Course
Peripheral Artery Disease
Course Highlights
- In this Peripheral Artery Disease course, we will learn about the definition and epidemiology of peripheral artery disease.
- You’ll also learn the signs, symptoms, and physical exam findings of peripheral artery disease.
- You’ll leave this course with a broader understanding of various treatments, patient education, and complications of peripheral artery disease.
About
Contact Hours Awarded: 2
Course By:
Amanda Marten MSN, FNP-C
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Peripheral artery disease (PAD) is a medical condition affecting arterial perfusion that typically affects older adults. It’s important for nurses and healthcare providers to understand the signs and symptoms of PAD, common physical exam findings, diagnostic tests, treatment, and potential complications. This course aims to equip learners with knowledge related to PAD by reviewing its definition, epidemiology, pathophysiology, and etiology. This course also describes the signs, symptoms, physical assessment findings, diagnostic tests, and treatment. Lastly, it reviews potential complications along with patient education.
Definitions
Peripheral artery disease (PAD) is a type of peripheral vascular disease. Also referred to as peripheral arterial disease, PAD is a circulation issue that causes decreased blood flow through the arteries due to a narrowing or blockage in the lower or upper extremities. Most patients refer to this condition as “poor circulation” [6].
Intermittent claudication is another term frequently used when discussing PAD. Intermittent claudication is a symptom of PAD, where individuals experience leg pain when exercising or walking. It can occur anywhere in the leg, like the thigh, feet, or calf [6].
Critical or acute limb ischemia is a severe peripheral artery disease where the risk of amputation is likely [4].

Self-Quiz
Ask Yourself...
- What is the definition of peripheral artery disease?
- What is intermittent claudication?
- What is critical or acute limb ischemia?
Pathophysiology
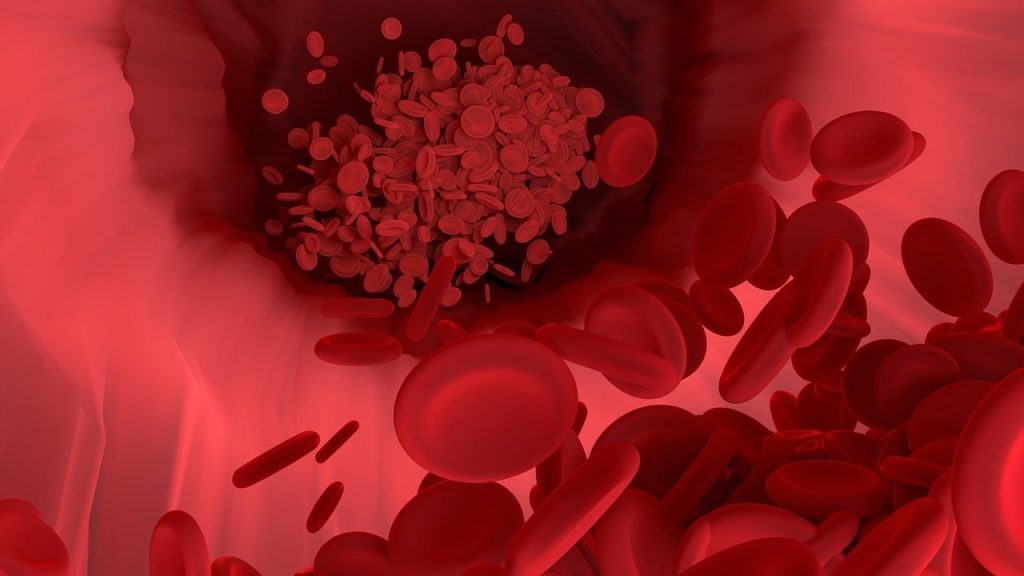
People with PAD have reduced arterial circulation or perfusion to their upper or lower extremities. The most common contributing factor to PAD is the development of atherosclerotic plaques (fatty buildup) that cause the arteries to narrow or become blocked. As the plaques build up along the arteries, blood flow is eventually restricted since the blood vessels cannot dilate any further. As blood flow is restricted, some patients experience leg pain when exercising or walking, also called intermittent claudication. This is caused by the arteries’ inability to perfuse enough oxygen-rich blood to the muscles of the lower extremities, causing symptoms like leg pain and cramping. Oftentimes, to compensate, the blood flow shits to the smaller arteries. This is why sometimes patients will only experience pain when walking or exercising [6].
Other medical conditions, like vasculitis, thrombocytosis, antiphospholipid syndrome, and fibromuscular dysplasia, can also contribute to developing PAD [3]. Additional risk factors are discussed in the section below.
There are four subtypes of peripheral artery disease, including asymptomatic, chronic symptomatic, acute limb ischemia, and critical or limb-threatening ischemia. Asymptomatic PAD occurs when patients do not have symptoms of PAD but may have functional impairment. Chronic symptomatic PAD is the most common type of PAD, where patients will report exertional leg symptoms and claudication. Critical or limb-threatening ischemia is a severe form of PAD. This type often leads to limb amputation. Acute limb ischemia is also severe, but patients will have a sudden decrease in perfusion and have clinical symptoms like pain, pallor, pulselessness, paresthesia, or paralysis. Most often, acute limb ischemia is caused by an embolism or thrombosis [2].

Self-Quiz
Ask Yourself...
- What is the pathophysiology of PAD?
- Why do only some patients experience intermittent claudication?
- What are the four subtypes of PAD?
- What is the most common subtype of PAD?
Epidemiology and Risk Factors
It’s estimated that around 200 million people worldwide have peripheral arterial disease [6]. In the United States, it’s estimated that there are around 6.5 million people aged 40 and older who have PAD. This condition affects both men and women equally, but women are more likely to be asymptomatic [1, 3]. However, African Americans are at increased risk for PAD, and the Hispanic population is at increased risk compared to the non-Hispanic White population [1]. Moreover, it’s estimated that more than 1 in 20 American Indians and Alaska Natives have this condition [3].
The risk of developing PAD increases with age, where individuals 65 years and older are more likely to have PAD [3]. Additionally, patients with PAD have an increased risk of coronary artery disease and cerebrovascular disease, likely due to atherosclerosis. This increases the individual’s likelihood of heart attack and stroke, respectively [1].
There are several risk factors for developing peripheral artery disease, and the most common is atherosclerosis, which is a plaque buildup in the arteries. Other risk factors include high blood pressure, high cholesterol, and diabetes. Age is also a risk factor, but sources have conflicting ages. Some sources report age 60 and above, while others report age 65 and older [1, 3]. Smoking and exposure to secondhand smoke also increase patient risk. Patients with certain lifestyle habits, like an unhealthy diet or not exercising, also have a higher likelihood of developing PAD [3]. Furthermore, a family history of PAD, stroke, and heart disease are also risk factors. People who are obese, with a body mass index (BMI) greater than 30, and who have high levels of homocysteine are also more likely to develop PAD [6].
Clinical Signs and Symptoms
The signs and symptoms of peripheral artery disease vary per individual. Some patients are asymptomatic, while others have the hallmark sign of intermittent claudication. Intermittent claudication can vary per individual as well, where some patients report pain while others report leg fatigue, aching, or weakness. Thigh, calf, buttock, and foot pain may also occur. Those with more severe PAD may report symptoms, like leg pain or a burning sensation in their feet, at rest. Some patients also report leg swelling, leg weakness, or frequent sores or ulcers on their legs. They may also report cold or numb toes [1, 6].

Self-Quiz
Ask Yourself...
- What is the epidemiology of PAD in the United States?
- What are some risk factors of PAD?
- What are some signs and symptoms of PAD?
- What is the hallmark sign of PAD?
Physical Examination Findings
Physical exam findings of peripheral arterial disease also vary per individual. When inspecting the legs, they may appear smooth, dry, and shiny, with little to no hair or evidence of hair loss. They may also have a pale appearance (pallor) or even look cyanotic (blue and mottled), and muscle atrophy may be evident. Muscle atrophy is often noticeable in the calf muscles. Upon palpation, the lower extremities may feel cool. Patients can also report pain or tenderness to the touch. Sores, wounds, or ulcers may also be present [1, 6].
In addition, nurses and providers should assess the patient’s lower extremity perfusion and pulses. Perfusion is typically assessed by applying a pulse oximeter to each extremity and checking capillary refill. Depending on the severity of the disease, pulses may be weak or absent. All lower extremity pulses, including the femoral, popliteal, posterior tibial, and dorsalis pedis, should be palpated. Pulses may be diminished (1+), and for pulses that are nonpalpable, the nurse or provider should attempt to locate the pulse with a vascular or pulse-Doppler. Nurses and providers may also hear a bruit in the affected artery upon auscultation with a stethoscope. During the physical exam, the provider should also have the patient walk for several minutes to see if symptoms or exam findings are exacerbated [1, 6].
When examining patients with suspected or confirmed peripheral arterial disease, an easy way to recall PAD clinical features is with the “Five P’s.” These include pain, pallor, pulselessness, paralysis, and paresthesia. Paralysis and paresthesia are more suggestive of limb ischemia and should be treated immediately [5].
- Pain: report leg cramping or pain or intermittent claudication
- Pallor: pale or cyanotic skin appearance
- Pulselessness: weakened or absent extremity pulses
- Paralysis: muscle weakness or evidence of atrophy
- Paresthesia: decreased sensation or reports of numbness and tingling [5].


Self-Quiz
Ask Yourself...
- What are some physical exam findings of PAD?
- What intervention should be implemented if a pulse is nonpalpable?
- What are the “Five P’s” of PAD?
Diagnostic Tests
If either the nurse or healthcare provider suspects PAD, diagnostic tests are ordered to confirm the diagnosis. After the physical exam, the initial diagnostic test is to complete an ankle-brachial index (ABI), usually completed right at the bedside. An ABI helps objectively measure lower extremity perfusion by comparing the systolic blood pressure of the ankles to the systolic pressure of the arms. To complete this test, the patient lies flat, and a manual blood pressure cuff is placed on the ankle while listening to the pedal pulse with a vascular Doppler. The blood pressure cuff is then inflated until the pedal Doppler pulse is no longer audible. The pressure from the cuff is then slowly released and as the pedal Doppler pulse becomes audible again, the systolic blood pressure is recorded at this moment. This process is completed and recorded on all four extremities. For the upper extremities, the cuff is placed on the wrist, and the radial or ulnar pulse is used. After this is complete, the ABI is calculated by taking the highest of the two systolic pressure in the lower extremities divided by the highest systolic pressure in the upper extremities. An ABI less than 0.9 is indicative of PAD. For patients with an ABI less than 0.5, this indicates severe ischemic disease. ABI greater than 1.3 can mean arterial stiffening, most commonly seen in patients with kidney disease and diabetes [6].
A toe-brachial index may also be measured to diagnose patients with possible PAD, especially when their initial ABI is greater than 1.4 [5]. Additional workups may include a complete blood count (CBC) and basic or comprehensive metabolic panel (BMP or CMP) to evaluate kidney function, electrolytes, blood glucose, and other potential underlying causes. Bloodwork may also include inflammatory biomarkers, such as a C-reactive protein (CRP), D-dimer, homocysteine, and interleukin 6 [5, 6]. Assessing the patient’s cholesterol levels by ordering a lipid panel is also used to help diagnose PAD [3]. Ordering an electrocardiogram may also be helpful if heart disease or arrhythmias are suspected [6].
Vascular imaging and Doppler studies are also useful in determining the extent of the disease. These tests help evaluate blood flow velocities and assess for potential areas of occlusion. CT or MR angiography may also be needed, especially if a patient needs an angioplasty or vascular bypass surgery [5, 6].

Self-Quiz
Ask Yourself...
- What is the initial diagnostic test when PAD is suspected?
- What ABI measurement indicates PAD is likely?
- What additional diagnostic tests may be ordered to diagnose PAD?
Treatment and Education
Once the diagnosis of PAD is made with an ABI and other diagnostics, treatment should be promptly initiated. The two goals of treatment are to improve the patient’s ability to walk or exercise and lower their cardiovascular risk [6]. Providers should follow the current guidelines from whichever organization they predominately use (typically the American Heart Association or American College of Cardiology) [2]. Patients are usually prescribed medications to control symptoms and reduce their cardiovascular risk. Statins are prescribed to reduce the progression of atherosclerosis [5]. If the patient has hypertension or diabetes, medications are also prescribed to manage these conditions. For hypertension management, angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are recommended [5, 6]. For claudication symptoms, cilostazol is commonly used to promote vasodilation but takes several weeks to begin working. Pentoxifylline may also be prescribed for claudication, as it increases oxygen delivery [6]. Antiplatelet medications, like aspirin or clopidogrel, may also be given to aid blood flow and prevent clot formation, but they are dependent on patient risk factors. Additionally, exercise therapy is indicated, where patients walk several times a week for about 30 to 45 minutes. The goal is to reach 30 minutes of exercise at least 30 times per week [3].
Oftentimes, patients with asymptomatic PAD can be managed with medications and exercise programs [2]. However, if the patient is not already being followed by a cardiologist or vascular specialist, then a referral should be considered to help manage the patient’s PAD. Additionally, a referral to vascular surgery may be needed as sometimes treatment involves vascular surgery. One vascular procedure that may be needed is angioplasty, where a small balloon is inflated within the artery to flatten and sometimes help remove the plaque. Sometimes, a stent is also placed within the artery to prevent it from occluding again in the future. Another procedure is a vascular bypass, which is typically reserved for patients with severe PAD or where angioplasty is not likely to work. This procedure involves “bypassing” the area of occlusion with a piece of another blood vessel or artificial vein to create a new path for blood flow [3]. Additionally, a referral to wound care may be needed if the patient has wounds or ulcers on their extremities.
In addition, patient education is key to treatment and disease progression. Patients who smoke should be encouraged to quit and provided education and counseling for smoking cessation. Implementing healthy lifestyle choices is also important. Individuals should be encouraged to consume heart-healthy foods, follow a low-sodium diet, and incorporate many fruits, vegetables, and lean protein into their diet. Regular exercise is helpful in reducing weight and cholesterol levels and managing high blood pressure. Weight loss should be encouraged for patients who are overweight or obese. Furthermore, managing stress can improve physical and mental health [3]. Management and education regarding diabetes and blood glucose control are also essential, where referral to endocrinology is warranted [6]. Patients should also be instructed to avoid medications that can cause vasoconstriction, like certain migraine, and over-the-counter and recreational drugs (e.g., cocaine). Activities like cold exposure can also exacerbate symptoms [5].
Emergency management is necessary for patients with acute limb ischemia. If patients have acute signs of pain, pallor, pulselessness, paresthesia, paralysis, or poikilothermia, Signs of compartment syndrome may quickly develop, so these individuals require prompt treatment via revascularization or fasciotomy [2].

Self-Quiz
Ask Yourself...
- What is the treatment for chronic PAD?
- When might a referral to a vascular specialist be considered?
- What is exercise therapy?
Potential Complications
Assessing patients for potential complications of peripheral arterial disease is also necessary. Common complications, like ischemia and gangrene, exist. Due to a lack of blood flow, patients may develop lower limb infections or ulcers. If perfusion is lacking and ischemia is present, limb amputation may also be necessary. Since patients with PAD often have atherosclerosis, complications of this condition may also develop, like heart attack, stroke, or blood clots [6].
Clinical signs and symptoms of these complications will vary, so monitoring and frequent follow-up are needed. For ischemia and gangrene, the nurse and provider should monitor for signs of worsening perfusion, like a cyanotic or mottling appearance, diminished or nonpalpable pulses, and paresthesia or paralysis of the limbs. If the patient has wounds or ulcers of their extremities, daily wound care and looking for signs of not healing and infection are needed. The nurse or healthcare provider should look for additional clinical clues, like an elevated white blood cell count, poor glucose control, fever, or purulent discharge. If infection is suspected, a wound culture and antibiotics may be prescribed [3, 6].
Emerging Research
Over the past several years, there has been research regarding peripheral arterial disease and improving patient outcomes. Until more recently, exercise programs for PAD were not covered by most insurance companies. A study termed Claudication: Exercise Versus Endoluminal Revascularization (CLEVER) proved a supervised exercise training (SET) program for PAD was more effective at improving a patient’s treadmill walking than if controlled by medications or angioplasty alone. This has recently led to many insurance providers, along with the Centers for Medicare & Medicaid, reimbursing SET programs. For patients participating in home-based exercise training programs, high versus low-intensity walking is also being studied [4].
Additionally, researchers discovered that patients who smoke are twice as likely to develop peripheral artery disease. New devices to help improve blood flow are also being researched, such as an ultrasound device and inflatable cuffs, worn when individuals are resting or sleeping. For patients who’ve undergone surgery for revascularization, small implantable seniors are also being researched to assess oxygen levels of tissue in the extremities. Lifestyle modifications, genetics, and the impacts of social determinants of health are also being studied [4].


Self-Quiz
Ask Yourself...
- What are some potential complications of PAD?
- What are the clinical signs of ischemia or gangrene?
- What is some emerging research regarding PAD?
- What is CLEVER?
- What lifestyle modifications should be implemented for patients with PAD?
- Why is diabetes also an important factor to manage?
- What are the clinical signs of acute limb ischemia?
- How is acute limb ischemia typically treated?
- Why might muscle atrophy be an assessment finding in patients with PAD?
- How might a provider screen patients for PAD?
- Why might the risk of PAD increase with age?
Conclusion
Many people are impacted globally and in the United States by peripheral arterial disease. Therefore, nurses and healthcare providers must be diligent and able to recognize the signs and symptoms of this condition, along with the importance of prompt intervention. A thorough history, assessment of patient risk factors, and physical exam must be completed to help guide the possible diagnosis. If there is suspicion of PAD, an ABI helps to guide the initial diagnosis. Oftentimes, atherosclerosis is the predominant cause of this condition, so frequent screening, monitoring, and follow-up are key. Patient education should be provided regarding this condition, as well as prevention strategies and lifestyle modifications to avoid potential complications and future recurrence.
References + Disclaimer
- Centers for Disease Control and Prevention. (2024, May 14). About Peripheral Arterial Disease (PAD). Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/heart-disease/about/peripheral-arterial-disease.html
- Gornik et al. (2024, May 14). 2024 ACC/AHA/AACVPR/APMA/ABC/SCAI/SVM/SVN/SVS/SIR/VESS Guideline for the Management of Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. https://doi.org/10.1161/CIR.0000000000001251
- National Heart, Lung, and Blood Institute. (2022, March 24). Peripheral Artery Disease. National Institutes of Health. Retrieved from https://www.nhlbi.nih.gov/health/peripheral-artery-disease/causes
- National Heart, Lung, and Blood Institute. (2022, March 24). Peripheral Artery Disease (PAD) Research. National Institutes of Health. Retrieved from https://www.nhlbi.nih.gov/research/peripheral-artery-disease
- Stephens, E. (Updated 2022, May 24). Peripheral Vascular Disease Clinical Presentation. Medscape. Retrieved from https://emedicine.medscape.com/article/761556-clinical
- Zemaitis, M.R., Boll, J.M., & Dreyer, M.A. (Updated 2023, May 23). Peripheral Arterial Disease. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430745/
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
