Nurse Preceptor Training
Contact Hours: 3
Author(s):
Charmaine Robinson MSN-Ed, BSN, RN, PHN, CMSRN
Course Highlights
- In this Nurse Preceptor Training course, we will learn about the characteristics of an effective preceptor.
- You’ll also learn how to apply learning theories to preceptorship training.
- You’ll leave this course with a broader understanding of the roles of the nurse preceptor.
Introduction
What makes a great nurse preceptor? Nurse preceptors offer much more than extensive professional experience. They are a valuable asset to both patient-facing nursing and nursing education. Preceptors assist nursing students and new nurses in transitioning to the real world of nursing by serving as trainers, evaluators, and mentors. Many nurse preceptors are chosen based on their expertise in the field and leadership skills. However, some are ushered into the role due to staffing shortages.
An ideal nurse preceptor is a nurse who has experience, leadership abilities, and a desire to teach or mentor. Amid the ever-present nursing shortage, a high demand remains for qualified nurse preceptors. Studies show that nurse preceptor development improves patient outcomes and staff retention (14). Yet many preceptors are provided with little to no training. This course will offer a look into the exciting world of nurse preceptorship and provide tips for nurses who have a desire to transition into this highly esteemed role.
Basics of Nursing Education
Although nurse preceptors may work as staff nurses at hospitals and other clinical facilities, they are often associated with nursing education. It is essential to develop a clear understanding of how the field of nursing education works. Nursing education focuses on the training and evaluation of nursing students and professionals. Nurse educators do more than they teach. They test and evaluate if nursing students (or new nurses) understand the material and can practice safely. Many nurse educators serve as mentors and role models; some even develop course curricula and other student learning materials. Nurse educators work in clinical and academic settings and fulfill various roles, including facility educators, lecturers, professors, simulation instructors, and clinical instructors.
Clinical Nurse Educator
In clinical settings (hospitals, clinics, nursing homes, etc.), the clinical nurse educator, also termed the “nursing professional development specialist,” is responsible for educating new and experienced nurses. They keep nurses up to date on current evidence-based practice protocols and guidelines and evaluate role performance, ensuring that nurses practice safely and according to evidence. Clinical nurse educators may also be responsible for managing new graduate nurse orientation training programs. Some educators may be responsible for managing several units/departments.
Academic Nurse Educator
In academic settings (colleges, universities, trade schools, etc.), the academic nurse educator is responsible for educating and evaluating nursing students at various levels of study. Evaluation methods include written tests, skills testing, and observation of clinical performance. Academic nurse educators work with nursing students in practical/vocational nursing programs, undergraduate registered nursing programs, and graduate nursing programs. The academic nurse educator may fulfill several roles concerning students, including class lecturer, simulation instructor, and clinical instructor [See Figure 1].
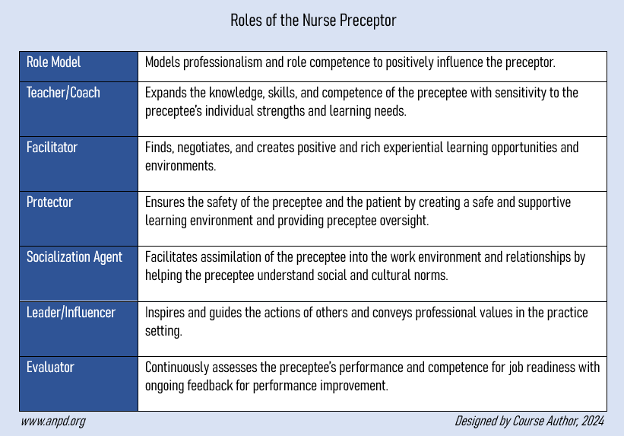
Figure 1: Nurse Educator Roles in Academic Settings
Although nurse preceptors typically do not work for nursing schools, they help by training students during clinical rotations and/or preceptorships at clinical sites. This allows the students to gain supervised clinical hours for educational and professional advancement.
Ask yourself...
- Have you ever fulfilled the role of a nurse educator, community educator (teaching CPR or other health classes), or teaching assistant?
- Can you think of any other nurse educator positions in either clinical or academic settings?
- What characteristics do you think are most important to possess when training nursing students in particular?
- In your opinion, what is the primary way in which nurse preceptorship relates to nursing education?
Nurse Preceptor: Definition and Characteristics
Nurse preceptors, also called clinical preceptors, are practicing nurses who have the knowledge and experience needed to train nursing professionals. Preceptors train nursing students at clinical sites during their clinical rotations and new nurses at clinical facilities during new graduate nurse orientation programs. They provide one-on-one relationships with preceptees (individuals who receive the training), guiding and validating the knowledge, skills, and attitudes necessary for a smooth transition to a new nursing role (7).
An effective nurse preceptor has certain characteristics that make them best suited for the role. These include (7,14):
- Nonjudgmental
- Positive demeanor
- Encouraging
- Respectful
- Active listener
- Authentic
- Supportive
- Caring
- Patient
Aside from training nursing students and new nurses, nurse preceptors provide orientation training to nurses transitioning to a new facility, department, or specialty, as well as those re-entering the field after being out of practice for an extended period. Nurse preceptors are critical to the success of a nursing facility/organization. The most effective preceptors help organizations move toward a goal or vision (14). Goals can include nurse recruitment and retention, and nurse job satisfaction
Ask yourself...
- What interests you about fulfilling the role of a nurse preceptor?
- If you have ever fulfilled the role of a nurse preceptor before, what were some challenges you faced?
- In your opinion, what is the most important characteristic a nurse preceptor should possess?
- When you were a nursing student (or new nurse), how was your experience with your assigned nurse preceptor?
Nurse Preceptor Task 1: Build the Relationship
The first step to becoming an effective preceptor is to build a strong, trusting relationship with the nursing student (or new nurse). The preceptee should feel comfortable when interacting with the preceptor, and fostering an environment of trust and safety plays a primary role in eliciting comfort in the relationship.
For example, nurse preceptors can get to know the preceptee by asking questions about their past educational experiences and future goals. Questions to ask may include:
- Was nursing school challenging for you?
- What about nursing school do/did you like?
- What do/did you like most about your nursing professors?
- Why did you choose nursing?
- How do/did you balance school and personal life?
- What nursing specialty interests you the most?
- What makes you the most nervous about your first workday on your own?
- Would you like to hear about my first workday as a nurse?
Communication between the nurse preceptor and preceptee should be open, honest, and reciprocal, including formal and informal discussions [14]. Supportive environments allow the preceptee to feel comfortable asking questions [10]. The preceptee should also think that they can share their fears and weaknesses with the preceptor without feeling judged.
For example, a new nurse may fear being challenged or questioned publicly. This may cause the new nurse to shy away from confrontations that might otherwise be unavoidable in the workplace, such as when advocating for patients. The nurse preceptor should be aware of these limitations and, therefore, should provide a safe environment for disclosure.
When nurse preceptors share their past and present fears and weaknesses, preceptees may feel more comfortable opening up, which helps to build trust in the relationship [14]. Nurse preceptors who are emotionally intelligent and respectful in their communication, attitudes, and behaviors are most likely to build trusting relationships with preceptees [14].
Additionally, nurses with an in-depth understanding of people will likely make great preceptors as people skills are a must [14]. Any nurse who desires to be a preceptor might benefit significantly from engaging in self-development.
Nurse Preceptor versus Clinical Instructor
The role of the nurse preceptor is ever-changing. At times, nursing schools rely on nurse preceptors to fill in when there is a need for clinical nursing faculty (11). In addition, preceptors fill in the knowledge gap when students graduate without adequate clinical training. This was the case during the COVID-19 pandemic when many students were forced to forego valuable training at clinical facilities, leaving many entering the profession with limited clinical exposure (13).
While nurse preceptors may have the clinical experience necessary to provide training, many have not learned the methods of clinical teaching that would otherwise be required to fulfill the role of a teacher (11,12). Teaching nursing students or new graduate nurses how to perform certain tasks and skills is only a part of clinical education. Although preceptors may be provided evaluation forms to fill out for each preceptee they train, many may not understand the basics of evaluation, including monitoring progress and giving feedback.
The clinical instructor typically has the knowledge base to effectively assess learning styles, apply teaching strategies, and evaluate whether students understand the material. This is what differentiates the nurse preceptor from the clinical instructor. In addition, nurse preceptors typically train one student at a time while clinical instructors train several students simultaneously. Nurse preceptors can be prepared for their roles when provided training on basic concepts of clinical education. With this knowledge, nurse preceptors can better understand the teaching goal and collaborate more effectively with the student’s clinical instructor (if training a student) or the clinical nurse educator (if training a newly graduated nurse).

Ask yourself...
- Did you notice a difference in how your clinical instructors taught you in nursing school and how your nurse preceptor trained you once you became a nurse?
- In your opinion, what is the most important skill a clinical instructor should have?
- How often do you witness clinical instructors teaching students at your facility?
- Do nurse preceptors at your facility also teach at nursing schools?
Skepticism of the Nurse Preceptor Role
Aside from the difficult task of teaching while managing a full patient load, nurse preceptors are responsible for all patients under their care, including those to whom the preceptee is assigned. The responsibility can be heavy for some nurses. Additionally, many nurse preceptors do not receive recognition for their roles. For nurse preceptors who have an interest in filling in as clinical faculty, skepticism about the role may be heightened as incentives are minimal. Many colleges and universities do not pay for clinical preceptors to help train their nursing students.
According to a 2020 Clinical Preceptor Survey report by the American Association of Colleges of Nursing (AACN) and the American Organization for Nursing Leadership (AONL), of 306 nursing schools surveyed, 90% do not pay for clinical preceptors for their students (3). To make matters worse, more than half of the schools with baccalaureate programs (and two-thirds of those with graduate programs) do not provide additional incentives for nursing preceptors. These include access to an online library, free continuing education opportunities, tuition waivers, recognition certificates and ceremonies, appreciation gifts, and tax credits.
Impact on the Nursing Shortage
A lack of nurse preceptors has been cited as a reason for the growing nursing shortage. Nursing school enrollment is unable to keep up with the demand for nurses in the field (2). While expanding enrollment would seem to be a plausible solution, there is a shortage of nurse preceptors available to train nursing students.
In 2021, U.S. nursing schools turned away over 90,000 qualified applicants from both baccalaureate and graduate nursing programs for reasons including lack of faculty, clinical sites, classroom space, finances, and clinical preceptors (1). This number includes nearly 10,000 qualified applicants for master’s programs and approximately 5,000 for doctoral programs.
Nurse preceptors are needed to train both entry-level and graduate-level nursing students. These include students enrolled in any nursing program that requires supervised clinical practice hours. Programs include licensed practical/vocational nursing (LPN/LVN), registered nursing (RN), and advanced practice registered nursing (APRN) (nurse practitioner, clinical nurse specialist, certified midwife, etc.).
A lack of preceptors may also contribute to new nurses leaving the profession early on. Nearly 18% of new graduate nurses leave the profession within the first year for reasons including stressful working conditions and lack of leadership and supervision (4). Nurse preceptors have the potential to positively influence the job satisfaction of the new nurse (10).
The nursing profession is in dire need of experienced nurses who are willing to serve as preceptors in several settings and at various practice levels.
Ask yourself...
- During your first year of nursing practice, did you want to leave the profession? If so, what were the reasons?
- What do you think is the primary reason some nurses do not want to fulfill the role of nurse preceptor?
- Does your facility offer any monetary or non-monetary incentives for fulfilling the role of nurse preceptor?
- What do you think facilities and nursing schools should do to help recruit more nurses to become preceptors?
- How often do you see nurse preceptors at your facility engaging with nursing students and new nurses?
- In your opinion, what is the most challenging part of trying to build relationships with nursing students and new nurses at your facility?
- What are some additional questions you could ask the nursing student or new nurse to help build a trusting relationship?
- What are some areas for improvement in your own professional life that may be a barrier to establishing a trusting relationship with a nursing student or new nurse?
Nurse Preceptor Task 2: Assess the Learner
To effectively teach, the nurse preceptor must understand each learner’s learning style. The most effective nurse preceptors understand the importance of assessing the learner and providing learner-specific teaching (14). Assessing the learner means studying the preceptee to see how they learn best. Nurse preceptors can also help preceptees understand their learning styles. For example, some nursing instructors start class by requiring new students to take a learner assessment quiz.
An excellent way for the nurse preceptor to assess learning styles is to ask the preceptee how they learn best during school. Do/did they prefer the classroom, skills/simulation laboratory, or clinical activities? Do/did they like listening to the material in class and then studying the textbook afterward, or vice versa?
The following are two theories/models that may be helpful in assessing nursing students and new nurses.
VARK Learning Style Model
The VARK learning style model is a way for nurse preceptors to discover a preceptee’s learning style. This tool can also help the preceptee learn their own learning style if they are unaware. VARK stands for Visual, Aural, Reading/writing, and Kinesthetic. Roger Fleming originally designed the model in 1987 to differentiate between the various types of learners.
The following four VARK learning styles are described concerning students enrolled in health science programs (medical, dental, pharmacy, and nursing students) (6):
- Visual: graphics, maps, diagrams, charts
- Auditory: lectures, group discussion, “talking things through”
- Read/write: manuals, essays, reports
- Kinesthetic: simulations, demonstrations, practical applications
Nurse preceptors should perform regular learning style assessments, as styles can overlap and even change over time. One 2020 study found that master’ s-level nursing students had multimodal (multiple learning styles) and kinesthetic learning styles (6). The researchers also found that 30% of the nursing students began the study with one preferred learning style but became multimodal later.
A doctor using a digital tablet in a hospital corridor
Kolb’s Experimental Learning Theory
Designed by theorist David A. Kolb in 1984, the Experimental Learning Theory suggests that knowledge occurs through experience and is based on how the learner perceives, organizes, processes, and understands information. The theory highlights four stages and four learning styles. Nursing preceptors can use Kolb’s Theory to understand how preceptors learn and, therefore, determine the best teaching strategy to employ.
Kolb’s four stages of learning include (7):
- Concrete Experience (CE): learns by feeling and/or being involved
- Reflective Observation (RO): learns by observing, reflecting, and/or listening
- Abstract Conceptualization (AC): learns through logic, reasoning, and/or creating ideas
- Active Experimentation (AE): learns through action and/or decision-making
After determining what stages fit the preceptee, the nurse preceptor assesses which learning style best applies. Each learning style is formed through the combination of two stages. According to the theory, practical learning occurs when learners move through the four learning styles cyclically, typically giving preference to one style.
The four learning styles include:
- Diverging (CE and RO): learns by listening, watching, and being involved
- Assimilating (RO and AC): learns by listening and watching, and “putting the pieces together”
- Converging (AC and AE): learns by “thinking things through” and making decisions
- Accommodating (AE and CE): learns by being actively involved and making decisions
Ask yourself...
- Have you ever assessed your own learning style using a theory or model, and if so, what prompted you to do so?
- What was your preferred learning style in nursing school and what is your preferred learning style now?
- Have you ever asked a nursing student or new nurse about their preferred learning style? If so, what were some answers?
- In your opinion, why might a nurse preceptor avoid assessing a new nurse’s learning style?
Nurse Preceptor Task 3: Tailor Teaching
After discovering a preceptee’s preferred learning style, nurse preceptors should use teaching strategies that would be most appropriate for the learner (14). Just as care plans should be tailored to each patient, teaching should be tailored to each preceptee. This does not mean to avoid different teaching strategies.
Preceptees still need a variety of teaching strategies to ensure that learning is effective (10). However, tailoring teaching to the preferred style is beneficial as the preceptee will likely be more engaged, which can lead to an easier learning experience.
For example, if a student learns best through demonstration, try to provide opportunities for the student to practice hands-on skills more often. If a student learns best by hearing a lecture, sit down frequently with the student after patient interactions to verbally go over what was learned during care. If the student learns best when working in groups, consider inviting one or two nurse coworkers to briefly discuss the plan of care for the student’s assigned patient. This way, the student can hear the perspective of multiple nurses and ask questions as needed.
Refer to the following table (Table 1) for ways to prepare the preceptee for tailored learning experiences based on their learning style.
| If the preceptee learns best when… | The nurse preceptor should… |
| Listening to lectures (face-to-face, audio, video) |
|
| Reading written materials (textbooks, written presentations) |
|
| Working in groups |
|
| Observing demonstrated skills (on video, or performed by the instructor) |
|
| Practicing hands-on skills |
|
| Studying Alone |
|
Table 3: Teaching According to Learning Styles
Ask yourself...
- What is another way a nurse preceptor can facilitate learning in a nursing student who learns best while working in groups?
- If you have ever had a nursing student or new nurse observe you performing a bedside skill, how was the experience?
- Have you ever asked a coworker to allow a new nurse you were training to perform a bedside skill on their patient?
- What are some other recommendations a nurse preceptor can make to a nursing student who learns best when studying alone?
Nurse Preceptor Task 4: Evaluate Learning
The primary difference between orienting an experienced nurse to a new facility and precepting a new graduate nurse is the process of formal evaluation of clinical competency. Clinical evaluation combines observing clinical performance (skills and professionalism), tracking the preceptee’s learning progress, and providing feedback to the preceptee (14).
Observing Skill Performance
Observing the preceptee during skill performance to assess accuracy and safety is likely the most notable part of the evaluation. Once the preceptee has been trained appropriately, the nurse preceptor should observe the preceptee perform the skill independently, only interrupting if patient safety may be compromised. Nursing students and new nurses must learn how to problem-solve without unnecessary interference from the preceptor. Unknowingly, the nurse preceptor may hinder the development of problem-solving skills in the preceptee when frequently stepping in to “take over” due to time constraints or frustration.
The goal of preceptorship is for the preceptee to provide safe care independently (10). Therefore, the nurse preceptor should employ the “sink or swim” method (when the nurse preceptor does not help the preceptee during the skill) (10).
This should only occur after the preceptee has been trained in the skill. While it may be challenging to remain inactive while observing, patience is one of the characteristics of an effective nurse preceptor. Only when the preceptee can perform the skill independently can the nurse preceptor truly know if the training/teaching was successful.
Observing for Professionalism
Aside from evaluating skill performance, nurse preceptors should observe the professionalism the preceptee demonstrates throughout the training experience, for example, remaining punctual, respecting others, and maintaining the confidentiality of patient information. Nurse preceptors should observe the preceptee in daily interactions with patients/families, nursing peers, managers, and other interdisciplinary team members, paying attention to the preceptee’s communication and people skills. Nurse preceptors should also be able to identify the cause of a preceptee’s behavior and avoid misinterpreting typical behaviors as a lack of professionalism.
Some preceptees (particularly nursing students) may be timid and nervous during training, leading to errors. For example, a nursing student may fear speaking with a particular physician over the phone, leading to a lack of confidence during the call. This may lead to a transfer of misinformation. In this case, a lack of professionalism is not the problem.
The nurse preceptor should recognize that this behavior is not unusual and support the student, offering tips to help. Tips can include writing down notes before making the call and keeping the patient’s medical record easily accessible in case the physician has a question. The preceptor can take it a step further and sit down with the student to discuss why they may feel intimidated by the physician. Other reasons why preceptees may struggle during training include knowledge gaps, personal problems, and poor communication skills (10).
Tracking Progress
Some clinical facilities track progress through weekly forms that the preceptor fills out. The forms contain objectives/competencies that the preceptee must meet before progressing through the various stages of the preceptorship program. Without properly tracking progress, there is a potential that a preceptee will reach the end of the preceptorship without the skills necessary to practice safely or effectively, similar to a student completing an entire four-year nursing program without completing one exam. Keeping track of the preceptee’s progress is a formal way for the nurse preceptor to know that the preceptee truly understands what is being taught at every stage of the clinical training.
Giving Feedback
Providing both positive and constructive feedback is the final piece of evaluation. The nurse preceptor should provide written and verbal feedback, addressing strengths, areas for improvement, and improvement tips. Addressing areas for improvement can be stressful for preceptors [10]. Some students may take offense at the negative feedback. However, when preceptees believe that constructive feedback is genuinely intended and not meant to be punitive, it is better received (14).
Feedback should be timely and confidential (10). Nurse preceptors should remain non-demeaning, use tact and consideration, and allow the preceptee time to ask questions and summarize what was said (14). The nurse preceptor should inform the preceptee of any progress made, as learning is enhanced when learners believe they are making progress (10). The nurse preceptor can also ask the student to assess their progress in the training program.
Questions to ask the preceptee may include:
- How do you feel about how you performed today/this week?
- Was there anything you felt like you missed today/this week?
- What was the most helpful tip you learned today/this week?
- Do you feel like you are progressing at a comfortable speed?
- Do you feel ready for the next training day?
- How can I help you improve for next time?
Ask yourself...
- Have you ever observed a nursing student or new nurse perform a skill incorrectly? If so, what steps did you take?
- What is your experience with handling unprofessional nursing student behaviors at your facility?
- In ways does your facility track the clinical progress of new graduate nurses?
- Have you ever experienced a nursing student or new nurse challenge you regarding feedback you gave them?
Nurse Preceptor Task 5: Encourage Independence
Along with managing patient care, new nurses (and nursing students) have to learn how to organize their day-to-day activities (12). One way nurse preceptors can encourage independence in new nurses, in particular, is to allow them to develop their own ways of organizing their activities, essentially creating their practice routines.
While introducing preceptees to the real world of nursing is essential, each nurse develops their routine over time. Nurse preceptors should understand that introducing preceptees to real-life clinical situations has more to do with guiding how to address problems that may arise in the workplace and less to do with forcing their personal practice routines on the preceptee. Many nurse preceptors may struggle to balance teaching personal routines and allowing the preceptee to develop their routines.
Although there may be some routines and tips (that do not compromise patient safety) that can help the preceptee save time, nurse preceptors should make it a priority to teach the standard way of practice (“according to the book”). The rule of thumb is to teach and evaluate the preceptee according to the universal way of practicing (as if a state surveyor is observing them) or based on facility culture/practices. Nursing students and new nurses can develop unique time-saving routines over time as they strengthen their practice. Personal time-saving tips should be shared as an optional routine style that the preceptee can adopt at will or as they become more confident in their role as a competent nurse.
The nurse preceptor can demonstrate their routines to the preceptee to show how they may be beneficial in practice. Additionally, it may be helpful for preceptors to share other routine styles. For example, one nurse may perform morning assessments on all their patients, and then administer morning medications afterward. Another nurse may prefer to evaluate one of their patients and then administer morning medications to that patient before moving on to the next patient. Nurse preceptors should consider facility protocols/practices when sharing routines.

Ask yourself...
- When you first became a nurse, did your preceptor train you according to their own practice routine? If so, what parts did you adopt as your own?
- How long did it take you to develop your own personal practice routine?
- Does your practice routine change when in the presence of a state surveyor or nursing manager/director?
- If you have previously trained a new nurse, what has been the most challenging part of training “by the book”?
Nurse Preceptor Roles and Competencies
Clinical competencies (abilities) are ways by which nursing practice is measured. Nursing students must meet competencies to progress academically. Nurses must meet competencies to continue safely practicing in the field. Nursing educators must meet competencies to teach effectively. Finally, nurse preceptors must also meet competencies to effectively train and mentor nursing students and new nurses. Meeting competencies proves that nurses are “competent” in their role.
The Association for Nursing Professional Development (ANPD) designed a set of 72 clinical competencies that are primarily categorized according to the seven roles (or role domains) of the nurse preceptor (7). The seven roles include role model, teacher/coach, facilitator, protector, socialization agent, leader/influencer, and evaluator [See Figure 2].
Six of the 72 competencies are considered “core competencies,” meaning they do not fall under a specific role domain. Every nurse preceptor should meet core competencies regardless of the specific role they fulfill.
For example, in basic nursing, some nurses may be required to maintain a sterile environment in their role (like surgical nurses) while others can simply maintain a generally clean environment. However, all nurses, no matter the specialty, must follow basic infection control measures like general handwashing. Core competencies are similar to “general handwashing.” All nurse preceptors must meet core competencies, but others who fulfill certain roles must also meet the competencies of that particular role. As a general rule, all nurse preceptors should aim to fulfill all seven preceptor roles.
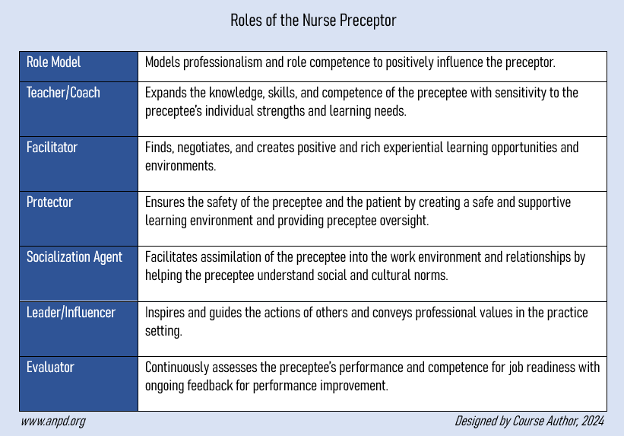
Figure 2: Roles (Role Domains) of the Nurse Preceptor (7).
Core Competencies
To meet core competencies, all nurse preceptors must apply evidence to practice when training preceptees. While preceptors may already engage in evidence-based practice as nurses, they must ensure that all information shared with the preceptee is based on current evidence. This competency requires that nurse preceptors stay up to date on current research. This may be done by regularly attending educational work meetings (like staff meetings and training sessions) and through self-learning, for example, enrolling in professional development courses (i.e., continuing education courses).
Other ways to meet core competencies are by solving problems, maintaining the preceptee’s confidentiality, and respecting diversity and others’ opinions [See Figure 3 below].
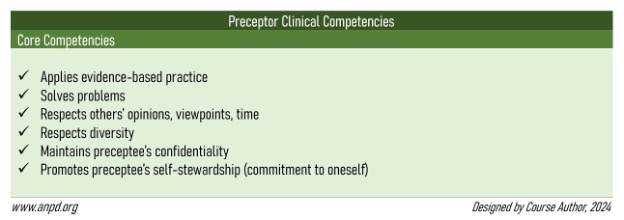
Figure 3: Nurse Preceptor Clinical Competencies Core Competencies (7).
Ask yourself...
- How do you ensure that you are practicing according to evidence?
- Have you ever witnessed a nurse preceptor disclosing (to other nurses) a new nurse’s challenges and weaknesses?
- What are some ways a nurse preceptor can teach problem-solving skills to a nursing student?
- Have you ever completed a nursing professional development course that was not required to renew your nursing license?
Role Model Competencies
Teaching by example is a way to influence the behavior of the preceptee [14] positively. Many people learn by watching the behavior of others in leadership roles. Modeling professional behavior is one of the primary roles of a preceptor. Nurse preceptors model time management skills, priority setting, critical thinking, problem-solving, and evidence-based practice (14).
To meet competencies for the role model domain, nurse preceptors should be aware of their own attitudes and behaviors, as these may impact the preceptee. The preceptor’s behaviors should align with what is being taught to the preceptee, as learners are most likely to remember what was done rather than what was said (10).
When mistakes are made, the nurse preceptor should demonstrate personal accountability. This way, the preceptee can not only learn the importance of taking accountability for their own actions in the workplace but also see what happens as a result (chain of events, rewards, disciplinary action, etc.). Preceptees should understand that disciplinary action is not meant to target the nurse but to promote positive changes in the workplace. Other competencies include modeling healthy and safe behaviors and demonstrating professional development [See Figure 4 below].
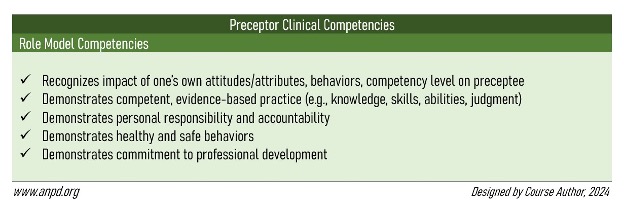
Figure 4: Nurse Preceptor Clinical Competencies for the Role Model Role (7)
Ask yourself...
- How confident do you feel about being a good role model to new nurses at your facility?
- If you have previously trained a new nurse, have you ever admitted to the new nurse a mistake you made during patient care?
- How often do you see new nurses adopting poor practice habits from their preceptors?
Teacher/Coach Competencies
Teaching is the cornerstone of clinical education. The primary goal of clinical education is to prepare the nursing student or new nurse for practice through clinical training and coaching/mentorship. As discussed earlier, effective teaching is learner-specific and tailored to the preceptee’s learning needs. To meet competencies for the teacher/coach role domain, nurse preceptors should incorporate the three domains of learning according to Bloom’s Taxonomy (5,9,13):
- Cognitive: attainment of knowledge (through written and verbal teaching)
- Psychomotor: development of hands-on skills (through demonstrative teaching)
- Affective: developing skills associated with attitudes, beliefs, values, or feelings (through ethics training, conflict resolution training, etc.)
Instilling critical thinking skills in the preceptee is also a primary goal when fulfilling the role of teacher/coach. Nurse preceptors might consider thinking aloud when observed by the preceptee, as this can show critical thinking and decision-making in action (7). When performing skills or care in the presence of the preceptee, speak aloud what is happening during each step. For example, if an elderly patient who is opioid-sensitive reports pain, review the medical record with the preceptee, stating out loud (or to the preceptee) thoughts such as:
“The patient already received a low-dose opioid for pain an hour ago. The patient’s most recent blood pressure is low. Since the patient is elderly, opioid-sensitive, and has low blood pressure, I will give a non-opioid medication for breakthrough pain instead. This way, the patient remains hemodynamically safe.”
The nurse preceptor can encourage the preceptee to ask questions or think aloud while caring for themselves. This way, the preceptor can evaluate the preceptee’s clinical reasoning skills [10]. Other competencies include helping the preceptee recognize errors and near misses, redirecting counterproductive behavior, showing the preceptee how to analyze situations and consider alternatives, and helping them differentiate between important and unimportant data.
[See Figure 5 below].
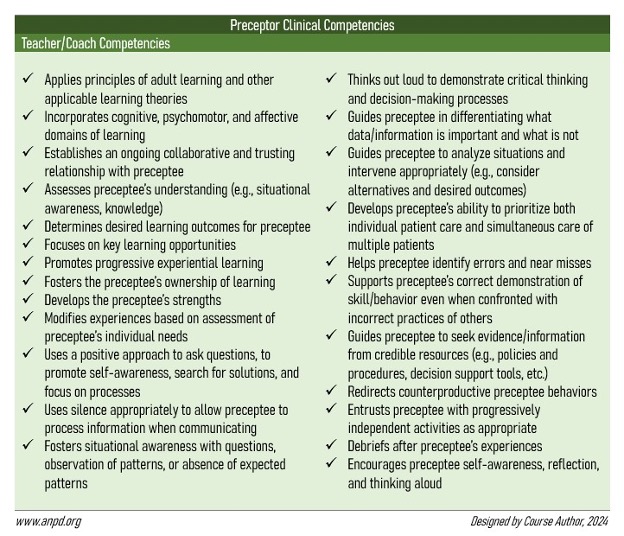
Figure 5: Nurse Preceptor Clinical Competencies for the Teacher/Coach Role (7)
Ask yourself...
- Have you ever had a coworker confront you about how you were training a new nurse? If so, how did you address the situation?
- How would you address a nursing student who frequently engages in excessive conversations with patients, ultimately disrupting care?
- If you have previously trained a nursing student, have you witnessed the student catch themselves before making an error?
- How else might a nurse preceptor encourage affective learning (learning domain) in a nursing student or new nurse?
Facilitator Competencies
To meet competencies for the facilitator role domain, nurse preceptors must identify learning needs in the preceptee and provide learning opportunities to meet those needs. Although similar to the teaching role, the facilitator makes a concerted effort to make learning easier for the preceptee. As mentioned earlier, nurse preceptors can arrange for the preceptee to observe or practice skills with other nurses within the facility/department. The nurse preceptor should take every opportunity to enhance the learning experiences of the preceptee.
For example, a nurse preceptor at a hospital can request patient assignments that might create optimal learning opportunities for a nursing student. This may include an assignment of patients who need certain skills/tasks performed that day (e.g., enteral feeding, wound care, intravenous insertions, pre-surgical preparation, etc.).
Other competencies include assessing the preceptee’s learning interests and providing resources for support [See Figure 6 below].
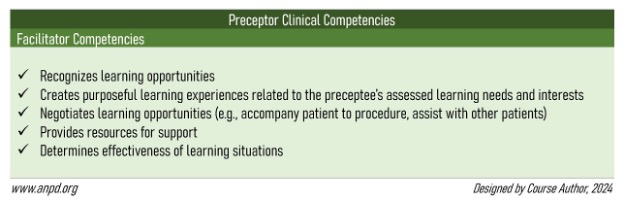
Figure 6: Nurse Preceptor Clinical Competencies for the Facilitator Role (7)
Ask yourself...
- Is your facility nursing-student-friendly? Do you find that your coworkers generally welcome students from local nursing schools?
- If you work in a hospital, do you find that patient assignments change when a nurse preceptor is on the floor?
- How open are you to allowing a group of nursing students to observe you perform a bedside skill?
- In what ways have you helped a nursing student gain additional learning opportunities within your department?
Protector Competencies
When training a nursing student, the nurse preceptor is fully responsible for the assigned patients, as only one nursing license exists. Although new nurses practice under their own licenses, nurse preceptors still have the responsibility of ensuring that the nurses practice safely. If a new nurse is reprimanded for a mistake made during a preceptorship, the preceptor is likely to be reprimanded as well. In a way, the nurse preceptor is “responsible” for the preceptee and serves as a protector.
To meet competencies for the protector role domain, nurse preceptors must ensure a safe environment for the preceptee. This may include protecting nursing students from physical abuse by teaching them how to properly interact with patients who display aggressive traits or standing up for new nurses to prevent incivility or bullying attempts by nursing peers (for example, when nurses “eat their young”). Other competencies include encouraging preceptees to advocate for themselves and anticipating issues that can cause moral distress to the preceptee [See Figure 7 below].
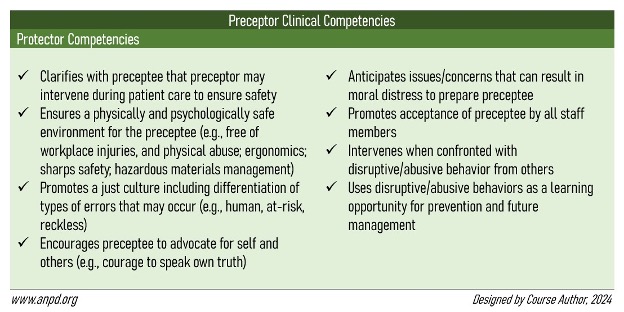
Figure 7: Nurse Preceptor Clinical Competencies for the Protector Role (7)
Ask yourself...
- Are you most comfortable with the idea of training nursing students or new nurses? What is your reasoning?
- Have you ever been reprimanded for a nursing student’s or a new nurse’s mistake while under your supervision?
- Can you think of another way a nurse preceptor can protect a nursing student or a new nurse from danger in the workplace?
- When you were a nursing student, were you ever bullied by a nurse? Did anyone speak up for you?
Socialization Agent Competencies
Many nursing students and new nurses experience a “reality shock” when entering the real world of nursing (7,12). While nursing school prepares the preceptee for clinical practice, some situations may arise in the workplace that may be hard to simulate in a controlled educational setting. To meet competencies for the socialization agent role domain, nurse preceptors must introduce preceptees to the unspoken rules and culture of both real-life nursing and the facility itself (7,14).
For example, a new graduate nurse may be unprepared for the many interruptions that often occur when practicing nursing in a clinical setting (e.g., phone calls, physician requests, family visits, and frequent documentation). The new nurse may also be unaware that the department in which they are training schedules interdisciplinary team rounding sessions at a specific time every day, which can make it difficult to establish a solid routine. The nurse preceptor has a responsibility to introduce the preceptee to these types of “real-life” situations.
Other competencies include providing the preceptee with opportunities for interprofessional engagement and inclusion in department activities (like work parties) [See Figure 8 below].
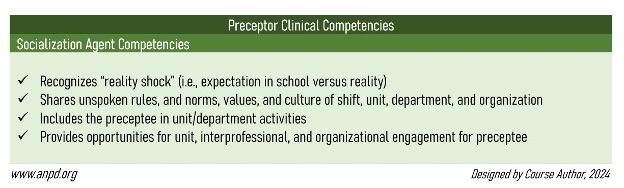
Figure 8: Nurse Preceptor Clinical Competencies for the Socialization Agent Role (7)
Ask yourself...
- How was your first day as a nurse? Did you experience a reality shock, or were you fairly prepared?
- What is something within the culture or practice of your facility that might cause a new nurse to experience a reality shock?
- How does your facility formally introduce new nurses to your department? Email, newsletter, work meeting, quick huddle?
- Have you ever had lunch (at work) with a nursing student or new nurse you were training?
Leader/Influencer Competencies
Leadership skills are vital when training others and serving as a role model. To meet competencies for the leader/influencer role domain, nurse preceptors must demonstrate professionalism and adhere to codes of conduct and regulations. Recognizing the scope of practice of preceptees (nursing students versus new nurses), delegating appropriate tasks, and providing recognition are additional leadership skills the preceptor should possess. Most importantly, the nurse preceptor can demonstrate leadership by advocating for patients.
When nurse preceptors possess excellent leadership skills, they can serve as change agents within the workplace, positively influencing decisions that affect patients, their peers, and the preceptees they train. To be a change agent, nurse preceptors must possess people skills and be able to work effectively in a team (qualities of a leader) (14)
Other competencies include participating in professional activities at the facility, engaging in self-reflection, and helping the preceptee develop a professional role identity [See Figure 9 below].
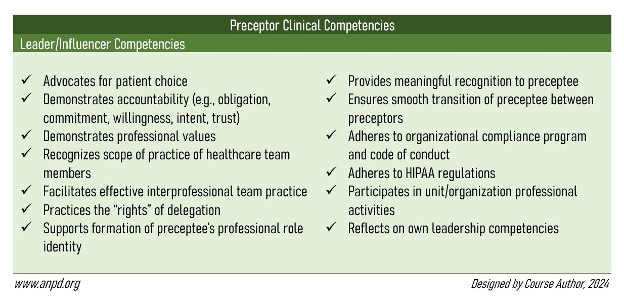
Figure 9: Nurse Preceptor Clinical Competencies for the Leader/Influencer Role (7).
Ask yourself...
- In what ways do you self-reflect? Do you find that self-reflection contributes to your professional growth?
- Have you ever advocated for a patient in the presence of a nursing student or a new nurse?
- Have you ever witnessed a nurse preceptor delegate a task to a nursing student that was out of their scope of practice?
- Think of a nurse within your department who you consider a leader. What sets them apart from other nurses?
Evaluator Competencies
As mentioned earlier, evaluation is the best way for the nurse preceptor to know that the preceptee understands what is being taught. To meet competencies for the evaluator role domain, nurse preceptors must assess preceptee performance and provide accurate, specific, and constructive feedback (both verbal and written). Preceptors must also hold the preceptee accountable for their practice. Other competencies include managing difficult conversations when providing constructive feedback, and informing preceptees of their strengths and areas where improvements are needed [See Figure 10 below].
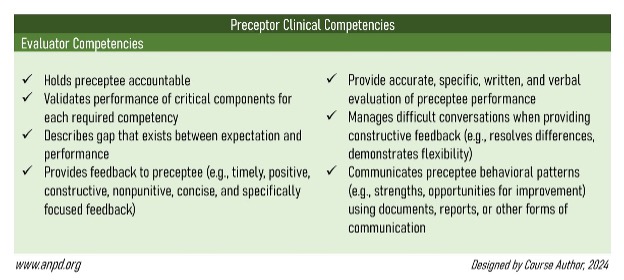
Figure 10: Nurse Preceptor Clinical Competencies for the Evaluator Role (7)
Ask yourself...
- What was the first compliment you received as a nurse? How important did it make you feel?
- In the past, have you ever felt offended or hurt when a manager gave you constructive feedback? What made you feel that way?
- If you have previously trained a new nurse, did you give written or verbal feedback (or both)?
- With the knowledge from this course, do you feel better prepared to begin your role as a nurse preceptor (or continue doing so)?
Conclusion
Nurse preceptors are a valuable asset to the nursing profession. They assess learners, build trusting relationships, tailor teaching to learning styles, evaluate performance, provide feedback, and encourage independence in the preceptee. Although nurse recruitment and retention are dependent on the availability and service of nurse preceptors, the position has its challenges.
The nurse preceptor role is not always given the recognition it deserves. However, when nurses are adequately prepared for the role, they have the potential to lead positive changes in the workplace, influencing the lives of nursing students and new nurses. Moreover, nurse preceptors can impact the healthcare field by contributing to the future of nursing, ultimately leading to better outcomes for patients.
References + Disclaimer
- American Association of Colleges of Nursing. (2022). Nursing faculty shortage sheet. https://www.aacnnursing.org/news-data/fact-sheets/nursing-faculty-shortage
- American Association of Colleges of Nursing. (2022). Nursing shortage fact sheet. https://www.aacnnursing.org/news-data/fact-sheets/nursing-shortage
- American Association of Colleges of Nursing – American Organization of Nursing Leaders, Advisory Committee. (2020). AACN-AONL clinical preceptor survey summary report. https://www.aacnnursing.org/Portals/0/PDFs/Data/AACN-AONL-Clinical-Preceptor-Survey-May-2020.pdf
- American Nurses Association. (n. d.). Why nurses quit and leave the profession? https://www.nursingworld.org/practice-policy/nurse-staffing/why-nurses-quit/
- Bloom, B. S. (1956). Taxonomy of educational objectives, handbook 1: The cognitive domain. David McKay Co.
- Childs-Kean, L., Edwards, M., & Smith, M. D. (2020). Use of learning style frameworks in health science education. American Journal of Pharmaceutical Education, 84(7), ajpe7885. https://doi.org/10.5688/ajpe7885
- Figueiredo, L. D. F., Silva, N. C. D., & Prado, M. L. D. (2022). Primary care nurses’ learning styles in the light of David Kolb. Brazilian Journal of Nursing, 75(6), e20210986. https://doi.org/10.1590/0034-7167-2021-0986
- Harper, M., Ulrich, B., MacDonald, R., Maloney, P., Warren, J. I., & Whiteside, D. (2023). Summary findings from the 2023 preceptor competency consensus study. Association for Nursing Professional Development. https://www.anpd.org/Portals/0/Files/ANPD_1127571-23_PreceptorCompetencies_Report.pdf
- Krathwohl, D. R., & Bloom, B. S. (1973). Taxonomy of educational objectives, the classification of educational goals, handbook II: Affective domain. David McKay Co.
- Loughran, M. C., & Koharchik, L. (2019). Ensuring a successful preceptorship. American Journal of Nursing 119(5):61-65. https://journals.lww.com/ajnonline/Fulltext/2019/05000/Ensuring_a_Successful_Preceptorship.32.aspx
- National Advisory Council on Nurse Education and Practice. (2021). Preparing nurse faculty and addressing the shortage of nurse faculty and clinical preceptors. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/nursing/reports/nacnep-17report-2021-508.pdf
- Powers, K., Herron, E., & Pagel, J. (2019). Nurse preceptor role in new graduate nurses’ transition to practice. Dimensions of Critical Care Nursing 38(3):131-136. https://journals.lww.com/dccnjournal/fulltext/2019/05000/nurse_preceptor_role_in_new_graduate_nurses_.4.aspx
- Robinson, C. (2022). Are nurse preceptors the new clinical instructors? MEDSURG Nursing, 31(1): 55-56. https://www.proquest.com/openview/5a19002dc1e28d48a357250377696db8/1.pdf?pq-origsite=gscholar&cbl=30764
- Sherrod, D., Holland, C., & Battle, L. (2020). Nurse preceptors: A valuable resource for adapting staff to change. Nursing Management (Springhouse), 51(3): 50-53. https://journals.lww.com/nursingmanagement/fulltext/2020/03000/nurse_preceptors__a_valuable_resource_for_adapting.9.aspx
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
