Pediatric Osteosarcoma
Contact Hours: 2
Author(s):
Sarah Schulze, MSN, APRN, CPNP
Course Highlights
- In this Pediatric Osteosarcoma course, we will learn about the risks of osteosarcoma across various demographics like race, age, and gender.
- You’ll also learn the normal process of ossification and identify where tumor production takes place.
- You’ll leave this course with a broader understanding of the distinctive appearance of osteosarcoma tumors.
Introduction
Osteosarcoma is a rare but very serious malignant bone growth diagnosis most commonly seen in children. This aggressive cancer has a high incidence of metastasis or disease recurrence and requires prompt and multimodal treatment to achieve the greatest outcomes and highest 5-year survival rate. Nurses may encounter clients in many different settings at various phases of the diagnostic, treatment, and recovery process and a baseline knowledge about this serious disorder is necessary for any clinician working with children. This course aims to provide a general overview of osteosarcoma, what causes it, how it presents, as well as common diagnostic and treatment options and their impact on recovery.
Epidemiology
Prevalence
The National Cancer Institute (NCI) reports that osteosarcoma accounts for about 5% of childhood tumors, impacting around 5.4 per 1 million people ages 0 -19 (or approximately 440 children) each year (12). More than half of these tumors occur in the long bones of the leg.
The prognosis for osteosarcoma has improved drastically in recent years, with a 5-year survival rate of around 71% in 2020, compared to only 40% in 1975. It is a somewhat aggressive cancer with the rate of metastasis within 6 months of initial diagnosis at about 15-20% and the rate of recurrent disease within 2 years at 30-40% (12).
For children with recurrent disease, the 5-year survival rate is only about 20%. A solitary tumor where complete resection can be achieved offers the best prognosis. Dual treatment with surgery and chemotherapy also significantly improves outcomes compared to surgical resections (9, 12).

Distribution
Important distinctions exist between demographics, like age, sex, and race, for the incidence of osteosarcoma. When considering race, Black children ages 0-9 years are at the highest risk with an incidence rate (IR) of 2.3%, compared to the general rate of 1.9% amongst all races. Asian and Pacific Islander children are the next most at risk, with an IR of 2%, followed by Hispanic children at 1.8%, then White children at 1.7%, and finally American Indian and Alaskan Native at just 1%.
The risk increases, and the ranking changes slightly when considering clients in the adolescent and young adult ages of 10-24. Black and Hispanic clients are most at risk, with an IR of 7.9%. White clients are next, with an IR of 6.8%, followed by Asian and Pacific Islander (6%) and American Indian and Alaskan Native (5.5%) (9).
The five-year survival rate is higher among females (63.9%) than male peers (56.5%) and was fairly similar across racial groups. Within the disease of osteosarcoma, parosteal disease has the highest survival rate at 91.9%, and Paget’s disease has the lowest survival rate at just 29.9% at 5 years (9).
Age of diagnosis also impacts the 5-year survival rate, with children diagnosed in the 0-9 years group having an overall survival rate of 71.8% and children/young adults diagnosed in the 10-24 years group dropping to 65.9% (9).
|
Race/Ethnicity |
Incidence Rate |
|
Ages 0-9 years |
|
|
White |
1.7% |
|
Black |
2.3% |
|
American Indian/Alaskan Native |
1.0% |
|
Asian or Pacific Islander |
2% |
|
Hispanic |
1.8% |
|
All races |
1.9% |
|
10-24 years |
|
| White |
6.8% |
| Black |
7.9% |
| American Indian/Alaskan Native |
5.5% |
| Asian or Pacific Islander |
6.0% |
| Hispanic |
7.9% |
| All races |
7.2% |
Table 1. Incidence of osteosarcoma by race/ethnicity and age (9)
Risk Factors
Given the above information, risk factors include (1):
- Adolescents and young adults age
- Male gender
- Black and Hispanic race and ethnicity
- Children who are tall for their age or are experiencing rapid growth
- History of other bone conditions
- People who have had radiation therapy for another condition
Ask yourself...
- What biological or social factors might contribute to the difference in 5-year survival rate between males and females?
- How might the higher incidence rates of osteosarcoma in Black and Hispanic children influence the focus of public health initiatives or research into prevention and treatment?
- Given the increased risk of osteosarcoma during periods of rapid growth, how could early detection strategies be adjusted to monitor children who are taller than average or going through growth spurts?
Pathophysiology
To properly understand osteosarcoma, it is important first to understand normal bone formation, known as osteogenesis or ossification. This process begins with mesenchymal stem cells that differentiate into several different types of specialized cells, including connective tissues, blood, and lymphatic tissue. Mesenchymal cells are found in various tissues and, notably for this course, the bone marrow.
Some mesenchymal cells differentiate into osteoblasts, which cluster together to create ossification centers. The osteoblasts secrete a calcium-binding material called osteoid that traps them together in progressive layers, forming hard bones. This process occurs during embryonic formation, periods of bone growth, and fracture healing. Further differentiation, depending on the type and size of bone and the inclusion of blood supply, occurs and is beyond the scope of this course (8).
Osteosarcoma, or osteogenic sarcoma, is a cancerous tumor originating in the bone. This malignant growth originates in the mesenchymal stem cells, which are beginning to differentiate into osteoblasts. The exact point in bone formation when the tumor begins is unclear (7, 11, 13).
These tumors most commonly occur at the site of bone growth, the metaphysis, and often during periods of rapid growth, which is why the peak incidence is during adolescence and young adulthood. Long bones, including the tibia, humerus, and femur, are frequently affected. They occur around the knee in 60% of cases, the hip in 15%, and less commonly in the shoulder and jaw (11, 13).
Osteosarcoma tumors are hard and irregularly shaped, made up of needle-like protrusions of calcified bone that infiltrate surrounding tissues. The bone spicules, known as Codman triangles, are arranged at right angles and give the tumor a “moth-eaten” or “fir-tree” appearance on x-ray. On a microscopic level, the tumor comprises osteoid cells occurring in various sizes (11, 13).
Osteosarcoma can be subclassified into two categories: primary and secondary. Primary osteosarcoma originates in bone cells without the presence of other cancers or bone diseases. Secondary osteosarcoma also originates in bone cells but occurs whenever a skeletal disease or another cancer is already present. Primary osteosarcoma is much more common in children and has a better prognosis than secondary osteosarcoma. In the adult population, secondary osteosarcoma is much more common and has a poorer prognosis (11). 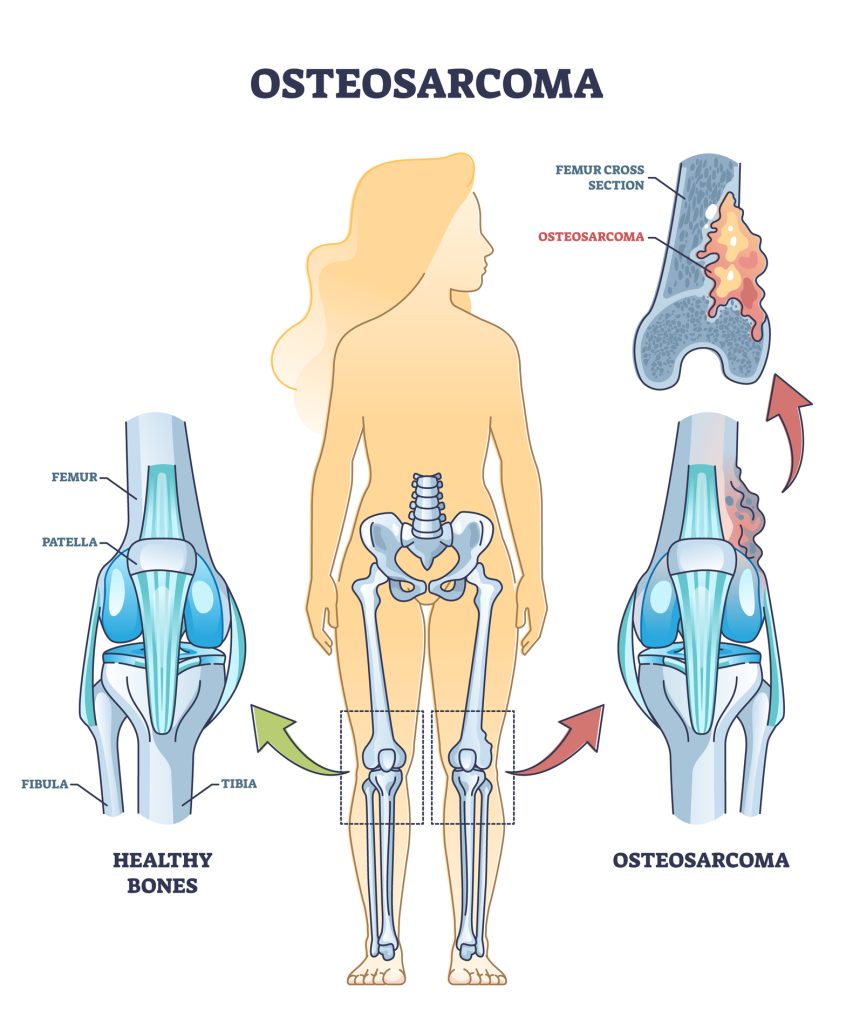
Ask yourself...
- Why do you think osteosarcoma tumors tend to form during periods of rapid growth?
- What might explain the difference in prognosis between primary and secondary osteosarcoma, and how does pre-existing conditions or diseases influence this?
- How might the irregular structure of osteosarcoma tumors, such as the formation of Codman triangles, affect the surrounding tissues and overall bone function?
- If osteosarcoma primarily affects long bones in adolescents and young adults, how might this affect our approach to screening or early detection in these populations compared to older adults?
Presentation
The most common first symptom of osteosarcoma is pain at the tumor site. For children and adolescents, this is frequently around the knee. The pain may not be constant at first and may present more often at night, coming and going throughout the day. It may worsen with activity or result in a limp. Depending on where the tumor is located, a hard, palpable lump may be present. Swelling may also occur as a tumor progresses.
Limb pain, bruising, swelling, and bumps are common complaints in children and teenagers, so symptoms may not seem too out of the ordinary or prompt further investigation from parents at first. There is often a history of several months of pain that is worsening or won’t go away, a decrease in activity, limping, or even movement restriction by the time children are brought in for evaluation (3).
Ask yourself...
- Why might parents and caregivers initially dismiss the early signs of osteosarcoma, and what could be done to increase awareness or prompt earlier investigation?
- What other differentials might you consider for a child presenting with leg pain?
- How do you think this delay in seeking evaluation might impact the overall prognosis?
Diagnosis and Staging
With limb pain or lumps that cannot be definitively diagnosed as another cause, osteosarcoma should be considered, and imaging is warranted. Various imaging techniques, including X-ray, MRI, and CT scans, can be used to locate and diagnose osteosarcoma. A plain X-ray is often the first type of imaging done and, while less sensitive than MRI, can offer a clear view of a mass on bone.
An MRI is often done after an x-ray or as initial imaging when a bone tumor is suspected. It offers a more detailed picture of the mass, helping to differentiate it from other causes. A CT scan is less likely to be used for bone mass because it is less detailed and specific than an MRI, and additional imaging may be needed anyway (5).
Once a bone tumor is located on imaging, osteosarcoma is highly suspected, but a biopsy is needed to confirm the diagnosis. This can be done through two methods, a core needle biopsy, or a surgical biopsy.
A core needle biopsy may be done under varying levels of anesthesia, from local to sedation or general anesthesia, depending on the age and developmental maturity of the child. This technique uses a hollow needle guided into the tumor either by feel or with the assistance of CT-guided radiology. A tumor sample is then taken and studied to confirm the presence of osteocytes.
Alternatively, a surgical (or open) biopsy is done under general anesthesia, and the area in question is opened up for the surgeon to visualize the tumor and excise it. Ideally, all of the tumors can be excised at once during the surgical biopsy, and additional surgery may not be needed (5).
The samples are then sent to pathology for grading. Tumors may first be categorized as localized or metastasized.
Most osteosarcomas appear localized to the bone without spreading to other tissues upon initial diagnosis. There is always a risk of microscopic metastasis, however, which is why chemotherapy is typically recommended even if the tumor is localized. Localized masses may be sub-categorized as resectable, where all visible tumors can be removed during the biopsy, or non-resectable, where the entire tumor is unable to be removed (2).
Metastasized tumors are much less common but are those that have already spread to other parts of the body, commonly the lung, brain, or other bones. The prognosis for metastatic osteosarcoma is less than that of localized disease (2).
For a more detailed staging, the Musculoskeletal Tumor Society staging system (MSTS), or Enneking system, may be used. This staging system comprises 3 details: grade, tumor, and metastasis (GTM).
Tumor grade (G) is based on how a tumor looks under the microscope and predicts its likelihood to grow and spread. G1 tumors look more consistent with normal cells and are slower to grow and spread, while G2 tumors are more abnormal in appearance and grow and spread aggressively (2).
The extent of the tumor (T) is either T1, where the tumor has remained contained to the bone, or T2, where the tumor has extended into nearby structures. T1 tumors are referred to as intracompartmental, and T2 tumors are considered extra compartmental.
And finally, metastasis (M) indicates whether a tumor has not spread to other organs (M0) or has spread (M1) (2).
These grading values are combined to provide a final staging from I to III. (2).
|
Stage |
Grade |
Tumor |
Metastasis |
|
IA |
G1 |
T1 |
M0 |
|
IB |
G1 |
T2 |
M0 |
|
IIA |
G2 |
T1 |
M0 |
|
IIB |
G2 |
T2 |
M0 |
|
III |
G1 or 2 |
T1 or 2 |
M1 |
Table 2. Diagnosing and Staging Osteosarcoma (2)
Ask yourself...
- Why is a biopsy necessary to confirm the diagnosis of osteosarcoma even after imaging suggests the presence of a tumor?
- Why might chemotherapy still be recommended for localized osteosarcoma, even when there is no clear evidence of metastasis?
- What factors determine whether a tumor is resectable or non-resectable, and how does this affect the treatment plan for osteosarcoma?
- What are the implications of a tumor being classified as T2 and extracompartmental?
- Why might a surgical biopsy be preferred to a core needle biopsy?
Treatment
Treatment for osteosarcoma often involves a combination of surgery, chemotherapy, and radiation. The exact treatment plan will vary based on the location and staging of the tumor and the client’s unique circumstances. The risks and benefits of each treatment modality should be explained thoroughly to clients prior to undergoing treatment.
Surgery
Surgery to biopsy and remove the tumor is part of the treatment for nearly every case of osteosarcoma. Ideally, the entire tumor can be excised with wide margins during the biopsy to prevent the need for future surgeries. The complexity and extent of the surgery depend heavily on tumor size and location. For small, well-located, and low-grade tumors, sometimes surgical resection may be the only treatment needed. More often than not, however, a combination of treatments is used.
Every effort is made to salvage the limb for tumors on the arms and legs; however, the involvement of surrounding tendons, ligaments, and blood vessels makes surgery and reconstruction very complex. A bone graft (either from the donor or another site on the client) or a prosthetic replacement must be fitted to the area to provide structural support to the limb.
For tumors that are very large and have spread into the surrounding nerves and blood vessels, amputation is sometimes the best option. The remainder of the limb is usually reconstructed and fitted for a prosthetic.
Tumors located on smaller bones such as the hip, jaw, spine, and skull are still more complicated. Chemotherapy and radiation are sometimes used prior to surgery to try and shrink the size of the tumor for easier removal.
The pelvis can sometimes be reconstructed with other bones in the body or donor grafts, but larger tumors may require removing an entire section of the pelvis and the leg on the affected side. Tumors on the skull or spine may be unable to be removed completely, increasing the risk of recurrent disease or metastasis.
If the osteosarcoma has metastasized to other organs or tissues, additional surgeries to remove those tumors are also needed. The most common site that osteosarcoma spreads to is the lungs. Removing tumors from one or both lungs is extremely complex, and the need for such surgery decreases a client’s overall prognosis (6).
Chemotherapy and Other Medications
Most people with osteosarcoma receive intravenous chemotherapy in addition to surgery because of the high risk of metastasis and secondary occurrence of tumors. Even when osteosarcoma does not appear to have spread, the recurrence rate remains high when only treated with surgery, therefore concomitant chemotherapy is now fairly routine.
Chemotherapy for osteosarcoma is given both prior to surgery to shrink the tumor (called neoadjuvant chemo) for around 10 weeks and then also after surgery (called adjuvant chemotherapy) for several months to a year. Chemo is typically given with 2 or more drugs given in combination and at high doses.
Common chemotherapy drugs for osteosarcoma include:
- Methotrexate
- Doxorubicin
- Cisplatin
- Ifosfamide
- Cyclophosphamide
- Etoposide
- Gemcitabine
Chemotherapy drugs often include unpleasant side effects but, in general, are better tolerated by children than adults. Common side effects include:
- Nausea and vomiting
- Loss of appetite
- Diarrhea
- Hair loss
- Mouth sores
- Increased risk of infection (reduced white blood cells)
- Bleeding or bruising (reduced platelets)
- Fatigue and shortness of breath (reduced red blood cells)
Some additional drugs are being studied for osteosarcoma and work differently than chemotherapy. Medications like regorafenib, sorafenib, and cabozantinib target specific tumor cells and reduce their ability to create a blood supply. These medications are not yet FDA-approved but may offer an additional treatment modality in the future (6).
Radiation
In general, osteosarcoma cells are not easily killed by high-energy radiation rays, but this treatment method is still sometimes used in combination with others, particularly when a complete tumor resection is not possible. Tumors occurring in bones of the face, pelvis, or spine often require radiation because they are difficult to remove completely with surgery.
Radiation may kill remaining cancer cells or slow tumor growth and manage symptoms when surgery is not possible. There are two main ways radiation is used for osteosarcoma: external beam radiation and radioactive drugs.
External beam radiation is the most commonly used type for osteosarcoma and involves a specific focus of high-energy beams on the tumor. The radiation dose and positioning of the beams are carefully executed using a detailed MRI of the tumor location.
The treatment takes only a few minutes and is administered five days a week for several weeks. Children do need to lie very still during the treatment, so younger children or those who are highly anxious may be given sedation to ensure they do not move.
Skin side effects like mild sunburn or hair loss may occur shortly after radiation treatment. Children may also experience nausea, diarrhea, and urinary issues if the radiation is given to the pelvis or abdomen.
Radiopharmaceuticals, which are less commonly used, are also available and include drugs like samarium-153-EDTMP and radium-233. These medications are given intravenously and can slow tumor growth or treat pain. Radiopharmaceuticals are often used when osteosarcoma has spread to many different bones, making surgery and external beam radiation difficult to use effectively (6).

Ask yourself...
- What factors might determine whether limb-salvage surgery or amputation is the best option for a client?
- Why is achieving wide margins in tumor resection critical for osteosarcoma surgery?
- What supportive measures would you include in the treatment plan for a child with osteosarcoma?
- How do you think the timing of chemotherapy (neoadjuvant vs adjuvant) impacts the treatment goals?
- Since osteosarcoma cells are not easily destroyed by radiation, why is radiation still considered in certain cases?
- How does the choice between external beam radiation and radiopharmaceuticals depend on the tumor’s characteristics?
Outcomes and Complications
Outcomes and survival rates depend heavily on the initial tumor grading as well as the size and location of the tumor. The American Cancer Society uses information from the Surveillance, Epidemiology, and End Results (SEER) database to group cancers into stages and outline their 5-year survival rate.
For osteosarcoma, SEER data suggests clients with tumors that are localized and respond well to surgery and chemotherapy have a 5-year survival rate of 76%. Those with regional tumors that have spread into nearby structures but are still able to be removed through careful surgery or limb amputation have a 5-year survival rate of 64%. Distant or invasive cancer at the time of diagnosis has only a 24% 5-year survival rate.
Children have better survival rates than adults, and females have a better prognosis than males. Tumors located on the arms and legs, as opposed to other sites like the hip or jaw, also have a better prognosis, though this is primarily due to the increased success of complete surgical resection. Overall, this is an aggressive cancer, and early detection is necessary to improve response to treatment and survival odds (4).
Regardless of ultimate 5-year survival, many potential complications can occur during and as a result of treatment and need to be considered.
Complications following surgery, particularly where a limb is salvaged, include infection and loose or broken prosthetics. Additional surgeries and wound care may be needed, and sometimes amputation ends up occurring anyway. Clients are at a high risk of excessive bleeding, blood clots, infection, and pain following a complex orthopedic surgery like osteosarcoma resection.
Extensive rehabilitation is needed after limb-sparing and amputation surgeries, with children learning to live with limb differences and use a prosthetic. Children who are still growing may need repeated surgeries to replace outgrown internal prosthetics or further reconstruct the affected limb to a growing body.
Children typically learn to walk with a prosthetic about 3-6 months following an amputation. Relearning to walk can take up to a year with a limb-salvaging surgery. Refunding and healing nerves and connective tissue is much more complex than amputation.
Self-esteem may be impacted, especially for adolescent clients, and it is important to monitor for comorbid depression and anxiety disorders due to changes in the appearance and function of limbs following surgery.
Chemotherapy significantly increases a child’s risk of infection due to damage to bone marrow and reduced white blood cell count. Children are already at a high risk of infection due to attendance at school with large numbers of children and the generally reduced hygiene practices, particularly for young children in preschool or elementary school. Infections acquired while receiving chemotherapy tend to be much more serious and can result in hospitalization for respiratory distress and dehydration.
Potential complications of radiation include slowed bone growth, which can lead to uneven growth and adult height for tumors located on long bones. Radiation to the jaw may negatively impact the function of the salivary glands and teeth.
Nerve damage, headaches, and problems with cognition may occur after radiation to the spine or skull. Pelvic radiation can cause problems with urination, bowel movements, and reproduction. Radiation also increases the risk of additional cancers forming, as radiation can be carcinogenic at high doses.
Radiopharmaceuticals are less commonly used but may damage bone marrow and lower blood counts, increasing the risk of infection and bleeding (6).
Ask yourself...
- Why do you think tumors on the arms and legs have a better prognosis than those in other locations?
- What factors might explain why children generally have better survival rates than adults with osteosarcoma?
- How would you help parents of a child with osteosarcoma weigh the risks of potential treatment methods when considering such an aggressive cancer?
- How could the potential need for multiple surgeries to replace outgrown prosthetics impact a child’s physical and emotional development?
- Given the increased risk of serious infections during chemotherapy, what strategies might help reduce infection risk for children attending school while undergoing treatment?
- What are some of the unique risks associated with radiation therapy in children with osteosarcoma, and how might these risks shape decisions regarding its use and dosage?
Nursing Care
Nursing care for osteosarcoma will vary depending on where the nurse encounters the client during the diagnosis and treatment process.
Early Recognition
For nurses in an outpatient or emergency setting, prompt recognition of symptoms and need for further evaluation is necessary. Nurses should never assume limb pain is a benign complaint in children and should take a careful history to gather details that may help confirm or refute suspicion of osteosarcoma.
Knowledge of risk factors and typical signs and symptoms is foundational for nurses who see children in primary care or urgent/emergent settings. For advanced-practice nurses, ordering imaging is a simple and cost-effective diagnostic that can be used when evaluating a child with limb pain (10).
Diagnostic Process
Nurses may care for clients during imaging procedures, such as MRIs and lesion biopsy procedures. Children are often given general anesthesia for procedures that may be painful or require them to lie still for extended periods of time. Clients and their parents may be anxious and nervous and have many questions.
Knowledge of developmental levels and how to properly communicate with and comfort clients at various ages is integral to nursing care. Knowledge of the process from start to finish is important so nurses can confidently answer questions and reduce family anxieties (10).
Active Treatment
Nurses in an inpatient setting are more likely to encounter clients with osteosarcoma immediately before and after surgery. At this time, clients often require high-acuity care. They must be monitored closely for signs of infection, blood clotting or excessive bleeding, and proper wound healing.
Parents and children may be anxious or have a lot of questions. Developmentally appropriate knowledge about communicating with and caring for children of all ages is important. Pain management is also important at this time, and frequent assessment and administration of ordered medications are necessary.
Clients should be monitored for fever, redness, or excessive swelling at the operative site, wound drainage amount and color, and signs of hemodynamic instability, such as hypotension and tachycardia.
Nurses working in oncology may also encounter clients throughout their chemotherapy treatment. Knowledge of common side effects and interventions to help cope with those side effects is necessary. Nurses may administer medications like ondansetron to help with side effects like nausea or may help with calming, deep breaths, or guided imagery for anxious clients before accessing a port.
Education about the risk of infection should also be provided, and nurses can help parents navigate challenges like school attendance, family gatherings, and what is acceptable versus what should be avoided (10).
Recovery and Rehabilitation
Nurses may encounter young clients in various settings during the recovery and rehabilitation. Roles may include wound care, coordinating physical therapy and prosthetic fittings, and continued screenings and follow-up care to assess for disease recurrence. Nurses also play a pivotal role in assessing young clients’ mental health throughout the process.
This can be a very trying time for children, teens, and their families, and frequent assessment for self-esteem changes, coping with frequent medical procedures and difficult side effects, and development of anxiety and depression is very important. Nurses can refer clients and families to support services, work through and educate them about coping mechanisms, and coordinate referrals for mental health treatment as needed (10).
Ask yourself...
- How might a nurse’s awareness of osteosarcoma risk factors and symptoms influence the initial assessment of a child with limb pain?
- Understanding the child’s developmental level and emotional needs could enhance the nurse’s communication ability during diagnostic procedures. What specific strategies might be useful?
- What risks of complications should the nurse be on the lookout for immediately following surgery for excision of an osteosarcoma lesion?
- How can nurses help foster positive self-esteem and resilience during long-term rehabilitation?
Case Study

Consider the following case study for Ethan Smith, a 7-year-old male client presenting to the pediatrician with complaints of right leg pain.
Ethan presents to the pediatrician with his mother, who reports he has had mild pain around the knee off and on for about two weeks. Ethan has recently started playing soccer, and his parents believed the leg pain was due to that. However, over time, the pain has become more frequent, particularly at night, and in the last two days, it has become nearly constant, and Ethan is limping. He has been avoiding activity during PE and recess at school and did not want to go to soccer practice yesterday.
Upon exam, Ethan is afebrile, alert-oriented, and otherwise healthy. His right leg does have tenderness around the distal femur, but there are no signs of edema, erythema, or bruising. Given the history, the pediatrician orders an X-ray, which shows a suspicious mass in a Codman’s triangle formation to the distal femur, raising concern for a potential bone tumor. A referral to an orthopedic oncologist and additional imaging are ordered.
Ethan undergoes an MRI with the orthopedic doctor, which shows a tumor extending into the surrounding soft tissue. It is determined that Ethan needs a biopsy of the lesion to determine the nature of the tumor. A core needle biopsy is performed under general anesthesia and confirms the presence of osteosarcoma, a malignant bone tumor.
A plan is made for treatment, including surgery and chemotherapy. Ethan and his parents are counseled on the different outcomes and recovery for limb-salvaging versus amputation surgery. Given Ethan’s young age, the likely need for repeated surgeries for internal prosthetic replacement as he grows, and the extended recovery time for limb-salvaging surgery, Ethan opts for an above-the-knee amputation.
Ethan also needs chemotherapy to minimize the risk of metastasis and disease recurrence. He begins with neoadjuvant chemotherapy for 10 weeks before his surgery to attempt to shrink the tumor. During this time, he wears a mask to school to reduce his risk of acquiring an infection from classmates. Ethan experiences common side effects, including nausea, fatigue, and hair loss.
After the neoadjuvant chemotherapy is complete, Ethan undergoes surgery for the removal of the tumor. Despite the neoadjuvant chemotherapy, the lesion involvement in surrounding tissues is extensive enough that his surgeon believes a limb-salvaging surgery would not have been possible.
Ethan begins a period of intensive rehabilitation in the hospital, including wound care and physical therapy. After about 2 weeks, he can be discharged home to continue rehab on an outpatient basis. He also begins adjuvant chemotherapy at this time to reduce the risk of recurrence. This continues for 6 months.
Around 6 months after his surgery, Ethan concludes his chemotherapy regimen and is learning to walk well with a prosthetic leg. He is resilient but has found the rigor of his treatment, as well as extended absences from school, to be challenging. About 3 months after his surgery, he begins play therapy with a counselor and is monitored closely for anxiety or depressive disorders.
Ethan’s early diagnosis and prompt treatment were positive factors in his favor. Given the regional scoring of his initial tumor, his 5-year survival rate is around 64%. He will need close and frequent follow-ups to monitor for recurrent disease.
Ethan’s experience with osteosarcoma highlights the importance of early detection and a multidisciplinary approach to treatment, especially for young clients facing aggressive cancers. His case illuminates the complexities of managing a diagnosis of osteosarcoma, from balancing effective treatments with minimizing physical and emotional impact to long-term care considerations.
Ask yourself...
- What factors might have led to Ethan’s delayed diagnosis, and how could awareness of early symptoms in pediatric clients help improve early detection?
- How might his diagnosis have been further delayed? What steps at the initial pediatrician appointment helped prevent further delay
- Why might Ethan and his family have chosen amputation over limb-salvaging surgery? What advantages or challenges could this decision present for his recovery and long-term mobility?
- How might Ethan’s experience with chemotherapy and its side effects influence his view of medical treatment? What supportive strategies could be used to help him cope with these challenges?
- How could Ethan’s extended absences from school and ongoing medical care impact his social and academic development?
- How does regular follow-up influence long-term outcomes and quality of life for pediatric clients like Ethan?
Conclusion
Osteosarcoma is a rare but aggressive and serious cancer. Even with prompt and multimodal treatment, the risk of recurrence and metastasis is high, and the 5-year survival rate varies greatly. Early recognition and treatment targeting the initial lesion and potential spread improves outcomes and prognosis. Clinicians should have a baseline understanding of osteosarcoma, how it forms, and what the initial signs and symptoms could be.
Limb pain is a common pediatric complaint and is unlikely to be osteosarcoma. Still, the risk of delayed detection makes this an important consideration for even the simplest of limb pain complaints. Understanding what to look for and how quickly diagnosis and the treatment process need to be initiated can help nurses act quickly and efficiently and improve outcomes for pediatric clients.
References + Disclaimer
- American Cancer Society. (2020a). Osteosarcoma risk factors. ACS. https://www.cancer.org/cancer/types/osteosarcoma/causes-risks-prevention/risk-factors.html#:~:text=The%20risk%20of%20osteosarcoma%20is,radiation%20both%20increase%20this%20risk.
- American Cancer Society. (2020b). Osteosarcoma staging. ACS. https://www.cancer.org/cancer/types/osteosarcoma/detection-diagnosis-staging/staging.html
- American Cancer Society. (2020c). Signs and symptoms of osteosarcoma. ACS. https://www.cancer.org/cancer/types/osteosarcoma/detection-diagnosis-staging/signs-and-symptoms.html
- American Cancer Society. (2020d). Survival rates for osteosarcoma. ACS. https://www.cancer.org/cancer/types/osteosarcoma/detection-diagnosis-staging/survival-rates.html
- American Cancer Society. (2020e). Tests for osteosarcoma. ACS. https://www.cancer.org/cancer/types/osteosarcoma/detection-diagnosis-staging/how-diagnosed.html
- American Cancer Society. (2020f). Treating osteosarcoma. ACS. https://www.cancer.org/cancer/types/osteosarcoma/treating.html
- American Cancer Society. (2020g). What is osteosarcoma. ACS. https://www.cancer.org/cancer/types/osteosarcoma/about/what-is-osteosarcoma.html
- Breeland, G., Sinkler, M.A., Menezes, R.G. (2024). Embryology, bone ossification. StatPearls. Treasure Island (FL): StatPearls Publishing; https://www.ncbi.nlm.nih.gov/books/NBK539718/
- Cole, S., Gianferante, D.M., Zhu, B., Mirabello, L. (2022) Osteosarcoma: a surveillance, epidemiology, and end results program-based analysis from 1975 to 2017. Cancer. https://doi.org/10.1002/cncr.34163
- Gao, Q., Yao, Y., & Xu, Q. (2022). Guideline and Implementation of Osteosarcoma Nursing Care for Children and Adolescents. Applied bionics and biomechanics, 2022, 2021162. https://doi.org/10.1155/2022/2021162 (Retraction published Appl Bionics Biomech. 2023:9852824. doi: 10.1155/2023/9852824)
- Menendez, N., Epelman, M., Shao, L., Douglas, D., Meyers, A. B. (2022). Pediatric osteosarcoma: pearls and pitfalls. Seminars in Ultrasound, CT and MRI. Volume 43, Issue 1, Pages 97-114, ISSN 0887-2171. https://doi.org/10.1053/j.sult.2021.05.010.
- National Cancer Institute. (2024). Osteosarcoma and Undifferentiated Pleomorphic Sarcoma of Bone Treatment. NCI. https://www.cancer.gov/types/bone/hp/osteosarcoma-treatment-pdq#:~:text=Osteosarcoma%20occurs%20predominantly%20in%20adolescents,the%20historical%20experience%20before%201970.
- Petriceks, A.H., Salmi, D. Educational case: primary steosarcoma. (2019) Acad Pathol.10;6:2374289518820337. doi: 10.1177/2374289518820337. PMID: 30733995; PMCID: PMC6343432.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
