Course
Obsessive Compulsive Disorder (OCD)
Course Highlights
- In this Obsessive Compulsive Disorder course, we will learn about clinical signs and symptoms of OCD.
- You’ll also learn about current medications for the treatment of OCD.
- You’ll leave this course with a broader understanding of ethical and cultural considerations in the care of patients with OCD.
About
Contact Hours Awarded: 2
Course By:
Abbie Schmitt
MSN-Ed, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Obsessive-Compulsive Disorder (OCD) is a chronic mental health condition characterized by uncontrollable, recurring thoughts and behaviors (compulsions). The impact of OCD on an individual’s life can be profound, affecting personal relationships, work, and overall quality of life. It is important to recognize the signs of OCD, offer appropriate interventions, and support patients and their families throughout the treatment process.
It is imperative to understand the clinical features, pathophysiology, and diagnostic criteria of OCD. There is meaningful research on the spectrum of obsessions and compulsions, and how they manifest in daily life.
There are evidence-based treatment options for OCD, including pharmacotherapy, cognitive-behavioral therapy (CBT), and emerging interventions. Nurses must consider the impact of cultural beliefs on the perception and treatment of mental health conditions.
Definition of Obsessive Compulsive Disorder
Obsessive-compulsive disorder (OCD) is a complex neuropsychiatric disorder with several genetic, epigenetic, and environmental factors contributing to its development. OCD is a condition in which the affected individual frequently has irresistible urges (obsessions) to perform repetitive rituals (compulsions). OCD is characterized by the presence of obsessions and/or compulsions, and knowledge of the differences between these behaviors is essential.
Obsessions are recurrent and persistent thoughts, urges, or images that are intrusive and unwanted experiences.
Compulsions are repetitive behaviors or mental (internal) acts that an individual feels compelled to perform in response to an obsession (3).
There are close correlations between anxiety disorders and OCD. Obsessive-compulsive and related disorders (OCDR) differ from developmentally normative preoccupations and rituals in that these disorders are excessive or persist beyond developmentally appropriate periods. The level of an individual’s distress and impairment in functioning is a key consideration when evaluating patients suspected of having OCD.
There is a constant cycle for those who struggle with OCD. Obsessional fears are developed through classical conditioning, whereby the conditioned stimulus (thoughts, objects, or situations) can trigger anxiety or discomfort because it is associated with an unpleasant stimulus. After experiencing the obsession, the patient may perform a compulsion to reduce the anxiety or discomfort triggered by the obsession. The compulsion is maintained through a process of negative reinforcement; in that it encourages continued behavior because the individual believes the compulsion was effective in reducing negative feelings or preventing feared consequences (11). This is called the behavioral model for OCD.
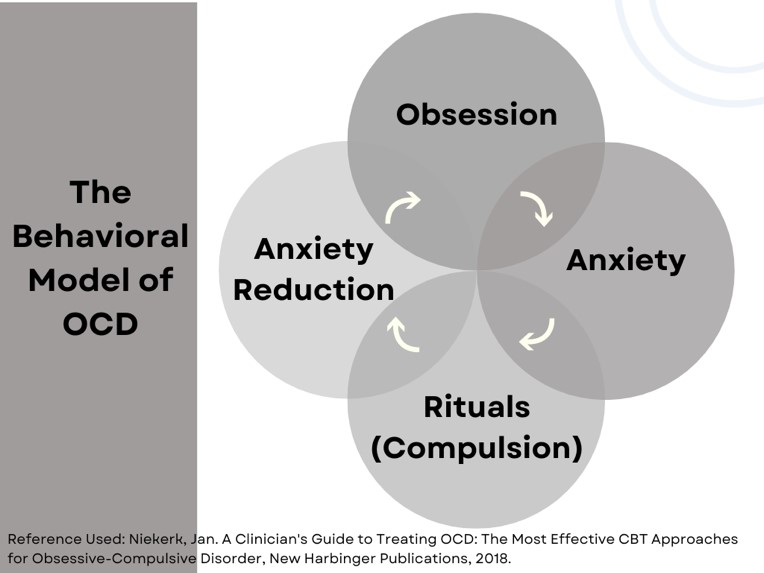
Image 1. The behavioral model for OCD. [Image designed by course author]
In The Diagnostic and Statistical Manual of Mental Disorders (DSM)-5, published by the American Psychiatric Association (APA), OCD is a category of obsessive-compulsive and related disorders (OCRD), which includes the following subcategories (1):
- Obsessive-compulsive disorder (OCD)
- Body dysmorphic disorder (BDD)
- Hoarding disorder
- Trichotillomania
- Excoriation (skin-picking) disorder
- Substance/medication-induced obsessive-compulsive and related disorder
- Obsessive-compulsive and related disorder as a result of another medical condition
- Other specified obsessive-compulsive and related disorder
- Unspecified obsessive-compulsive and related disorder

Self-Quiz
Ask Yourself...
- Can you describe the difference between obsessions and compulsions?
- Is the level of distress noted in an individual an important factor when assessing for OCD?
- Under which category is OCD in The Diagnostic and Statistical Manual of Mental Disorders (DSM)-5?
- Can you name a few examples of other disorders within the obsessive-compulsive and related disorders (OCRD) category in the (DSM)-5?
Epidemiology of Obsessive Compulsive Disorder
The prevalence of OCD in the general population is roughly 2–3% of the global population (2). Cultural, economic, and social factors play a role in the presentation of OCD, but genetic inheritance is the most commonly associated risk factor. OCD is a global phenomenon, with similarities across the world in symptomology, gender distribution, age of onset, and comorbidities (2). Similarly, OCD is found among individuals across socioeconomic classes, as well as in impoverished and high-income countries (10).
Substantial delays can occur before patients with OCD seek treatment. Barriers to seeking treatment include a lack of knowledge about this disorder, embarrassment about symptoms, or anxiety about exposure to feared stimuli. It is estimated there is a significant amount of undiagnosed and untreated individuals currently living with OCD.
Females are affected at a slightly higher rate than males in adulthood, although males are more commonly affected in childhood (3). Males have been shown to have an earlier age of onset than females: nearly 25% of males have onset before age 10 years (3).
In the United States, the mean age at onset of OCD is 19.5 years, and 25% of cases start by age 14 years (3). The onset of symptoms is typically gradual; however, acute onset has been reported.
Onset in childhood or adolescence can lead to a lifetime of a varying degree of symptoms; however, 40% of individuals with onset of OCD in childhood or adolescence may experience remission by early adulthood (2).

Self-Quiz
Ask Yourself...
- How common is OCD throughout the world?
- Is it possible for someone with the onset of OCD in childhood to have complete remission of symptoms by adulthood?
- Around what age is the mean age of onset for OCD?
- Are the symptoms of OCD usually gradual or acute?
Pathophysiology of Obsessive Compulsive Disorder
Many theories attempt to explain the pathophysiology of OCD, but prevailing theories indicate that OCD is a biological disease.
Functional brain imaging studies have produced a model explaining that hyperactivity in certain subcortical and cortical regions is an underlying component of the pathophysiology of OCD. Dysfunction in the orbitofrontal cortex, anterior cingulate cortex, and striatum have been strongly implicated in the pathophysiology of OCD (3). An overactivation of this orbitofrontal (OFC) and anterior cingulate (ACC) cortices, as well as the caudate, insula, and amygdala, and a hypoactivation of the dorsolateral prefrontal cortex (DLPFC) appear to be present in individuals with OCD (6).
Many researchers attribute the pathophysiology of OCD to a dysfunction in the neurobiology of cortico-striato-thalamo-cortical (CSTC) circuits, which are responsible for reward- and motivational-related processes, executive function, motor and response inhibition, and habit-based behavior (9). CSTC circuits project from the frontal-cortical area to the striatum, and then onward to thalamic sites, then loop back to the cortex (9). An imbalance between these pathways is suggested to contribute to OCD pathology. Research has shown enhanced activation of these CSTC circuits in patients with OCD following symptom provocation (9).
Antipsychotic drugs that modulate dopamine activity and serotonin reuptake inhibitors (SRIs) have been shown to improve OCD symptoms in a significant number of patients; this suggests dopamine and serotonin involvement in OCD and is consistent with imaging studies in OCD revealing increased dopamine concentrations in the basal ganglia (9).
However, researchers agree that a combination of biological activity with social and environmental factors is most likely the cause of symptomology among those with OCD.
Electroencephalographic (EEG) Approach to Understanding OCD
EEG measures have been increasingly applied in research in the fields of psychiatry, neurology, and neurosciences (6). The use of EEG measures attempts to clarify the underlying mechanisms with techniques such as:
- Quantitative EEG (QEEG)
- “Brain Mapping”
- An analytical technique that describes EEG parameters related to band power, synchronization, and activation patterns in the brain during electroencephalographic recordings (6).
- Intracerebral electroencephalography (iEEG).
- This technique involves placing electrodes directly onto the exposed surface of the brain to monitor activity from the cortex, providing excellent anatomical precision
A recent review of the electrophysiological literature on OCD has suggested frontal asymmetries in alpha and theta band power (6). Band types have been extensively studied in psychiatric disorders and help researchers understand cognitive functions from an observable perspective. Asymmetries are the difference between right and left activity over frontal regions of the brain, and the band power suggests which of the areas (left or right) is more strongly active.
Alpha band asymmetries have been linked to avoidance in OCD and are associated with difficulties in suppressing distractors or task-irrelevant details (6); theta band asymmetries are believed to interfere with inhibition during cognitive task performance. When these bands are present together, these asymmetries could explain the strains experienced by patients with OCD in suppressing obsessive thoughts.

Self-Quiz
Ask Yourself...
- How would you describe the role of CSTC circuits in the formulation of habits?
- What specific neurotransmitters are thought to correlate with OCD?
- What regions of the brain are implicated in the pathophysiological explanation of OCD?
- Are you familiar with SRIs and medications that modulate dopamine activity?
Etiology of Obsessive Compulsive Disorder
Genetic and Physiological
The role of genetics in the development of OCD has been confirmed through multiple studies and has established OCD prevalence in family members of patients with OCD. Studies hypothesize that OCD is inherited in 27% to 47%, while childhood-onset OCD has an even greater genetic component (45–65%) (2). In accordance, relatives of patients with OCD are twice as likely to develop OCD than those of healthy subjects. In contrast, rates in relatives of children and adolescents with OCD showed a tenfold increase relative to controls (2).
The rate of OCD among first-degree relatives of adults with OCD is approximately two times higher than those without a first-degree relative with the disorder (3). This is a major risk factor when considering the etiology of OCD.
Gene studies have suggested a potential role for variants in serotonergic, catecholaminergic, and glutamatergic genes in OCD (10).
Environmental
A wide range of environmental factors, including adverse perinatal events such as birth complications and stressful or traumatic events, have been identified as potential risk factors for OCD (10). Research is typically focused on cellular and molecular pathways by which genetic and environmental risk factors can have an impact. This includes genetic-imaging studies and genome-wide environmental interaction studies (10).
A sudden onset of symptoms consistent with OCD has been associated with different environmental factors, including various infectious agents and post-infectious autoimmune syndrome (3). Physical and sexual abuse in childhood and other stressful or traumatic events have been associated with an increased risk of developing OCD as well (3).
Individual Temperament
Individuals diagnosed with OCD have similar temperamental risk factors, including a higher negative outlook or emotional response, and behavioral inhibition in childhood (3). Behavioral inhibition (BI) is a temperament identified early in childhood that describes a fearful style of reacting when confronted with nonideal circumstances and increased risk for anxiety in adolescence.
Culture-Related Diagnostic Issues
As we mentioned, there is significant similarity across cultures in the gender distribution, age at onset, and comorbidity of OCD (3). For example, individuals from different cultures similarly express thoughts and actions about cleanliness or cleaning routines, symmetry of items, hoarding, taboo thoughts, and fearfulness of harm (3). However, variation does exist in more specific expressions, and cultural factors can shape the content of obsessions and compulsions.


Self-Quiz
Ask Yourself...
- Do genetics have a role in the development of OCD?
- How would you describe the risk for OCD if a first-degree relative has this diagnosis?
- In your own words, how would you describe the term temperament?
- Can you name examples of common thoughts and actions? (example: cleaning, symmetry)
Clinical Signs and Symptoms of Obsessive Compulsive Disorder
In this section, we will attempt to paint a picture of patients with OCD by providing possible obsessions and compulsions, as these are the most prominent signs and symptoms. You can consider obsession as an internal struggle and compulsion as an outward expression of that struggle. The obsession and compulsion will correlate to the patient, even if it does not correlate to others.
Essentially, the patient with OCD has thoughts or actions that:
- Take up at least an hour a day
- Are uncontrollable
- Cause significant distress
- Interfere with work or social life
Studies have found it useful to apply a five-factor model of OCD symptoms and dimensions; the dimensions include a ‘contamination’ dimension, a ‘harmful thoughts’ dimension, a ‘forbidden thoughts’ dimension, a ‘symmetry’ factor, and a ‘hoarding’ factor. Hoarding symptoms can be found in patients with OCD in some cases, but hoarding disorder is considered a separate entity in the DSM-5.
|
Dimension |
Obsessions |
Compulsions |
|
Contamination symptoms |
Fear of germs, dirt, or contamination |
Excessive cleaning and washing |
|
Harm-related symptoms |
Fear of harm to themselves or others |
Checking, repetitive actions |
|
Unacceptability symptoms |
Intrusive “taboo” thoughts (aggressive, sexual, violent) |
Mental rituals |
|
Symmetry symptoms |
Needing items lined up or arranged in a particular way (typically symmetrical) |
Straightening, excessively counting or repeating. |
|
Hoarding symptoms |
Hoarding |
Accumulating or hoarding actions in excess |
Compulsions are the behaviors that patients feel they must do to reduce their anxiety or stop their obsessive thoughts. Some common compulsions include:
- Excessive cleaning and/or handwashing
- Repeatedly checking on things, such as whether the door is locked or the oven is off
- Compulsive counting
- Repetitive mental rituals
- Ordering and arranging things in a particular, precise way
Individuals may also experience marked anxiety that can include recurrent panic attacks. Some report strong feelings of disgust, “incompleteness”, and a sense of uneasiness (3).
Patients with OCD experience a range of affective responses when confronted with situations that trigger obsessions and compulsions. It is common for those with OCD to avoid people, places, and things that trigger obsessions and compulsions. For example, individuals with contamination concerns might avoid public restrooms or crowded subways to reduce exposure to feared contaminants. Another example would be individuals with intrusive thoughts about symmetry or organization might avoid social interactions at the homes of others in case it is messy or unorganized. This avoidance may seem to relieve the symptoms, but it is overall distressful to the individual.

Self-Quiz
Ask Yourself...
- How would you describe the relationship between the obsessive and compulsive symptoms of OCD?
- Can you discuss the different dimensions in which symptoms are commonly classified?
- What is a common compulsion for an obsession about fears of harm to oneself or someone else?
- What is a possible obsession for the compulsion of excessively organizing, straightening, or ordering items in a precise way?
Diagnostic Criteria for Obsessive Compulsive Disorder
Diagnostic criteria (300.0) for OCD include:
- Presence of obsessions, compulsions, or both:
Obsessions are defined by both of the following:
-
- Recurrent and persistent thoughts, urges, or images that are experienced as intrusive and unwanted, and cause significant distress.
- The individual attempts to ignore, or divert the thoughts, urges, or images.
Compulsions are defined by both of the following:
-
- Repetitive behaviors that the individual feels driven to perform in response to an obsession. Examples: Hand washing, checking, counting, repeating words silently.
- The behaviors or mental acts are performed to prevent or reduce anxiety, distress, or a dreaded event; however, these behaviors are not connected realistically with what they are designed to prevent.
- The obsessions or compulsions are time-consuming, distressing (clinically), or cause impairment in social, occupational, or other important areas of functioning.
- Obsessive-compulsive symptoms are not caused by the physiological effects of a substance (medication or illicit drug) or another medical condition.
- The symptoms are not more appropriately attributed to another mental disorder (e.g., generalized anxiety disorder, body dysmorphic disorder, hoarding disorder, trichotillomania, substance-related and addictive disorders, preoccupation with having an illness, schizophrenia spectrum or repetitive patterns of behavior in autism spectrum disorder).
Diagnosis should specify if (3):
- With good or fair insight: The patient recognizes that OCD beliefs are definitely or probably not true.
- With poor insight: The patient thinks OCD beliefs are probably true.
- With absent insight/delusional beliefs: The patient is completely convinced that obsessive-compulsive disorder beliefs are true.
Diagnosis should specify if (3):
- Tic-related: The patient has a current or past history of a tic disorder.
It is helpful to classify OCD into endophenotypes. Endophenotypes are objective and quantitative traits. This approach has been used to gain a better understanding of psychiatric conditions in general because it turns theoretical data into quantifiable data to evaluate. Researchers theorize that endophenotypes are particularly useful in clarifying both the diagnostic status and etiology of complex neuropsychiatric conditions, such as OCD. Executive functioning deficits are one of the most researched endophenotypes for OCD (10).

Self-Quiz
Ask Yourself...
- Can you summarize each diagnostic criteria for OCD?
- What are endophenotypes?
- Would you describe a patient who believes their obsessions are probably true as having fair or poor insight?
- Can you think of reasons why patients with good insight into their obsessions may have better outcomes in treatment for OCD?
Impact of Obsessive Compulsive Disorder on Quality of Life and Functioning
Obsessive-compulsive disorder (OCD) is associated with reduced quality of life and disturbance of social and occupational functioning. This disturbance affects different domains of life and varies with symptom severity. The disturbance correlates to the amount of time spent obsessing and doing compulsions. Avoidance of situations that can trigger obsessions or compulsions can also severely restrict the patient’s ability to enjoy things they would otherwise enjoy.
In addition, specific symptoms can create harm to relationships with family and friends. Obsessions about symmetry can derail the timely completion of projects for work or school because the goal of “perfection” takes too long and can potentially result in school failure or job loss.
Poor health outcomes can also be a result of these obsessions and compulsions. For example, individuals with contamination concerns may avoid doctor visits because they fear being exposed to germs at the office. Another common development is dermatological problems in those who excessively wash their skin. Obsessions with medication contamination can also result in noncompliance with treatment regimens.

Self-Quiz
Ask Yourself...
- What are some examples of interference in a patient’s social life with OCD?
- How can family and friends inadvertently make the anxiety of a patient with OCD worse?
- Can you describe how work with various jobs could be impacted by OCD symptoms?
- What are some examples of poor health outcomes associated with OCD?
Comorbidities
Individuals with OCD often have additional psychopathology. Anxiety and depression are very common comorbidities of this disorder.
Research suggests that 70 – 80% of individuals with OCD also have an anxiety disorder (e.g., panic disorder, social anxiety disorder, generalized anxiety disorder, specific phobia) and approximately 60% also have a depressive or bipolar disorder (major depressive disorder is most common) (3). Post-traumatic stress disorder (PTSD) often precedes depressive disorders (3).
Some people with OCD also have Tourette syndrome or another tic disorder. Tics are sudden twitches, movements, or sounds that an individual does repeatedly. Those who have tics lack control and cannot stop their body from doing these things. Up to 30% of individuals with OCD have a lifetime tic disorder; this condition is most common in males with the onset of OCD in childhood (3).
Additional disorders that occur more frequently in those with OCD include body dysmorphic disorder, trichotillomania (hair-pulling disorder), and excoriation (skin-picking) disorder (3).
These comorbidities may be diagnosed before OCD, so if one of these other disorders is diagnosed, the individual should be assessed for OCD as well. For example, it is meaningful to assess for OCD in individuals with bipolar disorder, eating disorders, such as anorexia nervosa and bulimia nervosa, and Tourette’s disorder (3).

Self-Quiz
Ask Yourself...
- What percentage of people with OCD are believed to also have an anxiety disorder?
- How would you describe the difference between a compulsion and a tic?
- Can you name comorbidities commonly noted among patients with OCD?
- Can you describe ways OCD symptoms can impact an individual’s quality of life?
Treatment of Obsessive Compulsive Disorder
Obsessive-compulsive disorder (OCD) is most commonly treated with psychotherapy and pharmacology. Treatment options for OCD comprise several components: psychoeducation, psychological and/or pharmacological approaches, and, for patients with treatment-resistant OCD, neuromodulation, and neurosurgery (10).
Although similar therapies are used throughout the lifespan, some modifications are needed when treating children and adolescents (10).
Clinical research has led to the development of behavioral and cognitive–behavioral models of OCD, and have the foundational idea that obsessions can be conceptualized as noxious stimuli to which individuals fail to habituate (10). Essentially, there are deficits in mechanisms that are central to extinction learning, as obsessive thoughts require neutralizing behaviors (compulsions). In these models, behavioral therapy can be used for acclimation to fears, while cognitive therapy can be applied for belief disconfirmation. Model frameworks have the foundational concept that domains or meta-cognitions in OCD involve the overestimation of fears and excessive concern about the importance of controlling one’s thoughts.
Pharmacological therapies are also used in treating OCD. The medication classes most commonly used in the treatment of OCD are serotonin and norepinephrine reuptake inhibitors (SNRIs) and selective serotonin reuptake inhibitors (SSRIs).

Psychotherapy in Obsessive Compulsive Disorder
Cognitive–behavioral therapy (CBT)
Cognitive–behavioral therapy (CBT) is the most evidence-based form of psychotherapy for OCD (10). Studies have consistently demonstrated that CBT significantly improves OCD symptoms in both adults and children. CBT comprises two components: cognitive reevaluation and behavioral intervention. CBT involves reflection of inaccurate or negative thinking, challenging situations more clearly, and responding to them more effectively. Meta-analyses of randomized controlled trials have indicated that CBT has larger effect sizes than pharmacological therapy for the treatment of OCD. In cognitive behavioral therapy, the goal is to create a safe place to experience distressing thoughts or beliefs while avoiding compulsive behavior.
CBT is based on several core principles, including:
- Psychological problems are developed in part by faulty or unhelpful ways of thinking.
- These ways of thinking lead to learned patterns of unhelpful behavior.
- Those psychological problems can learn better ways of coping with the thoughts and patterns, thereby relieving their symptoms and becoming more effective in their lives.
Essentially, CBT treatment typically involves efforts to change the thinking patterns of those with OCD. These strategies might include:
- Learning to recognize these patterns is creating problems, and then reevaluating them in light of reality. An example is the compulsions interfering with work tasks.
- Using problem-solving skills to cope with difficult situations.
- Learning to develop a stronger sense of confidence and control of actions and behaviors.
For patients with OCD, the focus of CBT may be on the root cause of obsessions and reevaluating the obsession itself and why it is incorrect. An example would be a patient who has “taboo” thoughts and extreme anxiety from sexual thoughts that are perceived as unacceptable. A review of human anatomy and the basic physiology of hormonal and neural networks that are responsible for these thoughts can help patients understand that they are not “bad” for having these thoughts, but there is a physiological reason.
Exposure and Response Prevention (ERP) Therapy
Another effective approach for treating OCD is Exposure and Response Prevention (ERP) therapy. ERP therapy interrupts the OCD cycle of obsessions and compulsions to build tolerance to the discomfort felt when resisting compulsion. ERP involves gradual and prolonged exposure to fear-provoking stimuli combined with instructions to not complete compulsive behavior.
ERP is even more effective when combined with a discussion of feared consequences and dysfunctional beliefs. The goal of therapy is for the triggering stressor to cause less and less of a stressful response. Treatment itself can be very uncomfortable and difficult for some patients to adhere to.
An example of an ERP therapy session is for a patient diagnosed with OCD, specifically with germ-related fears, to touch a doorknob or shake another individual’s hand, followed by being encouraged by their mental health counselor to refrain from washing their hands for a certain amount of time. Another example would be if an adolescent has OCD with fears of harming themselves and specifically fears throwing themselves in front of oncoming traffic; treatment may incorporate walking calmly over a bridge above a busy highway.
Mindfulness-Based Therapy
Mindfulness-based therapies, such as mindfulness-based cognitive therapy (MBCT), focus on practicing being in the moment and being aware of harmful thoughts. Mindfulness-based therapies are effective in reducing symptoms of OCD as they can reduce symptoms of anxiety that come along with OCD.
The following quote reminds us of the concept of mindfulness in the treatment of OCD:
“Mindfulness gives you time. Time gives you choices. Choices, skillfully made, lead to freedom.” – Bhante H. Gunaratana
Regardless of which approach is used, the individual and therapist will work to address and reframe the underlying thoughts and fears that lead to anxiety-driven compulsive behaviors. Patients who also suffer from depression may need treatment for depression before initiating CBT or ERP because each individual must have the energy and internal motivation to engage in therapy.
Pharmacotherapy in Obsessive Compulsive Disorder
Medications might also be used to initiate the treatment of OCD. About 7 out of 10 people with OCD will benefit from a therapeutic medication regimen and those who benefit from medication have an approximately 40-60% reduction in their OCD symptoms (8).
Serotonin is believed to be associated with OCD. Serotonin is a neurotransmitter that has an important role in regulating various activities, including behavior, mood, and memory (1). It is often referred to as the “feel-good hormone” and delivers messages between brain cells, contributing to well-being, mood, appetite, and social behavior.
Selective serotonin reuptake inhibitors (SSRIs) are the first-line pharmacological treatment for OCD based on their evidence of efficacy, tolerability, safety, and low potential for abuse (10). SSRIs block the reabsorption of serotonin into neurons, which makes more serotonin available to assist the transmission of messages between neurons. In patients with OCD, this improved delivery of messages throughout the brain (especially the front part of the brain) can help with reasoning and behavior.
Higher doses of SSRIs are typically used for OCD than for other anxiety disorders or major depression; higher doses of SSRIs are associated with greater treatment efficacy, but also greater risks for undesirable side effects. Thus, a thorough assessment of SSRI adverse effects is crucial when establishing the therapeutic dose for each patient.
Serotonin and norepinephrine reuptake inhibitors (SNRIs) are also used in the treatment of OCD. Norepinephrine is a neurotransmitter in the brain that plays an essential role in the regulation of arousal, attention, cognitive function, and stress reactions (11). SNRI mechanism of action involves the inhibition of presynaptic neuronal uptake of serotonin and norepinephrine after release from the synaptic cleft, which blocks the reuptake of these neurotransmitters within the central nervous system (CNS) (11).
SSRI: fluoxetine, fluvoxamine, sertraline, citalopram, escitalopram and paroxetine.
SNRI: venlafaxine
OCD treatment guidelines indicate that 8–12 weeks is the optimal duration recommended to determine efficacy (10). The recommended maintenance duration of pharmacotherapy is a minimum of 12–24 months after successfully reducing symptoms, but longer treatment might be necessary for many patients.
Patients should be extensively educated on the purpose of prescribing, the dosing regimen, and the side effects of these drugs.

Self-Quiz
Ask Yourself...
- Can you explain the goals of CBT?
- How could these treatments possibly be stressful for patients with OCD?
- Are you familiar with the side effects of common SSRIs?
- What is the optimal duration to determine the efficacy of pharmacological therapy for OCD?
Nursing Advocacy and Interventions in Obsessive Compulsive Disorder
Patients and their loved ones often report considerable relief when they are told by a professional that they have a relatively common disorder that with available treatments can bring at least partial symptom reduction and improved quality of life. Nurses can empower patients diagnosed with this disease and reduce any feelings of embarrassment or stigmatization. It would be valuable to educate patients on the statistics and prevalence of OCD.
Building a therapeutic relationship is key. There is a stigma on this behavior, and it may cause patients to feel mistrust or self-consciousness in discussing them. Assessment and interviewing techniques can be helpful with patients who have OCD. These techniques focus on empathizing with the patient’s experience, discussing the symptoms and their impact on the patient’s daily routine, and exploring the benefits and costs of symptom reduction. Organizations such as the International OCD Foundation are incredible resources for education, support, and treatment.
Psychoeducation is vitally important to empower those with OCD to gain control. Nurses should teach patients about the symptoms of OCD, medication uses and side effects, and other treatments.
Nursing Diagnoses
- Anxiety
- Powerlessness
- Ineffective verbal communication
- Impaired social interaction
- Risk for injury
- Sleep pattern disturbances
Nursing Interventions
- Assist the patient in recognizing the onset of anxiety.
- Explore the meaning and purpose of the behavior with the client.
- Encourage family participation in therapy programs.
- Limit, but do not interrupt the compulsive acts.
- Teach the client to use alternate coping methods to decrease anxiety.
- Research shows that an environment that has structure and predictability is an effective strategy to decrease anxiety.
- Teaching topics and points:
- Create a consistent and healthy daily routine
- Take medications as directed by the provider
- Create a consistent sleep schedule
- Make regular exercise a part of your routine
- Importance of a healthy, balanced diet
- Seek support from trusted family and friends
- Risks associated with the use of alcohol and drug abuse.

Self-Quiz
Ask Yourself...
- Can you describe teaching points for medications commonly prescribed for OCD?
- How would you provide education to a patient with OCD on creating a healthy, consistent daily routine?
- Should you interrupt a ritual if your patient has already started it?
- How can you help in encouraging patients to limit rituals?

Conclusion
As we conclude our exploration into obsessive-compulsive disorder (OCD), it’s important to reflect on the multifaceted nature of this condition and its impact on individuals’ lives. OCD is more than just a series of compulsions or obsessions; it’s a complex disorder that can profoundly affect a person’s quality of life, relationships, work, ability to function daily, and overall physical well-being.
Throughout this course, we’ve explored the various manifestations of the disorder, diagnostic criteria, and the latest in treatment options, including pharmacological and therapeutic approaches. We’ve also explored the critical role that nurses and healthcare professionals play in supporting individuals with this condition.
Empathy, understanding, and ongoing education are essential in providing effective care for individuals with OCD. As nurses, we are often on the front lines witnessing the challenges that these individuals face. Therefore, it is our responsibility to not only offer the necessary medical support but also to advocate for our patients, ensuring they have access to the resources and support systems needed to manage their condition.
References + Disclaimer
- Brock H, Hany M. Obsessive-Compulsive Disorder. [Updated 2023 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553162/
- Carmi, L., Brakoulias, V., Arush, O.B. et al. A prospective clinical cohort-based study of the prevalence of OCD, obsessive compulsive and related disorders, and tics in families of patients with OCD. BMC Psychiatry 22, 190 (2022). https://doi.org/10.1186/s12888-022-03807-4
- Diagnostic and statistical manual of mental disorders : DSM-IV-TR. (Fourth edition, text revision.). (2000). American Psychiatric Association.
- Fanelli, D., Weller, G., & Liu, H. (2021). New Serotonin-Norepinephrine Reuptake Inhibitors and Their Anesthetic and Analgesic Considerations. Neurology international, 13(4), 497–509. https://doi.org/10.3390/neurolint13040049
- Fineberg, Naomi., & Robbins, T. W. (2021). The neurobiology and treatment of OCD : accelerating progress. Springer. https://doi.org/10.1007/978-3-030-75393-1
- Frota Lisbôa Pereira de Souza, A.M. (2021). Electroencephalographic Correlates of Obsessive-Compulsive Disorder. In: Fineberg, N.A., Robbins, T.W. (eds) The Neurobiology and Treatment of OCD: Accelerating Progress. Current Topics in Behavioral Neurosciences, vol 49. Springer, Cham. https://doi.org/10.1007/7854_2020_200
- Grünblatt, E. (2021). Genetics of OCD and Related Disorders; Searching for Shared Factors. In: Fineberg, N.A., Robbins, T.W. (eds) The Neurobiology and Treatment of OCD: Accelerating Progress. Current Topics in Behavioral Neurosciences, vol 49. Springer, Cham. https://doi.org/10.1007/7854_2020_194
- International OCD Foundation. Medications for OCD. Retrieved from https://iocdf.org/about-ocd/treatment/meds/
- Jalal, B., Chamberlain, S. R., & Sahakian, B. J. (2023). Obsessive-compulsive disorder: Etiology, neuropathology, and cognitive dysfunction. Brain and behavior, 13(6), e3000. https://doi.org/10.1002/brb3.3000
- Stein, D. J., Costa, D. L. C., Lochner, C., Miguel, E. C., Reddy, Y. C. J., Shavitt, R. G., van den Heuvel, O. A., & Simpson, H. B. (2019). Obsessive-compulsive disorder. Nature reviews. Disease primers, 5(1), 52. https://doi.org/10.1038/s41572-019-0102-3
- Vaghi MM. Neurocognitive Endophenotypes of OCD. Curr Top Behav Neurosci. 2021;49:97-124. doi: 10.1007/7854_2020_197. PMID: 33751501.
- Vallerand, A. H., & Sanoski, C. A. (2023). Davis’s drug guide for nurses (Eighteenth edition.). Philadelphia, PA. F. A. Davis Company. ISBN-10: 1-7196-4640-6. eISBN-10: 1-7196-4811-5.
- Van Niekerk, J. (2018). A clinician’s guide to treating OCD : the most effective CBT approaches for obsessive-compulsive disorder. New Harbinger Publications, Inc.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
