Course
Pyelonephritis: Management and Treatment
Course Highlights
- In this Pyelonephritis: Management and Treatment course, we will learn about the risk factors that are associated with acute pyelonephritis.
- You’ll also learn the clinical manifestations that patients may present with acute pyelonephritis.
- You’ll leave this course with a broader understanding of the various approaches used to diagnose pyelonephritis.
About
Contact Hours Awarded: 2
Course By:
Tabo Mwikisa-Kelly DNP, MSN, RN, CNEcl
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
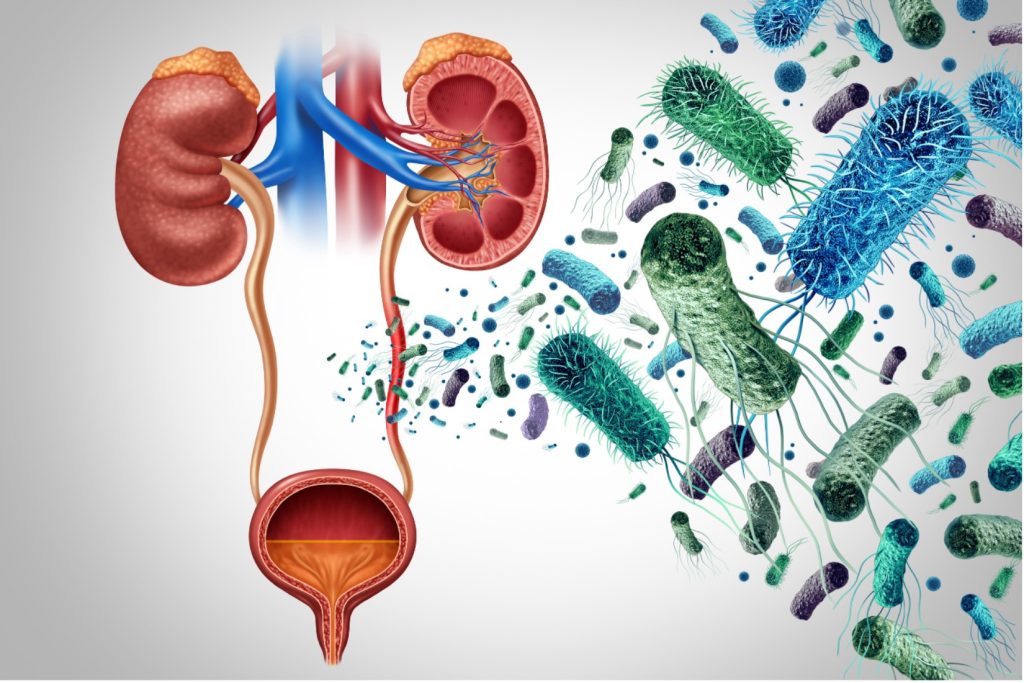
Pyelonephritis is a type of infection that affects the kidneys. It can present as an acute or chronic condition. Pyelonephritis is commonly caused by a bacterial infection from the pathogen known as Escherichia coli (E. coli). It can spread by ascending from the lower urinary tract system into the kidneys or through hematogenous means. It affects women more than men due to the anatomical structure of the urethra. Men are vulnerable to mortality rates caused by pyelonephritis. It is mainly treated with antibiotics. The prognosis is mainly dependent on diagnosing and treating the infection promptly [1][6].
Case study
A 37-year-old female presents to the outpatient urology clinic after an urgent referral is placed by the primary physician. The patient reports they have a history of chronic Urinary Tract Infections (UTI) and kidney stones. In the last 3 days, the patient has been experiencing fatigue, fevers, and chills in the last 24 hours, extreme nausea, suprapubic pain, dysuria, urinary frequency, and some moderate flank pain. The patient states, “Occasionally, my urine has a strong odor to it”. A urine dipstick is performed in the clinic and is positive for leukocyte esterase, nitrites, and blood. After performing a bladder scan on the patient, a bladder volume of 200ml was shown on the scan even though the patient had emptied their bladder.
Background
Pyelonephritis is an inflammatory disease caused by a bacterial infection involving the kidneys and renal pelvis [6]. Pyelonephritis, also known as a kidney infection, is a common type of urinary tract infection (UTI) that can also become life-threatening. It usually originates from the lower urinary tract system, which involves the urethra or the bladder, and ascends into the kidneys. Pyelonephritis can also spread through the bloodstream as a hematogenous infection resulting from systemic bacteremia [2] [6]. Pyelonephritis usually begins as cystitis, the bladder’s inflammation caused by an infection. It is typical for patients to present with symptoms resembling a lower urinary tract infection (UTI).
Classic symptoms of an upper UTI include fever, flank pain, dysuria, urinary frequency or urgency, nausea and vomiting, and costovertebral angle tenderness [2][3]. Pyelonephritis can be present as an acute or chronic condition, which can range from mild to life-threatening disease that often leads to scarring of the kidneys. Also, pyelonephritis can be divided into complicated and uncomplicated disease processes [2].
In this lesson, we focus on acute pyelonephritis.
Differences between Acute Pyelonephritis and Chronic Pyelonephritis
Chronic Pyelonephritis
It is important to understand the difference between acute and chronic pyelonephritis as the presentation of symptoms may vary. The difference is chronic pyelonephritis results from bouts of acute pyelonephritis which can cause scarring and fibrosis. Chronic pyelonephritis is commonly seen in children with major anatomical abnormalities in their urinary tract system [2][4]. 5% to 6% of cases in children are due to vesicoureteral reflux. 20% of the population may end up with end-stage renal disease [10]. Also, there is another form of a chronic bacterial infection of the kidney known as Xanthogranulomatous pyelonephritis: It is rare and characterized by granulomatous abscess formation, severe kidney destruction, and clinical pictures that resemble those of renal carcinoma and other renal inflammatory diseases that affect the parenchymal [4].
Acute pyelonephritis
This is the most common type of kidney infection, mainly caused by E. coli. The second most common cause of acute pyelonephritis is Klebsiella pneumoniae and Enterobacter, which are commonly found in bowel flora. These bacteria ascend from the lower urinary tract system and into the kidneys [1].
Acute pyelonephritis is often sudden and a severe form of kidney disease which can lead to possible kidney damage, acute kidney injury, formation of an abscess in or around the kidneys, urosepsis, septic shock, and organ failure. Acute pyelonephritis has the potential organ and life-threatening infection that can lead to renal scarring [2].
Acute pyelonephritis can occur as uncomplicated or complicated.
- Uncomplicated acute pyelonephritis is often seen in young healthy women who are without structural or functional abnormalities in their urinary tract system. Uncomplicated pyelonephritis is curable without any complications or scarring.
- Complicated acute pyelonephritis can result from abnormal anatomic structures and functional abnormalities of the urinary tract system accompanied by complicated UTIs. Complicated acute pyelonephritis varies based on patient characteristics, which include obstruction, nosocomial infection, use of foreign urologic objects such as catheters, impairment with voiding, and metabolic abnormalities [2][6].
- Obstruction: kidney stones, tumors in the urinary tract system, diverticular, renal calculi, which warrant urgent intervention such as decompression or surgery, benign prosthetic hyperplasia (BPH).
- Voiding disorder: Urinary retention caused by incomplete bladder emptying, vesicoureteral reflux, ileal conduit and cystocele.
- Metabolic abnormalities and hormonal changes: Diabetes, pregnancy, nosocomial infections, medullary sponge kidney and nephrocalcinosis.
- Structural abnormalities: congenital abnormalities, neurogenic, single kidney, spinal cord injury or nerve damage around the bladder, chronic indwelling catheters [6] polycystic kidney disease, vesicle ureteral reflux (VUR). VUR is a complication in which urine tends to back up or reflux into one or both kidneys. VUR is common in children in structural abnormalities of the urinary tract system.
- Metabolic or hormonal changes: These include diabetes or pregnancy which can result in complications that result in pyelonephritis in due to physiological changes that lead to increased risk of UTI. The high levels of glucose predispose the patients to infection. Long-term effects of diabetes can cause cytopathy, which causes vesicourethral reflux and recurrence of UTIs. With pregnancy, hormonal changes and a shift in the position of the urinary tract system put the patient at risk for bacteria to ascend into the kidneys, which could eventually lead to premature death. Patients with diabetes are vulnerable to complications such as emphysematous pyelonephritis.
- Immunocompromised patients: Organ transplant recipients, patients with AIDS and Sickle cell disease. Patients with a transplanted kidney are without a ureter, which puts them at risk for developing a UTI. Also, being on immunosuppressants makes it challenging for the body to fight infections [2].
- Increased risk of multi-drug-resistant organisms.
- Unusual pathogens like yeast infections.

Self-Quiz
Ask Yourself...
- What differentiates acute pyelonephritis from chronic pyelonephritis?
- Describe the rare form of chronic pyelonephritis and how it affects the kidneys.
- List some common factors that contribute to complicated acute pyelonephritis.
- Which patient populations are at risk for developing complicated acute pyelonephritis? Describe the disease processes that contribute to their complications.
- List the most common type of bacteria known to cause acute pyelonephritis.
Epidemiology
Acute pyelonephritis is a common and yet severe type of UTI that accounts for 15 to 17 cases per 100, 000 females and 3 to 4 cases for 10,000 males annually. There are approximately 250, 000 outpatient office visits and 200, 000 hospitalizations in the United States annually that are due to acute pyelonephritis [4]. Approximately 10% to 30% of the population require hospitalization when diagnosed with pyelonephritis. The highest incidents of pyelonephritis are among women between the ages of 15 to 29 years old, who are usually healthy. This is followed by infants and adults older than 60 years [2].
Acute pyelonephritis is known to affect younger women who are sexually active as it increases their risk of developing UTIs. Women are more likely to be diagnosed with pyelonephritis. 70 – 90% of predominant cases related to acute pyelonephritis are due to the bacteria Escherichia coli, which accounts for uncomplicated pyelonephritis [1][2].
Although a small percentage of men, pregnant women, and children get acute pyelonephritis, men have a higher mortality rate compared to women. 1% to 2% of women with pregnancy can suffer from pyelonephritis, which puts them at risk for premature births and can be severe during pregnancy. Women are likely to develop cystitis. During pregnancy, the gravid uterus becomes compressed, which causes the right kidney to be affected with pyelonephritis.
A rare form of pyelonephritis is emphysematous pyelonephritis, a necrotizing form of infection in the kidney that occurs in 95% of patients with diabetes. Females are six times more likely to develop emphysematous pyelonephritis than males. In terms of demographics, no racial predisposition is known to affect patients with pyelonephritis.
With acute pyelonephritis, 30 – 40% of females experience gross hematuria, which can occur between hours to days of developing the infection [6].
Pathophysiology of acute pyelonephritis
Acute pyelonephritis is mainly caused by gram-negative bacteria which invade the renal parenchyma. E. coli is the most common gram-negative pathogen associated with acute pyelonephritis. Other causative pathogens are klebsiella, proteus and Enterobacter. E. coli bacteria is unique because it has P–fimbriae appendages that combine with the receptors on the surface of the uroepithelia cells and trigger an inflammatory response that leads to an infection in the urinary tract system. E. coli accounts for 70 to 90 % of uncomplicated cases of acute pyelonephritis strains [1][2]
When kidneys are infected with E. coli, they release cytokines and other inflammatory factors that assist with fighting off an infection. The inflammatory response can sometimes lead to scarring of the renal parenchyma. Kidney infections also lead to complications such as pyonephrosis, perinephric abscess, and papillary necrosis.
The kidneys can also become infected when bacteria are spread through hematogenous means, also known as the bloodstream. The most common bacteria that is spread through the bloodstream is the gram-positive organism staphylococcus, which is transmitted through intravenous drug use and endocarditis [2].
Etiology of acute pyelonephritis
Several factors could lead to pyelonephritis, such as ischemia and obstruction (Vesicoureteral reflux), which can be congenital or due to bladder obstruction, which can cause urinary stasis, which leads to infection [2].
Pyelonephritis affects the upper urinary tract system, which consists of the ureters, renal pelvis, and kidney parenchyma. The renal pelvis is the joint between the ureters, and the kidney parenchyma is the tissue found in the kidneys or collecting system.
There are two mechanisms by which acute pyelonephritis can spread to the kidneys [1] [2] [6].
- Through an ascending urinary tract infection that can originate from the lower urinary tract system.
- Hematogenous spread
The most common form of acute pyelonephritis is through ascension of the bacteria secondary to cystitis, unlike the hematogenous spread, which is less common. The hematogenous mechanism spreads through the bloodstream, often due to bacteremia in patients with ureteral obstructions or immunocompromised. The bacteria Staph aureus commonly causes hematogenous infections that result in pyelonephritis. Hematogenous infections can be spread by the following: intravenous drug use, endocarditis, epidural abscess, and fungal skin infections.
Pyelonephritis due to hematogenous infection is mainly associated with (virulent) organisms such as Staph aureus, P. Aeruginosa, salmonella, and candida [1] [2].

Self-Quiz
Ask Yourself...
- List the hallmark signs and symptoms associated with acute pyelonephritis.
- What makes diagnosing acute pyelonephritis more challenging?
- What are the two main ways in which pyelonephritis can spread to the kidneys?
- What is the meaning of hematogenous infection concerning acute pyelonephritis?
- List ways in which pyelonephritis can spread through hematogenous means.
Risk factors that can lead to acute pyelonephritis
The following are risk factors that lead to the development of a kidney infection [2][3]
- Sexually active young women (most at risk)
- Pregnancy
- Age – Infants and those 60 years and older.
- Immunocompromised patients. HIV, polycystic disease, long-term catheter use, people with one kidney, corticosteroid use. Immunosuppression tends to favor silent pyelonephritis.
- Metabolic conditions or health conditions: Diabetes, organ transplant, sickle cell disease.
- Stress incontinence
- Chronically catheterized patients.
- Sexual orientation: Frequent sexual intercourse within a 30-day period, use of spermicide, menopausal women.
- Abnormalities related to anatomy: Congenital abnormalities of the urinary tract system, Horseshoe kidney, double ureters, ureterocele, neurogenic bladder
- Obstruction: Benign prostatic hyperplasia (BPH), stricture, renal calculi.
- Increase in multi-drug-resistant organisms.
Signs and symptoms of acute pyelonephritis
The signs and symptoms of acute pyelonephritis can resemble those associated with a lower urinary tract infection (UTI).
The signs and symptoms of acute pyelonephritis are not always consistent with the disease process, which sometimes makes it challenging for clinicians to identify. The hallmark symptoms of pyelonephritis are flank pain, fever, and chills. Patients who present with the following signs and symptoms must be suspected of having acute pyelonephritis: costovertebral angle pain or tenderness, suprapubic tenderness, guarding, fever with chills, and rigor. Perineal pelvic pain and flank pain are more common in men [3].
Other Symptoms in acute pyelonephritis include – dysuria, gross hematuria, urinary frequency and urgency, nausea, vomiting, anorexia, bladder spasms, and lower extremity spasms or autonomic dysreflexia [1][6].
Clinical Manifestations
- Fever and chills: Fevers can be greater than 102. Although fevers are usually present in patients with pyelonephritis, it is not a universal symptom.
- General malaise: Patients may report feeling weak for several days
- Nausea and vomiting, anorexia.
- Flank pain: This is almost universal in all patients but not always present. Flank pain can sometimes be accompanied in the presence of pyuria. It is highly suggestive of pyelonephritis which differentiates it from other forms of UTIs.
- Pyuria: most common finding in patients with acute pyelonephritis (cloudy or foul-smelling or turbid urine)
- Pain in the abdomen and pelvic region: The patient may describe abdominal pain as dull or sharp due to inflammation. This symptom is more common in men than women.
- Costovertebral angle pain, flank pain, and tenderness: (CVA) is located at the bottom edge of the rib cage. Pain is unilateral and patients may report pain as being severe or not present at all. Tenderness in the CVA is felt when a clinician taps on the patient’s lower back.
- Suprapubic pain that can be accompanied by tachycardia and hypotension (systolic BP of less than 90). This may be an indication that the patient is becoming septic.
- Dysuria: burning, painful or stinging sensation upon urinating.
- Urinary frequency or urgency: This can occur due to incomplete bladder emptying
- Gross hematuria: Visible blood in urine. This may occur in 30% – 40% of patients and is commonly seen in women.
- Lower Urinary Tract symptoms: 20% of patients may not be present with these symptoms.
- New or increased incontinence episodes.
- History of recurrent UTI
Vulnerable Patient Populations
- Pregnant women
- High-risk patients for developing pyelonephritis which may cause preterm delivery.
- Immunocompromised patients
- Patients with neurologic conditions such as spinal cord injury or paraplegic or quadriplegic.
- These patients generally have a loss of sensation in parts of their body making it challenging to diagnose acute pyelonephritis.
- Children less than 2 years of age
- Higher risk for altered mental status, fever, vomiting, and failure to thrive.
- Elderly patients
- Altered mental status, decompensation of other organs, generalized weakness due to deterioration.
- Male patients
- The mortality rate in men is much higher than in women


Self-Quiz
Ask Yourself...
- List 5 common clinical manifestations in patients with acute pyelonephritis.
- Which signs and symptoms may cause suspicion that a patient may have acute pyelonephritis?
- Which patient populations are at a higher risk for developing acute pyelonephritis?
- What is meant by costovertebral angle pain and describe where it is located?
- What urinary symptoms and clinical manifestations may indicate a patient may have acute pyelonephritis?
Complications of Acute Pyelonephritis
Acute pyelonephritis can lead to serious health complications that can be life-threatening. Complications of acute pyelonephritis can include septic shock, renal abscess, and permanent parenchymal destruction due to the inflammatory response that results in scarring and potential loss of kidney function. Acute Kidney Injury and multiorgan system failure also contribute to the increased morbidity and mortality rates [1][7].
- Acute kidney Injury: It is rare for acute kidney injury to occur with pyelonephritis
- Emphysematous pyelonephritis (EPN): This is a rare but life-threatening form of an acute necrotizing infection characterized by the presence of gas within the renal parenchyma, the collecting system or perinephric tissue of the urinary tract system. EPN is more common in patients with diabetes mellitus (DM) but occasionally in patients with ureteral obstruction. The mortality rate is 60% in patients who have localized gas in renal parenchyma. Irreversible scar formation and renal fibrosis tissue distortion and inflammation of the interstitial which can lead to renal insufficiency [2][5][9].
- Pyonephrosis and perinephric abscess
- Renal abscess: May follow after failed treatment of focal bacterial nephritis.
- Kidney infections: can lead to elevated blood pressure, kidney failure, and chronic kidney disease
- Preterm delivery in pregnant women
- Scarring of the kidneys: This is more common in women than men by 46%. Delayed treatment caused by cystitis, pyelonephritis, or recurrent UTIs increases the risk of patients developing scarring of the kidneys.

Self-Quiz
Ask Yourself...
- What are some common life-threatening complications that can result from untreated acute pyelonephritis?
- In which patient population is emphysematous pyelonephritis common?
- List and describe four common complications caused by acute pyelonephritis.
- Why are patients who received a kidney transplant at risk for developing acute pyelonephritis?
- Where would the nurse practitioner or provider palpate to assess for costovertebral pain in a patient reporting flank pain with suspicion of acute pyelonephritis?
Diagnosis
Diagnosing acute pyelonephritis can sometimes be complicated as it mimics other disease processes. The following are some disease processes that could mimic acute pyelonephritis: Acute appendicitis colitis cystitis, ectopic pregnancy, pancreatitis, perinephric Abscess, Pelvic inflammatory disease, and obstructive pyelonephritis.
Therefore, it is essential to conduct a comprehensive clinical assessment and laboratory testing. This should also include a health history and a physical exam to rule out pyelonephritis. Misdiagnosis of pyelonephritis may lead to serious health complications such as sepsis and even death.
The physical exam must include an assessment for fever and palpation of the costovertebral angle for tenderness and suprapubic pain.
Special consideration for diagnosis must be considered for the following patient populations:
- Young female patients who are sexually active must receive a pelvic exam to rule out UTI, as this could suggest pelvic inflammatory disease.
- In men, a digital rectal exam must be performed if they are experiencing pelvic and perineal pain to help rule out acute prostatitis.
Routine urinalysis
- According to the Infectious Disease Society of America (IDSA), a mid-stream urine culture with microscopic sensitivity must be collected from the patient.
- Susceptibility testing is recommended for patients with symptoms of acute pyelonephritis.
- Patients must only take the antibiotics once a urine sample has been obtained for testing.
- Urine Dipstick In patients with symptomatic urinary tract infections accompanied by pyuria, a urine dipstick must be performed when there is suspicion of a UTI (Pyuria means urine containing white blood cells or pus).
- Urine culture with susceptibility testing: This test is more accurate when the urine specimen is obtained before initiating antimicrobial therapy. It is used to confirm the UTI diagnosis and helps guide the most appropriate antibiotic regimen to treat the organisms and susceptibility.
- Blood test: Blood chemistry and complete blood count (CBC) assists in determining the severity of the disease. Blood tests are recommended for patients who are severely ill and may be used to detect elevated white blood cells and inflammatory markers.
- Basic metabolic function: Assess kidney function (creatinine and BUN), electrolytes,
- Kidney biopsy with bacterial culture (Ideal in patients with kidney transplant).
- Pregnancy test: This is useful in women of childbearing age when pregnancy is a possibility that is not excluded by the patient’s history alone.
Diagnostics Imaging
Diagnostic imaging must be performed in patients who do not respond to treatment within 48 to 72 hours of treatment. Imaging should be reserved for severely ill patients with recurrent UTI and suspected obstruction who have not improved from initial treatment within a few weeks or months. It is also reserved for patients with clinical manifestations despite receiving treatment within 48 to 72 hours of antibiotics. Imaging can also be used in patients with abnormalities such as spinal cord injury and patients with ileal conduit or nephrostomy tubes. [2] [6][10]
- Ultrasound: This is the initial imaging of the kidneys and pelvic region that can be done at the bedside. It can detect kidney stones and abscesses. It is less sensitive than a CT scan, which is useful in reducing radiation exposure in high-risk patients, i.e., pregnant women.
- Magnetic Resonance Imaging (MRI): Used to detect masses in the kidneys, kidney infections, and obstruction. It can also be used in pregnant patients when an ultrasound does not provide sufficient results. The new MRI can also assist with differentiating renal abscesses from other types of kidney infections.
- Pyelogram or Urogram CT scan of the Abdomen and pelvic region: CT scan is the golden standard imaging recommended for high-risk patients. It is a test used to evaluate the urinary tract system and involves using contrast/no contrast. Therefore, checking the patient’s kidney function before the test is essential, checking for alterations in the kidney’s parenchymal perfusion [1][2].
A CT scan is useful for detecting anatomic physiologic changes, such as renal scarring, that are associated with acute pyelonephritis. This test is used to evaluate the perfusion defection and the enlargement of the kidneys due to pyelonephritis. It can also be used to evaluate hematuria, perinephric fluid and gas-forming infections, inflammatory masses, and urinary obstruction or hemorrhage.
A CT scan may also show global enlargement of the kidney fat strands and decreased urinary contract excretion. A CT scan can help determine whether pyelonephritis is emphysematous or xanthogranulomatous as these are complex forms of acute pyelonephritis that may require more aggressive treatment [5].
- Voiding cystourethrography and nuclear renal scanning: Evaluates vesicourethral reflux (VSR) and kidney scarring. This test is suitable for pediatric patients.
- Other urologic assessments used to diagnose pyelonephritis may include:
Cystoscopy/ Retrograde pyelography: This involves using a scope with a camera to examine the urethra, ureters, and bladder. This procedure may assist the provider in identifying bladder infections, obstructions, or reflexes in the ureteral orifices, and bladder examination [2].


Self-Quiz
Ask Yourself...
- What is the primary approach to the diagnosis of acute pyelonephritis?
- When is imaging recommended when diagnosing patients with acute pyelonephritis?
- A nurse is caring for a patient who is undergoing a diagnosis of acute pyelonephritis. When would it be appropriate for the nurse to initiate the antibiotics ordered for the patient?
- Which diagnostic imaging test would be appropriate for a pregnant woman and why?
- Which patient population would be appropriate for a kidney biopsy?
Treatment of acute pyelonephritis
The severity of the infection determines the treatment goals for acute pyelonephritis. These goals include symptom relief, elimination of infection to avoid renal damage, and identification of predisposing factors to avoid future recurrences of kidney infections. If left untreated, pyelonephritis can lead to kidney damage. Ten percent to thirty percent of patients who present with urosepsis because of acute pyelonephritis often require hospitalization.
The pathogen that commonly leads to urosepsis is E. coli or other Enterobacteria, which are mainly treated with empiric antibiotics and aminoglycosides that cover a broad spectrum of pathogens, such as Pseudomonas and enterococci.
The recommendation for treating pyelonephritis is to use empirical therapy that is tailored appropriately to the infecting pathogens. The first line of treatment for mild pyelonephritis is oral fluoroquinolones for a duration of 7 days in uncomplicated cases to 14 days in complicated cases (IDSA). There is a 10% chance of resistance to fluoroquinolones such as ciprofloxacin for 7 days or levofloxacin for five days and 30% resistance to trimethoprim/sulfamethoxazole, therefore, a one-time dose of ceftriaxone or ertapenem IV must be preceded by oral antibiotics. 90% of patients respond well to oral antibiotics in uncomplicated cases of acute pyelonephritis [2][9].
Depending on the severity of pyelonephritis, patients may be treated in an outpatient or hospital setting. Empiric antibiotics should be selected based on the likelihood of the type of uro-pathogen and local sensitivity patterns to antibiotics [3].
Patients with uncomplicated acute pyelonephritis who are healthy and not pregnant are suitable for outpatient treatment.
Patients with complicated acute pyelonephritis can be treated initially with intravenous fluids and a higher dose of oral antibiotics.
- Rehydration is important to prevent kidney failure as most patients may be dehydrated from having an infection.
- Controlling fever with antipyretic may be necessary in some patients.
- Patients unable to tolerate oral antibiotics must be prescribed intravenous drugs.
Pyelonephritis is generally treated with antibiotics. Oral antibiotics are customarily prescribed for 7 to 14 days in patients with uncomplicated acute pyelonephritis [2] [9].
Key points for antibiotic use:
- For women not requiring hospitalization, oral ciprofloxacin 500 mg by mouth must be ordered twice a day for 7 days or levofloxacin (Levaquin) 750mg, once a day for 5 days.
- In cases where fluoroquinolone is >10% resistant in the local population, a single dose or more of ceftriaxone or ertapenem, gentamycin IV must be preceded by appropriate oral antibiotics.
- In young men, a 14-day course of oral antibiotics must be prescribed.
- Trimethoprim/sulfamethoxazole is often prescribed when the susceptibility from the urine culture is unknown. (Bactrim DS, Septra DS) 1 tablet by mouth for 14 days. Fluoroquinolones are generally effective in treating acute pyelonephritis. However, fluoroquinolones must be used with caution in the elderly due to a black box warning that can result in central nervous system effects. They can cause potential aortic aneurysm and dissection, tendonitis, hypoglycemia or worsening cognitive conditions like dementia
- Ertapenem: This antibiotic is exclusively reserved for those with resistant cases as aminoglycosides can be toxic to the kidney although getting a single dose is considered safe [9].
- Renal cysts and perirenal abscesses secondary to acute pyelonephritis may require a more conservative approach to treating the infection unless a complication is present.
Surgical treatment: Surgical drainage of renal abscess (carbuncle) or obstructive pyelonephritis may be helpful when there’s a renal calculus causing the infection. D
- Extracorporeal shockwave lithotripsy: Used to treat renal calculi that may be causing any obstruction in the kidneys
- Debridement: papillary necrosis
- Patients with urosepsis which is complicated by UTI – early antibiotic treatment and resuscitation by Intravenous fluids.
Pain management may also be provided using analgesics as needed.
Consuming fermented milk products, cranberry, and blueberry juice reduces bacteria’s adherence to the urinary tract and helps reduce UTIs [2][5].

Self-Quiz
Ask Yourself...
- When is surgical intervention appropriate in a patient with acute pyelonephritis?
- Why do male patients require more prolonged treatment with oral antibiotics?
- Explain why fluoroquinolones must be used with caution in elderly patients.
- A nurse cares for an elderly patient diagnosed with acute pyelonephritis and is prescribed fluoroquinolones. The patient starts to develop hallucinations. What must the nurse do?
- What must the nurse anticipate the provider will do when the patient reports they will be discharged the next day after they have been on intravenous antibiotics for 3 days to treat acute pyelonephritis?
Nursing Considerations
It is important to assess patients for signs of hypovolemia and dehydration that are associated with excess production of urine because of bacterial infection and inflammation of the kidneys.
Patients must be assessed for fluid volume deficits, which can manifest in their vital signs. These may include tachycardia, tachypnea, hypotension, hypothermia, or hyperthermia. This can help monitor patients for sepsis.
- Assessment of patient’s urine characteristics: Patients with acute pyelonephritis may have concentrated urine with a strong or foul odor.
- Monitoring patients for complications: acute pyelonephritis can result in urosepsis which is characterized by bacteremia and bacteria. Paying close attention to the patient’s signs and symptoms, including vital signs, could help prevent septic shock and further decline in the patient’s condition.
- Assess patients for intake: acute pyelonephritis can lead to nausea and vomiting which could cause the patient to be anorexic.
- Infants may present with failure to thrive which is manifested by difficulty feeding or vomiting. Older adult patients may experience fluid volume deficit which could lead to dehydration and affect their mental status and can also lead to decompensation of organ systems.
- Administration of intravenous fluids: In severe cases, patients admitted to the hospital may require intravenous fluid replacement to correct fluid volume deficits and dehydration.
- Nursing interventions may include the following: bladder scan to determine whether a patient is in urinary retention.
- Accurate measurement of fluid intake and output: this can assist with monitoring the progression of pyelonephritis.
- Patients must be instructed to avoid every two to three hours to assist with emptying the bladder.
- Communicate with the provider about the use of fluoroquinolones in high-risk patient populations, such as the elderly and those with diabetes.
- Follow-up must be facilitated in patients with complicated cases of acute pyelonephritis.
- Referral or Consultations: The patient may require a multidisciplinary approach for complicated cases. This can involve a urologist, nephrologist, and infectious disease providers.

Patient Education
It’s important to offer patient education as this may aid in the prevention or recurrence of pyelonephritis [2][11].
Key educational points include:
- Counsel patients on preventing urinary tract infections by stressing the importance of completing the prescribed antibiotic regimens.
- Ensure that patients understand the disease process prognosis and how acute pyelonephritis is treated to prevent reinfection.
- Stay hydrated: Encourage patients to drink plenty of fluids, like water up to 2 Liters, especially when there is no fluid restriction. This helps to promote blood flow, which will reduce bladder irritation and flush bacteria in the urinary tract system.
- Patients should be encouraged to urinate after having sexual intercourse.
- Counsel patients on the importance of voiding frequently as this helps to keep the bladder empty and reduces urine stasis and harboring of bacteria on the bladder
- Encourage patients to avoid drinking fluids that can cause bladder irritation, such as caffeinated drinks, alcoholic beverages, spices, and carbonated drinks.
- Explain that the patient should wipe from front to back, especially after a bowel movement. This helps to keep bacteria away from the urethra.
- Teach patients the importance of preventing constipation.

Self-Quiz
Ask Yourself...
- Why would it be necessary for a patient to have intravenous access in a complicated case of pyelonephritis?
- What are some nursing actions that must be considered in a patient who has urinary frequency due to incomplete bladder emptying?
- What signs and symptoms may infants present with acute pyelonephritis?
- What important nursing education points must be included for female patients with acute pyelonephritis and prevention of recurrence?
- How would the nurse explain the importance of emptying the bladder frequently to the patient?
- What makes E. coli a unique type of bacterial infection about acute pyelonephritis?
- How can an obstruction such as BPH cause acute pyelonephritis?
- The prognosis of acute pyelonephritis is dependent on which of the following factors?
- What clinical manifestations indicate that a patient may develop sepsis related to acute pyelonephritis?
- What would be one of the main reasons a pregnant woman would be at high risk for developing acute pyelonephritis?
- What would be one of the main reasons a patient who recently received a kidney transplant is at risk for developing acute pyelonephritis?
- What response would be given to a patient who questions the need for a pelvic examination?
- What are some of the ways an abscess can be treated to prevent complications associated with pyelonephritis?
- What workup may be included to assist with diagnosing acute pyelonephritis?
- What do the terms cystitis and pyuria mean? How do they contribute to acute pyelonephritis?
- How can resistance to antibiotics be prevented in patients who are probed to pyelonephritis?
Conclusion
Acute pyelonephritis is considered a common type of UTI that is treatable with early recognition of symptoms. Treating the underlying causes and using appropriate antibiotics can lead to better patient outcomes. It is also important to provide patients and caregivers with education that will be useful in preventing the recurrence of UTIs.
References + Disclaimer
- Johnson, J.R, Russo TA. Acute Pyelonephritis in Adults. N Engl J Med. 2018 Jan 4. 378 (1):48-59
- Kamal, A.I. (2024). Acute pyelonephritis. Medscape. https://emedicine.medscape.com/article/245559-overview
- Belyayeva M, Jeong JM. Acute Pyelonephritis. 2024 Jan. https://www.ncbi.nlm.nih.gov/books/NBK519537/
- Fogo, A. B., Lusco, M. A., Najafian, B., & Alpers, C. E. (2016). AJKD Atlas of Renal Pathology: chronic pyelonephritis. American Journal of Kidney Diseases, 68(4), e23-e25.
- Wu, S. Y., Yang, S. S., Chang, S. J., & Hsu, C. K. (2022). Emphysematous pyelonephritis: classification, management, and prognosis. Tzu Chi Medical Journal, 34(3), 297–302. https://doi.org/10.4103/tcmj.tcmj_257_21
- Herness, J., Buttolph, A., & Hammer, N. C. (2020). Acute pyelonephritis in adults: rapid evidence review. American family physician, 102(3), 173-180.
- Mainali, A., Adhikari, S., Chowdhury, T., Gousy, N., Uprety, N., Arora, A., & Palencia, C. J. (2022). Acute Non-Obstructive Bilateral Pyelonephritis with Acute Kidney Injury Requiring Hemodialysis. Cureus, 14(7), e26746. https://doi.org/10.7759/cureus.26746
- Pacaud, M., Colas, L., Kerleau, C., Le Borgne, F., Giral, M., Brouard, S., & Dantal, J. (2022). Impact of late and recurrent acute graft pyelonephritis on long-term kidney graft outcomes. Frontiers in Immunology, 13, 824425.
- Smith, D. R. (2013). Smith and Tanagho’s general urology. McGraw Hill Professional.
- Lawati, A. H., Blair, B. M., & Larnard, J. (2023). Urinary tract infections: core curriculum 2024. American Journal of Kidney Diseases.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
