Renal Cancer
Contact Hours: 2.5
Author(s):
R.E. Hengsterman MSN, RN
Course Highlights
- In this Renal cancer course, we will learn about the clinical symptoms of renal cancer.
- You’ll also learn the various treatment modalities for renal cancer.
- You’ll leave this course with a broader understanding of the epidemiological data on renal cancer incidence and survival rates.
Introduction
Renal cancer, referred to as kidney cancer, originates in the tissues of the kidneys, which are vital organs responsible for filtering waste from the blood and producing urine within the human body [1]. The most prevalent type of renal cancer is renal cell carcinoma (RCC), accounting for about 90% of cases [2]. Often, multiple tumors may develop in one or both kidneys and can be large by the time of diagnosis. RCC accounts for over 2-3% of all adult malignancies and is the most lethal urologic cancer [3].
The 5-year survival rate for RCC varies by histologic type and metastatic potential, with clear cell RCC often metastasizing to the lungs and chromophobe RCC spreading to the liver. Based on data from individuals diagnosed with cancers of the kidney (or renal pelvis) between 2013 and 2019, the 5-year relative survival rates are as follows: For localized cancer, the survival rate is 93% [4] [5].
Regional cancer rates drop to 74% [4] [5]. For distant cancer, the survival rate is significantly lower at 17% [4] [5]. When combining all SEER stages, the overall 5-year relative survival rate is 78% [4] [5].
Early detection and diagnosis improve prognosis when identifying cancer at a localized stage. The kidneys, two bean-shaped organs located in the middle to lower part of the back on either side of the spine, filter waste and excess fluid from the blood [14]. This waste exits the body as urine through tubes called ureters to the bladder and then through the urethra. Besides filtering waste, the kidneys regulate blood pressure and maintain adequate red blood cell levels.
Renal cancer presents with symptoms such as hematuria (blood in the urine), flank pain, and a palpable mass in the abdomen or side [6] [7]. However, many cases are asymptomatic and discovered during imaging studies for other conditions.
Treatment options depend on the stage and grade of the cancer and may include surgery, targeted therapy, immunotherapy, and radiation therapy. Advances in understanding renal cancer’s molecular and genetic underpinnings continue to enhance diagnostic and therapeutic strategies, offering hope for improved patient outcomes.
Ask yourself...
- What role do the kidneys play in the human body, and how does renal cancer impact their functions?
- How do survival rates for renal cell carcinoma (RCC) differ based on the cancer stage at diagnosis, and what factors might contribute to these differences?
- What are the common symptoms of renal cancer, and why might many cases be asymptomatic until advanced stages?
Case Study: Renal Cell Carcinoma in a 64-Year-Old Male
A 64-year-old male with a past medical history of nephrolithiasis, voiding dysfunction, hypertension, and a 30-pack-year smoking history presented to the emergency department (ED) with complaints of hematuria. He also reports intermittent flank pain and unintentional weight loss of 15 pounds over the past six months. Physical examination reveals a palpable mass in the right abdominal region.
Weeks prior, he presented to a neighboring hospital with the same primary complaint, where doctors found him anemic and required a transfusion. During that visit, doctors discovered a right renal mass and referred him to a urologist, but he failed to follow up. Over time, he experienced widespread weakness, fatigue, and discomfort, along with swelling in his left side and abdominal area.
On initial presentation to the ED and examination, the patient’s vital signs were as follows: blood pressure of 119/77 mmHg, pulse rate of 90 bpm, temperature of 98.6°F, respiratory rate of 17 breaths per minute, and oxygen saturation of 100% on room air. He was afebrile. Physical examination reveals pallor, a soft and distended left midline/lower abdomen, and tenderness to palpation (TTP) in the left flank, with normal bowel sounds.
The laboratory findings reveal significant abnormalities. The complete blood count (CBC) showed leukocytosis with a white blood cell count of 15,000/µL (normal range: 4,500-11,000/µL), anemia with a hemoglobin level of 9 g/dL (normal range: 13.8-17.2 g/dL), and thrombocytosis with a platelet count of 500,000/µL (normal range: 150,000-450,000/µL). These results suggest an underlying inflammatory process or malignancy.
The basic metabolic panel (BMP) shows an elevated creatinine at 2.1 mg/dL (normal range: 0.6-1.2 mg/dL) and blood urea nitrogen (BUN) at 30 mg/dL (normal range: 7-20 mg/dL), indicating renal dysfunction or impairment associated with renal cancer.
The diagnostic workup began with an initial ultrasonography, which indicated a suspicious mass in the right kidney. This prompted further evaluation with a CT scan, which confirmed the presence of a large, irregularly shaped mass consistent with renal cell carcinoma (RCC). The biopsy identified the mass as clear cell renal cell carcinoma (CCRCC), the most common subtype of RCC.
Additional imaging, including a chest CT, revealed metastasis to the lungs. The treatment plan included a radical nephrectomy to remove the affected kidney, adrenal gland, and surrounding tissues. Post-surgery, doctors initiated targeted therapy with sunitinib, a tyrosine kinase inhibitor, to manage metastatic disease [8]. The medical team also included immunotherapy with a T-cell checkpoint inhibitor to enhance the immune response against cancer cells and regular follow-up visits, with abdominal imaging every six months and chest CT scans to monitor lung metastasis [28].
The primary outcome goals were to prolong progression-free survival and improve overall patient outcomes. Despite the advanced stage of RCC, the combination treatment offered a hopeful prognosis, leveraging recent advancements in RCC management.
This case highlights the importance of early detection and comprehensive management of renal cell carcinoma (RCC). Well-timed diagnosis, surgical intervention, and advanced therapeutic strategies influence the patient’s prognosis and treatment success. Continued advancements in understanding RCC’s molecular and genetic underpinnings are essential in improving diagnostic accuracy and developing more effective treatment protocols for patients with renal cancer.
Ask yourself...
- What risk factors and clinical history in this patient might have contributed to the development of renal cell carcinoma (RCC)?
- How do the laboratory findings and imaging results support the diagnosis of clear cell renal cell carcinoma (CCRCC) in this patient?
- What are the key components of this patient’s treatment plan, and how do they address both the primary tumor and metastatic disease?
- Why is early detection critical in managing renal cell carcinoma, and what strategies can improve early diagnosis and treatment outcomes?
The Cell Growth and Death Cycle
Cancer arises when cells in the body undergo rapid abnormal growth [9]. The cycle of cell growth and death, also known as the cell cycle, is a series of stages that a cell undergoes to grow, replicate its DNA, and divide. This process ensures the maintenance, growth, and repair of tissues. The cell cycle consists of four main phases: G1 (Gap 1), S (Synthesis), G2 (Gap 2), and M (Mitosis) [10]. Cells can also enter a resting state called G0.
G1 Phase (Gap 1)
During G1, the cell grows and synthesizes various proteins and organelles [10]. This stage is essential for the cell to get ready for DNA replication. Cells also monitor their environment to ensure conditions are favorable for division.
S Phase (Synthesis)
In the S phase, the cell duplicates its DNA, ensuring each daughter cell has an identical set of chromosomes [10]. This replication regulates and involves synthesizing new DNA strands based on the existing templates.
G2 Phase (Gap 2)
During G2, the cell grows and produces proteins and organelles [10]. G2 examines the duplicated DNA for errors and performs any needed repairs. This phase guarantees that the cell is adequately prepared to proceed to mitosis.
M Phase (Mitosis)
Mitosis is the procedure through which a cell splits into two identical daughter cells. This process is composed of several stages:
- Prophase: Chromosomes condense, breaking the nuclear envelope down [10].
- Metaphase: Chromosomes align in the center of the cell [10].
- Anaphase: The cell pulls sister chromatids apart to opposite ends [10].
- Telophase: Nuclear envelopes re-form around the separated chromatids, called chromosomes [10].
- Cytokinesis: The cytoplasm divides, resulting in two daughter cells [10].
- G0 Phase (Resting-State)
Cells can enter a resting state called G0, where they are not prepared to divide [10. Some cells, such as nerve cells, may remain in G0 for an extended period. Other cells can re-enter the cell cycle when conditions become favorable.
Ask yourself...
- How does the cell cycle regulate the growth and division of cells, and what are the key phases involved in this process?
- What role does the S phase play in ensuring the accuracy of cell division, and how might errors during this phase contribute to cancer development?
- Why is the G2 phase critical for preparing a cell for mitosis, and what mechanisms are in place to repair DNA damage before cell division?
- How do abnormalities in the regulation of the cell cycle lead to uncontrolled cell growth, and what implications does this have for cancer treatment strategies?
Cell Death
Apoptosis is a regulated process that eliminates damaged or unnecessary cells [11] [12]. It is essential for maintaining tissue homeostasis and preventing the accumulation of harmful cells. Apoptosis involves a series of biochemical events that lead to characteristic cell changes and eventual death without causing an inflammatory response. Necrosis is an uncontrolled cell death that occurs in response to injury or infection [12]. Unlike apoptosis, necrosis often results in inflammation and damage to surrounding tissues.
The cell life-death cycle is repetitive, but cancer cells continue to grow, often forming a mass known as a tumor. Over time, these cancer cells can invade nearby tissues and spread to other body parts, a process called metastasis [13].
Ask yourself...
- How does apoptosis differ from necrosis regarding its processes and effects on surrounding tissues, and why is apoptosis critical for tissue homeostasis?
- What mechanisms allow cancer cells to evade apoptosis, and how does this contribute to tumor formation and metastasis?
Epidemiology
The incidence of renal cell carcinoma (RCC) varies across different regions across the globe, with the highest rates observed in the Czech Republic and North America [14][15]. In the United States, 82,000 new cases of RCC occur per year, with 15,000 resulting in death [14]. Worldwide, over 400,000 new cases of RCC arise each year, leading to over 170,000 deaths from kidney cancer [14][15].
RCC occurs about twice as often in males as in females and affects individuals aged 60 to 80, with a median age at diagnosis of around 64 years [16]. It is uncommon for those under 40 and children [17].
In the United States, the incidence of renal cancers is lowest among Asian American and Pacific Islander patients compared to other ethnicities [14][15]. The five-year survival rate for Black American patients is similar to that of White American patients, exceeding 75 percent [18].
Since 1975, the incidence of renal cell carcinoma (RCC) has increased, though this rise has slowed in recent years [19]. This trend is due to the detection of asymptomatic and early-stage renal cancer cases facilitated by advances in imaging techniques. Physicians detect over half (60%) of RCC cases as incidental findings [20].
RCC constitutes over 3% of all adult malignancies and has various histological subtypes [21]. The American Cancer Society expects the United States to see 81,610 new cases of kidney cancer in 2024, with 52,380 in men and 29,230 in women [16]. This number includes all types of kidney and renal pelvis cancers. The society also estimates that 14,390 people will die from kidney cancer in 2024, with 9,945 men and 4,940 women [16].
The overall 5-year relative survival rate in the United States for patients diagnosed with early-stage RCC is 93% [16][18]. Patients with early-stage disease represent about two-thirds of all diagnosed renal cancer cases [22]. The overall survival rate for kidney and renal pelvis cancers stands at 75% [16][18].
RCC, originating from the renal epithelium, includes over 10 histological and molecular subtypes [23]. Recent genomic studies have identified significant mutations and intra-tumor heterogeneity, impacting prognosis and treatment strategies [23]. Surgery can manage localized RCC, while conventional chemotherapy struggles to treat metastatic RCC [24].
However, researchers have significantly advanced in treating metastasis with targeted agents and immunotherapies [28]. This overview of RCC covers its biology, focusing on clear cell RCC, and provides updates on clinical guidelines and potential future research directions. RCC, also known as hypernephroma or Grawitz tumor, affects adults aged 50 to 70, with a male-to-female ratio of approximately 2:1 [25].
Ask yourself...
- How does the incidence and mortality of renal cell carcinoma (RCC) vary across different regions and demographics, and what factors might contribute to these variations?
- What trends have emerged in the incidence of renal cell carcinoma (RCC) since 1975, and how have advancements in imaging techniques influenced these trends?
- How do the survival rates for renal cell carcinoma (RCC) differ based on the stage at diagnosis, and what implications does this have for early detection and treatment strategies?
- What advancements exist in the treatment of metastatic renal cell carcinoma (RCC), and how do these developments change the prognosis for patients with advanced disease?
Etiology
Primary risk factors for RCC include tobacco use and obesity, with half of RCC cases having the potential to be preventable through the control of these factors [26]. Both cigarette smokers and users of pipes and cigars are at elevated risk [26]. Obesity in women is another significant contributor [26]. Studies estimate that eliminating tobacco use and excess body weight could reduce the incidence of kidney cancers by half [27].
Other risk factors include high blood pressure, chronic renal failure, and exposure to certain chemicals, specifically chemicals like trichloroethylene [28]. Moderate alcohol consumption (up to about two drinks per day), a diet rich in fruits and vegetables, and long-term consumption of fatty fish are associated with a reduced risk of kidney cancer [29].
RCC is a heterogeneous group of neoplasms with distinct histologic, cytogenetic, and imaging characteristics [30]. The three main subtypes are clear cell (70%), papillary (10%), and chromophobe (5%), each with unique radiologic appearances [30]. Less common subtypes include carcinoma of the collecting ducts of Bellini, renal medullary carcinoma, and Xp11.2 translocation carcinoma [21].
Genetic factors also play a crucial role in the development of RCC [31]. The VHL gene implicates both sporadic and familial types of clear cell RCC (CCRCC), while mutations in the MET gene characterize familial papillary RCC (PRCC) [31].
Almost 4% of renal cell cancers arise from rare hereditary conditions, including the following:
Von Hippel-Lindau (VHL) Syndrome: Associated with cysts and tumors in various organs, including pancreatic neuroendocrine tumors, cerebellar and spinal hemangioblastomas, and multiple bilateral tumor nodules of clear cell RCC [32].
Hereditary Leiomyomatosis and Aggressive Papillary Carcinoma Syndrome: An autosomal dominant disease caused by mutations in the FH gene, linked to uterine leiomyomatosis and early metastatic spread of papillary RCC [33].
Hereditary Papillary Carcinoma: An autosomal dominant condition characterized by mutations in the MET gene, resulting in bilateral and multiple papillary tumors with various cytogenetic abnormalities [34].
Birt-Hogg-Dubé Syndrome: This autosomal dominant disease involves mutations in the BHD gene, presenting a range of renal tumor histologies and associated features such as fibrofolliculomas, trichodiscomas, acrochordons, and pulmonary cysts [35].
Tuberous Sclerosis Syndrome: Caused by mutations in the TSC1 and TSC2 genes, leading to multiple bilateral renal angiomyolipomas, CCRCC, and various extra-renal manifestations [36].
Other less common types of kidney cancer include transitional cell carcinoma (also known as urothelial carcinoma), which begins where the ureter and kidney meet (renal pelvis) and resembles bladder cancer; Wilms’ tumor, which occurs primarily in children and is rare in adults; and renal sarcoma, a rare cancer originating in the blood vessels and connective tissue around the kidneys [37] [38].

Ask yourself...
- How do lifestyle factors like tobacco use and obesity contribute to the risk of developing renal cell carcinoma (RCC), and what measures can reduce this risk?
- What role do genetic factors and hereditary conditions play in the development of renal cell carcinoma (RCC), and how do specific genetic mutations influence different RCC subtypes?
- How do environmental exposures and dietary habits influence the risk of renal cell carcinoma (RCC), and what dietary recommendations might help reduce this risk?
- What are the main histologic subtypes of renal cell carcinoma (RCC), and how do their distinct characteristics affect diagnosis and treatment strategies?
Pathophysiology
Experts believe renal cell carcinomas (RCCs) originate from the epithelial cells of the nephron [39]. Clear cell renal cell carcinoma (CCRCC) links to the proximal tubular epithelium, papillary renal cell carcinoma (PRCC) to the distal tubular epithelium, and chromophobe RCC (ChRCC) to the intercalated cells of the collecting duct [39].
In CCRCC, the VHL tumor suppressor gene is the most often mutated [32]. The complete loss of VHL through genetic mechanisms (such as point mutations, indels, and 3p25 loss) and/or epigenetic mechanisms (such as promoter methylation) constitutes the earliest and most crucial oncogenic driving event [32].
Ask yourself...
- How do the origins of clear cell RCC (CCRCC), papillary RCC (PRCC), and chromophobe RCC (ChRCC) from distinct parts of the nephron influence their characteristics and behavior?
- What is the role of the VHL tumor suppressor gene in developing clear cell renal cell carcinoma (CCRCC), and how do genetic and epigenetic mechanisms contribute to its inactivation?
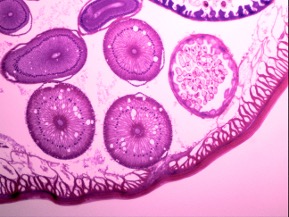
Histopathology
Renal cell carcinoma (RCC) encompasses several types, which a pathologist identifies through microscopic examination of cancer cells. The most common type is clear cell RCC, characterized by pale or clear cells [2]. Papillary RCC, the second most common type, features tumors with tiny fingerlike growths [40]. Chromophobe RCC is a rare form distinguished by larger cells compared to other RCC types [41].
Collecting duct RCC, another rare form, has cancer cells resembling irregular tubes [42]. Unclassified RCC consists of tumors with cells from more than one type of cancer or cells that do not fit into other categories [43]. The Modified 2016 World Health Organization (WHO) classification identifies over 14 types of renal cell carcinomas (RCCs) [44].
Clear cell RCC (CCRCC) is the most prevalent type, characterized by a yellow-cut surface due to lipid content, with areas of necrosis and hemorrhage [2]. Tumor cells appear rounded or polygonal with clear or pink granular cytoplasm [45]. Papillary RCC (PRCC), accounting for 10-15% of renal cancers, can be multifocal and bilateral, often presenting with central necrosis and hemorrhages [45]. It comprises two subtypes: Type 1, characterized by small cells with basophilic cytoplasm, and Type 2, identified by large cells with eosinophilic cytoplasm [45].
Chromophobe RCC (ChRCC), comprising about 5% of RCCs, arises from intercalated collecting duct cells and presents with a lobulated orange surface that turns grayish-white on formalin fixation [46]. Tumor cells have a transparent, reticulated cytoplasm and thick-walled vasculature [46]. Collecting duct carcinoma, making up about 1% of RCCs, originates from medullary collecting duct cells and features irregular channels lined by atypical epithelium within a prominent fibrotic stroma. Distinguish this type from medullary carcinoma associated with sickle cell trait [47] [48].
Ask yourself...
- What are the distinguishing microscopic characteristics of the distinct types of renal cell carcinoma (RCC), and how do these features help pathologists diagnose each type?
- How do the histopathological features of clear cell RCC (CCRCC) and papillary RCC (PRCC) differ, and what are the implications of these differences for prognosis and treatment?
- Why is it important to identify and differentiate between the various subtypes of renal cell carcinoma (RCC), including rare forms like collecting duct carcinoma, in clinical practice?
Differential Diagnosis
Half of the renal cell carcinomas (RCCs) are incidental findings, with the disease being often asymptomatic [20]. Consider RCC when detecting a renal mass in a radiologic study. Include various conditions in the differential diagnosis that can mimic RCC when a client presents with a renal mass.
These conditions include [49]:
- Abscess
- Angiomyolipoma (benign neoplasm)
- Renal oncocytoma (benign neoplasm)
- Renal adenoma (benign neoplasm)
- Renal lymphoma
- Renal cyst
- Renal infarction
- Sarcoma
- Metastasis from distant primary lesions, such as metastatic melanoma
Differential diagnoses based on clinical findings may include [50]:
- Acute pyelonephritis
- Bladder cancer
- Chronic pyelonephritis
- Non-Hodgkin lymphoma
- Differential Adult-type Wilms tumor
Renal cell carcinomas (RCCs) can remain asymptomatic until the disease has progressed. Only 10 to 15% of clients exhibit the “classic triad” of symptoms: flank pain, hematuria, and fullness [51]. More than 60% of clients present with asymptomatic hematuria [49]. Other common symptoms include fatigue, weight loss, fever, night sweats, malaise, hypertension, and anemia [49]. Varicocele can occur due to tumor invasion and growth into the renal vein and inferior vena cava, obstructing the testicular vein [52].
When present, Hypercalcemia indicates either bony metastasis or a paraneoplastic phenomenon [53]. Bone metastasis from RCC is often osteolytic, leading to pathologic fractures, spinal cord compression, and hypercalcemia [54].
Sharp, excruciating, band-like back pain may result from vertebral collapse and spinal cord compression caused by metastatic disease, aiding in the diagnosis of metastatic renal cell carcinoma [54].
One-third of clients with RCC have metastatic disease at the time of diagnosis [55]. Therefore, a thorough physical examination should include an evaluation for metastasis to the lungs (75%), bones (20%), liver (18%), central nervous system (8%), and other areas [56].

Ask yourself...
- What conditions should you consider in the differential diagnosis of a renal mass detected during a radiologic study, and how do these conditions mimic renal cell carcinoma (RCC)?
- Why is it important to include both benign and malignant conditions in the differential diagnosis of renal masses, and how does this impact the diagnostic approach and management plan?
- How do the symptoms and clinical findings of renal cell carcinoma (RCC) overlap with other conditions like acute pyelonephritis and bladder cancer, and what are the key indicators that can help distinguish RCC from these conditions?
- What are the implications of metastatic disease in renal cell carcinoma (RCC), and why is it crucial to perform a thorough physical examination and evaluation for metastasis at the time of diagnosis?
Diagnostic Testing
The most utilized tests for renal assessment include renal ultrasonography, which is often the initial study [57]. The initial evaluation may also involve a CT excretory urogram. Confirmation requires a staging CT of the abdomen and pelvis. To check for lung metastasis, perform a chest X-ray or CT scan. Use magnetic resonance imaging (MRI) to detect venous invasion and metastatic tumor progression [57].
After confirming renal cell carcinoma (RCC), conduct renal arteriography and venography if you suspect inferior vena cava involvement [57]. Measure bone scan and alkaline phosphatase levels to diagnose or assess bone metastasis and for follow-up [57]. Perform a CT head scan if you suspect cerebral metastasis. Recommend genetic testing for patients suspected of having a hereditary disease due to age at presentation or a family history of RCC [58]. Use ultrasound or CT-guided percutaneous needle biopsy for suspicious and cystic lesions suspected to be malignant [59].
Ask yourself...
- Why is renal ultrasonography often the initial study for renal assessment, and how does it guide subsequent diagnostic testing for renal cell carcinoma (RCC)?
- What is the significance of using multiple imaging modalities (CT, MRI, chest X-ray) and additional tests (bone scan, genetic testing) in the comprehensive evaluation and staging of renal cell carcinoma (RCC)?
Treatment
The management and prognosis of RCC depend on tumor staging, grading, and characteristics such as the degree of invasion, venous thromboembolic involvement, and the extent of necrosis [57]. Treatment varies based on tumor size and location. Smaller tumors confined to one kidney pole are treated with partial nephrectomy, while larger tumors may require partial or radical nephrectomy [60].
Targeted therapies, like tyrosine kinase inhibitors, have shown efficacy in improving progression-free survival. Novel immunotherapeutic agents, such as T-cell checkpoint inhibitors, show promise in treating metastatic RCC [61].
The primary treatment for kidney cancer involves surgery, known as nephrectomy. This procedure removes the kidney and includes distinct types. A radical nephrectomy removes the entire kidney, the adrenal gland, surrounding tissues, and sometimes nearby lymph nodes. A simple nephrectomy removes only. A partial nephrectomy involves removing only the tumor-containing part of the kidney. The remaining kidney can compensate and perform the functions of both kidneys.
Radiation therapy, which uses high-energy X-rays to destroy cancer cells, is sometimes employed to alleviate pain when kidney cancer metastasizes to the bones. Targeted therapy, which utilizes drugs designed to attack specific components of cancer cells, is often the first-line treatment for advanced kidney cancer due to its mild side effects compared to standard chemotherapy. Examples of first-line drugs include sunitinib, sorafenib, temsirolimus, everolimus, bevacizumab, and pazopanib [61].
Biological therapy, or immunotherapy, leverages the body’s immune system to combat cancer. Chemotherapy, the use of drugs to kill cancer cells, is less effective for kidney cancer due to the cancer’s resistance to these drugs. Arterial embolization is another treatment option that involves injecting small pieces of material through a catheter to block the main renal blood vessel, thus starving the tumor of necessary nutrients and oxygen. This method can shrink the tumor before surgery or relieve pain when surgery is not feasible.
Ask yourself...
- What is biological therapy?
- What is radiation therapy?
- What is the primary treatment for renal cancer?
Accurate Staging for Effective Management of Renal Cell Carcinoma
Stage 1a: Treat tumors confined to the kidney with curative intent using a nephron-sparing partial nephrectomy. The National Comprehensive Cancer Network (NCCN) recommends an abdominal CT or MRI within six months of starting surveillance, followed by annual imaging [57].
Stage 1b: Partial or radical nephrectomy yields similar outcomes. Post-surgery follow-up includes baseline abdominal imaging (CT, MRI, or ultrasound) 3-12 months after surgery, then annually for three years, and chest X-rays for three years [57].
Stages 2 and 3: Recommend radical nephrectomy and schedule follow-up imaging at 3 to 6 months post-surgery, then every 3-6 months for three years, and per year up to five years. Perform additional site-specific imaging as needed [57].
Stage 4: Systemic targeted molecular therapies, such as tyrosine kinase inhibitors (TKIs) targeting vascular endothelial growth factors (e.g., sunitinib, sorafenib, pazopanib, axitinib) or rapamycin inhibitors (e.g., temsirolimus, everolimus), have replaced immunotherapy (e.g., interferon-α). Nephrectomy followed by immunotherapy improves survival in patients with metastatic RCC compared to using immunotherapy or TKIs alone. Follow-up includes pretreatment imaging (CT or MRI of the chest, abdomen, and pelvis), with repeat imaging every 6 to 16 weeks based on clinical status [57][60][61].

Ask yourself...
- How do the size and location of renal cell carcinoma (RCC) tumors influence the choice between partial and radical nephrectomy, and what are the benefits and risks associated with each surgical approach?
- What roles do targeted therapies and immunotherapies play in treating metastatic RCC, and how have these treatments improved progression-free survival compared to traditional chemotherapy?
- Why is accurate staging critical for managing RCC, and how does the treatment approach differ across various stages of the disease?
- How does arterial embolization function as a treatment option for RCC, and in what scenarios is it particularly beneficial compared to other treatment methods?
- What is the difference between stage 4 and stage 3?
Prognosis
The 5-year relative survival rate for renal cell carcinoma (RCC) stands at 75%. Diagnosing two-thirds of cases at a local stage results in a 93% 5-year relative survival rate. Predict prognosis based on the stage and grade of the cancer [57]. Cancer-specific survival rates range from 85-90% for localized (stages 1 and 2) RCC.
The International Society of Urological Pathology (ISUP) Grading System, proposed in 2012 and later adopted by the World Health Organization (WHO), includes more objective criteria for tumor grading based on nuclear characteristics [57]. These criteria encompass the degree of tumor invasion, the presence and extent of venous thromboembolic involvement, adrenal gland involvement, tumor grade, sarcomatoid features if present, lymphovascular invasion, and the extent of necrosis. The ISUP system no longer grades chromophobe RCC. Higher grades correlate with larger tumor sizes and more aggressive tumors.
Categorize prognostic factors for RCC into three main groups: tumor-related factors, patient-related factors, and laboratory biochemical tests [57]. Integrating these factors into algorithms enhances prognostic accuracy beyond a simple anatomic tumor stage, thereby improving management decisions. Tumor-related factors include stage, tumor size, tumor grade, histologic type, histologic tumor necrosis, and sarcomatoid transformation [57].
Patient-related factors involve symptoms (asymptomatic, local symptoms, systemic symptoms), performance status, substantial weight loss, presence of well-defined paraneoplastic syndrome, metastasis-free interval, and history of prior nephrectomy [57]. Laboratory biochemical tests consider elevated LDH levels, hypercalcemia, anemia, thrombocytosis, and elevated ESR or CRP [57].

Ask yourself...
- How do the stage and grade of renal cell carcinoma (RCC) influence the 5-year relative survival rates, and why is early detection crucial for improving prognosis?
- What are the key tumor-related, patient-related, and laboratory biochemical factors that impact the prognosis of RCC, and how do these factors contribute to the overall assessment of a patient’s outlook?
- How does the International Society of Urological Pathology (ISUP) Grading System improve the objectivity and accuracy of tumor grading in RCC, and what are the implications of this system for patient management and treatment outcomes?
- How does early detection and diagnosis of renal cell carcinoma (RCC) improve prognosis, and what are the challenges in detecting RCC in its initial stages?
- What psychosocial resources do you have at your facility to help patients with their prognosis?
Conclusion
Renal cell carcinoma (RCC), a significant form of kidney cancer, originates in the kidneys’ tissues, essential organs that filter waste from the blood and produce urine. RCC accounts for about 90% of kidney cancer cases and is notable for its lethality and prevalence, comprising over 3% of all adult malignancies [2][3].
The most common subtype, clear cell RCC, often metastasizes to the lungs, while chromophobe RCC spreads to the liver. Early detection and diagnosis are crucial, as prognosis improves with early detection. The kidneys’ vital functions, including waste filtration, blood pressure regulation, and red blood cell maintenance, underscore the importance of early intervention in RCC [62].
Symptoms of RCC can include hematuria, flank pain, and a palpable mass, although many cases are asymptomatic and discovered through imaging studies for other conditions [6][7][20]. Treatment options, determined by the cancer’s stage and grade, range from surgery to targeted therapy, immunotherapy, and radiation therapy. Advances in understanding RCC’s molecular and genetic basis have improved diagnostic and therapeutic strategies, enhancing patient outcomes. Despite these advancements, RCC remains challenging to treat, particularly in its metastatic form, highlighting the need for continued research and innovation in therapeutic approaches.
References + Disclaimer
- What is kidney cancer? Renal cancer. (2024). American Cancer Society. https://www.cancer.org/cancer/types/kidney-cancer/about/what-is-kidney-cancer.html
- Tran, J., & Ornstein, M. C. (2022). Clinical Review of the Management of Metastatic Renal cell Carcinoma. JCO Oncology Practice, 18(3), 187–196. https://doi.org/10.1200/op.21.00419
- The Urology Group of Virginia. (2024). Kidney cancer: renal mass | The Urology Group of Virginia. https://www.urologygroupvirginia.com/urologic-cancer-center/kidney-cancer
- Survival rates for kidney cancer. (2024). American Cancer Society. https://www.cancer.org/cancer/types/kidney-cancer/detection-diagnosis-staging/survival-rates.html
- Cancer of the kidney and renal pelvis – Cancer Stat Facts. (2024). SEER. https://seer.cancer.gov/statfacts/html/kidrp.html
- Long, D., & Long, B. (2020). 55-year-old Female with Hematuria. Clinical Practice and Cases in Emergency Medicine, 4(2), 232–233. https://doi.org/10.5811/cpcem.2020.2.46271
- Kidney cancer – Symptoms and causes – Mayo Clinic. (2022, May 25). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/kidney-cancer/symptoms-causes/syc-20352664
- Rathmell, W. K., Rumble, R. B., Van Veldhuizen, P. J., Al-Ahmadie, H., Emamekhoo, H., Hauke, R. J., Louie, A. V., Milowsky, M. I., Molina, A. M., Rose, T. L., Siva, S., Zaorsky, N. G., Zhang, T., Qamar, R., Kungel, T. M., Lewis, B., & Singer, E. A. (2022). Management of Metastatic clear cell Renal cell Carcinoma: ASCO Guideline. Journal of Clinical Oncology, 40(25), 2957–2995. https://doi.org/10.1200/jco.22.00868
- Cancer Research UK. (2024, June 11). Cancer cells. https://www.cancerresearchuk.org/about-cancer/what-is-cancer/how-cancer-starts/cancer-cells
- Uzbekov, R., & Prigent, C. (2022). A Journey through Time on the Discovery of Cell Cycle Regulation. Cells, 11(4), 704. https://doi.org/10.3390/cells11040704
- Apoptosis. (2024). Genome.gov. https://www.genome.gov/genetics-glossary/apoptosis
- Park, W., Wei, S., Kim, B., Kim, B., Bae, S., Chae, Y. C., Ryu, D., & Ha, K. (2023). Diversity and complexity of cell death: a historical review. Experimental and Molecular Medicine/Experimental and Molecular Medicine, 55(8), 1573–1594. https://doi.org/10.1038/s12276-023-01078-x
- What is cancer? (2021, October 11). Cancer.gov. https://www.cancer.gov/about-cancer/understanding/what-is-cancer
- Epidemiology, pathology, and pathogenesis of renal cell carcinoma – UpToDate. (2024). UpToDate. https://www.uptodate.com/contents/epidemiology-pathology-and-pathogenesis-of-renal-cell-carcinoma
- Kim, I., & Lee, H. J. (2022). The Frontline Immunotherapy-Based Treatment of Advanced Clear Cell Renal Cell Carcinoma: Current evidence and Clinical perspective. Biomedicines, 10(2), 251. https://doi.org/10.3390/biomedicines10020251
- Key statistics about kidney Cancer. (2024). American Cancer Society. https://www.cancer.org/cancer/types/kidney-cancer/about/key-statistics.html
- Gopee-Ramanan, P., Chin, S., Lim, C., Shanbhogue, K. P., Schieda, N., & Krishna, S. (2022). Renal neoplasms in young adults. Radiographics, 42(2), 433–450. https://doi.org/10.1148/rg.210138
- Cancer of the kidney and renal pelvis – Cancer Stat Facts. (2024). SEER. https://seer.cancer.gov/statfacts/html/kidrp.html
- Mousavi, S. E., Najafi, M., Aslani, A., Fazlollahi, A., Yekta, Z., Sadri, M., & Nejadghaderi, S. A. (2024). A population-based study on incidence trends of kidney and renal pelvis cancers in the United States over 2000–2020. Scientific Reports, 14(1). https://doi.org/10.1038/s41598-024-61748-2
- Vasudev, N. S., Wilson, M., Stewart, G. D., Adeyoju, A., Cartledge, J., Kimuli, M., Datta, S., Hanbury, D., Hrouda, D., Oades, G., Patel, P., Soomro, N., Sullivan, M., Webster, J., Selby, P. J., & Banks, R. E. (2020). Challenges of early renal cancer detection: symptom patterns and incidental diagnosis rate in a multicentre prospective UK cohort of patients presenting with suspected renal cancer. BMJ Open, 10(5), e035938. https://doi.org/10.1136/bmjopen-2019-035938
- Sepe, P., Ottini, A., Pircher, C. C., Franza, A., Claps, M., Guadalupi, V., Verzoni, E., & Procopio, G. (2021). Characteristics and treatment challenges of Non-Clear cell Renal cell carcinoma. Cancers, 13(15), 3807. https://doi.org/10.3390/cancers13153807
- Padala, S. A., Barsouk, A., Thandra, K. C., Saginala, K., Mohammed, A., Vakiti, A., Rawla, P., & Barsouk, A. (2020). Epidemiology of renal cell Carcinoma. World Journal of Oncology, 11(3), 79–87. https://doi.org/10.14740/wjon1279
- Mohd, A. B., Ghannam, R. A., Mohd, O. B., Elayan, R., Albakri, K., Huneiti, N., Daraghmeh, F., Al-Khatatbeh, E., & Al-Thnaibat, M. (2022). Etiologies, gross appearance, histopathological patterns, prognosis, and best treatments for subtypes of renal carcinoma: an educational review. Curēus. https://doi.org/10.7759/cureus.32338
- Matuszczak, M., Kiljańczyk, A., & Salagierski, M. (2023). Surgical Approach in Metastatic Renal cell Carcinoma: A literature review. Cancers, 15(6), 1804. https://doi.org/10.3390/cancers15061804
- Neşiu, A., Neamţu, C., Nicolescu, C. M., Totolici, B. D., Mureşanu, H. D., Roşu, M. C., Ardelean, A., Silivestru, V. C., Stăniş, L. A., & Marţi, T. D. (2021). Sarcomatoid renal cell carcinoma with clear cells and eosinophilia: a case report and short review of the literature. Romanian Journal of Morphology and Embryology, 62(3), 835–839. https://doi.org/10.47162/rjme.62.3.22
- Makino, T., Kadomoto, S., Izumi, K., & Mizokami, A. (2022). Epidemiology and prevention of renal cell carcinoma. Cancers, 14(16), 4059. https://doi.org/10.3390/cancers14164059
- Safiri, S., Kolahi, A., Mansournia, M. A., Almasi-Hashiani, A., Ashrafi-Asgarabad, A., Sullman, M. J. M., Bettampadi, D., Qorbani, M., Moradi-Lakeh, M., Ardalan, M., Mokdad, A., & Fitzmaurice, C. (2020). The burden of kidney cancer and its attributable risk factors in 195 countries and territories, 1990–2017. Scientific Reports, 10(1). https://doi.org/10.1038/s41598-020-70840-2
- Cancer Research Institute. (2023, July 23). Immunotherapy for kidney cancer – Cancer Research Institute. https://www.cancerresearch.org/cancer-types/kidney-cancer
- Fan, Z., Yun, J., Yu, S., Yang, Q., & Song, L. (2019). Alcohol Consumption Can be a “Double-Edged Sword” for Chronic Kidney Disease Patients. Medical Science Monitor, 25, 7059–7072. https://doi.org/10.12659/msm.916121
- EAU Guidelines on RCC – EPIDEMIOLOGY AETIOLOGY AND PATHOLOGY – UROWeb. (n.d.). Uroweb – European Association of Urology. https://uroweb.org/guidelines/renal-cell-carcinoma/chapter/epidemiology-aetiology-and-pathology
- Alchoueiry, M., Cornejo, K., & Henske, E. P. (2023). Kidney cancer: Links between hereditary syndromes and sporadic tumorigenesis. Seminars in Diagnostic Pathology. https://doi.org/10.1053/j.semdp.2023.11.002
- Von Hippel-Lindau Disease (PDQ®). (2024, June 14). Cancer.gov. https://www.cancer.gov/publications/pdq/information-summaries/genetics/vhl-syndrome-hp-pdq
- Hereditary leiomyomatosis and renal cell carcinoma – Symptoms, causes, treatment | NORD. (2024). National Organization for Rare Disorders. https://rarediseases.org/rare-diseases/hereditary-leiomyomatosis-and-renal-cell-carcinoma/
- Mikhaylenko, D. S., Klimov, A. V., Matveev, V. B., Samoylova, S. I., Strelnikov, V. V., Zaletaev, D. V., Lubchenko, L. N., Alekseev, B. Y., & Nemtsova, M. V. (2020). Case of hereditary papillary renal cell carcinoma type I in a patient with a germline MET mutation in Russia. Frontiers in Oncology, 9. https://doi.org/10.3389/fonc.2019.01566
- Lakhani, D. A., Winkler, L., & Lisle, M. (2022). Birt-Hogg-Dubé syndrome: case report and brief review of the literature. Radiology Case Reports, 17(1), 250–253. https://doi.org/10.1016/j.radcr.2021.10.052
- Nair, N., Chakraborty, R., Mahajan, Z., Sharma, A., Sethi, S. K., & Raina, R. (2020). Renal manifestations of tuberous sclerosis complex. Journal of Kidney Cancer and VHL, 7(3), 5–19. https://doi.org/10.15586/jkcvhl.2020.131
- Upper urinary tract urothelial cancer. (2024). Cancer Research UK. https://www.cancerresearchuk.org/about-cancer/upper-urinary-tract-urothelial-cancer
- National Cancer Institute (US). (2024, June 14). Wilms Tumor and Other Childhood Kidney Tumors Treatment (PDQ®). PDQ Cancer Information Summaries – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK65842/
- Wolf, M. M., Rathmell, W. K., & Beckermann, K. E. (2020). Modeling clear cell renal cell carcinoma and therapeutic implications. Oncogene, 39(17), 3413–3426. https://doi.org/10.1038/s41388-020-1234-3
- Papillary renal cell carcinoma. (2020, March 17). Cancer.gov. https://www.cancer.gov/pediatric-adult-rare-tumor/rare-tumors/rare-kidney-tumors/papillary-renal-cell-carcinoma
- Garje, R., Elhag, D., Yasin, H. A., Acharya, L., Vaena, D., & Dahmoush, L. (2021). Comprehensive review of chromophobe renal cell carcinoma. Critical Reviews in Oncology/Hematology, 160, 103287. https://doi.org/10.1016/j.critrevonc.2021.103287
- Collecting duct carcinoma. (2024). https://www.pathologyoutlines.com/topic/kidneytumormalignantcollectingduct.html
- Sirohi, D., Smith, S. C., Agarwal, N., & Maughan, B. L. (2018). Unclassified renal cell carcinoma: diagnostic difficulties and treatment modalities. Research and Reports in Urology, Volume 10, 205–217. https://doi.org/10.2147/rru.s154932
- Cimadamore, A., Cheng, L., Scarpelli, M., Massari, F., Mollica, V., Santoni, M., Lopez-Beltran, A., Montironi, R., & Moch, H. (2021). Towards a new WHO classification of renal cell tumor: what the clinician needs to know—a narrative review. Translational Andrology and Urology, 10(3), 1506–1520. https://doi.org/10.21037/tau-20-1150
- Rysz, J., Franczyk, B., Ławiński, J., & Gluba-Brzózka, A. (2021). Characteristics of clear cell papillary Renal cell carcinoma (CCPRCC). International Journal of Molecular Sciences, 23(1), 151. https://doi.org/10.3390/ijms23010151
- Alaghehbandan, R., Przybycin, C. G., Verkarre, V., & Mehra, R. (2022). Chromophobe renal cell carcinoma: Novel molecular insights and clinicopathologic updates. Asian Journal of Urology, 9(1), 1–11. https://doi.org/10.1016/j.ajur.2021.11.010
- Suarez, C., Marmolejo, D., Valdivia, A., Morales-Barrera, R., Gonzalez, M., Mateo, J., Semidey, M. E., Lorente, D., Trilla, E., & Carles, J. (2022). Update in collecting duct carcinoma: Current aspects of the clinical and molecular characterization of an orphan disease. Frontiers in Oncology, 12. https://doi.org/10.3389/fonc.2022.970199
- Renal medullary carcinoma – Symptoms, causes, treatment | NORD. (2024). National Organization for Rare Disorders. https://rarediseases.org/rare-diseases/renal-medullary-carcinoma/
- Gray, R. E., & Harris, G. T. (2019, February 1). Renal cell carcinoma: Diagnosis and management. AAFP. https://www.aafp.org/pubs/afp/issues/2019/0201/p179.html
- Lohr, J. W., MD. (2024). Medscape Registration. https://emedicine.medscape.com/article/245464-differential?form=fpf
- Jeelani, H. M. A., Sheikh, M. M., Riaz, A., Jain, N., Tahir, N., Ehsan, H., & Vemireddy, L. (2021). Metastatic renal cell carcinoma complicated by right atrial thrombus. Clinical Case Reports, 9(4), 2332–2335. https://doi.org/10.1002/ccr3.4028
- Adhikari, P., Neeli, S. I., & Mohan, S. (2020). A rare case of right-sided varicocele in right renal tumor in the absence of venous thrombosis and IVC compression. Journal Africain D’urologie (French Additional)/African Journal of Urology/African Journal of Urology, 26(1). https://doi.org/10.1186/s12301-020-00072-3
- Aggarwal, G., Gupta, S., & Khwaunju, P. (2022). Hypercalcemia in Urological Malignancies: A review. Türk Üroloji Dergisi/Turkish Journal of Urology, 48(4), 243–253. https://doi.org/10.5152/tud.2022.22006
- Singh, Y., Barua, S. K., Trivedi, S., Tp, R., Kashyap, M. P., Agrawal, L. K., Pathak, U. K., & Garg, N. (2023). Skeletal-Related events in renal cell carcinoma: prediction with alkaline phosphatase (ALP), C-reactive Protein (CRP), haemoglobin (HB) and erythrocyte sedimentation Rate (ESR) (A.C.H.E.) score for risk stratification. Curēus. https://doi.org/10.7759/cureus.40835
- Assi, H. I., Patenaude, F., Toumishey, E., Ross, L., Abdelsalam, M., & Reiman, T. (2016). A simple prognostic model for overall survival in metastatic renal cell carcinoma. Canadian Urological Association Journal, 10(3–4), 113. https://doi.org/10.5489/cuaj.3351
- Baston, C., Parosanu, A. I., Stanciu, I., & Nitipir, C. (2024). Metastatic Kidney Cancer: Does the Location of the Metastases Matter? Moving towards Personalized Therapy for Metastatic Renal Cell Carcinoma. Biomedicines, 12(5), 1111. https://doi.org/10.3390/biomedicines12051111
- Pandey, J., & Syed, W. (2023, August 8). Renal cancer. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK558975/
- Genetics of Renal Cell Carcinoma (PDQ®). (2024, February 8). Cancer.gov. https://www.cancer.gov/types/kidney/hp/renal-cell-carcinoma-genetics
- Szaro, P., Wong, A., Blain, E., Gataa, K. G., & Geijer, M. (2021). The diagnostic value of ultrasound-guided percutaneous core needle biopsy of musculoskeletal soft tissue lesions. Journal of Ultrasonography, 21(84), e22–e33. https://doi.org/10.15557/jou.2021.0004
- Kidney cancer surgery. (2024). American Cancer Society. https://www.cancer.org/cancer/types/kidney-cancer/treating/surgery.html
- Vento, J. A., & Rini, B. I. (2022). Treatment of refractory metastatic renal cell carcinoma. Cancers, 14(20), 5005. https://doi.org/10.3390/cancers14205005
- Dybiec, J., Frąk, W., Kućmierz, J., Tokarek, J., Wojtasińska, A., Młynarska, E., Rysz, J., & Franczyk, B. (2024). Liquid Biopsy: a new avenue for the diagnosis of kidney disease: diabetic kidney disease, renal cancer, and IGA nephropathy. Genes, 15(1), 78. https://doi.org/10.3390/genes15010078
Disclaimer:
Use of Course Content. The courses provided by NCC are based on industry knowledge and input from professional nurses, experts, practitioners, and other individuals and institutions. The information presented in this course is intended solely for the use of healthcare professionals taking this course, for credit, from NCC. The information is designed to assist healthcare professionals, including nurses, in addressing issues associated with healthcare. The information provided in this course is general in nature and is not designed to address any specific situation. This publication in no way absolves facilities of their responsibility for the appropriate orientation of healthcare professionals. Hospitals or other organizations using this publication as a part of their own orientation processes should review the contents of this publication to ensure accuracy and compliance before using this publication. Knowledge, procedures or insight gained from the Student in the course of taking classes provided by NCC may be used at the Student’s discretion during their course of work or otherwise in a professional capacity. The Student understands and agrees that NCC shall not be held liable for any acts, errors, advice or omissions provided by the Student based on knowledge or advice acquired by NCC. The Student is solely responsible for his/her own actions, even if information and/or education was acquired from a NCC course pertaining to that action or actions. By clicking “complete” you are agreeing to these terms of use.
Complete Survey
Give us your thoughts and feedback!
