Course
Osteoporosis Management
Course Highlights
- In this Osteoporosis Management course, we will learn about the pathophysiology and epidemiology of osteoporosis and its impact on public health.
- You’ll also learn effective screening and diagnostic techniques for assessing bone mineral density and fracture risk.
- You’ll leave this course with a broader understanding of various non-pharmacological and pharmacological treatment options, considering cost-effectiveness and patient-specific factors.
About
Contact Hours Awarded: 2
Course By:
R.E. Hengsterman MSN, RN
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
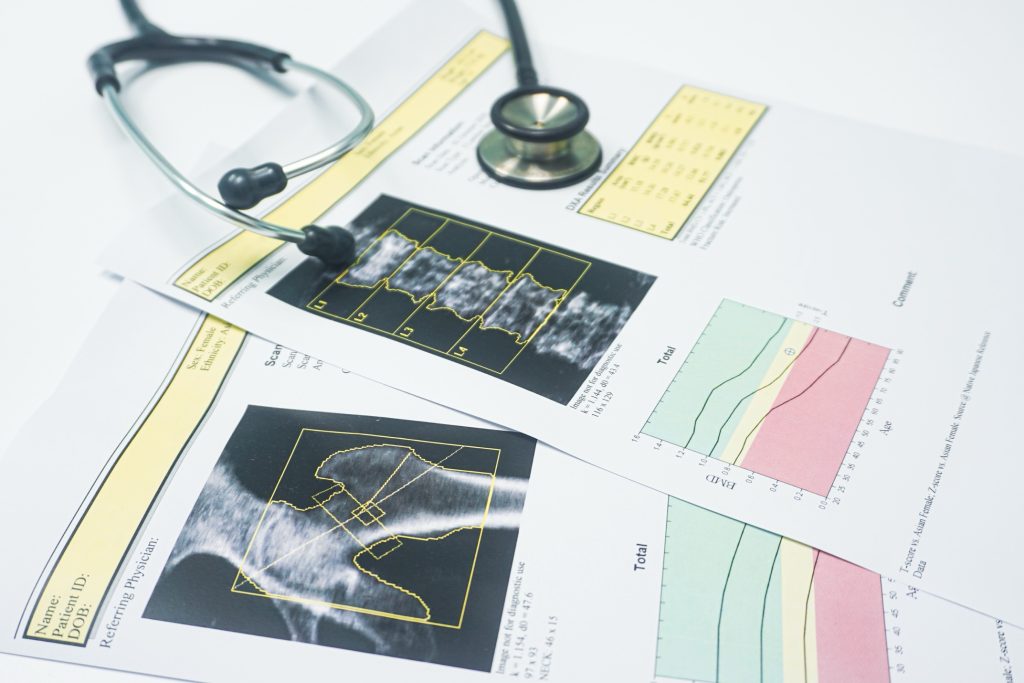
In the United States, 10 million individuals have osteoporosis, a disorder characterized by decreased bone density and weakened bone structure, increasing the risk of fractures [1]. Osteoporotic fractures can lead to pain, disability, the likelihood of nursing home admission, elevated health care costs, and mortality [2]. Diagnosis of osteoporosis focuses on bone mineral density assessment using dual-energy X-ray absorptiometry [3].
Treatment options include exercise, bisphosphonates, receptor activators of nuclear factor kappa-B ligand inhibitors, estrogen modulators, parathyroid hormone analogs, and calcitonin [4]. Additional therapies involve agents like cathepsin K inhibitors and monoclonal antibodies targeting sclerostin [5].
Although organizations have developed osteoporosis management guidelines, no single approach has universal endorsement, making economic evaluations valuable for decision-makers [1][9]. Cost-effectiveness research highlights oral bisphosphonates such as alendronate and risedronate as economical choices for women with low bone mineral density and no prior fractures [6]. The role of denosumab (Prolia) remains debated; it shows cost-effectiveness over risedronate and ibandronate and efficacy comparable to generic alendronate but at a higher cost [1] [7]. For older men, denosumab is also cost-effective compared to bisphosphonates and teriparatide (Forteo) [1][8].
Osteoporosis is a disease process that lowers bone mineral density and compromises bone strength, increasing fracture risk [1][9]. Often asymptomatic until a fracture occurs, it affects bones like the hip, spine, humerus, pelvis, or wrist, often resulting in hospitalization [1][9].
Epidemiology
Experts predict that the prevalence of osteoporosis in the United States will rise from 10 million to over 14 million individuals by 2020 [1][10]. Over 50% of postmenopausal white women will experience an osteoporotic fracture, and about 33% of senior women who suffer a hip fracture will return to independent living [9][11]. In white men, the risk of an osteoporotic fracture is 20%; however, the one-year mortality rate after a hip fracture is twice as high in men as in women [9][11]. Black males and females have a lower incidence of osteoporosis compared to white individuals, but those diagnosed face similar fracture risks [11]. As the American population ages, experts expect the number of osteoporotic fractures to triple [9].
By 2025, U.S. fracture treatment costs may exceed $25 billion per year, managing an estimated three million fractures [11]. Effective osteoporosis management improves the quality of life and reduces healthcare system demands by decreasing medical visits, hospital stays, and nursing home admissions.
Advancements in osteoporosis therapy arise from a deeper understanding of bone biology and the mechanisms of the disease. This includes the continued examination of osteoporosis pathophysiology, causes, screening and diagnosis methods, professional guidelines, nonpharmacologic strategies, pharmacologic treatments, and associated cost-effectiveness.

Self-Quiz
Ask Yourself...
- Considering that osteoporosis often remains asymptomatic until a fracture occurs, what preventive measures could be most effective in identifying and managing osteoporosis in high-risk populations before fractures happen?
- With various osteoporosis treatments available, including bisphosphonates, denosumab, and parathyroid hormone analogs, what factors should guide providers in selecting a cost-effective therapy for older adults with low bone density?
Case Study: Osteoporosis in a Postmenopausal Woman
- Name: Maria Rodriguez
- Age: 68 years
- Gender: Female
- Ethnicity: Hispanic
- Occupation: Retired schoolteacher
- Medical History: Hypertension (controlled with medication), menopause at age 50
- Family History: Mother had a hip fracture at age 72
- Lifestyle Factors: Non-smoker, moderate alcohol consumption (one glass of wine per day), low physical activity, diet low in calcium and vitamin D
Presentation: Maria visits her primary care physician after experiencing persistent lower back pain following a minor fall at home. She reports that the pain has been gradually increasing over the past few weeks. There is no history of major trauma.
Clinical Examination:
- Height: 160 cm (Prior notation 163 cm)
- Weight: 60 kg
- BMI: 23.4 kg/m²
- Blood pressure: 130/80 mmHg
- Physical exam reveals tenderness over the lumbar spine.
Diagnostic Workup:
- Dual-Energy X-Ray Absorptiometry (DXA):
- T-score at lumbar spine: -2.7
- T-score at femoral neck: -2.5
- Laboratory Tests:
- Serum calcium: Normal
- Vitamin D levels: Low
- Renal function tests: Creatinine clearance at 40 mL/min
Assessment: Maria has osteoporosis based on her T-scores being below -2.5 at the lumbar spine and femoral neck. The decrease in height suggests possible vertebral fractures. Her low vitamin D levels and inadequate calcium intake are contributing factors. The family history of hip fracture increases her risk.
Management Plan:
- Non-Pharmacological Interventions:
- Dietary Modifications:
- Increase intake of calcium-rich foods such as dairy products, leafy greens, and fortified foods.
- Vitamin D supplementation of 800 IU per day as recommended for individuals over 70.
- Lifestyle Changes:
- Initiate a weight-bearing and muscle-strengthening exercise program.
- Implement fall prevention strategies at home.
- Limit alcohol consumption to reduce further risk.
- Dietary Modifications:
- Pharmacological Treatment:
- Bisphosphonate Therapy:
- Medication: Oral Alendronate 70 mg once per week.
- Rationale: Alendronate is effective in increasing bone mineral density and reducing fracture risk in postmenopausal women [12].
- Renal Function Consideration: With a creatinine clearance of 40 mL/min, alendronate is appropriate because guidelines recommend it for patients with creatinine clearance ≥35 mL/min [14].
- Bisphosphonate Therapy:
- Monitoring:
- Schedule a follow-up DXA scan in one to two years to assess BMD changes.
- Monitor serum calcium and vitamin D levels.
Follow-Up: At her six-month follow-up, Maria reports improved back pain and adherence to her medication regimen. She has incorporated daily walks and light resistance exercises into her routine. Laboratory tests indicate that vitamin D levels have returned to normal, and no new fractures have occurred.

Self-Quiz
Ask Yourself...
- Given Maria’s family history of osteoporosis and recent lifestyle changes, how might further modifications to her exercise and diet impact her bone density and fracture risk over the long term?
- Considering Maria’s creatinine clearance level and current pharmacological treatment, what monitoring strategies could help her physician assess the effectiveness and safety of her ongoing osteoporosis management plan?
Pathophysiology
Human bone architecture provides structure, protects organs, and stores minerals such as calcium and phosphorus necessary for development and strength. Bone mass accumulates until about age 30, after which it declines [15]. Genetics determine peak bone mass, but factors like diet, exercise, diseases, or medications can affect bone density [15][16].
Bone remodeling involves osteoclasts breaking down bone and osteoblasts forming bone [17]. This balance maintains strength and supports repair. When resorption exceeds formation, bone loss occurs, as seen in osteoporosis. Estrogen and testosterone reduce bone breakdown [17]. Signaling molecules like RANKL, produced by osteoblasts, activate osteoclasts by binding to RANK receptors, promoting resorption. Cathepsin K (CatK), a protease from osteoclasts, degrades matrix and minerals [18]. Parathyroid hormone (PTH) influences growth by promoting osteoblast activity through the regulation of calcium [18][19].

Self-Quiz
Ask Yourself...
- How might hormonal changes, such as decreased estrogen and testosterone levels, disrupt the balance between osteoclast and osteoblast activity, leading to conditions like osteoporosis?
- In what ways do signaling molecules like RANKL and enzymes like Cathepsin K contribute to bone remodeling, and how might targeting these pathways help prevent excessive bone loss?
Primary Osteoporosis
Osteoporosis emerges with aging and changes in sex hormones. Aging leads to deterioration of trabeculae, while reductions in estrogen after menopause accelerate bone loss [17] [20]. In men, increased levels of sex-hormone–binding globulin reduce testosterone and estrogen, contributing to a decline in bone mineral density (BMD) [21].

Self-Quiz
Ask Yourself...
- How do age-related changes in hormone levels, such as decreased estrogen in women and reduced testosterone in men influence bone density and the risk of developing osteoporosis?
Secondary Osteoporosis
Secondary osteoporosis arises from diseases or medications. Conditions affecting osteoporosis disrupt calcium, vitamin D, or sex hormone balance [17]. For example, Cushing’s syndrome promotes bone loss due to glucocorticoids [22]. Inflammatory diseases like rheumatoid arthritis require glucocorticoid therapy, which is associated with secondary osteoporosis [22]. Glucocorticoids are medications linked to drug-induced osteoporosis, with BMD declining within three to six months of therapy [22]. The American College of Rheumatology (ACR) provides guidelines for the prevention and treatment of glucocorticoid-induced osteoporosis (GIO) [23].
Gender differences influence the causes of secondary osteoporosis. In men, alcohol intake, glucocorticoid use, and hypogonadism are contributors [22]. Men undergoing androgen-deprivation therapy (ADT) for prostate cancer face increased risk, with fracture rates higher among those treated with ADT compared to untreated men. In women, 32.4% of osteoporosis cases stem from secondary causes, including hypercalciuria, calcium malabsorption, hyperparathyroidism, vitamin D deficiency, hyperthyroidism, and Cushing’s disease [24]. Disorders of calcium metabolism and hyperparathyroidism account for a majority of these secondary causes [18][19][24].

Self-Quiz
Ask Yourself...
- How might glucocorticoid therapy, used to manage inflammatory conditions like rheumatoid arthritis, contribute to secondary osteoporosis, and what are the potential prevention strategies?
- What role do gender-specific risk factors, such as androgen deprivation therapy in men and calcium malabsorption in women, play in the development of secondary osteoporosis?
- How do disorders of calcium metabolism and hormone imbalances, such as hyperparathyroidism and vitamin D deficiency, influence bone density and fracture risk in individuals with secondary osteoporosis?
Screening and Diagnosis of Osteoporosis
Osteoporosis screening guidelines differ among organizations. Most recommend bone mineral density (BMD) screening for adults over 50 with a history of fracture [25]. The U.S. Preventive Services Task Force advises screening for women aged 65 and older, and for younger women with a fracture risk equal to or greater than that of a 65-year-old woman without additional risk factors [26]. The Endocrine Society recommends screening for men aged 70 and above and for men aged 50 to 69 with risk factors for osteoporosis [27].
Diagnosing osteoporosis relies on BMD measurements at the hip and spine using dual-energy x-ray absorptiometry (DXA) or identifying hip or vertebral fractures [28]. T-scores from BMD measurements interpret bone density results and correlate with fracture risk; lower BMD or more negative T-scores indicate higher fracture risk.
Randomized clinical trials provide limited evidence on the optimal frequency of BMD monitoring during treatment [1][29]. The National Osteoporosis Foundation recommends BMD assessment one to two years after starting treatment and every two years thereafter. Other studies suggest testing intervals of at least four years [1]. The North American Menopause Society suggests postponing repeated BMD testing for two to five years in untreated postmenopausal women and delaying testing until one to two years after treatment initiation in women undergoing therapy [1].

Self-Quiz
Ask Yourself...
- How might different screening guidelines for osteoporosis across organizations affect early detection and treatment, particularly for individuals with risk factors under the age of 65?
- Given the limited evidence on the optimal frequency of BMD monitoring, what factors should clinicians consider when deciding how often to assess bone mineral density in patients receiving osteoporosis treatment?
- How do T-score result from DXA scans inform the risk of fractures, and why might organizations vary in their recommendations for follow-up testing intervals?
Non-Pharmacological Management of Osteoporosis
Osteoporosis management involves intake of calcium and vitamin D, participation in weight-bearing exercises, smoking cessation, moderation of alcohol and caffeine consumption, and implementation of fall prevention strategies [1].
The Institute of Medicine (IOM) recommends capping dietary calcium intake at 1,000 mg per day for men aged 50 to 70, and at 1,200 mg per day for women aged 51 and older, as well as men over 71 [30]. Research links calcium intake with kidney stone risk; it is important to distinguish between dietary calcium and supplements and increase dietary calcium intake rather than rely on supplements to meet calcium needs. Calcium from supplements in substantial amounts may elevate kidney stone risk, whereas dietary calcium may offer protection [31].

Self-Quiz
Ask Yourself...
- How could the distinction between dietary calcium and calcium supplements impact the management of osteoporosis and kidney stone risk, and what considerations might guide an individual’s choice between these sources?
- What role do lifestyle changes, such as weight-bearing exercises and smoking cessation, play in strengthening bone health, and how might these non-pharmacological approaches affect long-term outcomes for individuals with osteoporosis?
Pharmacological Treatment
Pharmacological therapy for osteoporosis aims to prevent fractures and includes two types (such as bisphosphonates, estrogen agonists/antagonists, estrogens, calcitonin, and denosumab) and anabolic agents (such as teriparatide) [1][4]. Antiresorptive medications reduce bone resorption, whereas anabolic medications increase bone formation more than resorption [32]. Not all osteoporosis treatments have FDA approval for postmenopausal osteoporosis, osteoporosis in men, or glucocorticoid-induced osteoporosis [1][4].
Pharmacological options for patients at risk of fractures include alendronate, risedronate, zoledronic acid, and denosumab [1][4]. For patients who cannot tolerate oral therapies, alternatives include teriparatide, denosumab, or zoledronic acid [1][4]. Treatment duration for postmenopausal osteoporosis extends to five years [33]. Bisphosphonates serve as therapy for men with osteoporosis.
Several medications hold FDA approval for different osteoporosis-related indications. Alendronate (Fosamax) treats and prevents postmenopausal osteoporosis (PMO), manages osteoporosis in men, and both treat and prevent glucocorticoid-induced osteoporosis (GIO) [4][34]. Alendronate with cholecalciferol (Fosamax Plus D) treats postmenopausal osteoporosis (PMO) [1]. Risedronate immediate release (Actonel) treats and prevents postmenopausal osteoporosis (PMO), manages osteoporosis in men, and both treat and prevent glucocorticoid-induced osteoporosis (GIO) [1][4].
Zoledronic acid (Reclast) holds approvals identical to those of risedronate [35]. Denosumab (Prolia) treats postmenopausal osteoporosis (PMO) and osteoporosis in men [1]. Raloxifene (Evista) treats and prevents postmenopausal osteoporosis (PMO) [1][36]. Teriparatide (Forteo) treats postmenopausal osteoporosis and osteoporosis in men with high fracture risk [37]. Abaloparatide (Tymlos) treats postmenopausal osteoporosis (PMO) [38].

Self-Quiz
Ask Yourself...
- How do antiresorptive and anabolic medications differ in their approach to managing osteoporosis, and what factors might influence a healthcare provider’s choice between these types of treatments?
- Given the variety of FDA-approved osteoporosis medications with specific indications, how might a clinician decide on the most appropriate treatment for a patient with postmenopausal osteoporosis or glucocorticoid-induced osteoporosis?
Treatment Initiation Criteria
Pharmacological treatment initiation depends on factors like gender, fracture risk level, and other risk indicators, such as existing health conditions or medication regimens.
The American Association of Clinical Endocrinologists (AACE) guidelines suggest initiating treatment for [39]:
- Individuals with osteopenia or low bone mass and a history of fragility fractures in the hip or spine.
- Individuals with a T-score of -2.5 or lower at the lumbar spine, femoral neck, total hip, or 33% radius, regardless of fracture history.
- Individuals with a T-score between -1.0 and -2.5 if their FRAX 10-year probability of a major osteoporotic fracture is above 20% or a hip fracture probability above 3%.
The National Osteoporosis Foundation (NOF) and the Endocrine Society provide criteria for diagnosis and treatment, aligning with AACE standards.


Self-Quiz
Ask Yourself...
- How might clinicians weigh factors like T-scores, fracture history, and FRAX scores when deciding whether to initiate pharmacological treatment for osteoporosis in patients with varying levels of fracture risk?
Antiresorptive Agents: Bisphosphonates
Medical organizations recommend bisphosphonates (excluding ibandronate) as an option for preventing and treating osteoporosis in postmenopausal women, men, and cases of glucocorticoid-induced osteoporosis (GIO) [1][4]. Bisphosphonates bind to the bone mineral matrix, impeding osteoclast-mediated bone resorption, which reduces bone turnover and increases bone mass [40].
Alendronate, risedronate, and intravenous zoledronic acid have demonstrated effectiveness in improving bone mineral density and reducing fracture risk in men with osteoporosis, postmenopausal women, and GIO patients [1]. Ibandronate reduces vertebral fractures but lacks consideration as a first-line option due to limited data on its impact on hip and nonvertebral fracture risk [41].
Bisphosphonates are available in different formulations. Manufacturers offer alendronate, risedronate, and ibandronate as oral tablets. Alendronate also comes in effervescent tablets (Binosto) and as a vitamin D combination (Fosamax Plus D). Risedronate is available in immediate-release and delayed-release forms; studies indicate the delayed-release version is comparable to the immediate-release formulation. Zoledronic acid and ibandronate are available as intravenous injections. Dosing recommendations vary based on use for prevention or treatment, and many formulations support extended dosing intervals, such as weekly or monthly, due to the agents’ long half-lives.
Because the kidneys excrete bisphosphonates, patients with renal impairment risk toxicity from drug accumulation. Clinicians avoid bisphosphonates in patients with creatinine clearances below established limits [42].

Self-Quiz
Ask Yourself...
- How do the varying formulations and dosing intervals of bisphosphonates, like alendronate and zoledronic acid, offer advantages for different patient populations managing osteoporosis?
- Given the renal excretion of bisphosphonates, what considerations should clinicians consider when prescribing these medications to patients with compromised kidney function?
Conclusion
Osteoporosis is a widespread condition characterized by reduced bone mineral density and increased fracture risk, affecting millions of individuals, and imposing significant health care costs [1][4]. Effective management of osteoporosis is crucial to improving patient quality of life and reducing the burden on healthcare systems. Diagnosis primarily relies on bone mineral density assessments using dual-energy X-ray absorptiometry, with screening guidelines recommending evaluations for at-risk populations [3].
Management strategies encompass both nonpharmacological approaches—such as adequate calcium and vitamin D intake, exercise, and fall prevention—and pharmacological treatments. Leading medical organizations endorse bisphosphonates like alendronate, risedronate, and zoledronic acid for their efficacy in increasing bone mass and reducing fracture risk in postmenopausal women, men, and patients with glucocorticoid-induced osteoporosis [1][4]. Proper dosing and consideration of renal function are essential when prescribing these medications.
Continued advancements in understanding bone biology have led to the development of various therapeutic agents targeting various aspects of bone remodeling. While guidelines for osteoporosis management vary, economic evaluations highlight the cost-effectiveness of certain treatments, aiding clinicians, and policymakers in decision-making. Overall, a comprehensive approach combining prevention, accurate diagnosis, and effective treatment is vital in addressing the growing challenge of osteoporosis.
References + Disclaimer
References
- Tu, K. N., Lie, J. D., Wan, C. K. V., Cameron, M., Austel, A. G., Nguyen, J. K., Van, K., & Hyun, D. (2018, February 1). Osteoporosis: A Review of Treatment options. https://pmc.ncbi.nlm.nih.gov/articles/PMC5768298/
- Khan, A. A., Slart, R. H. J. A., Ali, D. S., Bock, O., Carey, J. J., Camacho, P., Engelke, K., Erba, P. A., Harvey, N. C., Lems, W. F., Morgan, S., Moseley, K. F., O’Brien, C., Probyn, L., Punda, M., Richmond, B., Schousboe, J. T., Shuhart, C., Ward, K. A., & Lewiecki, E. M. (2024). Osteoporotic fractures: Diagnosis, evaluation, and significance from the International Working Group on DXA Best Practices. Mayo Clinic Proceedings, 99(7), 1127–1141. https://doi.org/10.1016/j.mayocp.2024.01.011
- Krugh, M., & Langaker, M. D. (2024, May 20). Dual-Energy X-Ray Absorptiometry. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519042/
- Zaheer, S., & LeBoff, M. S. (2022, December 27). Osteoporosis: Prevention and treatment. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK279073/
- Tonk, C. H., Shoushrah, S. H., Babczyk, P., Khaldi-Hansen, B. E., Schulze, M., Herten, M., & Tobiasch, E. (2022). Therapeutic Treatments for Osteoporosis—Which Combination of Pills Is the Best among the Bad? International Journal of Molecular Sciences, 23(3), 1393. https://doi.org/10.3390/ijms23031393
- Fleurence, R. L., Iglesias, C. P., & Johnson, J. M. (2007). The cost effectiveness of bisphosphonates for the prevention and treatment of osteoporosis. PharmacoEconomics, 25(11), 913–933. https://doi.org/10.2165/00019053-200725110-00003
- Qaseem, A., Hicks, L. A., Etxeandia-Ikobaltzeta, I., Shamliyan, T., & Cooney, T. G. (2023). Pharmacologic treatment of primary osteoporosis or low bone mass to prevent fractures in adults: a living clinical guideline from the American College of Physicians. Annals of Internal Medicine, 176(2), 224–238. https://doi.org/10.7326/m22-1034
- Yuan, F., Peng, W., Yang, C., & Zheng, J. (2019). Teriparatide versus bisphosphonates for treatment of postmenopausal osteoporosis: A meta-analysis. International Journal of Surgery, 66, 1–11. https://doi.org/10.1016/j.ijsu.2019.03.004
- Porter, J. L., & Varacallo, M. (2023, August 4). Osteoporosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK441901/
- Curry, S. J., Krist, A. H., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., Doubeni, C. A., Epling, J. W., Kemper, A. R., Kubik, M., Landefeld, C. S., Mangione, C. M., Phipps, M. G., Pignone, M., Silverstein, M., Simon, M. A., Tseng, C., & Wong, J. B. (2018). Screening for osteoporosis to prevent fractures. JAMA, 319(24), 2521. https://doi.org/10.1001/jama.2018.7498
- Bao, Y., Xu, Y., Li, Z., & Wu, Q. (2023). Racial and ethnic difference in the risk of fractures in the United States: a systematic review and meta-analysis. Scientific Reports, 13(1). https://doi.org/10.1038/s41598-023-32776-1
- Singer, A., McClung, M. R., Tran, O., Morrow, C. D., Goldstein, S., Kagan, R., McDermott, M., & Yehoshua, A. (2023). Treatment rates and healthcare costs of patients with fragility fractures by site of care: a real-world data analysis. Archives of Osteoporosis, 18(1). https://doi.org/10.1007/s11657-023-01229-7
- Parker, L. R. W., & Preuss, C. V. (2023, November 12). Alendronate. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK526073/
- Naganathar, N., Yau, W.-., Mok, Z. H., Tan, Z. Y. F., & Chew, S. T. H. (2021). Alendronate use in older patients with reduced renal function: challenges and opportunities in clinical practice. Osteoporosis International, 32(10), 1981–1988. https://doi.org/10.1007/s00198-021-05907-5
- Bone mass throughout the life span. Bone accumulates rapidly in… (2019). ResearchGate. https://www.researchgate.net/figure/Bone-mass-throughout-the-life-span-Bone-accumulates-rapidly-in-childhood-and-grows-at_fig1_331976843
- Hereford, T., Kellish, A., Samora, J. B., & Nichols, L. R. (2024). Understanding the importance of peak bone mass. Journal of the Pediatric Orthopaedic Society of North America, 7, 100031. https://doi.org/10.1016/j.jposna.2024.100031
- Rowe, P., Koller, A., & Sharma, S. (2023, March 17). Physiology, bone remodeling. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK499863/
- Cheng, C., Chen, L., & Chen, K. (2022). Osteoporosis due to hormone imbalance: An overview of the effects of estrogen deficiency and glucocorticoid overuse on bone turnover. International Journal of Molecular Sciences, 23(3), 1376. https://doi.org/10.3390/ijms23031376
- Khan, M., Jose, A., & Sharma, S. (2022, October 29). Physiology, parathyroid hormone. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK499940/
- Charde, S. H., Joshi, A., & Raut, J. (2023). A Comprehensive review on Postmenopausal osteoporosis in women. Cureus. https://doi.org/10.7759/cureus.48582
- Yang, F., Yang, D., Zhou, Y., & Wu, J. (2021). Associations of Sex Hormone-binding Globulin with Bone Mineral Density Among US Adults, NHANES 2013–2016. International Journal of General Medicine, Volume 14, 7707–7717. https://doi.org/10.2147/ijgm.s329992
- Ilias, I., Milionis, C., & Zoumakis, E. (2022, March 19). An Overview of Glucocorticoid-Induced Osteoporosis. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK278968/
- Glucocorticoid-Induced Osteoporosis Clinical Practice Guidelines. (2024). https://rheumatology.org/glucocorticoid-induced-osteoporosis-guideline
- Ganesan, K., Jandu, J. S., Anastasopoulou, C., Ahsun, S., & Roane, D. (2023, March 2). Secondary osteoporosis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470166/
- Viswanathan, M., Reddy, S., Berkman, N., Cullen, K., Middleton, J. C., Nicholson, W. K., & Kahwati, L. C. (n.d.). Table 1, Recommendations about screening and treatment of osteoporosis from various professional and health organizations – Screening to prevent osteoporotic fractures: An evidence review for the U.S. Preventive Services Task Force – NCBI bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532080/table/table1/
- Osteoporosis to prevent fractures: screening. (2018, June 26). https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/osteoporosis-screening
- Bello, M. O., Sombra, L. R. S., Anastasopoulou, C., & Garla, V. V. (2023, July 10). Osteoporosis in males. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538531/
- Nissinen, T., Suoranta, S., Saavalainen, T., Sund, R., Hurskainen, O., Rikkonen, T., Kröger, H., Lähivaara, T., & Väänänen, S. P. (2021). Detecting pathological features and predicting fracture risk from dual-energy X-ray absorptiometry images using deep learning. Bone Reports, 14, 101070. https://doi.org/10.1016/j.bonr.2021.101070
- Bone densitometry. (2021, August 8). Johns Hopkins Medicine. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/bone-densitometry
- Office of Dietary Supplements – calcium. (2024). https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
- Chmiel, J. A., Stuivenberg, G. A., Al, K. F., Akouris, P. P., Razvi, H., Burton, J. P., & Bjazevic, J. (2023). Vitamins as regulators of calcium-containing kidney stones — new perspectives on the role of the gut microbiome. Nature Reviews Urology, 20(10), 615–637. https://doi.org/10.1038/s41585-023-00768-5
- Haas, A. V., & LeBoff, M. S. (2018). Osteoanabolic agents for osteoporosis. Journal of the Endocrine Society, 2(8), 922–932. https://doi.org/10.1210/js.2018-00118
- Lam, H. C., Thomas, C. M., & Shaver, J. M. (2018, April 1). Duration of bisphosphonate therapy. AAFP. https://www.aafp.org/pubs/afp/issues/2018/0401/od1.html
- Parker, L. R. W., & Preuss, C. V. (2023, November 12). Alendronate. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK526073/
- Greear, E. L., Patel, P., & Bankole, A. (2024, February 21). Zoledronate. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK585053/
- Rodriguez, B. S. Q., & Correa, R. (2023, February 13). Raloxifene. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK544233/
- Vall, H., Patel, P., & Parmar, M. (2024, February 29). Teriparatide. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK559248/
- Akel, M., Patel, P., & Parmar, M. (2024, January 29). Abaloparatide. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK587447/
- Camacho, P. M., Petak, S. M., Binkley, N., Diab, D. L., Eldeiry, L. S., Farooki, A., Harris, S. T., Hurley, D. L., Kelly, J., Lewiecki, E. M., Pessah-Pollack, R., McClung, M., Wimalawansa, S. J., & Watts, N. B. (2020). American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis—2020 update. Endocrine Practice, 26, 1–46. https://doi.org/10.4158/gl-2020-0524suppl
- Sun, S., Tao, J., Sedghizadeh, P. P., Cherian, P., Junka, A. F., Sodagar, E., Xing, L., Boeckman, R. K., Srinivasan, V., Yao, Z., Boyce, B. F., Lipe, B., Neighbors, J. D., Russell, R. G. G., McKenna, C. E., & Ebetino, F. H. (2020). Bisphosphonates for delivering drugs to bone. British Journal of Pharmacology, 178(9), 2008–2025. https://doi.org/10.1111/bph.15251
- Alves, C., Mendes, D., Penedones, A., Oliveira, T., Donato, A., & Batel-Marques, F. (2023). The effectiveness of ibandronate in reducing the risk of nonvertebral fractures in women with osteoporosis: systematic review and meta-analysis of observational studies. International Journal of Clinical Pharmacy, 46(2), 357–367. https://doi.org/10.1007/s11096-023-01666-x
- Robinson, D. E., Ali, M. S., Pallares, N., Tebé, C., Elhussein, L., Abrahamsen, B., Arden, N. K., Ben-Shlomo, Y., Caskey, F. J., Cooper, C., Dedman, D., Delmestri, A., Judge, A., Pérez-Sáez, M. J., Pascual, J., Nogues, X., Diez-Perez, A., Strauss, V. Y., Javaid, M. K., & Prieto-Alhambra, D. (2020). Safety of oral bisphosphonates in Moderate‐to‐Severe Chronic Kidney Disease: A Binational cohort analysis. Journal of Bone and Mineral Research, 36(5), 820–832. https://doi.org/10.1002/jbmr.4235
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
