pharmacodynamics/Kinetics
Pharmacodynamics/kinetics of buprenorphine includes (16):
- Onset of action: Immediate-release IM: ≥15 minutes
- Peak effect: Immediate-release IM: ~1 hour
- Duration: Immediate-release IM: ≥6 hours; Extended-release SubQ: 28 days
- Absorption: Immediate-release IM and SubQ: 30% to 40%.
- Application of a heating pad may increase blood concentrations of buprenorphine 26% to 55%.
- Distribution: CSF concentrations are 15% to 25% of plasma concentrations
- Protein binding: High (~96%, primarily to alpha- and beta globulin)
- Bioavailability (relative to IV administration): Buccal film: 46% to 65%; Immediate-release IM: 70%; Sublingual tablet: 29%; Transdermal patch: ~15%
- Half-life elimination in adults:
- IV: 2.2 to 3 hours
- Buccal film: 27.6 ± 11.2 hours
- Sublingual tablet: ~37 hours
- Transdermal patch: ~26 hours
- Time to peak, plasma:
- Buccal film: 2.5 to 3 hours
- Extended-release SubQ: 24 hours, with steady state achieved after 4 to 6 months
- Subdermal implant: 12 hours after insertion, with steady state achieved by week 4
- Sublingual: 30 minutes to 1 hour
- Transdermal patch: Steady state achieved by day 3
- Excretion: Most of the drug and its metabolite are eliminated through feces, with less than 20% excreted by the kidneys (6)
- Clearance: Related to hepatic blood flow
- Adults: 0.78 to 1.32 L/hour/kg
Adverse Effects
Buprenorphine has anticholinergic-like effects and may cause CNS depression, dry mouth, dizziness, hypotension, drowsiness, QT prolongation, and lower seizure threshold (6).
Additional adverse effects of buprenorphine include:
- Nausea
- Vomiting
- Headache
- Memory loss
- Orthostatic hypotension
- Urinary retention
Following buprenorphine treatment, a patient's tolerance to opioids decreases, increasing the risk for harm if they resume their previous opioid dosage. Patients should be strongly advised against using opioids without prior consultation with their healthcare provider.
Warnings
Prescribers should exercise caution when prescribing buprenorphine to patients with hepatic impairment, morbid obesity, thyroid dysfunction, a history of ileus or bowel obstruction, prostatic hyperplasia or urinary stricture, CNS depression or coma, delirium tremens, depression, anxiety disorders, posttraumatic stress disorder, and toxic psychosis (16).

Self Quiz
Ask yourself...
- Can you describe the mechanisms of action for buprenorphine?
- What are some comorbidities to be careful with when prescribing this drug?
- How does buprenorphine’s mechanism of action differ from that of opioids?
- Can you describe the analgesic effects of higher doses of buprenorphine?
Treatment of Opioid Use Disorder: Naltrexone
Naltrexone is effective in blocking the effects of opioid drugs. Naltrexone is a pure opioid antagonist, it acts as a competitive antagonist at opioid receptor sites, showing the highest affinity for mu receptors (17). Naltrexone was initially developed in 1963 for the treatment of alcohol use disorders; in 1984, naltrexone received approval for medical use in the United States.
Drug information for naltrexone includes:
Drug Class
- Antidote
- Opioid Antagonist
Uses
- Alcohol use disorder: FDA Approved.
- OUD: For the blockade of the effects of exogenously administered opioids; FDA-approved.
- Researchers are studying its use in patients with stimulant use disorder, particularly patients with polydrug dependence on opioids, heroin, and amphetamine (17)
Mechanism of Action
Naltrexone blocks the effect of opioids and prevents opioid intoxication and dependence in opioid users. Naltrexone also helps with alcohol dependency because it modifies the hypothalamic-pituitary-adrenal axis to suppress ethanol consumption (17). Opioids act mainly via the mu receptor, although they affect mu, delta, and kappa-opioid receptors. Naltrexone competes for the opiate receptors and displaces opioid drugs from these receptors, thus reversing their effects (17).
Exogenous opioids include the commonly prescribed pain relievers such as hydrocodone, oxycodone, and heroin. These typically induce euphoria at much higher doses than those prescribed by medical providers to relieve pain. If naltrexone occupies the receptors, the opioids are not going to provide these euphoric effects.
According to guidelines by the American Society of Addiction Medicine (ASAM), a combination of buprenorphine and low doses of oral naltrexone is effective for OUD for managing withdrawal (17).
Pharmacodynamics
Duration: Oral: 50 mg: 24 hours; 100 mg: 48 hours; 150 mg: 72 hours; IM: 4 weeks
- Absorption: Oral: Almost complete
- Distribution: Vd: ~1350 L; widely throughout the body but considerable interindividual variation exists
- Metabolism: Extensively metabolized via noncytochrome-mediated dehydrogenase conversion to 6-beta-naltrexol (primary metabolite) and related minor metabolites; glucuronide conjugates are also formed from naltrexone and its metabolites
- Oral: Extensive first-pass effect
- Protein binding: 21%
- Bioavailability: Oral: Variable range (5% to 40%)
- Half-life elimination:
- Oral: 4 hours; 6-beta-naltrexol: 13 hours
- IM: naltrexone and 6-beta-naltrexol: 5 to 10 days (dependent upon erosion of polymer)
- Time to peak, serum:
- Oral: ~60 minutes
- IM: Biphasic: ~2 hours (first peak), ~2 to 3 days (second peak)
- Excretion: Primarily urine (as metabolites and small amounts of unchanged drug)
Side Effects
Commonly reported side effects of naltrexone include:
- Gastrointestinal Distress
- Constipation
- Nausea and vomiting
- Diarrhea
- Abdominal pain
- Insomnia
- Joint and muscle pain
- Fatigue
- Decreased strength and energy
- Tooth or gum pain
- Dry mouth
- Increased thirst
Warnings
Patients should be opioid-free for a minimum of 7 to 10 days before taking naltrexone (14).
Prescribers must be aware that patients who have been treated with naltrexone may respond to lower opioid doses than previously used, which could result in potentially life-threatening or fatal opioid intoxication. Patients should be educated that they may be more sensitive to lower doses of opioids after naltrexone treatment is discontinued, after a missed dose, or near the end of the dosing interval (17).
Opioid withdrawal may be noted in patients, and symptoms include pain, hypertension, sweating, agitation, and irritability; in neonates: shrill cries and failure to feed (17).
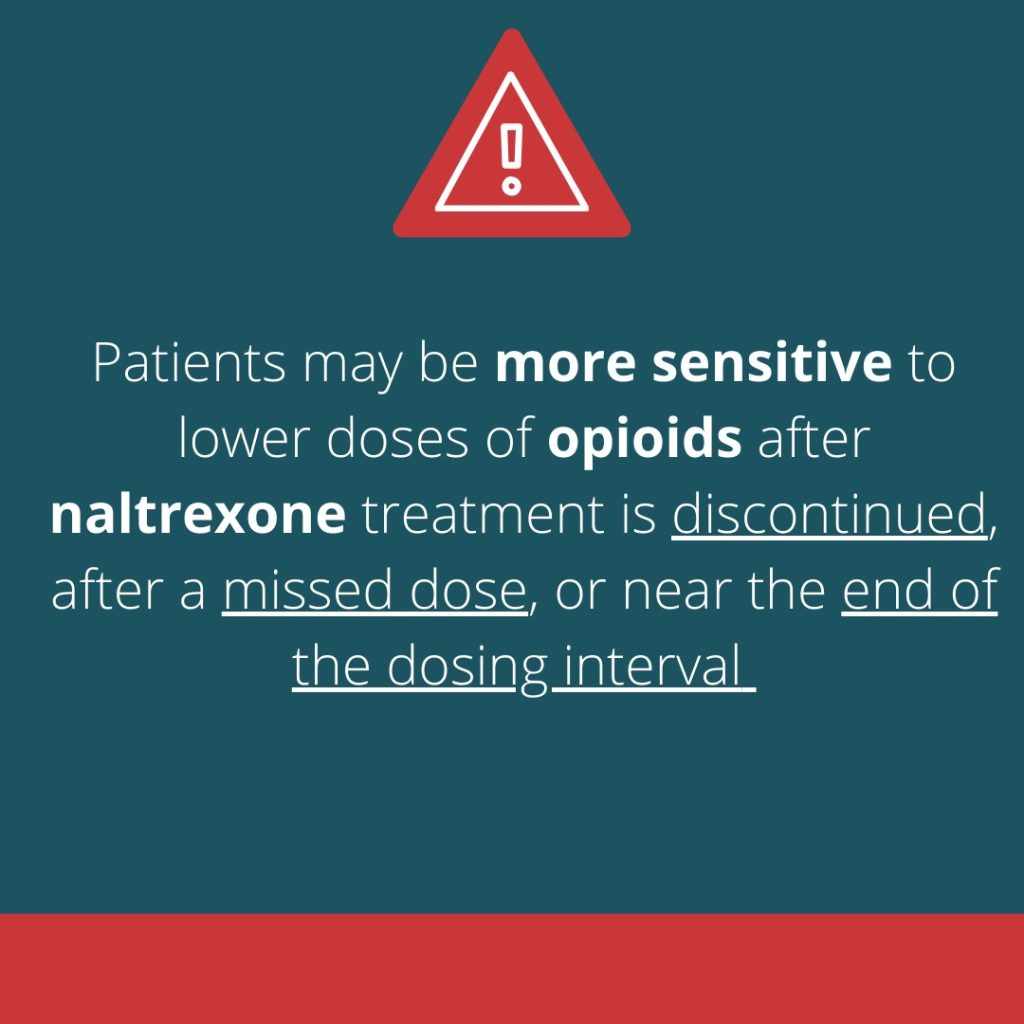

Self Quiz
Ask yourself...
- Can you explain the major uses of naltrexone?
- Can you describe the recommendations for missed doses of naltrexone?
- What are some potential side effects?
- How does the mechanism of action for this drug explain the reversal benefits of opioids?
Long-Term Advocacy in the Opioid Addiction Crisis
Long-term advocacy measures for addressing the opioid addiction crisis involve comprehensive strategies that focus on prevention, treatment, recovery, and policy reforms. These strategies require coordinated efforts across various sectors, including healthcare, policymakers, law enforcement, and community organizations.
Long-term advocacy measures:
- Expansion of Treatment and Recovery Services
- Increased Access to Treatment: Increasing access to evidence-based treatment options, including medication-assisted treatment (MAT), inpatient and outpatient rehabilitation, and mental health services.
- Policy and Legislative Reforms
- Improved Prescription Monitoring Programs (PMPs): Enhancing PMPs to track prescribing and dispensing of controlled substances more effectively, helping to identify and prevent prescription drug misuse.
- Regulation of Opioid Prescriptions
- Support for Harm Reduction Policies (needle exchange programs and widespread availability of naloxone)
- Public Education and Community-Based Programs
- Stigma Reduction: Launching campaigns to reduce the stigma associated with addiction, encouraging individuals to seek help without fear of judgment.
- Awareness Programs: Educate the public, especially youth, about the risks of opioid use and the signs of addiction through school programs, community workshops, and media campaigns.
- Community Coalitions: Forming coalitions of local stakeholders, including healthcare providers, law enforcement, educators, and community leaders, to develop and implement local strategies for addressing the opioid crisis (2).
- Peer Support Programs: Establishing programs that connect individuals with lived experience of addiction to those currently struggling, providing mentorship and support throughout the recovery process.
- Research and Data Collection
- Funding Research: Supporting research to better understand the causes of addiction, effective treatment methods, and the impact of various interventions.
- Data-Driven Approaches: Using data to monitor trends in opioid use and overdose rates, and to evaluate the effectiveness of policies and programs
- Social Support and Holistic Advocacy
- Addressing Social Determinants of Health: Tackling factors such as poverty, lack of education, and unemployment that contribute to substance use and hinder recovery.
- Job Training and Employment Programs
Palliative Care
Often the terms palliative care and hospice, seem interchangeable. However, this is not true. Both palliative and hospice care aim to improve the quality of life for patients with significant conditions and illnesses, but they differ in terms of timing, treatment goals, and patient eligibility.
Palliative care is the holistic and specialized treatment of a patient with chronic illness, seeking to reduce their symptom along with curative measures, and offers support and assistance to the patient and their family (3). Any individual with a serious illness, regardless of life expectancy or prognosis, is eligible for palliative care.
Palliative care services are underused globally, as patients and family members do not recognize the benefits and availability.
Palliative care has the following benefits (9):
- Improves the quality of life for patients.
- Reduces caregiver strain and fatigue.
- Lowers healthcare costs
Differences between palliative and hospice are outlined below:
| Differences in Care | Palliative Care | Hospice Care |
| Purpose and Focus |
Palliative care does not replace the patient’s primary treatment but involves collaboration with the primary treatment. The focus is on the pain, symptoms, and stress of serious illness most often as an adjunct to curative care modalities. Additionally, those who qualify for hospice service, but are not emotionally ready to elect hospice care could benefit from these services.
|
Hospice care focuses on the pain, symptoms, and stress of serious illness during the terminal phase. The terminal phase is defined by Medicare as an individual with a life expectancy of 6-months or less if the disease runs its natural course. This care is provided by an interdisciplinary team who provides care encompassing the individual patient and their family’s holistic needs. |
| Timing |
There is no time limit. Palliative care is available at any stage of an illness, alongside curative treatments.
|
Initiated when curative treatment is no longer pursued, and the patient is expected to live six months or less. |
| Scope |
Addresses physical, emotional, and spiritual needs, focusing on symptom management and support.
|
Focuses on pain and symptom relief, emotional support for the patient and loved ones, and enhancing their quality of life. |
Prescribing regulations for palliative care do not have many variations from the standard regulations. Prescribers must consult the Prescription Monitoring Program (PMP) Registry to review their patient's history of controlled substances before prescribing, and these narcotic prescriptions must be electronically prescribed unless an exception applies.
Appropriate use for prescriptions should be based on a legitimate medical need, and adherence to DEA schedules for controlled substances, with specific rules for different schedules (II-V), should be followed, along with proper documentation of the patient's condition and treatment plan.
While NY law limits the supply of a schedule II, III, or IV opioids that a provider may prescribe upon an initial consultation or treatment for acute pain to seven days, this limitation does not apply to such prescriptions for management of pain associated with palliative care practices, cancer care, hospice, or other end-of-life care.
Within the hospice setting, there are more lenient and specific regulatory exceptions.

Self Quiz
Ask yourself...
- How would you explain palliative care to someone?
- At what point in their disease progression are patients eligible for palliative care?
- How do palliative care and hospice care differ?
- What are the potential roles of a nurse providing palliative care?
Hospice Care
Hospice care is a specialized form of medical care aimed at providing comfort and support to patients in the final stages of life due to a terminal illness. The primary goal is to enhance the quality of life for both the patient and their families by addressing physical, emotional, social, and spiritual needs.
Hospice care focuses on symptom management and relief from pain and distress rather than curative treatment. It involves a multidisciplinary team approach, including physicians, nurse practitioners, nurses, social workers, spiritual counselors, and volunteers, to offer comprehensive care. This care can be provided in various settings, such as the patient's home, hospice centers, or inpatient facilities.
In New York, there are specific exceptions to NY controlled substance prescribing within hospice settings. Prescribers are still required to e-prescribe opioids to hospice patients; however, hospice providers are not required to review a hospice patient’s record in the state prescription monitoring program (PMP) registry before writing or renewing an opioid prescription (11). The NY state law that sets limitations on opioid prescriptions written to patients also does not apply to prescriptions for hospice patients.
Cultural competence is an essential skill for hospice nurses, cultural competence skills enable culturally sensitive care for diverse patients and families. This awareness of cultural values is vital to holistic advocacy and individualized care.
Hospice patients commonly experience distressing physical symptoms, including pain, nausea, and fatigue. Effective management reduces stress for patients and families, focusing on crucial end-of-life aspects.
Resources for Hospice Care Support:
- National Hospice and Palliative Care Organization (NHPCO)
- NHPCO is the largest nonprofit membership organization representing hospice and palliative care programs and professionals in the United States.
- The organization provides resources, education, and advocacy for high-quality end-of-life care; also provides information to patients and families on finding hospice care, understanding what to expect, and managing symptoms.
- Website: NHPCO
- CaringInfo
- CaringInfo provides free resources and information to help people make decisions about end-of-life care and services before a crisis.
- Website: CaringInfo
- American Cancer Society (ACS)
- ACS provides comprehensive education and resources about hospice care, particularly for cancer patients, including how to find hospice services and what to expect.
- Services include support for patients and caregivers, guidance on hospice care, and connections to local resources.
- Website: American Cancer Society
- Centers for Medicare & Medicaid Services (CMS)
- CMS provides guidelines and information on hospice care coverage under Medicare, including eligibility and benefits.
- Website: CMS- Hospice Center
- Hospice Foundation of America (HFA)
- HFA promotes hospice care and provides public and professional education about death, dying, and grief.
- Education includes webinars, publications, and resources for patients, families, and healthcare providers.
- Website: Hospice Foundation of America
- GetPalliativeCare.org
- Managed by the Center to Advance Palliative Care (CAPC), this site provides information on palliative care and hospice care.
- Services: Helps users find palliative and hospice care providers, offers educational materials and answers common questions about care.
- Website: GetPalliativeCare.org
Current Research and Opportunities
The United States is currently in the midst of an opioid epidemic with a significant increase in opioid use and overdose over the last two decades. Research extensively focuses on treatment alternatives, including medications, physical and occupational therapy modalities, exercise, injections, integrative medicine, implantable devices, and neuromodulation.
Advanced nurse practitioners are in significant demand, especially in rural areas, in the battle against controlled substance misuse and addiction.
Resources and Organizations
- New York Department of Health: Mandatory Prescriber Education
- NY DOH: Prescriber Education Webpage
- American Society of Addiction Medicine (ASAM)
- https://www.asam.org/
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- https://www.samhsa.gov/
- FindTreatment.gov: Locates treatment facilities for mental and substance abuse.
- https://findtreatment.gov/
- National Helpline
- 1-800-662-HELP
- 988 Suicide & Crisis Lifeline
- Call or Text 988

Conclusion
New York State's initiative to enhance substance misuse education for prescribers represents a critical step in addressing the opioid crisis and improving patient care. By mandating comprehensive training that covers pain management, palliative care, and addiction, the state aims to equip healthcare providers with the necessary knowledge and skills to prescribe responsibly, recognize signs of substance misuse, and offer appropriate interventions.
The ongoing commitment to prescriber education underscores New York's proactive approach to public health and dedication to combating substance misuse through informed, compassionate, and effective medical care.
References + Disclaimer
- American Society for the Positive Care of Children. (2020). Child abuse statistics in the U.S. Retrieved from: https://americanspcc.org/child-abuse-statistics/
- American Society for the Positive Care of Children. (2020). Indicators of child abuse. Retrieved from: https://americanspcc.org/indicators-child-abuse/
- Centers for Disease Control and Prevention (2023). Fast Facts: Preventing Adverse Childhood Experiences. Retrieved on July 27th, 2023, from https://www.cdc.gov/violenceprevention/aces/fastfact.html
- Child Welfare Information Gateway (2020). Protective Factors Approaches in Child Welfare. Retrieved on September 7th, 2023, from https://www.childwelfare.gov/topics/preventing/promoting/protectfactors/
- Child Welfare League of America. (2017). New York’s children at a glance. Retrieved from: https://www.cwla.org/wp-content/uploads/2017/04/NEW-YORK-.pdf
- Family Court Act. (n. d.) Article 10: child protective proceedings. Retrieved from: https://www.nysenate.gov/legislation/laws/FCT/A10
- FitzGerald, C., and Hurst, S. (2017). Implicit bias in healthcare professionals: a systematic review. BMC Med Ethics, 18, 19. https://doi.org/10.1186/s12910-017-0179-8
- National Children’s Alliance. (2020). National child abuse statistics. Retrieved from https://www.nationalchildrensalliance.org/media-room/national-statistics-on-child-abuse/
- New York Consolidated Law- Social Services. (2019). SOS 411-428 Child protective services. Retrieved from: https://law.justia.com/codes/new-york/2012/sos/article-6/title-6/415/
- New York Kid’s Well-being Indicators Clearinghouse. (2020). Child abuse and maltreatment. Retrieved from: https://www.nyskwic.org/get_data/indicator_profile.cfm?subIndicatorID=107
- New York State Office of Children and Family Services. (n.d.). Child protective services. Retrieved from: https://ocfs.ny.gov/programs/cps/#:~:text=The%20purpose%20of%20the%20Child,each%20county%20in%20New%20York.
- NY Office of Children and Family Services (2022). New York State Child Protective Services Manual. Retrieved on September 6th, 2023, from https://ocfs.ny.gov/programs/cps/manual/
- Palusci, V., Botash, A. (2021). Race and Bias in Child Maltreatment Diagnosis and Reporting. Pediatrics July 2021; 148 (1): e2020049625. 10.1542/peds.2020-049625 Retrieved from https://publications.aap.org/pediatrics/article/148/1/e2020049625/179923/Race-and-Bias-in-Child-Maltreatment-Diagnosis-and?autologincheck=redirected
- University of South Carolina (2020). Virtual Settings: Recognizing and Reporting Child Abuse & Neglect. Retrieved on September 7th 2023 from https://dc.statelibrary.sc.gov/bitstream/handle/10827/35104/CLC_Virtual_Settings_Recognizing_And_Reporting_Child_Abuse_2020-07.pdf?sequence=1&isAllowed=y
ELEMENT I
- https://www.op.nysed.gov/title8/rules-board-regents/part-29
- https://regs.health.ny.gov/content/section-92-11-course-work-or-training
- https://www.cdc.gov/oralhealth/infectioncontrol/summary-infection-prevention-practices/standard-precautions.html
- https://www.nursingworld.org/practice-policy/work-environment/health-safety/infection-prevention/
- https://www.cdc.gov/infectioncontrol/guidelines/core-practices/index.html
- https://www.cdc.gov/hai/data/portal/progress-report.html
- https://www.ncsbn.org/filing-a-complaint.htm
ELEMENT II
- Douedi, S., & Douedi, H. (2020) Precautions, bloodborne, contact, and droplet. In StatPearls. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK551555/
- https://www.cdc.gov/niosh/topics/healthcare/infectious.html
- Abbas AK, Lichtman AH, Pillai S. Properties and overview of immune responses. In: Abbas AK, Lichtman AH, Pillai S, eds. Cellular and Molecular Immunology. 9th ed. Philadelphia, PA: Elsevier; 2018:chap 1.
- https://www.cdc.gov/training/publichealth101/e-learning/prevention-effectiveness/
- https://www.cdc.gov/infectioncontrol/basics/standard-precautions.html
- https://www.cdc.gov/injectionsafety/spinalinjection-meningitis.html
- Carrico, R., Garrett, H., Balcom, D, & Burton Glowicz, J. (2018). Infection prevention and control core practice: a roadmap for nursing practice. Nursing, 48(8), 28-29. doi: 10.1097.NURSE.0000544318.36012.b2
- Sands, M.,& Aunger, R. (2020). Determinants of hand hygiene compliance among nurses in US hospitals: a formative research study. PLoS ONE, 15(4), 2-29. doi: 10.1371/journal. pone.0230573
- Pyrek, K. (2017). Cleanliness of hands and surfaces play key role in cross-contamination prevention. Infection Control Today, 21(5).Retrieved from https://www.infectioncontroltoday.com/view/cleanliness-hands-and-surfaces-plays-key-role-cross-contamination-prevention
- Assadian, O., Kramer, A., Cristiansen, B., Exner, M., Martiny, H., Sorger, A., & Suchomel, M. (2012). Recommendations and requirements for soap and hand rub dispensers in healthcare facilities. GMS Krankenhhyg Interdisziplinar, 7(1), 4-5. doi: 10.3205/dgkh000187
- https://www.cdc.gov/infectioncontrol/projectfirstline/resources/ppe-covid-19.html
- Watson, N. (2007). Isolation and cohort care. The Journal of the Intensive Care Society, 8(3). Retreived from https://journals.sagepub.com/doi/pdf/10.1177/175114370700800308
- https://www.cdc.gov/infectioncontrol/guidelines/isolation/
- https://www.hhs.gov/vaccines/vaccines-national-strategic-plan/vision-and-goals/index.html
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/environmental-guidelines-P.pdf
- https://www.dec.ny.gov/chemical/8789.html
- https://regs.health.ny.gov/content/section-83-117-linen-and-laundry
ELEMENT III
- https://www.osha.gov/etools/hospitals/hospital-wide-hazards/biological-hazards
- Kossover-Smith, R. Coutts, K., Hatfield, K., Cochran, R., Akselrod, H., Schaefer, . . . & Bruss, K. (2017). One needle, one syringe, only one time? A survey of physician and nurse knowledge, attitudes, and practices around injection safety. American Journal of Infection Control, 45(9), 1018-1023. doi: 10.1016/j.ajic.2017.04.292
- https://www.cdc.gov/sharpssafety/pdf/sharpsworkbook_2008.pdf
ELEMENT IV
- https://www.cdc.gov/infectioncontrol/pdf/strive/PPE103-508.pdf
- https://www.ventyv.com/blog/whats-the-difference-between-nitrile-latex-and-vinyl-gloves
- https://www.cdc.gov/niosh/npptl/topics/protectiveclothing/default.html
- https://www.cdc.gov/niosh/topics/respirators/
- https://www.cdc.gov/niosh/topics/bbp/
ELEMENT V
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines-H.pdf
- https://www.cdc.gov/infectioncontrol/guidelines/disinfection/efficacy.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3678066/
- https://www.cdc.gov/infectioncontrol/guidelines/disinfection/cleaning.html
- https://www.osha.gov/Publications/OSHA3512.pdf
ELEMENT VI
- https://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/evaluation.html
- https://www.cdc.gov/tb/topic/testing/tbtesttypes.htm
- https://www.cdc.gov/infectioncontrol/pdf/guidelines/infection-control-HCP-H.pdf
- https://www.nyc.gov/assets/doh/downloads/pdf/hcp/reporting-guide.pdf
- https://www.cdc.gov/tb/topic/treatment/decideltbi.htm
- https://www.health.ny.gov/publications/1852/appenb.htm
- https://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/exposures.html
ELEMENT VII
- https://www.health.ny.gov/diseases/conditions/sepsis/
- https://www.health.ny.gov/facilities/public_health_and_health_planning_council/meetings/2013-02-07/docs/13-01.pdf
- https://www.health.ny.gov/diseases/conditions/sepsis/docs/2019_sepsis_care_improvement_initiative.pdf
- https://www.sepsis.org/sepsis-basics/what-is-sepsis/
- https://www.nhsinform.scot/illnesses-and-conditions/blood-and-lymph/septic-shock
- Kim, H, & Park, S. (2019). Sepsis: Early recognition and optimized treatment. Tuberculosis and Respiratory Disease, 82(1), 6-14. doi: 10.4046/trd.2018.0041
- https://www.sccm.org/SurvivingSepsisCampaign/Guidelines/Adult-Patients
- https://www.mayoclinic.org/diseases-conditions/sepsis/diagnosis-treatment/drc-20351219
- https://www.cdc.gov/sepsis/pdfs/Consumer_fact-sheet_protect-yourself-and-your-family-P.pdf
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5.™ 5th ed. Arlington, VA: American Psychiatric Publishing, Inc.
- Alderson, K., & Gladding, S. T. (2021). A concise guide to opioid addiction for counselors. American Counseling Association.
- Centers for Disease Control and Prevention (CDC). (2023). Provisional drug overdose death counts. Retrieved from https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- Dydyk AM, Sizemore DC, Smock W, et al. Kentucky KASPER and Controlled Substance Prescribing. [Updated 2023 Jun 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567726/
- Ghlichloo I, Gerriets V. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547742/
- Horn, M. E., George, S. Z., Li, C., Luo, S., & Lentz, T. A. (2021). Derivation of a Risk Assessment Tool for Prediction of Long-Term Pain Intensity Reduction After Physical Therapy. Journal of pain research, 14, 1515–1524. https://doi.org/10.2147/JPR.S305973
- Lopez MJ, Preuss CV, Tadi P. Drug Enforcement Administration Drug Scheduling. [Updated 2023 Jul 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557426/
- National, Academies of Sciences, Engineering, and Medicine, et al. , edited by Michelle Mancher, and Alan I. Leshner. (2019). Medications for opioid use disorder save lives National Academies Press, 2019. ProQuest Ebook Central, https://ebookcentral.proquest.com/lib/liberty/detail.action?docID=5774508.
- National Center for Complementary and Integrative Health. (2022). Acupuncture: what you need to know. Retrieved from https://www.nccih.nih.gov/health/acupuncture-what-you-need-to-know#:~:text=Research%20has%20shown%20that%20acupuncture,in%20people%20with%20breast%20cancer.
- National Hospice and Palliative Care Organization (2019). Palliative Care or Hospice? https://www.nhpco.org/wp-content/uploads/2019/04/PalliativeCare_VS_Hospice.pdf
- New York State Department of Health. (2023). Mandatory Prescriber Education Guidelines. Retrieved from https://www.health.ny.gov/professionals/narcotic/mandatory_prescriber_education/docs/guidance.pdf
- New York State Department of Health. (2023). Electronic Prescribing of Controlled Substances (EPCS) FAQs. Retrieved from https://www.health.ny.gov/professionals/narcotic/electronic_prescribing/docs/epcs_faqs.pdf
- NYC Office of Chief Medical Examiner and NYC DOHMH Bureau of Vital Statistics, 2000–2022. (2023). Unintentional Drug Poisoning (Overdose) Deaths in New York City in 2022. https://www.nyc.gov/assets/doh/downloads/pdf/epi/databrief137.pdf
- U.S. Department of Veteran Affairs. (2023). Pain Management – Cognitive Behavioral Therapy for Chronic Pain (CBT-CP). Retrieved from https://www.va.gov/PAINMANAGEMENT/CBT_CP/Veterans.asp#:~:text=CBT%2DCP%20equips%20individuals%20with,pain%20experience%2C%20physically%20and%20emotionally.
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Fentanyl. Retrieved from Access Pharmacy. https://accesspharmacy.mhmedical.com/drugs.aspx#monoNumber=426639§ionID=243243556&tab=tab0
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Buprenorphine. Retrieved from Access Pharmacy. https://accesspharmacy.mhmedical.com/drugs.aspx?GbosID=426498#monoNumber=426498§ionID=241825553&tab=tab0
- Wolters Kluwer Clinical Drug Information, Inc. (2024). Naltrexone. Retrieved from Access Pharmacy. https://accesspharmacy.mhmedical.com/drugs.aspx?gbosID=426798#monoNumber=426798§ionID=239566147&tab=tab0
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2023). Methadone. Retrieved from https://www.samhsa.gov/medications-substance-use-disorders/medications-counseling-related-conditions/methadone
- Toney-Butler TJ, Siela D. Recognizing Alcohol and Drug Impairment in the Workplace in Florida. [Updated 2024 Mar 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507774/
- Bromley L, Kahan M, Regenstreif L, Srivastava A, Wyman J. Methadone treatment for people who use fentanyl: Recommendations. Toronto, ON: META:PHI; 2021. www.metaphi.ca.
- Wong-Baker FACES Foundation. (2022). Wong-Baker FACES® Pain Rating Scale. http://www.WongBakerFACES.org
- Ernstmeyer, K. & Christman, E. (2021). Pain assessment methods. In: Nursing Fundamentals [Internet]. Ernstmeyer K, Christman E, eds. Eau Claire (WI): Chippewa Valley Technical College; 2021. https://openwa.pressbooks.pub/nursingfundamentals/chapter/11-3-pain-assessment-methods/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate