Quality Improvement in Hospice Care
Contact Hours: 3
Author(s):
Charmaine Robinson MSN-Ed, BSN, RN, PHN, CMSRN
Course Highlights
- In this Quality Improvement in Hospice Care course, we will learn about quality improvement in hospice care.
- You’ll also learn ways to provide quality care to patients in hospice.
- You’ll leave this course with a broader understanding of the role of quality improvement teams in hospice care.
Introduction
Case Study
A hospice agency has received multiple complaints from three hospitals regarding delayed discharges due to patients waiting hours for transportation companies to take them home. After reviewing several patients’ medical records, agency leaders note that the hospice nurse case managers are not documenting their communication with transportation companies when setting up patient transfers to patients’ homes.
For this reason, the leaders cannot determine why the transport team continually arrives late. In this course, we will join the team as they work to build a quality improvement team and start a new project to address the problem.
Hospice Care Basics
This section will cover the definition, benefits, costs, and payment of hospice care.
Hospice Care: Definition
Both hospice and palliative care are often used interchangeably, however there is a distinct difference between the two.
Palliative care is a service focused on improving the quality of life for patients with life-threatening illnesses (and their families) through symptom management, regardless of life expectancy [11].
Hospice care, however, is a type of palliative care that occurs at the end of life when patients have a low life expectancy. The goal of hospice is to provide comfort care, which includes the management of pain, respiratory distress, psychological distress, and other discomfort [25]. Hospice care can be provided to patients living at home and in nursing homes, and some inpatient hospitals also provide it.
Ask yourself...
- What is your main priority when caring for patients on hospice?
- How does your care differ when caring for patients on hospice versus palliative?
- How does your workload change when caring for patients on hospice living at home versus in nursing homes?
- How do you address situations where patients or families resist hospice care?
- Do you feel like you have seen a change in the number of palliative/hospice patients? What do you think has impacted this change?
Benefits
Hospice takes a comprehensive holistic approach to end-of-life care [25]. The complexity of care requires expertise and assistance from various disciplines and services.
Patients (and families) who sign up for hospice are provided the opportunity to receive the following services, including any other service that has been deemed necessary and arranged by the hospice team (25):
- Services from a hospice-employed care provider
- Nursing care
- Medical supplies and equipment
- Medications to manage pain and symptoms
- Hospice aide and homemaker services
- Physical, occupational, and speech therapy
- Medical social services
- Dietary counseling
- Spiritual counseling
- Patient and family grief counseling
- Family grief and loss counseling after the patient’s death
- Short-term inpatient pain control and symptom management
- Respite care (patient stay in a care facility for up to 5 days, to give caregivers a rest)

Hospice care does not include any extra treatment, care, transportation services, or medications unrelated to the terminal illness (unless arranged by the hospice team).
Ask yourself...
- With whom do interdisciplinary hospice team members collaborate the most?
- What types of referrals do you frequently make for family members?
- Which hospice services are the most time-consuming to arrange?
- In your organization, how often do patients on hospice require hospital stays for pain management?
- What does hospice care not include?
Costs and Payment
The cost of hospice depends upon whether the care is provided routinely at home, continuously at home (24-hour around-the-clock care), in an inpatient respite care facility, or in a general inpatient facility.
The following are average hospice care costs in the U.S (21):
- Routine home care: $212 per day (from day 1 to 60)
- Routine home care: $167 per day (from day 61+)
- Continuous home care: $1,523 per day (or $63 per hour)
- Respite care: $518 per day
- Inpatient care: $1111 per day
While some private insurances cover hospice, most hospice care in the U.S. is covered by Medicare through the Centers for Medicare and Medicaid Services (CMS), a government entity that oversees federal health insurance plans. CMS pays hospice agencies for the care they provide. For this reason, hospice agencies must follow strict CMS requirements surrounding hospice care, which, if not adhered to, can lead to financial penalties.
For a patient to qualify for hospice care coverage through CMS, three criteria must be met (25):
- Care must be received from a hospice agency that is CMS-certified
- A hospice care provider (or primary care provider) must determine that the patient is terminally ill with a life expectancy of six months or less*
- The patient must agree that they will receive comfort care only (not curative care for their illness)
*CMS benefits can be extended if the patient lives longer than six months, but their diagnosis is still deemed terminal by the care provider.
Ask yourself...
- How well does your organization accommodate patients on hospice who need 24-hour care?
- How often do family members of patients on hospice request relief through respite care?
- What are some financial penalties your organization may face if CMS protocols are not followed?
- In your organization, how often have you seen a patient remain on hospice for the past six months?
- What resources does your facility have available to help patients pay for their hospice care?
Quality Improvement in Healthcare
Before understanding where quality improvement (QI) fits in hospice care, there needs to be an understanding of basic QI principles. Quality improvement as a stand-alone way to improve healthcare, is actually a new concept.
Quality improvement in healthcare is “a systematic, continuous approach that aims to solve problems in healthcare, improve service provision, and ultimately provide better outcomes for patients” (9). The ultimate goal of QI in healthcare is to ensure quality care (or service) by engaging staff and patients to change workplace culture, processes, and systems (9).
Skills, including enthusiasm, optimism, curiosity, and perseverance, are essential in QI as there will be challenges on the improvement journey (16). Relational skills are also vital as QI relies heavily on effective teams. QI is a great opportunity for front-line nurses to get involved in leadership and inspire change in an organization (9).
Case Study
The hospice agency leaders are ready to begin building the QI team, which will work on a project to determine why patient transports from the hospital to home are delayed. The project aims to improve hospice discharge times for patients. As a reminder, hospice nurse case managers do not document their communication with transportation companies when setting up patient transfers from the hospital to patients’ homes.
Ask yourself...
- Based on the problem and information from the section above, which staff group would be most appropriate to invite to the team?
Nursing Care Plan Similarity
QI involves identifying problems or needs, setting aims or goals, devising plans, implementing those plans, evaluating progress, and adjusting the plans as needed (16)(22).
QI can be compared to a comprehensive nursing care plan that addresses problems within healthcare systems rather than individual patients. For example, a hospice nurse may devise an individual care plan for a patient with a terminal illness. Just as the nurse has to consider other factors that can affect the plan of care (e.g., difficult family dynamics or poor access to healthcare), QI teams have to consider other functions and processes that may occur within an organization that can affect successful implementation of the QI plan (e.g., staffing issues or budget cuts).
In the same way that the hospice nurse must depend on other care team members (i.e., counselors and social workers) to help meet care plan goals, QI leaders assign projects/tasks to various team members or committees within organizations to help meet QI goals.

Ask yourself...
- How do budget cuts and staffing issues affect how well you provide quality care?
- What was a memorable quality improvement project in your organization?
- What role do hospice social workers play in your organization?
- How could front-line nurses get involved in quality improvement projects in your organization?
- How does your facility communicate staffing and budgeting needs to your facility?
History and Background
Quality improvement dates back to the 13th century, during medieval times in Europe (6). Craftsmen developed strict rules for the products and services they offered and performed inspections to ensure the quality of their goods.
QI continued into the Industrial Revolution era, when factories began devising plans to increase productivity. Teams of managers executed the plans, and inspectors ensured the quality of goods. During World War II, the armed forces began engaging in QI to ensure the safety of military equipment.
Before the early 20th century, QI focused primarily on product quality. As time progressed, industrial leaders began to evaluate the “processes” – or activities – by which products were created. QI eventually expanded beyond the manufacturing industry into service, education, government, and healthcare fields. The healthcare industry engaged in QI by establishing methods that ensured the delivery of high-quality care.
These included evaluating health providers for clinical competency through establishing educational and credentialing programs in the early 1900s and holding health facilities to specific standards of practice with the help of monitoring agencies (i.e., The Joint Commission, established in 1952) (12).
Ask yourself...
- What is one way that patient safety is prioritized in your organization?
- How often does your organization perform audits on nursing documentation?
- What special certifications are required for your role?
- Have you ever been questioned by a state surveyor about your practice?
- What is quality improvement?
Quality Improvement Models
QI models (including frameworks and programs) lay the groundwork for how teams should set goals, create plans, implement interventions, and evaluate results. These models also highlight QI’s continuous or cyclic nature – the repetitive process of assessing or reviewing plans for improvements and making regular adjustments as needed. Established QI models share standard features, including clear goals, leadership, activity monitoring, and use of structured processes to implement interventions (4).
The following are four standard models used in healthcare.
Model for Improvement
The Model for Improvement is a framework that QI teams can use to ensure that changes will lead to organizational improvement. The team makes changes on a smaller scale first (e.g., changing something for one day or changing something for one patient) before permanently implementing the change across the organization (14).
The Model for Improvement highlights the following three focus points for QI teams (14):
- Set a goal: “What are we trying to accomplish?”
- Select or develop quality measures: “How will we know that a change is an improvement?”
- Select a change intervention: “What change can we make that will result in improvement?”
The team then does a series of short test trials through a Plan-Do-Study-Act (PDSA) cycle (plan it, do it, study the results, and act on what is learned), also known as “Rapid Cycle Improvement” (22). When results are satisfactory, the team can implement the change on a broader scale.
Six Sigma Model
The Six Sigma model addresses “processes” or “the way things are done.” In healthcare, It is used to ensure that healthcare services are delivered reliably. The model focuses on eliminating errors by removing the causes of errors and minimizing external factors that might negatively impact care delivery (4).
DMAIC (Define, Measure, Analyze, Improve, and Control) is a strategy used in Six Sigma that outlines five steps for QI teams to follow:
- Define the problem, activity, and goals
- Measure the process (way care is delivered)
- Analyze the process to find out the root causes of poor performance (find out why the care delivery is not efficient)
- Improve the process performance by addressing or eliminating root causes (improve the way care is delivered by addressing barriers)
- Control the improved process and future process performance (make sure that the new way of care is delivered and is maintained)
Lean Model
The Lean model focuses on improving processes (how care is provided) by limiting wasted time, effort, and cost – essentially, keeping things “lean.” Lean emphasizes understanding and visualizing each step of the process (called mapping) and eliminating unnecessary steps [4]. Lean also outlines the following five focus points to help QI teams stay organized and shorten the time they spend preparing for projects (4)(7).
- Sort (eliminate whatever is not needed)
- Set in order (simplify and arrange whatever remains)
- Standardize (make whatever remains permanent)
- Sweep/shine (regularly check on whatever remains to be sure nothing changes)
- Initiate self-controls that will sustain the order of standardization (make the prior four steps a permanent part of the workplace culture)
Case Study
Four hospice nurse case managers (CMs) are invited to join the team. The leaders assign you the task of auditing the medical records of the patients who had delayed discharges. Your findings show that 60% of all CMs documented conversations with transportation companies. Although the ultimate goal is to improve the discharge process, an underlying problem needs to be addressed first.
Ask yourself...
- What ideas can you give the team?
- What types of improvement models have you used at your facility?
- What is a Six Sigma model?
- What is the lean model?
- Borrowing from the Model for Improvement framework in the section above, the team from the case study scenario asks you to answer, “What are we accomplishing here?”
Quality Care in Hospice
National Patient Quality Care Goals
The first step to QI in hospice care is understanding what quality care looks like for patients at the end-of-life. However, before learning how to effectively care for this particular group, hospice care organizations should understand the six basic national quality care goals that apply to patients in all care settings.
To establish a standard for quality care for all patients, the National Academy of Medicine, formerly the Institute of Medicine (IOM)—a nonprofit institution that gives national health advice—established the following six goals (or domains) for healthcare organizations to target [15][2].
Organizations should provide care that is:
- Safe
- Avoid harm to patients from the care that is intended to help them.
- Effective
- Provide services based on scientific knowledge to all who could benefit and refrain from providing services to those not likely to benefit (avoid underuse and misuse, respectively).
- Patient-centered
- Provide care that is respectful of and responsive to individual patient preferences, needs, and values and ensure that patient values guide all clinical decisions.
- Timely
- Reduce waits and sometimes harmful delays for both those who receive and those who give care.
- Efficient
- Avoid waste, including waste of equipment, supplies, ideas, and energy.
- Equitable
- Provide care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status.
Ask yourself...
- What are some hospice services that patients in your organization underuse?
- In what way is hospice care sometimes delayed in your organization?
- What is one way your organization avoids waste?
- What type of bias training does your organization offer?
- What is additional resources does your facility offer to families with loved ones on hospice care?
Quality Hospice/Palliative Care Guidelines
Once organization leaders understand what quality care looks like for all patients, they can begin to learn how to provide the best quality care for patients at the end-of-life.
The National Coalition for Hospice and Palliative Care’s Clinical Practice Guidelines for Quality Palliative Care is a great resource for any organization that services patients on palliative or hospice care. The guidelines offer step-by-step recommendations that address the following eight aspects of care (19).
Structure and Processes of Care
Organizations should develop a palliative/hospice care team, including health providers, nurses, social workers, and chaplains (or spiritual care specialists). The team should receive proper education and support to fulfill their role functions.
Organizations should ensure that comprehensive assessments are performed on patients and families, and every identified need is addressed in the care plan. Continuity of care should be assured when transferring patients to new care settings.
Physical Aspects of Care
Hospice nurses should be instructed to perform physical assessments for all patients, including those of pain, functional status, bowel function, and disease process. Care plans should address the treatment of symptoms (for example, pain or respiratory distress), and medications should be reviewed and adjusted according to the plan.
Psychological and Psychiatric Aspects of Care
Risk assessments (i.e., for emotional distress, anxiety, and depression) should be performed, and patients should be screened for a history of trauma or psychiatric disorders. Identified risks should be addressed in the care plan.
Hospice nurses should assess patients’ and families’ coping and grief and make referrals for treatments and therapies as needed (for example, chaplains or grief counselors).
Social Aspects of Care
The hospice nurse should identify social needs through a needs assessment. Needs may be associated with food security, housing, transportation, and equipment. Support systems and family dynamics should also be assessed, and referrals made as needed. Referrals may include transportation services, medical equipment and supply services, or social services.
Spiritual, Religious, and Existential Aspects of Care
Hospice nurses should perform a spiritual screening, history, and assessment. Patients and families should be encouraged to share their spiritual or existential beliefs and rituals surrounding death. Nurses should make efforts to accommodate patients’ and families’ spiritual practices. As with psychological and psychiatric aspects of care, referrals to chaplains or spiritual care specialists may be initiated.
Cultural Aspects of Care
Cultural assessments should help identify any needs that may require accommodation, such as language preferences and health literacy. Hospice nurses should respect the patients’ and families’ beliefs and preferred/taboo practices and arrange for cultural representatives as needed.
Care of the Patient Nearing the End-of-Life
Hospice nurses should assess for signs that patients are near death and teach families what to expect. They should also arrange the appropriate medication, supplies, and equipment as needed and initiate referrals for grief support.
Ethical and Legal Aspects of Care
Advance care planning needs should be identified, and arrangements made to accommodate patients’ wishes. Advance care planning includes preparing living wills, code status, treatment withdrawal, and assignment of medical decision-makers, among others.
Hospice nurses should frequently update patients’ preferences (as these may change over time) and arrange legal and ethical consultation if needed. Patients and families should also be educated on the financial costs and burdens associated with care.

Case Study
The team is still trying to reach a consensus on a formal goal for the new QI project. Other team members begin to give their opinions on the question: “What are we accomplishing here?” One CM says, “We need to find out why the 40% are not documenting.” Another CM says, “I agree, this is not an individual nurse case manager problem. There’s something wrong behind the scenes.” If you had this same thought, could you give the team some ideas to uncover the reasons for the lack of documentation?
Barriers to Quality Hospice Care
A 2022 Home Health and Hospice study of over 1,000 participating agencies nationwide highlighted best practices to empower home health and hospice organizations with ways to better care for their patients. Researchers compiled national hospice survey results from Hospice Centers of Excellence (HCEs) – hospice agencies that score in the top 15%. The study addressed potential barriers to quality hospice care. The following barriers were identified in the study [10]:
Delayed Admissions
The study showed that quality care scores worsened when admissions were delayed, and therefore, agencies should strive to admit patients to hospice within eight hours of receiving the hospice care order/referral from the health provider. Researchers found that most HCEs met this goal, with 76% conducting admissions within four hours (see figure 1).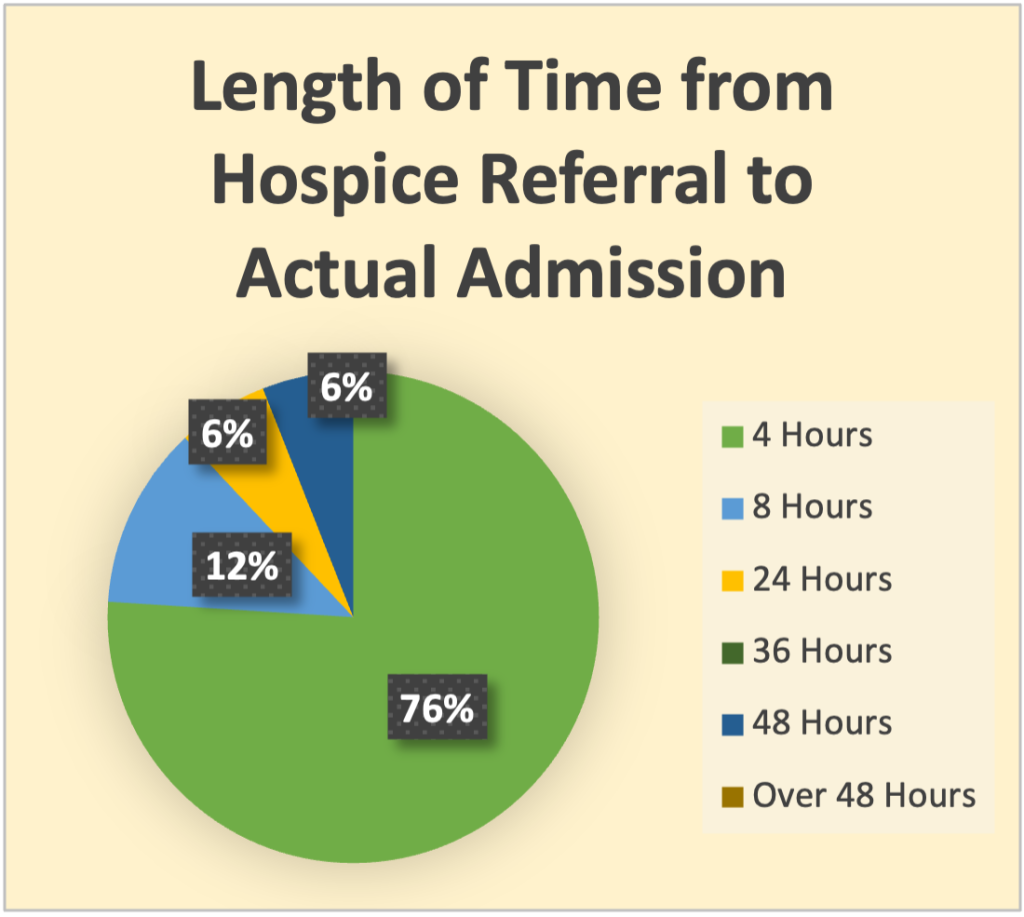
Reflects data from hospice agencies that scored highest on quality care surveys:
[Figure: Designed by course author]
Lack of Schedulers
Over half of all agencies use “schedulers” to schedule initial care visits for patients recently admitted to hospice [10]. Study results revealed that 79% of HCEs used schedulers this way, while 21% used a clinical team instead (see figure 2). Researchers ultimately found that quality care scores were lower when clinical teams were responsible for scheduling visits. As a result, agencies were recommended to assign dedicated schedulers for this role.

Reflects data from hospice agencies that scored highest on quality care surveys
[Figure: Designed by course author]
High Caseloads of Team Members
Historically, hospice nurse case managers have been assigned 10 to 12 patient caseloads [10]. However, study results show that 88% of HCEs actually had a higher nurse case manager caseload (13 to 18 patients) in in-home care settings (see Figure 3).
The difference was in the use of social workers. HCEs were able to manage higher caseloads with help from more social workers. While historically, social workers have been assigned to as many as 30 patient cases, social workers at HCEs were assigned only 13 to 18 patients (see Figure 4).
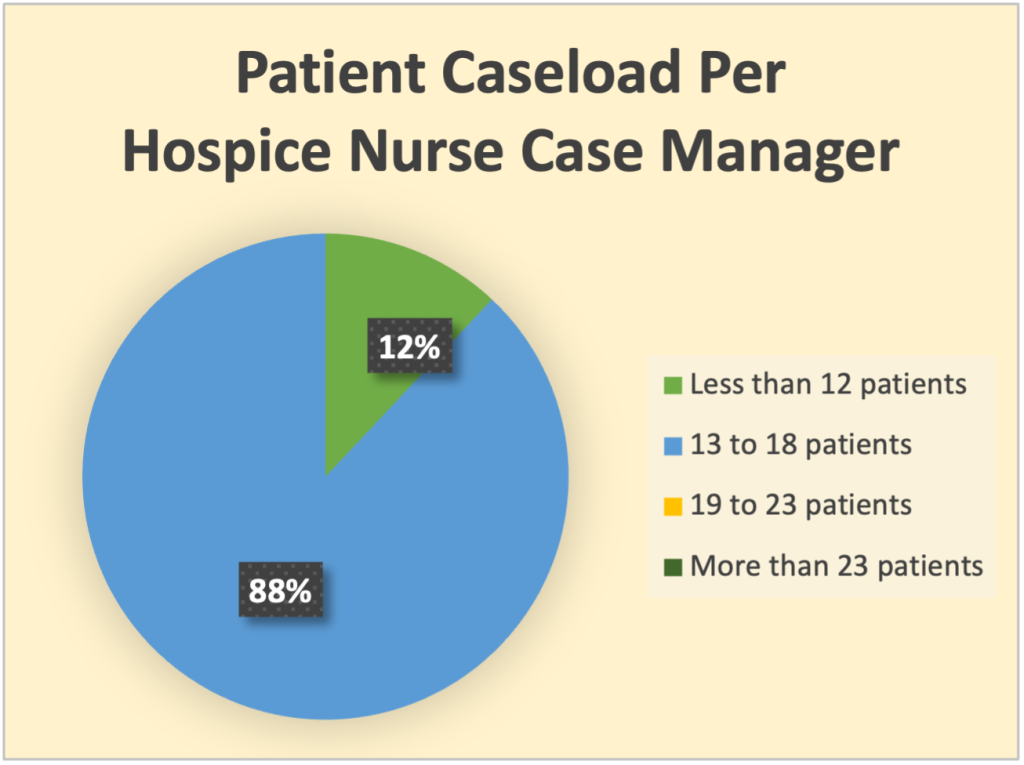
Reflects data from hospice agencies that scored highest on quality care surveys
[Figure: Designed by course author]
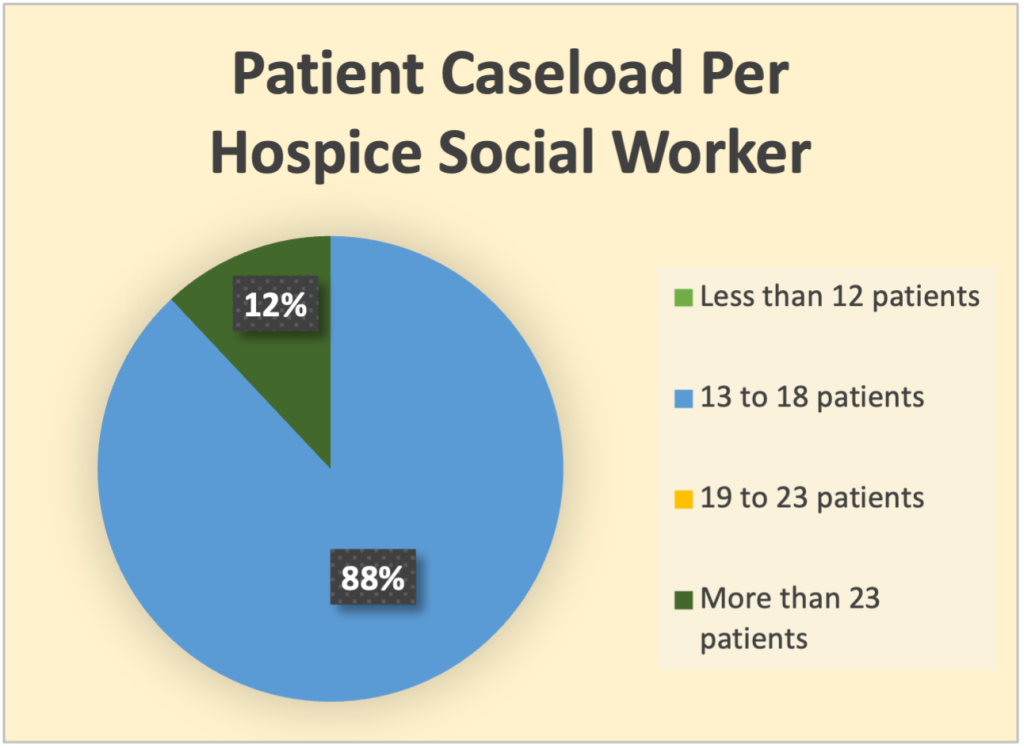
Reflects data from hospice agencies that scored highest on quality care surveys
[Figure: Designed by course author]
Case Study
The team knows that inviting front-line CMs to contribute to the QI project is beneficial as their insight can be highly beneficial to plan development. The leaders ask the CMs in the room if they have missed documentation when arranging patient transportation. One CM says, “I always document my conversations with the transport team.” The three other CMs agree. The leaders decide to ask the CMs about workplace factors that might contribute to the lack of documentation amongst their peers.
Ask yourself...
- If this was your thought, what could you ask the CMs about their workloads based on the information from the section above?
Quality Improvement Process in Hospice/Palliative Care
Poor quality hospice care can harm patients physically, emotionally, and spiritually (17). Once organization leaders know what quality hospice care looks like, they can identify the areas where improvements are needed within their own organization. At this point, they can begin to engage in QI.
Hospice QI is the process of identifying problem areas within an organization, putting together a plan of action, executing the plan, and continually evaluating the plan while adjusting to ensure that the organization always practices according to palliative/hospice quality standards (22). Hospice QI starts with developing a QI program or continuous QI program (CQI), which includes a team of leaders who monitor the organization for problems that need addressing.
If a hospice organization is CMS-certified, the QI team must comply with CMS regulations (or quality care standards). CMS serves as an “auditor” or “overseer” of hospice organizations, deciding how care should be provided. CMS also requires hospice organizations to develop, maintain, and document an ongoing quality improvement program (18).
Ask yourself...
- What is a common patient care problem area within your organization?
- Do you have regular contact with the quality improvement team in your organization?
- How well do you and your peers adapt to policy changes within your organization?
- Do leaders in your organization discuss CMS regulations in staff meetings?
- What quality improvement projects have you had or seen success with in practice? Which ones have been failures? Why do you think they had the outcomes they did?
How to Create a Hospice Quality Improvement Program
To create a QI program, hospice organizations should address the following steps, outlined by the National Hospice and Palliative Care Organization (18)(19)(22):
Step 1: Identify areas where improvement is needed
- The first step is discovering areas of need within the organization. QI leaders collect, track, and analyze data, such as adverse patient events. From the data, the team can identify areas of need and prioritize the areas based on patient care and safety needs. The areas should lead to measurable results.
Step 2: Design a QI project
- After identifying focus areas, leaders should create a QI project called “performance improvement project.” In this project, plans for improvement should be outlined by determining how significant the problem is, how it will impact patients, and if there is enough internal support to respond to the problem. Problem causes and contributing factors should also be considered (this is referred to as “root analysis”). Most importantly, leaders should ensure that the project supports the mission and values of the organization.
Step 3: Establish a QI team
Establishing a great QI team involves consulting the right people. The team should include representatives from every department or discipline involved in the identified problem areas, and a QI program representative should be designated.
Step 4: Setting goals
QI requires setting goals and outcome measures. The goals should be time-specific and measurable.
Step 5: Define goals
After establishing the team, clear goals (also termed “improvement targets” or “quality measures”) should be set through brainstorming and voting. Per CMS regulations, goals should target palliative outcomes, patient safety, and quality of care [18].
At every QI meeting, the team should acknowledge any progress made towards the goal and make revisions as needed (for example, resetting goals to a smaller patient population or longer timeframe).
The team should ensure that all goals are S.M.A.R.T:
- S (specific): address what will be achieved, by whom, when, and where
- M (measurable): quantified or can be proven objectively
- A (attainable): achievable within the organization
- R (relevant): problem-oriented and match the organization’s mission or vision
- T (time-based): completed within a specific timeframe
Step 6: Test change
Adopting the PDSA Model, the team can continuously trial changes (in increments) until there is improvement. The goal of testing is to evaluate the cost, impact, and side effects of changes and help the team determine which action will lead to the most desired result. Testing also helps reduce staff resistance to change once it is implemented across the organization.
Step 7: Implement change
Once the testing cycles have led to more minor improvements, the team can begin to act on a broader scale. During this step, the team should determine how the change may be assimilated in daily operations within the organization and consider the impact on education/training, hiring, documentation, and/or policies. The team should also document any unexpected problems that occur while implementing change.
Step 8: Evaluate change
The final step in developing a hospice QI program is reviewing the data, reflecting on what was learned, and determining what modifications should be made. At this stage, more testing cycles can begin until improvement is more consistent. Per CMS regulations, evaluation should occur annually [18].
Case Study
When asked about their workloads, the CMs reveal that caseloads have increased over the last few months as the agency is frequently short-staffed. One CM says, “Sometimes there’s a big pressure to chart everything in a short amount of time.” Another CM says, “I manage to get everything done on time, but some CMs are overwhelmed.” The other two CMs in the room agree. The leaders assign the CMs the task of surveying within their department. Results show that 50% of CMs sometimes forget to document because they have to arrange services for too many patients at once.
The team continues to brainstorm on an appropriate SMART goal. They know that delayed discharges can be a barrier to high-quality care, which might lead to poor CMS survey results over time. To avoid this, the team wants to make changes immediately and agrees on the short-term SMART goal “Over the next three months, 80% of all nurse case managers will document conversations with transportation companies in the medical record” (a 20% improvement).
Ask yourself...
- Based on these survey results and information from the section above, can you identify another SMART goal for the team?
- What interventions can the team implement to meet each goal?
- What performance improvement projects have you been a part of? What went well? What didn’t go well?
- What barriers have you encountered in creating and achieving a SMART goal?
- How often do the changes implemented from a project stick? Why do you think that is?
CMS Quality Measures
CMS monitors hospice organizations through various means, including surveys. The poor performance areas within these survey results can provide hospice QI project ideas. After identifying the problem areas, organization leaders can use CMS’s quality measures as goals for improvement.
Quality measures are “tools that measure a system’s health care goals and/or ability to provide high-quality care” (26). These measures show how organizations are making progress in meeting patient care goals. For example, in a nursing care plan, the nurse knows that if the goal is to “keep the patient comfortable,” there must be a way to prove that the patient is comfortable.
A quality measure in this case might be “pain control” or “less frequent use of pain medication.” CMS has developed its own quality measures to ensure patients are provided high-quality care. The following are two ways CMS monitors hospice agencies.
Hospice Item Set
The Hospice Item Set (HIS) is a CMS measure that specifies the proportion of patients who receive the following seven care elements from a hospice organization (as applicable) (26):
- Beliefs/values addressed (if desired by the patient)
- Treatment preferences
- Pain screening
- Pain assessment
- Dyspnea treatment
- Dyspnea screening
- Patients treated with an opioid who are given a bowel regimen
Hospice agencies must submit a HIS upon a patient’s admission and another at discharge [20]. Submission must be completed for the majority of their patients to remain compliant.
CAHPS® Hospice Survey Measures
After a patient on hospice dies, families receive a survey about the care provided by the hospice agency – the Consumer Assessment of Healthcare Providers and Systems Hospice Survey (CAHPS®). The following are six quality measures outlined in the survey (24):
Measure 1: Communication with Family
CMS uses this measure to determine how well hospice teams communicate with families.
Survey questions include:
- “How often did the hospice team keep you informed about when they would arrive to care for your family member?”
- “How often did the hospice team explain things in a way that was easy to understand?”
- “How often did the hospice team listen carefully to you when you talked with them about problems with your family member’s hospice care?”
- “How often did the hospice team keep you informed about your family member’s condition?”
Measure 2: Getting Timely Help
CMS uses this measure to determine hospice teams’ availability to patients and families.
Survey questions include:
- “When you or your family member asked for help from the hospice team, how often did you get help as soon as you needed it?”
- “How often did you get the help you needed from the hospice team during evenings, weekends, or holidays?”
Measure 3: Treating Patients with Respect
CMS uses this measure to determine if hospice teams respect and care for patients.
Survey questions include:
- “How often did the hospice team treat your family member with dignity and respect?”
- “How often did you feel that the hospice team really cared about your family member?”
Measure 4: Emotional and Spiritual Support
CMS uses this measure to determine if hospice teams address patients’ and families’ emotional and spiritual needs.
Survey questions include:
- “How much emotional support did you get from the hospice team?”
- “In the weeks after your family member died, how much emotional support did you get from the hospice team?”
- “How much support for your religious and spiritual beliefs did you get from the hospice team?”
Measure 5: Help for Pain and Symptoms
CMS uses this measure to determine if hospice teams provide appropriate comfort care.
Survey questions include:
- “Did your family member get as much help with pain as they needed?”
- “How often did your family member get the help they needed for trouble breathing?”
- “How often did your family member get the help they needed for trouble with constipation?”
- “How often did your family member receive the help they needed from the hospice team for feelings of anxiety or sadness?”
Measure 6: Training Family to Care for Patient
CMS uses this measure to determine if hospice teams provide end-of-life training to patients and/or families.
Survey questions include:
- “Were you trained on what side effects to watch for from pain medication?”
- “Were you trained on if and when to give more pain medicine to your family member?”
- “Were you trained on how to help your family member if they had trouble breathing?”
- “Were you trained on what to do if your family member became restless or agitated?”
CMS also measures the family’s rating of the hospice agency and whether they would recommend the agency to others. Along with data from “quality reporting” – a method in which hospice agencies are required to report certain types of data (e.g., number of patients served, number of patient visits per day, professional qualifications of team members, etc.)—CMS can determine if the organization is providing high-quality hospice care.
TeamSTEPPS Program: Overview
Good communication and teamwork can make the difference in how well an organization operates and keeps patients safe (1). TeamSTEPPS (Teams, Strategies, and Tools to Enhance Performance and Patient Safety) is a program aimed at helping organizations perform more efficiently by enhancing communication and teamwork.
The program is heavily backed by research on team performance and communication and relies on input from frontline workers in various healthcare settings. TeamSTEPPS highlights four skills that are needed for effective teamwork (1):
Communication
Communication is the basis of coordination, which is vital for teamwork. It is relaying verbal and nonverbal information between team members in a transparent, accurate, timely, and respectful way. Communication is comprised of the “who” (sender), “whom” (receiver), and “how” (the way information is exchanged). Often, messages from patients, family caregivers, and nonclinical staff are not given as much attention (1).
Societal and cultural influences can also hurt effective communication. Effective teams address these issues and ensure that every team member is heard and that every message is clearly understood.
Team Leadership
Team leadership involves leading and ensuring that members have clearly defined roles and responsibilities. Team leaders should also ensure each member has what is needed to function within the team. Patients and families are often not acknowledged as healthcare team members but play critical roles in the care process (8).
Understanding how patients want to engage with the team is essential for effective patient-centered teamwork (1). While some teams have a formal and permanent structure, rapid changes in the workplace or emergent patient needs can challenge the functions within the team.
Team leaders should ensure that all members understand any changes in team actions that may occur.
Situation Monitoring
Situation monitoring is continuously reviewing situations to better understand them and learn how to improve and support team functioning. It helps teams catch potential problems and diagnose others. A result of situation monitoring in healthcare is the ability to maintain situation awareness in an ever-changing environment (knowing the status of the patient, team, and environment at all times).
Situation monitoring can lead to a shared mental model within the organization (or “mental picture” outlining events or problems in the workplace). Shared mental models help team members mutually understand issues, goals, and strategies surrounding the plan of care. Team members can understand one another’s roles, anticipate team needs, and fill in as needed.
Mutual Support
Mutual support involves understanding each member’s role and responsibilities, assisting others when needed, and offering feedback. Team members also support the team’s mission by advocating for patient safety. Sometimes referred to as “backup behavior,” mutual support is vital for team performance and serves as a safety net for preventing errors and minimizing worker stress in the workplace.
Mutual support helps prevent staff work overload and burnout and fosters an environment of mutual trust and psychological safety (team members feel safe speaking up without retaliation) (1).
Ask yourself...
- What is one barrier to effective team communication within your organization?
- How do you facilitate plan of care discussions with patients and families?
- Are you clear on your role and responsibilities as a team member in your organization?
- When was the last time your situational awareness prevented an adverse event?
- What is one way your organization fosters a mutually supportive work environment?
TeamSTEPPS Program: Application to Hospice Care
Although frequently associated with hospitals, elements of TeamSTEPPS may be applicable to hospice care settings. Each of the four TeamSTEPPS skills (communication, team leadership, situation monitoring, and mutual support) can be achieved using more than 20 tools that can be integrated into the workflow to meet QI goals. The following are four tools hospice nurses can use to provide more efficient, quality care to patients at the end of life (1).
Handoff
Handoff is a standardized communication tool that nurses can use when reporting patient information to other team members. During care transitions, this tool helps ensure continuity and safety by preventing misinformation. For example, suppose a patient on hospice lives at home and is admitted to a respite care facility for a few days. In that case, the nurse can use handoff to relay important information to the care team at the facility (e.g., the last time an opioid medication was administered).
An effective handoff should include each of the following (1):
- Transfer of responsibility and accountability
- Clarity of information to ensure there is no ambiguity about responsibility
- Verbal communication is necessary to ensure the receiver understands the information
- Acknowledgement by the receiver (needed to relinquish responsibility from the sender)
- Opportunity for a set of “two eyes” to review situations for safety and quality
Teach-Back
Teach-back is a closed-loop communication tool (or verbal feedback tool) that ensures that verbal messages are clear. After teaching, rather than asking patients and families if they understood the information, nurses ask the patient or family to explain the information that was taught (recall) – essentially, teaching the information back to the nurse.
Recall is considered an essential factor in patients’ adherence to treatment and is associated with improved health outcomes (23). Hospice nurses can use the teach-back tool to assist patients and families in understanding the care plan, including medications and side effects, safety, symptom management, and stages of death. Teach-back has proven effective in various settings and populations (23).
Briefs
Briefs (or team meetings) are a team leadership tool used for sharing the plan of care with the team. During briefs, leaders discuss member roles and expectations, the current condition/status of the patient assigned to the team, patient care goals, and problems that may affect how the team functions.
Hospice nurses can lead briefings in the care setting, including patients, their families, and hospice care team members. During briefs, families can be made aware of their own roles during the patient’s end-of-life care. The following are questions for team members to consider during briefs:
Ask yourself...
- Do all team members understand and agree on the goals?
- What is the plan of care?
- How is the workload shared among team members?
- What are the available resources?
- What is important to each member (related to the focus of the brief)?
Task Assistance
Task assistance is a mutual support tool that helps build a strong, trusting team. All team members should protect one another from work overload by seeking and offering help as needed. The workplace culture should be psychologically safe. Patients and families are often a part of teams and should be offered help, supported in their roles, and depended upon when appropriate.
Studies have shown that palliative/hospice care staff experience moral distress, compassion fatigue, death anxiety, and burnout related to the job (13). Hospice nurses can apply task assistance in the workplace by providing shift relief to other team members when necessary.
Case Study
The team is discussing ways to meet the new SMART goal. As a reminder, the goal is “Over the next three months, 80% of all nurse case managers will document conversations with transportation companies in the medical record.” Several team members offer ideas. One CM says, “We just need to hire more CMs. It’s unfair that we must work under so much pressure.” Another CM says, “We need at least two new CMs.” The leaders reveal that the agency budget will not allow for new hires. Based on this new knowledge and information from the section above, what is a TeamSTEPPS intervention that does not lead to additional costs for the agency and would help the CMs who are overwhelmed?
Quality Improvement Example
This section will detail a quality improvement project implemented in a hospice/palliative care setting.
Quality Improvement Project: International Cancer Center
Although QI is a relatively new concept in hospice/palliative care, one group of clinical researchers implemented an intervention to improve the efficiency of care in a palliative care setting. According to a 2021 study in BMJ, the Palliative Care Department at an international tertiary care center observed that patients on palliative care occupied 35% – 50% of all beds in the Comprehensive Cancer Center (5).
The bed overcapacity contributed to staff shortages and increased provider workloads. According to the study, bed overcapacity also disrupts services, including emergency room (ER), internal medicine, and surgery, by displacing patients with cancer and unplanned ER visits. The length of hospital stay was also impacted, with patients staying for an average of 28 days.
The Palliative Care Department established a QI team to implement a new project to decrease bed occupancy.
Collecting and Reviewing the Data
First, data was collected, including bed occupancy rates, length of stay days, average number of unplanned ER visits, and cost of care for patients on palliative care. Data review revealed an average bed occupancy of 30 (out of 87 total beds in the cancer center), average length of stay of 28 days, an average of 7.9 collective unplanned ER visits in a year, and the collective annual cost of care of $18,170,000.
Establishing the QI Team
After reviewing data, the Palliative Care Department received support from leaders and established a QI team. The team included representatives from patient/family support (six members), hospice and home care services (four members), other disciplines (four members), and the national lead.
Utilizing a 100-Day Strategy, the team established additional tasks, including:
- Recruiting team members with appropriate skills to carry out the plan
- Coming to a consensus on the team members’ roles and responsibilities
- Assigning a project manager with leadership skills
- Assigning focus areas to individuals
The team planned frequent multidisciplinary meetings to address weekly challenges, obstacles, and successes.
Setting Goals and Measures
The team’s ultimate goal was to implement a plan to improve and manage patient flow by overcoming the center’s bed overcapacity problem. Two measures were identified: overbed capacity reduction and average length of stay.
While the team planned a total implementation phase of 4 years, two initial five-month SMART goals were set:
- Goal 1: Reduce the Comprehensive Cancer Center’s bed overcapacity for palliative care patients from 35% in January 2018 to 10% by May 2018.
- Goal 2: Reduce the average length of stay of palliative care patients from 28 days in January 2018 to 20% in May 2018.
Implementing the Intervention
After setting goals, the team initiated a Future State Pathway Map for Palliative Care—an approach in which patients admitted to palliative care are triaged appropriately, assessed, and given a referral by a health provider within a specified number of hours after admission. The map also included family meetings, advanced care planning, and assessment by a palliative care team at specific time intervals during the stay. The pathway map was tested using the PDSA cycle over five months.
Evaluating the Goals
After implementation, the team evaluated the initial project goals and found that bed capacity was reduced from 35% to 13.8%, and average length of stay decreased from 28 to 10.8 days. The team also found that unplanned ER visits declined from 7.9 to 5.5, and the total annual care cost was reduced by 69%.
After improvement was observed (although goal 1 was not entirely met), the plan was implemented over the following two years. In 2021, the team reviewed the project goals and found continual improvement each year until 2020, when length of stay and unplanned ER visits increased due to the COVID-19 pandemic.
Ultimately, the team recommended a systematic multidisciplinary approach to improve the capacity and efficiency of palliative care settings. The team also encouraged other organizations to implement the Future State Pathway Map for Palliative Care to validate further and improve this intervention.
Case Study
To relieve overworked CMs, you and your team decided to use the mutual support TeamSTEPPS tool “Task Assistance” to create a new teamwork policy to change the workplace culture. The agency adopted a new slogan, “My patient is your patient.” All CMs who are overwhelmed will now feel safe asking for help when needed, and all CMs who are able to help their peers.
The plan was successfully implemented over three months. Congratulations! After collecting data, brainstorming, setting goals, planning, and implementing, you and your team met the QI goal and will implement the intervention over the next three months. From there, your team can address the documented reasons for late transportation pickup times.

Conclusion
Quality improvement is a way for nurse leaders to make ongoing improvements within healthcare organizations by identifying relevant problems, selecting the right team, and implementing changes across systems. While quality improvement is often associated with hospitals, the principles and methodology may be applied to a vast number of healthcare settings. Quality improvement in hospice acts as a form of continual advocacy for patients at the end-of-life and their families by ensuring the highest level of quality care is provided at all times.
References + Disclaimer
- Agency for Healthcare Quality and Research. (2023). TeamSTEPPS program: Welcome guide for frontline providers. Retrieved from https://www.ahrq.gov/teamstepps-program/welcome-guides/frontline-providers.html
- Agency for Healthcare Research and Quality. (2022). Six domains of healthcare quality. Retrieved from https://www.ahrq.gov/talkingquality/measures/six-domains.html#_ftn1
- Agency for Healthcare Research and Quality. (2023). Talking quality: Measuring the quality of hospice care. Retrieved from https://www.ahrq.gov/talkingquality/measures/setting/long-term-care/hospice.html
- Agency of Healthcare Research and Quality. (2020). Consumer Assessment of Healthcare Providers and Systems (CAHPS): Section 4: Ways to approach the quality improvement process (Page 2 of 2). https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/4-approach-qi-process/sect4part2.html
- Alshammary, S. A., Abuzied, Y., & Ratnapalan, S. (2021). Enhancing palliative care occupancy and efficiency: A quality improvement project that uses a healthcare pathway for service integration and policy development. BMJ Open Quality, 10(4): e001391. Retrieved from https://doi.org/10.1136/bmjoq-2021-001391
- American Society for Quality. (2023). The history of quality. Retrieved from https://asq.org/quality-resources/history-of-quality
- American Society for Quality. (2023). What are the five s’s (5s) of Lean. Retrieved from https://asq.org/quality-resources/lean/five-s-tutorial
- Anderson, J. E., Lavelle, M., & Reedy, G. (2021). Understanding adaptive teamwork in health care: Progress and future directions. Journal of Health Services Research & Policy, 26(3):208-214. Retrieved from https://journals.sagepub.com/doi/10.1177/1355819620978436
- Backhouse, A., & Ogunlayi, F. (2020). Quality improvement into practice. BMJ 2020, 368:m865. Retrieved from https://doi.org/10.1136/bmj.m865
- BerryDunn. (2022). National healthcare at home best practices and future insights study: State of the industry and executive summary. Retrieved from https://advisors.berrydunn.com/hubfs/PDF_Downloads/Healthcare-at-Home-Study.pdf?gclid=LastTest
- Foxwell, A. M. (2022). Palliative and end-of-life care. In: Hinkle JL, Cheever KH, eds. Brunner & Suddarth’s Textbook of Medical-Surgical Nursing. 15th ed. Wolters Kluwer.
- Hines, K., Mouchtouris, N., Knightly, J.J., & Harrop, J. (2020). A brief history of quality improvement. Global Spine Journal, 10(1S):5S-9S. Retrieved from https://journals.sagepub.com/doi/pdf/10.1177/2192568219853529
- Hussain, F.A. (2021). Psychological challenges for nurses working in palliative care and recommendations for self-care. British Journal of Nursing, 30(8). Retrieved from https://www.britishjournalofnursing.com/content/professional/psychological-challenges-for-nurses-working-in-palliative-care-and-recommendations-for-self-care/
- Institute for Healthcare Improvement. (2023). How to improve: Model for Improvement. https://www.ihi.org/resources/how-to-improve
- Institute of Medicine (US) Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: A new health system for the 21st Century. Washington (DC): National Academies Press (US). Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK222265/
- Jones, B., Vaux, E., & Olsson-Brown, A. (2019). How to get started in quality improvement. BMJ, 364: k5408. Retrieved from https://doi.org/10.1136/bmj.k5437
- Leiter, R.E., Pu, C.T., Mazzola, E., et al. (2020). Engaging hospices in quality measurement and improvement: Early experiences of a large integrated health care system. Journal of Pain and Symptom Management, 60(4); P866-873.E4. Retrieved from https://doi.org/10.1016/j.jpainsymman.2020.05.027
- National Archives and Records Administration. (2023). Code of Federal regulations: Part 418 – hospice care. Retrieved from https://www.ecfr.gov/current/title-42/chapter-IV/subchapter-B/part-418
- National Consensus Project for Quality Palliative Care. (2018). Clinical practice guidelines for quality palliative care, 4th edition. National Coalition for Hospice and Palliative Care. Retrieved from https://nationalcoalitionhpc.org/wp-content/uploads/2018/10/NCHPC-NCPGuidelines_4thED_web_FINAL.pdf
- National Hospice and Palliative Care Organization. (2023). Hospice Item Set (HIS). Retrieved from https://www.nhpco.org/regulatory-and-quality/quality/hqrp-hospice-item-set-his/
- National Hospice and Palliative Care Organization. (2022). Regulatory alerts: FY 2023 Medicaid hospice rates and state/county rate charts. Retrieved from https://www.nhpco.org/wp-content/uploads/NHPCO-Reg-Alert_FY-2023-Medicaid-Hospice-Rates.pdf
- National Hospice and Palliative Care Organization. (2023). QAPI toolkit: Professional development and resource series. Retrieved from https://www.nhpco.org/regulatory-and-quality/quality/hospice-quality-updates-resources/qapi-toolkit/qapi-toolkit/
- Talevski, J., Wong Shee, A., Rasmussen, B., Kemp, G., & Beauchamp, A. (2020). Teach-back: A systematic review of implementation and impacts. PloS one, 15(4): e0231350. Retrieved from https://doi.org/10.1371/journal.pone.0231350
- U.S. Centers for Medicare and Medicaid Services. (2023). Hospital quality reporting program (HQRP): Current measures. Retrieved from https://www.cms.gov/medicare/quality/hospice/current-measures
- U.S. Centers for Medicare and Medicaid Services. (2023). Hospice. Retrieved from https://www.cms.gov/medicare/payment/fee-for-service-providers/hospice
- U.S. Centers for Medicare and Medicaid Services. (2023). Quality measures. Retrieved from https://www.cms.gov/medicare/quality/measures
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
