Course
Recognition and Treatment of Narcotic Overdose
Course Highlights
- In this Recognition and Treatment of Narcotic Overdose course, we will learn about the signs and symptoms of narcotic overdose.
- You’ll also learn how to treat and manage an opioid overdose.
- You’ll leave this course with a broader understanding of the important role nurses play in the treatment of a narcotic overdose.
About
Contact Hours Awarded: 2
Course By:
Devon Capristo
MSN, FNP-C
Begin Now
Read Course | Complete Survey | Claim Credit
➀ Read and Learn
The following course content
Introduction
Opioid overdose is a public health epidemic that has been a nationwide concern over the past few decades. In 2021, 106,699 drug overdose deaths occurred in the U.S. with opioids accounting for over 75% of these deaths (5). While data analysis and compilation since 2021 is still ongoing, experts expect the number to have increased over the previous years.
Overdose can happen from prescription or illicit use of opioids or other synthetic, “off the street” forms. Early recognition of symptoms of overdose can make the difference between life and death for patients. Nurses must have the assessment skills to evaluate for potential opioid toxicity and/or overdose when patients arrive in the emergency department (ED). Additionally, nurses should be educated on the proper treatment of opioid overdose in this setting. Proper education and training on this subject can lead to better patient outcomes.

Narcotic vs. Opioids vs. Opiates. What’s the difference?
Multiple terms are used interchangeably when discussing drug use, abuse, and overdose. The following are the most common terms used in healthcare.
Narcotic Drugs
Historically, “narcotic drugs” have been used when describing substances used to dull the senses and relieve pain. Some individuals will use this term to refer to all illicit drugs, but technically speaking, this only refers to opioids. The Centers for Disease Control and Prevention (CDC) now prefers the term “opioid” to avoid confusion (3).
Opiates
Opiates are chemical compounds that come from poppy plant matter. Examples include (15):
- Codeine
- Morphine
- Heroin
- Opium
Opioids
Opioids can be synthetic, semi-synthetic, or natural chemicals that interact with opioid receptors in the brain and body and therefore can reduce pain signals and feelings of pain. This drug class includes illicit heroin, synthetic opioids like fentanyl, and prescription pain medications like morphine, codeine, hydrocodone, oxycodone, and others (3).
Opioid Analgesics
Opioid analgesics are typically referred to as prescription opioids which can be used to treat moderate to severe pain. Additional categories used for mortality data within the CDC include (3):
- Natural opioid analgesics: such as codeine and morphine.
- Semi-synthetic opioid analgesics such as oxymorphone, oxycodone, hydromorphone, and hydrocodone.
- Methadone: synthetic opioid that can be prescribed for pain or used in medication-assisted treatment (MAT) for opioid use disorder (OUD).
- Synthetic opioid analgesics: include tramadol, fentanyl, and methadone

Self-Quiz
Ask Yourself...
- What is the difference between a narcotic, an opioid, and opiates?
- What terms do you use to describe prescription pain medication?
- Out of the three terms (narcotics, opioids, or opiates), which one do you use most frequently in your nursing role?
History of Opioids
As far back as the third millennium BC, the Sumerians cultivated the poppy plant and thus isolated opium from the seed capsules. This civilization called opium “gil” which means joy and they called the poppy “hul gil ” which means “plant of joy.” Over time opium has been used as a euphoriant in religious rituals, representation of different gods by priests, and for treatment of “excessive crying” in children. In the eighth century A.D., Arab traders brought opium to India and China, and then between the 10th and 13th centuries, opium made its way from Asia Minor to all of Europe (1).
After the 1800s, the active ingredient in opium was isolated and named morphine after the god of dreams, Morpheus. Years later codeine was eventually isolated from opium as well and was historically used as a cough suppressant. Around 1850, with the invention of the hypodermic needle, morphine was first used for chronic and post-operative pain (1).
Since this point in history, opioids have been used for pain control, to which the problem of abuse began to arise. The unwarranted use of narcotics (via hypodermic needles) was accelerated during the Civil War from 1861 to 1865 to such an extent that the terms “soldier’s illness” and “army disease” were considered synonymous with addictions to narcotics (16).
Heroin was then developed in the late 1800s, and then marketed by the pharmaceutical company Bayer (13). This “wonder drug” as many called it, was being used for tuberculosis, chronic cough, and respiratory diseases and was thought to be effective in combating addiction to morphine and codeine. It took several years and thousands of patients’ lives for prescribers to see the addictive nature of heroin use. By this time however, drug smugglers had already acquired large supplies of heroin once they realized the analgesic and euphoric properties of the drug, which were much greater per gram than those of morphine (13).

Self-Quiz
Ask Yourself...
- How have opioids been used throughout history?
- Where do opioids come from?
- How have opioids developed over time into what they are now?
- What pharmaceutical company marketed heroin in the late 1800s?
Which Opioid is Common in Overdoses Among Americans?
With so many different types of opioids available to Americans through prescriptions or illegally, it is important to know which ones are causing the most overdoses. Over 150 people daily are dying due to overdoses from synthetic opioids like fentanyl (7). In 2022, the CDC reported that 81.8% of fatal overdose deaths included at least one opioid and illegally made fentanyl (IMF) was the most involved opioid with 74.6% of the deaths. After these IMFs, prescription opioids accounted for 12.5% and heroin 6.1% of the deaths (9). In 2022, there were 96,332 nonfatal overdoses seen in ED visits (8).
The question could then be asked, why fentanyl? There are two types of fentanyl: IMF and pharmaceutical fentanyl. Both are considered synthetic opioids. When prescribed by healthcare providers, fentanyl is useful for severe pain associated with advanced-stage cancer and post-operative pain. IMF can be linked to more overdoses due to the fact it is made with extreme potency, can be made cheaper, is more addictive and dangerous, and is ultimately more powerful. Fentanyl is 50 times stronger than heroin and 100 times stronger than morphine (7).

Self-Quiz
Ask Yourself...
- What opioids are responsible for most overdoses?
- Why is fentanyl the most used drug in overdoses?
Epidemiology
Three Historic Waves
Opioid overdoses have quite an extensive history in the public health sector. Historically, there have been three waves of opioid overdose deaths since the 1990s.
The first wave started in the 1990s when there was an increase in prescription opioids including methadone, natural, and semi-synthetic opioids (4). The spark for this wave was the increased manufacturing of new opioid medications such as immediate release (IR) oxycodone. In 1999 the number of people who admitted to using oxycodone IR for non-medical purposes increased from 400,000 in 1999 to 2.8 million in 2003 (10).
The second wave began in 2010 with abrupt increases in overdose deaths which involved heroin (4). The increase in heroin during this time was possibly because oxycodone IR was reformulated to be abuse-deterrent which likely had an unintended consequence of driving the at-risk population of people misusing oxycodone IR to heroin (11).
The third wave started in 2013, with significant increases involving synthetic overdoses, specifically involving IMF. The market for IMF continues to evolve and can be found in combination with cocaine, counterfeit pills, and heroin (4).
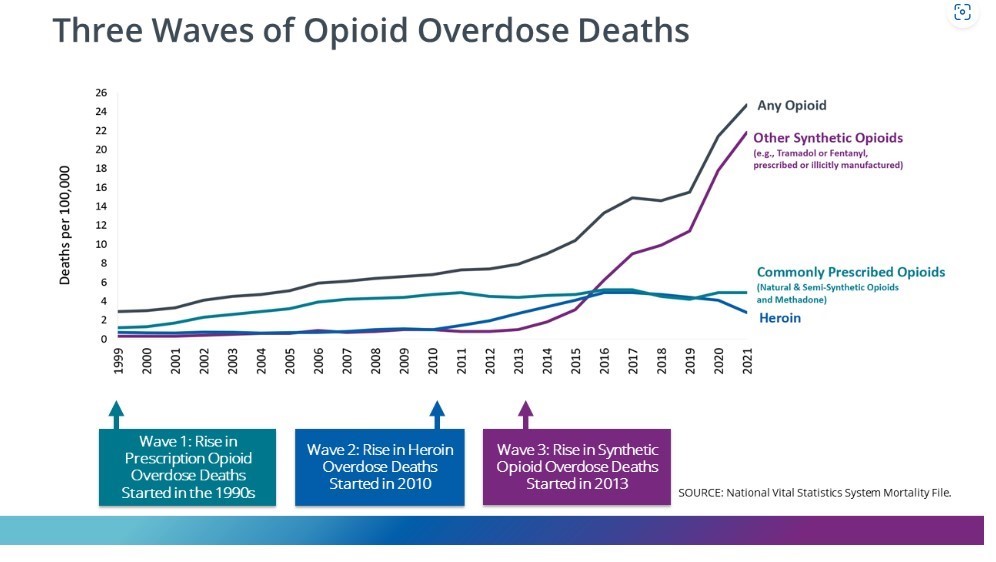
Figure 1. Graph explaining the three waves of opioid overdose deaths from the CDC. (4)

Self-Quiz
Ask Yourself...
- What prior knowledge do you have on the epidemiology of opioid overdoses?
- What were the causes of the three waves of opioid overdose deaths?
- What are the likely reasons that opioid overdoses increased during the COVID-19 pandemic?
Impact of COVID-19
As mentioned above, there have been different waves of increases in opioid overdose deaths. A recent increase happened during the COVID-19 pandemic. There was a 32% increase in opioid overdose deaths (OODs) from 2019 to 2020 (12). The factors that likely increased OODs include increased levels of stress due to isolation, loss of mental health resources, limited access to interventions, changes in the combinations and purity of drugs as well as patterns of drug use (12). It is important to recognize how a global pandemic can affect our society’s response to the opioid crisis and how it is managed.
Etiology
Causes of Overdose
Opioid overdose happens when a person has extreme unimpeded stimulation of the opiate pathway (17). Multiple causes of overdose include but are not limited to (18):
- Chronic problems with substance abuse
- Unintentional (accidental) overdose from:
- Misuse due to dosage errors, forgetting about ingested doses, or failing to read labels
- Over-prescription from healthcare providers accidentally prescribing too high of doses
- Unintentional pediatric exposures
- Failure to recognize active ingredients and taking more than is recommended
- Intentional overdose
- Suicide attempt/intended self-harm
- Attempt to hide drugs from law enforcement with the use of “body stuffing” or “body packing” (when drug-filled packets are ingested or stuffed into body orifices for later retrieval)
Factors Increasing the Risk of Overdose
Patients at increased risk of overdose include (17)(23):
- Patients who return to use after cessation
- Patients who take increasing doses or high prescribed dosages (i.e., more than 100 mg of morphine or equivalent daily)
- Patients with severe mental and medical conditions such as HIV, lung/liver disease, and depression
- Patients who combine opioids with sedatives, barbiturates, anesthetics, benzodiazepines, or other pain medications
- Male patients
- Patients aged 20-24 years old
- Non-Hispanic white patients
- Patients who use prescription opioids without medical supervision
- Patients who take opioids by injection
Pathophysiology
Opiates are derived from the poppy plant and opioids are the chemical substances that can act on these opiate receptors. These opioids function through the endogenous opioid system by acting as an agonist (a substance that acts like another substance) to the mu receptor. This all leads to signals within the cells releasing dopamine, blocking pain signals, and eliciting the sensation of euphoria. These opioid receptors can be found in the gut, spinal cord, and brain. During an overdose, there is an “excessive effect” on the area of the brain that results in respiratory depression and eventually death. Tolerance can occur quickly with opioids and with overdose, patients often succumb to respiratory failure (17). Three main opioid receptors facilitate the effects of opioids. These include delta, kappa, and mu. The chart below lists the three main opioid receptors and their clinical effects.
|
Opioid receptor |
Clinical Effects
|
|
Delta |
Analgesia (absence of pain), inhibition of dopamine release, and suppression of cough.
|
|
Kappa |
Analgesia, dysphoria, miosis and diuresis.
|
|
Mu |
Analgesia, sedation, euphoria, respiratory depression, gastrointestinal motility, physical dependence, decreased response in the medulla to hypercarbia (increase in carbon dioxide), and hypoxia which leads to a decreased stimulus to breathe and development of apnea.
|
Table 1. Opioid Effects by Opioid Receptor (17)(18)

Self-Quiz
Ask Yourself...
- What are the different causes of opioid overdose?
- What increases the risk of a person overdosing on opioids?
- What is the pathophysiology behind opioid overdose?
- What are the three types of opioid receptors that facilitate the effects of opioids?
Clinical Signs and Symptoms
One of the most important assessments of a potential opioid overdose is the history and physical. The clues that you will pick up from the patient and those around will be crucial to the patient’s survival. The typical signs seen in patients who overdose include decreased level of consciousness, pinpoint pupils, and respiratory depression. These are known as the “opioid overdose triad.” Since most patients who have overdosed will be comatose or lethargic, it is important to get as much history as possible from family, friends, bystanders, or even emergency medical providers. At the scene, there may be empty bottles, syringes, needles, pills, or other drug paraphernalia (17).
The following signs and symptoms may be present upon physical examination (17)(18):
Sensory
- Miosis (constricted pupils) (may not be universally present in all patients with opioid overdose)
- Eye redness
- Hearing loss
Integumentary
- Needle track marks
- Patch marks from fentanyl use
- Flushed skin due to urticaria and itching
- Hypothermia
Pulmonary
- Shallow breathing
- Respiratory depression
- Hypopnea (shallow or slow breathing for 10 seconds or longer)
- Bradypnea
- Dyspnea
- Wheezing
- Frothy sputum
Cardiovascular
- Severe hypotension
Gastrointestinal
- Nausea and vomiting
- Decreased bowel sounds
Neurological
- Generalized seizures
- Lethargy or decreased level of consciousness
- Generalized central nervous system (CNS) depression
- Drowsiness
- Alternation in mental status
Psychiatric
- Paranoia
- Anxiety
- Nightmares
- Agitation
- Hallucinations
- Depression
- Dysphoria
- Euphoria


Self-Quiz
Ask Yourself...
- What are the three symptoms of opioid overdose known as the “opioid overdose triad”?
- What is the difference between bradypnea and apnea?
- What body organ systems are present in the signs and symptoms of opioid overdose?
Evaluation
It is important to use additional clinical diagnostic tools to further assess for opioid overdose. Additional physical examinations may need to be performed as well if it appears the patient may have been “body stuffing” any opioids. A vaginal or rectal examination may be required if this has been suspected (17).
Laboratory Studies
The laboratory studies that are commonly performed on a suspected or confirmed opioid overdose patient can include (17)(18):
- Rapid serum glucose concentration: to rule out hypoglycemia which can be confused with opioid toxicity.
- Serum acetaminophen concentration: if an opioid (containing acetaminophen) was taken, or after any overdose resulting from intended self-harm.
- Serum creatinine phosphokinase: to rule out rhabdomyolysis for the patient presenting after prolonged immobilization.
- Arterial blood gases: to determine the oxygenation and ventilation status of the patient.
- Comprehensive metabolic panel: for general evaluation
- Complete blood count: for general evaluation
Diagnostic Studies
The following diagnostic studies are important tools in the treatment and management of an opioid overdose patient (18).
- Electrocardiogram (ECG): should be obtained if a patient is suspected of intended self-harm or if the overdosed drug is likely to cause cardiovascular complications.
- Chest X-ray (CXR): used for patients with adventitious lung sounds or hypoxia that is not corrected when hypoventilation is addressed.
- Abdominal Xray: used in suspected “body packing” patients

Self-Quiz
Ask Yourself...
- What laboratory studies are important to perform on a patient suffering from opioid overdose?
- Why would a serum creatine phosphokinase lab be drawn on an opioid overdose patient?
- Which laboratory study might indicate an overdose patient intended self-harm?
- Why should an ECG be obtained on a suspected opioid overdose patient?
- Why should a CXR be obtained on a suspected opioid overdose patient?
Treatment/Management
Airway
When an opioid overdose or toxicity is suspected, initial management and treatment should always focus on the patient’s airway and breathing. Nurses should pay attention to the depth and rate of ventilation (18). Pulse oximetry is used to monitor the patient’s oxygenation and ventilation is monitored with capnography (18). If airway control has not already been established on the patient at the scene and the patient is showing signs of respiratory failure or distress, the patient should be intubated. Additionally, if no spontaneous circulation is happening, CPR should also be initiated (17).
Antidote Therapy
While initiating the proper airway supportive measures on the patient, an order for naloxone may be ordered if the patient is having respiratory or CNS depression. Naloxone is a short-acting opioid antagonist (18). Naloxone attaches to opioid receptors and blocks and reverses the effects of other opioids which can restore normal breathing in a patient with respiratory depression (20). The goal of naloxone is not a normal level of consciousness but appropriate and adequate ventilation. The preferable route is intravenous in a patient with respiratory complications or impending respiratory arrest. If clinical effects do not occur after 5 to 10 mg of naloxone, additional differential diagnoses should be considered (18).
The following information indicates the dosing for naloxone based on patient presentation:
- Patient with apnea or imminent respiratory arrest:
Patients with apnea should receive higher initial doses of naloxone (0.2 to 1 mg). Patient with cardiorespiratory arrest following potential opioid overdose should be given a minimum of 2 mg. To reduce the risk of acute respiratory distress syndrome, patients with apnea, extremely low respiratory rates, or shallow respirations should be ventilated by a bag-valve mask attached to supplemental oxygen prior to and during naloxone administration (18).
- Patient with spontaneous ventilation:
Patients with spontaneous breathing should receive an initial dose of 0.04 to 0.05 mg intravenously and the dose should be titrated up every few minutes until the respiratory rate is 12 breaths per minute or more (14)(18).
- Patients without IV access:
Naloxone can be given nasally, subcutaneously, intramuscularly, or intraosseously. However, there is slower absorption and delayed elimination with these routes making the drug more difficult to titrate (14)(18).
- Administering naloxone via infusion:
After ventilation has been restored with naloxone, repeat doses may be required. This could be dependent on the quantity and duration of action of the opioid causing the overdose. Instead of repeating dosing, a naloxone infusion can be started by calculating the total initial dose that is required to re-establish breathing and deliver two-thirds of that dose every hour. If the patient begins to develop withdrawal symptoms during this infusion, the infusion needs to be stopped. If the toxicity should return, the infusion can be restarted at half of what the initial rate was. Additionally, if the patient develops respiratory depression during this time, readminister half of the initial starting bolus every few minutes until the patient’s symptoms improve. Then the infusion can be increased by half of the initial rate (18).
Follow-Up Care
Depending on the facility, and of course patient presentation, some patients are released from the ED within a few hours of treatment for opioid overdose. Except for overdoses involving long-acting opioids, such as methadone, most adult patients with opioid toxicity can be released or transferred for psychiatric evaluation once respiratory and mental status are normal and naloxone has not been given for the previous 2-3 hours (18). However, in the case of a large ingestion, the physician should consider the possibility of late absorption of the drug and a longer period of observation may be needed (18).

Self-Quiz
Ask Yourself...
- When an opioid overdose or toxicity is suspected, what should be the focus on treatment?
- What is one way ventilation can be monitored in patients with opioid overdose?
- How can a nurse check a patient’s oxygenation while in the emergency department?
- What is the goal of Narcan (naloxone)?
Prognosis
After an opiate overdose, the major cause of death and morbidity is due to the degree of respiratory depression the patient suffered. The risk of respiratory distress and death is higher in individuals with a prior lung condition. In rare cases, the patient may develop adverse cardiac events, seizures, and/or acute lung injury (17).
In patients who end up in the ED and survive an opioid overdose, the one-year mortality rate is at 5.5% and 20% of these patients will die in the first month after the overdose (21). The first month, and especially the first two days after overdose is the highest-risk period for death after surviving an overdose. These patients should be considered high-risk and receive interventions such as being offered opioid partial agonists like buprenorphine or methadone, counseling, and referred to treatment before discharge from the ED (19)(21). To increase the chances of patients surviving a possible future overdose, the nursing staff must be trained appropriately on these interventions.
Patient Education
Initiation of Medications for Opioid Use Disorder
One of the ways nurses can assist in the opioid epidemic is to educate patients on the medication regimen that can help keep them out of the ED for a future opioid overdose. Some EDs across the country are starting to offer partial opioid agonist, buprenorphine, at discharge. Individuals with opioid use disorder (OUD) who receive medications have been shown to have decreased mortality, ED visits, and overdose compared to those who did not receive medications for their OUD. Initiation of buprenorphine can be taken while still in the ED (directly observed) or at a later time (unobserved). In supplying patients with this medication before discharge, there is improved 30-day treatment retention and a decrease in the days of illicit opioid use (22).
Take-Home Naloxone
Additionally, nurses in the ED can educate patients on the importance of having naloxone readily available for friends, family, or even bystanders in the event of an opioid overdose. Providing naloxone along with education to patients with OUD can reduce overall death rates from opioid overdose. In one study, overdose deaths decreased from 46.6 to 29 per 100,000 after the implementation of an opioid overdose prevention program that included take-home naloxone (18). By 2018, all U.S. states enacted naloxone access laws which permitted the dispensing and administering of naloxone without a physician’s order. By the end of 2023, the U.S. Food and Drug Administration (FDA) approved naloxone for over-the-counter use (18). Making sure that patients are educated about this life-saving medication before discharge is imperative for ED nursing staff.
Harm Reduction Strategies
In addition to the above-mentioned patient education topics, further harm reduction strategies for patients to avoid additional opioid overdoses include but are not limited to peer recovery specialists, motivational interviewing, patient and family education, arranging next-day or same-day appointments at substance abuse disorder programs, distributing alcohol swabs and sterile injection equipment, and offering fentanyl test strips (18). These harm-reduction strategies have been proven to decrease opioid overdoses.

Self-Quiz
Ask Yourself...
- What is the one-year mortality rate after a patient survives an opioid overdose?
- When are patients most at risk of dying following a nonfatal opioid overdose?
- What are three important topics the nurse should focus on when teaching a patient who overdosed on an opioid?
Safety Considerations for Nurses
Occupational Exposure Risk
Nurses and healthcare workers in the ED are at high risk of being exposed to opioids when working with patients coming in from the community. One such opioid that poses the greatest risk and danger is illicit fentanyl and its analogues. Healthcare workers could be exposed when the patient and/or their items are contaminated with fentanyl either in liquid, tablet, or powder forms. The possible exposure routes of most concern include inhaling powder or aerosols, contact with mucous membranes, ingestion, or exposures secondary to a possible break in the skin (2). Any of these routes could lead to the rapid onset of respiratory depression.
Healthy Work Practices
The following work practices should be established when illicit fentanyl is potentially present or known to be present on patients in the healthcare setting (2).
- Coordinate communication with emergency medical services (EMS).
- Assess the area for potential hazards.
- Follow established work practices such as recognizing when entering and leaving potentially contaminated areas.
- Do not eat, drink, smoke, or use the bathroom while working in an area with known or suspected illicit fentanyl.
- Do not touch your nose, mouth, or eyes after touching possible contaminated surfaces.
- Wash hands with soap and water immediately after potential exposure. Do not use alcohol-based hand sanitizer as it can increase absorption through the skin.
- Avoid tasks that might aerosolize illicit fentanyl (i.e., shaking clothing or bedding).
- Notify other healthcare personnel involved with the care of the patient for potential illicit fentanyl contamination risk.
- Launder clothes worn by healthcare workers at the facility in-house if possible. Clothing should be carefully placed in labeled durable 6 mil polyethylene bags and segregated from other laundry until they are laundered.
Personal Protective Equipment (PPE)
Nurses should always be on the lookout for ways in which to protect themselves from accidental opioid exposure. Since healthcare personnel working in the ED could come into contact with fentanyl and other opioids through the patient, they must wear the correct PPE. Personnel should wear at a minimum an N100, R100, or a P100 disposable filtering facepiece respirator or a respirator that offers a higher level of protection. Additionally, face and eye protection can include goggles or a face shield when used with a filtering respirator. Powder-free nitrile gloves should be worn along with wrist and arm protection that can cover exposed skin (2).


Self-Quiz
Ask Yourself...
- What is the most dangerous opioid to be exposed to while working in the ED?
- Name three healthy work practices when working with patients who have overdosed on opioids to avoid possible self-exposure.
- What personal protective equipment (PPE) would you expect to use when taking care of patients who have overdosed?
- What key points can you take away from this course that can help you in recognizing and treating opioid overdose?
Conclusion
Opioid overdose is very common in the United States and with nurses at the frontline in the ED, this epidemic could have more positive outcomes if handled correctly. It is important for nurses to recognize the signs and symptoms of overdose in patients and to act quickly to provide the appropriate treatment for a patient in overdose. Additionally, nurses need to stay aware of any new treatments or guidelines to help those suffering from overdose. While staying up to date on this education, nurses can act quickly, treat appropriately, and educate patients to help save lives and make progress in the opioid overdose epidemic.
References + Disclaimer
- Brownstein, M. J. (1993). A brief history of opiates, opioid peptides, and opioid receptors. Proceedings of the National Academy of Sciences, 90(12), 5391–5393. https://doi.org/10.1073/pnas.90.12.5391
- Centers for Disease Control and Prevention. (2018, April 23). Preventing occupational exposure to Fentanyl. Centers for Disease Control and Prevention. https://www.cdc.gov/niosh/topics/fentanyl/healthcareprevention.html
- Centers for Disease Control and Prevention. (2021, January 26). Commonly used terms. Centers for Disease Control and Prevention. https://www.cdc.gov/opioids/basics/terms.html
- Centers for Disease Control and Prevention. (2023, August 8). Understanding the opioid overdose epidemic. Centers for Disease Control and Prevention. https://www.cdc.gov/opioids/basics/epidemic.html
- Centers for Disease Control and Prevention. (2023, August 22). Drug overdose deaths. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/deaths/index.html#:~:text=Drug%20Overdose%20Deaths%20Remained%20High,1999%20from%20a%20drug%20overdose.&text=In%202021%2C%20106%2C699%20drug%20overdose,2021%20(32.4%20per%20100%2C000).
- Centers for Disease Control and Prevention. (2023, August 23). Opioid overdose. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/deaths/opioid-overdose.html
- Centers for Disease Control and Prevention. (2023, September 6). Fentanyl facts. Centers for Disease Control and Prevention. https://www.cdc.gov/stopoverdose/fentanyl/index.html
- Centers for Disease Control and Prevention. (2024, January 22). Dose dashboard: Nonfatal overdose emergency department and inpatient hospitalization discharge data. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/nonfatal/dose/discharge/dashboard/index.html
- Centers for Disease Control and Prevention. (2024, February 26). Sudors dashboard: Fatal overdose data. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/fatal/dashboard/index.html
- Center for Drug Evaluation and Research. (n.d.). Substance use and overdose prevention timeline. U.S. Food and Drug Administration. https://www.fda.gov/drugs/information-drug-class/timeline-selected-fda-activities-and-significant-events-addressing-substance-use-and-overdose
- Ciccarone, D. (2019). The triple wave epidemic: Supply and demand drivers of the US opioid overdose crisis. International Journal of Drug Policy, 71, 183–188. https://doi.org/10.1016/j.drugpo.2019.01.010
- Ghose R, Forati AM, Mantsch JR. Impact of the COVID-19 Pandemic on Opioid Overdose Deaths: a Spatiotemporal Analysis. J Urban Health. 2022 Apr;99(2):316-327. doi: 10.1007/s11524-022-00610-0. Epub 2022 Feb 18. PMID: 35181834; PMCID: PMC8856931.
- History of Heroin. United Nations: Office on Drugs and Crime. (1953, January 1). https://www.unodc.org/unodc/en/data-and-analysis/bulletin/bulletin_1953-01-01_2_page004.html
- Naloxone: Drug Information. UpToDate Lexidrug. (n.d.). https://www.uptodate.com/contents/naloxone-drug-information?search=opioid+overdose&topicRef=300&source=see_link#references. Retrieved March 21, 2024
- Opiates or opioids – what’s the difference? Alcohol and Drug Policy Commission : Opiates or Opioids – What’s the difference? : State of Oregon. (n.d.). https://www.oregon.gov/adpc/pages/opiate-opioid.aspx
- Quinones, M. A. (1975). Drug abuse during the Civil War (1861–1865). International Journal of the Addictions, 10(6), 1007–1020. https://doi.org/10.3109/10826087509028357
- Schiller EY, Goyal A, Mechanic OJ. Opioid Overdose. 2023 Jul 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 29262202.
- Stolbach, A., & Hoffman, R., (2024). Acute opioid intoxication in adults. UpToDate. Retrieved March 20, 2024, from https://www.uptodate.com/contents/acute-opioid-intoxication-in-adults?search=opioid%20overdose&source=search_result&selectedTitle=1%7E150&usage_type=default&display_rank=1#H22
- Strain, E., & Peavy, M., (2024). Opioid use disorder: Treatment overview. UpToDate. Retrieved March 26, 2024, from https://www.uptodate.com/contents/opioid-use-disorder-treatment-overview?search=opioid%20use%20disorder&source=search_result&selectedTitle=1%7E150&usage_type=default&display_rank=1#H569784101
- U.S. Department of Health and Human Services. (2024, February 12). Naloxone drug facts. National Institutes of Health. https://nida.nih.gov/publications/drugfacts/naloxone#:~:text=It%20is%20an%20opioid%20antagonist,because%20of%20an%20opioid%20overdose.
- Weiner, S. G., Baker, O., Bernson, D., & Schuur, J. D. (2020). One-year mortality of patients after emergency department treatment for nonfatal opioid overdose. Annals of Emergency Medicine, 75(1), 13–17. https://doi.org/10.1016/j.annemergmed.2019.04.020
- Whiteside, L. K., D’Onofrio, G., Fiellin, D. A., Edelman, E. J., Richardson, L., O’Connor, P., Rothman, R. E., Cowan, E., Lyons, M. S., Fockele, C. E., Saheed, M., Freiermuth, C., Punches, B. E., Guo, C., Martel, S., Owens, P. H., Coupet, E., & Hawk, K. F. (2022). Models for implementing emergency department–initiated buprenorphine with referral for ongoing medication treatment at emergency department discharge in Diverse Academic Centers. Annals of Emergency Medicine, 80(5), 410–419. https://doi.org/10.1016/j.annemergmed.2022.05.010
- World Health Organization. (2023, August 29). Opioid overdose. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/opioid-overdose#:~:text=Opioids%20include%20heroin%2C%20morphine%2C%20codeine,overdose%20can%20lead%20to%20death.
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
➁ Complete Survey
Give us your thoughts and feedback
➂ Click Complete
To receive your certificate
