Course
Placental Uses in Modern Medicine
Course Highlights
- In this Placental Uses in Modern Medicine course, we will learn about the purpose of the placenta.
- You’ll also learn the implications of placenta use in modern medicine.
- You’ll leave this course with a broader understanding of reasons why a patient would want to choose to perform certain actions regarding their placenta.
About
Contact Hours Awarded: 1
Course By:
Sadia A, MPH, MSN, WHNP-BC
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
When hearing the phrase placenta, what comes to mind? Whether you’re new to nursing or have been a nurse for many years, you have heard of the placenta at some point in your nursing studies or career. If you work in women’s health, reproductive health, or regenerative medicine, the role of placentas is crucial and lifesaving. As technology and modern medicine evolve, so does the role of the placenta for patients, communities, and medical advances. People are alive because of the role of the placenta in someone’s body, and more science is emerging regarding the pivotal role of placentas in medicine. The information in this course will serve as a valuable resource for nurses of all specialties and backgrounds interested in learning more about the role of the placenta in modern medicine.
Defining the Placenta
To begin with, the placenta is the only organ a human creates and then discards. The placenta is an organ created in the uterus during pregnancy to sustain the pregnancy, and it is only created during pregnancy. Each pregnancy will have its placenta, and multiple gestation pregnancies need to have at least one placenta. Specifically, the placenta grows in the uterus, can be up to the size of a large dinner plate, and is expelled out of the uterus after delivery of the fetus during the third stage of labor.
The placenta is the lifeline between the pregnant person and the fetus, as it is responsible for cushioning the fetus, passing nutrition to the fetus, and communicating with the pregnant parent. Most placentas are developed in the first three months of pregnancy and form their finalized location in the uterus during the second trimester. Sometimes, there are complications with the placenta, such as placenta accreta (where the placenta grows too deeply into the uterus) or placenta previa (where the placenta is covering the cervix). Most of the time, the placenta can grow along the uterine lining with no complications, which is important since a healthy, developing fetus needs a healthy placenta (1,2).
Presently, in several American birth centers and hospitals, after the birthing person gives birth to the fetus, the placenta is typically expelled within an hour, if not sooner. If the placenta is not delivered within an hour at the latest or if the placenta is delivered incomplete, this can cause severe complications for the birthing patient, such as retained placenta infection, uterine hemorrhage, pelvic cramping, uterine pain, systemic infection, and even death.
As much as placentas are important to sustaining the pregnancy, oftentimes, after delivery, the placenta is delivered intact and then disposed of via facility policy by the delivery team. However, an increasing number of patients are requesting to be discharged from the birthing facility with their placenta for cultural reasons, emotional concerns, and medical advances.


Self-Quiz
Ask Yourself...
- What are some ways nurses can learn more about placental uses in modern medicine?
- What are some ways you have seen the placenta be used in your healthcare setting?
Placenta Pathophysiology and Purpose
While the placenta is the lifeline between the birthing parent and the fetus, it has significant pathophysiological properties that need to be considered and understood. Historically, the placenta was seen as an organ that was to be delivered after the fetus and then discarded. Now, placenta pathology has revealed several important aspects of placenta pathophysiology.
For instance, the placenta serves as the exchange between the pregnant person and fetus, exchanging hormones, nutrients, gases, electrolytes, and fetal waste. In addition, the placenta uses the pregnant person’s fatty acids and glucose for healthy fetal growth. The placenta also serves to provide immunity to the fetus and is a highlight for maternal-fetal specialists to discuss with patients in patient care. Some conditions that can affect the placenta include pre-eclampsia, chronic stress, viral infections, blunt trauma, and more (1,2).
In particular, the human chorionic gonadotropin (hCG) hormone is created and released from the syncytiotrophoblast to stimulate luteal progesterone production to maintain the pregnancy. Without hCG production, the absence of progesterone would trigger menses, and the pregnancy and placenta would be able to sustain itself. After the tenth week of pregnancy, hCG levels stabilize, and the placenta takes responsibility to produce progesterone. Because of this, blood tests to determine hCG levels can help determine the health and status of a pregnancy in the first trimester.
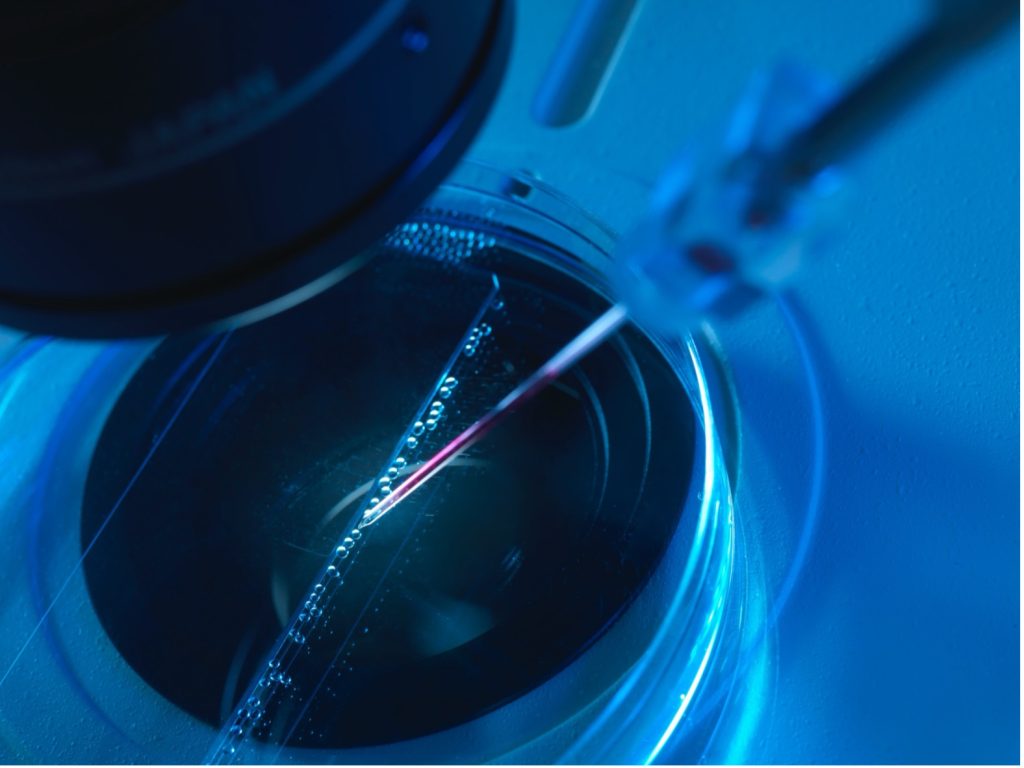
If a pregnancy complication is suspected in the first trimester, a medical doctor can perform a chorionic villus sampling (CVS) test, which is often done to determine genetic abnormalities between weeks 10 and 13. During a CVS test, the doctor will obtain a blood sample from the fetal part of the placental chorion. Because this is an invasive procedure and touches the placental tissue, there are risks of bleeding, limb defects, infection, and more. Because of the rise of other forms of genetic testing and placenta pathology, CVS tests are not as commonly used presently, but they provided (and still provide) great insight into the placenta’s pathophysiology when the placenta is still inside the uterus. Other than a CVS, blood tests and ultrasound imaging are used to determine the role of the placenta when it is in utero (1,2).
What Are Some Risks and Benefits of Placenta Uses in Modern Medicine?
In this course, placenta uses in modern medicine to be discussed include the role of placenta pathology, the role of placenta consumption post-delivery, and the role of placentas in regenerative medicine. It is important to educate patients that there are risks and benefits to all options, including cost. Placenta pathology is often done for most deliveries in major healthcare facilities, as placentas are typically sent to a pathology laboratory after delivery to determine if there were any placental complications during labor or delivery.
Most insurances will typically cover the cost of placenta pathologies, but the exact cost can vary significantly. Placenta pathology can be an important step in patient care if there are suspected parental or infant complications, genetic abnormalities, or emergent situations during labor and delivery. Some risks of placental pathology include incomplete reports and possible questions that are left unanswered; however, placental pathology is not known to have any complications to the birthing patient or infant directly (3,4,5,6).
Furthermore, the role of placenta consumption post-delivery has existed for centuries in several Indigenous cultures and has been slowly gaining traction in popularity in mainstream healthcare settings. Placenta consumption does not mean after the infant is delivered that the birthing parent starts consuming the placenta immediately in the delivery setting. Oftentimes, the parent would request the placenta to be released from the birthing facility and then sent home with the birthing parent.
Nowadays, there are several placental encapsulation services, placental burial services, or other culturally specific services, which is something to consider. There is mixed evidence on the role of consuming the placenta postpartum, which is why placenta consumption is often seen as a situation with more risks than benefits. Finally, the role of placentas has garnered much attention for the role of placentas in regenerative medicine and stem cell research. While this is still a new area of placenta use in modern medicine, several studies are suggesting that placentas can play a critical role in stem cell research, genetic testing, and regenerative medicine, possibly changing the ways health care and medicine view placentas.
Even though this might seem like a promising opportunity to become involved in research and science, this also poses the concern of bodies, state surveillance, and medical racism and misogyny that many birthing bodies might experience (7,8,9,10,11,12).

Self-Quiz
Ask Yourself...
- What are some ways newer technology can be used in patient care?
- What are some placental trends you are noticing in your workplace?
- Why would a patient want to embrace cultural traditions regarding their placenta?
- How does culture affect prenatal and postpartum care in America?
Defining Placenta Uses in Modern Medicine
Placenta Pathology and What It Means for Patients and Medicine
Placenta pathology is often performed after a placenta has been delivered. Oftentimes, in many healthcare settings, unless there is an objection from the patient or an emergent situation, placentas are sent immediately to pathology for gross examination of the surfaces, blood type confirmation, and assessment of placental health.
The placenta pathology can play a great insight into the health of the birthing parent and infant, such as ensuring adequate perfusion, oxygenation, and nutrition. In addition, placental pathology can also see what the human eye cannot visibly see, such as microscopic damage, ruptured blood vessels, and the like. Placental pathology can also play an essential role in determining fetal or maternal deaths, such as if the placenta had an infection, severe damage, or was not properly developed.
Upon completion of placental pathology, patients can request a report of their pathology and discuss results with their healthcare provider and vice versa. These reports can also look into causes and implications for fetal brain development, the role of genetics, maternal health complications, and possible future pregnancy outcomes. As the role of pathology and technology continues to evolve, placental pathology reports are becoming more detailed, providing more insight into future pregnancy health, pregnancy trends, placental health, fetal health, and maternal health (4,5,6).
Placenta Uses in Various Cultures, Including Placenta Encapsulation
In many cultures, particularly in indigenous or native cultures, the placenta is viewed as a critical part of postpartum and afterbirth care. While there are hundreds of indigenous cultures, many of these cultures view the placenta as an extension of the infant and often as an extension of the labor and time the birthing person has devoted to the pregnancy. Presently, around the world, many cultures experience birth and postpartum differently.
As healthcare systems in America embrace the roots of Indigenous people here and cultures from around the world, it is important to realize that many patients would not want their placenta to undergo pathology and would prefer to be discharged from the birthing facility with their placenta. For instance, some birthing patients from some cultures might request to be discharged with a placenta, and that person might bury that placenta. Another patient who might have ancestry from a specific Native American tribe might want to encapsulate that placenta and consume it after birth. While there are possible risks of consuming an external organ, such as infection, altered hormone levels, and gastrointestinal upset, many aspects of placenta consumption postpartum have become more modernized, thus reducing the risk of possible complications (7,8,9).
If you have never encountered a patient who would like to be discharged from the birthing facility with their placenta or who would like to engage in placental encapsulation, then it might be a bit shocking to you as a nurse working in health care. The majority of patients postpartum do not ever leave with their placenta, let alone consume or bury the placenta. That said, this is a learning opportunity for nurses to be aware of the various roles of health care, culture, and placenta uses can co-exist. If you encounter a patient who wishes to be discharged with their placenta, make sure the delivery provider is aware of their situation, and paperwork can be started before the delivery of the fetus.
Some things you can do if a patient wishes to have their placenta with them after delivery include: (1) making sure patients have completed all their consent forms before the procedures; (2) making sure the patient has their container for the placenta (unless your facility provides one); (3) documenting placenta findings during the birth per workplace policy; and (4) making sure the delivery team is aware that the placenta is to be given to the patient upon expulsion (7,8,9).
The Role of Placenta Consumption and Maternal Health
Historically, many cultures have recommended that people consume the placenta postpartum to aid with breastmilk production, parental-infant bonding, and postpartum mood. While the consumption of placentas postpartum has existed for centuries, very little evidence has shown a definitive role between postpartum mood and placental consumption. In general, anyone who gives birth is at risk for postpartum mood changes, such as postpartum depression, anxiety, and psychosis.
While some studies might suggest that placentas can influence mood and pregnancy changes, there is still no known definitive link between the role of placental consumption and improvements in maternal health in the immediate postpartum. However, this is a growing area of research, considering that zoologists and animal behavior specialists believe that many mammals in the wild also consume their placenta postpartum, assumingly for survival, nutrition, growth, and bonding.
Even though science has not confirmed a link between placental consumption, breastmilk production, parent-infant bonding, genetics, and maternal mental health, further research is needed to determine the long-term role of the placenta in postpartum modern medicine (1,2,7,8,9).
Placental Tissues and Regenerative Medicine
The placenta is considered the single most important link between the pregnant person and the fetus. Upon delivery, while the placental tissue can be sent to the pathology lab or home with the patient for their use, a new role of placental tissue use has emerged. While placental tissues have been studied for regenerative medicine research purposes since the 1990s, as technology and modern medicine have evolved, so has the role of the placenta in regenerative medicine. Placentas are highly regarded for their various types of cells, membranes, collagen, immunological properties, and antimicrobial properties. Many people can now donate their placentas after birth to scientific labs or birthing facilities directly for stem cell research, regenerative medicine research, genetic research, and more.
Some research has shown remarkable success with placental tissue cells for wound healing, burn healing, and vascular remodeling. While placentas can play a major role in regenerative medicine for the birthing parent, infant, and general society, there are also ethical considerations to be aware of. Many times, people of color, especially women of color, have been subjected to injustices within cell donations and scientific pursuits. If a patient is curious about the role of their placenta, stem cell research, and scientific knowledge, feel free to answer their questions and provide assurance on the realities of uses for placental stem cells (1,2,7,10,11,12).

Self-Quiz
Ask Yourself...
- What would be some reasons a patient might want to leave the birthing facility with their placenta?
- Have you ever seen a placenta pathology report? What did that report contain?
- What are some ways you would discuss with staff the importance of placenta uses in modern medicine?
- How would you approach conversations about various placental postpartum uses with other co-workers?
Nursing Considerations
What Is the Nurses’ Role in Placenta Uses in Modern Medicine?
Nurses remain the most trusted profession for a reason, and nurses are often pillars of patient care in several healthcare settings. Patients turn to nurses for guidance, education, and support. While the scope of work of nurses can vary state by state and by various workplaces, here are some general recommendations for the role of nurses in placenta uses in modern medicine (1,2,4,5,6,7,9):
- Take a detailed health history. Often, obtaining a detailed health history before birth is complex and sometimes dismissed in healthcare settings, even in emergencies. Nurses are known for their details of care. Even if there is an emergency delivery situation, making sure you are aware of the patient’s health history, desires, and placental preferences is a must. If this is not an emergency birth situation, ask about how long the symptoms have lasted, what treatments have been tried, if these symptoms interfere with their quality of life, and if anything alleviates any of these symptoms. If you feel like a patient’s complaint is not being taken seriously by other healthcare professionals, advocate for that patient to the best of your abilities. Take the time to establish care with that patient.
- Review medication history at every encounter. Whether you are working in outpatient or inpatient care, reviewing health records can be overwhelming. While millions of people take medications, many people take medications and are no longer benefiting from the medication. Ask patients how they are feeling on the medication, if their symptoms are improving, and if there are any changes to medication history. Make sure to specify if the patient is taking any over-the-counter supplements or herbs as well. Make sure you are aware of your facility’s anaphylaxis protocol in case of an allergic reaction.
- Be willing to be honest with yourself about your comfort level discussing topics and providing education on medication and medical procedures, including placenta encapsulation and placenta pathology. If you are not comfortable discussing something, please refer to another staff member.
- Communicate the care plan to other staff involved for continuity of care. For several patients, birth is the most life-changing event. Ensure that patients’ records are up to date for ease in record sharing and continuity of care.
- Review your documentation and facility protocols before the birth and before moving the placenta. If you suspect any complications or discrepancies with documentation, make sure you take time to review it again.
- Monitor the patient during the procedure, especially their vital signs and responses to pain. Birth is painful, and the placenta should be delivered intact regardless of the pain or mode of infant delivery. Ensuring the patient, fetus, and placenta are all intact is essential.
- Ensure that all staff and the patient are wearing appropriate PPE at all times during the birth and when handling the placenta per your workplace’s protocol.
- Stay up to date on continuing education related to nursing, placenta uses, and maternal health, as evidence-based information is always evolving and changing. You can then present your new learnings and findings to other healthcare professionals and educate your patients with the latest information.
- Many people, including health care professionals, are not aware of postpartum placental uses, including placental encapsulation and placental uses in regenerative medicine. Be willing to educate people on these topics, as some people may be uncomfortable with a patient leaving the facility with a placenta.

Self-Quiz
Ask Yourself...
- What are some ways patients can learn more about the uses of the placenta postpartum?
- What are some ways that nurses can take note of specific patient health concerns?
How can nurses identify if a patient wants to use their placenta for medical uses after birth?
Truly, a nursing career in reproductive health, birth work, women’s health, or postpartum health can be extremely rewarding personally, professionally, financially, and emotionally. If you are caring for a pregnant patient, be sure to ask what their plans for the placenta are without making assumptions. Oftentimes, patients might not be aware of the roles of the placenta in regenerative medicine, so they can request their placenta pathology report or modernized options for placenta encapsulation. Educating and informing patients about their options is the duty of a nurse working with pregnant patients (1,2,5,7,8).
What should patients know about placenta uses in modern medicine?
Patients should know that the placenta is the only organ that is ever created during every pregnancy. If a patient is interested in learning more about the role of the placenta postpartum, the patient should be willing to ask questions to their care teams, including their nurses (1,2,6,7,8).
- Tell the health care provider of any existing medical conditions or concerns (need to identify risk factors for postpartum placenta use)
- Ask the provider about options for performing placenta encapsulation or leaving the hospital with the placenta (need to identify if the provider is comfortable with this and aware of various placenta options)
- Ask the provider or care team for a placenta pathology report after delivery (need to ensure documentation is in place)
- Tell the health care provider of any existing lifestyle concerns, such as drug use, sleeping habits, diet, stress levels, incision site changes, or vaginal bleeding changes (need to identify lifestyle factors that can influence delivery medication use and therapy interventions)
- Tell the health care provider if you have any changes to your body, such as trouble with urination, GI complications, pain with movement, or increased fatigue (potential placental retention symptoms)
- Tell the nurse or health care provider if you experience any pain that increasingly becomes more severe or interferes with your quality of life
- Keep track of your health, medication use, and health concerns via an app, diary, or journal (self-monitoring for any changes)
- Tell the health care provider right away if you are having thoughts of hurting yourself or others (possible increased risk of suicidality with postpartum complications)
- Take all prescribed medications as indicated and ask questions about medications and possible other treatment options, such as non-pharmacological options

Self-Quiz
Ask Yourself...
- What are some patient experiences in health care that could influence how they perceive nurses and other health care professionals?
- How can modern advances in placental use in medicine influence the role of postpartum care?
- What are some laws or legislation that can influence placenta use in modern medicine?
- What are some perspectives a nurse can bring to the team compared to other members in clinical care, birth work, or stem cell research services?
Upcoming Research
What research on placenta uses in modern medicine exists presently?
There is extensive publicly available literature on placentas and prenatal and postpartum health via evidence-based journals and nursing research.

Self-Quiz
Ask Yourself...
- What are your predictions for placenta research?
- How do you think current and future nursing practices will affect the role of placenta use in modern medicine?
- Why would the role of the placenta be a growing topic in research?
- In your nursing studies, what were you educated on regarding the placenta and its uses in modern medicine?
- How does your culture typically view the role of the placenta?
Conclusion
Nursing and placental uses in modern medicine are here to stay, and nurses are at the forefront of patient care in many settings. While many people are unaware of the role of placentas, nurses provide essential health care to thousands of people every day in America, including pregnant people. From inpatient prenatal care visits to emergency room deliveries, nurses are collecting patient histories, performing assessments, and educating people on their bodies. Now is the time to make sure you are aware of the various roles of the placenta in modern medicine.
References + Disclaimer
- Herrick EJ, Bordoni B. Embryology, Placenta. 2023. In: Stat Pearls. Treasure Island (FL): Stat Pearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551634/
- Kapila V, Chaudhry K. Physiology, Placenta. 2023. In: Stat Pearls. Treasure Island (FL): Stat Pearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538332/
- Rohatgi, KW, et al. 2021. Medication Adherence and Characteristics of Patients Who Spend Less on Basic Needs to Afford Medications. Journal of the American Board of Family Medicine: JABFM, 34(3), 561–570. doi.org/10.3122/jabfm.2021.03.200361
- Redline, RW. Placental pathology: Pathways leading to or associated with perinatal brain injury in experimental neurology, special issue: Placental mediated mechanisms of perinatal brain injury. 2022. Experimental Neurology. 347. doi.org/10.1016/j.expneurol.2021.113917
- Chen S, Shenoy A. Placenta Pathology and the Developing Brain. 2022. Seminars in Pediatric Neurology. 42. doi.org/10.1016/j.spen.2022.100975
- Redline RW, et al. Placental pathology is necessary to understand common pregnancy complications and achieve an improved taxonomy of obstetrical disease. 2023. American College of Obstetrics and Gynecology. 228(2):187-202. doi.org/10.1016/j.ajog.2022.08.010
- Moeti C, et al. The Disposal of Placenta among Indigenous Groups Globally: An Integrative Literature Review. 2023. International Journal of Reproductive Medicine. doi.org/10.1155/2023/6676809
- Creeth HDJ, John RM. The placental programming hypothesis: Placental endocrine insufficiency and the co-occurrence of low birth weight and maternal mood disorders. 2020. Placenta. 98:52-59. doi.org/10.1016/j.placenta.2020.03.011
- Mir, IN, et al. Placental origins of neonatal diseases: toward a precision medicine approach. Pediatric Research 89, 377–383. 2021. doi.org/10.1038/s41390-020-01293-6
- Roy A, et al. Placental Tissues as Biomaterials in Regenerative Medicine. Biochemistry Research International. 2022:6751456. doi:10.1155/2022/6751456
- Laorden EH, et al. 2023. Human placenta-derived mesenchymal stem cells stimulate neuronal regeneration by promoting axon growth and restoring neuronal activity. Front. Cell Dev. Biol. 11:1328261. doi:10.3389/fcell.2023.1328261
- Pethe P, Kale V. Placenta: A gold mine for translational research and regenerative medicine. 2021. Reproductive Biology. 21(2):100508. doi.org/10.1016/j.repbio.2021.100508
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
